Abstract
The Central Brain Tumor Registry of the United States (CBTRUS), in collaboration with the Centers for Disease Control and Prevention and National Cancer Institute, is the largest population-based registry focused exclusively on primary brain and other central nervous system (CNS) tumors in the United States (US) and represents the entire US population. This report contains the most up-to-date population-based data on primary brain tumors available and supersedes all previous reports in terms of completeness and accuracy. All rates are age-adjusted using the 2000 US standard population and presented per 100,000 population. The average annual age-adjusted incidence rate (AAAIR) of all malignant and non-malignant brain and other CNS tumors was 23.41 (Malignant AAAIR = 7.08, non-Malignant AAAIR = 16.33). This rate was higher in females compared to males (25.84 versus 20.82), Whites compared to Blacks (23.50 versus 23.34), and non-Hispanics compared to Hispanics (23.84 versus 21.28). The most commonly occurring malignant brain and other CNS tumor was glioblastoma (14.6% of all tumors), and the most common non-malignant tumor was meningioma (37.6% of all tumors). Glioblastoma was more common in males, and meningioma was more common in females. In children and adolescents (age 0–19 years), the incidence rate of all primary brain and other CNS tumors was 6.06. An estimated 86,010 new cases of malignant and non-malignant brain and other CNS tumors are expected to be diagnosed in the US in 2019 (25,510 malignant and 60,490 non-malignant). There were 79,718 deaths attributed to malignant brain and other CNS tumors between 2012 and 2016. This represents an average annual mortality rate of 4.42. The five-year relative survival rate following diagnosis of a malignant brain and other CNS tumor was 35.8%, and the five-year relative survival rate following diagnosis of a non-malignant brain and other CNS tumors was 91.5%.
Executive Summary
The Central Brain Tumor Registry of the United States (CBTRUS), in collaboration with the Centers for Disease Control and Prevention (CDC) and National Cancer Institute (NCI), is the largest population-based registry focused exclusively on primary brain and other central nervous system (CNS) tumors in the United States (US) and represents the entire US population. The CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016 contains the most up-to-date population-based data on primary brain tumors available through the surveillance system in the US and supersedes all previous reports in terms of completeness and accuracy, thereby providing a current comprehensive source for the descriptive epidemiology of these tumors. All rates are age-adjusted using the 2000 US standard population and presented per 100,000 population.
Incidence
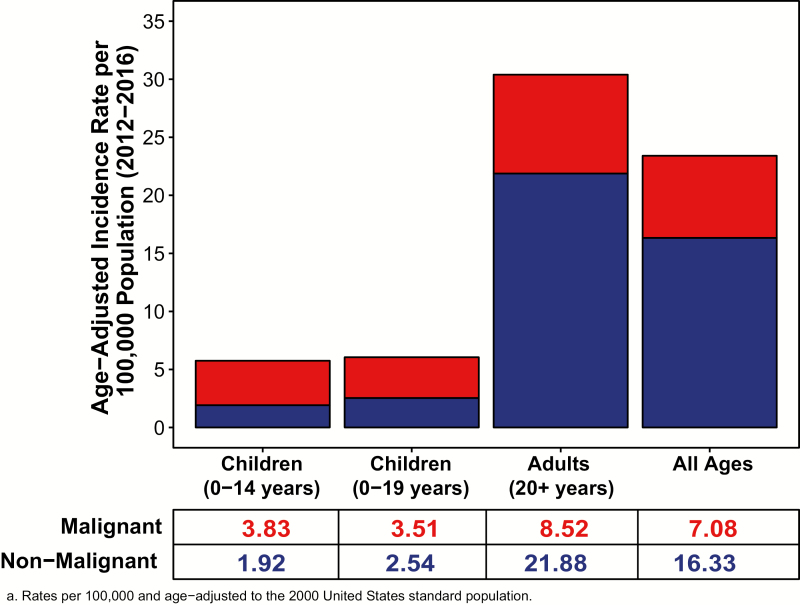
The average annual age-adjusted incidence rate of all malignant and non-malignant brain and other CNS tumors was 23.41 per 100,000 between 2012 and 2016. This rate was higher in females compared to males (25.84 versus 20.82 per 100,000), Whites compared to Blacks (23.50 versus 23.34 per 100,000), and non-Hispanics (of any race) compared to Hispanics (23.84 versus 21.28 per 100,000).
The average annual age-adjusted incidence rate of malignant brain and other CNS tumors was 7.08 per 100,000.
The average annual age-adjusted incidence rate of non-malignant brain and other CNS tumors was 16.33 per 100,000.
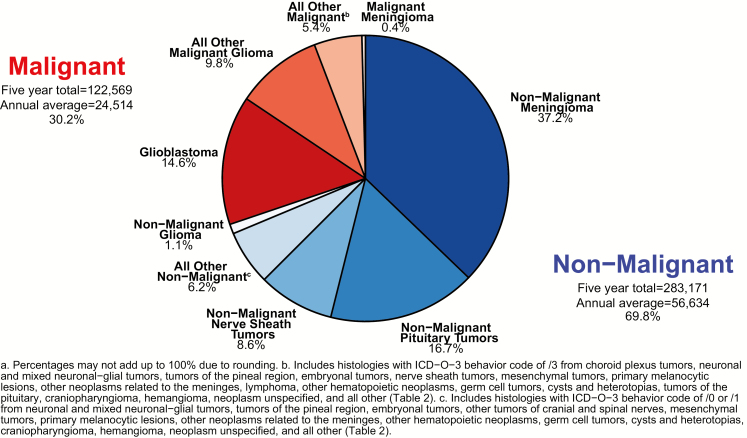
Approximately 30.2% of all brain and other CNS tumors were malignant and 69.8% were non-malignant, which makes non-malignant tumors more than twice as common as malignant tumors.
The most commonly occurring malignant brain and other CNS tumor was glioblastoma (14.6% of all tumors and 48.3% of malignant tumors), and the most common non-malignant tumor was meningioma (37.6% of all tumors and 53.3% of non-malignant tumors). Glioblastoma was more common in males, and meningioma was more common in females.
In children and adolescents (age 0–19 years), the incidence rate of malignant and non–malignant brain and other CNS tumors was 6.06 per 100,000 between 2012 and 2016. Incidence was higher in females compared to males (6.13 versus 5.98 per 100,000), Whites compared to Blacks (6.29 versus 4.71 per 100,000), and non-Hispanics compared to Hispanics (6.35 versus 5.14 per 100,000).
An estimated 86,010 new cases of malignant and non-malignant brain and other CNS tumors are expected to be diagnosed in the US in 2019. This includes an expected 25,510 malignant and 60,490 non-malignant tumors.
Mortality
There were 79,718 deaths attributed to malignant brain and other CNS tumors between 2012 and 2016. This represents an average annual mortality rate of 4.42 per 100,000, and an average of 15,944 deaths per year caused by malignant brain and other CNS tumors.
Survival
The five-year relative survival rate following diagnosis of a malignant brain and other CNS tumor was 35.8%. Five-year relative survival was lowest for glioblastoma (6.8%). Survival following diagnosis with a malignant brain and other CNS tumor was highest in persons age 0–14 years (74.7%), compared to those ages 15–39 years (71.3%) or 40+ years (21.3%).
The five-year relative survival rate following diagnosis of a non-malignant brain and other CNS tumor was 91.5%. Five-year relative survival was highest for nerve sheath tumors (99.3%) and lowest for primary melanocytic lesions (63.3%) and craniopharyngioma (86.1%). Survival following diagnosis with a non-malignant brain and other CNS tumor was highest in persons age 15–39 years (98.1%), compared to those ages 0–14 years (97.2%) or 40+ years (90.1%).
Introduction
The objective of the CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016 is to provide a comprehensive summary of the current descriptive epidemiology of primary brain and other central nervous system (CNS) tumors in the United States (US) population. CBTRUS obtained the latest available population-based data on all newly diagnosed primary brain and CNS tumors from the CDC’s National Program of Cancer Registries (NPCR), and the NCI’s Surveillance, Epidemiology, and End Results (SEER) program for diagnosis years 2012–2016. Incidence counts and rates of primary malignant and non-malignant brain and other CNS tumors are presented by histology, sex, age, race, and Hispanic ethnicity. Mortality rates calculated using the National Vital Statistics System (NVSS) data from 2012–2016, and relative survival rates for selected malignant and non-malignant histologies calculated using NPCR data for the period 2001–2015, are also presented.
Background
CBTRUS is a unique professional research organization that focuses exclusively on providing high-quality statistical data on the population-based incidence of primary brain and other CNS tumors in the US (for more information on CBTRUS see: http://www.cbtrus.org/aboutus.html).1 CBTRUS was incorporated as a nonprofit 501(c)(3) in 1992 following a study conducted by the American Brain Tumor Association (ABTA) to determine the feasibility of a central registry focused on primary brain and other CNS tumors in the US.
This report represents the twenty-seventh (27 th ) anniversary of CBTRUS and the twenty-second (22 nd ) statistical report published by CBTRUS. For this eighth (8th) report published as a supplement to Neuro-Oncology, the official journal of the Society for Neuro-Oncology (http://www.soc-neuro-onc.org), CBTRUS continues its past efforts to provide the most up-to-date population-based incidence rates for all primary brain and other CNS tumors by behavior (malignant, non-malignant), histology, age, sex, race, and Hispanic ethnicity. These data have been organized by clinically relevant histology groupings and reflect the 2007 World Health Organization (WHO) Classification of Tumours of the Central Nervous System.2,3 The 2007 WHO Classification has not been fully implemented into US collection practices and histologies with new codes included in 2007 are recoded to existing ICD-0-3 codes and included in cancer registration reports. These data provide important information for allocation and planning of specialty healthcare services such as clinical trials, disease prevention and control programs, and research activities. These data may also lead to clues that will stimulate research into the causes of this group of diseases, which often result in significant morbidity and mortality.
CBTRUS is currently the only population-based site-specific registry in the US that works in partnership with a public cancer surveillance organization, the CDC’s NPCR, and from which data are directly received through the NPCR Cancer Surveillance System (NPCR-CSS) Submission Specifications mechanism4 under a special agreement. Collection of central (state) cancer data was mandated in 1992 by Public Law 102–515, the Cancer Registries Amendment Act.5 This mandate was expanded to include non-malignant CNS tumors with the 2002 passage of Public Law 107–260, starting January 1, 2004.6 CBTRUS combines the NPCR data with data from the NCI’s SEER program,7 which was established for national cancer surveillance in the early 1970s. All data from NPCR and SEER originate from tumor registrars who adhere to the Uniform Data Standards (UDS) for malignant and non-malignant brain and other CNS tumors as directed by the North American Association of Cancer Registries (NAACCR) (http://www.naaccr.org). Along with the UDS, there are quality control checks and a system for rating each central cancer registry (CCR) to ensure that these data are as accurate and complete as possible. As a surveillance partner, CBTRUS reports high-quality data on a all primary brain and other CNS tumors with histological specificity useful to the communities it serves.
The CBTRUS database is comprised of the largest histology-specific aggregation of population-based data limited to the incidence of primary brain and other CNS tumors in the US, and it is likely the largest histology-specific aggregation of primary brain and other CNS tumor cases in the world. There are several other brain-specific registry systems in existence, including the Austrian Brain Tumor Registry8 and the Swedish Brain Tumor Registry,9 as well as other population-based epidemiological studies of primary brain and other CNS tumors that cover a smaller population base. Due to the demographics of the US as compared to European countries, CBTRUS includes increased numbers of cases of primary brain and other CNS tumors in non-White persons. Aggregate information on all cancers from all CCR in the US, including primary brain and other CNS tumors, is available from the United States Cancer Statistics (USCS).10
Technical Notes
Data Collection
CBTRUS does not collect data directly from patients’ medical records. Registration of individual cases (tumors) is conducted by cancer registrars at the institution where diagnosis and/or treatment occurs and is then transmitted to the CCR, which further transmits this information to NPCR. Some CCR also send their data to SEER. As noted, data for CBTRUS analyses come from the NPCR and SEER programs. By law, all primary malignant and non-malignant CNS tumors are reportable diseases and CCR play an essential role in the collection process. Tumor registrars in treatment centers collect these data and send this information to the CCR in their state where they are collated, de-identified, and sent to NPCR and SEER. Primary brain and other CNS tumors are reported using the site definition described in Public Law 107–260.6 These data are population-based and represent a comprehensive documentation of all reported cancers diagnosed within a geographic region for the years included in this report.
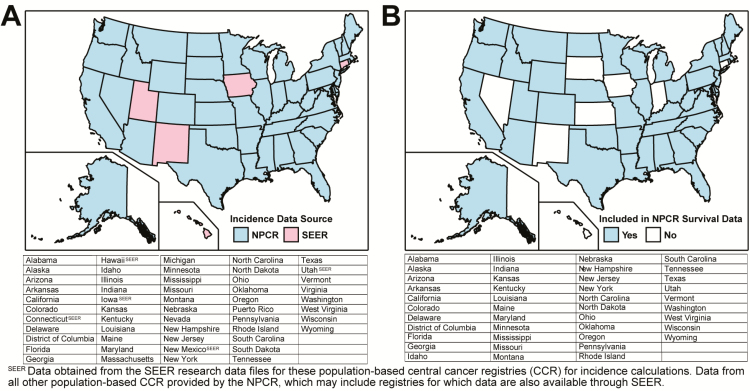
CBTRUS obtained incidence data from 52 CCR (47 NPCR and 5 SEER) that include cases of malignant and non-malignant (benign and uncertain behaviors) primary brain and other CNS tumors. The population-based CCR include 50 state registries, the District of Columbia, and Puerto Rico (Fig. 1A). Data were requested for all newly-diagnosed primary malignant and non-malignant tumors from 2012 to 2016 at any of the following International Classification of Diseases for Oncology, 3rdEdition (ICD-O-3) anatomic sites: brain, meninges, spinal cord, cranial nerves, and other parts of the central nervous system, pituitary and pineal glands, and olfactory tumors of the nasal cavity (Table 1).11
Fig. 1.
Availability by Central Cancer Registry for A) SEER and NPCR Incidence Data (2000–2016) and B) NPCR Survival Data (2001–2015)
Table 1.
Central Brain Tumor Registry of the United States (CBTRUS), brain and other central nervous system tumor site groupings
| Site | ICD-O-3a Site Code |
|---|---|
| Cerebrum | C71.0 |
| Frontal lobe of brain | C71.1 |
| Temporal lobe of brain | C71.2 |
| Parietal lobe of brain | C71.3 |
| Occipital lobe of brain | C71.4 |
| Ventricle | C71.5 |
| Cerebellum | C71.6 |
| Brain stem | C71.7 |
| Other brain | C71.8-C71.9 |
| Overlapping lesion of brain | C71.8 |
| Brain, NOS | C71.9 |
| Spinal cord and cauda equina | C72.0-C72.1 |
| Spinal cord | C72.0 |
| Cauda equine | C72.1 |
| Cranial nerves | C72.2-C72.5 |
| Olfactory nerve | C72.2 |
| Optic nerve | C72.3 |
| Acoustic nerve | C72.4 |
| Cranial nerve, NOS | C72.5 |
| Other nervous system | C72.8-C72.9 |
| Overlapping lesion of brain and central nervous system | C72.8 |
| Nervous system, NOS | C72.9 |
| Meninges (cerebral & spinal) | C70.0-C70.9 |
| Cerebral meninges | C70.0 |
| Spinal meninges | C70.1 |
| Meninges, NOS | C70.9 |
| Pituitary and craniopharyngeal duct | C75.1-C75.2 |
| Pituitary gland | C75.1 |
| Craniopharyngeal duct | C75.2 |
| Pineal gland | C75.3 |
| Olfactory tumors of the nasal cavityb | C30.0 |
a.International Classification of Diseases for Oncology, 3rd Edition, 2000. World Health Organization, Geneva, Switzerland.
b.ICD-O-3 histology codes 9522–9523 only.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NOS, Not otherwise specified
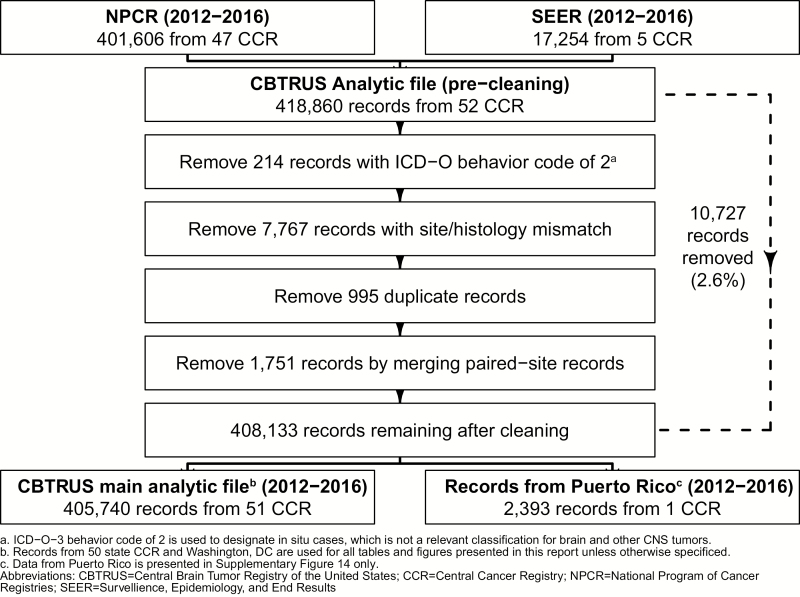
NPCR provided data on 401,606 primary brain and other CNS tumors diagnosed from 2012 to 2016 (Fig. 2). An additional 17,254 primary brain and CNS tumor case records for the period were obtained from SEER. These data were combined into a single dataset of 418,860 records for quality control as part of the CBTRUS Edits program. A total of 10,727 records (2.6%) were deleted from the final analytic dataset for one or more of the following reasons (Fig. 2):
Fig. 2.
Overview of CBTRUS Data Edits Workflow
Records with ICD-O behavior code of 2.
Records with invalid site/histology combination according to the CBTRUS histology grouping scheme
Possible duplicate records that included a less accurate reporting source than microscopic confirmation, also referred to as histologic confirmation (eg, radiographic versus microscopic confirmation), possible duplicate record for recurrent disease, or errors in time sequence of diagnosis
Possible duplicate records for bilateral vestibular schwannoma or meningioma that were merged to one paired-site record.
The final analytic dataset had 408,133 records, which included 405,740 records from the 50 state CCR and the District of Columbia used in the analytic dataset, and an additional 2,393 records from Puerto Rico. Records from Puerto Rico were included only in a supplementary analysis, and these cases are not included in the overall statistics presented in this report.
Age-adjusted incidence rates per 100,000 population for the entire US for selected other cancers were obtained from the United States Cancer Statistics (USCS), produced by the CDC and the NCI, for the purpose of comparison with brain and other CNS tumor incidence rates.10 This database includes both NPCR and SEER data and represents the entire US population.
As of the 2019 annual report, CBTRUS now presents survival statistics based on the NPCR’s USCS survival data ( Fig. 1B ). Survival data for malignant brain and other CNS tumors were obtained from the USCS program for 43 NPCR registries for the years 2001 to 2015, and for non-malignant brain and other CNS tumors for the years 2004 to 2015. This dataset provides population-based information for approximately 93% of the US population for the years 2001 to 2015, and is a subset of the data used for the incidence calculations presented in this report. Survival information is derived from both active and passive follow-up.
Mortality data used in this report are from the National Center for Health Statistics (NCHS) and include deaths where primary brain or other CNS tumor was listed as cause of death on the death certificate for individuals from all 50 states and the District of Columbia. These data were obtained from the National Vital Statistics System (NVSS)12 (includes death certification data for 100% of the US population) for malignant brain and other CNS tumors and comparison via SEER*Stat (for malignant brain tumors and comparison cancers). NVSS data are not collected through the cancer registration system, and therefore these data are not included under cancer registration mandates. These data represent the primary cause of death listed on each individual death certificate, and as a result, deaths in persons with cancer may be recorded as non-cancer deaths.
Definitions
Measures in surveillance epidemiology
The CBTRUS Report presents the following population-based measures: incidence rates, mortality rates, and relative survival rates (for more information on definitions of terms and measures used see: http://www.cbtrus.org/glossary/glossary1.html).
Classification by behavior, histology, and WHO grade
There are over 100 histologically distinct types of primary CNS tumors, each with its own spectrum of clinical presentations, treatments, and outcomes. This report uses the most recent 2012 CBTRUS Histology Grouping (Table 2). This classification scheme utilizes ICD-O-3 codes11 and may include morphology codes that were not previously reported to CBTRUS.13 In this report, incidence rates are provided for major histology groupings and for specific histologies.
Table 2.
Central Brain Tumor Registry of the United States (CBTRUS), Brain and Other Central Nervous System Tumor Histology Groupings
| Histology | ICD-O-3a Histology Codesb | ICD-O-3a Histology and Behavior Codeb | |
|---|---|---|---|
| Malignant (ICD-O-3 Behavior code /3) | Non-Malignant (ICD-O-3 Behavior Codes /0 and /1) | ||
| Tumors of Neuroepithelial Tissue | |||
| Pilocytic astrocytoma* | 9421, 9425c | 9421/1d, 9425/3c | None |
| Diffuse astrocytoma* | 9400, 9410, 9411, 9420 | 9400/3, 9410/3, 9411/3, 9420/3 | None |
| Anaplastic astrocytoma* | 9401 | 9401/3 | None |
| Unique astrocytoma variants* | 9381, 9384, 9424 | 9381/3, 9424/3 | 9384/1 |
| Glioblastoma* | 9440, 9441, 9442/3e | 9440/3, 9441/3, 9442/3 | None |
| Oligodendroglioma* | 9450 | 9450/3 | None |
| Anaplastic oligodendroglioma* | 9451, 9460 | 9451/3, 9460/3 | None |
| Oligoastrocytic tumors* | 9382 | 9382/3 | None |
| Ependymal tumors* | 9383, 9391, 9392, 9393, 9394 | 9391/3, 9392/3, 9393/3 | 9383/1, 9394/1 |
| Glioma malignant, NOS* | 9380, 9431c, 9432c | 9380/3, 9431/1c, 9432/1c | None |
| Choroid plexus tumors | 9390 | 9390/3 | 9390/0,1 |
| Other neuroepithelial tumors* | 9363, 9423, 9430, 9444 | 9423/3, 9430/3 | 9363/0, 9444/1 |
| Neuronal and mixed neuronal-glial tumors* | 8680, 8681, 8690, 8693, 9412, 9413, 9442/1f, 9492 (excluding site C75.1), 9493, 9505, 9506, 9522, 9523 | 8680/3, 8693/3, 9505/3, 9522/3, 9523/3 | 8680/0,1, 8681/1, 8690/1, 8693/1, 9412/1, 9413/0, 9442/1, 9492/0 (excluding site C75.1), 9493/0, 9505/1, 9506/1, 9509/1, |
| Tumors of the pineal region | 9360, 9361, 9362, 9395c | 9362/3, 9395/3c | 9360/1, 9361/1 |
| Embryonal tumors | 8963, 9364, 9470–9474, 9480, 9490, 9500–9502, 9508 | 8963/3, 9364/3, 9470/3, 9471/3, 9472/3, 9473/3, 9474/3, 9480/3, 9490/3, 9500/3, 9501/3, 9502/3, 9508/3 | 9490/0 |
| Medulloblastoma | 9470–9472, 9474 | 9470/3, 9471/3, 9472/3, 9474/3. | None |
| Primitive neuroectodermal tumor | 9508 | 9508/3. | None |
| Atypical teratoid/rhabdoid tumor | 9473 | 9473/3 | None |
| Tumors of Cranial and Spinal Nerves | |||
| Nerve sheath tumors | 9540, 9541, 9550, 9560, 9561, 9570, 9571 | 9540/3, 9560/3, 9561/3, 9571/3 | 9540/0,1, 9541/0, 9550/0, 9560/0, 1, 9570/0, 9571/0 |
| Vestibular schwannoma (acoustic neuroma) | 9560 | None | 9560/0 |
| Other tumors of cranial and spinal nerves | 9562 | None | 9562/0 |
| Tumors of Meninges | |||
| Meningioma | 9530–9534, 9537–9539 | 9530/3, 9538/3, 9539/3 | 9530/0,1, 9531/0, 9532/0, 9533/0, 9534/0, 9537/0, 9538/1, 9539/1 |
| Mesenchymal tumors | 8324, 8800–8806, 8810, 8815, 8824, 8830, 8831, 8835, 8836, 8850–8854, 8857, 8861, 8870, 8880, 8890, 8897, 8900–8902, 8910, 8912, 8920, 8921, 8935, 8990, 9040, 9136, 9150, 9170, 9180, 9210, 9241, 9260, 9373 | 8800/3, 8801/3, 8802/3, 8803/3, 8804/3, 8805/3, 8806/3, 8810/3, 8815/3, 8830/3, 8850/3, 8851/3, 8852/3, 8853/3, 8854/3, 8857/3, 8890/3, 8900/3, 8901/3, 8902/3, 8910/3, 8912/3, 8920/3, 8921/3, 8990/3, 9040/3, 9150/3, 9170/3, 9180/3, 9260/3 | 8324/0, 8800/0, 8810/0, 8815/0, 8824/0,1, 8830/0,1, 8831/0, 8835/1, 8836/1, 8850/0,1, 8851/0, 8852/0, 8854/0, 8857/0, 8861/0, 8870/0, 8880/0, 8890/0,1, 8897/1, 8900/0, 8920/1, 8935/0,1, 8990/0,1, 9040/0, 9136/1, 9150/0,1, 9170/0, 9180/0, 9210/0, 9241/0, 9373/0 |
| Primary melanocytic lesions | 8720, 8728, 8770, 8771 | 8720/3, 8728/3, 8770/3, 8771/3 | 8728/0,1, 8770/0, 8771/0 |
| Other neoplasms related to the meninges | 9161, 9220, 9231, 9240, 9243, 9370–9372, 9535 | 9220/3, 9231/3, 9240/3, 9243/3, 9370/3, 9371/3, 9372/3 | 9161/1, 9220/0,1, 9535/0 |
| Lymphomas and Hematopoietic Neoplasms | |||
| Lymphoma | 9590, 9591, 9596, 9650–9655, 9659, 9661–9665, 9667, 9670, 9671, 9673, 9675, 9680, 9684, 9687, 9690, 9691, 9695, 9698, 9699, 9701, 9702, 9705, 9714, 9719, 9728, 9729 | 9590/3, 9591/3, 9596/3, 9650/3, 9651/3, 9652/3, 9653/3, 9654/3, 9655/3, 9659/3, 9661/3, 9662/3, 9663/3, 9664/3, 9665/3, 9667/3, 9670/3, 9671/3, 9673/3, 9675/3, 9680/3, 9684/3, 9687/3, 9690/3, 9691/3, 9695/3, 9698/3, 9699/3, 9701/3, 9702/3, 9705/3, 9714/3, 9719/3, 9728/3, 9729/3 | None |
| Other hematopoietic neoplasms | 9727, 9731, 9733, 9734, 9740, 9741, 9750–9758, 9760, 9766, 9823, 9826, 9827, 9832, 9837, 9860, 9861, 9866, 9930, 9970 | 9727/3, 9731/3, 9733/3, 9734/3, 9740/3, 9741/3, 9750/3, 9754/3, 9755/3, 9756/3, 9757/3, 9758/3, 9760/3, 9823/3, 9826/3, 9827/3, 9832/3, 9837/3, 9860/3, 9861/3, 9866/3, 9930/3 | 9740/1, 9751/1, 9752/1, 9753/1, 9766/1, 9970/1 |
| Germ Cell Tumors and Cysts | |||
| Germ cell tumors, cysts, and heterotopias | 8020, 8440, 9060, 9061, 9064, 9065, 9070–9072, 9080–9085, 9100, 9101 | 8020/3, 8440/3, 9060/3, 9061/3, 9064/3, 9065/3, 9070/3, 9071/3, 9072/3, 9080/3, 9081/3, 9082/3, 9083/3, 9084/3, 9085/3, 9100/3, 9101/3 | 8440/0, 9080/0,1, 9084/0 |
| Tumors of Sellar Region | |||
| Tumors of the pituitary | 8040, 8140, 8146, 8246, 8260, 8270– 8272, 8280, 8281, 8290, 8300, 8310, 8323, 9492 (Site C75.1 only), 9582 | 8140/3, 8246/3, 8260/3, 8270/3, 8272/3, 8280/3, 8281/3, 8290/3, 8300/3, 8310/3, 8323/3 | 8040/0,1, 8140/0,1, 8146/0, 8260/0, 8270/0, 8271/0, 8272/0, 8280/0, 8281/0, 8290/0, 8300/0, 8310/0, 8323/0, 9492/0 (site C75.1 only), 9582/0 |
| Pituitary adenoma | 8272 | None | 8272/0 |
| Craniopharyngioma | 9350, 9351, 9352 | None | 9350/1, 9351/1, 9352/1 |
| Unclassified Tumors | |||
| Hemangioma | 9120–9123, 9125, 9130, 9131, 9133, 9140 | 9120/3, 9130/3, 9133/3, 9140/3 | 9120/0, 9121/0, 9122/0, 9123/0, 9125/0, 9130/0,1, 9131/0, 9133/1 |
| Neoplasm, unspecified | 8000–8005, 8010, 8021 | 8000/3, 8001/3, 8002/3, 8003/3, 8004/3, 8005/3, 8010/3, 8021/3 | 8000/0,1, 8001/0,1, 8005/0, 8010/0 |
| All other | 8320, 8452, 8710, 8711, 8713, 8811, 8840, 8896, 8980, 9173, 9503, 9580 | 8320/3, 8710/3, 8711/3, 8811/3, 8840/3, 8896/3, 8980/3, 9503/3, 9580/3 | 8452/1, 8711/0, 8713/0, 8811/0, 8840/0, 9173/0, 9580/0 |
a.International Classification of Diseases for Oncology, 3rd Edition, 2000. World Health Organization, Geneva, Switzerland.
b.See the CBTRUS website for additional information about the specific histology codes included in each group: http://www.cbtrus.org.
c.Histology only included starting with diagnosis year 2015.
d.While the WHO classification of CNS tumors classifies pilocytic astrocytoma as a non-malignant tumor, this histology has been historically included as a malignant histology for the purposes of mandatory reporting in US cancer registration. As a result of this, CBTRUS classifies pilocytic astrocytoma as a malignant tumor for comparability with both historical data and other reporting sources.
e.ICD-O-3histology and behavior Codes 9442/3 only.
f.ICD-O-3 histology and behavior Codes 9442/1 only.
* All or some of this histology is included in the CBTRUS definition of gliomas, including ICD-O-3 histology codes 9380–9384 and 9391–9460. All or some of the histologies listed under Glioma, NOS are 2007 WHO Classification new histologies that had not been fully implemented in collection practices during the years covered in this report but were recoded to existing ICD-O-3 histology codes. Starting January 1, 2018, these ICD-O-3 codes are fully implemented.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NOS, Not otherwise specified
Gliomas are tumors that arise from glial or precursor cells and include astrocytoma (including glioblastoma), oligodendroglioma, ependymoma, oligoastrocytoma (mixed glioma), malignant glioma, not otherwise specified (NOS), and a few rare histologies. Because there is no standard definition for glioma, CBTRUS defines glioma as ICD-O-3 histology codes 9380–9384, and 9391–9460 in accordance with the recode rules for 2007 WHO Classification of CNS tumors as starred inTable 2. It is also important to note that the statistics for lymphomas and hematopoietic neoplasms contained in this report refer only to those lymphomas and hematopoietic neoplasms that arise in the brain and other CNS ICD-O-3 topography codes.
This report also utilizes the International Classification of Childhood Cancer (ICCC) grouping system for pediatric cancers. ICCC categories for this report were generated using the SEER Site/Histology ICCC-3 Recode14 based on the ICCC, Third edition15 and 2007 WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues16 (See Supplementary Table 1 for more information on this classification scheme). The ICCC was developed in order to provide a standard classification of childhood tumors for comparing incidence and survival across regions and time periods. As shown, the Supplementary Table 10 age-group category total, age 0–19 year age-group count, and age-specific and age-adjusted rates are equivalent to those presented throughout this report, even though the histology grouping scheme differs from that used by CBTRUS.
Unlike other types of cancer, primary brain and other CNS tumors are not staged. They are classified according to the WHO 2000 Classification of Tumours of the Central Nervous System17 which assigns a grade (grade I through grade IV) based on predicted clinical behavior. Though the WHO classification scheme was also updated in 20072 and 201618 these updated schema will not be fully implemented by US CCR until collection year 2018 or reporting year 2021. Updates made in 2007 may affect diagnostic practices used in characterization of individual tumors included in this report, though the newest revision would not affect any cases included in this report. With the increased recognition of the value of biomarkers for specific brain tumor histologies in classification, the WHO Classification of Tumours of the Central Nervous System has included biomarkers in its 2016 revision. However, implementing the collection of these markers in cancer registration is multi-faceted and includes an ongoing educational and training component. Collection of these markers began in the US on January 1, 2018.
WHO grading assignments are recorded by cancer registrars as Collaborative Stage Site-Specific Factor 1 - WHO Grade Classification according to the American Joint Commission on Cancer’s (AJCC) Collaborative Staging (CS) schema.19 This variable has been a required component of cancer registry data collection for brain and other CNS tumors since 2004 for SEER registries, and since 2011 for NPCR registries, and completeness of this variable has improved significantly over time.20 Completeness of this variable is defined as having a value equal to WHO grade I, II, III, or IV. Cases where WHO grade is marked as not applicable or not documented are considered incomplete. It is not possible to conclusively determine WHO grade, which is based on the appearance of tumor cells, when a tumor is radiographically confirmed only. Some tumor types (including tumors of the pituitary and lymphomas) are often not assigned a WHO grade. This information may also be assigned but not included in the pathology report.
Anatomic location of tumor sites
Various terms are used to describe the regions of the brain and other CNS. The specific sites used in this report are broadly based on the categories and site codes defined in the SEER Site/Histology Validation List.21 See Table 1 for an overview of CBTRUS primary site groupings. The CBTRUS Site/Validation List can be found on the CBTRUS website (http://www.cbtrus.org).
Measurement and statistical methods
Counts, means, rates, ratios, proportions, and other relevant statistics were calculated using R 3.5 statistical software22 and/or SEER*Stat 8.3.5.23 Figures were created in R 3.5 using the following packages: rgeos, rgdal, maptools, ggplot2, and SEER2R.24–28 Tables were created in R 3.5 using the following packages: officer, flextable, magritter, and SEER2R.27,29–31 As per the NPCR and CBTRUS agreement, rates are suppressed when counts are fewer than 16 within a cell but included in totals, except when data are suppressed from only one cell to prevent identification of the number in the suppressed cell. NOTE: reported percentages may not add up to 100% due to rounding.
Population data for each geographic region were obtained from the SEER program website32 for the purpose of rate calculation. All rates presented in this statistical report are age-adjusted. Crude incidence rates are calculated by dividing the total number of cases by the total population, and cannot be compared to crude rates from other populations where the age distribution is different. Age-adjustment is a technique that is used to enable comparison between groups with different age distributions, such as rates between different states. Rates that have been age-adjusted are estimates of what the crude rate would be if the age distribution was equivalent to a standard population. Average annual age-adjusted incidence rates (AAAIR) and 95% confidence intervals (95% CI) were estimated per 100,000 population, based on one-year age groupings and standardized to the 2000 US standard population.33 The age distribution of the 2000 US standard population is shown in Supplementary Table 2. Combined populations for the regions included in this report are also shown in Supplementary Table 3, Supplementary Table 4, 5.
CBTRUS presents statistics on the pediatric and adolescent age- group 0–19 years as suggested by clinicians, for clinical relevance. However, the 0–14 year age- group is a standard age category for childhood cancer used by other cancer surveillance organizations and has been included in this report for consistency and comparison purposes. Race categories in this report are all races, White, Black, American Indian/Alaskan Native (AIAN), and Asian/Pacific Islander (API). Other race, unspecified, and unknown race are included in statistics that are not race-specific. Hispanic ethnicity was defined using the NAACCR Hispanic Identification Algorithm, version 2, data element, which utilizes a combination of cancer registry data fields (Spanish/Hispanic Origin data element, birthplace, race, and surnames) to directly and indirectly classify cases as Hispanic or non-Hispanic.34 The United States Department of Agriculture’s 2013 Rural Urban Continuum Codes (RUCCs), which classify counties by population size and proximity to a metropolitan area, were used to classify counties either as rural or urban (rural RUCC = 4–9; urban RUCC = 1–3).35
When comparing two rates to one another, it is important to consider whether they are truly different or whether the difference in the estimates may be due to random error. Two methods are used in this report for determining whether two values are ‘significantly different,’ meaning whether the evidence meets a level of strength (usually a 5% chance of error) where the difference can be assumed to not be due to random error. The first is through the use of 95% confidence interval (CI), which were calculated for all presented rates. A 95% CI is a range around an estimate, which, if sampling of the population were to be repeated, should contain the ‘true’ value for the population 95% of the time. If the CI of two estimates do not overlap, these values are considered significantly different with a less than 5% probability of happening by chance. The second method used is the calculation of p-values. A p-value is the probability of finding the observed or more extreme results by chance alone, and a P-value of <0.05 (or <5% chance of results being due to chance) is conventionally used as a cut-off for considering a value statistically significant. Therefore, a P-value <0.0001 could be interpreted as meaning the observed value (or a more extreme value) had a <0.01% chance of occurring by chance alone and the difference can be considered statistically significant at the 0.01% level.
Brain tumor definition differences
NPCR, SEER, and NAACCR report brain and other CNS tumors differently from CBTRUS. The definition of primary brain and other CNS tumors used by these organizations in their published incidence and mortality statistics includes tumors located in the following sites with their ICD-O-3 site codes in parentheses: brain, meninges, and other central nervous system tumors (C70.0–9, C71.0–9, and C72.0–9), but excludes lymphoma and leukemia histologies (9590–9989) from all brain and other CNS sites.3 In contrast, CBTRUS reports data on all tumor morphologies located within the Consensus Conference site definition including lymphoma and other hematopoietic histologies, as well as olfactory tumors of the nasal cavity [C30.0 (9522–9523)].13 Additionally, CBTRUS reports data on all primary brain and other CNS tumors irrespective of behavior, whereas many reporting organizations may only publish rates for primary malignant brain and other CNS tumors due to the original mandate that focused only on malignant tumors, sometimes using the term cancer to broadly identify these tumors in their reports. These differences in definition therefore influence the direct comparison of published rates.
