Abstract
Introduction
Mental health disorders in pregnant women living with HIV are associated with poor maternal and child outcomes, and undermine the global goals of prevention of mother-to-child transmission of HIV (PMTCT). This study aimed to determine prevalence of depression and anxiety and identify factors associated with these common mental health disorders among HIV-infeced pregnant women in Tanzania.
Methods
We enrolled 200 pregnant women living with HIV from antenatal care clinics in the Kilimanjaro region. Women were eligible if they were in the second or third trimester of pregnancy and had been in PMTCT care for a minimum of one month. Data were collected via interviewer administered surveys. Participants self reported depression symptoms (Edinburgh Postnatal Depression Scale, EPDS) and anxiety symptoms (Brief Symptom Index, BSI). Multivariate logistic regression models examined factors associated with depression, anxiety, and comorbid depression and anxiety.
Results
25.0% of women met screening criteria for depression (EPDS ≥10). Depression was significantly associated with being single (aOR = 4.2, 95% CI = 1.1–15.5), food insecurity (aOR = 2.4, 95% CI = 1.0–6.4), and HIV shame (aOR = 1.2, 95% CI = 1.1–1.3). 23.5% of participants met screening criteria for anxiety (BSI ≥1.01). Anxiety was associated with being single (aOR = 3.6, 95%CI = 1.1–11.1), HIV shame (aOR = 1.1, 95% CI = 1.1–1.2) and lifetime experience of violence (aOR = 2.3, 95% CI = 1.0–5.1). 17.8% of the sample met screening criteria for both depression and anxiety. Comorbid depression and anxiety was associated with being single (aOR = 4.5, 95%CI = 1.0–19.1), HIV shame (aOR = 1.2, 95%CI = 1.1–1.3) and lifetime experience of violence (aOR = 3.4, 95% CI = 1.2–9.6).
Conclusion
Depression and anxiety symptomatology was common in this sample of pregnant women living with HIV, with a sizable number screening positive for comorbid depression and anxiety. In order to successfully engage women in PMTCT care and support their well-being, strategies to screen for mental health disorders and support women with mental illnesses are needed.
Background
The HIV epidemic remains a significant global health challenge. At the end of 2018, an estimated 36.9 million people were living with HIV worldwide, with the large majority being in sub-Saharan Africa [1]. In Tanzania, an estimated 1.5 million people are living with HIV, with substantially higher prevalence among women (6.2%) compared to men (3.8%) [2]. Although HIV affects people of all ages, women of childbearing age are at a greater risk of acquiring HIV compared with their counterpart. In 2011, the prevalence of HIV among women attending antenatal clinics in Tanzania was reported at 5.6% [3].
Not only are people living with HIV (PLHIV) more likely to have a number of physical co-morbidities [4], but they are also more likely to suffer from common mental health disorders (CMDs) such as depression [5] and anxiety [6]. A meta-analysis of ten studies found depression to be nearly twice as high in PLHIV compared to the general population [7]. The current evidence supports the association between HIV infection and mental illnesses as a vicious cycle, where each illness is a risk factor for the other [8].
Pregnancy and the postpartum period are vulnerable times for depressive [9] and anxiety disorders [10]. Studies from low and middle income countries (LMICs) have reported a higher prevalence of depression and anxiety among pregnant women [11]. Further, in a systematic review of studies among HIV-positive African women, the prevalence of antenatal depression ranged between 23% and 44%, more than double the estimated rates in the general population of pregnant women [12].
Antenatal depression and anxiety are associated with a number of poor HIV-related maternal outcomes and child. For example, pregnant women with mental illness are at greater risk for poor adherence to antiretroviral therapy [13], which can lead to vertical transmission of HIV to the fetus and breastfeeding child [14], with up to 11% vertical transmission in Tanzania. Pregnant women living with HIV with depression progress faster to the advanced stages of HIV compared to those without depression [15], and they are two times more likely to die from AIDS-related deaths, especially in LMICs [15,16]. Additionally, there is evidence that antenatal anxiety among women living with HIV may negatively impact child growth and development [17].
A number of factors contribute to perinatal mental health disorders among pregnant women living with HIV, ranging from individual to health system level factors. A systematic review of studies in Ethiopia reported individual and inter-personal factors that are associated with perinatal depression. In their review younger age, unmarried women, low monthly income, employed, history of the previous mental health disorder, irregular or no prevous antenatal follow-up, unplanned pregnancy, previous maternal and/or fetal complication (s) during pregnancy, conflict, and low social support were associated with antenatal depression [18].
Mental health disorders in HIV-positive pregnant women must be understood in the context of women’s life circumstances. Many women are newly diagnosed with HIV during pregnancy. Receiving a positive HIV test result is a shocking life event, creating worry about one’s future and the fear of transmitting the virus to one’s unborn child [19]. Additionally, stigma and discrimination following HIV status disclosure remains of concern in many communities. In one study in Tanzania, 32% of women reported being discriminated against due to HIV, and 12% reported abandonment or divorce following their HIV status disclosure [20].
In Tanzania, although one study has investigated the prevalence of depression among pregnant women living with HIV [21], no studies have included anxiety disorder. Therefore, the present study determined the prevalence of both depression and anxiety among HIV-positive pregnant women in northern Tanzania and examined factors associated with these common depression and anxiety.
Materials and methods
Study design and setting
This was a cross-sectional study among HIV-positive pregnant women in the Kilimanjaro Region. Participants were recruited at nine antenatal clinics, including six from the Moshi municipality and three from the Moshi district.
Participants
As per Tanzanian national PMTCT guidelines, all pregnant women who test positive for HIV initiate antiretroviral therapy (ART) for lifetime use [22]. Women were eligible to enroll in the study if they were in the second or third trimester of pregnancy and had enrolled in PMTCT care at one of the study antenatal clinics at least one month prior. Additionally, age 18 years and above and provided a written informed consent.
