Highlights
-
•
PNF training statistically improves pain intensity, disability and static balance of working-age CLBP people.
-
•
Magnitudes of difference of outcomes between PNF training and general trunk exercises did not reach clinical important changes.
-
•
The therapist should take into account to use these interventions in rehabilitation programme for CLBP patients.
Keywords: Training, Low back pain, Disability, Balance
Abstract
Background
Proprioceptive neuromuscular facilitation training and general trunk exercises have been applied to treat chronic low back pain patients. However, there is currently little study to support the use of one treated intervention over the other to improve clinical outcomes and balance ability.
Objective
To examine the effects of proprioceptive neuromuscular facilitation training on pain intensity, disability and static balance ability in working-age patients with chronic low back pain.
Methods
Forty-four chronic low back pain participants aged 18–50 years were randomized either to a three-week proprioceptive neuromuscular facilitation training or to a control group receiving general trunk exercises. Pain intensity, disability and static balance ability were measured before and after the three-week intervention.
Results
The proprioceptive neuromuscular facilitation training intervention showed a statistically significantly greater reduction in pain intensity and improved functional disability than the controls at three weeks (between-group difference: pain intensity 1.22 score, 95% CI: 0.58 to 1.88, p < 0.001; disability 2.23 score, 95% CI: 1.22 to 3.24, p < 0.001. The proprioceptive neuromuscular facilitation training intervention also had statistically better parameters of static balance ability than the control group (between-group difference: ellipse sway area during eye opened and closed conditions 129.09 mm2, 95% CI: 64.93 to 175.25, p < 0.01 and 336.27 mm2, 95% CI: 109.67 to 562.87, p < 0.05, respectively; the centre of pressure velocity during eye opened and eye closed conditions 6.68 mm/s, 95% CI: 4.41 to 8.95, p < 0.01 and 6.77 mm/s, 95% CI: 4.01 to 9.54, p < 0.01, respectively).
Conclusion
The three-week proprioceptive neuromuscular facilitation training provides better pain intensity, disability and static balance ability than general trunk exercises for working-age individuals with chronic low back pain but the effects do not reach the clinical meaningful level. The therapists should consider carefully when making recommendations regarding these interventions, taking into account effectiveness and costs.
Introduction
Low back pain (LBP) is a common, challenging medical and socioeconomic problem in working-age adults.1, 2 LBP is the significant cause of years lived with disability, work absenteeism and high compensation in modern societies.2, 3 Although the majority of LBP patients recover within six weeks without medical treatment, almost 20% of these cases become chronic.4 More than 90% of chronic low back pain (CLBP) patients presenting to the primary care have non-specific LBP.4
Physical and psychosocial factors are commonly associated with CLBP.2 However, trunk muscle weakness or delayed activation, an important deficit of the neural control unit of the spinal stabilizing system, and impairment in lumbar proprioception have been frequently reported as a contributing factor of persistent LBP.5, 6, 7, 8, 9, 10, 11, 12 The consequences of altered trunk muscle activation, and impaired hip strategy and lumbar proprioception may be the determining factors in the alterations in static balance ability in CLBP patients.5, 6, 7, 8, 9, 11, 12, 13 Balance ability is the performance of maintaining the centre of gravity of the body within the base of support.11 Compared with the asymptomatic controls, CLBP patients presented a higher velocity of centre of pressure (CoP) and a larger CoP area, which is thought to represent a decreased ability to control postural balance, during one-legged stand condition6 and greater difficulty adapting to changing conditions.14 Therefore, treatment interventions improving trunk muscle strength and proprioception may improve the pain-related and balance outcomes of CLBP individuals who do not have problems in visual and vestibular systems which play important roles for controlling postural balance.15
Although there is no a clear conclusion on which type of non-pharmacologic therapy is the most effective for treating CLBP, exercise therapy is recommended as a first-line intervention for CLBP patients.2, 16 Proprioceptive neuromuscular facilitation (PNF) training has been used for treating CLBP cases by physical therapists to gain neuromuscular responses by facilitating proprioceptors.17, 18, 19, 20, 21, 22 The patterns of PNF training have diagonal and spiral directions that has been proposed to hasten the performance of numerous muscles through its patterns and to be more effective than conventional single-direction exercises.17 They also are in accordance with the topographic arrangement of the muscles being used in daily activities and sports.17, 19, 23 Moreover, PNF training may stimulate the proprioceptors of the muscles and joints in the lumbar region and may be useful for improving sensorimotor regulation and balance performance.21 Previous studies suggested three commonly applied PNF techniques for CLBP, namely, rhythmic stabilization (RS), combination of isotonics (COI) and ‘chop and lift’ (CL) as described previously.17, 18, 19, 20, 21, 22, 23, 24
Many authors have proposed the effectiveness of the PNF training in pain-related outcomes, trunk muscle activity and range of motion to manage CLBP.18, 19, 20, 21, 22, 25 However, studies supporting the effect of PNF training on the balance ability in CLBP are scarce. To the authors’ knowledge, only Young et al.22 reported that PNF training improved the balance of seniors with CLBP. Although the authors22 used the CoP measurement device, which is recommended as an optimal outcome for postural balance,26, 27 they did not screen other potential disorders, such as vestibular and visual disorders, or lower extremity strength, which could affect the balance of CLBP patients. Furthermore, the blinding method to eliminate the measurement bias was not stated. Additionally, they investigated the effects of PNF training in seniors with CLBP, but the findings could not be generalized to other age groups, especially working-age adults. A robust methodology to evaluate the effects of the PNF training on pain-related and balance parameters in working-age people is still needed. Thus, this study aimed to investigate the effectiveness of a three-week PNF training in pain intensity, functional disability and static balance in working-age patients with CLBP. It was hypothesized that CLBP participants receiving three-week PNF training may have greater decreased pain intensity, and improving functional ability and static balance than those receiving the general trunk exercises.