In the US, cancer registries and surveillance groups only collect data on primary CNS tumors (meaning tumors that originate within the brain and spinal cord) and do not collect data on tumors that metastasize to the brain or spinal cord from other primary sites. As a result, only primary brain and other CNS tumors are included in this report.
Estimation of expected numbers of brain and other CNS tumors in 2019 and 2020
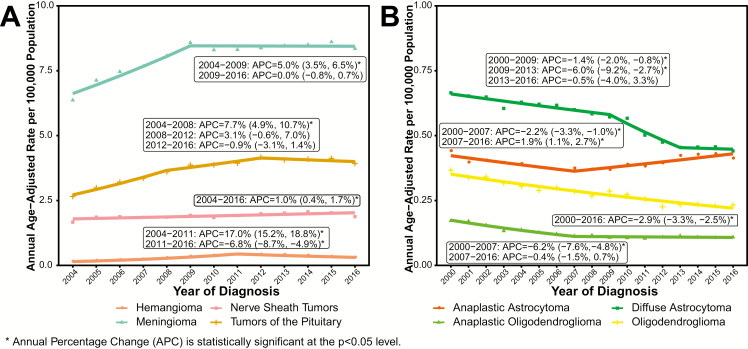
Estimated numbers of expected malignant and non-malignant primary brain and other CNS tumors were calculated for 2019 and 2020. To project estimates of newly diagnosed brain and other CNS tumors in 2019 and 2020, age-adjusted annual brain tumor incidence rates were generated for 2000–2016 for malignant tumors, and 2006–2016 for non-malignant tumors. These were generated by state, age, and histologic type. Joinpoint 4.7.0.036 was used to fit regression models to these incidence rates,37 which were used to predict numbers of cases in future years using the parameter from the selected models. Joinpoint regression allows for multiple lines to be fitted to incidence data across time, rather than assuming a consistent trend across the whole period. The points where these lines intersect are called ‘joinpoints’. The models allowed for a maximum of two joinpoints (one for non-malignant tumors), a minimum of three observations from a joinpoint to either end of the data, and a minimum of three observations between joinpoints.38 Modified Bayesian Information Criterion procedures included in Joinpoint were used to select the best fitting model. The overall totals presented are based on total malignant and non-malignant incidence, and the presented stratified rates may not add up to these totals. Estimated numbers of cases are highly dependent on input data. Different patterns of incidence within strata can significantly affect the projected estimates, especially when the number of cases within a stratum is low. For state-specific projections, a model with no joinpoints was used to generate predictions as annual variability within some states was extremely high. As a result, strata-specific estimates may not equal the total estimate presented. Caution should be used when utilizing these estimates.
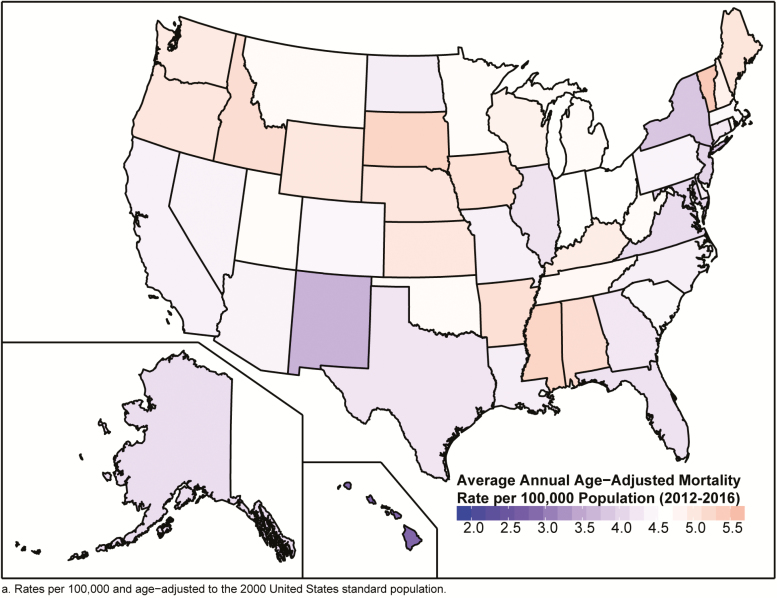
Estimation of mortality rates for brain and other CNS tumors
Age-adjusted mortality rates for deaths resulting from all primary malignant brain and other CNS tumors were calculated using the mortality data available in SEER*Stat Online Database provided by NCHS from death certificates per 100,000 population.12 In addition to the total age-adjusted rate for the US, age-adjusted rates are presented by sex and state.
Estimation of survival rates
SEER*Stat 8.3.5 statistical software was used to estimate one-, two-, three-, four-, five-, and ten-year relative survival rates for primary malignant CNS tumor cases diagnosed between 2001–2015 in 43 NPCR CCRs and for primary non-malignant CNS tumor cases diagnosed between 2004–2015. This software utilizes life-table (actuarial) methods to compute survival estimates and accounts for current follow-up. Second or later primary tumors, cases diagnosed at autopsy, cases in which race or sex is coded as other or unknown, and cases known to be alive but for whom follow-up time could not be calculated, were excluded from survival data analyses.
Estimation of time trends
Joinpoint 4.7.0.036 was used to estimate incidence time trends, and generate annual percentage changes (APC) and 95% CI. The models allowed for a maximum of two joinpoints (two for non-malignant tumors), a minimum of three observations from a joinpoint to either end of the data, and a minimum of three observations between joinpoints.38 APC is the average percent change in incidence per year over the period included in the trend segment. Time trends analysis methods were used to estimate if the APC was significantly different from 0% (meaning no change in incidence from year to year). The 95% CI is a range around an estimate that, if sampling of the population were to be repeated, should contain the ‘true’ value for the population 95% of the time. If the 95% CI contains zero, one cannot be confident that the ‘true’ population APC value is significantly different from 0%. The joinpoint regression program fits a linear regression to annual incidence rates to test significance of changes overtime, with different trends lines connected at ‘joinpoints’ where there are changes in the direction of incidence trends. The best fitting model was determined through permutation tests, with a minimum of three observations required between two joinpoints, as well as a minimum of three observations required between a joinpoint and either end of the data.
Data interpretation
CBTRUS works diligently to support the broader surveillance efforts aimed at improving the collection and reporting of primary brain and other CNS tumors. CCR data provided to NPCR and SEER and, subsequently, to CBTRUS vary from year-to-year due to ongoing updates in collection and data refinement aimed to improve completeness and accuracy. Therefore, it is important to note that data from previous CBTRUS Reports cannot be compared to data in this current report, CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016. This current report supersedes all previous reports in terms of coverage of the US population with the most up-to-date population-based information available, making these data the most accurate and timely to reference.
Several factors should be considered when interpreting the data presented in this report:
Incident counts of cases represent individual tumors and not persons. A single person could contribute multiple counted primary tumor cases to the data included in this report. The 405,740 tumors cases, from 50 state CCR and the District of Columbia, included in this report came from 400,337 individuals. Of these 400,337 individuals, there were 5,153 individuals (1.3%) that contributed information on multiple tumors (two or more) to this report.
Random fluctuations in average annual rates are common, especially for rates based on small case counts. The CBTRUS policy to suppress data presentation for cells with counts of fewer than 16 cases is consistent with the NPCR policy.
A 2007 policy change guiding the Veterans Health Administration (VHA) resulted in underreporting of cancer data—especially for men—to CCR. Recent investigations suggest that underreporting for VHA facilities has diminished over time, and that the Veterans Affairs Central Cancer Registry (VACCR) now captures approximately 87–90% of cases.40,41 It is important to note that improved reporting to VACCR does not necessarily mean that reporting to the state CCR has improved. The VACCR does not submit data to NPCR or SEER.
Delays in reporting and late ascertainment are a reality and a known issue influencing registry completeness and, consequently, rate underestimations occur, especially for the most recent years.42,43 The SEER and NPCR programs allow for reporting delay of up to 22–23 months prior to public data release, but additional cases may still be discovered after that point.44 On average across all cancer sites, the submissions for the most recent diagnosis year are approximately 4% lower than the total number of cases that will eventually be submitted. This problem may be even more likely to occur in the reporting of non-malignant brain and other CNS tumors, where reporting often comes from non-hospital-based sources, such as free standing clinics or outpatient facilities.
Type of diagnostic confirmation may also lead to increased reporting delay, with histologically confirmed tumors being subject to less reporting delay than radiographically confirmed tumors. In 2016, a study assessing the incidence of non-malignant brain and other CNS tumors corroborated the large variation in incidence between CCR reported in this statistical report.45 The reasons for this variation remain inconclusive but what is consistently noted is the correlation between high incidence and high proportion of non-malignant cases collected without microscopic confirmation or surgery, in other words, clinically diagnosed cases of non-malignant brain tumors. At this current time, given the variation across CCR, there is potential evidence of underreporting of non-malignant brain and other CNS tumors, the extent to which cannot be quantified.45
Population estimates used for denominators affect incidence rates. CBTRUS has utilized population estimates based on the 2000 US Census for calculation of incidence and mortality rates in this report, as is standard practice in US cancer registry reporting.46,47
CBTRUS editing practices are reviewed, revised, and conducted yearly. These practices are aimed at refining the data for accuracy and clinical relevance and play a role in interpreting these report data. Exclusion of site and histology combinations considered invalid by the consulting neuropathologists who revised the CBTRUS site/histology validation list in 2012 may have the impact of underestimating the incidence of primary brain and other CNS tumors. Editing changes, such as the Multiple Primary and Histology Rules issued in 2007 and revised in 2018,48,49 also incorporate updates to the cancer registration coding rules that influence case ascertainment and data collection.3
Supplemental Data
CBTRUS has made supplemental additional figures and tables available. These materials are noted in the text as Supplementary Tables and Figures.
Results
Incidence and Mortality in Comparison to Other Common Neoplasms in the US
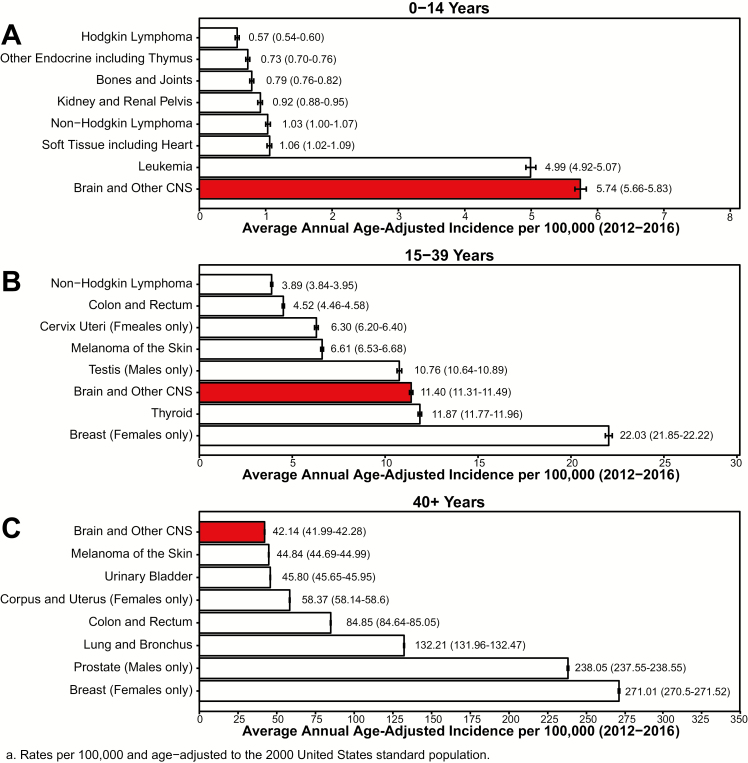
AAAIR for all primary brain and other CNS tumors (2012–2016) and a selection of common cancers (USCS, 2012–2016) in the US are presented by age in Figure 3A: Children (Age 0–14 Years), Figure 3B: Adolescents and Young Adults (Age 15–39 Years), and Figure 3C: Older Adults (Age 40+ Years). Incidence rates stratified by sex are presented by age in Supplementary Figure 1 and Supplementary Figure 2, respectively. Please see Supplementary Table 6 for incidence rates of comparison cancers.
Fig. 3.
Average Annual Age-Adjusted Incidence Ratesa with 95% Confidence Intervals of All Primary Brain and Other CNS Tumors in Comparison To Top Eight Highest Incidence Cancers for A) Children Age 0–14 Years, B) Adolescents and Young Adults Age 15–39 Years, and C) Older Adults Age 40+ Years, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER 2012–2016
Brain and other CNS tumors (both malignant and non-malignant) were the most common cancer site in persons age 0–14 years, with AAAIR of 5.74 per 100,000 population. Brain and other CNS tumors were the most common cancer in both males and females in this age group.
Leukemia was the second most common neoplasm in persons age 0–14 years, with an AAAIR of 4.99 per 100,000 population. Leukemia was the second most common cancer in both males and females in this age group.
Brain and other CNS tumors (both malignant and non-malignant) among those age 15–39 years had an AAAIR of 11.40 per 100,000 population. These tumors were the third most common cancer overall, the second most common cancer in males in this age group, and the third most common cancer in females in this age group.
Testicular cancer was the most common cancer in males age 15–39 years, with an AAAIR of 10.76 per 100,000.
Breast cancer was the most common cancer among females age 15–39 years, with an AAAIR of 22.03 per 100,000.
Brain and other CNS tumors (both malignant and non-malignant) were the eighth most common cancer among persons age 40+ years with an AAAIR of 42.14 per 100,000 population. These tumors were the eighth most common cancer among males and the fifth most common cancer among females in this age group.
Prostate and breast cancer were the most common cancers among those age 40+ years in the US, with an AAAIR of 238.05 per 100,000 population (males only) and 271.01 per 100,000 (females only) population, respectively.10
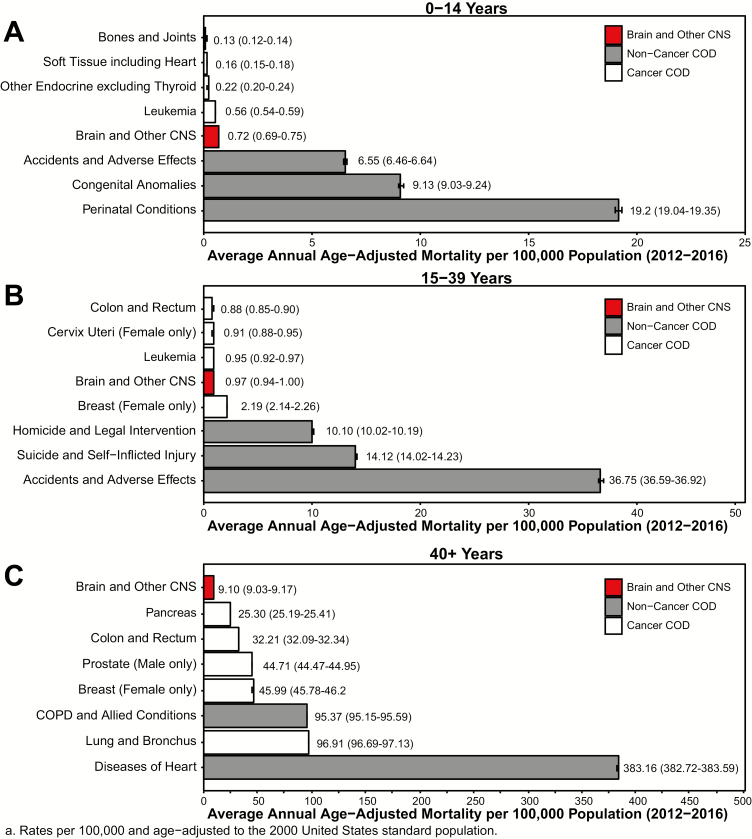
Average annual age-adjusted mortality rates (AAAMR) for primary malignant brain and other CNS tumors (NVSS 2012–2016), a selection of common cancers, and the top three non-cancer causes of death in the US are presented by age in Figure 4A: (Age 0–14 Years), Figure 4B: (Age 15–39 Years), and Figure 4C: (Age 40+ Years). Mortality rates for males only and females only are presented by age in Supplementary Figure 3 and Supplementary Figure 4, respectively. Please see Supplementary Table 7 for mortality rates in relation to comparison cancers and other non-cancer conditions.
Fig. 4.
Average Annual Age-Adjusted Mortality Ratesa with 95% Confidence Intervals of All Primary Brain and Other CNS Tumors in Comparison To Top Five Causes of Cancer Death and Top Three Non-Cancer Causes of Death (COD) for A) Children Age 0–14 Years, B) Adolescents and Young Adults Age 15–39 Years, and C) Older Adults Age 40+ Years, CBTRUS Statistical Report: NVSS 2012–2016
Malignant brain and other CNS tumors among persons age 0–14 years had an AAAMR of 0.72 per 100,000 and were the seventh most common cause of death in this age-group, and the most common cause of cancer death.
Childhood brain and CNS cancer, while rare, contributes substantially to cancer-related mortality in this population, surpassing other cancers as the top reason for cancer mortality in those age 0–14 years at death. 50
The most common causes of death in persons age 0–14 years were conditions originating in the perinatal period (19.20 per 100,000).
Malignant brain and other CNS tumors among persons age 15–39 years had an AAAMR of 0.97 per 100,000 and were the twelfth most common cause of death in this age group and the second most common cause of cancer death, where their AAAMR was equal to that of leukemia. The most common cause of cancer death in this age-group was female breast cancer.
Accidents and adverse effects were the leading causes of death in persons age 15–39 years (36.75 per 100,000).
Malignant brain and other CNS tumors among persons age 40+ years had an AAAMR of 9.10 per 100,000, and were the twenty-seventh most common cause of death and the thirteenth most common cause of cancer death. The most common cause of cancer death in this age-group was lung and bronchus cancer.
Heart disease was the largest contributor to mortality in persons age 40+ years in the US, with an AAAMR of 383.16 per 100,000 for major cardiovascular diseases.
Distributions and Incidence by Site, Behavior, Histology, and Year
Counts and rates from the 405,740 incident brain and other CNS tumors (122,569 malignant; 283,171 non-malignant shown in Figure 5) reported to 50 state CCR and the District of Columbia during 2012–2016 by histology, behavior, and sex for all ages are presented in Table 3. Counts and rates are shown by histology and behaviors for selected histologies where there is a sufficient number of cases to calculate rates. The predominant tumor categories by behavior are presented in Supplementary Figures 5, 6.
Fig. 5.
Distributiona of Primary Brain and Other CNS Tumors by Behavior (Five-Year Total = 405,740; Annual Average Cases = 81,148), CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Table 3.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for all brain and other central nervous system tumors by major histology grouping, histology, behavior, and sex, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | Total | Male | Female | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5 year Total | Annual average | % of all tumors | Median Age | Rate | 95% CI | 5 year Total | Annual average | % Malignant | % Non- Malignant | Rate | 95% CI | 5 year Total | Annual average | % Malignant | % Non- Malignant | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 112,280 | 22,456 | 27.7% | 57.0 | 6.56 | 6.52–6.60 | 62,981 | 12,596 | 92.8% | 7.2% | 7.69 | 7.62–7.75 | 49,299 | 9,860 | 92.3% | 7.7% | 5.56 | 5.51–5.61 |
| Pilocytic Astrocytoma | 5,166 | 1,033 | 1.3% | 12.0 | 0.35 | 0.34–0.36 | 2,686 | 537 | 100.0% | 0.0% | 0.36 | 0.34–0.37 | 2,480 | 496 | 100.0% | 0.0% | 0.34 | 0.33–0.36 |
| Diffuse Astrocytoma | 7,500 | 1,500 | 1.8% | 47.0 | 0.46 | 0.45–0.47 | 4,127 | 825 | 100.0% | 0.0% | 0.52 | 0.50–0.53 | 3,373 | 675 | 100.0% | 0.0% | 0.40 | 0.39–0.42 |
| Anaplastic Astrocytoma | 7,015 | 1,403 | 1.7% | 53.0 | 0.42 | 0.41–0.43 | 3,868 | 774 | 100.0% | 0.0% | 0.48 | 0.46–0.49 | 3,147 | 629 | 100.0% | 0.0% | 0.36 | 0.35–0.37 |
| Unique Astrocytoma Variants | 1,161 | 232 | 0.3% | 23.0 | 0.07 | 0.07–0.08 | 628 | 126 | 68.3% | 31.7% | 0.08 | 0.08–0.09 | 533 | 107 | 66.8% | 33.2% | 0.07 | 0.06–0.07 |
| Malignant | 785 | 157 | 0.2% | 32.0 | 0.05 | 0.05-0.05 | 429 | 86 | -- | -- | 0.05 | 0.05–0.06 | 356 | 71 | -- | -- | 0.04 | 0.04–0.05 |
| Non-Malignant | 376 | 75 | 0.1% | 10.0 | 0.03 | 0.02–0.03 | 199 | 40 | -- | -- | 0.03 | 0.02–0.03 | 177 | 35 | -- | -- | 0.02 | 0.02–0.03 |
| Glioblastoma | 59,164 | 11,833 | 14.6% | 65.0 | 3.22 | 3.19–3.24 | 34,149 | 6,830 | 100.0% | 0.0% | 4.00 | 3.96–4.05 | 25,015 | 5,003 | 100.0% | 0.0% | 2.54 | 2.51–2.57 |
| Oligodendroglioma | 3,668 | 734 | 0.9% | 43.0 | 0.23 | 0.22–0.24 | 2,006 | 401 | 100.0% | 0.0% | 0.26 | 0.25–0.27 | 1,662 | 332 | 100.0% | 0.0% | 0.21 | 0.20–0.22 |
| Anaplastic Oligodendroglioma | 1,808 | 362 | 0.4% | 50.0 | 0.11 | 0.10–0.11 | 1,000 | 200 | 100.0% | 0.0% | 0.12 | 0.12–0.13 | 808 | 162 | 99.9% | 0.1% | 0.10 | 0.09–0.10 |
| Oligoastrocytic Tumors | 2,103 | 421 | 0.5% | 41.0 | 0.13 | 0.13–0.14 | 1,208 | 242 | 100.0% | 0.0% | 0.15 | 0.15–0.16 | 895 | 179 | 99.9% | 0.1% | 0.11 | 0.10–0.12 |
| Ependymal Tumors | 6,877 | 1,375 | 1.7% | 45.0 | 0.43 | 0.41–0.44 | 3,913 | 783 | 55.9% | 44.1% | 0.49 | 0.47–0.50 | 2,964 | 593 | 61.3% | 38.7% | 0.37 | 0.35–0.38 |
| Malignant | 4,005 | 801 | 1.0% | 23.0 | 0.25 | 0.24–0.26 | 2,189 | 438 | -- | -- | 0.28 | 0.26–0.29 | 1,816 | 363 | -- | -- | 0.23 | 0.22–0.24 |
| Non-Malignant | 2,872 | 574 | 0.7% | 47.0 | 0.17 | 0.17–0.18 | 1,724 | 345 | -- | -- | 0.21 | 0.20–0.22 | 1,148 | 230 | -- | -- | 0.14 | 0.13–0.15 |
| Glioma Malignant, NOS | 7,751 | 1,550 | 1.9% | 36.0 | 0.49 | 0.47–0.50 | 3,920 | 784 | 100.0% | 0.0% | 0.51 | 0.49–0.53 | 3,831 | 766 | 100.0% | 0.0% | 0.47 | 0.45–0.48 |
| Choroid Plexus Tumors | 817 | 163 | 0.2% | 19.0 | 0.05 | 0.05–0.06 | 412 | 82 | 16.0% | 84.0% | 0.05 | 0.05–0.06 | 405 | 81 | 16.0% | 84.0% | 0.05 | 0.05–0.06 |
| Malignant | 131 | 26 | 0.0% | 2.0 | 0.01 | 0.01-0.01 | 66 | 13 | -- | -- | 0.01 | 0.01-0.01 | 65 | 13 | -- | -- | 0.01 | 0.01-0.01 |
| Non-Malignant | 686 | 137 | 0.2% | 23.5 | 0.04 | 0.04–0.05 | 346 | 69 | -- | -- | 0.04 | 0.04–0.05 | 340 | 68 | -- | -- | 0.04 | 0.04–0.05 |
| Other Neuroepithelial Tumors | 109 | 22 | 0.0% | 30.0 | 0.01 | 0.01-0.01 | 40 | 8 | 47.5% | 52.5% | 0.01 | 0.00–0.01 | 69 | 14 | 76.8% | 23.2% | 0.01 | 0.01-0.01 |
| Malignant | 72 | 14 | 0.0% | 26.5 | 0.00 | 0.00–0.01 | 19 | 4 | -- | -- | 0.00 | 0.00-0.00 | 53 | 11 | -- | -- | 0.01 | 0.01-0.01 |
| Non-Malignant | 37 | 7 | 0.0% | 38.0 | 0.00 | 0.00-0.00 | 21 | 4 | -- | -- | 0.00 | 0.00-0.00 | 16 | 3 | -- | -- | 0.00 | 0.00-0.00 |
| Neuronal and Mixed Neuronal Glial Tumors | 4,852 | 970 | 1.2% | 27.0 | 0.31 | 0.30–0.32 | 2,640 | 528 | 21.6% | 78.4% | 0.34 | 0.33–0.35 | 2,212 | 442 | 18.4% | 81.6% | 0.29 | 0.27–0.30 |
| Malignant | 976 | 195 | 0.2% | 53.0 | 0.06 | 0.05–0.06 | 570 | 114 | -- | -- | 0.07 | 0.06–0.08 | 406 | 81 | -- | -- | 0.05 | 0.04–0.05 |
| Non-Malignant | 3,876 | 775 | 1.0% | 22.0 | 0.25 | 0.25–0.26 | 2,070 | 414 | -- | -- | 0.27 | 0.26–0.28 | 1,806 | 361 | -- | -- | 0.24 | 0.23–0.25 |
| Tumors of the Pineal Region | 796 | 159 | 0.2% | 34.5 | 0.05 | 0.05-0.05 | 340 | 68 | 67.9% | 32.1% | 0.04 | 0.04–0.05 | 456 | 91 | 46.9% | 53.1% | 0.06 | 0.05–0.06 |
| Malignant | 445 | 89 | 0.1% | 27.0. | 0.03 | 0.03-0.03 | 231 | 46 | -- | -- | 0.03 | 0.03-0.03 | 214 | 43 | -- | -- | 0.03 | 0.02–0.03 |
| Non-Malignant | 351 | 70 | 0.1% | 42.0 | 0.02 | 0.02-0.02 | 109 | 22 | -- | -- | 0.01 | 0.01–0.02 | 242 | 48 | -- | -- | 0.03 | 0.03-0.03 |
| Embryonal Tumors | 3,493 | 699 | 0.9% | 8.0 | 0.24 | 0.23–0.24 | 2044 | 409 | 97.8% | 2.2% | 0.27 | 0.26–0.29 | 1,449 | 290 | 95.7% | 4.3% | 0.20 | 0.19–0.21 |
| Tumors of Cranial and Spinal Nerves | 35,053 | 7,011 | 8.6% | 56 | 2.01 | 1.99–2.03 | 16,811 | 3,362 | 0.7% | 99.3% | 2.01 | 1.98–2.04 | 18,242 | 3,648 | 0.7% | 99.3% | 2.02 | 1.99–2.05 |
| Nerve Sheath Tumors | 35,017 | 7,003 | 8.6% | 56.0 | 2.01 | 1.99–2.03 | 16,789 | 3,358 | 0.7% | 99.3% | 2.01 | 1.98–2.04 | 18,228 | 3,646 | 0.7% | 99.3% | 2.02 | 1.99–2.05 |
| Malignant | 231 | 46 | 0.1% | 53.0 | 0.01 | 0.01–0.02 | 112 | 22 | -- | -- | 0.01 | 0.01–0.02 | 119 | 24 | -- | -- | 0.01 | 0.01–0.02 |
| Non-Malignant | 34,786 | 6,957 | 8.6% | 56.0 | 1.99 | 1.97–2.02 | 16,677 | 3,335 | -- | -- | 1.99 | 1.96–2.02 | 18,109 | 3,622 | -- | -- | 2.00 | 1.97–2.03 |
| Other Tumors of Cranial and Spinal Nerves | 36 | 7 | 0.0% | 54.0 | 0.00 | 0.00-0.00 | 22 | 4 | 0.0% | 100.0% | 0.00 | 0.00-0.00 | -- | -- | 0.0% | 100.0% | -- | -- |
| Tumors of Meninges | 157,310 | 31,462 | 38.8% | 65.0 | 8.83 | 8.79–8.88 | 43,396 | 8,679 | 2.8% | 97.2% | 5.37 | 5.32–5.42 | 113,914 | 22,783 | 1.2% | 98.8% | 11.89 | 11.82–11.96 |
| Meningioma | 152,756 | 30,551 | 37.6% | 66.0 | 8.56 | 8.51–8.60 | 41,032 | 8,206 | 1.9% | 98.1% | 5.08 | 5.03–5.13 | 111,724 | 22,345 | 0.9% | 99.1% | 11.63 | 11.56–11.70 |
| Malignant | 1,774 | 355 | 0.4% | 65.0 | 0.10 | 0.09–0.10 | 772 | 154 | -- | -- | 0.09 | 0.09–0.10 | 1,002 | 200 | -- | -- | 0.10 | 0.10–0.11 |
| Non-Malignant | 150,982 | 30,196 | 37.2% | 66.0 | 8.46 | 8.42–8.50 | 40,260 | 8,052 | -- | -- | 4.98 | 4.93–5.03 | 110,722 | 22,144 | -- | -- | 11.53 | 11.46–11.60 |
| Mesenchymal Tumors | 1,433 | 287 | 0.4% | 49.0 | 0.09 | 0.08–0.09 | 705 | 141 | 34.5% | 65.5% | 0.09 | 0.08–0.10 | 728 | 146 | 28.7% | 71.3% | 0.09 | 0.08–0.09 |
| Primary Melanocytic Lesions | 109 | 22 | 0.0% | 57.0 | 0.01 | 0.01-0.01 | 61 | 12 | 82.0% | 18.0% | 0.01 | 0.01-0.01 | 48 | 10 | 58.3% | 41.7% | 0.01 | 0.00–0.01 |
| Other Neoplasms Related to the Meninges | 3,012 | 602 | 0.7% | 49.0 | 0.18 | 0.17–0.19 | 1,598 | 320 | 8.6% | 91.4% | 0.20 | 0.19–0.21 | 1,414 | 283 | 8.7% | 91.3% | 0.17 | 0.16–0.18 |
| Lymphomas and Hematopoietic Neoplasms | 7,914 | 1,583 | 2.0% | 66.0 | 0.44 | 0.43–0.45 | 4,018 | 804 | 99.9% | 0.1% | 0.48 | 0.47–0.50 | 3,896 | 779 | 99.8% | 0.2% | 0.40 | 0.39–0.42 |
| Lymphoma | 7,680 | 1,536 | 1.9% | 66.0 | 0.43 | 0.42–0.44 | 3,881 | 776 | 100.0% | 0.0% | 0.47 | 0.45–0.48 | 3,799 | 760 | 100.0% | 0.0% | 0.39 | 0.38–0.41 |
| Other Hematopoietic Neoplasms | 234 | 47 | 0.1% | 43.0 | 0.01 | 0.01–0.02 | 137 | 27 | 95.6% | 4.4% | 0.02 | 0.01–0.02 | 97 | 19 | 91.8% | 8.2% | 0.01 | 0.01-0.01 |
| Germ Cell Tumors and Cysts | 1,543 | 309 | 0.4% | 16.0 | 0.10 | 0.10–0.11 | 1,056 | 211 | 75.8% | 24.2% | 0.14 | 0.13–0.15 | 487 | 97 | 48.7% | 51.3% | 0.07 | 0.06–0.07 |
| Germ cell tumors, cysts, and heterotopias | 1,543 | 309 | 0.4% | 16.0 | 0.10 | 0.10–0.11 | 1056 | 211 | 75.8% | 24.2% | 0.14 | 0.13–0.15 | 487 | 97 | 48.7% | 51.3% | 0.07 | 0.06–0.07 |
| Malignant | 1,037 | 207 | 0.3% | 15.0 | 0.07 | 0.07-0.07 | 800 | 160 | -- | -- | 0.10 | 0.10–0.11 | 237 | 47 | -- | -- | 0.03 | 0.03–0.04 |
| Non-Malignant | 506 | 101 | 0.1% | 25.5 | 0.03 | 0.03–0.04 | 256 | 51 | -- | -- | 0.03 | 0.03–0.04 | 250 | 50 | -- | -- | 0.03 | 0.03–0.04 |
| Tumors of Sellar Region | 71,084 | 14,217 | 17.5% | 51.0 | 4.27 | 4.24–4.31 | 32,262 | 6,452 | 0.3% | 99.7% | 3.94 | 3.89–3.98 | 38,822 | 7,764 | 0.2% | 99.8% | 4.69 | 4.65–4.74 |
| Tumors of the Pituitary | 68,020 | 13,604 | 16.8% | 51.0 | 4.08 | 4.05–4.12 | 30,726 | 6,145 | 0.3% | 99.7% | 3.74 | 3.70–3.79 | 37,294 | 7,459 | 0.2% | 99.8% | 4.51 | 4.46–4.56 |
| Malignant | 157 | 31 | 0.0% | 57.0 | 0.01 | 0.01-0.01 | 89 | 18 | -- | -- | 0.01 | 0.01-0.01 | 68 | 14 | -- | -- | 0.01 | 0.01-0.01 |
| Non-Malignant | 67,863 | 13,573 | 16.7% | 51.0 | 4.07 | 4.04–4.11 | 30,637 | 6,127 | -- | -- | 3.73 | 3.69–3.78 | 37,226 | 7,445 | -- | -- | 4.50 | 4.45–4.55 |
| Craniopharyngioma | 3,064 | 613 | 0.8% | 43.0 | 0.19 | 0.18–0.20 | 1,536 | 307 | 0.7% | 99.3% | 0.19 | 0.18–0.20 | 1,528 | 306 | 0.2% | 99.8% | 0.19 | 0.18–0.20 |
| Unclassified Tumors | 20,556 | 4,111 | 5.1% | 63.0 | 1.19 | 1.18–1.21 | 9,344 | 1,869 | 34.6% | 65.4% | 1.19 | 1.17–1.22 | 11,212 | 2,242 | 30.8% | 69.2% | 1.21 | 1.19–1.23 |
| Hemangioma | 5,982 | 1,196 | 1.5% | 50.0 | 0.36 | 0.35–0.37 | 2,600 | 520 | 0.3% | 99.7% | 0.32 | 0.31–0.34 | 3,382 | 676 | 0.3% | 99.7% | 0.40 | 0.38–0.41 |
| Neoplasm Unspecified | 14,418 | 2,884 | 3.6% | 69.0 | 0.83 | 0.81–0.84 | 6,647 | 1,329 | 48.2% | 51.8% | 0.86 | 0.84–0.88 | 7,771 | 1,554 | 44.1% | 55.9% | 0.81 | 0.79–0.82 |
| Malignant | 6,634 | 1,327 | 1.6% | 76.0 | 0.37 | 0.36–0.38 | 3,205 | 641 | -- | -- | 0.42 | 0.40–0.43 | 3,429 | 686 | -- | -- | 0.34 | 0.32–0.35 |
| Non-Malignant | 7,784 | 1,557 | 1.9% | 63.0 | 0.45 | 0.44–0.46 | 3,442 | 688 | -- | -- | 0.44 | 0.43–0.46 | 4,342 | 868 | -- | -- | 0.47 | 0.45–0.48 |
| All Other | 156 | 31 | 0.0% | 67.0 | 0.01 | 0.01-0.01 | 97 | 19 | 23.7% | 76.3% | 0.01 | 0.01–0.02 | 59 | 12 | 32.2% | 67.8% | 0.01 | 0.01-0.01 |
| TOTAL c | 405,740 | 81,148 | 100% | 60.0 | 23.41 | 23.34–23.49 | 169,868 | 33,974 | 40% | 60% | 20.82 | 20.72–20.92 | 235,872 | 47,174 | 23.2% | 76.8% | 25.84 | 25.73–25.95 |
| Malignant | 122,569 | 24,514 | 30.2% | 60.0 | 7.08 | 7.04–7.12 | 67,930 | 13,586 | -- | -- | 8.29 | 8.23–8.35 | 54,639 | 10,928 | -- | -- | 6.02 | 5.97–6.07 |
| Non-Malignant | 283,171 | 56,634 | 69.8% | 60.0 | 16.33 | 16.27–16.39 | 101,938 | 20,388 | -- | -- | 12.53 | 12.45–12.61 | 181,233 | 36,247 | -- | -- | 19.82 | 19.73–19.91 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. Refers to all brain tumors including histologies not presented in this table.
-- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations : CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
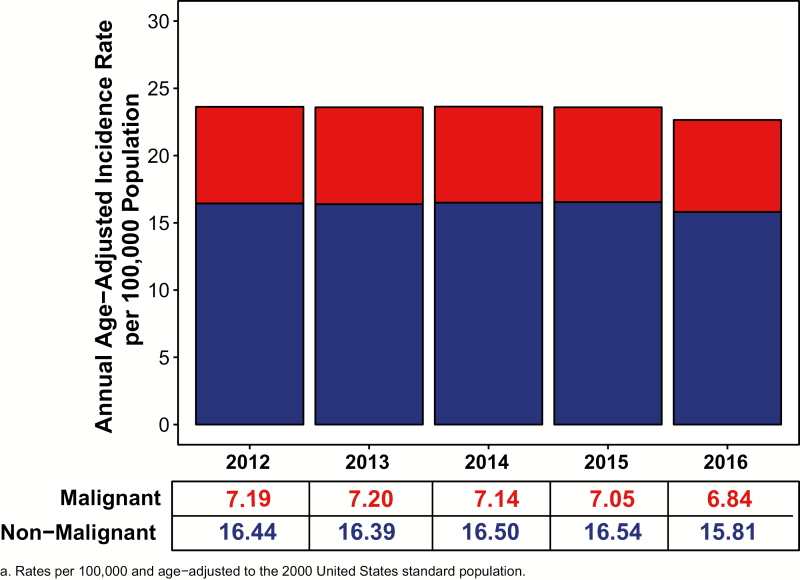
Incidence by year and behavior
Figure 6 presents the overall AAAIR of all primary brain and other CNS tumors by year, 2012–2016, and behavior. AAAIR for all primary brain and other CNS tumors, 2012–2016, did not differ substantially by year (both overall and by behavior). AAAIR stratified by sex are presented in Supplementary Figure 7.