Procedure
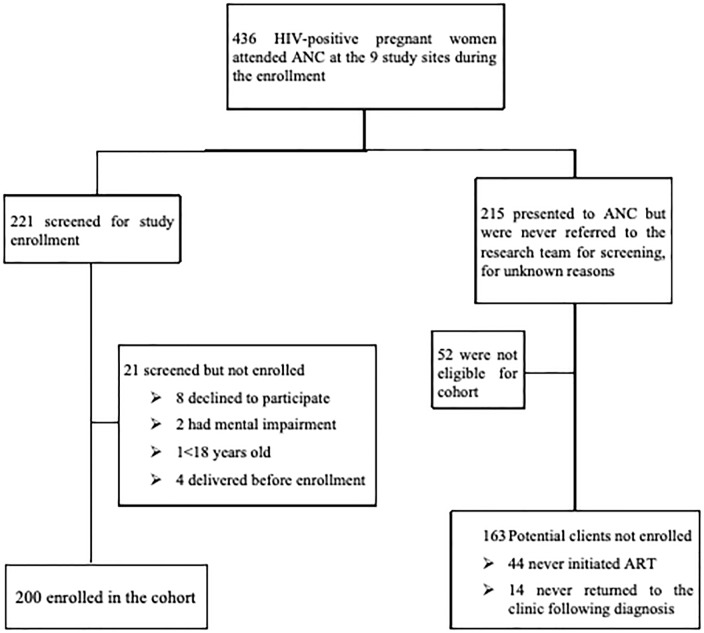
The structured survey was based on the baseline survey of a 12 month longitudinal survey of HIV-positve pregnant women in the Kilimanjaro Region [23]. Pregnant women living with HIV presenting for their routine antenatal care were consecutively approached by the clinic nurses informed of the study and asked if they were interested in obtaining more information. Between Juy 2016 and August 2017 436 pregant women living with HIV who attended ANC were approached, 221 experessed interest in the study and were referred to the research office for screening and enrollment (Fig 1).
Fig 1. Participant screening and enrollment flow diagram.
After obtaining informed consent, a structured survey was verbally administered in Swahili by a trained data collector. Study activities were conducted in private offices located within the study clinics. The assessment took approximately 60 minutes to complete. Participants were reimbursed for transportation costs (5,000 Tanzania shillings; approximately $2.30 U.S.) and were provided with light snacks during the interview. Participants with distress and thought of self-harm were counselled by the study nurse and also helped to create an individualized safety plan. Additionally, they were referred back to the clinic counsellor for further support.
Measures
The data collection tools were translated into Swahili and then back-translated into English by two independent translators. If there was a difference between the two after back translation, a team of Swahili and English-speaking study staff reached consensus on the final wording.
In addition to socio-demographic variables (age, level of education, employment status, prior pregnancy, and relationship status), the following measures were included in the survey.
Depression
Depression was measured using the Edinburgh Postnatal Depression Scale (EPDS) [24]. The EPDS contains ten questions asking about depressive symptoms over the past seven days. Each question has four possible responses, with a score of 0 to 3. Items were summed, with a possible range of 0 to 30 and higher scores indicating more depression symptoms (α = 0.88). A score of 10 was used as a cut-off to indicate possible depression [25].
Anxiety
Anxiety was measured using the six-item anxiety subscale of the Brief Symptom Index (BSI-18) [26]. Items asked about anxiety symptoms over the past seven days, with response options on a 5-point scale, ranging from 0 (not at all) to 4 (extremely). Items were averaged, with a possible range of 0 to 5 (α = 0.92). Based on instrument norms for a non-clinical, female population, a score of 1.01 or higher was used as a cut-off to indicate probable anxiety [27].
Attitudes about pregnancy
An 8-item measure was adapted from Speizer and colleagues to assess attitudes about pregnancy [28]. Items were summed, with a possible range from 0 to 24 and higher scores indicating more positive attitudes about the pregnancy (α = 0.91).
Intimate partner violence
The modified WHO intimate partner violence tool was used to assess for history of intimate partner violence, including questions about emotional, physical, and sexual abuse. The violence scores were dichotomised, with a yes to any of the aforementioned questions being indicative of a lifetime history of violence [29].
Enacted Stigma
A stigma measure was adapted from the Holzemer HIV/AIDS Stigma Instrument (HASI) [30]. The 11 items asked about stigmatizing experiences as a result of HIV (e.g., someone stopped being a friend). Items were summed, with a possible range from 0 to 33 and higher scores indicating greater experience with stigma (α = 0.88).
HIV Shame
The HIV and Abuse Related Shame Inventory (HARSI) was used to measure HIV shame [31]. The current study adapted 13 statements from the 14-item HIV-related shame subscale of the measure. The 13 items asked about internalized feelings related to living with HIV (e.g., I put myself down for becoming HIV positive, I am ashamed that I’m HIV positive). Items were summed, with a possible range from 0 to 52 and higher scores indicating greater shame (α = 0.86).
Food security
Four items from the Household Food Insecurity Access Scale (HFIAS) were used to assess household food availability over the past 30 days [32]. We adapted four questions from the nine-item household food insecurity scale (e.g. In the past month, how often could you not feed your family?). The measure was dichotomized into whether or not someone reported any food insecurity.
Social support
The Perceived Availability of Support Scale (PASS) was used to measure social support [33]. The participants were asked to respond to 8 questions (e.g., Would someone be available to talk to you if you were upset, nervous, or depressed?). Scores ranged from 8 to 40 with higher scores indicating greater perceived support from others (α = 0.82).
Of the tools used to measure outcomes and the explanotory variables, only food security and enacted stigma assessment tools have been validated in Tanzania [32]. Though not in Tanzania, some have been validated in other East African countries, for example, anxiety measure (BSI) has been validated in Kenya [34]
HIV-related variables
Women enrolled were asked if they had disclosed their HIV status to anyone or a sexual partner (Have you told anyone about your HIV status?). Also, their partner HIV status.
Ethical consideration
Ethical approval for the study was provided by the University of Cape Town Human Research Ethics Committee. The ethical review boards of the Tanzanian National Institute for Medical Research and Kilimanjaro Christian Medical University.
