This editorial refers to ‘Genetic variation at the coronary artery disease locus GUCY1A3 modifies cardiovascular disease prevention effects of aspirin’†, by K.T. Hall et al., on page 3385.
Meta-analyses of individual participant data from randomized trials have shown clearly that, when used for the secondary prevention of cardiovascular disease, the benefits of low-dose aspirin (75–100 mg daily) clearly outweigh the risks of bleeding,1 but the net benefit of aspirin for the primary prevention of cardiovascular disease is less clear,2 and has long been debated. The issue is topical, because last year three new trials assessing low-dose aspirin therapy (100 mg daily) vs. placebo for the primary prevention of atherosclerotic vascular disease (ASCVD) were reported: the ASPREE trial3 in elderly individuals, the ASCEND trial4 in patients with diabetes, and the ARRIVE trial5 in non-diabetic individuals with multiple risk factors for cardiovascular disease. An updated meta-analysis incorporating data from 13 primary prevention trials indicated that, even with the additional evidence provided by these three new trials, the absolute benefits of aspirin appear small, and are of a similar magnitude to the small absolute risks of major bleeding.6 It is unclear whether it is possible to identify people who might derive above average vascular benefit without also experiencing above average risks of bleeding. Since the relative risk reduction in serious vascular events (myocardial infarction, stroke, or vascular death) does not vary according to baseline prognostic factors,2 the absolute benefits of aspirin are proportional to the baseline risk of ASCVD. Therefore, it might be postulated that aspirin should be targeted at apparently healthy people at elevated ASCVD risk in whom the risks of bleeding are low. However, the risks of ASCVD and of bleeding are strongly correlated (chiefly because the risks of both outcomes are strongly determined by age), so few individuals are at increased risk of ASCVD without also being at higher risk of bleeding.2 Given the difficulty of selecting healthy individuals for aspirin use using conventional risk markers, it is of interest to consider whether subgroups defined by allelic variation might offer an alternative method of selecting people in whom the benefits of aspirin greatly exceed the bleeding risks.
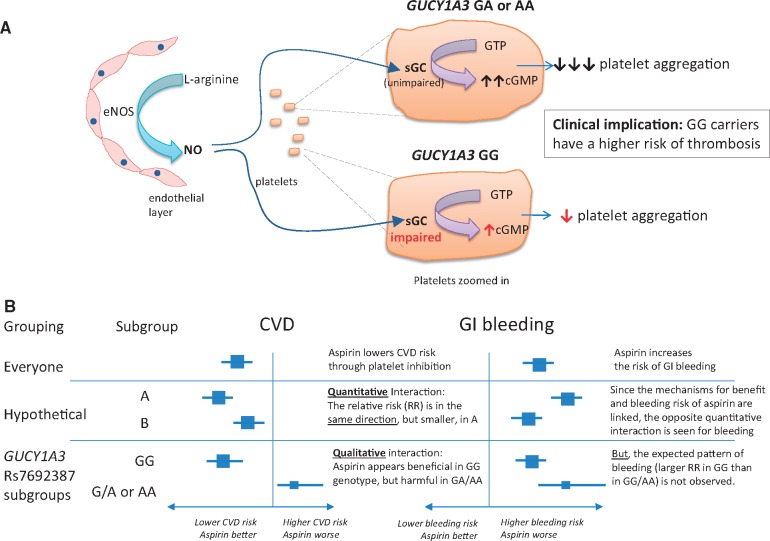
Genome-wide association studies have shown that several chromosomal loci are associated with an increased risk of coronary artery disease7 and hypertension.8 One such variant is on chromosome 4q32.1, located within an intron and regulating expression of the GUCY1A3 gene, which encodes the alpha-1-subunit of soluble guanylyl cyclase (sGC). One important mechanism through which platelet aggregation is inhibited in vivo is by endothelial production of nitric oxide (NO), which stimulates sGC to produce the second messenger cGMP, thereby inhibiting platelet aggregation (and promoting smooth muscle relaxation)9 (see Figure 1A). Patients homozygous for the common risk allele GUCY1A3 rs7692387 (G) undergoing coronary intervention have been shown to display increased platelet reactivity.10 The authors of a new study reported in this issue of the European Heart Journal hypothesized that, because of this, individuals with the GG genotype may derive greater benefit from aspirin. They tested this hypothesis in genetic analyses of populations drawn from two randomized trials of aspirin vs. placebo in apparently healthy individuals.11
Figure 1.
