Abstract
Background
Pyelonephritis is a type of urinary tract infection (UTI) that affects the upper urinary tract and kidneys, and is one of the most common conditions for hospitalisation among pregnant women, aside from delivery. Samples of urine and blood are obtained and used for cultures as part of the diagnosis and management of the condition. Acute pyelonephritis requires hospitalisation with intravenous administration of antimicrobial agents. Several studies have questioned the necessity of obtaining blood cultures in addition to urine cultures, citing cost and questioning whether blood testing is superfluous. Pregnant women with bacteraemia require a change in the initial empirical treatment based on the blood culture. However, these cases are not common, and represent approximately 15% to 20% of cases. It is unclear whether blood cultures are essential for the effective management of the condition.
Objectives
To assess the effectiveness of routine blood cultures to improve health outcomes in the management of pyelonephritis in pregnant women.
Search methods
We searched the Cochrane Pregnancy and Childbirth Group's Trials Register without language or date restrictions (31 December 2014).
Selection criteria
Randomised controlled trials and quasi‐randomised trials comparing outcomes among pregnant women with pyelonephritis who received initial management with or without blood cultures. Cluster‐randomised trials were eligible for inclusion in this review but none were identified. Clinical trials using a cross‐over design were not eligible for inclusion.
Data collection and analysis
Two review authors independently assessed one trial report for inclusion.
Main results
We identified one trial report but this was excluded. No clinical trials met the inclusion criteria for this review.
Authors' conclusions
There are no large‐scale randomised controlled trials to assess outcomes in the management of pyelonephritis in pregnancy with or without blood cultures. Randomised controlled trials are needed to evaluate the effectiveness of managing pyelonephritis in pregnant women with or without blood cultures, and to assess any adverse outcomes as well as the cost‐effectiveness of excluding blood cultures from treatment.
Keywords: Adult; Female; Humans; Pregnancy; Microbiological Techniques; Pregnancy Complications, Infectious; Pregnancy Complications, Infectious/blood; Pregnancy Complications, Infectious/therapy; Pyelonephritis; Pyelonephritis/blood
Plain language summary
The effectiveness of blood testing in the management of pyelonephritis in pregnancy for improving outcomes
Urinary tract infections (UTIs) are a common infection among women, with most women having developed a UTI at least once in their lifetime. Pyelonephritis, a UTI which affects the upper urinary tract and kidneys, is one of the most prevalent conditions that require hospitalisation among pregnant women. In general, both urine and blood samples are taken for diagnosis and to tailor the necessary antibiotic therapy to the needs of the patient. Some severe cases of pyelonephritis require hospitalisation and intravenous administration of antibiotics. Several previous studies have reported that excluding blood testing or 'blood culture' samples and using only urine samples in managing the condition could be as safe and effective as the current approach, in which both urine and blood samples are analysed. Previous research has also suggested that urine samples render blood samples superfluous, as blood samples offer no additional clinical value for the management of pyelonephritis. Testing only urine samples could also be significantly cost‐saving.
This review aims to evaluate the effectiveness of routine blood cultures in the management of pyelonephritis in pregnancy. However, we did not identify any data from randomised controlled trials in order to examine the efficacy of routine blood cultures in the management of the condition among pregnant women. Further research is required to assess the effectiveness of managing pyelonephritis in pregnant women with or without blood culture samples, as well as to address possible adverse outcomes and the potential cost‐effectiveness of excluding blood cultures from treatment.
Background
Description of the condition
Pyelonephritis in pregnancy
Urinary tract infections (UTIs) are more common in women during pregnancy (Cunningham 2009; Nicolle 2005). The two main types of UTI are cystitis (a bladder infection in the lower urinary tract) and pyelonephritis (a kidney infection in the upper urinary tract). In pregnancy, anatomical and physiological changes occur in the urinary tract, such as dilation of the renal pelvis and ureter, displacement of the bladder, and mechanical compression of the ureters by the uterus, which increase the risk of developing a UTI (Shanarr 2008). A reversed flow of urine into the upper urinary tract can lead to acute pyelonephritis, which affects the renal pelvis, calyces, and parenchyma. Symptoms include fever, nausea, vomiting, or flank pain with or without the cystitis symptoms of painful, frequent or urgent urination. Acute pyelonephritis is diagnosed by clinical findings of fever, flank pain, and costovertebral angle tenderness, and by laboratory findings of either bacteriuria or pyuria. This condition also causes some of the most serious complications among UTIs in pregnancy, including anaemia, septic shock and preterm labour and delivery (Cunningham 2009).
