Abstract
We reported previously that overexpression of heterogeneous nuclear ribonucleoprotein F (Hnrnpf) in renal proximal tubular cells (RPTCs) suppresses angiotensinogen (Agt) expression, and attenuates systemic hypertension and renal injury in diabetic Hnrnpf-transgenic (Tg) mice. We thus hypothesized that deletion of Hnrnpf in the renal proximal tubules (RPT) of mice would worsen systemic hypertension and kidney injury, perhaps revealing novel mechanism(s). Tubule-specific Hnrnpf knockout (KO) mice were generated by crossbreeding Pax8-Cre mice with floxed Hnrnpf mice on a C57BL/6 background. Both male and female KO mice exhibited elevated systolic blood pressure, increased urinary albumin/creatinine ratio, tubulo-interstitial fibrosis and glycosuria without changes in blood glucose or glomerular filtration rate compared with control littermates. However, glycosuria disappeared in male KO mice at the age of 12 weeks, while female KO mice had persistent glycosuria. Agt expression was elevated, whereas sodium-glucose co-transporter 2 (Sglt2) expression was down-regulated in RPTs of both male and female KO mice as compared to control littermates. In vitro, KO of HNRNPF in human RPTCs (HK-2) by CRISPR gRNA up-regulated AGT and down-regulated SGLT2 expression. The Sglt2 inhibitor canagliflozin treatment had no effect on Agt and Sglt2 expression in HK-2 and in RPTCs of wild-type mice but induced glycosuria. Our results demonstrate that Hnrnpf plays a role in the development of hypertension and glycosuria through modulation of renal Agt and Sglt2 expression in mice, respectively.
Subject terms: Molecular biology, Physiology, Systems biology, Zoology, Endocrinology, Nephrology
Introduction
The kidney contains all components of the renin-angiotensin system (RAS)1–4. Over-activation of the intrarenal RAS appears to be involved in various kidney diseases5–7. We and others have reported that overexpression of angiotensinogen (Agt, the sole precursor of all angiotensins) in RPTCs leads to systemic hypertension and kidney injury in transgenic (Tg) mice8–10, supporting the notion that enhanced intrarenal Agt expression and RAS activation play an important role in the development of hypertension and kidney injury.
Our lab has reported that heterogeneous nuclear ribonucleoprotein F (Hnrnpf) mediates insulin inhibition of Agt gene transcription through binding to the putative insulin-responsive element (IRE) in the rat Agt promoter11,12. We recently reported that overexpression of Hnrnpf in RPTCs suppresses Agt expression, and attenuates systemic hypertension and renal injury in male Akita (type 1 diabetic murine model) Hnrnpf-Tg mice13 and db/db (type 2 diabetic murine model) Hnrnpf-Tg mice14. Since sex differences may modulate the development of systolic blood pressure (SBP)15,16, we investigated whether Hnrnpf would affect intrarenal Agt expression in a sex-dependent manner. We generated tubule-specific Hnrnpf KO mice by employing the Pax8-Cre/lox system17 and monitored the development of phenotype in both male and female mice.
Here, we report that tubule-specific (Pax8) Hnrnpf KO leads to elevated SBP and kidney injury via up-regulation of Agt and down-regulation of Sglt2 expression in RPTCs in both sexes and also results in glycosuria in a sex-dependent manner. KO of HNRNPF by CRISPR gRNA confirmed the up-regulation and down-regulation of AGT and SGLT2 expression in human RPTCs (HK-2), respectively. Treatment with canagliflozin (an inhibitor of Sglt2) had no effect on Agt and Sglt2 expression in HK-2 and in RPTCs of wild-type mice, whereas it induced glycosuria.
Results
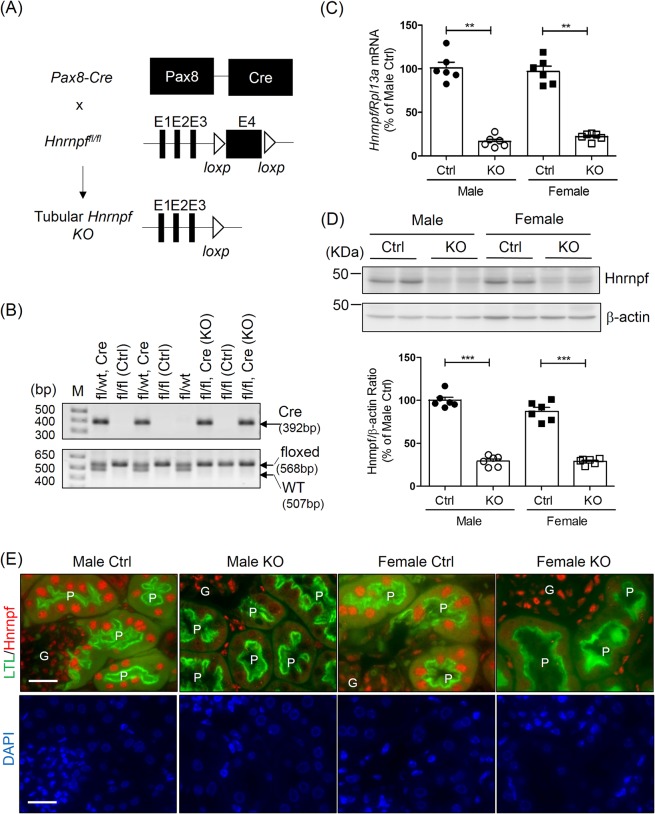
Generation of tubular Hnrnpf KO Mice
Renal tubular Hnrnpf KO mice were generated by using Pax8-Cre/lox recombination strategy (Fig. 1A). LoxP sites were inserted to flank exon 4 of mouse Hnrnpf gene (Gene ID: 98758) which is localized on chromosome 6. Heterozygous of Hnrnpf-floxed allele mice were generated by cross-breeding male Hnrnpf-floxed mice with female Pax8-Cre mice. These mice were further crossbred to generate homozygous Hnrnpf-floxed allele and carried the Cre allele. PCR analysis of genomic DNA extracted from ear punch tissues to distinguish the genotype of Cre (392 bp), floxed (568 bp) and WT (507 bp) is shown in Fig. 1B. RT-qPCR revealed Hnrnpf mRNA expression in RPTs freshly isolated from male and female Ctrl and KO mice at the age of 8 weeks (Supplemental Fig. 1a) and 24 weeks (Fig. 1C). Hnrnpf mRNA was barely detectable in RPTs of both male and female KO mice at 8 and 24 weeks of age.
Figure 1.
Generation of tubular Hnrnpf KO mice. (A) Schematic diagram describing the strategy of generating tubular Hnrnpf gene knockout mice. Exon 4 (E4) of the Hnrnpf gene is deleted; arrowheads: loxP sites. (B) Genotyping identification, the PCR bands of Cre (392 bp), floxed (568 bp) and wild-type (507 bp) alleles of Hnrnpf are indicated. Genotyping of representative litters are indicated; fl, Hnrnpf floxed; Control (Ctrl) (genotype: fl/fl) and KO (genotype: fl/fl, Cre). (C) Quantitative Hnrnpf mRNA expression level in male and female Ctrl and KO 24 week-old mice. **P < 0.01, KO versus Ctrl; n = 6 per group. (D) Representative WB and quantification of Hnrnpf protein expression in male and female Ctrl and KO 24 week-old mice. ***P < 0.005, KO versus Ctrl; n = 6 per group. (E) Immunostaining for Hnrnpf (red color) and a proximal tubular marker (lotus tetragonolobus lectin, LTL)(green color) in Ctrl and KO mice (original magnification ×600). DAPI staining (blue color) for cellular nucleus. Scale bars = 20 μm. G, glomerulus; P, proximal tubule.
WB of isolated RPTs confirmed the expression of Hnrnpf at the age of 8 (Supplemental Fig. 1b) and 24 weeks (Fig. 1D) in Ctrl whereas Hnrnpf expression was significantly down-regulated in KO mice. No significant difference of Hnrnpf expression in RPTs was observed between male and female Ctrl as well as between male and female KO mice. Double immunofluorescence of kidney sections (Fig. 1E) with an anti-Hnrnpf antibody and LTL-FITC antibody, confirmed significantly higher Hnrnpf expression in RPTs from Ctrl than in KO mice.
