Abstract
Background:
Shorter gestational age at birth is associated with worse academic performance in childhood. Socioeconomic and demographic factors that affect a child’s development may modify the relationship between gestational age and later academic performance
Objective:
The purpose of this study was to investigate socioeconomic and demographic effect modification of gestational age’s association with kindergarten-level literacy skills in a longitudinal Wisconsin birth cohort.
Methods:
We sampled 153,145 singleton births (2007–2010) that linked to Phonological Awareness Literacy Screening – Kindergarten (PALS-K) scores (2012–2016 school years). PALS-K outcomes included meeting the screening benchmark (≥28 points, range 0–102 points) and the standardized score. Multivariable linear regressions of PALS-K outcomes on gestational age (completed weeks) included individual interactions for five maternal attributes measured at delivery: Medicaid coverage, education, age, race/ethnicity, and marital status.
Results:
Each additional completed gestational week was associated with a 0.5 percentage point increase in the probability of meeting the PALS-K literacy benchmark. The benefit of an additional week of gestational age was 0.5 percentage points (95% confidence interval 0.3, 0.7 percentage points) greater for Medicaid-covered births (0.8 percentage points) relative to non-Medicaid births (0.3 percentage points). Relative to only completing high school, having college education weakened this association by 0.3–0.6 percentage points, depending on years in college. Similar but modest relations emerged with standardized scores.
Conclusions:
Socioeconomic advantage as indicated by non-Medicaid coverage or higher levels of completed maternal education may diminish the cost of preterm birth on a child’s kindergarten-level literacy skills.
Keywords: Education, effect modification, health disparities, life course, preterm birth
BACKGROUND
The relationship between gestational age at birth and childhood school performance is well established. On average, children who are born preterm (<37 completed weeks) or very preterm (<32 completed weeks) have worse academic achievement in childhood and adolescence relative to their peers.1–4 Emerging evidence suggests a graded relationship even among those born near or at term, finding worse school performance among children who were born 34–36 weeks or 37–38 weeks gestation relative to children born after 39 weeks gestation.5–10 Childhood academic performance predicts health and socioeconomic stability in adulthood,11–13 so the influence of gestational age may cascade far beyond early schooling.
In this literature, conventional wisdom treats socioeconomic or demographic factors as confounders of gestational age’s association with academic performance.14–17 A competing theory suggests that socioeconomic and demographic factors may also modify this relationship. Protective factors afforded through socioeconomic advantage such as high-quality parenting, wealth, engagement in early intervention programs and other investments in childhood development can compensate for the deleterious effects of preterm birth.18,19 Additionally, there are demographic health disparities in the United States, and intergenerational social disadvantage may amplify the determinant of poor health on childhood development.20–22 At an individual level, the disproportionate psychosocial stress perpetuated by racism, young motherhood, or single motherhood may not only limit the parent’s ability to support the child’s development23–26 but also exacerbate the long-term impact of preterm birth on children.
Recent evidence suggests that less maternal education or living in a poorer neighborhood may increase the relationship between gestational age and academic performance.5,27 However, other contemporary studies find no evidence of modification by socioeconomic or demographic factors,28–33 perhaps due to differences in the methods across studies. Some studies tested modification with composite measures27,32,33 – for example, a socioeconomic index based on parents’ education, occupation, and income32 – which may conceal the precise mechanisms of modification. Several that found no evidence of modification categorized gestational age and had samples with fewer than 15,000 children,29–33 three of which drew samples from the same cohort.29–31 Categorized predictor variables and small samples may limit statistical power for testing modification. Lastly, only two prior studies investigated modification by demographic factors,28,30 as most studies focused on children’s socioeconomic background.
This purpose of this study was to determine if socioeconomic or demographic factors modify the association between a child’s gestational age and literacy skills at kindergarten entry using a large, population-based cohort of children who completed a standardized kindergarten-level literacy screener in Wisconsin public schools during 2012–2016. We examined this relationship across strata of five maternal characteristics that were measured at delivery: Medicaid obstetrical delivery coverage, completed education, age, race and ethnicity, and marital status.
METHODS
Sample
We drew our sample from Big Data for Little Kids (BD4LK), an integrated data source including all Wisconsin in-state resident live births in 2007–2012.34 The cohort links birth records to four administrative sources: Medicaid claims and encounters (henceforth “claims”), a longitudinal social services data system for Wisconsin,35 Phonologic Awareness Literacy Screening-Kindergarten (PALS-K) testing data from Wisconsin public schools (2012–2016 school years), and public county-level characteristics.36 BD4LK includes two versions of the birth record: the 1989 Revision of the U.S. Standard Certificate of Live Birth (2007–2010 deliveries) and the 2003 Revision of the U.S. Standard Certificate of Live Birth (2011–2012 deliveries). BD4LK has 405,864 unique birth records with few (<1%) imperfect linkages across data sources, so potential bias from data linkage is minimal.
BD4LK has 274,422 unique birth records for 2007–2010 deliveries. PALS-K scores were not available for children born during 2011–2012, so we did not sample their records. From 2007–2010 records, we used variables from the birth record, PALS-K tests, and Medicaid claims. We excluded 1,053 records (0.4%) that did not link uniquely across data sources within the subsample, 1,676 birth records (0.6%) that indicated infant death, and 21,569 birth records (7.9%) of children who were younger than five years-of-age by September 1, 2015, as they were too young to enroll in kindergarten during the 2012–2016 school years.37 Our eligibility pool comprised 250,124 children, of which 176,938 (70.3%) linked to a PALS-K test. Match rates to PALS-K were consistent across birth-year cohorts, albeit somewhat lower for eligible birth records from 2010 (eTable 1).
We sequentially excluded 23,033 children (13.0%) on seven criteria: Spanish-language PALS-K test (n=2,222); <5 years-old at testing (n=66); birth weight <350 grams or >7,000 grams (n=15); gestational age <24 weeks or >42 weeks (n=150); plural birth (n=5,481); foreign-born mother (n=14,306); mother with no high school education at delivery (n=854). We excluded children who took the Spanish-language PALS-K test because it is unknown whether the Spanish-language and English-language versions are comparable. We excluded children on age due to technical ineligibility for PALS-K evaluation,37 on birth weight and gestational age for implausible reported values from birth records,38 and on plurality to reduce correlations between children. We excluded children with foreign-born mothers because we were uncertain how consistently children were directed to the Spanish-language PALS-K test and because the test is not offered in other languages. Finally, we excluded children whose mothers had no high school education due to limited generalizability. Among children whose mothers had no high school education and who met inclusion criteria, only 854 of 4,154 (20.6%) took the PALS-K test (match rates in other educational subgroups were generally >70%). Within the no high school education subgroup, there was differential selection into PALS-K by maternal race/ethnicity and residence county. This systematic selection into testing and substantial data missingness compromised our ability to generalize findings of this subgroup.
Our analytic sample was 153,145 children to 134,925 mothers, and 36,066 children (23.5% of the sample) were in-sample siblings to 17,786 mothers. We tracked sample inclusion by birth-year cohort, compared tested and untested children who met inclusion criteria, compared analyzed children to all live in-state resident deliveries in Wisconsin during 2007–2010, and provided a sampling flow chart (eTables 1–3, eFigure 1).