Methods
Study design
Conducted at the Physical Therapy Laboratory at Mae Fah Luang University, Thailand, this study was an assessor-blinded, randomized, controlled trial, with two measurement points: baseline assessment and at the end of the three-week intervention. This study was approved by the Ethics Committee for Human Research at Mae Fah Luang University (REH 59122), Chiang Rai, Thailand, based on the Declaration of Helsinki. This trial was prospectively registered at the Thai Clinical Trial Registry (TCTR20161219001) in December 2016.
Participants
Between February and May 2017, CLBP patients were recruited to the study. An advertisement was used in the Physical Therapy Department of Mae Fah Luang University Hospital in Chiang Rai, Thailand, for the purpose of patient recruitment. Male or female non-specific CLBP patients, aged 18–50 years, with pain intensity at least two points of the 0–10 numerical rating scale (NRS) were invited to participate in this study. A medical doctor who was unaware of the intervention screened the patients using oral illness history taking and a physical examination for eligibility before participation. The patients were excluded if they presented any of the following criteria: history of lumbopelvic surgery, specific LBP (e.g., disc herniation, spondylolisthesis and sacroiliac joint dysfunction) screened by using an X-ray investigation and clinical tests, cancer, autoimmune diseases, neurologic deficits, lower limb arthritis, vestibular and visual disorders, pregnancy, cardiopulmonary disorders or having exercise contraindications. Those who regularly performed PNF or general trunk exercise training were also excluded. All eligible participants signed an informed consent form before participation.
Sample size estimation
A repeated measures ANOVA formula was used to calculate the sample size. The sample size was estimated with a 90% power of test, an alpha level of 0.05 and standard deviation (SD) of 1.30 and 0.96 for the PNF training and the control groups, respectively to detect a between-group clinically significant change in two scores of the 11-point NRS at three-weeks intervention.28 The attrition rate of 10% was added to the estimation to confirm it even with a potential drop-out. In total, a sample size of 44 was obtained.
Treatment intervention
Before starting the study, participants were randomly allocated into two groups: three-week PNF training (22 participants) and control (22 participants) groups, using block randomization with block sizes of two and four. The randomization results were concealed in sealed and opaque envelopes with consecutive numbering. Randomization was performed by a researcher assistant who was unaware of the intervention and evaluation processes. All training sessions of both groups were conducted at the Physical Therapy Laboratory three times a week over three weeks. The exercise interventions of both groups were implemented by a researcher with over 10-year experience of exercise therapy in LBP who was unaware of the outcome measurement. All participants were scheduled and checked for their intervention adherence.
PNF training group
The three-week PNF training intervention was modified from the study of Areeudomwong et al.18 This training aimed at improving trunk muscle strength, trunk stabilization and controlled movements.17, 18, 23 For three weeks, the participants attended each individual training session lasting for about 30–40 min three times a week. They received three sets of 15 repetitions for each PNF training, with a 30 s rest between repetitions. A 60 s rest after completing the 15 repetitions was provided. The training intervention was divided into three phases and progression of training was based on the individual's performance.
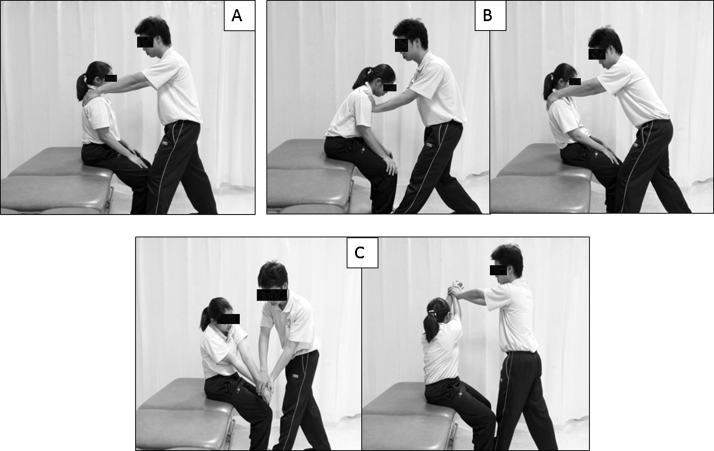
For week 1, the participants were trained in alternate isometric contractions of the trunk flexors and extensors against maximum force. The training was provided by the physical therapist for 10 s in a sitting position (Fig. 1A).