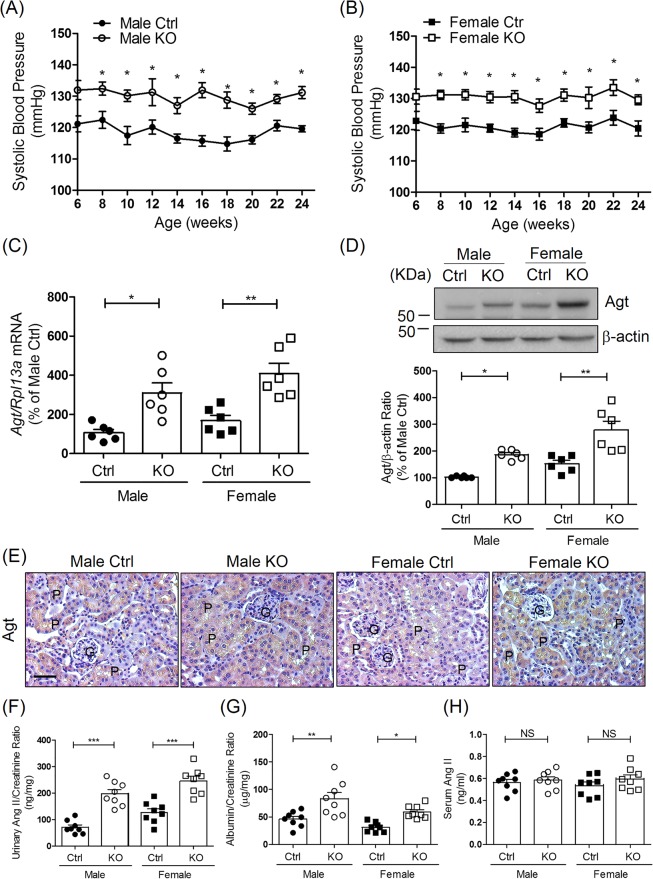
Physiological measurements in Hnrnpf KO mice
Deletion of renal tubular Hnrnpf did not influence body weight gain nor the non-fasting blood glucose levels in both male and female mice from the age of 6 to 24 weeks (Supplemental Fig. 1c–f, respectively). Longitudinal SBP measurements revealed consistently higher SBP in both male (Fig. 2A) and female (Fig. 2B) KO mice aged week 6 to 24 compared to Ctrl. Significant increases of Agt mRNA and protein expression were detected in both male and female KO mice compared to Ctrl at 8 weeks (Supplemental Fig. 2a) and 24 weeks of age (Fig. 2C,D, respectively). No significant difference of Agt expression in RPTs was observed between male and female Ctrl as well as between male and female KO mice. These were confirmed with immunostaining (Fig. 2E).
Figure 2.
Systolic blood pressure (SBP) and intrarenal angiotensinogen (Agt) expression in tubular Hnrnpf KO mice. (A) Longitudinal average SBP measurement (performed two or three times per mouse per week in the morning without fasting) in (A) male and (B) female mice. Baseline SBP was measured daily over a 5-day period before initiation of actual measurement at week 6. Values are means ± SEM, n = 10 for each group. *P < 0.05, KO versus Ctrl. (C) Agt mRNA levels in male and female Ctrl and KO mice at the age of 24 weeks. *P < 0.05, **P < 0.01, n = 6 per group, KO versus Ctrl. (D) Representative WB of Agt protein expression and quantitation of Agt expression in Ctrl and KO groups from 24 week-old male and female mice. *P < 0.05, **P < 0.01, n = 6 per group, KO versus Ctrl. (E) Representative immunostaining for Agt in Ctrl and KO mice (original magnification ×200). Scale bars = 50 μm. G, Glomerulus; P, proximal tubule. (F) Urinary Ang II, (G) ACR and (H) serum Ang II levels at week 24 in Ctrl and KO mice. Urinary Ang II and albumin levels were normalized with urinary creatinine levels. Values are mean ± SEM, n = 8 per group. *P < 0.05, **P < 0.01 and ***P < 0.005; KO versus Ctrl.
Increased urinary Ang II and urinary albumin/creatinine ratio (ACR) were also observed in both male and female KO mice compared to Ctrl at 24 weeks of age with no significant difference between male and female Ctrl as well as between male and female KO mice. (Fig. 2F,G, respectively). In contrast, body weight (BW), kidney weight (KW)/BW, GFR and glomerular tuft volume did not differ significantly between KO mice and Ctrl at 24 weeks of age (Table 1). Twenty-four h urine volume were significantly increased but not food and water intake in both male and female KO mice as compared to Ctrl. No differences were detected in serum and urine levels of sodium, calcium and phosphorus between male and female Ctrl and KO mice. We detected no significant differences in serum Ang II among different groups of mice (Fig. 2H).
Table 1.
Physiological parameters of mice at 24 weeks of age.
| Male | Female | |||||
|---|---|---|---|---|---|---|
| Ctrl | Hnrnpf KO | p | Ctrl | Hnrnpf KO | p | |
| Body weight (g) | 34.35 ± 0.96 | 34.94 ± 0.68 | NS | 24.81 ± 0.89 | 23.55 ± 0.86 | NS |
| KW/BW (mg/g) | 9.35 ± 0.58 | 8.38 ± 0.41 | NS | 9.97 ± 0.29 | 9.05 ± 0.45 | NS |
| GFR(µL/min)/BW(g) | 7.5 ± 0.45 | 7.7 ± 0.57 | NS | 7.9 ± 0.64 | 6.8 ± 0.34 | NS |
| Glomerular tuft volume (103 µm3) | 117.3 ± 8.92 | 128.2 ± 10.94 | NS | 120.2 ± 9.90 | 129.5 ± 5.88 | NS |
| Urine volume (µl/24 h) | 871.7 ± 36.1 | 1198.0 ± 102.7 | * | 265.0 ± 63.3 | 505.8 ± 41.5 | ** |
| Food intake (mg/24 h) | 333.3 ± 42.2 | 333.3 ± 33.3 | NS | 566.7 ± 76.0 | 516.7 ± 54.3 | NS |
| Water intake (ml/24 h) | 1.97 ± 0.08 | 2.37 ± 0.24 | NS | 2.30 ± 0.29 | 2.55 ± 0.13 | NS |
| Serum Na (mmol/L) | 149.7 ± 2.3 | 151.5 ± 1.4 | NS | 147.6 ± 2.1 # | 148.7 ± 1.4 | NS |
| Serum Ca (mmol/L) | 2.22 ± 0.03 | 2.21 ± 0.04 | NS | 2.34 ± 0.11 # | 2.20 ± 0.03 | NS |
| Serum P (mmol/L) | 2.89 ± 0.20 | 2.95 ± 0.29 | NS | 3.37 ± 0.36 | 3.13 ± 0.14 | NS |
| Urine Na/Cr (mmol/g Cr) | 741.0 ± 73.1 | 709.8 ± 25.0 | NS | 398.5 ± 61.1 | 353.2 ± 32.9 | NS |
| Urine P/Cr (mmol/g Cr) | 107.2 ± 17.2 | 101.2 ± 17.9 | NS | 73.3 ± 10.9 | 79.7 ± 12.6 | NS |
Values are mean ± SEM; n = 6/group.
KW/BW. Kidney Weight/Body Weight; Na. sodium; Ca. calcium; P. phosphorus; Cr. creatinine.