Incidence and risks of pyelonephritis in pregnancy
Acute pyelonephritis occurs in 1% to 2% of pregnancies (Cunningham 1973; Hill 2005) and the condition is the second most common reason for hospitalisation during pregnancy that is not related to delivery (Scott 1997). In addition, pyelonephritis is the leading cause of septic shock during pregnancy (Mabie 1997).
The incidence of asymptomatic bacteriuria varies from 2% to 7% in non‐pregnant women and during pregnancy (Nicolle 2005). Asymptomatic bacteriuria increases the risk of developing acute pyelonephritis by 20‐ to 30‐fold in pregnant women, compared to women without bacteriuria (Nicolle 2005). If asymptomatic bacteriuria is left untreated, approximately 25% of infected pregnant women will develop symptomatic UTIs including pyelonephritis (Cunningham 2009).
Among pregnant women with pyelonephritis, approximately 10% to 20% were found to have concurrent bacteraemia. In recent studies, 15% (21 of 137 cases) (MacMillan 1991), 9% (35 of 388 cases) (Wing 2000), and 17% (30 of 172 cases) (Hill 2005) were reported to have positive blood cultures with acute pyelonephritis in pregnancy.
Adverse maternal and fetal outcomes of UTIs during pregnancy
It has been reported that pregnant women with acute pyelonephritis are more likely to have premature delivery and a low birthweight infant (Lang 1996; Millar 2003; Wing 2014). However, pregnant women with asymptomatic bacteriuria seemed to be more likely to have premature delivery and a low birthweight infant. Recommendations have been made to treat all pregnant women with asymptomatic bacteriuria (Nicolle 2005; Smaill 2007), although in recent years the relationship between asymptomatic bacteriuria and preterm delivery is not clear (Wing 2014). Jacobsson 2002 has indicated that urosepsis may be related to an increased incidence of cerebral palsy among preterm infants.
Description of the intervention
The general approach to treating pregnant women with acute pyelonephritis includes hospitalisation, obtaining urine and blood samples for cultures and the administration of intravenous antimicrobial agents (Cunningham 2009; MacMillan 1991). Previous randomised studies have shown that ampicillin, gentamicin, cefazolin, or ceftriaxone were effective as empirical therapy for this condition (Sanchez‐Ramos 1995; Wing 2000). If women are unresponsive to initial antimicrobial therapy, appropriate alternative therapies are designed based on the susceptibility testing results of urine and blood cultures. Recent studies, however, have reported limited usefulness of urine and blood cultures. MacMillan 1991 and Wing 2000 demonstrated that the management of pyelonephritis in pregnancy by using only pretreatment urine cultures without blood cultures may be safe and effective without compromising women's care. It was argued that since organisms isolated from blood cultures seldom varied from the urine isolates (5/388, 1.29%), these discrepancies were caused by contamination from skin flora (Wing 2000). Blood samples do not offer any additional information to change the management of the condition. In these studies, most changes in antimicrobial therapy were made on the basis of clinical response rather than susceptibility test results. Only a few cases required a change in therapy after blood culture results were confirmed.
From a practical standpoint, there are three different strategies to manage pyelonephritis during pregnancy (Wing 2000). The first approach is to base treatment on both urine and blood cultures. The second is to treat patients based on urine cultures only, and the third option is to perform both urine and blood cultures for low‐risk patients only if a clinical response is not observed within 48 hours.
From an economic point of view, Wing 2000 estimated that in 1999, If the cost of a blood culture with aerobic and anaerobic sensitivity tests changed to approximately $150, a total saving of $15 million would be made annually in the United States if only urine cultures, not blood cultures, were obtained from pregnant women with pyelonephritis. Further, in general, urine cultures are cheaper than blood cultures. If only one type of specimen is required to identify causative organisms and susceptibility, urine testing would be the most cost‐effective choice.