Figure 1.
Proprioceptive neuromuscular facilitation training, rhythmic stabilization (A), combination of isotonics (B) and chop and lift (C).
For week 2, the participants concentrated in alternating isometric concentric and eccentric contractions of the trunk agonistic muscles with a 5 s resisted concentric contraction of the trunk flexors in forward bending, followed by a 5 s resisted eccentric contraction of the trunk flexors in the return to trunk neutral position and a 5 s hold resisted isometric contraction of the trunk muscles in a neutral position. The same method was applied in the backward bending of the trunk (Fig. 1B).
For week 3, the participants focused on training the upper extremities by alternately performing the chop and lift movement patterns in diagonal and spiral directions for 10 s. The maximum resistance was generated by the physical therapist (Fig. 1C).
General trunk exercise group (control group)
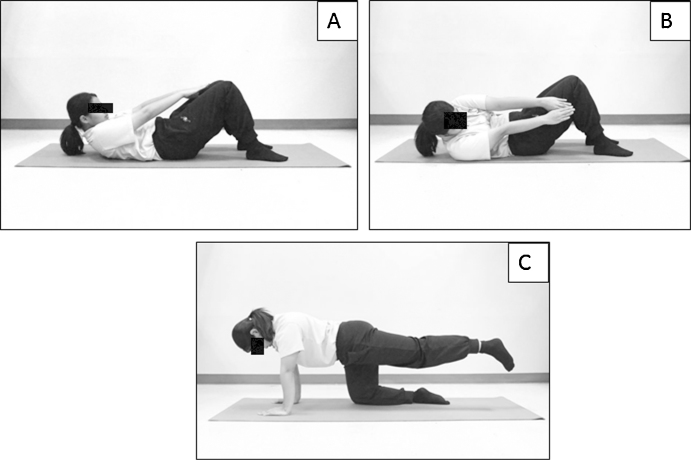
The general trunk exercise programme consisted of trunk curl-up (Fig. 2A), diagonal trunk curl (Fig. 2B) and single-legged extension (Fig. 2C). These exercises promote the strengthening of the lumbopelvic muscles, as proposed by Imai et al.29 and Koumantakis et al.30 The participants attended three exercises lasting for about 30 min three times a week over three weeks. All exercises were performed in three sets of 10 repetitions, with a 30 s rest between repetitions and a 60 s rest between sets.
Figure 2.
General trunk exercises, trunk curl-up (A), diagonal trunk curl (B) and single-legged extension (C).
All the participants were asked for any adverse effects of the intervention upon the completion of intervention. They were also asked to avoid medications and other treatments throughout the study period. A log book was given to each participant for recording other co-interventions.
Outcome measures
All outcome measures were assessed by an assessor who was blinded to the randomization procedure. The primary outcome measure was pain intensity, which was estimated using the 11-point NRS, with scores ranging from 0 (no pain) to 10 (very severe pain).31 It showed high reliability (r = 0.95–0.96) and validity (r = 0.86–0.95).32 The participants circled the numerical value on the segmented scale to indicate pain level. A clinically important change for the 11-point NRS is approximately two points for the CLBP.28
The secondary outcomes were composed of disability and static balance. The Thai version of the Roland–Morris Disability Questionnaire (RMDQ) was employed to assess disability.33 The questionnaire consists of 24 items to assess disability specific to LBP. The participants put a tick on the blank in front of each item if they had such disability on the evaluation day. The total score ranged from 0 (no disability) to 24 (maximum disability). The Thai RMDQ showed high reliability (K = 0.71–0.93).33
The one-legged stand test (OLST), which is an easy, quick and low-cost test for measuring static balance in a clinical setting, was performed for measuring static balance ability.26 The participants practiced this test three times before data collection. This test was conducted using a force platform (PDM-S, Multifunction Force Measuring Plate, Zebris, Germany) operating with 2560 embedded force sensors arranged in a 35 cm × 54 cm matrix that showed high reliability (intraclass correlation coefficient, ICC = 0.75–0.83).34 The measured pressure ranged at 1–120 N/cm2, and the sampling rate was 120 Hz. The platform was calibrated before the recording. The participants stood barefoot on the platform with the dominant leg, which was defined as the preferred kicking leg to a ball, and the contralateral leg was lifted from the floor approximately 10 cm and placed behind the weight-bearing leg. The stance foot was standardized with an angle of 30° between the foot and the imaginary line on a sagittal plane. The participants also crossed their arms over their chest. The participants performed the test with eye opened (EO), focusing on a point 2 m ahead, and with eye closed (EC). The static balance was considered by the time while standing on the dominant leg. Timing was terminated after 60 s EO or 30 s EC, or when the tested position could no longer be maintained.26 The set of outcome measures taken from the CoP data while performing the OLST consisted of the following: (1) Ellipse sway area (mm2), which represents a 95% confidence ellipse for the average of the CoP anterior, posterior, medial and lateral coordinates. (2) CoP velocity (mm/s), which represents the mean velocity of movement of the CoP over the assessment period in the X- and Y-axes. The ellipse sway area and CoP velocity are the recommended outcome measures for postural balance.26, 27, 35
The OLST was performed three times for each condition, with a 30 s rest period between trials.26 The average value of the OLST trials in each condition represented the static balance, with a less ellipse sway area and CoP velocity indicating better balance performance.