**p < 0.01, *p < 0.05, NS, not significant.
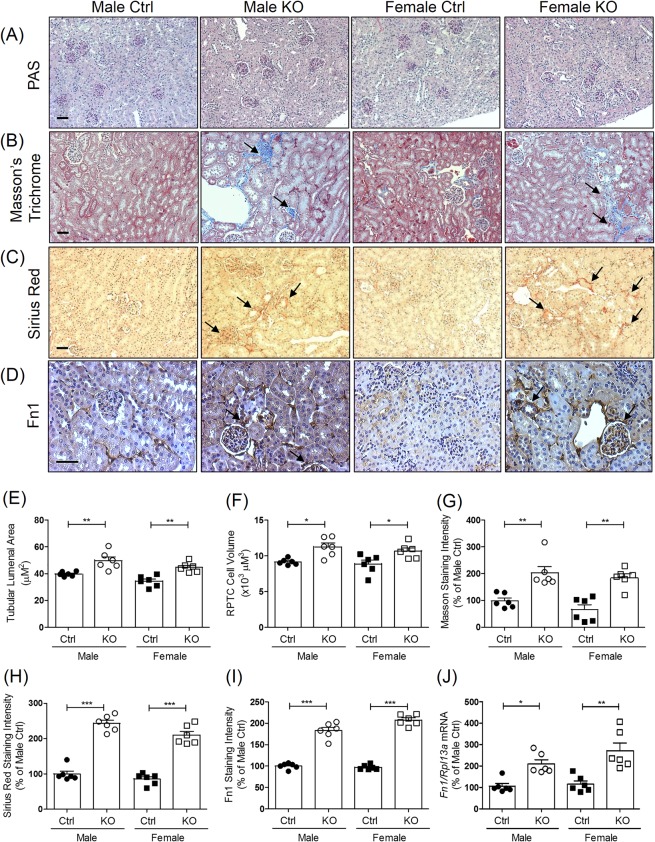
Tubulo-interstitial fibrosis in Hnrnpf KO mice
PAS staining of kidney sections showed no obvious structural changes in KO mice at the age of 24 weeks (Fig. 3A). Increased fibrosis on Masson’s Trichrome staining (Fig. 3B) and increased expression of collagen on Sirius Red staining (Fig. 3C), and fibronectin 1 (Fn1) immunostaining (Fig. 3D) was, however, noted in glomerulo-tubular regions in KO mice as compared to Ctrl at the age of 24 weeks. Semi-quantification of tubular lumenal area (Fig. 3E), RPTC volume (Fig. 3F), Masson’s Trichrome staining (Fig. 3G), Sirius Red staining (Fig. 3H) and Fn1 immunostaining (Fig. 3I) revealed an increase of tubular lumenal area, RPTC volume, Masson’s Trichrome and Sirius Red staining and Fn1 immunostaining in KO mice as compared to Ctrl, respectively. These findings were associated with significant increases of mRNA expression of Fn1 (Fig. 3J) by RT-qPCR in isolated RPTs of KO mice as compared with Ctrl.
Figure 3.
Tubulo-interstitial fibrosis in mouse kidneys. (A) Representative image of Periodic acid-Schiff (PAS) staining, (B) Masson’s trichrome staining, (C) Sirius Red staining and (D) fibronectin-1 (Fn1) immunostaining (original magnification ×100) in kidneys from male and female Ctrl and KO mice at the age of 24 weeks. (G) Glomerulus; P, proximal tubule. Scale bars = 50 μm. Semi-quantitation of tubule lumenal area (E), RPTC volume (F), Masson’s trichrome staining (G), Sirius Red staining (H) and Fn1 immunostaining (I) of Ctrl and KO mice at the age of 24 weeks. RT-qPCR of Fn1(J) in freshly RPTs from male and female Ctrl and KO mice. Values are means ± SEM, n = 6. *P < 0.05, **P < 0.01, ***P < 0.005; KO versus Ctrl.
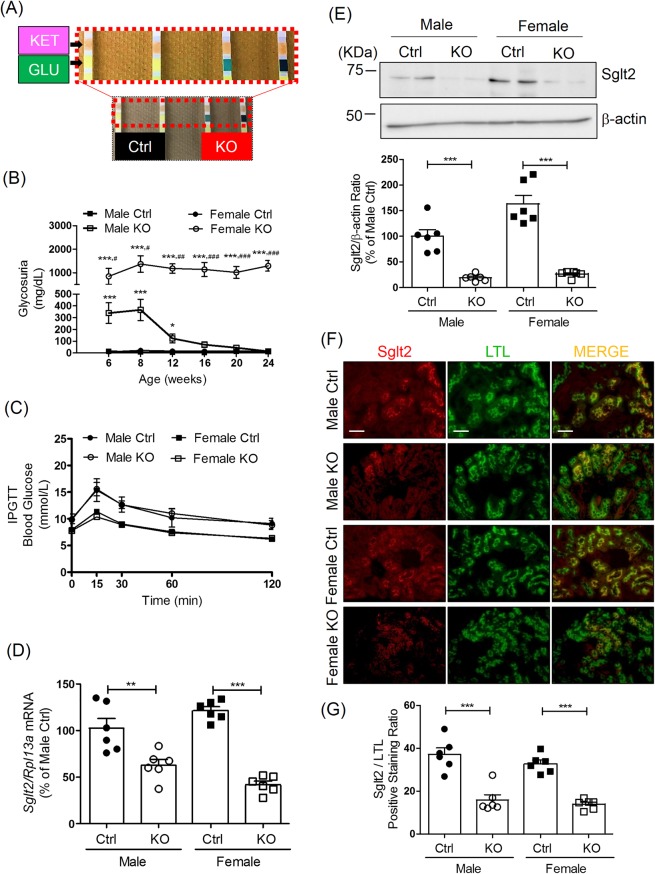
Glycosuria and Sglt2 expression in Hnrnpf KO mice
Unexpectedly, increased glucose excretion was detected in the urine using dipsticks in both male and female KO mice at age 6 weeks (Fig. 4A). From 8 weeks of age, urinary glucose levels in male KO mice steadily decreased and returned to levels similar to Ctrl mice at 12 weeks of age (Fig. 4B). In contrast, urinary glucose excretion steadily increased from week 6 in female KO mice, reached an apparent plateau at the age of 12 weeks and did not abate (Fig. 4B). No changes in urinary glucose level were detected in male and female Ctrl.
Figure 4.
Glycosuria and Sglt2 expression in Hnrnpf KO mice. (A) Urinary glucose in Ctrl and KO mice detected by dipstick test at the age of 6 weeks. (B) Longitudinal urinary glucose levels in male and female KO mice and Ctrl from the age of 6 weeks to 24 weeks measured by glucose colorimetric kit. Values are means ± SEM, n = 6. **P < 0.01; ***P < 0.005. KO versus Ctrl. ##P < 0.01; ###P < 0.005, female KO versus male KO. IPGTT test in male and female (C) Ctrl and KO mice at the age of 23 weeks. (D) Ratio of Sglt2/Rpl13a mRNA expression quantified by RT-qPCR and (E) Representative WB of Sglt2 protein expression in male and female mouse RPTs at the age of 24 weeks. Values are means ± SEM, n = 6. ***P < 0.005; KO versus Ctrl. (F) Double immunostaining of Sglt2 and LTL (magnification x100) and semi-quantification of Sglt2/LTL immunostaining ratio (G) in male and female Ctrl and KO mouse kidneys at the age of 24 weeks. Values are Sglt2/LTL positive staining ratio, n = 6. ***P < 0.005, KO versus Ctrl.
Having observed that both male and female Hnrnpf KO mice develop glycosuria, we performed intraperitoneal glucose tolerance test (IPGTT) at the age of 23 weeks in male and female mice (Fig. 4C). KO of Hnrnpf in RPTs did not influence the glucose tolerance in either male or female KO mice.
RT-qPCR revealed lower Sglt2 expression in RPTs isolated from both male and female KO mice at 8 weeks of age (Supplemental Fig. 2b) and 24 weeks of age (Fig. 4D) as compared with Ctrl. At both 8 and 24 weeks of age, Sglt2 expression decreased by ~40% in RPTs of male Hnrnpf KO mice as compared to Ctrl, whereas persistently lower Sglt2 expression (decreased by ~60% of baseline level) was observed in RPTs from female KO mice. However, no significant difference of Sglt2 expression in RPTs was observed between male and female Ctrl as well as between male and female KO mice. WB of isolated RPTs confirmed these changes at the protein level (Fig. 4E). Consistently, semi-quantitation of immunofluorescence staining with anti-Sglt2 antibodies and LTL-FITC confirmed reduced Sglt2 expression in RPTs of 24 week-old KO mice as compared to Ctrl (Fig. 4F,G, respectively). No significant changes were detectable in Slc5a1 (Sglt1) mRNA expression in RPTs isolated from both male and female KO mice as compared to Ctrl (Supplemental Fig. 2c).