Variables
Birth records supplied all variables aside from Medicaid delivery coverage and PALS-K score. The exposure was the clinical estimate of gestational age (completed weeks), which was estimated with data from the date of last menstrual period and the first accurate ultrasound.39 Maternal attributes at delivery included age in years (<20; 20–24; 25–34; 35–39; 40+), race/ethnicity (Asian non-Hispanic [NH], black NH; Hispanic; Native American NH; white NH; other NH), education (1–3 years high school; high school diploma/equivalent; 1–3 years college; 4 years college; 5+ years college), marital status (unmarried; married), Medicaid delivery coverage (no; yes), and parity (first birth; second birth; third birth; fourth or later birth). Medicaid is a federal- and state-funded health insurance program for low-income residents. Eligibility depends on household income and varies by state.40 We also included child’s biological sex (female; male).
PALS-K
PALS-K evaluates readiness for kindergarten-level literacy instruction.41,42 The test includes six domains (rhyme awareness; beginning sound awareness; alphabet knowledge; letter sounds; spelling; word concept) with a range of 0–102 points. Wisconsin public schools administered PALS-K to all eligible kindergarten students in fall semesters during the 2012–2016 school years to identify children who were at risk of grade-level reading difficulties and may require literacy intervention.43-45
Our outcomes were the standardized PALS-K score (mean 0, standard deviation [SD] 1) and meeting the PALS-K literacy benchmark (28+ points). Scoring below the benchmark signals elevated risk of reading difficulty and is used by schools as an indicator for further evaluation.41,42,45
Statistical analysis
We measured the distribution of all variables and of birth year. For each stratum of categorical variables, we calculated the mean PALS-K score (raw and standardized) and the percent of children who met the PALS-K benchmark. We assessed linearity with locally weighted regression plots of raw PALS-K scores against gestational age both overall and stratified by maternal characteristics (eFigures 2–7).
Figure 1 depicts the hypothesized relations among variables that guided the analysis. We constructed multivariable linear regression models that regressed PALS-K outcomes on gestational age (completed weeks). For the standardized PALS-K score outcome, the gestational age coefficient was the expected change in the standardized PALS-K score for each gestational week. For the PALS-K benchmark outcome, the gestational age coefficient was the percentage point change in the probability of meeting the benchmark for each gestational week.46 Both models adjusted for all previously listed covariates except gestational age category and birth year. We clustered standard errors at the mother-level to relax the assumption of independence between observed siblings.47 Aside from outcomes, both models were functionally identical.
Figure 1.
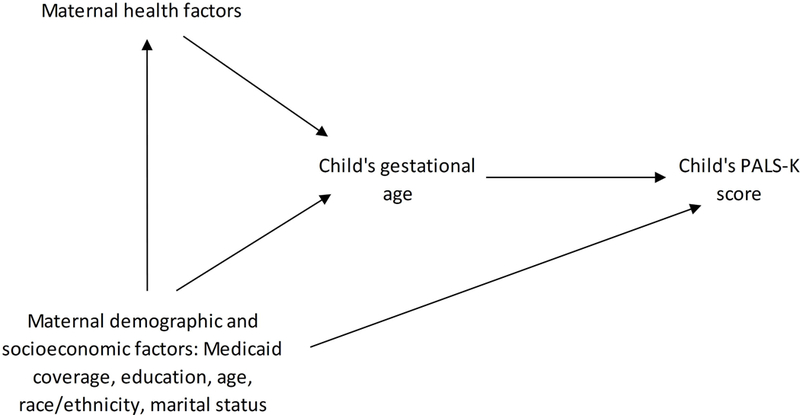
Directed Acyclic Graph of the Relationship Between Gestational Age and Phonological Awareness Literacy Screening – Kindergarten (PALS-K) Test Performance
We tested modification by five maternal attributes: Medicaid obstetrical delivery coverage, education, age, race/ethnicity, and marital status. We considered these five attributes because they represent both socioeconomic (Medicaid coverage; education) and demographic (age; race/ethnicity; marital status) backgrounds. For each attribute, we estimated two regression models (one per outcome) with a gestational age-attribute interaction. We then generated plots of attribute-stratified predictions of the outcomes for each week of gestational age between 24–42 weeks. Additionally, we estimated stratum-specific coefficients for all categories of interaction variable to observe the variation in the gestational age-PALS-K associations. Subgroups with the largest sample size were our references for testing interactions.
Missing data
As discussed previously, only 760 otherwise eligible children were excluded for missing data on relevant variables, and their exclusion decreased the sample size by <0.5%. Given the minimal data missingness, we did not use multiple imputation.
Sensitivity analyses
We conducted two sensitivity analyses. First, we repeated the effect modification analyses after excluding very preterm deliveries (1,134 records; 0.7% of the sample) and after excluding children who were small for gestational age (SGA) (14,274 records; 9.3% of the sample) to investigate outlier influence. We defined SGA as a birth weight in the bottom decile of that gestational age using a United States’ (US) national reference.48 Second, we repeated the modification analyses and controlled for birth record-reported maternal tobacco smoking to investigate modification via differential confounding. Maternal smoking may confound the gestational age-academic performance relationship and is disproportionately prevalent among less educated US mothers.49–52
We calculated 95% confidence intervals for estimates and performed all analyses in Stata statistical software, release 15.53 The University of Wisconsin-Madison minimal risk institutional review board approved our project.
RESULTS
The average PALS-K score was 64.9 points (SD 23.1 points), and 91.6% of children met the PALS-K benchmark (Table 1). The average gestational age was 38.9 weeks (SD 1.7 weeks), and 6.3% of children were born preterm. The average PALS-K score for term-birth children was roughly 10 points greater than that of very preterm children, and 87% of all preterm children met the PALS-K benchmark compared to 92% of term-birth children. We observed a positive dose-response relationship between gestational age and meeting the literacy benchmark, and gestational age was linearly related to PALS-K scores overall and within maternal socioeconomic and demographic strata except for the other NH race subgroup (eFigures 2–7).
Table 1.
