Abstract
Lipofibromatous hamartoma (LFH) is a rare, benign tumor found in the peripheral nerves which is challenging to diagnose. We present a case report of the use of ultra-high-frequency ultrasound (UHFUS) on a patient with an LFH to provide valuable information not available on other imaging modalities regarding tumor invasion of the nerve fascicles.
Keywords: ultra-high-frequency ultrasound, lipofibromatous hamartoma
Introduction
Lipofibromatous hamartoma (LFH) is a rare, benign peripheral nerve tumor that most commonly affects the median nerve but can also occur in other peripheral nerves [1-3]. Affected individuals may experience swelling of the tissue, and the nerve may increase in length and diameter in the affected area and may be associated with macrodactyly [4]. Nerve compression occurs and can gradually lead to neural symptoms of pain, numbness, paresthesia, and carpal tunnel syndrome. Fibro-fatty strands form in the perineurium and endoneurium, intertwining in the nerves [5]. Therefore, physicians are discouraged to completely excise the tumor due to its invasion within the nerve. Permanent nerve damage is highly likely if the tumor is completely removed by surgery, so treatment for the relief of symptoms is the common practice. Moreover, the macroscopic appearance of the LFH as a yellow mass imposes a challenging differential diagnosis of other nerve tumors, such as neurofibromatosis.
Ultrasound is a non-invasive diagnostic modality that is well-established and used in medicine. It is simple to perform and allows a dynamic image [6-8]. Moreover, it is cost-efficient, being on average 75% less expensive than computed tomography (CT) and 80% less expensive than magnetic resonance imaging (MRI) [9]. However, conventional ultrasound transducers (5 - 20 megahertz (MHz)) are not good at evaluating small structures, such as branches of peripheral nerves [6, 8, 10]. Ultra-high-frequency ultrasound (UHFUS) transducers (frequencies up to 70 MHz) are one of the main improvements that the medical industry has recently made to advance the field of the ultrasonography [7-8, 11-13]. The higher frequency allows a high-resolution image of tiny structures up to 30 μm [6, 8]. UHFUS is a new technology that only a few hospitals have had access to, and few clinical applications have been described in the literature [14-15]. This case report illustrates the UHFUS technology to evaluate a patient with an LFH.
Technical report
A 27-year-old woman presented complaining about soft tissue swelling on the volar surface of her left wrist that had been present for over six years. She occasionally experienced paresthesia and numbness around the swollen area. The patient complained of progressive sensory disturbance with increasing pain which occurred along the distribution of the median nerve. Both Phalen’s test and Tinel’s sign were positive, indicating carpal tunnel syndrome. The patient underwent exploratory carpal tunnel release surgery with no improvement of her symptoms with biopsy and a histological diagnosis of lipofibromatous hamartoma. The patient then had a T1 MRI which showed common characteristic features correlating with an LFH (Figure 1).
Figure 1. T1 magnetic resonance imaging (MRI) of the left median nerve at the wrist.
White arrows median nerve
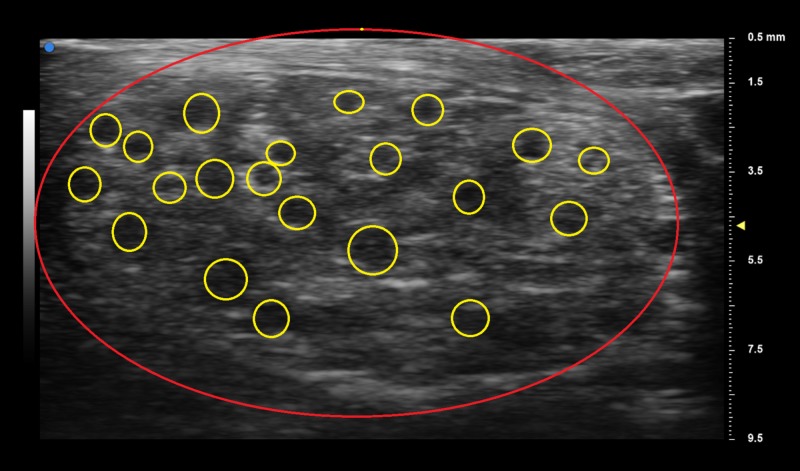
UHFUS exam was performed on the affected left distal median nerve at the wrist with the Vevo MD ultrasound device (FUJIFILM Visual Sonics, Amsterdam, the Netherlands) using a 70 MHz linear array transducer. Sonography results showed an enlarged cross-section of the median nerve with infiltration of hyperechoic fat separating the nerve fascicles (Figure 2).