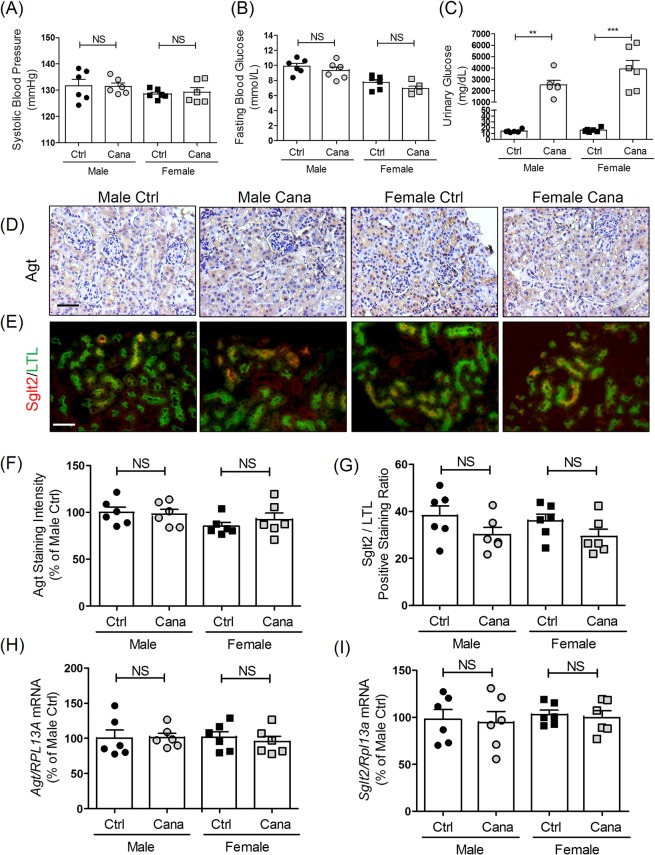
Effect of canagliflozin treatment on Agt and Sglt2 expression in RPTCs in vivo
To investigate the role of Sglt2 on Agt and Sglt2 expression in RPTCs in vivo, wild-type mice were treated with the selective Sglt2 inhibitor canagliflozin (0.2 mg/ml in drinking water). Four weeks of canagliflozin treatment had no detectable effects on SBP (Fig. 5A) and blood glucose levels (Fig. 5B) in either male or female mice but enhanced the development of glycosuria in both male and female mice (Fig. 5C) as compared to non-treated mice. Immunostaining for Agt (Fig. 5D) and immunofluorescent staining for Sglt2 (Fig. 5E) revealed that canagliflozin treatment had no effect on Agt expression or Sglt2 expression in RPTCs of either male or female mice. These observations were confirmed by semi-quantitation of Agt (Fig. 5F) and Sglt2 (Fig. 5G) expression and qPCR of Agt and Sglt2 mRNA expression in isolated RPTs (Fig. 5H,I, respectively).
Figure 5.
Effect of canagliflozin treatment on blood and urinary glucose levels, AGT and SGLT2 expression in mice. (A) SBP, (B) blood glucose and (C) urinary glucose levels after 4 weeks of treatment with or without canagliflozin in adult male and female wild-type (WT) mice. Values are means ± SEM, n = 6. **P < 0.01, ***P < 0.005; canagliflozin-treated versus non-treated mice. Immunostaining for Agt (D) and immunoflourescent staining of Sglt2 (E) in the kidneys of WT male and female mice with or without 4 weeks of canagliflozin treatment. Magnification x 200. Scale bars = 50 μm. Semi-quantification of Agt (F) and Sglt2 (G) immunostaining in male and female WT mouse kidneys after 4 weeks of treatment with or without canagliflozin. RT-qPCR of Agt (H) and Sglt2 (I) expression in isolated RPTs of WT male and female mice with or without 4 weeks of canagliflozin treatment. Values are means ± SEM, n = 6. NS, not significant; canagliflozin treated versus non-treated mice.
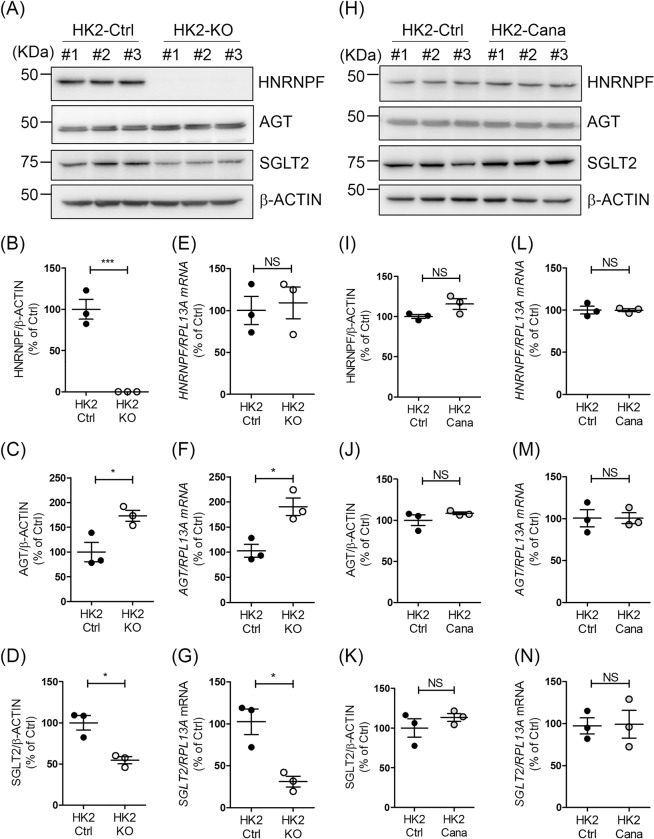
AGT and SGLT2 expression in HK-2 with or without HNRNPF KO
To validate our in vivo observations, we generated HK-2 cells with HNRNPF KO by CRISPR gRNA technology. Consistent with our in vivo observation, immunoblots revealed that HK-2 cells with HNRNPF KO exhibited non-detectable HNRNPF (Fig. 6A,B), higher AGT (Fig. 6A,C) and lower SGLT2 protein expression (Fig. 6A,D) as compared to control HK-2. These findings were confirmed by RT-qPCR of HNRNPF (Fig. 6E), AGT (Fig. 6F) and SGLT2 expression (Fig. 6G), respectively. Finally, in human cells expression of HNRNPF (Fig. 6H,I), AGT (Fig. 6H,J) and SGLT2 protein (Fig. 6H,K) and mRNA (Fig. 6L–N, respectively) did not differ significantly in HK-2 cells treated with canagliflozin and untreated cells, indicating a lack of causality of inhibition of SGLT2 activity and AGT and SGLT2 expression in RPTCs.
Figure 6.
AGT and SGLT2 expression in HK-2 with or without HNRNPF KO. (A) WB, (B–D) semi-quantitation of WB and (E–G) RT-qPCR of HNRNPF, AGT, SGLT2 and β-ACTIN in different clones of HK-2 Ctrl and HK-2 with HNRNPF KO by CRISPR gRNA. Values are means ± SEM, n = 3. *P < 0.05, **P < 0.01; HK-2-HNRNPF KO versus HK-2 Ctrl. (H) WB, (I–K) semi-quantitation of WB and (L)(M)(N) RT-qPCR of HNRNPF, AGT, SGLT2 and β-ACTIN of expression in HK-2 with or without canagliflozin (Cana) (0.5 mM) treatment for 24 hours. Values are means ± SEM, n = 3. NS, not significant. HK-2-Cana versus HK-2 Ctrl.
Discussion
Our results identify a novel mechanism by which Hnrnpf affects the development of hypertension and glycosuria in mice through modulation of intrarenal Agt and Sglt2 expression, respectively.
Hnrnpf, a member of the 30 pre-mRNA-binding protein family, modulates gene expression at both transcriptional and post-transcriptional levels11–14,18–21. Hnrnpf engages in alternative splicing of various genes and associates with TATA-binding protein, RNA polymerase II, nuclear cap-binding protein complex and various transcription factors to modulate gene expression22. We have reported previously that Hnrnpf overexpression in RPTCs attenuates hypertension and kidney injury in both diabetic Akita13 and db/db14 mice via inhibition of intrarenal Agt expression, implying an important role for Hnrnpf in modulating the development of hypertension and nephropathy in diabetic mice.