Eligible participants were asked to sign a form providing informed consent before their participation. Participants who could not read or write were asked to provide a thumbprint and their consent was verified by the signature of an impartial witness of the participant’s choice.
Data analysis
Stata Version 14.0 was used to analyse the data. Frequency distributions and descriptive statistics were calculated for categorical and continuous variables. Three multivariate logistic regression models were developed to assess the factors associated with depression, anxiety, and comorbid depression and anxiety. To control for confounders and reduce residual confounding effects, factors with a p-value of 0.15 or less in bivariate analysis were considered eligible for inclusion in the multivariate analysis, along with demographic variables (age, level of education and marital status) that were selected a priori. Factors with a p-value of less than 0.05 in the final model were considered statistically significant.
Results
A total of 208 pregnant women living with HIV were referred and deemed eligible for participation. Of those, 8 (3.8%) declined to participate, leaving a final sample of 200. The median age was 30 years (IQR 25–35). About half of participants knew they were HIV-positive prior to the current pregnancy (n = 106, 53.0%), and 88 (44.0%) had initiated ARV prior to the current pregnancy. When asked whether they had disclosed their status to anyone, 159 (79.5%) had disclosed to at least one person, and more than two-thirds (n = 119, 70.0%) reported that they had disclosed to a male partner (Table 1).
Table 1. Characteristics of study participants (n = 200).
| Characteristics | n | % |
|---|---|---|
| Median(IQR) age in years | 30 (25–35) | |
| Education level attained | ||
| No formal education | 4 | 2.0 |
| Any primary education | 113 | 56.5 |
| Any secondary education | 70 | 35.0 |
| Any college | 13 | 6.5 |
| Marital status | ||
| Married | 98 | 49.0 |
| In a relationship | 74 | 37.0 |
| Single | 19 | 9.5 |
| Separated/Divorced | 9 | 4.5 |
| Polygamous relationship | ||
| Yes | 36 | 18.0 |
| No | 164 | 82.0 |
| Income-earning activities | ||
| None | 60 | 30.0 |
| Informal activities | 111 | 55.5 |
| Formal employment | 29 | 14.5 |
| First pregnancy | ||
| Yes | 44 | 22.0 |
| No | 156 | 78.0 |
| Gestational age mean (±SD) | 28.4 (±5.6) | |
| Prior pregnancy outcome (n = 156) | ||
| No problems | 85 | 54.5 |
| Negative outcomes | 71 | 45.5 |
| Negative outcomes (n = 71) | ||
| Abortion | 7 | 9.9 |
| Miscarriage | 32 | 45.1 |
| Still birth | 12 | 16.9 |
| HIV+ child | 11 | 15.5 |
| Death of a child | 23 | 32.4 |
| HIV diagnosis | ||
| New diagnosis | 94 | 47.0 |
| Established diagnosis | 106 | 53.0 |
| Any HIV status disclosure | ||
| Yes | 159 | 79.5 |
| No | 41 | 20.5 |
| Disclosed to partner (n = 172) | ||
| No | 53 | 16.2 |
| Yes | 119 | 83.8 |
Fifty (25.0%) women met screening criteria for possible depression. Twenty-eight (14.1%) participants reported thoughts of self-harm, of whom 8 reported that they had these thoughts “quite often”. Forty-nine (24.6%) met screening criteria for probable anxiety disorder. The prevalence of comorbid anxiety and depression was 18.1% (n = 36). The majority (72%) of women who met screening criteria for depression also met screening criteria for anxiety.
In the first multivariate logistic regression model examining factors associated with depressive symptoms (Table 2), relationship status, food insecurity and HIV shame were significantly associated with depression. Women who were single had 4.2 times higher odds of possible depression compared with women who were married or in a relationship (aOR = 4.2, 95% CI = 1.1–15.5). Women who reported some food insecurity had 2.4 times higher odds of possible depression compared with those without food insecurity (aOR = 2.4, 95% CI = 1.0–6.4). Women with greater HIV shame had higher odds of depression; with each unit increase in HIV shame score, the odds of depression increased by 1.2 (aOR = 1.2, 95% CI = 1.1–1.3).
Table 2. Factors associated with depression among pregnant women living with HIV (n = 200).
| Variables | Possible depression | cOR (95%CI) | p-value | aOR (95%CI) | p-value | |
| No (n = 150) n(%) |
Yes (n = 50) n(%) |
|||||
| Education level attained | ||||||
| Primary | 83(70.9) | 34 (29.1) | 1.7(0.9–3.4) | 0.118 | 1.6(0.6–4.1) | 0.314 |
| Secondary and above | 67 (80.7) | 16 (19.3) | Ref | |||
| Marital status | ||||||
| Married | 135 (78.5) | 37 (21.5) | Ref | Ref | ||
| Single | 15 (53.6) | 13 (46.4) | 3.2(1.4–7.2) | 0.006 | 4.2 (1.1–14.6) | 0.030 |
| Income-earning activities | ||||||
| None | 43 (71.7) | 17 (23.8) | 1.2(0.6–2.5) | 0.477 | ||
| Informal/Formal | 107 (76.4) | 33 (23.6) | Ref | |||
| First pregnancy | ||||||
| Yes | 34 (77.3) | 10 (22.7) | ||||
| No | 116 (74.4) | 40 (25.6) | 1.2(0.5–2.6) | 0.694 | ||
| HIV diagnosis | ||||||
| New diagnosis | 71 (75.5) | 23 (24.5) | Ref | |||
| Established diagnosis | 79 (74.5) | 27 (25.5) | 1.0(0.5–2.0) | 0.870 | ||
| Disclosure to anyone | ||||||
| No | 34 (82.9) | 7 (17.1) | 0.5 (0.2–1.3) | 0.193 | ||
