Abstract
Purpose
To assess the clinical and radiographic outcomes of coronoid process fractures surgically managed with buttress plate fixation via a medial approach.
Methods
A retrospective review of all coronoid fractures surgically fixed in our institution using a buttress plate technique via a medial approach between June 2012 and April 2015 by the senior author was performed. These fractures were all sizeable fractures contributing to persistent elbow instability in terrible triad or varus posteromedial rotatory instability injury patterns. A prospective telephone questionnaire was conducted to assess patient outcomes using the disabilities of the arm, shoulder and hand (DASH) score and Mayo hlbow performance score (MEPS).
Results
Twelve patients were included in the study, comprising 10 males and 2 females with an average age of 39 years (range, 19–72 years). Mean follow-up was 16 months (range, 4–18 months). The average time to radiographic union was 4 months (range, 3–7 months). Range of motion measurements at final follow-up were obtained in 11 out of 12 patients, with one patient defaulting follow-up. All 11 patients displayed a functional elbow range of motion of at least 30°-130°, with an average arc of motion of 130° (range, 110° −140°), mean elbow flexion of 134° (range, 110° −140°) and mean flexion contracture of 3° (range, 0° −20°). The mean DASH score was 16 (range, 2.5–43.8) and the mean MEPS was 75 (range, 65–100). Complications observed included one patient with a superficial wound infection which resolved with a course of oral antibiotics and one patient with radiographic evidence of heterotopic ossification which was conservatively managed. No residual elbow instability was observed and no reoperations were performed.
Conclusion
Buttress plate fixation via a medial approach of coronoid process fractures that contribute to persistent elbow instability represents a reliable method of treatment that produces satisfactory and predictable outcomes.
Keywords: Coronoid process, Anteromedial facet fracture, Complex elbow instability, Terrible triad injury
Introduction
Coronoid process fractures are rarely isolated injuries and typically occur in the setting of complex elbow fracture-dislocations.1, 2, 3, 4, 5, 6 These fractures may be classified according to the Reagan and Morrey7 or O'Driscoll classifications,3 and are typically observed occurring in one of three injury patterns5: (1) terrible triad injuries – these are typically a result of posterolateral elbow dislocation and are often associated with a small (O'Driscoll tip fracture, Reagan-Morrey type I and II) coronoid fragment; (2) varus posteromedial rotatory instability – this injury mechanism typically results in an anteromedial coronoid fragment (O'Driscoll anteromedial fracture) with concomitant injury to the lateral collateral ligament (LCL) complex, most important of which being the lateral ulnar collateral ligament (LUCL); (3) trans-olecranon fracture-dislocations – these are usually associated with a large basal coronoid fragment (O'Driscoll base fracture, Reagan-Morrey type III).
While not all coronoid fractures need to be addressed surgically, the exact indications and optimal techniques for surgical fixation are not well established.7, 8, 9, 10, 11, 12, 13 Because of the heterogeneity of injury patterns in which coronoid fractures occur, evidence guiding the management of these fractures is difficult to interpret in light of the concomitant elbow injuries they are often associated with. 2 significant questions remain unanswered. (1) Should all coronoid fractures associated with terrible triad injuries and anteromedial coronoid fractures associated with varus posteromedial instability routinely be fixed? (2) What is the optimum method of coronoid fracture fixation?
The technique of surgically fixing coronoid process fractures using a buttress plate through a formal medial approach has been described in the literature and represents a biomechanically sound method of fixation for coronoid fractures of a shear type.1, 2, 3, 4, 5 No study in the literature has specifically investigated the outcomes of coronoid fractures treated in this fashion. Concerns remain about the potential risks associated with a medial approach, including surgeon's unfamiliarity, the potential risks for increased stiffness, as well as iatrogenic injury to the ulnar nerve and the medial antebrachial cutaneous nerve to the forearm.14 The objective of this study was to assess the clinical and radiographic outcomes of coronoid process fractures surgically managed with buttress plate fixation via a medial approach.