Baseline Characteristics of 2007–2010 Wisconsin Birth Records that Linked to PALS-K Tests (n = 153,145)
| Characteristic | Mean (SD) or % | Mean PALS-K Score (SD), Range 0–102 |
Mean Standardized PALS-K Scorea (SD) |
Met PALS-K Literacy Benchmarkb, % |
|---|---|---|---|---|
| Overall | 64.89 (23.14) | 0.00 (1.00) | 91.6 | |
| Birth Year Cohort | ||||
| 2007 | 28.5 | 64.25 (23.04) | −0.03 (1.00) | 91.4 |
| 2008 | 28.0 | 65.18 (23.05) | 0.01 (1.00) | 91.8 |
| 2009 | 27.2 | 65.78 (23.16) | 0.04 (1.00) | 92.0 |
| 2010 | 16.3 | 64.03 (23.39) | −0.04 (1.01) | 90.7 |
| Gestational age (weeks) | 38.93 (1.73)c | |||
| <32 (very preterm) | 0.7 | 56.42 (25.90) | −0.37 (1.12) | 82.0 |
| 32–35 (preterm) | 2.8 | 59.62 (24.48) | −0.23 (1.06) | 87.3 |
| 36 (late preterm) | 2.8 | 61.84 (23.82) | −0.13 (1.03) | 89.4 |
| 37–38 (early term) | 22.3 | 63.52 (23.46) | −0.06 (1.01) | 90.6 |
| 39–41 (term) | 70.3 | 65.72 (22.85) | 0.04 (0.99) | 92.2 |
| 42 (post-term) | 1.0 | 66.79 (22.91) | 0.08 (0.99) | 92.8 |
| Maternal age (years) | 27.38 (5.67)c | |||
| <20 | 8.8 | 55.47 (24.21) | −0.401 (1.05) | 83.9 |
| 20–24 | 23.8 | 59.71 (23.73) | −0.22 (1.03) | 88.0 |
| 25–34 | 56.1 | 67.73 (22.16) | 0.12 (0.96) | 93.7 |
| 35–39 | 9.6 | 69.15 (21.79) | 0.18 (0.94) | 94.7 |
| 40+ | 1.8 | 68.26 (22.18) | 0.15 (0.96) | 93.8 |
| Maternal education | ||||
| 1–3 years HS | 10.1 | 51.25 (24.59) | −0.59 (1.06) | 79.0 |
| HS graduate/equivalent | 30.8 | 58.89 (23.58) | −0.26 (1.02) | 87.5 |
| 1–3 years college | 28.7 | 65.48 (21.80) | 0.03 (0.94) | 93.5 |
| 4 years college | 21.1 | 74.25 (18.90) | 0.40 (0.82) | 97.9 |
| 5+ years college | 9.3 | 76.56 (18.04) | 0.50 (0.78) | 98.4 |
| Maternal race/ethnicity | ||||
| Asian NH | 1.2 | 62.06 (24.64) | −0.12 (1.06) | 88.7 |
| Black NH | 9.3 | 57.23 (25.34) | −0.33 (1.10) | 84.0 |
| Hispanic | 4.1 | 55.37 (25.27) | −0.41 (1.09) | 82.1 |
| Native American NH | 1.8 | 52.88 (24.64) | −0.52 (1.06) | 80.1 |
| Other NH | 0.0 | 62.60 (25.97) | −0.10 (1.12) | 86.8 |
| White NH | 83.6 | 66.51 (22.34) | 0.07 (0.97) | 93.2 |
| Maternal marital status | ||||
| Unmarried | 39.1 | 58.06 (24.02) | −0.29 (1.04) | 86.4 |
| Married | 60.9 | 69.27 (21.44) | 0.19 (0.93) | 94.9 |
| Medicaid coverage | ||||
| Yes | 39.0 | 57.29 (24.10) | −0.33 (1.04) | 85.7 |
| No | 61.0 | 69.74 (21.13) | 0.21 (0.91) | 95.3 |
| Parity | ||||
| First birth | 41.2 | 66.94 (22.67) | 0.09 (0.98) | 92.9 |
| Second birth | 33.7 | 65.85 (22.54) | 0.04 (0.97) | 92.7 |
| Third birth | 16.0 | 61.98 (23.50) | −0.13 (1.02) | 89.8 |
| Fourth or later birth | 9.1 | 57.17 (24.70) | −0.33 (1.07) | 84.7 |
| Child’s sex | ||||
| Female | 49.2 | 67.39 (22.08) | 0.11 (0.95) | 93.4 |
| Male | 50.8 | 62.47 (23.88) | −0.10 (1.03) | 89.8 |
Abbreviations: HS, high school; NH, non-Hispanic, PALS-K, Phonological Awareness Literacy Screening-Kindergarten; SD, standard deviation.
We standardized the PALS-K score to mean 0 and standard deviation 1.
The PALS-K benchmark is a score of 28 points or greater on the test (range: 0–102 points). Failure to meet the benchmark signals that a child may need early literacy intervention.
Mean value (standard deviation).
We also observed expected patterns of association between other variables and PALS-K performance. Overall, 85.7% of Medicaid-covered children met the literacy benchmark compared to 95.3% of non-Medicaid children, and non-Medicaid children earned, on average, 11.2 more points on the PALS-K score relative to their Medicaid-covered peers (69.3 points vs. 58.1 points). Similarly, roughly 80% of children of mothers without a complete high school education met the PALS-K benchmark and earned an average PALS-K score of 51.3 points, whereas approximately 98% of children whose mothers completed 4+ years of college met the benchmark and earned an average score of 75 points. Maternal characteristics negatively associated with children’s PALS-K performance included younger age and being unmarried.
Each completed gestational week was associated with a 0.03 SD increase in the PALS-K score and a half-percentage point increase in the probability of meeting the school literacy benchmark (Table 2). Observed socioeconomic factors modified this association. Each completed week of gestation was associated with a 0.01 SD greater increase in the PALS-K score (95% confidence interval [CI] 0.00, 0.01 SD) and a half-percentage point greater increase in the probability of meeting the literacy benchmark (95% CI 0.3, 0.7 percentage points) for Medicaid-covered births relative to non-Medicaid covered births. Higher levels of maternal education also attenuated the relation between gestational age and PALS-K outcomes. The association between gestational age and the standardized PALS-K score was 0.01 SD smaller for children of mothers with 5+ years of college education relative to children of mothers who ended their education after high school (95% CI −0.02, −0.00 SD). College education also attenuated the association between gestational age and the probability of meeting the literacy benchmark by 0.3–0.6 percentage points, depending on the level of college education. Additionally, maternal age <20 years was associated with a 0.01 SD decrease in the standardized score for each gestational week (95% CI −0.02, −0.00 SD) relative to maternal age 25–34 years. There was no evidence of modification by maternal race/ethnicity or marital status. Estimated stratified coefficients for interaction variables illustrate the heterogeneity of the gestational age-PALS-K association across strata of Medicaid coverage and maternal education (Table 3). Likewise, they highlight that the association was relatively consistent across strata of maternal age, race/ethnicity, and marital status.
Table 2.