Postulated effects of GUCY1A3 variants on platelet function. (A) Platelet response to nitric oxide; (B) relationship of genotype with response to aspirin on risk of cardiovascular disease and gastrointestinal bleeding. eNOS, endothelial nitric oxide synthase; NO, nitric oxide; sGC, soluble guanylyl cyclase.
The ‘hypothesis-generating’ sample included 23 294 women of European ancestry drawn from the Women’s Genome Health Study (WGHS).12 The WGHS was a genetic substudy in women who participated in the Women’s Health Study, a randomized trial of 39 876 healthy female healthcare professionals aged ≥45 years comparing aspirin 100 mg on alternate days vs. placebo (and, in a 2 × 2 factorial design, of vitamin E 600 IU vs. placebo).13 The validation (or ‘hypothesis-testing’) study included European men from case–control studies of myocardial infarction (MI) and of stroke embedded within the Physician’s Health Study (PHS) of 22 071 male physicians randomized to aspirin 325 mg on alternate days vs. placebo (and, in a 2 × 2 factorial design, to beta-carotene 50 mg vs. placebo).14
Estimates for the effects of aspirin in the WGHS were derived from subgroup analyses of the aspirin vs. placebo comparison among each genotypic category (GG, GA, or AA) that were designed to test for a treatment × genotype interaction. Since women were invited to participate in the WGHS prior to treatment allocation, such analyses would be expected to be unbiased with respect to aspirin assignment. In the PHS, however, the case–control structure did not allow for an analogous comparison of aspirin vs. placebo, so the effects of aspirin in each genotypic category were estimated using conditional logistic regression matched on age and smoking, and adjusted for randomized treatment assignment; as a consequence of this design, the effects of aspirin estimated within genotypic categories within the PHS may be subject to bias or confounding. The PHS therefore has limitations as a means of testing the hypothesis raised by the WGHS.
In the WGHS, there was an interaction between aspirin efficacy and GUCY1A3 rs7692387 genotype (GG vs. GA/AA) such that aspirin appeared to reduce the risk of major cardiovascular events by 17% in women with the GG genotype (P = 0.08), but increased the risk by 39% in those with a GA or AA genotype (P = 0.03; Supplementary table S4 of Hall et al.). There was a similar pattern in the PHS sample, with a 37% reduction in the composite of MI or stroke in men with the GG genotype (P = 0.07), and a 32% increase in those with a GA or AA genotype (P = 0.47). It is of particular interest that the interaction observed in the WGHS was qualitative (i.e. aspirin yielded benefit in one subgroup and harm in the other), rather than quantitative (i.e there were differences in magnitude, but not the direction, of the effects of aspirin between subgroups); see Figure 1B. Such an interaction is extremely unusual, and immediately raises the question: are the findings biologically plausible?
An obvious way in which the plausibility of the results would be reinforced is if the observed effects of aspirin on gastrointestinal bleeding (or other measures of bleeding risk) exhibited the opposite pattern to that observed on ischaemic outcomes in each of the GUCY1A3 genotypes (illustrated in the ‘hypothetical’ example in Figure 1B). This would be expected as both the anti-ischaemic effects of aspirin and its propensity to cause gastrointestinal bleeding result from the same mechanism (i.e. inhibition of prostaglandin synthesis in platelets, as well as in the gastroduodenum). In the WGHS, however, there was a quantitative, not a qualitative, interaction on gastrointestinal bleeding: aspirin increased gastrointestinal bleeding risk in both genotypes [the hazard ratios (HRs) and 95% confidence intervals were GG 1.10, 0.95–1.29; and GA 1.49, 1.19–1.86]. Consistency with the results on ischaemia would have required that aspirin caused a higher risk of bleeding in GG carriers than in GA carriers (indeed with the possibility that aspirin might even reduce the risk of gastrointestinal bleeding in GA carriers)—the opposite of the pattern that was actually observed. (Note that, while the HR for aspirin vs. placebo on gastrointestinal bleeding in the AA group was 0.85, there were only 29 cases of gastrointestinal bleeding in this category, and so there were too few events to calculate the HR precisely.)
It is well recognized that certain individuals may be resistant to the antiplatelet effects of aspirin, and many biological mechanisms have been proposed to explain such ‘aspirin resistance’.15 However, in this instance, an explanation for the observed results requires positing a mechanism by which the presence of a non-risk A allele for GUCY1A3 rs7692387 leads not just to ‘aspirin resistance’ but to a phenotype in which aspirin induces a higher risk of thrombosis. Not only that, but the findings would imply that aspirin induces both a prothrombotic state and a bleeding diathesis among such individuals (who represent around one-third of the population). This seems to be inconsistent with our current understanding of the mechanism of action of aspirin, and is therefore somewhat implausible.