Fig. 6.
Annual Age-Adjusted Incidence Ratesa of Primary Brain and Other CNS Tumors by Year and Behavior, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
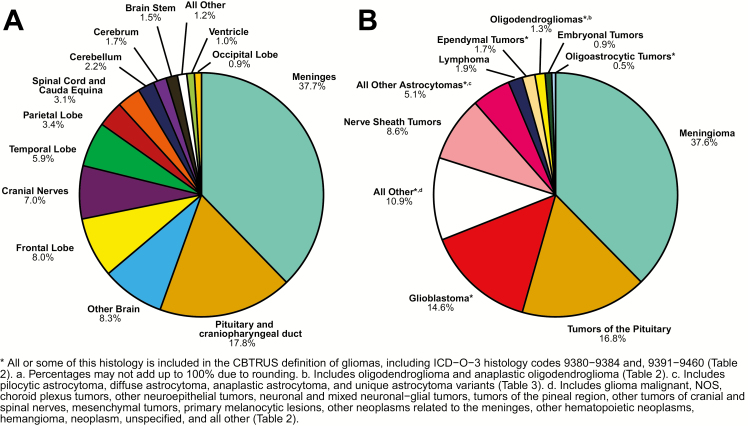
Distribution of tumors by site and histology
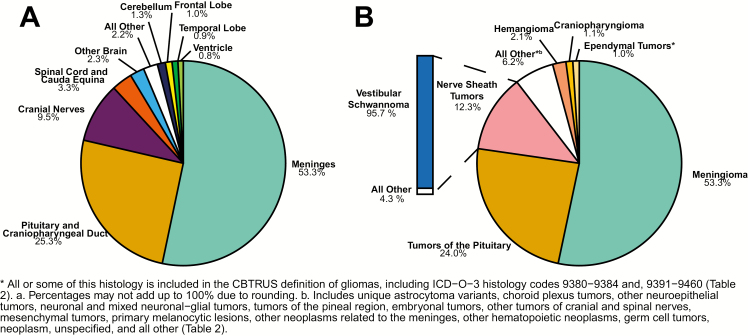
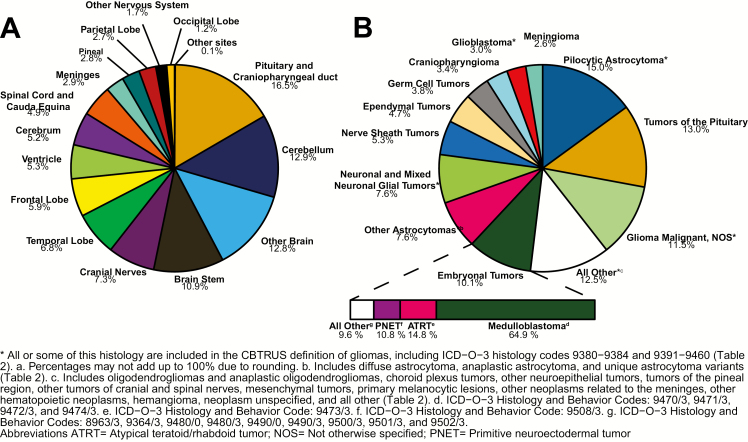
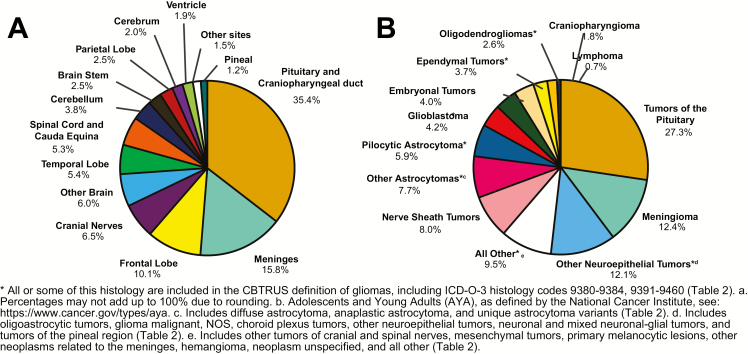
The distribution of all brain and other CNS tumors by site is shown in Figure 7A.
Fig. 7.
Distributiona of All Primary Brain and Other CNS Tumors (Five-Year Total = 405,740; Annual Average Cases = 81,148), by A) Site and B) Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Overall, the most common tumor site was the meninges, representing 37.7% of all tumors.
Frontal (8.0%), temporal (5.9%), parietal (3.4%), and occipital lobes (0.9%) accounted for 18.2% of all tumors.
The cranial nerves and the spinal cord/cauda equina accounted for 10.1% of all tumors.
The pituitary and craniopharyngeal duct accounted for 17.8% of all tumors.
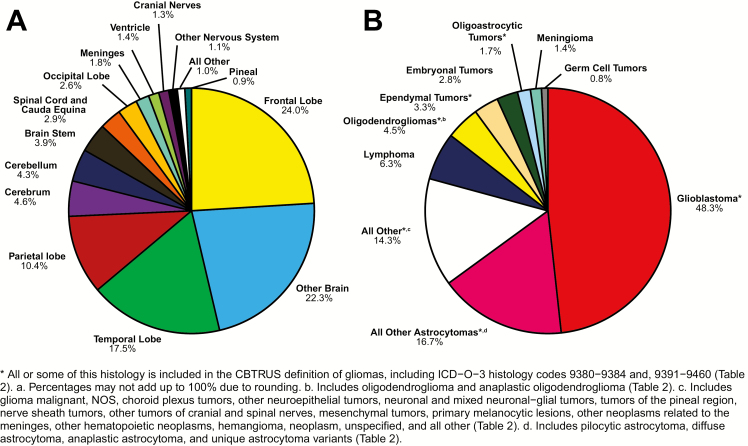
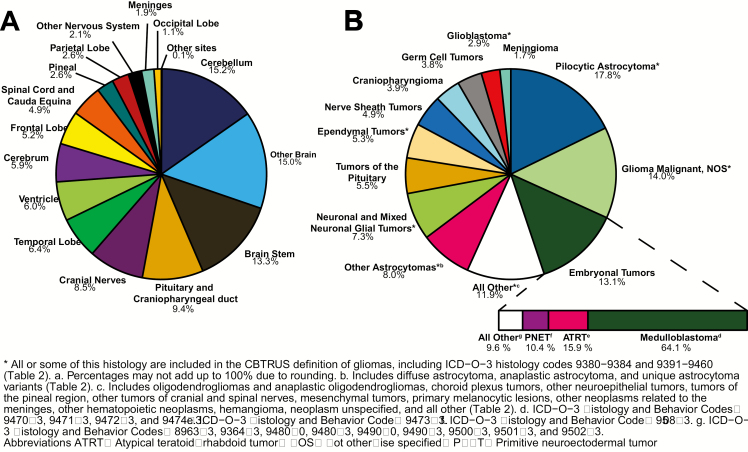
For malignant tumors, frontal (24.0%), temporal (17.5%), parietal (10.4%), and occipital (2.6%) accounted for 54.5% of tumors (Figure 8A).
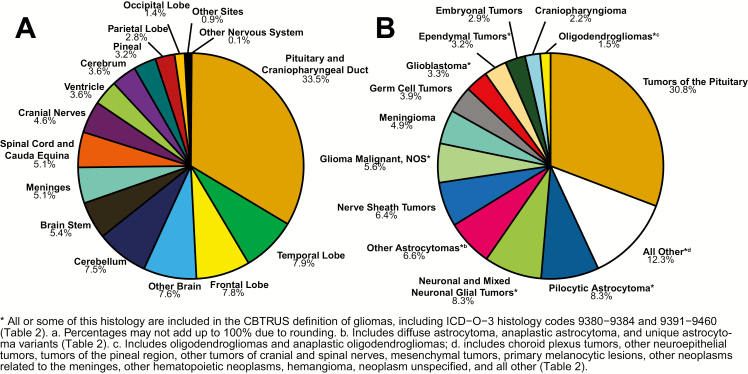
For non-malignant tumors, 53.3% of all tumors occurred in the meninges (Figure 9A).
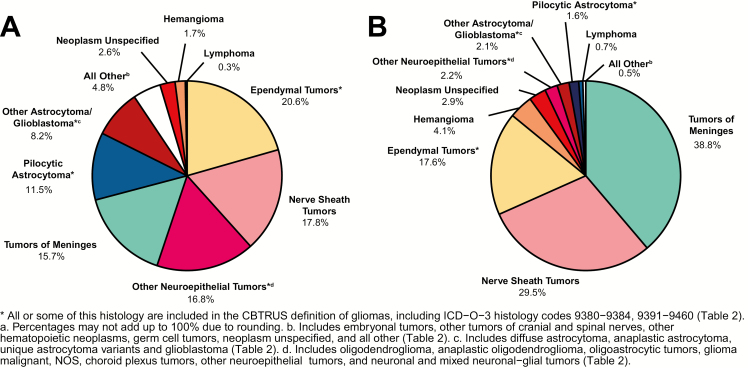
Fig. 8.
Distributiona of Malignant Primary Brain and Other CNS Tumors (Five-Year Total = 122,569; Annual Average Cases = 24,514), by A) Site and B) Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Fig. 9.
Distributiona of Non-Malignant Primary Brain and Other CNS Tumors (Five-Year Total = 283,171; Annual Average Cases = 56,634), by A) Site and B) Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Distribution of all brain and other CNS tumors by site in males only is shown in Supplementary Figure 8, and distribution of all brain and other CNS tumors by site in females only is shown in Supplementary Figure 9.
The distribution of all primary brain and other CNS tumors by histologies is shown in Figure 7B.
The most frequently reported histology overall was meningioma (37.6%), followed by tumors of the pituitary (16.8%) and glioblastoma (14.6%).
Tumors of the pituitary and nerve sheath tumors combined accounted for slightly more than one-fourth of all tumors (25.4%), the vast majority of which were non-malignant.
The distribution of malignant and non-malignant brain and other CNS tumors by histology are shown in Figure 8B and Figure 9B, respectively, as well as in Table 3.
The most common of all malignant CNS tumors was glioblastoma (48.3%).
The most common of all non-malignant tumors was meningioma (53.3%).
The most common non-malignant nerve sheath tumor (based on multiple sites in the brain and CNS) was vestibular schwannoma (defined by histology code 9560, also formerly called acoustic neuromas) (95.7%).
Distribution of all brain and other CNS tumors by histology in males only is shown in Supplementary Figure 10, and distribution of all brain and other CNS tumors by histology in females only is shown in Supplementary Figure 11.
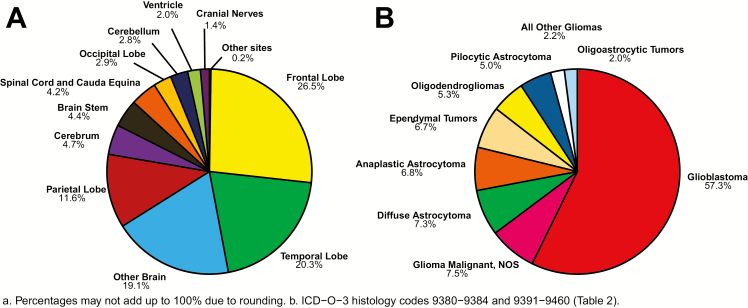
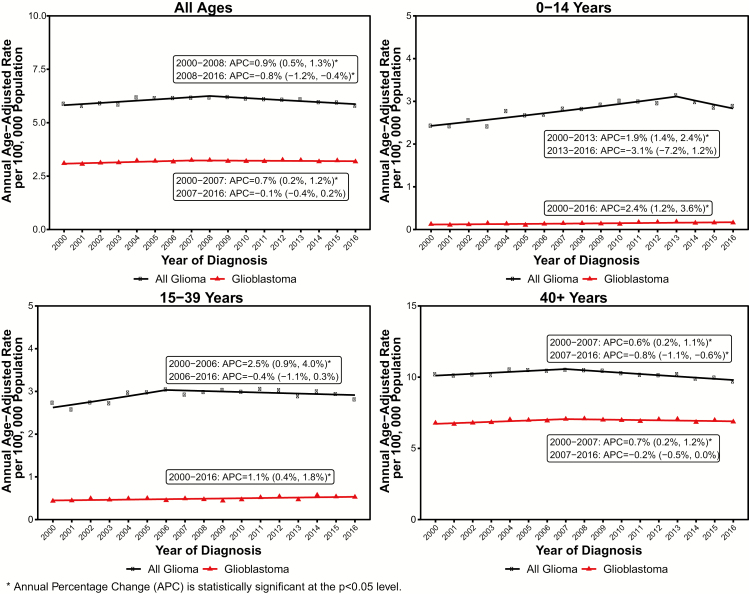
Distribution of Gliomas by site and histology
The broad category glioma (ICD-O-3 histology codes 9380–9384, 9391–9460, see Table 2 and footnotes for more information) represented approximately 25.5% of all primary brain and other CNS tumors and 80.8% of malignant tumors. The distribution of gliomas by site and histology are shown in Figure 10A and Figure 10B, respectively.
Fig. 10.
Distributiona of Primary Brain and Other CNS Gliomasb (Five-Year Total = 39,917; Annual Average Cases = 7,983) by A) Site and B) Histology Subtypes, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
The majority of gliomas occurred in the supra-tentorium (frontal, temporal, parietal, and occipital lobes combined) (61.3%). Only a very small proportion of gliomas occurred in areas of the CNS other than the brain.
Glioblastoma accounted for the majority of gliomas (57.3%).
Astrocytic tumors (pilocytic astrocytoma, anaplastic astrocytoma, diffuse astrocytoma, glioblastoma, all other gliomas) accounted for 76.4% of all gliomas.
Incidence rates by major histology grouping, specific histologies, and behavior
Incidence rates overall by major histology grouping, specific histology, and behavior are provided in Table 3.
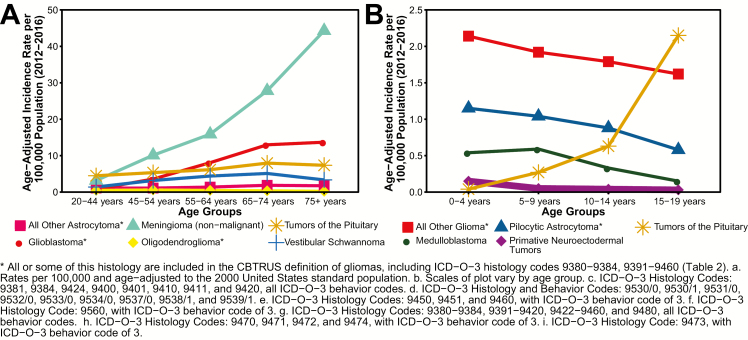
Among CBTRUS major histology groupings, AAAIR were highest for tumors of the meninges (8.83 per 100,000 population), followed by tumors of the neuroepithelial tissue (6.56 per 100,000 population), tumors of the sellar region (4.27 per 100,000 population), and tumors of the cranial and spinal nerves (2.01 per 100,000 population).
Among CBTRUS specific histologies, AAAIR were highest for meningiomas (8.58 per 100,000 population), tumors of the pituitary (4.08 per 100,000 population), glioblastomas (3.22 per 100,000 population), and nerve sheath tumors (2.01 per 100,000 population).
The majority of nerve sheath tumors are vestibular schwannoma (1.90 per 100,000, Table 4)
For malignant tumors, AAAIR was highest for glioblastoma (3.22 per 100,000 population), followed by glioma malignant, NOS (0.49 per 100,000), diffuse astrocytoma (0.46 per 100,000 population), and lymphoma (0.43 per 100,000 population).
For non-malignant tumors, AAAIR was highest for meningioma (8.6 per 100,000 population), followed by tumors of the pituitary (4.07 per 100,000 population).
Table 4.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for selected non-malignant brain and other central nervous system histologies by sex, age-groups, race, and ethnicity, CBTRUS Statistical Reportt: NPCR and SEER, 2012–2016
| Group | Vestibular Schwannomac | Pituitary Adenomad | WHO Grade I Meningiomae | WHO Grade II Meningiomaf | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-Year Total | Annual Average | Rate | 95% CI | 5-Year Total | Annual Average | Rate | 95% CI | 5-Year Total | Annual Average | Rate | 95% CI | 5-Year Total | Annual Average | Rate | 95% CI | |
| Male | 15,868 | 3,174 | 1.89 | 1.86–1.92 | 26,537 | 5,307 | 3.23 | 3.19–3.27 | 37,301 | 7,460 | 4.63 | 4.58–4.67 | 2,959 | 592 | 0.36 | 0.34–0.37 |
| Female | 17,379 | 3,476 | 1.91 | 1.88–1.94 | 31,893 | 6,379 | 3.84 | 3.80–3.88 | 106,423 | 21,285 | 11.06 | 10.99–11.13 | 4,299 | 860 | 0.47 | 0.45–0.48 |
| 0–14 years | 290 | 58 | 0.10 | 0.08–0.11 | 787 | 157 | 0.26 | 0.24–0.28 | 197 | 39 | 0.06 | 0.06–0.07 | 73 | 15 | 0.02 | 0.02–0.03 |
| 15–39 years | 4,942 | 988 | 0.96 | 0.93–0.99 | 16,599 | 3,320 | 3.15 | 3.10–3.20 | 8315 | 1,663 | 1.67 | 1.64–1.71 | 827 | 165 | 0.16 | 0.15–0.17 |
| 40–64 years | 18,137 | 3,627 | 3.29 | 3.24–3.34 | 25,604 | 5,121 | 4.83 | 4.77–4.89 | 57,454 | 11,491 | 10.18 | 10.09–10.26 | 3,387 | 677 | 0.61 | 0.59–0.63 |
| 65+ years | 9,878 | 1,976 | 4.24 | 4.16–4.33 | 15,440 | 3,088 | 6.75 | 6.65–6.86 | 77,758 | 15,552 | 34.38 | 34.13–34.62 | 2,971 | 594 | 1.30 | 1.26–1.35 |
| White | 28,481 | 5,696 | 2.00 | 1.98–2.03 | 42,232 | 8,446 | 3.16 | 3.13–3.19 | 117,347 | 23,469 | 7.88 | 7.84–7.93 | 5,687 | 1,137 | 0.39 | 0.38–0.41 |
| Black | 1,900 | 380 | 0.91 | 0.87–0.95 | 11,425 | 2,285 | 5.58 | 5.48–5.69 | 17,723 | 3,545 | 9.25 | 9.11–9.39 | 1,061 | 212 | 0.53 | 0.50–0.57 |
| American Indian/Alaska Native | 207 | 41 | 1.02 | 0.88–1.17 | 502 | 100 | 2.54 | 2.32–2.79 | 860 | 172 | 5.18 | 4.81–5.56 | 32 | 6 | 0.19 | 0.13–0.28 |
| Asian or Pacific Islander | 1,860 | 372 | 1.89 | 1.80–1.98 | 3,063 | 613 | 3.14 | 3.03–3.26 | 5,946 | 1,189 | 6.72 | 6.54–6.89 | 371 | 74 | 0.39 | 0.35–0.43 |
| Non-Hispanic | 30,369 | 6,074 | 1.99 | 1.97–2.01 | 49,190 | 9,838 | 3.43 | 3.40–3.46 | 129,882 | 25,976 | 8.13 | 8.08–8.17 | 6,602 | 1,320 | 0.43 | 0.42–0.44 |
| Hispanic | 2,878 | 576 | 1.32 | 1.27–1.37 | 9,240 | 1,848 | 3.97 | 3.88–4.05 | 13,842 | 2,768 | 7.70 | 7.56–7.83 | 656 | 131 | 0.32 | 0.30–0.35 |
| TOTAL | 33,247 | 6,649 | 1.90 | 1.88–1.92 | 58,430 | 11,686 | 3.50 | 3.47–3.53 | 143,724 | 28,745 | 8.05 | 8.00–8.09 | 7,258 | 1,452 | 0.41 | 0.40–0.42 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. ICD-O-3 histology code 9560/0.
d. ICD-O-3 histology code 8272/0 and ICD-O-3 topography code C75.1.
e. ICD-O-3 histology codes 9530/0, 9531/0, 9532/0, 9533/0, 9534/0, and 9537/0.
f. ICD-O-3 histology codes 9530/1, 9531/1, 9532/1, 9533/1, 9534/1, 9537/1, 9538/1, and 9539/1.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
Distributions and Incidence by Age
Incidence rates by age
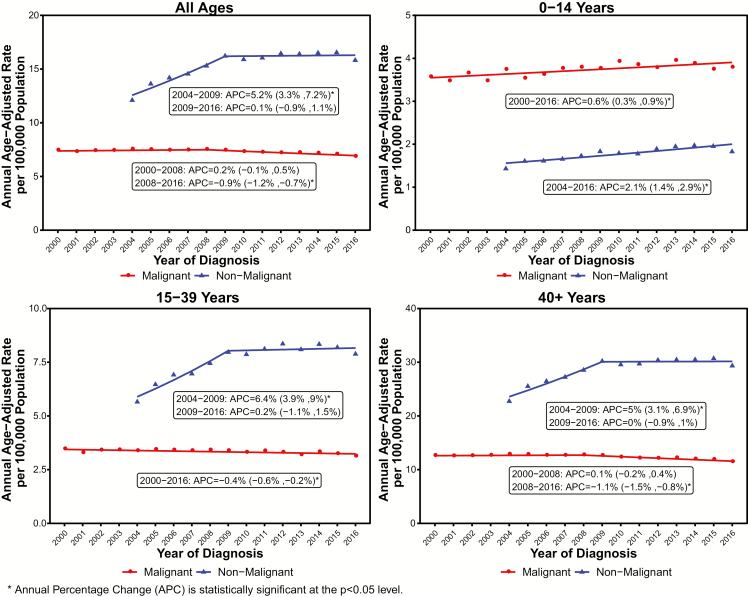
The overall AAAIR for 2012–2016 for all primary brain and other CNS tumors was 23.41 per 100,000 population (Table 3). The AAAIR was 5.74 per 100,000 population for children age 0–14 years, 11.40 per 100,000 population for adolescents and young adults age 15–39 years, and 42.14 per 100,000 population for adults age 40+ years (Table 5). AAAIR of tumors by behavior and age group (age 0–19 years and 20+ years) are shown in Figure 11. AAAIR stratified by sex are presented in Supplementary Figure 12.
Table 5.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals of all brain and other central nervous system tumors by major histology grouping, histology, and NCI age-groups, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | Age at Diagnosis | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Childrenc (Age 0–14 Years) | AYAd (Age 15–39 Years) | Adults (Age 40+ Years) | ||||||||||
| 5-year Total | Annual Average | Rate | 95% CI | 5-year Total | Annual Average | Rate | 95% CI | 5-year Total | Annual Average | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 12,693 | 2,539 | 4.15 | 4.08–4.23 | 18,297 | 3,659 | 3.46 | 3.41–3.51 | 81,290 | 16,258 | 10.31 | 10.24–10.39 |
| Pilocytic Astrocytoma | 3,118 | 624 | 1.02 | 0.98–1.06 | 1,463 | 293 | 0.27 | 0.26–0.28 | 585 | 117 | 0.08 | 0.07–0.09 |
| Diffuse Astrocytoma | 708 | 142 | 0.23 | 0.21–0.25 | 2,316 | 463 | 0.44 | 0.42–0.45 | 4,476 | 895 | 0.59 | 0.57–0.60 |
| Anaplastic Astrocytoma | 292 | 58 | 0.10 | 0.09–0.11 | 1,793 | 359 | 0.34 | 0.32–0.35 | 4,930 | 986 | 0.64 | 0.62–0.66 |
| Unique Astrocytoma Variants | 402 | 80 | 0.13 | 0.12–0.15 | 394 | 79 | 0.07 | 0.07–0.08 | 365 | 73 | 0.05 | 0.04–0.05 |
| Malignant | 162 | 32 | 0.05 | 0.05–0.06 | 292 | 58 | 0.05 | 0.05–0.06 | 331 | 66 | 0.04 | 0.04–0.05 |
| Non-Malignant | 240 | 48 | 0.08 | 0.07–0.09 | 102 | 20 | 0.02 | 0.02-0.02 | 34 | 7 | 0.00 | 0.00–0.01 |
| Glioblastoma | 503 | 101 | 0.17 | 0.15–0.18 | 2,713 | 543 | 0.53 | 0.51–0.55 | 55,948 | 11,190 | 6.95 | 6.89–7.01 |
| Oligodendroglioma | 101 | 20 | 0.03 | 0.03–0.04 | 1,429 | 286 | 0.27 | 0.26–0.29 | 2,138 | 428 | 0.30 | 0.28–0.31 |
| Anaplastic Oligodendroglioma | -- | -- | -- | -- | 465 | 93 | 0.09 | 0.08–0.10 | 1,332 | 266 | 0.18 | 0.17–0.19 |
| Oligoastrocytic Tumors | 47 | 9 | 0.02 | 0.01–0.02 | 920 | 184 | 0.17 | 0.16–0.19 | 1,136 | 227 | 0.16 | 0.15–0.17 |
| Ependymal Tumors | 934 | 187 | 0.31 | 0.29–0.33 | 1,932 | 386 | 0.37 | 0.35–0.38 | 4,011 | 802 | 0.53 | 0.52–0.55 |
| Malignant | 822 | 164 | 0.27 | 0.25–0.29 | 1,055 | 211 | 0.20 | 0.19–0.21 | 2,128 | 426 | 0.28 | 0.27–0.30 |
| Non-Malignant | 112 | 22 | 0.04 | 0.03–0.04 | 877 | 175 | 0.17 | 0.16–0.18 | 1,883 | 377 | 0.25 | 0.24–0.26 |
| Glioma Malignant, NOS | 2,456 | 491 | 0.80 | 0.77–0.84 | 1,599 | 320 | 0.30 | 0.28–0.31 | 3,696 | 739 | 0.48 | 0.47–0.50 |
| Choroid Plexus Tumors | 360 | 72 | 0.12 | 0.11–0.13 | 216 | 43 | 0.04 | 0.04–0.05 | 241 | 48 | 0.03 | 0.03–0.04 |
| Malignant | 102 | 20 | 0.03 | 0.03–0.04 | -- | -- | -- | -- | 16 | 3 | 0.00 | 0.00-0.00 |
| Non-Malignant | 258 | 52 | 0.08 | 0.07–0.10 | -- | -- | -- | -- | 225 | 45 | 0.03 | 0.03-0.03 |
| Other Neuroepithelial Tumors | 31 | 6 | 0.01 | 0.01-0.01 | 35 | 7 | 0.01 | 0.00–0.01 | 43 | 9 | 0.01 | 0.00–0.01 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | 26 | 5 | 0.00 | 0.00–0.01 |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | 17 | 3 | 0.00 | 0.00-0.00 |
| Neuronal and Mixed Neuronal Glial Tumors | 1,278 | 256 | 0.42 | 0.40–0.44 | 1,903 | 381 | 0.35 | 0.34–0.37 | 1,671 | 334 | 0.23 | 0.21–0.24 |
| Malignant | 65 | 13 | 0.02 | 0.02–0.03 | 199 | 40 | 0.04 | 0.03–0.04 | 712 | 142 | 0.09 | 0.09–0.10 |
| Non-Malignant | 1,213 | 243 | 0.40 | 0.38–0.42 | 1,704 | 341 | 0.32 | 0.30–0.33 | 959 | 192 | 0.13 | 0.12–0.14 |
| Tumors of the Pineal Region | 158 | 32 | 0.05 | 0.04–0.06 | 293 | 59 | 0.05 | 0.05–0.06 | 345 | 69 | 0.05 | 0.04–0.05 |
| Malignant | 138 | 28 | 0.05 | 0.04–0.05 | 155 | 31 | 0.03 | 0.02–0.03 | 152 | 30 | 0.02 | 0.02-0.02 |
| Non-Malignant | 20 | 4 | 0.01 | 0.00–0.01 | 138 | 28 | 0.03 | 0.02–0.03 | 193 | 39 | 0.03 | 0.02–0.03 |
| Embryonal Tumors | 2,294 | 459 | 0.75 | 0.72–0.78 | 826 | 165 | 0.15 | 0.14–0.16 | 373 | 75 | 0.05 | 0.05–0.06 |
| Medulloblastoma | 1,475 | 295 | 0.48 | 0.46–0.51 | 596 | 119 | 0.11 | 0.10–0.12 | 163 | 33 | 0.02 | 0.02–0.03 |
| Primitive Neuroectodermal Tumors | 239 | 48 | 0.08 | 0.07–0.09 | 129 | 26 | 0.02 | 0.02–0.03 | 124 | 25 | 0.02 | 0.01–0.02 |
| Atypical Teratoid/Rhabdoid Tumor | 365 | 73 | 0.12 | 0.11–0.13 | 23 | 5 | 0.00 | 0.00–0.01 | -- | -- | -- | -- |
| Other Embryonal Histologies e | 215 | 43 | 0.07 | 0.06–0.08 | 78 | 16 | 0.01 | 0.01–0.02 | -- | -- | -- | -- |
| Tumors of Cranial and Spinal Nerves | 862 | 172 | 0.28 | 0.26–0.30 | 5,325 | 1,065 | 1.03 | 1.01–1.06 | 28,866 | 5,773 | 3.68 | 3.64–3.72 |
| Nerve Sheath Tumors | 862 | 172 | 0.28 | 0.26–0.30 | 5,316 | 1,063 | 1.03 | 1.00–1.06 | 28,839 | 5,768 | 3.68 | 3.63–3.72 |
| Malignant | -- | -- | -- | -- | 49 | 10 | 0.01 | 0.01-0.01 | 170 | 34 | 0.02 | 0.02–0.03 |
| Non-Malignant | -- | -- | -- | -- | 5,267 | 1,053 | 1.02 | 0.99–1.05 | 28,669 | 5,734 | 3.65 | 3.61–3.70 |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | 27 | 5 | 0.00 | 0.00–0.01 |
| Tumors of Meninges | 563 | 113 | 0.18 | 0.17–0.20 | 10,583 | 2,117 | 2.11 | 2.07–2.15 | 146,164 | 29,233 | 18.69 | 18.59–18.79 |
| Meningioma | 293 | 59 | 0.10 | 0.09–0.11 | 9,260 | 1,852 | 1.86 | 1.82–1.90 | 143,203 | 28,641 | 18.30 | 18.21–18.40 |
| Malignant | 23 | 5 | 0.01 | 0.00–0.01 | 118 | 24 | 0.02 | 0.02–0.03 | 1,633 | 327 | 0.21 | 0.20–0.22 |
| Non-Malignant | 270 | 54 | 0.09 | 0.08–0.10 | 9,142 | 1,828 | 1.84 | 1.80–1.87 | 141,570 | 28,314 | 18.10 | 18.00–18.19 |
| Mesenchymal Tumors | 203 | 41 | 0.07 | 0.06–0.08 | 342 | 68 | 0.06 | 0.06–0.07 | 888 | 178 | 0.12 | 0.11–0.12 |
| Primary Melanocytic Lesions | -- | -- | -- | -- | 16 | 3 | 0.00 | 0.00-0.00 | 85 | 17 | 0.01 | 0.01-0.01 |
| Other Neoplasms Related to the Meninges | -- | -- | -- | -- | 965 | 193 | 0.18 | 0.17–0.19 | 1,988 | 398 | 0.26 | 0.25–0.27 |
| Lymphomas and Hematopoietic Neoplasms | 82 | 16 | 0.03 | 0.02–0.03 | 561 | 112 | 0.11 | 0.10–0.12 | 7,271 | 1,454 | 0.92 | 0.90–0.95 |
| Lymphoma | 30 | 6 | 0.01 | 0.01-0.01 | 502 | 100 | 0.10 | 0.09–0.11 | 7,148 | 1,430 | 0.91 | 0.89–0.93 |
| Other Hematopoietic Neoplasms | 52 | 10 | 0.02 | 0.01–0.02 | 59 | 12 | 0.01 | 0.01-0.01 | 123 | 25 | 0.02 | 0.01–0.02 |
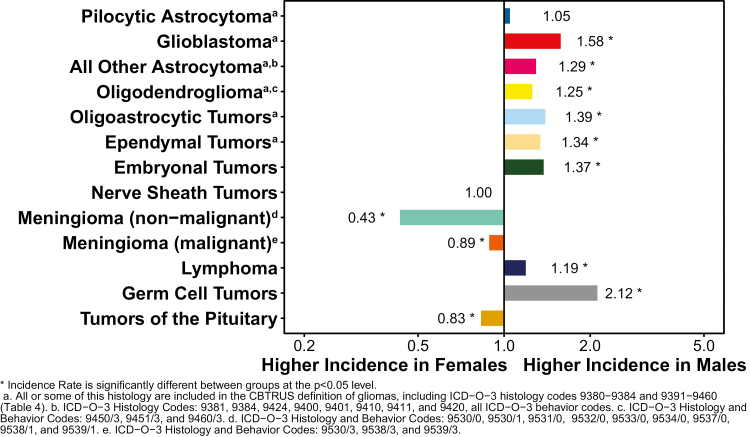
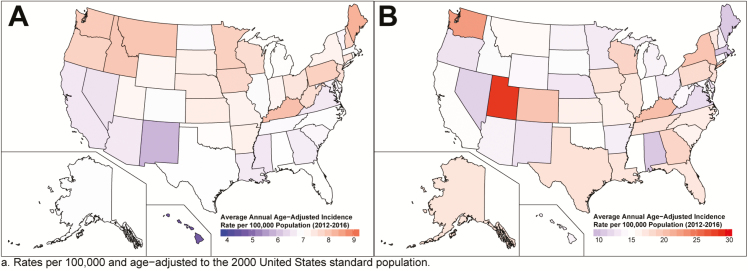
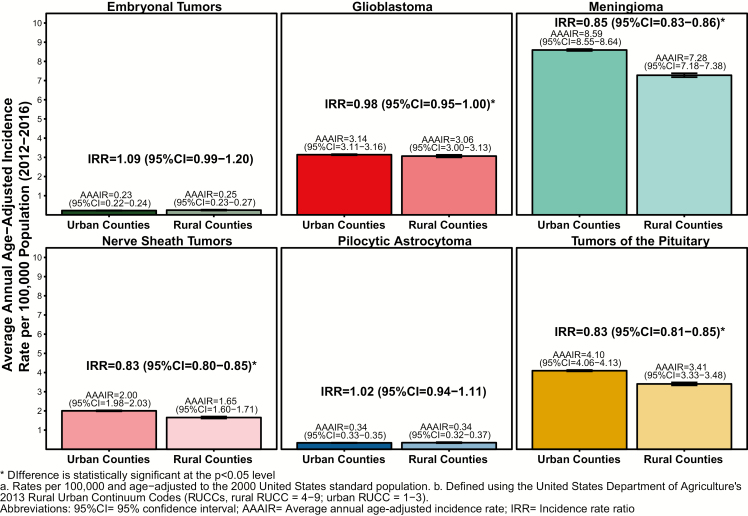
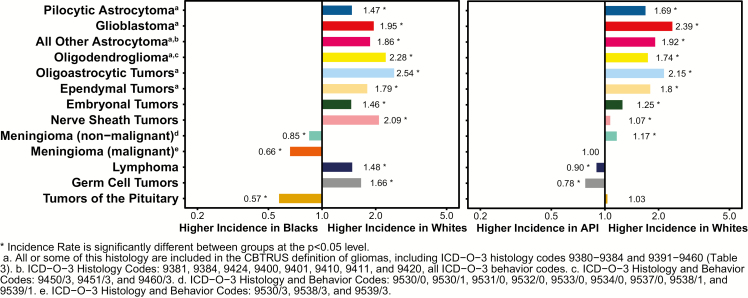
| Germ Cell Tumors and Cysts | 666 | 133 | 0.22 | 0.20–0.24 | 682 | 136 | 0.12 | 0.12–0.13 | 195 | 39 | 0.03 | 0.02–0.03 |
| Germ cell tumors, cysts, and heterotopias | 666 | 133 | 0.22 | 0.20–0.24 | 682 | 136 | 0.12 | 0.12–0.13 | 195 | 39 | 0.03 | 0.02–0.03 |
| Malignant | 479 | 96 | 0.16 | 0.14–0.17 | 530 | 106 | 0.10 | 0.09–0.10 | 28 | 6 | 0.00 | 0.00–0.01 |
| Non-Malignant | 187 | 37 | 0.06 | 0.05–0.07 | 152 | 30 | 0.03 | 0.02–0.03 | 167 | 33 | 0.02 | 0.02–0.03 |
| Tumors of Sellar Region | 1,646 | 329 | 0.54 | 0.52–0.57 | 20,816 | 4,163 | 3.95 | 3.90–4.00 | 48,622 | 9,724 | 6.40 | 6.34–6.46 |
| Tumors of the Pituitary | 958 | 192 | 0.32 | 0.30–0.34 | 20,115 | 4,023 | 3.82 | 3.76–3.87 | 46,947 | 9,389 | 6.18 | 6.13–6.24 |
| Malignant | -- | -- | -- | -- | 26 | 5 | 0.01 | 0.00–0.01 | 131 | 26 | 0.02 | 0.01–0.02 |
| Non-Malignant | -- | -- | -- | -- | 20,089 | 4018 | 3.81 | 3.76–3.87 | 46,816 | 9,363 | 6.17 | 6.11–6.22 |
| Craniopharyngioma | 688 | 138 | 0.23 | 0.21–0.24 | 701 | 140 | 0.13 | 0.12–0.14 | 1,675 | 335 | 0.22 | 0.21–0.23 |
| Unclassified Tumors | 1,028 | 206 | 0.34 | 0.32–0.36 | 3,251 | 650 | 0.62 | 0.60–0.64 | 16,277 | 3,255 | 2.10 | 2.07–2.13 |
| Hemangioma | 375 | 75 | 0.12 | 0.11–0.14 | 1,605 | 321 | 0.31 | 0.29–0.32 | 4,002 | 800 | 0.52 | 0.51–0.54 |
| Neoplasm Unspecified | 623 | 125 | 0.20 | 0.19–0.22 | 1,632 | 326 | 0.31 | 0.29–0.33 | 12,163 | 2,433 | 1.56 | 1.53–1.59 |
| Malignant | 174 | 35 | 0.06 | 0.05–0.07 | 373 | 75 | 0.07 | 0.06–0.08 | 6,087 | 1,217 | 0.77 | 0.75–0.79 |
| Non-Malignant | 449 | 90 | 0.15 | 0.13–0.16 | 1,259 | 252 | 0.24 | 0.23–0.25 | 6,076 | 1,215 | 0.79 | 0.77–0.81 |
| All Other | 30 | 6 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | 112 | 22 | 0.01 | 0.01–0.02 |
| TOTAL f | 17,540 | 3,508 | 5.74 | 5.66–5.83 | 59,515 | 11,903 | 11.40 | 11.31–11.49 | 328,685 | 65,737 | 42.14 | 41.99–42.28 |
| Malignant | 11,697 | 2,339 | 3.83 | 3.76–3.90 | 17,066 | 3,413 | 3.23 | 3.18–3.28 | 93,806 | 18,761 | 11.88 | 11.80–11.96 |
| Non-Malignant | 5,843 | 1,169 | 1.92 | 1.87–1.97 | 42,449 | 8,490 | 8.17 | 8.09–8.25 | 234,879 | 46,976 | 30.26 | 30.13–30.38 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. Children as defined by the National Cancer Institute, see: https://www.cancer.gov/research/areas/childhood.
d. Adolescents and Young Adults (AYA), as defined by the National Cancer Institute, see: https://www.cancer.gov/types/aya.
e. ICD-O-3 histology and behavior codes: 8963/3, 9364/3, 9480/3, 9490/0, 9490/3, 9500/3, 9501/3, and 9502/3.
f. Refers to all brain tumors including histologies not presented in this table.
-- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: AYA, Adolescents and young adults; CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
Fig. 11.
Average Annual Age-Adjusted Incidence Ratesa of All Primary Brain and Other CNS Tumors by Age and Behavior, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Incidence rates by age and histology
AAAIR by age and histology at diagnosis are presented in Tables 5–7, as well as in Figure 12A (Age 20+ Years), and Figure 12B (Age 0–19 Years).
Table 6.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for children and adolescents (age 0–19 years), brain and other central nervous system tumors by major histology grouping, histology, and age at diagnosis, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | Age at Diagnosis | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–19 Years | 0–4 Years | 5–9 Years | 10–14 Years | 15–19 Years | ||||||||||||||||
| 5-Year Total | Annual Average | Rate | 95% CI | 5-Year Total | Annual Average | Rate | 95% CI | 5-Year Total | Annual Average | Rate | 95% CI | 5-Year Total | Annual Average | Rate | 95% CI | 5-Year Total | Annual Average | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 15,778 | 3,156 | 3.84 | 3.78–3.90 | 4,972 | 994 | 4.99 | 4.86–5.14 | 4072 | 814 | 3.97 | 3.85–4.10 | 3,649 | 730 | 3.53 | 3.42–3.65 | 3,085 | 617 | 2.91 | 2.81–3.02 |
| Pilocytic Astrocytoma | 3,730 | 746 | 0.91 | 0.88–0.94 | 1143 | 229 | 1.15 | 1.08–1.22 | 1068 | 214 | 1.04 | 0.98–1.11 | 907 | 181 | 0.88 | 0.82–0.94 | 612 | 122 | 0.58 | 0.53–0.63 |
| Diffuse Astrocytoma | 968 | 194 | 0.24 | 0.22–0.25 | 272 | 54 | 0.27 | 0.24–0.31 | 197 | 39 | 0.19 | 0.17–0.22 | 239 | 48 | 0.23 | 0.20–0.26 | 260 | 52 | 0.25 | 0.22–0.28 |
| Anaplastic Astrocytoma | 406 | 81 | 0.10 | 0.09–0.11 | 69 | 14 | 0.07 | 0.05–0.09 | 116 | 23 | 0.11 | 0.09–0.14 | 107 | 21 | 0.10 | 0.08–0.13 | 114 | 23 | 0.11 | 0.09–0.13 |
| Unique Astrocytoma Variants | 519 | 104 | 0.13 | 0.12–0.14 | 112 | 22 | 0.11 | 0.09–0.14 | 139 | 28 | 0.14 | 0.11–0.16 | 151 | 30 | 0.15 | 0.12–0.17 | 117 | 23 | 0.11 | 0.09–0.13 |
| Malignant | 243 | 49 | 0.06 | 0.05–0.07 | 18 | 4 | 0.02 | 0.01–0.03 | 57 | 11 | 0.06 | 0.04–0.07 | 87 | 17 | 0.08 | 0.07–0.10 | 81 | 16 | 0.08 | 0.06–0.10 |
| Non-Malignant | 276 | 55 | 0.07 | 0.06–0.08 | 94 | 19 | 0.09 | 0.08–0.12 | 82 | 16 | 0.08 | 0.06–0.10 | 64 | 13 | 0.06 | 0.05–0.08 | 36 | 7 | 0.03 | 0.02–0.05 |
| Glioblastoma | 744 | 149 | 0.18 | 0.17–0.19 | 124 | 25 | 0.12 | 0.10–0.15 | 175 | 35 | 0.17 | 0.15–0.20 | 204 | 41 | 0.20 | 0.17–0.23 | 241 | 48 | 0.23 | 0.20–0.26 |
| Oligodendroglioma | 195 | 39 | 0.05 | 0.04–0.05 | 20 | 4 | 0.02 | 0.01–0.03 | 34 | 7 | 0.03 | 0.02–0.05 | 47 | 9 | 0.05 | 0.03–0.06 | 94 | 19 | 0.09 | 0.07–0.11 |
| Anaplastic Oligodendroglioma | 27 | 5 | 0.01 | 0.00–0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 16 | 3 | 0.02 | 0.01–0.02 |
| Oligoastrocytic Tumors | 84 | 17 | 0.02 | 0.02–0.03 | -- | -- | -- | -- | 18 | 4 | 0.02 | 0.01–0.03 | 17 | 3 | 0.02 | 0.01–0.03 | 37 | 7 | 0.03 | 0.02–0.05 |
| Ependymal Tumors | 1,173 | 235 | 0.29 | 0.27–0.30 | 435 | 87 | 0.44 | 0.40–0.48 | 242 | 48 | 0.24 | 0.21–0.27 | 257 | 51 | 0.25 | 0.22–0.28 | 239 | 48 | 0.23 | 0.20–0.26 |
| Malignant | 985 | 197 | 0.24 | 0.22–0.26 | 418 | 84 | 0.42 | 0.38–0.46 | 217 | 43 | 0.21 | 0.18–0.24 | 187 | 37 | 0.18 | 0.16–0.21 | 163 | 33 | 0.15 | 0.13–0.18 |
| Non-Malignant | 188 | 38 | 0.05 | 0.04–0.05 | 17 | 3 | 0.02 | 0.01–0.03 | 25 | 5 | 0.02 | 0.02–0.04 | 70 | 14 | 0.07 | 0.05–0.09 | 76 | 15 | 0.07 | 0.06–0.09 |
| Glioma Malignant, NOS | 2,870 | 574 | 0.70 | 0.67–0.73 | 936 | 187 | 0.94 | 0.88–1.00 | 902 | 180 | 0.88 | 0.82–0.94 | 618 | 124 | 0.60 | 0.55–0.65 | 414 | 83 | 0.39 | 0.35–0.43 |
| Choroid Plexus Tumors | 409 | 82 | 0.10 | 0.09–0.11 | 258 | 52 | 0.26 | 0.23–0.29 | 52 | 10 | 0.05 | 0.04–0.07 | 50 | 10 | 0.05 | 0.04–0.06 | 49 | 10 | 0.05 | 0.03–0.06 |
| Malignant | 105 | 21 | 0.03 | 0.02–0.03 | 85 | 17 | 0.09 | 0.07–0.11 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 304 | 61 | 0.07 | 0.07–0.08 | 173 | 35 | 0.17 | 0.15–0.20 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neuroepithelial Tumors | 38 | 8 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Neuronal and Mixed Neuronal Glial Tumors | 1,889 | 378 | 0.46 | 0.44–0.48 | 332 | 66 | 0.33 | 0.30–0.37 | 360 | 72 | 0.35 | 0.32–0.39 | 586 | 117 | 0.57 | 0.52–0.62 | 611 | 122 | 0.58 | 0.53–0.62 |
| Malignant | 100 | 20 | 0.02 | 0.02–0.03 | 25 | 5 | 0.03 | 0.02–0.04 | 16 | 3 | 0.02 | 0.01–0.03 | 24 | 5 | 0.02 | 0.01–0.03 | 35 | 7 | 0.03 | 0.02–0.05 |
| Non-Malignant | 1,789 | 358 | 0.43 | 0.41–0.46 | 307 | 61 | 0.31 | 0.27–0.35 | 344 | 69 | 0.34 | 0.30–0.37 | 562 | 112 | 0.54 | 0.50–0.59 | 576 | 115 | 0.54 | 0.50–0.59 |
| Tumors of the Pineal Region | 218 | 44 | 0.05 | 0.05–0.06 | 70 | 14 | 0.07 | 0.05–0.09 | 43 | 9 | 0.04 | 0.03–0.06 | 45 | 9 | 0.04 | 0.03–0.06 | 60 | 12 | 0.06 | 0.04–0.07 |
| Malignant | 180 | 36 | 0.04 | 0.04–0.05 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 42 | 8 | 0.04 | 0.03–0.05 |
| Non-Malignant | 38 | 8 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 18 | 4 | 0.02 | 0.01–0.03 |
| Embryonal Tumors | 2,508 | 502 | 0.61 | 0.59–0.64 | 1,173 | 235 | 1.18 | 1.11–1.25 | 713 | 143 | 0.70 | 0.65–0.75 | 408 | 82 | 0.40 | 0.36–0.44 | 214 | 43 | 0.20 | 0.18–0.23 |
| Medulloblastoma | 1,632 | 326 | 0.40 | 0.38–0.42 | 535 | 107 | 0.54 | 0.49–0.58 | 603 | 121 | 0.59 | 0.54–0.64 | 337 | 67 | 0.33 | 0.29–0.36 | 157 | 31 | 0.15 | 0.13–0.17 |
| Primitive Neuroectodermal Tumors | 270 | 54 | 0.07 | 0.06–0.07 | 145 | 29 | 0.15 | 0.12–0.17 | 55 | 11 | 0.05 | 0.04–0.07 | 39 | 8 | 0.04 | 0.03–0.05 | 31 | 6 | 0.03 | 0.02–0.04 |
| Atypical Teratoid/Rhabdoid Tumor | 370 | 74 | 0.09 | 0.08–0.10 | 322 | 64 | 0.32 | 0.29–0.36 | 30 | 6 | 0.03 | 0.02–0.04 | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Embryonal Histologies c | 236 | 47 | 0.06 | 0.05–0.07 | 171 | 34 | 0.17 | 0.15–0.20 | 25 | 5 | 0.02 | 0.02–0.04 | 19 | 4 | 0.02 | 0.01–0.03 | 21 | 4 | 0.02 | 0.01–0.03 |
| Tumors of Cranial and Spinal Nerves | 1,336 | 267 | 0.32 | 0.31–0.34 | 303 | 61 | 0.30 | 0.27–0.34 | 252 | 50 | 0.25 | 0.22–0.28 | 307 | 61 | 0.30 | 0.27–0.33 | 474 | 95 | 0.45 | 0.41–0.49 |
| Nerve Sheath Tumors | 1,333 | 267 | 0.32 | 0.31–0.34 | 303 | 61 | 0.30 | 0.27–0.34 | 252 | 50 | 0.25 | 0.22–0.28 | 307 | 61 | 0.30 | 0.27–0.33 | 471 | 94 | 0.44 | 0.41–0.49 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Meninges | 1,132 | 226 | 0.27 | 0.26–0.29 | 185 | 37 | 0.19 | 0.16–0.22 | 133 | 27 | 0.13 | 0.11–0.15 | 245 | 49 | 0.24 | 0.21–0.27 | 569 | 114 | 0.54 | 0.49–0.58 |
| Meningioma | 653 | 131 | 0.16 | 0.15–0.17 | 73 | 15 | 0.07 | 0.06–0.09 | 73 | 15 | 0.07 | 0.06–0.09 | 147 | 29 | 0.14 | 0.12–0.17 | 360 | 72 | 0.34 | 0.31–0.38 |
| Malignant | 37 | 7 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 616 | 123 | 0.15 | 0.14–0.16 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Mesenchymal Tumors | 254 | 51 | 0.06 | 0.05–0.07 | 105 | 21 | 0.11 | 0.09–0.13 | 50 | 10 | 0.05 | 0.04–0.06 | 48 | 10 | 0.05 | 0.03–0.06 | 51 | 10 | 0.05 | 0.04–0.06 |
| Primary Melanocytic Lesions | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neoplasms Related to the Meninges | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Lymphomas and Hematopoietic Neoplasms | 131 | 26 | 0.03 | 0.03–0.04 | -- | -- | -- | -- | 37 | 7 | 0.04 | 0.03–0.05 | 30 | 6 | 0.03 | 0.02–0.04 | 49 | 10 | 0.05 | 0.03–0.06 |
| Lymphoma | 64 | 13 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 34 | 7 | 0.03 | 0.02–0.04 |
| Other Hematopoietic Neoplasms | 67 | 13 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Germ Cell Tumors and Cysts | 951 | 190 | 0.23 | 0.22–0.25 | 186 | 37 | 0.19 | 0.16–0.22 | 153 | 31 | 0.15 | 0.13–0.17 | 327 | 65 | 0.32 | 0.28–0.35 | 285 | 57 | 0.27 | 0.24–0.30 |
| Germ cell tumors, cysts, and heterotopias | 951 | 190 | 0.23 | 0.22–0.25 | 186 | 37 | 0.19 | 0.16–0.22 | 153 | 31 | 0.15 | 0.13–0.17 | 327 | 65 | 0.32 | 0.28–0.35 | 285 | 57 | 0.27 | 0.24–0.30 |
| Malignant | 733 | 147 | 0.18 | 0.17–0.19 | 77 | 15 | 0.08 | 0.06–0.10 | 110 | 22 | 0.11 | 0.09–0.13 | 292 | 58 | 0.28 | 0.25–0.32 | 254 | 51 | 0.24 | 0.21–0.27 |
| Non-Malignant | 218 | 44 | 0.05 | 0.05–0.06 | 109 | 22 | 0.11 | 0.09–0.13 | 43 | 9 | 0.04 | 0.03–0.06 | 35 | 7 | 0.03 | 0.02–0.05 | 31 | 6 | 0.03 | 0.02–0.04 |
| Tumors of Sellar Region | 4,080 | 816 | 0.98 | 0.95–1.01 | 179 | 36 | 0.18 | 0.15–0.21 | 583 | 117 | 0.57 | 0.52–0.62 | 884 | 177 | 0.86 | 0.80–0.91 | 2,434 | 487 | 2.30 | 2.21–2.39 |
| Tumors of the Pituitary | 3,232 | 646 | 0.78 | 0.75–0.80 | 40 | 8 | 0.04 | 0.03–0.05 | 272 | 54 | 0.27 | 0.23–0.30 | 646 | 129 | 0.63 | 0.58–0.68 | 2,274 | 455 | 2.15 | 2.06–2.24 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | --- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Craniopharyngioma | 848 | 170 | 0.21 | 0.19–0.22 | 139 | 28 | 0.14 | 0.12–0.16 | 311 | 62 | 0.30 | 0.27–0.34 | 238 | 48 | 0.23 | 0.20–0.26 | 160 | 32 | 0.15 | 0.13–0.18 |
| Unclassified Tumors | 1,523 | 305 | 0.37 | 0.35–0.39 | 354 | 71 | 0.36 | 0.32–0.40 | 287 | 57 | 0.28 | 0.25–0.31 | 387 | 77 | 0.37 | 0.34–0.41 | 495 | 99 | 0.47 | 0.43–0.51 |
| Hemangioma | 601 | 120 | 0.15 | 0.13–0.16 | 139 | 28 | 0.14 | 0.12–0.17 | 95 | 19 | 0.09 | 0.08–0.11 | 141 | 28 | 0.14 | 0.11–0.16 | 226 | 45 | 0.21 | 0.19–0.24 |
| Neoplasm Unspecified | 886 | 177 | 0.22 | 0.20–0.23 | 199 | 40 | 0.20 | 0.17–0.23 | 187 | 37 | 0.18 | 0.16–0.21 | 237 | 47 | 0.23 | 0.20–0.26 | 263 | 53 | 0.25 | 0.22–0.28 |
| Malignant | 225 | 45 | 0.05 | 0.05–0.06 | 74 | 15 | 0.07 | 0.06–0.09 | 52 | 10 | 0.05 | 0.04–0.07 | 48 | 10 | 0.05 | 0.03–0.06 | 51 | 10 | 0.05 | 0.04–0.06 |
| Non-Malignant | 661 | 132 | 0.16 | 0.15–0.17 | 125 | 25 | 0.13 | 0.10–0.15 | 135 | 27 | 0.13 | 0.11–0.16 | 189 | 38 | 0.18 | 0.16–0.21 | 212 | 42 | 0.20 | 0.17–0.23 |
| All Other | 36 | 7 | 0.01 | 0.01-0.01 | 16 | 3 | 0.02 | 0.01–0.03 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| TOTAL d | 24,931 | 4,986 | 6.06 | 5.98–6.13 | 6,194 | 1,239 | 6.22 | 6.07–6.38 | 5,517 | 1,103 | 5.38 | 5.24–5.53 | 5,829 | 1,166 | 5.65 | 5.50–5.79 | 7,391 | 1,478 | 6.98 | 6.82–7.14 |
| Malignant | 14,421 | 2,884 | 3.51 | 3.45–3.57 | 4,580 | 916 | 4.60 | 4.47–4.74 | 3,807 | 761 | 3.72 | 3.60–3.84 | 3,310 | 662 | 3.21 | 3.10–3.32 | 2,724 | 545 | 2.57 | 2.48–2.67 |
| Non-Malignant | 10,510 | 2,102 | 2.54 | 2.50–2.59 | 1,614 | 323 | 1.62 | 1.54–1.70 | 1,710 | 342 | 1.67 | 1.59–1.75 | 2,519 | 504 | 2.44 | 2.35–2.54 | 4,667 | 933 | 4.41 | 4.28–4.54 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. ICD-O-3 histology and behavior codes: 8963/3, 9364/3, 9480/3, 9490/0, 9490/3, 9500/3, 9501/3, and 9502/3.
d. Refers to all brain tumors including histologies not presented in this table.
-- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
Table 7.
Average annual age-specific incidence ratesa with 95% confidence intervals for all brain and other central nervous system tumors by major histology grouping, histology, and age at diagnosis, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | Age At Diagnosis | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 20–34 Years | 35–44 Years | 45–54 Years | 55–64 Years | 65–74 Years | 75–84 Years | 85+ Years | ||||||||
| Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 3.34 | 3.28–3.40 | 4.44 | 4.35–4.54 | 6.67 | 6.56–6.78 | 11.32 | 11.17–11.47 | 16.88 | 16.65–17.10 | 19.34 | 19.01–19.67 | 12.21 | 11.82–12.60 |
| Pilocytic Astrocytoma | 0.21 | 0.20–0.23 | 0.12 | 0.11–0.14 | 0.09 | 0.08–0.11 | 0.07 | 0.06–0.08 | 0.06 | 0.05–0.08 | 0.07 | 0.05–0.09 | -- | -- |
| Diffuse Astrocytoma | 0.47 | 0.44–0.49 | 0.49 | 0.46–0.52 | 0.47 | 0.44–0.50 | 0.59 | 0.56–0.63 | 0.80 | 0.75–0.85 | 0.89 | 0.82–0.96 | 0.49 | 0.42–0.58 |
| Anaplastic Astrocytoma | 0.37 | 0.35–0.39 | 0.47 | 0.44–0.50 | 0.50 | 0.47–0.53 | 0.67 | 0.64–0.71 | 0.93 | 0.88–0.99 | 0.94 | 0.87–1.02 | 0.42 | 0.35–0.50 |
| Unique Astrocytoma Variants | 0.07 | 0.06–0.08 | 0.04 | 0.04–0.06 | 0.03 | 0.03–0.04 | 0.04 | 0.03–0.05 | 0.07 | 0.05–0.08 | 0.08 | 0.06–0.11 | 0.07 | 0.05–0.11 |
| Malignant | 0.05 | 0.04–0.06 | 0.04 | 0.03–0.05 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 0.02 | 0.01–0.02 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Glioblastoma | 0.46 | 0.44–0.49 | 1.24 | 1.19–1.29 | 3.57 | 3.49–3.65 | 8.07 | 7.94–8.19 | 12.98 | 12.78–13.17 | 15.29 | 14.99–15.58 | 9.06 | 8.73–9.41 |
| Oligodendroglioma | 0.28 | 0.26–0.30 | 0.42 | 0.39–0.44 | 0.37 | 0.34–0.40 | 0.28 | 0.25–0.30 | 0.19 | 0.17–0.22 | 0.13 | 0.11–0.16 | 0.08 | 0.05–0.12 |
| Anaplastic Oligodendroglioma | 0.09 | 0.08–0.10 | 0.18 | 0.16–0.20 | 0.21 | 0.19–0.23 | 0.19 | 0.17–0.21 | 0.16 | 0.14–0.19 | 0.12 | 0.09–0.15 | -- | -- |
| Oligoastrocytic Tumors | 0.19 | 0.18–0.21 | 0.24 | 0.21–0.26 | 0.17 | 0.15–0.19 | 0.15 | 0.13–0.17 | 0.14 | 0.12–0.16 | 0.09 | 0.06–0.11 | -- | -- |
| Ependymal Tumors | 0.36 | 0.34–0.38 | 0.52 | 0.49–0.56 | 0.57 | 0.54–0.60 | 0.55 | 0.52–0.59 | 0.60 | 0.56–0.64 | 0.42 | 0.37–0.47 | 0.13 | 0.10–0.18 |
| Malignant | 0.19 | 0.17–0.20 | 0.28 | 0.26–0.30 | 0.29 | 0.27–0.31 | 0.30 | 0.27–0.32 | 0.32 | 0.29–0.35 | 0.25 | 0.22–0.29 | 0.06 | 0.04–0.10 |
| Non-Malignant | 0.17 | 0.16–0.19 | 0.25 | 0.22–0.27 | 0.28 | 0.26–0.31 | 0.25 | 0.23–0.28 | 0.28 | 0.25–0.31 | 0.16 | 0.14–0.20 | 0.07 | 0.04–0.11 |
| Glioma Malignant, NOS | 0.27 | 0.26–0.29 | 0.26 | 0.24–0.29 | 0.31 | 0.29–0.34 | 0.36 | 0.34–0.39 | 0.59 | 0.55–0.64 | 1.04 | 0.96–1.12 | 1.74 | 1.60–1.90 |
| Choroid Plexus Tumors | 0.04 | 0.03–0.04 | 0.04 | 0.03–0.05 | 0.03 | 0.02–0.04 | 0.03 | 0.02–0.04 | 0.04 | 0.03–0.05 | 0.03 | 0.02–0.05 | -- | -- |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neuroepithelial Tumors | 0.01 | 0.00–0.01 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Neuronal and Mixed Neuronal Glial Tumors | 0.31 | 0.29–0.33 | 0.26 | 0.24–0.28 | 0.24 | 0.22–0.26 | 0.22 | 0.20–0.24 | 0.23 | 0.20–0.25 | 0.18 | 0.15–0.21 | 0.08 | 0.06–0.12 |
| Malignant | 0.03 | 0.03–0.04 | 0.07 | 0.05–0.08 | 0.08 | 0.07–0.09 | 0.10 | 0.08–0.11 | 0.12 | 0.10–0.14 | 0.11 | 0.08–0.13 | -- | -- |
| Non-Malignant | 0.28 | 0.26–0.30 | 0.19 | 0.18–0.21 | 0.16 | 0.14–0.18 | 0.12 | 0.10–0.13 | 0.10 | 0.09–0.12 | 0.07 | 0.05–0.09 | -- | -- |
| Tumors of the Pineal Region | 0.05 | 0.05–0.06 | 0.06 | 0.05–0.07 | 0.05 | 0.04–0.06 | 0.04 | 0.03–0.05 | 0.05 | 0.04–0.06 | 0.03 | 0.02–0.05 | -- | -- |
| Malignant | 0.03 | 0.02–0.03 | 0.02 | 0.02–0.03 | 0.03 | 0.02–0.03 | 0.02 | 0.01–0.03 | 0.02 | 0.01–0.03 | -- | -- | -- | -- |
| Non-Malignant | 0.03 | 0.02–0.03 | 0.03 | 0.03–0.04 | 0.03 | 0.02–0.03 | 0.02 | 0.02–0.03 | 0.03 | 0.02–0.04 | -- | -- | -- | -- |
| Embryonal Tumors | 0.15 | 0.14–0.17 | 0.09 | 0.08–0.11 | 0.05 | 0.04–0.06 | 0.05 | 0.04–0.06 | 0.04 | 0.03–0.05 | 0.04 | 0.02–0.05 | -- | -- |
| Tumors of Cranial and Spinal Nerves | 0.94 | 0.90–0.97 | 2.11 | 2.05–2.17 | 3.27 | 3.20–3.35 | 4.50 | 4.40–4.59 | 5.23 | 5.11–5.36 | 4.01 | 3.86–4.16 | 1.75 | 1.60–1.90 |
| Nerve Sheath Tumors | 0.94 | 0.90–0.97 | 2.11 | 2.04–2.17 | 3.27 | 3.19–3.35 | 4.49 | 4.40–4.59 | 5.23 | 5.10–5.35 | 4.00 | 3.85–4.16 | 1.75 | 1.60–1.90 |
| Malignant | 0.01 | 0.01-0.01 | 0.02 | 0.01–0.02 | 0.02 | 0.01–0.03 | 0.02 | 0.01–0.03 | 0.03 | 0.02–0.05 | 0.03 | 0.02–0.05 | -- | -- |
| Non-Malignant | 0.93 | 0.89–0.96 | 2.09 | 2.03–2.15 | 3.25 | 3.17–3.33 | 4.47 | 4.38–4.57 | 5.19 | 5.07–5.32 | 3.97 | 3.83–4.13 | -- | -- |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Meninges | 1.69 | 1.64–1.73 | 5.71 | 5.61–5.82 | 10.60 | 10.47–10.74 | 16.52 | 16.34–16.70 | 28.62 | 28.32–28.91 | 42.23 | 41.74–42.72 | 53.52 | 52.70–54.34 |
| Meningioma | 1.44 | 1.40–1.48 | 5.39 | 5.29–5.50 | 10.22 | 10.09–10.36 | 16.09 | 15.92–16.27 | 28.16 | 27.87–28.46 | 41.80 | 41.31–42.28 | 53.37 | 52.56–54.20 |
| Malignant | 0.02 | 0.01–0.02 | 0.05 | 0.04–0.06 | 0.11 | 0.09–0.12 | 0.20 | 0.18–0.22 | 0.35 | 0.32–0.38 | 0.45 | 0.40–0.50 | 0.57 | 0.49–0.66 |
| Non-Malignant | 1.42 | 1.38–1.46 | 5.34 | 5.24–5.45 | 10.12 | 9.98–10.25 | 15.89 | 15.72–16.07 | 27.81 | 27.52–28.10 | 41.35 | 40.87–41.83 | 52.81 | 52.00–53.62 |
| Mesenchymal Tumors | -- | -- | -- | -- | 0.12 | 0.11–0.14 | 0.12 | 0.11–0.14 | -- | -- | -- | -- | -- | -- |
| Primary Melanocytic Lesions | -- | -- | -- | -- | 0.01 | 0.00–0.01 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | -- | -- |
| Other Neoplasms Related to the Meninges | 0.18 | 0.17–0.20 | 0.23 | 0.21–0.26 | 0.25 | 0.23–0.27 | 0.29 | 0.27–0.31 | 0.30 | 0.27–0.33 | 0.27 | 0.23–0.31 | 0.08 | 0.05–0.12 |
| Lymphomas and Hematopoietic Neoplasms | 0.10 | 0.09–0.11 | 0.23 | 0.21–0.25 | 0.40 | 0.38–0.43 | 0.87 | 0.83–0.91 | 1.81 | 1.73–1.88 | 2.41 | 2.30–2.53 | 1.18 | 1.06–1.31 |
| Lymphoma | 0.09 | 0.08–0.10 | 0.21 | 0.19–0.23 | 0.39 | 0.36–0.42 | 0.85 | 0.81–0.89 | 1.78 | 1.71–1.85 | 2.39 | 2.28–2.51 | 1.16 | 1.05–1.29 |
| Other hematopoietic Neoplasms | 0.01 | 0.01-0.01 | 0.01 | 0.01–0.02 | 0.01 | 0.01–0.02 | 0.01 | 0.01–0.02 | 0.03 | 0.02–0.04 | -- | -- | -- | -- |
| Germ Cell Tumors and Cysts | 0.11 | 0.10–0.12 | 0.04 | 0.03–0.05 | 0.03 | 0.02–0.04 | 0.02 | 0.02–0.03 | 0.02 | 0.02–0.03 | -- | -- | -- | -- |
| Germ cell tumors, cysts, and heterotopias | 0.11 | 0.10–0.12 | 0.04 | 0.03–0.05 | 0.03 | 0.02–0.04 | 0.02 | 0.02–0.03 | 0.02 | 0.02–0.03 | -- | -- | -- | -- |
| Malignant | 0.08 | 0.07–0.09 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 0.03 | 0.02–0.03 | 0.03 | 0.02–0.04 | 0.03 | 0.02–0.03 | 0.02 | 0.01–0.03 | 0.02 | 0.02–0.03 | -- | -- | -- | -- |
| Tumors of Sellar Region | 3.96 | 3.89–4.03 | 5.45 | 5.35–5.55 | 5.56 | 5.46–5.66 | 6.39 | 6.28–6.51 | 8.22 | 8.06–8.38 | 8.41 | 8.19–8.63 | 5.03 | 4.78–5.29 |
| Tumors of the Pituitary | 3.84 | 3.77–3.91 | 5.28 | 5.18–5.38 | 5.34 | 5.24–5.44 | 6.15 | 6.04–6.26 | 7.95 | 7.80–8.11 | 8.18 | 7.97–8.40 | 4.95 | 4.70–5.21 |
| Malignant | -- | -- | 0.01 | 0.01–0.02 | 0.01 | 0.01–0.02 | 0.02 | 0.01–0.03 | 0.02 | 0.01–0.03 | -- | -- | -- | -- |
| Non-Malignant | -- | -- | 5.27 | 5.17–5.37 | 5.33 | 5.23–5.43 | 6.13 | 6.02–6.24 | 7.93 | 7.78–8.09 | -- | -- | -- | -- |
| Craniopharyngioma | 0.12 | 0.11–0.13 | 0.17 | 0.15–0.18 | 0.22 | 0.20–0.24 | 0.24 | 0.22–0.26 | 0.27 | 0.24–0.30 | 0.22 | 0.19–0.26 | 0.08 | 0.05–0.12 |
| Unclassified Tumors | 0.59 | 0.57–0.62 | 0.86 | 0.82–0.90 | 1.10 | 1.05–1.14 | 1.51 | 1.45–1.56 | 2.48 | 2.39–2.57 | 4.88 | 4.72–5.05 | 10.79 | 10.42–11.16 |
| Hemangioma | 0.30 | 0.28–0.32 | 0.42 | 0.39–0.45 | 0.47 | 0.45–0.50 | 0.53 | 0.50–0.56 | 0.65 | 0.60–0.69 | 0.65 | 0.59–0.72 | 0.54 | 0.46–0.63 |
| Neoplasm Unspecified | 0.30 | 0.28–0.31 | 0.43 | 0.40–0.46 | 0.62 | 0.59–0.65 | 0.97 | 0.93–1.02 | 1.80 | 1.73–1.88 | 4.19 | 4.04–4.35 | 10.18 | 9.83–10.55 |
| Malignant | 0.07 | 0.06–0.07 | 0.11 | 0.10–0.13 | 0.21 | 0.19–0.23 | 0.43 | 0.41–0.46 | 0.88 | 0.83–0.94 | 2.37 | 2.26–2.49 | 5.99 | 5.72–6.27 |
| Non-Malignant | 0.23 | 0.21–0.25 | 0.32 | 0.30–0.35 | 0.41 | 0.38–0.44 | 0.54 | 0.51–0.57 | 0.92 | 0.86–0.97 | 1.82 | 1.72–1.93 | 4.19 | 3.97–4.43 |
| All Other | -- | -- | -- | -- | -- | -- | -- | -- | 0.03 | 0.02–0.04 | 0.04 | 0.02–0.05 | 0.07 | 0.04–0.10 |
| TOTAL b | 10.72 | 10.61–10.84 | 18.83 | 18.65–19.02 | 27.63 | 27.41–27.86 | 41.13 | 40.85–41.41 | 63.25 | 62.82–63.69 | 81.29 | 80.62–81.97 | 84.48 | 83.46–85.52 |
| Malignant | 3.12 | 3.06–3.18 | 4.39 | 4.30–4.48 | 6.98 | 6.87–7.09 | 12.51 | 12.36–12.67 | 19.61 | 19.36–19.85 | 24.43 | 24.06–24.80 | 19.89 | 19.39–20.39 |
| Non-Malignant | 7.61 | 7.51–7.70 | 14.44 | 14.28–14.61 | 20.65 | 20.46–20.85 | 28.62 | 28.38–28.85 | 43.65 | 43.29–44.01 | 56.87 | 56.30–57.43 | 64.59 | 63.70–65.50 |
a. Rates are per 100,000 and age-adjusted to the 2000 US standard population.
b. Refers to all brain tumors including histologies not presented in this table.
-- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
Fig. 12.
Age-Adjusted Incidence Ratesa of Brain and Other CNS Tumors by Selected Histologies and Age Group A) Age 20+ Yearsb and B) Age 0–19 Yearsb, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
The incidence rate for all brain and other CNS tumors was highest among age 85+ years (84.48 per 100,000 population) and
The incidence rate for all brain and other CNS tumors was lowest among children and adolescents age 0–19 years (6.06 per 100,000 population), while incidence among those 20+ was 30.40 per 100,000 population.
Incidence rates of pilocytic astrocytoma, germ cell tumors, and embryonal tumors were higher in the younger age groups and decreased with advancing age.
Incidence rates of meningioma increased with age.
Incidence rates declined with increasing age for those ages 0–19 years, particularly for the gliomas and embryonal tumors (primitive neuroectodermal tumor (PNET), Atypical teratoid/rhabdoid tumor (ATRT), and medulloblastoma).
Incidence rates increased with age for tumors of the pituitary.
Median age at diagnosis
The median age at diagnosis for all primary brain and other CNS tumors was 60 years (Table 3), and was 60 years for both males and females (data not shown).
The histology-specific median ages ranged from 8 years for embryonal tumors to 69 years for neoplasm, unspecified.
Pilocytic astrocytoma, choroid plexus tumors, neuronal and mixed neuronal-glial tumors, tumors of the pineal region, embryonal tumors, and germ cell tumors and cysts were histologies with younger median ages at diagnosis compared to other histologies.
Meningioma and glioblastoma were primarily diagnosed at older ages (median age of 66 and 65 years, respectively).
Distributions and Incidence by Sex
Distribution by sex and behavior
Overall, 41.9% of all tumors diagnosed between 2012 and 2016 occurred in males (169,868 tumors) and 58.1% in females (235,872 tumors) (Table 3).
Approximately 55.4% of the malignant tumors occurred in males (67,930 tumors between 2011 and 2016) and 44.6% in females (54,639 tumors between 2012 and 2016).
Approximately 36.0% of the non-malignant tumors occurred in males (101,938 tumors between 2012 and 2016) and 64.0% in females (181,233 tumors between 2012 and 2016).
Incidence rates by site and sex
Incidence counts and AAAIR for all brain and other CNS tumors by site and sex are provided in Table 8.
