Abstract
A 40-year-old male, diagnosed to have WPW syndrome and symptomatic with recurrent palpitations, was taken up for radiofrequency ablation. There was difficulty in coronary sinus cannulation. Coronary venogram revealed coronary sinus atresia with persistent left superior vena cava, and collateral venous pathways draining into the right atrium. This case is discussed for the rare coronary venous anomaly, its embryology and the difficulties in the management during electrophysiological studies.
1. Introduction
Coronary sinus ostial atresia is a rare venous anomaly of the heart and is often associated with a persistent left superior vena cava or drainage via venous collateral pathways into the right or left atrium [1]. Though a benign anomaly, it poses difficulties in coronary sinus cannulation during surgeries and electrophysiology interventions [2].
We report a case of coronary sinus ostial atresia with persistent left sided superior vena cava with venous collateral pathways draining into the right atrium that was not possible to cannulate.
2. Case report
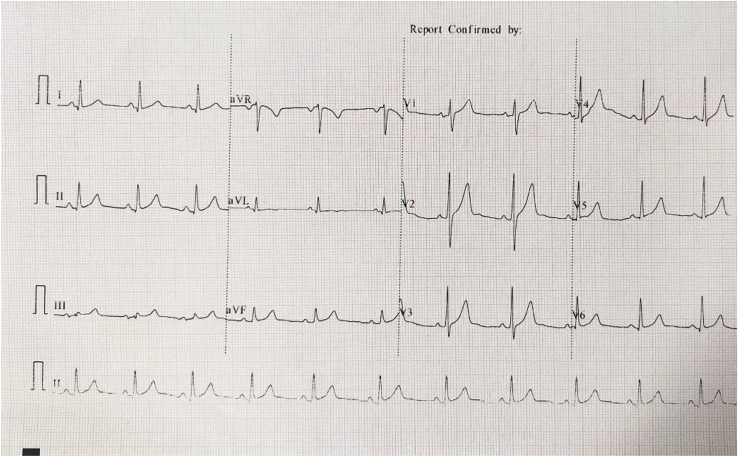
A 40-year-old male presented with history of recurrent palpitation with no history of syncope. On evaluation, his electrocardiogram (ECG) (Fig. 1) revealed a pre-excitation pattern with negative delta wave in lead 1, positive in V1 with no transition across the pre-cordial leads suggestive of a left lateral pathway. The patient was planned for an electrophysiological study with radio-frequency ablation.
Fig. 1.
Baseline 12-lead ECG of patient – negative delta wave in Lead I, no transition of delta wave suggestive of a left-lateral pathway.
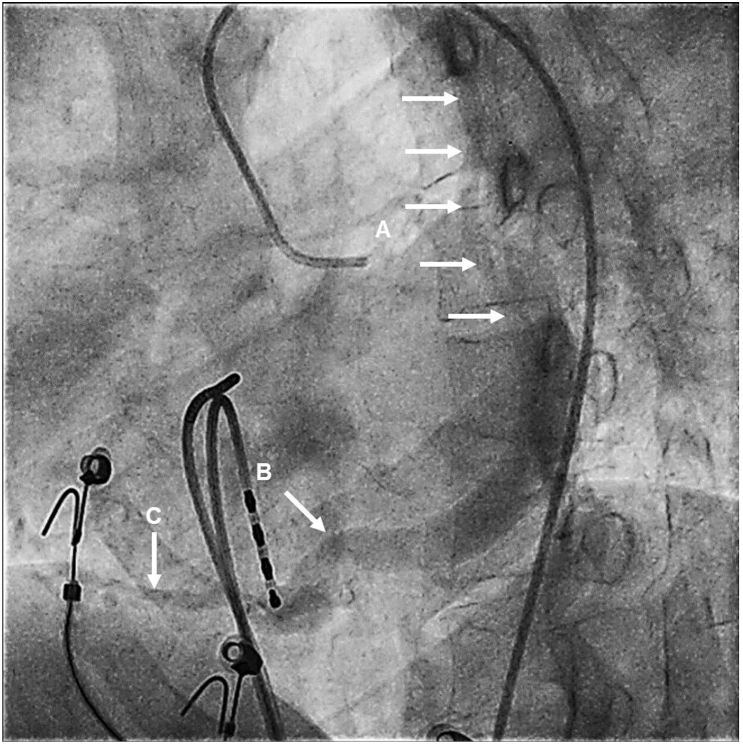
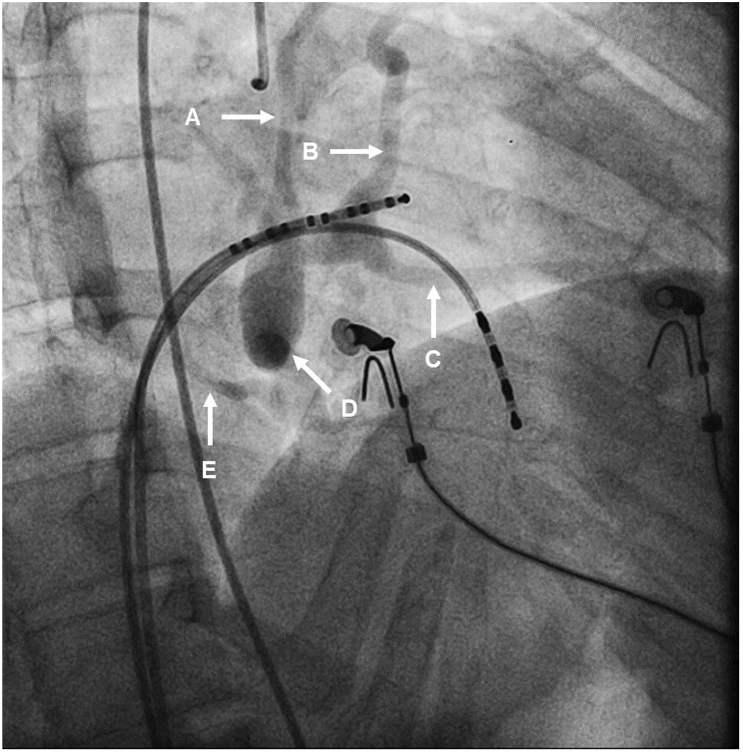