| Yes | 116 (73.0) | 43 (27.0) | ||||
| Yes | 91 (76.5) | 28 (23.5) | ||||
| Food Insecurity (FHI) | ||||||
| Never | 112 (84.2) | 21 (15.8) | ||||
| Sometimes | 38 (56.7) | 29 (43.3) | 4.1 (2.1–8.0) | <0.001 | 2.4 (1.0–6.4) | 0.056 |
| Ever experienced violence | ||||||
| No | 106 (81.5) | 24 (18.5) | ||||
| Yes | 44 (62.9) | 26 (37.1) | 2.6 (1.3–5.0) | 0.004 | 1.5 (0.6–3.6) | 0.409 |
| Variables | Median(IQR) | Median(IQR) | cOR (95%CI) | P value | aOR | P-value |
| Age in years | 30 (26–35) | 30 (24–35) | 1.0 (0.9–1.0) | 0.532 | 1.0 (0.9–1.1) | 0.892 |
| Social support | 30 (24–36) | 26.5 (23–30) | 0.9 (0.9–1.0) | 0.001 | 1.0 (0.9–1.0) | 0.303 |
| HIV Shame | 15 (10.7–20) | 29 (22.7–35) | 1.2 (1.1–1.3) | <0.001 | 1.2 (1.1–1.3) | <0.001 |
| Enacted stigma | 0 (0–0) | 0 (0–2) | 1.3 (1.0–1.5) | 0.014 | 1.0 (0.9–1.2) | 0.621 |
| Attitude about pregnancy | 16 (13–19.5) | 14 (9.7–16) | 0.9 (0.9–1.0) | 0.007 | 0.9 (0.8–1.0) | 0.134 |
cOR, crude odds ratio, aOR, adjusted odds ratio
Adjusted for social support, enacted stigma, attitude about pregnancy, HIV shame, level of education, marital status, food insecurity and violence
In the second multivariate logistic regression model examining factors associated with probable anxiety (Table 3), relationship status, HIV shame and lifetime experience of violence were significantly associated with anxiety. Women who were single had 3.6 times higher odds of probable anxiety compared with women who were married or in a relationship (aOR = 3.6, 95% CI = 1.1–11.1). Women with greater HIV shame had higher odds of probable anxiety; a one unit increase in HIV shame score was associated with 1.1 times increased odds of probable anxiety (aOR = 1.1, 95% CI = 1.1–1.2). Women who reported a history of lifetime violence had 2.3 times higher odds of probable anxiety compared to those who had never experienced violence (aOR = 2.3, 95% CI = 1.0–5.1).
Table 3. Bivariate and multivariate analysis of factors associated with probable anxiety among pregnant women living with HIV (n = 199).
| Variables | Probable anxiety | cOR (95%CI) | p-value | aOR(95%CI) | p-value | |
| No(n = 150) n(%) |
Yes(n = 49) n(%) |
|||||
| Education level attained | ||||||
| Primary/No formal | 84 (71.8) | 33 (28.2) | 1.6 (0.8–3.2) | 0.163 | 1.5(0.6–3.4) | 0.363 |
| Secondary and above | 66 (80.5) | 16 (19.5) | ||||
| Marital status | ||||||
| Married | 135 (78.9) | 36 (21.0) | ||||
| Single | 15 (53.6) | 13 (46.4) | 3.2 (1.4–7.4) | 0.005 | 3.6 (1.1–11.1) | 0.027 |
| Income-earning activities | ||||||
| None | 43 (71.7) | 17 (28.3) | 1.3 (0.7–2.6) | 0.426 | ||
| Informal/Formal | 107 (77.0) | 32 (23.0) | ||||
| First pregnancy | ||||||
| Yes | 30 (69.8) | 13 (30.2) | 1.4 (0.7–3.0) | 0.336 | ||
| No | 120 (76.9) | 36 (23.1) | ||||
| HIV diagnosis | ||||||
| New diagnosis | 71 (76.3) | 22 (23.7) | ||||
| Established diagnosis | 79 (74.5) | 27 (25.5) | 1.1 (0.6–2.1) | 0.767 | ||
| Partner recent test | ||||||
| HIV-negative/Unknown | 101 (73.2) | 37 (26.8) | 1.5 (0.7–3.1) | 0.283 | ||
| HIV-infected | 49 (80.3) | 12 (19.7) | ||||
| Disclosure to anyone | ||||||
| No | 32 (78.0) | 9 (22.0) | ||||
| Yes | 118(74.7) | 40 (25.3) | 1.2 (0.5–2.7) | 0.748 | ||
| Food Insecurity (FHI) | ||||||
| Never | 107 (81.1) | 25 (18.9) | ||||
| Sometimes | 43 (64.2) | 24 (35.8) | 2.4 (1.2–4.6) | 0.010 | 1.2 (0.5–2.8) | 0.676 |
| Ever experienced violence | ||||||
| No | 107 (82.9) | 22 (17.1) | ||||
| Yes | 43 (61.4) | 27 (38.6) | 3.0 (1.6–5.9) | 0.001 | 2.3 (1.0–5.1) | 0.045 |
| Variables | Median(IQR) | Median(IQR) | cOR(95%CI) | p-value | aOR(95%CI) | p-value |
| Age in years | 30.5 (26–35) | 28 (24–35) | 1.0 (0.9–1.0) | 0.153 | 1.0 (0.9–1.0) | 0.445 |
| Social support(PAS) | 29(24–34) | 27 (23–31.5) | 1.0 (0.9–1.0) | 0.104 | 1.0 (1.0–1.1) | 0.566 |
| HIV Shame | 15.5(11–21.2) | 28 (17–34.5) | 1.1 (1.1–1.2) | <0.001 | 1.1 (1.1–1.2) | <0.001 |
| Enacted stigma | 0 (0–0) | 0 (0–2) | 1.3 (1.1–1.6) | 0.011 | 1.1 (0.9–1.3) | 0.205 |
| Attitude about pregnancy | 16 (12.4–19) | 14(9.5–19) | 0.9 (0.9–1.0) | 0.081 | 0.9 (0.9–1.0) | 0.351 |
crude odds ratio, cOR; adjusted odds ratio, aOR
adjusted for level of education, marital status, perceived availability of social support, HIV shame, enacted stigma and attitude about current pregnancy
One participant did not complete anxiety screening instrument (BSI)
In the third multivariate logistic regression model examining factors associated with comorbid symptoms of depression and anxiety (Table 4), relationship status, HIV shame and lifetime experience of violence were significant predictors. Women who were single had 4.5 times higher odds of possible comorbid depression and anxiety compared with women who were married or in a relationship (aOR = 4.5, 95% CI = 1.0–19.1). Women with greater HIV shame had higher odds of experiencing comorbid depression and anxiety; for each unit increase in HIV shame score, the odds of comorbidity increased by 1.2 times (aOR = 1.2, 95% CI = 1.1–1.3). Women who had a lifetime history of violence had 3.5 times higher odds of comorbid depression and anxiety, compared to those with no history of violence (aOR = 3.5, 95% CI = 1.3–9.9).