Methods
A retrospective review of all coronoid fractures surgically fixed in our institution between June 2012 and April 2015 by the senior author (n = 13) was performed after obtaining ethics approval from our Institutional Review Board. One patient with a trans-olecranon fracture pattern was excluded from the study because a different fixation strategy was used (the coronoid fragment in this case was approached posteriorly through the olecranon fracture site and fixed with a headless compression screw), leaving 12 patients with coronoid fractures that were fixed with a buttress plate via a medial approach.
Patient demographics
10 males and 2 females with coronoid fractures were reviewed in our study. The mean age was 39 years (range, 19–72 years). The right elbow was injured in 5 cases and the left in 7. The most common mechanism of injury was a road traffic accident (5 cases), followed by a fall from standing height (4 cases) and a fall from height greater than 1 m (3 cases). All fractures were closed. Concomitant fractures of the same limb occurred in 4 cases, with 3 ipsilateral distal radius fractures and one ipsilateral proximal humerus fractures. Mean follow-up duration was 16 months (range, 4–18 months).
Indications for fixation
Our indications for fixation were all coronoid fractures which contributed to persistent elbow instability if left unfixed. This fell into 2 broad categories: anteromedial coronoid fractures (subtype II or III) with accompanying LCL injury, and terrible triad injuries in which the elbow continued to demonstrate instability after the lateral sided structures (radial head and LCL) had been addressed. For terrible triad injuries, our clinical protocol followed a specific sequence. (1) The radial head was first addressed (open reduction with internal fixation or radial head replacement based on the degree of fracture comminution) via a lateral (Kocher or Kaplan) approach. (2) The LCL and common extensor origin were repaired with transosseous sutures and/or suture anchors. (3) Stability of the elbow was reassessed intra-operatively through a full range of motion. Persistent instability is diagnosed if a dislocation or subluxation of the ulnohumeral joint was clinically or fluoroscopically detected through a full range of elbow motion. Any fluoroscopic evidence of a non-congruent ulnohumeral articulation throughout the entire elbow range of motion would also deem the elbow as being unstable. (4) If persistent instability was demonstrated, usually in the setting of a sizeable coronoid fracture (Regan-Morrey type II fracture or larger O'Driscoll tip fracture approximating 50% of the total coronoid height), a separate medial approach was used to fix the coronoid fracture with a buttress plate and repair the medial collateral ligament (MCL) and common flexor origin with transosseous sutures and/or suture anchors.
Surgical technique
Under general or regional anaesthesia, the patient was placed in a supine position with the injured extremity supported on a hand table. Depending on the size of the coronoid fracture, the specific medial approach to the elbow was chosen. For smaller fractures not involving the sublime tubercle, the “over the top” approach splitting the flexor-pronator mass as described by Hotchkiss15 was utilised. Larger coronoid fractures were approached more posteriorly with elevation of the entire flexor-pronator mass anteriorly. Additional anterior exposure of the coronoid could be obtained by sub-periosteal elevation of the brachialis muscle off its insertion on the proximal ulna. In the setting of a terrible triad injury with significant disruption of the medial flexor pronator mass, the most relevant soft tissue window was extended and utilised. In all cases, the antebrachial cutaneous nerve was identified and avoided, while the ulnar nerve was identified, decompressed, and protected prior to the deep dissection. We did not routinely perform ulnar nerve transposition. Only if the nerve was found to be subluxable prior to wound closure would a subcutaneous transposition be performed.
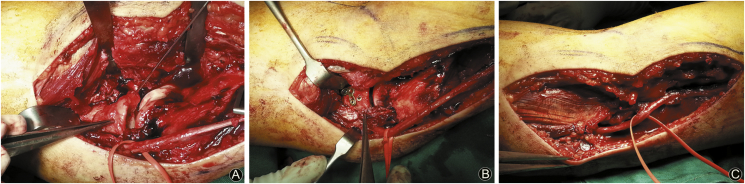
Once the coronoid fracture was exposed, preliminary reduction with K-wires was performed and checked on fluoroscopy, followed by definitive fixation with a 1.5 mm or 2.0 mm T-plate as a buttress plate and augmented with headless compression screws if the fracture pattern allowed. The flexor-pronator mass was then repaired using sutures (if a split of the flexor-pronator mass had been performed) or suture anchors (if elevation of the entire flexor-pronator mass from its origin on the medial epicondyle had been performed) (Fig. 1). Avulsion of the MCL from the medial epicondyle was also repaired at the same time if present. This was usually in the setting of a terrible triad injury.