How the intervention might work
Blood cultures determine the presence of bacteraemia and are particularly useful in patients with risk factors for endocarditis (MacMillan 1991) and complicated pyelonephritis, such as diabetes, immunosuppression, urolithiasis, urologic, anatomic or functional abnormalities, and renal diseases. They may optimise antimicrobial therapy with appropriate selection of agents and duration of therapy, as well as improve outcomes among pregnant women with pyelonephritis. Blood cultures may also provide a more cost‐effective approach for managing the condition by guiding antimicrobial therapy and detecting serious complications due to bacteraemia, compared with urine samples alone.
Why it is important to do this review
Medical costs overall have increased in most countries. If blood cultures are excluded from the routine management of pyelonephritis in pregnant women, the potential financial savings would be enormous. It is also useful to determine the factors which lead to performing blood cultures in addition to urine cultures from pregnant women with pyelonephritis. Moreover, there are many resource‐limited countries where routine blood cultures may not be available to pregnant women (Islam 2009; Kongnyuy 2009). Increasing antimicrobial resistance among Enterobacteriaceae, such as Escherichia coli, is also of growing global concern (Al‐Hasan 2009; Al‐Hasan 2010; EARSS 2008; Hsueh 2010; Masinde 2009). It is therefore important to compare the outcomes among patients with pyelonephritis in pregnancy who are treated with or without blood cultures in addition to urine cultures. It also makes a significant impact on daily clinical practice to optimise therapy for pregnant women with pyelonephritis by using the most safe, effective and cost‐conscious approach.
Objectives
To assess the effectiveness of routine blood cultures for improving health outcomes in the management of pyelonephritis in pregnant women.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (including those using a cluster‐randomised design and quasi‐randomised trials) comparing outcomes among pregnant women with pyelonephritis who received initial management with or without blood cultures. Trials using a cross‐over design were not eligible for inclusion.
Types of participants
Pregnant women who develop pyelonephritis during the antepartum period.
Types of interventions
Management of pyelonephritis among pregnant women with or without routine blood cultures in addition to urine cultures.
Types of outcome measures
Primary outcomes
Maternal sepsis
Perinatal or neonatal mortality
Secondary outcomes
Maternal outcomes
Maternal mortality
Preterm delivery
Clinical and microbiological cure defined as resolution of symptoms and elimination of bacteriuria
Neonatal outcomes
Incidence of low birthweight
Treatment failure
We considered the following secondary outcomes in this area. If the included studies already featured predefined categories, we planned to use these. Otherwise we developed the following categories.
Delay of improving symptoms (fever, flank pain, costophrenic angle tenderness) within 48 hours
Persistent positive urine culture after 48 hours of treatment
Recurrent pyelonephritis; early recurrence defined as pyelonephritis due to the same strain or different strain within two weeks after treatment, and late recurrence defined as pyelonephritis due to the same strain or different strain after two weeks of treatment
Asymptomatic bacteriuria during pregnancy at any point after treatment
Progression to renal dysfunction during or after treatment
Health service indicators
Cutting costs in managing the condition by performing only urine cultures, instead of performing both urine cultures and blood cultures.
Search methods for identification of studies
The following methods section of this review is based on a standard template used by the Cochrane Pregnancy and Childbirth Group.
Electronic searches
We searched the Cochrane Pregnancy and Childbirth Group’s Trials Register by contacting the Trials Search Co‐ordinator (31 December 2014).
The Cochrane Pregnancy and Childbirth Group’s Trials Register is maintained by the Trials Search Co‐ordinator and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Details of the search strategies for CENTRAL, MEDLINE and Embase, the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service can be found in the ‘Specialized Register’ section within the editorial information about the Cochrane Pregnancy and Childbirth Group.
We did not apply any language or date restrictions.
Data collection and analysis
Selection of studies
Two review authors, H Gomi and Y Goto, independently assessed for inclusion the one potential study we identified as a result of the search strategy. We resolved any disagreements through discussion.
There are no included studies in this review. Full methods of data collection and analysis to be used in future data updates of this review are provided in Appendix 1.