Table 4. Bivariate and multivariate analysis of factors associated with comorbidity of depression and anxiety (n = 199).
| Variables | Probable Anxiety and possible Depression | cOR(95%CI) | p-value | aOR(95%CI) | p-value | |
| No (n = 163) n(%) |
Yes (n = 36) n(%) |
|||||
| Education level attained | ||||||
| Primary/No formal | 92 (78.6) | 25 (21.4) | 1.7 (0.8–3.8) | 0.155 | 1.6(0.5–4.8) | 0.379 |
| Secondary/Higher education | 73 (86.6) | 11 (13.4) | ||||
| Marital status | ||||||
| Married | 146 (85.4) | 25 (14.6) | ||||
| Single | 17 (60.7) | 11 (39.3) | 3.8 (1.6–9.0) | 0.003 | 4.5 (1.0–19.1) | 0.042 |
| Income-earning activities | ||||||
| None | 46 (76.7) | 14 (23.3) | 1.6 (0.8–3.4) | 0.209 | ||
| Informal/Formal | 117 (84.2) | 22 (15.8) | ||||
| First pregnancy | ||||||
| No | 129 (82.7) | 27 (17.3) | ||||
| Yes | 34 (79.1) | 9 (20.9) | 1.3 (0.5–2.9) | 0.585 | ||
| HIV diagnosis | ||||||
| New diagnosis | 78 (83.9) | 15 (16.1) | ||||
| Established diagnosis | 85 (80.2) | 21 (19.8) | 1.3 (0.6–2.7) | 0.501 | ||
| Partner recent test | ||||||
| HIV-negative/Unknown | 110 (79.7) | 28 (20.3) | 1.7 (0.7–3.9) | 0.229 | ||
| HIV-infected | 53 (86.9) | 8 (13.1) | ||||
| Disclosure to anyone | ||||||
| No | 36 (87.8) | 5 (12.2) | 0.6 (0.2–1.6) | 0.276 | ||
| Yes | 127 (80.4) | 31 (19.6) | ||||
| Food Insecurity (FHI) | ||||||
| Never | 117 (88.6) | 15 (11.4) | ||||
| Sometimes | 46 (68.7) | 21 (31.3) | 3.6 (1.7–7.5) | 0.001 | 1.5(0.5–4.5) | 0.420 |
| Ever experienced violence | ||||||
| No | 116 (89.9) | 13 (10.1) | ||||
| Yes | 47 (67.1) | 23 (32.9) | 4.4 (2.1–9.3) | <0.001 | 3.5(1.3–9.9) | 0.016 |
| Variables | Median(IQR) | Median(IQR) | cOR(95%CI) | p-value | aOR(95%CI) | p-value |
| Age | 30 (26–35) | 28 (23–35) | 0.9 (0.9–1.0) | 1.0 (0.9–1.1) | 0.575 | |
| Social support(PAS) | 30 (24–35) | 26 (22.2–29) | 0.9 (0.9–1.0) | 0.004 | 1.0 (0.9–1.1) | 0.515 |
| HIV Shame (HARSIH) | 16 (11–22) | 30 (23–36) | 1.1 (1.1–1.2) | <0.001 | 1.2 (1.1–1.3) | <0.001 |
| Enacted stigma(HASI) | 0 (0–0) | 0 (0–3) | 1.3 (1.1–1.6) | 0.006 | 1.1 (0.9–1.3) | 0.186 |
| Attitude about pregnancy(PREGAT) | 16 (12.6–19) | 14 (9–16.7) | 0.9 (0.8–1.0) | 0.010 | 0.9 (0.8–1.0) | 0.150 |
cOR, crude odds ratio; aOR, adjusted odds ratio, CI, confidence interval
adjusted for marital status, violence, food insecurity, attitude about current pregnancy, enacted stigma, perceived availability of social support, and HIV shame
Discussion
The main results of this study are that: 1) the prevalence of possible depression was 25% and was associated with relationship status, food insecurity, and HIV shame; 2) symptoms of anxiety were common (24.6%) and were associated with relationship status, HIV shame and lifetime experience of violence; and 3) a high rate of comorbidity was reported by participants, with 18.1% meeting criteria for both possible depression and probable anxiety. HIV shame, relationship status, and lifetime experience of violence were found to be significantly associated with comorbid depression and anxiety.
In the present study, one out of every four pregnant women living with HIV had possible depression. Although these findings are comparable to the US prevalence of 22% [35], compared to studies conducted in other African countries and other studies in Tanzania, this prevalence is low. For example, in Uganda and South Africa, depression rates of 42.7% and 41.0% have been reported, respectively [36,37]. Similarly, in Dar es Salaam, the prevalence of antenatal depression among women living with HIV was reported to be about twice (42.4%) or three times (74.3%) that of the prevalence in Moshi [38,39]. There are a number of explanations that may account for the different rates of depression reported in the present study compared to the available literature in other African countries. The use of different depression screening tools might have contributed to the observed difference in the prevalence. In the previous studies conducted in Tanzania and Uganda, the Hopkins Symptoms Checklist [40] was used to screen for depression [39], while this study used EPDS [36]. Also, the difference in the study design of the previous studies might have contributed to the observed difference. For instance, in the mentioned study in Tanzania, participants were enrolled from an ongoing trial [39], while the current study is cross-sectional.