Table 8.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals of brain and other central nervous system tumors by site and sex, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Site (ICD-O-3 Code)c | Total | Male | Female | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-Year Total | Annual Average | % of All Tumors | Rate | 95% CI | 5-Year Total | Annual Average | % Malignant | % Non- Malignant | Rate | 95% CI | 5-Year Total | Annual Average | % Malignant | % Non- Malignant | Rate | 95% CI | |
| Frontal, temporal, parietal, and occipital lobes of the brain (C71.1-C71.4) | 74,346 | 14,869 | 18.3% | 4.24 | 4.21–4.27 | 41,349 | 8,270 | 91.4% | 8.6% | 4.99 | 4.94–5.04 | 32,997 | 6,599 | 88.2% | 11.8% | 3.58 | 3.54–3.62 |
| Frontal lobe (C71.1) | 32,419 | 6,484 | 8.0% | 1.87 | 1.85–1.89 | 17,232 | 3,446 | 92.1% | 7.9% | 2.10 | 2.06–2.13 | 15,187 | 3,037 | 89.4% | 10.6% | 1.67 | 1.64–1.70 |
| Temporal lobe (C71.2) | 24,129 | 4,826 | 5.9% | 1.37 | 1.35–1.38 | 14,353 | 2,871 | 90.6% | 9.4% | 1.72 | 1.69–1.75 | 9,776 | 1,955 | 86.9% | 13.1% | 1.06 | 1.04–1.08 |
| Parietal lobe (C71.3) | 13,987 | 2,797 | 3.4% | 0.78 | 0.77–0.80 | 7,653 | 1,531 | 93.0% | 7.0% | 0.92 | 0.90–0.94 | 6,334 | 1,267 | 89.2% | 10.8% | 0.67 | 0.65–0.69 |
| Occipital lobe (C71.4) | 3,811 | 762 | 0.9% | 0.22 | 0.21–0.22 | 2,111 | 422 | 86.0% | 14.0% | 0.26 | 0.24–0.27 | 1,700 | 340 | 82.5% | 17.5% | 0.18 | 0.17–0.19 |
| Cerebrum (C71.0) | 6,985 | 1,397 | 1.7% | 0.41 | 0.40–0.42 | 3,783 | 757 | 82.9% | 17.1% | 0.46 | 0.45–0.48 | 3,202 | 640 | 79.8% | 20.2% | 0.36 | 0.35–0.38 |
| Ventricle (C71.5) | 4,071 | 814 | 1.0% | 0.25 | 0.25–0.26 | 2,167 | 433 | 42.4% | 57.6% | 0.27 | 0.26–0.29 | 1,904 | 381 | 40.3% | 59.7% | 0.24 | 0.23–0.25 |
| Cerebellum (C71.6) | 8,838 | 1,768 | 2.2% | 0.56 | 0.55–0.57 | 4,685 | 937 | 62.9% | 37.1% | 0.60 | 0.59–0.62 | 4,153 | 831 | 55.3% | 44.7% | 0.52 | 0.50–0.53 |
| Brain stem (C71.7) | 6,171 | 1,234 | 1.5% | 0.40 | 0.39–0.41 | 3,363 | 673 | 76.1% | 23.9% | 0.43 | 0.42–0.45 | 2,808 | 562 | 77.2% | 22.8% | 0.36 | 0.35–0.38 |
| Other brain (C71.8-C71.9) | 33,741 | 6,748 | 8.3% | 1.93 | 1.91–1.95 | 17,694 | 3,539 | 83.3% | 16.7% | 2.18 | 2.15–2.21 | 16,047 | 3,209 | 78.5% | 21.5% | 1.72 | 1.69–1.74 |
| Spinal cord and cauda equina (C72.0-C72.1) | 12,775 | 2,555 | 3.1% | 0.77 | 0.75–0.78 | 6,687 | 1,337 | 28.3% | 71.7% | 0.83 | 0.81–0.85 | 6,088 | 1,218 | 26.7% | 73.3% | 0.71 | 0.69–0.73 |
| Cranial nerves (C72.2-C72.5) | 28,534 | 5,707 | 7.0% | 1.64 | 1.62–1.66 | 13,398 | 2,680 | 6.0% | 94.0% | 1.60 | 1.57–1.63 | 15,136 | 3,027 | 5.4% | 94.6% | 1.68 | 1.65–1.70 |
| Other nervous system (C72.8-C72.9) | 2,510 | 502 | 0.6% | 0.15 | 0.14–0.15 | 1,269 | 254 | 55.8% | 44.2% | 0.16 | 0.15–0.17 | 1,241 | 248 | 54.2% | 45.8% | 0.14 | 0.13–0.15 |
| Meninges (cerebral and spinal) (C70.0-C70.9) | 153,078 | 30,616 | 37.7% | 8.58 | 8.53–8.62 | 41,300 | 8,260 | 2.3% | 97.7% | 5.11 | 5.06–5.16 | 111,778 | 22,356 | 1.1% | 98.9% | 11.64 | 11.57–11.71 |
| Pituitary and craniopharyngeal duct (C75.1-C75.2) | 72,162 | 14,432 | 17.8% | 4.34 | 4.31–4.37 | 32,701 | 6,540 | 0.8% | 99.2% | 3.99 | 3.95–4.04 | 39,461 | 7,892 | 0.5% | 99.5% | 4.77 | 4.72–4.82 |
| Pineal (C75.3) | 1,762 | 352 | 0.4% | 0.11 | 0.11–0.12 | 1,018 | 204 | 74.2% | 25.8% | 0.13 | 0.12–0.14 | 744 | 149 | 42.3% | 57.7% | 0.09 | 0.09–0.10 |
| Olfactory tumors of the nasal cavity (C30.0 d) | 767 | 153 | 0.2% | 0.04 | 0.04–0.05 | 454 | 91 | 100.0% | 0.0% | 0.05 | 0.05–0.06 | 313 | 63 | 100.0% | 0.0% | 0.04 | 0.03–0.04 |
| TOTAL | 405,740 | 81,148 | 100.0% | 23.41 | 23.34–23.49 | 169,868 | 33,974 | 40.0% | 60.0% | 20.82 | 20.72–20.92 | 235,872 | 47,174 | 23.2% | 76.8% | 25.84 | 25.73–25.95 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. The sites referred to in this table are loosely based on the categories and site code defined in the SEER site/histology validation list.
d. ICD-O-3 histology codes 9522–9523 only.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
AAAIR were highest for tumors located in the meninges (8.58 per 100,000 population) and lowest for olfactory tumors of the nasal cavity (0.04 per 100,000 population).
AAAIR were higher in females than in males for tumors located in the meninges (11.64 per 100,000 in females vs 5.11 per 100,000 in males), pituitary and craniopharyngeal duct (4.77 per 100,000 in females vs 3.99 per 100,000 in males), and cranial nerves (1.68 per 100,000 in females vs 1.60 per 100,000 in males) while males had higher AAAIR for tumors located in most other locations.
Incidence rates by sex and histology
AAAIR by sex and histology are presented in Table 3. AAAIR for all primary brain and other CNS tumors combined were higher among females (25.84 per 100,000 population) than males (20.82 per 100,000 population).
The AAAIR of tumors of neuroepithelial tissue was higher in males (7.69 per 100,000 population) than in females 5.56 per 100,000 population).
The AAAIR of tumors of meninges was higher in females (11.89 per 100,000 population) than in males (5.37 per 100,000 population).
Incidence rate ratios (male:female) for selected histologies and histology groupings are shown in Figure 13.
Fig. 13.
Incidence Rate Ratios by Sex (Males:Females) for Selected Primary Brain and Other CNS Tumor Histologies, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Incidence was higher in males for many histologies, such as germ cell tumors (P < 0.001), most glial tumors, lymphomas (P < 0.001), and embryonal tumors (P < 0.001).
Incidence was higher in females for non-malignant (P < 0.001) and malignant (P = 0.0153) meningiomas and tumors of the pituitary (P < 0.001).
Distribution and Incidence Rates by CCR, Age, Diagnostic Confirmation, and Behavior
The overall number of reported tumors is listed by CCR in Table 9. While most malignant tumors are diagnosed by histologic confirmation (where the patient receives surgery and diagnosis is confirmed by a pathologist), brain and other CNS tumors may also be diagnosed by radiographic confirmation only (where the tumor was visualized on MRI, CT, X-ray, or other imaging technology but surgery, including biopsy, was not performed and tissue therefore could not be collected).
Table 9.
Characteristics of all brain and other central nervous system tumors by central cancer registry and behavior, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| State | Total | Malignant | Non-Malignant | Average Annual Populationa | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-Year Total | Annual Average | Histologically Confirmed (%) | Radiographically Confirmed (%) | 5-Year Total | % Malignant | Histologically Confirmed (%) | Radiographically Confirmed (%) | 5-Year Total | % Non-Malignant | Histologically Confirmed (%) | Radiographically Confirmed (%) | ||
| Alabama | 4,817 | 963 | 65.2% | 29.5% | 1868 | 38.8% | 81.7% | 6.91% | 2949 | 61.2% | 54.7% | 43.8% | 4,838,609 |
| Alaska | 855 | 171 | 48.8% | 47.7% | 246 | 28.8% | 82.5% | 11.38% | 609 | 71.2% | 35.1% | 62.4% | 736,769 |
| Arizona | 7,570 | 1,514 | 62.7% | 31.9% | 2,477 | 32.7% | 82.8% | 7.95% | 5,093 | 67.3% | 52.9% | 43.5% | 6,715,535 |
| Arkansas | 3,451 | 690 | 54.8% | 40.0% | 1,213 | 35.1% | 79.6% | 11.29% | 2,238 | 64.8% | 41.4% | 55.6% | 2,966,929 |
| California | 43,842 | 8,768 | 59.9% | 35.7% | 13,179 | 30.1% | 85.9% | 8.60% | 30,663 | 69.9% | 48.7% | 47.4% | 38,679,317 |
| Colorado | 7,454 | 1,491 | 49.1% | 47.8% | 1,919 | 25.7% | 81.0% | 12.92% | 5,535 | 74.3% | 38.1% | 59.9% | 5,352,349 |
| Connecticut | 4,461 | 892 | 67.7% | 30.1% | 1,526 | 34.2% | 88.4% | 9.04% | 2,935 | 65.8% | 57.0% | 41.1% | 3,596,382 |
| Delaware | 1,050 | 210 | 67.9% | 28.9% | 372 | 35.4% | 82.3% | 12.37% | 678 | 64.6% | 60.0% | 37.9% | 934,718 |
| District of Columbia | 716 | 143 | 63.1% | 34.6% | 196 | 27.4% | 90.3% | 4.59% | 520 | 72.6% | 52.9% | 46.0% | 660,723 |
| Florida | 29,531 | 5,906 | 53.1% | 43.4% | 8,333 | 28.2% | 84.7% | 10.40% | 21,198 | 71.8% | 40.7% | 56.4% | 19,949,831 |
| Georgia | 13,037 | 2,607 | 50.7% | 45.2% | 3,427 | 26.3% | 84.1% | 11.50% | 9,610 | 73.7% | 38.7% | 57.2% | 10,097,989 |
| Hawaii | 1,517 | 303 | 53.0% | 39.1% | 384 | 25.3% | 85.2% | 8.33% | 1,133 | 74.7% | 42.1% | 49.5% | 1,414,705 |
| Idaho | 1,943 | 389 | 63.7% | 33.1% | 694 | 35.7% | 84.4% | 11.53% | 1,249 | 64.3% | 52.1% | 45.2% | 1,632,920 |
| Illinois | 16,780 | 3,356 | 57.0% | 40.9% | 4,786 | 28.5% | 87.5% | 8.67% | 11,994 | 71.5% | 44.8% | 53.7% | 12,869,822 |
| Indiana | 7,902 | 1,580 | 53.2% | 43.5% | 2,557 | 32.4% | 84.0% | 11.73% | 5,345 | 67.6% | 38.4% | 58.7% | 6,588,187 |
| Iowa | 4,408 | 882 | 56.8% | 40.7% | 1,354 | 30.7% | 84.5% | 11.08% | 3,054 | 69.3% | 44.5% | 53.8% | 3,103,833 |
| Kansas | 3,686 | 737 | 53.4% | 43.1% | 1,149 | 31.2% | 84.9% | 10.36% | 2,537 | 68.8% | 39.2% | 57.9% | 2,898,258 |
| Kentucky | 6,875 | 1,375 | 48.5% | 46.6% | 1,953 | 28.4% | 78.9% | 12.65% | 4,922 | 71.6% | 36.4% | 60.1% | 4,410,276 |
| Louisiana | 5,953 | 1,191 | 57.5% | 37.4% | 1,642 | 27.6% | 85.1% | 10.17% | 4,311 | 72.4% | 47.0% | 47.8% | 4,647,128 |
| Maine | 1,565 | 313 | 65.1% | 31.6% | 670 | 42.8% | 84.0% | 10.75% | 895 | 57.2% | 50.9% | 47.3% | 1,328,600 |
| Maryland | 6,862 | 1,372 | 64.8% | 31.0% | 2,161 | 31.5% | 86.8% | 6.71% | 4,701 | 68.5% | 54.7% | 42.1% | 5,963,978 |
| Massachusetts | 6,712 | 1,342 | 70.8% | 25.7% | 2,595 | 38.7% | 87.6% | 7.59% | 4,117 | 61.3% | 60.2% | 37.1% | 6,749,283 |
| Michigan | 11,686 | 2,337 | 59.6% | 35.9% | 3,921 | 33.5% | 84.0% | 8.67% | 7,765 | 66.5% | 47.3% | 49.6% | 9,910,424 |
| Minnesota | 6,273 | 1,255 | 72.8% | 23.5% | 2,312 | 36.9% | 88.3% | 7.70% | 3,961 | 63.1% | 63.7% | 32.7% | 5,450,941 |
| Mississippi | 3,445 | 689 | 58.8% | 37.7% | 1,066 | 30.9% | 85.4% | 11.16% | 2,379 | 69.1% | 47.0% | 49.6% | 2,985,995 |
| Missouri | 8,021 | 1,604 | 54.6% | 41.5% | 2,463 | 30.7% | 86.3% | 8.08% | 5,558 | 69.3% | 40.5% | 56.3% | 6,057,248 |
| Montana | 1,402 | 280 | 54.3% | 41.8% | 479 | 34.2% | 82.3% | 12.73% | 923 | 65.8% | 39.8% | 56.9% | 1,020,469 |
| Nebraska | 2,055 | 411 | 59.4% | 37.2% | 749 | 36.5% | 84.6% | 8.81% | 1,306 | 63.5% | 44.9% | 53.4% | 1,880,873 |
| Nevada | 2,776 | 555 | 58.3% | 36.0% | 1,010 | 36.4% | 82.9% | 6.73% | 1,766 | 63.6% | 44.3% | 52.7% | 2,838,600 |
| New Hampshire | 1,671 | 334 | 64.6% | 32.9% | 598 | 35.8% | 89.6% | 6.19% | 1,073 | 64.2% | 50.7% | 47.7% | 1,327,476 |
| New Jersey | 12,551 | 2,510 | 56.5% | 38.7% | 3,724 | 29.7% | 87.1% | 9.10% | 8,827 | 70.3% | 43.6% | 51.2% | 8,935,451 |
| New Mexico | 2,127 | 425 | 65.0% | 28.7% | 681 | 32.0% | 86.8% | 7.05% | 1,446 | 68.0% | 54.8% | 38.9% | 2,083,931 |
| New York | 29,691 | 5,938 | 52.4% | 44.4% | 7,854 | 26.4% | 84.1% | 11.33% | 21,837 | 73.5% | 41.0% | 56.3% | 19,753,427 |
| North Carolina | 12,947 | 2,589 | 56.0% | 40.4% | 3,771 | 29.1% | 84.3% | 10.26% | 9,176 | 70.9% | 44.4% | 52.8% | 9,948,946 |
| North Dakota | 796 | 159 | 53.6% | 43.7% | 273 | 34.3% | 85.0% | 10.99% | 523 | 65.7% | 37.3% | 60.8% | 734,671 |
| Ohio | 13,537 | 2,707 | 64.9% | 30.8% | 4,873 | 36.0% | 85.3% | 7.74% | 8,664 | 64.0% | 53.5% | 43.7% | 11,587,427 |
| Oklahoma | 4,595 | 919 | 53.7% | 42.8% | 1,490 | 32.4% | 81.6% | 11.07% | 3,105 | 67.6% | 40.3% | 58.1% | 3,873,141 |
| Oregon | 4,592 | 918 | 66.7% | 28.7% | 1,744 | 38.0% | 83.1% | 7.34% | 2,848 | 62.0% | 56.7% | 41.8% | 3,975,357 |
| Pennsylvania | 19,515 | 3,903 | 51.3% | 44.5% | 5,785 | 29.6% | 82.0% | 10.49% | 13,730 | 70.4% | 38.4% | 58.9% | 12,783,007 |
| Rhode Island | 1,144 | 229 | 67.7% | 29.9% | 425 | 37.1% | 89.6% | 7.53% | 719 | 62.9% | 54.8% | 43.1% | 1,054,762 |
| South Carolina | 6,320 | 1,264 | 51.9% | 42.5% | 1,861 | 29.4% | 83.2% | 9.94% | 4,459 | 70.5% | 38.9% | 56.0% | 4,832,375 |
| South Dakota | 1,013 | 203 | 49.7% | 47.3% | 342 | 33.8% | 80.4% | 15.50% | 671 | 66.2% | 34.0% | 63.5% | 848,024 |
| Tennessee | 8,866 | 1,773 | 53.0% | 44.5% | 2,479 | 28.0% | 86.5% | 9.72% | 6,387 | 72.0% | 40.0% | 58.0% | 6,544,313 |
| Texas | 32,412 | 6,482 | 50.7% | 42.9% | 9,267 | 28.6% | 80.3% | 13.11% | 23,145 | 71.4% | 38.9% | 54.8% | 26,974,357 |
| Utah | 4,614 | 923 | 49.4% | 49.4% | 964 | 20.9% | 85.3% | 12.86% | 3,650 | 79.1% | 40.0% | 59.0% | 2,944,418 |
| Vermont | 877 | 175 | 56.8% | 40.6% | 249 | 28.4% | 90.4% | 5.22% | 628 | 71.6% | 43.5% | 54.6% | 625,025 |
| Virginia | 8,537 | 1,707 | 64.5% | 31.0% | 2,963 | 34.7% | 84.8% | 6.41% | 5,574 | 65.3% | 53.8% | 44.0% | 8,309,679 |
| Washington | 11,704 | 2,341 | 47.4% | 48.7% | 3,014 | 25.8% | 82.1% | 11.51% | 8,690 | 74.2% | 35.3% | 61.5% | 7,066,998 |
| West Virginia | 2,387 | 477 | 57.6% | 39.5% | 824 | 34.5% | 88.2% | 8.98% | 1,563 | 65.5% | 41.5% | 55.7% | 1,844,744 |
| Wisconsin | 8,525 | 1,705 | 51.2% | 45.4% | 2,457 | 28.8% | 84.0% | 11.52% | 6,068 | 71.2% | 37.9% | 59.1% | 5,748,336 |
| Wyoming | 674 | 135 | 65.1% | 33.7% | 230 | 34.1% | 87.8% | 10.43% | 444 | 65.9% | 53.4% | 45.7% | 582,659 |
| TOTAL | 405,740 | 81,148 | 56.3% | 39.7% | 122,569 | 30.2% | 84.4% | 9.85% | 283,171 | 69.8% | 44.1% | 52.6% | 318,659,215 |
a. Population estimates were obtained from the United States Bureau of the Census available on the SEER program website.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program
Approximately 69.8% of tumors were non-malignant, but there was variation by cancer registry (range: 57.2%-79.1%).
Overall, 56.3% of tumors were histologically confirmed. A larger proportion of malignant tumors were histologically confirmed (84.4%) compared to non-malignant tumors (44.1%).
A slight majority of non-malignant brain and other CNS tumors were radiographically confirmed (52.6%).
The overall AAAIR by age, behavior, and CCR are presented in Table 10 and Figure 14.
Table 10.
Average annual age-adjusted incidence ratesa with 95% confidence intervals for all brain and other central nervous system tumors by age, behavior, and central cancer registry, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| State | 0–19 Years | 20+ Years | All Ages | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Malignant | Non-Malignant | All Tumors | Malignant | Non-Malignant | All Tumors | Malignant | Non-Malignant | All Tumors | ||||||||||
| Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | Rate | 95% CI | |
| Alabama | 3.77 | 3.30–4.29 | 1.33 | 1.06–1.65 | 5.11 | 4.56–5.70 | 8.24 | 7.84–8.66 | 14.73 | 14.18–15.30 | 22.98 | 22.29–23.68 | 6.96 | 6.64–7.29 | 10.89 | 10.49–11.30 | 17.85 | 17.34–18.38 |
| Alaska | 2.61 | 1.72–3.79 | 3.93 | 2.79–5.37 | 6.54 | 5.05–8.32 | 8.68 | 7.49–10.00 | 23.03 | 21.05–25.14 | 31.71 | 29.38–34.17 | 6.94 | 6.05–7.92 | 17.55 | 16.09–19.10 | 24.49 | 22.77–26.30 |
| Arizona | 3.03 | 2.68–3.41 | 2.43 | 2.12–2.77 | 5.46 | 4.99–5.96 | 8.11 | 7.77–8.46 | 18.44 | 17.92–18.98 | 26.55 | 25.92–27.19 | 6.65 | 6.39–6.93 | 13.85 | 13.46–14.24 | 20.50 | 20.03–20.98 |
| Arkansas | 3.46 | 2.90–4.09 | 2.39 | 1.94–2.93 | 5.85 | 5.12–6.66 | 8.88 | 8.34–9.44 | 18.09 | 17.31–18.89 | 26.97 | 26.02–27.94 | 7.32 | 6.91–7.76 | 13.59 | 13.02–14.18 | 20.91 | 20.20–21.64 |
| California | 3.07 | 2.92–3.23 | 2.24 | 2.12–2.38 | 5.32 | 5.12–5.52 | 8.01 | 7.86–8.16 | 20.59 | 20.35–20.83 | 28.60 | 28.32–28.88 | 6.59 | 6.48–6.71 | 15.33 | 15.15–15.50 | 21.92 | 21.71–22.13 |
| Colorado | 3.27 | 2.86–3.72 | 2.14 | 1.81–2.52 | 5.41 | 4.88–5.99 | 8.38 | 7.98–8.80 | 27.30 | 26.56–28.06 | 35.69 | 34.84–36.55 | 6.92 | 6.60–7.24 | 20.09 | 19.55–20.64 | 27.00 | 26.38–27.64 |
| Connecticut | 3.57 | 3.02–4.18 | 2.67 | 2.22–3.20 | 6.24 | 5.53–7.02 | 9.10 | 8.61–9.61 | 19.19 | 18.47–19.94 | 28.30 | 27.42–29.20 | 7.52 | 7.13–7.91 | 14.45 | 13.92–15.01 | 21.97 | 21.31–22.65 |
| Delaware | 3.84 | 2.79–5.15 | 2.92 | 2.03–4.09 | 6.76 | 5.35–8.44 | 8.21 | 7.32–9.18 | 16.88 | 15.56–18.29 | 25.09 | 23.49–26.78 | 6.95 | 6.25–7.72 | 12.88 | 11.90–13.92 | 19.83 | 18.61–21.11 |
| District of Columbia | 4.25 | 2.85–6.10 | 2.41 | 1.36–3.94 | 6.67 | 4.85–8.93 | 6.95 | 5.91–8.12 | 21.59 | 19.69–23.61 | 28.53 | 26.36–30.84 | 6.18 | 5.32–7.13 | 16.09 | 14.69–17.57 | 22.26 | 20.61–24.01 |
| Florida | 3.54 | 3.30–3.80 | 3.06 | 2.84–3.29 | 6.60 | 6.27–6.95 | 8.37 | 8.17–8.56 | 23.12 | 22.79–23.45 | 31.49 | 31.11–31.87 | 6.98 | 6.83–7.14 | 17.37 | 17.12–17.61 | 24.35 | 24.06–24.64 |
| Georgia | 3.49 | 3.18–3.81 | 2.68 | 2.41–2.96 | 6.16 | 5.76–6.59 | 7.97 | 7.68–8.27 | 25.30 | 24.78–25.84 | 33.28 | 32.68–33.88 | 6.68 | 6.46–6.92 | 18.81 | 18.43–19.20 | 25.50 | 25.05–25.95 |
| Hawaii | 1.72 | 1.15–2.46 | 1.89 | 1.28–2.68 | 3.61 | 2.75–4.64 | 5.94 | 5.32–6.62 | 18.78 | 17.65–19.97 | 24.73 | 23.43–26.08 | 4.73 | 4.25–5.25 | 13.94 | 13.11–14.81 | 18.67 | 17.71–19.67 |
| Idaho | 3.69 | 2.96–4.55 | 1.96 | 1.43–2.61 | 5.65 | 4.73–6.69 | 9.73 | 8.95–10.56 | 19.61 | 18.49–20.78 | 29.34 | 27.97–30.76 | 8.00 | 7.40–8.63 | 14.55 | 13.73–15.39 | 22.54 | 21.53–23.59 |
| Illinois | 3.35 | 3.08–3.64 | 2.54 | 2.31–2.79 | 5.89 | 5.53–6.27 | 8.34 | 8.09–8.60 | 23.28 | 22.85–23.72 | 31.62 | 31.12–32.13 | 6.91 | 6.71–7.11 | 17.33 | 17.02–17.65 | 24.24 | 23.87–24.62 |
| Indiana | 3.37 | 3.00–3.77 | 2.47 | 2.16–2.82 | 5.84 | 5.35–6.36 | 8.78 | 8.41–9.16 | 20.04 | 19.48–20.61 | 28.82 | 28.15–29.50 | 7.23 | 6.94–7.52 | 15.00 | 14.59–15.42 | 22.22 | 21.73–22.73 |
| Iowa | 3.59 | 3.04–4.22 | 3.66 | 3.10–4.29 | 7.25 | 6.45–8.12 | 9.39 | 8.85–9.96 | 23.26 | 22.40–24.16 | 32.66 | 31.63–33.71 | 7.73 | 7.31–8.17 | 17.64 | 17.00–18.30 | 25.37 | 24.60–26.15 |
| Kansas | 3.68 | 3.11–4.32 | 2.51 | 2.04–3.06 | 6.19 | 5.44–7.01 | 8.85 | 8.29–9.43 | 22.14 | 21.25–23.06 | 30.99 | 29.93–32.07 | 7.36 | 6.93–7.81 | 16.51 | 15.86–17.18 | 23.87 | 23.09–24.68 |
| Kentucky | 4.12 | 3.61–4.69 | 3.58 | 3.10–4.11 | 7.70 | 7.00–8.46 | 9.70 | 9.24–10.18 | 27.13 | 26.34–27.94 | 36.83 | 35.91–37.76 | 8.10 | 7.74–8.48 | 20.37 | 19.79–20.97 | 28.47 | 27.79–29.17 |
| Louisiana | 3.75 | 3.28–4.26 | 2.60 | 2.21–3.04 | 6.35 | 5.73–7.01 | 7.81 | 7.40–8.24 | 23.48 | 22.76–24.22 | 31.29 | 30.45–32.14 | 6.64 | 6.32–6.98 | 17.49 | 16.96–18.03 | 24.14 | 23.51–24.77 |
| Maine | 3.77 | 2.84–4.91 | 1.63 | 1.05–2.41 | 5.40 | 4.28–6.72 | 10.14 | 9.32–11.02 | 14.81 | 13.79–15.88 | 24.95 | 23.63–26.33 | 8.32 | 7.66–9.01 | 11.03 | 10.28–11.82 | 19.34 | 18.34–20.38 |
| Maryland | 3.26 | 2.86–3.69 | 1.62 | 1.35–1.94 | 4.88 | 4.39–5.41 | 8.17 | 7.80–8.55 | 19.55 | 18.97–20.13 | 27.72 | 27.03–28.42 | 6.76 | 6.47–7.06 | 14.40 | 13.99–14.83 | 21.17 | 20.66–21.69 |
| Massachusetts | 3.27 | 2.89–3.70 | 2.22 | 1.91–2.57 | 5.50 | 4.99–6.03 | 8.39 | 8.04–8.74 | 14.26 | 13.80–14.72 | 22.64 | 22.07–23.23 | 6.92 | 6.65–7.20 | 10.80 | 10.47–11.15 | 17.72 | 17.29–18.17 |
| Michigan | 3.50 | 3.18–3.85 | 1.88 | 1.65–2.13 | 5.38 | 4.98–5.81 | 8.51 | 8.22–8.80 | 18.73 | 18.29–19.17 | 27.23 | 26.71–27.77 | 7.07 | 6.84–7.30 | 13.90 | 13.58–14.22 | 20.97 | 20.58–21.36 |
| Minnesota | 3.95 | 3.50–4.43 | 2.42 | 2.07–2.81 | 6.36 | 5.79–6.98 | 9.44 | 9.02–9.87 | 17.62 | 17.05–18.21 | 27.07 | 26.36–27.79 | 7.86 | 7.54–8.20 | 13.26 | 12.84–13.69 | 21.13 | 20.59–21.67 |
| Mississippi | 2.72 | 2.24–3.28 | 2.42 | 1.97–2.95 | 5.15 | 4.47–5.89 | 8.18 | 7.66–8.73 | 19.96 | 19.13–20.81 | 28.14 | 27.15–29.15 | 6.61 | 6.22–7.03 | 14.93 | 14.32–15.55 | 21.54 | 20.81–22.29 |
| Missouri | 3.98 | 3.55–4.45 | 2.30 | 1.97–2.66 | 6.28 | 5.73–6.86 | 8.62 | 8.25–9.01 | 22.21 | 21.60–22.83 | 30.83 | 30.12–31.56 | 7.29 | 7.00–7.59 | 16.50 | 16.05–16.95 | 23.79 | 23.26–24.33 |
| Montana | 2.71 | 1.88–3.78 | 1.90 | 1.22–2.83 | 4.61 | 3.50–5.96 | 10.16 | 9.20–11.20 | 21.34 | 19.91–22.86 | 31.51 | 29.77–33.32 | 8.02 | 7.29–8.81 | 15.77 | 14.72–16.87 | 23.79 | 22.51–25.13 |
| Nebraska | 3.93 | 3.21–4.77 | 3.12 | 2.48–3.88 | 7.05 | 6.07–8.15 | 8.81 | 8.12–9.53 | 17.13 | 16.16–18.15 | 25.94 | 24.75–27.17 | 7.41 | 6.87–7.97 | 13.11 | 12.39–13.86 | 20.52 | 19.62–21.45 |
| Nevada | 3.03 | 2.49–3.65 | 1.45 | 1.08–1.90 | 4.48 | 3.82–5.22 | 7.96 | 7.43–8.51 | 15.60 | 14.85–16.38 | 23.56 | 22.64–24.50 | 6.54 | 6.14–6.97 | 11.54 | 11.00–12.11 | 18.08 | 17.40–18.79 |
| New Hampshire | 4.63 | 3.60–5.86 | 2.01 | 1.38–2.84 | 6.64 | 5.41–8.07 | 9.12 | 8.33–9.96 | 18.60 | 17.44–19.82 | 27.72 | 26.31–29.19 | 7.83 | 7.19–8.52 | 13.84 | 12.99–14.73 | 21.67 | 20.60–22.79 |
| New Jersey | 3.70 | 3.35–4.07 | 2.92 | 2.62–3.26 | 6.62 | 6.15–7.12 | 9.14 | 8.83–9.47 | 23.69 | 23.18–24.21 | 32.83 | 32.23–33.44 | 7.58 | 7.33–7.83 | 17.73 | 17.36–18.11 | 25.31 | 24.86–25.77 |
| New Mexico | 2.44 | 1.89–3.09 | 1.69 | 1.24–2.24 | 4.12 | 3.40–4.95 | 7.28 | 6.70–7.90 | 17.10 | 16.19–18.05 | 24.38 | 23.29–25.50 | 5.89 | 5.44–6.36 | 12.68 | 12.02–13.37 | 18.57 | 17.77–19.40 |
| New York | 4.03 | 3.78–4.29 | 3.88 | 3.64–4.14 | 7.91 | 7.56–8.27 | 8.58 | 8.37–8.79 | 26.50 | 26.14–26.87 | 35.08 | 34.66–35.51 | 7.27 | 7.11–7.44 | 20.01 | 19.74–20.29 | 27.29 | 26.97–27.61 |
| North Carolina | 3.53 | 3.22–3.88 | 2.31 | 2.05–2.59 | 5.84 | 5.43–6.28 | 8.31 | 8.03–8.61 | 22.70 | 22.22–23.18 | 31.01 | 30.45–31.58 | 6.94 | 6.72–7.17 | 16.85 | 16.50–17.20 | 23.79 | 23.37–24.21 |
| North Dakota | 2.78 | 1.83–4.05 | 2.82 | 1.86–4.11 | 5.60 | 4.20–7.31 | 8.55 | 7.48–9.73 | 18.38 | 16.74–20.14 | 26.93 | 24.96–29.01 | 6.89 | 6.08–7.79 | 13.92 | 12.71–15.21 | 20.81 | 19.34–22.36 |
| Ohio | 4.10 | 3.78–4.44 | 2.61 | 2.36–2.88 | 6.71 | 6.30–7.14 | 8.89 | 8.62–9.17 | 17.68 | 17.29–18.08 | 26.58 | 26.10–27.06 | 7.52 | 7.30–7.74 | 13.36 | 13.07–13.65 | 20.88 | 20.52–21.24 |
| Oklahoma | 3.27 | 2.80–3.80 | 2.16 | 1.78–2.59 | 5.43 | 4.82–6.09 | 8.61 | 8.14–9.10 | 20.08 | 19.35–20.83 | 28.69 | 27.82–29.58 | 7.08 | 6.72–7.45 | 14.94 | 14.41–15.49 | 22.02 | 21.37–22.68 |
| Oregon | 3.92 | 3.38–4.52 | 2.79 | 2.34–3.30 | 6.71 | 5.99–7.48 | 9.37 | 8.90–9.86 | 16.74 | 16.10–17.41 | 26.12 | 25.32–26.94 | 7.81 | 7.43–8.20 | 12.74 | 12.26–13.23 | 20.55 | 19.94–21.17 |
| Pennsylvania | 4.15 | 3.83–4.49 | 2.44 | 2.20–2.69 | 6.59 | 6.19–7.01 | 9.34 | 9.08–9.61 | 24.72 | 24.29–25.16 | 34.06 | 33.55–34.57 | 7.85 | 7.64–8.06 | 18.33 | 18.01–18.65 | 26.18 | 25.80–26.56 |
| Rhode Island | 2.23 | 1.47–3.25 | 1.69 | 1.05–2.57 | 3.92 | 2.89–5.19 | 8.90 | 8.02–9.85 | 15.79 | 14.60–17.05 | 24.69 | 23.20–26.25 | 6.99 | 6.32–7.71 | 11.74 | 10.87–12.67 | 18.73 | 17.62–19.89 |
| South Carolina | 3.14 | 2.71–3.62 | 2.27 | 1.91–2.68 | 5.41 | 4.84–6.02 | 8.29 | 7.89–8.71 | 22.03 | 21.36–22.72 | 30.32 | 29.54–31.12 | 6.81 | 6.50–7.14 | 16.36 | 15.87–16.86 | 23.17 | 22.59–23.77 |
| South Dakota | 3.38 | 2.42–4.61 | 1.36 | 0.78–2.21 | 4.74 | 3.58–6.16 | 8.91 | 7.90–10.02 | 19.93 | 18.38–21.58 | 28.84 | 26.98–30.80 | 7.33 | 6.55–8.17 | 14.60 | 13.48–15.79 | 21.93 | 20.56–23.37 |
| Tennessee | 3.56 | 3.17–3.99 | 2.72 | 2.38–3.10 | 6.28 | 5.76–6.85 | 8.20 | 7.86–8.56 | 23.75 | 23.15–24.37 | 31.96 | 31.26–32.67 | 6.87 | 6.60–7.16 | 17.72 | 17.28–18.17 | 24.59 | 24.07–25.12 |
| Texas | 3.59 | 3.41–3.78 | 2.54 | 2.39–2.71 | 6.13 | 5.89–6.38 | 8.31 | 8.12–8.50 | 23.91 | 23.59–24.23 | 32.22 | 31.85–32.59 | 6.96 | 6.81–7.10 | 17.78 | 17.55–18.01 | 24.73 | 24.46–25.01 |
| Utah | 2.73 | 2.29–3.23 | 3.25 | 2.76–3.81 | 5.98 | 5.31–6.71 | 9.03 | 8.41–9.68 | 38.65 | 37.35–39.97 | 47.68 | 46.24–49.15 | 7.22 | 6.76–7.70 | 28.49 | 27.56–29.45 | 35.71 | 34.67–36.78 |
| Vermont | -- | -- | 3.66 | 2.42–5.33 | 5.50 | 3.92–7.52 | 8.83 | 7.69–10.08 | 22.68 | 20.81–24.67 | 31.50 | 29.31–33.82 | 6.82 | 5.96–7.78 | 17.22 | 15.84–18.70 | 24.05 | 22.40–25.78 |
| Virginia | 3.09 | 2.77–3.45 | 1.76 | 1.51–2.03 | 4.85 | 4.44–5.29 | 8.06 | 7.75–8.38 | 16.61 | 16.16–17.07 | 24.67 | 24.12–25.22 | 6.63 | 6.39–6.88 | 12.35 | 12.02–12.68 | 18.98 | 18.57–19.40 |
| Washington | 4.11 | 3.70–4.55 | 3.49 | 3.11–3.90 | 7.60 | 7.03–8.19 | 9.49 | 9.12–9.87 | 30.63 | 29.97–31.31 | 40.12 | 39.36–40.90 | 7.94 | 7.66–8.24 | 22.85 | 22.36–23.34 | 30.79 | 30.22–31.37 |
| West Virginia | 3.91 | 3.11–4.85 | 2.28 | 1.68–3.01 | 6.18 | 5.17–7.34 | 9.12 | 8.45–9.83 | 19.11 | 18.12–20.14 | 28.23 | 27.03–29.47 | 7.63 | 7.09–8.19 | 14.28 | 13.55–15.04 | 21.90 | 21.00–22.84 |
| Wisconsin | 3.70 | 3.27–4.18 | 2.68 | 2.32–3.08 | 6.39 | 5.82–6.99 | 9.23 | 8.84–9.64 | 25.36 | 24.70–26.04 | 34.59 | 33.82–35.38 | 7.65 | 7.34–7.96 | 18.85 | 18.37–19.35 | 26.50 | 25.92–27.09 |
| Wyoming | 2.45 | 1.47–3.82 | -- | -- | 3.65 | 2.43–5.28 | 9.13 | 7.90–10.51 | 19.50 | 17.65–21.48 | 28.63 | 26.39–31.01 | 7.22 | 6.28–8.25 | 14.25 | 12.91–15.69 | 21.46 | 19.82–23.21 |
| TOTAL | 3.51 | 3.45–3.57 | 2.54 | 2.50–2.59 | 6.06 | 5.98–6.13 | 8.52 | 8.47–8.57 | 21.88 | 21.79–21.96 | 30.40 | 30.30–30.49 | 7.08 | 7.04–7.12 | 16.33 | 16.27–16.39 | 23.41 | 23.34–23.49 |
a. Rates are per 100,000 and are age-adjusted to the 2000 United States standard population.
- Counts are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals. Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval
Fig. 14.
Average Annual Age-Adjusted Incidence Ratesa of A) Malignant and B) Non-Malignant Primary Brain and Other CNS Tumors by Central Cancer Registry, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
The overall AAAIR of all tumors (malignant and non-malignant) for each individual CCR ranged from 17.72 to 35.71 per 100,000 population. Please see Supplementary Figure 13 for combined incidence of malignant and non-malignant tumors by CCR.
AAAIR of all primary malignant tumors ranged from 4.73 to 8.32 per 100,000 population, and AAAIR of all primary non-malignant tumors ranged from 10.80 to 28.49 per 100,000 population.
There was less variation by region for malignant tumor incidence rates (Fig. 14A) compared to incidence rates for non-malignant tumors (Fig. 14B). CCR and regional variations likely reflect differences in reporting and case ascertainment practices.
Among adults 20 years of age and older, CCR-specific AAAIR ranged from 5.94 to 10.16 per 100,000 population for malignant tumors and from 14.26 to 38.65 per 100,000 population for non-malignant tumors.
In persons less than 20 years of age, incidence rates ranged from 1.72 to 4.63 per 100,000 population for malignant tumors and from 1.33 to 3.93 per 100,000 population for non-malignant tumors.
Distribution by histology, WHO grade, diagnostic confirmation, and treatment completeness
The distribution of reported tumors with histologically confirmed diagnosis from 2012 to 2016 is listed by histology and reported WHO grade in Table 11.
Table 11.
