Abstract
Background
Panic disorder can be treated with pharmacotherapy, psychotherapy or in combination, but the relative merits of combined therapy have not been well established.
Objectives
To review evidence concerning short‐ and long‐term advantages and disadvantages of combined psychotherapy plus antidepressant treatment for panic disorder with or without agoraphobia, in comparison with either therapy alone.
Search methods
The Cochrane Collaboration Depression, Anxiety and Neurosis Controlled Trials Registers (CCDANCTR‐Studies and CCDANCTR‐References) were searched on 11/10/2005, together with a complementary search of the Cochrane Central Register of Controlled Trials and MEDLINE, using the keywords antidepressant and panic. A reference search, SciSearch and personal contact with experts were carried out.
Selection criteria
Two independent review authors identified randomised controlled trials comparing the combined therapy against either of the monotherapies among adult patients with panic disorder with or without agoraphobia.
Data collection and analysis
Two independent review authors extracted data using predefined data formats, including study quality indicators. The primary outcome was relative risk (RR) of "response" i.e. substantial overall improvement from baseline as defined by the original investigators. Secondary outcomes included standardised weighted mean differences in global severity, panic attack frequency, phobic avoidance, general anxiety, depression and social functioning and relative risks of overall dropouts and dropouts due to side effects.
Main results
We identified 23 randomised comparisons (representing 21 trials, 1709 patients), 21 of which involved behaviour or cognitive‐behaviour therapies. In the acute phase treatment, the combined therapy was superior to antidepressant pharmacotherapy (RR 1.24, 95% confidence interval (CI) 1.02 to 1.52) or psychotherapy (RR 1.17, 95% CI 1.05 to 1.31). The combined therapy produced more dropouts due to side effects than psychotherapy (number needed to harm (NNH) around 26). After the acute phase treatment, as long as the drug was continued, the superiority of the combination over either monotherapy appeared to persist. After termination of the acute phase and continuation treatment, the combined therapy was more effective than pharmacotherapy alone (RR 1.61, 95% CI 1.23 to 2.11) and was as effective as psychotherapy (RR 0.96, 95% CI 0.79 to 1.16).
Authors' conclusions
Either combined therapy or psychotherapy alone may be chosen as first line treatment for panic disorder with or without agoraphobia, depending on patient preference.
Keywords: Humans, Agoraphobia, Agoraphobia/psychology, Agoraphobia/therapy, Antidepressive Agents, Antidepressive Agents/therapeutic use, Combined Modality Therapy, Combined Modality Therapy/methods, Panic Disorder, Panic Disorder/psychology, Panic Disorder/therapy, Psychotherapy, Psychotherapy/methods, Randomized Controlled Trials as Topic, Treatment Outcome
Psychotherapy combined with antidepressants for panic disorder
Psychotherapy plus antidepressant treatment were compared with each of the two individual treatments alone for panic disorder. At the end of the acute phase treatment, the combined therapy was superior to psychotherapy or antidepressant treatment alone. After termination of active treatment, the combined therapy was superior to antidepressants alone and was as effective as psychotherapy alone. Either combined therapy or psychotherapy alone may be chosen as first line treatment for panic disorder with or without agoraphobia, depending on patient preference.
Background
Panic disorder is characterised by recurrent, unexpected panic attacks and persistent concern about having an additional attack, or worry about the implications of an attack or its consequences. It is estimated to affect around 2% of the population for any one year and around 2% to 5% of the population sometime during their lifetime (Kessler 2006; Carlbring 2002). One third to one half of individuals diagnosed with panic disorder in community samples also have agoraphobia, although a much higher rate of agoraphobia is encountered in clinical samples (Weissman 1997). It is estimated to account for 0.5% of the global burden of disease for humankind in 2002, a percentage figure as great as epilepsy and greater than breast cancer, for example (WHO 2004).
Two broad categories of treatment have been shown to be effective in treating panic disorder with or without agoraphobia; one is psychotherapy and cognitive‐behaviour therapy in particular, and the other is pharmacotherapy with antidepressants and benzodiazepines (Nathan 2002; APA 1998). It remains to be seen, however, whether combining these two effective forms of treatment confers any additional benefit over and above either of the treatments alone, especially with regard to long‐term outcomes.
It is important to examine this issue for many reasons. Firstly, typical response rates for these two effective therapies are only in the range of 50% to 70% at the end of acute phase treatment. Moreover, it is now increasingly recognised that pharmacotherapy alone tends to result in substantial relapse rates, not only when discontinued (Mavissakalian 2002; Pecknold 1988), but even when maintained at adequate dosage (Simon 2002; Toni 2000). Cognitive‐behaviour therapy may not always be able to prevent relapses over the long term either (Burns 1986; Fava 2001). We are therefore in need of "stronger" treatment. Secondly, combination therapy appears to be practiced very frequently in the real world, possibly because of the above‐mentioned inadequacy of either of the monotherapies. For example, Schmidt et al reported that, at their research laboratory, 75% of patients with panic disorder had received at least one medication and 65% were receiving medication at the time of their initial assessment (Schmidt 2001).
However, the evidence regarding the incremental effectiveness of combined therapy remains inconclusive. Several reviews can be found in the literature but their conclusions have been variable, with some favouring the combination therapy (Mattick 1990; van Balkom 1997; Pollack 2003), some favouring monotherapy (Taylor 2000; Westra 1998; Gould 1995) and others with mixed or guarded conclusions (Clum 1993; Telch 1994; APA 1998; Schmidt 1999; Schmidt 2001). Unfortunately most of these reviews have been either unsystematic or narrative only (Schmidt 1999; Schmidt 2001; Taylor 2000; APA 1998) or, where meta‐analytic summary was essayed, did not focus on head‐to‐head comparisons (van Balkom 1997; Gould 1995; Clum 1993; Mattick 1990). The precariousness of comparing different treatment conditions by way of their within‐group effect sizes or between‐group effect sizes against placebo conditions has been well documented (Bucher 1997; Klein 2000; Song 2003).
Not only does the incremental effectiveness remain unproven, but there is a possibility that combination harms. Several reports have suggested that benzodiazepines are not only associated with several disadvantages including sedation, reduced coordination and development of dependence but that they may actually interfere with and detract from cognitive‐behavioural interventions (van Balkom 1996; Brown 1995; Otto 1996; Westra 1998). We do not yet know if the same applies to the other form of pharmacotherapy, i.e. antidepressant medication, although there are some suggestive findings (Barlow 2000).
Therefore, the primary objective of this systematic review is to evaluate and synthesise evidence from randomised controlled trials that examined effectiveness and adverse effects of combined treatment by psychotherapy and antidepressants in comparison with either therapy alone in the treatment of panic disorder with or without agoraphobia. This review focuses on antidepressants, and a separate companion review focuses on benzodiazepines (Watanabe 2005).
Objectives
The primary objective of the present systematic review is to evaluate evidence from randomised controlled trials that examined effectiveness and adverse effects of combined treatment by psychotherapy and antidepressants in comparison with either therapy alone in the treatment of panic disorder with or without agoraphobia.
Methods
Criteria for considering studies for this review
Types of studies
All relevant randomised controlled trials (RCTs). Quasi‐randomised trials, such as those allocated by using alternate days of the week, were excluded. For trials using a cross‐over design, we used the first comparative phase only.
Types of participants
Adult patients with panic disorder with or without agoraphobia, diagnosed according to any of the following criteria: Feighner criteria, Research Diagnostic Criteria, DSM‐III, DSM‐III‐R, DSM‐IV or ICD‐10. When the study eligibility focused on agoraphobia, rather than panic disorder, and was operationally diagnosed according to the above‐named criteria and when it could be safely assumed that at least some of the patients were suffering from panic disorder as defined by the above criteria, such a study could still be included. An informed estimate tells us that over 95% of patients with agoraphobia seen clinically suffer from panic disorder as well (Goisman 1995). However, the effect of their inclusion was examined in a sensitivity analysis. The patients had to be 18 years old or older. Patients with comorbid physical or mental disorders were not excluded but the effect of including these patients was examined in sensitivity analyses.
Types of interventions
Trials were included if they compared the combined psychotherapy and antidepressant pharmacotherapy against either of these single approaches for at least one week.
The following individual, group, extensive or intensive psychological treatments were included: (i) Behaviour therapy that used some kind of exposure. (ii) Cognitive therapy that used some kind of cognitive restructuring. (iii) Cognitive‐behaviour therapy that contained both cognitive and behavioural therapy elements. (iv) Psychodynamic therapy that used interpretation of current maladaptive patterns as repetition of earlier childhood experiences. (v) Any other psychological approach, such as Rogerian therapy, Morita therapy or Eye Movement and Desensitisation Reprocessing (EMSR).
The following antidepressants were included: (i) Tricyclic antidepressants (TCA): imipramine, amitriptyline, clomipramine, desipramine, nortryptiline, doxepin, dosulepin/dothiepin, trimipramine, lofepramine. (ii) Selective serotonin reuptake inhibitors (SSRI): fluoxetine, sertraline, paroxetine, citalopram, fluvoxamine, escitalopram. (iii) Monoamine oxidase inhibitors (MAOI): phenelzine, isocarboxazide, tranylcipromine, moclobemide, brofaromine. (iv) Serotonin‐noradrenaline reuptake inhibitors (SNRI): venlafaxine, milnacipran. (v) Others: bupropion, trazodone, nefazodone, mianserin, maprotilin, mirtazapine.
Studies where irregular use of benzodiazepines took place were included. Excluding such studies would be meaningless because it has been documented that a minority of patients take benzodiazepines and antidepressants surreptitiously when they are prohibited by the protocol (Clark 1990). Studies where benzodiazepines were regularly administered at a constant dosage for long‐time users were also included but the effect of this decision was examined in a sensitivity analysis. Studies where benzodiazepines were regularly administered as part of the study medication were excluded.
The value of psychotherapy in helping medication discontinuation is not the focus of this review and, therefore, such trials were not included.
Types of outcome measures
(A) Effectiveness
(1) Short‐term, i.e. during the acute phase treatment which normally would last 2 to 4 months
(i) Our primary outcome was the rate of "response", i.e. substantial improvement from baseline as defined by the original investigators. Examples would be "very much or much improved" according to the Clinical Global Impression Change Scale, more than 40% reduction in the Panic Disorder Severity Scale score, and more than 50% reduction in the Fear Questionnaire Agoraphobia Subscale. (ii) Rate of "remission", i.e. satisfactory end‐state as defined by global judgement of the original investigators. Examples would be "panic free" and "no or minimal symptom" according to the Clinical Global Impression Severity Scale. (iii) Global judgement on a continuous scale. Examples would be Panic Disorder Severity Scale total score (0 to 28), Clinical Global Impression Severity Scale (1 to 7), Clinical Global Impression Change Scale (1 to 7), etc. When multiple measures were used, preference was given in the order as above, and the actual measure entered into meta‐analysis was indicated at the top of the listings in the Table of Included Studies. (iv) Frequency of panic attacks, as recorded, for example, by a panic diary. (v) Agoraphobia, as measured, for example, by Fear Questionnaire, Mobility Inventory, behavioural avoidance test etc. (vi) General anxiety, as measured, for example, by Hamilton Rating Scale for Anxiety, Beck Anxiety Inventory, State‐Trait Anxiety Index, Sheehan Patient‐Rated Anxiety Scale, Anxiety Subscale of SCL‐90‐R etc. (vii) Depression, as measured, for example, by Hamilton Rating Scale for Depression, Beck Depression Inventory, Depression Subscale of SCL‐90‐R etc. (viii) Social functioning, as measured, for example, by Sheehan Disability Scale, Global Assessment Scale, Social Adjustment Scale‐Self Report etc. (ix) Quality of life, as measured for example by SF‐36, SF‐12 etc. (x) Patient satisfaction with treatment. (xi) Economic costs.
(2) Long‐term, i.e. after the acute phase treatment
(2.1) On continued treatment
(i) Response/remission on continued treatment. Although some studies reported on remission but not on response, we also pooled such studies under the outcome "response/remission", in order to increase statistical power. (ii) Quality of life. (iii) Patient satisfaction.
(2.2) On treatment discontinuation
(i) Withdrawal symptoms on treatment discontinuation within one month. (ii) Response/remission after treatment discontinuation at 6 to 24 months. Although some studies reported on remission but not on response, we pooled such studies as well under the outcome "response/remission" in order to increase statistical power.
(B) Adverse effects
(i) Total number of dropouts for any reason as a proxy measure of treatment acceptability. (ii) Number of dropouts due to adverse effects. (iii) Number of patients experiencing at least one adverse effect.
Search methods for identification of studies
1. Electronic search We searched the Cochrane Collaboration Depression, Anxiety and Neurosis Controlled Trials Registers (CCDANCTR‐Studies and CCDANCTR‐References), a study‐based register of randomised trials incorporating results of group searches of MEDLINE (1966 onwards), EMBASE (1980 onwards), CINAHL (1982 onwards), PsycINFO (1974 onwards), PSYNDEX (1977 onwards) and LILACS (1982 to 1999), and conducted handsearches of major psychiatric and medical journals (see Collaborative Review Group Search Strategy). Because the concomitant administration of psychotherapy was often either not mentioned in the abstract or indexed in the database, we used the following simple search terms: panic AND antidepressants, which included: CCDANCTR‐Studies (searched on 11/10/2005) Diagnosis = Panic and Free‐text = "Antidepressive Agents" or "Monoamine Oxidase Inhibitors" or "Selective Serotonin Reuptake Inhibitors" or "Tricyclic Drugs" or Acetylcarnitine or Alaproclate or Amersergide or Amiflamine or Amineptine or Amitriptyline or Amoxapine or Befloxatone or Benactyzine or Brofaromine or Bupropion or Butriptyline or Caroxazone or Chlorpoxiten or Cilosamine or Cimoxatone or Citalopram or Clomipramine or Clorgyline or Clorimipramine or Clovoxamine or Deanol or Demexiptiline or Deprenyl or Desipramine or Dibenzipin or Diclofensine or Dothiepin or Doxepin or Duloxetine or Escitalopram or Etoperidone or Femoxetine or Fluotracen or Fluoxetine or Fluparoxan or Fluvoxamine or Idazoxan or Imipramine or Iprindole or Iproniazid or isocarboxazid or Litoxetine or Lofepramine or Maprotiline or Medifoxamine or Melitracen or Metapramine or Mianserin or Milnacipran or Minaprine or Mirtazapine or Moclobemide or Nefazodone or Nialamide or Nomifensine or Nortriptyline or Noxiptiline or Opipramol or Oxaflozane or Oxaprotiline or Pargyline or Paroxetine or Phenelzine or Piribedil or Pirlindole or Pivagabine or Prosulpride or Protriptyline or Quinupramine or Reboxetine or Rolipram or Sertraline or Setiptiline or Teniloxine or Tetrindole or Thiazesim or Thozalinone or Tianeptine or Toloxatone or Tomoxetine or Tranylcypromine or Trazodone or Trimipramine or Venlafaxine or Viloxazine or Viqualine or Zimeldine
CCDANCTR‐References (searched on 11/10/2005) Keyword = Panic and Free‐text = "Antidepressive Agents" or "Monoamine Oxidase Inhibitors" or "Selective Serotonin Reuptake Inhibitors" or "Tricyclic Drugs" or Acetylcarnitine or Alaproclate or Amersergide or Amiflamine or Amineptine or Amitriptyline or Amoxapine or Befloxatone or Benactyzine or Brofaromine or Bupropion or Butriptyline or Caroxazone or Chlorpoxiten or Cilosamine or Cionotome or Citalopram or Clomipramine or Clorgyline or Chlormerodrin or Scopolamine or Deanol or Demerit or Deprenyl or Desipramine or Dibenzyline or Diclofenac or Dothiepin or Doxepin or Sulbentine or Sialograms or Metroperitoneal or Entoretina or Fluorescent or Fluoxetine or Guaroa or Fluvoxamine or Midrazolam or Imipramine or Iprindole or Iproniazid or isocarboxazid or Alloxanthine or Lobelamine or Maprotiline or Etidocaine or Melitracen or Metathrombin or Mianserin or Mulaire or Inapsine or Oracaine or Moclobemide or Nefazodone or Nialamide or Nomifensine or Nortriptyline or Mexitil or Opipramol or Oxaflozane or Oxaprotiline or Pargyline or Paroxetine or Phenelzine or Piribedil or Pirlindole or Pivagabine or Prosulpride or Protriptyline or Quinupramine or Reboxetine or Rolipram or Sertraline or Setiptiline or Teniloxine or Tetrindole or Thiazesim or Thozalinone or Tianeptine or Toloxatone or Tomoxetine or Tranylcypromine or Trazodone or Trimipramine or Venlafaxine or Viloxazine or Viqualine or Zimeldine We therefore sought all randomised controlled trials with antidepressants for panic disorder and manually checked to ascertain if they had co‐administered any credible psychotherapy. The searches were conducted with the assistance of the Depression, Anxiety and Neurosis Review Group.
Two complementary searches for additional relevant trials were conducted on the Cochrane Central Controlled Trials Register with the search terms: panic AND antidepress*, and on MEDLINE using the search terms: panic disorder [MeSH] AND psychotherapy [MeSH] limited to Randomized Controlled Trial [Publication type]. No language restriction was imposed.
2. Reference search The references of all selected studies were inspected for more published reports and citations of unpublished research. In addition, relevant review papers, both systematic and traditional ones, were checked (Schmidt 2001; Taylor 2000; Schmidt 1999; APA 1998; van Balkom 1997; Gould 1995; Telch 1994; Mavissakalian 1993; Mattick 1990).
3. SciSearch All the selected studies were sought as a citation in the SciSearch database in order to identify more studies.
4. Personal communication To ensure that all RCTs were identified, the authors of significant papers and other experts in the field were contacted (Isaac Marks and authors of included trials).
Data collection and analysis
1. Selection of trials Two review authors (TAF and NW) examined titles and abstracts of references identified by the electronic search strategies described above to check whether the study was likely to be relevant. Full articles of all the studies identified by either of the two review authors were then obtained and inspected by the same two review authors for trials meeting the following broad and simple criteria: (1) Randomised trial. (2) Panic disorder as diagnosed by operationalised criteria. (3) Combination of any form of psychotherapy plus antidepressant versus either of these treatments. Two independent review authors (TAF and NW) then examined the strict eligibility of these broadly defined trials. The eligibility criteria consisted of five items which operationalised the above‐listed criteria for considering studies. The inter‐rater reliability of these judgements was evaluated by means of weighted kappas.
2. Quality assessment Two independent review authors (TAF and NW) assessed the methodological quality of the selected studies. The criteria for the quality assessment were based on the recommendations of the Cochrane Reviewers' Handbook (Clark & Oxman 2000). Firstly, on the basis of explicit criteria (available from the authors upon request), quality of randomisation in treatment conditions was assessed, and trials were assigned to one of the three categories: A: adequate concealment, B: unclear concealment, and C: inadequate concealment. There is empirical evidence that quality of randomisation can produce biased results (Schulz 1995, Moher 1998, Chalmers 1983, Egger 2003). Secondly, we also rated the study as 'blinded' when at least one outcome measure was assessed by an independent assessor blind to treatment allocation and 'unblinded' when the outcomes were assessed by someone who was aware of the allocated treatment. There is some evidence to suggest that trials that are not double blind yield biased results (Schulz 1995, Coldiz 1989). In addition to the methodological quality assessment of the selected trials, we assessed the adequacy of the psychotherapy according to the following criteria. We determined the quality of the administered psychotherapy according to the following criteria: A, when the psychotherapy alone arm was shown to be superior to the placebo arm in the same trial or when the same group of investigators had proved effectiveness in a separate randomised controlled trial; B, when the conduct of psychotherapy was examined by a third reviewer through audiotapes etc; and C, when the authors gave sufficiently detailed descriptions of the therapy procedure. We did not include trials which did not give detailed descriptions of the psychotherapies they administered. The effect of including studies with lower quality ("unblinded" for blinding, and C on adequacy of psychotherapy) was examined in a sensitivity analysis.
3. Data extraction Two review authors (RC and NW) independently extracted data from the original reports using data extraction forms. Any disagreement was resolved by consensus between the two or, where necessary, between all three review authors. Some studies did not provide response rates but reported the baseline and endpoint means and standard deviations (SD) of their global severity, agoraphobia and/or panic frequency measures. In such instances, response rates can be imputed by calculating the percentage of subjects scoring less than half of the baseline score from the endpoint mean and SD. This imputation method has been shown to work excellently when imputing response in depression trials, the agreement between the imputed and actual values being an ANOVA ICC of 0.97 (95% CI 0.95 to 0.98) (Furukawa 2005).
4. Data synthesis Data were entered into Review Manager 4.2 and double‐checked for accuracy by TAF. For dichotomous outcomes, relative risks and their 95% confidence intervals were calculated using a random‐effects model. The random‐effects model's relative risk has been shown to be superior in clinical interpretation and external generalisation compared to fixed‐effects models and odds ratios or risk differences (Furukawa 2002). For dichotomous outcomes, we used intention‐to‐treat (ITT) analyses according to the following principle. When data on dropouts were carried forward and included in the efficacy evaluation by the last‐observation‐carried‐forward (LOCF) in the original reports, they were included as such. When drop outs were excluded from any assessment in the primary studies (for example, those who never returned for assessment after randomisation), they were considered to be non‐responders in both active and comparison groups. The same principles applied to outcomes at or after end of maintenance treatment, because we were interested in the percentage of patients remaining well among those who had entered the trials at all, and not among those who successfully entered and/or finished the maintenance treatment phase. For continuous outcomes, the standardised weighted mean difference (WMD) and their 95% confidence intervals were calculated using a random‐effects model. When the study failed to report SD, it was imputed from the other studies in this review that employed the same scale (Furukawa 2006). The ITT approach was not feasible as studies only perform LOCF or endpoint analyses. Therefore, continuous outcomes were analysed on an endpoint basis, including only patients with a final assessment or with a last observation carried forward to the final assessment.
5. Assessment of heterogeneity Heterogeneity between studies was assessed by the I‐squared statistic, the Q statistic and by visual inspection of the results. If significant heterogeneity was noted, sources were investigated (I‐squared > 50% was taken to be indicative of moderate heterogeneity (Higgins 2003); due to the known low sensitivity of the Q statistic, P < 0.10 was taken to be suggestive of heterogeneity).
6. Funnel plot analysis Funnel plot analysis was performed to check for small study effects, including publication bias.
7. Subgroup analyses Subgroup analyses should be performed and interpreted with caution because multiple analyses lead to false positive conclusions (Oxman 1992). However, we performed the following subgroups analyses, where possible, for the following a priori reasons: (1) For each type of psychotherapy separately (behaviour therapy, cognitive therapy, cognitive‐behaviour therapy and psychodynamic therapy and others), because they may not, a priori, have the same degree of effectiveness when administered alone or the same degree of combinability with pharmacotherapy. (2) For classes of antidepressants, such as tricylic antidepressants, selective serotonin reuptake inhibitors, and others. (3) For patients with agoraphobia and for those without agoraphobia, because the same treatment may have differential effectiveness with regard to panic and agoraphobia. (4) For patients with and without depressive disorder, because it is likely that antidepressants may confer more benefit for those patients with panic disorder comorbid with depression.
8. Sensitivity analyses The following sensitivity analyses were planned a priori. By limiting the studies for inclusion to those with higher quality, we examined if the results changed and aimed to check for the robustness of the observed findings by limiting to: (1) Randomised controlled trials where at least one measure was assessed by an independent assessor blind to treatment allocation. (2) Randomised controlled trials where the administered psychotherapy had a demonstrated effectiveness rating of A or B according to the above criteria. (3) Randomised controlled trials which used operational diagnostic criteria for panic disorder with or without agoraphobia. (4) Studies whose participants were clearly without significant psychiatric or physical comorbidities including primary or secondary depressive disorders. (5) Studies whose protocols explicitly prohibited concomitant use of benzodiazepines. According to Clark 1990, 10% to 20% of those assigned to placebo or imipramine arms in a randomised controlled trial took explicitly prohibited anxiolytic medication.
Results
Description of studies
The electronic search identified 139 studies from the CCDANCTR, an additional 164 from the CCCTR and 35 from MEDLINE. Browsing their titles and abstracts, 135 articles were identified by either of the two independent review authors (TAF and NW) as possible candidates, and their full copies were obtained. The inter‐rater reliability of the two raters with regard to the first‐stage broad criteria was percentage agreement = 91% and kappa = 0.79 (95% CI 0.68 to 0.90). Discrepancies were resolved by consensus. Two independent review authors (TAF and NW) then examined the strict eligibility of these 42 papers, representing 20 RCTs. The inter‐rater reliability of these strict eligibility criteria was percentage agreement = 94% (weighted kappa = 0.35, 95% CI 0.06 to 0.64). Disagreement was resolved by consensus between the two review authors. Ba 1999 was excluded because the investigators prescribed both an antidepressant and alprazolam at the same time as a pharmacological intervention. Therefore we arrived at 19 studies that compared the combined therapy against monotherapy.
Once this preliminary list of selected studies became available, their references, along with references of other relevant review papers, were checked by TAF for further reports and four additional studies were identified (Agras 1991; Sheehan 1980a; Solyom 1981; Lipsedge 1973). All the selected studies were sought as a citation in the SciSearch database; seven additional articles reported on already identified trials, and one new trial was identified (Johnston 1995). Authors of significant papers and other experts in the field were contacted, who were able to identify no further studies. When the five additional studies were examined for their strict eligibility, Agras 1991 reported that their randomisation procedure was flawed and they could not obtain groups with comparable baseline characteristics (personal communication). Solyom 1981 did not report separate results for their social phobia and agoraphobia patients; the original author was contacted by telephone but could not provide suitable data. Lipsedge 1973 did not use operational diagnostic criteria; moreover, they used iproniazid, which has some MAO inhibiting effect, but which is not a widely recognised antidepressant.
All total, we identified 21 studies which satisfied the strict eligibility and validity criteria. Because two studies provided two comparisons each (Mavissakalian 1986a; Mavissakalian 1986b; Sheehan 1980a; Sheehan 1980b), we had 23 comparisons from the 21 studies, comprising 1709 participants altogether.
1. Participants For diagnostic criteria, four studies used DSM‐IV panic disorder with or without agoraphobia, nine studies used DSM‐III‐R panic disorder with or without agoraphobia and three studies used DSM‐III agoraphobia with panic disorder. Seven studies (Johnston 1995; Marks 1983; Mavissakalian 1983; Sheehan 1980a; Sheehan 1980b; Zitrin 1980; Zitrin 1983) focused on agoraphobia, but contained descriptions indicating that the participants were suffering from panic attacks as well (e.g., moderate to high scores on measures of panic attacks); they were therefore included in the present meta‐analysis.
Only one study (Barlow 2000) focused on patients with panic disorder without agoraphobia. On the other hand, 13 studies (de Beurs 1995; Fava 1997; Johnston 1995; Loerch 1999; Marks 1983; Mavissakalian 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sheehan 1980a; Sheehan 1980b; Telch 1985; Zitrin 1980; Zitrin 1983) focused on patients with panic disorder with agoraphobia. In the remaining studies, either the percentage of participants with agoraphobia was not specified or, when it was given, between 42% and 85% of participants suffered from agoraphobia.
Typically, the majority of the participants were women, and their average age was in the 30s. They had suffered from panic disorder for 5 to 10 years.
Eleven studies explicitly limited their participants to those without significant comorbid psychiatric (including depressive) and medical comorbidities (Loerch 1999; Marks 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sharp 1996; Zitrin 1983; Oehrberg 1995; Spinhoven 1996; Stein 2000; Telch 1985; Zitrin 1980). The other studies included patients with major depression (primary or secondary to panic disorder) or personality disorders. No study focused on patients with comorbid panic disorder and depression, or reported results separately for such a sub‐population.
2. Interventions Twelve studies administered behaviour therapy that consisted of exposure and/or breathing retraining and/or relaxation exercises (de Beurs 1995; Fava 1997; Johnston 1995; Marks 1983; Mavissakalian 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sheehan 1980a; Sheehan 1980b; Telch 1985; Zitrin 1980; Zitrin 1983). No study used narrowly‐defined cognitive therapy relying only on cognitive restructuring. Nine studies administered cognitive‐behaviour therapy consisting of both behaviour and cognitive therapy elements (Azhar 2000; Barlow 2000; Fahy 1992; Kampman 2002; Loerch 1999; Oehrberg 1995; Sharp 1996; Spinhoven 1996; Stein 2000). For two studies, their psychotherapies were classified in the "psychodynamic and others" category: Berger 2004 administered cognitive‐interpersonal group therapy, involving elements of cognitive‐behaviour therapy and interpersonal psychotherapy; Wiborg 1996 used brief dynamic psychotherapy without encouraging exposure.
Six studies used a psychotherapy alone arm (de Beurs 1995; Fava 1997; Azhar 2000; Barlow 2000; Sharp 1996; Spinhoven 1996), whereas 17 studies used a psychotherapy plus placebo arm (de Beurs 1995; Johnston 1995; Marks 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sheehan 1980a; Sheehan 1980b; Telch 1985; Zitrin 1980; Zitrin 1983; Barlow 2000; Fahy 1992; Kampman 2002; Loerch 1999; Oehrberg 1995; Sharp 1996; Stein 2000).
With regard to medications, 14 studies used tricyclic antidepressants (imipramine in ten, clomipramine in three, trazodone in one study), seven studies used selective serotonin‐reuptake inhibitors (paroxetine in four, fluvoxamine in three), and two other studies used monoamine oxidase inhibitors (moclobemide and phenelzine).
The typical length of the acute phase active treatment was between 8 and 12 weeks; two studies were shorter (Fahy 1992 and Spinhoven 1996 lasted six weeks only), and two studies were much longer (20 weeks for Berger 2004 and 26 weeks for Zitrin 1983). Seven studies took explicit caution for the study participants not to take benzodiazepines during the trial (Fahy 1992; Loerch 1999; Marks 1983; Mavissakalian 1983; Oehrberg 1995; Sharp 1996; Sheehan 1980a; Sheehan 1980b; Stein 2000). Three studies (Oehrberg 1995; Stein 2000; Barlow 2000) screened the urine for surreptitious benzodiazepine use but in the others the success of this prohibition was not ascertained.
Five studies provided continuation treatment, in which the drug regimen of the acute phase treatment was continued (Johnston 1995; Marks 1983; Telch 1985; Wiborg 1996; Zitrin 1980). It was extremely important to know the outcomes of patients after the active treatment phases consisting of acute phase treatment and, in some cases, continuation treatment. Eleven studies provided follow‐up data for the study participants after discontinuation of active treatments (Barlow 2000; Berger 2004; de Beurs 1995; Fava 1997; Loerch 1999; Marks 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sharp 1996; Wiborg 1996; Zitrin 1983). The patients were mostly free to seek further treatment between trial termination and follow‐up assessment. Of the originally randomised cohorts, between 33% to 100% were successfully followed up at 6 to 24 months after termination of active treatment, and between 30% and 77% of these participants are reported to have received further treatment in the interim.
3. Outcomes Among the 21 included studies, there was no standard measurement instrument for panic disorder or no agreed‐upon definition of response or remission. We therefore used the following scale scores for meta‐analyses: Global severity of panic disorder was measured with PDSS (Barlow 2000), with CGI Severity and/or Change (Fahy 1992; Loerch 1999; Sharp 1996; Zitrin 1980; Zitrin 1983), or with the authors' original scales (de Beurs 1995; Mavissakalian 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sheehan 1980a; Sheehan 1980b; Wiborg 1996). Panic attack frequency/severity was measured by counting the number of panic attacks for a certain time period preceding assessment (Azhar 2000; Berger 2004; de Beurs 1995; Johnston 1995; Marks 1983; Oehrberg 1995; Spinhoven 1996; Stein 2000; Telch 1985) or with the authors' original scales (Fava 1997; Mavissakalian 1986a; Mavissakalian 1986b; Wiborg 1996; Zitrin 1980; Zitrin 1983). Agoraphobia was assessed with FQ Agoraphobia subscale (Fava 1997; Johnston 1995; Loerch 1999; Marks 1983; Mavissakalian 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sharp 1996; Stein 2000; Telch 1985), Mobility Inventory (Kampman 2002), Fear Survey Schedule (Sheehan 1980a; Sheehan 1980b) or with the authors' original scales (Berger 2004; de Beurs 1995; Fahy 1992; Spinhoven 1996; Wiborg 1996; Zitrin 1980; Zitrin 1983). General anxiety was measured with HAM‐A (Azhar 2000; Fahy 1992; Loerch 1999; Sharp 1996; Wiborg 1996), Beck Anxiety Inventory (Stein 2000), Zung Self‐Rating Anxiety Scale (Mavissakalian 1983; Mavissakalian 1986a; Mavissakalian 1986b; Oehrberg 1995), SCL Anxiety subscale (Sheehan 1980a; Sheehan 1980b), Taylor Manifest Anxiety ( Zitrin 1983), FQ General Anxiety (Kampman 2002) or with the authors' original scales (Berger 2004; de Beurs 1995; Fava 1997; Marks 1983). Depression was measured with HAM‐D (Azhar 2000; Fahy 1992; Loerch 1999; Marks 1983; Mavissakalian 1983; Wiborg 1996), MADRS (Sharp 1996), Beck Depression Inventory (Mavissakalian 1986a; Mavissakalian 1986b; Stein 2000; Telch 1985), SCL Depression subscale (Johnston 1995), Zung Self‐Rating Depression Scale (Sheehan 1980a; Sheehan 1980b; Spinhoven 1996 or with the authors' original scales (de Beurs 1995; Fava 1997; Zitrin 1983). Social functioning was reported in 13 studies; they used Sheehan Disability Scale (Berger 2004; Loerch 1999; Sharp 1996; Sheehan 1980a; Sheehan 1980b; Stein 2000; Wiborg 1996), SAS‐SR (Johnston 1995) and some ad hoc measures (Mavissakalian 1983; Mavissakalian 1986a; Mavissakalian 1986b; Zitrin 1980; Zitrin 1983).
The definition of response and remission varied from study to study. We therefore sought to re‐define "response" as substantial improvement from baseline, and "remission" as satisfactory end state. The operational definition of "response" then corresponded with "very much or much improved" on CGI Change (Berger 2004; Loerch 1999; Sharp 1996; Stein 2000; Zitrin 1980; Zitrin 1983), more than 40% reduction in the PDSS (Barlow 2000), more than 50% reduction in self‐rated severity of phobia (Mavissakalian 1983), more than 50% reduction in panic frequency (Oehrberg 1995) or some other original definitions by the authors (Kampman 2002; Marks 1983; Sheehan 1980a; Sheehan 1980b). In addition, we imputed response rates by the method described above in the Methods section by defining response as more than 40% reduction in the CGI Severity (Fahy 1992) or an ad hoc global severity scale (Wiborg 1996), more than 50% reduction in the FQ Agoraphobia subscale (de Beurs 1995; Johnston 1995; Telch 1985), more than 50% reduction in the self‐rated severity of phobia (Mavissakalian 1986a; Mavissakalian 1986b), or more than 50% reduction in the frequency of panic attacks (Azhar 2000; Spinhoven 1996). The validity of this imputation method was confirmed because the agreement between the actual values and the imputed values, when both were given in the original reports, was an ANOVA ICC of 0.93 (one‐way random, single rater, 95% CI 0.83 to 0.99). "Remission" was operationally defined as "panic free" (Berger 2004; de Beurs 1995; Fahy 1992; Fava 1997; Kampman 2002; Mavissakalian 1983; Oehrberg 1995; Sharp 1996; Stein 2000; Wiborg 1996), "no or minimal symptom" according to the Clinical Global Impression Severity Scale (Barlow 2000; Loerch 1999) or some other original definitions by the authors (Marks 1983; Mavissakalian 1986a; Mavissakalian 1986b; Sheehan 1980a; Sheehan 1980b; Zitrin 1980; Zitrin 1983).
No study reported on the quality of life, patient satisfaction and economic costs during the acute phase treatment or continuation treatment. Some studies reported the number of patients who dropped out due to side effects, but no study reported on the total number of patients reporting side effects or on the withdrawal symptoms upon discontinuation of treatment. Total number of dropouts during the acute phase treatment were in the range of 0% to 9% (Fava 1997; Stein 2000; Wiborg 1996), 10% to 19% (de Beurs 1995; Spinhoven 1996; Mavissakalian 1983; Kampman 2002; Oehrberg 1995), 20% to 29% (Telch 1985; Zitrin 1983; Azhar 2000; Spinhoven 1996; Berger 2004; Barlow 2000; Loerch 1999; Sharp 1996; Sheehan 1980a; Sheehan 1980b) and over 30% (Johnston 1995; Marks 1983).
4. Commercial involvement Four studies acknowledged financial support from pharmaceutical companies (de Beurs 1995; Fahy 1992; Loerch 1999; Sharp 1996); these companies marketed the drugs involved in the trials. Sharp 1996 had some drug company employees as co‐authors. Oehrberg 1995 did not acknowledge financial support from a drug company but three of the co‐authors were company employees.
See Tables of Excluded Studies and Included Studies for further details.
Risk of bias in included studies
With regard to validity, based on information from published materials, all but two (Mavissakalian 1986a; Mavissakalian 1986b) of the 23 comparisons scored B for allocation concealment. Personal contact with the original authors revealed two more trials with adequate concealment (Berger 2004; Wiborg 1996). Nineteen trials conducted blind outcome assessments, and four trials were unblinded (Azhar 2000; Berger 2004; Mavissakalian 1983; Spinhoven 1996). The inter‐rater reliability of these two validity criteria was a percentage agreement of 94% (kappa was incalculable because one rater's ratings were constant) for allocation concealment and 83% (weighted kappa = 0.51, 95% CI 0.16 to 0.87) for blinding; any disagreement was resolved by consensus between the two raters.
With regard to quality of the psychotherapies provided, only three studies scored A, i.e. provided direct evidence of operationalising an effective psychotherapy compared with a drug placebo arm; these were Barlow 2000, Loerch 1999 and Sharp 1996. Four more studies scored B, i.e. examined the adequacy of the psychotherapies through audiotapes; these were Kampman 2002, de Beurs 1995, Fava 1997 and Zitrin 1983.
Effects of interventions
1. Psychotherapy plus antidepressant versus antidepressant alone (1.1) Acute phase treatment Combining 322 patients in the psychotherapy plus antidepressant arm and 347 patients in the antidepressant alone arm from 11 studies, the combination arm was 1.24 (95% CI 1.02 to 1.52) times more likely to produce response at the end of two to four months of acute phase treatment than the antidepressant alone arm. The test for heterogeneity was significant with p = 0.05, and moderate with I‐squared at 44.9%. Furthermore, the funnel plot (Figure 1) was suggestive of some publication bias, with one small study reporting an extreme result (Telch 1985). When we omitted this outlying study and studies which used "psychodynamic and other" therapies (Berger 2004; Wiborg 1996), thus limiting the included studies to those employing behaviour or cognitive‐behaviour therapies, the RR was similar (RR 1.28, 95% CI 1.08 to 1.52) and there was no longer statistical heterogeneity (p = 0.18, I‐squared = 30.5%) or funnel plot asymmetry. The superiority of the combination therapy was no longer apparent, though, when we looked at the remission rates rather than the response rates (RR 1.12, 95% CI 0.84 to 1.48), possibly because of the smaller number of included studies (seven instead of 11 studies).
Figure 1.
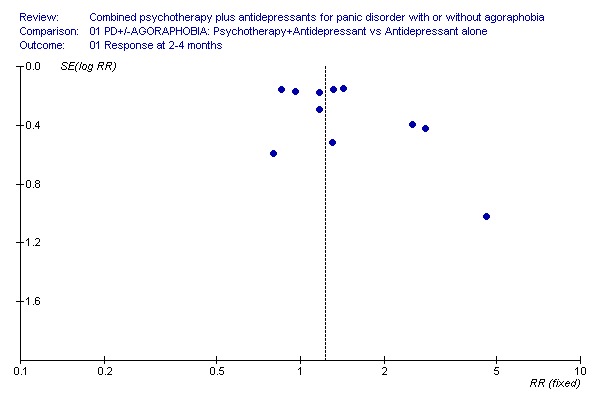
Funnel plot for response at 2‐4 months on PT+AD vs AD alone
The superiority of the combination therapy was corroborated by secondary analyses employing continuous data. The combination arm decreased global severity of the disorder (SMD ‐0.36, 95% CI ‐0.60 to ‐0.11), depression (SMD ‐0.52, 95% CI ‐0.76 to ‐0.28), and social malfunctioning (SMD ‐0.47, 95% CI ‐0.89 to ‐0.05). Non‐significant trends in favour of the combination therapy were noted for panic frequency (SMD ‐0.20, 95% CI ‐0.56 to 0.16), phobic avoidance (SMD ‐0.32, 95% CI ‐0.68 to 0.05) and general anxiety (SMD ‐0.43, 95% CI ‐0.88 to 0.03). Limiting the studies to those administering behaviour and cognitive‐behaviour therapies decreased heterogeneity but did not materially affect the overall effect estimates.
There was no difference in overall dropouts, or in dropouts due to side effects.
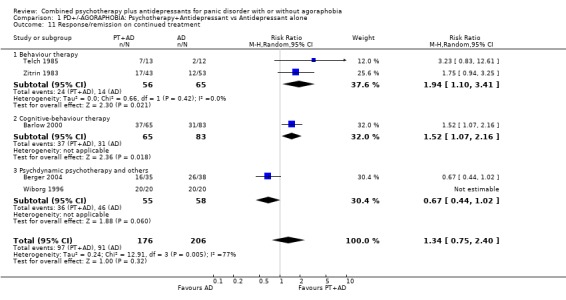
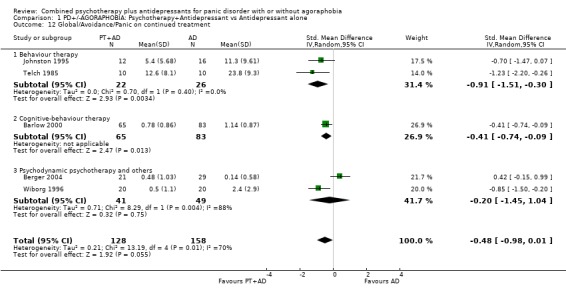
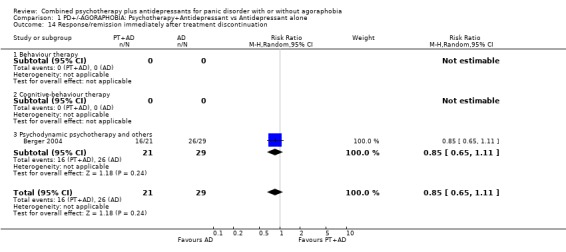
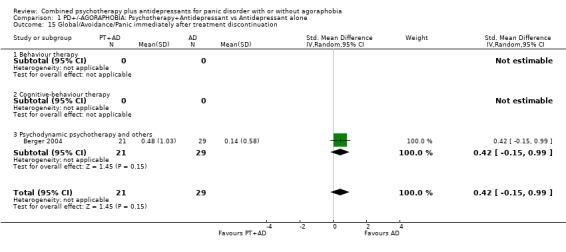
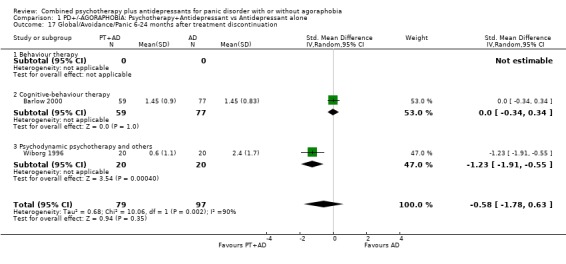
(1.2) Continued treatment There was strong heterogeneity (p = 0.005, I‐squared = 76.8%). Limiting the studies to behaviour and cognitive‐behaviour therapies, heterogeneity disappeared (p = 0.55, I‐squared = 0%), and the combination therapy was 1.63 (95% CI 1.21 to 2.19) times more likely to produce response/remission than the antidepressant alone treatment. The effect size in reducing global/avoidance/panic severity was also statistically significant in favour of the combination therapy (SMD ‐0.60, 95% CI ‐1.00 to ‐0.19). (1.3) After treatment discontinuation There was only one study that reported outcomes immediately after tapering paroxetine over four weeks (Berger 2004): no statistically significant difference was noted for dichotomous or continuous measures.
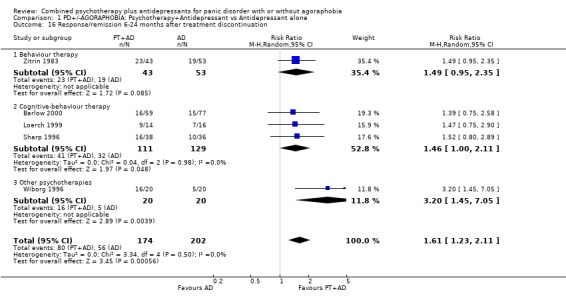
Five studies reported outcomes after 6 to 24 months of naturalistic follow‐up. Combining outcomes based on 376 participants, the combination therapy was still superior to antidepressants alone in terms of response/remission (RR 1.61, 95% CI 1.23 to 2.11). No heterogeneity was noted (p = 0.50, I‐squared = 0%). This advantage was not apparent on a continuous measure, probably because of the smaller number of trials reporting such outcomes.
2. Psychotherapy plus antidepressant versus psychotherapy alone Although the comparison psychotherapy plus antidepressant versus psychotherapy alone is theoretically different from the comparison psychotherapy plus antidepressant versus psychotherapy plus placebo (Hollon 1981), our meta‐analytic summaries for the former comparison were surprisingly in accordance with those for the latter comparison, save for the fact that the former comparison had a smaller number of studies and produced a smaller number of statistically significant results.
(2.1) Acute phase treatment Five studies compared, in total, 169 participants in the combination arm and 183 participants in the psychotherapy alone arm. None of the comparisons of effectiveness between these two arms were statistically significant, but their point estimates were very similar to those between psychotherapy plus antidepressant versus psychotherapy plus placebo. For example, RR of response was 1.09 (95% CI 0.91 to 1.32), that of remission was 1.22 (95% CI 0.99 to 1.51), and SMR for global severity was ‐0.31 (95% CI ‐0.63 to 0.02). None of these meta‐analytic comparisons were heterogeneous; unfortunately, there were too few studies for the funnel plot to be meaningful.
The two arms did not differ in terms of dropouts for any reason, but dropouts due to side effects were more frequent in the combination arm (RR 7.46, 95% CI 1.73 to 32.26).
(2.2) Continuation treatment There was only one study which examined the effect of continued treatment (Barlow 2000). Again, the advantage of the combination therapy appeared to continue as long as the treatments were continued. Only the SMD was significant (‐0.46, 95% CI ‐0.80 to ‐0.13).
(2.3) After treatment discontinuation Two hundred and seventy two patients were assessed at 6 to 24 months after treatment discontinuation. Any advantage of the combination therapy seemed to disappear (RR 0.97, 95% CI 0.71 to 1.33).
3. Psychotherapy plus antidepressant versus psychotherapy plus placebo
(3.1) Acute phase treatment Comparing 550 patients in the psychotherapy plus antidepressant arm and 482 patients in the psychotherapy plus placebo arm from 17 studies, the former was 1.17 (95% CI 1.04 to 1.32) times more likely to produce response at the end of two to four months of acute phase treatment than the latter. The test for heterogeneity was not significant, with I‐squared of 12.0%. Funnel plot of response (Figure 2) was somewhat suggestive of publication bias, with one small study reporting results much in favour of the combination therapy (Telch 1985). Excluding it reduced heterogeneity further, and the RR was unaffected.
Figure 2.
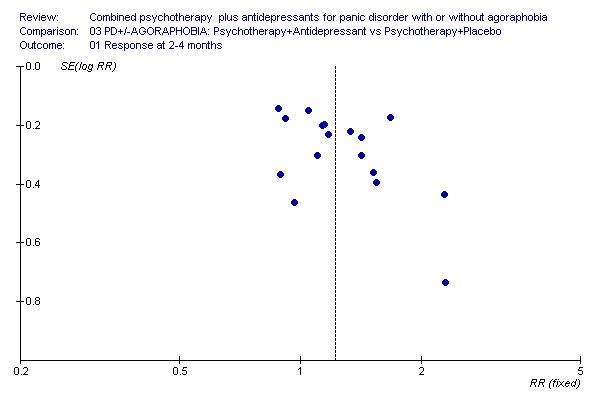
The same tendencies in favour of the combined therapy were noted for the remission rate (RR 1.30, 95% CI 1.10 to 1.54) and global severity (SMD ‐0.45, 95% CI ‐0.63 to ‐0.26). Looking at different aspects of panic disorder, although no statistically significant difference was found for frequency of panic attacks, the combination therapy was again significantly superior in terms of reduction in phobic avoidance, general anxiety, depression and social functioning.
Although the two arms did not differ in overall dropout rates, dropouts due to side effects were more frequent in the combined therapy arm than the psychotherapy plus placebo arm (random effects RR 2.43, 95% CI 1.23 to 4.81).
(3.2) Continuation treatment As long as the treatments were continued, the advantage of the combination therapy appeared to continue, as the response rate at the end of continuation treatment was non‐significantly in favour of the combination therapy (RR 1.29, 95% CI 1.03 to 1.62) and the global severity was significantly lower in the combination arm (SMD ‐0.65, 95% CI ‐0.97 to ‐0.33). The test for heterogeneity was not significant for either of these two meta‐analyses, although the I‐squared was 52.7% for the global severity; for the response rate, it was only 3.1%. During the continuation treatment, there were no differential dropout rates between the two arms.
(3.3) After treatment discontinuation In total, 658 patients were assessed at 6‐24 months after discontinuing treatment. Any advantage of the combination therapy seems to disappear, because neither the response rate (RR 0.96, 95%CI 0.79 to 1.16) nor the global severity measures were significantly different between the two arms. The test for heterogeneity was significant for neither of these meta‐analyses.
4. Psychotherapy plus antidepressant versus psychotherapy alone or plus placebo Here and in the following subgroup and sensitivity analyses, we examine the aggregate results of trials comparing psychotherapy plus antidepressant with psychotherapy alone and those comparing the former with psychotherapy plus placebo. Although these two types of comparisons are theoretically different from one another (Hollon 1981), our meta‐analytical summaries were remarkably similar for the acute phase and follow‐up evaluations. We therefore made a post hoc (i.e. after the data were collected) decision to increase the statistical power by combining them. When one study contributed both comparisons, i.e. one between the combination versus psychotherapy alone and another between the combination versus psychotherapy plus placebo, the name of the study was automatically given a suffix of i or ii; such was the case with Barlow 2000, de Beurs 1995 and Sharp 1996. We will here briefly summarize the combined results.