Similar to prevalence rates of depression reported in the present study, 24.6% of women screened positive for anxiety. One study in the US reported a much higher prevalence (71.1%) compared to what we found [10]. However, that study had a sample size of 45. The sample size, study design, anxiety measures, and the difference in the cultural context of mental illness might have contributed to the observed difference. In Sub-saharan Africa, there is a paucity of data on the prevalence of anxiety among pregnant women living with HIV.
Interestingly, in the present study, 18.1% of women met screening criteria for comorbid depression and anxiety. Literature shows that the comorbidity of anxiety and depression is common among pregnant women, similar to the general population (10%) [41]. However, the data in pregnant women living with HIV is limited. Previous literature suggests that comorbidity is even more common compared to the presence of either depression or anxiety alone, with up to 52% of low income pregnant women in one study in urban South Africa diagnosed with depression also presenting symptoms of anxiety [42].
A number of factors were associated with these CMDs among pregnant living with HIV. To begin with, single women were at higher risk of depression, anxiety and comorbid compared to married women. The results are consistent with one previous study in the USA [10]. Being single and pregnant might not be a women’s choice, but rather may be a result of unintended pregnancies or being abandoned by a partner for reasons related to pregnancy, HIV or both. The circumstances resulting in a pregnant woman being single in the Tanzanian context might contribute to depression.
Second, this study found that women who reported food insecurity in their households had higher odds of CMDs. Associations between food insecurity and depression have been highlighted in Uganda, South Africa and the United States [43–45]. In addition to the stress of not having sufficient food for one’s household, there is an added stress of not being able to take the advice of HIV health care providers to eat a balanced diet and take HIV medication with food. The finding raises concerns about social disparities among PLHIV and shows that interventions should not only focus on physical health but should also address the socio-economic circumstance of clients.
Third, pregnant women who had greater HIV shame had higher odds of anxiety. One study from Bangkok Thailand reported similar findings [46]. Many PLHIV feel ashamed of their status and feel that they have let their families down [47]. Additionally, many believe that having HIV is a punishment for their behaviour [47,48], resulting in self blame and distress. One strategy that individuals use to cope with a shameful life event is to avoid the related events and situations that bring back shameful memories [47], in this case, avoidance is not an option adding to the risk of anxiety. Women who are in HIV care and take medications have a constant reminder of their HIV status, which may contribute to anxiety. Despite the fact that HIV is now a treatable chronic condition, it remains a stigmatized condition. In particular, since HIV transmission is commonly associated with sexuality, women in particularly may feel that they have diverged from the norm and feel ashamed as a result putting them at risk of anxiety [49].
Finally, women with a history of violence were at increased risk of anxiety and co-morbid anxiety and depression. Because women often learn their status first in a relationship through routine antenatal HIV testing [22], they may be blamed for introducing the disease into the relationship [50]. Because of this, some marriages end in separation or divorce, and others may be the victims of violence [20]. In order to achieve the ambitious targets set forth, more efforts are needed to overcome HIV-related shame, violence, and resulting symptoms of mental health disorders.
This study has demonstrated that mental health disorders are common in pregnant women living with HIV in the two districts of the Kilimanjaro region Tanzania. Although both depression and anxiety are common in this population, mental health services are nearly non-existent and there are no clear strategies or guidelines for medical staff on how to screen, diagnose and manage these conditions. Antenatal care facilities, including PMTCT clinics, are a vital entry point to detect and manage depression and anxiety among this vulnerable population. The findings of this study point to the need to train and deploy mental health care providers in order to provide mental health services at the PMTCT clinics. In order to successfully engage women in HIV care and support their well-being, and in turn eliminate mother to child transmission of HIV, strategies to screen for mental health and support women with mental health disorders are needed.
Limitations
The results of this study should be interpreted with some caution. The study enrolled only the subset of women attending the antenatal clinic who were referred to the study, and those who were not recruited may have differed in their presentation. Some of the assessment tools have not been validated in Tanzania, which might have impacted our findings, and cut off scores for depression and anxiety were based on non-Tanzanian norms. Finally, the cross sectional design of this study precludes any conclusions about causation.
Conclusion
In this population of women living with HIV, we found a substantial prevalence of possible depression, anxiety, and comorbid depression and anxiety. In order to meet the target of elimination of mother-to-child transmission of HIV, mental health needs to be addressed with a similar emphasis to that of physical health. Unmarried women, women with a history of experiencing violence, women with food insecurity, and those who felt ashamed (i.e., self-stigma) related to their HIV had higher odds of mental illness. These factors are deeply rooted in culture and personal beliefs, which emphasies the importance of tailored interventions that provide psycho-social support that reflect the local context.