Distribution of all histologically-confirmed brain and other central nervous system tumors by WHO grade, treatment information completeness, and major histology grouping, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | Number of Newly Diagnosed Tumors | Histologically Confirmed (%) | WHO Grade Completeness (%) | Assigned WHO Grade | Radiation Information Completenessb (%) | Surgical Extent of Resection Information Completenessc (%) | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Completea | Incomplete | Not Applicable | WHO Grade I | WHO Grade II | WHO Grade III |
WHO Grade IV | |||||
| Tumors of Neuroepithelial Tissue | 112,280 | 89.2% | 85.6% | 12.9% | 1.5% | 10.6% | 14.0% | 13.3% | 62.0% | 54.9% | 98.0% |
| Pilocytic Astrocytoma | 5,166 | 90.8% | 87.4% | 12.1% | 0.5% | 92.9% | 5.9% | 0.8% | 0.4% | 6.0% | 99.1% |
| Diffuse Astrocytoma | 7,500 | 92.4% | 85.6% | 14.3% | 0.1% | 3.4% | 64.1% | 19.5% | 13.0% | 49.6% | 97.7% |
| Anaplastic Astrocytoma | 7,015 | 99.2% | 94.8% | 5.1% | 0.1% | 0.1% | 1.3% | 90.2% | 8.5% | 77.3% | 99.2% |
| Unique Astrocytoma Variants | 1,161 | 75.5% | 75.8% | 23.9% | 0.3% | 21.4% | 55.3% | 18.1% | 5.3% | 20.9% | 98.2% |
| Malignant | 785 | 87.1% | 78.4% | 21.3% | 0.3% | 2.6% | 68.5% | 22.4% | 6.5% | 30.2% | 97.9% |
| Non-Malignant | 376 | 51.1% | 66.7% | 32.8% | 0.5% | 100.0% | 0.0% | 0.0% | 0.0% | 1.7% | 98.8% |
| Glioblastoma | 59,164 | 93.2% | 88.7% | 11.2% | 0.0% | 0.2% | 0.2% | 0.8% | 98.9% | 69.4% | 97.7% |
| Oligodendroglioma | 3,668 | 96.9% | 92.9% | 7.1% | 0.0% | 1.5% | 87.9% | 5.8% | 4.8% | 32.7% | 98.4% |
| Anaplastic Oligodendroglioma | 1,808 | 98.9% | 95.1% | 4.9% | 0.0% | 0.1% | 2.9% | 88.7% | 8.3% | 69.3% | 98.5% |
| Oligoastrocytic Tumors | 2,103 | 99.2% | 95.0% | 5.0% | 0.0% | 0.8% | 51.1% | 40.1% | 8.0% | 56.5% | 99.3% |
| Ependymal Tumors | 6,877 | 89.2% | 86.1% | 13.9% | 0.0% | 36.2% | 48.9% | 14.1% | 0.8% | 26.2% | 98.5% |
| Malignant | 4,005 | 93.6% | 89.0% | 11.0% | 0.1% | 2.5% | 74.2% | 22.1% | 1.1% | 38.2% | 98.6% |
| Non-Malignant | 2,872 | 82.9% | 81.5% | 18.5% | 0.0% | 94.1% | 5.5% | 0.3% | 0.1% | 9.4% | 98.4% |
| Glioma Malignant, NOS | 7,751 | 33.8% | 46.5% | 52.4% | 1.1% | 18.2% | 28.0% | 25.3% | 28.5% | 27.5% | 97.5% |
| Choroid Plexus Tumors | 817 | 88.1% | 76.1% | 23.9% | 0.0% | 63.9% | 18.8% | 16.4% | 0.9% | 4.5% | 98.2% |
| Malignant | 131 | 96.9% | 82.7% | 17.3% | 0.0% | 5.7% | 3.8% | 85.7% | 4.8% | 14.9% | 100.0% |
| Non-Malignant | 686 | 86.4% | 74.7% | 25.3% | 0.0% | 77.7% | 22.3% | 0.0% | 0.0% | 2.5% | 98.0% |
| Other Neuroepithelial Tumors | 109 | 93.6% | 48.0% | 51.0% | 1.0% | 8.2% | 53.1% | 26.5% | 12.2% | 37.6% | 100.0% |
| Malignant | 72 | 98.6% | 40.8% | 57.7% | 1.4% | 10.3% | 24.1% | 44.8% | 20.7% | 50.8% | 100.0% |
| Non-Malignant | 37 | 83.8% | 64.5% | 35.5% | 0.0% | 5.0% | 95.0% | 0.0% | 0.0% | 13.9% | 100.0% |
| Neuronal and Mixed Neuronal Glial Tumors | 4,852 | 92.7% | 62.7% | 20.0% | 17.3% | 80.5% | 15.1% | 3.6% | 0.7% | 15.9% | 98.6% |
| Malignant | 976 | 98.8% | 16.3% | 5.0% | 78.7% | 25.5% | 8.9% | 56.7% | 8.9% | 62.0% | 98.1% |
| Non-Malignant | 3,876 | 91.1% | 75.4% | 24.0% | 0.5% | 83.7% | 15.5% | 0.5% | 0.3% | 4.4% | 98.7% |
| Tumors of the Pineal Region | 796 | 76.0% | 0.0% | 0.0% | 100.0% | -- | -- | -- | -- | 40.4% | 97.7% |
| Malignant | 445 | 95.7% | 0.0% | 0.0% | 100.0% | -- | -- | -- | -- | 65.2% | 98.6% |
| Non-Malignant | 351 | 51.0% | 0.0% | 0.0% | 100.0% | -- | -- | -- | -- | 9.3% | 97.0% |
| Embryonal Tumors | 3,493 | 98.0% | 75.2% | 24.1% | 0.7% | 1.4% | 0.2% | 1.4% | 97.0% | 61.9% | 97.6% |
| Tumors of Cranial and Spinal Nerves | 35,053 | 50.6% | 34.1% | 65.9% | 0.0% | 99.0% | 0.5% | 0.2% | 0.2% | 18.2% | 98.2% |
| Nerve Sheath Tumors | 35,017 | 50.6% | 34.1% | 65.9% | 0.0% | 99.0% | 0.5% | 0.2% | 0.2% | 18.2% | 98.2% |
| Malignant | 231 | 80.5% | 21.5% | 78.5% | 0.0% | 47.5% | 17.5% | 20.0% | 15.0% | 38.6% | 83.2% |
| Non-Malignant | 34,786 | 50.4% | 34.2% | 65.8% | 0.0% | 99.4% | 0.4% | 0.1% | 0.1% | 18.1% | 98.3% |
| Other Tumors of Cranial and Spinal Nerves | 36 | 41.7% | 26.7% | 73.3% | 0.0% | 100.0% | 0.0% | 0.0% | 0.0% | 2.8% | 100.0% |
| Tumors of Meninges | 157,310 | 41.3% | 77.7% | 22.2% | 0.1% | 80.3% | 17.5% | 2.1% | 0.1% | 7.5% | 97.7% |
| Meningioma | 152,756 | 40.0% | 79.3% | 20.7% | 0.0% | 80.5% | 17.7% | 1.7% | 0.1% | 7.2% | 97.7% |
| Malignant | 1,774 | 79.0% | 84.9% | 15.1% | 0.0% | 21.9% | 17.3% | 59.6% | 1.2% | 38.4% | 85.3% |
| Non-Malignant | 150,982 | 39.5% | 79.1% | 20.8% | 0.0% | 82.0% | 17.7% | 0.2% | 0.1% | 6.9% | 97.8% |
| Mesenchymal Tumors | 1,433 | 72.8% | 52.3% | 47.2% | 0.5% | 8.1% | 47.4% | 39.9% | 4.6% | 30.6% | 98.1% |
| Primary Melanocytic Lesions | 109 | 91.7% | 13.0% | 84.0% | 3.0% | 53.8% | 30.8% | 7.7% | 7.7% | 43.6% | 89.7% |
| Other Neoplasms Related to the Meninges | 3,012 | 91.5% | 55.2% | 43.4% | 1.3% | 99.2% | 0.5% | 0.1% | 0.2% | 7.3% | 98.4% |
| Lymphoma and Hematopoietic Neoplasms | 7,914 | 94.6% | 5.1% | 94.0% | 0.8% | 100.0% | 0.0% | 0.0% | 0.0% | 22.0% | 99.2% |
| Lymphoma | 7,680 | 94.8% | 5.4% | 94.2% | 0.4% | 100.0% | 0.0% | 0.0% | 0.0% | 21.7% | 99.1% |
| Other Hematopoietic Neoplasms | 234 | 88.5% | 0.0% | 88.8% | 11.2% | -- | -- | -- | -- | 31.7% | 99.2% |
| Germ Cell Tumors and Cysts | 1,543 | 81.1% | 3.0% | 55.3% | 41.8% | 24.3% | 5.4% | 5.4% | 64.9% | 46.4% | 98.5% |
| Germ cell tumors, cysts, and heterotopias | 1,543 | 81.1% | 3.0% | 55.3% | 41.8% | 24.3% | 5.4% | 5.4% | 64.9% | 46.4% | 98.5% |
| Malignant | 1,037 | 88.4% | 3.3% | 43.4% | 53.3% | 6.7% | 6.7% | 6.7% | 80.0% | 68.0% | 98.7% |
| Non-Malignant | 506 | 66.2% | 2.1% | 87.8% | 10.1% | 100.0% | 0.0% | 0.0% | 0.0% | 2.5% | 97.9% |
| Tumors of Sellar Region | 71,084 | 48.3% | 0.4% | 0.6% | 99.0% | 100.0% | 0.0% | 0.0% | 0.0% | 3.2% | 97.8% |
| Tumors of the Pituitary | 68,020 | 46.7% | 0.0% | 0.0% | 100.0% | -- | -- | -- | -- | 2.3% | 97.8% |
| Malignant | 157 | 66.9% | 0.0% | 0.0% | 100.0% | -- | -- | -- | -- | 17.4% | 87.0% |
| Non-Malignant | 67,863 | 46.6% | 0.0% | 0.0% | 100.0% | -- | -- | -- | -- | 2.3% | 97.8% |
| Craniopharyngioma | 3,064 | 83.5% | 5.7% | 7.5% | 86.7% | 100.0% | 0.0% | 0.0% | 0.0% | 22.0% | 97.8% |
| Unclassified Tumors | 20,556 | 17.5% | 4.4% | 87.5% | 8.1% | 64.2% | 8.2% | 8.2% | 19.5% | 4.0% | 70.2% |
| Hemangioma | 5,982 | 29.3% | 2.3% | 97.2% | 0.5% | 87.8% | 7.3% | 2.4% | 2.4% | 2.1% | 97.6% |
| Neoplasm Unspecified | 14,418 | 12.3% | 6.1% | 78.7% | 15.3% | 57.4% | 9.3% | 9.3% | 24.1% | 5.1% | 60.3% |
| Malignant | 6,634 | 8.7% | 7.7% | 85.7% | 6.6% | 13.6% | 11.4% | 20.5% | 54.5% | 9.9% | 42.7% |
| Non-Malignant | 7,784 | 15.4% | 5.3% | 75.3% | 19.4% | 87.5% | 7.8% | 1.6% | 3.1% | 2.7% | 75.8% |
| All Other | 156 | 38.5% | 16.7% | 66.7% | 16.7% | 40.0% | 0.0% | 20.0% | 40.0% | 12.7% | 89.6% |
| TOTAL | 405,740 | 56.5% | 62.9% | 21.1% | 16.0% | 39.3% | 14.7% | 8.8% | 37.3% | 21.3% | 95.9% |
| Malignant | 122,569 | 85.3% | 80.5% | 17.5% | 2.0% | 6.2% | 14.2% | 15.0% | 64.7% | 54.8% | 92.3% |
| Non-Malignant | 283,171 | 44.1% | 48.4% | 24.0% | 27.5% | 84.3% | 15.3% | 0.3% | 0.1% | 7.1% | 97.1% |
a. Completeness is defined as having an assigned code that corresponds with a WHO grade as defined by the American Joint Commission on Cancer’s Collaborative Staging schema.
b. Radiation is defined using a recoded variable based on NAACCR Item #1360 (http://datadictionary.naaccr.org/default.aspx?c=10#136). Completeness is defined as having a value other than ‘none’ or ‘unknown.’
c. Surgery is defined using a recoded variable based on NAACCR Item #1290 (http://datadictionary.naaccr.org/default.aspx?c=10#1290). Please see the SEER site-specific surgery codes for more information on coding for this variable (https://seer.cancer.gov/archive/tools/SEER2003.surg.prim.site.codes.pdf). Completeness is defined as having a value other than ‘unknown.’
- Percentages are not presented when category is not applicable.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; CNS, central nervous system; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; WHO, World Health Organization
Overall, 56.5% of tumors had histologic confirmation (85.3% of malignant tumors and 44.1% of non-malignant tumors).
The proportion of tumors with histologic confirmation varied substantially by histology, with the highest proportion in anaplastic astrocytoma (99.2%) and oligoastrocytic tumors (99.2%). The proportion with histologic confirmation was lowest in neoplasm unspecific (12.3%), hemangioma (29.3%), glioma malignant, NOS (33.8%) and non-malignant meningioma (39.5%).
Overall, 62.9% of tumors had complete WHO grade information, but there was substantial variation by histology.
The histologic types with the highest WHO grade completeness were anaplastic oligodendroglioma (95.1%), oligoastrocytic tumors (95.0%), and anaplastic astrocytoma (94.8%).
Incidence by urban or rural residence
Incidence counts and AAAIR for brain and other CNS tumors are shown by urban/rural residence and histology in Supplementary Table 8. Incidence of selected histologies by urban/rural residence is show in Figure 15.
Fig. 15.
Average Annual Age-Adjusted Incidence Ratesa with 95% Confidence Intervals of Selected Primary Brain and Other CNS Tumor Histologies by Urban Or Rural Location of Residenceb, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
The overall incidence of brain and other CNS tumors was 11% higher in urban areas as compared to rural areas (23.22 per 100,000 and 20.80 per 100,000, respectively, P < 0.0001).
Incidence of malignant brain and other CNS tumors was slightly higher in urban areas (6.90 per 100,000) as compared to rural areas (6.80 per 100,000, P = 0.0822).
Incidence of non-malignant brain and other CNS tumors was 17% higher in urban areas as compared to rural areas (16.33 per 100,000 and 14.00 per 100,000, respectively, P < 0.0001).
Incidence of glioblastoma (3%, P = 0.436) was higher in urban as compared to rural areas.
Non-malignant histologies were primarily diagnosed more frequently in urban areas, including meningioma (18% higher, P < 0.0001), nerve sheath tumors (20% higher, P < 0.0001), and tumors of the pituitary (20% higher, P < 0.0001).
Distribution of tumors in Puerto Rico
The distribution of all brain and other CNS tumors diagnosed among residents of Puerto Rico by histology is shown in Supplementary Figure 14.
Approximately 39.4% of tumors were malignant and 60.6% were non-malignant.
Non-malignant meningioma was the most common tumor type (26.3%), followed by glioblastoma (18.1%).
Incidence Rates by Race and Histology
AAAIR by race and histology are shown in Table 12.
Table 12.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for all brain and other central nervous system tumors by major histology grouping, histology, and racec, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | White | Black | American Indian/Alaska Native | Asian/Pacific Islander | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 98,423 | 19,685 | 7.09 | 7.04–7.13 | 8,480 | 1696 | 3.97 | 3.89–4.06 | 625 | 125 | 3.12 | 2.86–3.39 | 3,348 | 670 | 3.57 | 3.45–3.69 |
| Pilocytic Astrocytoma | 4,218 | 844 | 0.38 | 0.36–0.39 | 601 | 120 | 0.26 | 0.24–0.28 | 38 | 8 | 0.15 | 0.10–0.20 | 200 | 40 | 0.22 | 0.19–0.26 |
| Diffuse Astrocytoma | 6,513 | 1,303 | 0.50 | 0.49–0.51 | 585 | 117 | 0.27 | 0.25–0.29 | 58 | 12 | 0.28 | 0.21–0.37 | 254 | 51 | 0.26 | 0.23–0.30 |
| Anaplastic Astrocytoma | 6,227 | 1,245 | 0.46 | 0.45–0.47 | 465 | 93 | 0.22 | 0.20–0.24 | 41 | 8 | 0.20 | 0.14–0.27 | 201 | 40 | 0.21 | 0.18–0.24 |
| Unique Astrocytoma Variants | 919 | 184 | 0.08 | 0.07–0.08 | 150 | 30 | 0.07 | 0.06–0.08 | -- | -- | -- | -- | 64 | 13 | 0.07 | 0.05–0.09 |
| Malignant | 643 | 129 | 0.05 | 0.05–0.06 | 78 | 16 | 0.04 | 0.03–0.04 | -- | -- | -- | -- | 44 | 9 | 0.05 | 0.03–0.06 |
| Non-Malignant | 276 | 55 | 0.02 | 0.02–0.03 | 72 | 14 | 0.03 | 0.02–0.04 | -- | -- | -- | -- | 20 | 4 | 0.02 | 0.01–0.04 |
| Glioblastoma | 53,426 | 10,685 | 3.49 | 3.46–3.52 | 3,647 | 729 | 1.79 | 1.73–1.85 | 242 | 48 | 1.43 | 1.25–1.64 | 1,345 | 269 | 1.46 | 1.38–1.54 |
| Oligodendroglioma | 3,200 | 640 | 0.26 | 0.25–0.27 | 247 | 49 | 0.12 | 0.10–0.13 | 28 | 6 | 0.12 | 0.08–0.18 | 126 | 25 | 0.13 | 0.10–0.15 |
| Anaplastic Oligodendroglioma | 1,576 | 315 | 0.12 | 0.11–0.13 | 101 | 20 | 0.05 | 0.04–0.06 | -- | -- | -- | -- | 89 | 18 | 0.09 | 0.07–0.11 |
| Oligoastrocytic Tumors | 1,860 | 372 | 0.15 | 0.14–0.16 | 123 | 25 | 0.06 | 0.05–0.07 | -- | -- | -- | -- | 72 | 14 | 0.07 | 0.05–0.09 |
| Ependymal Tumors | 5,890 | 1,178 | 0.46 | 0.45–0.47 | 565 | 113 | 0.26 | 0.24–0.28 | 50 | 10 | 0.22 | 0.17–0.30 | 251 | 50 | 0.26 | 0.23–0.29 |
| Malignant | 3,372 | 674 | 0.27 | 0.26–0.28 | 375 | 75 | 0.17 | 0.15–0.19 | 25 | 5 | 0.11 | 0.07–0.16 | 161 | 32 | 0.17 | 0.14–0.20 |
| Non-Malignant | 2,518 | 504 | 0.19 | 0.19–0.20 | 190 | 38 | 0.09 | 0.07–0.10 | 25 | 5 | 0.12 | 0.07–0.17 | 90 | 18 | 0.09 | 0.07–0.11 |
| Glioma Malignant, NOS | 6,415 | 1,283 | 0.51 | 0.49–0.52 | 869 | 174 | 0.40 | 0.38–0.43 | 48 | 10 | 0.22 | 0.16–0.29 | 277 | 55 | 0.30 | 0.27–0.34 |
| Choroid Plexus Tumors | 677 | 135 | 0.06 | 0.05–0.06 | 77 | 15 | 0.03 | 0.03–0.04 | -- | -- | -- | -- | 36 | 7 | 0.04 | 0.03–0.05 |
| Malignant | 100 | 20 | 0.01 | 0.01-0.01 | 17 | 3 | 0.01 | 0.00–0.01 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 577 | 115 | 0.05 | 0.04–0.05 | 60 | 12 | 0.03 | 0.02–0.03 | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neuroepithelial Tumors | 86 | 17 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Malignant | 56 | 11 | 0.00 | 0.00–0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 30 | 6 | 0.00 | 0.00-0.00 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Neuronal and Mixed Neuronal Glial Tumors | 3,990 | 798 | 0.33 | 0.32–0.34 | 518 | 104 | 0.23 | 0.21–0.25 | 39 | 8 | 0.16 | 0.11–0.23 | 219 | 44 | 0.23 | 0.20–0.26 |
| Malignant | 819 | 164 | 0.06 | 0.06-0.06 | 75 | 15 | 0.04 | 0.03–0.05 | -- | -- | -- | -- | 59 | 12 | 0.06 | 0.05–0.08 |
| Non-Malignant | 3,171 | 634 | 0.27 | 0.26–0.28 | 443 | 89 | 0.19 | 0.17–0.21 | 29 | 6 | 0.11 | 0.08–0.17 | 160 | 32 | 0.17 | 0.14–0.19 |
| Tumors of the Pineal Region | 630 | 126 | 0.05 | 0.05–0.06 | 116 | 23 | 0.05 | 0.04–0.06 | -- | -- | -- | -- | 29 | 6 | 0.03 | 0.02–0.04 |
| Malignant | 333 | 67 | 0.03 | 0.02–0.03 | 79 | 16 | 0.04 | 0.03–0.04 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 297 | 59 | 0.02 | 0.02–0.03 | 37 | 7 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- |
| Embryonal Tumors | 2,796 | 559 | 0.25 | 0.24–0.26 | 406 | 81 | 0.17 | 0.15–0.19 | 34 | 7 | 0.13 | 0.09–0.19 | 179 | 36 | 0.20 | 0.17–0.23 |
| Tumors of Cranial and Spinal Nerves | 29,894 | 5,979 | 2.11 | 2.09–2.14 | 2137 | 427 | 1.01 | 0.97–1.06 | 229 | 46 | 1.12 | 0.98–1.29 | 1,943 | 389 | 1.98 | 1.89–2.07 |
| Nerve Sheath Tumors | 29,864 | 5,973 | 2.11 | 2.09–2.14 | 2,135 | 427 | 1.01 | 0.97–1.06 | 228 | 46 | 1.12 | 0.97–1.28 | 1,940 | 388 | 1.97 | 1.88–2.06 |
| Malignant | 177 | 35 | 0.01 | 0.01–0.02 | 28 | 6 | 0.01 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 29,687 | 5,937 | 2.10 | 2.07–2.12 | 2107 | 421 | 1.00 | 0.96–1.04 | -- | -- | - | -- | -- | -- | -- | -- |
| Other Tumors of Cranial and Spinal Nerves | 30 | 6 | 0.00 | 0.00-0.00 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Meninges | 128,202 | 25,640 | 8.66 | 8.61–8.70 | 19,519 | 3,904 | 10.13 | 9.99–10.28 | 929 | 186 | 5.55 | 5.18–5.95 | 6,616 | 1,323 | 7.42 | 7.23–7.60 |
| Meningioma | 124,430 | 24,886 | 8.37 | 8.32–8.42 | 19,053 | 3,811 | 9.92 | 9.77–10.06 | 902 | 180 | 5.43 | 5.06–5.82 | 6,400 | 1,280 | 7.20 | 7.02–7.38 |
| Malignant | 1,396 | 279 | 0.09 | 0.09–0.10 | 269 | 54 | 0.14 | 0.12–0.16 | -- | -- | -- | -- | 83 | 17 | 0.09 | 0.07–0.12 |
| Non-Malignant | 123,034 | 24,607 | 8.28 | 8.23–8.32 | 18,784 | 3,757 | 9.78 | 9.63–9.92 | -- | -- | -- | -- | 6,317 | 1,263 | 7.10 | 6.93–7.29 |
| Mesenchymal Tumors | 1,195 | 239 | 0.09 | 0.09–0.10 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Primary Melanocytic Lesions | 102 | 20 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neoplasms Related to the Meninges | 2,475 | 495 | 0.19 | 0.18–0.20 | 325 | 65 | 0.15 | 0.13–0.17 | 22 | 4 | 0.10 | 0.06–0.16 | 137 | 27 | 0.14 | 0.11–0.16 |
| Lymphoma and Hematopoietic Neoplasms | 6,691 | 1,338 | 0.45 | 0.44–0.46 | 6,25 | 125 | 0.31 | 0.28–0.33 | 46 | 9 | 0.26 | 0.19–0.36 | 446 | 89 | 0.50 | 0.45–0.55 |
| Lymphoma | 6,504 | 1,301 | 0.43 | 0.42–0.44 | 597 | 119 | 0.29 | 0.27–0.32 | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Hematopoietic Neoplasms | 187 | 37 | 0.01 | 0.01–0.02 | 28 | 6 | 0.01 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- |
| Germ Cell Tumors and Cysts | 1,221 | 244 | 0.11 | 0.10–0.11 | 151 | 30 | 0.06 | 0.05–0.08 | -- | -- | -- | -- | 126 | 25 | 0.14 | 0.11–0.16 |
| Germ cell tumors, cysts, and heterotopias | 1,221 | 244 | 0.11 | 0.10–0.11 | 151 | 30 | 0.06 | 0.05–0.08 | -- | -- | -- | -- | 126 | 25 | 0.14 | 0.11–0.16 |
| Malignant | 813 | 163 | 0.07 | 0.07–0.08 | 94 | 19 | 0.04 | 0.03–0.05 | -- | -- | -- | -- | 101 | 20 | 0.11 | 0.09–0.14 |
| Non-Malignant | 408 | 82 | 0.03 | 0.03–0.04 | 57 | 11 | 0.03 | 0.02–0.03 | -- | -- | -- | -- | 25 | 5 | 0.03 | 0.02–0.04 |
| Tumors of Sellar Region | 51,448 | 10,290 | 3.88 | 3.84–3.91 | 13,875 | 2,775 | 6.75 | 6.64–6.87 | 636 | 127 | 3.20 | 2.94–3.47 | 3,669 | 734 | 3.76 | 3.63–3.88 |
| Tumors of the Pituitary | 49,254 | 9,851 | 3.71 | 3.67–3.74 | 13,243 | 2,649 | 6.46 | 6.35–6.58 | 610 | 122 | 3.07 | 2.81–3.33 | 3,508 | 702 | 3.59 | 3.47–3.71 |
| Malignant | 114 | 23 | 0.01 | 0.01-0.01 | 32 | 6 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 49,140 | 9,828 | 3.70 | 3.66–3.73 | 13,211 | 2,642 | 6.45 | 6.33–6.56 | -- | -- | -- | -- | -- | -- | -- | -- |
| Craniopharyngioma | 2,194 | 439 | 0.17 | 0.16–0.18 | 632 | 126 | 0.29 | 0.27–0.32 | 26 | 5 | 0.13 | 0.08–0.19 | 161 | 32 | 0.17 | 0.14–0.20 |
| Unclassified Tumors | 17,220 | 3,444 | 1.22 | 1.20–1.23 | 2,149 | 430 | 1.10 | 1.05–1.15 | 178 | 36 | 0.99 | 0.84–1.16 | 732 | 146 | 0.83 | 0.77–0.90 |
| Hemangioma | 5,000 | 1,000 | 0.38 | 0.37–0.39 | 547 | 109 | 0.26 | 0.24–0.28 | 71 | 14 | 0.36 | 0.27–0.45 | 268 | 54 | 0.28 | 0.25–0.32 |
| Neoplasm Unspecified | 12,109 | 2,422 | 0.83 | 0.82–0.85 | 1,570 | 314 | 0.83 | 0.78–0.87 | 105 | 21 | 0.61 | 0.49–0.75 | 457 | 91 | 0.54 | 0.49–0.60 |
| Malignant | 5,749 | 1,150 | 0.38 | 0.37–0.39 | 571 | 114 | 0.32 | 0.29–0.34 | 51 | 10 | 0.30 | 0.22–0.41 | 189 | 38 | 0.24 | 0.20–0.27 |
| Non-Malignant | 6,360 | 1,272 | 0.45 | 0.44–0.46 | 999 | 200 | 0.51 | 0.48–0.54 | 54 | 11 | 0.31 | 0.23–0.41 | 268 | 54 | 0.31 | 0.27–0.35 |
| All Other | 111 | 22 | 0.01 | 0.01-0.01 | 32 | 6 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- |
| TOTAL d | 333,099 | 66,620 | 23.50 | 23.42–23.59 | 46,936 | 9,387 | 23.34 | 23.13–23.56 | 2,652 | 530 | 14.28 | 13.70–14.87 | 16,880 | 3,376 | 18.18 | 17.90–18.46 |
| Malignant | 107,119 | 21,424 | 7.58 | 7.54–7.63 | 9356 | 1,871 | 4.48 | 4.38–4.57 | 677 | 135 | 3.51 | 3.24–3.81 | 3,928 | 786 | 4.25 | 4.12–4.39 |
| Non-Malignant | 225,980 | 45,196 | 15.92 | 15.85–15.99 | 37,580 | 7,516 | 18.87 | 18.67–19.06 | 1,975 | 395 | 10.76 | 10.26–11.28 | 12,952 | 2,590 | 13.93 | 13.68–14.17 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. Individuals with unknown race were excluded (N = 6173).
d. Refers to all brain tumors including histologies not presented in this table.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
AAAIR for all primary brain and other CNS tumors combined were lower for race groups AIAN (14.28 per 100,000 population) compared to Whites (23.50 per 100,000 population), Blacks (23.34 per 100,000 population), and API (18.18 per 100,000 population).
AAAIR for non-malignant primary brain and other CNS tumors were highest in Blacks (18.87 per 100,000) compared to Whites (15.92 per 100,000), AIAN (10.76 per 100,000), and API (13.93 per 100,000).
AAAIR for malignant primary brain and other CNS tumors were highest in Whites (7.58 per 100,000) compared to Blacks (4.48 per 100,000), AIAN (3.51 per 100,000), and API (4.25 per 100,000).
AAAIR for meningioma, tumors of the pituitary, and craniopharyngioma observed for Blacks exceeded those observed for Whites, AIAN, and API.
The AAAIR for tumors of the cranial and spinal nerves in the API group was the highest for all racial groups.
Incidence rate ratios (White:Black) for selected histologies are shown in Figure 16.
Fig. 16.
Incidence Rate Ratios by Race (Whites:Blacks and Whites:Asian Or Pacific Islanders [API]) for Selected Selected Primary Brain and Other CNS Tumor Histologies, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Incidence rates for glioblastoma (P < 0.0001), all other astrocytoma (P < 0.0001), and nerve sheath tumors (P < 0.0001) were approximately 2 times greater in Whites than in Blacks.
Incidence of oligodendroglioma was approximately 2.28 times greater in Whites than in Blacks (P < 0.0001).
Incidence rates for pilocytic astrocytoma (P < 0.0001), ependymal tumors (P < 0.0001), embryonal tumors (P < 0.0001), lymphoma (P < 0.0001), and germ cell tumors (P < 0.0001) were also higher among Whites than Blacks.
Incidence rates for non-malignant (P < 0.0001) and malignant (P < 0.0001) meningioma and tumors of the pituitary (P < 0.0001) were higher among Blacks than Whites.
Incidence rate ratios (White:API) for selected histologies are shown in Figure 16.
Incidence rates for glioblastoma (P < 0.0001) were over 2.39 times greater in Whites than in API.
Incidence of germ cell tumors was approximately 22% higher in API compared to Whites (P < 0.0001).
Incidence Rates by Hispanic Ethnicity and Histology
AAAIR by Hispanic ethnicity and histology are shown in Table 13.
Table 13.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for all brain and other central nervous system tumors by major histology grouping, histology, hispanic ethnicityc, and race, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | All Hispanic | White Hispanic | Black Hispanic | All Non-Hispanic | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 11,414 | 2,283 | 4.96 | 4.86–5.06 | 10,492 | 2,098 | 5.04 | 4.94–5.15 | 276 | 55 | 2.51 | 2.18–2.87 | 100,866 | 20,173 | 6.85 | 6.81–6.89 |
| Pilocytic Astrocytoma | 826 | 165 | 0.25 | 0.23–0.27 | 744 | 149 | 0.25 | 0.23–0.27 | 25 | 5 | 0.13 | 0.08–0.20 | 4,340 | 868 | 0.38 | 0.37–0.39 |
| Diffuse Astrocytoma | 804 | 161 | 0.33 | 0.31–0.36 | 732 | 146 | 0.33 | 0.31–0.36 | 17 | 3 | 0.13 | 0.07–0.23 | 6,696 | 1,339 | 0.49 | 0.47–0.50 |
| Anaplastic Astrocytoma | 659 | 132 | 0.29 | 0.26–0.31 | 611 | 122 | 0.29 | 0.27–0.32 | 17 | 3 | 0.15 | 0.08–0.25 | 6,356 | 1,271 | 0.44 | 0.43–0.45 |
| Unique Astrocytoma Variants | 189 | 38 | 0.06 | 0.06–0.08 | 175 | 35 | 0.07 | 0.06–0.08 | -- | -- | -- | -- | 972 | 194 | 0.08 | 0.07–0.08 |
| Malignant | 115 | 23 | 0.04 | 0.03–0.05 | 109 | 22 | 0.04 | 0.04–0.05 | -- | -- | -- | -- | 670 | 134 | 0.05 | 0.05–0.06 |
| Non-Malignant | 74 | 15 | 0.02 | 0.02–0.03 | 66 | 13 | 0.02 | 0.02–0.03 | -- | -- | -- | -- | 302 | 60 | 0.03 | 0.02–0.03 |
| Glioblastoma | 4,491 | 898 | 2.41 | 2.33–2.48 | 4,208 | 842 | 2.46 | 2.39–2.54 | 111 | 22 | 1.35 | 1.09–1.65 | 54,673 | 10,935 | 3.31 | 3.29–3.34 |
| Oligodendroglioma | 429 | 86 | 0.17 | 0.15–0.18 | 386 | 77 | 0.17 | 0.15–0.18 | -- | -- | -- | -- | 3,239 | 648 | 0.25 | 0.24–0.26 |
| Anaplastic Oligodendroglioma | 217 | 43 | 0.09 | 0.08–0.11 | 199 | 40 | 0.09 | 0.08–0.11 | -- | -- | -- | -- | 1,591 | 318 | 0.11 | 0.11–0.12 |
| Oligoastrocytic Tumors | 223 | 45 | 0.09 | 0.08–0.10 | 207 | 41 | 0.09 | 0.08–0.11 | -- | -- | -- | -- | 1,880 | 376 | 0.14 | 0.14–0.15 |
| Ependymal Tumors | 950 | 190 | 0.36 | 0.34–0.39 | 858 | 172 | 0.36 | 0.34–0.39 | 18 | 4 | 0.15 | 0.08–0.26 | 5,927 | 1,185 | 0.44 | 0.43–0.45 |
| Malignant | 632 | 126 | 0.23 | 0.21–0.25 | 580 | 116 | 0.24 | 0.22–0.26 | -- | -- | -- | -- | 3,373 | 675 | 0.25 | 0.25–0.26 |
| Non-Malignant | 318 | 64 | 0.13 | 0.12–0.15 | 278 | 56 | 0.13 | 0.11–0.14 | -- | -- | -- | -- | 2,554 | 511 | 0.18 | 0.18–0.19 |
| Glioma Malignant, NOS | 966 | 193 | 0.37 | 0.34–0.40 | 874 | 175 | 0.37 | 0.35–0.40 | 30 | 6 | 0.20 | 0.13–0.31 | 6,785 | 1,357 | 0.52 | 0.50–0.53 |
| Choroid Plexus Tumors | 152 | 30 | 0.05 | 0.04–0.06 | 137 | 27 | 0.05 | 0.04–0.06 | -- | -- | -- | -- | 665 | 133 | 0.05 | 0.05–0.06 |
| Malignant | 23 | 5 | 0.01 | 0.00–0.01 | 20 | 4 | 0.01 | 0.00–0.01 | -- | -- | -- | -- | 108 | 22 | 0.01 | 0.01-0.01 |
| Non-Malignant | 129 | 26 | 0.04 | 0.04–0.05 | 117 | 23 | 0.04 | 0.04–0.05 | -- | -- | -- | -- | 557 | 111 | 0.05 | 0.04–0.05 |
| Other Neuroepithelial Tumors | 21 | 4 | 0.01 | 0.00–0.01 | 18 | 4 | 0.01 | 0.00–0.01 | -- | -- | -- | -- | 88 | 18 | 0.01 | 0.01-0.01 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 60 | 12 | 0.00 | 0.00–0.01 |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 28 | 6 | 0.00 | 0.00-0.00 |
| Neuronal and Mixed Neuronal Glial Tumors | 631 | 126 | 0.22 | 0.20–0.24 | 556 | 111 | 0.21 | 0.19–0.23 | -- | -- | -- | -- | 4,221 | 844 | 0.34 | 0.33–0.35 |
| Malignant | 127 | 25 | 0.05 | 0.04–0.06 | 113 | 23 | 0.05 | 0.04–0.06 | -- | -- | -- | -- | 849 | 170 | 0.06 | 0.05–0.06 |
| Non-Malignant | 504 | 101 | 0.16 | 0.15–0.18 | 443 | 89 | 0.16 | 0.15–0.18 | -- | -- | -- | -- | 3,372 | 674 | 0.28 | 0.27–0.29 |
| Tumors of the Pineal Region | 108 | 22 | 0.04 | 0.03–0.05 | 99 | 20 | 0.04 | 0.03–0.05 | -- | -- | -- | -- | 688 | 138 | 0.05 | 0.05–0.06 |
| Malignant | 71 | 14 | 0.02 | 0.02–0.03 | 65 | 13 | 0.02 | 0.02–0.03 | -- | -- | -- | -- | 374 | 75 | 0.03 | 0.03-0.03 |
| Non-Malignant | 37 | 7 | 0.01 | 0.01–0.02 | 34 | 7 | 0.01 | 0.01–0.02 | -- | -- | -- | -- | 314 | 63 | 0.02 | 0.02–0.03 |
| Embryonal Tumors | 748 | 150 | 0.22 | 0.21–0.24 | 688 | 138 | 0.23 | 0.22–0.25 | -- | -- | -- | -- | 2,745 | 549 | 0.24 | 0.23–0.25 |
| Tumors of Cranial and Spinal Nerves | 3,128 | 626 | 1.41 | 1.36–1.46 | 2,794 | 559 | 1.39 | 1.34–1.44 | 81 | 16 | 0.77 | 0.60–0.98 | 31,925 | 6,385 | 2.11 | 2.09–2.14 |
| Nerve Sheath Tumors | 3,122 | 624 | 1.41 | 1.36–1.46 | 2,788 | 558 | 1.39 | 1.33–1.44 | 81 | 16 | 0.77 | 0.60–0.98 | 31,895 | 6,379 | 2.11 | 2.09–2.13 |
| Malignant | 37 | 7 | 0.02 | 0.01–0.02 | 33 | 7 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | 194 | 39 | 0.01 | 0.01–0.02 |
| Non-Malignant | 3,085 | 617 | 1.39 | 1.34–1.44 | 2,755 | 551 | 1.37 | 1.32–1.42 | -- | -- | -- | -- | 31,701 | 6,340 | 2.10 | 2.07–2.12 |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 30 | 6 | 0.00 | 0.00-0.00 |
| Tumors of Meninges | 15,279 | 3,056 | 8.36 | 8.22–8.50 | 13,917 | 2,783 | 8.32 | 8.18–8.47 | 438 | 88 | 5.56 | 5.01–6.15 | 142,031 | 28,406 | 8.93 | 8.89–8.98 |
| Meningioma | 14,679 | 2,936 | 8.11 | 7.98–8.25 | 13,359 | 2,672 | 8.07 | 7.93–8.22 | 428 | 86 | 5.48 | 4.93–6.07 | 138,077 | 27,615 | 8.65 | 8.61–8.70 |
| Malignant | 181 | 36 | 0.09 | 0.08–0.11 | 170 | 34 | 0.10 | 0.08–0.11 | -- | -- | -- | -- | 1,593 | 319 | 0.10 | 0.09–0.10 |
| Non-Malignant | 14,498 | 2,900 | 8.02 | 7.88–8.16 | 13,189 | 2,638 | 7.97 | 7.83–8.12 | -- | -- | -- | -- | 136,484 | 27,297 | 8.55 | 8.51–8.60 |
| Mesenchymal Tumors | 206 | 41 | 0.09 | 0.07–0.10 | 193 | 39 | 0.09 | 0.08–0.10 | -- | -- | -- | -- | 1,227 | 245 | 0.09 | 0.08–0.09 |
| Primary Melanocytic Lesions | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 99 | 20 | 0.01 | 0.01-0.01 |
| Other Neoplasms Related to the Meninges | 384 | 77 | 0.16 | 0.14–0.17 | 356 | 71 | 0.16 | 0.14–0.18 | -- | -- | -- | -- | 2,628 | 526 | 0.19 | 0.18–0.19 |
| Lymphoma and Hematopoietic Neoplasms | 920 | 184 | 0.49 | 0.46–0.52 | 864 | 173 | 0.51 | 0.47–0.54 | 16 | 3 | 0.14 | 0.08–0.23 | 6,994 | 1,399 | 0.44 | 0.43–0.45 |
| Lymphoma | 879 | 176 | 0.47 | 0.44–0.51 | 828 | 166 | 0.49 | 0.46–0.53 | -- | -- | -- | -- | 6,801 | 1,360 | 0.42 | 0.41–0.43 |
| Other Hematopoietic Neoplasms | 41 | 8 | 0.02 | 0.01–0.02 | 36 | 7 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | 193 | 39 | 0.01 | 0.01–0.02 |
| Germ Cell Tumors and Cysts | 334 | 67 | 0.10 | 0.09–0.12 | 300 | 60 | 0.10 | 0.09–0.12 | -- | -- | -- | -- | 1,209 | 242 | 0.10 | 0.10–0.11 |
| Germ cell tumors, cysts, and heterotopias | 334 | 67 | 0.10 | 0.09–0.12 | 300 | 60 | 0.10 | 0.09–0.12 | -- | -- | -- | -- | 1,209 | 242 | 0.10 | 0.10–0.11 |
| Malignant | 235 | 47 | 0.07 | 0.06–0.08 | 215 | 43 | 0.07 | 0.06–0.08 | -- | -- | -- | -- | 802 | 160 | 0.07 | 0.06–0.07 |
| Non-Malignant | 99 | 20 | 0.03 | 0.03–0.04 | 85 | 17 | 0.03 | 0.03–0.04 | -- | -- | -- | -- | 407 | 81 | 0.03 | 0.03–0.04 |
| Tumors of Sellar Region | 11,235 | 2,247 | 4.77 | 4.68–4.86 | 10,015 | 2,003 | 4.71 | 4.61–4.80 | 370 | 74 | 3.32 | 2.95–3.71 | 59,849 | 11,970 | 4.20 | 4.17–4.24 |
| Tumors of the Pituitary | 10,775 | 2,155 | 4.60 | 4.51–4.69 | 9,593 | 1,919 | 4.53 | 4.44–4.63 | 357 | 71 | 3.24 | 2.88–3.63 | 57,245 | 11,449 | 4.01 | 3.98–4.04 |
| Malignant | 28 | 6 | 0.01 | 0.01–0.02 | 22 | 4 | 0.01 | 0.01–0.02 | -- | -- | -- | -- | 129 | 26 | 0.01 | 0.01-0.01 |
| Non-Malignant | 10,747 | 2,149 | 4.58 | 4.49–4.68 | 9,571 | 1,914 | 4.52 | 4.42–4.62 | 356 | 71 | 3.23 | 2.87–3.62 | 57,116 | 11,423 | 4.00 | 3.97–4.03 |
| Craniopharyngioma | 460 | 92 | 0.17 | 0.16–0.19 | 422 | 84 | 0.18 | 0.16–0.20 | -- | -- | -- | -- | 2,604 | 521 | 0.19 | 0.19–0.20 |
| Unclassified Tumors | 2,379 | 476 | 1.19 | 1.13–1.24 | 2,172 | 434 | 1.19 | 1.14–1.25 | 67 | 13 | 0.70 | 0.52–0.92 | 18,177 | 3,635 | 1.21 | 1.19–1.22 |
| Hemangioma | 807 | 161 | 0.34 | 0.32–0.37 | 736 | 147 | 0.35 | 0.32–0.38 | 22 | 4 | 0.19 | 0.11–0.30 | 5,175 | 1,035 | 0.37 | 0.36–0.38 |
| Neoplasm Unspecified | 1,548 | 310 | 0.83 | 0.78–0.87 | 1,414 | 283 | 0.83 | 0.79–0.88 | 45 | 9 | 0.51 | 0.35–0.71 | 12,870 | 2,574 | 0.83 | 0.81–0.84 |
| Malignant | 600 | 120 | 0.36 | 0.33–0.39 | 552 | 110 | 0.36 | 0.33–0.39 | -- | -- | -- | -- | 6,034 | 1,207 | 0.37 | 0.36–0.38 |
| Non-Malignant | 948 | 190 | 0.47 | 0.44–0.50 | 862 | 172 | 0.47 | 0.44–0.51 | -- | -- | -- | -- | 6,836 | 1,367 | 0.46 | 0.45–0.47 |
| All Other | 24 | 5 | 0.01 | 0.01–0.02 | 22 | 4 | 0.01 | 0.01–0.02 | -- | -- | -- | -- | 132 | 26 | 0.01 | 0.01-0.01 |
| TOTAL d | 44,689 | 8,938 | 21.28 | 21.07–21.49 | 40,554 | 8,111 | 21.27 | 21.05–21.49 | 1,257 | 251 | 13.04 | 12.25–13.87 | 361,051 | 72,210 | 23.84 | 23.76–23.92 |
| Malignant | 12,451 | 2,490 | 5.66 | 5.56–5.77 | 11,507 | 2,301 | 5.78 | 5.67–5.90 | 287 | 57 | 2.64 | 2.30–3.01 | 110,118 | 22,024 | 7.33 | 7.29–7.38 |
| Non-Malignant | 32,238 | 6,448 | 15.61 | 15.43–15.80 | 29,047 | 5,809 | 15.49 | 15.30–15.68 | 970 | 194 | 10.40 | 9.69–11.15 | 250,933 | 50,187 | 16.51 | 16.44–16.58 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. Hispanic ethnicity is not mutually exclusive of race; Classified using the North American Association of Central Cancer Registries Hispanic Identification Algorithm, version 2 (NHIA v2).