Ordinary Least Squares Regressionsa of PALS-K Outcomes on Gestational Age in Completed Weeks (n = 153,145)
| Outcome: Standardized PALS-K Scoreb | Outcome: Probability of Meeting Literacy Benchmarkc, Percentage Points |
|
|---|---|---|
| β Coefficient (95% CI) | β Coefficient (95% CI) | |
| MODEL 1: NO INTERACTIONS | ||
| Gestational Age (week) | 0.03 (0.02, 0.03) | 0.54 (0.43, 0.61) |
| Medicaid Delivery Coverage | ||
| Non-Medicaid | 0.00 (Reference) | 0.00 (Reference) |
| Medicaid | −0.16 (−0.17, −0.15) | −3.16 (−3.56, −2.75) |
| Maternal Education | ||
| 1–3 years HS | −0.23 (−0.25, −0.21) | −6.29 (−7.05, −5.54) |
| HS Grad/equivalent | 0.00 (Reference) | 0.00 (Reference) |
| 1–3 years college | 0.19 (0.17, 0.20) | 4.10 (3.70, 4.49) |
| 4 years college | 0.44 (0.43, 0.46) | 6.22 (5.82, 6.61) |
| 5+ years college | 0.52 (0.51, 0.54) | 6.46 (6.03, 6.88) |
| Maternal Age | ||
| <20 years | −0.14 (−0.16, −0.11) | −1.59 (−2.37, −0.81) |
| 20–24 years | −0.08 (−0.10, −0.07) | −1.12 (−1.56, −0.69) |
| 25–34 years | 0.00 (Reference) | 0.00 (Reference) |
| 35–39 years | 0.04 (0.02, 0.05) | 0.73 (0.33, 1.13) |
| 40+ years | 0.05 (0.01, 0.08) | 0.74 (−0.16, 01.63) |
| Maternal Race/Ethnicity | ||
| Asian NH | 0.02 (−0.03, 0.07) | −1.02 (−2.50, 0.46) |
| Black NH | 0.02 (0.00, 0.04) | −1.93 (−2.60, −1.26) |
| Hispanic | −0.13 (−0.16, −0.10) | −5.01 (−5.98, −4.04) |
| Native Am. NH | −0.25 (−0.29, −0.21) | −7.41 (−8.92, −5.90) |
| Other NH | 0.08 (−0.19, 0.34) | −2.69 (−11.56, 6.18) |
| White NH | 0.00 (Reference) | 0.00 (Reference) |
| Maternal Marital Status | ||
| Married | 0.00 (Reference) | 0.00 (Reference) |
| Unmarried | −0.10 (−0.12, −0.09) | −1.41 (−1.83, −0.98) |
| Parity | ||
| First birth | 0.00 (Reference) | 0.00 (Reference) |
| Second birth | −0.12 (−0.13, −0.11) | −1.35 (−1.64, −1.05) |
| Third birth | −0.24 (−0.26, −0.23) | −3.31 (−3.74, −2.88) |
| Fourth or later birth | −0.35 (−0.37, −0.33) | −6.39 (−7.04, −5.73) |
| Child’s Sex | ||
| Female | 0.00 (Reference) | 0.00 (Reference) |
| Male | −0.21 (−0.22, −0.20) | −3.64 (−3.91, −3.37) |
| MODEL 2: MEDICAID DELIVERY COVERAGE INTERACTION | ||
| Gestational Age (week) | 0.02 (0.02, 0.03) | 0.32 (0.23, 0.42) |
| Gestational Age*Medicaid Delivery Coverage | ||
| Non-Medicaid | 0.00 (Reference) | 0.00 (Reference) |
| Medicaid | 0.01 (0.00, 0.01) | 0.47 (0.27, 0.66) |
| MODEL 3: MATERNAL EDUCATION INTERACTION | ||
| Gestational Age (week) | 0.03 (0.02, 0.03) | 0.72 (0.54, 0.90) |
| Gestational Age*Maternal Education | ||
| 1–3 years HS | −0.00 (−0.01, 0.01) | −0.11 (−0.50, 0.28) |
| HS grad/equivalent | 0.00 (Reference) | 0.00 (Reference) |
| 1–3 years college | 0.01 (−0.00, 0.01) | −0.24 (−0.47, −0.01) |
| 4 years college | 0.00 (−0.01, 0.01) | −0.38 (−0.60, −0.15) |
| 5+ years college | −0.01 (−0.02, −0.00) | −0.63 (−0.87, −0.39) |
| MODEL 4: MATERNAL AGE INTERACTION | ||
| Gestational Age (week) | 0.03 (0.02, 0.03) | 0.43 (0.32, 0.54) |
| Gestational Age*Maternal Age | ||
| <20 years | −0.01 (−0.02, −0.00) | 0.01 (−0.35, 0.37) |
| 20–24 years | 0.01 (0.00, 0.01) | 0.33 (0.01. 0.57) |
| 25–34 years | 0.00 (Reference) | 0.00 (Reference) |
| 35–39 years | 0.00 (−0.01, 0.01) | 0.12 (−0.16, 0.39) |
| 40+ years | 0.01 (−0.01, 0.03) | −0.00 (−0.58, 0.57) |
| MODEL 5: MATERNAL RACE/ETHNICITY INTERACTION | ||
| Gestational Age (week) | 0.03 (0.02, 0.03) | 0.50 (0.41, 0.60) |
| Gestational Age*Maternal Race/Ethnicity | ||
| Asian NH | 0.00 (−0.02, 0.03) | 0.22 (−0.66, 1.11) |
| Black NH | 0.00 (−0.01, 0.01) | 0.04 (−0.28, 0.36) |
| Hispanic | 0.00 (−0.01, 0.02) | 0.22 (−0.36, 0.80) |
| Native Am. NH | −0.01 (−0.03, 0.02) | 0.22 (−0.70, 1.14) |
| Other NH | 0.01 (−0.16, 0.17) | −3.45 (−7.55, 6.59) |
| White NH | 0.00 (Reference) | 0.00 (Reference) |
| MODEL 6: MATERNAL MARITAL STATUS INTERACTION | ||
| Gestational Age (week) | 0.03 (0.02, 0.03) | 0.45 (0.35, 0.55) |
| Gestational Age*Maternal Marital Status | ||
| Married | 0.00 (Reference) | 0.00 (Reference) |
| Unmarried | −0.00 (−0.01, 0.00) | 0.12 (−0.06, 0.31) |
Abbreviations: Am, American; β, beta; CI, confidence interval; grad, graduate; HS, high school; NH, non-Hispanic; PALS-K, Phonological Awareness Literacy Screening – Kindergarten.
All regressions adjusted for maternal age, maternal education, maternal race/ethnicity, maternal marital status, Medicaid delivery coverage, parity, and child’s sex. Regressions cluster standard errors at the mother level.
We standardized the PALS-K score to mean 0 and standard deviation 1.
The PALS-K benchmark is a score of 28 points or greater on the test (range: 0–102 points). Failure to meet the benchmark signals that a child may need early literacy intervention.
Table 3.
