Abstract
Background
Attention‐deficit/hyperactivity disorder (ADHD) is one of the most common developmental disorders experienced in childhood and can persist into adulthood. The disorder has early onset and is characterized by a combination of overactive, poorly modulated behavior with marked inattention. In the long term it can impair academic performance, vocational success and social‐emotional development. Meditation is increasingly used for psychological conditions and could be used as a tool for attentional training in the ADHD population.
Objectives
To assess the effectiveness of meditation therapies as a treatment for ADHD.
Search methods
Our extensive search included: CENTRAL, MEDLINE, EMBASE, CINAHL, ERIC, PsycINFO, C2‐SPECTR, dissertation abstracts, LILACS, Virtual Health Library (VHL) in BIREME, Complementary and Alternative Medicine specific databases, HSTAT, Informit, JST, Thai Psychiatric databases and ISI Proceedings, plus grey literature and trial registries from inception to January 2010.
Selection criteria
Randomized controlled trials that investigated the efficacy of meditation therapy in children or adults diagnosed with ADHD.
Data collection and analysis
Two authors extracted data independently using a pre‐designed data extraction form. We contacted study authors for additional information required. We analyzed data using mean difference (MD) to calculate the treatment effect. The results are presented in tables, figures and narrative form.
Main results
Four studies, including 83 participants, are included in this review. Two studies used mantra meditation while the other two used yoga compared with drugs, relaxation training, non‐specific exercises and standard treatment control. Design limitations caused high risk of bias across the studies. Only one out of four studies provided data appropriate for analysis. For this study there was no statistically significant difference between the meditation therapy group and the drug therapy group on the teacher rating ADHD scale (MD ‐2.72, 95% CI ‐8.49 to 3.05, 15 patients). Likewise, there was no statistically significant difference between the meditation therapy group and the standard therapy group on the teacher rating ADHD scale (MD ‐0.52, 95% CI ‐5.88 to 4.84, 17 patients). There was also no statistically significant difference between the meditation therapy group and the standard therapy group in the distraction test (MD ‐8.34, 95% CI ‐107.05 to 90.37, 17 patients).
Authors' conclusions
As a result of the limited number of included studies, the small sample sizes and the high risk of bias, we are unable to draw any conclusions regarding the effectiveness of meditation therapy for ADHD. The adverse effects of meditation have not been reported. More trials are needed.
Keywords: Adolescent, Child, Female, Humans, Male, Yoga, Attention Deficit Disorder with Hyperactivity, Attention Deficit Disorder with Hyperactivity/drug therapy, Attention Deficit Disorder with Hyperactivity/therapy, Meditation, Meditation/methods, Relaxation Therapy, Relaxation Therapy/methods
Meditation therapies for attention‐deficit/hyperactivity disorder (ADHD)
Attention‐deficit/hyperactivity disorder (ADHD) is a disorder that affects a significant number of children and adults in a variety of ways. It is characterized by chronic levels of inattention, impulsiveness and hyperactivity. Meditation therapy could be a beneficial treatment for those diagnosed with ADHD. The objective of this review was to assess the efficacy of this treatment. As a result of the small number of studies that we were able to include in this review and the limitations of those studies, we were unable to draw any conclusions regarding the effectiveness of meditation therapy for ADHD. No adverse effects of meditation in children have been reported. More trials are needed on meditation therapies for ADHD so that conclusions can be drawn regarding its effectiveness.
Summary of findings
Summary of findings for the main comparison.
Meditation therapy versus drug therapy for attention deficit /hyperactivity disorder
| Meditation therapy versus drug therapy for attention deficit /hyperactivity disorder | ||||||
| Patient or population: patients with attention deficit /hyperactivity disorder Settings: Intervention: meditation therapy versus drug therapy | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | meditation therapy versus drug therapy | |||||
| Teacher rating ADHD overall scale The Abbreviated Parent‐Teacher Questionnaire (Conners, 1973) Follow‐up: mean 4 weeks | The mean teacher rating adhd overall scale in the control groups was 14.83 | The mean Teacher rating ADHD overall scale in the intervention groups was 2.72 lower (8.49 lower to 3.05 higher) | 15 (1 study4) | ⊕⊝⊝⊝ very low1,2,3 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Unclear randomization method, unclear allocation concealment, no blinding, unclear attrition rate, other biases presented 2 Wide confidence interval, small sample size 3 Only one study( since 1987) presented for this outcome 4 Study Moretti‐Altuna, 1987
Summary of findings 2.
meditation therapy versus standard treatment without drug for attention deficit /hyperactivity disorder
| meditation therapy versus standard treatment without drug for attention deficit /hyperactivity disorder | ||||||
| Patient or population: patients with attention deficit /hyperactivity disorder Settings: Intervention: meditation therapy versus standard treatment without drug | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Control | meditation therapy versus standard treatment without drug | |||||
| Teacher rating ADHD overall scale Abbreviated Parent‐Teacher Questionnaire (Conner, 1973) Follow‐up: mean 4 weeks | The mean teacher rating adhd overall scale in the control groups was 12.63 | The mean Teacher rating ADHD overall scale in the intervention groups was 0.52 lower (5.88 lower to 4.84 higher) | 17 (1 study4) | ⊕⊝⊝⊝ very low1,2,3 | ||
| *The basis for the assumed risk (e.g. the median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1 Unclear randomization, unclear allocation concealment, no blinding, unclear attrition rate, other biases presented 2 Wide confidence interval, small sample size 3 Only one study(since 1987) present for this outcome 4 Study Moretti‐Altuna, 1987
Background
Description of the condition
Attention‐deficit/hyperactivity disorder (ADHD) is one of the most common developmental problems experienced in childhood and can persist into adulthood. The major symptoms are inconsistent development and chronic levels of inattention, impulsiveness and hyperactivity (Scahill 2000).
Prevalence estimates vary according to the diagnostic criteria used and the population sampled. These estimates can be further affected by influences on the diagnosis, such as the cultural environment and the differing attitudes of parents, clinicians and society towards acceptable children's behavior (Dwivedi 2005). According to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition, Text Revision (DSM‐IV‐TR) (APA 2000), prevalence estimates among school children in the US are between 3% and 7% (APA 2000), but other estimates range from 1.7% to 16.0% (Pritchard 2005). Boys are diagnosed with ADHD three times more often than girls. Evidence attests to the strong influence of genetic factors on the expression of symptoms, however psychosocial, environmental and cultural factors also play a role (Swanson 2001).
An independent diagnostic test for ADHD does not exist, thus the diagnosis of ADHD is clinically based. The essential criteria for a diagnosis of ADHD are a persistent pattern of inattention and/or hyperactivity‐impulsivity that is more frequently displayed and more severe than is typically observed in individuals at a comparable level of development, and is not better explained by the presence of another mental disorder. Symptoms evolve over time. In adolescence, signs of excessive gross motor activity (e.g. excessive running and climbing, not remaining seated) are less common, and hyperactivity symptoms may be confined to fidgeting or an inner feeling of jitteriness or restlessness. In adulthood, restlessness may lead to difficulty in participating in sedentary activities and to avoiding pastimes or occupations that provide limited opportunity for spontaneous movement (e.g. desk jobs) (APA 2000). Other adults may retain only some of the symptoms, in which case the diagnosis should be ADHD in partial remission.
In order to qualify for a diagnosis of ADHD, hyperactive‐impulsive or inattentive symptoms must have presented before the age of seven, with some impairment from the symptoms present in at least two settings (e.g. at home and at school). There must be clear evidence of interference with developmentally appropriate social, academic or occupational functioning. Care must be taken to ensure that the disturbance does not occur exclusively during the course of a pervasive developmental disorder, schizophrenia or other psychotic disorder and is not better accounted for by another mental disorder (APA 2000).
The DSM‐IV‐TR provides subtypes for specifying the predominant symptom presentation: predominantly inattentive type, predominantly hyperactive/impulsive type and combined type. In the International Classification of Diseases (ICD‐10) (WHO 1992) the disorders are defined under the category of 'Hyperkinetic Disorders' and are characterized by early onset, a combination of overactive, poorly modulated behavior with marked inattention and lack of persistent task involvement, pervasiveness across situations and persistence over time (WHO 1992).
Children with ADHD have pronounced impairments and can experience enduring adverse effects in their academic performance, vocational success and social‐emotional development. These impairments, in turn, can have a profound impact on individuals, families, schools and society (NIH 1998). Moreover, studies indicate that children diagnosed as having ADHD and a comorbid anxiety or depressive disorder have higher levels of coexisting life stresses and parental symptoms than children who have the single diagnosis of ADHD (Jensen 1993).
Description of the intervention
Non‐pharmacological treatment of ADHD in childhood can be divided into three categories: parent‐ or family‐focused strategies, child‐directed interventions and school‐based interventions (ICSI 2005). Psychostimulant medications are considered first‐line therapy as they are effective in 70% to 80% of children with ADHD, although their use may be limited both by tolerability and acceptability (AAP 2001). Augmentation of psychostimulant treatment with psychosocial interventions provides no advantage over medication alone for the core symptoms of ADHD, but appears to have an advantage for associated problems such as anxiety disorders, social skills difficulties, consumer satisfaction and possibly academic achievement (MTA 1999).
Due to an increase in scientific evidence, clinical experience and community attitudes are encouraging a shift towards more natural and holistic forms of therapy as alternatives or adjuncts to pharmacological approaches in a variety of conditions (Arias 2006; Krisanaprakornkit 2006; Mansky 2006).
Meditation is becoming increasingly popular as a treatment for psychological conditions and has a wide range of applications. A psychologically‐oriented definition states that "meditation is a set of attentional practices leading to an altered state or trait of consciousness characterized by expanded awareness, greater presence, and a more integrated sense of self" (Davis 1998), which suggests that meditation might be a useful tool for attentional training in the ADHD population. In addition to increased attention, meditation may produce a state of calmness and contentment which is generally lacking in the ADHD population (Jensen 2004). Adequately trained practitioners who have first‐hand experience can easily adapt meditation to the general medical setting (Hassed 1996).
Meditation originated in India more than three thousand years ago and has played a prominent role in the ritual practice of major religions and secular organizations alike. Meditation can be divided into two general types: concentrative meditation and mindfulness meditation (Barrows 2002).
Concentrative meditation is best represented in modern medicine by two programs: Transcendental Meditation® (TM®) which was introduced to the West during 1960s and the 'Relaxation Response' developed subsequently by Benson (Benson 1975). Concentrative meditation involves focusing attention on an object and sustaining attention until the mind achieves stillness. A diverse range of items could be chosen as the focal object, for example words, light, colors, geometric forms, ideas etc. Continuous practice should result in relaxation, clarity of mind and calmness.
Mindfulness meditation emphasizes an open awareness to any contents of the mind that are emerging. After a period of practice the patient should develop a sustainable attentive observational capability, without reacting to their own thoughts and emotions. Achieving this state of mindfulness and equanimity helps to retrain or decondition previous patterns of reaction which are usually poorly adapted to external reality. This form of meditation is commonly represented by mindfulness‐based stress reduction programs (Kabat‐Zinn 1992). The techniques of mindfulness meditation, with their emphasis on developing detached observation and awareness of the contents of consciousness, may represent a powerful cognitive behavioral coping strategy for transforming the ways in which we respond to life events (Astin 1997).
Meditation, either concentrative or mindfulness, is able to enhance the attentional ability of the practitioners. Whilst concentrative meditation emphasizes sustained attention, mindfulness meditation aims to improve self‐control and inhibitions to various internal and external stimuli, thereby helping to relieve the core symptoms of ADHD. However, any single meditation program will usually use both concentrative and mindfulness together.
Recently, five broad categories of meditation practices were identified by a group of experts using modified Delphi methodology (Ospina 2007).
Mantra meditation (comprising the Transcendental Meditation® technique (TM®), Relaxation Response (RR) and Clinically Standardized Meditation (CSM)).
Mindfulness meditation (comprising Vipassana, Zen Buddhist meditation, Mindfulness‐based Stress Reduction (MBSR) and Mindfulness‐based Cognitive Therapy (MBCT)).
Yoga (various yogic meditative techniques).
Tai Chi (encompassing Chinese traditional exercises that promote posture, flexibility, relaxation, well‐being and mental concentration).
Qi Gong (a category of 'energy healing', including Reiki, therapeutic touch and the Korean practice of Chundosunbup).
However, in this review we adhere to the old classification since it is generally well accepted and commonly used in the literature, although both classifications substantially overlap.
Thus, the operational definitions of meditation are the specific techniques of mind training which have two fundamental attentional strategies (Barrows 2002).
Concentrative meditation entails sustained attention directed towards a single object or point of focus. The aim is one‐pointed attention to a single perception without distraction in order to produce concentration or a one‐minded state.
Mindfulness meditation (opening‐up, insight meditation) involves the continual maintenance of a specific perceptual‐cognitive mind set towards objects as they spontaneously arise in ones awareness with a non‐reactive attitude. The salient features are full awareness or mindfulness of any contents of consciousness with equanimity.
There are many methods which represent meditation in the above definitions, i.e. insight meditation, mindfulness‐based meditation, Vipassana, Qiqong therapy, yoga (Asana, Pranayama, Raja yoga, Asthanga yoga, Laya yoga, Sahaj Marg etc), Tai Chi, Transcendental Meditation, Kundalini yoga, Anapanasathi (Buddhist breathing meditation), Zen and ChunDoSupBup. It is noted that Asana yoga (yoga of posture) and Tai Chi are also considered to be dynamic aspects of concentrative meditation.
Although historically meditation is associated with religious or spiritual movements, this is no longer always the case. It is now necessary to confirm the effectiveness of these meditation techniques by using non‐cult, faith‐free and specifically designed methods to treat patients. Nowadays there are increasing numbers of organizations which use scientific‐based, less mystical terms to identify their techniques (Krisanaprakornkit 2006).