d. Refers to all brain tumors including histologies not presented in this table.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
The overall incidence rate for primary brain and other CNS tumors was 21.28 per 100,000 population among Hispanics and 23.84 per 100,000 population among non-Hispanics.
Tumors of the pituitary, lymphoma, and other hematopoietic neoplasms were the only histologies that were higher in Hispanics than in non-Hispanics.
While there are multiple histologies, discussed above, where significant differences in incidence were observed by race and/or ethnicity, in most cases the actual difference in incidence rates is small and may not be biologically significant.
Incidence and Distribution of Primary Brain and Other CNS Tumors in Childhood and Adolescence by Site, Histology, Sex, and Age
Distribution of tumors by site and histology in children and adolescents (age 0–19 years)
The distribution of brain and other CNS tumors for children and adolescents age 0–19 years by site is shown in Figure 17A. Brain and other CNS tumors are the most common form of solid tumors in children50 and account for the majority of cancer mortality in this age group.51 About 6.1% of the reported brain and other CNS tumors during 2012–2016 occurred in children and adolescents age 0–19 years.
The largest percentages of tumors in childhood and adolescence were located in the pituitary and craniopharyngeal duct (16.5%).
Frontal, temporal, parietal, and occipital lobes of the brain accounted for 5.9%, 6.8%, 2.7%, and 1.2% of all brain and other CNS tumors in childhood and adolescence, respectively.
Cerebrum, ventricle, brain stem, and cerebellum tumors accounted for 5.2%, 5.3%, 10.9%, and 12.9% of all brain and other CNS tumors in childhood and adolescence, respectively.
Tumors of the meninges represented 2.9% of all tumors in childhood and adolescence.
The cranial nerves and the spinal cord and cauda equina accounted for 7.3% and 4.9% of all brain and other CNS tumors in childhood and adolescence, respectively.
Figure 17B presents the most common brain and other CNS histologies in children and adolescents age 0–19 years.
Fig. 17.
Distributiona in Children and Adolescents (Age 0–19 Years) of Primary Brain and CNS Tumors (Five-Year Total = 24,931; Annual Average Cases = 4,986) by A) Site and B) Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
For children and adolescents age 0–19 years, pilocytic astrocytoma, glioma malignant, NOS, and embryonal tumors accounted for 15.0%, 7.6%, and 11.5%, respectively.
Tumors of the pituitary were the most common non-malignant histology, and accounted for 13.0% of all tumors in this age group.
Gliomas accounted for approximately 45.7% of tumors in children and adolescents age 0–19 years.
Medulloblastoma accounted for 64.9% of all embryonal tumors in this age group.
Distribution of tumors by site and histology in children (age 0–14 years)
The distribution of brain and other CNS tumors for children age 0–14 years by site is shown in Figure 18A. Approximately 4.3% of all reported tumors occurred in children age 0–14 years.
Fig. 18.
Distributiona in Children (Age 0–14 Years) of Primary Brain and Other CNS Tumors (Five-Year Total = 17,540; Annual Average Cases = 3,508) by A) Site and B) Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Tumors of cerebellum (15.2%) comprised the largest proportion of tumors followed by the other brain (15.0%) and brain stem (13.3%).
Figure 18B presents the most common brain and other CNS histologies in children age 0–14 years.
For children age 0–14 years, pilocytic astrocytoma, glioma malignant, NOS, and embryonal tumors accounted for 17.8%, 14.0%, and 13.1%, respectively.
Gliomas accounted for approximately 51.6% of tumors in children age 0–14 years of embryonal tumors, medulloblastoma, ATRT, and PNET accounted for 64.1%, 15.9%, and 10.4%, respectively.
Distribution of tumors by site and histology in adolescents (age 15–19 years)
The distribution of these tumors by site is presented in Figure 19A. About 1.8% of all brain and other CNS tumors occurred in adolescents age 15–19 years for a total of 7,391 tumors diagnosed between 2012 and 2016 (Table 3).
Fig. 19.
Distributiona in Adolescents (Age 15–19 Years) of Primary Brain and Other CNS Tumors (Five-Year Total = 7,391; Annual Average Cases = 1,478) by A) Site and B) Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
33.5% of these tumors were diagnosed in the pituitary and craniopharyngeal duct.
The frontal lobe, temporal lobe, occipital lobe, and parietal lobe accounted for 19.9% of tumors in this age group.
The distribution of brain and other CNS tumors in adolescents age 15–19 years by histology is presented in Figure 19B.
The most common histology in adolescents was tumors of the pituitary (30.8%).
Gliomas accounted for approximately 31.5% of tumors in adolescents. Of these gliomas, the histology pilocytic astrocytoma accounted for 8.3% of all tumors in this age group.
Incidence rates by histology, histology groupings, and sex in children and adolescents (age 0–19 years)
The incidence rates of the most common brain and other CNS tumors in children and adolescents by major histology grouping, histology, and sex are shown in Table 14.
Table 14.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for children and adolescents (age 0–19 years), brain and other central nervous system tumors by major histology grouping, histology, and sex, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | Total | Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 15,778 | 3,156 | 3.84 | 3.78–3.90 | 8,535 | 1,707 | 4.07 | 3.98–4.15 | 7,243 | 1,449 | 3.61 | 3.52–3.69 |
| Pilocytic Astrocytoma | 3,730 | 746 | 0.91 | 0.88–0.94 | 1,948 | 390 | 0.93 | 0.89–0.97 | 1782 | 356 | 0.89 | 0.85–0.93 |
| Diffuse Astrocytoma | 968 | 194 | 0.24 | 0.22–0.25 | 508 | 102 | 0.24 | 0.22–0.26 | 460 | 92 | 0.23 | 0.21–0.25 |
| Anaplastic Astrocytoma | 406 | 81 | 0.10 | 0.09–0.11 | 229 | 46 | 0.11 | 0.10–0.12 | 177 | 35 | 0.09 | 0.08–0.10 |
| Unique Astrocytoma Variants | 519 | 104 | 0.13 | 0.12–0.14 | 292 | 58 | 0.14 | 0.12–0.16 | 227 | 45 | 0.11 | 0.10–0.13 |
| Malignant | 243 | 49 | 0.06 | 0.05–0.07 | 139 | 28 | 0.07 | 0.06–0.08 | 104 | 21 | 0.05 | 0.04–0.06 |
| Non-Malignant | 276 | 55 | 0.07 | 0.06–0.08 | 153 | 31 | 0.07 | 0.06–0.09 | 123 | 25 | 0.06 | 0.05–0.07 |
| Glioblastoma | 744 | 149 | 0.18 | 0.17–0.19 | 410 | 82 | 0.19 | 0.18–0.21 | 334 | 67 | 0.17 | 0.15–0.18 |
| Oligodendroglioma | 195 | 39 | 0.05 | 0.04–0.05 | 98 | 20 | 0.05 | 0.04–0.06 | 97 | 19 | 0.05 | 0.04–0.06 |
| Anaplastic Oligodendroglioma | 27 | 5 | 0.01 | 0.00–0.01 | -- | -- | -- | -- | -- | -- | -- | -- |
| Oligoastrocytic Tumors | 84 | 17 | 0.02 | 0.02–0.03 | 44 | 9 | 0.02 | 0.02–0.03 | 40 | 8 | 0.02 | 0.01–0.03 |
| Ependymal Tumors | 1,173 | 235 | 0.29 | 0.27–0.30 | 650 | 130 | 0.31 | 0.29–0.33 | 523 | 105 | 0.26 | 0.24–0.28 |
| Malignant | 985 | 197 | 0.24 | 0.22–0.26 | 548 | 110 | 0.26 | 0.24–0.28 | 437 | 87 | 0.22 | 0.20–0.24 |
| Non-Malignant | 188 | 38 | 0.05 | 0.04–0.05 | 102 | 20 | 0.05 | 0.04–0.06 | 86 | 17 | 0.04 | 0.03–0.05 |
| Glioma Malignant, NOS | 2,870 | 574 | 0.70 | 0.67–0.73 | 1,460 | 292 | 0.70 | 0.66–0.73 | 1,410 | 282 | 0.70 | 0.67–0.74 |
| Choroid Plexus Tumors | 409 | 82 | 0.10 | 0.09–0.11 | 230 | 46 | 0.11 | 0.10–0.12 | 179 | 36 | 0.09 | 0.08–0.10 |
| Malignant | 105 | 21 | 0.03 | 0.02–0.03 | 53 | 11 | 0.03 | 0.02–0.03 | 52 | 10 | 0.03 | 0.02–0.03 |
| Non-Malignant | 304 | 61 | 0.07 | 0.07–0.08 | 177 | 35 | 0.08 | 0.07–0.10 | 127 | 25 | 0.06 | 0.05–0.08 |
| Other Neuroepithelial Tumors | 38 | 8 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Neuronal and Mixed Neuronal Glial Tumors | 1,889 | 378 | 0.46 | 0.44–0.48 | 1,041 | 208 | 0.49 | 0.47–0.53 | 848 | 170 | 0.42 | 0.39–0.45 |
| Malignant | 100 | 20 | 0.02 | 0.02–0.03 | 59 | 12 | 0.03 | 0.02–0.04 | 41 | 8 | 0.02 | 0.01–0.03 |
| Non-Malignant | 1,789 | 358 | 0.43 | 0.41–0.46 | 982 | 196 | 0.47 | 0.44–0.50 | 807 | 161 | 0.40 | 0.37–0.43 |
| Tumors of the Pineal Region | 218 | 44 | 0.05 | 0.05–0.06 | 111 | 22 | 0.05 | 0.04–0.06 | 107 | 21 | 0.05 | 0.04–0.06 |
| Malignant | 180 | 36 | 0.04 | 0.04–0.05 | -- | -- | -- | -- | 81 | 16 | 0.04 | 0.03–0.05 |
| Non-Malignant | 38 | 8 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- |
| Embryonal Tumors | 2,508 | 502 | 0.61 | 0.59–0.64 | 1,487 | 297 | 0.71 | 0.67–0.75 | 1,021 | 204 | 0.51 | 0.48–0.54 |
| Medulloblastoma | 1,632 | 326 | 0.40 | 0.38–0.42 | 1,047 | 209 | 0.50 | 0.47–0.53 | 585 | 117 | 0.29 | 0.27–0.32 |
| Primitive Neuroectodermal Tumors | 270 | 54 | 0.07 | 0.06–0.07 | 139 | 28 | 0.07 | 0.06–0.08 | 131 | 26 | 0.07 | 0.05–0.08 |
| Atypical Teratoid/Rhabdoid Tumor | 370 | 74 | 0.09 | 0.08–0.10 | 180 | 36 | 0.09 | 0.07–0.10 | 190 | 38 | 0.09 | 0.08–0.11 |
| Other Embryonal Histologies c | 236 | 47 | 0.06 | 0.05–0.07 | 121 | 24 | 0.06 | 0.05–0.07 | 115 | 23 | 0.06 | 0.05–0.07 |
| Tumors of Cranial and Spinal Nerves | 1,336 | 267 | 0.32 | 0.31–0.34 | 716 | 143 | 0.34 | 0.32–0.37 | 620 | 124 | 0.31 | 0.28–0.33 |
| Nerve Sheath Tumors | 1,333 | 267 | 0.32 | 0.31–0.34 | 713 | 143 | 0.34 | 0.31–0.36 | 620 | 124 | 0.31 | 0.28–0.33 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Meninges | 1,132 | 226 | 0.27 | 0.26–0.29 | 538 | 108 | 0.25 | 0.23–0.28 | 594 | 119 | 0.29 | 0.27–0.32 |
| Meningioma | 653 | 131 | 0.16 | 0.15–0.17 | 299 | 60 | 0.14 | 0.13–0.16 | 354 | 71 | 0.17 | 0.16–0.19 |
| Malignant | 37 | 7 | 0.01 | 0.01-0.01 | 16 | 3 | 0.01 | 0.00–0.01 | 21 | 4 | 0.01 | 0.01–0.02 |
| Non-Malignant | 616 | 123 | 0.15 | 0.14–0.16 | 283 | 57 | 0.13 | 0.12–0.15 | 333 | 67 | 0.16 | 0.15–0.18 |
| Mesenchymal Tumors | 254 | 51 | 0.06 | 0.05–0.07 | 132 | 26 | 0.06 | 0.05–0.07 | 122 | 24 | 0.06 | 0.05–0.07 |
| Primary Melanocytic Lesions | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neoplasms Related to the Meninges | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Lymphoma and Hematopoietic Neoplasms | 131 | 26 | 0.03 | 0.03–0.04 | 82 | 16 | 0.04 | 0.03–0.05 | 49 | 10 | 0.02 | 0.02–0.03 |
| Lymphoma | 64 | 13 | 0.02 | 0.01–0.02 | 42 | 8 | 0.02 | 0.01–0.03 | 22 | 4 | 0.01 | 0.01–0.02 |
| Other Hematopoietic Neoplasms | 67 | 13 | 0.02 | 0.01–0.02 | 40 | 8 | 0.02 | 0.01–0.03 | 27 | 5 | 0.01 | 0.01–0.02 |
| Germ Cell Tumors and Cysts | 951 | 190 | 0.23 | 0.22–0.25 | 651 | 130 | 0.31 | 0.29–0.33 | 300 | 60 | 0.15 | 0.13–0.17 |
| Germ cell tumors, cysts, and heterotopias | 951 | 190 | 0.23 | 0.22–0.25 | 651 | 130 | 0.31 | 0.29–0.33 | 300 | 60 | 0.15 | 0.13–0.17 |
| Malignant | 733 | 147 | 0.18 | 0.17–0.19 | 531 | 106 | 0.25 | 0.23–0.27 | 202 | 40 | 0.10 | 0.09–0.12 |
| Non-Malignant | 218 | 44 | 0.05 | 0.05–0.06 | 120 | 24 | 0.06 | 0.05–0.07 | 98 | 20 | 0.05 | 0.04–0.06 |
| Tumors of Sellar Region | 4,080 | 816 | 0.98 | 0.95–1.01 | 1,301 | 260 | 0.62 | 0.58–0.65 | 2,779 | 556 | 1.37 | 1.32–1.42 |
| Tumors of the Pituitary | 3,232 | 646 | 0.78 | 0.75–0.80 | 856 | 171 | 0.40 | 0.38–0.43 | 2,376 | 475 | 1.17 | 1.12–1.22 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Craniopharyngioma | 848 | 170 | 0.21 | 0.19–0.22 | 445 | 89 | 0.21 | 0.19–0.23 | 403 | 81 | 0.20 | 0.18–0.22 |
| Unclassified Tumors | 1,523 | 305 | 0.37 | 0.35–0.39 | 753 | 151 | 0.36 | 0.33–0.38 | 770 | 154 | 0.38 | 0.36–0.41 |
| Hemangioma | 601 | 120 | 0.15 | 0.13–0.16 | 302 | 60 | 0.14 | 0.13–0.16 | 299 | 60 | 0.15 | 0.13–0.17 |
| Neoplasm Unspecified | 886 | 177 | 0.22 | 0.20–0.23 | 432 | 86 | 0.21 | 0.19–0.23 | 454 | 91 | 0.23 | 0.21–0.25 |
| Malignant | 225 | 45 | 0.05 | 0.05–0.06 | 116 | 23 | 0.06 | 0.05–0.07 | 109 | 22 | 0.05 | 0.04–0.07 |
| Non-Malignant | 661 | 132 | 0.16 | 0.15–0.17 | 316 | 63 | 0.15 | 0.13–0.17 | 345 | 69 | 0.17 | 0.15–0.19 |
| All Other | 36 | 7 | 0.01 | 0.01-0.01 | 19 | 4 | 0.01 | 0.01-0.01 | 17 | 3 | 0.01 | 0.00–0.01 |
| TOTAL d | 24,931 | 4,986 | 6.06 | 5.98–6.13 | 12,576 | 2,515 | 5.98 | 5.88–6.09 | 12,355 | 2,471 | 6.13 | 6.02–6.24 |
| Malignant | 14,421 | 2,884 | 3.51 | 3.45–3.57 | 7,922 | 1,584 | 3.77 | 3.69–3.86 | 6,499 | 1,300 | 3.24 | 3.16–3.32 |
| Non-Malignant | 10,510 | 2,102 | 2.54 | 2.50–2.59 | 4,654 | 931 | 2.21 | 2.15–2.27 | 5,856 | 1,171 | 2.89 | 2.82–2.97 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. ICD-O-3 histology and behavior codes: 8963/3, 9364/3, 9480/3, 9490/0, 9490/3, 9500/3, 9501/3, and 9502/3.
d. Refers to all brain tumors including histologies not presented in this table.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
Average annual incidence rates were highest for tumors of neuroepithelial tissue (3.84 per 100,000 population). Among these tumors, the most common histologies were pilocytic astrocytoma (0.91 per 100,000 population), glioma malignant, NOS (0.70 per 100,000 population), and embryonal tumors (0.61 per 100,000 population).
There were notable differences in incidence rates between males and females for ependymal tumors, embryonal tumors, germ cell tumors, and tumors of the pituitary.
Incidence rates by histology and race in children and adolescents (age 0–19 years)
Table 15 shows incidence rates for brain and other CNS tumors by histology and race for children and adolescents age 0–19 years.
Table 15.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for children and adolescents (age 0–19 years), brain and other central nervous system tumors by major histology grouping, histology, and racec, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | White | Black | American Indian/Alaska Native | Asian/Pacific Islander | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 12,505 | 2,501 | 4.04 | 3.97–4.11 | 2,021 | 404 | 2.95 | 2.82–3.08 | 142 | 28 | 1.85 | 1.56–2.18 | 750 | 150 | 3.01 | 2.80–3.23 |
| Pilocytic Astrocytoma | 3,008 | 602 | 0.97 | 0.94–1.01 | 451 | 90 | 0.66 | 0.60–0.72 | 30 | 6 | 0.39 | 0.26–0.55 | 157 | 31 | 0.63 | 0.53–0.74 |
| Diffuse Astrocytoma | 779 | 156 | 0.25 | 0.23–0.27 | 113 | 23 | 0.17 | 0.14–0.20 | -- | -- | -- | -- | 45 | 9 | 0.18 | 0.13–0.24 |
| Anaplastic Astrocytoma | 318 | 64 | 0.10 | 0.09–0.11 | 55 | 11 | 0.08 | 0.06–0.11 | -- | -- | -- | -- | 23 | 5 | 0.09 | 0.06–0.14 |
| Unique Astrocytoma Variants | 390 | 78 | 0.13 | 0.11–0.14 | 82 | 16 | 0.12 | 0.10–0.15 | -- | -- | -- | -- | 32 | 6 | 0.13 | 0.09–0.18 |
| Malignant | 194 | 39 | 0.06 | 0.05–0.07 | 25 | 5 | 0.04 | 0.02–0.05 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 196 | 39 | 0.06 | 0.05–0.07 | 57 | 11 | 0.08 | 0.06–0.11 | -- | -- | -- | -- | -- | -- | -- | -- |
| Glioblastoma | 580 | 116 | 0.19 | 0.17–0.20 | 99 | 20 | 0.14 | 0.12–0.18 | -- | -- | -- | -- | 39 | 8 | 0.16 | 0.11–0.22 |
| Oligodendroglioma | 151 | 30 | 0.05 | 0.04–0.06 | 26 | 5 | 0.04 | 0.02–0.06 | -- | -- | -- | -- | -- | -- | -- | -- |
| Anaplastic Oligodendroglioma | 19 | 4 | 0.01 | 0.00–0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Oligoastrocytic Tumors | 70 | 14 | 0.02 | 0.02–0.03 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Ependymal Tumors | 945 | 189 | 0.30 | 0.29–0.33 | 135 | 27 | 0.20 | 0.16–0.23 | -- | -- | -- | -- | 53 | 11 | 0.21 | 0.16–0.28 |
| Malignant | 787 | 157 | 0.25 | 0.24–0.27 | 122 | 24 | 0.18 | 0.15–0.21 | -- | -- | -- | -- | 44 | 9 | 0.18 | 0.13–0.24 |
| Non-Malignant | 158 | 32 | 0.05 | 0.04–0.06 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Glioma Malignant, NOS | 2,263 | 453 | 0.73 | 0.70–0.76 | 392 | 78 | 0.57 | 0.52–0.63 | 20 | 4 | 0.26 | 0.16–0.40 | 127 | 25 | 0.51 | 0.42–0.60 |
| Choroid Plexus Tumors | 319 | 64 | 0.10 | 0.09–0.12 | 54 | 11 | 0.08 | 0.06–0.10 | -- | -- | -- | -- | 24 | 5 | 0.10 | 0.06–0.14 |
| Malignant | 78 | 16 | 0.03 | 0.02–0.03 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 241 | 48 | 0.08 | 0.07–0.09 | 39 | 8 | 0.06 | 0.04–0.08 | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neuroepithelial Tumors | 28 | 6 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Malignant | 21 | 4 | 0.01 | 0.00–0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Neuronal and Mixed Neuronal Glial Tumors | 1,512 | 302 | 0.49 | 0.46–0.51 | 243 | 49 | 0.36 | 0.31–0.40 | 16 | 3 | 0.21 | 0.12–0.34 | 82 | 16 | 0.33 | 0.26–0.41 |
| Malignant | 76 | 15 | 0.02 | 0.02–0.03 | 18 | 4 | 0.03 | 0.02–0.04 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 1,436 | 287 | 0.46 | 0.44–0.49 | 225 | 45 | 0.33 | 0.29–0.38 | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of the Pineal Region | 148 | 30 | 0.05 | 0.04–0.06 | 48 | 10 | 0.07 | 0.05–0.09 | -- | -- | -- | -- | -- | -- | -- | -- |
| Malignant | 117 | 23 | 0.04 | 0.03–0.05 | 44 | 9 | 0.06 | 0.05–0.09 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 31 | 6 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Embryonal Tumors | 1,975 | 395 | 0.64 | 0.61–0.67 | 304 | 61 | 0.44 | 0.39–0.49 | 26 | 5 | 0.33 | 0.22–0.49 | 144 | 29 | 0.58 | 0.49–0.68 |
| Medulloblastoma | 1,307 | 261 | 0.42 | 0.40–0.45 | 173 | 35 | 0.25 | 0.22–0.29 | 18 | 4 | 0.23 | 0.14–0.37 | 101 | 20 | 0.40 | 0.33–0.49 |
| Primitive Neuroectodermal Tumors | 207 | 41 | 0.07 | 0.06–0.08 | 43 | 9 | 0.06 | 0.05–0.08 | -- | -- | -- | -- | -- | -- | -- | -- |
| Atypical Teratoid/Rhabdoid Tumor | 275 | 55 | 0.09 | 0.08–0.10 | 59 | 12 | 0.08 | 0.06–0.11 | -- | -- | -- | -- | 25 | 5 | 0.10 | 0.06–0.15 |
| Other Embryonal Histologies d | 186 | 37 | 0.06 | 0.05–0.07 | 29 | 6 | 0.04 | 0.03–0.06 | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Cranial and Spinal Nerves | 1,034 | 207 | 0.33 | 0.31–0.35 | 170 | 34 | 0.25 | 0.21–0.29 | -- | -- | -- | -- | 75 | 15 | 0.30 | 0.24–0.38 |
| Nerve Sheath Tumors | 1,031 | 206 | 0.33 | 0.31–0.35 | 170 | 34 | 0.25 | 0.21–0.29 | -- | -- | -- | -- | 75 | 15 | 0.30 | 0.24–0.38 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 1,020 | 204 | 0.33 | 0.31–0.35 | 166 | 33 | 0.24 | 0.21–0.28 | -- | -- | -- | -- | 75 | 15 | 0.30 | 0.24–0.38 |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Meninges | 901 | 180 | 0.29 | 0.27–0.31 | 146 | 29 | 0.21 | 0.18–0.25 | -- | -- | -- | -- | 51 | 10 | 0.21 | 0.15–0.27 |
| Meningioma | 514 | 103 | 0.16 | 0.15–0.18 | 92 | 18 | 0.13 | 0.11–0.16 | -- | -- | -- | -- | 28 | 6 | 0.11 | 0.08–0.16 |
| Malignant | 30 | 6 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 484 | 97 | 0.15 | 0.14–0.17 | 87 | 17 | 0.13 | 0.10–0.16 | -- | -- | -- | -- | 26 | 5 | 0.11 | 0.07–0.16 |
| Mesenchymal Tumors | 201 | 40 | 0.06 | 0.06–0.07 | 28 | 6 | 0.04 | 0.03–0.06 | -- | -- | -- | -- | 16 | 3 | 0.06 | 0.04–0.10 |
| Primary Melanocytic Lesions | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neoplasms Related to the Meninges | 174 | 35 | 0.06 | 0.05–0.06 | 26 | 5 | 0.04 | 0.02–0.06 | -- | -- | -- | -- | -- | -- | -- | -- |
| Lymphoma and Hematopoietic Neoplasms | 97 | 19 | 0.03 | 0.03–0.04 | -- | -- | -- | -- | -- | -- | -- | -- | 17 | 3 | 0.07 | 0.04–0.11 |
| Lymphoma | 46 | 9 | 0.01 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Hematopoietic Neoplasms | 51 | 10 | 0.02 | 0.01–0.02 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Germ Cell Tumors and Cysts | 739 | 148 | 0.24 | 0.22–0.26 | 93 | 19 | 0.14 | 0.11–0.17 | -- | -- | -- | -- | 88 | 18 | 0.36 | 0.29–0.44 |
| Germ cell tumors, cysts, and heterotopias | 739 | 148 | 0.24 | 0.22–0.26 | 93 | 19 | 0.14 | 0.11–0.17 | -- | -- | -- | -- | 88 | 18 | 0.36 | 0.29–0.44 |
| Malignant | 571 | 114 | 0.18 | 0.17–0.20 | 66 | 13 | 0.10 | 0.08–0.12 | -- | -- | -- | -- | 76 | 15 | 0.31 | 0.24–0.39 |
| Non-Malignant | 168 | 34 | 0.05 | 0.05–0.06 | 27 | 5 | 0.04 | 0.03–0.06 | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Sellar Region | 3,055 | 611 | 0.97 | 0.94–1.01 | 605 | 121 | 0.88 | 0.81–0.96 | 59 | 12 | 0.79 | 0.60–1.02 | 231 | 46 | 0.94 | 0.82–1.07 |
| Tumors of the Pituitary | 2,436 | 487 | 0.77 | 0.74–0.80 | 449 | 90 | 0.65 | 0.59–0.72 | 52 | 10 | 0.70 | 0.52–0.91 | 183 | 37 | 0.74 | 0.64–0.86 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 2,435 | 487 | 0.77 | 0.74–0.80 | 449 | 90 | 0.65 | 0.59–0.72 | 51 | 10 | 0.68 | 0.51–0.90 | 182 | 36 | 0.74 | 0.64–0.86 |
| Craniopharyngioma | 619 | 124 | 0.20 | 0.18–0.22 | 156 | 31 | 0.23 | 0.20–0.27 | -- | -- | -- | -- | 48 | 10 | 0.19 | 0.14–0.26 |
| Unclassified Tumors | 1,200 | 240 | 0.39 | 0.36–0.41 | 184 | 37 | 0.27 | 0.23–0.31 | 24 | 5 | 0.32 | 0.20–0.47 | 71 | 14 | 0.29 | 0.22–0.36 |
| Hemangioma | 497 | 99 | 0.16 | 0.15–0.17 | 54 | 11 | 0.08 | 0.06–0.10 | -- | -- | -- | -- | 28 | 6 | 0.11 | 0.07–0.16 |
| Neoplasm Unspecified | 678 | 136 | 0.22 | 0.20–0.24 | 122 | 24 | 0.18 | 0.15–0.21 | 18 | 4 | 0.24 | 0.14–0.38 | 43 | 9 | 0.17 | 0.13–0.23 |
| Malignant | 162 | 32 | 0.05 | 0.04–0.06 | 37 | 7 | 0.05 | 0.04–0.07 | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | 516 | 103 | 0.17 | 0.15–0.18 | 85 | 17 | 0.12 | 0.10–0.15 | -- | -- | -- | -- | 28 | 6 | 0.11 | 0.08–0.16 |
| All Other | 25 | 5 | 0.01 | 0.01-0.01 | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| TOTAL e | 19,531 | 3,906 | 6.29 | 6.20–6.37 | 3,231 | 646 | 4.71 | 4.55–4.88 | 256 | 51 | 3.37 | 2.97–3.80 | 1,283 | 257 | 5.17 | 4.89–5.46 |
| Malignant | 11,393 | 2,279 | 3.68 | 3.61–3.75 | 1,821 | 364 | 2.66 | 2.54–2.78 | 139 | 28 | 1.81 | 1.52–2.14 | 742 | 148 | 2.98 | 2.77–3.20 |
| Non-Malignant | 8,138 | 1,628 | 2.61 | 2.55–2.66 | 1,410 | 282 | 2.06 | 1.95–2.17 | 117 | 23 | 1.56 | 1.29–1.86 | 541 | 108 | 2.19 | 2.01–2.38 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. Individuals with unknown race were excluded (N = 630).
d. ICD-O-3 histology and behavior codes: 8963/3, 9364/3, 9480/3, 9490/0, 9490/3, 9500/3, 9501/3, and 9502/3.
e. Refers to all brain tumors including histologies not presented in this table.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
Incidence rates were highest among White (6.29 per 100,000 population) compared to Blacks (4.71 per 100,000 population), AIAN (3.37 per 100,000 population), and API (5.17 per 100,000 population).
Incidence rates by histology and hispanic ethnicity in children and adolescents (age 0–19 years)
AAAIR of brain and other CNS tumors for children and adolescents age 0–19 years by Hispanic ethnicity are shown in Table 16.
Table 16.