Estimated Linear Combinations of Interaction Coefficients from Ordinary Least Squares Regressionsa of PALS-K Outcomes on Gestational Age in Completed Weeks (n = 153,145)
| Outcome: Standardized PALS-K Scoreb | Outcome: Probability of Meeting Literacy Benchmarkc, Percentage Point |
|
|---|---|---|
| β Coefficient (95% CI) | β Coefficient (95% CI) | |
| MEDICAID DELIVERY COVERAGE-GESTATIONAL AGE INTERACTION | ||
| Non-Medicaid | 0.02 (0.02, 0.03) | 0.32 (0.22, 0.42) |
| Medicaid | 0.03 (0.03, 0.04) | 0.79 (0.62, 0.96) |
| MATERNAL EDUCATION-GESTATIONAL AGE INTERACTION | ||
| 1–3 years HS | 0.02 (0.01, 0.03) | 0.61 (0.26, 0.95) |
| HS grad/equivalent | 0.03 (0.02, 0.03) | 0.72 (0.54, 0.90) |
| 1–3 years college | 0.03 (0.03, 0.04) | 0.48 (0.33, 0.63) |
| 4 years college | 0.03 (0.02, 0.03) | 0.35 (0.22, 0.48) |
| 5+ years college | 0.01 (0.01, 0.02) | 0.09 (−0.07, 0.25) |
| MATERNAL AGE-GESTATIONAL AGE INTERACTION | ||
| <20 years | 0.02 (0.01, 0.02) | 0.44 (0.10, 0.78) |
| 20–24 years | 0.03 (0.03, 0.04) | 0.76 (0.55, 0.97) |
| 25–34 years | 0.03 (0.02, 0.03) | 0.43 (0.32, 0.54) |
| 35–39 years | 0.03 (0.02, 0.04) | 0.54 (0.29, 0.80) |
| 40+ years | 0.03 (0.01, 0.05) | 0.43 (−0.14, 0.99) |
| MATERNAL RACE/ETHNICITY-GESTATIONAL AGE INTERACTION | ||
| Asian NH | 0.03 (0.02, 0.05) | 0.72 (−0.15, 1.60) |
| Black NH | 0.03 (0.02, 0.04) | 0.54 (0.24, 0.85) |
| Hispanic | 0.03 (0.01, 0.04) | 0.72 (0.15, 1.29) |
| Native Am. NH | 0.02 (−0.00, 0.04) | 0.73 (−0.19, 1.64) |
| Other NH | 0.03 (−0.13, 0.20) | −2.94 (−7.05, 1.16) |
| White NH | 0.03 (0.02, 0.03) | 0.50 (0.41, 0.60) |
| MATERNAL MARITAL STATUS-GESTATIONAL AGE INTERACTION | ||
| Married | 0.03 (0.02, 0.03) | 0.45 (0.35, 0.55) |
| Unmarried | 0.03 (0.02, 0.03) | 0.57 (0.41, 0.73) |
Abbreviations: Am., American; CI, confidence interval; grad, graduate; HS, high school; NH, non-Hispanic; PALS-K, Phonological Awareness Literacy Screening-Kindergarten.
All regressions adjusted for maternal age, maternal education, maternal race/ethnicity, maternal marital status, Medicaid delivery coverage, parity, and child’s sex. Regressions cluster standard errors at the mother level.
We standardized the PALS-K score to mean 0 and standard deviation 1.
The PALS-K benchmark is a score of 28 points or greater on the test (range: 0–102 points). Failure to meet the benchmark signals that a child may need early literacy intervention.
We predicted standardized PALS-K scores and probabilities of meeting its literacy benchmark for each week of gestational age, stratified by Medicaid coverage or by maternal education (Figures 2A–B). Modification is most apparent in predicted probabilities of meeting the literacy benchmark (Figure 2B). The relation between gestational age and the predicted probability of meeting the benchmark was stronger for children with Medicaid-covered births relative to their non-Medicaid peers. Similarly, this relation gradually attenuated with greater maternal education. Indeed, there was no apparent relation between gestational age and the probability of meeting the benchmark among children whose mothers had 5+ years of college education: their predicted probability of meeting the benchmark was approximately 95% regardless of gestational age. We observed similar albeit more modest patterns when predicting the standardized PALS-K score (Figure 2A). Moreover, non-Medicaid coverage and greater education were consistently associated with better PALS-K performance at all weeks of gestational age. A post-hoc analysis predicted the probabilities of meeting the PALS-K benchmark by preterm birth status overall, by Medicaid coverage, and by maternal education (Table 4). Again, non-Medicaid coverage and higher levels of maternal education attenuated preterm birth’s negative association with the probability of meeting the benchmark.
Figure 2.
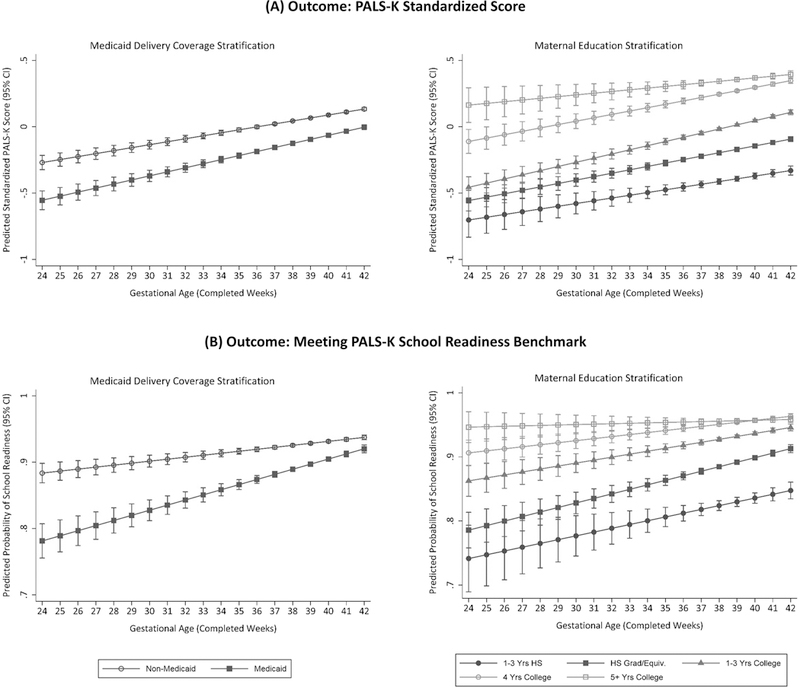
Predicted PALS-K Outcomes by Gestational Age, Stratified by Maternal Education or Medicaid Delivery Coverage (n = 151,592)
Legend for Maternal Education: shaded circle = 1–3 years of high school; shaded square = high school degree or equivalent; shaded triangle = 1–3 years of college; clear circle = 4 years of college; clear square = 5+ years of college.
Legend for Medicaid Delivery Coverage: shaded circle = non-Medicaid; shaded square = Medicaid.
Notes: The standardized PALS-K score has a mean of 0 and a standard deviation of 1. The literacy benchmark is a PALS-K score of at least 28 points (range 0–102). All predictions generated by ordinary least squares regression models adjusted for maternal age, maternal education, maternal race/ethnicity, maternal marital status, Medicaid delivery coverage, parity, and child’s sex. We included a gestational age-Medicaid delivery coverage interaction to stratify predictions by Medicaid delivery coverage, and we included a gestational age-maternal education interaction to stratify predictions by maternal education. Regressions are clustered at the mother level.
Table 4.
Predicted Probabilitiesa of Meeting the PALS-K Literacy Benchmarkb, Stratified by Preterm Birth (n = 153,145)
| Term Birth (Gestational Age ≥37 Weeks) |
Preterm Birth (Gestational Age <37 Weeks) |
|
|---|---|---|
| Predicted Probability, % (95% CI) | Predicted Probability, % (95% CI) | |
| Overall | 91.74 (91.60, 91.89) | 88.92 (88.29, 89.56) |
| By Medicaid Delivery Coverage | ||
| Non-Medicaid | 92.91 (92.71, 93.11) | 91.39 (90.73, 92.62) |
| Medicaid | 89.93 (89.62, 90.23) | 85.46 (84.29, 86.63) |
| By Maternal Education | ||
| 1–3 years HS | 83.19 (82.46, 83.92) | 79.16 (76.85, 81.48) |
| HS grad/equivalent | 89.35 (89.04, 89.66) | 85.54 (84.28, 86.81) |
| 1–3 years college | 93.30 (93.06, 93.55) | 91.07 (90.02, 92.13) |
| 4 years college | 95.49 (95.26, 95.72) | 93.80 (92.88, 94.71) |
| 5+ years college | 95.70 (95.42, 95.97) | 94.69 (93.50, 95.89) |
Abbreviations: CI, confidence interval; grad, graduate; HS, high school; PALS-K, Phonological Awareness Literacy Screening-Kindergarten.