How the intervention might work
Some reports exist which detail the usefulness of meditation for children with ADHD. Grosswald (reported in Micucci 2005) conducted a study in April 2004 at Chelsea School in Silver Spring, Maryland, a private school for children with learning disabilities. The study compared ten students with ADHD before and after they learned and practiced Transcendental Meditation for ten minutes twice daily for three months. Participants reported being calmer, less distracted, less stressed and better able to control their anger and frustration. However, there was no control/comparison group in this study.
Preliminary bibliographic searching has not identified many studies using meditation therapy for ADHD. Jensen et al conducted a randomized controlled trial of the effect of yoga on boys with ADHD (n = 11) (Jensen 2004). This program consisted of respiratory training, postural training, relaxation training and concentration training and involved a technique called Trataka where participants focused on a word or shape, followed by seeing the image with their eyes closed and continuing to see the image on a blank piece of paper. The results only slightly supported the use of yoga for ADHD and there were some limitations of this study, such as low statistical power and inconsistency of home practices.
Hassasiri et al (Hassasiri 2002) developed a meditation program for children with ADHD in Thailand based on neo‐humanist concepts which comprised meditation and imagery. The program was tested in a before‐after design and found a statistically significant difference in change scores (P < 0.05).
In terms of adverse effects, reports exist suggesting that meditation can cause temporary depersonalization and derealization (Castillo 1990), and there are several reports of a possible association between meditation and psychotic state (Chan‐Ob 1999; French 1975; Lazarus 1976; Walsh 1979). Studies of meditation in pediatric populations are still limited. It is not considered advisable for children to sit for extended lengths of time with closed eyes, which might in any case 'go against the grain' of the active nature of children. Different meditation techniques have different recommended practices for children, e.g. Sahaj Marg Meditation, a system of Raja yoga, recommends a minimum age of 18 before beginning the practice of meditation, implying that this technique is not suitable for younger people. In Transcendental Meditation, it is recommended that children of five years old meditate twice a day for five minutes at a time and thereafter add one minute for each year of their age until reaching 20‐minute sessions when aged 20 and above. Reports of adverse effects of meditation in children are lacking.
Why it is important to do this review
To our knowledge no systematic review has been carried out specifically considering the effectiveness of meditation for ADHD, although several clinical trials have been conducted. This review aims to address that evidence gap.
Objectives
To assess the effects of concentrative and mindfulness meditation therapies for treating attention‐deficit/hyperactivity disorders (ADHD) in children, adolescents and adults.
Methods
Criteria for considering studies for this review
Types of studies
Randomized controlled trials comparing meditation therapy alone or in combination with conventional treatment (consisting of drugs or any other psychological interventions) to i) conventional treatment or ii) no intervention/waiting list control.
We excluded studies where meditation therapy was not a well‐organized program (i.e. no structure, no schedule of practice, no formal setting).
Types of participants
Participants of any age diagnosed with attention‐deficit/hyperactivity disorder (ADHD) or hyperkinetic disorders (HKD) according to established diagnostic criteria.
Types of interventions
Meditation therapy, consisting of concentrative meditation, mindfulness meditation or a combination of both, provided as the main intervention in the case of multi‐component therapy.
Comparison conditions could be one or a combination of the following:
pharmacological therapy;
no intervention or waiting list;
other psychological treatment: cognitive behavioral therapy, parent training program, counseling etc.
Types of outcome measures
Primary outcomes
A. Symptoms of ADHD
Incidence/severity of the core symptoms (inattention, impulsivity, hyperactivity) measured by a validated symptoms rating scale ;
The revised Conners' Parent Rating Scale (CPRS‐R) (Conners 1997; Conners 1998).
Conners' Teacher Rating Scale (CTRS‐R) (Conners 1998/2).
ADHD Rating Scale IV (Zhang 2005).
Attention‐Deficit Disorder Evaluation Scale (ADDES) (Adesman 1991).
Conners' Continuous Performance Test (Conners 1995).
Yale Children's Inventory (Shaywitz 1988).
The ADD/H Adolescent Self‐Report Scale (Robin 1996).
The Internal Restlessness Scale (Weyandt 2003).
B. Quantitative laboratory assessment measures of ADHD symptoms
1. Psychological test
Continuous Performance Test (CPT).
The Gordon Diagnostic System (GDS).
The Children's Checking Task (CCT).
Test of Variable of Attention (TOVA) (Greenberg 1999).
Delay of Gratification Tasks.
The Choice‐Delay Task (C‐DT).
The Stop Signal Task (SST) (Nichols 2004).
The Auditory Continuous Performance Test (Riccio 1996).
2. Psychophysiological measures
Electroencephalography (EEG).
Actograph pedometer which uses devices to monitor a child's movements and displays these as an actograph which provides an objective indicator of general motor activity.
C. Overall incidence/severity of the problem behaviors
Child Behavior Checklist (CBCL) (Achenbach 2000).
The Adolescent Behavior Checklist (Adams 1997).
Children's Aggression Scale ‐ Parent Version (Halperin 2002).
Children's Aggression Scale ‐ Teacher Version (Halperin 2003).
Swanson Kotkin Atkins M‐Flynn Pelham Scale (SKAMP) (Wigal 1998).
Behavior Assessment System for Children (BASC) (Reynolds 1992).
Secondary outcomes
A. Intelligence
Standardized measures, including these intelligence scales.
Wechsler Intelligence Scale for Children‐III (Wechsler 1991).
Stanford‐Binet Intelligence Scales (Becker 2003).
Tower of London Test (Shallice 1988).
B. School/academic performance
Measured by scale, grades or teacher reports, including:
Wechsler Individual Achievement Test (WIAT) (Wechsler 1992);
The Peabody Individual Achievement Test (Klinge 1974).
C. Psychopathology outcomes
Depression/anxiety‐related outcome including:
The Diagnostic Inventory for Depression (Zimmerman 2004);
Multidimensional Anxiety Scale for Children (MASC) (March 1997).
Conduct/oppositional disorder outcomes, including:
The Oppositional Defiant Behavior Inventory (Harada 2004).
D. Family and social outcomes
Parenting Stress Index (Loyd 1985).
Parenting Scale for Parents of Children with ADHD (Harvey 2001).
Social Adjustment Inventory for Children and Adolescents (SAICA) (Biederman 1993).
E. Quality of life scales
The ADHD Impact Module (Landgraf 2002).
Adult Attention‐Deficit/Hyperactivity Disorder Quality‐of‐Life Scale (AAQoL) (Brod 2006).
Clinical Global Impression score changes (NIMH 1985).
Children's Global Assessment Scale (CGAS) (Shaffer 1983).
F. Any adverse effects of meditation reported in the trials
Search methods for identification of studies
To determine whether meditation is the main intervention in multi‐component therapy, the authors of the studies must specify meditation or related words in the title or keywords of the articles. Operational definitions of meditation are mentioned in the background section.
The following searches were conducted without language restriction.
Electronic searches
We searched the following electronic databases with the help of the Trials Search Co‐ordinator of the Cochrane Developmental, Psychosocial and Learning Problems Group (CDPLPG).
Cochrane Central Register of Controlled Trials (CENTRAL) (2010, Issue 1);
MEDLINE (from 1966 to Jan 2010);
OLDMEDLINE (pre 1966);
EMBASE from 1980 to 2010 week 5;
CINAHL from 1982 to Jan 2010;
the Campbell Collaboration SPECTR (C2‐SPECTR) database to Jan 2010;
Educational Resources Information Center (ERIC) to Jan 2010;
Virtual Health Library (VHL) in BIREME: Pan American Health Organization (PAHO) Specialized Center;
LILACS (Latin American Health Sciences Literature) to Jan 2010;
PsycINFO (psychological literature) to Feb 2010 week 2; and
UMI Dissertation Express.
We searched the following complementary and alternative medicine specific databases to January 2010:
CAM on PubMed;
Cochrane Complementary and Alternative Medicine field;
Complementary Medicine Resources for Health Professionals and Researchers;
Complementary and Alternative Medicine Specialist Library in the National Library for Health (supported by the NHS); and
Complementary and Alternative Therapies databases of Bandolier.
We also searched the following sources to January 2010:
OpenSIGLE ‐ System for Information on Grey Literature in Europe;
Health Services/Technology Assessment Text (HSTAT) database;
Informit Databases: Humanities and Social Sciences Collection, Australia;
English Databases of the Japan Science and Technology Agency (JST); and
Research database of Thailand psychiatry and mental health and Thai Thesis Online.
The search strategies for these databases are shown in the appendices two to seven (see Appendices).
Searching other resources
We carried out a search of conference proceedings at ISI Proceedings from 1990 to January 2010 and searched for relevant studies cited in book chapters on the treatment of ADHD.
Personal communication
We consulted the authors of the included studies and experts in the fields to find out whether they knew of any published or unpublished RCTs/ CCTs of meditation therapy and ADHD, which have not yet been identified. We contacted persons and organizations whose work relates to meditation (i.e. Associacion de Medicinas Complementarias (AMC), the National Center for Complementary and Alternative Medicine (NCCAM), Sat Bir Sinah Khalas). We contacted religious/spiritual organizations around the world (internet web sites were extensively searched) to find out whether they had conducted or knew of the application of meditation in ADHD.
We also contacted worldwide organizations with resources for ADHD: Attention‐Deficit Disorder Association, Attention‐Deficit Disorder Resources; ADHD Support, Children and Adults with Attention‐Deficit/Hyperactivity Disorder (CHADD), the National Resource Center on AD/HD (NRC), Children and Adults with Attention‐Deficit Disorders, Learning Disabilities Association of America, the Attention‐Deficit Resource Network (ADRN) and the National Center for Girls and Women with AD/HD.
Ongoing trials
We sought ongoing trials by searching the metaRegister of Controlled Trials (mRCT) ; Health Services Research Projects in Progress (HSRProj); the National Centre for Complementary and Alternative Medicine sponsored trials; www.ClinicalTrials.gov; UKCRN Clinical Research Portfolio and the Trials Register of Promoting Health Interventions (TRoPHI). All trial registry were search to January 2010.
We checked the reference lists of all relevant studies for further references.
Data collection and analysis
Selection of studies
KT and WC independently screened the titles and abstracts obtained by the search strategies against the eligibility criteria stated above. KT and WC verified study eligibility before data extraction with no disagreement on inclusion/exclusion decisions. For articles that appeared to be eligible RCTs, we obtained the full articles and inspected these to assess their relevance, based on the pre‐defined inclusion criteria.
Data extraction and management
Two authors independently extracted data using a pre‐designed data collection form, which was saved electronically. Any unpublished information, if used, was recorded and coded with a specific remark. We contacted authors either by e‐mail or telephone call to obtain any missing data. KT entered all relevant data into RevMan 5 (RevMan 2008) and NC checked data for correctness. The reliability of data extraction and data entry were examined throughout the process.
For cross‐over designs, we extracted all data but, because of the strong carry‐over effect of meditation, we used only data from the first phase of study in our analyses. The data from the second phase after crossing over were described in the 'Characteristics of included studies' table and recorded in an additional table.
Assessment of risk of bias in included studies
We assessed risk of bias in the included studies using The Cochrane Collaboration's tool, which is based on multiple domain evaluation (Higgins 2008). There are six domains as follows:
1. Sequence generation
Was the allocation sequence adequately generated?
2. Allocation concealment
Was allocation adequately concealed?
3. Blinding of participants, personnel, outcome assessors
Was knowledge of the allocated intervention adequately prevented during the study?
4. Incomplete outcome data
Were incomplete outcome data adequately addressed?
5. Selective outcome reporting
Are reports of the study free of suggestion of selective outcome reporting?
6. Others sources of bias
Was the study apparently free of other problems that could put it at a high risk of bias?
The review authors' judgments involved answering these questions for each entry, i.e. 'Yes' indicates low risk of bias; 'No' indicates high risk of bias; 'Unclear' indicates insufficient detail is reported or the risk of bias is unknown.
The risk of bias is presented in the 'Risk of bias' table with two additional figures: a 'Risk of bias graph' (Figure 1) and a 'Risk of bias summary' (Figure 2).
Figure 1.
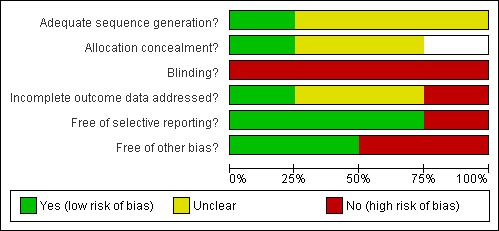
Methodological quality graph: review authors' judgments about each methodological quality item presented as percentages across all included studies.
Figure 2.
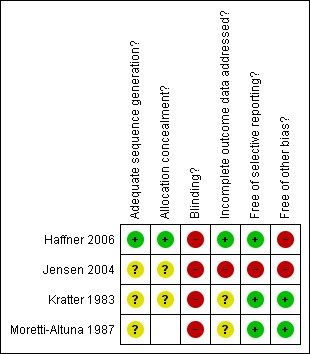
Methodological quality summary: review authors' judgments about each methodological quality item for each included study.
To determine selective outcome reporting we planned to compare the study with its protocol, which might be registered in trial registries, however no included studies were registered in any trial registries. Two out of four included studies, however, came from PhD dissertations which had an extensive published report which could be used to determine the completeness of reporting indirectly (Kratter 1983; Moretti‐Altuna 1987).
The summary assessment of risk of bias used the authors' judgment for primary outcomes (symptoms of ADHD, quantitative laboratory assessment measures of ADHD symptoms, overall incidence/severity of the problem behaviors) both within and across studies.
Disagreements were discussed with a third author (WC) and resolved through consensus.
Measures of treatment effect
Dichotomous outcomes
Dichotomous outcomes were not presented in any of the included studies.
Continuous outcomes
We analyzed the endpoint score (because the change score data were not reported in the included studies) in RevMan 5 using mean differences (MD) and their 95% confidence intervals (CI). When considering the skewed data, we compared the mean to the standard deviation. If the mean was smaller than twice the standard deviation the data were probably skewed (Altman 1996). We present the skewed data in Additional table.