Supporting information
(XLS)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This research was partly supported by the US National Institutes of Health (R21 AI 124344 to MHW) and AIDS International Training and Research Program - AITRP; Fogarty International Center (1D43 TW009595). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.UNAIDS data 2018 | UNAIDS [Internet]. [cited 2 Jun 2019]. https://www.unaids.org/en/resources/documents/2018/unaids-data-2018
- 2.Unaids. UNAIDS Data 2017. Programme on HIV/AIDS. 2017. 978-92-9173-945-5
- 3.Manyahi J, Jullu BS, Abuya MI, Juma J, Ndayongeje J, Kilama B, et al. Prevalence of HIV and syphilis infections among pregnant women attending antenatal clinics in Tanzania, 2011. BMC Public Health. 2015;15: 501 10.1186/s12889-015-1848-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Walensky RP, Paltiel a D, Losina E, Mercincavage LM, Schackman BR, Sax PE, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194: 11–9. 10.1086/505147 [DOI] [PubMed] [Google Scholar]
- 5.Hartzell JD, Janke IE, Weintrob AC. Impact of depression on HIV outcomes in the HAART era. J Antimicrob Chemother. 2008;62: 246–255. 10.1093/jac/dkn193 [DOI] [PubMed] [Google Scholar]
- 6.Fadzil A, Balakrishnan K, Razali R, Sidi H, Malapan T, Japaraj RP, et al. Risk factors for depression and anxiety among pregnant women in Hospital Tuanku Bainun, Ipoh, Malaysia. Asia-Pacific Psychiatry. 2013;5: 7–13. 10.1111/appy.12036 [DOI] [PubMed] [Google Scholar]
- 7.Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. Am J Psychiatry. 2001;158: 725–730. 10.1176/appi.ajp.158.5.725 [DOI] [PubMed] [Google Scholar]
- 8.Stringer EM, Meltzer-Brody S, Kasaro M, Stuebe AM, Wiegand S, Paul R, et al. Depression, pregnancy, and HIV: the case to strengthen mental health services for pregnant and post-partum women in sub-Saharan Africa. The lancet Psychiatry. 2014;1: 159–62. 10.1016/S2215-0366(14)70273-1 [DOI] [PubMed] [Google Scholar]
- 9.Bell AF, Andersson E. The birth experience and women’s postnatal depression: A systematic review. Midwifery. 2016;39: 112–123. 10.1016/j.midw.2016.04.014 [DOI] [PubMed] [Google Scholar]
- 10.Villar-Loubet OM, Illa L, Echenique M, Cook R, Messick B, Duthely LM, et al. Prenatal and Mental Health Care Among Trauma-Exposed, HIV-Infected, Pregnant Women in the United States. J Assoc Nurses AIDS Care. 2014;25 10.1016/j.jana.2013.06.006 [DOI] [PubMed] [Google Scholar]
- 11.Fisher J, de Mello MC, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: A systematic review. Bull World Health Organ. 2012;90: 139–149. 10.2471/BLT.11.091850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sowa NA, Cholera R, Pence BW, Gaynes BN. Perinatal depression in HIV-infected African women: a systematic review. J Clin Psychiatry. 2015;76: 1385–96. 10.4088/JCP.14r09186 [DOI] [PubMed] [Google Scholar]
- 13.Starace F, Ammassari A, Trotta MP, Murri R, De Longis P, Izzo C, et al. Depression is a risk factor for suboptimal adherence to highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;31 Suppl 3: S136–9. 31:S136-S139@2002 [DOI] [PubMed] [Google Scholar]
- 14.Townsend CL, Cortina-Borja M, Peckham CS, de Ruiter A, Lyall H, Tookey PA. Low rates of mother-to-child transmission of HIV following effective pregnancy interventions in the United Kingdom and Ireland, 2000–2006. AIDS. 2008;22: 973–81. 10.1097/QAD.0b013e3282f9b67a [DOI] [PubMed] [Google Scholar]
- 15.Antelman G, Kaaya S, Wei R, Mbwambo J, Msamanga GI, Fawzi WW, et al. Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. J Acquir Immune Defic Syndr. United States; 2007;44: 470–477. 10.1097/QAI.0b013e31802f1318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ickovics JR, Hamburger ME, Vlahov D, Schoenbaum EE, Schuman P, Boland RJ, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285: 1466–1474. 10.1001/jama.285.11.1466 [DOI] [PubMed] [Google Scholar]
- 17.Talge NM, Neal C, Glover V. Antenatal maternal stress and long-term effects on child neurodevelopment: How and why? J Child Psychol Psychiatry Allied Discip. 2007;48: 245–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Getinet W, Amare T, Boru B, Shumet S, Worku W, Azale T. Prevalence and Risk Factors for Antenatal Depression in Ethiopia: Systematic Review. Depress Res Treat. Hindawi Limited; 2018;2018: 3649269 10.1155/2018/3649269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shannon M, Lee KA. HIV-infected mothers’ perceptions of uncertainty, stress, depression and social support during HIV viral testing of their infants. Arch Womens Ment Health. 2008;11: 259–67. 10.1007/s00737-008-0023-8 [DOI] [PubMed] [Google Scholar]
- 20.Yonah G, Fredrick F, Leyna G. HIV serostatus disclosure among people living with HIV/AIDS in Mwanza, Tanzania. AIDS Res Ther. 2014;11: 5 10.1186/1742-6405-11-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaaya SF, Mbwambo JK, Kilonzo GP, Van Den Borne H, Leshabari MT, Fawzi MCS, et al. Socio-economic and partner relationship factors associated with antenatal depressive morbidity among pregnant women in Dar es Salaam, Tanzania. Tanzan J Health Res. 2010;12: 23–35. 10.4314/thrb.v12i1.56276 [DOI] [PubMed] [Google Scholar]
- 22.Tanzania Ministry of Health and Social Welfare. National Guidelines for Comprehensive Care Services for Prevention of Mother-to-Child Transmission of HIV and Keeping Mothers Alive. Cartographic Perspectives. 2013. [Google Scholar]
- 23.Watt MH, Cichowitz C, Kisigo G, Minja L, Knettel BA, Knippler ET, et al. Predictors of postpartum HIV care engagement for women enrolled in prevention of mother-to-child transmission (PMTCT) programs in Tanzania. AIDS Care. 2019;31: 687–698. 10.1080/09540121.2018.1550248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150: 782–6. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 25.Shrestha SD, Pradhan R, Tran TD, Gualano RC, Fisher JRW. Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting perinatal common mental disorders (PCMDs) among women in low-and lower-middle-income countries: A systematic review. BMC Pregnancy Childbirth. BMC Pregnancy and Childbirth; 2016;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13: 595–605. 10.1017/S0033291700048017 [DOI] [PubMed] [Google Scholar]