(4.1) Acute phase treatment Comparing 599 patients in the psychotherapy+antidepressant arm and 672 patients in the psychotherapy alone or +placebo arm from 23 studies, the former was 1.17 (95% CI: 1.05 to 1.31) times more likely to produce response at the end of 2‐4 months of acute phase treatment than the latter. The test for heterogeneity was not significant, with I‐squared of 12.6%.
The same tendencies in favour of the combined therapy were noted for the remission rate (RR1.26, 95%CI 1.10 to 1.44) and global severity (SMD ‐0.43, 95%CI ‐0.60 to ‐0.26). Looking at different aspects of panic disorder, although no statistically significant difference was found for frequency of panic attacks, the combination therapy was again significantly superior in terms of reduction in phobic avoidance, general anxiety, depression and social dysfunction.
Although the two arms did not differ in overall dropout rates, dropouts due to side effects were more frequent in the combined therapy arm than the psychotherapy alone or +placebo arm (RR 3.01, 95%CI 1.61 to 5.63).
5. Subgroup analyses (5.1) Types of psychotherapy For all the outcomes during the acute phase or continuation treatments or after treatment discontinuation, the confidence intervals of the pooled estimates of the effectiveness of behaviour therapy and cognitive‐behaviour therapy overlapped to a significant degree. Pooling these two kinds of psychotherapies together seldom resulted in statistically significant (p < 0.10) or substantive (I‐squared > 30%) heterogeneity.
The only exceptions were "Psychodynamic psychotherapy and others" category for the comparison psychotherapy plus antidepressant versus antidepressant alone. Berger 2004 administered what the authors called cognitive‐interpersonal group therapy for panic disorder, adapted from cognitive therapy and interpersonal psychotherapy. Wiborg 1996 administered brief dynamic psychotherapy, developed from concepts and techniques from Davanloo, Malan and Strupp. The results from these two studies were often qualitatively different not only from one another but also from the other studies administering behaviour or cognitive‐behaviour therapies, and combining them altogether often resulted in significant and substantive heterogeneity.
(5.2) Classes of antidepressants We performed a meta‐analysis of 14 studies that used TCAs and seven studies that used SSRIs as antidepressants. The pooled estimates of effect size of these two meta‐analyses were very similar to each other, and to the overall results. For the TCA meta‐analysis, only one out of 15 major outcomes had a qualitatively different estimate than the overall results; for the SSRI meta‐analysis, only two had such. In all these instances, the 95% confidence intervals were rather wide and overlapped significantly with the overall results.
(5.3) Panic disorder with agoraphobia versus panic disorder without agoraphobia We performed a meta‐analysis of 13 studies which focused on patients with agoraphobia only and compared their response/remission rates and changes in global severity. The point estimates of the pooled effectiveness were qualitatively different from those of the only study which focused on patients without agoraphobia (Barlow 2000) in only two out of 15 comparisons; in either case, the confidence intervals were very wide and there was overlap between those for agoraphobic patients and those for non‐agoraphobic patients.
(5.4) Patients without depression Because there was no study that focused on patients with comorbid panic disorder and depressive disorder, and no study reported results for depressed and non‐depressed participants separately, it was not possible to examine if the effect sizes were comparable when the participants suffered from depression or when they did not. We therefore performed a separate subgroup meta‐analysis of 12 studies which explicitly excluded subjects with comorbid psychiatric (including depressive) and medical conditions. The pooled estimates of effectiveness from those studies focusing on pure panic disorder patients were again largely in accordance with the overall estimates. In two out of 15 comparisons, the point estimates were qualitatively different, but the confidence intervals overlapped between those focusing on patients without comorbidities and those including all the trials found for this systematic review.
6. Sensitivity analyses (6.1) Limited to RCTs where at least one measure was assessed by an independent rater blind to treatment allocation. Nineteen studies were included. The pooled estimates were virtually identical to and qualitatively no different from the overall results.
(6.2) Limited to RCTs where the administered psychotherapy had a demonstrated effectiveness rating of A or B. Seven studies were included. Again the pooled estimates were virtually identical to and qualitatively no different from the overall results.
(6.3) Limited to RCTs that used operationalised diagnostic criteria for panic disorder with or without agoraphobia. Sixteen studies were included. Again the pooled estimates were virtually identical to and qualitatively no different from the overall results.
(6.4) Limited to studies whose participants were explicitly without significant psychiatric or medical comorbidities. Please see the subgroup analysis 5.4 above.
(6.5) Limited to studies whose protocols explicitly prohibited concomitant use of benzodiazepines. Nine studies could be included. There were three point estimates of effectiveness that were qualitatively different from the overall estimates out of 15 comparisons we made, but the small number of trials included allowed wide confidence intervals which overlapped significantly with those from the overall estimates. Otherwise the pooled point estimates were very similar between the overall results and those which prohibited benzodiazepines.
Discussion
The combined psychotherapy plus antidepressant treatment turned out to be robustly superior to either monotherapy for the acute phase treatment of panic disorder with or without agoraphobia. Taking the average response rates of between 50% to 70% for monotherapy, the pooled RR of 1.2 for the combination therapy was translated into NNTs between seven and ten. During the acute phase treatment, combination therapy resulted in more drop‐outs due to side effects than psychotherapy alone, and the NNH was around 26. The superiority of the combination appeared to hold as long as the antidepressant treatment was continued. There was, however, a differential advantage to the combination therapy vis‐a‐vis antidepressant alone or psychotherapy alone after the acute phase and continuation treatments were discontinued. The naturalistic follow‐up of the included RCTs demonstrated the sustained advantage of the combination therapy over antidepressant alone for 6 to 24 months but no differential effectiveness over psychotherapy alone at 6 to 24 months. At 6 to 24 months after treatment discontinuation, the combined therapy still showed an NNT around six over antidepressant pharmacotherapy alone. With regard to the comparison between the combination therapy and psychotherapy, there was no evidence of long‐term benefit of the former compared with the latter. In this respect, it is important to note that, despite recent admonitions from several experts (Foa 2002; Schmidt 2001; Taylor 2000), no disadvantage was observed for the combination therapy in the long term. These results were robust against several sensitivity analyses. We observed similar effectiveness for three of the four a priori defined subgroup analyses, namely for TCAs and SSRIs, for patients with agoraphobia and those without, and for patients without comorbid depression. In terms of differential effectiveness of various forms of psychotherapy, however, only behaviour therapy and cognitive‐behaviour therapy were homogeneously effective; the other two therapy modalities, brief psychodynamic therapy and cognitive‐interpersonal therapy, produced mixed results which lead to increased heterogeneity. Funnel plot analyses were suggestive of some publication bias. However, excluding outliers and limiting to behaviour and cognitive‐behaviour therapies, we were able to arrive at effect estimates which were more homogeneous, and yet materially no different from the overall results.
The major strengths of the present systematic review may be as follows: (1) We performed a systematic and comprehensive search of the relevant trials: we identified 23 comparisons from 21 studies, whereas the previous reviews were able to include a maximum of 11 to 13 studies (Telch 1994; Taylor 2000; Schmidt 2001). (2) We contacted the original authors for missing data and applied empirically validated imputation methods (Furukawa 2005; Furukawa 2006) to represent the identified trials in the meta‐analytic summary as much as possible. (3) We abode by the ITT principle when meta‐analysing dichotomous outcomes by counting all the dropouts as non‐responders. This policy is especially pertinent when considering the relative merits of the combination therapy over monotherapy in the long term, because we were interested in the number of patients doing well out of those who started the acute phase therapy, and not out of those who successfully completed it. (4) The a priori planned sensitivity analyses and subgroup analyses confirmed the overall findings.
Several possible weaknesses of the present study must also be highlighted: (1) Firstly, the funnel plot analyses suggested the possibility of publication bias among the identified trials. Excluding outliers, however, did not affect the pooled estimates. (2) Secondly, generalisability of the present findings beyond specialist psychiatric settings is not straightforward. Only one study (Sharp 1996) was conducted in the primary care setting but in this study patients were seen in their local GP clinics but by qualified clinical psychologists. Only two studies in this review assessed a psychological approach other than CBT. Where CBT therapists were not available, the research evidence, as accumulated and presented in this systematic review, would not be readily applicable to clinical practices. (3) Up until recently, there have not been widely accepted and validated rating scales for panic disorder, and many studies included in this systematic review used the authors' original scales. One study has indicated that rating scales which have not been validated or standardised are more likely to report statistically significant findings than those which are validated (Marshall 2000). Due to this lack of accepted assessment methods for panic disorder, the definition of "response" (our primary outcome) had to be operationalised by a variety of measures. However, these overall results were corroborated by analyses that focused on specific aspects of the symptoms of panic disorder. (4) Last, but most importantly, the comparability of the treatment arms after termination of acute phase and continuation treatments may have been compromised by the naturalistic nature of the follow‐ups. Except for Sharp 1996, which explicitly required patients not to receive any psychotropic drugs or psychotherapies, participants were free to seek further treatment between treatment termination and follow‐up assessments, and 30% to 77% did receive additional therapies. This does not necessarily undermine the comparability of the treatment arms per se; had the published studies reported number of patients who did well without further treatment, the interpretation of the relative merits of the combination versus single therapies would have been more straightforward. It is also important to note that overall only about half of the acute phase treatment studies included long term follow ups after the acute phase (five out of 11 that compared the combined treatment against antidepressant pharmacotherapy, and 12 out of 23 that compared the combination against psychotherapy alone or psychotherapy plus placebo).
It must be noted that our review does not answer the question of relative merits of combination versus sequential treatments. However, this is not, strictly speaking, a weakness of our study, because we did not plan our review to answer such questions. Given the present findings, some might argue for psychotherapy alone as first line treatment, and to consider combination therapy only when the former fails; it appears to be a viable option but remains unproven as far as the present review is concerned.
In conclusion, the current findings from the best available evidence suggest that either combined therapy or psychotherapy alone may be chosen as first line treatment for panic disorder with or without agoraphobia. Treatment decisions might depend on patient preference and values. Antidepressant pharmacotherapy alone is not to be recommended as first line treatment where appropriate resources are available. Although none of the included studies examined cost issues, economic consideration of years of medication versus one‐off psychological treatment would also favour inclusion of psychotherapy (Otto 2000). It remains, however, that where quality psychotherapy is hard to obtain (which unfortunately is the case for most parts of the world, and which therefore needs to be remedied through national health policies), antidepressant medication alone will still remain the only treatment accessible.
Authors' conclusions
Combined therapy is more effective than psychotherapy alone or antidepressant pharmacotherapy alone in the short term. Combined therapy is as effective as psychotherapy alone and is more effective than antidepressant pharmacotherapy alone in the long term. The strongest evidence existed for behaviour or cognitive‐behaviour therapy. It therefore follows that either combined cognitive‐behaviour and pharmacotherapy or cognitive‐behaviour therapy alone may be chosen as first line treatment for panic disorder with or without agoraphobia, depending on patient preference. Antidepressant pharmacotherapy alone is not to be recommended as first line treatment where appropriate resources are available.
Three lines of inquiry warrant further investigation. Firstly, in the acute phase treatment, if we adhere to the strict ITT principle, the remission rates are only slightly above 50% for combination therapy and slightly below 50% for psychotherapy alone. We need to develop strategies to deal with partial and non‐responders to these therapies. Secondly, for the long term outcome, our review suggested that combined therapy does not interfere with or detract from psychotherapy. Further research is necessary to confirm this finding by counting the number of patients completely recovered, without further treatment at follow up. Lastly, there are currently only limited data available on the effects of combining antidepressants with non‐cognitive‐behavioural therapies, such as psychodynamic and interpersonal therapies. In this review, the only available trial that involved psychodynamic therapy showed increased benefit when combined with antidepressants. This suggests the potential value of future trials designed to investigate this type of combination in the treatment of panic disorder.
Acknowledgements
The review was supported in part by Health and Labour Sciences Research Grants (Research on Health and Technology Assessment) H13‐018 from the Ministry of Health, Labour and Welfare, Japan.
Data and analyses
Comparison 1.
PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 11 | 669 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.02, 1.51] |
| 1.1 Behaviour therapy | 4 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.80, 1.40] |
| 1.2 Cognitive‐behaviour therapy | 5 | 336 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.05, 2.02] |
| 1.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.65, 1.85] |
| 2 Remission at 2‐4 months | 7 | 506 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.84, 1.48] |
| 2.1 Behaviour therapy | 2 | 114 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.62, 1.51] |
| 2.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.92, 2.14] |
| 2.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.28, 2.61] |
| 3 Global severity at 2‐4 months | 5 | 336 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.60, ‐0.11] |
| 3.1 Behaviour therapy | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.45, 0.44] |
| 3.2 Cognitive‐behaviour therapy | 2 | 206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.57, ‐0.02] |
| 3.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.33, ‐0.05] |
| 4 Frequency of panic attacks at 2‐4 months | 8 | 355 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.56, 0.16] |
| 4.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.49, 0.19] |
| 4.2 Cognitive‐behaviour therapy | 3 | 125 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐1.42, 0.50] |
| 4.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.53, 0.59] |
| 5 Phobic avoidance at 2‐4 months | 9 | 357 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.68, 0.05] |
| 5.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.01, ‐0.06] |
| 5.2 Cognitive‐behaviour therapy | 3 | 127 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.94, 0.44] |
| 5.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐1.15, 1.13] |
| 6 General anxiety at 2‐4 months | 7 | 356 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.88, 0.03] |
| 6.1 Behaviour therapy | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.60, 0.23] |
| 6.2 Cognitive‐behaviour therapy | 4 | 174 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.20, 0.18] |
| 6.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐2.12, 1.22] |
| 7 Depression at 2‐4 months | 8 | 281 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.76, ‐0.28] |
| 7.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.69, ‐0.01] |
| 7.2 Cognitive‐behaviour therapy | 3 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.10, ‐0.20] |
| 7.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.44, ‐0.14] |
| 8 Social malfunctioning at 2‐4 months | 6 | 246 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.89, ‐0.05] |
| 8.1 Behavour therapy | 3 | 118 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.85, 0.39] |
| 8.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.39, 0.12] |
| 8.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.46, ‐0.16] |
| 9 Dropouts for any reason within 2‐4 months | 11 | 669 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.75, 1.23] |
| 9.1 Behaviour therapy | 4 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.78, 1.88] |
| 9.2 Cognitive‐behaviour therapy | 5 | 336 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.55, 1.08] |
| 9.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [0.69, 2.45] |
| 10 Dropouts due to side effects within 2‐4 months | 6 | 345 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.45, 1.87] |
| 10.1 Behaviour therapy | 2 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.58] |
| 10.2 Cognitive‐behaviour therapy | 3 | 262 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.25, 2.68] |
| 10.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 11 Response/remission on continued treatment | 5 | 382 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.75, 2.40] |
| 11.1 Behaviour therapy | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.10, 3.41] |
| 11.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.07, 2.16] |
| 11.3 Psychdynamic psychotherapy and others | 2 | 113 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.44, 1.02] |
| 12 Global/Avoidance/Panic on continued treatment | 5 | 286 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.98, 0.01] |
| 12.1 Behaviour therapy | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.51, ‐0.30] |
| 12.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.74, ‐0.09] |
| 12.3 Psychodynamic psychotherapy and others | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.45, 1.04] |
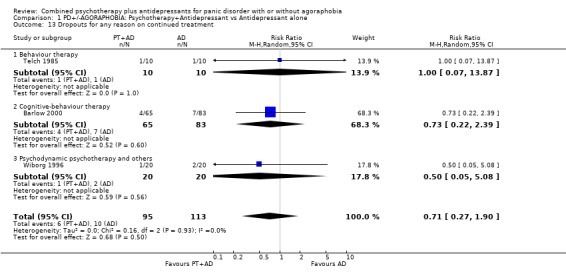
| 13 Dropouts for any reason on continued treatment | 3 | 208 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.27, 1.90] |
| 13.1 Behaviour therapy | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.22, 2.39] |
| 13.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.05, 5.08] |
| 14 Response/remission immediately after treatment discontinuation | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 14.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Psychodynamic psychotherapy and others | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 15 Global/Avoidance/Panic immediately after treatment discontinuation | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 15.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Psychodynamic psychotherapy and others | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 5 | 376 | Risk Ratio (M‐H, Random, 95% CI) | 1.61 [1.23, 2.11] |
| 16.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.95, 2.35] |
| 16.2 Cognitive‐behaviour therapy | 3 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.00, 2.11] |
| 16.3 Other psychotherapies | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.2 [1.45, 7.05] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.78, 0.63] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 1 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.34, 0.34] |
| 17.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐1.91, ‐0.55] |
Analysis 1.1.
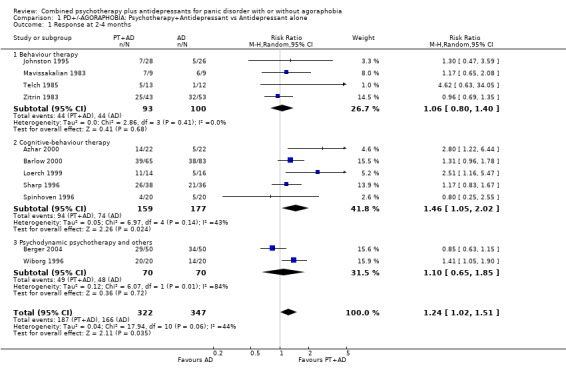
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 1.2.
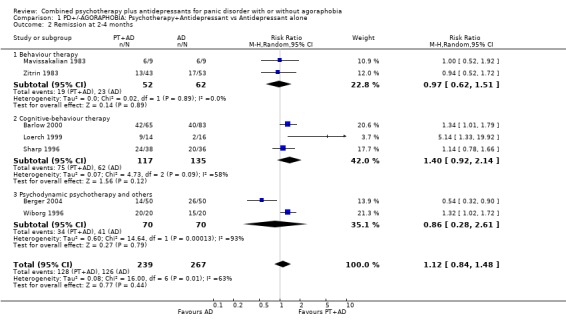
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 1.3.
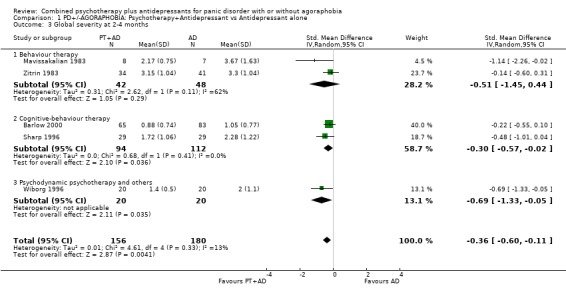
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 1.4.
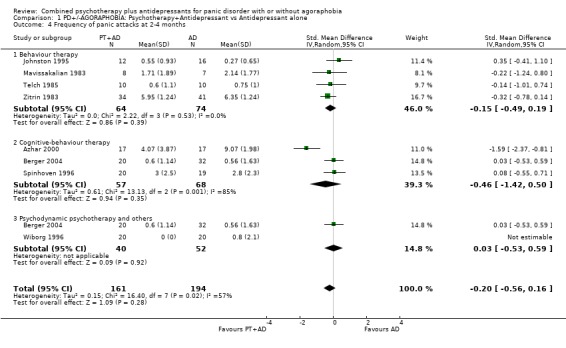
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 1.5.
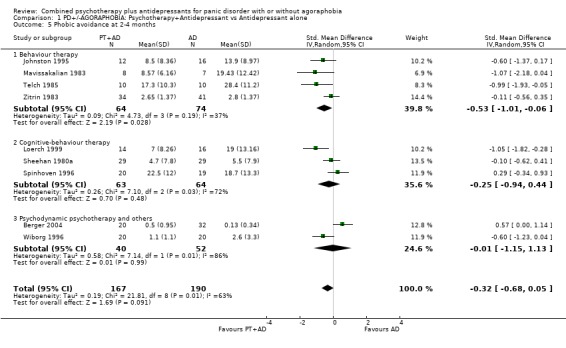
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 1.6.
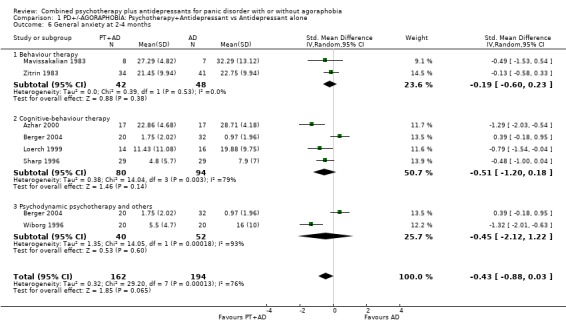
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 1.7.
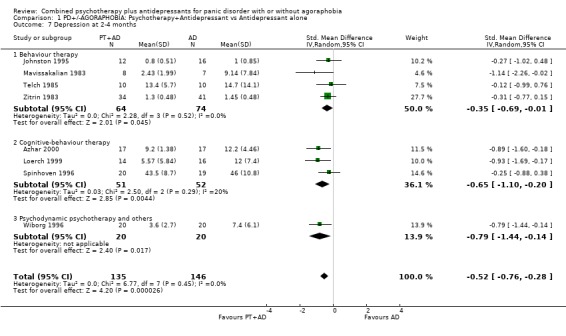
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 1.8.
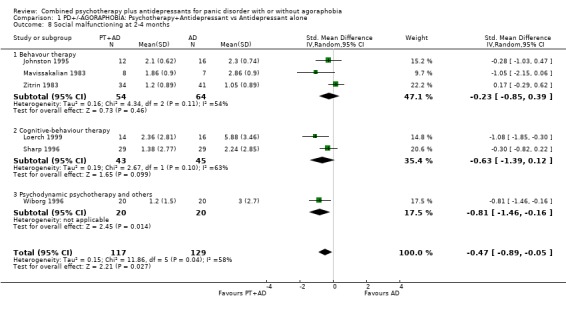
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social malfunctioning at 2‐4 months.
Analysis 1.9.
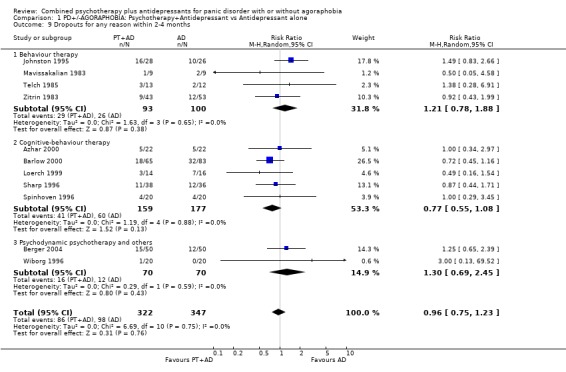
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 1.10.
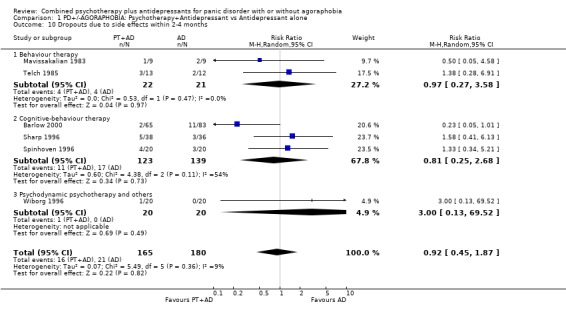
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 1.11.
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 1.12.
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 1.13.
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 1.14.
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 14 Response/remission immediately after treatment discontinuation.
Analysis 1.15.
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 15 Global/Avoidance/Panic immediately after treatment discontinuation.
Analysis 1.16.
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Analysis 1.17.
Comparison 1 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 2.
PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 6 | 366 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.85, 1.50] |
| 1.1 Behaviour therapy | 2 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.11, 7.30] |
| 1.2 Cognitive‐behaviour therapy | 4 | 307 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.90, 1.31] |
| 2 Remission at 2‐4 months | 4 | 282 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.97, 1.45] |
| 2.1 Behaviour therapy | 2 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.70 [0.16, 3.15] |
| 2.2 Cognitive‐behaviour therapy | 2 | 223 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.98, 1.52] |
| 3 Global severity at 2‐4 months | 3 | 238 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.63, 0.02] |
| 3.1 Behaviour therapy | 1 | 37 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.68 [‐1.34, ‐0.01] |
| 3.2 Cognitive‐behaviour therapy | 2 | 201 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.56, 0.13] |
| 4 Frequency of panic attacks at 2‐4 months | 4 | 122 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.45, 0.49] |
| 4.1 Behaviour therapy | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐1.30, 1.28] |
| 4.2 Cognitive‐behaviour therapy | 2 | 74 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.33, 0.58] |
| 5 Phobic avoidance at 2‐4 months | 4 | 150 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.73, 0.35] |
| 5.1 Behaviour therapy | 2 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐1.77, 1.22] |
| 5.2 Cognitive‐behaviour therapy | 2 | 99 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.44, 0.35] |
| 6 General anxiety at 2‐4 months | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.69, 0.35] |
| 6.1 Behaviour therapy | 2 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.44, 0.34] |
| 6.2 Cognitive‐behaviour therapy | 2 | 93 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.32, 0.49] |
| 7 Depression at 2‐4 months | 4 | 125 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.15, 0.12] |
| 7.1 Behaviour therapy | 2 | 51 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.94 [‐1.62, ‐0.25] |
| 7.2 Cognitive‐behaviour therapy | 2 | 74 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐1.12, 0.49] |
| 8 Social malfunctioning at 2‐4 months | 1 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.69, 0.33] |
| 8.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cognitive‐behaviour therapy | 1 | 59 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.69, 0.33] |
| 9 Dropouts for any reason within 2‐4 months | 5 | 322 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.72, 1.59] |
| 9.1 Behaviour therapy | 2 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [0.40, 5.38] |
| 9.2 Cognitive‐behaviour therapy | 3 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.65, 1.72] |
| 10 Dropouts due to side effects within 2‐4 months | 4 | 308 | Risk Ratio (M‐H, Random, 95% CI) | 7.46 [1.73, 32.26] |
| 10.1 Behaviour therapy | 1 | 45 | Risk Ratio (M‐H, Random, 95% CI) | 4.4 [0.22, 86.78] |
| 10.2 Cognitive‐behaviour therapy | 3 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 8.82 [1.64, 47.37] |
| 11 Response/remission on continued treatment | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.98, 1.92] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.98, 1.92] |
| 12 GlobalAvoidance/Panic on continued treatment | 1 | 142 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.80, ‐0.13] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 1 | 142 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.80, ‐0.13] |
| 13 Dropouts for any reason on continued treatment | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.21, 2.21] |
| 13.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Cognitive‐behaviour therapy | 1 | 142 | Risk Ratio (M‐H, Random, 95% CI) | 0.68 [0.21, 2.21] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 4 | 272 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.71, 1.33] |
| 14.1 Behaviour therapy | 2 | 59 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.54, 1.60] |
| 14.2 Cognitive‐behaviour therapy | 2 | 213 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.68, 1.45] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 167 | Std. Mean Difference (IV, Random, 95% CI) | 0.09 [‐0.21, 0.40] |
| 15.1 Behaviour therapy | 1 | 35 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.71, 0.61] |
| 15.2 Cognitive‐behaviour therapy | 1 | 132 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.21, 0.47] |
Analysis 2.1.
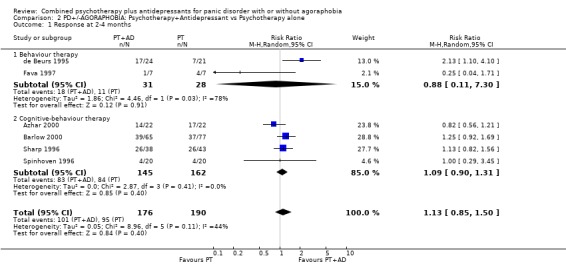
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 1 Response at 2‐4 months.
Analysis 2.2.
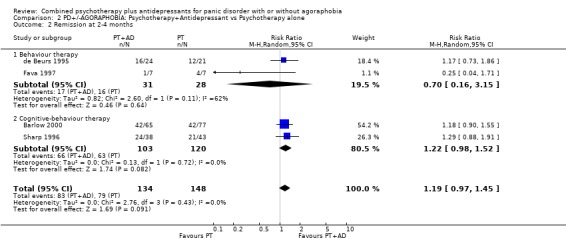
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 2 Remission at 2‐4 months.
Analysis 2.3.
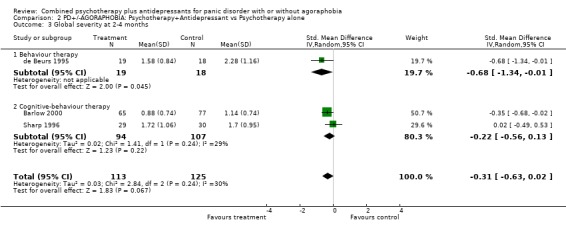
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 3 Global severity at 2‐4 months.
Analysis 2.4.
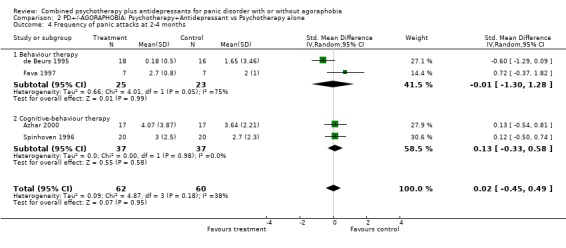
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 2.5.
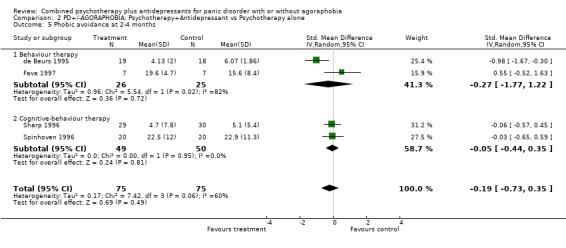
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 2.6.
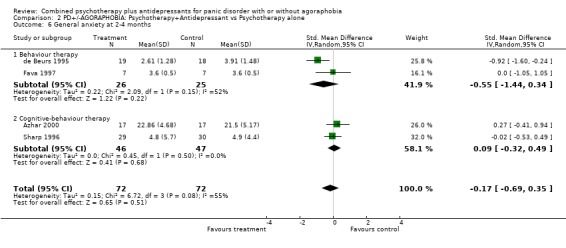
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 2.7.
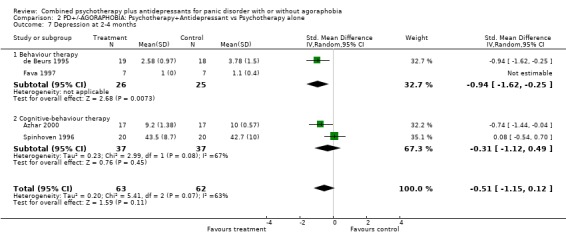
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 7 Depression at 2‐4 months.
Analysis 2.8.
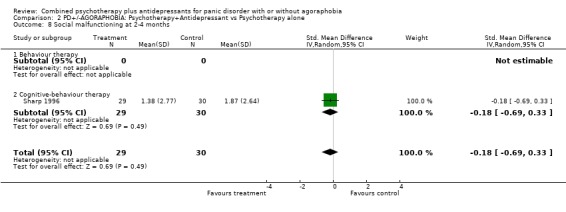
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 8 Social malfunctioning at 2‐4 months.
Analysis 2.9.
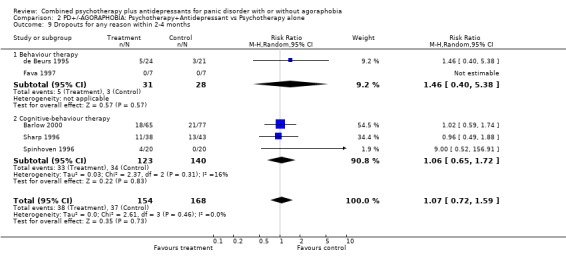
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 2.10.
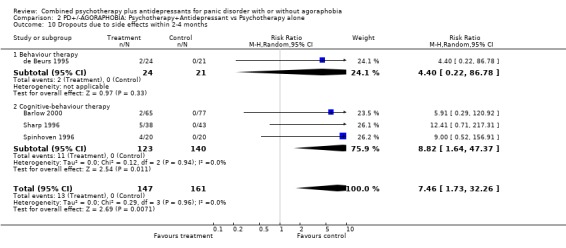
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 2.11.
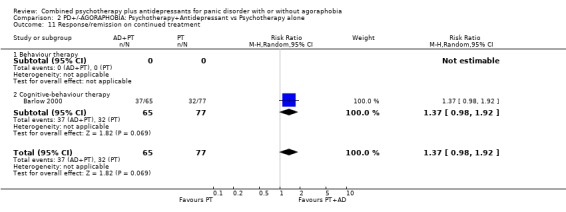
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 11 Response/remission on continued treatment.
Analysis 2.12.
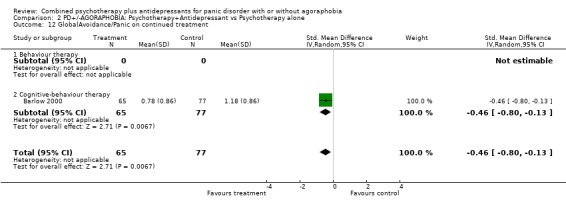
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 12 GlobalAvoidance/Panic on continued treatment.
Analysis 2.13.
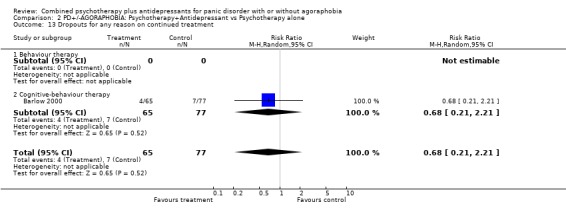
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 2.14.
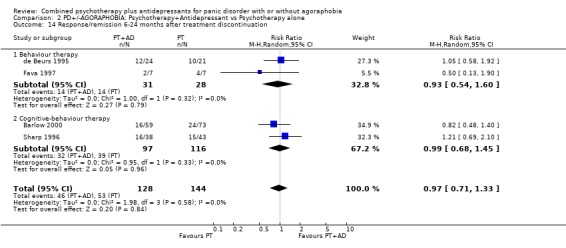
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 2.15.
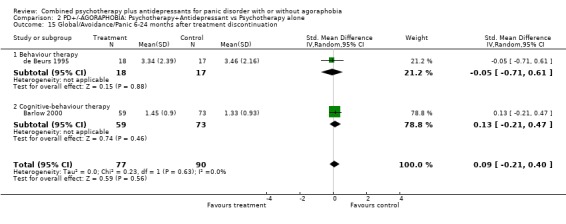
Comparison 2 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 3.
PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 17 | 1032 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.04, 1.32] |
| 1.1 Behaviour therapy | 10 | 527 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.03, 1.48] |
| 1.2 Cognitive‐behaviour therapy | 7 | 505 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.93, 1.47] |
| 2 Remission at 2‐4 months | 15 | 952 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.10, 1.54] |
| 2.1 Behaviour therapy | 8 | 447 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [1.10, 1.91] |
| 2.2 Cognitive‐behaviour therapy | 7 | 505 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.99, 1.60] |
| 3 Global severity at 2‐4 months | 8 | 477 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.63, ‐0.26] |
| 3.1 Behaviour therapy | 5 | 221 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐0.88, ‐0.33] |
| 3.2 Cognitive‐behaviour therapy | 3 | 256 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.69, ‐0.00] |
| 4 Frequency of panic attacks at 2‐4 months | 9 | 393 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.06 [‐0.27, 0.15] |
| 4.1 Behaviour therapy | 7 | 248 | Std. Mean Difference (IV, Random, 95% CI) | 0.07 [‐0.19, 0.32] |
| 4.2 Cognitive‐behaviour therapy | 2 | 145 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.61, 0.04] |
| 5 Phobic avoidance at 2‐4 months | 15 | 582 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.54, ‐0.15] |
| 5.1 Behaviour therapy | 10 | 364 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.72, ‐0.11] |
| 5.2 Cognitive‐behaviour therapy | 5 | 218 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.26 [‐0.53, 0.01] |
| 6 General anxiety at 2‐4 months | 13 | 595 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.65, ‐0.29] |
| 6.1 Behaviour therapy | 7 | 270 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐0.96, ‐0.38] |
| 6.2 Cognitive‐behaviour therapy | 6 | 325 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.54, ‐0.09] |
| 7 Depression at 2‐4 months | 12 | 436 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.60, ‐0.19] |
| 7.1 Behaviour therapy | 9 | 318 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.68, ‐0.13] |
| 7.2 Cognitive‐behaviour therapy | 3 | 118 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.76, ‐0.01] |
| 8 Social malfunctioning at 2‐4 months | 10 | 374 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.65, ‐0.10] |
| 8.1 Behaviour therapy | 7 | 260 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.84, ‐0.26] |
| 8.2 Cognitive‐behaviour therapy | 3 | 114 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.41, 0.33] |
| 9 Dropouts for any reason within 2‐4 months | 15 | 950 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.94, 1.50] |
| 9.1 Behaviour therapy | 8 | 445 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.88, 1.58] |
| 9.2 Cognitive‐behaviour therapy | 7 | 505 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.81, 1.78] |
| 10 Dropouts due to side effects within 2‐4 months | 9 | 665 | Risk Ratio (M‐H, Random, 95% CI) | 2.43 [1.23, 4.81] |
| 10.1 Behaviour therapy | 4 | 221 | Risk Ratio (M‐H, Random, 95% CI) | 1.84 [0.77, 4.41] |
| 10.2 Cognitive‐behaviour therapy | 5 | 444 | Risk Ratio (M‐H, Random, 95% CI) | 3.78 [1.26, 11.33] |
| 11 Response/remission on continued treatment | 3 | 229 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.93, 1.67] |
| 11.1 Behaviour therapy | 2 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [0.74, 3.61] |
| 11.2 Cognitive‐behaviour therapy | 1 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.81, 1.55] |
| 12 Global/Avoidance/Panic on continued treatment | 4 | 229 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.22, ‐0.31] |
| 12.1 Behaviour therapy | 3 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.53] |
| 12.2 Cognitive‐behaviour therapy | 1 | 128 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.71, ‐0.01] |
| 13 Dropouts for any reason on continued treatment | 2 | 147 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.25, 2.43] |
| 13.1 Behaviour therapy | 1 | 19 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 13.2 Cognitive‐behaviour therapy | 1 | 128 | Risk Ratio (M‐H, Random, 95% CI) | 0.65 [0.19, 2.18] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 8 | 507 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.76, 1.15] |
| 14.1 Behaviour therapy | 5 | 284 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.78, 1.36] |
| 14.2 Cognitive‐behaviour therapy | 3 | 223 | Risk Ratio (M‐H, Random, 95% CI) | 0.84 [0.62, 1.13] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 5 | 245 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.15, 0.48] |
| 15.1 Behaviour therapy | 4 | 124 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.37, 0.53] |
| 15.2 Cognitive‐behviour therapy | 1 | 121 | Std. Mean Difference (IV, Random, 95% CI) | 0.29 [‐0.06, 0.65] |
Analysis 3.1.
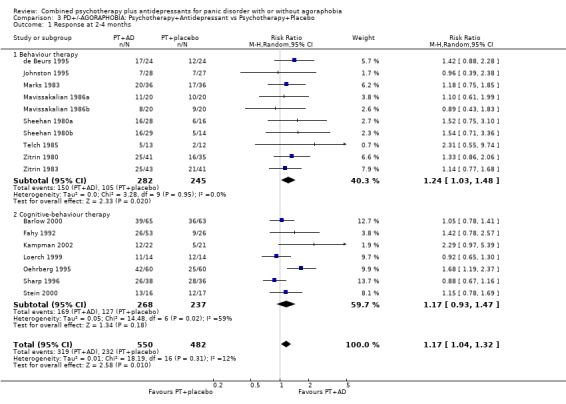
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 1 Response at 2‐4 months.
Analysis 3.2.
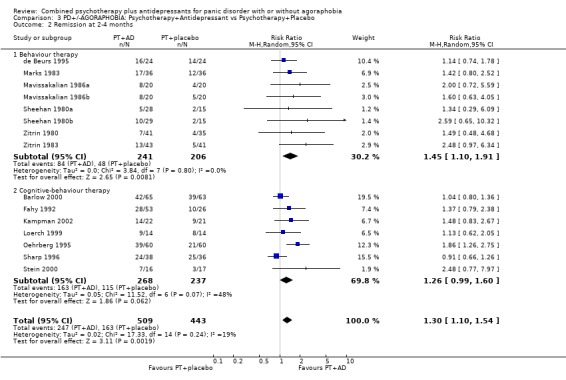
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 3.3.
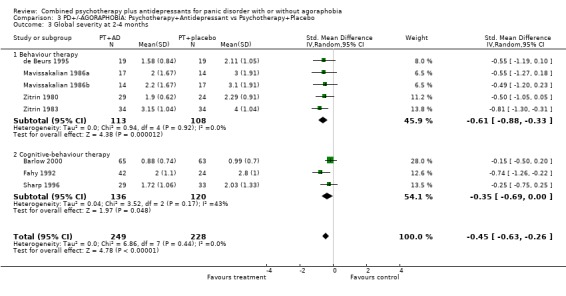
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 3.4.
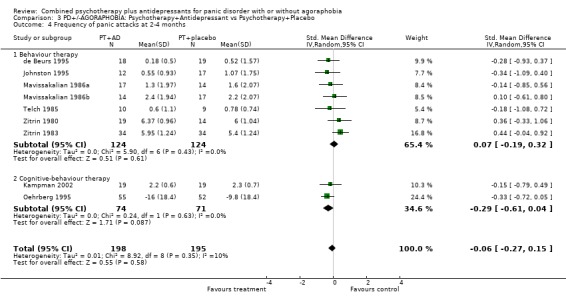
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 3.5.
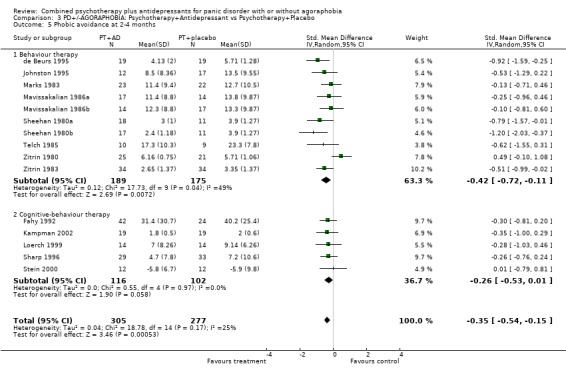
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 3.6.
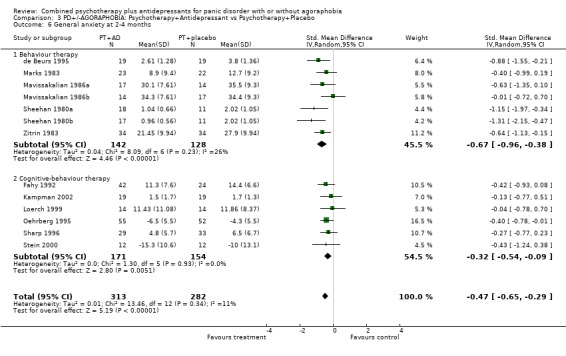
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 3.7.
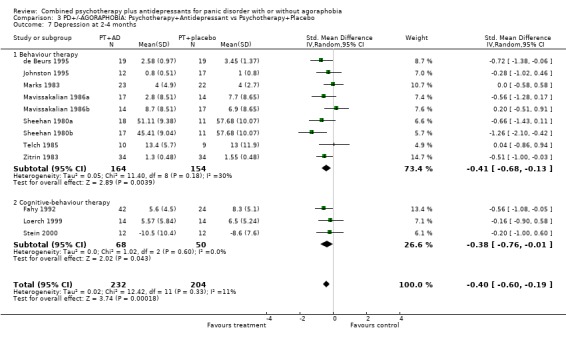
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 3.8.
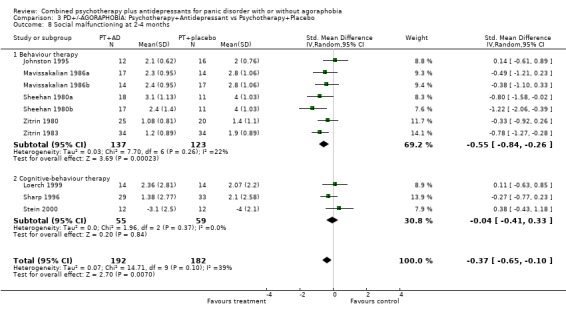
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 8 Social malfunctioning at 2‐4 months.
Analysis 3.9.
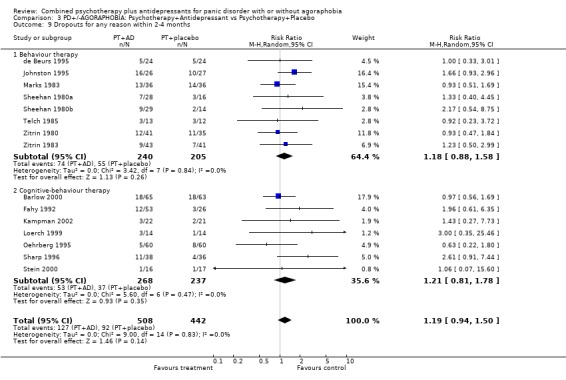
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 3.10.
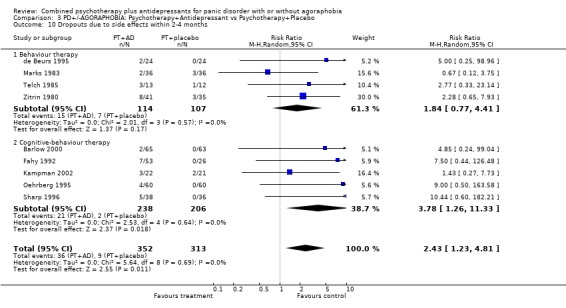
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 3.11.
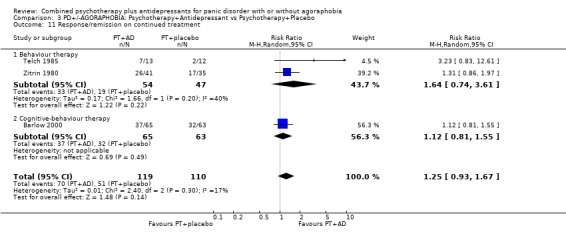
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 3.12.
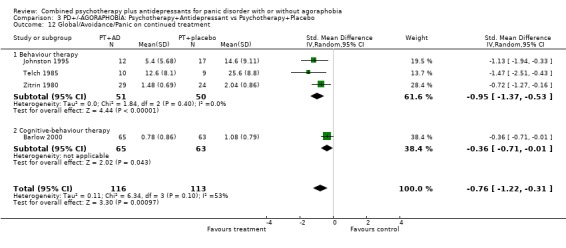
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 3.13.
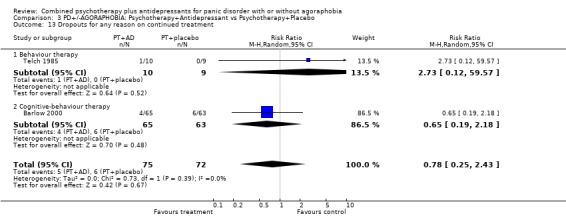
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 3.14.
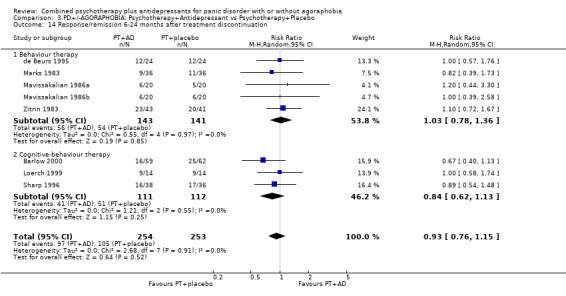
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 3.15.
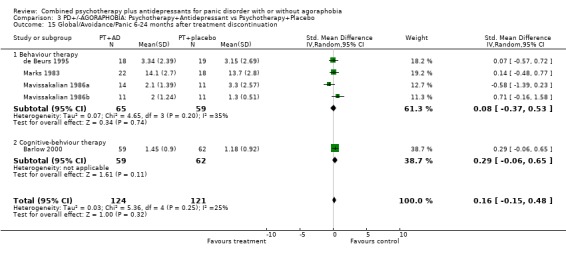
Comparison 3 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy+Placebo, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 4.
PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 23 | 1271 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.05, 1.31] |
| 1.1 Behaviour therapy | 12 | 562 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.05, 1.50] |
| 1.2 Cognitive‐behaviour therapy | 11 | 709 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.96, 1.33] |
| 2 Remission at 2‐4 months | 19 | 1107 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.10, 1.44] |
| 2.1 Behaviour therapy | 10 | 482 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [1.06, 1.77] |
| 2.2 Cognitive‐behaviour therapy | 9 | 625 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.02, 1.47] |
| 3 Global severity at 2‐4 months | 11 | 602 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.60, ‐0.26] |
| 3.1 Behaviour therapy | 6 | 239 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐0.87, ‐0.34] |
| 3.2 Cognitive‐behaviour therapy | 5 | 363 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.54, ‐0.08] |
| 4 Frequency of panic attacks at 2‐4 months | 13 | 497 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.21, 0.16] |
| 4.1 Behaviour therapy | 9 | 278 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.19, 0.31] |
| 4.2 Cognitive‐behaviour therapy | 4 | 219 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.41, 0.12] |
| 5 Phobic avoidance at 2‐4 months | 19 | 684 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.49, ‐0.12] |
| 5.1 Behaviour therapy | 12 | 396 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.70, ‐0.11] |
| 5.2 Cognitive‐behaviour therapy | 7 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.44, 0.04] |
| 6 General anxiety at 2‐4 months | 17 | 691 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.59, ‐0.23] |
| 6.1 Behaviour therapy | 9 | 302 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐0.90, ‐0.37] |
| 6.2 Cognitive‐behaviour therapy | 8 | 389 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.44, ‐0.03] |
| 7 Depression at 2‐4 months | 16 | 542 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.59, ‐0.20] |
| 7.1 Behaviour therapy | 11 | 350 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.69, ‐0.17] |
| 7.2 Cognitive‐behaviour therapy | 5 | 192 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.64, ‐0.05] |
| 8 Social malfunctioning at 2‐4 months | 11 | 404 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.61, ‐0.11] |
| 8.1 Behaviour therapy | 7 | 260 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.84, ‐0.26] |
| 8.2 Cognitive‐behaviour therapy | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.39, 0.30] |
| 9 Dropouts for any reason within 2‐4 months | 20 | 1145 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.95, 1.47] |
| 9.1 Behaviour therapy | 10 | 480 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.90, 1.60] |
| 9.2 Cognitive‐behaviour therapy | 10 | 665 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.83, 1.62] |
| 10 Dropouts due to side effects within 2‐4 months | 13 | 846 | Risk Ratio (M‐H, Random, 95% CI) | 3.01 [1.61, 5.63] |
| 10.1 Behaviour therapy | 5 | 242 | Risk Ratio (M‐H, Random, 95% CI) | 1.99 [0.85, 4.62] |
| 10.2 Cognitive‐behaviour therapy | 8 | 604 | Risk Ratio (M‐H, Random, 95% CI) | 5.00 [1.96, 12.72] |
| 11 Response/remission on continued treatment | 4 | 306 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [1.03, 1.62] |
| 11.1 Behaviour therapy | 2 | 101 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [0.74, 3.61] |
| 11.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 12 Global/Avoidance/Panic on continued treatment | 5 | 306 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐0.97, ‐0.33] |
| 12.1 Behaviour therapy | 3 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.53] |
| 12.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 13 Dropouts for any reason on continued treatment | 3 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.28, 2.15] |
| 13.1 Behaviour therapy | 1 | 19 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 13.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 12 | 658 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.79, 1.16] |
| 14.1 Behaviour therapy | 7 | 319 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.77, 1.31] |
| 14.2 Cognitive‐behaviour therapy | 5 | 339 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.69, 1.21] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 7 | 335 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.09, 0.37] |
| 15.1 Behaviour therapy | 5 | 141 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.32, 0.43] |
| 15.2 Cognitive‐behviour therapy | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
Analysis 4.1.