Unit of analysis issues
In trials of cross‐over design (two included studies), because of the strong carry‐over effect of meditation, we only used the data from phase one before crossing over in meta‐analysis. The additional data were described in the 'Characteristics of included studies' table.
In a study with multiple treatment groups (meditation versus drug versus standard treatment control), we carried out the analysis for each pair between meditation and other treatments.
No cluster‐randomized trials were identified.
Dealing with missing data
All of the included studies for this review used per protocol analysis. The reasons for missing data were clarified by the study authors and were described in the Notes sections of the 'Characteristics of included studies' table.
Assessment of heterogeneity
This review included one trial for each comparison. We therefore did not conduct assessment of heterogeneity. We have provided full methods for assessment of heterogeneity for future updates of this review in Appendix 1.
Assessment of reporting biases
If possible, we will use a funnel plot (Egger 1997; Light 1984) to determine potential publication bias.
The authors dealt with selective outcome reporting by searching for the original protocols for each included study in trial registries and comparing these (where available) with the list of outcomes in the methods section of the final report. In cases where there is a suspicion of selective outcome reporting, we contacted the study authors. The assessment of risk of bias due to selective reporting of outcome was made for each study as a whole.
This review included one trial for each comparison. We therefore did not create funnel plots to assess publication bias. For future updates of this review, we have provided full methods for assessment of reporting biases in Appendix 1.
Any other types of bias encountered in each study are reported in the Results and Discussion.
Data synthesis
Each comparison had only one included trial and had continuous outcomes. We therefore calculated MDs with their 95% CIs.
Subgroup analysis and investigation of heterogeneity
We did not conduct subgroup analysis because there was only one included trial for each comparison.
Sensitivity analysis
We did not conduct sensitivity analysis due to the limited number of included studies in the review.
Results
Description of studies
Results of the search
We carried out extensive searches, as described in 'Search methods for identification of studies'. We searched the electronic databases from their inception without language restrictions. We checked the titles from the preliminary search results and there were 17 potentially relevant studies at this stage. After checking the abstracts, we excluded 7 studies that were obviously irrelevant to the review. We obtained the full text of the 11 potentially relevant studies which required further clarification. Four studies met the eligibility criteria while 7 studies were put into the excluded studies category. All included studies were carried out by different research teams between 1983 and 2006. We contacted the first authors of three of the included studies to ask for additional data and details of their studies. One author (Kratter 1983) could not be contacted. One author (Haffner 2006) sent an original article in German and an English translated version.
Included studies
Settings
Two of the four studies included in this review were carried out in the USA. Both studies were dissertations submitted to the faculty of the Department of Psychology at St. John's University, New York (Kratter 1983; Moretti‐Altuna 1987). Haffner 2006 was carried out in Germany and Jensen 2004 was carried out in Australia. Only one study (Kratter 1983) mentioned the meditation room, which was a quiet room with low lighting and comfortable chairs. Both studies of mind‐based meditation (Kratter 1983; Moretti‐Altuna 1987) used a padded, straight‐back chair. Haffner 2006 and Jensen 2004 did not give details about their settings. None of the studies reported the time of year of the study, therefore it is unclear whether participants were in school or on holiday/vacation during the trials.
Participants
All participants were children with ADHD, with an age range between six and 13 years old. Three of the studies indicated that participants must be boys in the inclusion criteria; only (Haffner 2006) included girls. Three studies reported that they used the DSM diagnostic system (DSM‐III, DSM‐IV). One study, which was carried out in Germany (Haffner 2006), used the Diagnostic System for Psychic Disorders in Childhood and Adolescence, which corresponded to ICD‐10 diagnosis. Jensen 2004 used Conners’ Parent Rating Scales: Long (CPRS: R (L)) that demonstrated scores (over 70 t‐score) to confirm the diagnosis of ADHD in all participants. Moretti‐Altuna 1987 used a multidisciplinary intake committee to confirm the diagnosis. In the other two studies (Haffner 2006; Kratter 1983) no diagnostic re‐confirmation procedures were used.
Interventions
Two studies used mantra meditation, which is mind‐based. Kratter 1983 used the word "Ahnam", a Sanskrit word which means "nameless". Moretti‐Altuna 1987 used "One", with the aim that by repeating the word the participants would learn to focus and re‐focus their attention. These techniques were adapted from the well‐known concentrative meditation developed by Benson 1975 and Carrington 1975, which has some roots in the Hindu religion. Apart from the different mantra used in their studies, other aspects of the intervention (duration, frequency, sitting position, passive attitude) were almost the same.
Haffner 2006 and Jensen 2004 used Hatha yoga, which is more physical‐based. However, Jensen 2004 also used a visualization technique to accompany Hatha yoga and Haffner 2006 used breathing meditation combined with postures. They claimed that their yoga program was a standardized program and developed by a yoga instructor. The yoga program consisted of multiple components (respiratory, postural, relaxation concentration training). The details of each program are described below.
Concerning the qualification and skills of the meditation instructors, only Haffner 2006 used a well‐trained yoga teacher while in the other three included studies the subjects were taught by the investigators themselves.
The intervention program ranged from four weeks (Kratter 1983; Moretti‐Altuna 1987), to eight weeks (Haffner 2006) to 20 weeks (Jensen 2004). The frequency of visits varied from one session per week (Jensen 2004) to three sessions per week (Haffner 2006; Kratter 1983; Moretti‐Altuna 1987). Some studies used the parents to assist and supervise their children while practicing meditation at home (Jensen 2004; Kratter 1983; Moretti‐Altuna 1987), while Haffner 2006 just let the children practice yoga freely on their own at home or at school during the intervention period.
The intensity of meditation is determined from the duration of practice. Haffner 2006 and Jensen 2004 used a one‐hour training session but do not mention the exact time spent in meditation. Kratter 1983 and Moretti‐Altuna 1987 state that the actual meditation duration was gradually increased from one minute to eight minutes by the end of the four‐week training period.
Comparator/control group
Haffner 2006 and Jensen 2004 compared yoga versus co‐operative games/activities. Medicated participants were unevenly distributed between intervention groups. In Haffner 2006 five out of nine of the yoga group were medicated while three out of 11 of the control group were medicated.
Kratter 1983 compared three intervention groups: meditation training versus relaxation training versus waiting list control. The medicated participants were distributed evenly between treatment groups using a modified randomization method.
Moretti‐Altuna 1987 compared meditation training versus drug therapy versus standard therapy control. Only participants in the drug therapy group received medication.
Outcome measures
The reported outcomes were:
1. Validated outcome scales rated by parents/teacher, which reflected the core symptoms of ADHD.
Fremdbeurteilungsbogen für hyperkinetische Störungen (FBB‐HKS), used in Haffner 2006.
Conners' Parent (CPRS–R:L) Teacher (CTRS–R:L) Rating Scales – Revised: Long (Conners 1997), used in Jensen 2004.
Abbreviated Parent‐Teacher Questionnaire (PTQ) (Conners 1973), used in Kratter 1983 and Moretti‐Altuna 1987.
Werry‐Weiss‐Peters Activity Scale (WWPAS) (Werry 1968), used in Kratter 1983 and Moretti‐Altuna 1987.
Nowicki‐Strickland Locus of Control Scale (LCS), used in Kratter 1983.
2. Psychological testing to measure the symptoms profile of ADHD.
Dortmund Attention Test (DAT), used in Haffner 2006.
Test of Variables of Attention (TOVA) (Greenburg 1991), used in Jensen 2004.
Matching Familiar Figure Test (MFFT) (Kagan 1996), used in Kratter 1983 and Moretti‐Altuna 1987.
Fruit Distraction Test (FDT) (Santostefano 1978), used in Kratter 1983 and Moretti‐Altuna 1987.
The Children's Embedded Figures Test (CEFT) (Karp 1963), used in Moretti‐Altuna 1987.
3. Psychophysiological measurements.
Motion logger ‐ Actigraph, used in Jensen 2004.
Study design
Haffner 2006 used a cross‐over design in which the participants in the yoga group and the control (motor exercise) group crossed over to the other treatment after eight weeks, with a six‐week break (wash‐out period). As stated earlier, to prevent carry‐over effects, we have only included the data from the first phase of each study in the analysis. Data from the second phase after cross‐over are recorded in Tables. Jensen 2004 also stated that the study had a "randomized cross‐over design", but only the participants in the control group were allowed to move to the yoga group; the yoga group did not cross over to the control group. This design cannot therefore be described as cross‐over. The study is downgraded from RCT to only a before‐after design when the study authors pooled all data together.
Excluded studies
There were 7 excluded studies. Four were carried out in the USA (Evans 2007; Kratter 1982; Peck 2005; Zylowska 2008), one was from Australia (Harrison 2004) one from Thailand (Hassasiri 2002) and one was carried out in Iran but get published in India (Abadi 2008) . One of the excluded studies involved development of an audio program for the treatment of adult ADHD and used a group of experts to give opinions about the program (Evans 2007). Three used a before‐after design which did not have a control group (Harrison 2004; Hassasiri 2002; Zylowska 2008). One study (Peck 2005) was excluded due to the participants not having been diagnosed with ADHD. We also excluded one duplicate report (Kratter 1982). One study(Abadi 2008) have a control group but did not mention about the randomization.
Risk of bias in included studies
Systematic biases directly affected the validity of the included studies. See also the 'Risk of bias' graph (Figure 1) and 'Risk of bias' summary (Figure 2).
Allocation
Only one of the four included studies reported the method of randomization which was the use of drawing lots (Haffner 2006). The other three studies just mentioned randomization without giving any details in their methods. The method of allocation concealment was not reported in any trial but because Haffner 2006 used the drawing of lots we have assumed that allocation concealment automatically occurred because the sequence cannot be known in advance. In one trial (Jensen 2004) the process of randomization was terminated when five participants from the control group were allowed to move to the treatment group after 20 weeks. Allocation concealment was therefore not carried out in this trial. In Kratter 1983 the randomization method was modified to equalize the medicated children evenly between each group. This modification made the study potentially more susceptible to bias, as randomization could not guarantee the distribution of confounding factors and allocation concealment was not adequate.
Moretti‐Altuna 1987 did not give details of randomization methods and we therefore judged the adequacy of randomization and allocation concealment to be 'Unclear'.
Blinding
Only the blinding of of raters/assessors is possible in such trials. However, no trials reported blinding of the raters/assessors.
Incomplete outcome data
No studies in the included studies carried out an intention‐to‐treat analysis. Only patients who completed the entire trial were analyzed by per‐protocol analysis.
In Haffner 2006 one nine‐year old boy left the study because of a change of residence during the 21st week. The reason why the child left the study was adequately described and it would not have had a clinically relevant impact on the observed effect size.
Jensen 2004 reported the number of boys who began the trial (n = 16) but only data for 14 boys were used in analysis. No reasons for drop‐outs were described.
Kratter 1983 reported that 24 boys participated the study but did not mention the attrition of participants at the end of the study. Moreover, the analysis table did not give the number of participants left in each group, therefore the data were not used in meta‐analysis but are shown in Table 5.
Table 1.
Data from Kratter 1983
| Outcome | Meditation | Relaxation |
Waiting list Control |
||||||
| Mean | SD | n | Mean | SD | n | Mean | SD | n | |
| MFFT latency scores |
12.412 | 6.675 | ‐ | 10.462 | 3.986 | ‐ | 10.962 | 5.125 | ‐ |
| FDT card 1 Latency |
40.312 | 9.051 | ‐ | 41.687 | 8.062 | ‐ | 42.375 | 10.905 | ‐ |
| FDT card 2 Latency |
44.812 | 10.261 | ‐ | 49.500 | 14.310 | ‐ | 49.687 | 13.905 | ‐ |
| FDT card 3 Latency |
45.687 | 8.856 | ‐ | 46.625 | 8.895 | ‐ | 53.375 | 16.153 | ‐ |
| FDT card 4 Latency |
70.750 | 8.912 | ‐ | 83.250 | 24.036 | ‐ | 83.437 | 20.576 | ‐ |
| LCS scores | 14.000 | 3.295 | ‐ | 18.875 | 4.824 | ‐ | 16.000 | 5.555 | ‐ |
| TRS scores | 15.625 | 8.141 | ‐ | 16.625 | 8.158 | ‐ | 13.500 | 6.024 | ‐ |
| PTQ scores | 14.250 | 6.840 | ‐ | 15.375 | 2.774 | ‐ | 18.625 | 1.061 | ‐ |
| WWPAS | 25.000 | 7.709 | ‐ | 26.375 | 10.169 | ‐ | 28.125 | 7.827 | ‐ |
No N in each group provided.
FDT = Fruit Distraction Test LCS = Nowicki‐Strickland Locus of Control Scale MFFT = Matching Familiar Figure Test PTQ = Parent‐Teacher Questionnaire TRS = Teacher Rating Scale WWPAS = Werry‐Weiss‐Peters Activity Scale
In Moretti‐Altuna 1987 there was no mention of the number of enrolled participants at the beginning of the trial. The authors reported that 23 boys participated in the trial and used this number in the final analysis. Completeness of outcome data is therefore doubtful.
Selective reporting
None of the four included studies appeared in trial registries and therefore we were not able to obtain protocols for these studies. Pre‐specified outcomes were therefore not known and it is difficult to determine whether outcomes were omitted from reporting.
Haffner 2006, Kratter 1983 and Moretti‐Altuna 1987 reported all the outcomes specified in their Methods section. Moreover, Kratter 1983 and Moretti‐Altuna 1987 were dissertations which should guarantee the completeness of reporting.
Jensen 2004 used an Actigraph motion logger (a portable electronic activity monitor designed to be worn on the wrist, waist or ankle) and reported that "there were many technical problems encountered mainly due to their use in a naturalistic setting. On occasions they were damaged, stopped recording data, or failed to be activated at set times. As a consequence an incomplete set of data was collected. Due to these problems, data were deemed unreliable and were discarded." Even though the study authors had addressed the reason for non‐reported outcomes, we still judged that this outcome was selectively reported.