Fig. 1.
(A) Medial approach with flexor-pronator mass elevated to expose coronoid fragment (held with K-wire); (B) Coronoid fragment fixed with lag screw and buttress plate; (C) Final repair with flexor-pronator mass repaired with suture anchors and ulnar nerve protected.
Stability of the elbow through its entire range of motion was confirmed on-table and using fluoroscopy. In cases of anteromedial coronoid fractures without radial head fractures, if persistent varus laxity was noted after the medial side had been addressed, as in majority of the cases (6 out of 8 cases), then a separate lateral incision was made to repair the LUCL and common extensor origin.
Post-operatively all patients were started on gentle mobilisation of the elbow on the first day following surgery, with gradual progression to passive and active-assisted range of motion exercises as tolerated. Active range of motion and strengthening exercises were permitted from the 6th week onwards. We did not routinely use a hinged elbow brace for our patients.
Clinical and radiographic evaluation
Patients were routinely followed-up in the outpatient setting with clinical and radiographic evaluation by the senior author at each follow-up visit. Active elbow arc of motion was measured and elbow instability was assessed noting any symptoms or signs of subluxation throughout the entire elbow range of motion. Standard anteroposterior and lateral radiographs of the elbow were reviewed for assessment of joint concentricity, fracture reduction, implant position, fracture union, heterotopic ossification and evidence of arthrosis. Stress radiographs were not routinely performed.
Complications assessed included wound infection, post-operative elbow instability, malunion or non-union, implant loosening or screw back-out, re-fracture, neurologic injury and heterotopic ossification. Radiographs and medical records of all patients were reviewed retrospectively. In addition, a prospective telephone questionnaire was administered and final functional outcome was evaluated using the Mayo elbow performance score (MEPS) and disabilities of the arm, shoulder and hand (DASH) score.
Results
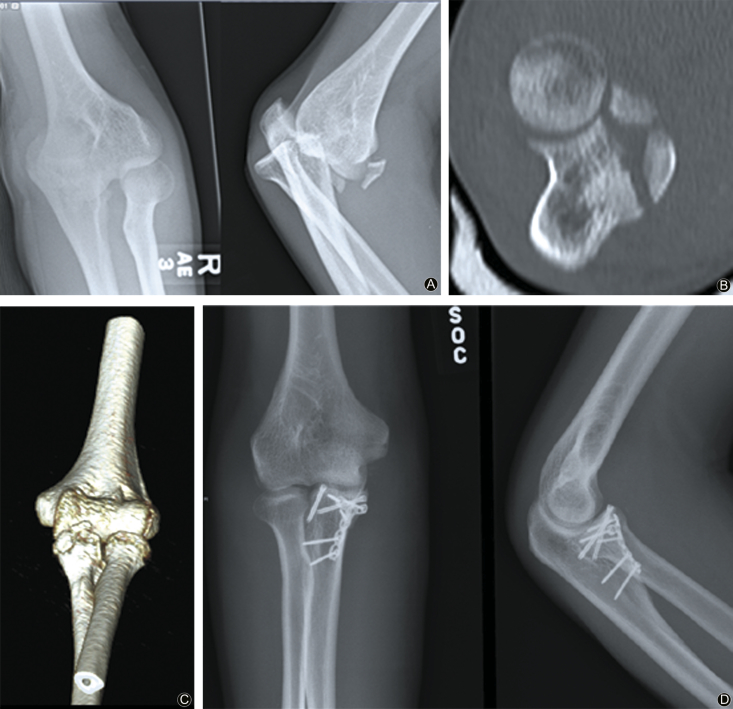
O'Driscoll anteromedial type coronoid fractures accounted for 8 out of the 12 cases in our series (Fig. 2). Terrible triad injuries accounted for 4 cases, with the coronoid fracture in all of these cases being a sizeable O'Driscoll tip fracture (Regan Morrey type II) involving at least 50% of the height of the coronoid process (Fig. 3).