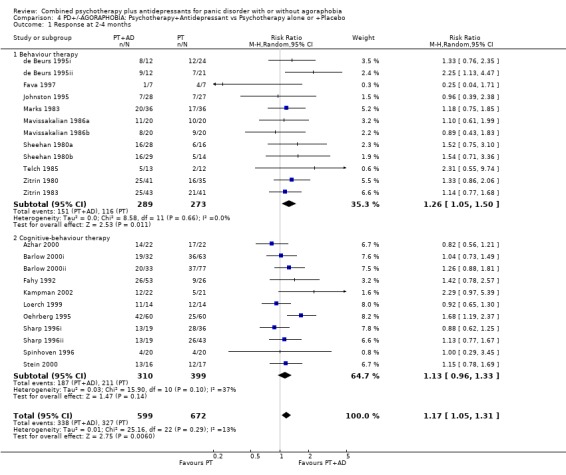
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 4.2.
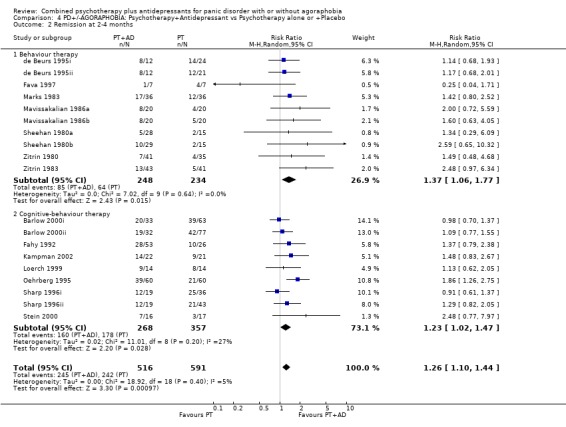
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 4.3.
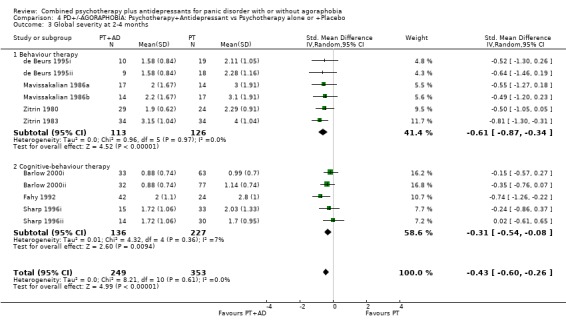
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 4.4.
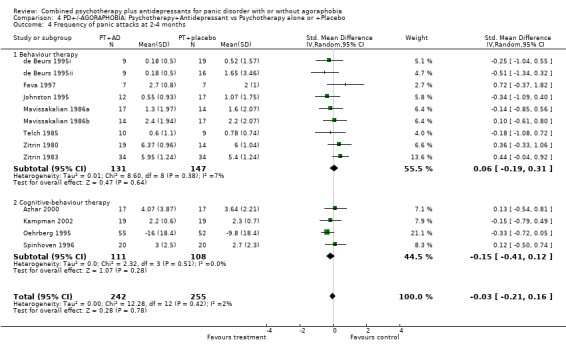
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 4.5.
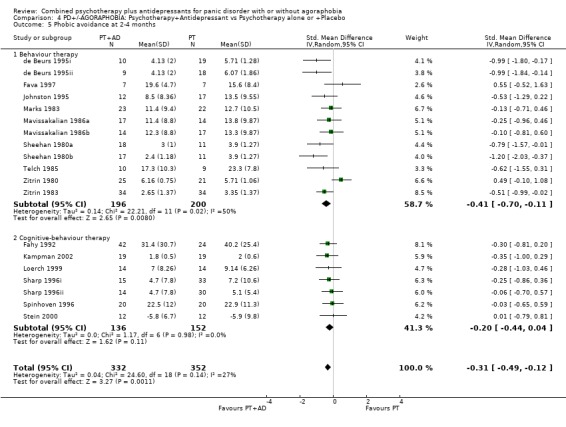
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 4.6.
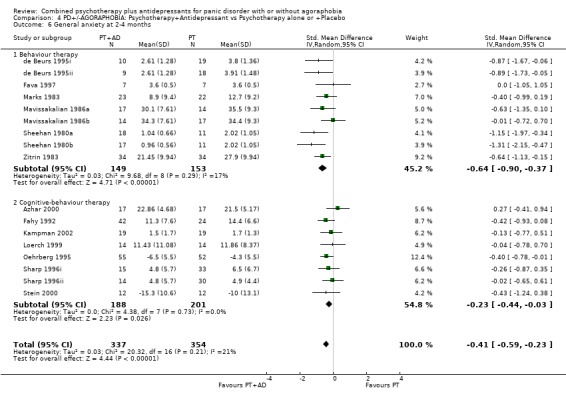
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 4.7.
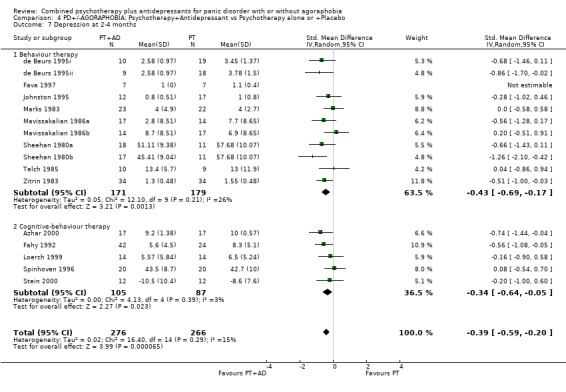
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 4.8.
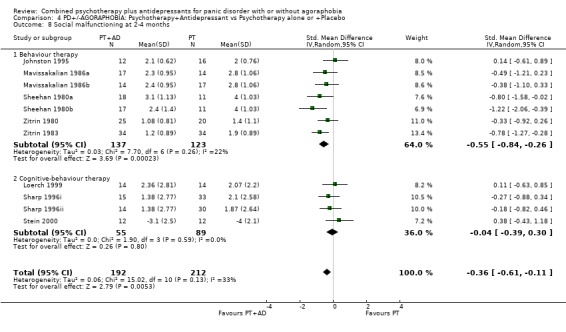
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social malfunctioning at 2‐4 months.
Analysis 4.9.
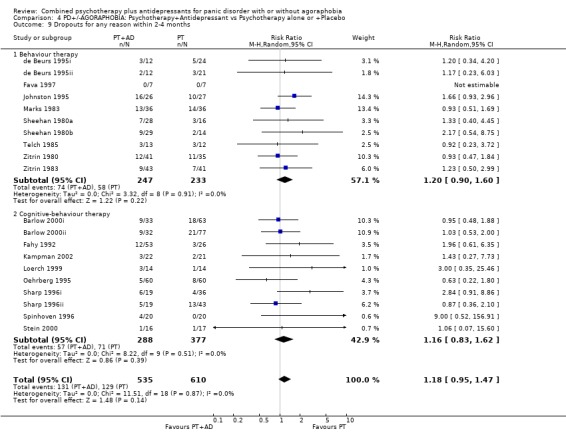
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 4.10.
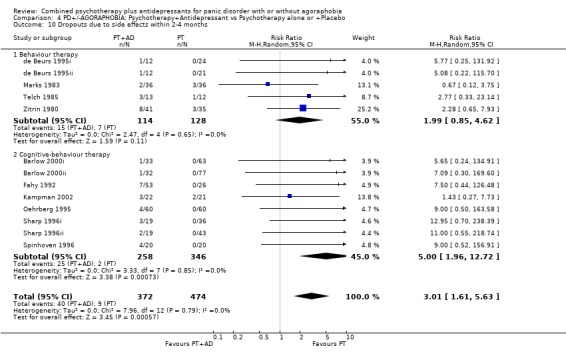
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 4.11.
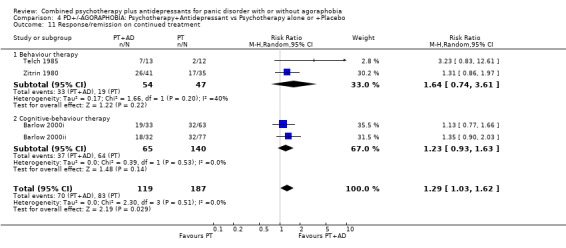
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 4.12.
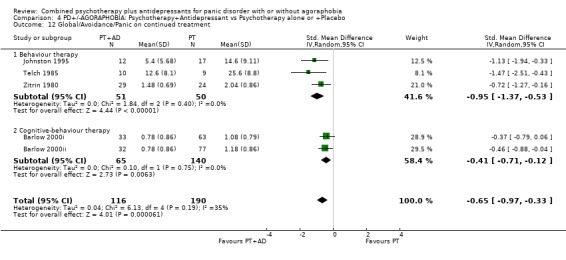
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 4.13.
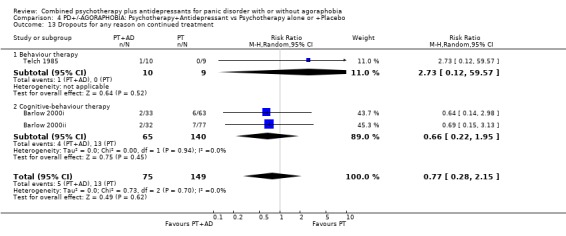
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 4.14.
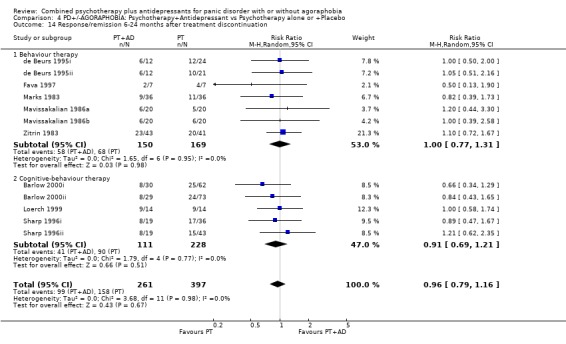
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 4.15.
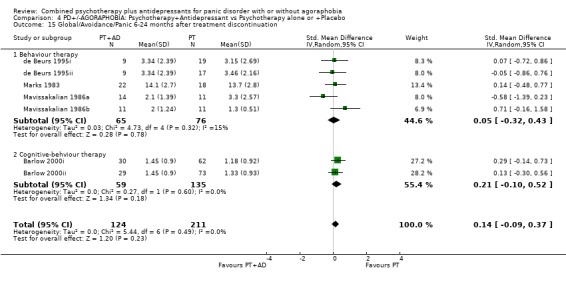
Comparison 4 PD+/‐AGORAPHOBIA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 5.
SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 7 | 421 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.04, 1.45] |
| 1.1 Behaviour therapy | 4 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.80, 1.40] |
| 1.2 Cognitive‐behaviour therapy | 2 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.94, 1.71] |
| 1.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.41 [1.05, 1.90] |
| 2 Remission at 2‐4 months | 4 | 302 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.06, 1.51] |
| 2.1 Behaviour therapy | 2 | 114 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.62, 1.51] |
| 2.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [1.01, 1.79] |
| 2.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.02, 1.72] |
| 3 Global severity at 2‐4 months | 4 | 278 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.66, ‐0.04] |
| 3.1 Behaviour therapy | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.45, 0.44] |
| 3.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.55, 0.10] |
| 3.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.33, ‐0.05] |
| 4 Frequency of panic attacks at 2‐4 months | 6 | 217 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.10 [‐0.39, 0.20] |
| 4.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.49, 0.19] |
| 4.2 Cognitive‐behaviour therapy | 1 | 39 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.55, 0.71] |
| 4.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 7 | 275 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.65, ‐0.00] |
| 5.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.01, ‐0.06] |
| 5.2 Cognitive‐behaviour therapy | 2 | 97 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.34, 0.46] |
| 5.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.23, 0.04] |
| 6 General anxiety at 2‐4 months | 3 | 130 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.43, 0.17] |
| 6.1 Behaviour therapy | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.60, 0.23] |
| 6.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.01, ‐0.63] |
| 7 Depression at 2‐4 months | 6 | 217 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.68, ‐0.14] |
| 7.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.69, ‐0.01] |
| 7.2 Cognitive‐behaviour therapy | 1 | 39 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.88, 0.38] |
| 7.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.44, ‐0.14] |
| 8 Social functioning at 2‐4 months | 4 | 158 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.84, ‐0.07] |
| 8.1 Behavour therapy | 3 | 118 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.68, 0.08] |
| 8.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.46, ‐0.16] |
| 9 Dropouts for any reason within 2‐4 months | 7 | 421 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.71, 1.32] |
| 9.1 Behaviour therapy | 4 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.78, 1.88] |
| 9.2 Cognitive‐behaviour therapy | 2 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.48, 1.17] |
| 9.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 10 Dropouts due to side effects within 2‐4 months | 5 | 271 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.34, 1.83] |
| 10.1 Behaviour therapy | 2 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.58] |
| 10.2 Cognitive‐behaviour therapy | 2 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.10, 3.28] |
| 10.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 11 Response/remission on continued treatment | 4 | 309 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.21, 2.19] |
| 11.1 Behaviour therapy | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.10, 3.41] |
| 11.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.07, 2.16] |
| 11.3 Psychdynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 4 | 236 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐0.92, ‐0.31] |
| 12.1 Behaviour therapy | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.51, ‐0.30] |
| 12.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.74, ‐0.09] |
| 12.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐1.50, ‐0.20] |
| 13 Dropouts for any reason on continued treatment | 3 | 208 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.27, 1.90] |
| 13.1 Behaviour therapy | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.22, 2.39] |
| 13.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.05, 5.08] |
| 14 Response/remission immediately after treatment discontinuation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Global/Avoidance/Panic immediately after treatment discontinuation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 3 | 272 | Risk Ratio (M‐H, Random, 95% CI) | 1.74 [1.12, 2.69] |
| 16.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.95, 2.35] |
| 16.2 Cognitive‐behaviour therapy | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.75, 2.58] |
| 16.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.2 [1.45, 7.05] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.78, 0.63] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 1 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.34, 0.34] |
| 17.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐1.91, ‐0.55] |
Analysis 5.1.
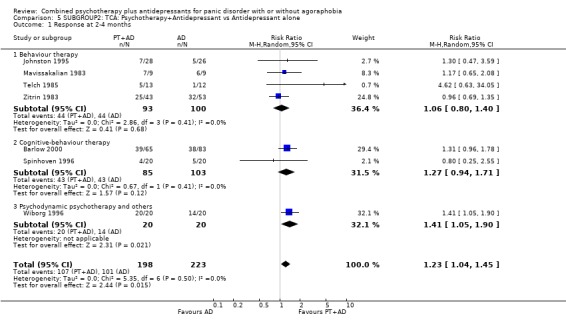
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 5.2.
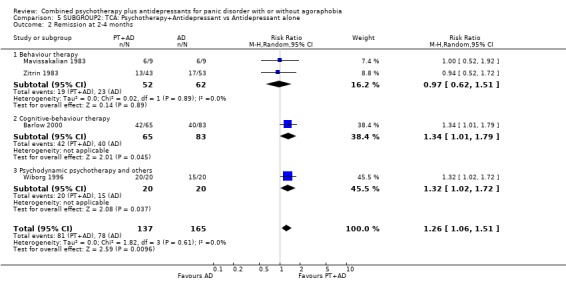
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 5.3.
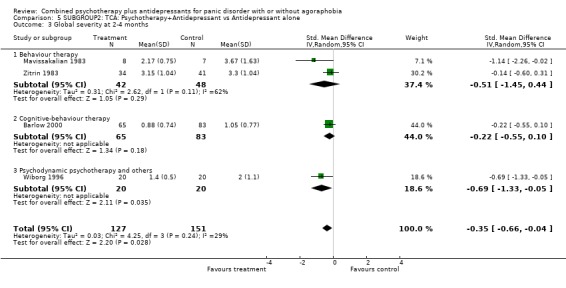
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 5.4.
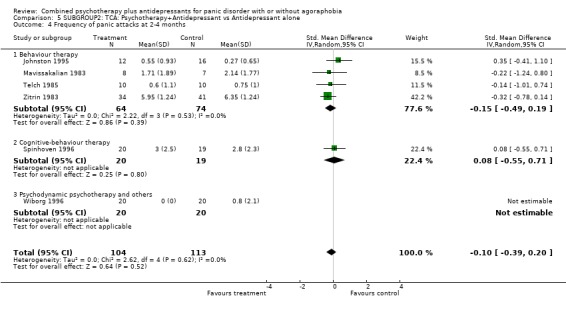
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 5.5.
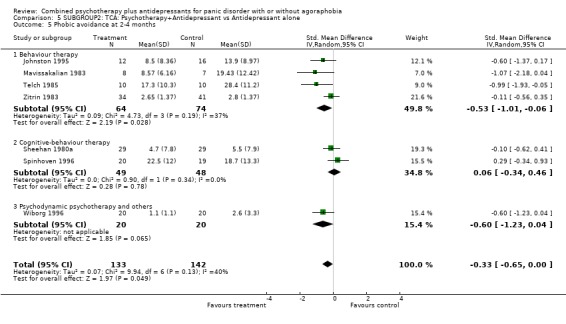
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 5.6.
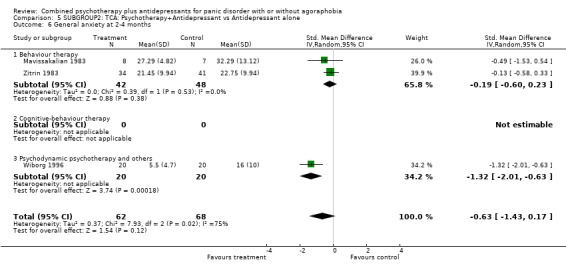
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 5.7.
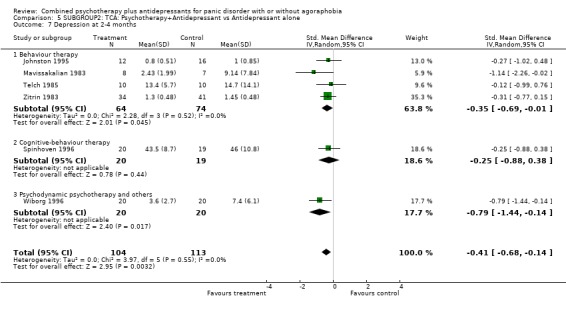
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 5.8.
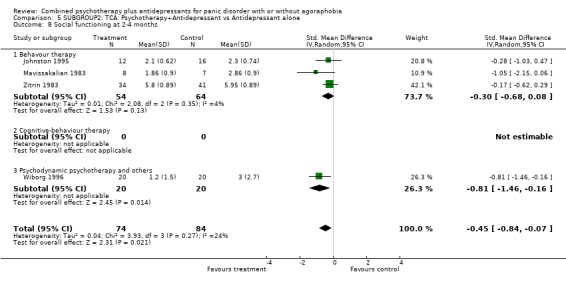
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 5.9.
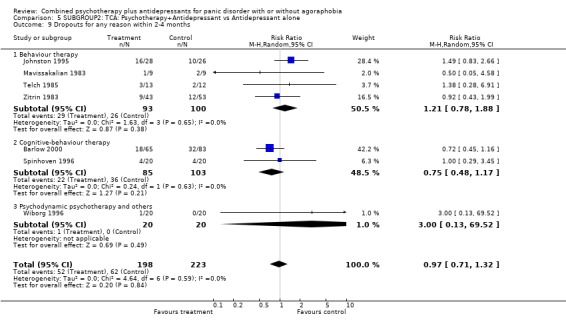
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 5.10.
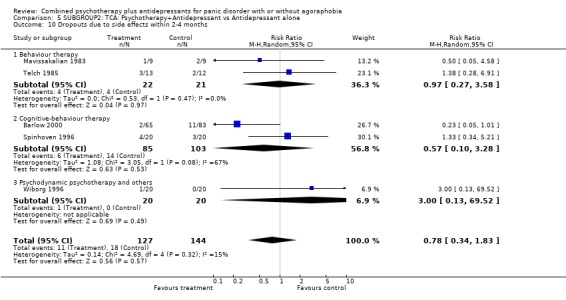
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 5.11.
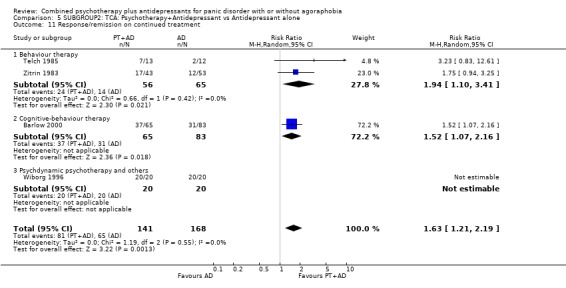
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 5.12.
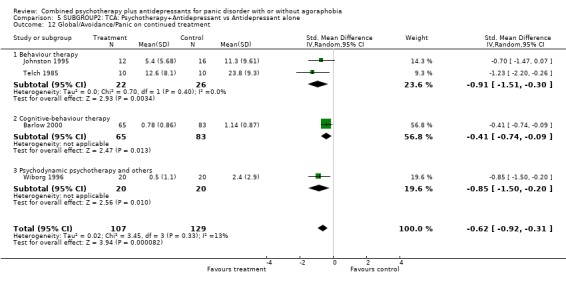
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 5.13.
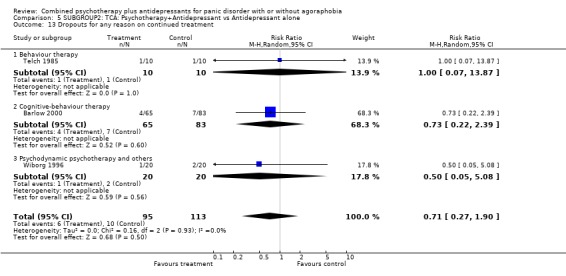
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 5.16.
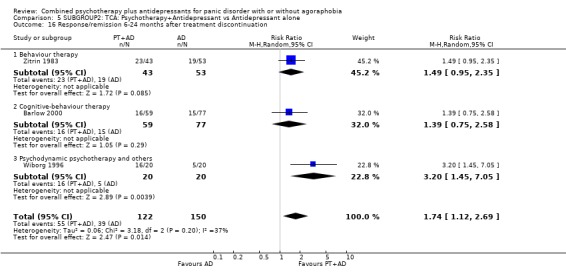
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Analysis 5.17.
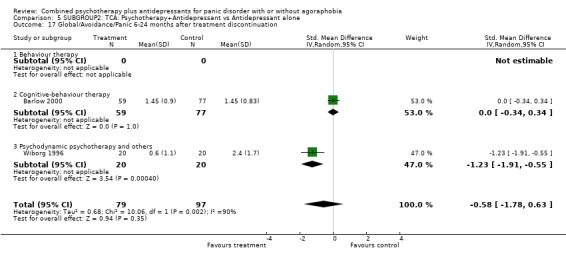
Comparison 5 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 6.
SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 12 | 760 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [1.01, 1.36] |
| 1.1 Behaviour therapy | 8 | 436 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.99, 1.50] |
| 1.2 Cognitive‐behaviour therapy | 4 | 324 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.89, 1.40] |
| 2 Remission at 2‐4 months | 10 | 653 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.00, 1.45] |
| 2.1 Behaviour therapy | 7 | 369 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [1.00, 1.90] |
| 2.2 Cognitive‐behaviour therapy | 3 | 284 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.90, 1.42] |
| 3 Global severity at 2‐4 months | 7 | 454 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.67, ‐0.28] |
| 3.1 Behaviour therapy | 4 | 183 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐0.92, ‐0.32] |
| 3.2 Cognitive‐behaviour therapy | 3 | 271 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.70, ‐0.07] |
| 4 Frequency of panic attacks at 2‐4 months | 8 | 265 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.09, 0.40] |
| 4.1 Behaviour therapy | 7 | 225 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.10, 0.43] |
| 4.2 Cognitive‐behaviour therapy | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [‐0.50, 0.74] |
| 5 Phobic avoidance at 2‐4 months | 11 | 418 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.44, 0.02] |
| 5.1 Behaviour therapy | 9 | 312 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.51, 0.07] |
| 5.2 Cognitive‐behaviour therapy | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.59, 0.20] |
| 6 General anxiety at 2‐4 months | 7 | 284 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.73, ‐0.25] |
| 6.1 Behaviour therapy | 6 | 218 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐0.80, ‐0.21] |
| 6.2 Cognitive‐behaviour therapy | 1 | 66 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.42 [‐0.93, 0.08] |
| 7 Depression at 2‐4 months | 10 | 372 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.50, ‐0.07] |
| 7.1 Behaviour therapy | 8 | 266 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.53, ‐0.03] |
| 7.2 Cognitive‐behaviour therapy | 2 | 106 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.90, 0.37] |
| 8 Social malfunctioning at 2‐4 months | 6 | 232 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.75, ‐0.22] |
| 8.1 Behaviour therapy | 6 | 232 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐0.75, ‐0.22] |
| 8.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 11 | 692 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.90, 1.49] |
| 9.1 Behaviour therapy | 7 | 368 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.85, 1.59] |
| 9.2 Cognitive‐behaviour therapy | 4 | 324 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.73, 1.89] |
| 10 Dropouts due to side effects within 2‐4 months | 7 | 497 | Risk Ratio (M‐H, Random, 95% CI) | 2.50 [1.15, 5.45] |
| 10.1 Behaviour therapy | 3 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.68 [0.67, 4.18] |
| 10.2 Cognitive‐behaviour therapy | 4 | 324 | Risk Ratio (M‐H, Random, 95% CI) | 7.31 [1.64, 32.67] |
| 11 Response/remission on continued treatment | 5 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.00, 1.51] |
| 11.1 Behaviour therapy | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.90] |
| 11.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 12 Global/Avoidance/Panic on continued treatment | 5 | 306 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐0.97, ‐0.33] |
| 12.1 Behaviour therapy | 3 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.53] |
| 12.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 13 Dropouts for any reason on continued treatment | 3 | 224 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.28, 2.15] |
| 13.1 Behaviour therapy | 1 | 19 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 13.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 18 Response 6‐24 months after treatment discontinuation | 7 | 444 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.70, 1.18] |
| 18.1 Behaviour therapy | 5 | 250 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.73, 1.36] |
| 18.2 Cognitive‐behaviour therapy | 2 | 194 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.46, 1.19] |
| 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 5 | 281 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.14, 0.45] |
| 19.1 Behaviour therapy | 3 | 87 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.59, 0.75] |
| 19.2 Cognitive‐behviour therapy | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
Analysis 6.1.
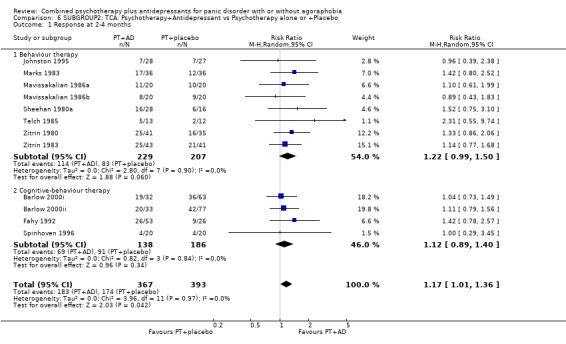
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 6.2.
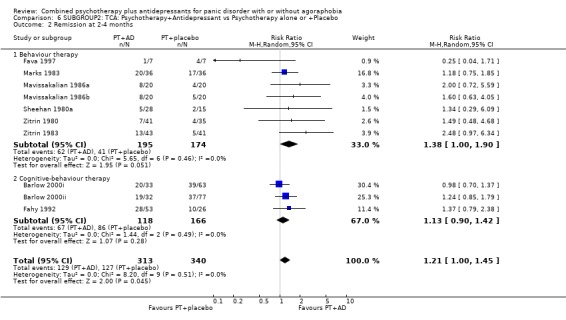
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 6.3.
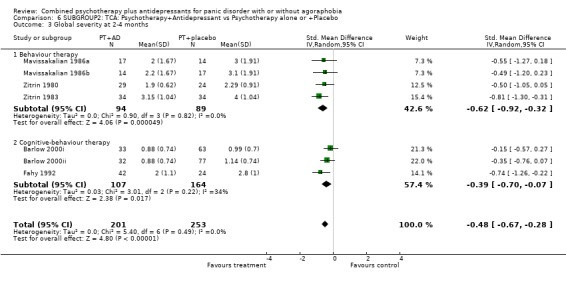
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 6.4.
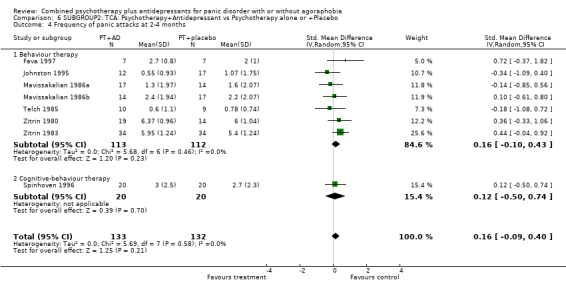
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 6.5.
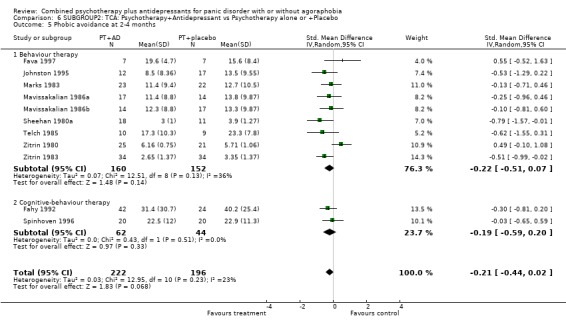
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 6.6.
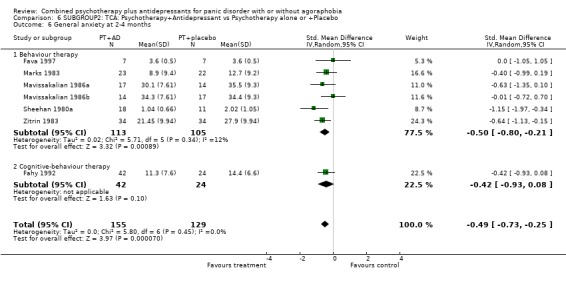
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 6.7.
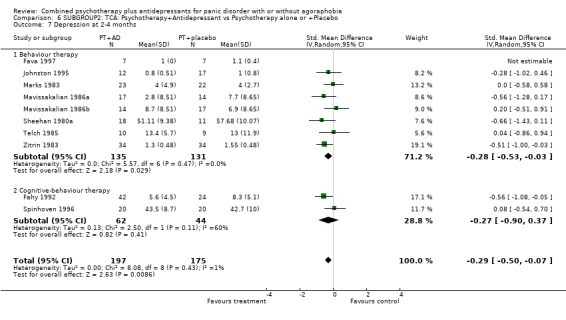
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 6.8.
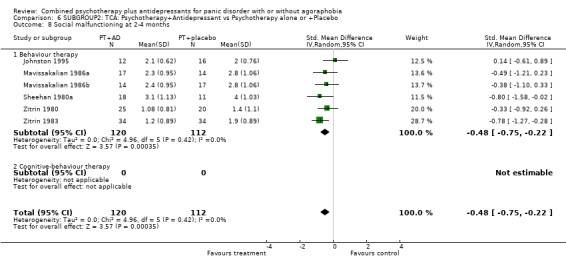
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social malfunctioning at 2‐4 months.
Analysis 6.9.
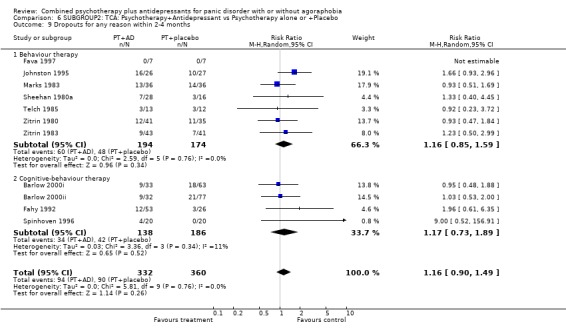
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 6.10.
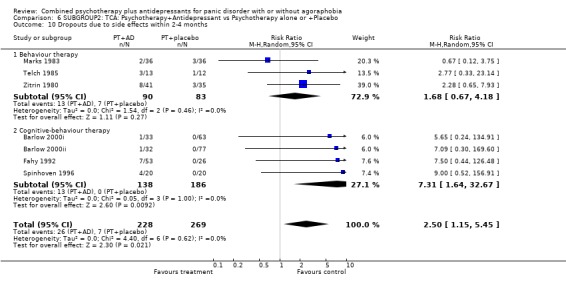
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 6.11.
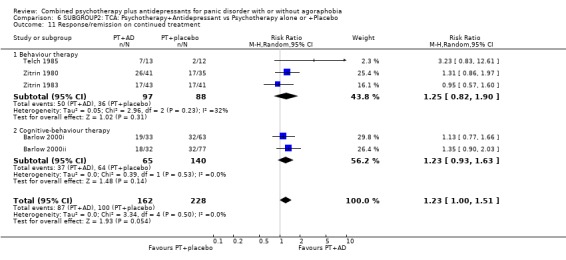
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 6.12.
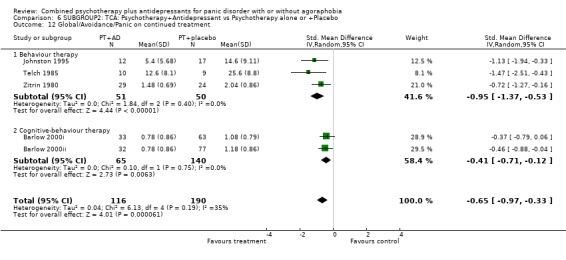
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 6.13.
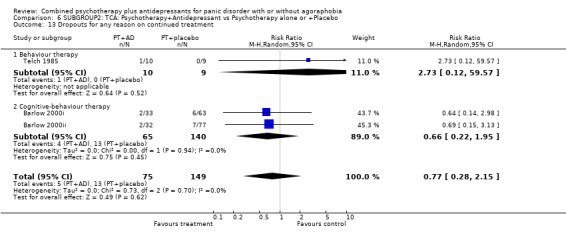
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 6.18.
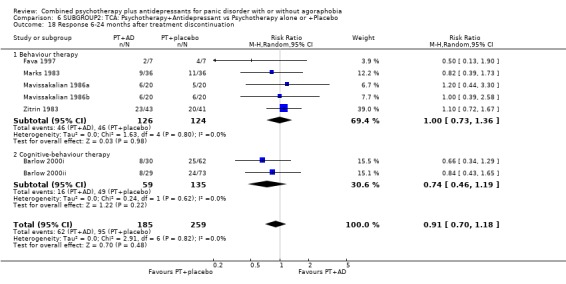
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 18 Response 6‐24 months after treatment discontinuation.
Analysis 6.19.
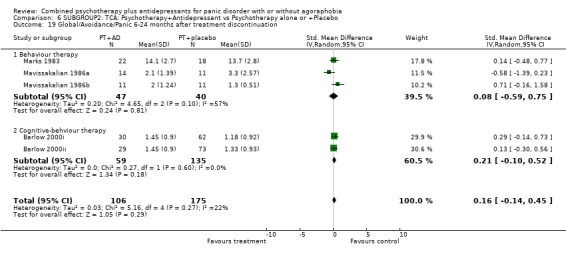
Comparison 6 SUBGROUP2: TCA: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 7.
SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 3 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.75, 2.03] |
| 1.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Cognitive‐behaviour therapy | 2 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 1.68 [0.69, 4.05] |
| 1.3 Psychodynamic psychotherapy and others | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.63, 1.15] |
| 2 Remission at 2‐4 months | 2 | 174 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.38, 1.70] |
| 2.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Cognitive‐behaviour therapy | 1 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.78, 1.66] |
| 2.3 Psychodynamic psychotherapy and others | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 0.54 [0.32, 0.90] |
| 3 Global severity at 2‐4 months | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.01, 0.04] |
| 3.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Cognitive‐behaviour therapy | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.01, 0.04] |
| 3.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 2 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐1.39, 0.45] |
| 4.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Cognitive‐behaviour therapy | 2 | 86 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐2.34, 0.83] |
| 4.3 Psychodynamic psychotherapy and others | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.53, 0.59] |
| 5 Phobic avoidance at 2‐4 months | 1 | 104 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [0.16, 0.97] |
| 5.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Cognitive‐behaviour therapy | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [‐0.00, 1.14] |
| 5.3 Psychodynamic psychotherapy and others | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.57 [‐0.00, 1.14] |
| 6 General anxiety at 2‐4 months | 3 | 196 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.93, 0.49] |
| 6.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Cognitive‐behaviour therapy | 3 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐1.32, 0.45] |
| 6.3 Psychodynamic psychotherapy and others | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [‐0.18, 0.95] |
| 7 Depression at 2‐4 months | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.60, ‐0.18] |
| 7.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Cognitive‐behaviour therapy | 1 | 34 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.60, ‐0.18] |
| 7.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.82, 0.22] |
| 8.1 Behavour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cognitive‐behaviour therapy | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.82, 0.22] |
| 8.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 3 | 218 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.68, 1.60] |
| 9.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Cognitive‐behaviour therapy | 2 | 118 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.51, 1.61] |
| 9.3 Psychodynamic psychotherapy and others | 1 | 100 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.65, 2.39] |
| 10 Dropouts due to side effects within 2‐4 months | 1 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [0.41, 6.13] |
| 10.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Cognitive‐behaviour therapy | 1 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [0.41, 6.13] |
| 10.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Response/remission on continued treatment | 1 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.44, 1.02] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Psychdynamic psychotherapy and others | 1 | 73 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.44, 1.02] |
| 12 Global/Avoidance/Panic on continued treatment | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 Psychodynamic psychotherapy and others | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 13 Dropouts for any reason on continued treatment | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Response/remission immediately after treatment discontinuation | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 14.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Psychodynamic psychotherapy and others | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 15 Global/Avoidance/Panic immediately after treatment discontinuation | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 15.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Psychodynamic psychotherapy and others | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 1 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.80, 2.89] |
| 16.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Cognitive‐behaviour therapy | 1 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [0.80, 2.89] |
| 16.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 7.1.
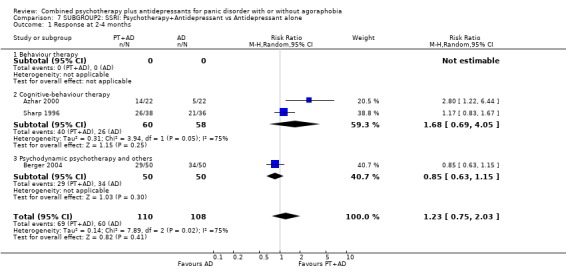
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 7.2.
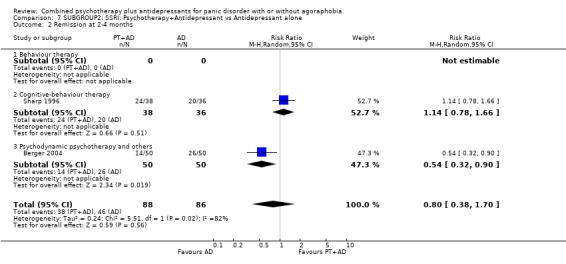
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 7.3.
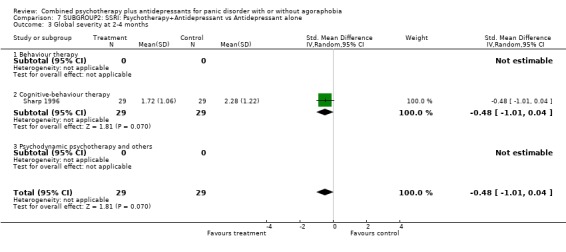
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 7.4.
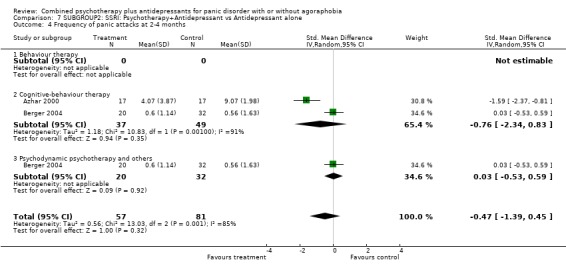
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 7.5.
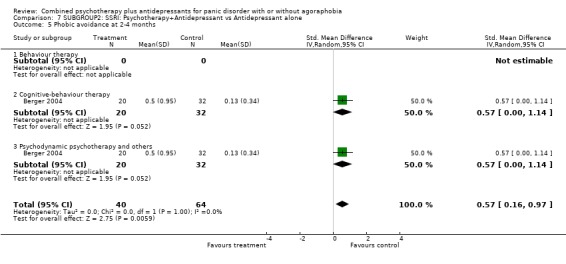
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 7.6.
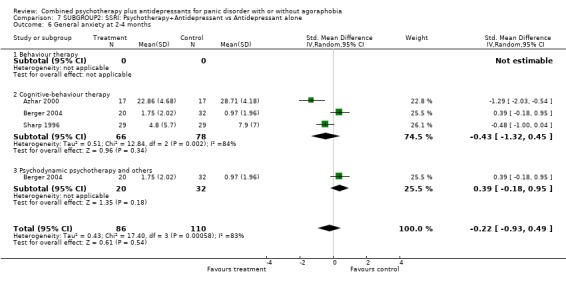
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 7.7.
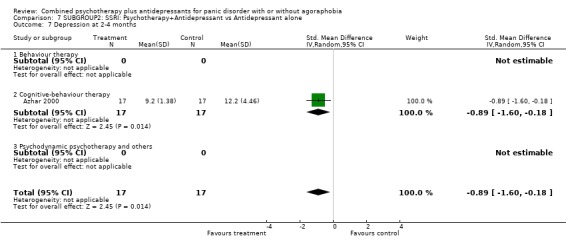
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 7.8.
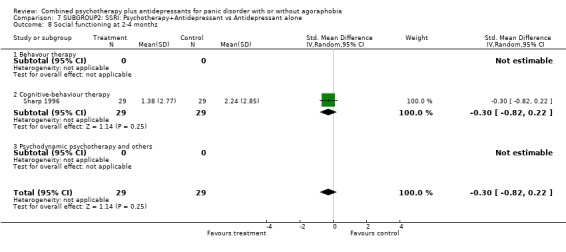
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 7.9.
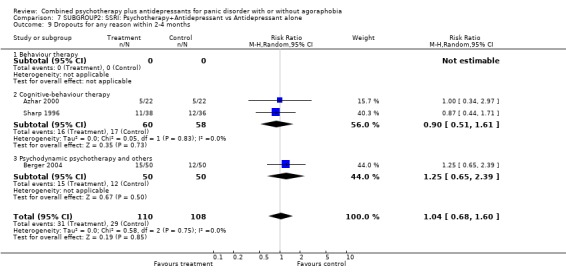
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 7.10.
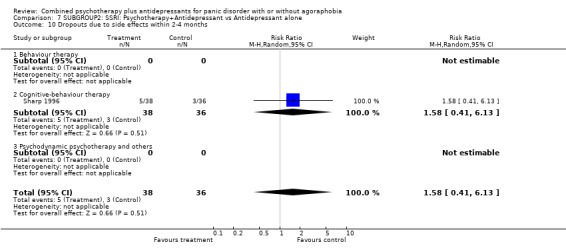
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 7.11.

Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 7.12.
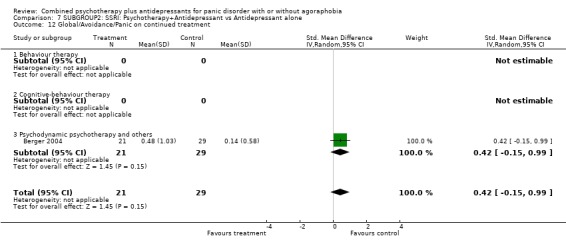
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 7.14.
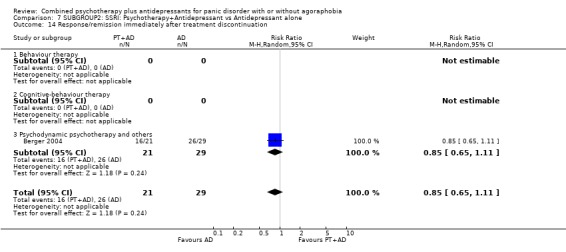
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 14 Response/remission immediately after treatment discontinuation.
Analysis 7.15.
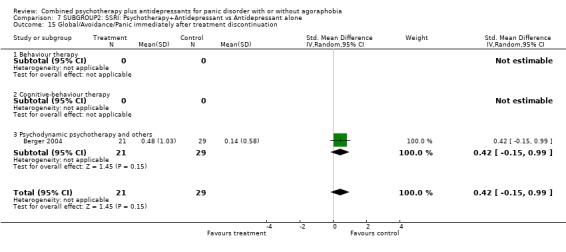
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 15 Global/Avoidance/Panic immediately after treatment discontinuation.
Analysis 7.16.
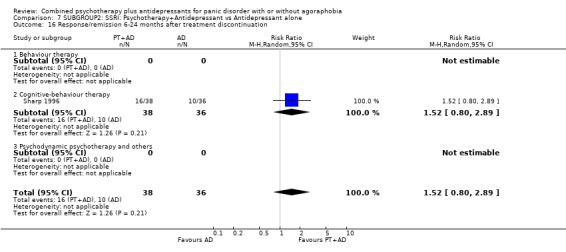
Comparison 7 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Comparison 8.
SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 8 | 426 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [0.94, 1.65] |
| 1.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 2.93 [1.07, 7.99] |
| 1.2 Cognitive‐behaviour therapy | 6 | 357 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.89, 1.53] |
| 2 Remission at 2‐4 months | 7 | 382 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.04, 1.65] |
| 2.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.79, 1.68] |
| 2.2 Cognitive‐behaviour therapy | 5 | 313 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [1.01, 1.92] |
| 3 Global severity at 2‐4 months | 4 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.64, 0.06] |
| 3.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.14, ‐0.01] |
| 3.2 Cognitive‐behaviour therapy | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.56, 0.32] |
| 4 Frequency of panic attacks at 2‐4 months | 5 | 232 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.24 [‐0.50, 0.02] |
| 4.1 Behaviour therapy | 2 | 53 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.95, 0.20] |
| 4.2 Cognitive‐behaviour therapy | 3 | 179 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.50, 0.09] |
| 5 Phobic avoidance at 2‐4 months | 6 | 210 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.71, ‐0.06] |
| 5.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.99 [‐1.57, ‐0.40] |
| 5.2 Cognitive‐behaviour therapy | 4 | 154 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.51, 0.15] |
| 6 General anxiety at 2‐4 months | 8 | 351 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.54, ‐0.07] |
| 6.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.46, ‐0.30] |
| 6.2 Cognitive‐behaviour therapy | 6 | 295 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.45, 0.02] |
| 7 Depression at 2‐4 months | 4 | 114 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.01, ‐0.24] |
| 7.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.34, ‐0.19] |
| 7.2 Cognitive‐behaviour therapy | 2 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.03, 0.02] |
| 8 Social malfunctioning at 2‐4 months | 3 | 116 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.47, 0.30] |
| 8.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cognitive‐behaviour therapy | 3 | 116 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.47, 0.30] |
| 9 Dropouts for any reason within 2‐4 months | 7 | 382 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.70, 1.80] |
| 9.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.44, 3.22] |
| 9.2 Cognitive‐behaviour therapy | 5 | 313 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.64, 1.93] |
| 10 Dropouts due to side effects within 2‐4 months | 6 | 349 | Risk Ratio (M‐H, Random, 95% CI) | 4.22 [1.47, 12.08] |
| 10.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 5.41 [0.59, 49.42] |
| 10.2 Cognitive‐behaviour therapy | 4 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 3.93 [1.19, 12.97] |
| 11 Response/remission on continued treatment | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 1 | 38 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.31] |
| 13.1 Behaviour therapy | 1 | 38 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.31] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Response 6‐24 months after treatment discontinuation | 4 | 186 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.73, 1.44] |
| 18.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.62, 1.69] |
| 18.2 Cognitive‐behaviour therapy | 2 | 117 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.65, 1.63] |
| 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.56, 0.58] |
| 19.1 Behaviour therapy | 2 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.56, 0.58] |
| 19.2 Cognitive‐behviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 8.1.
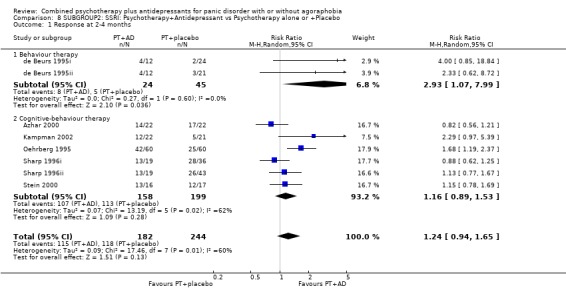
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 8.2.