All predictions generated by ordinary least squares regression models adjusted for maternal age, maternal education, maternal race/ethnicity, maternal marital status, Medicaid delivery coverage, parity, and child’s sex. We included a gestational age-Medicaid delivery coverage interaction to stratify predictions by Medicaid delivery coverage, and we included a gestational age-maternal education interaction to stratify predictions by maternal education. Regressions are clustered at the mother level.
The PALS-K benchmark is a score of 28 points or greater on the test (range: 0–102 points). Failure to meet the benchmark signals that a child may need early literacy intervention.
After excluding very preterm or SGA deliveries, Medicaid delivery coverage, maternal education, and maternal age no longer modified the association between gestational age and the standardized score. However, Medicaid delivery coverage and maternal college education still modified the association of gestational age with the probability of meeting the benchmark both in magnitude and direction. Excluding very preterm or SGA births did not change other results, and controlling for maternal smoking did not notably alter any result.
COMMENT
Principal findings
The positive association of gestational age with standardized kindergarten-level literacy measures is greater for children whose birth was Medicaid-covered and for those whose mothers had less education at the time of their birth. These results emphasize that preterm birth’s potential cost on early literacy skills disproportionately impacts children from socioeconomically disadvantaged backgrounds, and, likewise, that preterm children of more affluent mothers may be able to overcome the potential harms associated with shorter gestation.
Strengths of the study
Our study had two key strengths. First, we investigated modification of the gestational age-literacy relationship with several socioeconomic and demographic variables. This captured a broad dimension of a child’s background and allowed us to investigate specific potential modifiers, the latter of which is incompatible with composite measures. Second, we studied continuous and dichotomous outcomes using a standardized assessment. The standardized PALS-K score allowed us to investigate modification on a finer gradient with respect to average literacy. With the PALS-K benchmark, we examined modification on the lower-performing end of the literacy distribution, and it represented a discrete outcome with explicit interpretation – whether a child is sufficiently prepared for kindergarten-level instruction.
Limitations of the data
We acknowledge some limitations. First, we only observed maternal characteristics at delivery and they may have changed before the child’s PALS-K assessment. Second, we did not observe potentially important socioeconomic or demographic variables. BD4LK does not have direct measures of economic status, such as household income, and we excluded all paternal information due to non-random missingness on birth records. Third, our findings may have limited generalizability outside of Wisconsin. Approximately 8.8% of all singleton deliveries in the US (2007–2010) were born preterm,52,53 but preterm births comprised only 6.3% of our sample. Moreover, relative to all US singleton deliveries (2006–2013),53 our sample had a greater composition of white NH mothers (83.6% vs. 59.4%) and college-educated mothers (59.1% vs. 54.4%), reflecting the characteristics of Wisconsin. Finally, our analysis does not elucidate how specific maternal factors modify the gestational age-early literacy relationship. Whether early interventions for preterm children, differential confounders, or another source drives effect heterogeneity remains uncertain. Identifying mechanisms of socioeconomic modification can guide and inform interventions to reduce shorter gestation’s harm on early literacy for children from disadvantaged backgrounds.
Interpretation
Heterogeneous associations of gestational age with kindergarten-level literacy were most apparent when we focused on the probability that a child exceeded the threshold for remedial services. Children whose births were Medicaid-covered or whose mothers had no college education had considerably lower probabilities of meeting the PALS-K benchmark if they were born preterm. In contrast, shorter gestational age had little or no adverse association with the probability of meeting the benchmark among non-Medicaid-born children and children with college-educated mothers. For example, with gestational age <39 weeks, the predicted probabilities of meeting the benchmark were often <90% and sometimes <80% for Medicaid children and for children from less educated backgrounds. Shorter gestation’s penalty was more forgiving otherwise: non-Medicaid children and children with college-educated mothers almost consistently had a >90% probability of meeting the benchmark regardless of gestational age. The magnitude of modification is striking when we predict the number of children who score below the benchmark. Our sample included 4,384 preterm children of Medicaid-paid deliveries. We expect that 3,748 (85.5%) of these children meet the benchmark. Had these children belonged to non-Medicaid deliveries – holding all else constant – 4,016 (91.6%) would meet the benchmark. This suggests an excess of 268 children who are not prepared for kindergarten-level literacy instruction that is not explained by observed socioeconomic or demographic factors.
These findings persisted after excluding very preterm or SGA births, suggesting they are not driven by outliers. Therefore, Medicaid coverage or maternal education modifies gestational age’s association with the probability of meeting the benchmark for the general population of children across the gestational age spectrum.
Evidence of socioeconomic modification was less compelling when we considered continuous literacy scores. In the full sample, the association of gestational age with the standardized PALS-K score was slightly greater for children with Medicaid-covered births and slightly less for children with highly-educated or, perhaps unexpectedly, younger mothers. Still, the absolute differences in the association across these strata were modest, suggesting that the role of socioeconomic modification may be more relevant for children scoring at the lower end of the PALS-K scale than throughout the distribution of scores using this test. Moreover, these relationships were dependent on the scoring patterns among very preterm or SGA children. Excluding these children nullified modification with the continuous score. This could be an artifact of the PALS-K test; its benchmark for identifying children at risk of literacy delay is well validated,42 but the test may not accurately discriminate among children with average or above average literacy skills. If so, then measurement error might attenuate estimates of modification on the standardized score.
Children of socioeconomically disadvantaged mothers not only disproportionately experience preterm birth,14–16 but our findings suggest the consequences of preterm birth on early literacy are greater for these children, emphasizing underlying disparities of preterm birth and its downstream effects. Still, how these disparities manifest remains disputed. Socioeconomic factors may allay preterm birth’s consequences on literacy, as affluent families may have better access to early interventions for preterm infants that facilitate cognitive development.17–19 These programs are beneficial, but their effectiveness depends on their services, frequency of contact, and the child’s age upon enrollment.54
Socioeconomic variation in unobserved confounding of the gestational age-academic performance relationships may also explain observed modification. As stated previously, tobacco use may be such a confounder that is more prevalent among socioeconomically disadvantaged mothers,50–52 but controlling for maternal smoking did not explain modification in our study. Absent a clear causal pathway, our results nonetheless highlight that the cost of preterm birth on academic performance is disproportionately greater for children from socioeconomically disadvantaged backgrounds. In contrast, we found no compelling evidence of modification by mother’s demographic characteristics, potentially indicating that demographic disparities not amplify these relationships.