Fig. 2.
(A) Pre-operative radiographs; (B) Computed tomography image; (C) 3D reconstruction image; (D) Post-operative radiographs of terrible triad injury with sizeable coronoid fragment treated with buttress plating via a medial approach.
Fig. 3.
(A) Pre-operative radiographs; (B) Computed tomography image; (C) 3D reconstruction; (D) Post-operative radiographs of anteromedial coronoid fracture treated with buttress plating via a medial approach.
Range of motion measurements at final follow-up were obtained in 11 out of 12 patients, with one patient defaulting follow-up. The mean elbow flexion at final follow-up was 134° (range, 110°-140°) and the mean flexion contracture was 3° (range, 0°-20°) with a mean arc of ulnohumeral motion of 130° (range, 110°-140°). All patients achieved a functional elbow range of motion defined as a flexion-extension arc of 30°-130°.16
The mean DASH score was 16 (range, 2.5–43.8) and the mean MEPS was 75 (range, 65–100). Complications observed in our series included one case of a superficial wound infection that was successfully treated with a short course of oral antibiotics. There were no cases of recurrent dislocation or subluxation, nor any clinically detectable ulnar nerve palsy or neuropraxia, medial antebrachial cutaneous nerve of forearm neuroma or medial forearm sensory deficits.
Radiographic evaluation demonstrated bony union of all coronoid fractures. The mean time to radiographic union was 4 months (range 3–7 months). No malunions or implant failures were observed. One patient with radiologically apparent heterotopic ossification was noted which was conservatively managed as he was otherwise clinically asymptomatic. No radiographic evidence of ulnohumeral arthrosis was observed in our series at the time of our last follow-up.
Discussion
It is widely accepted that the coronoid process plays a vital role in maintaining the stability of the elbow joint by acting as a buttress against posterior translation and varus rotation of the ulna on the distal humerus.2, 17, 18 While the original Regan and Morrey classification system divided coronoid fractures based solely on their size on the lateral view of the plain radiograph, current thinking places greater emphasis on the fracture morphology seen on the computed tomography scan, the mechanism of injury, and the ability of the residual intact coronoid to maintain elbow stability than the size of the fracture fragment alone.5 Accordingly, the critical size and morphology of coronoid fracture that renders an elbow unstable and hence necessitates surgical fixation remains unclear.
The anteromedial facet of the coronoid acts as a buttress to varus posteromedial instability, and even seemingly small fractures of this facet have been shown to lead to poor functional outcomes with conservative management, due to the propensity of elbows with these injuries to go into varus collapse and eventually develop ulnohumeral arthrosis.6, 19, 20 A biomechanical study comparing the kinematics of the elbow joint with operative and non-operative management of anteromedial facet fractures in conjunction with LCL repair found that only the smallest of these fractures (subtype I) allowed elbow stability to be maintained with non-operative management, whereas all other fracture sizes demonstrated significantly improved stability with operative fixation.21 In line with these findings, our protocol surgically addresses all subtype 2 and 3 anteromedial coronoid fractures which contribute to elbow instability. In such fractures, a medial plate which helps to restore the anteromedial buttressing effect of the coronoid seems to be most logical from a biomechanical point of view. It is worth mentioning that in all the 8 cases of anteromedial fractures that we fixed, there was pre-operative evidence of significant elbow instability and soft tissue disruption which necessitated fixation. This is usually in the setting of a frank ulnohumeral subluxation or dislocation which required closed reduction, a residual incongruent joint reduction on radiographs, or significant elbow varus laxity on examination. For subtype 1 anteromedial coronoid fractures, we elected to treat them non-operatively, as the literature is still unclear if treating these fractures non-operatively will result in significant consequences. This decision is also based on the senior author's experience that some of these small subtype 1 anteromedial fractures regain good elbow function and range of motion when managed non-operatively.