Our present findings document that genetic deletion of Hnrnpf in tubules enhances renal Agt expression, hypertension development and kidney injury in both non-diabetic male and female mice. These observations are consistent with our hypothesis that Hnrnpf plays an important role in the development of hypertension and tubulo-interstitial fibrosis via modulation of Agt and pro-fibrotic genes expression in RPTs.
Initially, we generated global Hnrnpf KO mice by cross-breeding a general Cre-deleter mouse line (CMV-Cre; B6.C-Tg(CMV-cre)1Cgn/J) with our Hnrnpffl/fl mice on a C57BL/6 background to explore the phenotype of global Hnrnpf KO mice and found that like the global Hnrnpk deletion23, global Hnrnpf KO also results in embryonic death (Supplemental Fig. 3). To circumvent this issue, we generated renal tubule-specific Hnrnpf KO mice by cross-breeding our Hnrnpffl/fl mice with a renal tubule-specific Cre deleter (Pax8-Cre; B6.129P2(Cg)-Pax8tm1.1(cre)Mbu/J) mouse line17. Several labs have also successfully employed Pax8-Cre mice to delete genes in renal tubules24–26. Our homozygous Pax8-Hnrnpf KO mice are viable and fertile without symptoms of body weight loss, physiological imbalance and altered hearing. However, they develop hypertension and elevated ACR with increased Agt expression in RPTCs by 8 weeks of age (Supplemental Fig. 4a,b). Since Pax8 is also expressed in the thyroid gland and hindbrain17, it is possible that Pax8-Hnrnpf KO mice might exhibit abnormality in thyroid gland and hindbrain thereby indirectly affecting cardiac and renal function. However, we did not detect significant changes in Hnrnpf mRNA levels or serum T4 levels in Pax8-Hnrnpf KO mice (Supplemental Fig. 5) or histological changes in thyroid gland and hindbrain. Thus, our Pax8-Hnrnpf KO mouse appears to be a valid murine model with which to study the phenotype with tubule-specific Hnrnpf KO.
An unexpected finding of our present study was that Hnrnpf deletion led to glycosuria with reduced expression of Sglt2 in RPTs of Hnrnpf KO mice. Intriguingly, serum and urine levels of Na, Ca and P did not differ between Hnrnpf KO mice and Ctrl. The phenotype of glycosuria appears to be similar to that reported in Sglt2 deficient mice27 and in patients with familial renal glycosuria (FRG)28–30 but differs from that in Sweet Pee mice, which are characterized by elevated urinary excretion of calcium and magnesium and growth retardation31, as well as from that in patients with renal Fanconi syndrome32. Intriguingly, male Hnrnpf KO mice exhibited a transient glycosuria between the ages of 6 and 12 weeks and then returned to levels similar to Ctrl. Furthermore, glycosuria correlates with reduced Sglt2 expression in RPTs of male Hnrnpf KO mice. In contrast, female Hnrnpf KO mice displayed persistent glycosuria throughout 6 to 24 weeks of age with similar inhibition of Sglt2 expression observed at both 8 and 24 weeks of age. These data would indicate that male sex hormones rather than female sex hormones may modulate Sglt2 expression in Hnrnpf KO mice. Indeed, this notion had been suggested by Sabolic’s group33,34 who implicated androgen, but not estradiol up-regulates Sglt2 expression and activity in mice.
To explore the impact of Sglt2 inhibition on Agt expression, we treated HK-2 cells and WT mice with canagliflozin. Canagliflozin had no detectable effects on SBP and blood glucose levels but enhanced the development of glycosuria in both male and female mice as compared to non-treated mice. Furthermore, canagliflozin treatment had no effect on the expression of Agt and Sglt2 expression in RPTs of mice. Thus, our data would argue against a causal relationship between Sglt2 inhibition and Agt expression in RPTCs; rather our data would indicate that inhibition of Hnrnpf expression modulates both Agt and Sglt2 expression in RPTCs.
Finally, to replicate our in vivo observations, we studied a human renal proximal tubular cell line (HK-2)35. By employing CRISPR gRNA technology, we obtained several clones of HK-2 cells with HNRNPF KO. Consistent with our findings in Hnrnpf KO mice, HK-2 with HNRNPF KO displayed significantly higher AGT and lower SGLT2 expression as compared to HK-2 controls. These data lend further support our previous observations that Hnrnpf down-regulates RPT Agt expression and RAS activation, leading to improve tubulo-interstitial fibrosis in the kidney. Moreover, consistent with our in vivo results, canagliflozin treatment had no effect on SGLT2 and AGT expression in HK-2 cells.
At present, the underlying mechanism(s) by which genetic deletion of HNRNPF led to down-regulation of SGLT2 transcription in HK-2 cells are unclear. One possibility might be that HNRNPF affects SGLT2 transcription at the promoter activity level. This is unlikely since transfection of the HNRNPF cDNA did not affect the SGLT2 promoter activity (pGL4.2/SGLT2-N-1,986/+22 promoter) in HK-2 cells (Supplemental Fig. 6a). However, we could not rule out the possibility of putative HNRNPF-response element(s) upstream of 2 kb of the SGLT2 promoter. The second possibility is that HNRNPF deletion might alter the splicing of SGLT2 to yield mutant forms of SGLT2. This is also unlikely since only one species of SGLT2 was detectable in HK-2 cells with HNRNPF KO, which was similar to the size of SGLT2 in HK-2 (Supplemental Fig. 6b). The third possibility is that HNRNPF might affect SGLT2 mRNA stability. This notion is supported by the observations of Chu et al.19 that HNRNPF regulates YAP expression via binding to the 3′UTR of YAP to affect its mRNA stability and of Decorsiere et al.21 that Hnrnph/f interacts with a G-quadruplex in maintaining p53 pre-mRNA 3′-end processing during DNA damage. The fourth possibility is that deletion of HNRNPF might suppress other un-defined signaling pathway(s) or factor(s) that might have a greater impact (stimulation) on SGLT2 expression and activity. Clearly, further studies are needed to elucidate the mechanisms underlying HNRNPF down-regulation of SGLT2 expression.
The exact mechanism(s) of Hnrnpf regulation of Agt expression is unknown. One possibility is that Hnrnpf binds to the insulin-responsive element (IRE) in the Agt promoter11,12 and functions as a negative trans-acting protein to inhibit the binding of other positive trans-acting factor(s) to TATA-binding protein (TBP) and RNA polymerase II, subsequently attenuating Agt transcription. This possibility is supported by the studies of Yoshida et al.22 showing that Hnrnpf is associated with TBP, RNA polymerase II and nuclear cap-binding protein complex. A second possibility is that Hnrnpf is associated with Hnrnpk to form an Hnrnpf/k complex and that the Hnrnpf/k complex is more effective in inhibiting Agt transcription. Indeed, we have previously reported that Hnrnpf co-immunoprecipitated with Hnrnpk and that co-transfection of Hnrnpf with HnrnpK was more effective in inhibiting Agt transcription than either Hnrnpf or HnrnpK alone35. A third possibility is that the Hnrnpf/k complex might recruit unidentified repressor molecules and subsequently repress Agt transcription. This third possibility is supported by the studies of Denisenko et al.36 demonstrating that Hnrnpk could bind the murine repressor Zik1. Clearly, more work is needed to elucidate the precise molecular mechanism of action of Hnrnpf on Agt transcription in RPTCs.
In summary, the present study reveals a novel role for Hnrnpf in the development of hypertension, tubule-interstitial fibrosis and glycosuria in mice via up-regulation of Agt and down-regulation of Sglt2 expression in RPTs, respectively. With the recent development of SGLT2 inhibitors as a novel treatment for diabetic patients37–41, it would be important to understand the regulation of SGLT2 expression at the molecular level. Our findings raise the possibility that Hnrnpf KO mice may be a useful animal model for advancing studies on SGLT2 regulation and familial renal glycosuria in human.