Prior to data collection, the reliability test for the measurement of the OLST was determined by the assessor. Intra-rater reliability showed high reliability (ICC = 0.90; 95% confidence interval, CI = 0.70–0.97, p < 0.001).
Statistical analysis
The characteristics of the participants were presented using descriptive statistics. Data were analyzed using SPSS version 20 (IBM Corporation, Armonk, NY, USA) and based on the intention-to-treat approach. The mean, SD and the 95% CI of the values were calculated for each variable. The Shapiro–Wilk test showed that all data were normally distributed. A 2 × 2 (group × time) repeated measures ANOVA was used to compare between-group differences for each outcome. If a significant interaction effect was observed, multiple comparisons with Bonferroni adjustment would be applied. The significance level was set to 0.05. The effect size (ES) was calculated using the difference between two means divided by a pooled SD. The interpretation of the ES was performed on the basis of Cohen's recommendation, where d = 0.20 is the small ES, d = 0.50 is the medium ES and d = 0.80 is the large ES.36
Results
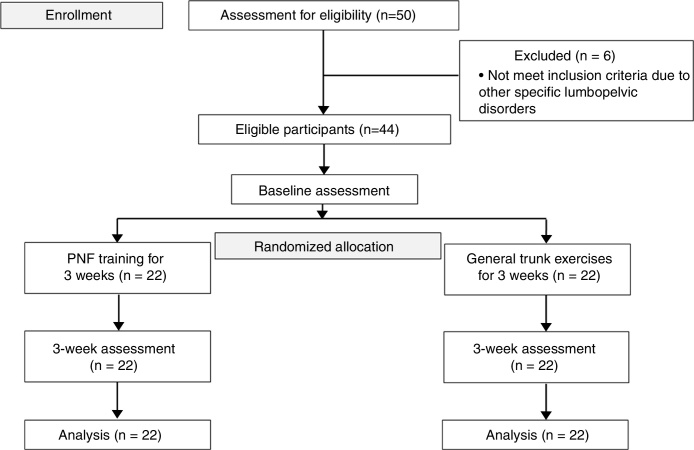
Fifty CLBP patients were initially screened for eligibility. Forty-four eligible participants met the inclusion criteria, willed to participate in this study, and were allocated to either the PNF training or the control group equally. Six patients were excluded from the study because they had disc herniation and sacroiliac joint dysfunction (Fig. 3). All participants attended the three weeks of the study, and none of the participants reported any adverse effects and used other co-interventions during the intervention period. Table 1 showed the baseline characteristics of the participants and they were homogenous between the groups.
Figure 3.
Flow of the participants.
Table 1.
Demographic and baseline clinical characteristics.
| Characteristics | PNF training group (n = 22) | Control group (n = 22) |
|---|---|---|
| Age (year) | 38.20 ± 9.40 | 39.57 ± 10.63 |
| Gender | 10 (45.50) | 9 (40.91) |
| Height (cm) | 165.30 ± 13.21 | 166.80 ± 10.11 |
| Weight (kg) | 59.60 ± 5.80 | 60.10 ± 7.70 |
| Low back pain duration (month) | 8.20 ± 4.50 | 9.20 ± 7.10 |
| Physical work | ||
| University student | 5 | 7 |
| Officer | 34 | 29 |
| Business owner | 15 | 10 |
| Pain intensity (0–10) | 4.56 ± 1.06 | 4.00 ± 1.23 |
| Disability (0–24) | 8.00 ± 1.23 | 7.41 ± 1.47 |
| Ellipse sway area (mm2) in EO condition | 664.50 ± 136.00 | 612.36 ± 118.46 |
| CoP velocity (mm/s) in EO condition | 33.96 ± 6.33 | 33.09 ± 8.84 |
| Ellipse sway area (mm2) in EC condition | 1751.55 ± 282.39 | 1731.36 ± 272.10 |
| CoP velocity (mm/s) in EC condition | 61.00 ± 13.65 | 60.36 ± 10.52 |
Note: Continuous variables are expressed as mean (standard deviation) and categorical variables are expressed as number (percentage).
PNF, proprioceptive neuromuscular facilitation; SD, standard deviation; CoP, centre of pressure; EO, eye opened; EC, eye closed.