During the procedure, a 6F JSN Quadripolar catheter was inserted into the right ventricle and a 6F CRD2 Quadripolar catheter was placed at the His-bundle. The coronary sinus cannulation was attempted initially by the right femoral venous route and then by the right sided internal jugular route using a 6F deflectable decapolar catheter. Multiple attempts were made to cannulate the coronary sinus but failed. Then, via a 6F right femoral arterial access, a left coronary artery angiogram was performed with 6F Judkins Left – 4 catheter and the cardiac venous anatomy was visualized during the levo-phase of the injection (Fig. 2, 3).
Fig. 2.
Venous phase of the left coronary angiogram in left anterior oblique view – (A) Persistent left superior vena cava (multiple arrows) (B) Absence of coronary sinus drainage into the right atrium (C) Collateral pathways from coronary sinus to the right atrium.
Fig. 3.
Venous phase of the left coronary angiogram in right anterior oblique view – (A) Persistent left superior vena cava (B) Coronary sinus (C) Marginal vein (D) Absence of coronary sinus drainage into the right atrium (E) Collateral pathways from coronary sinus to the right atrium.
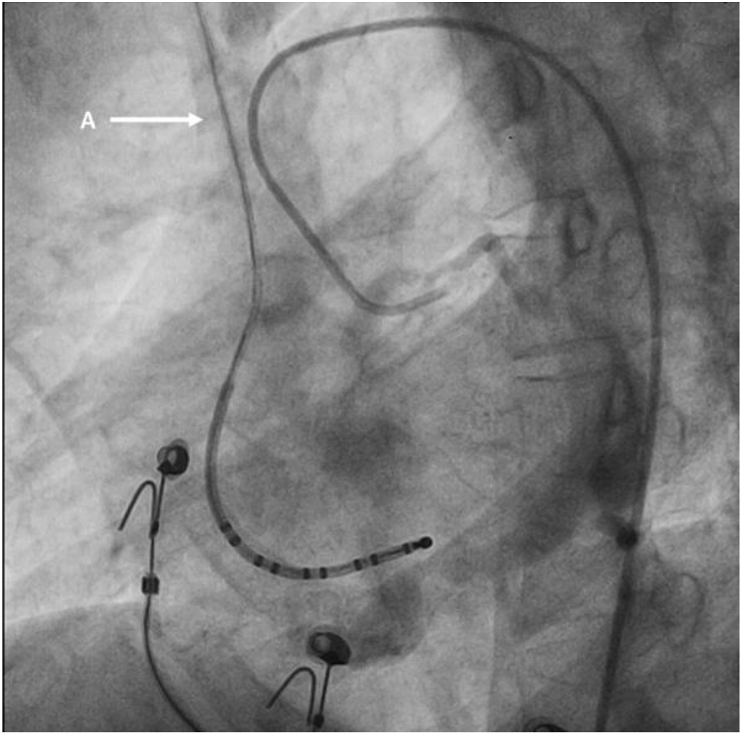
The venous phase of the coronary angiogram revealed coronary sinus atresia with persistent left superior vena cava draining retrogradely into right superior vena cava through communicating cava (Fig. 4). With absence of reference electrodes, the pathway was directly mapped with 7F Webster Green ablation catheter. The earliest ventricular activation was noted at 3 o’ clock position of the mitral valve annulus and successfully ablated with 30 W for 60 seconds. There was no recurrence of symptoms of the patient on follow up.