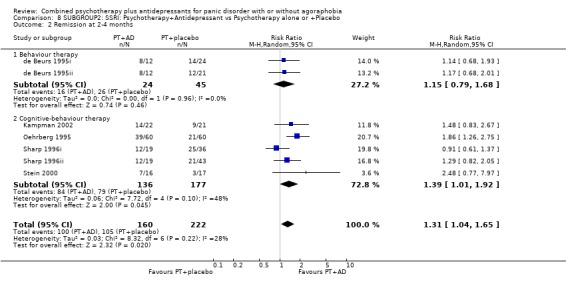
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 8.3.
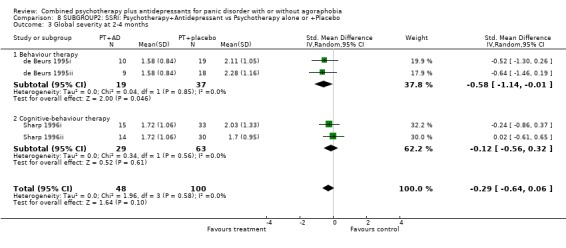
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 8.4.
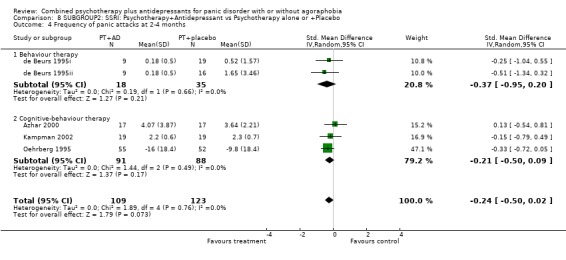
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 8.5.
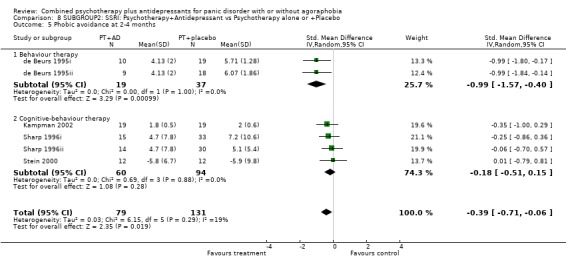
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 8.6.
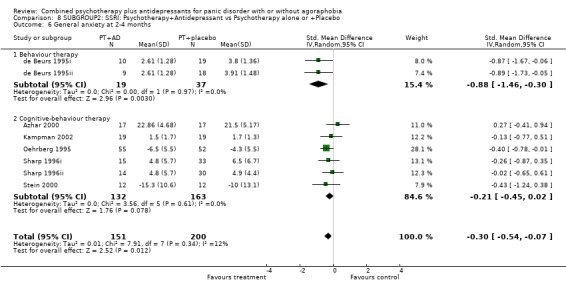
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 8.7.
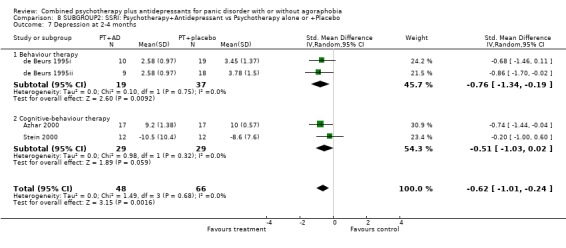
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 8.8.
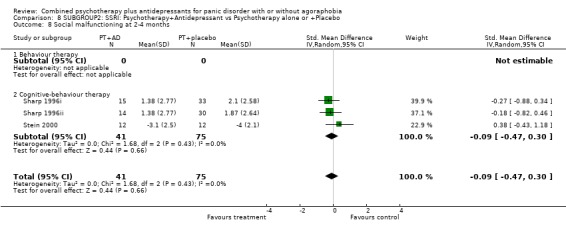
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social malfunctioning at 2‐4 months.
Analysis 8.9.
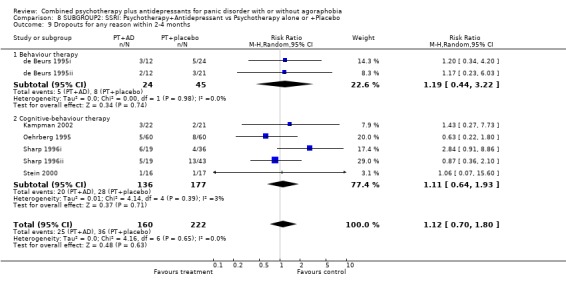
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 8.10.
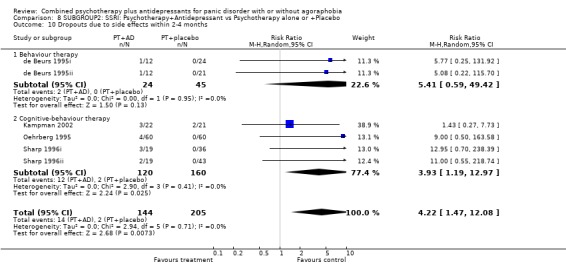
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 8.13.
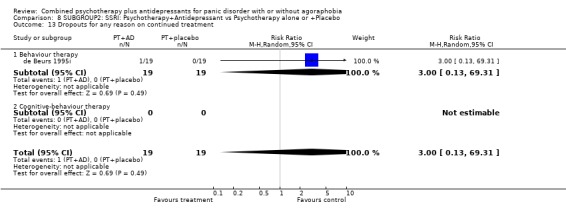
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 8.18.
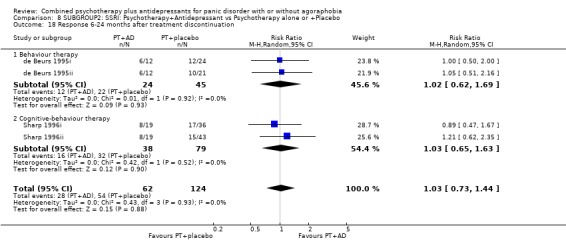
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 18 Response 6‐24 months after treatment discontinuation.
Analysis 8.19.
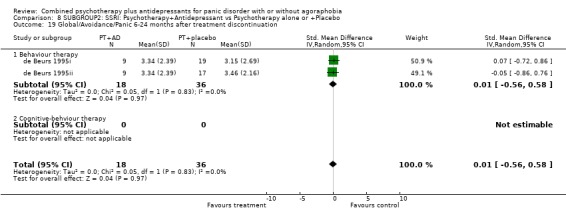
Comparison 8 SUBGROUP2: SSRI: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 9.
SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 5 | 223 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.88, 2.08] |
| 1.1 Behaviour therapy | 4 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.80, 1.40] |
| 1.2 Cognitive‐behaviour therapy | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 2.51 [1.16, 5.47] |
| 1.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 3 | 144 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [0.63, 2.96] |
| 2.1 Behaviour therapy | 2 | 114 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.62, 1.51] |
| 2.2 Cognitive‐behaviour therapy | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 5.14 [1.33, 19.92] |
| 2.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.45, 0.44] |
| 3.1 Behaviour therapy | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.45, 0.44] |
| 3.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.49, 0.19] |
| 4.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.49, 0.19] |
| 4.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 6 | 226 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐0.89, ‐0.13] |
| 5.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.01, ‐0.06] |
| 5.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.45, 0.39] |
| 5.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 3 | 120 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.77, 0.05] |
| 6.1 Behaviour therapy | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.60, 0.23] |
| 6.2 Cognitive‐behaviour therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.54, ‐0.04] |
| 6.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 5 | 168 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.77, ‐0.13] |
| 7.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.69, ‐0.01] |
| 7.2 Cognitive‐behaviour therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.69, ‐0.17] |
| 7.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 4 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.02, ‐0.05] |
| 8.1 Behavour therapy | 3 | 118 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.68, 0.08] |
| 8.2 Cognitive‐behaviour therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.08 [‐1.85, ‐0.30] |
| 8.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 5 | 223 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.72, 1.63] |
| 9.1 Behaviour therapy | 4 | 193 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.78, 1.88] |
| 9.2 Cognitive‐behaviour therapy | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 0.49 [0.16, 1.54] |
| 9.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 2 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.58] |
| 10.1 Behaviour therapy | 2 | 43 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.27, 3.58] |
| 10.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Response/remission on continued treatment | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.10, 3.41] |
| 11.1 Behaviour therapy | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.10, 3.41] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Psychdynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.51, ‐0.30] |
| 12.1 Behaviour therapy | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.51, ‐0.30] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.1 Behaviour therapy | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Response/remission immediately after treatment discontinuation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Global/Avoidance/Panic immediately after treatment discontinuation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 2 | 126 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [1.02, 2.17] |
| 16.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.95, 2.35] |
| 16.2 Cognitive‐behaviour therapy | 1 | 30 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [0.75, 2.90] |
| 16.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 9.1.
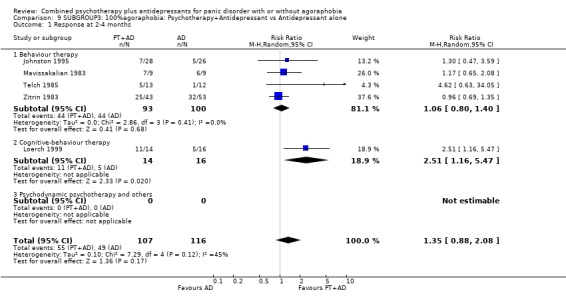
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 9.2.
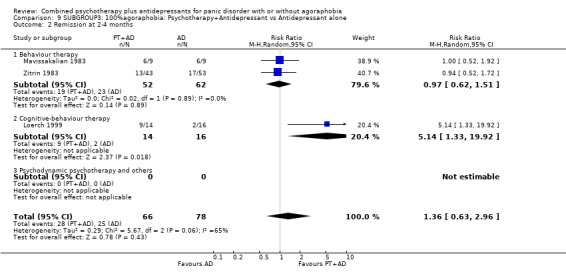
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 9.3.
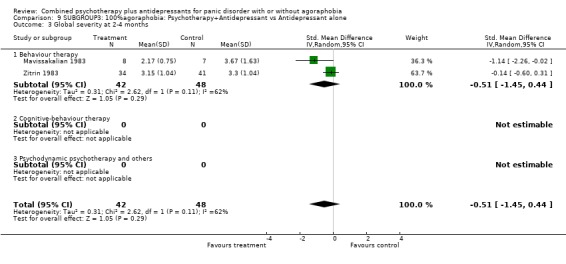
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 9.4.
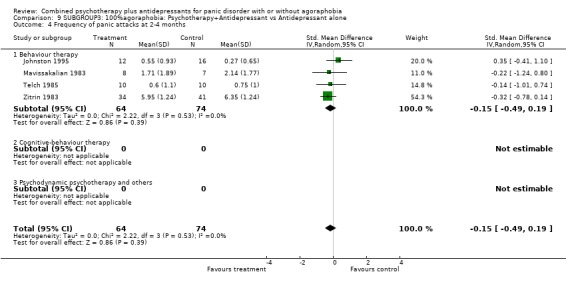
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 9.5.
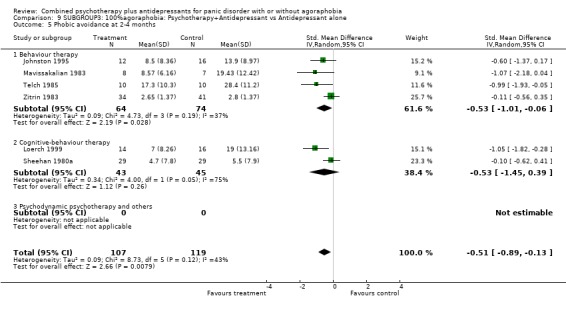
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 9.6.
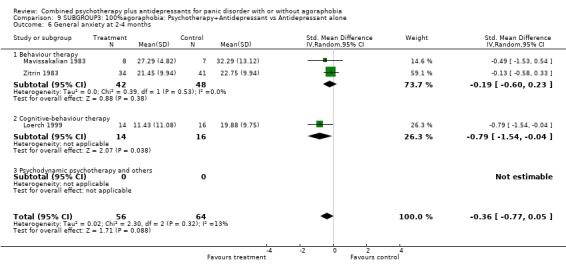
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 9.7.
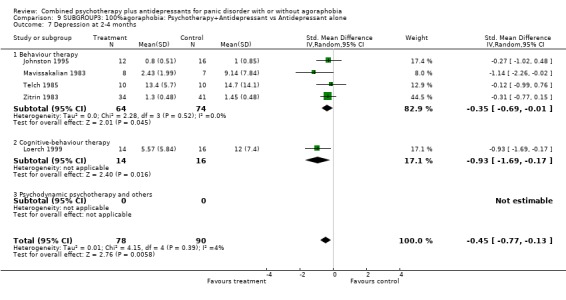
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 9.8.
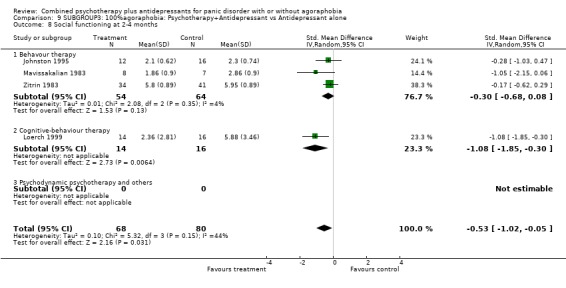
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 9.9.
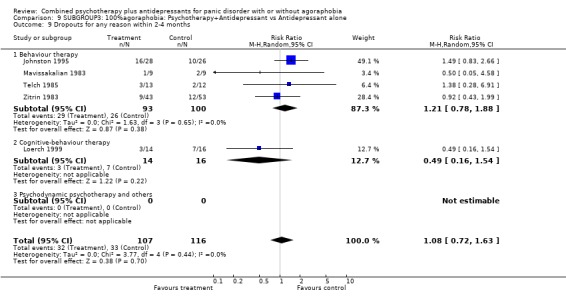
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 9.10.
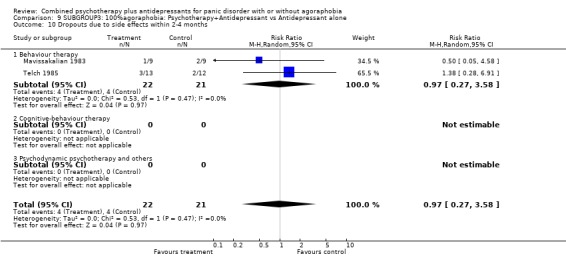
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 9.11.
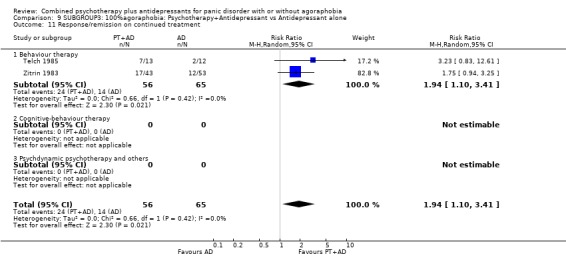
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 9.12.
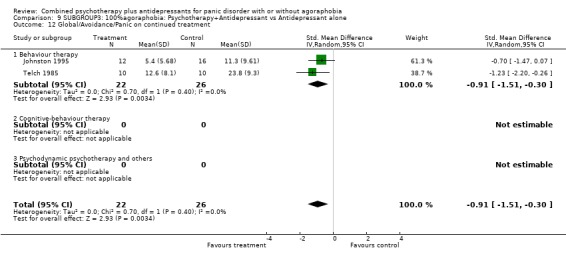
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 9.13.
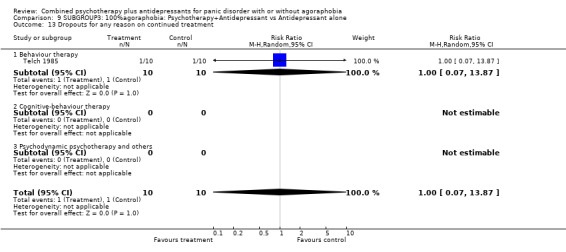
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 9.16.
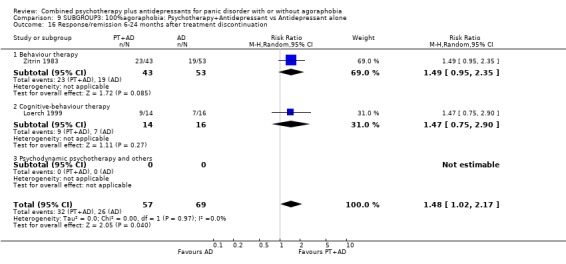
Comparison 9 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Comparison 10.
SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 12 | 576 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [1.00, 1.40] |
| 1.1 Behaviour therapy | 11 | 548 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.05, 1.56] |
| 1.2 Cognitive‐behaviour therapy | 1 | 28 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.65, 1.30] |
| 2 Remission at 2‐4 months | 11 | 510 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.02, 1.60] |
| 2.1 Behaviour therapy | 10 | 482 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.03, 1.66] |
| 2.2 Cognitive‐behaviour therapy | 1 | 28 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.62, 2.05] |
| 3 Global severity at 2‐4 months | 6 | 239 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐0.87, ‐0.34] |
| 3.1 Behaviour therapy | 6 | 239 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐0.87, ‐0.34] |
| 3.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 9 | 278 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.19, 0.31] |
| 4.1 Behaviour therapy | 9 | 278 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.19, 0.31] |
| 4.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 13 | 424 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [‐0.67, ‐0.12] |
| 5.1 Behaviour therapy | 12 | 396 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.70, ‐0.11] |
| 5.2 Cognitive‐behaviour therapy | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐1.03, 0.46] |
| 6 General anxiety at 2‐4 months | 10 | 330 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐0.85, ‐0.32] |
| 6.1 Behaviour therapy | 9 | 302 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐0.90, ‐0.37] |
| 6.2 Cognitive‐behaviour therapy | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.78, 0.70] |
| 7 Depression at 2‐4 months | 12 | 378 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.65, ‐0.16] |
| 7.1 Behaviour therapy | 11 | 350 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.69, ‐0.17] |
| 7.2 Cognitive‐behaviour therapy | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.90, 0.58] |
| 8 Social malfunctioning at 2‐4 months | 8 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.77, ‐0.17] |
| 8.1 Behaviour therapy | 7 | 260 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐0.84, ‐0.26] |
| 8.2 Cognitive‐behaviour therapy | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | 0.11 [‐0.63, 0.85] |
| 9 Dropouts for any reason within 2‐4 months | 11 | 508 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.91, 1.62] |
| 9.1 Behaviour therapy | 10 | 480 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.90, 1.60] |
| 9.2 Cognitive‐behaviour therapy | 1 | 28 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.35, 25.46] |
| 10 Dropouts due to side effects within 2‐4 months | 5 | 242 | Risk Ratio (M‐H, Random, 95% CI) | 1.99 [0.85, 4.62] |
| 10.1 Behaviour therapy | 5 | 242 | Risk Ratio (M‐H, Random, 95% CI) | 1.99 [0.85, 4.62] |
| 10.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Response/remission on continued treatment | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.90] |
| 11.1 Behaviour therapy | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.90] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 3 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.53] |
| 12.1 Behaviour therapy | 3 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.53] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 2 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 2.86 [0.32, 25.80] |
| 13.1 Behaviour therapy | 2 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 2.86 [0.32, 25.80] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18 Response 6‐24 months after treatment discontinuation | 8 | 347 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.79, 1.27] |
| 18.1 Behaviour therapy | 7 | 319 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.77, 1.31] |
| 18.2 Cognitive‐behaviour therapy | 1 | 28 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.58, 1.74] |
| 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 5 | 141 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.32, 0.43] |
| 19.1 Behaviour therapy | 5 | 141 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.32, 0.43] |
| 19.2 Cognitive‐behviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 10.1.
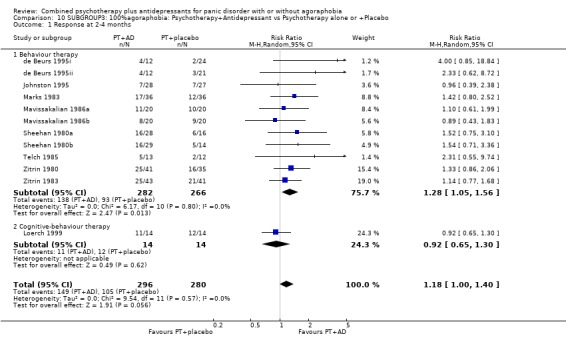
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 10.2.
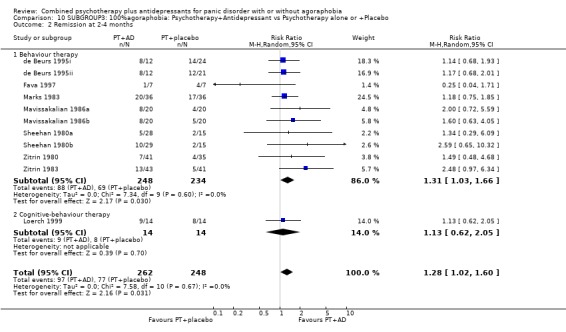
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 10.3.
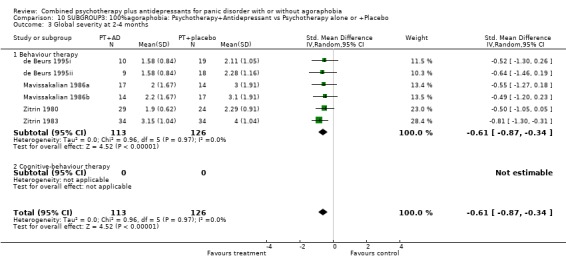
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 10.4.
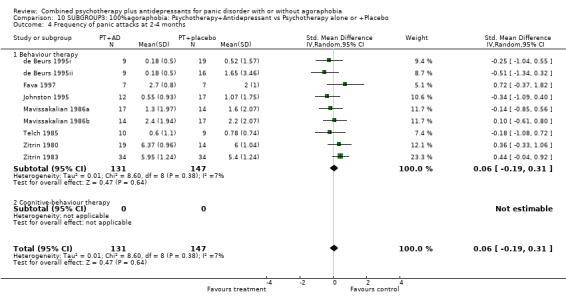
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 10.5.
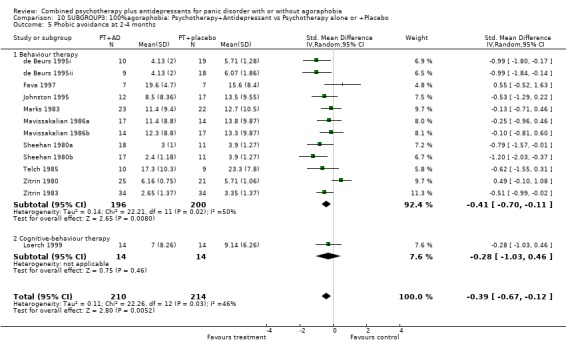
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 10.6.
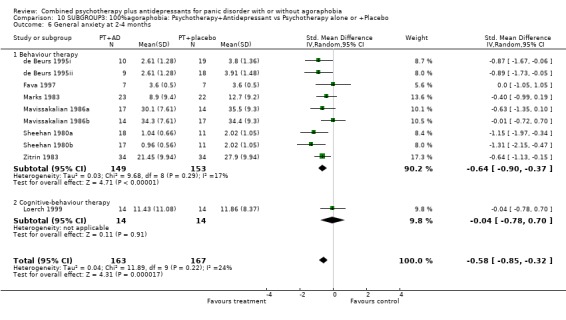
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 10.7.
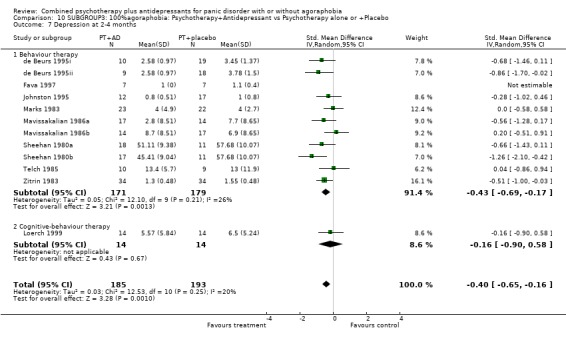
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 10.8.
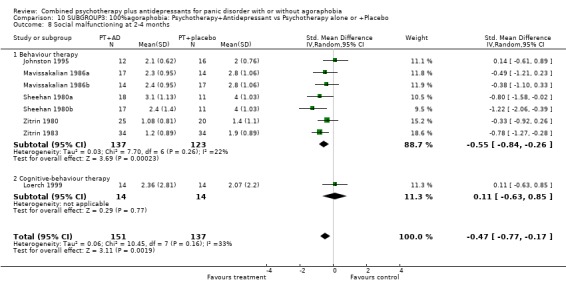
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social malfunctioning at 2‐4 months.
Analysis 10.9.
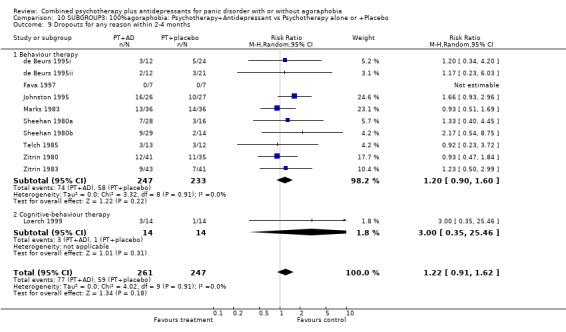
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 10.10.
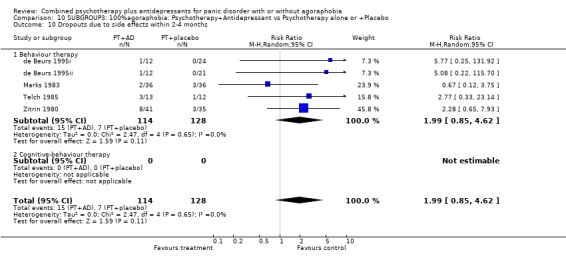
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 10.11.
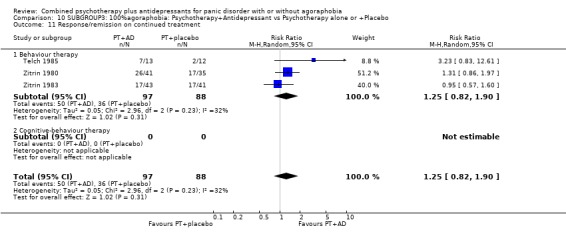
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 10.12.
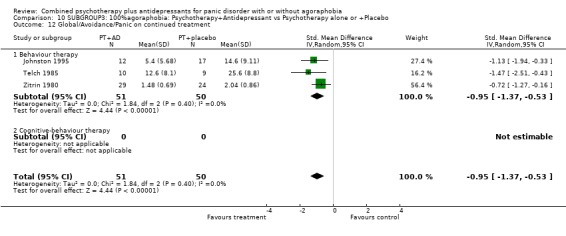
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 10.13.
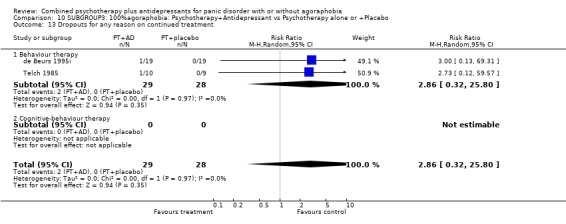
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 10.18.
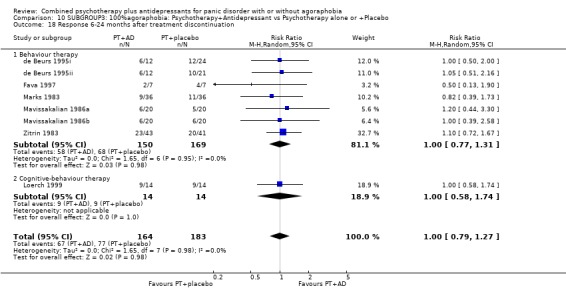
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 18 Response 6‐24 months after treatment discontinuation.
Analysis 10.19.
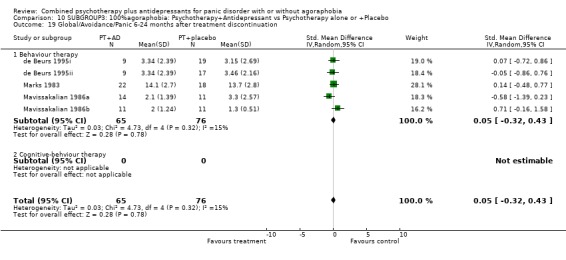
Comparison 10 SUBGROUP3: 100%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 11.
SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.84, 1.38] |
| 1.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.84, 1.38] |
| 2 Remission at 2‐4 months | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.85, 1.40] |
| 2.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.85, 1.40] |
| 3 Global severity at 2‐4 months | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.55, 0.04] |
| 3.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.55, 0.04] |
| 4 Frequency of panic attacks at 2‐4 months | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social malfunctioning at 2‐4 months | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.62, 1.60] |
| 9.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.62, 1.60] |
| 10 Dropouts due to side effects within 2‐4 months | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 6.33 [0.67, 59.70] |
| 10.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 6.33 [0.67, 59.70] |
| 11 Response/remission on continued treatment | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 12 Global/Avoidance/Panic on continued treatment | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 13 Dropouts for any reason on continued treatment | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 13.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 18 Response 6‐24 months after treatment discontinuation | 2 | 194 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.46, 1.19] |
| 18.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 18.2 Cognitive‐behaviour therapy | 2 | 194 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.46, 1.19] |
| 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
| 19.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 19.2 Cognitive‐behviour therapy | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
Analysis 11.1.
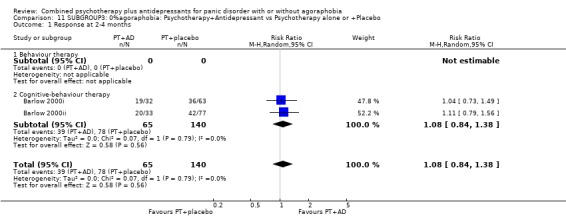
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 11.2.
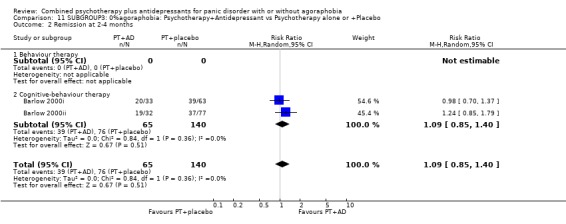
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 11.3.
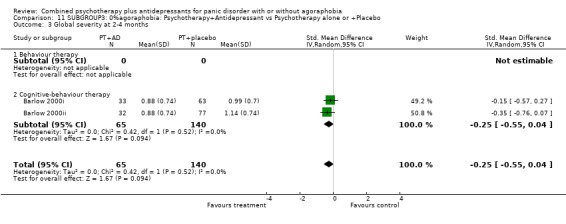
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 11.9.
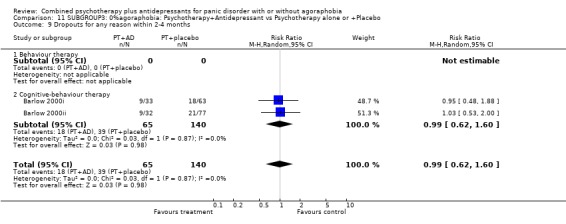
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 11.10.
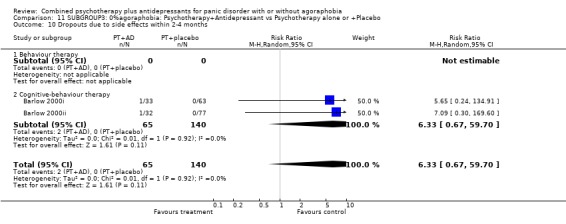
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 11.11.
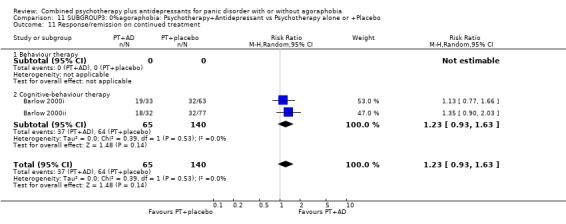
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 11.12.
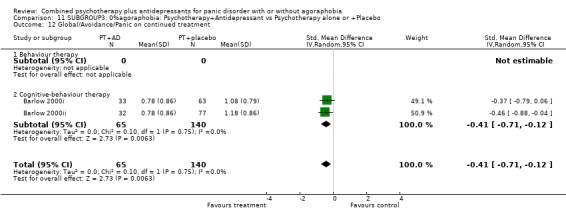
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 11.13.
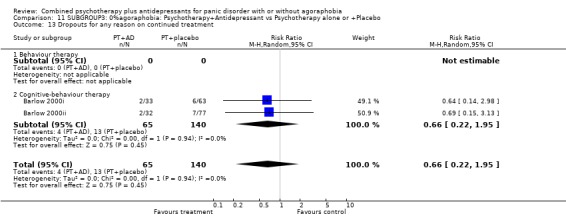
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 11.18.
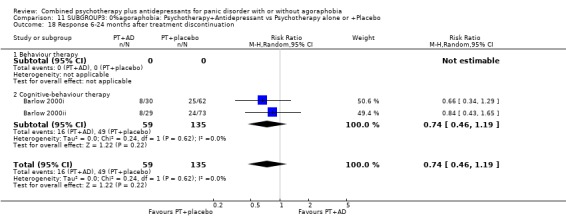
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 18 Response 6‐24 months after treatment discontinuation.
Analysis 11.19.
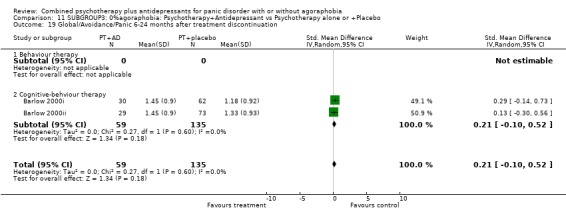
Comparison 11 SUBGROUP3: 0%agoraphobia: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 19 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 12.
SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 5 | 265 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.86, 1.82] |
| 1.1 Behaviour therapy | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [0.35, 7.03] |
| 1.2 Cognitive‐behaviour therapy | 3 | 144 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.79, 2.39] |
| 1.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 3 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.72, 2.51] |
| 2.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.52, 1.72] |
| 2.2 Cognitive‐behaviour therapy | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 2.13 [0.45, 10.10] |
| 2.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 2 | 133 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.63, 0.05] |
| 3.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.60, 0.31] |
| 3.2 Cognitive‐behaviour therapy | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.01, 0.04] |
| 3.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 3 | 134 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.51, 0.17] |
| 4.1 Behaviour therapy | 2 | 95 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.69, 0.13] |
| 4.2 Cognitive‐behaviour therapy | 1 | 39 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.55, 0.71] |
| 4.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 4 | 164 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.39 [1.00, 0.21] |
| 5.1 Behaviour therapy | 2 | 95 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.29, 0.39] |
| 5.2 Cognitive‐behaviour therapy | 2 | 69 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐1.67, 0.96] |
| 5.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 3 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.74, ‐0.03] |
| 6.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.58, 0.33] |
| 6.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.01, ‐0.15] |
| 6.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 4 | 164 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.69, ‐0.06] |
| 7.1 Behaviour therapy | 2 | 95 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.67, 0.14] |
| 7.2 Cognitive‐behaviour therapy | 2 | 69 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐1.22, 0.11] |
| 7.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 3 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.89, 0.04] |
| 8.1 Behavour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.62, 0.29] |
| 8.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.39, 0.12] |
| 8.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 5 | 265 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.57, 1.31] |
| 9.1 Behaviour therapy | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.00 [0.50, 1.99] |
| 9.2 Cognitive‐behaviour therapy | 3 | 144 | Risk Ratio (M‐H, Random, 95% CI) | 0.79 [0.46, 1.34] |
| 9.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 3 | 139 | Risk Ratio (M‐H, Random, 95% CI) | 1.43 [0.63, 3.27] |
| 10.1 Behaviour therapy | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.28, 6.91] |
| 10.2 Cognitive‐behaviour therapy | 2 | 114 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [0.55, 3.80] |
| 10.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Response/remission on continued treatment | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.10, 3.41] |
| 11.1 Behaviour therapy | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.10, 3.41] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Psychdynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐2.20, ‐0.26] |
| 12.1 Behaviour therapy | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐2.20, ‐0.26] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.1 Behaviour therapy | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Response/remission immediately after treatment discontinuation | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15 Global/Avoidance/Panic immediately after treatment discontinuation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 3 | 200 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [1.08, 2.07] |
| 16.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.95, 2.35] |
| 16.2 Cognitive‐behaviour therapy | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.94, 2.38] |
| 16.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 12.1.
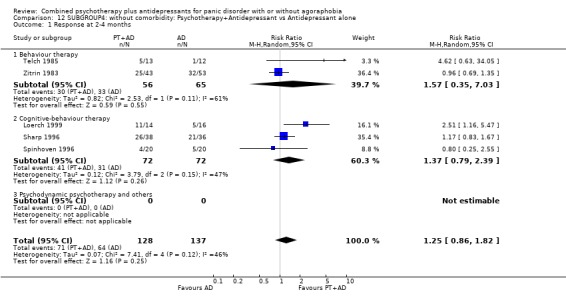
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 12.2.
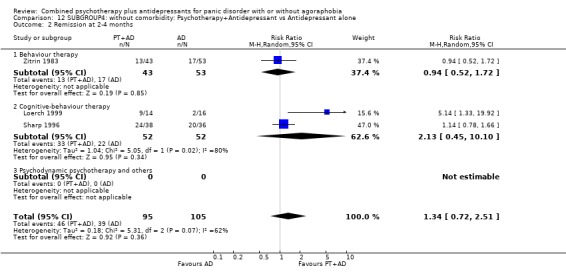
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 12.3.
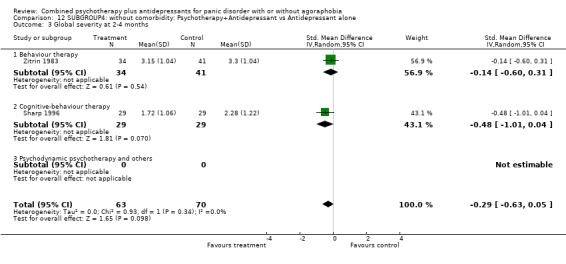
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 12.4.
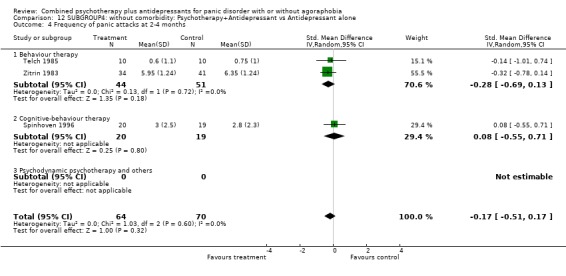
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 12.5.
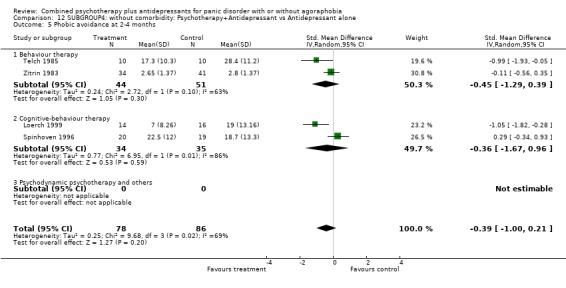
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 12.6.
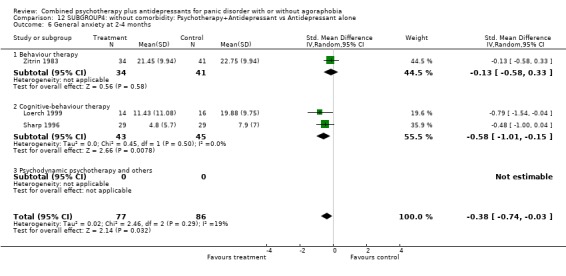
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 12.7.
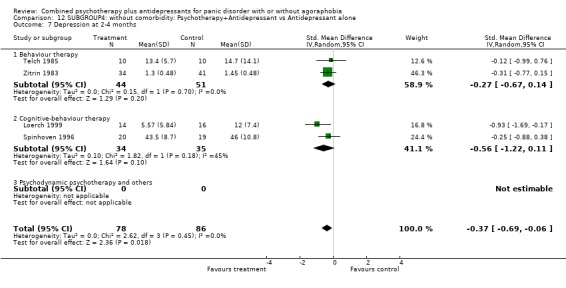
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 12.8.
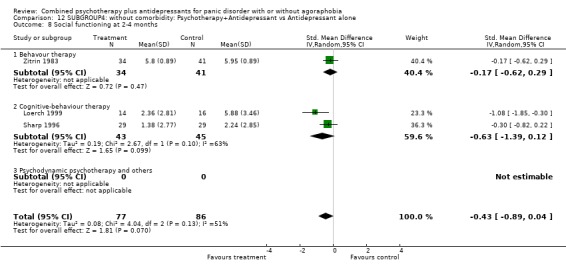
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 12.9.
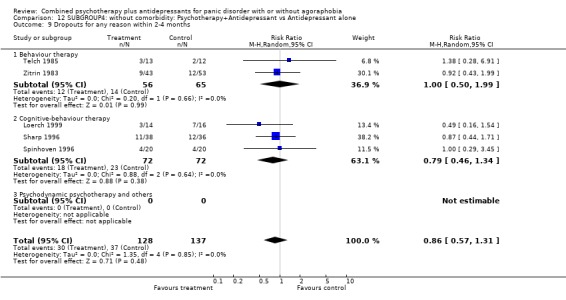
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 12.10.
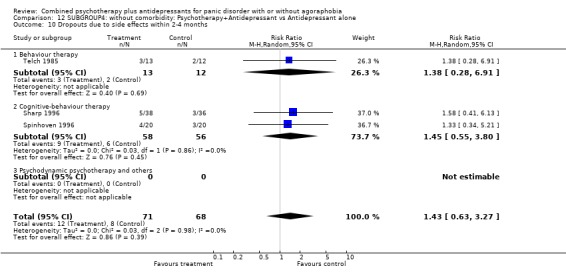
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 12.11.
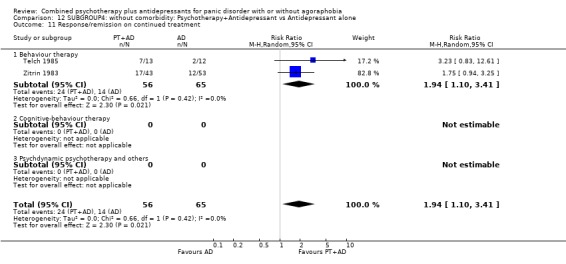
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 12.12.
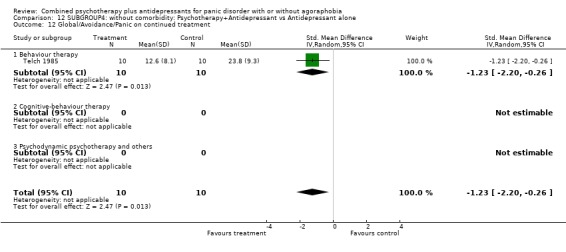
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 12.13.
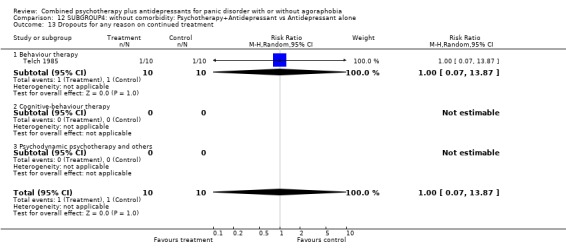
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 12.16.
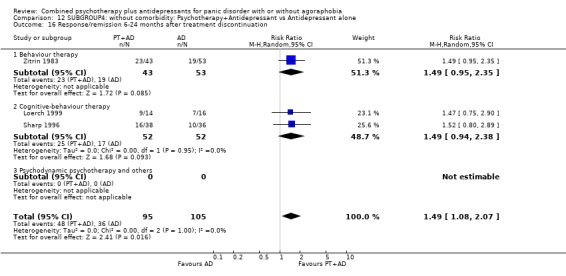
Comparison 12 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Comparison 13.
SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 12 | 675 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [1.01, 1.32] |
| 1.1 Behaviour therapy | 6 | 337 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.97, 1.51] |
| 1.2 Cognitive‐behaviour therapy | 6 | 338 | Risk Ratio (M‐H, Random, 95% CI) | 1.12 [0.89, 1.40] |
| 2 Remission at 2‐4 months | 10 | 610 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [1.11, 1.70] |
| 2.1 Behaviour therapy | 5 | 312 | Risk Ratio (M‐H, Random, 95% CI) | 1.45 [1.04, 2.03] |
| 2.2 Cognitive‐behaviour therapy | 5 | 298 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [0.95, 1.84] |
| 3 Global severity at 2‐4 months | 6 | 275 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.71, ‐0.21] |
| 3.1 Behaviour therapy | 4 | 183 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐0.92, ‐0.32] |
| 3.2 Cognitive‐behaviour therapy | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.56, 0.32] |
| 4 Frequency of panic attacks at 2‐4 months | 7 | 329 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.22, 0.29] |
| 4.1 Behaviour therapy | 5 | 182 | Std. Mean Difference (IV, Random, 95% CI) | 0.20 [‐0.09, 0.49] |
| 4.2 Cognitive‐behaviour therapy | 2 | 147 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.60, 0.25] |
| 5 Phobic avoidance at 2‐4 months | 11 | 424 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.35, 0.04] |
| 5.1 Behaviour therapy | 6 | 240 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.49, 0.16] |
| 5.2 Cognitive‐behaviour therapy | 5 | 184 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.43, 0.17] |
| 6 General anxiety at 2‐4 months | 9 | 426 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.55, ‐0.16] |
| 6.1 Behaviour therapy | 4 | 175 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.76, ‐0.16] |
| 6.2 Cognitive‐behaviour therapy | 5 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.53, ‐0.02] |
| 7 Depression at 2‐4 months | 8 | 286 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.41, 0.06] |
| 7.1 Behaviour therapy | 5 | 194 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.52, 0.09] |
| 7.2 Cognitive‐behaviour therapy | 3 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.07 [‐0.47, 0.34] |
| 8 Social functioning at 2‐4 months | 8 | 319 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.27, 0.39] |
| 8.1 Behaviour therapy | 4 | 175 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.51, 0.71] |
| 8.2 Cognitive‐behaviour therapy | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.39, 0.30] |
| 9 Dropouts for any reason within 2‐4 months | 10 | 595 | Risk Ratio (M‐H, Random, 95% CI) | 1.06 [0.77, 1.45] |
| 9.1 Behaviour therapy | 4 | 257 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.67, 1.44] |
| 9.2 Cognitive‐behaviour therapy | 6 | 338 | Risk Ratio (M‐H, Random, 95% CI) | 1.35 [0.68, 2.68] |
| 10 Dropouts due to side effects within 2‐4 months | 7 | 450 | Risk Ratio (M‐H, Random, 95% CI) | 2.81 [1.29, 6.11] |
| 10.1 Behaviour therapy | 3 | 173 | Risk Ratio (M‐H, Random, 95% CI) | 1.68 [0.67, 4.18] |
| 10.2 Cognitive‐behaviour therapy | 4 | 277 | Risk Ratio (M‐H, Random, 95% CI) | 10.34 [2.41, 44.39] |
| 11 Response/remission on continued treatment | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.90] |
| 11.1 Behaviour therapy | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.90] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 2 | 72 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.65, ‐0.27] |
| 12.1 Behaviour therapy | 2 | 72 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.96 [‐1.65, ‐0.27] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 1 | 19 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 13.1 Behaviour therapy | 1 | 19 | Risk Ratio (M‐H, Random, 95% CI) | 2.73 [0.12, 59.57] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Response/remission 6 months after treatment discontinuation | 6 | 297 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.80, 1.52] |
| 14.1 Behaviour therapy | 3 | 152 | Risk Ratio (M‐H, Random, 95% CI) | 1.42 [0.61, 3.32] |
| 14.2 Cognitive‐behaviour therapy | 3 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.71, 1.45] |
| 15 Global/Avoidance/Panic 6 months after treatment discontinuation | 3 | 90 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.43, 0.49] |
| 15.1 Behaviour therapy | 3 | 90 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.43, 0.49] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Response/remission 18‐24 months after treatment discontinuation | 4 | 236 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.75, 1.43] |
| 16.1 Behaviour therapy | 4 | 236 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.75, 1.43] |
| 16.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Global/Avoidance/Panic 18‐24 months after treatment discontinuation | 3 | 87 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.59, 0.75] |
| 17.1 Behaviour therapy | 3 | 87 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.59, 0.75] |
| 17.2 Cognitive‐behviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 13.1.
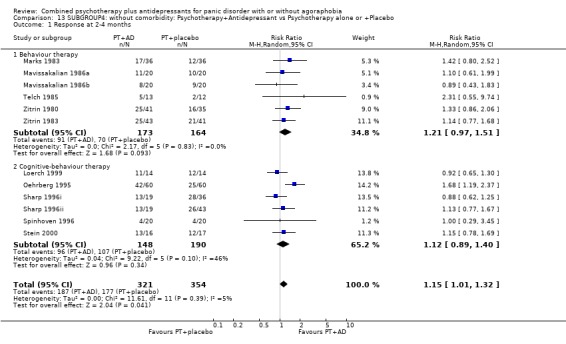
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 13.2.
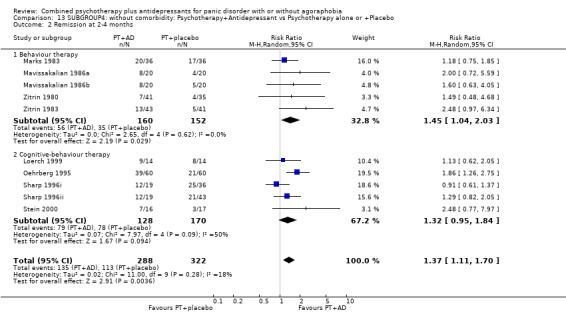
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 13.3.
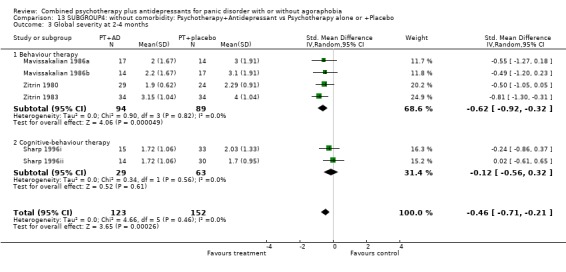
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 13.4.
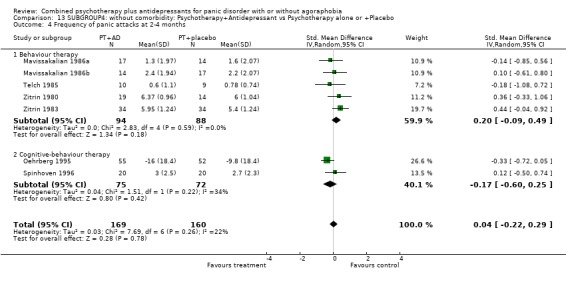
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 13.5.