Results
Description of studies
Results of the search
The search of the Cochrane Pregnancy and Childbirth Group's Trials Register retrieved one trial report (Dozier 1997), which we subsequently excluded. See Figure 1.
1.
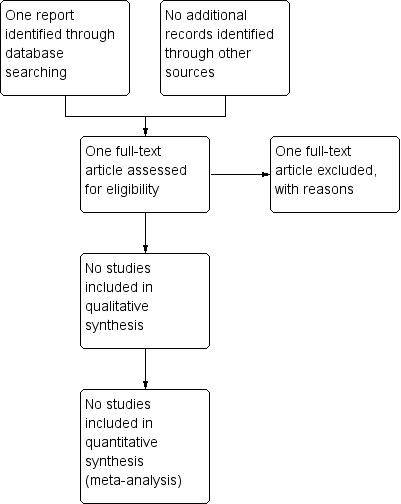
Study flow diagram.
Excluded studies
We excluded one trial (Dozier 1997) reported in abstract form. We contacted the authors for further detailed information, but did not receive a reply.
Risk of bias in included studies
There are no included studies for this review.
Effects of interventions
There are no included studies for this review.
Discussion
At present, there is no supporting evidence from randomised controlled trials to evaluate whether routine blood cultures improve outcomes in the management of pyelonephritis in pregnancy.
Previous research has questioned the utility of blood cultures in the management of pyelonephritis in pregnant women highlighting that most women have been treated successfully without the need for culture reports and susceptibility testing (Nicolle 2005). For example, only two women's blood culture isolates (1.3%) differed from their corresponding urine culture isolates (Wing 2000), and only five pregnant women with acute pyelonephritis (1.3%), had blood cultures with pathogens that differed from those found in the urine (Chen 2006). Treatment decisions to change initial antibiotic regimens were more affected by clinical course than by culture results.The exclusion of blood cultures has also been considered in clinical practice in the management of other conditions such as pneumonia (Benenson 2007; Cham 2009) or intra‐abdominal infections (Solomkin 2010). In addition, the use of more rapid identification methods that incorporate molecular technologies, such as polymerase chain reaction testing, have been performed in the emergency treatment of patients with bacteraemia (Stoneking 2013). This retrospective study indicated that the rapid molecular method was significantly more useful in providing accurate antimicrobial therapy than were guidelines or protocols by academic associations such as the Infectious Diseases Society of America.
The most common pathogen among women with pyelonephritis in pregnancy is E. coli. In general, gram‐negative Enterobacteriaceae are less likely to cause infective endocarditis than gram‐positive cocci, which is one of the most significant complications of bacteraemia (Chen 2006). In future it is important to re‐assess the value of obtaining blood cultures and documenting the existence of bloodstream infections in clinical practice.
A blood culture is relatively easy and less invasive than other diagnostic procedures such as tissue biopsy to perform and has the capability to determine causative organisms. On the one hand, when blood cultures are performed, the organisms from blood — which is sterile — are in general the targets for antimicrobial treatment, and are not usually considered as 'contaminants'. On the other hand, when other specimens such as urine, sputum, or pus are available, and depending on which organisms are being sought, there may be no additional clinical value in obtaining blood cultures. It is also argued that urine cultures provide sufficient information with which to adjust antimicrobial therapy when required (Nicolle 2005).
If blood cultures can be excluded without compromising the quality of women's care in conditions such as uncomplicated pyelonephritis in pregnancy, significant cost savings could be made. This implies more practical and affordable management for resource‐limited areas where blood cultures may not always be available, and a reduction in the high costs associated with blood cultures for developed countries where overall medical costs are on the rise.
Authors' conclusions
Implications for practice.
There are no randomised controlled trials to assess outcomes in the management of pyelonephritis in pregnancy with or without blood cultures. If management of the condition using both blood and urine cultures does not change the outcomes of pyelonephritis in pregnancy, blood cultures could be safely excluded. This approach could save considerable costs and streamline management of the condition.
Implications for research.