Other potential sources of bias
In Haffner 2006 more boys in the yoga group received medication (five of nine) than in the exercise group (three of 11). This unequal co‐intervention could have substantial effects. Using a cross‐over design in a trial of an intervention which needs practicing by the participants means it is difficult to discard the carry‐over effect during phase two of the trial. Even during phase one (before crossing over) participants in both intervention arms might have some expectations of the treatment effects of the next intervention.
In Jensen 2004 there were significant differences between the control and yoga groups' pretest sub‐scale scores on almost all Conners' Rating Scales for both parents and teachers.
Effects of interventions
We collected data for three comparisons from the included studies which were non‐skewed outcome data to put into the analyses and present in the 'Summary of Findings' table: this was the teacher rating ADHD overall scale . The distraction test was considered to be the intermediate outcomes which reflected psychological state but might not directly related to behavior of the child.
The effects of interventions are compared in a pair‐wise manner as follows.
Meditation therapy versus drug therapy for ADHD
One study (Moretti‐Altuna 1987) compared mantra meditation and drug therapy for ADHD. There were six outcomes which are considered to be the primary outcomes in this review. The study provided both endpoint scores with standard deviations (SD) and change scores with SD for each outcome after four weeks of treatment. The endpoint scores were selected for use in analysis. There was no statistically significant difference between the meditation therapy group and the drug therapy group in the teacher rating ADHD overall scale (MD ‐2.72, 95% CI ‐8.49 to 3.05, 15 patients, see Figure 3). In addition, we found that five outcomes had skewed data (see Table 6).
Table 2.
Meditation therapy versus drug therapy (skewed data) (Moretti‐Altuna 1987)
| Outcome | Study | Meditation | Drug | ||||
| Mean | SD | Total | Mean | SD | Total | ||
| 1. Parent rating ADHD overall scale | Moretti‐Altuna 1987 | 15.78 | 8.74 | 9 | 18.17 | 7.39 | 6 |
| 2. Parent rating activity level scale | Moretti‐Altuna 1987 | 28.0 | 16.87 | 9 | 30.83 | 22.31 | 6 |
| 3. Impulsivity test (error scores) | Moretti‐Altuna 1987 | 12.22 | 8.03 | 9 | 17.00 | 4.98 | 6 |
| 4. Distraction test | Moretti‐Altuna 1987 | 247.72 | 117.77 | 9 | 238.25 | 123.07 | 6 |
| 5. Attention test | Moretti‐Altuna 1987 | 14.11 | 6.09 | 9 | 11.0 | 5.76 | 6 |
Meditation therapy versus standard treatment without drugs for ADHD
Moretti‐Altuna 1987 also compared mantra meditation and standard treatment without drugs for ADHD using the same outcome measures as the above comparison. The analysis was done by calculating the endpoint scores after four weeks of treatment. There was no statistically significant difference between the meditation therapy group and the standard therapy group in the teacher rating ADHD scale (MD ‐0.52, 95% CI ‐5.88 to 4.84, 17 patients, see Figure 4). In the same way there was no statistically significant difference between the meditation therapy group and the standard therapy group in the distraction test (MD ‐8.34, 95% CI ‐107.05 to 90.37, 17 patients, see Figure 5). Skewed data for this comparison are shown in Table 7.
Table 3.
Meditation therapy versus standard treatment without drug (Moretti‐Altuna 1987)
| Outcome | Study | Meditation | Standard therapy control | ||||
| Mean | SD | Total | Mean | SD | Total | ||
| 1. Parent rating ADHD scale | Moretti‐Altuna 1987 | 15.78 | 8.74 | 9 | 19.0 | 7.29 | 8 |
| 2. Parent rating activity level scale | Moretti‐Altuna 1987 | 28.0 | 16.87 | 9 | 30.75 | 14.25 | 8 |
| 3. Attention test | Moretti‐Altuna 1987 | 14.11 | 6.09 | 9 | 12.13 | 7.36 | 8 |
| 4. Impulsivity test (error scores) | Moretti‐Altuna 1987 | 12.22 | 8.03 | 9 | 17.50 | 9.78 | 8 |
Meditation therapy versus relaxation training versus waiting list controls with drugs for ADHD
In Kratter 1983 there were three intervention groups. Mantra meditation was compared to relaxation training and to waiting list controls with drugs. The three groups had an equal number of medicated participants. There were five outcomes which are considered to be the primary outcomes in this review. The study provided both endpoint scores with SD and change scores with SD for each outcome. The data are shown in Table 5. From the published report, the authors used ANOVA to analyze the treatment effects. The findings were that mantra meditation as well as relaxation training significantly decreased impulsivity and improved behavior at home when rated by the parents. Only the meditation group improved in the selective deployment of attention, which was claimed as an essential aspect of meditation training. The sense of internal control and classroom behavior were not improved in any treatment group.
Hatha yoga versus non‐specific physical exercise for ADHD
There were two studies which compared Hatha yoga and non‐specific physical exercise for ADHD (Haffner 2006; Jensen 2004). However, only Haffner 2006 provided data for this comparison.
In the study by Jensen 2004, the authors did not provide the data from truly randomized participants. In the published report analysis the authors combine the data from true randomized participants with data from the control group who moved to the treatment group. Mixing the participants from the two groups together ruined the randomization effects. We decided to discard these data from analysis, but the data are shown in Table 8.
Table 4.
Yoga versus control for ADHD (Jensen 2004)
| Conners' Parent Rating Scales ‐ Revised: Long (Conners 1997) (Figure 6) |
| Conners' Teacher Rating Scale ‐ Revised: Long (Conners 1997) (Figure 7) |
| Test of Variables of Attention (TOV) (Greenburg 1991) (Figure 8) |
To eliminate the carry‐over effect in Haffner 2006 only the data from the first phase of trial were extracted and put into the comparison for meta‐analysis. There were five outcomes for this comparison but their data were skewed (see Table 9). The data from phase two of the trial (after crossing over) are shown in Table 10.
Table 5.
Hatha yoga versus non‐specific physical exercise (skewed data)
| Outcome | Study | Hatha yoga | Non‐specific exercises | ||||
| Mean | SD | Total | Mean | SD | Total | ||
| 1. Parent rating ADHD overall scale | Haffner 2006 | 0.93 | 0.53 | 8 | 1.47 | 0.7 | 11 |
| 2. Parent rating attention‐deficit | Haffner 2006 | 0.92 | 0.5 | 8 | 1.65 | 0.65 | 11 |
| 3. Parent rating hyperactivity | Haffner 2006 | 0.75 | 0.57 | 8 | 1.29 | 0.84 | 11 |
| 4. Parent rating impulsivity | Haffner 2006 | 1.26 | 0.67 | 8 | 1.39 | 0.88 | 11 |
| 5. Attention test | Haffner 2006 | 8.37 | 1.8 | 8 | 4.36 | 3.1 | 11 |
Table 6.
Hatha yoga versus non‐specific exercise for ADHD (phase 2: after crossing over) (Haffner 2006)
| Measurements |
Hatha Yoga N = 11 Mean (SD) |
Exercise N = 8 Mean (SD) |
| DAT | 9.81(1.5) | 7.0(2.7) |
| FBB‐HKS | — | — |
| Total scale | 1.18(0.76) | 1.03(0.65) |
| Attention‐deficit | 1.34(0.73) | 0.9(0.6) |
| Hyperactivity | 1.07(0.82) | 0.86(0.72) |
| Impulsiveness | 1.02(0.88) | 1.61(0.79) |
DAT = Dortmund Attention Test FBB‐HKS = Fremdbeurteilungsbogen für hyperkinetische Störungen (FBB‐HKS): a rating scale for parents, teachers and educators
Discussion
Summary of main results
Four studies were included in this review. Two studies were dissertations submitted to the faculty of the Department of Psychology at St. John's University, New York in 1983 and 1987 (Kratter 1983; Moretti‐Altuna 1987). One study was carried out in Sydney, Australia (Jensen 2004) and the other in Heidelburg, Germany (Haffner 2006). The first randomized controlled trial using meditation for ADHD was the study of Kratter 1983, which took place 25 years ago. Further studies have followed Kratter's trial but many of these have used a before‐after design which has several methodological limitations. These studies were excluded from the review (Harrison 2004; Hassasiri 2002; Zylowska 2008). Haffner 2006, Jensen 2004 and Moretti‐Altuna 1987 were randomized controlled trials with different comparators: 1) meditation therapy versus drug therapy, 2) meditation therapy versus standard treatment without drugs, 3) meditation therapy versus relaxation training versus waiting list controls with drugs and 4) Hatha yoga versus non‐specific physical exercise.
The type of meditation used in these trials can be differentiated into two groups according to the different characteristics of meditation. Mind‐based meditation (mantra meditation) was used in the Kratter 1983 and Moretti‐Altuna 1987 studies. Physical‐based meditation was used in Jensen 2004 and Haffner 2006. Mind‐based meditation emphasizes the cognitive process which focuses on the use of selective deployment of attention: the participants learned to focus and re‐focus their attention (Kratter 1983). Physical‐based meditation (Hatha yoga, moving meditation) focuses on behavioral control. However, due to the complexity of body‐mind interaction, and the concept of holistic approach, it is hard to differentiate body and mind and each meditation technique usually incorporates both components together. Due to the variety of theories and practices of meditation the inclusion of different techniques under the same umbrella of meditation is inappropriate. Five broad categories of meditation practice were identified by a group of experts using modified Delphi methodology: mantra meditation (comprising the Transcendental Meditation® technique (TM®), Relaxation Response (RR) and Clinically Standardized Meditation (CSM)), mindfulness meditation (comprising Vipassana, Zen Buddhist meditation, Mindfulness‐based Stress Reduction (MBSR) and Mindfulness‐based Cognitive Therapy (MBCT)), yoga, Tai Chi and Qi Gong (Ospina 2007)). The classifications in this system are more suited to defining the broad range and variety of meditation than the previously used classification (concentrative meditation and mindfulness meditation). The four included studies in this review fell into the categories of mantra meditation and yoga by this classification.
Only Haffner 2006 used a well‐trained yoga teacher while participants in Jensen 2004, Kratter 1983 and Moretti‐Altuna 1987 were taught by the investigators themselves. Qualification and experience in teaching meditation are important to guarantee proper teaching. When applying meditation therapy in clinical settings, the knowledge, attitude and skill of the therapist should be considered (Krisanaprakornkit 2006).
There were only two studies from which the data were appropriate for meta‐analysis. Due to the limited number of studies, small sample size in each trial, apparent risk of bias and skew‐ness of data we found no consistent evidence that meditation (either mind‐based or physical‐based) had a significant effect on core ADHD symptoms or psychological tests of attention, impulsivity and distraction. Mind‐based meditation did not yield any significantly different effects compared to drugs and standard therapy controls. While physical‐based meditation (Hatha yoga) showed some positive effects (parent rating attention‐deficit, attention test), it did not show consistent results.
All of the included studies had differences in the number of meditation sessions and the amount and quality of home practice, which could affect the treatment effects. Some studies used the parents to assist and supervise their children while practicing meditation at home (Jensen 2004; Kratter 1983; Moretti‐Altuna 1987). Haffner 2006 just let the children practice yoga freely on their own at home, at school and during lessons. Therefore the intensity of practice differed widely among participants and studies. There were no descriptions of monitoring of practice at home in any studies, therefore the quality and quantity of self‐practice could not be guaranteed. This might be affected the results of each studies.
Data for the side effects of meditation and quality of life were not reported in any trials. Randomized trials usually focus on intended effects and focus less on possible adverse effects. Data on adverse effects are often sparse but the absence of information does not mean that the intervention is safe (Higgins 2008). The issue of side effects should therefore be addressed in any future meditation trials.
There is insufficient evidence to support the effectiveness of any types of meditation for ADHD at present given that only four randomized controlled trials have been carried out, and all were relatively small in size and limited in design, with inconsistent results across the outcomes.
Overall completeness and applicability of evidence
We considered the parent rating, teacher rating and self‐rating ADHD symptoms scales to be the most important outcomes for patients. Quantitative laboratory assessment measures of ADHD symptoms, psychological testing etc. are surrogate outcomes which are less important. In the included studies all the participants were children with ADHD, therefore a self‐rating scale is not necessary to measure outcomes because it is difficult for school‐age children to rate their symptoms accurately.
No studies gave details of adverse effects, but this is an important outcome to be considered in every study, especially in trials in children. Despite this, a well‐structured meditation program is considered safe and is promoted for children in many settings, including schools (Helen 2004).
In our protocol for this review we defined 'Overall severity of problem behaviors' and 'Quality of life' as outcome measures because these outcomes provide a broader perspective on the patient's life rather than merely focusing on symptoms. Meditation can not only improve attention but also the quality of mind (calmness, equanimity, contentment), all of which can affect the life of a patient as a whole (Ospina 2007). Outcomes which are measured at the end of a program cannot detect intermediate‐term and long‐term changes in personality profile. Data will be more complete if trials can follow up outcomes for six months to 12 months afterwards.
Due to the lack of consistent evidence to support the use of meditation for ADHD in the present review, we cannot comment on applicability and generalizability at this time. In some countries, for example Thailand, meditation is accepted as a means to improve attention, temperament, discipline, school performance, character, morals and for religious purposes (Krisanaprakornkit 2006). The included studies were carried out in the USA, Germany and Australia. As the effects of globalization and the holistic view of health expand, meditation may become more accepted and widely used in the clinical setting. Therefore, if the effectiveness of meditation can be established, it may be used more widely as a therapy in the future.
Quality of the evidence
In a Cochrane Review the quality of evidence reflects the extent to which we are confident that an estimate of the effect is correct. We therefore rate the quality of evidence for each outcome separately.
Two included studies were dissertations submitted to the faculty of the Department of Psychology at St. John's University, New York in 1983 and 1987 (Kratter 1983; Moretti‐Altuna 1987). We have assumed that the dissertations were generally supervised and verified by the committee. The inclusion of dissertations may mean more balanced results as they are less likely to overestimate treatment effects, as can occur in published trials (McLeod 2004).