Figure 2. Ultra-high-frequency ultrasound (UHFUS) showing the lipofibromatous hamartoma of the median nerve.
The red line indicates the circumference of the median nerve; yellow circles surround the nerve fascicles
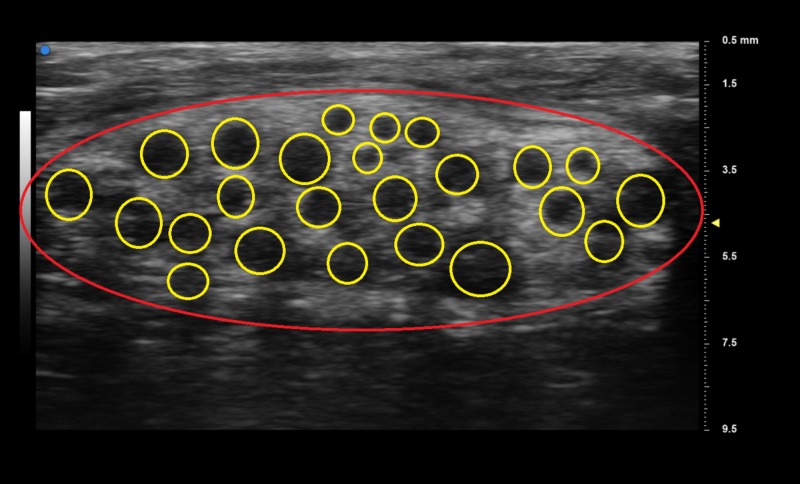
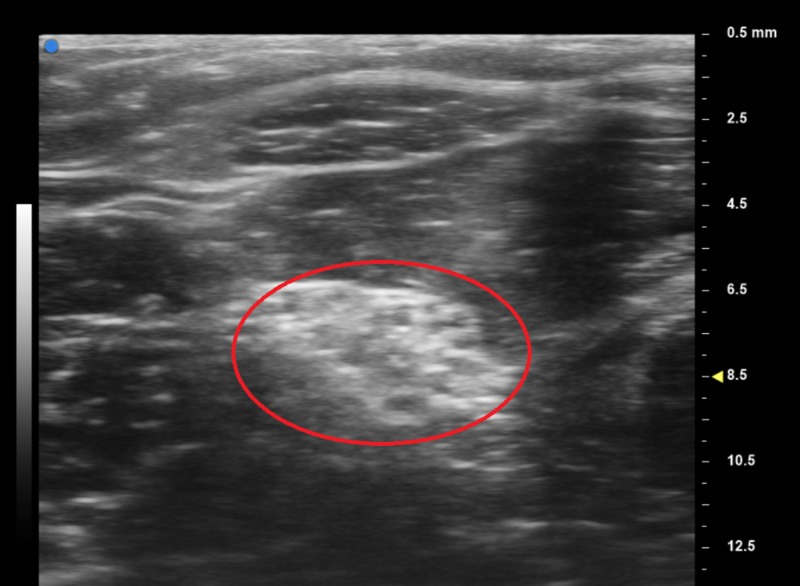
Proximally tracing the nerve from the wrist to the forearm demonstrates the beginning of the fibro-fatty infiltration of the median nerve (Figure 3). UHFUS of the patient's left forearm demonstrated a normal-appearing median nerve (Figure 4).
Figure 3. Beginning of the fibro-fatty infiltration of the median nerve in the left forearm.
The red circle indicates the circumference of the left median nerve; yellow circle surrounds the nerve fascicles.
Figure 4. Ultra-high-frequency ultrasound (UHFUS) normal median nerve left forearm.
The red circle surrounds the left median nerve
UHFUS of the patient's right wrist shows a normal median nerve (Figure 4).
Discussion
To our knowledge, this is the first report of UHFUS use in LFH. We demonstrated that UHFUS can be used to assist in identifying an LFH and the extension of the pathology. Moreover, the comparison between images generated by ultrasound on the normal and affected arms showed a potential application of using USFUS to evaluate the progression of the LFH.