The effect of the significant group × time interaction on pain intensity was observed (p < 0.001). The PNF training group showed a statistically significant higher reduction in pain intensity than the control group after the completion of three-week intervention period (between-group difference 1.22 ± 0.32 points, 95% CI: 0.58 to 1.88, p < 0.001) (Table 2). A moderate effect size was found (d = 0.50). A significant interaction effect on functional disability was also found (p < 0.001). The PNF training group demonstrated a statistically significant greater reduced functional disability than the controls after the three-week intervention period ceased (between-group difference 2.23 ± 0.50 score, 95% CI: 1.22 to 3.24, p < 0.001) (Table 2) with a moderate effect size (d = 0.56). In measuring the CoP outcomes while performing OLST with the EO condition, significant interaction effects on the ellipse sway area and CoP velocity were detected (p < 0.001). The PNF training group provided a statistically significant greater reduction in the ellipse sway area and CoP velocity than the controls (between-group difference 129.09 ± 27.33 mm2, 95% CI: 64.93 to 175.25, p = 0.003 for ellipse sway area and between-group difference 6.68 ± 1.12 mm/s, 95% CI: 4.41 to 8.95, p = 0.004 for CoP velocity) (Table 2). Moderate effect sizes (d = 0.56 and d = 0.67 for the ellipse sway area and CoP velocity, respectively) were demonstrated.
Table 2.
Comparison between proprioceptive neuromuscular facilitation (PNF) training (n = 22) and control (n = 22) groups on pain intensity, functional disability and static balance ability at baseline and 3-week assessment.
| Variables | PNF training group Mean ± SD |
Control group Mean ± SD |
PNF training group versus control group Mean ± SD (95% CI) |
|---|---|---|---|
| Pain intensity (score) | |||
| Baseline | 4.56 ± 1.06 | 4.00 ± 1.23 | NS |
| 3-week assessment | 1.78 ± 1.23 | 3.00 ± 0.87 | 1.22 ± 0.32 (0.58 to 1.88)*** |
| Functional disability (score) | |||
| Baseline | 8.00 ± 1.23 | 7.41 ± 1.47 | NS |
| 3-week assessment | 3.77 ± 1.51 | 6.00 ± 1.80 | 2.23 ± 0.50 (1.22 to 3.24)*** |
| Ellipse sway area (mm2) in EO condition | |||
| Baseline | 664.50 ± 136.00 | 612.36 ± 118.46 | NS |
| 3-week assessment | 479.23 ± 85.54 | 599.32 ± 95.49 | 129.09 ± 27.33 (64.93 to 175.25)** |
| CoP velocity (mm/s) in EO condition | |||
| Baseline | 33.96 ± 6.33 | 33.09 ± 8.84 | NS |
| 3-week assessment | 25.18 ± 4.36 | 31.86 ± 2.96 | 6.68 ± 1.12 (4.41 to 8.95)** |
| Ellipse sway area (mm2) in EC condition | |||
| Baseline | 1751.55 ± 282.39 | 1731.36 ± 272.10 | NS |
| 3-week assessment | 1292.82 ± 268.45 | 1629.09 ± 453.10 | 336.27 ± 112.28 (109.67 to 562.87)* |
| CoP velocity (mm/s) in EC condition | |||
| Baseline | 61.00 ± 13.65 | 60.36 ± 10.52 | NS |
| 3-week assessment | 49.50 ± 5.54 | 56.27 ± 3.27 | 6.77 ± 1.37 (4.01 to 9.54)** |
CoP, centre of pressure; EO, eye opened; EC, eye closed; SD, standard deviation; 95% CI, 95% confidence interval.
p < 0.05.
p < 0.01.
p < 0.001.
Table 2 shows the results of the CoP outcomes while performing OLST with the EC condition. A significant group by time interaction effect of the ellipse sway area (p = 0.02) and CoP velocity (p = 0.007) was found. The PNF training group provided a statistically significant greater reduction in all CoP outcomes than the control group (between–group difference 336.27 ± 112.28 mm2, 95% CI: 109.67 to 562.87, p = 0.005 for the ellipse sway area and between-group difference 6.77 ± 1.37 mm/s, 95% CI: 4.01 to 9.54, p < 0.001 for the CoP velocity). A small effect size (d = 0.41) was found for the ellipse sway area and a moderate effect size for the CoP velocity (d = 0.60).
Discussion
This study investigated the effectiveness of a three-week PNF training programme on pain-related and static balance parameters among working-age individuals with CLBP. The findings of this study supported our hypothesis that the PNF training provided positive, but small, effects not only by decreasing pain intensity and disability but also by improving static balance.