Trial quality is discussed in the 'Assessment of risk of bias in included studies' section, with graphical presentations in Figure 1 and Figure 2. We then assessed the risk of bias for an outcome across studies using the GRADE system. We judged the quality of the evidence by assessing limitations in design, inconsistency, indirectness, imprecision and publication bias.
As such a limited number of trials was found, we suspect the possibility of publication bias. Concentrative meditation (mantra meditation) was introduced to the West during the 1960s and many pioneers in the field have developed modified forms of meditation suitable for use in the clinical setting, for example the 'relaxation response' of Herbert Benson (Bensonian meditation) (Benson 1975). Mindfulness meditation has emerged as a new approach to stress reduction and is an important innovation in the treatment of psychiatric disorders (Baer 2003). The Mindfulness‐based Stress Reduction Program (Kabat‐Zinn 1992) has subsequently been researched in ADHD adults and adolescents (Zylowska 2008). A Google search results in more than 1,170,000 hits for "meditation AND ADHD". This issue has also appeared in the news (e.g. 'Meditation helps kids with ADHD' (Helen 2004)) and meditation has gained acceptability in many primary and junior school in England (Eliaz 2008). Another reason for the small number of studies might be that meditation trials are less supported than medication trials, which may be funded by drug companies.
The graphical risk of bias presentations (Figure 1; Figure 2) show the serious limitations in design (high risk of bias) in the included studies overall. Randomization methods are not mentioned, therefore we cannot assess the adequacy of allocation concealment. Only the study of Kratter 1983 described the use of the drawing of lots, which automatically concealed the allocation. There was no mention of blinding. In Haffner 2006, the yoga instructors themselves carried out the assessment of the participants in both the yoga and control group; detection bias was therefore inevitable. Only Haffner 2006 described the reason for drop‐out of one participant (moved home). The attrition rate of the other three studies was unclear or not described. The drop‐out rate might be related to adverse effects or to some discomfort with meditation.
The consistency of results across studies could not be determined because there was only one study to provide data for each comparison. However, when checking the direction of the result in any one study the inconsistency of outcomes in each study was obvious. Each study measured many outcomes. Some outcomes were considered to be important, while others were surrogate outcomes (e.g. attention test, distractibility test). When many outcomes are used in one study this will increase the possibility of a significant difference which occurred by chance. The authors may also selectively accentuate the significance of positive outcomes while omitting to clarify the negative outcomes (reporting bias).
Most of the means differences had wide confidence intervals reflecting the small sample size, differences in baseline characteristics of study samples and different treatment effects in individuals.
No studies had problems of indirectness of evidence.
We therefore summarized quality for each comparison as follows.
Meditation therapy compared to drug therapy for attention‐deficit/hyperactivity disorder
The quality of evidence was "very low" according to the GRADE classification for 'Teacher rating ADHD overall scale' (see Summary of findings table 1).
Meditation therapy compared to standard treatment without drug for attention‐deficit/hyperactivity disorder
The quality of evidence was "very low" according to the GRADE classification for 'Teacher rating ADHD overall scale' (see Summary of findings table 2).
Potential biases in the review process
Due to limited access our literature searching could not cover some sources, such as literature in Chinese.
Agreements and disagreements with other studies or reviews
Meditation for ADHD has been reviewed as a psychological treatment along with other psychosocial interventions. At this time there is no specific systematic review of meditation for ADHD only. Arnold 2001 was a narrative review on alternative treatment for adults with ADHD. This review included the two studies of Kratter 1983 and Moretti‐Altuna 1987, which were carried out in children with ADHD. The authors concluded that meditation showed some benefit and warrants further study for both children and adults. The recent narrative review by Greydanus 2007 emphasized medication and meditation was only mentioned under the heading of psychological management, which included many types of psychological interventions (psychotherapy, cognitive behavioral therapy, support groups, parent training, educator/teacher training, biofeedback, meditation and social skills training). The authors stated that empirical evidence regarding these interventions was inconsistent (Greydanus 2007). These narrative reviews commonly failed to assess the methodological quality of the primary studies, therefore the results tend to overestimate the effects.
Authors' conclusions
There is insufficient evidence to draw conclusions about the effectiveness of any types of meditation for attention‐deficit/hyperactivity disorder (ADHD). The adverse effects of meditation in children with ADHD are unknown.
There is a lack of evidence to support the effectiveness of meditation for ADHD. This review has highlighted the need for further research. Meditation therapy research protocols need to be rigorous in design and delivery, and use standardized meditation therapy programs which can be replicated by other researchers. The operational definition of meditation techniques used should be specified and relate to ADHD core symptoms. The trainers should be skilled or be experts in the meditation methods used. The monitoring of meditation practice at home in addition to the therapy sessions is a crucial element of adherence. The involvement of parents in practice should be considered and controlled. The concomitant use of medication should be distributed evenly between comparison groups. All the outcomes should be validated and described, including adverse effects. We plan to update this review within 24 months to incorporate any new studies and respond to any comments or criticisms.
Acknowledgements
Professor Dr. Pisake Lumbiganon for initiating and supporting this review.
Appendices
Appendix 1. Methods for data analysis in future updates of this review
Data analysis
Measures of treatment effect
Dichotomous outcomes
We will pool dichotomous outcomes using the risk ratio (RR) as the summary statistic. In cases where the numbers of participants and numbers of events are not available, but results calculated from them are (risk ratio, odds ratio, adjusted odds ratio), we will include the data in meta‐analyses only if they are accompanied by measures of uncertainty such as 95% confidence intervals or exact P values. We will then pool the study‐specific effect sizes using the generic inverse variance method in RevMan 5.0 (RevMan 2008).
Continuous outcomes
We will analyze data for continuous outcomes in RevMan 5.0 using either mean differences (MD) or standardized mean differences (SMD) if continuous outcomes are measured with similar, but not identical, instruments across studies. If the studies provide another statistic other than means and standard deviations (e.g. standard error, t‐value, P value) we will perform the proper mathematical transformation to obtain standard deviations.
To ensure the appropriateness of meta‐analysis, the following standards will be applied to all data before inclusion. To check for skewed data we will compare the mean to the standard deviation. If the mean is smaller than twice the standard deviation the data is probably skewed (Altman 1996). For data with finite limits, such as endpoint data, the observed mean minus the lowest possible value (or the highest possible value minus the observed mean), and dividing by the standard deviation. If the ratio is less than 1 there is strong evidence of a skewed distribution (Altman 1996). We will reveal the skewed data in additional tables. The endpoint score with standard deviation will be considered first in analysis if both endpoint score and change score are available. In cases where only change score is reported, we will contact authors of studies for endpoint figures. If only the change score is available, standard deviation of change score is needed for analysis and, if available, we will combine the data with endpoint scores (unless the standardized mean difference is used). If the available data cannot be managed by the above methods, we will present the data in 'other data' tables and use a narrative approach to synthesis.
If adjusted estimates of mean differences are presented from multiple regression analyses and analyses of covariance, the process of data extraction and analysis using the generic inverse variance method will be performed.
Unit of analysis issues
For cross‐over studies, to exclude the potential additive effect in the second or further stages of these trials, we will only use data from the first stage in analysis. In studies with multiple treatment groups, we will carry out the analysis for each pair between meditation and other treatments. In studies with cluster‐randomization (e.g. randomization by clinician or treatment settings), unless the cluster effect was accounted for, analysis and pooling of clustered data will result in unit of analysis error and overestimate statistical significance. In these cases, we will contact the authors of studies will be contacted to obtain intra‐class correlation coefficients (ICC) of their clustered data and adjust by using accepted methods after consulting the Cochrane Developmental, Psychosocial and Learning Problems Group. Where clustering has been incorporated into the analysis of primary studies, we will also present these data as if from a non‐clustered randomized study. If the cluster effect was not accounted for in primary studies and the ICC was not available, we will present the data in a table, with a (*) symbol to indicate the presence of a probable unit of analysis error. The imputation of appropriate effect will be done by using the 'design effect' to calculate effective sample size. The design effect is 1+(m ‐ 1)r, where m is the average cluster size and r is the intra‐cluster correlation coefficient. If the ICC was not reported it will be assumed to be 0.05 (Higgins 2008).
In studies with repeated measures, we will carry out the analysis by separating the outcomes into short‐term (up to three months), intermediate‐term (three to 12 months) and long‐term (more than 12 months).
Dealing with missing data
For included studies which used an intention‐to‐treat analysis by filling in or imputation of data for missing cases (such as last observation carried forward method or assumed no changes), we will contact authors for available data.
Assessment of heterogeneity
We will carry out a test for homogeneity and calculate the I2statistic, which provides an estimate of the percentage of variability due to heterogeneity, using Review Manager 5.0 (RevMan 2008).
Heterogeneity can occur from many sources. An important aspect of every meta‐analysis is to consider and emphasize the existence of heterogeneity and to take account of this in the interpretation of results. Sources of heterogeneity (clinical heterogeneity) can be divided in to two groups: clinical data and type of meditation.
Clinical data:
Subtypes of attention deficit/hyperactivity disorders, etc.
Disorder severity and chronicity: mild, moderate, severe.
Comorbidity of emotional/psychiatric problems, speech /language problems, learning problems, psychosocial problems, conduct disorder.
Type of meditation:
(a) Techniques:
Concentrative, mindfulness meditation or combination.
Combination of different techniques of meditation (physical and mental practice, such as yoga).
Other ingredients of treatment: group activities, prayer, recreational activities, etc.
(b) Intensity and frequency of practice: duration of meditation per treatment session, frequency of practice, duration of practice.
Different follow‐up periods: at the end of trial, any specified period after trial, repeated follow‐up measures.
Multi‐component intervention: drugs, counseling, biofeedback, parent training, psychotherapy, family therapy, etc.
Data synthesis
Meta‐analysis should only be considered when a group of trials is sufficiently homogeneous in terms of participants, interventions and outcomes to provide a meaningful summary. We will use a fixed‐effect model for all analyses if there is no statistical heterogeneity. We may use a random‐effects meta‐analysis to incorporate heterogeneity among trials only after exploring the causes of heterogeneity or when heterogeneity cannot readily be explained.
The data analysis will seek to answer the following questions.
What is the direction of effect of meditation?
What is the size of the effect of meditation?
Is the effect of meditation consistent across studies?
What is the strength of evidence for the effect of meditation?
Any meta‐analysis will consider the following.
Different types of outcome (dichotomous, continuous, survival data).
Study design.
Follow up length (short‐term, intermediate, long‐term).
Subgroup analysis and investigation of heterogeneity
Due to clear differences in characteristics, rather than undertaking an overall pooled analysis, we will analyze the data in subgroups according to the following categories.
Childhood (under 13 years).
Adolescence (13 to 18 years).
Adult ADHD (age more than 18 years).
We will only undertake subgroup analyses if a sufficient number of studies is identified.
Sensitivity analysis
We will use a sensitivity analysis to test the robustness of effects of assumptions by examining the influence of the following on the results of the statistical analyses:
the effect of the quality criteria (determine the effect of studies with high risk of bias on the overall effect); and
blinding (masking) of raters.
Appendix 2. PubMed search strategy
("meditation"[mh] OR meditation[tw] OR "mindfulness‐based"[tw] OR vipassana[tw] OR Zen[tw] OR yoga[tw] OR yogic[tw] OR pranayama[tw] OR Sudarshan[tw] OR Qi‐gong[tw] OR Qigong [tw] OR "Chi kung "[tw] OR Kundalini[tw] OR ChunDoSunBup[tw] OR Reiki[tw] OR Tai Chi[tw]) AND ( "Attention Deficit Disorder with Hyperactivity" [mh] OR "attention deficit/hyperactivity"[tw] OR attention def* [tw] OR ADHD [tw] OR ADD [tw] OR ADDH [tw] OR ADHS [tw] OR hyperactiv*[tw] OR hyperkin*[tw] OR "brain dysfunction"[tw]) AND (randomised controlled trial [pt] OR controlled clinical trial [pt] OR randomised controlled trials[mh] OR random allocation [mh] OR double‐blind method [mh] OR single‐blind method [mh] OR clinical trial [pt] OR clinical trials [mh] OR "clinical trial" [tw] OR singl* [tw] OR doubl* [tw] OR trebl* [tw] OR tripl* [tw] OR mask* [tw] OR blind* [tw] OR placebos [mh] OR placebo* [tw] OR random* [tw] OR research design [mh:noexp] OR comparative study [mh] OR evaluation studies [mh] OR follow‐up studies [mh] OR prospective studies [mh] OR control* [tw] OR prospectiv* [tw] OR volunteer* [tw]) NOT (animals [mh] NOT human [mh]).
Appendix 3. EMBASE search strategy
1 meditation/
2 meditation.tw.
3 mindfulness‐based.tw.
4 vipassana.tw.
5 zen.tw.
6 yoga/
7 yoga.tw.
8 yogic.tw.
9 pranayama.tw.
10 sudarshan.tw.
11 qi‐gong.tw.
12 qigong.tw.
13 chi kung.tw.
14 kundalini.tw.
15 ChunDoSunBup.tw.
16 reiki.tw.
17 tai chi.tw.
18 or/1‐17
19 Attention Deficit Disorder/
20 (attention adj3 deficit$).tw.
21 adhd.tw.
22 addh.tw.
23 adhs.tw.
24 hyperactiv$.tw.
25 hyperkin$.tw.
26 minimal brain dysfunction$.tw.
27 or/19‐26
28 18 and 27
29 clin$.tw.
30 trial$.tw.
31 (clin$ adj3 trial$).tw.
32 singl$.tw.
33 doubl$.tw.
34 trebl$.tw.
35 tripl$.tw.
36 blind$.tw.
37 mask$.tw.
38 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
39 randomi$.tw.
40 random$.tw.
41 allocat$.tw.
42 assign$.tw.
43 (random$ adj3 (allocat$ or assign$)).tw.