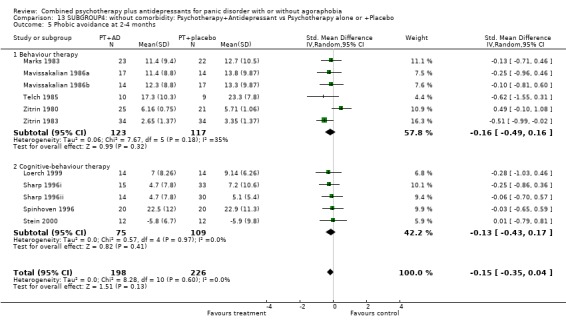
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 13.6.
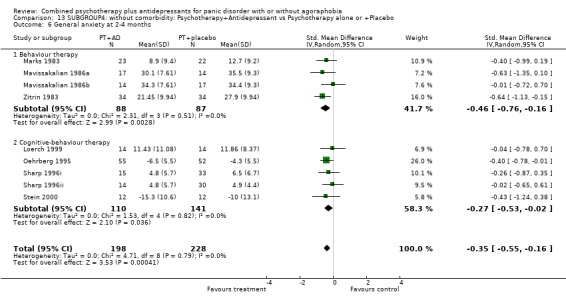
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 13.7.
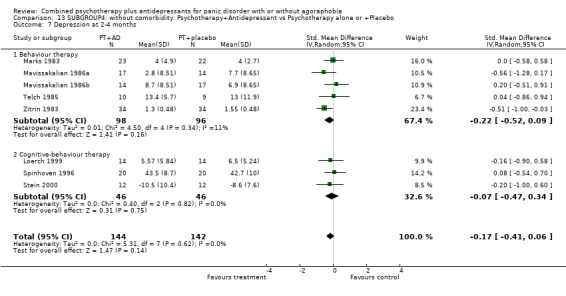
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 13.8.
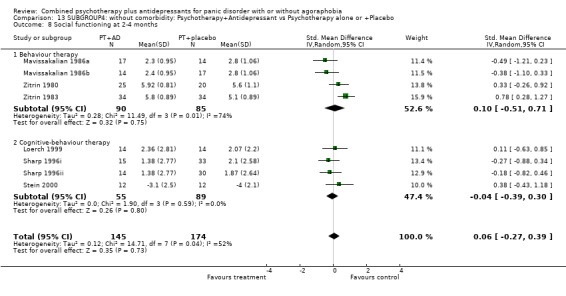
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social functioning at 2‐4 months.
Analysis 13.9.
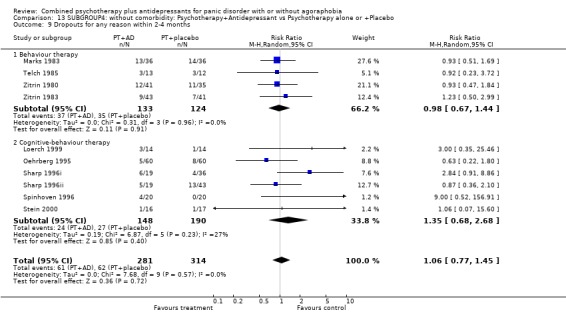
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 13.10.
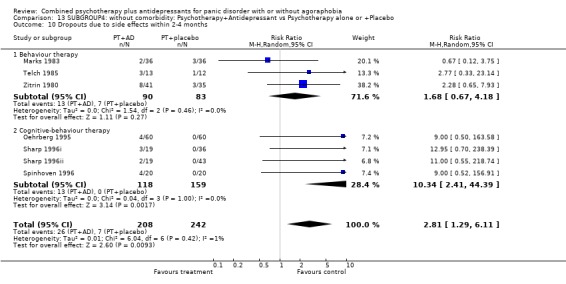
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 13.11.
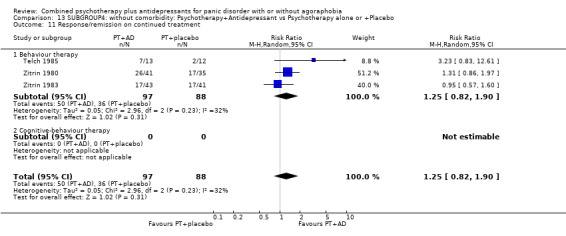
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 13.12.
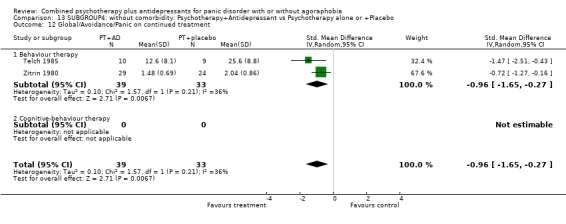
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 13.13.
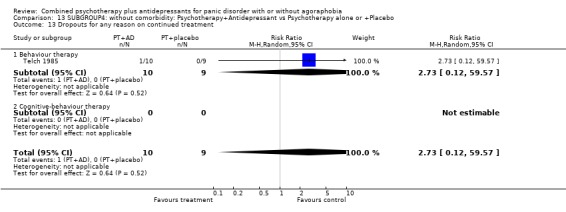
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 13.14.
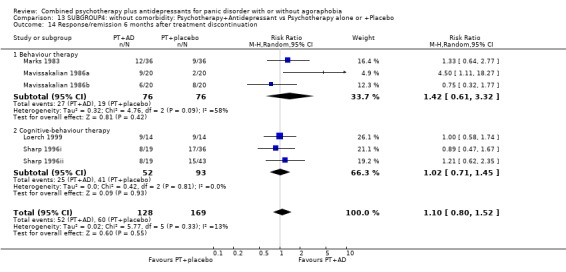
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 14 Response/remission 6 months after treatment discontinuation.
Analysis 13.15.
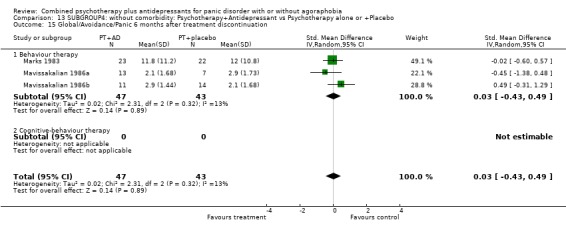
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 15 Global/Avoidance/Panic 6 months after treatment discontinuation.
Analysis 13.16.
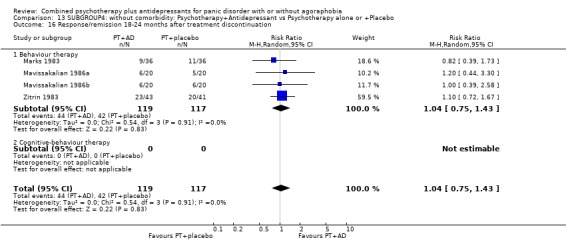
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 16 Response/remission 18‐24 months after treatment discontinuation.
Analysis 13.17.
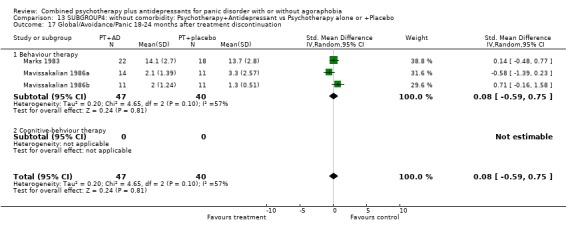
Comparison 13 SUBGROUP4: without comorbidity: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 17 Global/Avoidance/Panic 18‐24 months after treatment discontinuation.
Comparison 14.
SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 7 | 467 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.05, 1.64] |
| 1.1 Behaviour therapy | 3 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.66, 2.07] |
| 1.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [1.01, 1.84] |
| 1.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.64 [1.07, 2.50] |
| 2 Remission at 2‐4 months | 5 | 388 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [1.04, 1.58] |
| 2.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.52, 1.72] |
| 2.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.92, 2.14] |
| 2.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.02, 1.72] |
| 3 Global severity at 2‐4 months | 4 | 321 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.53, ‐0.09] |
| 3.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.60, 0.31] |
| 3.2 Cognitive‐behaviour therapy | 2 | 206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.57, ‐0.02] |
| 3.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.33, ‐0.05] |
| 4 Frequency of panic attacks at 2‐4 months | 4 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.51, 0.26] |
| 4.1 Behaviour therapy | 3 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.51, 0.26] |
| 4.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 6 | 251 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.79, ‐0.14] |
| 5.1 Behaviour therapy | 3 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.95, 0.07] |
| 5.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.45, 0.39] |
| 5.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.60 [‐1.23, 0.04] |
| 6 General anxiety at 2‐4 months | 4 | 203 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.12, ‐0.13] |
| 6.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.58, 0.33] |
| 6.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.01, ‐0.15] |
| 6.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.32 [‐2.01, ‐0.63] |
| 7 Depression at 2‐4 months | 5 | 193 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.47 [‐0.76, ‐0.18] |
| 7.1 Behaviour therapy | 3 | 123 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.27 [‐0.62, 0.09] |
| 7.2 Cognitive‐behaviour therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.69, ‐0.17] |
| 7.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.44, ‐0.14] |
| 8 Social functioning at 2‐4 months | 5 | 231 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐0.78, ‐0.14] |
| 8.1 Behavour therapy | 2 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.59, 0.19] |
| 8.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.39, 0.12] |
| 8.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.46, ‐0.16] |
| 9 Dropouts for any reason within 2‐4 months | 7 | 467 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.69, 1.22] |
| 9.1 Behaviour therapy | 3 | 175 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.81, 1.96] |
| 9.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.06] |
| 9.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 10 Dropouts due to side effects within 2‐4 months | 4 | 287 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.31, 2.73] |
| 10.1 Behaviour therapy | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.28, 6.91] |
| 10.2 Cognitive‐behaviour therapy | 2 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.09, 4.15] |
| 10.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 11 Response/remission on continued treatment | 4 | 309 | Risk Ratio (M‐H, Random, 95% CI) | 1.63 [1.21, 2.19] |
| 11.1 Behaviour therapy | 2 | 121 | Risk Ratio (M‐H, Random, 95% CI) | 1.94 [1.10, 3.41] |
| 11.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.07, 2.16] |
| 11.3 Psychdynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 4 | 236 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐0.92, ‐0.31] |
| 12.1 Behaviour therapy | 2 | 48 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.91 [‐1.51, ‐0.30] |
| 12.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.74, ‐0.09] |
| 12.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.85 [‐1.50, ‐0.20] |
| 13 Dropouts for any reason on continued treatment | 3 | 208 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.27, 1.90] |
| 13.1 Behaviour therapy | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.22, 2.39] |
| 13.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.05, 5.08] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 5 | 376 | Risk Ratio (M‐H, Random, 95% CI) | 1.61 [1.23, 2.11] |
| 16.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.95, 2.35] |
| 16.2 Cognitive‐behaviour therapy | 3 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.00, 2.11] |
| 16.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.2 [1.45, 7.05] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.78, 0.63] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 1 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.34, 0.34] |
| 17.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐1.91, ‐0.55] |
Analysis 14.1.
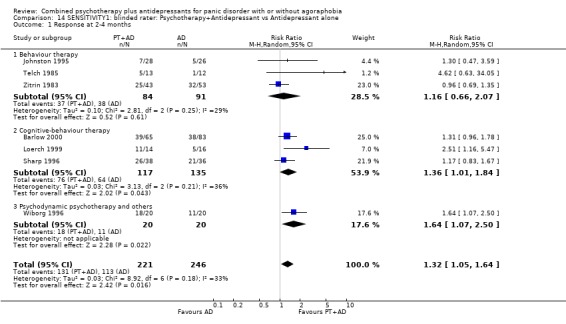
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 14.2.
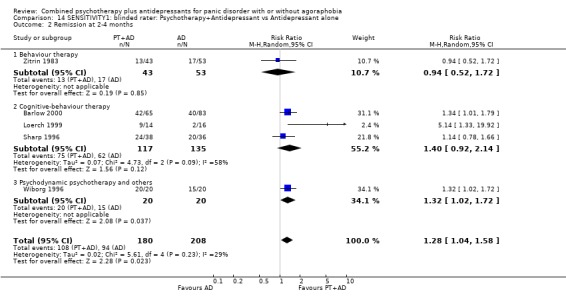
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 14.3.
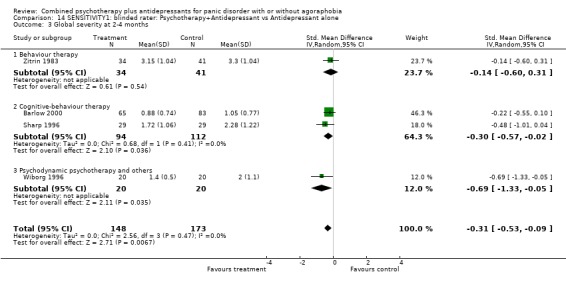
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 14.4.
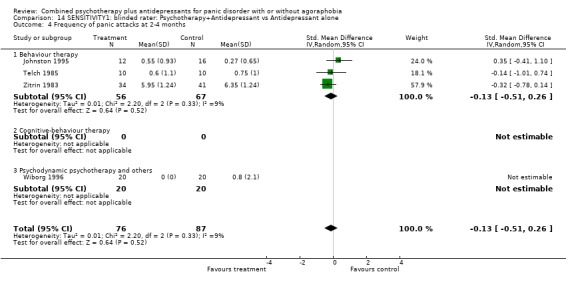
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 14.5.
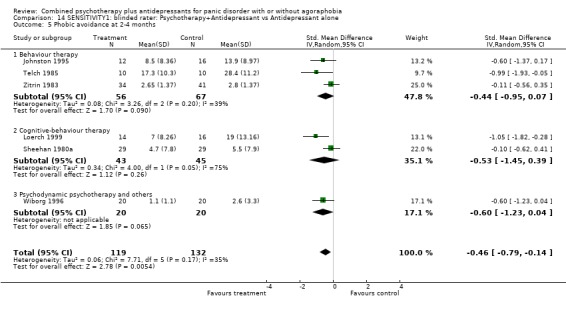
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 14.6.
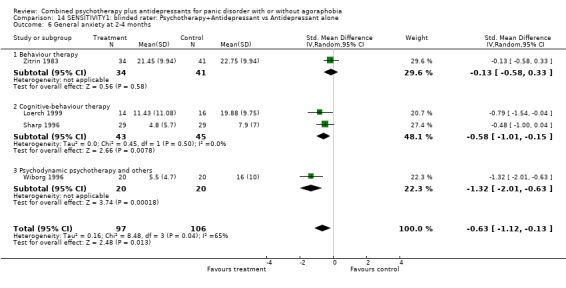
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 14.7.
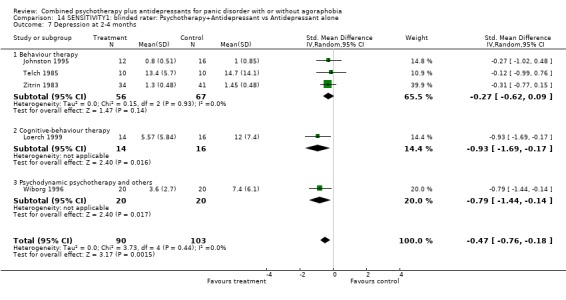
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 14.8.
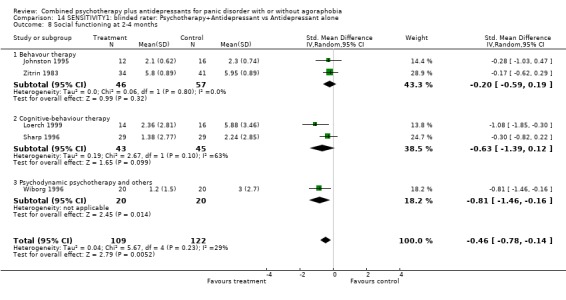
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 14.9.
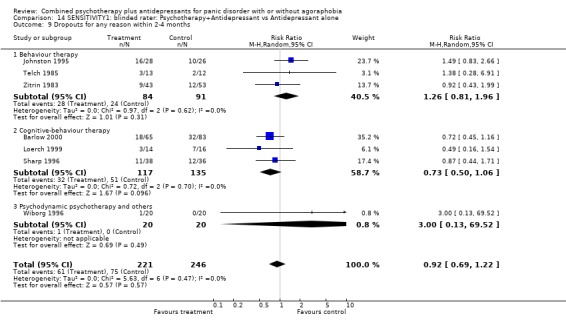
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 14.10.
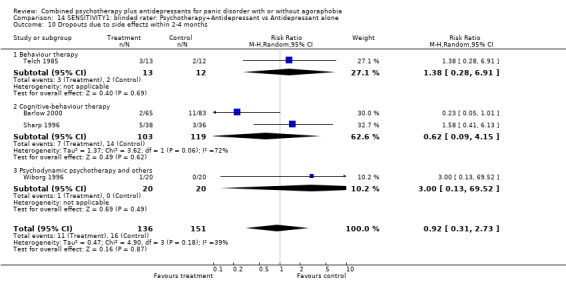
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 14.11.
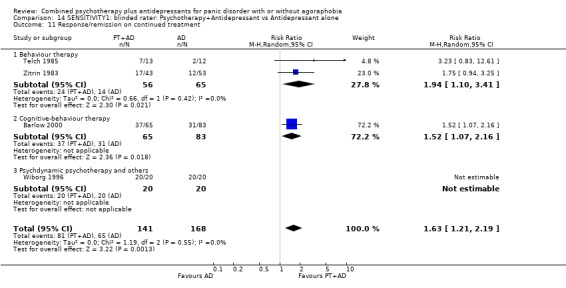
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 14.12.
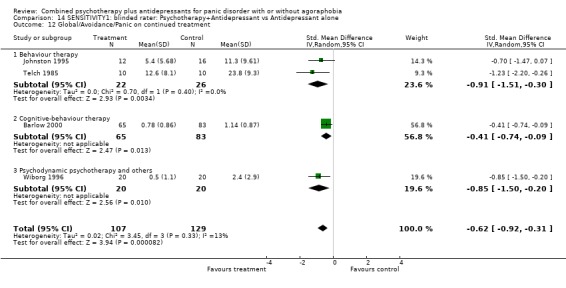
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 14.13.
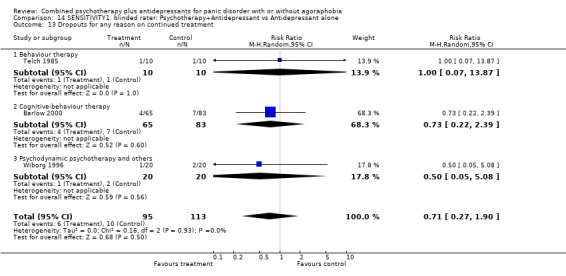
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 14.16.
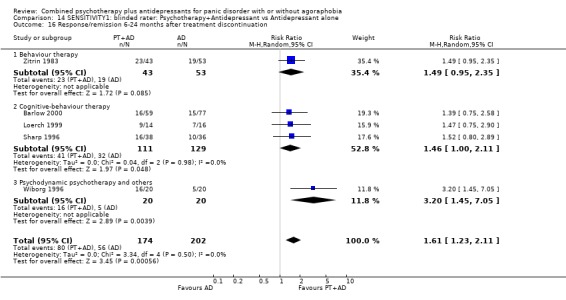
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Analysis 14.17.
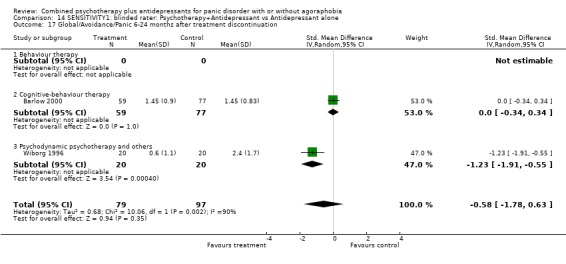
Comparison 14 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 15.
SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 20 | 1173 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [1.08, 1.35] |
| 1.1 Behaviour therapy | 11 | 548 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [1.09, 1.56] |
| 1.2 Cognitive‐behaviour therapy | 9 | 625 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.99, 1.40] |
| 1.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 19 | 1107 | Risk Ratio (M‐H, Random, 95% CI) | 1.24 [1.09, 1.42] |
| 2.1 Behaviour therapy | 10 | 482 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.03, 1.66] |
| 2.2 Cognitive‐behaviour therapy | 9 | 625 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.02, 1.47] |
| 2.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 11 | 602 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.60, ‐0.26] |
| 3.1 Behaviour therapy | 6 | 239 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐0.87, ‐0.34] |
| 3.2 Cognitive‐behaviour therapy | 5 | 363 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.54, ‐0.08] |
| 3.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 11 | 423 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.05 [‐0.26, 0.17] |
| 4.1 Behaviour therapy | 9 | 278 | Std. Mean Difference (IV, Random, 95% CI) | 0.06 [‐0.19, 0.31] |
| 4.2 Cognitive‐behaviour therapy | 2 | 145 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.29 [‐0.61, 0.04] |
| 5 Phobic avoidance at 2‐4 months | 18 | 644 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.52, ‐0.13] |
| 5.1 Behaviour therapy | 12 | 396 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.70, ‐0.11] |
| 5.2 Cognitive‐behaviour therapy | 6 | 248 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.49, 0.03] |
| 5.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 16 | 657 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.61, ‐0.27] |
| 6.1 Behaviour therapy | 9 | 302 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.64 [‐0.90, ‐0.37] |
| 6.2 Cognitive‐behaviour therapy | 7 | 355 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.50, ‐0.07] |
| 6.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 14 | 468 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.61, ‐0.21] |
| 7.1 Behaviour therapy | 11 | 350 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.69, ‐0.17] |
| 7.2 Cognitive‐behaviour therapy | 3 | 118 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.76, ‐0.01] |
| 7.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 11 | 404 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.46, 0.23] |
| 8.1 Behaviour therapy | 7 | 260 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.73, 0.34] |
| 8.2 Cognitive‐behaviour therapy | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.39, 0.30] |
| 9 Dropouts for any reason within 2‐4 months | 19 | 1105 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.94, 1.45] |
| 9.1 Behaviour therapy | 10 | 480 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.90, 1.60] |
| 9.2 Cognitive‐behaviour therapy | 9 | 625 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.80, 1.58] |
| 9.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 12 | 806 | Risk Ratio (M‐H, Random, 95% CI) | 2.85 [1.50, 5.41] |
| 10.1 Behaviour therapy | 5 | 242 | Risk Ratio (M‐H, Random, 95% CI) | 1.99 [0.85, 4.62] |
| 10.2 Cognitive‐behaviour therapy | 7 | 564 | Risk Ratio (M‐H, Random, 95% CI) | 4.66 [1.73, 12.52] |
| 11 Response/remission on continued treatment | 5 | 390 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.00, 1.51] |
| 11.1 Behaviour therapy | 3 | 185 | Risk Ratio (M‐H, Random, 95% CI) | 1.25 [0.82, 1.90] |
| 11.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 12 Global/Avoidance/Panic on continued treatment | 5 | 306 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐0.97, ‐0.33] |
| 12.1 Behaviour therapy | 3 | 101 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.95 [‐1.37, ‐0.53] |
| 12.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 13 Dropouts for any reason on continued treatment | 4 | 262 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.33, 2.32] |
| 13.1 Behaviour therapy | 2 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 2.86 [0.32, 25.80] |
| 13.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 11 | 644 | Risk Ratio (M‐H, Random, 95% CI) | 0.97 [0.80, 1.18] |
| 14.1 Behaviour therapy | 6 | 305 | Risk Ratio (M‐H, Random, 95% CI) | 1.03 [0.79, 1.36] |
| 14.2 Cognitive‐behaviour therapy | 5 | 339 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.69, 1.21] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 7 | 335 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.09, 0.37] |
| 15.1 Behaviour therapy | 5 | 141 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.32, 0.43] |
| 15.2 Cognitive‐behaviour therapy | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
Analysis 15.1.
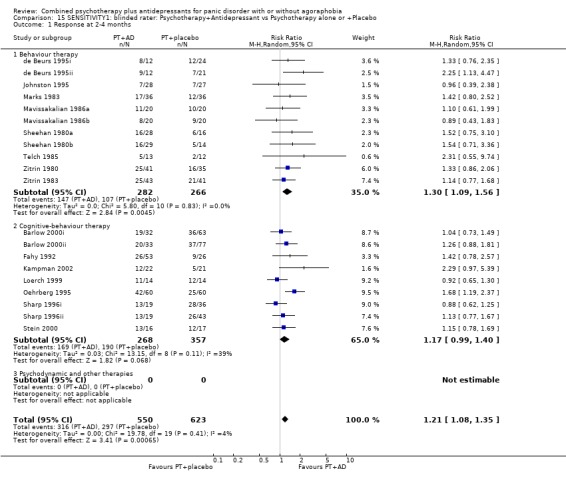
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 15.2.
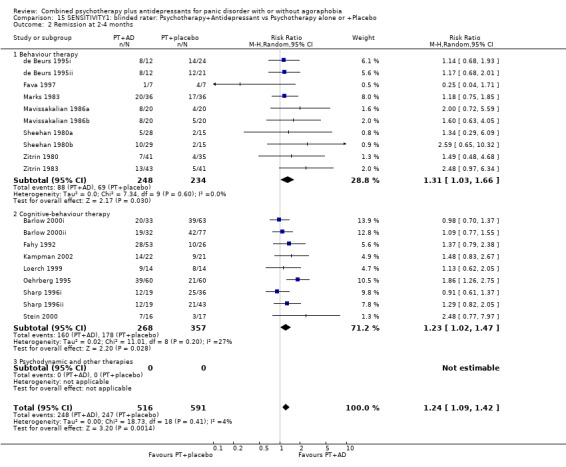
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 15.3.
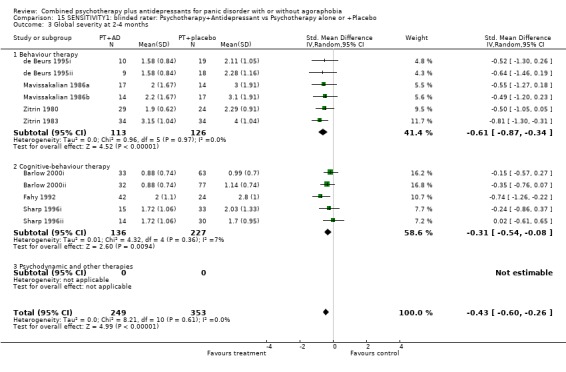
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 15.4.
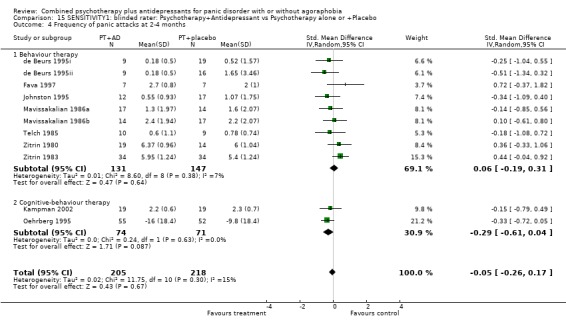
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 15.5.
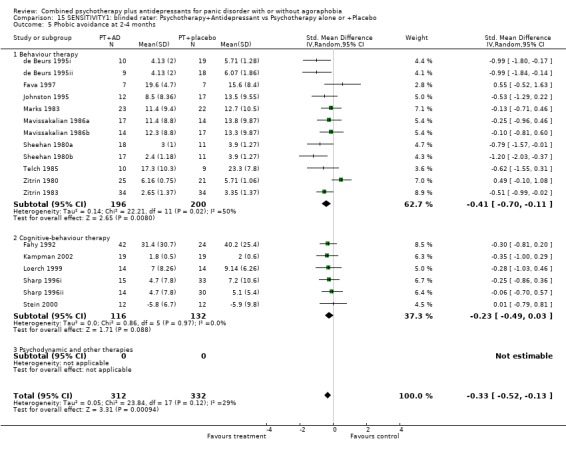
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 15.6.
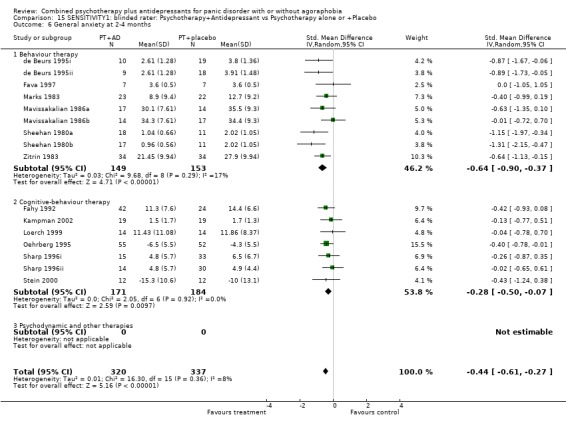
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 15.7.
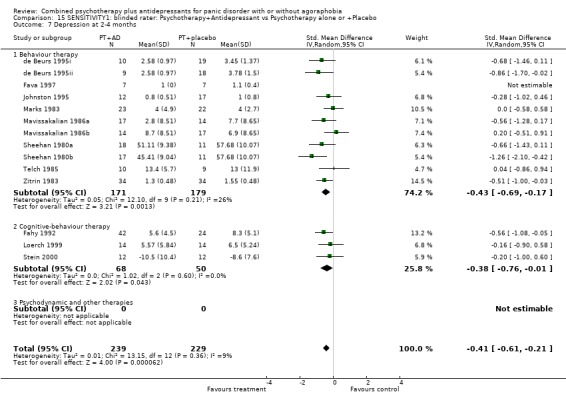
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 15.8.
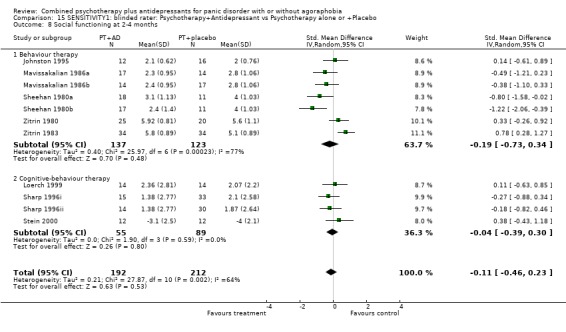
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social functioning at 2‐4 months.
Analysis 15.9.
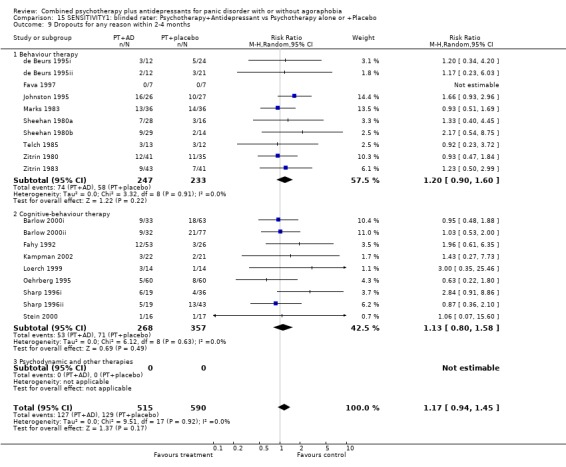
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 15.10.
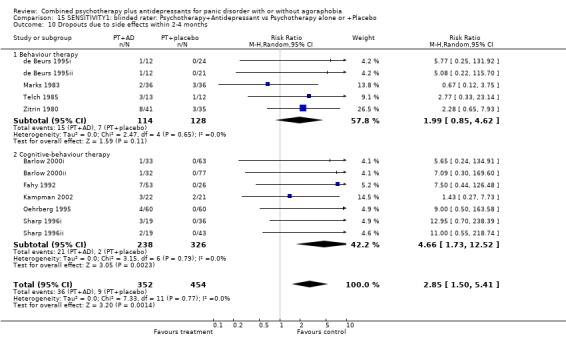
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 15.11.
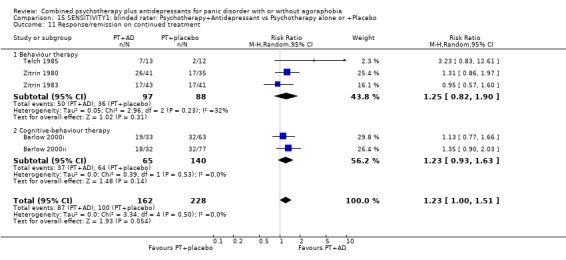
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 15.12.
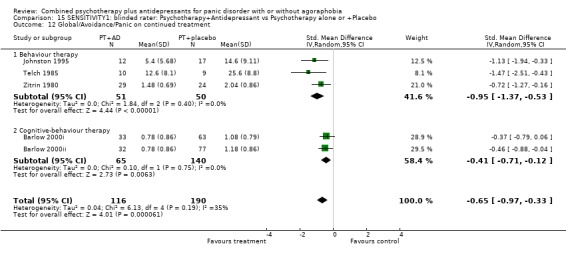
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 15.13.
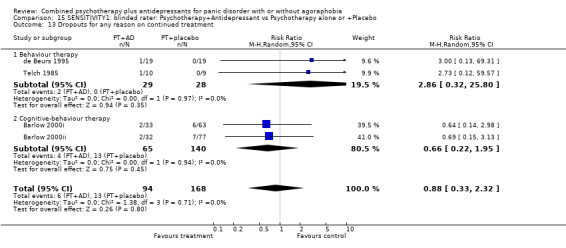
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 15.14.
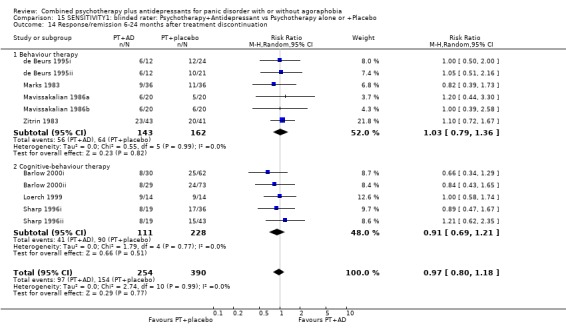
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 15.15.
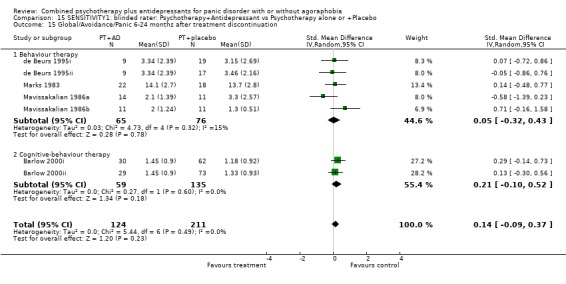
Comparison 15 SENSITIVITY1: blinded rater: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 16.
SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 4 | 348 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.95, 1.61] |
| 1.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.69, 1.35] |
| 1.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.36 [1.01, 1.84] |
| 1.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 4 | 348 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.91, 1.78] |
| 2.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.94 [0.52, 1.72] |
| 2.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.92, 2.14] |
| 2.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 3 | 281 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.49, ‐0.02] |
| 3.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.60, 0.31] |
| 3.2 Cognitive‐behaviour therapy | 2 | 206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.57, ‐0.02] |
| 3.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.78, 0.14] |
| 4.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.78, 0.14] |
| 4.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 2 | 105 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.44, 0.39] |
| 5.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.11 [‐0.56, 0.35] |
| 5.2 Cognitive‐behaviour therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐1.82, ‐0.28] |
| 5.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 3 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.74, ‐0.03] |
| 6.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.58, 0.33] |
| 6.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.01, ‐0.15] |
| 6.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 2 | 105 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐1.13, 0.05] |
| 7.1 Behaviour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.77, 0.15] |
| 7.2 Cognitive‐behaviour therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.69, ‐0.17] |
| 7.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 3 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.89, 0.04] |
| 8.1 Behavour therapy | 1 | 75 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.62, 0.29] |
| 8.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.39, 0.12] |
| 8.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 4 | 348 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.55, 1.07] |
| 9.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 0.92 [0.43, 1.99] |
| 9.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.50, 1.06] |
| 9.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 2 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.09, 4.15] |
| 10.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Cognitive‐behaviour therapy | 2 | 222 | Risk Ratio (M‐H, Random, 95% CI) | 0.62 [0.09, 4.15] |
| 10.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Response/remission on continued treatment | 2 | 244 | Risk Ratio (M‐H, Random, 95% CI) | 1.57 [1.16, 2.14] |
| 11.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.75 [0.94, 3.25] |
| 11.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.07, 2.16] |
| 11.3 Psychdynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.74, ‐0.09] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.74, ‐0.09] |
| 12.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.22, 2.39] |
| 13.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.22, 2.39] |
| 13.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 4 | 336 | Risk Ratio (M‐H, Random, 95% CI) | 1.47 [1.10, 1.96] |
| 16.1 Behaviour therapy | 1 | 96 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.95, 2.35] |
| 16.2 Cognitive‐behaviour therapy | 3 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.00, 2.11] |
| 16.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 1 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.34, 0.34] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 1 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.34, 0.34] |
| 17.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 16.1.
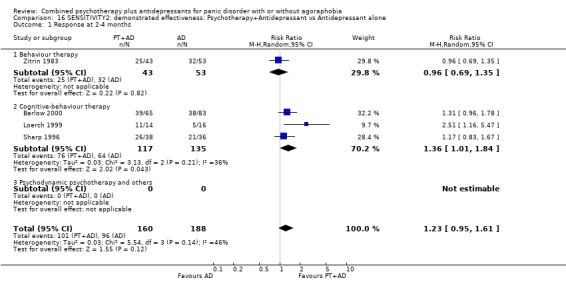
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 16.2.
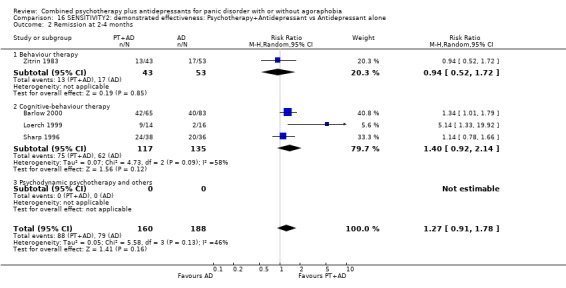
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 16.3.
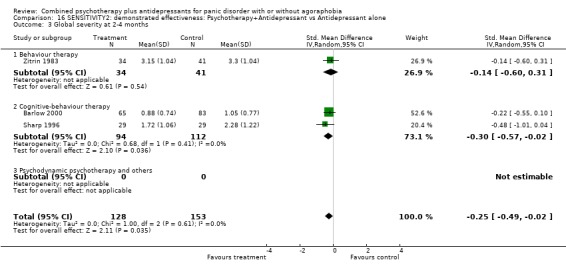
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 16.4.
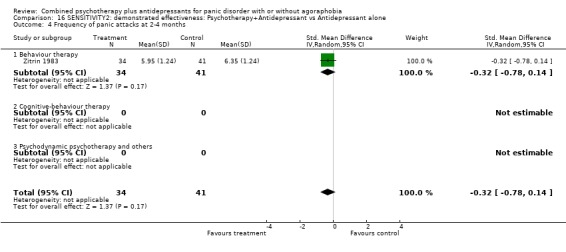
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 16.5.
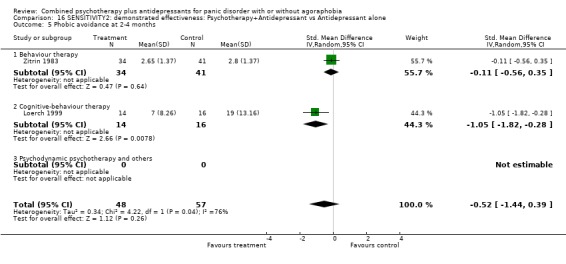
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 16.6.
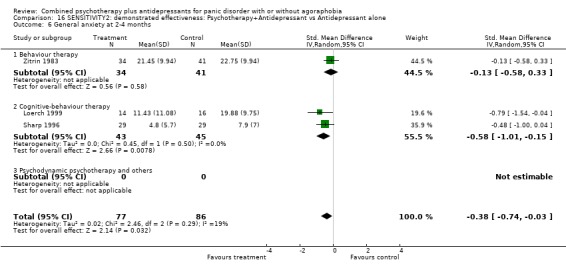
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 16.7.
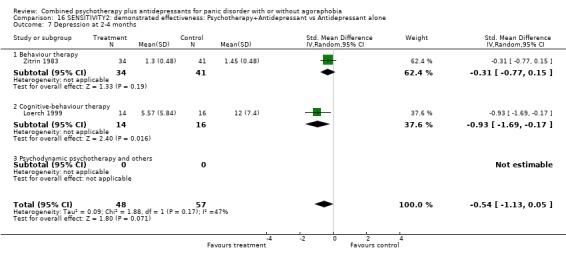
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 16.8.
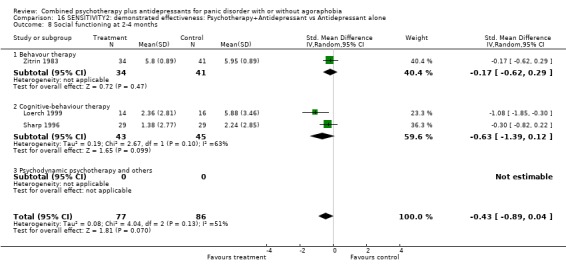
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 16.9.
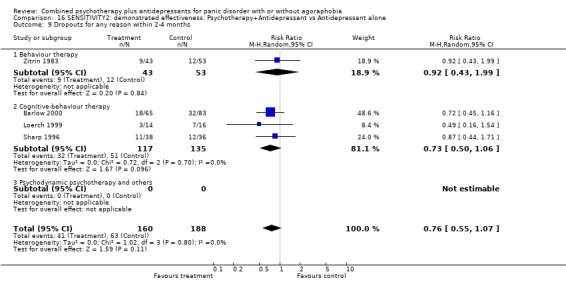
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 16.10.
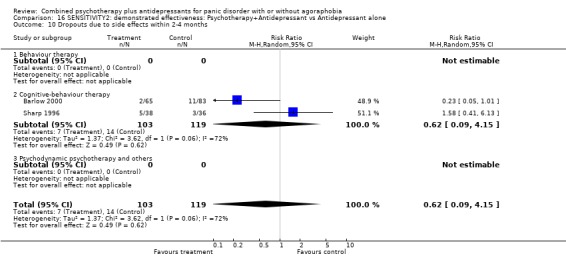
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 16.11.
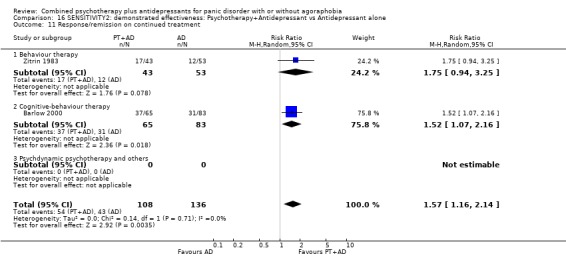
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 16.12.
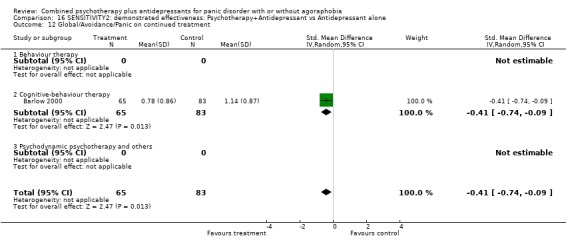
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 16.13.
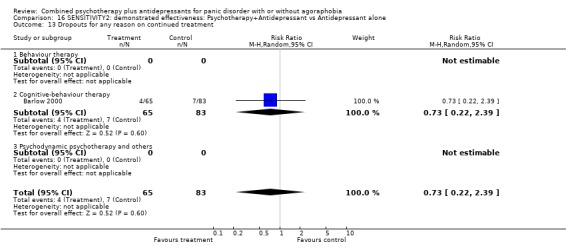
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 16.16.
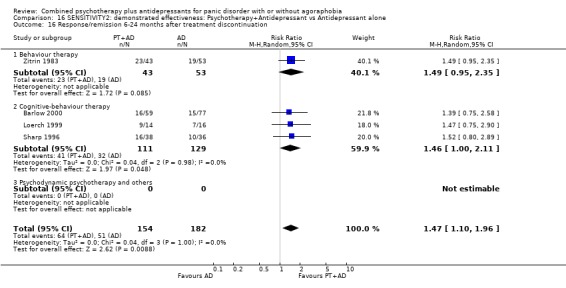
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Analysis 16.17.
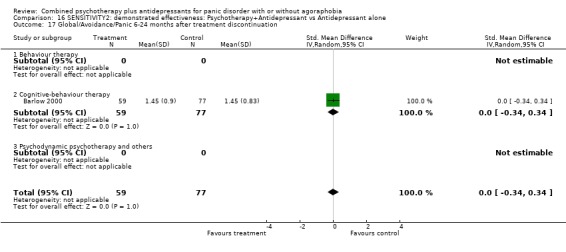
Comparison 16 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 17.
SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 9 | 546 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.96, 1.35] |
| 1.1 Behaviour therapy | 3 | 153 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.96, 2.00] |
| 1.2 Cognitive‐behaviour therapy | 6 | 393 | Risk Ratio (M‐H, Random, 95% CI) | 1.07 [0.89, 1.28] |
| 1.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 10 | 560 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.95, 1.29] |
| 2.1 Behaviour therapy | 4 | 167 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.75, 2.00] |
| 2.2 Cognitive‐behaviour therapy | 6 | 393 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.91, 1.29] |
| 2.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 7 | 421 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.57, ‐0.15] |
| 3.1 Behaviour therapy | 3 | 124 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.08, ‐0.33] |
| 3.2 Cognitive‐behaviour therapy | 4 | 297 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.21 [‐0.46, 0.04] |
| 3.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 5 | 173 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.36, 0.46] |
| 4.1 Behaviour therapy | 4 | 135 | Std. Mean Difference (IV, Random, 95% CI) | 0.10 [‐0.43, 0.63] |
| 4.2 Cognitive‐behaviour therapy | 1 | 38 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.79, 0.49] |
| 5 Phobic avoidance at 2‐4 months | 8 | 296 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.65, ‐0.12] |
| 5.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.55 [‐1.10, 0.00] |
| 5.2 Cognitive‐behaviour therapy | 4 | 158 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.56, 0.09] |
| 5.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 8 | 296 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.61, ‐0.12] |
| 6.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.01, ‐0.30] |
| 6.2 Cognitive‐behaviour therapy | 4 | 158 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.45, 0.20] |
| 6.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 5 | 166 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐0.86, ‐0.20] |
| 7.1 Behaviour therapy | 4 | 138 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐0.99, ‐0.25] |
| 7.2 Cognitive‐behaviour therapy | 1 | 28 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐0.90, 0.58] |
| 7.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 4 | 188 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.39, 0.66] |
| 8.1 Behaviour therapy | 1 | 68 | Std. Mean Difference (IV, Random, 95% CI) | 0.78 [0.28, 1.27] |
| 8.2 Cognitive‐behaviour therapy | 3 | 120 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐0.52, 0.24] |
| 9 Dropouts for any reason within 2‐4 months | 10 | 560 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.84, 1.61] |
| 9.1 Behaviour therapy | 4 | 167 | Risk Ratio (M‐H, Random, 95% CI) | 1.21 [0.62, 2.35] |
| 9.2 Cognitive‐behaviour therapy | 6 | 393 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.79, 1.67] |
| 9.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 7 | 434 | Risk Ratio (M‐H, Random, 95% CI) | 4.18 [1.53, 11.45] |
| 10.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 5.41 [0.59, 49.42] |
| 10.2 Cognitive‐behaviour therapy | 5 | 365 | Risk Ratio (M‐H, Random, 95% CI) | 3.91 [1.26, 12.12] |
| 11 Response/remission on continued treatment | 3 | 289 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.91, 1.49] |
| 11.1 Behaviour therapy | 1 | 84 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.57, 1.60] |
| 11.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 12 Global/Avoidance/Panic on continued treatment | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 13 Dropouts for any reason on continued treatment | 3 | 243 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.28, 2.16] |
| 13.1 Behaviour therapy | 1 | 38 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.31] |
| 13.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 8 | 485 | Risk Ratio (M‐H, Random, 95% CI) | 0.95 [0.77, 1.18] |
| 14.1 Behaviour therapy | 3 | 146 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.73, 1.41] |
| 14.2 Cognitive‐behaviour therapy | 5 | 339 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.69, 1.21] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 4 | 248 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.11, 0.43] |
| 15.1 Behaviour therapy | 2 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.56, 0.58] |
| 15.2 Cognitive‐behaviour therapy | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
Analysis 17.1.
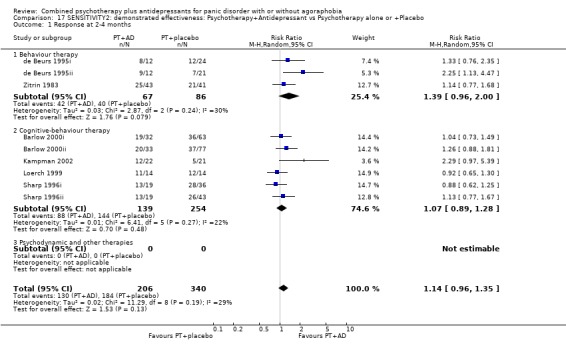
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 17.2.
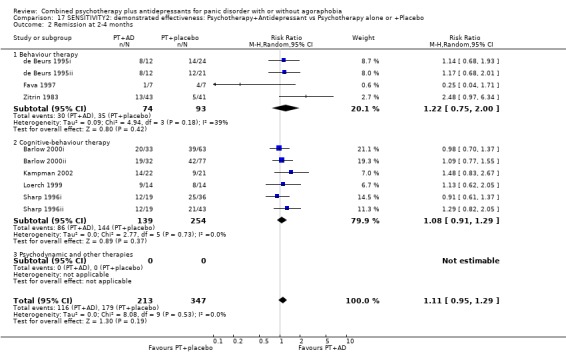
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 17.3.
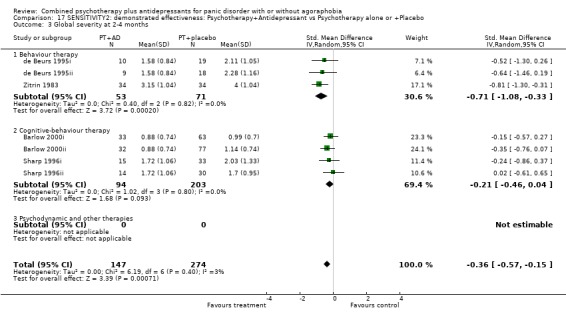
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 17.4.