In terrible triad injuries, the coronoid fracture that occurs is usually small and transverse in orientation, resulting from shearing of the tip of the coronoid process as it contacts the trochlea with posterolateral dislocation of the elbow.5 Some authors routinely fix the coronoid from the lateral side prior to addressing the radial head,22 but the necessity to fix all of these (usually small) coronoid fractures has been questioned.13 Closkey et al.23 found no significant difference in elbow stability with isolated fractures involving up to 50% of the coronoid process. Similarly, Schneeberger et al.24 found that in the presence of an intact radial head (either uninjured or surgically replaced with a prosthesis), only fractures involving greater than 50% of the coronoid height destabilised the elbow. Another biomechanical study by Beingessner et al.25 tested suture fixation of small type 1 coronoid fractures in a terrible triad model and found that such repair conferred little effect on overall elbow stability. Similarly we believe that most small coronoid fractures do not need to be fixed surgically, and the lateral approach in our surgical protocol for terrible triads is only used for addressing the radial head and LCL complex. In fact, the majority of terrible triads surgically treated by the senior author had a small (less than 50% height) coronoid tip fracture which were left unfixed (and hence were not included in this study). These patients undergo radial head fixation or replacement, followed by repair of the LCL complex, and the elbows were all found to be stable intra-operatively without the need to address the small coronoid tip fractures. In the senior author's experience, these patients regain good elbow function and range of motion post-operatively.
Only if the elbow continues to demonstrate persistent instability after the radial head and LCL complex have been addressed do we then proceed to fix the coronoid. There were 4 of such cases during the period of our research, which were included in our study, and all 4 of these patients were noted to have fairly sizeable coronoid tip fractures of about 50% of the coronoid height. For such large fracture fragments we again believe that plate fixation from the medial side provides the most rigid and biomechanically sound method of restoring the buttress effect of the coronoid. The utilisation of a medial approach also gives us the ability to repair the MCL which is often compromised in terrible triad injuries. This treatment algorithm to ‘go medial’ in the setting of persistent elbow instability after addressing the radial head and LCL, is also supported by the findings of Beingessner et al.,25 which demonstrated that a MCL repair conferred more stability than suture fixation of a small coronoid fracture through the lateral approach in the setting of persistent elbow instability after radial head replacement and LCL repair in a terrible triad model.
The clinical and radiographic results of our case series are comparable with other case series in the literature studying surgical fixation of coronoid fractures.26, 27, 28, 29, 30 Significantly, a functional elbow arc of motion of at least 30-130° of flexion-extension was achieved in all our patients, and persistent symptomatic elbow instability or major complications requiring revision surgery were observed in none. We believe this represents a satisfactory outcome in patients with a complex and challenging elbow injury. We also hope to impress upon the reader that the utilisation of a medial approach to address sizeable coronoid fixation confers the surgeon the ability to rigidly fix the fracture with a buttress plate, and at the same time address any MCL injury especially in the setting of a terrible triad injury. The use of a medial approach is also safe with no patients having significant ulnar nerve or medial antebrachial nerve injuries or stiffness in our series.
There are several limitations of this study. Firstly, this was a retrospective case series including a relatively small number of patients with no control group for comparison. While unsurprising given the low incidence of coronoid fractures in the first place, this limitation makes it difficult to substantiate any treatment recommendations based on our study alone. Secondly, the lack of long-term follow-up in our study prevents us from being able to make conclusions about the effect of our interventions on the development of ulnohumeral arthrosis. A contributing factor to this was that the majority of our patients had achieved adequate functional recovery and hence elected not to return for further follow-up or treatment.
Nonetheless, we believe that our study lends further support to various articles in the literature in recommending fixation of sizeable coronoid fractures (anteromedial subtype 2 and 3 coronoid fractures, and more than 50% height coronoid fractures in the setting of a terrible triad injury), and is the first in the literature to show good outcomes with no significant complications using a medial approach and a rigid buttress plating technique to address coronoid fractures in all our cases.