44 crossover.tw.
45 44 or 43 or 39 or 38 or 31[M1]
46 exp Randomized Controlled Trial/
47 exp Double Blind Procedure/
48 exp Crossover Procedure/
49 exp Single Blind Procedure/
50 exp RANDOMIZATION/
51 46 or 47 or 48 or 49 or 50 or 45
52 51 and 28
Appendix 4. PSYCInfo Search Strategy
1. meditation/
2 meditation.tw.
3 mindfulness‐based.tw.
4 vipassana.tw.
5 zen.tw.
6 yoga/
7 yoga.tw.
8 yogic.tw.
9 pranayama.tw.
10 sudarshan.tw.
11 qi‐gong.tw.
12 qigong.tw.
13 chi kung.tw.
14 kundalini.tw.
15 ChunDoSunBup.tw.
16 reiki.tw.
17 tai chi.tw.
18 or/1‐17
19 Attention Deficit Disorder/
20 (attention adj3 deficit$).tw.
21 adhd.tw.
22 addh.tw.
23 adhs.tw.
24 hyperactiv$.tw.
25 hyperkin$.tw.
26 minimal brain dysfunction$.tw.
27 or/19‐26
28 18 and 27
29 Treatment Effectiveness Evaluation/
30 exp Treatment Outcomes/
31 Psychotherapeutic Outcomes/
32 PLACEBO/
33 exp Followup Studies/
34 placebo$.tw.
35 random$.tw.
36 comparative stud$.tw.
37 randomi#ed controlled trial$.tw.
38 (clinical adj3 trial$).tw.
39 (research adj3 design).tw.
40 (evaluat$ adj3 stud$).tw.
41 (prospectiv$ adj3 stud$).tw.
42 ((singl$ or doubl$ or trebl$ or tripl$) adj3 (blind$ or mask$)).tw.
43 control$.tw.
44 43 or 35 or 33 or 41 or 40 or 36 or 29 or 34 or 30 or 42 or 38 or 32 or 31 or 39 or 37
45 28 and 44
Appendix 5. CINAHL Search Strategy
1 meditation/
2 meditation.tw.
3 mindfulness‐based.tw.
4 vipassana.tw.
5 zen.tw.
6 yoga/
7 yoga.tw.
8 yogic.tw.
9 pranayama.tw.
10 sudarshan.tw.
11 qi‐gong.tw.
12 qigong.tw.
13 chi kung.tw.
14 kundalini.tw.
15 ChunDoSunBup.tw.
16 reiki.tw.
17 tai chi.tw.
18 or/1‐17
19 Attention Deficit Disorder/
20 (attention adj3 deficit$).tw.
21 adhd.tw.
22 addh.tw.
23 adhs.tw.
24 hyperactiv$.tw.
25 hyperkin$.tw.
26 minimal brain dysfunction$.tw.
27 or/19‐26
28 18 and 27
29 randomi$.mp.
30 clin$.mp.
31 trial$.mp.
32 (clin$ adj3 trial$).mp.
33 singl$.mp.
34 doubl$.mp.
35 tripl$.mp.
36 trebl$.mp.
37 mask$.mp.
38 blind$.mp.
39 (33 or 34 or 35 or 36) and (37 or 38)
40 crossover.mp.
41 random$.mp.
42 allocate$.mp.
43 assign$.mp.
44 (random$ adj3 (allocate$ or assign$)).mp.
45 Random Assignment/
46 exp Clinical Trials/
47 exp Meta Analysis/
48 44 or 40 or 39 or 32 or 29 or 45 or 46 or 47
49 28 and 48
Appendix 6. LILACS search strategy
mediation or yoga or tai chi or reiki or mindfulness‐based [Palavras] and attention deficit or adhd or addh or adhs
Appendix 7. OPENSIGLE search strategy
((meditation or yoga or reiki or tai chi or zen or mindfulness or vipassana or yogic or qigong or chi kung or kundalini or ChunDoSunBup))
AND
((attention deficit or adhd or addh or adhs or hyperactiv* or hyperkin* or minimal brain))
Data and analyses
Comparison 1.
Meditation therapy versus drug therapy
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Teacher rating ADHD overall scale | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Analysis 1.1.
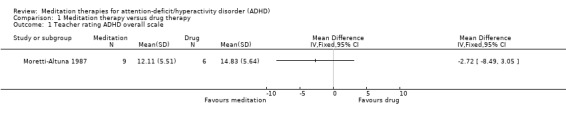
Comparison 1 Meditation therapy versus drug therapy, Outcome 1 Teacher rating ADHD overall scale.
Comparison 2.
Meditation therapy versus standard treatment without drug
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Teacher rating ADHD scale | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Distraction test | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected |
Analysis 2.1.
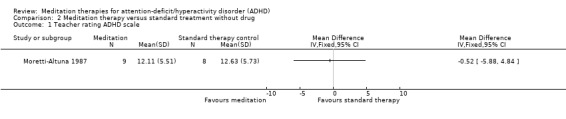
Comparison 2 Meditation therapy versus standard treatment without drug, Outcome 1 Teacher rating ADHD scale.
Analysis 2.2.
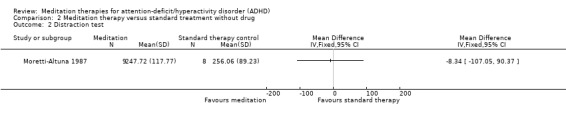
Comparison 2 Meditation therapy versus standard treatment without drug, Outcome 2 Distraction test.
Differences between protocol and review
We changed some sources of databases to be searched. We searched LILACS through the Virtual Health Library (VHL) in BIREME: Pan American Health Organization (PAHO), which incorporates many bibliographic databases in general health science (LILACS, MEDLINE, The Cochrane Library, SciELO), specialized areas (ADOLEC, BBO, BDENF, DESASTRES, HISA, HOMEOINDEX, LEYES, MEDCARIB, REPIDISCA) and international agencies (PAHO, WHOLIS).
The CISCOM database of The Research Council for Complementary Medicine was closed, therefore we searched other complementary and alternative medicine databases, i.e. CAM on PubMed, the web‐site of the Cochrane Complementary and Alternative Health field, the Complementary Medicine Resources for Health Professionals and Researchers, and the Complementary and Alternative Therapies databases of Bandolier.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | Randomized controlled trial 2 x 2 cross‐over design using the drawing of lots Analyzed by means of an analysis of variance for repeated measurements |
|
| Participants | 20 grade school age children (13 boys and 7 girls) diagnosed with ADHD (Diagnostic System for Psychic Disorders in childhood and adolescence according to ICD‐10 and DSM‐IV (DISYPS‐KJ)) Trial was conducted in the University Hospital in Heidelberg, Germany between May 2000 and March 2001 Yoga group (n = 9 ; 8 boys + 1 girl) Exercise group (n = 11; 5 boys + 6 girls) One 9‐year old boy in the yoga group left the study because of a change of residence during the 21st week Exclusion criteria: severe developmental disturbances, low intelligence level (IQ < 70), and extreme behavioral disturbances which would be incompatible with participation in a group |
|
| Interventions | Intervention 1: body‐oriented yoga exercise program A standardized program consisting of elements of Hatha yoga (postures, breathing exercises, meditative exercises) especially developed for children with ADHD, consisting of 16 exercise units for children and documented in a therapy manual Individual practice of yoga at home or school was carried out by each participant independently, without schedule Intervention 2: conventional motor training exercises A program of various well‐known active games was put together. These contained all the elements that occur in normal grade school and leisure‐sport activities (running games, throwing and catching games, agility games, ball games, concentration games, social games) and are thus fundamentally different from the yoga exercises. Using a cross‐over study design, both groups received 2 consecutive 8‐week intervention/training sessions (each with 2 training sessions of 1 hour per week), separated by a training break of 6 weeks |
|
| Outcomes | 1. Fremdbeurteilungsbogen für hyperkinetische Störungen (FBB‐HKS) Döpfner 2000, Brühl 2000: 20 items each with 4 levels (0 = not at all, 1 = a little, 2 = to a large extent, 3 = especially), summarized in 3 symptom groups: attention‐deficit, hyperactivity and impulsiveness. Categorized severity scores: 0 to ‐0.5 = not at all, 0.5 to 1.5 = a little, 1.5 to 2.5 = quite/to a large extent, 2.5 to 3.0 = very much/especially 2. Dortmund Attention Test (DAT) Lauth 1993 : comparison of differed pictures to determine the response latency and rate of error, which reflects attention‐deficit Measurements: first baseline (baseline 1 / period of 6 weeks with parents ratings of ADHD symptoms, 1 measurement per week, using a standardized rating scale for parents, teachers and educators: FBB‐HKS). A second baseline was taken after the 8‐week intervention (baseline 2 / period of 6 weeks with standardized parent ratings of ADHD symptoms) by means of weekly measurements. Following the program, a third baseline was measured (baseline 3 / period of 6 weeks), with one assessment done per week. During both training phases weekly assessments were made. The Dortmund Attention Test was carried out in all 3 baseline time periods. |
|
| Notes | Data were abstracted from the translated original German paper (translation was done by the investigator) 8 received medication (in 7 cases methylphenidate, in 1 case pipamperone) 7 received complementary therapy (in 3 cases ergotherapy, in 2 cases dyslexia therapy and in 2 cases behavioral therapy) Only the data from the first phase of the study (before cross over) were included in the analysis |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Low risk | Quote: "the children were randomly (by drawing lots) assigned" Comment: probably done |
| Allocation concealment? | Low risk | Comment: automatically done by drawing lots for each participant at the time of sequence generation |
| Blinding? All outcomes | High risk | Comment: the intervention cannot be blinded |
| Incomplete outcome data addressed? All outcomes | Low risk | Quote: "one 9‐year‐old boy left the study because of a change of residence during the 21st week" Comment: the drop‐out case would not have had a clinically relevant impact on the observed effect size |
| Free of selective reporting? | Low risk | Comment: the outcomes were reported as mentioned in the methods section. The study author was contacted and completeness of outcome reporting was confirmed. |
| Free of other bias? | High risk | Comment: co‐intervention ‐ more boys in the yoga group received medication (5 of 9) than the exercise group (3 of 11) |
| Methods | Randomized controlled trial Initially a 20‐week program. After 20 weeks, 5 of the control group moved to the treatment group |
|
| Participants | 16 boys aged 8 to 13 years. Mean age for boys in the yoga group 10.63 years (SD = 1.78 years) and for boys in the control group 9.35 years (SD = 1.70 years). Participants diagnosed with ADHD according to DSM‐IV criteria by experienced pediatricians and diagnosis confirmed by the results of pre‐test Conners’ Parent Rating Scales: Long (CPRS: R (L)). All medicated participants were stabilized after appropriate periods of titration on dexamphetamine and/or methylphenidate. All participants were Caucasian except one (Chinese) and were assessed as having average or high intelligence Participants were also required to be fluent in English and free from serious family pathology (e.g. parental clinical depression or substance abuse, criminality in one or both parents, or domestic violence). Families with these characteristics were excluded because they were unlikely to be compliant with the extensive time commitment required. Participants were excluded if they were receiving other forms of treatment (except medication for ADHD). Participants had to be able to attend weekly classes for the 20‐week duration of the yoga program. Yoga group: 11 boys (6 originally randomized to yoga group, 5 crossed over from control group) Control group: 8 boys |
|
| Interventions | 1. Yoga program Nagendra 1988, Saraswati 1990 which incorporated standard yogic practices and comprised: ‐ Respiratory training: selective use of oral and nasal passages for respiratory flow intended to increase the child's breath awareness as well as train him to breathe naturally through both nares. All exercises were repeated several times during each session and in a regulated rhythmical manner. ‐ Postural training: involved stretching, load bearing, backward, forward, lateral flexion, and extensions and inversions performed in sitting, standing, supine and prone positions. These were performed in combination with respiratory exercises in static and dynamic positions. ‐ Relaxation training: involved becoming progressively aware of and relaxing body parts and tensing and relaxing muscles ‐ Concentration training: involved a technique called Trataka where participants focused on a word or shape, followed by seeing the image with eyes closed and continuing to see the image on a blank piece of paper 20 1‐hour weekly instructional group sessions took place at Westmead Hospital, New South Wales, Australia. Parents were encouraged to assist with daily practice sessions at home. 2. Control group: engaged in co‐operative games and activities. These groups were conducted for 1 hour, once a month and at the same location as the yoga groups |
|
| Outcomes | 1. Conners' Parent (CPRS–R:L) Teacher (CTRS–R:L) Rating Scales – Revised: Long (Conners 1997) 2. Test of Variables of Attention (TOVA) Greenberg 1991: a continuous performance test designed to avoid confounding attention with language processing skills or short‐term memory problems 3. Motion Logger ‐ Actigraph. The Actigraph is a portable electronic activity monitor designed to be worn on the wrist, waist or ankle. |
|
| Notes | Of the 14 boys who completed the trials, 6 participated in the yoga group only, 5 who were originally in the control group moved from the control group to the yoga group, and 3 were in the control group only. This gave a total of 11 boys who completed the yoga training and 8 boys who acted as controls. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "boys who were randomly allocated to the control group in the first allocation" |
| Allocation concealment? | Unclear risk | Comment: not mentioned in the report |
| Blinding? All outcomes | High risk | Comment: the intervention cannot be blinded. Probably not done. |
| Incomplete outcome data addressed? All outcomes | High risk | Quote "Letters were sent to 80 parents with eligible sons. Of the 25 who responded, 16 began the trials and completed them." Comment: the attrition rate and reason for drop‐out were not reported in each intervention group |
| Free of selective reporting? | High risk | Quote: "On the Actigraph motion logger, many technical problems were encountered ... Due to these problems, data were deemed unreliable and were discarded." Comment: not all of the pre‐specified outcomes were reported |
| Free of other bias? | High risk | Quote: "there were significant differences between the control and yoga groups on pretest sub‐scale scores on almost all Conners’ Rating Scales for both parents and teachers." Comment: significant baseline differences. |
| Methods | Randomized controlled trial, but used a modified randomization method to ensure the medicated subjects were equally distributed between the 3 groups Dissertation submitted to the faculty of the Department of Psychology at St. John's University, New York in 1983 |
|
| Participants | 24 boys from the Five Towns area of Lang Island, New York, USA diagnosed with ADHD (DSM‐III) based on parent and child interviews Age range 93 to 142 months (mean = 120.63 months) Participants had a minimum score of 15 on the Abbreviated Parent‐Teacher Questionnaire and were free from neurological disease or psychosis. The participants who received stimulants were equally assigned into each group |
|
| Interventions | Three intervention groups: 1. Meditation training (MT): individual sessions twice weekly for 4 weeks. Meditation technique was modified from Benson 1975 and Carrington 1975: repeating the word "Ahnam" out loud and progressively more softly until the word was repeated silently. The actual meditation duration was gradually increased from 2 minutes to 8 minutes by the end of the 4‐week training period. Practice was at least 3 times per week at home. 2. Relaxation training (RT): individual sessions twice weekly for 4 weeks, using modified progressive muscle relaxation by reduction in the number of muscle groups when compare to the standard progressive muscle relaxation, deep and slowing breathing phase before and after the tension‐relaxation cycles and 5‐second tension periods. The actual relaxation training duration was gradually increased from 2 minutes to 8 minutes by the end of 4 weeks. Practice was at least 3 times per week at home. 3. Waiting list controls (WLC): received no experimental manipulation |