- 27.Kalichman SC. Psychological and social correlates of high-risk sexual behaviour among men and women living with HIV/AIDS. AIDS Care. 1999;11: 415–27. 10.1080/09540129947794 [DOI] [PubMed] [Google Scholar]
- 28.Speizer IS, Santelli JS, Afable-Munsuz A, Kendall C. Measuring Factors Underlying Intendedness of Women’s First and Later Pregnancies. Perspect Sex Reprod Health. 2004;36: 198–205. [DOI] [PubMed] [Google Scholar]
- 29.Garcia-Moreno C, Jansen H a FM, Ellsberg M, Heise L, Watts CH. WHO Multi-country Study on Women ‘ s Health and Domestic Initial results on prevalence. Genetics. 2005;151: 277–83. [Google Scholar]
- 30.Holzemer WL, Uys LR, Chirwa ML, Greeff M, Makoae LN, Kohi TW, et al. Validation of the HIV/AIDS Stigma Instrument—PLWA (HASI-P). AIDS Care. 2007;19: 1002–12. 10.1080/09540120701245999 [DOI] [PubMed] [Google Scholar]
- 31.Neufeld SAS, Sikkema KJ, Lee RS, Kochman A, Hansen NB. The development and psychometric properties of the HIV and Abuse Related Shame Inventory (HARSI). AIDS Behav. 2012;16: 1063–74. 10.1007/s10461-011-0086-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Knueppel D, Demment M, Kaiser L. Validation of the Household Food Insecurity Access Scale in rural Tanzania. Public Health Nutr. 2010;13: 360–7. 10.1017/S1368980009991121 [DOI] [PubMed] [Google Scholar]
- 33.Broadhead WE, Gehlbach SH, de Gruy FV, Berton HK. The Duke-UNC Functional Social Support Questionnaire: Measurement of Social Support in Family Medicine Patients. Med Care. 1988;26: 709–723. 10.1097/00005650-198807000-00006 [DOI] [PubMed] [Google Scholar]
- 34.Shacham E, Reece M, Monahan PO, Yebei V, Omollo O, Ong’or WO, et al. Measuring psychological distress symptoms in individuals living with HIV in western Kenya. J Ment Heal. 2008;17: 424–434. 10.1080/09638230701530192 [DOI] [Google Scholar]
- 35.Kapetanovic S, Christensen S, Karim R, Lin F, Mack WJ, Operskalski E, et al. Correlates of perinatal depression in HIV-infected women. AIDS Patient Care STDS. 2009;23: 101–108. 10.1089/apc.2008.0125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kaida A, Matthews LT, Ashaba S, Tsai AC, Kanters S, Robak M, et al. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr. 2014;67 Suppl 4: S179–87. 10.1097/QAI.0000000000000370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rochat TJ, Richter LM, Doll HA, Buthelezi NP, Tomkins A, Stein A. Depression Among Pregnant Rural South African Women Undergoing HIV Testing. JAMA. 2006;295: 1373 10.1001/jama.295.12.1373 [DOI] [PubMed] [Google Scholar]
- 38.Kaaya SF, Blander J, Antelman G, Cyprian F, Emmons KM, Matsumoto K, et al. Randomized controlled trial evaluating the effect of an interactive group counseling intervention for HIV-positive women on prenatal depression and disclosure of HIV status. AIDS Care. 2013;25: 854–62. 10.1080/09540121.2013.763891 [DOI] [PubMed] [Google Scholar]
- 39.Smith Fawzi MC, Kaaya SF, Mbwambo J, Msamanga GI, Antelman G, Wei R, et al. Multivitamin supplementation in HIV-positive pregnant women: impact on depression and quality of life in a resource-poor setting. HIV Med. 2007;8: 203–12. 10.1111/j.1468-1293.2007.00454.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist (HSCL). A measure of primary symptom dimensions. Mod Probl Pharmacopsychiatry. 1974;7: 79–110. 10.1002/bs.3830190102 [DOI] [PubMed] [Google Scholar]
- 41.Hirschfeld RMA. The Comorbidity of Major Depression and Anxiety Disorders: Recognition and Management in Primary Care. Prim Care Companion J Clin Psychiatry. 2001;3: 244–254. 10.4088/pcc.v03n0609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.van Heyningen T, Honikman S, Myer L, Onah MN, Field S, Tomlinson M. Prevalence and predictors of anxiety disorders amongst low-income pregnant women in urban South Africa: a cross-sectional study. Arch Womens Ment Health. Archives of Women’s Mental Health; 2017; 1–11. 10.1007/s00737-017-0768-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Blaney NT, Fernandez MI, Ethier K a, Wilson TE, Walter E, Koenig LJ. Psychosocial and behavioral correlates of depression among HIV-infected pregnant women. AIDS Patient Care STDS. 2004;18: 405–15. 10.1089/1087291041518201 [DOI] [PubMed] [Google Scholar]
- 44.Tsai AC, Bangsberg DR, Frongillo EA, Hunt PW, Muzoora C, Martin JN, et al. Food insecurity, depression and the modifying role of social support among people living with HIV/AIDS in rural Uganda. Soc Sci Med. 2012;74: 2012–9. 10.1016/j.socscimed.2012.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sorsdahl K, Slopen N, Siefert K, Seedat S, Stein DJ, Williams DR. Household food insufficiency and mental health in South Africa. J Epidemiol Community Health. 2011;65: 426–31. 10.1136/jech.2009.091462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bennetts A, Shaffer N, Manopaiboon C, Chaiyakul P, Siriwasin W, Mock P, et al. Determinants of depression and HIV-related worry among HIV-positive women who have recently given birth, Bangkok, Thailand. Soc Sci Med. 1999;49: 737–49. 10.1016/s0277-9536(99)00108-2 [DOI] [PubMed] [Google Scholar]
- 47.Bennett DS, Traub K, Mace L, Juarascio A, O’Hayer CV. Shame among people living with HIV: a literature review. AIDS Care. 2016;28: 87–91. 10.1080/09540121.2015.1066749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Olaore IB, Olaore AY. Is HIV/AIDS a consequence or divine judgment? Implications for faith-based social services. A Nigerian faith-based university’s study. SAHARA J J Soc Asp HIV/AIDS Res Alliance. Taylor & Francis; 2014;11: 20–5. 10.1080/17290376.2014.910134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arkell J, Osborn DPJ, Ivens D, King MB. Factors associated with anxiety in patients attending a sexually transmitted infection clinic: Qualitative survey. Int J STD AIDS. 2006;17: 299–303. 10.1258/095646206776790097 [DOI] [PubMed] [Google Scholar]
- 50.Colombini M, James C, Ndwiga C, Team I, Mayhew SH. The risks of partner violence following HIV status disclosure, and health service responses: Narratives of women attending reproductive health services in Kenya. J Int AIDS Soc. 2016;19: 1–7. 10.7448/IAS.19.1.20766 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLS)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.