Methods
Chemical and reagents
Fluorescein isothiocyanate-labeled inulin and canagliflozin (Invokana) were purchased from Sigma-Aldrich (Oakville, ON, Canada) and Janssen Inc. (Toronto, ON, Canada), respectively. Dulbecco Modified Eagle Medium (DMEM) (Cat. No. 11966-025), Ham’s F12 medium (Cat. No. 11765-054) and fetal bovine serum (FBS) were bought from Gibco (Thermo Fisher Scientific, Montreal, QC, Canada). Oligonucleotides were synthesized by Integrated DNA Technologies, Inc. (Coralville, IA) and listed in Supplemental Table 1. Restriction and modifying enzymes were purchased from New England Biolabs (Whitby, ON, Canada). The sources of antibodies used are listed in Supplemental Table 2. HK-2 (an immortalized human renal proximal tubular cell line) (Cat. No. CRL-2190) was obtained from American Tissue Cell Collection (ATCC) (Manassas, VA) (http://www.atcc.org). Human SGLT2 gene promoter (N-1,986/+22) was amplified from HK-2 genomic DNA by PCR with specific primers (Supplemental Table 1) and then inserted into pGL4.20 reporter vector (Promega, Sunnyvale, CA) at Xho1and Bgl II restriction sites.
Generation of tubular Hnrnpf KO mice
Tubule-specific Hnrnpf KO mice were generated by cross-breeding male Hnrnpf-floxed mice with female Pax8-Cre mice17 (Stock number: 028196; Jackson Laboratory, Bar Harbor, ME). Briefly, the mouse Hnrnpf gene (Gene ID: 98758) is localized on chromosome 6: 117,900,340-117,925,622. Four exons have been identified in Hnrnpf with the ATG start codon and TAG stop codon both located in exon 4. The lox-modified Hnrnpf targeting vector was created by including 5′ and 3′ homology arms as well as two loxP sites flanking the fourth exon region amplified from SV129 BAC genomic DNA and confirmed by sequencing. C57BL/6 ES cells were used for gene targeting (Cyagen Biosciences, Santa Clara, CA). These mice allow the excision of exon 4 of Hnrnpf gene and disruption of the protein expression in the presence of Cre recombinase. By cross-breeding male Hnrnpf-floxed mice with female Pax8-Cre mice, heterozygous Hnrnpf-floxed allele mice were generated (genotype: Hnrnpffl/wt,Cre). These mice were back-crossbred to generate homozygous Hnrnpf-floxed allele and carrying the Cre allele (genotype: Hnrnpffl/fl,Cre). The Pax8-Hnrnpf KO mice (genotype: Hnrnpffl/fl,Cre) and control littermates (Ctrl) (genotype: Hnrnpffl/fl) as well as heterozygous littermates (genotype: Hnrnpffl/wt,Cre and Hnrnpffl/wt) were used in the present studies. Experimental mice were generated from at least three different breeding couples. Offspring were genotyped by PCR to detect the Cre-recombinase as well as the presence or absence of the 5′ loxP site using specific primers (Supplemental Table 1).
Physiological studies
Age- and sex-matched male and female KO (genotype: Hnrnpffl/fl:Cre) and control littermates (Ctrl) (genotype: Hnrnpffl/fl) were studied. Animal care and procedures followed the Principles of Laboratory Animal Care (NIH Publication No. 85-23, revised 1985 (http://grants1.nih.gov/grants/olaw/references/phspol.htm) and were approved by the CRCHUM Animal Care Committee.
Weekly random blood glucose levels were measured in mice by Accu-Chek Performa (Roche Diagnostics, Laval, QC, Canada). SBP was measured with BP-2000 tail-cuff (Visitech Systems, Apex, NC) at least 2 to 3 times per week per animal in the morning without fasting as previously described13,14. Baseline SBP was measured daily over a 5-day period before initiation of actual measurement at 6 weeks of age.
At 24 weeks of age, twenty-four h prior to euthanasia, mice were housed individually in metabolic cages. Food, water consumption, and urine output were recorded. Mouse serum and urine samples were extracted with C18 Sep-Pak columns (Waters, Mississauga, ON) and assayed for Ang II by specific ELISA (Bachem America, Torrence, CA) according to the recommended number III protocol13,14,20,43. Urines were also assayed for levels of albumin and creatinine (ELISA, Albuwell and Creatinine Companion, Exocell, Inc., Philadelphia, PA)13,14 and glucose (Glucose colorimetric kit, Cayman Chemical, Ann Arbor, MI).
For tissue studies, mice were euthanized at the age of 8 or 24 weeks. Blood samples were collected by cardiac puncture. The kidneys were isolated, decapsulated and weighed. The left kidneys were processed for histology and immunostaining, and the right kidneys were used for isolation of renal proximal tubules (RPTs) by Percoll gradient13,14,20,42,43. Aliquots of freshly-isolated RPTs from individual animals were used immediately for total RNA isolation and Western blotting.
Serum and urine biochemical measurements
Serum and urine sodium, phosphorus and calcium were measured by the Comparative Medicine and Animal Resources Centre, McGill University (Montreal, QC, Canada).
Glomerular filtration rate
The glomerular filtration rate (GFR) was estimated with fluorescein isothiocyanate inulin as recommended by the Animal Models of Diabetic Complications Consortium (http://www.diacomp.org/) with slight modifications13,14.
Intraperitoneal glucose tolerance Test
An intraperitoneal glucose tolerance test (IPGTT) was performed after 6 h fasting in non-anesthetized mice at the age of 23 weeks, as described previously44.
Real time-quantitative polymerase chain reaction
Real time-quantitative polymerase chain reaction (RT-qPCR) analyses were performed to quantify the relative expression of Hnrnpf, Agt, Sglt2, fibronectin I (FN1) and ribosomal protein L13A (RPL13A) in isolated RPTs as described previously13,14,20,43 with specific primers (Supplemental Table 1).
Western blotting
Western Blotting (WB) was performed in isolated RPTs as described previously13,14,20,43. Details of the sources of antibodies and working dilutions are listed in Supplemental Table 2.
Histology
Kidney sections were stained with periodic acid Schiff (PAS) as previously described13,14,20,43. Masson’s Trichrome staining, Sirius Red staining and immunostaining for Fn1 were performed to assess tubule-interstitial fibrosis. Semi-quantitation of the relative staining was done by NIH Image J software (http://rsb.info.nih.gov/ij/). Mean glomerular tuft and RPTC volumes, and the tubular luminal area were determined by the methods of Weibel45 and Gundersen46, as described previously47,48.
Immunofluorescence staining
Immunofluorescence (IF) staining was performed on 3-μm tissue sections from mouse kidney fixed in formalin and embedded in paraffin followed by staining with ALEXA FLUOR-594-labeled secondary antibody (Invitrogen). Proximal tubules were identified by fluorescein-labeled lotus tetragonolobus lectin (LTL, a marker of renal proximal tubule49) (Vector Labs, Burlingame, CA). Image quantification and merge were assessed by ImageJ software (http://rsb.info.nih.gov/ij/). To quantify the amount of Sglt2 expression, the pixel intensity of Sglt2 was divided by LTL intensity. To calculate the average ratio, 6 sections per mouse, 6 mice per group were analyzed.
Human renal proximal tubular cells with or without HNRNPF
Human renal proximal tubular cells (RPTCs) (HK-2) cells are derived from a normal adult male human kidney transfected with the human papilloma virus 16 (HPV-16) E6/E7 genes50. KO of HNRNPF in HK-2 was performed by the CRISPR-Cas9 genome editing method provided by Invitrogen (TrueGuide™). Briefly, the day before transfection, HK-2 cells (2.5 × 105 cells per well) were cultured in a 1:1 mixture of DMEM and Ham’s F12 medium containing 10% of FBS in 6-well plate. OPTI-MEM medium with Lipofectamine Cas9 Plus™ Reagent (Cat. No. CMAX00001, Invitrogen) and the mixture of 37.5 pmol TruCut™ Cas9 Protein v2 (Cat. No. A36497, Invitrogen) and 37.5 pmol gRNA (crRNA (Cat. No. A35509, CRISPR1099776_CR, Invitrogen):tracrRNA (Cat. No. A35506, Invitrogen)) were transfected to HK-2 and cultured for 2 days at 37 °C. Single cell clones were then isolated by using limiting dilution cloning in 96-well plates. The positive clones were identified for the absence of HNRNPF by WB of cellular extracts and confirmed by PCR of genomic sequence. The clones with HNRNPF expression were used as controls.