Although ultrasound has been used in hand surgery for decades to evaluate carpal tunnel syndrome, the literature about the use of UHFUS to assess peripheral nerve conditions is still in its infancy. Stokvis et al. described the visualization of small cutaneous branches of hand nerves using UHFUS probes [8]. Viviano et al. went further in proposing UFHUS as a diagnostic tool in hand surgery after they conducted a study on one patient and five healthy volunteers. Interestingly, they pointed out that UHFUS can be easily performed by physicians without formal training in ultrasound and without harming the quality of the exam [16]. Schneeberger et al. used UFHUS to monitor graft rejection in a patient with hand allotransplantation [17]. Other applications of UHFUS were described for ophthalmology, cardiovascular, and dermatology [13, 18-20].
LHF is difficult to diagnose and a standard of diagnosis has yet to be established; therefore, physicians follow a diagnostic guideline based on their own knowledge and judgment. Symptoms of LFH vary from patient to patient. MRI or sonography is used to diagnose LFH without a necessary need for biopsy. Sonographic results show smooth, rounded, thickened fascicles surrounded by echogenic fatty tissue. MRI results show enlargement of the nerve containing thickened axonal bundles encased in epineural fibrous tissue. The nerve is described as cable-like in the MRI images with a description of an oval appearance [4]. Long cylindrical bands of low T1 and T2-weighted signals are commonly seen.
A differential diagnosis is needed for ganglion cyst, vascular malformation, traumatic neuroma, schwannoma, neurofibroma, and lipoma. LFH is an intraneural tumor, meaning the tumor is found within and around the nerve. It differs from other tumors that are of non-neural sheath origin. Fibro-fatty infiltration around the nerve fascicles pathologically distinguishes LFH, and it has no association with neurofibromatosis. LFH needs radiologic and microscopic investigation for accurate differentiation from neurofibromatosis. Accurate differentiation is essential because neurofibromatosis can progress to malignancy while LFH remains benign.
Although this study is limited to a case report, we were able to demonstrate the UFHUS capacity to assess nerve fascicles on a patient with LFH. Even though UHFUS provides a high-resolution image of tiny structures, high frequencies imply low pulse length, causing lower tissue penetration and difficulty in the assessment of deep anatomical structures [6, 8, 13]. Therefore, we encourage prospective clinical studies evaluating the use of UHFUS in LFH treatment.
Conclusions
We reported the use of UHFUS on a patient with an LFH, in which it provided us information not available through other imaging modalities regarding tumor invasion in the nerve fascicles. We believe this paper could benefit physicians to develop further diagnostic and treatment guidelines for LFH, as well as further research on the use of UHFUS.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
Animal Ethics
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
References
- 1.Lipofibromatous hamartoma of the median nerve. Al-Jabri T, Garg S, Mani GV. http://josr-online.biomedcentral.com/articles/10.1186/1749-799X-5-71. J Orthop Surg Res. 2010;5:71. doi: 10.1186/1749-799X-5-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lipofibromatous hamartoma of the radial nerve: an unusual location. Pomares G, Pedeutour B, Dap F, Dautel G. Hand Surg Rehabil. 2017;36:58–61. doi: 10.1016/j.hansur.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 3.Operative resection is a viable treatment of macrodactyly of the foot caused by lipofibromatous hamartoma: a case study with 5 year follow-up. Fransen BL, Broeders MG, van Oosterom FJ, Gilhuijs ND, Burger BJ. http://www.sciencedirect.com/science/article/abs/pii/S1268773114000666. Foot Ankle Surg. 2014;20:0–50. doi: 10.1016/j.fas.2014.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Lipofibromatous hamartoma: review of early diagnosis and treatment. Razzaghi A, Anastakis DJ. http://canjsurg.ca/wp-content/uploads/2014/03/48-5-394.pdf. Can J Surg. 2005;48:394–399. [PMC free article] [PubMed] [Google Scholar]