|
| Outcomes | 1. Matching Familiar Figure Test (MFFT) Kagan 1966 which measures the dimension of reflection‐impulsivity by participants choosing identical pictures from an array of 6 variants. Errors reflect impulsivity. 2. Fruit Distraction Test (FDT) Santostefano 1978 which tests the selective deployment of attention between relevant and irrelevant stimuli by naming the color with and without distraction and contradictions 3. Nowicki‐Strickland Locus of Control Scale (LCS) which is used in the identification of hyperactive children and to evaluate treatment effectiveness (consists of 39‐items; 4‐point scale) 4. Abbreviated Parent ‐Teacher Questionnaire (PTQ)Conners 1973 consisted of 10 overlapping items from the Conners' Teacher Rating Scale and the Parent Symptoms Questionnaire 5. Werry‐Weiss‐Peters Activity Scale (WWPAS) Werry 1968: a rating scale which assesses activity level in specific situations |
|
| Notes | Parents were to be included in the training sessions Results table did not show number in each group. Data cannot be used in meta‐analysis. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "were randomly assigned to one of three conditions" Quote: "subjects who received stimulant medication... were assigned in a modified random fashion such that they were represented in approximately equal numbers" Comment: the randomization was not adequately done |
| Allocation concealment? | Unclear risk | Comment: No mention about allocation concealment. |
| Blinding? All outcomes | High risk | Comment: the intervention cannot be blinded. No description of blinding of the assessors. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Comment: no mention of attrition |
| Free of selective reporting? | Low risk | Comment: all outcomes were reported as mentioned in the method section |
| Free of other bias? | Low risk | |
| Methods | Randomized controlled trial Conducted in New York, USA Dissertation submitted to the faculty of the Department of Psychology at St. John's University, New York in 1987. This study has many similar characteristics to Kratter 1983, which was also a dissertation from the same university. |
|
| Participants | 23 boys, age range 6 to 10 years, 5 black, 5 white, 13 Hispanic Participants diagnosed with ADHD (DSM‐III), confirmed by an intake committee (administrative team leader, a psychiatrist, multidisciplinary staff member). The participants had to be free from psychosis, neurological disease and not currently on psychoactive medication. |
|
| Interventions | 1) Drug therapy (DT): medication + conventional treatment 2) Meditation‐relaxation training (MT): individual sessions, 30 minutes twice weekly for 4 weeks. Meditation technique was modified from Benson 1975: participants repeated the word "One" out loud and progressively more softly until the word was repeated silently. The actual meditation duration was gradually increased from 1 minute to 8 minutes by the end of the 4‐week training period. Practice was at least 3 times per week at home. 3) Standard therapy control (STC): conventional treatment without medication, i.e. milieu, individual, group and/or family therapy |
|
| Outcomes | 1. Matching Familiar Figure Test (MFFT) Kagan 1966, which measures the dimension of reflection‐impulsivity by participants choosing identical pictures from array of 6 variants. Errors reflected impulsivity. 2. Fruit Distraction Test(FDT) Santostefano 1978, which tests the selective deployment of attention between relevant and irrelevant stimuli by naming the color with and without distraction and contradictions 3. The Children's Embedded Figures Test (CEFT) Karp 1963, which measures the extent to which perception of part of a stimulus field is influenced by the entire field and requires the subject to find a simple form in a complex one 4. Abbreviated Parent‐Teacher Questionnaire (PTQ) Conners 1973, which consists of 10 overlapping items from the Conners' Teacher Rating Scale and the Parent Symptoms Questionnaire 5. Werry‐Weiss‐Peters Activity Scale (WWPAS) Werry 1968: a rating scale which assesses activity level in specific situations |
|
| Notes | Parents were to be included in the training sessions | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Adequate sequence generation? | Unclear risk | Quote: "Subjects were randomly assigned to one of three conditions" |
| Blinding? All outcomes | High risk | Comment: the intervention cannot be blinded. No description of blinding of the assessors. |
| Incomplete outcome data addressed? All outcomes | Unclear risk | Comment: no mention of attrition rate |
| Free of selective reporting? | Low risk | Comment: all outcome were reported as mentioned in the methods section |
| Free of other bias? | Low risk | |
ADHD = attention‐deficit/hyperactivity disorder
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abadi 2008 | No randomization |
| Evans 2007 | Not a clinical trial |
| Harrison 2004 | Before‐after design in 2 sequential groups, no true control group |
| Hassasiri 2002 | Before‐after design, no control group |
| Kratter 1982 | Duplicate publication, less detailed than Kratter 1983 |
| Peck 2005 | Not diagnosed with ADHD |
| Zylowska 2008 | Before‐after design, no control group |
Characteristics of ongoing studies [ordered by study ID]
| Trial name or title | Breathing meditation with methylphenidate for the treatment of attention‐deficit/hyperactivity disorder children: a randomized controlled trial |
| Methods | Randomized controlled trial |
| Participants | Inclusion criteria: ‐ Children diagnosed with ADHD by a child psychiatrist using DSM‐IV‐TR criteria ‐ Any religious background ‐ Aged between 7 and 12 years Exclusion criteria: ‐ Autistic spectrum disorders ‐ Mental retardation |
| Interventions | Breathing meditation versus standard treatment control |
| Outcomes | 1. Conners' Abbreviated Parent Questionnaire (continuous outcome) assessed by the parents at baseline, at the end of 4 weeks, at 8 weeks and at 12 weeks 2. Child Attention Problems (CAP) Rating Scale assessed at the same time |
| Starting date | April 2006 |
| Contact information | Associate Professor Thawatchai Krisanaprakornkit Department of Psychiatry, Faculty of Medicine, Khon Kaen University, Thailand |
| Notes | Registered at www.ClinicalTrials.gov |
Contributions of authors
TK: protocol development, searching, data extraction, quality assessment and analysis. CN: data extraction, quality assessment and statistical analysis. CW: screening the potential included studies. NP: quality assessment.
Sources of support
Internal sources
Thai Cochrane Network, Thailand.
Faculty of Medicine, Khon Kaen University, Thailand.
Cochrane Developmental, Psychosocial and Learning Problems Group (CDPLPG), UK.
External sources
Thailand Research Fund, Senior Research Scholar, Thailand.
Declarations of interest
TK runs the Meditation Therapy Clinic for various types of patients at the Department of Psychiatry, Faculty of Medicine, Khon Kaen University, Thailand.
TK is conducting a randomized controlled trial 'Breathing meditation with methylphenidate for the treatment of attention‐deficit/hyperactivity disorder children', which is registered at www.ClinicalTrials.gov (Krisanaprakornkit 2008).
There are no potential conflict of interest for the other authors.
New
References
References to studies included in this review
- Haffner J, Roos J, Goldstein N, Parzer P, Resch F. The effectiveness of body‐oriented methods of therapy in the treatment of attention‐deficit hyperactivity disorder (ADHD): results of a controlled pilot study [Zur Wirksamkeit körperorientierter Therapieverfahren bei der Behandlung hyperaktiverStörungen: Ergebnisse einer kontrollierten Pilotstudie]. Zeitschrift für Kinder und Jugendpsychiatrie und Psychotherapie 2006;34(1):34‐47. [DOI] [PubMed] [Google Scholar]
- Jensen PS, Kenny DT. The effects of yoga on the attention and behavior of boys with attention deficit hyperactivity disorder (ADHD). Journal of Attention Disorders 2004;7(4):205‐16. [DOI] [PubMed] [Google Scholar]
- Kratter J. The use of meditation in the treatment of attention deficit disorder with hyperactivity. A dissertation submitted to the faculty of the Department of Psychology at St. John's University, New York1983.
- Moretti‐Altuna GE. The effects of meditation versus medication in the treatment of attention deficit disorder with hyperactivity. A dissertation submitted to the faculty of the Department of Psychology at St. John's University, New York1987.
References to studies excluded from this review
- Abadi MS, Madgaonkar J, Venkatesan S. Effect of Yoga on Children with Attention Deficit/Hyperactivity Disorder. National Academy of Psychology 2008;53(2):154‐9. [Google Scholar]
- Evans BT. Mindfulness meditation as an intervention for adult attention deficit hyperactivity disorder. A dissertation presented to the faculty of the California School of Professional Psychology, San Francisco Campus, Alliant International University2007.
- Harrison LJ, Manocha R, Rubia K. Sahaja yoga meditation as a family treatment programme for children with attention deficit‐hyperactivity disorder. Clinical Child Psychology and Psychiatry 2004;9(4):479‐97. [Google Scholar]
- Hassasiri A, Dhammakhanto K, Wongpunya S. Manual of meditation and imagery training for attention deficit children: age 5‐11. 8th International Congress of Department of Mental Health, Thailand. 2002:171‐2. [Google Scholar]
- Kratter J, Hagan JD. The use of meditation in the treatment of attention deficit disorder with hyperactivity. Educational Resources Information Center at http://www.eric.ed.gov/1982.
- Peck HL, Kehle TJ, Bray MA, Theodore LA. Yoga as an intervention for children with attention problems. School Psychology Review 2005;34(3):415‐24. [Google Scholar]
- Zylowska L, Ackerman DL, Yang MH, Futrell JL, Horton NL, Hale TS, et al. Mindfulness meditation training in adults and adolescents with ADHD: a feasibility study. Journal of Attention Disorders 2008;11(6):737‐46. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
- Breathing meditation with methylphenidate for the treatment of attention deficit hyperactivity disorder. www.ClinicalTrials.gov (accessed 1 February 2010).
Additional references
- American Academy of Pediatrics. Clinical practice guideline: treatment of the school‐aged child with attention‐deficit /hyperactivity disorder. Pediatrics 2001;108(4):1033‐44. [DOI] [PubMed] [Google Scholar]
- Achenbach TM, Ruffle TM. The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatrics in Review 2000;21(8):255‐6. [DOI] [PubMed] [Google Scholar]
- Adams CD, Kelly ML, McCarthy M. The Adolescent Behavior Checklist: development and initial psychometric properties of a self‐report measure for adolescents with ADHD. Journal of Clinical Child Psychology 1997;26(1):77‐86. [DOI] [PubMed] [Google Scholar]
- Adesman AR. The Attention Deficit Disorders Evaluation Scale. Journal of Developmental & Behavioral Pediatrics 1991;12(1):65‐6. [PubMed] [Google Scholar]
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313:1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM‐IV‐TR. 4th Edition. Washington DC: American Psychiatric Publishing Inc, 2000. [Google Scholar]
- Arias A J, Steinberg K, Banga A, Trestman RL. Systematic review of the efficacy of meditation techniques as treatments for medical illness. Journal of Alternative and Complementary Medicine 2006;12:817‐32. [DOI] [PubMed] [Google Scholar]
- Arnold LE. Alternative treatments for adults with attention‐deficit hyperactivity disorder (ADHD). Annals of the New York Academy of Sciences 2001;931:310‐41. [PUBMED: 11462750] [DOI] [PubMed] [Google Scholar]
- Astin JA. Stress reduction through mindfulness meditation: effects on psychological symptomatology, sense of control and spiritual experiences. Psychotherapy and Psychosomatics 1997;66(2):97‐106. [DOI] [PubMed] [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clinical Psychology: Science and Practice 2003;10:125‐43. [Google Scholar]
- Barrows KA, Jacobs BP. Mind‐body medicine: an introduction and review of the literature. Medical Clinics of North America 2002;86(1):11‐31. [DOI] [PubMed] [Google Scholar]
- Becker KA. History of the Stanford‐Binet Intelligence Scales: Content and Psychometrics. Stanford‐Binet Intelligence Scales, Fifth Edition Assessment Service Bulletin No. 1. Itasca, IL: Riverside Publishing, 2003. [Google Scholar]
- Benson H, Klipper MZ. The Relaxation Response. New York, NY: Harper Torch, 1975. [Google Scholar]
- Biederman J, Faraone SV, Chen WJ. Social Adjustment Inventory for children and adolescents: concurrent validity in ADHD children. Journal of the American Academy of Child and Adolescent Psychiatry 1993;32(5):1059‐64. [DOI] [PubMed] [Google Scholar]
- Brod M, Johnston J, Able S, Swindle R. Validation of the adult attention‐deficit/hyperactivity disorder quality‐of‐life scale (AAQoL): a disease‐specific quality‐of‐life measure. Quality of Life Research 2006;15(1):117‐29. [DOI] [PubMed] [Google Scholar]
- Brühl B, Döpfner M, Lehmkuhl G. Der Fremdbeurteilungsbogen fürhyperkinetische Störungen (FBB‐HKS) – Prävalenz Hyperkinetischer Störungen imElternurteil und psychometrische Kriterien. Kindheit und Entwicklung 2000;9:115‐25. [Google Scholar]
- Carrington P, Ephron HS. Clinical use of meditation. Current Psychiatric Therapies 1975;15:101‐8. [PubMed] [Google Scholar]
- Castillo RJ. Depersonalization and meditation. Psychiatry 1990;53(2):158‐68. [DOI] [PubMed] [Google Scholar]
- Chan‐Ob T, Boonyanaruthee V. Meditation in association with psychosis. Journal of the Medical Association of Thailand 1999;82(9):925‐30. [PubMed] [Google Scholar]
- Conners CK. Rating scales for use in drug studies with children [Pharmacotherapy with children]. Psychopharmacology Bulletin. Washington, DC: Government Printing Office, 1973. [Google Scholar]
- Conners CK. Conners' Continuous Performance Test. North Tonawanda, NY: Multi‐Health Systems, 1995. [Google Scholar]
- Conners CK. Conners Rating Scale Revised. North Tonawanda, NY: Multi‐Health Systems, Inc, 1997. [Google Scholar]
- Conners CK, Sitarenios G, Parker JD, Epstein JN. The revised Conners' Parent Rating Scale (CPRS‐R): factor structure, reliability, and criterion validity. Journal of Abnormal Child Psychology 1998;26(4):257‐68. [DOI] [PubMed] [Google Scholar]
- Conners CK, Sitarenios G, Parker JD, Epstein JN. Revision and restandardization of the Conners Teacher Rating Scale (CTRS‐R): factor structure, reliability, and criterion validity. Journal of Abnormal Child Psychology 1998;26(4):279‐91. [DOI] [PubMed] [Google Scholar]
- Davis J. Notes on the psychology of meditation Part 1: definition. http://www.naropa.edu/faculty/johndavis/tp/medit2.html updated on 18 December 1998:Accessed 10 September 2008.