Our findings do not wholly align with prior research. Although two studies’ findings suggest that socioeconomic advantage may slightly mitigate shorter gestation’s detriment to academic performance,5,27 most contemporary research observed no such modification.28–33 Our results may stand in greatest contrast to a 2016 study that found no evidence of modification by maternal age, race/ethnicity, education, and poverty status (which determines Medicaid eligibility).30 However, this particular study used a much smaller sample (5,250 children) and categorized gestational age, thereby limiting statistical power to test modification. Many similar studies faced such constraints.29,31–33 Moreover, some studies that found no evidence of modification used composite socioeconomic measures.31,33 Composite measures smooth over errors in measurement, offering more reliable indicators of latent attributes like socioeconomic status. However, they sacrifice the ability to identify specific modifiers and may obscure modification that is induced by one or more variables within the composite. We avoided this shortcoming by using individual modifiers.
Conclusions
Socioeconomic advantage, as measured by maternal education and Medicaid delivery coverage, may buffer shorter gestation’s harm on early childhood literacy. Future investigations should explore mechanisms of socioeconomic modification.
Supplementary Material
SOCIAL MEDIA QUOTE.
Tweet
The adverse association between gestational age and kindergarten literacy is attenuated for children born to more socioeconomically advantaged mothers.
SYNOPSIS.
Research Question
Do maternal socioeconomic or demographic factors modify the association between gestational age and children’s scores on a standardized test of kindergarten-level literacy?
What’s Already Known
Shorter gestational age is associated with lower cognitive skills in early childhood. Findings from prior studies suggest that less completed maternal education, lower socioeconomic status, or neighborhood poverty may amplify this relationship. Other studies found no evidence of modification by socioeconomic or demographic factors.
What this Study Adds
We found that the relationship between gestational age and the probability of demonstrating grade-level literacy skills upon kindergarten enrollment was greater for children whose deliveries were Medicaid-paid relative to their non-Medicaid peers and for children whose mothers only completed high school relative to those whose mothers attended college.
ACKNOWLEDGEMENTS
This work was supported by the University of Wisconsin-Madison Clinical and Translational Science Award program through the National Institutes of Health National Center for Advancing Translational Sciences (Grant UL1TR00427), by the University of Wisconsin-Madison School of Medicine and Public Health’s Wisconsin Partnership Program, and by the University of Wisconsin-Madison Institute for Research on Poverty. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the University of Wisconsin-Madison School Medicine and Public Health’s Wisconsin Partnership Program, or the Institute for Research on Poverty.
We thank Steven T. Cook, Dan Ross, Jane A. Smith, Kristen Voskuil, and Lynn Wimer for data access and programming assistance, and we thank Lawrence M. Berger and Russell S. Kirby for their feedback on this analysis. We also thank the Wisconsin Department of Children and Families, Department of Health Services and Department of Workforce Development for the use of data for this analysis, but these agencies do not certify the accuracy of the analyses presented.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Brandt P, Magyary D, Hammond M, Barnard K. Learning and behavioral-emotional problems of children born preterm at second grade. Journal of Pediatric Psychology. 1992; 17:291–311. [DOI] [PubMed] [Google Scholar]
- 2.Johnson S, Hennessy E, Smith R, Trikic R, Wolke D, Marlow N. Academic attainment and special educational needs in extremely preterm children at 11 years of age: the EPICure study. Archives of Disease in Childhood. Fetal and Neonatal Edition. 2009; 94:F283–289. [DOI] [PubMed] [Google Scholar]
- 3.Lipkind HS, Slopen ME, Pfeiffer MR, McVeigh KH. School-age outcomes of late preterm infants in New York City. American Journal of Obstetrics & Gynecology. 2012; 206:222.e1–222.e6. [DOI] [PubMed] [Google Scholar]
- 4.Mathiasen R, Hansen BM, Andersen AM, Forman JL, Greisen G. Gestational age and basic school achievements: a national follow-up study in Denmark. Pediatrics. 2010; 126:e1553–e1561. [DOI] [PubMed] [Google Scholar]
- 5.Figlio DN, Guryan J, Karbownik K, Roth J. Long-term cognitive and health outcomes of school-aged children who were born late-term vs full-term. JAMA Pediatrics. 2016; 170:758–764. [DOI] [PubMed] [Google Scholar]
- 6.Kirkegaard I, Obel C, Hedegaard M, Henriksen TB. Gestational age and birth weight in relation to school performance of 10-year-old children: a follow-up study of children born after 32 completed weeks. Pediatrics. 2006; 118:1600–1606. [DOI] [PubMed] [Google Scholar]
- 7.Noble KG, Fifer WP, Rauh VA, Nomura Y, Andrews HF. Academic achievement varies with gestational age among children born at term. Pediatrics. 2012; 130:E257–E264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quigley MA, Poulsen G, Boyle E, Wolke D, Field D, Alfirevic Z, et al. Early term and late preterm birth are associated with poorer school performance at age 5 years: a cohort study. Archives of Disease in Childhood. Fetal and Neonatal Edition. 2012; 97:F167–F173. [DOI] [PubMed] [Google Scholar]
- 9.Richards JL, Drews-Botsch C, Sales JM, Flanders WD, Kramer ML. Describing the shape of the relationship between gestational age at birth and cognitive development in a nationally representative U.S. birth cohort. Paediatric and Perinatal Epidemiology. 2016; 30:571–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Searle AK, Smithers LG, Chittleborough CR, Gregory TA, Lynch JW. Gestational age and school achievement: a population study. Archives of Disease in Childhood. Fetal and Neonatal Edition. 2017; 102:F409–F416. [DOI] [PubMed] [Google Scholar]
- 11.Bakken L, Brown, N, Downing B. Early childhood education: the long-term benefits. Journal of Research in Childhood Education. 2017; 31:255–269. [Google Scholar]
- 12.Duncan GJ, Dowsett CJ, Claessens A, Magnuson K, Huston AC, Klebanov P, et al. School readiness and later achievement. Developmental Psychology. 2007; 43:1428–1446. [DOI] [PubMed] [Google Scholar]
- 13.Heckman JJ. The economics of inequality: the value of early childhood education. American Educator. 2011; 35:31–35. [Google Scholar]
- 14.Blumenshine PM, Egerter SA, Barclay CJ, Cubbin C, Braveman PA. Socioeconomic disparities in adverse birth outcomes. American Journal of Preventive Medicine. 2010; 39:263–272. [DOI] [PubMed] [Google Scholar]
- 15.Blumenshine PM, Egerter SA, Libet ML, Braveman PA. Father’s education: an independent marker of risk for preterm birth. Maternal and Child Health Journal. 2011; 15:60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Daoud N, O’Campo P, Minh A, Urquia ML, Dzakpasu S, Heaman M, et al. Patterns of social inequalities across pregnancy and birth outcomes: a comparison of individual and neighborhood socioeconomic measures. BMC Pregnancy and Childbirth. 2014; 14:E393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Datar A, Kilburn MR, Loughran DS. Endowments and parental investments in infancy and early childhood. Demography. 2010; 47:145–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sirin SR. Socioeconomic status and academic achievement: a meta-analytic review of research. Review of Educational Research. 2005; 75:417–453. [Google Scholar]