The selection of the PNF training aimed at promoting the activation of the trunk muscles through the diagonal and spiral directions, consistent with the topographic arrangement of the muscles being used in daily living.17 The previous studies found that impaired trunk muscle activation and coordination resulting in excessive movement and instability of the lumbar spine may be associated with greater pain and functional disability.37, 38, 39 Moreover, altered trunk muscle activation was found to be related to a disturbance in mechanoreceptors and possibly to an association with inaccurate information processing from the higher centres of the central nervous system related to motor control.8, 38, 39 Three-week PNF training group of the present study had statistically significant more decreased pain and functional disability than the controls. The ES for the between-group differences was moderate, suggesting a moderate clinical effect of three-week PNF training for treating CLBP patients; however, the between group differences did not surpass the reported of clinically important change of two points of the NRS28 and 3.5 scores of the RMDQ.40 This finding is in agreement with those of other studies despite some differences in the training protocols and outcome measures. George et al.25 revealed an additional positive effects of a three-week PNF training for trunk muscles plus general trunk exercises on pain intensity measured by a visual analogue scale (VAS) and function measured by the Oswestry Disability Index compared with general trunk exercises alone in CLBP patients. Young et al.22 reported that a six-week PNF training improved pain intensity measured by a VAS in seniors with CLBP. The RS, COI and CL techniques were chosen for this study, and they could hasten the performance of numerous muscles through their patterns.17, 23 The RS technique may promote trunk stability, and the COI and CL techniques promote muscle co-contraction and mobilization to enhance joint controlled mobility and human movement.17, 23 Therefore, the improvements in pain intensity and function may result from the better activation of the trunk muscles to increase lumbar stabilization in daily activities.18, 23, 25
The finding of this study showed a greater improvement in the static balance in the EO and EC conditions after three-week PNF training than in the controls. This result is consistent with the study of George et al.,25 which reported better static balance after receiving a PNF programme than after trunk strengthening exercises in seniors with CLBP. The previous studies showed that pain, altered lumbopelvic muscle activation and impairment of the lumbar proprioception could be contributing factors in the lack of balance ability of CLBP patients.13, 35, 41 Ruhe et al.35 reported a linear relationship between increasing pain and increasing COP velocity. Mok et al.13 proposed that CLBP patients present impaired hip strategy during balance challenge which may be because of decreased lumbar proprioception and improper activation of lumbopelvic muscles. Balance dysfunction in CLBP individuals may associate with altered proprioceptive input or central processing.41 The improvements in static balance in this study may be related to the significant subsidence of pain intensity35 and improved muscle activity, such as the transversus abdominis and lumbar erector spinae muscles, to stabilize the lumbar spine as described previously.18, 25 Additionally, PNF training is speculated to stimulate the proprioceptors of the muscles and joints of the lumbar spine, and it may improve sensorimotor regulation and balance performance.21
This study has several advantages. First, the study was designed as an assessor-blinded, randomized controlled trial to eliminate selection and measurement bias.42 Second, this study used the criteria to exclude other conditions that could affect balance ability, such as vestibular disorders, visual disorders, or lower limb problems, to include CLBP patients who did not have such conditions. Third, as all participants completed the interventions, participant attrition was not an issue.
This study has its limitations. It only considered the effects of PNF training on pain, disability and static balance. Further studies should examine other outcomes, such as quality of life, fear of movement, or dynamic balance. This study did not measure the responses of trunk muscles during static balance test, and thus we were not aware whether the PNF training improved such muscles to stabilize the lumbar spine directly during the test. The general trunk exercise programme was set as the control intervention in this study. A comparison with other balance exercise or conventional interventions could provide an extensive knowledge of PNF training in CLBP individuals. Further, the findings can only be generalized to the working-age population with CLBP. Future studies should assess the effects of PNF training on other LBP conditions, such as lumbar disc herniation or lumbar spondylosis, and on other age ranges, including adolescents or the elderly. As the long-term effect of PNF training was not investigated, studies with long-term follow-up should be conducted. The sample size of this study was small, limiting a precise estimate of the effect. Additionally, this study had one physical therapist to administer PNF and general trunk exercise interventions and it may be associated with possible preference bias of the physical therapist.
Conclusion
The application of a three-week PNF training programme could provide a greater reduction in pain intensity, and improving the functional ability and static balance than the general trunk exercises in working-age patients with CLBP. As the magnitudes of difference do not reach the clinical meaningful level, the therapists should prescribe either intervention to the patients based on its effectiveness and costs.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Trial Registration: TCTR20161219001 (http://www.clinicaltrials.in.th/index.php?tp=regtrials&menu=trialsearch&smenu=fulltext&task=search&task2=view1&id=2250).