Fig. 4.
Venous phase of the left coronary angiogram in left anterior oblique view – (A) Right superior vena cava, filling from left superior vena cava through connecting cava (not seen in the picture) and draining into the right atrium.
3. Discussion
The failure to cannulate coronary sinus occurs in 5–10% of cardiac procedures. The causes include coronary sinus stenosis, angulation of the coronary sinus and rarely coronary sinus ostial atresia.
In the embryological development, the sinus venosus divides into two horns, the right and the left. The transverse segment of the sinus venosus shifts rightward and is separated from the left horn of the sinus venosus and the left atrium. This shift pulls the left horn along the posterior atrioventricular groove. The residual left horn progressively degenerates to form the ligament of Marshall. The proximal part of the left horn and the transverse part of the sinus venosus forms the coronary sinus.
At the end of 8 weeks, an anastomosis develops between the right and the left common cardinal veins, that fuse to form the brachiocephalic vein. The left anterior cardinal vein caudal to this anastomosis usually involutes into the ligament of Marshall. Failure of this involution leads to the persistence of left-sided superior vena cava. In coronary sinus atresia, the absence of a direct drainage into the right atrium probably helps maintain the patency of the left sided superior vena cava.
Coronary sinus ostial atresia is a rare coronary anomaly known to occur at an incidence of 0.1% [1] and usually consists of a membranous occlusion at the ostium, with or without interruption along the coronary sinus [2], which prevents drainage of the coronary sinus to the right atrium. In the absence of drainage to the right atrium, the venous return occurs via anomalous pathways and is commonly associated with a persistent left sided superior vena cava. In such a situation, the coronary sinus drains retrogradely into the left sided superior vena cava to the right sided superior vena cava through the connecting cava (with variations of drainage through hemiazygous, or hemiazygous-azygous venous connections) and finally into the right atrium [3]. Additionally, the coronary sinus can drain via anomalous right atrial anastomoses, coronary artery fistulae and through unroofed coronary sinus into the left atrium.
Coronary sinus atresia was first described during autopsy studies. These anomalies are asymptomatic and come to attention only when patients undergo invasive electrophysiological studies or coronary sinus lead placements for cardiac resynchronisation therapy.
Echocardiographic diagnosis of coronary sinus atresia requires high degree of suspicion and a good window and hence rarely reported [4]. The course of the coronary sinus can be delineated by the venous phase of the angiogram. Alternatively, a multidetector computed tomography (MDCT (Fig. 5)) or magnetic resonance imaging (MRI) of the heart can be performed to delineate the coronary sinus anatomy. Further imaging also allows for detection of concomitant abnormalities such as coronary artery fistulas or unroofed coronary sinus with left to right shunting, since these anomalies are noted in approximately 53% patients with coronary sinus atresia [1].
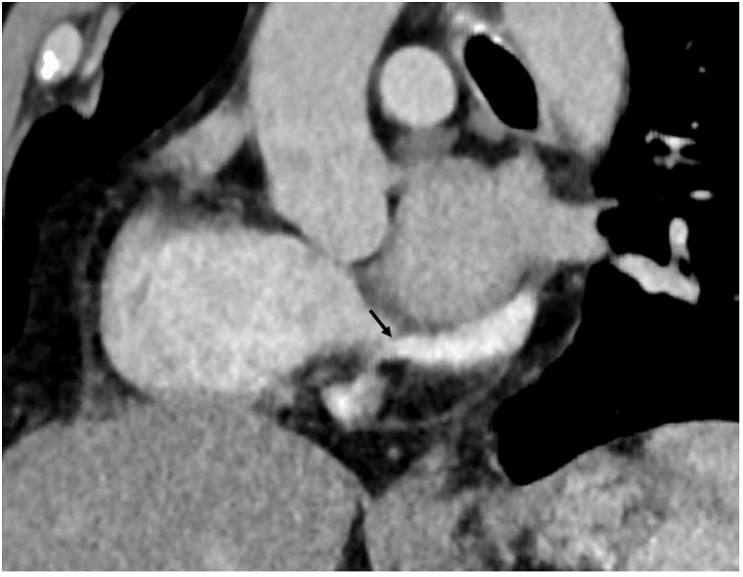
Fig. 5.