- 19.Restrepo BJ. Parental investment responses to a low birth weight outcome: who compensates and who reinforces? Journal of Population Economics. 2016; 29:969–989. [Google Scholar]
- 20.Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009; 124:S163. [DOI] [PubMed] [Google Scholar]
- 21.Shonkoff JP. Leveraging the biology of adversity to address the roots of disparities in health and development. Proceedings of the National Academy of Sciences. 2012; 109:17302–17307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Reports. 2014; 129:19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Dominguez TP, Dunkel-Schetter C, Glynn LM, Hobel C, Sandman CA. Racial differences in birth outcomes: the role of general, pregnancy, and racism stress. Health Psychology. 2008; 27:194–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alhusen JL, Bower K, Epstein E, Sharps P. Racial discrimination and adverse birth outcomes: an integrative review. Journal of Midwifery & Women’s Health. 2016; 61:707–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jaffee S, Caspi A, Moffitt TE, Belsky J, Silva P. Why are children born to teen mothers at risk for adverse outcomes in young adulthood? Results from a 20-year longitudinal study. Development and Psycholpathology. 2001; 13:377–397. [DOI] [PubMed] [Google Scholar]
- 26.Aquilino WS. The life course of children born to unmarried mothers: childhood living arrangements and young adult outcomes. Journal of Marriage and Family. 1996; 58:293–310. [Google Scholar]
- 27.Richards JL, Chapple-McGruder T, Williams BL, Kramer MR. Does neighborhood deprivation modify the effect of preterm birth on children’s first grade academic performance? Social Science & Medicine. 2015; 132:122–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Figlio DN, Guryan J, Karbownik K, Roth J. The effects of poor neonatal health on children’s cognitive development. American Economic Review. 2014; 140:3921–3955. [DOI] [PubMed] [Google Scholar]
- 29.Kull MA, Coley RL. Early physical health conditions and school readiness skills in a prospective birth cohort of U.S. children. Social Science & Medicine. 2015; 142:145–153. [DOI] [PubMed] [Google Scholar]
- 30.Shah PE, Kaciroti N, Richards B, Lumeng JC. Gestational age and kindergarten school readiness in a national sample of preterm infants. The Journal of Pediatrics. 2016; 178:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beauregard JL, Drews-Botsch C, Sales JM, Flanders WD, Kramer MR. Does socioeconomic status modify the association between preterm birth and children’s early cognitive ability and kindergarten academic achievement in the United States? American Journal of Epidemiology. 2018; 187:1704–1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beauregard JL, Drews-Botsch C, Sales JM, Flanders WD, Kramer MR. Preterm birth, poverty, and cognitive development. Pediatrics. 2018; 141:E20170509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.ElHassan NO, Bai S, Gibson N, Holland G, Robbins JM, Kaiser JR. The impact of prematurity and maternal socioeconomic status and education level on achievement-test scores up to 8th grade. PLoS ONE. 2018; 13:E0198083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Larson A, Berger LM, Mallinson DC, Grodsky E, Ehrenthal DB. Variable uptake of Medicaid-covered prenatal care coordination: the relevance of treatment level and service context. Journal of Community Health. 2019; 44:32–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brown PR, Ross D, Smith JA, Thornton K, Wimer L. Technical Report on Lessons Learned from the Development of the Institute for Research on Poverty’s Multi-Sample Person File (Multi-Sample Person File) Data System. Madison, WI: University of Wisconsin-Madison Institute for Research on Poverty; 2011. [Google Scholar]
- 36.Health Resources and Services Administration, US Department of Health and Human Services. HRSA data warehouse – area health resource file 2017–18 release. North Bethesda, MD: Health Resources and Services Administration; 2018. https://data.hrsa.gov/data/download. Accessed October 11 2018. [Google Scholar]
- 37.Wisconsin Department of Public Instruction. Admissions and early entrance to four- and five-year-old kindergarten. https://dpi.wi.gov/early-childhood/kind/admission. Accessed March 1, 2019.
- 38.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstetrics & Gynecology. 1996; 87:163–168. [DOI] [PubMed] [Google Scholar]
- 39.American College of Obstetricians and Gynecologists. Methods for estimating the due date. Committee Opinion No. 700. Obstetrics & Gynecology. 2017; 129:E150–E154. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Centers for Medicare & Medicaid Services. Medicaid & CHIP coverage. https://www.healthcare.gov/medicaid-chip/getting-medicaid-chip/. Accessed May 24, 2019. [Google Scholar]
- 41.Invernizzi M, Justice L, Landrum TJ, Booker K. Early literacy screening in kindergarten: widespread implementation in Virginia. Journal of Literacy Research. 2004; 36:479–500. [Google Scholar]
- 42.Invernizzi M, Juel C, Swank L, Meier J. PALS K Technical Reference. Charlottesville, VA: University of Virginia Curry School of Education; 2015. [Google Scholar]
- 43.Grodsky E, Huangfu Y, Miesner HR, Packard C. Kindergarten Readiness in Wisconsin. Madison, WI: University of Wisconsin-Madison Wisconsin Center for Education Research; 2017 (WCER Working Paper No. 2017–3). [Google Scholar]
- 44.Wisconsin Department of Public Instruction. PALS early literacy screener. https://dpi.wi.gov/assessment/historical/pals. Accessed March 1, 2019.
- 45.Wisconsin Department of Public Instruction. Using PALS data. https://dpi.wi.gov/assessment/historical/pals/data. Accessed March 13, 2019.
- 46.Cheung YB. A modified least-squares regression approach to the estimation of risk difference. American Journal of Epidemiology. 2007; 166:1337–1344. [DOI] [PubMed] [Google Scholar]
- 47.Williams RL. A note on robust variance estimation for cluster-correlated data. Biometrics. 2000; 56:645–646. [DOI] [PubMed] [Google Scholar]
- 48.Oken E, Kleinman KP, Rich-Edwards J, Gillman MW. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatrics. 2003; 3:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Causes of preterm birth. In: Preterm Birth: Causes, Consequences, and Prevention. Editors: Butler A, Behrman R Washington, DC: National Academies Press; 2007; 87–258. [PubMed] [Google Scholar]
- 50.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. The Lancet. 2008; 371:75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clifford A, Lang L, Chen R. Effects of maternal cigarette smoking during pregnancy on cognitive parameters of children and young adults: a literature review. Neurotoxicology and Teratology. 2012; 34:560–570. [DOI] [PubMed] [Google Scholar]
- 52.Drake P, Driscoll AK, Mathews TJ. Cigarette Smoking During Pregnancy: United States, 2016. Hyattsville, MD: National Centers for Health Statistics; 2018. (NCHS Data Brief, No. 305). [PubMed] [Google Scholar]
- 53.Stata Corporation. Stata statistical software, release 15. College Station, TX: Stata Corporation; 2017. [Google Scholar]
- 54.Guralnick MJ. Preventive interventions for preterm children: effectiveness and developmental mechanisms. Journal of Developmental & Behavioral Pediatrics. 2012; 33:352–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