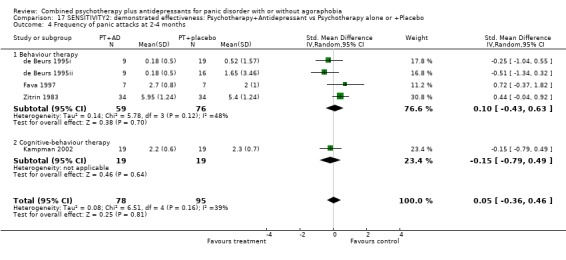
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 17.5.
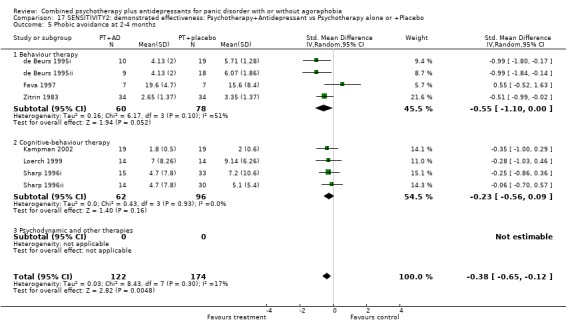
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 17.6.
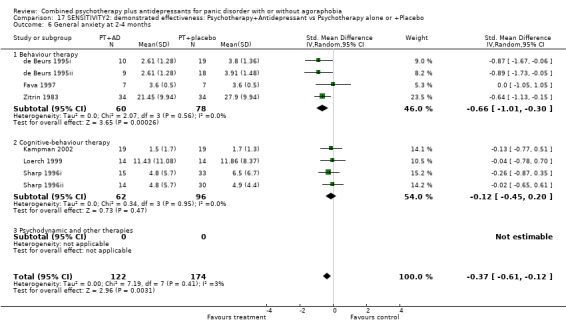
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 17.7.
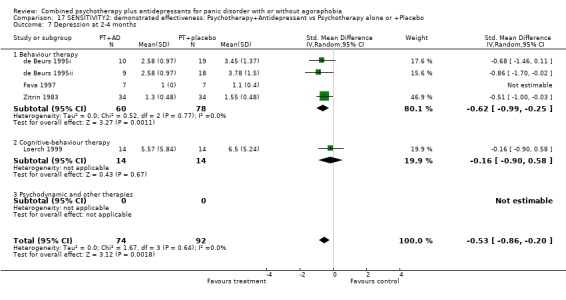
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 17.8.
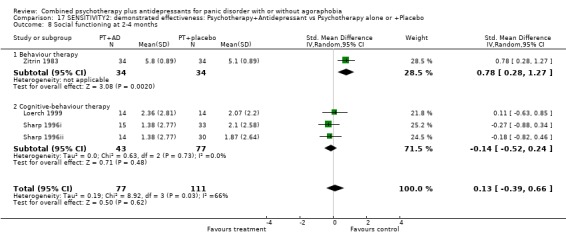
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social functioning at 2‐4 months.
Analysis 17.9.
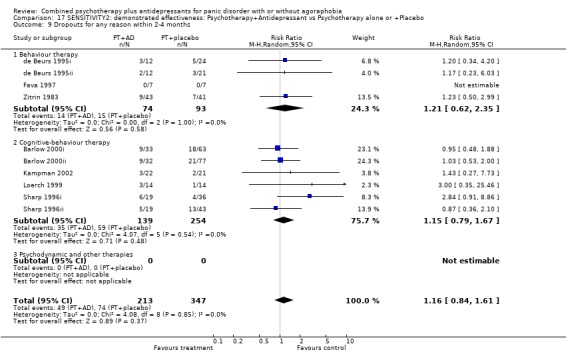
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 17.10.
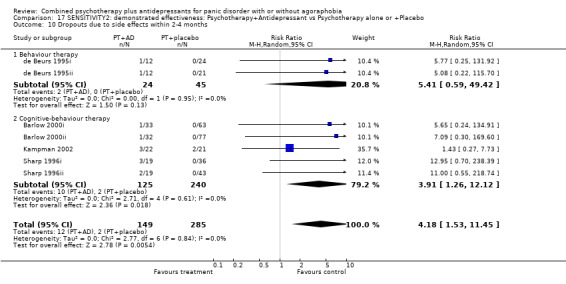
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 17.11.
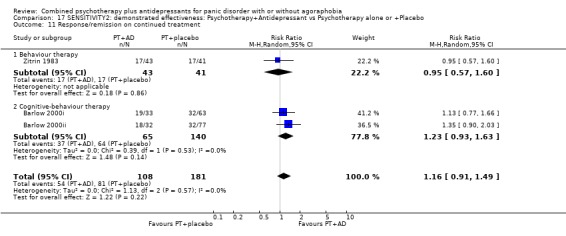
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 17.12.
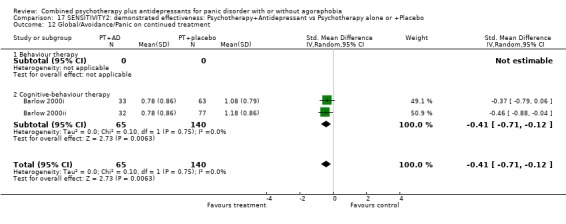
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 17.13.
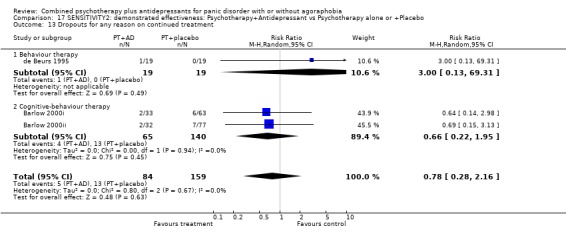
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 17.14.
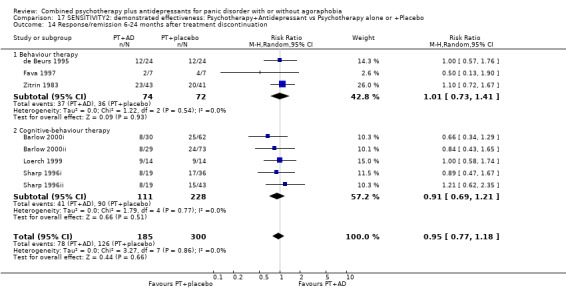
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 17.15.
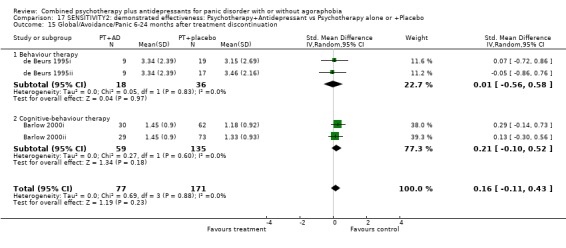
Comparison 17 SENSITIVITY2: demonstrated effectiveness: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 18.
SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 8 | 501 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [1.03, 1.85] |
| 1.1 Behaviour therapy | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 4.62 [0.63, 34.05] |
| 1.2 Cognitive‐behaviour therapy | 5 | 336 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.05, 2.02] |
| 1.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.61, 2.20] |
| 2 Remission at 2‐4 months | 5 | 392 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.82, 1.67] |
| 2.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Cognitive‐behaviour therapy | 3 | 252 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.92, 2.14] |
| 2.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.28, 2.61] |
| 3 Global severity at 2‐4 months | 3 | 246 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.61, ‐0.10] |
| 3.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Cognitive‐behaviour therapy | 2 | 206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.57, ‐0.02] |
| 3.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.33, ‐0.05] |
| 4 Frequency of panic attacks at 2‐4 months | 5 | 237 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.84, 0.28] |
| 4.1 Behaviour therapy | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.14 [‐1.01, 0.74] |
| 4.2 Cognitive‐behaviour therapy | 3 | 125 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.46 [‐1.42, 0.50] |
| 4.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.53, 0.59] |
| 5 Phobic avoidance at 2‐4 months | 5 | 233 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.74, 0.44] |
| 5.1 Behaviour therapy | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.99 [‐1.93, ‐0.05] |
| 5.2 Cognitive‐behaviour therapy | 3 | 121 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.03 [‐0.93, 0.87] |
| 5.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐1.15, 1.13] |
| 6 General anxiety at 2‐4 months | 5 | 266 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.10, 0.12] |
| 6.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Cognitive‐behaviour therapy | 4 | 174 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐1.20, 0.18] |
| 6.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐2.12, 1.22] |
| 7 Depression at 2‐4 months | 5 | 163 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.61 [‐0.93, ‐0.29] |
| 7.1 Behaviour therapy | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.99, 0.76] |
| 7.2 Cognitive‐behaviour therapy | 3 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.10, ‐0.20] |
| 7.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.44, ‐0.14] |
| 8 Social functioning at 2‐4 months | 3 | 128 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.12, ‐0.20] |
| 8.1 Behavour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.39, 0.12] |
| 8.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.46, ‐0.16] |
| 9 Dropouts for any reason within 2‐4 months | 7 | 401 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.58, 1.11] |
| 9.1 Behaviour therapy | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.28, 6.91] |
| 9.2 Cognitive‐behaviour therapy | 5 | 336 | Risk Ratio (M‐H, Random, 95% CI) | 0.77 [0.55, 1.08] |
| 9.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 10 Dropouts due to side effects within 2‐4 months | 5 | 327 | Risk Ratio (M‐H, Random, 95% CI) | 0.99 [0.44, 2.24] |
| 10.1 Behaviour therapy | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 1.38 [0.28, 6.91] |
| 10.2 Cognitive‐behaviour therapy | 3 | 262 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.25, 2.68] |
| 10.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 11 Response/remission on continued treatment | 4 | 286 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [0.59, 2.67] |
| 11.1 Behaviour therapy | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 3.23 [0.83, 12.61] |
| 11.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.07, 2.16] |
| 11.3 Psychdynamic psychotherapy and others | 2 | 113 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.44, 1.02] |
| 12 Global/Avoidance/Panic on continued treatment | 4 | 258 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐1.04, 0.15] |
| 12.1 Behaviour therapy | 1 | 20 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐2.20, ‐0.26] |
| 12.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.74, ‐0.09] |
| 12.3 Psychodynamic psychotherapy and others | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.45, 1.04] |
| 13 Dropouts for any reason on continued treatment | 3 | 208 | Risk Ratio (M‐H, Random, 95% CI) | 0.71 [0.27, 1.90] |
| 13.1 Behaviour therapy | 1 | 20 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.07, 13.87] |
| 13.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.22, 2.39] |
| 13.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.05, 5.08] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 4 | 280 | Risk Ratio (M‐H, Random, 95% CI) | 1.68 [1.19, 2.38] |
| 16.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Cognitive‐behaviour therapy | 3 | 240 | Risk Ratio (M‐H, Random, 95% CI) | 1.46 [1.00, 2.11] |
| 16.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.2 [1.45, 7.05] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.78, 0.63] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 1 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.34, 0.34] |
| 17.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐1.91, ‐0.55] |
Analysis 18.1.
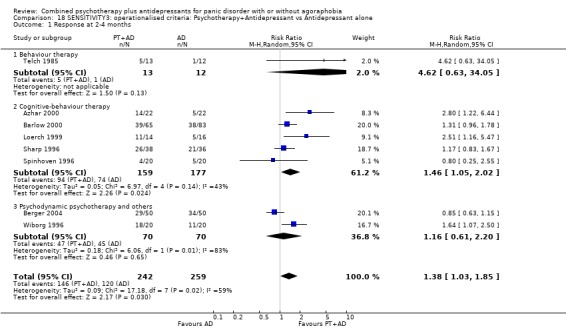
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 18.2.
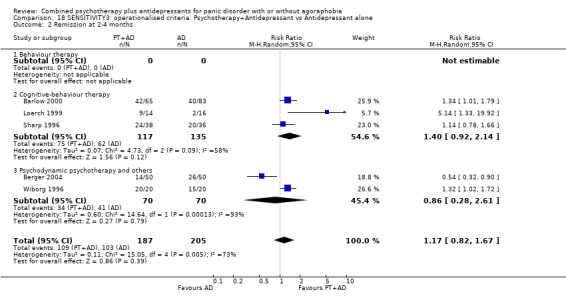
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 18.3.
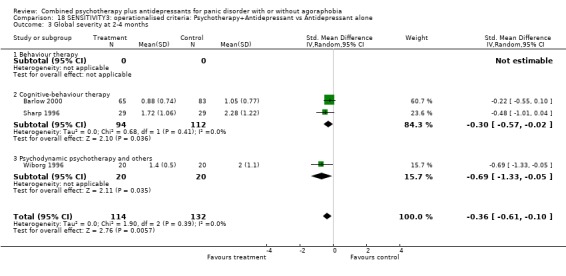
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 18.4.
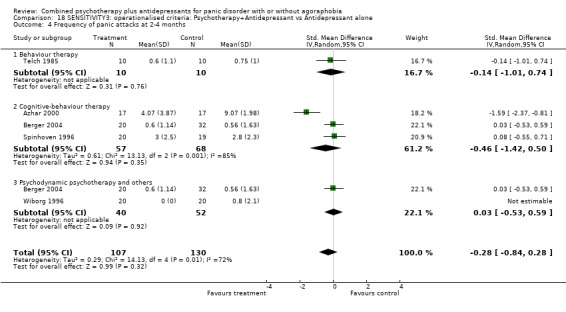
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 18.5.
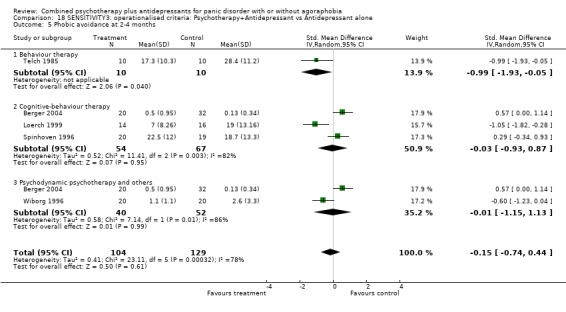
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 18.6.
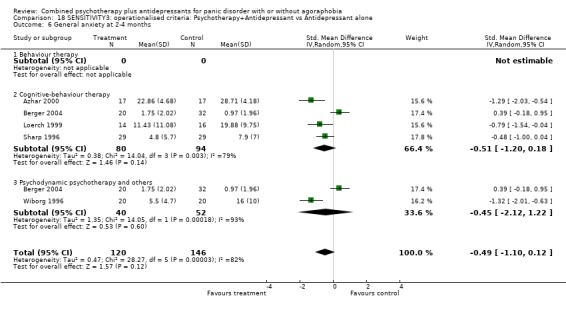
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 18.7.
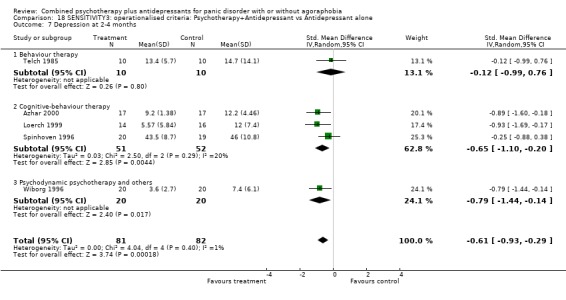
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 18.8.
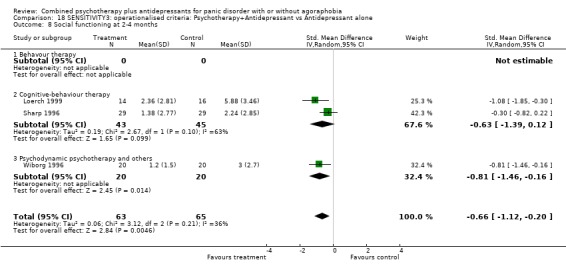
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 18.9.
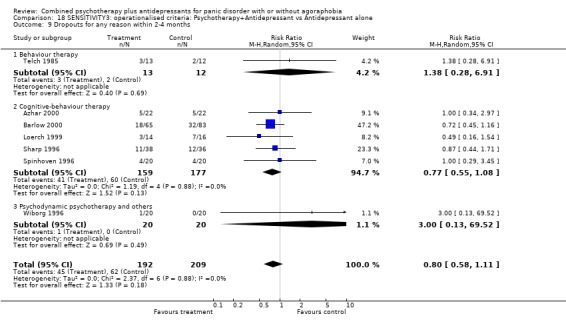
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 18.10.
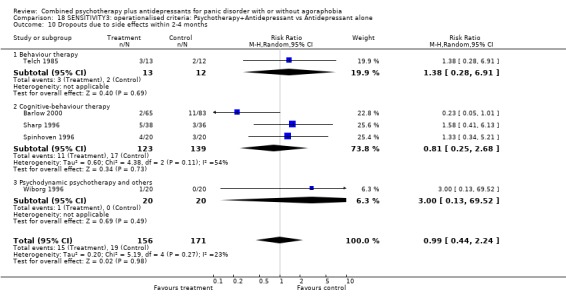
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 18.11.
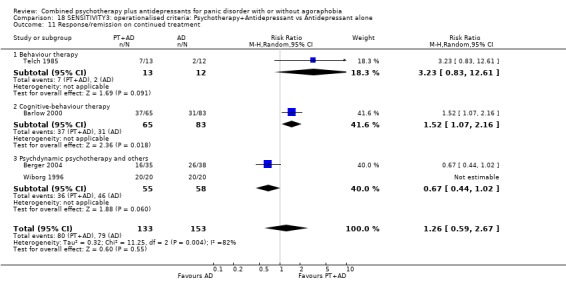
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 18.12.
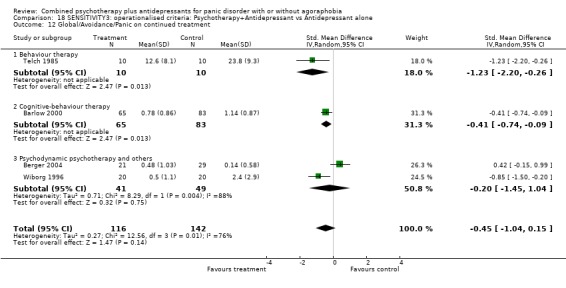
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 18.13.
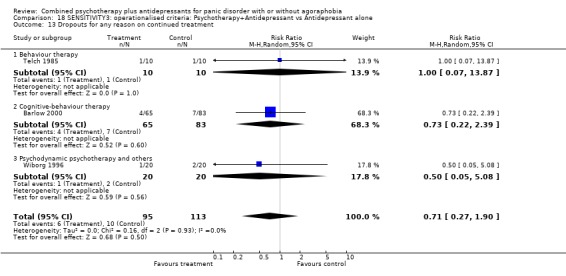
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 18.16.
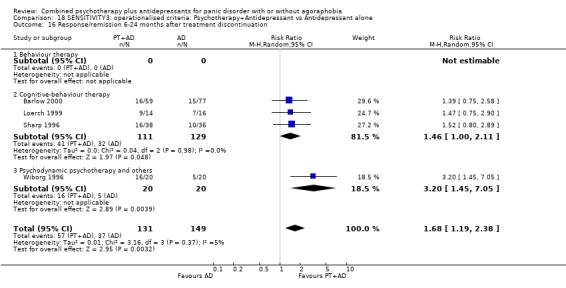
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Analysis 18.17.
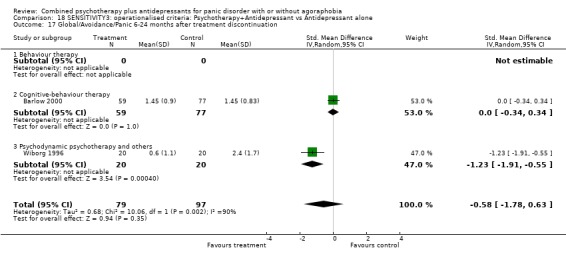
Comparison 18 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 19.
SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 16 | 883 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [1.01, 1.35] |
| 1.1 Behaviour therapy | 5 | 174 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [0.97, 1.86] |
| 1.2 Cognitive‐behaviour therapy | 11 | 709 | Risk Ratio (M‐H, Random, 95% CI) | 1.13 [0.96, 1.33] |
| 1.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 14 | 788 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [1.05, 1.42] |
| 2.1 Behaviour therapy | 5 | 163 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.88, 1.68] |
| 2.2 Cognitive‐behaviour therapy | 9 | 625 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [1.02, 1.47] |
| 2.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 9 | 481 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.56, ‐0.18] |
| 3.1 Behaviour therapy | 4 | 118 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.54 [‐0.92, ‐0.16] |
| 3.2 Cognitive‐behaviour therapy | 5 | 363 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.54, ‐0.08] |
| 3.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 10 | 367 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.33, 0.08] |
| 4.1 Behaviour therapy | 6 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.09 [‐0.42, 0.24] |
| 4.2 Cognitive‐behaviour therapy | 4 | 219 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.41, 0.12] |
| 5 Phobic avoidance at 2‐4 months | 13 | 439 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.47, ‐0.08] |
| 5.1 Behaviour therapy | 6 | 151 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.85, ‐0.00] |
| 5.2 Cognitive‐behaviour therapy | 7 | 288 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.44, 0.04] |
| 5.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 13 | 521 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.47, ‐0.12] |
| 6.1 Behaviour therapy | 5 | 132 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐0.87, ‐0.11] |
| 6.2 Cognitive‐behaviour therapy | 8 | 389 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.23 [‐0.44, ‐0.03] |
| 6.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 11 | 343 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.58, ‐0.12] |
| 7.1 Behaviour therapy | 6 | 151 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.77, 0.05] |
| 7.2 Cognitive‐behaviour therapy | 5 | 192 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.34 [‐0.64, ‐0.05] |
| 7.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 6 | 206 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.45, 0.12] |
| 8.1 Behaviour therapy | 2 | 62 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.94, 0.07] |
| 8.2 Cognitive‐behaviour therapy | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.39, 0.30] |
| 9 Dropouts for any reason within 2‐4 months | 14 | 773 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.84, 1.56] |
| 9.1 Behaviour therapy | 4 | 108 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.48, 2.45] |
| 9.2 Cognitive‐behaviour therapy | 10 | 665 | Risk Ratio (M‐H, Random, 95% CI) | 1.16 [0.83, 1.62] |
| 9.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 11 | 698 | Risk Ratio (M‐H, Random, 95% CI) | 4.65 [2.09, 10.32] |
| 10.1 Behaviour therapy | 3 | 94 | Risk Ratio (M‐H, Random, 95% CI) | 3.82 [0.83, 17.66] |
| 10.2 Cognitive‐behaviour therapy | 8 | 604 | Risk Ratio (M‐H, Random, 95% CI) | 5.00 [1.96, 12.72] |
| 11 Response/remission on continued treatment | 3 | 230 | Risk Ratio (M‐H, Random, 95% CI) | 1.29 [0.95, 1.76] |
| 11.1 Behaviour therapy | 1 | 25 | Risk Ratio (M‐H, Random, 95% CI) | 3.23 [0.83, 12.61] |
| 11.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 12 Global/Avoidance/Panic on continued treatment | 3 | 224 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.56 [‐0.99, ‐0.13] |
| 12.1 Behaviour therapy | 1 | 19 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.47 [‐2.51, ‐0.43] |
| 12.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 13 Dropouts for any reason on continued treatment | 4 | 262 | Risk Ratio (M‐H, Random, 95% CI) | 0.88 [0.33, 2.32] |
| 13.1 Behaviour therapy | 2 | 57 | Risk Ratio (M‐H, Random, 95% CI) | 2.86 [0.32, 25.80] |
| 13.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 10 | 502 | Risk Ratio (M‐H, Random, 95% CI) | 0.93 [0.74, 1.17] |
| 14.1 Behaviour therapy | 5 | 163 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.67, 1.45] |
| 14.2 Cognitive‐behaviour therapy | 5 | 339 | Risk Ratio (M‐H, Random, 95% CI) | 0.91 [0.69, 1.21] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 6 | 295 | Std. Mean Difference (IV, Random, 95% CI) | 0.13 [‐0.13, 0.40] |
| 15.1 Behaviour therapy | 4 | 101 | Std. Mean Difference (IV, Random, 95% CI) | 0.02 [‐0.49, 0.53] |
| 15.2 Cognitive‐behaviour therapy | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
Analysis 19.1.
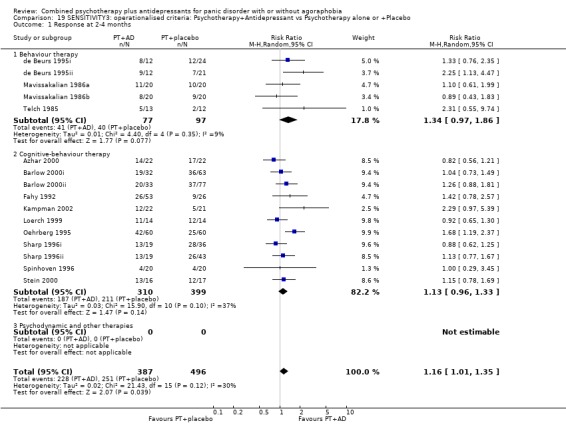
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 19.2.
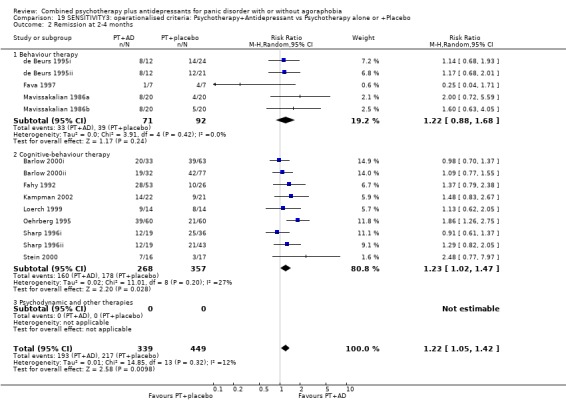
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 19.3.
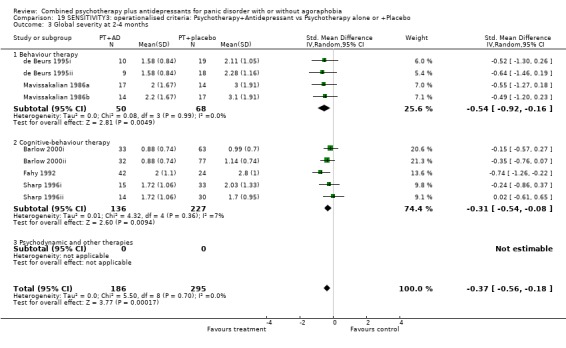
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 19.4.
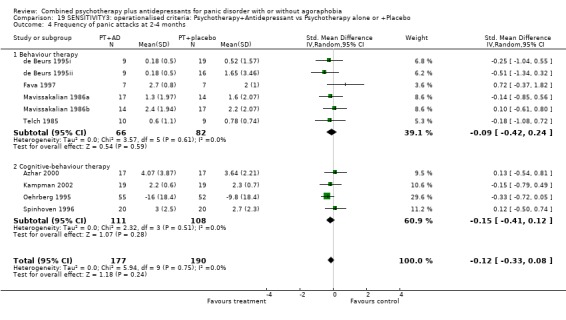
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 19.5.
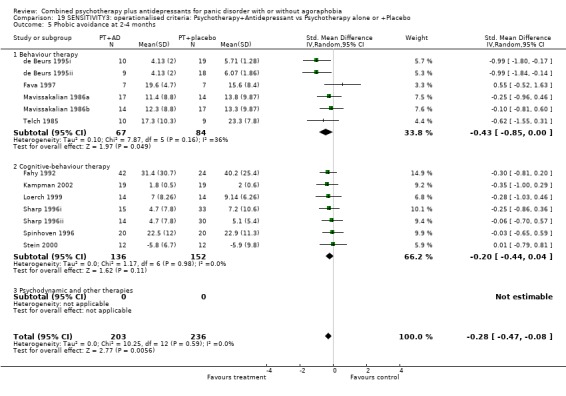
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 19.6.
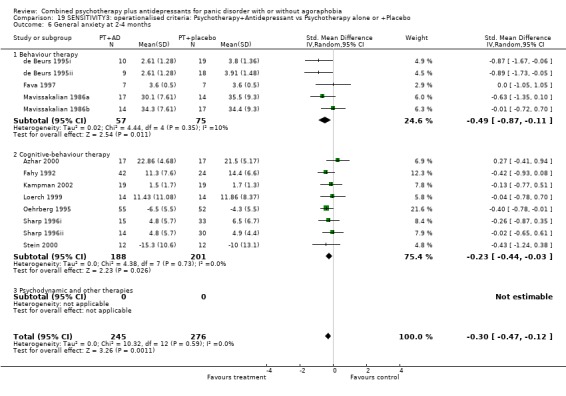
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 19.7.
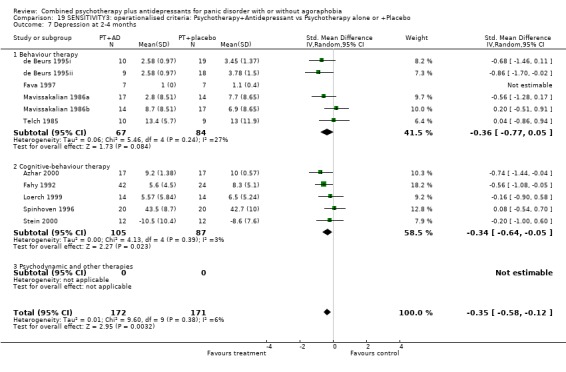
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 19.8.
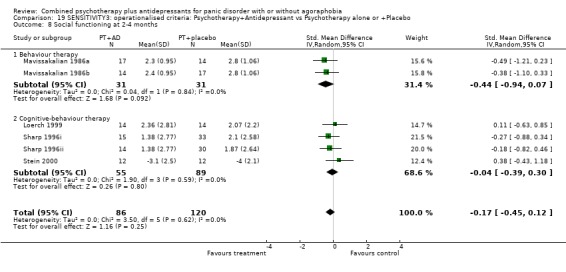
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social functioning at 2‐4 months.
Analysis 19.9.
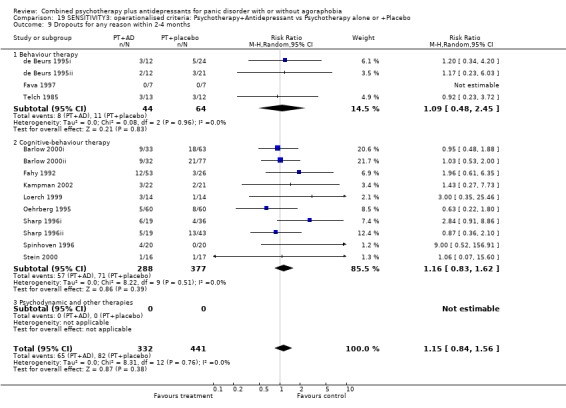
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 19.10.
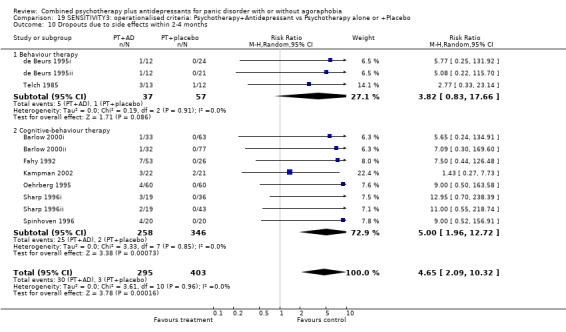
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 19.11.
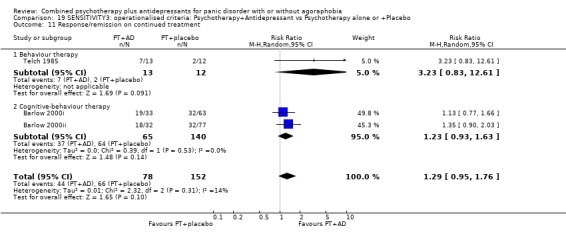
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 19.12.
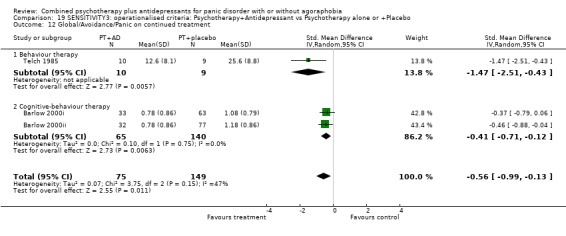
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 19.13.
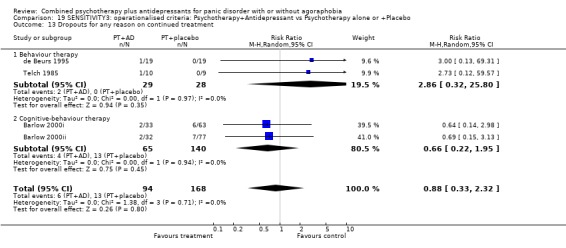
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 19.14.
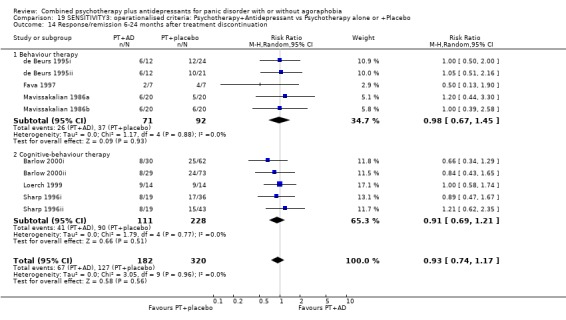
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 19.15.
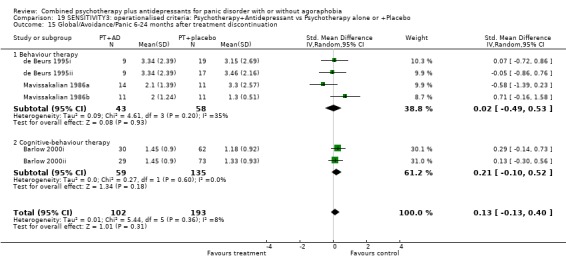
Comparison 19 SENSITIVITY3: operationalised criteria: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 20.
SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 3 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 1.37 [0.91, 2.05] |
| 1.1 Behaviour therapy | 1 | 18 | Risk Ratio (M‐H, Random, 95% CI) | 1.17 [0.65, 2.08] |
| 1.2 Cognitive‐behaviour therapy | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 1.59 [0.75, 3.34] |
| 1.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 3 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 1.40 [0.72, 2.73] |
| 2.1 Behaviour therapy | 1 | 18 | Risk Ratio (M‐H, Random, 95% CI) | 1.0 [0.52, 1.92] |
| 2.2 Cognitive‐behaviour therapy | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 2.13 [0.45, 10.10] |
| 2.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 2 | 73 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.62 [‐1.14, ‐0.10] |
| 3.1 Behaviour therapy | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.14 [‐2.26, ‐0.02] |
| 3.2 Cognitive‐behaviour therapy | 1 | 58 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.48 [‐1.01, 0.04] |
| 3.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐1.24, 0.80] |
| 4.1 Behaviour therapy | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐1.24, 0.80] |
| 4.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5 Phobic avoidance at 2‐4 months | 3 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.37, 0.07] |
| 5.1 Behaviour therapy | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.07 [‐2.18, 0.04] |
| 5.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.53 [‐1.45, 0.39] |
| 5.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 3 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐0.96, ‐0.17] |
| 6.1 Behaviour therapy | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.49 [‐1.53, 0.54] |
| 6.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.01, ‐0.15] |
| 6.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 2 | 45 | Std. Mean Difference (IV, Random, 95% CI) | 1.00 [‐1.63, ‐0.37] |
| 7.1 Behaviour therapy | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.14 [‐2.26, ‐0.02] |
| 7.2 Cognitive‐behaviour therapy | 1 | 30 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.93 [‐1.69, ‐0.17] |
| 7.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 3 | 103 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.70 [‐1.26, ‐0.13] |
| 8.1 Behavour therapy | 1 | 15 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.05 [‐2.15, 0.06] |
| 8.2 Cognitive‐behaviour therapy | 2 | 88 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.63 [‐1.39, 0.12] |
| 8.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 3 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.41, 1.28] |
| 9.1 Behaviour therapy | 1 | 18 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.05, 4.58] |
| 9.2 Cognitive‐behaviour therapy | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.42, 1.34] |
| 9.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 2 | 92 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.36, 3.67] |
| 10.1 Behaviour therapy | 1 | 18 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.05, 4.58] |
| 10.2 Cognitive‐behaviour therapy | 1 | 74 | Risk Ratio (M‐H, Random, 95% CI) | 1.58 [0.41, 6.13] |
| 10.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11 Response/remission on continued treatment | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.3 Psychdynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.94, 2.38] |
| 16.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Cognitive‐behaviour therapy | 2 | 104 | Risk Ratio (M‐H, Random, 95% CI) | 1.49 [0.94, 2.38] |
| 16.3 Psychodynamic psychotherapy and others | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.3 Psychodynamic psychotherapy and others | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 20.1.
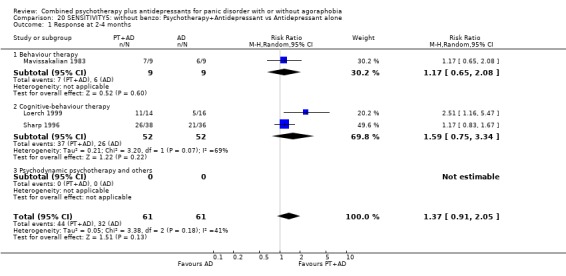
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 20.2.
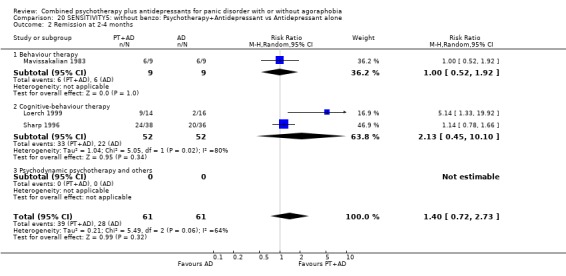
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 20.3.
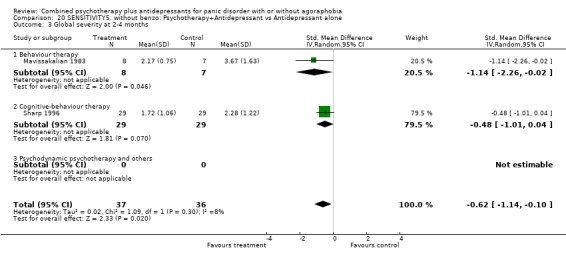
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 20.4.
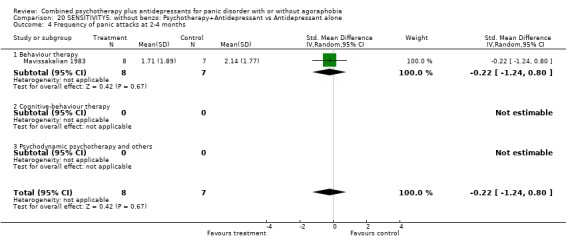
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 20.5.
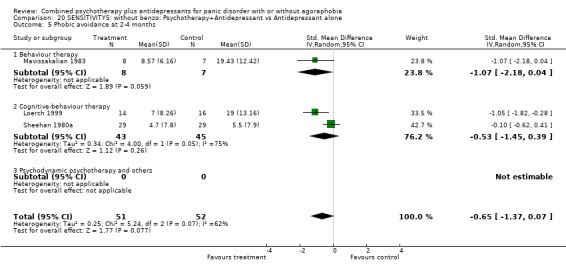
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 20.6.
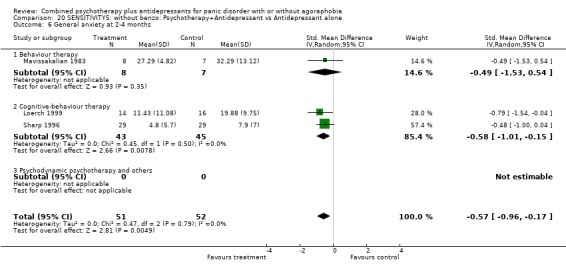
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 20.7.
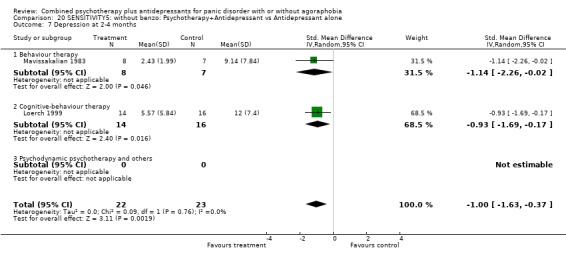
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 20.8.
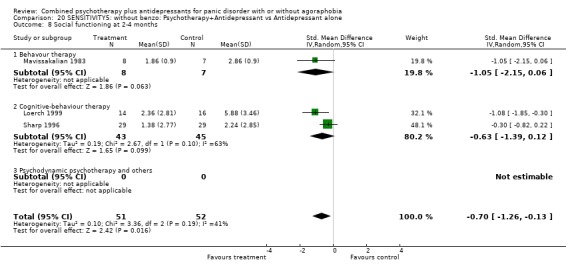
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 20.9.
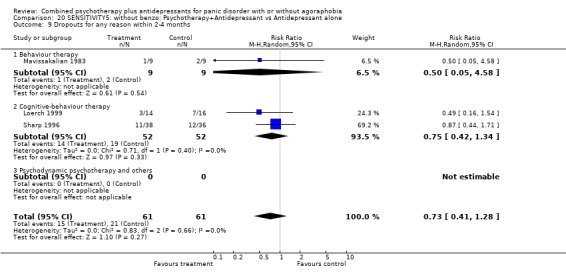
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 20.10.
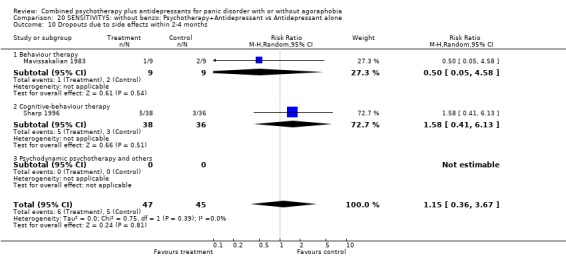
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 20.16.
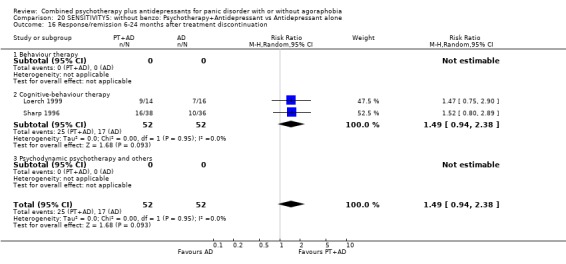
Comparison 20 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Comparison 21.
SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 8 | 481 | Risk Ratio (M‐H, Random, 95% CI) | 1.26 [1.06, 1.51] |
| 1.1 Behaviour therapy | 3 | 159 | Risk Ratio (M‐H, Random, 95% CI) | 1.48 [1.00, 2.18] |
| 1.2 Cognitive‐behaviour therapy | 5 | 322 | Risk Ratio (M‐H, Random, 95% CI) | 1.22 [0.96, 1.55] |
| 1.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2 Remission at 2‐4 months | 9 | 536 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.08, 1.61] |
| 2.1 Behaviour therapy | 3 | 159 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.84, 1.93] |
| 2.2 Cognitive‐behaviour therapy | 6 | 377 | Risk Ratio (M‐H, Random, 95% CI) | 1.33 [1.02, 1.73] |
| 2.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3 Global severity at 2‐4 months | 3 | 158 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.81, 0.10] |
| 3.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Cognitive‐behaviour therapy | 3 | 158 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.35 [‐0.81, 0.10] |
| 3.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4 Frequency of panic attacks at 2‐4 months | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.72, 0.05] |
| 4.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Cognitive‐behaviour therapy | 1 | 107 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.33 [‐0.72, 0.05] |
| 5 Phobic avoidance at 2‐4 months | 8 | 312 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.56, ‐0.08] |
| 5.1 Behaviour therapy | 3 | 102 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.65 [‐1.29, ‐0.01] |
| 5.2 Cognitive‐behaviour therapy | 5 | 210 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.48, 0.08] |
| 5.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6 General anxiety at 2‐4 months | 9 | 419 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐0.67, ‐0.20] |
| 6.1 Behaviour therapy | 3 | 102 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.89 [‐1.49, ‐0.29] |
| 6.2 Cognitive‐behaviour therapy | 6 | 317 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.30 [‐0.53, ‐0.08] |
| 6.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7 Depression at 2‐4 months | 6 | 220 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.44 [‐0.78, ‐0.10] |
| 7.1 Behaviour therapy | 3 | 102 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.59 [‐1.33, 0.14] |
| 7.2 Cognitive‐behaviour therapy | 3 | 118 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.38 [‐0.76, ‐0.01] |
| 7.3 Psychodynamic and other therapies | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8 Social functioning at 2‐4 months | 6 | 201 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.31 [‐0.74, 0.11] |
| 8.1 Behaviour therapy | 2 | 57 | Std. Mean Difference (IV, Random, 95% CI) | 1.00 [‐1.57, ‐0.43] |
| 8.2 Cognitive‐behaviour therapy | 4 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.04 [‐0.39, 0.30] |
| 9 Dropouts for any reason within 2‐4 months | 9 | 536 | Risk Ratio (M‐H, Random, 95% CI) | 1.18 [0.83, 1.68] |
| 9.1 Behaviour therapy | 3 | 159 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.67, 1.82] |
| 9.2 Cognitive‐behaviour therapy | 6 | 377 | Risk Ratio (M‐H, Random, 95% CI) | 1.28 [0.75, 2.19] |
| 9.3 Psychodynamic and other therapies | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10 Dropouts due to side effects within 2‐4 months | 5 | 388 | Risk Ratio (M‐H, Random, 95% CI) | 4.09 [1.03, 16.22] |
| 10.1 Behaviour therapy | 1 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.12, 3.75] |
| 10.2 Cognitive‐behaviour therapy | 4 | 316 | Risk Ratio (M‐H, Random, 95% CI) | 9.84 [2.30, 42.08] |
| 11 Response/remission on continued treatment | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12 Global/Avoidance/Panic on continued treatment | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13 Dropouts for any reason on continued treatment | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 4 | 217 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.71, 1.35] |
| 14.1 Behaviour therapy | 1 | 72 | Risk Ratio (M‐H, Random, 95% CI) | 0.82 [0.39, 1.73] |
| 14.2 Cognitive‐behaviour therapy | 3 | 145 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.71, 1.45] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.48, 0.77] |
| 15.1 Behaviour therapy | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.48, 0.77] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
Analysis 21.1.
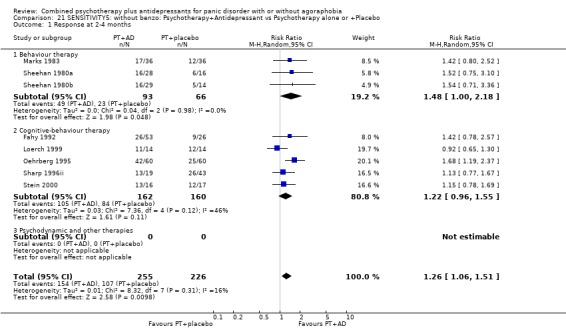
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 21.2.
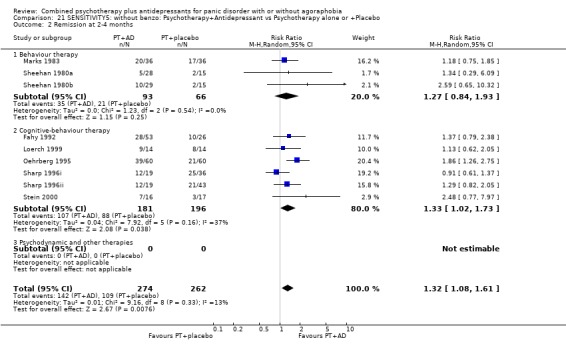
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 21.3.
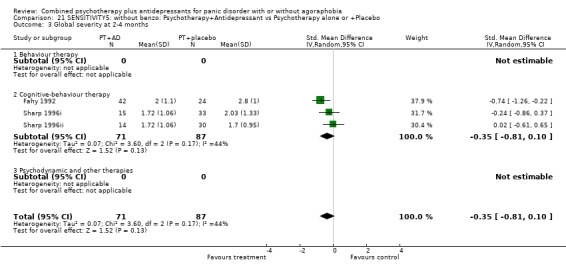
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 21.4.
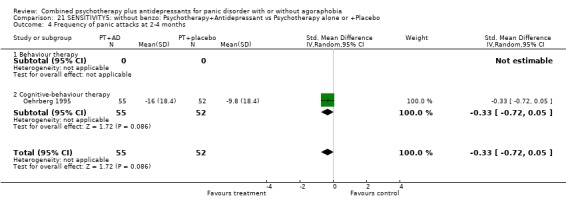
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 21.5.
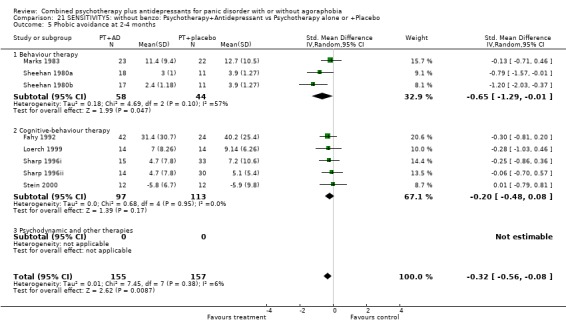
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 21.6.
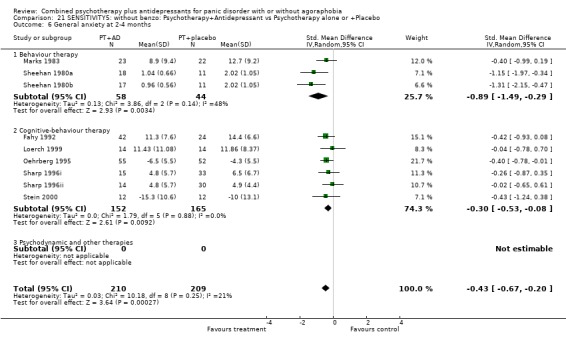
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 21.7.