Randomised controlled trials are needed to evaluate outcomes of managing pyelonephritis in pregnant women with or without blood cultures. It is important to investigate outcomes related to treatment or hospital duration, and to assess whether additional blood cultures provide additional information which helps to shorten antibiotic treatment or admission duration. It is also important to assess any compromises made or adverse outcomes in managing the condition without blood cultures, the frequency of such adverse outcomes, and the overall cost‐effectiveness of excluding blood cultures from treatment. Further randomised controlled trials are justified. Since only a few women with acute pyelonephritis require a prompt change in the initial antibiotic treatment based on the blood culture, the indication for taking blood cultures is for those women with suspected bacteraemia and sepsis. There is no need to take blood cultures routinely.
Acknowledgements
We thank Professor Pisake Lumbiganon for his valuable advice on methodological and clinical perspectives, and Emma Barber for English language editing.
As part of the pre‐publication editorial process, this review has been commented on by four peers (an editor and three referees who are external to the editorial team) and the Group's Statistical Adviser.
Appendices
Appendix 1. Full methods of data collection and analysis for future use
Data extraction and management
We will design a form to extract data. For eligible studies, two review authors will extract the data using the agreed form. We will resolve discrepancies through discussion or, if required, we will consult an additional review author. We will enter data into Review Manager software (RevMan 2014) and will check for accuracy.
When information regarding any of the above is unclear, we will attempt to contact authors of the original reports to provide further details.
Assessment of risk of bias in included studies
Two review authors will independently assess risk of bias for the study identified using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We will resolve any disagreement by discussion or by involving an additional assessor.
(1) Sequence generation (checking for possible selection bias)
We will describe for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We will assess the method as:
low risk (any truly random process, e.g. random number table; computer random number generator);
high risk (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear.
(2) Allocation concealment (checking for possible selection bias)
We will describe for each included study the method used to conceal the allocation sequence and determine whether intervention allocation could have been foreseen in advance of or during recruitment, or changed after assignment.
We will assess the methods as:
low risk (e.g. telephone or central randomisation; consecutively numbered sealed opaque envelopes);
high risk (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We will describe for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We will consider that studies are at low risk of bias if they were blinded, or if we judge that the lack of blinding would be unlikely to affect results. We will assess blinding separately for different outcomes or classes of outcomes.
We will assess the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We will describe for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We will assess blinding separately for different outcomes or classes of outcomes.
We will assess methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias through withdrawals, dropouts, protocol deviations)
We will describe for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We will state whether attrition and exclusions are reported, the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data are balanced across groups or are related to outcomes. Where sufficient information is reported, or could have been supplied by the trial authors, we will re‐include missing data in the analyses which we will undertake. We will assess methods as:
low risk; loss to follow‐up less than 10%;
high risk; loss to follow‐up 10% or more;
unclear.
We will consider the data from a trial adequate if missing data constitute less than or equal to 20% of the trial data. We will resolve discrepancies by discussion.
(5) Selective reporting bias
We will describe for each included study how we investigate the possibility of selective outcome reporting bias and what we find.
We will assess the methods as:
adequate (where it is clear that all of the study's pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
inadequate (where not all the study's pre‐specified outcomes have been reported; one or more reported primary outcomes are not pre‐specified; outcomes of interest are reported incompletely and so cannot be used; study fails to include results of a key outcome that would be expected to be reported);
unclear.
(6) Other sources of bias
We will describe for each included study any important concerns we have about other possible sources of bias.
We will assess whether each study is free of other problems that could put it at risk of bias:
yes;
no;
unclear.
(7) Overall risk of bias
We will make explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Handbook (Higgins 2011). With reference to (1) to (6) above, we will assess the likely magnitude and direction of the bias and whether we will consider it is likely to impact on the findings. We will explore the impact of the high risk of bias through undertaking sensitivity analyses ‐ seeSensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, such as maternal mortality, we will present results as summary risk ratio with 95% confidence intervals.
Continuous data
For continuous data, such as length of hospital stay, we will use the mean difference if outcomes are measured in the same way between trials. We will use the standardised mean difference to combine trials that measure the same outcome, but use different methods.