To test the pharmacologic effect of SGLT2 inhibition on SGLT2 and AGT expression, HK-2 cells were harvested after 24 hours of culture in serum-free normal glucose (5 mM) DMEM in the absence or presence of 0.5 mM canagliflozin as described by Pirklbauer et al.51. WB and RT-qPCR were used to quantify SGLT2 and AGT protein and mRNA expression, respectively.
Canagliflozin treatment in wild-type (WT) mice
To investigate the impact of Sglt2 inhibition and Agt expression in RPTCs in vivo, male and female WT mice were treated with or without canagliflozin (0.2 mg/ml in drinking water) at the age of 4 weeks as described previously52. Body weight, blood and urinary glucose and SBP were monitored weekly. The mice were euthanized at the age of 8 weeks. The left kidneys were processed for histology and immunostaining, and the right kidneys were used for isolation of RPTs and were used immediately for total protein and RNA isolation to quantify protein and mRNA expression of Agt and Sglt2 by WB and RT-qPCR, respectively.
Statistical analysis
The data are expressed as means ± SEM. Statistical significance between the experimental groups was analyzed by Student’s t-test or 1-way ANOVA (analysis of variance) and the Bonferroni test as appropriate. p < 0.05 values were considered to be statistically significant.
Supplementary information
Acknowledgements
This manuscript or any significant part of it is not under consideration for publication elsewhere. The data were presented, in part, as an oral communication at the Annual Meeting of the American Society of Nephrology, San Diego, CA, USA, October 23–28, 2018. This work was supported, in part, by grants from the Canadian Institutes of Health Research (MOP-84363 and MOP-106688 to JSDC, MOP-86450 to SLZ, and MOP-97742 to JGF), Kidney Foundation of Canada (KFOC 170006 to JSDC) and National Institutes of Health (NIH) of USA (HL-48455 to JRI). KNM is the recipient of a fellowship from the Consortium de Néphrologie de l’Université de Montréal (2018) and the American Society of Nephrology (2019).
Author contributions
J.S.D.C. and S.L.Z. are co-guarantors (principal investigators) responsible for study conception and design and, as such, have full access to all study data, taking responsibility for data integrity and the accuracy of data analysis. C.S.L. contributed to data research and discussion and drafted the manuscript. K.N.M., S.Z., A.G., S.Y.C. and I.C. contributed to the in vivo and in vitro experiments and data collection. J.G.F. and J.R.I. contributed to the discussion, and reviewed/edited the manuscript. All authors approved the final version for publication.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Shao-Ling Zhang, Email: shao.ling.zhang@umontreal.ca.
John S. D. Chan, Email: john.chan@umontreal.ca
Supplementary information
is available for this paper at 10.1038/s41598-019-52323-1.
References
- 1.Ingelfinger JR, Zuo WM, Fon EA, Ellison KE, Dzau VJ. In situ hybridization evidence for angiotensinogen messenger RNA in the rat proximal tubule. An hypothesis for the intrarenal renin angiotensin system. The Journal of clinical investigation. 1990;85:417–423. doi: 10.1172/jci114454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gomez RA, et al. Renin and angiotensinogen gene expression in maturing rat kidney. The American journal of physiology. 1988;254:F582–587. doi: 10.1152/ajpcell.1988.254.4.C582. [DOI] [PubMed] [Google Scholar]
- 3.Kamiyama M, Farragut KM, Garner MK, Navar LG, Kobori H. Divergent localization of angiotensinogen mRNA and protein in proximal tubule segments of normal rat kidney. Journal of hypertension. 2012;30:2365–2372. doi: 10.1097/HJH.0b013e3283598eed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tang SS, et al. Temperature-sensitive SV40 immortalized rat proximal tubule cell line has functional renin-angiotensin system. Am J Physiol. 1995;268:F435–446. doi: 10.1152/ajprenal.1995.268.3.F435. [DOI] [PubMed] [Google Scholar]
- 5.Siragy HM, Carey RM. Role of the intrarenal renin-angiotensin-aldosterone system in chronic kidney disease. American journal of nephrology. 2010;31:541–550. doi: 10.1159/000313363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kobori H, Nangaku M, Navar LG, Nishiyama A. The intrarenal renin-angiotensin system: from physiology to the pathobiology of hypertension and kidney disease. Pharmacological reviews. 2007;59:251–287. doi: 10.1124/pr.59.3.3. [DOI] [PubMed] [Google Scholar]
- 7.Navar LG. Translational studies on augmentation of intratubular renin-angiotensin system in hypertension. Kidney international supplements. 2013;3:321–325. doi: 10.1038/kisup.2013.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lavoie JL, Lake-Bruse KD, Sigmund CD. Increased blood pressure in transgenic mice expressing both human renin and angiotensinogen in the renal proximal tubule. American journal of physiology. Renal physiology. 2004;286:F965–971. doi: 10.1152/ajprenal.00402.2003. [DOI] [PubMed] [Google Scholar]
- 9.Sachetelli S, et al. RAS blockade decreases blood pressure and proteinuria in transgenic mice overexpressing rat angiotensinogen gene in the kidney. Kidney international. 2006;69:1016–1023. doi: 10.1038/sj.ki.5000210. [DOI] [PubMed] [Google Scholar]
- 10.Ying J, et al. Overexpression of mouse angiotensinogen in renal proximal tubule causes salt-sensitive hypertension in mice. American journal of hypertension. 2012;25:684–689. doi: 10.1038/ajh.2012.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei CC, Guo DF, Zhang SL, Ingelfinger JR, Chan JS. Heterogenous nuclear ribonucleoprotein F modulates angiotensinogen gene expression in rat kidney proximal tubular cells. Journal of the American Society of Nephrology: JASN. 2005;16:616–628. doi: 10.1681/asn.2004080715. [DOI] [PubMed] [Google Scholar]
- 12.Chen X, et al. Characterization of a putative insulin-responsive element and its binding protein(s) in rat angiotensinogen gene promoter: regulation by glucose and insulin. Endocrinology. 2001;142:2577–2585. doi: 10.1210/endo.142.6.8214. [DOI] [PubMed] [Google Scholar]
- 13.Lo CS, et al. Heterogeneous nuclear ribonucleoprotein F suppresses angiotensinogen gene expression and attenuates hypertension and kidney injury in diabetic mice. Diabetes. 2012;61:2597–2608. doi: 10.2337/db11-1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lo CS, et al. Heterogeneous Nuclear Ribonucleoprotein F Stimulates Sirtuin-1 Gene Expression and Attenuates Nephropathy Progression in Diabetic Mice. Diabetes. 2017;66:1964–1978. doi: 10.2337/db16-1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barsha G, Denton KM, Mirabito Colafella KM. Sex- and age-related differences in arterial pressure and albuminuria in mice. Biology of sex differences. 2016;7:57. doi: 10.1186/s13293-016-0110-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maranon Rodrigo, Reckelhoff Jane F. Sex and gender differences in control of blood pressure: Figure 1. Clinical Science. 2013;125(7):311–318. doi: 10.1042/CS20130140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouchard Maxime, Souabni Abdallah, Busslinger Meinrad. Tissue-specific expression of cre recombinase from thePax8 locus. genesis. 2004;38(3):105–109. doi: 10.1002/gene.20008. [DOI] [PubMed] [Google Scholar]
- 18.Chu WK, Hung LM, Hou CW, Chen JK. Heterogeneous ribonucleoprotein F regulates YAP expression via a G-tract in 3′UTR. Biochimica et biophysica acta. Gene regulatory mechanisms. 2019;1862:12–24. doi: 10.1016/j.bbagrm.2018.10.003. [DOI] [PubMed] [Google Scholar]