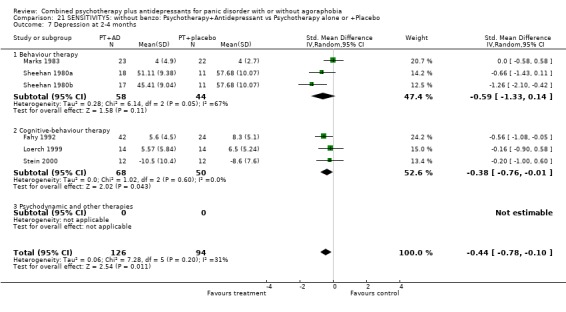
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 21.8.
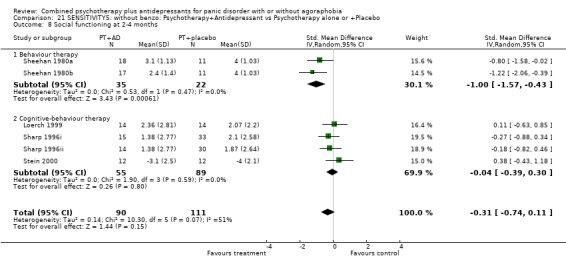
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 8 Social functioning at 2‐4 months.
Analysis 21.9.
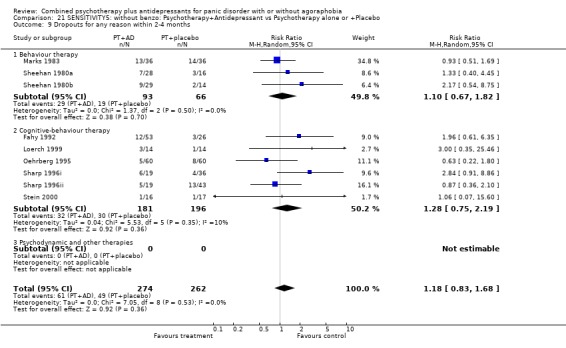
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 21.10.
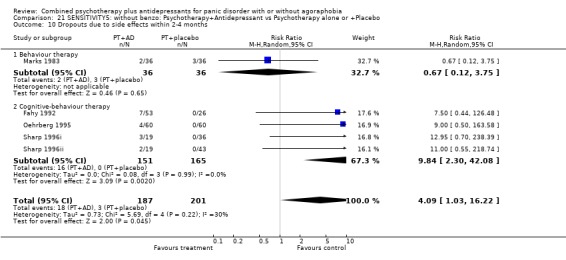
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 21.14.
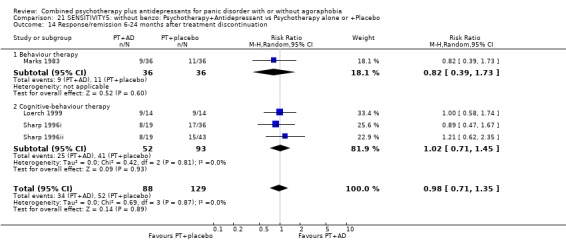
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 21.15.
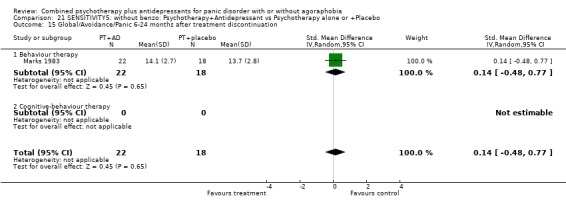
Comparison 21 SENSITIVITY5: without benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 22.
SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 4 | 328 | Risk Ratio (M‐H, Random, 95% CI) | 1.14 [0.86, 1.52] |
| 1.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 1.2 Cognitive‐behaviour therapy | 2 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [0.94, 1.71] |
| 1.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.65, 1.85] |
| 2 Remission at 2‐4 months | 3 | 288 | Risk Ratio (M‐H, Random, 95% CI) | 1.04 [0.65, 1.66] |
| 2.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 2.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.34 [1.01, 1.79] |
| 2.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.86 [0.28, 2.61] |
| 3 Global severity at 2‐4 months | 2 | 188 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.80, 0.05] |
| 3.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 3.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.55, 0.10] |
| 3.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.69 [‐1.33, ‐0.05] |
| 4 Frequency of panic attacks at 2‐4 months | 3 | 183 | Std. Mean Difference (IV, Random, 95% CI) | 0.04 [‐0.29, 0.38] |
| 4.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 4.2 Cognitive‐behaviour therapy | 2 | 91 | Std. Mean Difference (IV, Random, 95% CI) | 0.05 [‐0.37, 0.47] |
| 4.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | 0.03 [‐0.53, 0.59] |
| 5 Phobic avoidance at 2‐4 months | 3 | 183 | Std. Mean Difference (IV, Random, 95% CI) | 0.22 [‐0.31, 0.75] |
| 5.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 5.2 Cognitive‐behaviour therapy | 2 | 91 | Std. Mean Difference (IV, Random, 95% CI) | 0.44 [0.02, 0.87] |
| 5.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐1.15, 1.13] |
| 6 General anxiety at 2‐4 months | 2 | 144 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.16 [‐1.19, 0.87] |
| 6.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 6.2 Cognitive‐behaviour therapy | 1 | 52 | Std. Mean Difference (IV, Random, 95% CI) | 0.39 [‐0.18, 0.95] |
| 6.3 Psychodynamic psychotherapy and others | 2 | 92 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐2.12, 1.22] |
| 7 Depression at 2‐4 months | 2 | 79 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐1.04, 0.01] |
| 7.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 7.2 Cognitive‐behaviour therapy | 1 | 39 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.88, 0.38] |
| 7.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.79 [‐1.44, ‐0.14] |
| 8 Social functioning at 2‐4 months | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.46, ‐0.16] |
| 8.1 Behavour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.81 [‐1.46, ‐0.16] |
| 9 Dropouts for any reason within 2‐4 months | 4 | 328 | Risk Ratio (M‐H, Random, 95% CI) | 0.90 [0.62, 1.29] |
| 9.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9.2 Cognitive‐behaviour therapy | 2 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.48, 1.17] |
| 9.3 Psychodynamic psychotherapy and others | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 1.30 [0.69, 2.45] |
| 10 Dropouts due to side effects within 2‐4 months | 3 | 228 | Risk Ratio (M‐H, Random, 95% CI) | 0.75 [0.17, 3.22] |
| 10.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 10.2 Cognitive‐behaviour therapy | 2 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.57 [0.10, 3.28] |
| 10.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.52] |
| 11 Response/remission on continued treatment | 3 | 261 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.45, 2.29] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 1.52 [1.07, 2.16] |
| 11.3 Psychdynamic psychotherapy and others | 2 | 113 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.44, 1.02] |
| 12 Global/Avoidance/Panic on continued treatment | 3 | 238 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.91, 0.36] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 1 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.74, ‐0.09] |
| 12.3 Psychodynamic psychotherapy and others | 2 | 90 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐1.45, 1.04] |
| 13 Dropouts for any reason on continued treatment | 2 | 188 | Risk Ratio (M‐H, Random, 95% CI) | 0.67 [0.23, 1.94] |
| 13.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 13.2 Cognitive‐behaviour therapy | 1 | 148 | Risk Ratio (M‐H, Random, 95% CI) | 0.73 [0.22, 2.39] |
| 13.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 0.5 [0.05, 5.08] |
| 14 Response/remission immediately after treatment discontinuation | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 14.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.2 Cognitive‐behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 14.3 Psychodynamic psychotherapy and others | 1 | 50 | Risk Ratio (M‐H, Random, 95% CI) | 0.85 [0.65, 1.11] |
| 15 Global/Avoidance/Panic immediately after treatment discontinuation | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 15.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 15.3 Psychodynamic psychotherapy and others | 1 | 50 | Std. Mean Difference (IV, Random, 95% CI) | 0.42 [‐0.15, 0.99] |
| 16 Response/remission 6‐24 months after treatment discontinuation | 2 | 176 | Risk Ratio (M‐H, Random, 95% CI) | 2.03 [0.90, 4.58] |
| 16.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 16.2 Cognitive‐behaviour therapy | 1 | 136 | Risk Ratio (M‐H, Random, 95% CI) | 1.39 [0.75, 2.58] |
| 16.3 Psychodynamic psychotherapy and others | 1 | 40 | Risk Ratio (M‐H, Random, 95% CI) | 3.2 [1.45, 7.05] |
| 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 2 | 176 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.78, 0.63] |
| 17.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 17.2 Cognitive‐behaviour therapy | 1 | 136 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [‐0.34, 0.34] |
| 17.3 Psychodynamic psychotherapy and others | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | ‐1.23 [‐1.91, ‐0.55] |
Analysis 22.1.
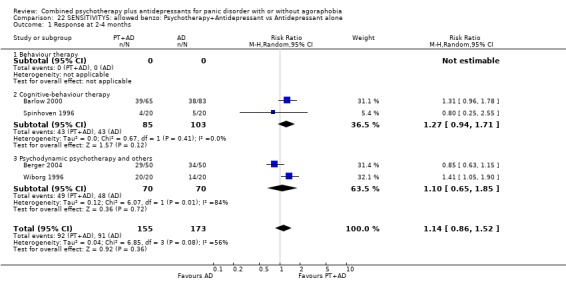
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 1 Response at 2‐4 months.
Analysis 22.2.
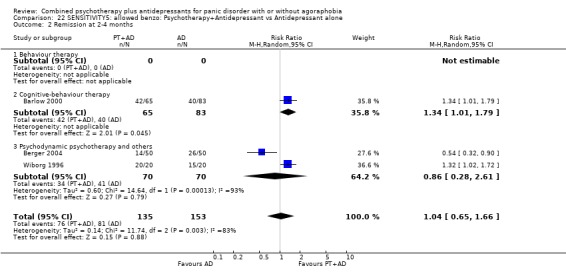
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 2 Remission at 2‐4 months.
Analysis 22.3.
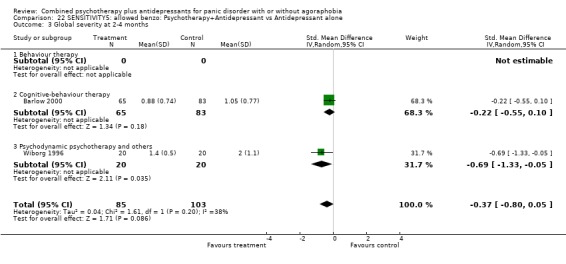
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 3 Global severity at 2‐4 months.
Analysis 22.4.
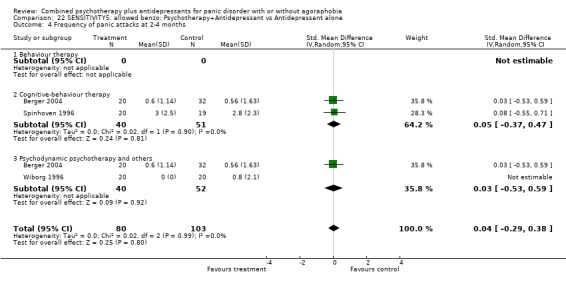
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 22.5.
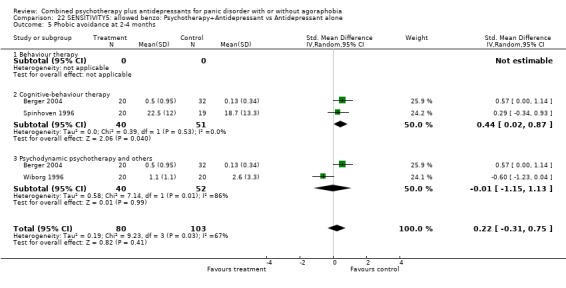
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 22.6.
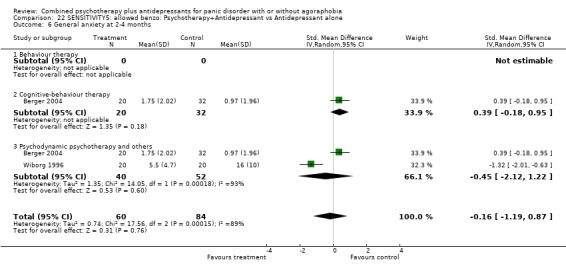
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 6 General anxiety at 2‐4 months.
Analysis 22.7.
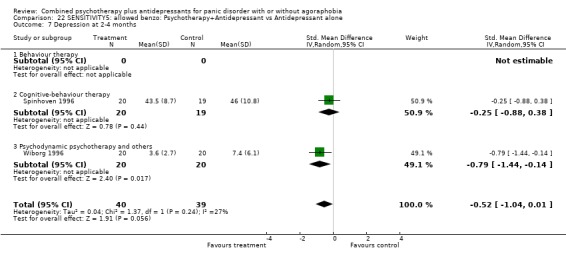
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 7 Depression at 2‐4 months.
Analysis 22.8.
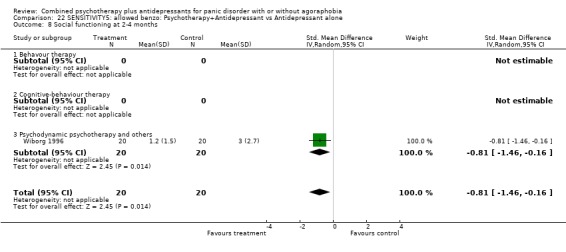
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 8 Social functioning at 2‐4 months.
Analysis 22.9.
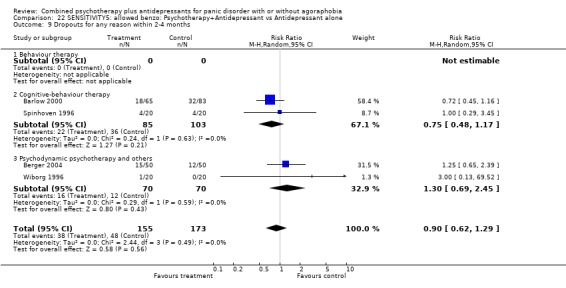
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 22.10.
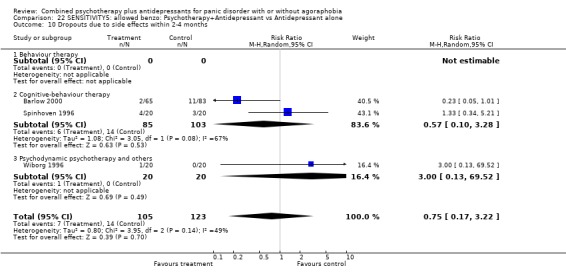
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 22.11.
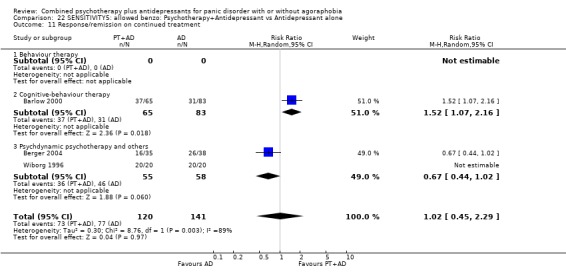
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 11 Response/remission on continued treatment.
Analysis 22.12.
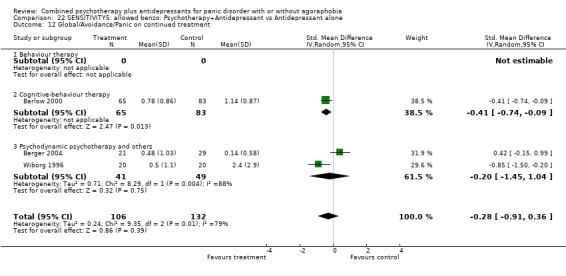
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 22.13.
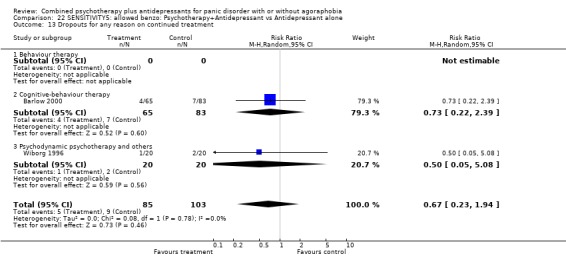
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 22.14.
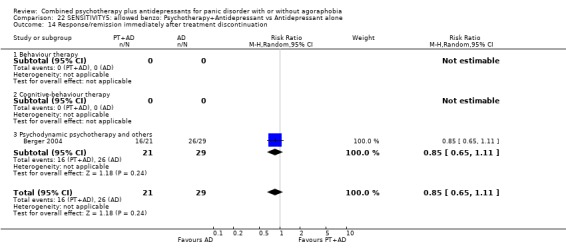
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 14 Response/remission immediately after treatment discontinuation.
Analysis 22.15.
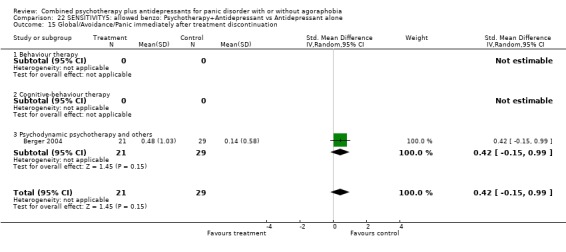
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 15 Global/Avoidance/Panic immediately after treatment discontinuation.
Analysis 22.16.
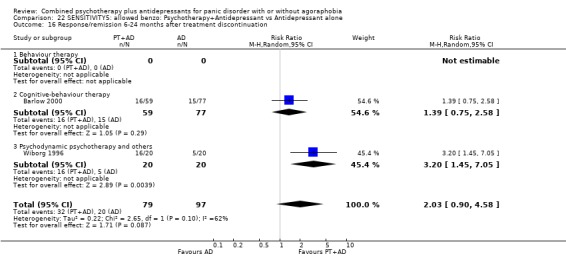
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 16 Response/remission 6‐24 months after treatment discontinuation.
Analysis 22.17.
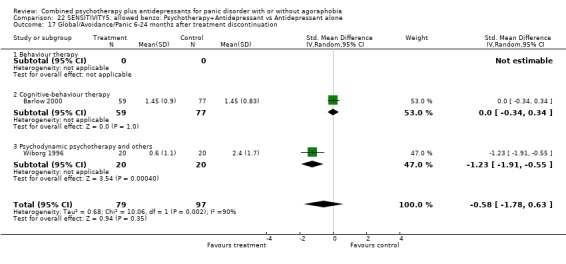
Comparison 22 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Antidepressant alone, Outcome 17 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
Comparison 23.
SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Response at 2‐4 months | 6 | 357 | Risk Ratio (M‐H, Random, 95% CI) | 1.32 [1.04, 1.68] |
| 1.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.67 [1.00, 2.78] |
| 1.2 Cognitive‐behaviour therapy | 4 | 288 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [0.94, 1.53] |
| 2 Remission at 2‐4 months | 5 | 317 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.91, 1.34] |
| 2.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.15 [0.79, 1.68] |
| 2.2 Cognitive‐behaviour therapy | 3 | 248 | Risk Ratio (M‐H, Random, 95% CI) | 1.09 [0.87, 1.36] |
| 3 Global severity at 2‐4 months | 4 | 261 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.32 [‐0.58, ‐0.06] |
| 3.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.58 [‐1.14, ‐0.01] |
| 3.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.25 [‐0.55, 0.04] |
| 4 Frequency of panic attacks at 2‐4 months | 4 | 131 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.15 [‐0.50, 0.21] |
| 4.1 Behaviour therapy | 2 | 53 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.37 [‐0.95, 0.20] |
| 4.2 Cognitive‐behaviour therapy | 2 | 78 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.01 [‐0.45, 0.43] |
| 5 Phobic avoidance at 2‐4 months | 4 | 134 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.52 [‐0.99, ‐0.06] |
| 5.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.99 [‐1.57, ‐0.40] |
| 5.2 Cognitive‐behaviour therapy | 2 | 78 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.19 [‐0.63, 0.26] |
| 6 General anxiety at 2‐4 months | 3 | 94 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.57 [‐1.09, ‐0.05] |
| 6.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.88 [‐1.46, ‐0.30] |
| 6.2 Cognitive‐behaviour therapy | 1 | 38 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.13 [‐0.77, 0.51] |
| 7 Depression at 2‐4 months | 3 | 96 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.43 [‐1.03, 0.17] |
| 7.1 Behaviour therapy | 2 | 56 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.76 [‐1.34, ‐0.19] |
| 7.2 Cognitive‐behaviour therapy | 1 | 40 | Std. Mean Difference (IV, Random, 95% CI) | 0.08 [‐0.54, 0.70] |
| 8 Social functioning at 2‐4 months | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 8.2 Cognitive‐behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 9 Dropouts for any reason within 2‐4 months | 6 | 357 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [0.73, 1.65] |
| 9.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.19 [0.44, 3.22] |
| 9.2 Cognitive‐behaviour therapy | 4 | 288 | Risk Ratio (M‐H, Random, 95% CI) | 1.08 [0.69, 1.69] |
| 10 Dropouts due to side effects within 2‐4 months | 6 | 357 | Risk Ratio (M‐H, Random, 95% CI) | 3.53 [1.21, 10.27] |
| 10.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 5.41 [0.59, 49.42] |
| 10.2 Cognitive‐behaviour therapy | 4 | 288 | Risk Ratio (M‐H, Random, 95% CI) | 3.10 [0.92, 10.50] |
| 11 Response/remission on continued treatment | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 11.1 Behaviour therapy | 0 | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 11.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 1.23 [0.93, 1.63] |
| 12 Global/Avoidance/Panic on continued treatment | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 12.1 Behaviour therapy | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
| 12.2 Cognitive‐behaviour therapy | 2 | 205 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.41 [‐0.71, ‐0.12] |
| 13 Dropouts for any reason on continued treatment | 3 | 243 | Risk Ratio (M‐H, Random, 95% CI) | 0.78 [0.28, 2.16] |
| 13.1 Behaviour therapy | 1 | 38 | Risk Ratio (M‐H, Random, 95% CI) | 3.00 [0.13, 69.31] |
| 13.2 Cognitive‐behaviour therapy | 2 | 205 | Risk Ratio (M‐H, Random, 95% CI) | 0.66 [0.22, 1.95] |
| 14 Response/remission 6‐24 months after treatment discontinuation | 4 | 263 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.61, 1.22] |
| 14.1 Behaviour therapy | 2 | 69 | Risk Ratio (M‐H, Random, 95% CI) | 1.02 [0.62, 1.69] |
| 14.2 Cognitive‐behaviour therapy | 2 | 194 | Risk Ratio (M‐H, Random, 95% CI) | 0.74 [0.46, 1.19] |
| 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation | 4 | 248 | Std. Mean Difference (IV, Random, 95% CI) | 0.16 [‐0.11, 0.43] |
| 15.1 Behaviour therapy | 2 | 54 | Std. Mean Difference (IV, Random, 95% CI) | 0.01 [‐0.56, 0.58] |
| 15.2 Cognitive‐behaviour therapy | 2 | 194 | Std. Mean Difference (IV, Random, 95% CI) | 0.21 [‐0.10, 0.52] |
Analysis 23.1.
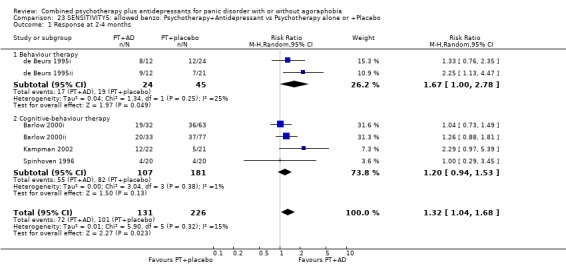
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 1 Response at 2‐4 months.
Analysis 23.2.
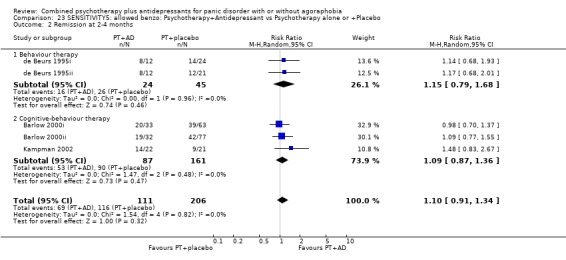
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 2 Remission at 2‐4 months.
Analysis 23.3.
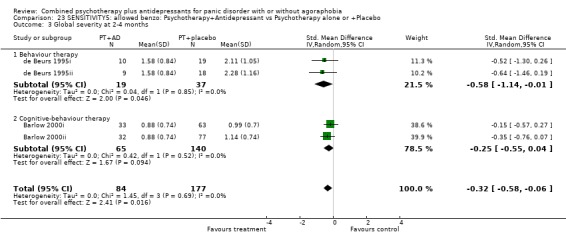
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 3 Global severity at 2‐4 months.
Analysis 23.4.
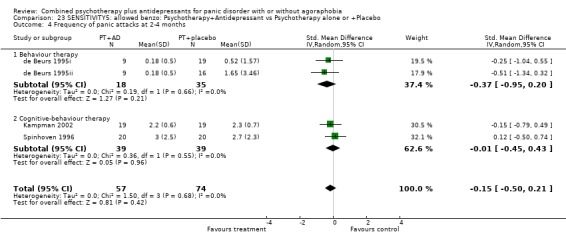
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 4 Frequency of panic attacks at 2‐4 months.
Analysis 23.5.
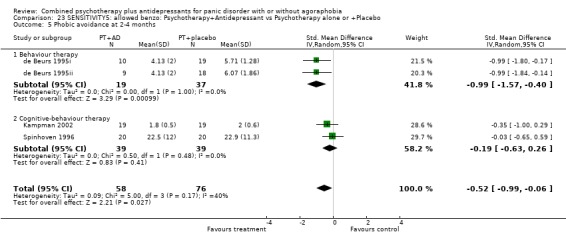
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 5 Phobic avoidance at 2‐4 months.
Analysis 23.6.
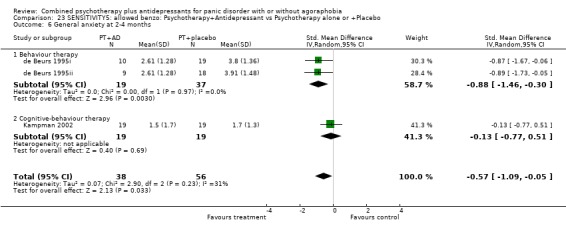
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 6 General anxiety at 2‐4 months.
Analysis 23.7.
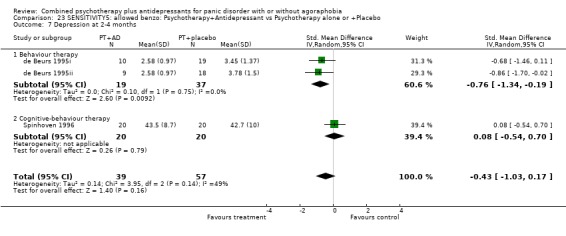
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 7 Depression at 2‐4 months.
Analysis 23.9.
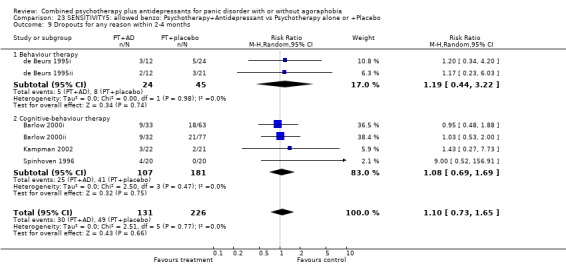
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 9 Dropouts for any reason within 2‐4 months.
Analysis 23.10.
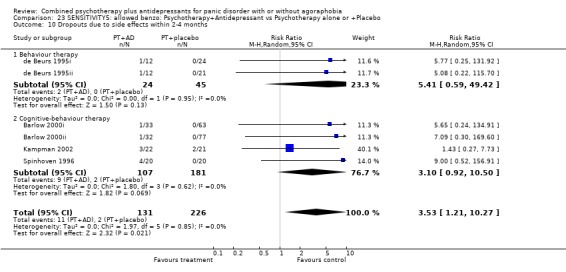
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 10 Dropouts due to side effects within 2‐4 months.
Analysis 23.11.
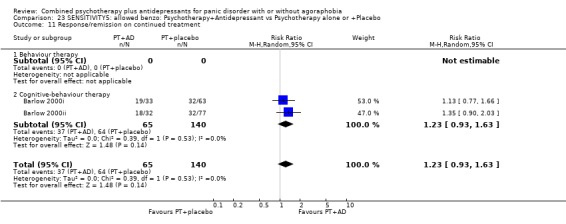
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 11 Response/remission on continued treatment.
Analysis 23.12.
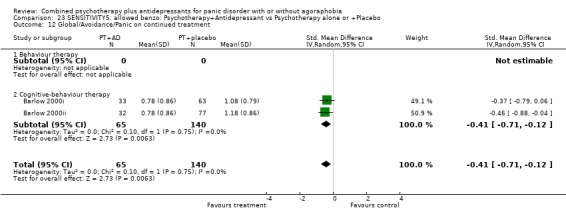
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 12 Global/Avoidance/Panic on continued treatment.
Analysis 23.13.
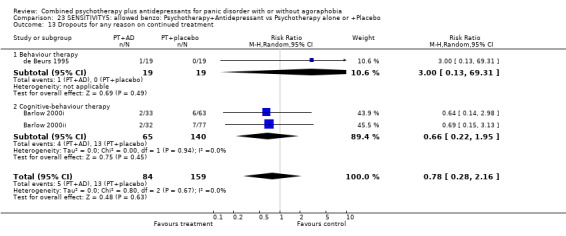
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 13 Dropouts for any reason on continued treatment.
Analysis 23.14.
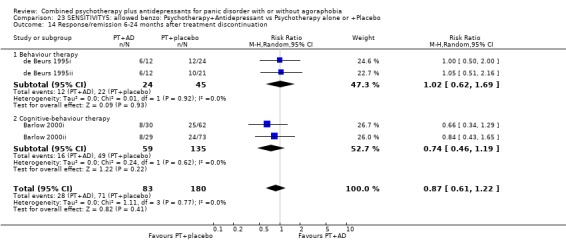
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 14 Response/remission 6‐24 months after treatment discontinuation.
Analysis 23.15.
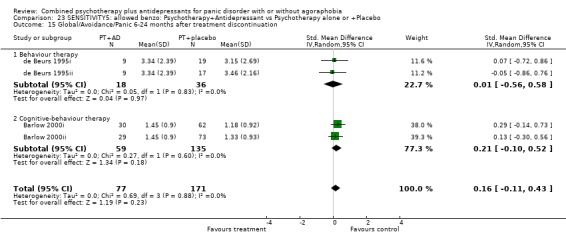
Comparison 23 SENSITIVITY5: allowed benzo: Psychotherapy+Antidepressant vs Psychotherapy alone or +Placebo, Outcome 15 Global/Avoidance/Panic 6‐24 months after treatment discontinuation.
What's new
| Date | Event | Description |
|---|---|---|
| 1 November 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 3, 2003 Review first published: Issue 1, 2007
| Date | Event | Description |
|---|---|---|
| 9 September 2006 | New citation required and conclusions have changed | Substantive amendment |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: not blind | |
| Participants | DIAGNOSIS: DSM‐IV panic disorder (% agoraphobic unspecified) AGE: mean=31.4 to 31.7 years SEX: men and women HISTORY: ‐ PSYCHIATRIC COMORBIDITY: No comorbidity was allowed. MEDICAL COMORBIDITY: ‐ | |
| Interventions | ACUTE PHASE: 9 weeks 1. fluvoxamine (mean=64 mg/d) + CBT (9 weekly sessions) 2. fluvoxamine alone (mean=154 mg/d) 3. CBT alone ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE: None. FOLLOW‐UP: None. |
|
| Outcomes | RESPONSE: >=50% reduction in panic frequency [imputed from mean&SD] REMISSION: ‐ GLOBAL: ‐ PANIC ATTACK: panic frequency AGORAPHOBIA: ‐ GENERAL ANXIETY: HAM‐A, BAI DEPRESSION: HAM‐D, BDI FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with mild to no agoraphobia AGE: mean=34.1 to 37.8 years SEX: 62% women HISTORY: mean duration of panic disorder=5.5 to 6.6 years During wash‐out, up to 10 doses of benzos were allowed during 2 weeks. PSYCHIATRIC COMORBIDITY: 27% suffered from current major depression. MEDICAL COMORBIDITY: Significant medical illness was excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. imipramine (mean=214 to 239 mg/d by week 12) + CBT (11sessions during 3 months) 2. imipramine alone 3. CBT alone 4. CBT + placebo 5. placebo alone (not used in the current meta‐analysis) ACUTE PHASE CO‐INTERVENTION: Patients were permitted up to 20 doses of benzo (0.5 mg of alprazolam equivalent) during 3 months after the study started. MAINTENANCE: 6 months of monthly appointments MODE OF DISCONTINUATION: Abrupt (?) FOLLOW‐UP: at 6 months after treatment discontinuation. 33% of the original cohort was successfully followed up. INTERVENTIONS AFTER TRIAL DISCONTINUATION: described as "no treatment" but more details lacking |
|
| Outcomes | RESPONSE: >= 40% reduction on PDSS; "much improved" or better on CGI Improvement and "mild" or less on CGI Severity REMISSION: 2 or better on CGI Severity GLOBAL: PDSS, CGI PANIC ATTACK: ‐ AGORAPHOBIA: ‐ GENERAL ANXIETY: ‐ DEPRESSION: ‐ FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Same as (Barlow 2000) but refers only to comparison with psychotherapy + placebo. | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Same as (Barlow 2000) but refers only to comparison with psychotherapy alone. | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ALLOCATION CONCEALMENT: adequate BLINDING:unclear | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with or without agoraphobia (81% with agoraphobia) AGE: mean=33.9 SEX: 66% women HISTORY: mean duration of panic disorder=4.8 years PSYCHIATRIC COMORBIDITY: 19% with major depression, 27% with social phobia, 16% with simple phobia, 10% with GAD, 32% with personality disorder. Melancholic depression, bipolar disorder, OCD, substance abuse/dependence were excluded. MEDICAL COMORBIDITY: Concurrent medical illness was excluded. | |
| Interventions | ACUTE PHASE: 20 weeks 1. paroxetine (mean=31 mg/d, range: 10‐60 mg/d) + cognitive‐interpersonal group therapy (2 individual sessions + 20 weekly group sessions, including elements of CBT and IPT) 2. paroxetine alone ACUTE PHASE CO‐INTERVENTION: Concomitant p.r.n. intake of alprazolam up to 1 mg/d was allowed. MAINTENANCE: None. MODE OF DISCONTINUATION: tapering from week 20 to week 24 FOLLOW‐UP: at 24 weeks, i.e. at the end of tapering. 50% of the original cohort were successfully followed up. |
|
| Outcomes | RESPONSE: Much or very much improved on CGI REMISSION: Free of panic attacks GLOBAL: ‐ PANIC ATTACK: panic frequency AGORAPHOBIA: 4‐point rating of agoraphobia GENERAL ANXIETY: 11‐point rating of anticipatory anxiety DEPRESSION: ‐ FUNCTIONING: Sheehan Disability Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with moderate to severe agoraphobia AGE: mean=38.8 SEX: 75% women HISTORY: mean duration of panic disorder=9.4 years PSYCHIATRIC COMORBIDITY: Current major depression was included if it developed after panic disorder. Patients with psychotic disorders, organic mental disorders, or psychoactive substance use disorders were excluded. MEDICAL COMORBIDITY: Patients with severe medical illness, pregnant and lactating women were excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. fluvoxamine (100‐150 mg/day) + exposure (12 weekly sessions) 2. exposure alone 3. placebo + exposure 4. psychological panic management plus exposure (not used in the current meta‐analysis) ACUTE PHASE CO‐INTERVENTION: 18 out of 97 patients used benzo during the trial. Concomitant use of benzo was permitted when patients had been taking benzo for more than 3 months and were willing to keep use at a constant dosage during the trial. MAINTENANCE: None. MODE OF DISCONTINUATION: Continue the drug for the time being FOLLOW‐UP: at 24 months after trial termination. 74% was successfully followed up. INTERVENTIONS AFTER TRIAL DISCONTINUATION: 77% received additional treatment, equally divided over four arms |
|
| Outcomes | RESPONSE: >=50% reduction in FQ‐Ag [imputed from mean&SD] REMISSION: panic‐free GLOBAL: Global outcome (1‐9; the larger, the better) PANIC ATTACK: panic frequency AGORAPHOBIA: Agoraphobia composite, FQ‐Ag, Multi‐Task Behavioral Avoidence Test GENERAL ANXIETY: Somatic Anxeity composite DEPRESSION: Depression composite, BDI FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Same as (de Beurs 1995) but refers only to the comparison with psychotherapy + placebo. | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Same as (de Beurs 1995) but refers only to the comparison with psychotherapy alone. | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with or without agoraphobia (42% with moderate or severe agoraphobia) AGE: mean=33.6 to 37.8 years SEX: 65% women HISTORY: mean duration of panic disorder=4.6 years PSYCHIATRIC COMORBIDITY: Major depression was included if it preceded panic. Those with history of seizures, bipolar or melancholic depression, cyclothymic disorder, obsessive‐compulsive disorder or current drug or alcohol dependence were excluded. MEDICAL COMORBIDITY: "In good physical health." | |
| Interventions | ACUTE PHASE: 6 weeks 1. clomipramine (100 mg/d) or lofepramine (140 mg/d) + CBT (6 one‐hour sessions over eight weeks) 2. placebo + CBT ACUTE PHASE CO‐INTERVENTION: No psychotropic drug was allowed. MAINTENANCE: None. MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: None (After 6 weeks, those on placebo received antidepressants and the double‐blind was broken at 8 weeks) |
|
| Outcomes | RESPONSE: >=40% reduction in CGI [imputed from mean&SD] REMISSION: panic‐free GLOBAL: CGI Severity, CGI Change PANIC ATTACK: ‐ AGORAPHOBIA: Fear Inventory GENERAL ANXIETY: HAM‐A DEPRESSION: HAM‐D, MADRS, CGI Depression, BDI, Wakefield Self Assessment Depressiion Inventory FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐IV panic disorder with agoraphobia AGE: mean=29.8 years SEX: 52% women HISTORY: mean duration of illness=3.5 years before start of first exposure therapy; resistant to twelve 30‐minute sessions for exposure PSYCHIATRIC COMORBIDITY: Current major depression was excluded. 38% suffered from personality disorder. MEDICAL COMORBIDITY: ‐ | |
| Interventions | ACUTE PHASE: 8 weeks 1. imipramine (mean=72 mg/d) + behaviour therapy (eight 45‐minute sessions) 2. behaviour therapy alone 3. behaviour therapy plus congitive therapy (not used in the present meta‐analysis) ACUTE PHASE CO‐INTERVENTION: not specifid MAINTENANCE: None. MODE OF DISCONTINUATION: naturalistic FOLLOW‐UP: at 24 months after acute phase treatment. 57% was successfully followed up. INTERVENTIONS AFTER TRIAL DISCONTINUATION: Those who faild to respond received further 16 weeks of exposure with or without imipramine treatments. |
|
| Outcomes | RESPONSE: ‐ REMISSION: panic‐free for a month and 1or 2 on CID‐agoraphobia GLOBAL: ‐ PANIC ATTACK: CID‐panic AGORAPHOBIA: FQ‐Ag, CID‐Agoraphobia GENERAL ANXIETY: CID‐generalized anxiety DEPRESSION: CID‐depression FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III agoraphobia AGE: mean=37 years SEX: 100% women HISTORY: mean duration of illness=9.5 years PSYCHIATRIC COMORBIDITY: ‐ MEDICAL COMORBIDITY: ‐ | |
| Interventions | ACUTE PHASE: 17 weeks 1. clomipramine (mean=95 mg/d) + behavior therapy (twice weekly for eight weeks) 2. clomipramine alone 3. placebo + behavior therapy 4. placebo alone ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE: 12 weeks On clomipraime or placebo only; no psychological intervention MODE OF DISCONTINUATION: naturalistic FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: >=50% reduction in FQ‐AG [imputed from mean&SD] REMISSION: ‐ GLOBAL: ‐ PANIC ATTACK: Number of days per week when panic was reported AGORAPHOBIA: FQ‐Ag, FSS‐III‐Ag, BAT GENERAL ANXIETY: ‐ DEPRESSION: SCL‐90‐R Depression FUNCTIONING: SAS‐SR Social Leisure | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐IV panic disorder with or without agoraphobia (% agoraphobic unspecified) AGE: between 18 and 65 SEX: unspecified HISTORY: unresponsive to initial 15 sessions of CBT (51% of the original sample) PSYCHIATRIC COMORBIDITY: 16% suffered from mood disorders, 16% from additional anxiety disorders, and 9% suffered from somatoform disorders. MEDICAL COMORBIDITY: ‐ | |
| Interventions | ACUTE PHASE: 8 weeks 1. paroxetine (40 mg/d) + CBT (4 sessions over 8 weeks) 2. placebo + CBT ACUTE PHASE CO‐INTERVENTION: Patients who had been using benzo were asked either to discontinue their medication under supervision or to adhere to a fixed daily dose throughout the study. MAINTENANCE: ‐ MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: 30% improvement in panic frequency, ACQ and ADS REMISSION: panic‐free GLOBAL: ‐ PANIC ATTACK: ‐ AGORAPHOBIA: MI, (ACQ, BSQ, ADS) GENERAL ANXIETY: FQ‐general anxiety DEPRESSION: ‐ FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with agoraphobia AGE: mean=35.1 years SEX: 75% women HISTORY: mean duration of illness=6.1 years PSYCHIATRIC COMORBIDITY: Depressed patients with 19‐item HAM‐D >=17 were excluded. Patients with bipolar disorder, obsessive‐compulsive disorder, organic mental disorder, schizophrenia, alcohol or drug dependence during the preceding 12 months, suicidality were excluded. MEDICAL COMORBIDITY: Clinically relevant organic diseases, significant laboratory abnormalities, known allergic reactions to monoamine oxidase inhibitors, pregnancy, lactation period were excluded. | |
| Interventions | ACUTE PHASE: 8 weeks 1. moclobemide (mean=551 mg/d) + CBT (nine 50‐minute individual sessions + two 6‐hour therapist‐aided exposure sessions) 2. moclobemide + clinical management 3. placebo + CBT 4. placebo + clinical management (not used in the present meta‐analysis) ACUTE PHASE CO‐INTERVENTION: If patiens had been taing benzo, tapering lasted upt to 4 weeks and withdrawal symptoms had to end at least 1 week prior to treatment. MAINTENANCE: ‐ MODE OF DISCONTINUATION: tapered off over two weeks (from week 8 to week 10). However, 70% of patients received treatment during follow‐up, defined either as at least one intake of a drug such as benzodiazepine, antidepressant or beta‐blocker or ast least one psychosocial treatmetn session. FOLLOW‐UP: at 6 months after treatment discontinuation. 67% was successfully followed‐up. INTERVENTIONS AFTER TRIAL DISCONTINUATION: 70% received at least some treatment after discontinuing moclobemide. |
|
| Outcomes | RESPONSE: "Much" or "very much improved" on CGI Improvement REMISSION: "Normal" or "borderline mentally ill" on CGI Severity GLOBAL: CGI Severity, CGI Improvement PANIC ATTACK: ‐ AGORAPHOBIA: FQ‐Ag, MI GENERAL ANXIETY: HAM‐A DEPRESSION: HAM‐D FUNCTIONING: Sheehan Disability Scale‐work, ‐leisure, ‐home life | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: approximately DSM‐III agoraphobia (96% had spontaneous panic attacks) AGE: mean=34 years SEX: 84% women HISTORY: mean duration of illness=8 years PSYCHIATRIC COMORBIDITY: Moderate to severe depression was excluded. MEDICAL COMORBIDITY: ‐ | |
| Interventions | ACUTE PHASE: 14 weeks 1. imipramine (mean=124‐158 mg/d) + behavior therapy (six bi‐weekly 1‐hour sessions; self‐exposure + therapist‐guided exposure or + relaxation) 2. placebo + behavior therapy ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE: 14 weeks MODE OF DISCONTINUATION: tapered off over 2 weeks (from week 26 to 28) FOLLOW‐UP: at 6 months and at 18 months after treatment discontinuation. 63% and 56% were successfully followed up, respectively. INTERVENTIONS AFTER TRIAL DISCONTINUATION: 47% received some treatment (antidepressant, benzodiazepine, therapist‐aided exposure) |
|
| Outcomes | RESPONSE: >= 2 points reduction in total phobic targets REMISSION: >= 4 points reduction in total phobic targets GLOBAL: ‐ PANIC ATTACK: spontaneous panics AGORAPHOBIA: FQ‐Ag, 4 phobic targets, FQ‐Global GENERAL ANXIETY: Non‐phobic anxiety, FQ‐Anxiety‐Depression, DEPRESSION: HAM‐D FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: not blind | |
| Participants | DIAGNOSIS: DSM‐III agoraphobia (patients scored, on average, 5.5 on an 0‐8 point scale of panic severity) AGE: mean=33.5 years SEX: 100% women HISTORY: mean duration of illness=7 years PSYCHIATRIC COMORBIDITY: Primary affective disorder, schizophrenia, organic brain syndrome and OCD were excluded. MEDICAL COMORBIDITY: Physical illness precluding imipramine was excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. imipramine (mean=125 mg/d) + programmd practice (self‐directed in vivo graded exposure with behavioural diary, eight 1‐hour sessions) 2. imipramine + anti‐exposure instruction ACUTE PHASE CO‐INTERVENTION: Patients had to be free of all psychotropic medications at least 2 weeks before starting treatment. MAINTENANCE: ‐ MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: >=50% reduction on Self‐Rated Severity REMISSION: no spontaneous panic GLOBAL: Self‐Rated Panic Overall Severity [0‐8] PANIC ATTACK: ‐ AGORAPHOBIA: FQ‐Ag GENERAL ANXIETY: Zung Anxiety Scale DEPRESSION: HAM‐D FUNCTIONING: Clinician's Global Assessment [1‐5] | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: adequate BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III agoraphobia with panic AGE: mean=36.5 years SEX: 84% women HISTORY: mean duration of illness=10.5 years PSYCHIATRIC COMORBIDITY: Primary affective disorder or concurrent major depressive episode, schizophrenia, organic brain syndrome, OCD, somatization disorder, substance abuse, or severe personality disorder were excluded. MEDICAL COMORBIDITY: Physical illness precluding imipramine was excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. imipramine (mean=130 mg/d) + programmed practice (self‐directed in vivo graded exposure, twelve 90‐min group sessions) 2. placebo + programmed practice ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE: ‐ MODE OF DISCONTINUATION: naturalistic FOLLOW‐UP: at 6 months and 24 months after acute phase treatment. 50% and 63% were successfully followed up, respectively. INTERVENTIONS AFTER TRIAL DISCONTINUATION: 30% had interim treatment (individual therapy, group therapy, anxiolytics, antidepressants) |
|
| Outcomes | RESPONSE: >=50% reduction in self‐rated severity of phobia (imputed from mean & SD) REMISSION: High end‐state functioning GLOBAL: Self‐rated Severity of Phobia [0‐8] PANIC ATTACK: Self‐rated Panic Overall Severity [0‐8] AGORAPHOBIA: FQ‐Ag [0‐40], Individualized phobic anxiety‐avoidance [0‐8], Behavioral avoidance‐anxiety index [0‐8] GENERAL ANXIETY: Zung Anxiety Scale [20‐80] DEPRESSION: Beck Depression Inventory [0‐63] FUNCTIONING: Clinician's Global Assessment [1‐5] | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ALLOCATION CONCEALMENT: adequate BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III agoraphobia with panic AGE: mean=36.5 years SEX: 84% women HISTORY: mean duration of illness=10.5 years PSYCHIATRIC COMORBIDITY: Primary affective disorder or concurrent major depressive episode, schizophrenia, organic brain syndrome, OCD, somatization disorder, substance abuse, or severe personality disorder were excluded. MEDICAL COMORBIDITY: Physical illness precluding imipramine was excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. imipramine (mean=130 mg/d) + programmed practice (self‐directed in vivo graded exposure) + flooding twelve 90‐min group sessions (twelve 90‐min group sessions) 2. placebo + programmed practice + flooding ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE: ‐ MODE OF DISCONTINUATION: naturalistic FOLLOW‐UP: at 6 months and 12 months after acute phase treatment. 63% and 55% were successfully followed up, respectively. INTERVENTIONS AFTER TRIAL DISCONTINUATION: 30% had interim treatment (individual therapy, group therapy, anxiolytics, antidepressants) |
|
| Outcomes | RESPONSE: >=50% reduction in self‐rated severity of phobia (imputed from mean & SD) REMISSION: High end‐state functioning GLOBAL: SElf‐rated Severity of Phobia [0‐8] PANIC ATTACK: Self‐rated Panic Overall Severity [0‐8] AGORAPHOBIA: FQ‐Ag [0‐40], Individualized phobic anxiety‐avoidance [0‐8], Behavioral avoidance‐anxiety index [0‐8] GENERAL ANXIETY: Zung Anxiety Scale [20‐80] DEPRESSION: Beck Depression Inventory [0‐63] FUNCTIONING: Clinician's Global Assessment [1‐5] | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with or without agoraphobia (64% reported moderate to severe agoraphobia) AGE: mean=37.4 years SEX: 76% women HISTORY: unspecified PSYCHIATRIC COMORBIDITY: Primary diagnosis of major depression, generalized anxiety disorder, schizophrenia, dementia, organic brain disease, alcohol or drug abuse, or concomitant treatment with psychotropics and anticoagulants were excluded. The baseline 17‐item HAM‐D had to be 14 or less. MEDICAL COMORBIDITY: ‐ | |
| Interventions | ACUTE PHASE: 12 weeks 1. paroxetine (40‐60 mg/d) + CBT (details not given) 2. placebo + CBT ACUTE PHASE CO‐INTERVENTION: Concomitant use of benzo was prohibited. The urine was screened. MAINTENANCE: ‐ MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: >=50% reduction in panic frequency REMISSION: "mildly ill" or less on CGI GLOBAL: ‐ PANIC ATTACK: panic frequency AGORAPHOBIA: ‐ GENERAL ANXIETY: Zung Anxiety Scale DEPRESSION: ‐ FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with or without agoraphobia (% agoraphobia unclear; however, the average score for FQ‐Ag was around 15, indicating most had at least some agoraphobia) AGE: mean=33.2 to 38.8 SEX: 78% women HISTORY: mean duration of panic disorder = 5.1 to 7.3 years Patients who had received psychotherapy within 6 months were excluded. Drugs were washed out over 4 weeks. PSYCHIATRIC COMORBIDITY: Concurrent major depression (defined as MADRS>=21) was excluded. OCD, paranoid personality disorder, schizophrenia, schizoaffective disorder, manic disorder, other unspecified psychosis, epilepsy, organic brain disease, alcohol dependence, drug dependence were excluded. MEDICAL COMORBIDITY: Severe concurrent somatic disease and a physical disability that severely restricted mobility were excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. fluvoxamine (100‐150 mg/day) + CBT (12 sessions) 2. fluvoxamine alone 3. CBT alone 4. CBT + placebo 5. placebo alone [not included in the present meta‐analysis] ACUTE PHASE CO‐INTERVENTION: Patients were required to undergo a 4‐week washout from psychotropics before entry into the study. MAINTENANCE: No maintenance phase MODE OF DISCONTINUATION: Abrupt FOLLOW‐UP: At 6 months after treatment discontinuation. 79% was successfully followed up. INTERVENTIONS AFTER TRIAL DISCONTINUATION: Patients were required not to receive any psychotropic drugs or psychotherapies but at least 33% received further treatment. |
|
| Outcomes | RESPONSE: "Very much" or "Much improved" on CGI Change REMISSION: "Normal" or "borderline" on CGI Severity GLOBAL: CGI Severity, CGI Change PANIC ATTACK: ‐ AGORAPHOBIA: FQ‐Ag GENERAL ANXIETY: HAM‐A DEPRESSION: MADRS FUNCTIONING: Sheehan Disability Scale‐work, ‐social, ‐home | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Same as (Sharp 1996) but refers only to the comparison with psychotherapy + placebo. | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | Same as (Sharp 1996) but refers only to the comparison with psychotherapy alone. | |
| Participants | ||
| Interventions | ||
| Outcomes | ||
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | D ‐ Not used |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: authors' own criteria, very similar to DSM‐IV panic disorder with agoraphobia AGE: mean=37.1 years SEX: 82% women HISTORY: mean duration of panic disorder = 11.5 to 13.5 years. On average, patients had received 4 years of psychoanalysis or behavior therapy. PSYCHIATRIC COMORBIDITY: Psychosis was excluded. MEDICAL COMORBIDITY: Physicall illness was excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. imipramine (150 mg/d) + group behavior therapy (1‐hour supportive group therapy every two weeks for three months; Patients were encouraged to gradually reapproach phobic situations and objects, and were rewarded emotionally when they did so) 2. placebo + group behavior therapy ACUTE PHASE CO‐INTERVENTION: Patients were required to avoid all psychtropic drugs other than imipramine and phenelzine. MAINTENANCE: ‐ MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: Partial or marked improvement on Symptom Severity and Avoidance Scale REMISSION: Marked improvement on Symptom Severity and Phobic Avoidance Scale GLOBAL: Symptom Severity and Phobic Avoidacne Scale[1‐5] PANIC ATTACK: ‐ AGORAPHOBIA: Wolpe‐Lang FSS GENERAL ANXIETY: SCL anxiety DEPRESSION: Zung Depression Scale FUNCTIONING: Work and Social Disability Scale [1‐5] | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: authors' own criteria, very similar to DSM‐IV panic disorder with agoraphobia AGE: mean=37.1 years SEX: 82% women HISTORY: mean duration of panci disorder = 13.0 to 13.5 years. On average, patients had received 4 years of psychoanalysis or behavior therapy. PSYCHIATRIC COMORBIDITY: Psychosis was excluded. MEDICAL COMORBIDITY: Physicall illness was excluded. | |
| Interventions | ACUTE PHASE: 12 weeks 1. phenelzine (45 mg/d) + group behavior therapy (1‐hour supportive group therapy every two weeks for three months; Patients were encouraged to gradually reapproach phobic situations and objects, and were rewarded emotionally when they did so) 2. placebo + group behavior therapy ACUTE PHASE CO‐INTERVENTION: Patients were required to avoid all psychtropic drugs other than imipramine and phenelzine. MAINTENANCE: ‐ MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: Partial or marked improvement on Symptom Severity and Avoidance Scale REMISSION: Marked improvement on Symptom Severity and Phobic Avoidance Scale GLOBAL: Symptom Severity and Phobic Avoidacne Scale[1‐5] PANIC ATTACK: ‐ AGORAPHOBIA: Wolpe‐Lang FSS GENERAL ANXIETY: SCL anxiety DEPRESSION: Zung Depression Scale FUNCTIONING: Work and Social Disability Scale [1‐5] | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: not blind | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with or without agoraphobia (85% agoraphobic) AGE: mean=35.6 years SEX: 57% women HISTORY: mean duration of illness=6.2 years PSYCHIATRIC COMORBIDITY: Psychosis, major depression, alcohol abuse or dependence were excluded. MEDICAL COMORBIDITY: Hyperthyroidism, pheochromocytome, bronchial asthma or angina were excluded. | |
| Interventions | ACUTE PHASE: 6 weeks 1. tranzodone (mean=178 mg/d) + CBT (breathing retraining, progressive relaxation, catastrophic cognitions, voluntary hyperventilation, BUT NO in vivo exposure; 6 sessions) 2. tranzodone alone 3. CBT alone ACUTE PHASE CO‐INTERVENTION: 25 out of 60 patients were taking low potency benzo at the start of the study. They were required to keep the dosage constant throughout the study. MAINTENANCE: ‐ MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: >=50% reduction in agoraphobic avoidance [imputed from mean&SD] REMISSION: ‐ GLOBAL: ‐ PANIC ATTACK: panic frequency for two weeks; panic intensity [0‐10] AGORAPHOBIA: agoraphobic avoidance [0‐40]; agoraphobic anxiety [0‐40] GENERAL ANXIETY: ‐ DEPRESSION: Zung Depression Scale [20‐80] FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐IV panic disorder with or without agoraphobia (percent agoraphobic not given; however, the average score for FQ‐Ag was around 10.5 and 16.1, indicating most had at least some agoraphobia) AGE: mean=33.8 years SEX: 73% women HISTORY: None of the enrolled subjects reported taking benzodiazepines. PSYCHIATRIC COMORBIDITY: Major depressive disorder with melancholic features, schizophrenia, current substance abuse/dependence were excluded. MEDICAL COMORBIDITY: Seizure disorder, thyroid disease were excluded. | |
| Interventions | ACUTE PHASE: 10 weeks 1. paroxetine (mean=32.4 mg/d) + CBT (2 sessions only, using self‐help book, relaxation tape, cognitive restructuring, breathing control, graded exposure) 2. placebo + CBT ACUTE PHASE CO‐INTERVENTION: None of the subjected entrolled reported taking benzo. MAINTENANCE: ‐ MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: "Much" or "very much improved" on CGI Improvement REMISSION: panic free GLOBAL: ‐ PANIC ATTACK: frequency of panic attacks AGORAPHOBIA: FQ‐Ag GENERAL ANXIETY: Beck Anxiety Inventory DEPRESSION: Beck Depression Inventory FUNCTIONING: Sheehan Disability Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III agoraphobia with panic attacks AGE: mean=41.5 years SEX: 92% women HISTORY: mean duration of illness=12.2 years PSYCHIATRIC COMORBIDITY: None met criteria for major affective disorder. MEDICAL COMORBIDITY: | |
| Interventions | ACUTE PHASE: 8 weeks 1. imipramine (ca 180 mg/d) + behavior therapy (three 3‐hour group sessions + three 1.5‐hour individual sessions) 2. imipramine (with anti‐exposure) 3. placebo + behavior therapy ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE: 18 weeks MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: >=50% reduction in FQ‐Ag [imputed from mean&SD] REMISSION: GLOBAL: ‐ PANIC ATTACK: frequency of panic attacks AGORAPHOBIA: FQ‐Ag; BAT GENERAL ANXIETY: ‐ DEPRESSION: Beck Depression Inventory FUNCTIONING: ‐ | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: adequate [data provided by the original author] BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: DSM‐III‐R panic disorder with or without agoraphobia (80% agoraphobic) AGE: mean=31.7 years SEX: 58% women HISTORY: mean duration of illness=3.2 years PSYCHIATRIC COMORBIDITY: Personality disorder, primary major depression, psychosis, substance abuse, eating disorder, agoraphobia with or without panic attacks were excluded. MEDICAL COMORBIDITY: Significant medical illness, pregnancy and lactation were excluded. | |
| Interventions | ACUTE PHASE: 12‐15 weeks 1. clomipramine (mean=108‐113 mg/d) + psychodynamic psychotherapy (15 weekly brief dynamic psychotherapy sessions, without encouraging exposure) 2. clomipramine alone ACUTE PHASE CO‐INTERVENTION: 11 out of 40 took benzo in the first month; 4 used benzo irregularly for six months. MAINTENANCE: 33‐36 weeks MODE OF DISCONTINUATION: tapered off over 6 weeks FOLLOW‐UP: at 9 months after treatment discontinuation. 100% follow‐up was achieved. INTERVENTIONS AFTER TRIAL DISCONTINUATION: Of 20 patients in the first arm, 4 took effective medication. Of 20 patients in the second arm, 14 took effective medication and 4 received psychological treatment. |
|
| Outcomes | RESPONSE: >=40% reduction in Patient Status Scale [imputed from mean&SD] REMISSION: panic free GLOBAL: Patient Status Scale PANIC ATTACK: Panic Attack and Anxiety Scale AGORAPHOBIA: Phobia Scale GENERAL ANXIETY: HAM‐A DEPRESSION: HAM‐D FUNCTIONING: Sheehan Disability Scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: "agoraphobia" (the average severity being 5.9 to 6.3 on a scale between 1 through 7) with "spontaneous panic" (again the average severity being 4.1 to 4.9 on a scale between 1 through 7) AGE: mean=35.6 years SEX: 100% women HISTORY: mean duration of illness=8.6 years PSYCHIATRIC COMORBIDITY: Schizophrenia and significant current depression were excluded. MEDICAL COMORBIDITY: ‐ | |
| Interventions | ACUTE PHASE: 14 weeks 1. imipramine (ca 200 mg/d) + behavior therapy (group in vivo exposure, ten 3‐4‐hour sessions) 2. placebo + behavior therapy ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE: 12 weeks MODE OF DISCONTINUATION: ‐ FOLLOW‐UP: ‐ |
|
| Outcomes | RESPONSE: "moderate" to "marked" improvement on CGI Change by an independent evaluator REMISSION: "Marked" improvement on CGI Change by an independent evaluator GLOBAL: CGI Change PANIC ATTACK: spontaneous panic scale [1‐7] AGORAPHOBIA: primary phobia scale [1‐7] GENERAL ANXIETY: ‐ DEPRESSION: ‐ FUNCTIONING: functioning scale [1‐7] | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | ALLOCATION CONCEALMENT: unclear BLINDING: at least one measure was assessed by an independent assessor blind to treatment allocation | |
| Participants | DIAGNOSIS: authors' own criteria, similar to DSM‐III agoraphobia with panic attacks or DSM‐IV panic disorder with moderate to severe agoraphobia AGE: mean=35.5 years SEX: 65% women HISTORY: mean duration of illness=10.6 years PSYCHIATRIC COMORBIDITY: Patients rated as more than moderately depressed on BPRS were excluded. MEDICAL COMORBIDITY: not specified | |
| Interventions | ACUTE PHASE: 26 weeks 1. imipramine (mean=204 mg/d) + supportive therapy (dynamically oriented and non‐directive) + behavior therapy (twenty‐six 45‐minute sessions including relaxation training, imaginary desensitization, in vivo desensitization, assertiveness training) 2. imipramine + supportive therapy 3. placebo + supportive therapy + behavior therapy ACUTE PHASE CO‐INTERVENTION: not specified MAINTENANCE:‐ MODE OF DISCONTINUATION: naturalisitc FOLLOW‐UP: At 24 months after treatment discontinuation. 59% was successfully followed up. INTERVENTIONS AFTER TRIAL DISCONTINUATION: not specified |
|
| Outcomes | RESPONSE: "Moderate" to "marked" improvement on CGI Change by an independent evaluator REMISSION: "Marked" improvement on CGI Change by an independent evaluator GLOBAL: CGI Severity; CGI Improvement PANIC ATTACK: spontaneous panic AGORAPHOBIA: primary phobia GENERAL ANXIETY: Taylor Manifest Anxiety DEPRESSION: Self‐rating Symptom Scale depression FUNCTIONING: functioning scale | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
ACQ: Agoraphobic Cognitiions Questionnaire ADS: Anxiety Discomfort Scale BAI: Beck Anxiety Inventory BDI: Beck Depression Inventory BAT: Behavioral Avoidance Test BPRS: Bief Psychiatric Rating Scale BSQ: Body Sensations Questionnaire CGI: Clinical Global Impression CID: Clinical Interview for Depression FQ‐Ag: Fear Questionnaire Agoraphobia Subscale FSS: Fear Survey Schedule HAM‐A: Hamilton Rating Scale for Anxiety HAM‐D: Hamilton Rating Scale for Depression IPT: Interpersonalty Therapy MADRS: Montgomery‐Asberg Depression Rating Scale MI: Mobility Inventory PDSS: Panic Disorder Severity Scale SAS‐SR: Social Adjustment Scale‐Self Report SCL‐90‐R: Symptom Checklist 90 Revised
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agras 1991 | Randomization was flawed and the groups were not comparable (Personal communication from Dr Agras on Oct 14, 2003). |
| Ba 1999 | Although 3 arms had been planned (pharmacotherpay alone, pharmacotherapy plus CBT, pharmacotherapy plus CBT plus psychodynamic therapy), only the last two were successfully completed. Moreover, pharmacotherapy always consisted of SSRI plus alprazolam. |
| Chambless 1979 | Flooding versus Flooding + barbiturate |
| Cox 1988 | Randomized comparison between high serum level vs low serum level of imipramine, combined with behavior therapy |
| Lipsedge 1973 | No operational diagnostic criteria used. Iproniazid, though with MAO inhibiting effect, is not a widely recognized antidepressant. |
| Solyom 1981 | Although the overall study design appears to satisfy the inclusion criteria of this systematic review, the authors did not separately report the results for agoraphobia and social phobia. The original author was contacted but could not provide separate data for patients with agoraphobia. |
Contributions of authors
TAF, NW and RC contributed to the planning and writing of the protocol. TAF and NW selected the studies, assessed their quality and extracted data. All contributed to the writing of the final manuscript.