In the absence of a clear biological explanation for the counterintuitive findings, it remains relevant to ask why they might have emerged in the WGHS, and why they appear to be supported by the results of a second study (the PHS). Whilst this question cannot be answered with any certainty, it is worth pointing out that the observed interaction in WGHS on the effects of aspirin on major cardiovasular diseases between genotypic categories GG vs. GA/AA was not statistically extreme, and the ability of PHS to confirm the finding was constrained by the limitations of its case–control design. It remains possible that the findings were attributable to the play of chance. Therefore, they need to be replicated in other data sets, whether in the context of primary or secondary prevention, in which subgroup analyses of randomized comparisons of aspirin vs. placebo can evaluate reliably whether there are (directionally opposite) interactions between GUCY1A3 genotypes and the effects of aspirin on ischaemic and bleeding outcomes. Until then, given the apparent incompatibility of these findings with what is known about platelet biology, the results of this study should be treated with caution.
Conflict of interest: C.B. reports grants from the Medical Research Council, UK, the British Heart Foundation, UK, and Boehringer Ingelheim, during the conduct of the study; and grants from Pfizer, Merck & Co., and Novartis outside the submitted work. M.V.H. reports collaborating with Boehringer Ingelheim in research, and fellowship funding from the British Heart Foundation, UK (FS/18/23/33512).
Footnotes
† doi:10.1093/eurheartj/ehz384.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1.Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002;324:71–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antithrombotic Trialists (ATT) Collaboration, Baigent C, Blackwell L, Collins R, Emberson J, Godwin J, Peto R, Buring J, Hennekens C, Kearney P, Meade T, Patrono C, Roncaglioni MC, Zanchetti A.. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009;373:1849–1860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. McNeil JJ, Wolfe R, Woods RL, Tonkin AM, Donnan GA, Nelson MR, Reid CM, Lockery JE, Kirpach B, Storey E, Shah RC, Williamson JD, Margolis KL, Ernst ME, Abhayaratna WP, Stocks N, Fitzgerald SM, Orchard SG, Trevaks RE, Beilin LJ, Johnston CI, Ryan J, Radziszewska B, Jelinek M, Malik M, Eaton CB, Brauer D, Cloud G, Wood EM, Mahady SE, Satterfield S, Grimm R, Murray AM; ASPREE Investigator Group. Effect of aspirin on cardiovascular events and bleeding in the healthy elderly. N Engl J Med 2018;379:1509–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ASCEND Study Collaborative Group, Bowman L, Mafham M, Wallendszus K, Stevens W, Buck G, Barton J, Murphy K, Aung T, Haynes R, Cox J, Murawska A, Young A, Lay M, Chen F, Sammons E, Waters E, Adler A, Bodansky J, Farmer A, McPherson R, Neil A, Simpson D, Peto R, Baigent C, Collins R, Parish S, Armitage J.. Effects of aspirin for primary prevention in persons with diabetes mellitus. N Engl J Med 2018;379:1529–1539. [DOI] [PubMed] [Google Scholar]
- 5. Gaziano JM, Brotons C, Coppolecchia R, Critelli C, Darius H, Gorelick PB, Howard G, Pearson TA, Rothwell PM, Ruilope LM, Tendera M, Tognoni G; ARRIVE Executive Committee. Use of aspirin to reduce risk of initial vascular events in patients at moderate risk of cardiovascular disease (ARRIVE): a randomised, double-blind, placebo-controlled trial. Lancet 2018;392:1036–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Zheng SL, Roddick AJ.. Association of aspirin use for primary prevention with cardiovascular events and bleeding events: a systematic review and meta-analysis. JAMA 