The optimal treatment method for treating coronoid fractures remains unclear, although current thinking places significant emphasis on the restoration of elbow stability sufficiently to enable early mobilisation and rehabilitation. We believe that buttress plate fixation of coronoid process fractures that contribute to persistent elbow instability via a medial approach represents a reliable method of treatment that produces satisfactory and predictable short-term outcomes.
Funding
Nil.
Acknowledgements
The authors wish to thank doctors, nurses and allied health colleagues from Khoo Teck Puat Hospital involved in the care of the patients.
Footnotes
Peer review under responsibility of Chinese Medical Association.
Ethical statement
Ethics approval for this study was obtained from the National Healthcare Group Domain Specific Review Board.
Conflicts of interest
The authors declare that there are no conflicts of interest.
References
- 1.Steinmann S.P. Coronoid process fracture. J Am Acad Orthop Surg. 2008;16:519–529. [PubMed] [Google Scholar]
- 2.Budoff J.E. Coronoid fractures. J Hand Surg Am. 2012;37:2418–2423. doi: 10.1016/j.jhsa.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 3.O'Driscoll S.W., Jupiter J.B., Cohen M.S. Difficult elbow fractures: pearls and pitfalls. Instr Course Lect. 2003;52:113–134. [PubMed] [Google Scholar]
- 4.Ring D. Fractures of the coronoid process of the ulna. J Hand Surg Am. 2006;31:1679–1689. doi: 10.1016/j.jhsa.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 5.Doornberg J.N., Ring D. Coronoid fracture patterns. J Hand Surg Am. 2006;31:45–52. doi: 10.1016/j.jhsa.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Doornberg J.N., Ring D.C. Fracture of the anteromedial facet of the coronoid process. J Bone Joint Surg Am. 2006;88:2216–2224. doi: 10.2106/JBJS.E.01127. [DOI] [PubMed] [Google Scholar]
- 7.Regan W., Morrey B.F. Classification and treatment of coronoid process fractures. Orthopedics. 1992;15:845–848. doi: 10.3928/0147-7447-19920701-09. [DOI] [PubMed] [Google Scholar]
- 8.Morrey B.F. Complex instability of the elbow. Instr Course Lect. 1998;47:157–164. [PubMed] [Google Scholar]
- 9.Tashjian R.Z., Katarincic J.A. Complex elbow instability. J Am Acad Orthop Surg. 2006;14:278–286. doi: 10.5435/00124635-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Wells J., Ablove R.H. Coronoid fractures of the elbow. Clin Med Res. 2008;6:40–44. doi: 10.3121/cmr.2008.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garrigues G.E., Wray W.H., 3rd, Lindenhovius A.L. Fixation of the coronoid process in elbow fracture-dislocations. J Bone Joint Surg Am. 2011;93:1873–1881. doi: 10.2106/JBJS.I.01673. [DOI] [PubMed] [Google Scholar]
- 12.Mathew P.K., Athwal G.S., King G.J. Terrible triad injury of the elbow: current concepts. J Am Acad Orthop Surg. 2009;17:137–151. doi: 10.5435/00124635-200903000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Papatheodorou L.K., Rubright J.H., Heim K.A. Terrible triad injuries of the elbow: does the coronoid always need to be fixed? Clin Orthop Relat Res. 2014;472:2084–2091. doi: 10.1007/s11999-014-3471-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhou C.W., Xu J.X., Lin J.T. Comparison of a single approach versus double approaches for the treatment of terrible triad of elbow – a retrospective study. Int J Surg. 2018;51:49–55. doi: 10.1016/j.ijsu.2018.01.012. [DOI] [PubMed] [Google Scholar]
- 15.Hotchkiss R.N., Kasparyan G.N. The medial “Over the top” approach to the elbow. Tech Orthop. 2000;15:105–112. [Google Scholar]