- Dwivedi KN, Banhatti RG. Attention deficit/hyperactivity disorder and ethnicity. Archives of Disease in Childhood 2005;90(Suppl 1):10‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Döpfner M, Lehmkuhl G. Diagnostik‐System für psychische Störungen im Kindesund Jugendalter nach ICD‐10 und DSM‐IV (DISYPS‐KJ). Diagnostik‐System für psychische Störungen im Kindesund Jugendalter nach ICD‐10 und DSM‐IV (DISYPS‐KJ). Bern: Huber, 2000. [Google Scholar]
- Egger M, Davey Smith G, Schneider M, Minder CE. Bias in meta‐analysis detected by a simple, graphical test. BMJ 1997;315(7109):629‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliaz I. Children and meditation (Our Kids Sake). http://ourkidssake.org/content/view/46/Accessed 10 September 2008.
- French AP, Schmid AC, Ingalls E. Transcendental meditation, altered reality testing, and behavioural change: a case report. Journal of Nervous and Mental Disease 1975;161(1):55‐8. [DOI] [PubMed] [Google Scholar]
- Greenberg LM. TOVA manual. Minneapolis, MN: Author, 1991. [Google Scholar]
- Greenberg LM, Kindschi RN. Test of Variables of Attention: clinical guide. Los Alamitos, CA: Universal Attention Disorders, Inc, 1999. [Google Scholar]
- Greydanus DE. Attention deficit hyperactivity disorder across the lifespan: the child, adolescent, and adult. Disease‐a‐Month 2007;53:70‐131. [DOI: 10.1016/j.disamonth.2007.01.001] [DOI] [PubMed] [Google Scholar]
- Halperin JM, McKay KE, Newcorn JH. Development, reliability, and validity of the children's aggression scale‐parent version. Journal of the American Academy of Child and Adolescent Psychiatry 2002;41(3):245‐52. [DOI] [PubMed] [Google Scholar]
- Halperin JM, McKay KE, Grayson RH, Newcorn JH. Reliability, validity, and preliminary normative data for the Children's Aggression Scale ‐ Teacher Version. Journal of the American Academy of Child and Adolescent Psychiatry 2003;42(8):965‐71. [DOI] [PubMed] [Google Scholar]
- Harada Y, Saitoh K, Iida J, Sakuma A, Iwasaka H, Imai J, et al. The reliability and validity of the Oppositional Defiant Behavior Inventory. European Child and Adolescent Psychiatry 2004;13(3):185‐90. [DOI] [PubMed] [Google Scholar]
- Harvey E, Danforth JS, Ulaszek WR, Eberhardt TL. Validity of the parenting scale for parents of children with attention‐deficit/hyperactivity disorder. Behaviour Research and Therapy 2001;39(6):731‐43. [DOI] [PubMed] [Google Scholar]
- Hassed C. Meditation in medical practice. Australian Family Physician 1996;25(8):1257‐60. [PubMed] [Google Scholar]
- Helen C. Meditation helps kids with ADHD [ABC News]. http://www.abc.net.au/science/articles/2007/11/30/2106111.htm2004:Accessed 10 September 2008.
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions version 5.0.0 [updated February 2008]. The Cochrane Collaboration. Available from www.cochrane‐handbook.org.
- Institute for Clinical Systems Improvement. Diagnosis and management of attention deficit hyperactivity disorder in primary care for school age children and adolescents (guideline) (available at: http://www.icsi.org/adhd/adhd_2300.html) (accessed February 2007). 6th Edition. Bloomington, MN: ICSI, 2005. [Google Scholar]
- Jensen PS, Shervette RE, Xenakis SN, Richters J. Anxiety and depressive disorders in attention deficit disorder with hyperactivity: new findings. American Journal of Psychiatry 1993;150(8):1203‐9. [DOI] [PubMed] [Google Scholar]
- Kabat‐Zinn J, Massion AO, Kristeller J, Peterson LG, Fletcher KE, Pbert L, et al. Effectiveness of a meditation‐based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry 1992;149(7):936‐43. [DOI] [PubMed] [Google Scholar]
- Kagan J. Reflection‐impulsivity: The generality and dynamics of conceptual tempo. Journal of Abnormal Psychology 1966;71:17‐24. [DOI] [PubMed] [Google Scholar]
- Karp SA. Field dependence and overcoming embeddedness. Journal of Consulting Psychology 1963;27:294‐302. [DOI] [PubMed] [Google Scholar]
- Klinge V, Harper S, Vaziri H. The Peabody Individual Achievement Test. A validity study with adolescent psychiatric inpatients. Journal of Abnormal Child Psychology 1974;2(2):133‐41. [DOI] [PubMed] [Google Scholar]
- Krisanaprakornkit T, Krisanaprakornkit W, Piyavhatkul N, Laopaiboon M. Meditation therapy for anxiety disorders. Cochrane Database of Systematic Reviews 2006, Issue 1. [DOI: 10.1002/14651858.CD004998.pub2] [DOI] [PubMed] [Google Scholar]
- Landgraf JM, Rich M, Rappaport L. Measuring quality of life in children with attention‐deficit/hyperactivity disorder and their families: development and evaluation of a new tool. Archives of Pediatrics & Adolescent Medicine 2002;156(4):384‐91. [DOI] [PubMed] [Google Scholar]
- Lauth GW. Dortmunder Aufmerksamkeitstest –DAT–KI. : .. Göttingen: Hogrefe, 1993. [Google Scholar]
- Lazarus AA. Psychiatric problems precipitated by transcendental meditation. Psychological Reports 1976;39(2):601‐2. [DOI] [PubMed] [Google Scholar]
- Light RJ, Pillemer DB. Organizing a reviewing strategy. Summing Up: The Science of Reviewing Research. Cambridge, MA: Harvard University Press, 1984:13‐31. [Google Scholar]
- Loyd BH, Abidin RR. Revision of the Parenting Stress Index. Journal of Pediatric Psychology 1985;10(2):169‐77. [DOI] [PubMed] [Google Scholar]
- Mansky PJ, Wallerstedt DB. Complementary medicine in palliative care and cancer symptom management. Cancer Journal 2006;12:425‐31. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JDA, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability and validity. Journal of the American Academy of Child and Adolescent Psychiatry 1997;36:554–65. [DOI] [PubMed] [Google Scholar]
- McLeod BD, Weisz JR. Using dissertations to examine potential bias in child and adolescent clinical trials. Journal of Consulting and Clinical Psychology 2004;72(2):235‐51. [DOI] [PubMed] [Google Scholar]
- Micucci D. International education: meditation helps students. International Herald Tribune 15 February 2005.
- Multimodal Treatment Study of ADHD Cooperative Group. A 14‐month randomized clinical trial of treatment strategies for attention‐deficit/hyperactivity disorder. Archives of General Psychiatry 1999;56(12):1073‐86. [DOI] [PubMed] [Google Scholar]
- Nagendra HR, Mohan T, Shriram A. Yoga inEducation. Bangalore, India: VKYRF, 1988. [Google Scholar]
- Nichols SL, Waschbusch DA. A review of the validity of laboratory cognitive tasks used to assess symptoms of ADHD. Child Psychiatry & Human Development 2004;34(4):297‐315. [DOI] [PubMed] [Google Scholar]
- National Institute of Health. Diagnosis and treatment of attention deficit hyperactivity disorder. NIH Consensus Statement Online Nov 16‐18 1998;16(2):1‐37. [PubMed] [Google Scholar]
- National Institute of Mental Health (NIMH). CGI (Clinical Global Impression) Scale. Psychopharmacology Bulletin 1985;21:839‐44. [Google Scholar]
- Ospina MB, Bond TK, Karkhaneh M, Tjosvold L, Vandermeer B, Liang Y, et al. Meditation practices for health: state of the research. Evidence Report/Technology Assessment No. 155 (prepared by the University of Alberta Evidence‐based Practice Center under Contract No. 290‐02‐0023) AHRQ Publication No.07‐E010. Rockville, MD: Agency for Healthcare Research and QualityJune 2007. [PMC free article] [PubMed]
- Pritchard D. Attention deficit hyperactivity disorder in children. Clinical Evidence 2006;15:1‐3. [PubMed] [Google Scholar]
- The Nordic Cochrane Centre. The Cochrane Collaboration. Review Manager (RevMan). Version 5.0. Copenhagen: The Nordic Cochrane Centre. The Cochrane Collaboration, 2008.
- Reynolds CR, Kamphaus RW. Behavior assessment system for children (BASC). Circle Pines, MN: American Guidance Service, 1992. [Google Scholar]
- Riccio CA, Cohen MJ, Hynd GW, Keith RW. Validity of the Auditory Continuous Performance Test in differentiating central processing auditory disorders with and without ADHD. Journal of Learning Disability 1996;29(5):561‐6. [DOI] [PubMed] [Google Scholar]
- Robin AL, Vandermay SJ. Validation of a measure for adolescent self‐report of attention deficit disorder symptoms. Journal of Developmental and Behavioral Pediatrics 1996;17(4):211‐5. [PubMed] [Google Scholar]
- Santostafano S. A Biodevelopmental Approach to Clinical Child Psychology: Cognitive Controls and Cognitive Control Therapy. Wiley, 1978. [ISBN: 9780471753803] [Google Scholar]
- Saraswati S. Yoga Education for Children. AManual for Teaching Yoga to Children. Bihar School ofYoga. Munger: Bihar, 1990. [Google Scholar]
- Scahill L, Schwab‐Stone M. Epidemiology of ADHD in school‐age children. Child and Adolescent Psychiatric Clinics of North America 2000;9(3):541‐55. [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children's global assessment scale (CGAS). Archives of General Psychiatry 1983;40(11):1228‐31. [DOI] [PubMed] [Google Scholar]
- Shallice T. From Neuropsychology to Mental Structure. Cambridge: Cambridge University Press, 1988. [Google Scholar]
- Shaywitz SE, Shaywitz BA, Schnell C, Towle VR. Concurrent and predictive validity of the Yale Children's Inventory: an instrument to assess children with attentional deficits and learning disabilities. Pediatrics 1988;81(4):562‐71. [PubMed] [Google Scholar]
- Swanson J, Posner M, Fusella J, Wasdell M, Sommer T, Fan J. Genes and attention deficit hyperactivity disorder. Current Psychiatry Reports 2001;3(2):92‐100. [DOI] [PubMed] [Google Scholar]
- Walsh R, Roche L. Precipitation of acute psychotic episodes by intensive meditation in individuals with a history of schizophrenia. American Journal of Psychiatry 1979;136(8):1085‐6. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Wechsler intelligence scale for children. 3rd Edition. San Antonio, TX: Psychological Corporation, 1991. [Google Scholar]
- Wechsler D. Wechsler Individual Achievement Test Manual. San Antonio, TX: Psychological Corporation, 1992. [Google Scholar]
- Werry JS. Developmental hyperactivity. Pediatric Clinics of North America 1968;15:581‐99. [DOI] [PubMed] [Google Scholar]
- Weyandt LL, Iwaszuk W, Fulton K, Ollerton M, Beatty N, Fouts H, et al. The internal restlessness scale: performance of college students with and without ADHD. Journal of Learning Disabilities 2003;36(4):382‐9. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The ICD‐10 Classification of mental and behavioural disorders. Geneva and New York: World Health Organization, 1992. [Google Scholar]
- Wigal SB, Gupta S, Guinta D, Swanson JM. Reliability and validity of the SKAMP rating scale in a laboratory school setting. Psychopharmacology Bulletin 1998;34(1):47‐53. [PubMed] [Google Scholar]
- Zhang S, Faries DE, Vowles M, Michelson D. ADHD Rating Scale IV: psychometric properties from a multinational study as a clinician‐administered instrument. International Journal of Methods in Psychiatric Research 2005;14(4):186‐201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, Sheeran T, Young D. The Diagnostic Inventory for Depression: a self‐report scale to diagnose DSM‐IV major depressive disorder. Journal of Clinical Psychology 2004;60(1):87‐110. [DOI] [PubMed] [Google Scholar]