2019;321:277–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.CARDIoGRAMplusC4D ConsortiumDeloukas P, Kanoni S, Willenborg C, Farrall M, Assimes TL, Thompson JR, Ingelsson E, Saleheen D, Erdmann J, Goldstein BA, Stirrups K, König IR, Cazier JB, Johansson A, Hall AS, Lee JY, Willer CJ, Chambers JC, Esko T, Folkersen L, Goel A, Grundberg E, Havulinna AS, Ho WK, Hopewell JC, Eriksson N, Kleber ME, Kristiansson K, Lundmark P, Lyytikäinen LP, Rafelt S, Shungin D, Strawbridge RJ, Thorleifsson G, Tikkanen E, Van Zuydam N, Voight BF, Waite LL, Zhang W, Ziegler A, Absher D, Altshuler D, Balmforth AJ, Barroso I, Braund PS, Burgdorf C, Claudi-Boehm S, Cox D, Dimitriou M, Do RDIAGRAM Consortium; CARDIOGENICS ConsortiumDoney AS, El Mokhtari N, Eriksson P, Fischer K, Fontanillas P, Franco-Cereceda A, Gigante B, Groop L, Gustafsson S, Hager J, Hallmans G, Han BG, Hunt SE, Kang HM, Illig T, Kessler T, Knowles JW, Kolovou G, Kuusisto J, Langenberg C, Langford C, Leander K, Lokki ML, Lundmark A, McCarthy MI, Meisinger C, Melander O, Mihailov E, Maouche S, Morris AD, Müller-Nurasyid MMuTHER ConsortiumNikus K, Peden JF, Rayner NW, Rasheed A, Rosinger S, Rubin D, Rumpf MP, Schäfer A, Sivananthan M, Song C, Stewart AF, Tan ST, Thorgeirsson G, van der Schoot CE, Wagner PJWellcome Trust Case Control ConsortiumWells GA, Wild PS, Yang TP, Amouyel P, Arveiler D, Basart H, Boehnke M, Boerwinkle E, Brambilla P, Cambien F, Cupples AL, de Faire U, Dehghan A, Diemert P, Epstein SE, Evans A, Ferrario MM, Ferrières J, Gauguier D, Go AS, Goodall AH, Gudnason V, Hazen SL, Holm H, Iribarren C, Jang Y, Kähönen M, Kee F, Kim HS, Klopp N, Koenig W, Kratzer W, Kuulasmaa K, Laakso M, Laaksonen R, Lee JY, Lind L, Ouwehand WH, Parish S, Park JE, Pedersen NL, Peters A, Quertermous T, Rader DJ, Salomaa V, Schadt E, Shah SH, Sinisalo J, Stark K, Stefansson K, Trégouët DA, Virtamo J, Wallentin L, Wareham N, Zimmermann ME, Nieminen MS, Hengstenberg C, Sandhu MS, Pastinen T, Syvänen AC, Hovingh GK, Dedoussis G, Franks PW, Lehtimäki T, Metspalu A, Zalloua PA, Siegbahn A, Schreiber S, Ripatti S, Blankenberg SS, Perola M, Clarke R, Boehm BO, O'Donnell C, Reilly MP, März W, Collins R, Kathiresan S, Hamsten A, Kooner JS, Thorsteinsdottir U, Danesh J, Palmer CN, Roberts R, Watkins H, Schunkert H, Samani NJ.. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet 2013;45:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Surendran P, Drenos F, Young R, Warren H, Cook JP, Manning AK, Grarup N, Sim X, Barnes DR, Witkowska K, Staley JR, Tragante V, Tukiainen T, Yaghootkar H, Masca N, Freitag DF, Ferreira T, Giannakopoulou O, Tinker A, Harakalova M, Mihailov E, Liu C, Kraja AT, Fallgaard Nielsen S, Rasheed A, Samuel M, Zhao W, Bonnycastle LL, Jackson AU, Narisu N, Swift AJ, Southam L, Marten J, Huyghe JR, Stančáková A, Fava C, Ohlsson T, Matchan A, Stirrups KE, Bork-Jensen J, Gjesing AP, Kontto J, Perola M, Shaw-Hawkins S, Havulinna AS, Zhang H, Donnelly LA, Groves CJ, Rayner NW, Neville MJ, Robertson NR, Yiorkas AM, Herzig KH, Kajantie E, Zhang W, Willems SM, Lannfelt L, Malerba G, Soranzo N, Trabetti E, Verweij N, Evangelou E, Moayyeri A, Vergnaud AC, Nelson CP, Poveda A, Varga TV, Caslake M, de Craen AJ, Trompet S, Luan J, Scott RA, Harris SE, Liewald DC, Marioni R, Menni C, Farmaki AE, Hallmans G, Renström F, Huffman JE, Hassinen M, Burgess S, Vasan RS, Felix JFCHARGE-Heart Failure ConsortiumUria-Nickelsen M, Malarstig A, Reily DF, Hoek M, Vogt T, Lin H, Lieb WEchoGen ConsortiumTraylor M, Markus HFMETASTROKE ConsortiumHighland HM, Justice AE, Marouli EGIANT ConsortiumLindström J, Uusitupa M, Komulainen P, Lakka TA, Rauramaa R, Polasek O, Rudan I, Rolandsson O, Franks PW, Dedoussis G, Spector TDEPIC-InterAct