References
- 1.Guo H.R., Chang Y.C., Yeh W.Y., Chen C.W., Guo Y.L. Prevalence of musculoskeletal disorder among workers in Taiwan: a nationwide study. J Occup Health. 2004;46(1):26–36. doi: 10.1539/joh.46.26. [DOI] [PubMed] [Google Scholar]
- 2.Oliveira I.S., Costa L.O., Garcia A.N., Miyamoto G.C., Cabral C.M., Costa L.D. Can demographic and anthropometric characteristics predict clinical improvement in patients with chronic non-specific low back pain? Braz J Phys Ther. 2018;22(4):328–335. doi: 10.1016/j.bjpt.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dagenais S., Roffey D.M., Wai E.K., Haldeman S., Caro J. Can cost utility evaluations inform decision making about interventions for low back pain? Spine J. 2009;9(11):944–957. doi: 10.1016/j.spinee.2009.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Costa L.D., Maher C.G., Hancock M.J., McAuley J.H., Herbert R.D., Costa L.O. The prognosis of acute and persistent low-back pain: a meta-analysis. Can Med Assoc J. 2012;184(11):E613–E624. doi: 10.1503/cmaj.111271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho K.H., Beom J.W., Lee T.S., Lim J.H., Lee T.H., Yuk J.H. Trunk muscles strength as a risk factor for nonspecific low back pain: a pilot study. Ann Rehabil Med. 2014;38(2):234–240. doi: 10.5535/arm.2014.38.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Radebold A., Cholewicki J., Polzhofer G.K., Greene H.S. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine. 2001;26(7):724–730. doi: 10.1097/00007632-200104010-00004. [DOI] [PubMed] [Google Scholar]
- 7.Sanders T., Foster N.E., Bishop A., Ong B.N. Biopsychosocial care and the physiotherapy encounter: physiotherapists’ accounts of back pain consultations. BMC Musculoskelet Disord. 2013;14:1. doi: 10.1186/1471-2474-14-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leinonen V., Airaksinen M., Taimela S. Low back pain suppresses preparatory and triggered upper-limb activation after sudden upper-limb loading. Spine. 2007;32(5):E150–E155. doi: 10.1097/01.brs.0000256886.94791.94. [DOI] [PubMed] [Google Scholar]
- 9.Tong M.H., Mousavi S.J., Kiers H., Ferreira P., Refshauge K., van Dieën J. Is there a relationship between lumbar proprioception and low back pain? A systematic review with meta-analysis. Arch Phys Med Rehab. 2017;98(1):120–136. doi: 10.1016/j.apmr.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 10.da Silva R.A., Vieira E.R., Fernandes K.B. People with chronic low back pain have poorer balance than controls in challenging tasks. Disabil Rehabil. 2017;27:1–7. doi: 10.1080/09638288.2017.1294627. [DOI] [PubMed] [Google Scholar]
- 11.Tsigkanos C., Gaskell L., Smirniotou A., Tsigkanos G. Static and dynamic balance deficiencies in chronic low back pain. J Back Musculoskelet Rehabil. 2016;29(4):887–893. doi: 10.3233/BMR-160721. [DOI] [PubMed] [Google Scholar]
- 12.Tong M.H., Mousavi S.J., Kiers H., Ferreira P., Refshauge K., van Dieën J. Is there a relationship between lumbar proprioception and low back pain? A systematic review with meta-analysis. Arch Phys Med Rehabil. 2017;98(1):120–136. doi: 10.1016/j.apmr.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 13.Mok N.W., Brauer S.G., Hodges P.W. Hip strategy for balance control in quiet standing is reduced in people with low back pain. Spine. 2004;29(6):E107–E112. doi: 10.1097/01.brs.0000115134.97854.c9. [DOI] [PubMed] [Google Scholar]
- 14.Mientjes M.I., Frank J.S. Balance in chronic low back pain patients compared to healthy people under various conditions in upright standing. Clin Biomech. 1999;14(10):710–716. doi: 10.1016/s0268-0033(99)00025-x. [DOI] [PubMed] [Google Scholar]
- 15.Grace Gaerlan M., Alpert P.T., Cross C., Louis M., Kowalski S. Postural balance in young adults: the role of visual, vestibular and somatosensory systems. J Am Acad Nurse Pract. 2012;24(6):375–381. doi: 10.1111/j.1745-7599.2012.00699.x. [DOI] [PubMed] [Google Scholar]
- 16.Qaseem A., Wilt T.J., McLean R.M., Forciea M.A. Noninvasive treatments for acute, subacute, and chronic Low Back Pain: a clinical practice guideline from the American College of Physicians Noninvasive Treatments for acute, subacute, and chronic low back pain. Annals Intern Med. 2017;166(7):514–530. doi: 10.7326/M16-2367. [DOI] [PubMed] [Google Scholar]
- 17.Adler S.S., Beckers D., Buck M. 4th ed. Springer-Medizin; Berlin: 2014. PNF in Practice. [Google Scholar]
- 18.Areeudomwong P., Wongrat W., Neammesri N., Thongsakul T. A randomized controlled trial on the long-term effects of proprioceptive neuromuscular facilitation training, on pain-related outcomes and back muscle activity, in patients with chronic low back pain. Musculoskelet Care. 2017;15(3):218–229. doi: 10.1002/msc.1165. [DOI] [PubMed] [Google Scholar]
- 19.Kofotolis N., Kellis E. Effects of two 4-week proprioceptive neuromuscular facilitation programs on muscle endurance, flexibility and functional performance in women with chronic low back pain. Phys Ther. 2006;86(7):1001–1012. [PubMed] [Google Scholar]
- 20.Kofotolis N., Vlachopoulos S.P., Kellis E. Sequentially allocated clinical trial of rhythmic stabilization exercises and TENS in women with chronic low back pain. Clin Rehabil. 2008;22(2):99–111. doi: 10.1177/0269215507080122. [DOI] [PubMed] [Google Scholar]