Sources of support
Internal sources
No sources of support supplied
External sources
Health and Labour Sciences Research Grants (Research on Health Technology Assessment) H13‐018, Japan.
Declarations of interest
TAF has received research funding and fees for speaking from the following pharmaceutical companies: Asahi Kasei, Astellas, Dai‐Nippon, Eisai, Eli Lilly, GlaxoSmithKline, Janssen, Kyowa Hakko, Meiji, Organon, Pfizer, Tsumura and Yoshitomi.
Edited (no change to conclusions)
References
References to studies included in this review
- Azhar MZ. Comparison of fluvoxamine alone, fluvoxamine and cognitive psychotherapy and psychotherapy alone in the treatment of panic disorder in Kelantan‐‐implications for management by family doctors. Medical Journal of Malaysia 2000;55:402‐8. [PubMed] [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive‐behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA 2000;283:2529‐36. [DOI] [PubMed] [Google Scholar]; Gorman JM, Martinez JM, Goetz R, Huppert JD, Ray S, Barlow DH, et al. The effect of pharmacotherapist characteristics on treatment outcome in panic disorder. Depression and Anxiety 2003;17:88‐93. [DOI] [PubMed] [Google Scholar]; Grilo CM, Money R, Barlow DH, Goddard AW, Gorman JM, Hofmann SG, et al. Pretreatment patient factors predicting attrition from a multicenter randomized controlled treatment study for panic disorder. Comprehensive Psychiatry 1998;39(6):323‐32. [DOI] [PubMed] [Google Scholar]; Hofmann SG, Barlow DH, Papp LA, Detweiler MF, Ray SE, Shear MK, et al. Pretreatment attrition in a comparative treatment outcome study on panic disorder. American Journal of Psychiatry 1998;155(1):43‐7. [DOI] [PubMed] [Google Scholar]; Hofmann SG, Shear MK, Barlow DH, Gorman JM, Hershberger D, Patterson M, et al. Effects of panic disorder treatments on personality disorder characteristics. Depression and Anxiety 1998;8(1):14‐20. [PubMed] [Google Scholar]; Huppert JD, Bufka LF, Barlow DH, Gorman JM, Shear MK, Woods SW. Therapists, therapist variables, and cognitive‐behavioral therapy outcome in a multicenter trial for panic disorder. Journal of Consulting and Clinical Psychology 2001;69:747‐55. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive‐behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA 2000;283:2529‐36. [DOI] [PubMed] [Google Scholar]; Gorman JM, Martinez JM, Goetz R, Huppert JD, Ray S, Barlow DH, et al. The effect of pharmacotherapist characteristics on treatment outcome in panic disorder. Depression and Anxiety 2003;17:88‐93. [DOI] [PubMed] [Google Scholar]; Grilo CM, Money R, Barlow DH, Goddard AW, Gorman JM, Hofmann SG, et al. Pretreatment patient factors predicting attrition from a multicenter randomized controlled treatment study for panic disorder. Comprrehensive Psychiatry 1998;39(6):323‐32. [DOI] [PubMed] [Google Scholar]; Hofmann SG, Barlow DH, Papp LA, Detweiler MF, Ray SE, Shear MK, et al. Pretreatment attrition in a comparative treatment outcome study on panic disorder. American Journal of Psychiatry 1998;155(1):43‐7. [DOI] [PubMed] [Google Scholar]; Hofmann SG, Shear MK, Barlow DH, Gorman JM, Hershberger D, Patterson M, et al. Effects of panic disorder treatments on personality disorder characteristics. Depression and Anxiety 1998;8(1):14‐20. [PubMed] [Google Scholar]; Huppert JD, Bufka LF, Barlow DH, Gorman JM, Shear MK, Woods SW. Therapists, therapist variables, and cognitive‐behavioral therapy outcome in a multicenter trial for panic disorder. Journal of Consulting and Clinical Psychology 2001;69:747‐55. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Gorman JM, Shear MK, Woods SW. Cognitive‐behavioral therapy, imipramine, or their combination for panic disorder: A randomized controlled trial. JAMA 2000;283:2529‐36. [DOI] [PubMed] [Google Scholar]; Gorman JM, Martinez JM, Goetz R, Huppert JD, Ray S, Barlow DH, et al. The effect of pharmacotherapist characteristics on treatment outcome in panic disorder. Depression and Anxiety 2003;17:88‐93. [DOI] [PubMed] [Google Scholar]; Grilo CM, Money R, Barlow DH, Goddard AW, Gorman JM, Hofmann SG, et al. Pretreatment patient factors predicting attrition from a multicenter randomized controlled treatment study for panic disorder. Comprehensive Psychiatry 1998;39(6):323‐32. [DOI] [PubMed] [Google Scholar]; Hofmann SG, Barlow DH, Papp LA, Detweiler MF, Ray SE, Shear MK, et al. Pretreatment attrition in a comparative treatment outcome study on panic disorder. American Journal of Psychiatry 1998;155(1):43‐7. [DOI] [PubMed] [Google Scholar]; Hofmann SG, Shear MK, Barlow DH, Gorman JM, Hershberger D, Patterson M, et al. Effects of panic disorder treatments on personality disorder characteristics. Depression and Anxiety 1998;8(1):14‐20. [PubMed] [Google Scholar]; Huppert JD, Bufka LF, Barlow DH, Gorman JM, Shear MK, Woods SW. Therapists, therapist variables, and cognitive‐behavioral therapy outcome in a multicenter trial for panic disorder. Journal of Consulting and Clinical Psychology 2001;69:747‐55. [DOI] [PubMed] [Google Scholar]
- Berger P, Sachs G, Amering M, Holzinger A, Bankier B, Katschnig H. Personality disorder and social anxiety predict delayed response in drug and behavioral treatment of panic disorder. Journal of Affective Disorders 2004;80:75‐8. [DOI] [PubMed] [Google Scholar]; Berger P, Sachs G, Amering M, Holzinger A, Maierhofer D, Bankier B, et al. Predictors of treatment‐response in panic disorder. 151st Annual Meeting of the American Psychiatric Association. 1998. [Google Scholar]; Katschnig H, Berger P, Sachs G, Amering M, Holzinger A, Maierhofer D, et al. Drugs and psychotherapy in panic disorder: methodological issues. 151st Annual Meeting of the American Psychiatric Association. 1998. [Google Scholar]
- Beurs E, Balkom AJ, Lange A, Koele P, Dyck R. Treatment of panic disorder with agoraphobia: comparison of fluvoxamine, placebo, and psychological panic management combined with exposure and of exposure in vivo alone. American Journal of Psychiatry 1995;152:683‐91. [DOI] [PubMed] [Google Scholar]; Beurs E, Balkom AJ, Dyck R, Lange A. Long‐term outcome of pharmacological and psychological treatment for panic disorder with agoraphobia: a 2‐year naturalistic follow‐up. Acta Psychiatrica Scandinavica 1999;99:59‐67. [DOI] [PubMed] [Google Scholar]; Beurs E, Dyck R, Lange A, Balkom AJ. Perceived upbringing and its relation to treatment outcome in agoraphobia. Clinical Psychology and Psychotherapy 1995;2:78‐85. [Google Scholar]; Balkom AJ, Beurs E, Koele P, Lange A, Dyck R. Long‐term benzodiazepine use is associated with smaller treatment gain in panic disorder with agoraphobia. Journal of Nervous and Mental Disease 1996;184(2):133‐5. [DOI] [PubMed] [Google Scholar]; Balkom AJ, Beurs E, Dyck R, Lange A. Two‐year follow‐up after treatment of panic disorder with agoraphobia. 8th European College of Neuropsychopharmacology Congress. 8th European College of Neuropsychopharmacology Congress. 1995. [Google Scholar]
- Beurs E, Balkom AJ, Lange A, Koele P, Dyck R. Treatment of panic disorder with agoraphobia: comparison of fluvoxamine, placebo, and psychological panic management combined with exposure and of exposure in vivo alone. American Journal of Psychiatry 1995;152:683‐91. [DOI] [PubMed] [Google Scholar]; Beurs E, Balkom AJ, Dyck R, Lange A. Long‐term outcome of pharmacological and psychological treatment for panic disorder with agoraphobia: a 2‐year naturalistic follow‐up. Acta Psychiatrica Scandinavica 1999;99:59‐67. [DOI] [PubMed] [Google Scholar]; Beurs E, Dyck R, Lange A, Balkom AJ. Perceived upbringing and its relation to treatment outcome in agoraphobia. Clinical Psychology and Psychotherapy 1995;2:78‐85. [Google Scholar]; Balkom AJ, Beurs E, Koele P, Lange A, Dyck R. Long‐term benzodiazepine use is associated with smaller treatment gain in panic disorder with agoraphobia. Journal of Nervous and Mental Disease 1996;184(2):133‐5. [DOI] [PubMed] [Google Scholar]; Balkom AJ, Beurs E, Dyck R, Lange A. Two‐year follow‐up after treatment of panic disorder with agoraphobia. 8th European College of Neuropsychopharmacology Congress. 8th European College of Neuropsychopharmacology Congress. 1995. [Google Scholar]
- Beurs E, Balkom AJ, Lange A, Koele P, Dyck R. Treatment of panic disorder with agoraphobia: comparison of fluvoxamine, placebo, and psychological panic management combined with exposure and of exposure in vivo alone. American Journal of Psychiatry 1995;152:683‐91. [DOI] [PubMed] [Google Scholar]; Beurs E, Balkom AJ, Dyck R, Lange A. Long‐term outcome of pharmacological and psychological treatment for panic disorder with agoraphobia: a 2‐year naturalistic follow‐up. Acta Psychiatrica Scandinavica 1999;99:59‐67. [DOI] [PubMed] [Google Scholar]; Beurs E, Dyck R, Lange A, Balkom AJ. Perceived upbringing and its relation to treatment outcome in agoraphobia. Clinical Psychology and Psychotherapy 1995;2:78‐85. [Google Scholar]; Balkom AJ, Beurs E, Koele P, Lange A, Dyck R. Long‐term benzodiazepine use is associated with smaller treatment gain in panic disorder with agoraphobia. Journal of Nervous and Mental Disease 1996;184(2):133‐5. [DOI] [PubMed] [Google Scholar]; Balkom AJ, Beurs E, Dyck R, Lange A. Two‐year follow‐up after treatment of panic disorder with agoraphobia. 8th European College of Neuropsychopharmacology Congress. 8th European College of Neuropsychopharmacology Congress. 1995. [Google Scholar]
- Fahy TJ, O'Rourke D, Brophy J, Schazmann W, Sciascia S. The Galway Study of Panic Disorder. I: Clomipramine and lofepramine in DSM III‐R panic disorder: a placebo controlled trial. Journal of Affective Disorders 1992;25:63‐75. [DOI] [PubMed] [Google Scholar]; O'Rourke D, Fahy TJ, Brophy J, Prescott P. The Galway study of panic disorder III: Outcome at 5 to 6 years. British Journal of Psychiatry 1996;168:462‐9. [DOI] [PubMed] [Google Scholar]
- Fava GA, Savron G, Zielezny M, Grandi S, Rafanelli C, Conti S. Overcoming resistance to exposure in panic disorder with agoraphobia. Acta Psychiatrica Scandinavica 1997;95:306‐12. [DOI] [PubMed] [Google Scholar]
- Johnson DG, Troyer IE, Whitsett SF, Dalby JT. Clomipramine therapy and behavior therapy with agoraphobic women. Canadian Journal of Psychiatry ‐ Revue Canadienne De Psychiatrie 1995;40:192‐9. [PubMed] [Google Scholar]
- Kampman M, Keijsers GP, Hoogduin CA, Hendriks GJ. A randomized, double‐blind, placebo‐controlled study of the effects of adjunctive paroxetine in panic disorder patients unsuccessfully treated with cognitive‐behavioral therapy alone. Journal of Clinial Psychiatry 2002;63(9):772‐7. [DOI] [PubMed] [Google Scholar]
- Loerch B, Graf‐Morgenstern M, Hautzinger M, Schlegel S, Hain C, Sandmann J, et al. Randomised placebo‐controlled trial of moclobemide, cognitive‐ behavioural therapy and their combination in panic disorder with agoraphobia. British Journal of Psychiatry 1999;174:205‐12. [DOI] [PubMed] [Google Scholar]
- Cohen SD, Monteiro W, Marks IM. Two‐year follow‐up of agoraphobics after exposure and imipramine. British Journal of Psychiatry 1984;144:276‐81. [DOI] [PubMed] [Google Scholar]; Lelliott PT, Marks IM, Monteiro WO, Tsakiris F, Noshirvani H. Agoraphobics 5 years after imipramine and exposure. Outcome and predictors. Journal of Nervous and Mental Disease 1987;175(10):599‐605. [DOI] [PubMed] [Google Scholar]; Marks IM, Gray S, Cohen D, Hill R, Mawson D, Ramm E, et al. Imipramine and brief therapists‐aided exposure in agoraphobics having self‐exposure homework. Archives of General Psychiatry 1983;40(2):153‐62. [DOI] [PubMed] [Google Scholar]
- Mavissakalian M, Michelson L, Dealy RS. Pharmacological treatment of agoraphobia: imipramine versus imipramine with programmed practice. British Journal of Psychiatry 1983;143:348‐55. [DOI] [PubMed] [Google Scholar]
- Mavissakalian M. Combined behavioral‐therapy and pharmacotherapy of agoraphobia. Journal of Psychiatric Research 1993;27:179‐91. [DOI] [PubMed] [Google Scholar]; Mavissakalian M, Michelson L. Agoraphobia: behavioral and pharmacological treatments, preliminary outcome, and process findings. Psychopharmacology Bulletin 1982;18:91‐103. [PubMed] [Google Scholar]; Mavissakalian M, Michelson L. Agoraphobia: relative and combined effectiveness of therapist‐assisted in vivo exposure and imipramine. Journal of Clinical Psychiatry 1986;47:117‐22. [PubMed] [Google Scholar]; Mavissakalian M, Michelson L. Self‐directed in vivo exposure practice in behavioral and pharmacological treatments of agoraphobia. Behavior Therapy 1983;14:506‐19. [Google Scholar]; Mavissakalian M, Michelson L. Two‐year follow‐up of exposure and imipramine treatment of agoraphobia. American Journal of Psychiatry 1986;143:1106‐12. [DOI] [PubMed] [Google Scholar]; Mavissakalian M, Perel J. Imipramine in the treatment of agoraphobia: dose‐response relationships. American Journal of Psychiatry 1985;142:1032‐6. [DOI] [PubMed] [Google Scholar]
- Mavissakalian M. Combined behavioral‐therapy and pharmacotherapy of agoraphobia. Journal of Psychiatric Research 1993;27:179‐91. [DOI] [PubMed] [Google Scholar]; Mavissakalian M, Michelson L. Agoraphobia: behavioral and pharmacological treatments, preliminary outcome, and process findings. Psychopharmacology Bulletin 1982;18:91‐103. [PubMed] [Google Scholar]; Mavissakalian M, Michelson L. Agoraphobia: relative and combined effectiveness of therapist‐assisted in vivo exposure and imipramine. Journal of Clinial Psychiatry 1986;47:117‐22. [PubMed] [Google Scholar]; Mavissakalian M, Michelson L. Self‐directed in vivo exposure practice in behavioral and pharmacological treatments of agoraphobia. Behavior Therapy 1983;14:506‐19. [Google Scholar]; Mavissakalian M, Michelson L. Two‐year follow‐up of exposure and imipramine treatment of agoraphobia. American Journal of Psychiatry 1986;143:1106‐12. [DOI] [PubMed] [Google Scholar]; Mavissakalian M, Perel J. Imipramine in the treatment of agoraphobia: dose‐response relationships. American Journal of Psychiatry 1985;142:1032‐6. [DOI] [PubMed] [Google Scholar]
- Oehrberg S, Christiansen PE, Behnke K, Borup AL, Severin B, Soegaard J, et al. Paroxetine in the treatment of panic disorder. A randomised, double‐ blind, placebo‐controlled study. British Journal of Psychiatry 1995;167:374‐9. [DOI] [PubMed] [Google Scholar]
- Sharp DM, Power KG. Predicting treatment outcome for panic disorder and agoraphobia in primary care. Clinical Psychology and Psychotherapy 1999;6(5):336‐48. [Google Scholar]; Sharp DM, Power KG. Psychologist, patient, and general practitioneer ratings of outcome of pharmacological and psychological treatments for panic disorder and agoraphobia in primary care. Behavioural and Cognitive Psychotherapy 1998;26:13‐27. [Google Scholar]; Sharp DM, Power KG. Treatment‐outcome research in panic disorder: Dilemmas in reconciling the demands of pharmacological and psychological methodologies. Journal of Psychopharmacology 1997;11(4):373‐80. [DOI] [PubMed] [Google Scholar]; Sharp DM, Power KG, Simpson RJ, Swanson V, Anstee JA. Global measures of outcome in a controlled comparison of pharmacological and psychological treatment of panic disorder and agoraphobia in primary care. British Journal of General Practice 1997;47(416):150‐5. [PMC free article] [PubMed] [Google Scholar]; Sharp DM, Power KG, Simpson RJ, Swanson V, Moodie E, Anstee JA, et al. Fluvoxamine, placebo and cognitive behaviour therapy used alone and in combination in the treatment of ppanic disorder and agoraphobia. Journal of Anxiety Disorders 1996;10:219‐42. [MEDLINE: ] [Google Scholar]
- Sharp DM, Power KG. Predicting treatment outcome for panic disorder and agoraphobia in primary care. Clinical Psychology and Psychotherapy 1999;6(5):336‐48. [Google Scholar]; Sharp DM, Power KG. Psychologist, patient, and general practitioneer ratings of outcome of pharmacological and psychological treatments for panic disorder and agoraphobia in primary care. Behavioural and Cognitive Psychotherapy 1998;26:13‐27. [Google Scholar]; Sharp DM, Power KG. Treatment‐outcome research in panic disorder: Dilemmas in reconciling the demands of pharmacological and psychological methodologies. Journal of Psychopharmacology 1997;11(4):373‐80. [DOI] [PubMed] [Google Scholar]; Sharp DM, Power KG, Simpson RJ, Swanson V, Anstee JA. Global measures of outcome in a controlled comparison of pharmacological and psychological treatment of panic disorder and agoraphobia in primary care. British Journal of General Practice 1997;47(416):150‐5. [PMC free article] [PubMed] [Google Scholar]; Sharp DM, Power KG, Simpson RJ, Swanson V, Moodie E, Anstee JA, et al. Fluvoxamine, placebo and cognitive behaviour therapy used alone and in combination in the treatment of ppanic disorder and agoraphobia. Journal of Anxiety Disorders 1996;10:219‐42. [Google Scholar]
- Sharp DM, Power KG. Predicting treatment outcome for panic disorder and agoraphobia in primary care. Clinical Psychology and Psychotherapy 1999;6(5):336‐48. [Google Scholar]; Sharp DM, Power KG. Psychologist, patient, and general practitioneer ratings of outcome of pharmacological and psychological treatments for panic disorder and agoraphobia in primary care. Behavioural and Cognitive Psychotherapy 1998;26:13‐27. [Google Scholar]; Sharp DM, Power KG. Treatment‐outcome research in panic disorder: Dilemmas in reconciling the demands of pharmacological and psychological methodologies. Journal of Psychopharmacology 1997;11(4):373‐80. [DOI] [PubMed] [Google Scholar]; Sharp DM, Power KG, Simpson RJ, Swanson V, Anstee JA. Global measures of outcome in a controlled comparison of pharmacological and psychological treatment of panic disorder and agoraphobia in primary care. British Journal of General Practice 1997;47(416):150‐5. [PMC free article] [PubMed] [Google Scholar]; Sharp DM, Power KG, Simpson RJ, Swanson V, Moodie E, Anstee JA, et al. Fluvoxamine, placebo and cognitive behaviour therapy used alone and in combination in the treatment of ppanic disorder and agoraphobia. Journal of Anxiety Disorders 1996;10:219‐42. [Google Scholar]
- Sheehan DV, Ballanger J, Jacobsen G. Treatment of endogenous anxiety with phobic, hysterical, and hypochondriachal symptoms. Archives of General Psychiatry 1980;37:51‐9. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Ballanger J, Jacobsen G. Treatment of endogenous anxiety with phobic, hysterical, and hypochondriachal symptoms. Archives of General Psychiatry 1980;37:51‐9. [DOI] [PubMed] [Google Scholar]
- Spinhoven P, Onstein EJ, Klinkhamer RA, Klein EA. Panic management, trazodone and a combination of both in the treatment of panic disorder. Clinical Psychology and Psychotherapy 1996;3:86‐92. [Google Scholar]
- Stein MB, Ron Norton G, Walker JR, Chartier MJ, Graham R. Do selective serotonin re‐uptake inhibitors enhance the efficacy of very brief cognitive behavioral therapy for panic disorder? A pilot study. Psychiatry Research 2000;94:191‐200. [DOI] [PubMed] [Google Scholar]
- Roth WT, Telch MJ, Taylor CB, Agras WS. Autonomic changes after treatment of agoraphobia with panic attacks. Psychiatry Research 1988;24(1):95‐107. [DOI] [PubMed] [Google Scholar]; Telch MJ, Agras WS, Taylor CB, Roth WT, Gallen CC. Combined pharmacological and behavioral treatment for agoraphobia. Behavior Research and Therapy 1985;23:325‐35. [DOI] [PubMed] [Google Scholar]
- Dahl AA, Wiborg IM. Pharmacotherapy and brief dynamic psychotherapy of panic disorder. 9th European College of Neuropsychopharmacology Congress. Amsterdam, The Netherlands, 1996. [Google Scholar]; Wiborg IM, Dahl AA. Does brief dynamic psychotherapy reduce the relapse rate of panic disorder?. Archives of General Psychiatry 1996;53:689‐94. [DOI] [PubMed] [Google Scholar]; Wiborg IM, Dahl AA. Pharmacotherapy and brief dynamic psychotherapy of panic disorder. Xth World Congress of Psychiatry. Madrid, Spain, 1996. [Google Scholar]
- Zitrin CM. Differential treatment of phobias: Use of imipramine for panic attacks. Journal of Behavior Therapy and Experimental Psychiatry 1983;14(1):11‐8. [DOI] [PubMed] [Google Scholar]; Zitrin CM, Klein DF, Woerner MG. Treatment of agoraphobia with group exposure in vivo and imipramine. Archives of General Psychiatry 1980;37:63‐72. [DOI] [PubMed] [Google Scholar]
- Klein DF, Ross DC, Cohen P. Panic and avoidance in agoraphobia. Application of path analysis to treatment studies. Archives of General Psychiatry 1987;44(4):377‐85. [DOI] [PubMed] [Google Scholar]; Klein DF, Zitrin CM, Woerner MG, Ross DC. Treatment of phobias. II. Behavior therapy and supportive psychotherapy: are there any specific ingredients?. Archives of General Psychiatry 1983;40(2):139‐45. [DOI] [PubMed] [Google Scholar]; Lipsitz JD, Mannuzza S, Klein DF, Ross DC, Fyer AJ. Specific phobia 10‐16 years after treatment. Depression and Anxiety 1999;10(3):105‐11. [PubMed] [Google Scholar]; Zitrin CM. Differential treatment of phobias: Use of imipramine for panic attacks. Journal of Behavior Therapy and Experimental Psychiatry 1983;14(1):11‐8. [DOI] [PubMed] [Google Scholar]; Zitrin CM, Klein DF, Lindemann C, Kaplan JH, Ganz VH. Comparison of short‐term treatment regimens in phobic patients: a preliminary report. In: Spitzer RL, Klein DF editor(s). Evaluation of Psychological Therapies. Baltimore, MD: Johns Hopkins Press, 1976:233‐250. [PubMed] [Google Scholar]; Zitrin CM, Klein DF, Woerner MG. Behavior therapy, supportive psychotherapy, imipramine, and phobias. Archives of General Psychiatry 1978;35:307‐16. [DOI] [PubMed] [Google Scholar]; Zitrin CM, Klein DF, Woerner MG, Ross DC. Treatment of phobias. I. Comparison of imipramine hydrochloride and placebo. Archives of General Psychiatry 1983;40:125‐38. [DOI] [PubMed] [Google Scholar]; Zitrin CM, Woerner MG, Klein DF. Differentiation of panic anxiety from anticipatory anxiety and avoidance behavior. In: Klein DF, Rabkin J editor(s). Anxiety: New Research and Changing Concepts. New York, NY: Raven Press, 1981. [Google Scholar]
References to studies excluded from this review
- Agras, WS, Telch, MJ, Taylor, CB, Roth, WT, Brouillard, M. Imipramine and exposure therapy in agoraphobia: untangling the actions and interactions. Telch and Lucas (1984).
- Ba G, Vigano C. Integrated therapy of panic disorder: a controlled study. 152nd Annual Meeting of the American Psychiatric Association. Washington DC, USA, 1999. [Google Scholar]; Ba G, Vigano C. Integrated therapy of panic disorders: a controlled study. Unpublished manuscript. ; Vigano C, Bielli A, Carozzi A, Divino T, Pagliarulo E, Ba G. Panic disorder: A two‐year follow‐up of an integrated treatment approach. [Il disturbo di panico: follow up a due anni di un modello di trattamento integrato]. Italian Journal of Psychopathology in press.
- Chambless DL, Foa EB, Groves GA, Goldstein AJ. Exposure and communications training in the treatment of agoraphobia. Behavior Research and Therapy 1982;20:219‐31. [DOI] [PubMed] [Google Scholar]; Chambless DL, Foa EB, Groves GA, Goldstein AJ. Flooding with Brevital in the treatment of agoraphobia: countereffective?. Behavior Research and Therapy 1979;17(3):243‐51. [DOI] [PubMed] [Google Scholar]
- Cox DJ, Ballanger JC, Laraia M, Hobbs WR, Peterson GA, Hucek A. Different rates of improvement of different symptoms in combined pharmacological and behavioral treatment of agoraphobia. Journal of Behavior Therapy and Experimental Psychiatry 1988;19(2):119‐26. [DOI] [PubMed] [Google Scholar]
- Lipsedge, MS, Hajioff, J, Huggins, P, Napier, L, Pearce, J, Pike, et al. The management of severe agoraphobia: a comparison of ipronizaid and systematic desensitization. Psychopharmacologia 1973;32(1):67‐80. [DOI] [PubMed] [Google Scholar]
- Solyom, C, Solyom, L, LaPierre, Y, Pecknold, J, Morton, L. Phenelzine and exposure in the treatment of phobias. Biological Psychiatry 1981;16(3):239‐47. [PubMed] [Google Scholar]
Additional references
- American Psychiatric Association. Practice guideline for the treatment of patients with panic disorder. American Journal of Psychiatry 1998;155 Supplement:1‐34. [PubMed] [Google Scholar]
- Brown, TA, Barlow, DH. Long‐term outcome in cognitive‐behavioral treatment of panic disorder: clinical predictors and alternative strategies for assessment. Journal of Consulting and Clinical Psychology 1995;63:754‐65. [DOI] [PubMed] [Google Scholar]
- Bucher HC, Guyatt GH, Griffith LE, Walter SD. The results of direct and indirect treatment comparisons in meta‐analysis of randomized controlled trials. Journal of Clinical Epidemiology 1997;50(6):683‐91. [DOI] [PubMed] [Google Scholar]
- Burns, LE, Thorpe, CL, Cavallaro, LA. Agoraphobia 8 years after behavioral treatment: a follow‐up study with interview, self‐report, and behavioral data. Behavior Therapy 1986;17:580‐91. [Google Scholar]
- Carlbring, P, Gustafsson, H, Ekselius, L, Andersson, G. 12‐month prevalence of panic disorder with or without agoraphobia in the Swedish general population. Social Psychiatry and Psychiatric Epidemiology 2002;37:207‐11. [DOI] [PubMed] [Google Scholar]
- Chalmers TC, Celano P, Sacks HS, Smith H Jr. Bias in treatment assignment in controlled clinical trials. New England Journal of Medicine 1983;309:1358‐61. [DOI] [PubMed] [Google Scholar]
- Calrk DB, Taylor CB, Roth WT, Hayward C, Ahlers A, Margraf J, et al. Surreptitious drug use by patients in a panic disorder study. American Journal of Psychiatry 1990;147:507‐9. [DOI] [PubMed] [Google Scholar]
- Clum GA, Clum GA, Surls R. A meta‐analysis of treatments for panic disorder. Journal of Consulting and Clinical Psychology 1993;61:317‐26. [DOI] [PubMed] [Google Scholar]
- Coldiz, GA, Miller, JN, Mosteller, F. How study design affects outcomes in comparisons of therapy. I: medical. Statistics in Medicine 1989;9:441‐54. [DOI] [PubMed] [Google Scholar]
- Egger M, Juni P, Bartlett C, Holenstein F, Sterne J. How important are comprehensive literature searches and the assessment of trial quality in systematic reviews? Empirical study. Health Technology Assessment 2003;7(1):1‐76. [PubMed] [Google Scholar]
- Fava, GA, Rafanelli, C, Grandi, S, Conti, S, Ruini, C, Mangelli, L, et al. Long‐term outcome of panic disorder with agoraphobia treated by exposure. Psychological Medicine 2001;31:891‐8. [DOI] [PubMed] [Google Scholar]
- Foa EB, Franklin ME, Moser J. Context in the clinic: How well do cognitive‐behavioral therapies and medications work in combination?. Biological Psychiatry 2002;52:987‐97. [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Guyatt GH, Grifitth LE. Can we individualize the Number Needed to Treat (NNT)? An empirical study of summary effect measures in meta‐analyses. International Journal of Epidemiology 2002;31:72‐6. [DOI] [PubMed] [Google Scholar]
- Furukawa T, Cipriani A, Barbui C, Brambilla P, Watanabe N. Imputing response rates from means and standard deviations in meta‐analysis. International Clinical Psychopharmacology 2005;20(1):49‐52. [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Barbui C, Cipriani A, Brambilla P, Watanabe N. Imputing missing standard deviations in meta‐analyses can provide accurate results. Journal of Clinical Epidemiology 2006;59:7‐10. [DOI] [PubMed] [Google Scholar]
- Goisman RM, Warshaw MG, Steketee GS, Fierman EJ, Rogers MP, Goldenberg I, et al. DSM‐IV and the disappearnace of agoraphobia without history of panic disorder: new data on a controversial diagnosis. American Journal of Psychiatry 1995;152:1438‐43. [DOI] [PubMed] [Google Scholar]
- Gould RA, Otto MW, Pollack MH. A meta‐analysis of treatment outcome for panic disorder. Clinical Psychology Review 1995;15:819‐44. [Google Scholar]
- Higgins, JP, Thompson, SG, Deeks, JJ, Altman, DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollon, SD, DeRubeis, RJ. Placebo‐psychotherapy combinations: inappropriate representations of psychotherapy in drug‐psychotherapy comparative trials. Psychological Bulletin 1981;90:467‐77. [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Jin R, Ruscio AM, Shear K, Walters EE. The epidemiology of panic attacks, panic disorder, and agoraphobia in the National Comorbidity Survey Replication. Archives of General Psychiatry 2006;63:415‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DF. Flawed meta‐analyses comparing psychotherapy with pharmacotherapy. American Journal of Psychiatry 2000;157:1204‐11. [DOI] [PubMed] [Google Scholar]
- Marshall M, Lockwood A, Bradley C, Adams C, Joy C, Fenton M. Unpublished rating scales: a major source of bias in randomised controlled trials of treatments for schizophrenia. British Journal of Psychiatry 2000;176:249‐52. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Andrews G, Hadzi‐Pavlovic D, Christensen H. Treatment of panic and agoraphobia: an integrative review. Journal of Nervous and Mental Disease 1990;178:567‐76. [DOI] [PubMed] [Google Scholar]
- Mavissakalian M. Combined behavioral therapy and pharmacotherapy of agoraphobia. Journal of Psychiatric Research 1993;27 Suppl 1:179‐91. [DOI] [PubMed] [Google Scholar]
- Mavissakalian MR, Perel JM. Duration of imipramine therapy and relapse in panic disorder with agoraphobia. Journal of Clinical Psychopharmacology 2002;22:294‐9. [DOI] [PubMed] [Google Scholar]
- Moher D, Pham B, Jones A, Cook DJ, Jadad AR, Moher M, et al. Does quality of reports of randomised trials affect estimates of intervention efficacy reported in meta‐analyses?. Lancet 1998;352:609‐13. [DOI] [PubMed] [Google Scholar]
- Nathan PE, Gorman JM. A Guide to Treatments that Work. 2nd Edition. Oxford: Oxford University Press, 2002. [Google Scholar]
- Otto MW, Pollack MH, Sabatino SA. Maintenance of remission following cognitive behavior therapy for panic disorder: possible deleterious effects of concurrent medication treatment. Behavior Therapy 1996;27:473‐82. [Google Scholar]
- Otto MW, Pollack MH, Maki KM. Empirically supported treatments for panic disorder: costs, benefits, and stepped care. Journal of Consulting and Clinical Psychology 2000;68:556‐63. [PubMed] [Google Scholar]
- Oxman AD, Guyatt GH. A consumer's guide to subgroup analyses. Annals of Internal Medicine 1992;116:78‐84. [DOI] [PubMed] [Google Scholar]
- Pecknold JC, Swinson RP, Kuch K, Lewis CP. Alprazolam in panic disorder and agoraphobia: results from a multicenter trial. III. Discontinuation effects. Archives of General Psychiatry 1988;45:429‐36. [DOI] [PubMed] [Google Scholar]
- Pollack MH, Allgulander C, Bandelow B, Cassano GB, Greist JH, Hollander E, et al. WCA recommendations for the long‐term treatment of panic disorder. CNS Spectrums 2003;8:17‐30. [DOI] [PubMed] [Google Scholar]
- Schmidt NB. Panic disorder: cognitive behavioral and pharmacological treatment strategies. Journal of Clinical Psychology in Medical Settings 1999;6:89‐111. [Google Scholar]
- Schmidt NB, Koselka M, Woolaway‐Bickel K. Combined treatments for phobic anxiety disorders. In: Sammons, MT, Schmidt, NB editor(s). Combined Treatments for Mental Disorders: A Guide to Psychological and Pharmacological Interventions. Washington, DC: American Psychological Association, 2001:81‐110. [Google Scholar]
- Schulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias: dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA 1995;273:408‐12. [DOI] [PubMed] [Google Scholar]
- Simon NM, Safren SA, Otto MW, Sharma SG, Lanka GD, Pollack MH. Longitudinal outcome with pharmacotherapy in a naturalistic study of panic disorder. Journal of Affective Disorders 2002;69:201‐8. [DOI] [PubMed] [Google Scholar]
- Song F, Altman DG, Glenny AM, Deeks JJ. Validity of indirect comparison for estimating efficacy of competing interventions: empirical evidence from published meta‐analyses. BMJ 2003;326(7387):472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S. Understanding and Treating Panic Disorder. Chichester: John Wiley & Sons, 2000. [Google Scholar]
- Telch MJ, Lucas R. A. Combined pharmacological and psychological tretment of panic disorder: Current status and future directions.. In: Wolfe BE, Maser JD editor(s). Treatment of Panic Disorder: A Consensus Development Conference. Washington, DC: American Psychiatric Press, Inc., 1994:177‐97. [Google Scholar]
- Toni, C, Perugi, G, Frare, F, Mata, B, Vitale, B, Mengali, F, et al. A prospective naturalistic study of 326 panic‐agoraphobic patients treated with antidepressants. Pharmacopsychiatry 2000;33:121‐31. [DOI] [PubMed] [Google Scholar]
- Balkom AJ, Beurs E, Koele P, Lange A, Dyck R. Long‐term benzodiazepine use is associated with smaller treatment gain in panic disorder with agoraphobia. Journal of Nervous and Mental Disease 1996;184(2):133‐5. [DOI] [PubMed] [Google Scholar]
- Balkom AJ, Bakker A, Spinhoven P, Blaauw BM, Smeenk S, Ruesink B. A meta‐analysis of the treatment of panic disorder with or without agoraphobia: a comparison of psychopharmacological, cognitive‐behavioral, and combination treatments. Journal of Nervous and Mental Disease 1997;185:510‐6. [DOI] [PubMed] [Google Scholar]
- Watanabe N, Churchill R, Furukawa TA. Combined psychotherapy plus benzodiazepines for panic disorder with or without agoraphobia [Protocol]. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, et al. The cross‐national epidemiology of panic disorder. Archives of General Psychiatry 1997;54:305‐9. [DOI] [PubMed] [Google Scholar]
- Westra HA, Stewart SH. Cognitive behavioural therapy and pharmacotherapy: complementary or contradictory approaches to the treatment of anxiety?. Clinical Psychology Review 1998;18(3):307‐40. [DOI] [PubMed] [Google Scholar]
- World Health Report 2004. WHO.