ConsortiumJousilahti P, Männistö S, Deary IJ, Starr JM, Langenberg C, Wareham NJ, Brown MJ, Dominiczak AF, Connell JM, Jukema JW, Sattar N, Ford I, Packard CJ, Esko T, Mägi R, Metspalu A, de Boer RA, van der Meer P, van der Harst PLifelines Cohort StudyGambaro G, Ingelsson E, Lind L, de Bakker PI, Numans ME, Brandslund I, Christensen C, Petersen ER, Korpi-Hyövälti E, Oksa H, Chambers JC, Kooner JS, Blakemore AI, Franks S, Jarvelin MR, Husemoen LL, Linneberg A, Skaaby T, Thuesen B, Karpe F, Tuomilehto J, Doney AS, Morris AD, Palmer CN, Holmen OL, Hveem K, Willer CJ, Tuomi T, Groop L, Käräjämäki A, Palotie A, Ripatti S, Salomaa V, Alam DS, Shafi Majumder AA, Di Angelantonio E, Chowdhury R, McCarthy MI, Poulter N, Stanton AV, Sever P, Amouyel P, Arveiler D, Blankenberg S, Ferrières J, Kee F, Kuulasmaa K, Müller-Nurasyid M, Veronesi G, Virtamo J, Deloukas PWellcome Trust Case Control ConsortiumElliott PUnderstanding Society Scientific GroupZeggini E, Kathiresan S, Melander O, Kuusisto J, Laakso M, Padmanabhan S, Porteous D, Hayward C, Scotland G, Collins FS, Mohlke KL, Hansen T, Pedersen O, Boehnke M, Stringham HMEPIC-CVD ConsortiumFrossard P, Newton-Cheh CCHARGE+ Exome Chip Blood Pressure ConsortiumTobin MD, Nordestgaard BGT2D-GENES Consortium; GoT2DGenes Consortium; ExomeBP Consortium; CHD Exome+ ConsortiumCaulfield MJ, Mahajan A, Morris AP, Tomaszewski M, Samani NJ, Saleheen D, Asselbergs FW, Lindgren CM, Danesh J, Wain LV, Butterworth AS, Howson JM, Munroe PB.. Trans-ancestry meta-analyses identify rare and common variants associated with blood pressure and hypertension. Nat Genet 2016;48:1151–1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Moro MA, Russell RJ, Cellek S, Lizasoain I, Su YC, Darley-Usmar VM, Radomski MW, Moncada S.. cGMP mediates the vascular and platelet actions of nitric oxide: confirmation using an inhibitor of the soluble guanylyl cyclase. Proc Natl Acad Sci USA 1996;93:1480–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kessler T, Wolf B, Eriksson N, Kofink D, Mahmoodi BK, Rai H, Tragante V, Åkerblom A, Becker RC, Bernlochner I, Bopp R, James S, Katus HA, Mayer K, Munz M, Nordio F, O'Donoghue ML, Sager HB, Sibbing D, Solakov L, Storey RF, Wobst J, Asselbergs FW, Byrne RA, Erdmann J, Koenig W, Laugwitz KL, Ten Berg JM, Wallentin L, Kastrati A, Schunkert H.. Association of the coronary artery disease risk gene GUCY1A3 with ischaemic events after coronary intervention. Cardiovasc Res 2019;115:1512--1518. [DOI] [PubMed] [Google Scholar]
- 11. Hall KT, Kessler T, Buring JE, Passow D, Sesso HD, Zee RYL, Ridker PM, Chasman DI, Schunkert H.. Genetic variation at the coronary artery disease locus GUCY1A3 modifies cardiovascular disease prevention effects of aspirin. Eur Heart J 2019;40:3385--3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ridker PM, Chasman DI, Zee RYL, Parker A, Rose L, Cook NR, Buring JE; Women’s Genome Health Study Working Group. Rationale, design, and methodology of the women’s genome health study: a genome-wide association study of more than 25 000 initially healthy American women. Clin Chem 2008;54:249–255. [DOI] [PubMed] [Google Scholar]
- 13. Ridker PM, Cook NR, Lee IM, Gordon D, Gaziano JM, Manson JE, Hennekens CH, Buring JE.. A randomized trial of low-dose aspirin in the primary prevention of cardiovascular disease in women. N Engl J Med 2005;352:1293–1304. [DOI] [PubMed] [Google Scholar]
- 14. Hennekens CH. Final report on the aspirin component of the ongoing Physicians Health Study. N Engl J Med 1989;321:129–135. [DOI] [PubMed] [Google Scholar]
- 15. Patrono C, Rocca B.. Drug insight: aspirin resistance—fact or fashion? Nat Clin Pract Cardiovasc Med 2007;4:42–50. [DOI] [PubMed] [Google Scholar]