Unit of analysis issues
Cluster‐randomised trials
We will include cluster‐randomised trials (CRTs) in the analyses along with individually‐randomised trials. If we have unadjusted treatment effect of the CRT, we will adjust the standard error of the treatment effect as suggested in the Handbook (Higgins 2011) using an estimate of the intracluster correlation co‐efficient (ICC) derived from the information available in the trial (if possible), from a similar trial or from a study of a similar population. If we use ICCs from other sources, we will report this and conduct sensitivity analyses to investigate the effect of variation in the ICC. If we identify both cluster‐randomised trials and individually‐randomised trials, we will synthesise the relevant information. We will consider it reasonable to combine the results from both if there is little heterogeneity between the study designs and the interaction between the effect of intervention and the choice of randomisation unit is considered to be unlikely.
We will also acknowledge heterogeneity in the randomisation unit and we will perform a sensitivity analysis to investigate the effects of the randomisation unit.
Dealing with missing data
For included studies, we will note levels of attrition. We will explore the impact of including studies with high levels of missing data in the overall assessment of treatment effect by using sensitivity analysis.
For all outcomes, we will carry out analyses, as far as possible, on an intention‐to‐treat basis, i.e. we will attempt to include all participants randomised to each group in the analyses, and analyse all participants in the group to which they have been allocated, regardless of whether or not they received the allocated intervention. The denominator for each outcome in each trial will be the number randomised minus any participants whose outcomes are known to be missing.
Assessment of heterogeneity
We will assess statistical heterogeneity in each meta‐analysis using the T², I² and Chi² statistics. We will regard heterogeneity as substantial if an I² is greater than 30% and either a T² is greater than zero, or there is a low P value (less than 0.10) in the Chi² test for heterogeneity.
Assessment of reporting biases
If there are 10 or more studies in the meta‐analysis, we will investigate reporting biases (such as publication bias) using funnel plots. We will assess funnel plot asymmetry visually. If asymmetry is suggested by a visual assessment, we will perform exploratory analyses to investigate it.
Data synthesis
We will carry out statistical analysis using the Review Manager software (RevMan 2014). We will use fixed‐effect meta‐analysis for combining data where it is reasonable to assume that studies are estimating the same underlying treatment effect: i.e. where trials are examining the same intervention, and the trials’ populations and methods are judged sufficiently similar. If there is clinical heterogeneity sufficient to expect that the underlying treatment effects differ between trials, or if substantial statistical heterogeneity is detected, we will use random‐effects meta‐analysis to produce an overall summary if an average treatment effect across trials is considered clinically meaningful. We will treat the random‐effects summary as the average range of possible treatment effects and we will discuss the clinical implications of treatment effects differing between trials. If the average treatment effect is not clinically meaningful, we will not combine trials.
If we use random‐effects analyses, we will present the results as the average treatment effect with its 95% confidence interval, and the estimates of T² and I².
Subgroup analysis and investigation of heterogeneity
If we identify substantial heterogeneity, we will investigate it using subgroup analyses and sensitivity analyses. We will consider whether an overall summary is meaningful, and if it is, used random‐effects analysis to produce it.
We plan to carry out the following subgroup analyses for maternal sepsis.
Women with uncomplicated pyelonephritis versus those with risk factors for complicated pyelonephritis such as diabetes, immunosuppression, urolithiasis, urologic, anatomic or functional abnormalities, and renal diseases.
Women in developed countries versus those in resource‐limited countries.
Women in a setting with a high prevalence of antimicrobial resistance versus those in a area of low prevalence.
We will assess subgroup differences by interaction tests available within RevMan (RevMan 2014). We will report the results of subgroup analyses quoting the χ2 statistic and P value, and the interaction test I² value.
Sensitivity analysis
If identify substantial heterogeneity we will carry out sensitivity analysis to explore the effects of high risk of bias for each of the risk of bias domains to examine the impact on the estimated pooled effect. We will also examine the effect of the randomisation unit (where cluster‐trials are included along with the individually‐randomised trials). We will use maternal sepsis as the outcome for this analysis.
Characteristics of studies
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Dozier 1997 | This study was reported as an abstract only and no further detailed information was available. We attempted to contact the study authors, but we did not receive a reply. |
Differences between protocol and review
We have edited our methods 'sensivity analysis' to clarify our planned sensitivity analyses in future updates of this review.