- 16.Morrey B.F., Askew L.J., Chao E.Y. A biomechanical study of normal functional elbow motion. J Bone Joint Surg Am. 1981;63:872–877. [PubMed] [Google Scholar]
- 17.Reichel L.M., Milam G.S., Hillin C.D. Osteology of the coronoid process with clinical correlation to coronoid fractures in terrible triad injuries. J Shoulder Elbow Surg. 2013;22:323–328. doi: 10.1016/j.jse.2012.10.038. [DOI] [PubMed] [Google Scholar]
- 18.Reichel L.M., Morales O.A. Gross anatomy of the elbow capsule: a cadaveric study. J Hand Surg Am. 2013;38:110–116. doi: 10.1016/j.jhsa.2012.09.031. [DOI] [PubMed] [Google Scholar]
- 19.Sanchez-Sotelo J., O'Driscoll S.W., Morrey B.F. Medial oblique compression fracture of the coronoid process of the ulna. J Shoulder Elbow Surg. 2005;14:60–64. doi: 10.1016/j.jse.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 20.Sanchez-Sotelo J., O'Driscoll S.W., Morrey B.F. Anteromedial fracture of the coronoid process of the ulna. J Shoulder Elbow Surg. 2006;15:e5–e8. doi: 10.1016/j.jse.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 21.Pollock J.W., Brownhill J., Ferreira L. The effect of anteromedial facet fractures of the coronoid and lateral collateral ligament injury on elbow stability and kinematics. J Bone Joint Surg Am. 2009;91:1448–1458. doi: 10.2106/JBJS.H.00222. [DOI] [PubMed] [Google Scholar]
- 22.Kovacevic D., Vogel L.A., Levine W.N. Complex elbow instability: radial head and coronoid. Hand Clin. 2015;31:547–556. doi: 10.1016/j.hcl.2015.06.004. [DOI] [PubMed] [Google Scholar]
- 23.Closkey R.F., Goode J.R., Kirschenbaum D. The role of the coronoid process in elbow stability. A biomechanical analysis of axial loading. J Bone Joint Surg Am. 2000;82:1749–1753. doi: 10.2106/00004623-200012000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Schneeberger A.G., Sadowski M.M., Jacob H.A. Coronoid process and radial head as posterolateral rotatory stabilizers of the elbow. J Bone Joint Surg Am. 2004;86:975–982. doi: 10.2106/00004623-200405000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Beingessner D.M., Stacpoole R.A., Dunning C.E. The effect of suture fixation of type I coronoid fractures on the kinematics and stability of the elbow with and without medial collateral ligament repair. J Shoulder Elbow Surg. 2007;16:213–217. doi: 10.1016/j.jse.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 26.Pugh D.M., Wild L.M., Schemitsch E.H. Standard surgical protocol to treat elbow dislocations with radial head and coronoid fractures. J Bone Joint Surg Am. 2004;86:1122–1130. doi: 10.2106/00004623-200406000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Forthman C., Henket M., Ring D.C. Elbow dislocation with intraarticular fracture: the results of operative treatment without repair of the medial collateral ligament. J Hand Surg Am. 2007;32:1200–1209. doi: 10.1016/j.jhsa.2007.06.019. [DOI] [PubMed] [Google Scholar]
- 28.Lindenhovius A.L., Jupiter J.B., Ring D. Comparison of acute versus subacute treatment of terrible triad injuries of the elbow. J Hand Surg Am. 2008;33:920–926. doi: 10.1016/j.jhsa.2008.02.007. [DOI] [PubMed] [Google Scholar]
- 29.Rhyou I.H., Kim K.C., Lee J.H. Strategic approach to O'Driscoll type 2 anteromedial coronoid facet fracture. J Shoulder Elbow Surg. 2014;23:924–932. doi: 10.1016/j.jse.2014.02.016. [DOI] [PubMed] [Google Scholar]
- 30.Park S.M., Lee J.S., Jung J.Y. How should anteromedial coronoid facet fracture be managed? A surgical strategy based on O'Driscoll classification and ligament injury. J Shoulder Elbow Surg. 2015;24:74–82. doi: 10.1016/j.jse.2014.07.010. [DOI] [PubMed] [Google Scholar]