- 21.Westwater-Wood S., Adams N., Kerry R. The use of proprioceptive neuromuscular facilitation in physiotherapy practice. Phys Ther Rev. 2010;15(1):23–28. [Google Scholar]
- 22.Young K.J., Je C.W., Hwa S.T. Effect of proprioceptive neuromuscular facilitation integration pattern and Swiss ball training on pain and balance in elderly patients with chronic back pain. J Phys Ther Sci. 2015;27(10):3237–3240. doi: 10.1589/jpts.27.3237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Westwater-Wood S., Adams N., Kerry R. The use of proprioceptive neuromuscular facilitation in physiotherapy practice. Phys Ther Rev. 2010;15(1):23–28. [Google Scholar]
- 24.Voight M.L., Hoogenboom B.J., Cook G. The chop and lift reconsidered: integration neuromuscular principles into orthopedic and sports rehabilitation. N Am J Sports Phys Ther. 2008;3(3):151–159. [PMC free article] [PubMed] [Google Scholar]
- 25.George A.J., Kumar D., Nikhil N.P. Effectiveness of trunk proprioceptive neuromuscular facilitation training in mechanical low back pain. Int J Curr Res. 2013;5(7):1965–1968. [Google Scholar]
- 26.Maribo T., Stengaard-Pedersen K., Jensen L.D., Andersen N.T., Schiøttz-Christensen B. Postural balance in low back pain patients: intra-session reliability of center of pressure on a portable force platform and of the one leg stand test. Gait Posture. 2011;34(2):213–217. doi: 10.1016/j.gaitpost.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 27.Ruhe A., Fejer R., Walker B. The test-retest reliability of centre of pressure measures in bipedal static task conditions-a systematic review of the literature. Gait Posture. 2011;32(4):436–445. doi: 10.1016/j.gaitpost.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 28.Dworkin R.H., Turk D.C., Wyrwich K.W. Interpreting the clinical importance of treatment outcomes in chronic pain clinical trials: IMMPACT recommendations. J Pain. 2008;9(2):105–121. doi: 10.1016/j.jpain.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 29.Imai A., Kaneoka K., Okubo Y., Shiraki H. Comparison of the immediate effect of different types of trunk exercise on the star excursion balance test in male adolescent soccer players. Int J Sports Phys Ther. 2014;9(4):428–435. [PMC free article] [PubMed] [Google Scholar]
- 30.Koumantakis G.A., Watson P.J., Oldham J.A. Trunk muscle stabilization training plus general exercise versus general exercise only: randomized controlled trial of patients with recurrent low back pain. Phys Ther. 2005;85(3):209–225. [PubMed] [Google Scholar]
- 31.Chiarotto A., Deyo R.A., Terwee C.B. Core outcome domains for clinical trials in non-specific low back pain. Eur Spine J. 2015;24(6):1127–1142. doi: 10.1007/s00586-015-3892-3. [DOI] [PubMed] [Google Scholar]
- 32.Hawker G.A., Mian S., Kendzerska T., French M. Measures of adult pain: Visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res. 2011;63(S11):S240–S252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 33.Jirarattanphochai K., Jung S., Sumananont C., Saengnipanthkul S. Reliability of the Roland-Morris Disability Questionnaire (Thai version) for the evaluation of low back pain patients. J Med Assoc Thai. 2005;88(3):407–411. [PubMed] [Google Scholar]
- 34.Golriz S., Hebert J.J., Foreman K.B., Walker B.F. The reliability of a portable clinical force plate used for the assessment of static postural control: repeated measures reliability study. Chiropr Man Therap. 2012;20(1):14. doi: 10.1186/2045-709X-20-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruhe A., Fejer R., Walker B. Is there a relationship between pain intensity and postural sway in patients with non-specific low back pain? BMC Musculoskelet Disord. 2011;12(1):162. doi: 10.1186/1471-2474-12-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ringheim I., Austein H., Indahl A., Roeleveld K. Postural strategy and trunk muscle activation during prolonged standing in chronic low back pain patients. Gait Posture. 2015;42(4):584–589. doi: 10.1016/j.gaitpost.2015.09.008. [DOI] [PubMed] [Google Scholar]
- 38.Tsao H., Druitt T.R., Schollum T.M., Hodges P.W. Motor training of the lumbar paraspinal muscles induces immediate changes in motor coordination in patients with recurrent low back pain. J Pain. 2010;11(11):1120–1128. doi: 10.1016/j.jpain.2010.02.004. [DOI] [PubMed] [Google Scholar]
- 39.Borghuis J., Hof L.A., Lemmink K.A. The importance of sensory-motor control in providing core stability. Sports Med. 2008;38(11):893–916. doi: 10.2165/00007256-200838110-00002. [DOI] [PubMed] [Google Scholar]
- 40.Ostelo R.W., de Vet H.C. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol. 2005;19(4):593–607. doi: 10.1016/j.berh.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 41.Popa T., Bonifazi M., Della Volpe R., Rossi A., Mazzocchio R. Adaptive changes in postural strategy selection in chronic low back pain. Exp Brain Res. 2007;177(3):411–418. doi: 10.1007/s00221-006-0683-4. [DOI] [PubMed] [Google Scholar]
- 42.Suresh K. An overview of randomized techniques: an unbiased assessment of outcome in clinical research. J Hum Reprod Sci. 2011;4(1):8–11. doi: 10.4103/0974-1208.82352. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]