Contributions of authors
H Gomi prepared the draft of this review. H Gomi and Y Goto independently assessed the one identified trial report. R Mori, M Laopaiboon and Y Goto contributed to the writing of this review. R Usui commented on the review. All the authors approved the final version of the review.
Sources of support
Internal sources
Jichi Medical University, Japan.
External sources
-
Ministry of Health, Labour and Welfare of Japan, Japan.
Health Labour Sciences Research Grant
Declarations of interest
None known.
New
References
References to studies excluded from this review
Dozier 1997 {published data only}
- Dozier B, Nathan L. A prospective evaluation of the utility of blood cultures in treating antepartum pyelonephritis. American Journal of Obstetrics and Gynecology 1997;176(1 Pt 2):S24. [Google Scholar]
Additional references
Al‐Hasan 2009
- Al‐Hasan MN, Lahr BD, Eckel‐Passow JE, Baddour LM. Antimicrobial resistance trends of Escherichia coli bloodstream isolates: a population‐based study, 1998–2007. Journal of Antimicrobial Chemotherapy 2009;64:169‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Al‐Hasan 2010
- Al‐Hasan MN, Eckel‐Passow JE, Baddour LM. Bacteremia complicating gram‐negative urinary tract infections: a population‐based study. Journal of Infection 2010;60:278‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Benenson 2007
- Benenson RS, Kepner AM, Pyle DN 2nd, Cavanaugh S. Selective use of blood cultures in emergency department pneumonia patients. Journal of Emergency Medicine 2007;33(1):1‐8. [DOI] [PubMed] [Google Scholar]
Cham 2009
- Cham G, Yan S, Hoon HB, Seow E. Predicting positive blood cultures in patients presenting with pneumonia at an emergency department in Singapore. Annals of Academic Medicine in Singapore 2009;38:508‐14. [PubMed] [Google Scholar]
Chen 2006
- Chen Y, Nitzan O, Saliba W, Chazan B, Colodner R, Raz R. Are blood cultures necessary in the management of women with complicated pyelonephritis?. Journal of Infection 2006;53(4):235‐40. [PUBMED: 16434102] [DOI] [PubMed] [Google Scholar]
Cunningham 1973
- Cunningham FG, Morris GB, Mickal A. Acute pyelonephritis of pregnancy: a clinical review. Obstetrics & Gynecology 1973;42:112‐7. [PubMed] [Google Scholar]
Cunningham 2009
- Cunningham FG, Leveno KJ, Bloom SL, Hauth JC, Rouse DJ, Spong KY. Williams Obstetrics. McGraw‐Hill Professional, 2009. [Google Scholar]
EARSS 2008
- European Antimicrobial Resistance Surveillance System (EARSS). European Antimicrobial Resistance Surveillance System Annual Report 2008. EARSS, 2008. [Google Scholar]
Higgins 2011
- Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hill 2005
- Hill JB, Sheffield JS, McIntire DD, Wendel GD Jr. Acute pyelonephritis in pregnancy. Obstetrics & Gynecology 2005;105:18‐23. [DOI] [PubMed] [Google Scholar]
Hsueh 2010
- Hsueh PR, Badal RE, Hawser SP, Hoban DJ, Bouchillon SK, Ni Y, et al. Epidemiology and antimicrobial susceptibility profiles of aerobic and facultative Gram‐negative bacilli isolated from patients with intra‐abdominal infections in the Asia‐Pacific region: 2008 results from SMART (Study for Monitoring Antimicrobial Resistance Trends). International Journal of Antimicrobial Agents 2010;36:408‐14. [DOI] [PubMed] [Google Scholar]
Islam 2009
- Islam M, Yoshida S. Women are still deprived of access to lifesaving essential and emergency obstetric care. International Journal of Gynecology & Obstetrics 2009;106:120‐4. [DOI] [PubMed] [Google Scholar]
Jacobsson 2002