- 5.Lipofibromatous hamartoma of the median nerve in association with or without macrodactyly. Kini JR, Kini H, Rau A, Kamath J, Kini A. Turk Patoloji Derg. 2018;34:87–91. doi: 10.5146/tjpath.2014.01282. [DOI] [PubMed] [Google Scholar]
- 6.Ultra high-frequency ultrasound: new capabilities for nail anatomy exploration. Berritto D, Iacobellis F, Rossi C, Reginelli A, Cappabianca S, Grassi R. J Dermatol. 2017;44:43–46. doi: 10.1111/1346-8138.13495. [DOI] [PubMed] [Google Scholar]
- 7.The value of ultrasonography in hand surgery. Furrer M, Schweizer A, Rufibach K, Meuli-Simmen C. Hand (N Y) 2009;4:385–390. doi: 10.1007/s11552-009-9188-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.High-resolution ultrasonography of the cutaneous nerve branches in the hand and wrist. Stokvis A, Van Neck JW, Van Dijke CF, Van Wamel A, Coert JH. J Hand Surg Eur Vol. 2009;34:766–771. doi: 10.1177/1753193409102268. [DOI] [PubMed] [Google Scholar]
- 9.Costs, charges, and revenues for hospital diagnostic imaging procedures: differences by modality and hospital characteristics. Sistrom CL, McKay NL. J Am Coll Radiol. 2005;2:511–519. doi: 10.1016/j.jacr.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 10.US findings in traumatic wrist and hand injuries. Karabay N. Diagn Interv Radiol. 2013;19:320–325. doi: 10.5152/dir.2013.030. [DOI] [PubMed] [Google Scholar]
- 11.Normal sonographic anatomy of the wrist with emphasis on assessment of tendons, nerves, and ligaments. Gitto S, Draghi F. J Ultrasound Med. 2016;35:1081–1094. doi: 10.7863/ultra.15.06105. [DOI] [PubMed] [Google Scholar]
- 12.Advances in ultrasound. Harvey CJ, Pilcher JM, Eckersley RJ, Blomley MJ, Cosgrove DO. Clin Radiol. 2002;57:157–177. doi: 10.1053/crad.2001.0918. [DOI] [PubMed] [Google Scholar]
- 13.High frequency ultrasound: a new frontier for ultrasound. Shung K, Cannata J, Qifa Zhou M, Lee J. Conf Proc IEEE Eng Med Biol Soc. 2009;2009:1953–1955. doi: 10.1109/IEMBS.2009.5333463. [DOI] [PubMed] [Google Scholar]
- 14.Intraoperative evaluation of cervical nerve root avulsion using ultra-high-frequency ultrasound system. Boczar D, Forte AJ, Oliver JD, McClain RL, Murray P, Clendenen SR. Case Reports Plast Surg Hand Surg. 2019;6:43–46. doi: 10.1080/23320885.2019.1583569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ultra-high-frequency ultrasound to assess nerve fascicles in median nerve traumatic neuroma. Forte AJ, Boczar D, Oliver JD, Sisti A, Clendenen SR. Cureus. 2019;11:0. doi: 10.7759/cureus.4871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ultrahigh frequency ultrasound imaging of the hand: a new diagnostic tool for hand surgery. Viviano SL, Chandler LK, Keith JD. Hand (N Y) 2018;13:720–725. doi: 10.1177/1558944717731856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Upper-extremity transplantation using a cell-based protocol to minimize immunosuppression. Schneeberger S, Gorantla VS, Brandacher G, et al. Ann Surg. 2013;257:345–351. doi: 10.1097/SLA.0b013e31826d90bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feasibility of a novel blood noise reduction algorithm to enhance reproducibility of ultra-high-frequency intravascular ultrasound images. Hibi K, Takagi A, Zhang X, Teo TJ, Bonneau HN, Yock PG, Fitzgerald PJ. Circulation. 2000;102:1657–1663. doi: 10.1161/01.cir.102.14.1657. [DOI] [PubMed] [Google Scholar]
- 19.High-frequency sonography in the evaluation of nail psoriasis. Marina ME, Solomon C, Bolboaca SD, Bocsa C, Mihu CM, Tătaru AD. Med Ultrason. 2016;18:312–317. doi: 10.11152/mu.2013.2066.183.hgh. [DOI] [PubMed] [Google Scholar]
- 20.Lipofibromatous hamartoma of the digital branches of the median nerve presenting as carpal tunnel syndrome: a rare case report with review of the literature. Agrawal R, Garg C, Agarwal A, Kumar P. https://pdfs.semanticscholar.org/d4df/fc4fd223ead831a392228e8b7efa73ca8ea1.pdf. Indian J Pathol Microbiol. 2016;59:96–98. doi: 10.4103/0377-4929.178241. [DOI] [PubMed] [Google Scholar]