- 19.Decorsiere A, Cayrel A, Vagner S, Millevoi S. Essential role for the interaction between hnRNP H/F and a G quadruplex in maintaining p53 pre-mRNA 3′-end processing and function during DNA damage. Genes & development. 2011;25:220–225. doi: 10.1101/gad.607011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lo CS, et al. Overexpression of heterogeneous nuclear ribonucleoprotein F stimulates renal Ace-2 gene expression and prevents TGF-β1-induced kidney injury in a mouse model of diabetes. Diabetologia. 2015;58:2443–2454. doi: 10.1007/s00125-015-3700-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song KY, Choi HS, Law PY, Wei LN, Loh HH. Post-transcriptional regulation of mu-opioid receptor: role of the RNA-binding proteins heterogeneous nuclear ribonucleoprotein H1 and F. Cellular and molecular life sciences: CMLS. 2012;69:599–610. doi: 10.1007/s00018-011-0761-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoshida T, Kokura K, Makino Y, Ossipow V, Tamura T. Heterogeneous nuclear RNA-ribonucleoprotein F binds to DNA via an oligo(dG)-motif and is associated with RNA polymerase II. Genes to cells: devoted to molecular & cellular mechanisms. 1999;4:707–719. doi: 10.1046/j.1365-2443.1999.00295.x. [DOI] [PubMed] [Google Scholar]
- 23.Gallardo M, et al. hnRNP K Is a Haploinsufficient Tumor Suppressor that Regulates Proliferation and Differentiation Programs in Hematologic Malignancies. Cancer Cell. 2015;28:486–499. doi: 10.1016/j.ccell.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramkumar Nirupama, Stuart Deborah, Calquin Matias, Wang Shuping, Niimura Fumio, Matsusaka Taiji, Kohan Donald E. Possible role for nephron-derived angiotensinogen in angiotensin-II dependent hypertension. Physiological Reports. 2016;4(1):e12675. doi: 10.14814/phy2.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Federico G, et al. Tubular Dickkopf-3 promotes the development of renal atrophy and fibrosis. JCI Insight. 2016;1:e84916. doi: 10.1172/jci.insight.84916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Iervolino A, et al. Selective dicer suppression in the kidney alters GSK3beta/beta-catenin pathways promoting a glomerulocystic disease. PLoS One. 2015;10:e0119142. doi: 10.1371/journal.pone.0119142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vallon V, et al. SGLT2 mediates glucose reabsorption in the early proximal tubule. Journal of the American Society of Nephrology: JASN. 2011;22:104–112. doi: 10.1681/asn.2010030246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santer R, et al. Molecular analysis of the SGLT2 gene in patients with renal glucosuria. Journal of the American Society of Nephrology: JASN. 2003;14:2873–2882. doi: 10.1097/01.ASN.0000092790.89332.D2. [DOI] [PubMed] [Google Scholar]
- 29.Wright EM, Ghezzi C, Loo DDF. Novel and Unexpected Functions of SGLTs. Physiology (Bethesda, Md.) 2017;32:435–443. doi: 10.1152/physiol.00021.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhao X, et al. A recurrent deletion in the SLC5A2 gene including the intron 7 branch site responsible for familial renal glucosuria. Scientific reports. 2016;6:33920. doi: 10.1038/srep33920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ly JP, et al. The Sweet Pee model for Sglt2 mutation. Journal of the American Society of Nephrology: JASN. 2011;22:113–123. doi: 10.1681/asn.2010080888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Klootwijk ED, et al. Renal Fanconi syndrome: taking a proximal look at the nephron. Nephrol Dial Transplant. 2015;30:1456–1460. doi: 10.1093/ndt/gfu377. [DOI] [PubMed] [Google Scholar]
- 33.Sabolic I, et al. Expression of Na+-D-glucose cotransporter SGLT2 in rodents is kidney-specific and exhibits sex and species differences. American journal of physiology. Cell physiology. 2012;302:C1174–1188. doi: 10.1152/ajpcell.00450.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabolic I, et al. Gender differences in kidney function. Pflugers Archiv: European journal of physiology. 2007;455:397–429. doi: 10.1007/s00424-007-0308-1. [DOI] [PubMed] [Google Scholar]
- 35.Wei CC, et al. Heterogeneous nuclear ribonucleoprotein K modulates angiotensinogen gene expression in kidney cells. Journal of Biological Chemistry. 2006;281:25344–25355. doi: 10.1074/jbc.M601945200. [DOI] [PubMed] [Google Scholar]
- 36.Denisenko ON, O’Neill B, Ostrowski J, Van Seuningen I, Bomsztyk K. Zik 1, a transcriptional repressor that interacts with the heterogeneous nuclear ribonucleoprotein particle K protein. Journal of Biological Chemistry. 1996;271:27701–27706. doi: 10.1074/jbc.271.44.27701. [DOI] [PubMed] [Google Scholar]
- 37.Dandona P, et al. Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes (DEPICT-1): 24 week results from a multicentre, double-blind, phase 3, randomised controlled trial. The lancet. Diabetes & endocrinology. 2017;5:864–876. doi: 10.1016/s2213-8587(17)30308-x. [DOI] [PubMed] [Google Scholar]
- 38.Neal B, Perkovic V, Matthews DR. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. The New England journal of medicine. 2017;377:2099. doi: 10.1056/NEJMc1712572. [DOI] [PubMed] [Google Scholar]
- 39.Wanner C, et al. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. The New England journal of medicine. 2016;375:323–334. doi: 10.1056/NEJMoa1515920. [DOI] [PubMed] [Google Scholar]
- 40.Zinman B, et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. The New England journal of medicine. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 41.Perkovic V, et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. The New England journal of medicine. 2019;380:2295–2306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 42.Vinay P, Gougoux A, Lemieux G. Isolation of a pure suspension of rat proximal tubules. Am J Physiol. 1981;241:F403–411. doi: 10.1152/ajprenal.1981.241.4.F403. [DOI] [PubMed] [Google Scholar]
- 43.Lo CS, et al. Dual RAS blockade normalizes angiotensin-converting enzyme-2 expression and prevents hypertension and tubular apoptosis in Akita angiotensinogen-transgenic mice. Am. J. Physiol. Renal Physiol. 2012;302:F840–852. doi: 10.1152/ajprenal.00340.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen YW, et al. Maternal diabetes programs hypertension and kidney injury in offspring. Pediatr Nephrol. 2010;25:1319–1329. doi: 10.1007/s00467-010-1506-1. [DOI] [PubMed] [Google Scholar]
- 45.Weibel ER. Stereological Methods: Theoretical Foundations. London: Academic Press. 1980;2:149–152. [Google Scholar]
- 46.Gundersen HJ. The nucleator. Journal of microscopy. 1988;151:3–21. doi: 10.1111/j.1365-2818.1988.tb04609.x. [DOI] [PubMed] [Google Scholar]
- 47.Ghosh A, et al. Heterogeneous Nuclear Ribonucleoprotein F Mediates Insulin Inhibition of Bcl2-Modifying Factor Expression and Tubulopathy in Diabetic Kidney. Scientific reports. 2019;9:6687. doi: 10.1038/s41598-019-43218-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brezniceanu ML, et al. Attenuation of interstitial fibrosis and tubular apoptosis in db/db transgenic mice overexpressing catalase in renal proximal tubular cells. Diabetes. 2008;57:451–459. doi: 10.2337/db07-0013. [DOI] [PubMed] [Google Scholar]
- 49.Schulte BA, Spicer SS. Histochemical evaluation of mouse and rat kidneys with lectin-horseradish peroxidase conjugates. Am J Anat. 1983;168:345–362. doi: 10.1002/aja.1001680308. [DOI] [PubMed] [Google Scholar]
- 50.Ryan MJ, et al. HK-2: an immortalized proximal tubule epithelial cell line from normal adult human kidney. Kidney international. 1994;45:48–57. doi: 10.1038/ki.1994.6. [DOI] [PubMed] [Google Scholar]
- 51.Pirklbauer M, et al. Unraveling reno-protective effects of SGLT2 inhibition in human proximal tubular cells. American journal of physiology. Renal physiology. 2019;316:F449–f462. doi: 10.1152/ajprenal.00431.2018. [DOI] [PubMed] [Google Scholar]
- 52.Chan JSD, et al. Canagliflozin, a sodium-glucose co-transporter 2 (SGLT-2) blocker, normalizes blood glucose without affecting systemic blood pressure, oxidative stress, intrarenal angiotensinogen gene expression and kidney injury in type 1 diabetic mice. Nephrol Dial Transplant. 2016;31:i214. doi: 10.1093/ndt/gfw168.01. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.