- Jacobsson B, Hagberg G, Hagberg B, Ladfors L, Niklasson A, Hagberg H. Cerebral palsy in preterm infants: a population‐based case‐control study of antenatal and intrapartal risk factors. Acta Paediatrica 2002;91:946‐51. [DOI] [PubMed] [Google Scholar]
Kongnyuy 2009
- Kongnyuy E, Hofman J, Mlava G, Mhango C, Broek N. Availability, utilisation and quality of basic and comprehensive emergency obstetric care services in Malawi. Maternal and Child Health Journal 2009;13:687‐94. [DOI] [PubMed] [Google Scholar]
Lang 1996
- Lang JM, Lieberman E, Cohen A. A comparison of risk factors for preterm labor and term small‐for‐gestation‐age birth. Epidemiology 1996;7:369‐76. [DOI] [PubMed] [Google Scholar]
Mabie 1997
- Mabie WC, Barton JR, Sibai B. Septic shock in pregnancy. Obstetrics & Gynecology 1997;90:553‐61. [DOI] [PubMed] [Google Scholar]
MacMillan 1991
- MacMillan MC, Grimes DA. The limited usefulness of urine and blood cultures in treating pyelonephritis in pregnancy. Obstetrics & Gynecology 1991;78:745‐8. [PubMed] [Google Scholar]
Masinde 2009
- Masinde A, Gumodoka B, Kilonzo A, Mshana SE. Prevalence of urinary tract infection among pregnant women at Bugando Medical Centre, Mwanza, Tanzania. Tanzanian Journal of Health Research 2009;11:154‐9. [DOI] [PubMed] [Google Scholar]
Millar 2003
- Millar LK, Debuque L, Wing DA. Uterine contraction frequency during treatment of pyelonephritis in pregnancy and subsequent risk of preterm birth. Journal of Perinatal Medicine 2003;31:41‐6. [DOI] [PubMed] [Google Scholar]
Nicolle 2005
- Nicolle LE, Bradley S, Colgan R, Rice JC, Schaeffer A, Hooton TM. Infectious Diseases Society of America guidelines for the diagnosis and treatment of asymptomatic bacteriuria in adults. Clinical Infectious Diseases 2005;40:643‐54. [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Sanchez‐Ramos 1995
- Sanchez‐Ramos L, McAlpine KJ, Adair CD, Kaunitz AM, Delke I, Briones DK. Pyelonephritis in pregnancy: once‐a‐day ceftriaxone versus multiple doses of cefazolin: a randomized, double‐blind trial. American Journal of Obstetrics and Gynecology 1995;172:129‐33. [DOI] [PubMed] [Google Scholar]
Scott 1997
- Scott CL, Chavez GF, Atrash HK, Taylor DJ, Shah RS, Rowley D. Hospitalizations for severe complications of pregnancy, 1987‐1992. Obstetrics & Gynecology 1997;90:225‐9. [DOI] [PubMed] [Google Scholar]
Shanarr 2008
- Shanarr J, Smaill F. Asymptomatic bacteriuria and symptomatic urinary tract infections in pregnancy. European Journal of Clinical Investigation 2008;38:50‐6. [DOI] [PubMed] [Google Scholar]
Smaill 2007
- Smaill F, Vaquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD000490.pub2] [DOI] [PubMed] [Google Scholar]
Solomkin 2010
- Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJC, Baron EJ, et al. Diagnosis and management of complicated intra‐abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Clinical Infectious Diseases 2010;50:133‐64. [DOI] [PubMed] [Google Scholar]
Stoneking 2013
- Stoneking LR, Patanwala AE, Winkler JP, Fiorello AB, Lee ES, Olson DP, et al. Would earlier microbe identification alter antibiotic therapy in bacteremic emergency department patients?. Journal of Emergency Medicine 2013;44:1‐8. [DOI] [PubMed] [Google Scholar]
Wing 2000
- Wing DA, Park AS, DeBuque L, Millar LK. Limited clinical utility of blood and urine cultures in the treatment of acute pyelonephritis during pregnancy. American Journal of Obstetrics and Gynecology 2000;182:1437‐40. [DOI] [PubMed] [Google Scholar]
Wing 2014
- Wing DA, Fassett MJ, Getahun D. Acute pyelonephritis in pregnancy: an 18‐year retrospective analysis. American Journal of Obstetrics and Gynecology 2014;210(3):219.e1‐219.e6. [PUBMED: 24100227] [DOI] [PubMed] [Google Scholar]