Computed tomography – coronal section – Black arrow pointing to the membrane at the coronary sinus. Note the higher opacification in the coronary sinus compared to the right atrium.
Coronary sinus atresia carries a great importance during cardiac surgeries. Inadvertent ligation of the left-sided superior vena cava during Fontan or bi-directional Glenn in a patient with coronary sinus atresia will result in the venous congestion and myocardial ischemia due to the elevation of the trans-capillary pressure with reduced myocardial perfusion pressure. Rarely, catheter induced thrombosis of left superior vena cava can present as acute coronary syndrome [5].
Accessory pathway (AP) development and coronary sinus development occur at similar time (7–8 weeks). Atrioventricular re-entrant tachycardias are more commonly associated with coronary sinus anomalies than atrioventricular nodal re-entrant tachycardias. Additionally, AP are more often located in the left free wall (seen in our patient) and the postero-septal wall. Epithelially derived cells (EDC) is necessary for development of proper arteriovenous boundary and also are essential to provide the electrical isolation between the atria and ventricle [6]. Thus both AP and coronary sinus abnormalities rely on intact targeting by EDC.
Catheter ablation of a left free-wall accessory pathway is usually performed under the guidance of a reference electrode (CS electrodes), though ablation without a reference catheter has been reported in a few experienced centres [7]. The other options include placement of multipolar electrode catheters in the left-atrium after transseptal catheterization which might have facilitated the mapping of the mitral annulus. However, these may lead to unexpected complications given the undefined relationship between the atrial septum and the venous structures. Alternatively, the coronary sinus can be cannulated retrogradely through a persistent left sided vena cava. Mapping of the mitral valve annulus without a reference catheter may be inaccurate but nevertheless achievable with good success rate [7].
4. Conclusion
Coronary sinus atresia with a persistent left-sided superior vena cava is a rare condition that usually comes to attention when there is failure to cannulate the coronary sinus from the right atrium. A coronary angiogram can be performed on table to confirm coronary sinus atresia and delineate cardiac venous anatomy. In electrophysiological studies, alternate ways to map the mitral valve annulus can be tried or direct ablation can be attempted with modest success. Although it increases the technical difficulty of coronary sinus cannulation, it does not prevent successful ablation of a left sided accessory pathway.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Shum J.S., Kim S.M., Choe Y.H. Multidetector CT and MRI of ostial atresia of the coronary sinus, associated collateral venous pathways and cardiac anomalies. Clin Radiol. 2012;67(12):e47–e52. doi: 10.1016/j.crad.2012.07.013. [DOI] [PubMed] [Google Scholar]
- 2.Santoscoy R., Walters H.L., 3rd, Ross R.D., Lyons J.M., Hakimi M. Coronary sinus ostial atresia with persistent left superior vena cava. Ann Thorac Surg. 1996;61(3):879–882. doi: 10.1016/0003-4975(95)01137-4. [DOI] [PubMed] [Google Scholar]
- 3.Saremi F., Muresian H., Sánchez-Quintana D. Coronary veins: comprehensive CT-anatomic classification and review of variants and clinical implications. RadioGraphics. 2012;32(1):E1–E32. doi: 10.1148/rg.321115014. [DOI] [PubMed] [Google Scholar]
- 4.Paul J.J., Williams R.V., Minich L.L.A., Tani L.Y. Echocardiographic diagnosis of coronary sinus ostial atresia. J Am Soc Echocardiogr. 2002;15(9):991–993. doi: 10.1067/mje.2002.120893. [DOI] [PubMed] [Google Scholar]
- 5.Qanadli S.D., Rolf T., Glauser F., Delay D., Beigelman-Aubry C., Pretre R. Coronary sinus atresia with persistent left superior vena cava: unusual clinical presentation and endovascular management. Cardiovasc Interv Radiol. 2014;37(3):825–828. doi: 10.1007/s00270-013-0719-7. [DOI] [PubMed] [Google Scholar]
- 6.Patel S.M., McLeod C.J., Friedman P.A., Liu X., Asirvatham S.J. Successful ablation of a left-sided accessory pathway in a patient with coronary sinus atresia and arteriovenous fistula: clinical and developmental insights. Indian Pacing Electrophysiol J. 2011;11(2):43–49. [PMC free article] [PubMed] [Google Scholar]
- 7.Kuck K.H., Schluter M. Single-catheter approach to radiofrequency current ablation of left-sided accessory pathways in patients with Wolff-Parkinson-White syndrome. Circulation. 1991;84(6):2366–2375. doi: 10.1161/01.cir.84.6.2366. [DOI] [PubMed] [Google Scholar]