Five-year total, annual average totala, and average annual age-adjusted incidence ratesb with 95% confidence intervals for children and adolescents (age 0–19 years), brain and other central nervous system tumors by major histology grouping, histology, hispanic ethnicityc, and race, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
| Histology | All Hispanic | White Hispanic | Black Hispanic | All Non-Hispanic | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-year total | Annual average | Rate | 95% CI | 5-year total | Annual average | Rate | 95% CI | 5-year total | Annual average | Rate | 95% CI | 5- year total | Annual average | Rate | 95% CI | |
| Tumors of Neuroepithelial Tissue | 2,942 | 588 | 2.93 | 2.82–3.03 | 2,679 | 536 | 3.02 | 2.91–3.14 | 82 | 16 | 1.35 | 1.07–1.67 | 12,836 | 2,567 | 4.13 | 4.06–4.21 |
| Pilocytic Astrocytoma | 656 | 131 | 0.65 | 0.60–0.70 | 594 | 119 | 0.67 | 0.61–0.72 | 20 | 4 | 0.33 | 0.20–0.51 | 3,074 | 615 | 0.99 | 0.96–1.03 |
| Diffuse Astrocytoma | 131 | 26 | 0.13 | 0.11–0.16 | 119 | 24 | 0.14 | 0.11–0.16 | -- | -- | -- | -- | 837 | 167 | 0.27 | 0.25–0.29 |
| Anaplastic Astrocytoma | 86 | 17 | 0.09 | 0.07–0.11 | 78 | 16 | 0.09 | 0.07–0.11 | -- | -- | -- | -- | 320 | 64 | 0.10 | 0.09–0.11 |
| Unique Astrocytoma Variants | 115 | 23 | 0.12 | 0.10–0.14 | 105 | 21 | 0.12 | 0.10–0.15 | -- | -- | -- | -- | 404 | 81 | 0.13 | 0.12–0.14 |
| Malignant | 57 | 11 | 0.06 | 0.04–0.08 | 54 | 11 | 0.06 | 0.05–0.08 | -- | -- | -- | -- | 186 | 37 | 0.06 | 0.05–0.07 |
| Non-Malignant | 58 | 12 | 0.06 | 0.04–0.07 | 51 | 10 | 0.06 | 0.04–0.08 | -- | -- | -- | -- | 218 | 44 | 0.07 | 0.06–0.08 |
| Glioblastoma | 163 | 33 | 0.17 | 0.14–0.19 | 156 | 31 | 0.18 | 0.15–0.21 | -- | -- | -- | -- | 581 | 116 | 0.19 | 0.17–0.20 |
| Oligodendroglioma | 25 | 5 | 0.03 | 0.02–0.04 | 24 | 5 | 0.03 | 0.02–0.04 | -- | -- | -- | -- | 170 | 34 | 0.05 | 0.05–0.06 |
| Anaplastic Oligodendroglioma | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 23 | 5 | 0.01 | 0.00–0.01 |
| Oligoastrocytic Tumors | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 71 | 14 | 0.02 | 0.02–0.03 |
| Ependymal Tumors | 272 | 54 | 0.27 | 0.24–0.30 | 249 | 50 | 0.28 | 0.25–0.32 | -- | -- | -- | -- | 901 | 180 | 0.29 | 0.27–0.31 |
| Malignant | 240 | 48 | 0.24 | 0.21–0.27 | 223 | 45 | 0.25 | 0.22–0.28 | -- | -- | -- | -- | 745 | 149 | 0.24 | 0.22–0.26 |
| Non-Malignant | 32 | 6 | 0.03 | 0.02–0.05 | 26 | 5 | 0.03 | 0.02–0.04 | -- | -- | -- | -- | 156 | 31 | 0.05 | 0.04–0.06 |
| Glioma Malignant, NOS | 489 | 98 | 0.48 | 0.44–0.53 | 437 | 87 | 0.49 | 0.45–0.54 | 18 | 4 | 0.29 | 0.17–0.46 | 2,381 | 476 | 0.77 | 0.74–0.80 |
| Choroid Plexus Tumors | 90 | 18 | 0.09 | 0.07–0.11 | 80 | 16 | 0.09 | 0.07–0.11 | -- | -- | -- | -- | 319 | 64 | 0.10 | 0.09–0.12 |
| Malignant | 20 | 4 | 0.02 | 0.01–0.03 | 18 | 4 | 0.02 | 0.01–0.03 | -- | -- | -- | -- | 85 | 17 | 0.03 | 0.02–0.03 |
| Non-Malignant | 70 | 14 | 0.07 | 0.05–0.09 | 62 | 12 | 0.07 | 0.05–0.09 | -- | -- | -- | -- | 234 | 47 | 0.08 | 0.07–0.09 |
| Other Neuroepithelial Tumors | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 30 | 6 | 0.01 | 0.01-0.01 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 24 | 5 | 0.01 | 0.00–0.01 |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Neuronal and Mixed Neuronal Glial Tumors | 298 | 60 | 0.30 | 0.27–0.34 | 269 | 54 | 0.31 | 0.27–0.35 | -- | -- | -- | -- | 1,591 | 318 | 0.51 | 0.48–0.53 |
| Malignant | 22 | 4 | 0.02 | 0.01–0.03 | 21 | 4 | 0.02 | 0.01–0.04 | -- | -- | -- | -- | 78 | 16 | 0.02 | 0.02–0.03 |
| Non-Malignant | 276 | 55 | 0.28 | 0.25–0.32 | 248 | 50 | 0.29 | 0.25–0.32 | -- | -- | -- | -- | 1,513 | 303 | 0.48 | 0.46–0.51 |
| Tumors of the Pineal Region | 44 | 9 | 0.04 | 0.03–0.06 | 37 | 7 | 0.04 | 0.03–0.06 | -- | -- | -- | -- | 174 | 35 | 0.06 | 0.05–0.06 |
| Malignant | 37 | 7 | 0.04 | 0.03–0.05 | 32 | 6 | 0.04 | 0.02–0.05 | -- | -- | -- | -- | 143 | 29 | 0.05 | 0.04–0.05 |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 31 | 6 | 0.01 | 0.01-0.01 |
| Embryonal Tumors | 548 | 110 | 0.53 | 0.49–0.58 | 507 | 101 | 0.56 | 0.51–0.61 | -- | -- | -- | -- | 1,960 | 392 | 0.64 | 0.61–0.67 |
| Medulloblastoma | 347 | 69 | 0.34 | 0.31–0.38 | 323 | 65 | 0.36 | 0.32–0.40 | -- | -- | -- | -- | 1,285 | 257 | 0.42 | 0.39–0.44 |
| Primitive Neuroectodermal Tumors | 63 | 13 | 0.06 | 0.05–0.08 | 57 | 11 | 0.06 | 0.05–0.08 | -- | -- | -- | -- | 207 | 41 | 0.07 | 0.06–0.08 |
| Atypical Teratoid/Rhabdoid Tumor | 91 | 18 | 0.09 | 0.07–0.11 | 85 | 17 | 0.09 | 0.07–0.11 | -- | -- | -- | -- | 279 | 56 | 0.09 | 0.08–0.10 |
| Other Embryonal Histologies d | 47 | 9 | 0.05 | 0.03–0.06 | 42 | 8 | 0.05 | 0.03–0.06 | -- | -- | -- | -- | 189 | 38 | 0.06 | 0.05–0.07 |
| Tumors of Cranial and Spinal Nerves | 238 | 48 | 0.24 | 0.21–0.27 | 207 | 41 | 0.24 | 0.21–0.27 | -- | -- | -- | -- | 1,098 | 220 | 0.35 | 0.33–0.37 |
| Nerve Sheath Tumors | 237 | 47 | 0.24 | 0.21–0.27 | 206 | 41 | 0.24 | 0.21–0.27 | -- | -- | -- | -- | 1,096 | 219 | 0.35 | 0.33–0.37 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Meninges | 227 | 45 | 0.23 | 0.21–0.27 | 205 | 41 | 0.24 | 0.21–0.27 | -- | -- | -- | -- | 905 | 181 | 0.29 | 0.27–0.30 |
| Meningioma | 127 | 25 | 0.13 | 0.11–0.16 | 113 | 23 | 0.13 | 0.11–0.16 | -- | -- | -- | -- | 526 | 105 | 0.17 | 0.15–0.18 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 28 | 6 | 0.01 | 0.01-0.01 |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 498 | 100 | 0.16 | 0.14–0.17 |
| Mesenchymal Tumors | 52 | 10 | 0.05 | 0.04–0.07 | 46 | 9 | 0.05 | 0.04–0.07 | -- | -- | -- | -- | 202 | 40 | 0.07 | 0.06–0.07 |
| Primary Melanocytic Lesions | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neoplasms Related to the Meninges | 46 | 9 | 0.05 | 0.04–0.06 | 44 | 9 | 0.05 | 0.04–0.07 | -- | -- | -- | -- | 167 | 33 | 0.05 | 0.04–0.06 |
| Lymphoma and Hematopoietic Neoplasms | 28 | 6 | 0.03 | 0.02–0.04 | 24 | 5 | 0.03 | 0.02–0.04 | -- | -- | -- | -- | 103 | 21 | 0.03 | 0.03–0.04 |
| Lymphoma | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 50 | 10 | 0.02 | 0.01–0.02 |
| Other Hemopoietic Neoplasms | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 53 | 11 | 0.02 | 0.01–0.02 |
| Germ Cell Tumors and Cysts | 234 | 47 | 0.24 | 0.21–0.27 | 215 | 43 | 0.25 | 0.22–0.28 | -- | -- | -- | -- | 717 | 143 | 0.23 | 0.21–0.25 |
| Germ Cell Tumors, Cysts and Heterotopias | 234 | 47 | 0.24 | 0.21–0.27 | 215 | 43 | 0.25 | 0.22–0.28 | -- | -- | -- | -- | 717 | 143 | 0.23 | 0.21–0.25 |
| Malignant | 184 | 37 | 0.19 | 0.16–0.22 | 170 | 34 | 0.20 | 0.17–0.23 | -- | -- | -- | -- | 549 | 110 | 0.17 | 0.16–0.19 |
| Non-Malignant | 50 | 10 | 0.05 | 0.04–0.06 | 45 | 9 | 0.05 | 0.04–0.07 | -- | -- | -- | -- | 168 | 34 | 0.05 | 0.05–0.06 |
| Tumors of Sellar Region | 1,100 | 220 | 1.16 | 1.09–1.23 | 971 | 194 | 1.15 | 1.08–1.22 | 34 | 7 | 0.61 | 0.42–0.85 | 2,980 | 596 | 0.93 | 0.90–0.97 |
| Tumors of the Pituitary | 908 | 182 | 0.96 | 0.90–1.03 | 792 | 158 | 0.94 | 0.88–1.01 | 27 | 5 | 0.49 | 0.32–0.71 | 2,324 | 465 | 0.72 | 0.69–0.75 |
| Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Non-Malignant | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Craniopharyngioma | 192 | 38 | 0.19 | 0.17–0.22 | 179 | 36 | 0.20 | 0.18–0.24 | -- | -- | -- | -- | 656 | 131 | 0.21 | 0.20–0.23 |
| Unclassified Tumors | 310 | 62 | 0.32 | 0.28–0.35 | 271 | 54 | 0.31 | 0.28–0.35 | -- | -- | -- | -- | 1,213 | 243 | 0.39 | 0.37–0.41 |
| Hemangioma | 121 | 24 | 0.12 | 0.10–0.15 | 110 | 22 | 0.13 | 0.10–0.15 | -- | -- | -- | -- | 480 | 96 | 0.15 | 0.14–0.17 |
| Neoplasm Unspecified | 182 | 36 | 0.19 | 0.16–0.21 | 154 | 31 | 0.18 | 0.15–0.21 | -- | -- | -- | -- | 704 | 141 | 0.23 | 0.21–0.24 |
| Malignant | 46 | 9 | 0.05 | 0.03–0.06 | 38 | 8 | 0.04 | 0.03–0.06 | -- | -- | -- | -- | 179 | 36 | 0.06 | 0.05–0.07 |
| Non-Malignant | 136 | 27 | 0.14 | 0.12–0.17 | 116 | 23 | 0.13 | 0.11–0.16 | -- | -- | -- | -- | 525 | 105 | 0.17 | 0.15–0.18 |
| All Other | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 29 | 6 | 0.01 | 0.01-0.01 |
| TOTAL e | 5,079 | 1,016 | 5.14 | 5.00–5.29 | 4,572 | 914 | 5.23 | 5.08–5.39 | 145 | 29 | 2.45 | 2.06–2.88 | 19,852 | 3,970 | 6.35 | 6.26–6.44 |
| Malignant | 2,796 | 559 | 2.78 | 2.68–2.89 | 2,556 | 511 | 2.88 | 2.77–3.00 | 75 | 15 | 1.23 | 0.97–1.55 | 11,625 | 2,325 | 3.75 | 3.68–3.81 |
| Non-Malignant | 2,283 | 457 | 2.36 | 2.26–2.46 | 2,016 | 403 | 2.35 | 2.25–2.46 | 70 | 14 | 1.21 | 0.94–1.53 | 8,227 | 1,645 | 2.60 | 2.55–2.66 |
a. Annual average cases are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. Hispanic ethnicity is not mutually exclusive of race; Classified using the North American Association of Central Cancer Registries Hispanic Identification Algorithm, version 2 (NHIA v2).
d. ICD-O-3 histology and behavior codes: 8963/3, 9364/3, 9480/3, 9490/0, 9490/3, 9500/3, 9501/3, and 9502/3.
e. Refers to all brain tumors including histologies not presented in this table.
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program; CI, Confidence Interval; NOS, Not otherwise specified
Incidence rates for non-Hispanics (6.35 per 100,000 population; 19,852 total tumors) were higher than those for Hispanics (5.14 per 100,000 population; 5,079 total tumors).
The largest differences between non-Hispanics and Hispanics were in incidence rates of tumors of neuroepithelial tissue and tumors of cranial and spinal nerves.
Incidence of most histologic types was higher among non-Hispanics than Hispanics, with the exception of tumors of the pituitary where incidence was 0.96 per 100,000 in Hispanics and 0.72 per 100,000 in non-Hispanics.
Incidence rates by age and histology in children and adolescents (age 0–19 years)
The detailed AAAIR for brain and other CNS tumors by histology for, children and adolescents age 0–19 years overall, and age-groups 0–4 years, 5–9 years, 10–14 years, and 15–19 years are shown in Table 6.
Overall, incidence rates for age-groups 0–4 years (6.22 per 100,000 population) and 15–19 years (6.98 per 100,000 population) exceeded those observed in age-groups 5–9 years (5.38 per 100,000 population) and 10–14 years (5.65 per 100,000 population).
Individual histology distributions varied substantially within these age-groups.
Incidence rates of pilocytic astrocytoma, glioma malignant, NOS, ependymal tumors, choroid plexus tumors, and embryonal tumors decreased with increasing age.
Incidence rates by histology defined by ICCC in children and adolescents (age 0–19 years)
Supplementary Table 10 presents the CBTRUS brain and other CNS tumor data for children and adolescents used for this report according to the ICCC grouping system for pediatric cancers (See Supplementary Table 1 for more additional information on the ICCC classification scheme).15
Estimated Numbers of Expected Cases, Mortality Rates, and Relative Survival
Estimated numbers of expected cases of all primary brain and other CNS tumors by state
Overall total rates presented are based on total malignant and non-malignant incidence, and presented stratified rates may not add up to these totals. Estimated numbers of cases are highly dependent on input data. Different patterns of incidence within strata can substantively affect the projected estimates, and strata-specific estimates may not equal the total estimate presented. Caution should be used when utilizing these estimates.
The total number of new cases of all primary brain and other CNS tumors for all 50 states and the District of Columbia in 2019 is estimated to be 86,010, with 25,510 malignant and 60,490 non-malignant cases (Table 17).
For 2020, the estimate is 87,240 new cases of all primary brain and other CNS tumors of which 25,800 and 61,430 are expected to be malignant and non-malignant, respectively.
Table 17.
Estimated number of casesa,b of brain and other central nervous system tumors overall and by behavior by state, 2019, 2020
| State | 2019 Estimated Cases | 2020 Estimated Cases | ||||
|---|---|---|---|---|---|---|
| All | Malignant | Non-Malignant | All | Malignant | Non-Malignant | |
| Alabama | 1,050 | 390 | 660 | 1,070 | 400 | 680 |
| Alaska | 190 | 60 | 130 | 200 | 60 | 130 |
| Arizona | 1,640 | 570 | 1,070 | 1,660 | 580 | 1,080 |
| Arkansas | 770 | 280 | 500 | 790 | 280 | 500 |
| California | 9,790 | 2,800 | 6,980 | 10,000 | 2,840 | 7,160 |
| Colorado | 1,650 | 430 | 1,230 | 1,690 | 440 | 1,250 |
| Connecticut | 1,000 | 310 | 680 | 1,020 | 310 | 700 |
| Delaware | 230 | 80 | 140 | 230 | 80 | 150 |
| District of Columbia | 190 | -- | -- | 200 | -- | -- |
| Florida | 6,430 | 17,60 | 4,670 | 6,540 | 1,780 | 4,760 |
| Georgia | 3,290 | 760 | 2,530 | 3,440 | 780 | 2,670 |
| Hawaii | 320 | 80 | 240 | 320 | 80 | 240 |
| Idaho | 450 | 150 | 310 | 470 | 150 | 320 |
| Illinois | 3,720 | 1,020 | 2,700 | 3,800 | 1,030 | 2,760 |
| Indiana | 1,720 | 550 | 1,170 | 1,750 | 560 | 1,190 |
| Iowa | 1,000 | 280 | 720 | 1,030 | 280 | 740 |
| Kansas | 840 | 240 | 600 | 860 | 240 | 620 |
| Kentucky | 1,520 | 450 | 1,070 | 1,550 | 460 | 1,090 |
| Louisiana | 1,420 | 340 | 1,080 | 1,480 | 350 | 1,130 |
| Maine | 320 | 140 | 180 | 320 | 140 | 180 |
| Maryland | 1,610 | 460 | 1,150 | 1,660 | 460 | 1,200 |
| Massachusetts | 1,360 | 520 | 850 | 1,360 | 520 | 850 |
| Michigan | 2,420 | 800 | 1,630 | 2,430 | 800 | 1,640 |
| Minnesota | 1,540 | 500 | 1,040 | 1,620 | 510 | 1,100 |
| Mississippi | 780 | 230 | 550 | 800 | 230 | 570 |
| Missouri | 1,750 | 520 | 1,230 | 1,780 | 520 | 1,260 |
| Montana | 300 | 100 | 200 | 310 | 100 | 200 |
| Nebraska | 450 | 160 | 280 | 450 | 160 | 290 |
| Nevada | 680 | 230 | 450 | 710 | 240 | 470 |
| New Hampshire | 380 | 130 | 250 | 390 | 140 | 250 |
| New Jersey | 2,970 | 760 | 2,210 | 3,080 | 770 | 2,310 |
| New Mexico | 470 | 150 | 320 | 480 | 150 | 330 |
| New York | 6,540 | 1,560 | 4,980 | 6,680 | 1,570 | 5,110 |
| North Carolina | 3,010 | 850 | 2,150 | 3,090 | 870 | 2,220 |
| North Dakota | 190 | 60 | 140 | 200 | 60 | 140 |
| Ohio | 3,070 | 1,020 | 2,050 | 3,150 | 1,030 | 2,120 |
| Oklahoma | 1,100 | 310 | 790 | 1,140 | 310 | 830 |
| Oregon | 970 | 380 | 590 | 980 | 380 | 600 |
| Pennsylvania | 4,250 | 1,220 | 3,030 | 4,320 | 1,240 | 3,090 |
| Rhode Island | 220 | 80 | 140 | 220 | 80 | 140 |
| South Carolina | 1,520 | 420 | 1,100 | 1,580 | 430 | 1,150 |
| South Dakota | 230 | 70 | 160 | 240 | 70 | 170 |
| Tennessee | 2,040 | 560 | 1,490 | 2,090 | 570 | 1,530 |
| Texas | 7,220 | 2,010 | 5,210 | 7,370 | 2,040 | 5,330 |
| Utah | 1,330 | 220 | 1,110 | 1,440 | 230 | 1,210 |
| Vermont | 180 | 60 | 130 | 180 | 60 | 130 |
| Virginia | 1,850 | 670 | 1,180 | 1,870 | 690 | 1,190 |
| Washington | 2,830 | 670 | 2,170 | 2,940 | 680 | 2,260 |
| West Virginia | 500 | 160 | 340 | 510 | 160 | 350 |
| Wisconsin | 2,000 | 540 | 1,460 | 2,060 | 550 | 1,520 |
| Wyoming | 160 | 50 | 100 | 160 | 60 | 110 |
| US TOTAL c | 86,010 | 25,510 | 60,490 | 87,240 | 25,800 | 61,430 |
a. Source: Estimation based on CBTRUS NPCR and SEER 2000–2016 data for malignant tumors, and NPCR and SEER 2006–2016 data for non-malignant tumors.
b. Rounded to the nearest 10. Numbers may not add up due to rounding.
c. Total estimate is based on overall estimate. Histology-specific estimates may not add up to Total.
– Estimated number is less than 50. These cases are included in overall rates.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program
Estimated number of expected cases of all primary brain and other CNS tumors by histology, histology grouping, and age
The estimated number of cases of all primary brain and other CNS tumors for 2019 and 2020 by histology and age are shown in Table 18.
Table 18.
Estimated number of casesa,b of brain and other central nervous system tumors overall and by behavior, by age, major histology groupingc, and histology, 2019, 2020
| Histology | 2019 Estimated Cases | 2020 Estimated Cases | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | Malignant | Non-Malignant | All | Malignant | Non-Malignant | |||||||||||
| All Ages | 0–14 | 0–19 | 15–39 | 40–64 | 65+ | All Ages | All Ages | All Ages | 0–14 | 0–19 | 15–39 | 40–64 | 65+ | All Ages | All Ages | |
| Tumors of Neuroepithelial Tissue | 23,440 | 2,530 | 2,950 | 3,760 | 8,550 | 8,600 | 21,600 | 1,840 | 23,720 | 2,530 | 2,940 | 3,810 | 8,600 | 8,790 | 21,850 | 1,870 |
| Pilocytic Astrocytoma | 960 | 540 | 600 | 280 | 100 | -- | 960 | -- | 940 | 530 | 580 | 280 | 100 | -- | 940 | -- |
| Diffuse Astrocytoma | 1,340 | 130 | 170 | 460 | 420 | 330 | 1,340 | -- | 1,310 | 120 | 160 | 460 | 400 | 330 | 1,310 | -- |
| Anaplastic Astrocytoma | 1,640 | 60 | 80 | 500 | 660 | 410 | 1,640 | -- | 1,690 | 70 | 90 | 530 | 670 | 420 | 1,690 | -- |
| Unique Astrocytoma Variants | 250 | 80 | 100 | 90 | -- | -- | 180 | 80 | 260 | 90 | 100 | 90 | -- | 50 | 180 | 80 |
| Glioblastoma | 12,900 | 110 | 160 | 570 | 5,430 | 6,780 | 12,900 | -- | 13,140 | 120 | 170 | 580 | 5,490 | 6,950 | 13,140 | -- |
| Oligodendroglioma | 680 | -- | -- | 250 | 340 | 70 | 680 | -- | 660 | -- | -- | 240 | 330 | 70 | 660 | -- |
| Anaplastic Oligodendroglioma | 380 | -- | -- | 110 | 210 | 60 | 380 | -- | 390 | -- | -- | 110 | 210 | 60 | 390 | -- |
| Oligoastrocytic Tumors | 50 | -- | -- | -- | -- | -- | 50 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Ependymal Tumors | 1,410 | 200 | 230 | 380 | 560 | 280 | 770 | 640 | 1,420 | 200 | 230 | 380 | 560 | 290 | 760 | 660 |
| Glioma Malignant, NOS | 1,670 | 510 | 580 | 400 | 350 | 420 | 1,670 | -- | 1,690 | 510 | 590 | 410 | 350 | 420 | 1,690 | -- |
| Choroid Plexus Tumors | 160 | 70 | 60 | -- | -- | -- | -- | 130 | 160 | 70 | 60 | -- | -- | -- | -- | 130 |
| Other Neuroepithelial Tumors | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Neuronal and Mixed Neuronal Glial Tumors | 1,100 | 290 | 420 | 430 | 270 | 100 | 220 | 880 | 1,120 | 300 | 440 | 440 | 280 | 110 | 230 | 900 |
| Tumors of the Pineal Region | 190 | -- | -- | 70 | 70 | -- | 110 | 80 | 200 | -- | -- | 70 | 70 | -- | 120 | 80 |
| Embryonal Tumors | 700 | 470 | 450 | 170 | 50 | -- | 670 | -- | 690 | 470 | 450 | 170 | -- | -- | 670 | -- |
| Tumors of Cranial and Spinal Nerves | 7,520 | 160 | 250 | 1,140 | 4,010 | 2,210 | -- | 7,480 | 7,640 | 150 | 250 | 1,160 | 4,070 | 2,250 | -- | 7,600 |
| Nerve Sheath Tumors | 7,510 | 160 | 250 | 1,140 | 4,000 | 2,210 | -- | 7,470 | 7,620 | 150 | 250 | 1,160 | 4,070 | 2,250 | -- | 7,580 |
| Other Tumors of Cranial and Spinal Nerves | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Tumors of Meninges | 34,530 | 130 | 250 | 2,160 | 13,520 | 18,720 | 480 | 34,050 | 35,200 | 130 | 260 | 2,170 | 13,690 | 19,200 | 470 | 34,720 |
| Meningioma | 33,560 | 60 | 140 | 1,900 | 13,110 | 18,490 | 300 | 33,260 | 34,210 | 60 | 140 | 1,910 | 13,280 | 18,970 | 290 | 33,920 |
| Mesenchymal Tumors | 310 | 60 | 60 | 60 | 120 | 80 | 100 | 210 | 320 | 60 | 60 | 60 | 120 | 80 | 100 | 220 |
| Primary Melanocytic Lesions | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| Other Neoplasms Related to the Meninges | 630 | -- | 50 | 200 | 280 | 140 | 50 | 570 | 630 | -- | 50 | 200 | 280 | 140 | 50 | 570 |
| Lymphoma and Hematopoietic Neoplasms | 1,740 | -- | -- | 110 | 580 | 1,020 | 1,740 | -- | 1,770 | -- | -- | 110 | 580 | 1,050 | 1,770 | -- |
| Lymphoma | 1,670 | -- | -- | 90 | 570 | 1,010 | 1,670 | -- | 1,690 | -- | -- | 90 | 570 | 1,040 | 1,690 | -- |
| Other Hematopoietic Neoplasms | 70 | -- | -- | -- | -- | -- | 70 | -- | 80 | -- | -- | -- | -- | -- | 80 | -- |
| Germ Cell Tumors and Cysts | 340 | 150 | 190 | 150 | -- | -- | 230 | 110 | 340 | 150 | 190 | 150 | -- | -- | 230 | 110 |
| Germ cell tumors, cysts, and heterotopias | 340 | 150 | 190 | 150 | -- | -- | 230 | 110 | 340 | 150 | 190 | 150 | -- | -- | 230 | 110 |
| Tumors of Sellar Region | 14,650 | 310 | 820 | 4,150 | 6,250 | 3,950 | -- | 14,620 | 14,750 | 310 | 820 | 4,140 | 6,290 | 4,020 | -- | 14,720 |
| Tumors of the Pituitary | 14,020 | 170 | 650 | 4,010 | 6,020 | 3,820 | -- | 13,990 | 14,120 | 170 | 650 | 4,000 | 6,050 | 3,890 | -- | 14,090 |
| Craniopharyngioma | 630 | 140 | 170 | 140 | 230 | 120 | -- | 630 | 640 | 140 | 170 | 130 | 230 | 130 | -- | 630 |
| Unclassified Tumors | 3,790 | 230 | 260 | 560 | 900 | 2,100 | 1,400 | 2,390 | 3,810 | 240 | 260 | 540 | 840 | 2,190 | 1,410 | 2,400 |
| Hemangioma | 870 | 70 | 100 | 250 | 330 | 210 | -- | 860 | 820 | 70 | 100 | 240 | 300 | 200 | -- | 810 |
| Neoplasm Unspecified | 2,750 | 140 | 140 | 300 | 570 | 1,740 | 1,380 | 1,370 | 2,730 | 150 | 140 | 300 | 540 | 1,750 | 1,390 | 1,340 |
| All Other | 170 | -- | -- | -- | -- | 150 | -- | 160 | 260 | -- | -- | -- | -- | 240 | -- | 250 |
| TOTAL d | 86,010 | 3,540 | 4,750 | 12,030 | 33,840 | 36,600 | 25,510 | 60,490 | 87,240 | 3,540 | 4,760 | 12,090 | 34,100 | 37,500 | 25,800 | 61,430 |
a. Source: Estimation based on CBTRUS NPCR and SEER 2000–2016 data for malignant tumors, and NPCR and SEER 2006–2016 data for non-malignant tumors.
b. Rounded to the nearest 10. Numbers may not add up due to rounding.
c. Major histology grouping estimates are calculated by summing estimates for all included histologies.
d. Total estimate is based on overall estimate. Histology-specific estimates may not add up to Total.
– Estimated number is less than 50. These cases are included in overall rates.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; SEER, Surveillance, Epidemiology, and End Results Program
Meningiomas have the highest number of all estimated new cases, with 33,560 cases projected in 2019 and 34,210 in 2020.
Glioblastoma has the highest number of cases of all malignant tumors, with 12,900 cases projected in 2019 and 13,140 in 2020.
For 2019, the highest number of new cases is predicted in those age 65+ years, with 36,600 cases.
For 2020, the highest number of new cases is estimated to be in those age 65+ years, with 37,500 cases.
For 2019 and 2020, children age 0–14 years are estimated to have 3,540 and 3,540 new cases of primary brain and other CNS tumors each year, respectively.
For 2019 and 2020, children age 0–19 years are estimated to have 4,750 and 4,760 new cases of primary brain and other CNS tumors each year, respectively.
Estimated mortality rates formalignant brain and other CNS tumors by state, sex, and urban/ rural residence
Table 19 and Figure 20 show average annual age-adjusted mortality rates for primary malignant brain and other CNS tumors in the US during 2012–2016 by state and sex. Average annual age-adjusted mortality rates for primary malignant brain and other CNS tumors by state and urban/rural residence are shown in Supplementary Table 9.
Table 19.
Five-year total, average annual totala, and average annual age-adjusted mortality ratesb for malignant brain and other central nervous system cancer overall and by state and sex, United States, 2012-2016c
| State | Total | Male | Female | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | 5-year Total | Annual average | Rate | 95% CI | |
| Alabama | 1,470 | 294 | 5.18 | 4.91–5.46 | 816 | 163 | 6.34 | 5.90–6.80 | 654 | 131 | 4.23 | 3.90–4.58 |
| Alaska | 141 | 28 | 4.13 | 3.42–4.93 | 74 | 15 | 4.28 | 3.26–5.50 | 67 | 13 | 3.97 | 3.03–5.11 |
| Arizona | 1,704 | 341 | 4.41 | 4.20–4.63 | 961 | 192 | 5.25 | 4.92–5.60 | 743 | 149 | 3.66 | 3.39–3.94 |
| Arkansas | 889 | 178 | 5.12 | 4.78–5.48 | 489 | 98 | 6.16 | 5.62–6.75 | 400 | 80 | 4.29 | 3.87–4.74 |
| California | 8,885 | 1,777 | 4.38 | 4.29–4.48 | 5,039 | 1,008 | 5.39 | 5.24–5.54 | 3,846 | 769 | 3.53 | 3.41–3.64 |
| Colorado | 1,255 | 251 | 4.44 | 4.19–4.70 | 682 | 136 | 5.11 | 4.72–5.52 | 573 | 115 | 3.87 | 3.55–4.20 |
| Connecticut | 927 | 185 | 4.28 | 4.00–4.57 | 532 | 106 | 5.43 | 4.96–5.92 | 395 | 79 | 3.30 | 2.97–3.66 |
| Delaware | 248 | 50 | 4.35 | 3.81–4.95 | 130 | 26 | 5.08 | 4.22–6.07 | 118 | 24 | 3.82 | 3.14–4.61 |
| Washington DC | 78 | 16 | 2.40 | 1.89–3.02 | 46 | 9 | 3.11 | 2.26–4.19 | 32 | 6 | 1.82 | 1.23–2.60 |
| Florida | 5,491 | 1,098 | 4.19 | 4.08–4.31 | 3,070 | 614 | 5.09 | 4.91–5.28 | 2,421 | 484 | 3.39 | 3.25–3.53 |
| Georgia | 2,212 | 442 | 4.25 | 4.07–4.43 | 1,242 | 248 | 5.23 | 4.94–5.55 | 970 | 194 | 3.42 | 3.21–3.65 |
| Hawaii | 245 | 49 | 2.83 | 2.48–3.22 | 139 | 28 | 3.35 | 2.80–3.98 | 106 | 21 | 2.35 | 1.91–2.87 |
| Idaho | 468 | 94 | 5.16 | 4.69–5.66 | 296 | 59 | 6.88 | 6.09–7.73 | 172 | 34 | 3.59 | 3.07–4.19 |
| Illinois | 3,020 | 604 | 4.20 | 4.05–4.36 | 1,694 | 339 | 5.16 | 4.91–5.42 | 1,326 | 265 | 3.40 | 3.22–3.60 |
| Indiana | 1,712 | 342 | 4.63 | 4.41–4.86 | 976 | 195 | 5.69 | 5.33–6.06 | 736 | 147 | 3.75 | 3.48–4.04 |
| Iowa | 938 | 188 | 5.10 | 4.77–5.45 | 532 | 106 | 6.20 | 5.67–6.76 | 406 | 81 | 4.09 | 3.69–4.53 |
| Kansas | 819 | 164 | 5.03 | 4.68–5.40 | 471 | 94 | 6.17 | 5.62–6.77 | 348 | 70 | 4.04 | 3.62–4.51 |
| Kentucky | 1,252 | 250 | 4.92 | 4.64–5.20 | 696 | 139 | 5.89 | 5.45–6.36 | 556 | 111 | 4.06 | 3.72–4.42 |
| Louisiana | 1,106 | 221 | 4.34 | 4.09–4.61 | 618 | 124 | 5.34 | 4.91–5.79 | 488 | 98 | 3.53 | 3.22–3.86 |
| Maine | 451 | 90 | 5.06 | 4.58–5.58 | 277 | 55 | 6.64 | 5.85–7.51 | 174 | 35 | 3.70 | 3.14–4.34 |
| Maryland | 1,356 | 271 | 4.08 | 3.86–4.31 | 755 | 151 | 5.01 | 4.65–5.39 | 601 | 120 | 3.32 | 3.05–3.60 |
| Massachusetts | 1,777 | 355 | 4.49 | 4.28–4.71 | 993 | 199 | 5.56 | 5.21–5.92 | 784 | 157 | 3.61 | 3.35–3.88 |
| Michigan | 2,780 | 556 | 4.70 | 4.52–4.88 | 1,568 | 314 | 5.73 | 5.44–6.03 | 1,212 | 242 | 3.81 | 3.60–4.04 |
| Minnesota | 1,438 | 288 | 4.68 | 4.43–4.93 | 859 | 172 | 5.91 | 5.51–6.33 | 579 | 116 | 3.57 | 3.28–3.89 |
| Mississippi | 880 | 176 | 5.29 | 4.94–5.66 | 466 | 93 | 6.29 | 5.72–6.91 | 414 | 83 | 4.51 | 4.07–4.97 |
| Missouri | 1,571 | 314 | 4.37 | 4.15–4.60 | 869 | 174 | 5.31 | 4.95–5.68 | 702 | 140 | 3.58 | 3.31–3.86 |
| Montana | 306 | 61 | 4.72 | 4.19–5.31 | 176 | 35 | 5.67 | 4.83–6.61 | 130 | 26 | 3.80 | 3.15–4.55 |
| Nebraska | 527 | 105 | 5.04 | 4.61–5.50 | 298 | 60 | 6.11 | 5.42–6.86 | 229 | 46 | 4.12 | 3.58–4.71 |
| Nevada | 690 | 138 | 4.40 | 4.07–4.75 | 388 | 78 | 5.04 | 4.54–5.59 | 302 | 60 | 3.78 | 3.36–4.24 |
| New Hampshire | 397 | 79 | 4.88 | 4.39–5.40 | 236 | 47 | 6.13 | 5.35–7.01 | 161 | 32 | 3.83 | 3.23–4.50 |
| New Jersey | 2,092 | 418 | 4.02 | 3.84–4.20 | 1,172 | 234 | 4.96 | 4.68–5.26 | 920 | 184 | 3.24 | 3.03–3.46 |
| New Mexico | 434 | 87 | 3.60 | 3.26–3.97 | 237 | 47 | 4.15 | 3.62–4.73 | 197 | 39 | 3.12 | 2.69–3.60 |
| New York | 4,385 | 877 | 3.84 | 3.72–3.96 | 2,370 | 474 | 4.61 | 4.42–4.80 | 2,015 | 403 | 3.21 | 3.07–3.36 |
| North Carolina | 2,459 | 492 | 4.36 | 4.19–4.54 | 1,362 | 272 | 5.36 | 5.07–5.66 | 1,097 | 219 | 3.52 | 3.31–3.74 |
| North Dakota | 181 | 36 | 4.33 | 3.71–5.03 | 109 | 22 | 5.59 | 4.57–6.77 | 72 | 14 | 3.29 | 2.56–4.18 |
| Ohio | 3,176 | 635 | 4.60 | 4.44–4.77 | 1,831 | 366 | 5.78 | 5.51–6.06 | 1,345 | 269 | 3.60 | 3.41–3.81 |
| Oklahoma | 1,017 | 203 | 4.70 | 4.41–5.00 | 571 | 114 | 5.72 | 5.25–6.22 | 446 | 89 | 3.82 | 3.47–4.20 |
| Oregon | 1,198 | 240 | 5.04 | 4.75–5.34 | 686 | 137 | 6.08 | 5.62–6.57 | 512 | 102 | 4.10 | 3.74–4.48 |
| Pennsylvania | 3,514 | 703 | 4.42 | 4.27–4.58 | 1,964 | 393 | 5.41 | 5.16–5.66 | 1,550 | 310 | 3.61 | 3.42–3.80 |
| Rhode Island | 297 | 59 | 4.67 | 4.14–5.26 | 168 | 34 | 5.77 | 4.90–6.74 | 129 | 26 | 3.72 | 3.08–4.45 |
| South Carolina | 1,288 | 258 | 4.49 | 4.25–4.75 | 741 | 148 | 5.69 | 5.27–6.13 | 547 | 109 | 3.49 | 3.20–3.81 |
| South Dakota | 264 | 53 | 5.29 | 4.66–6.00 | 150 | 30 | 6.31 | 5.32–7.44 | 114 | 23 | 4.48 | 3.66–5.43 |
| Tennessee | 1,784 | 357 | 4.75 | 4.53–4.98 | 1,029 | 206 | 5.99 | 5.62–6.38 | 755 | 151 | 3.69 | 3.42–3.97 |
| Texas | 5,548 | 1,110 | 4.22 | 4.10–4.33 | 3,080 | 616 | 5.03 | 4.85–5.22 | 2,468 | 494 | 3.52 | 3.38–3.66 |
| Utah | 599 | 120 | 4.68 | 4.30–5.08 | 361 | 72 | 5.96 | 5.35–6.63 | 238 | 48 | 3.52 | 3.08–4.00 |
| Vermont | 212 | 42 | 5.44 | 4.70–6.26 | 114 | 23 | 6.20 | 5.07–7.52 | 98 | 20 | 4.78 | 3.84–5.89 |
| Virginia | 1,902 | 380 | 4.12 | 3.93–4.31 | 1,014 | 203 | 4.81 | 4.51–5.12 | 888 | 178 | 3.56 | 3.32–3.81 |
| Washington | 1,963 | 393 | 4.96 | 4.74–5.19 | 1,128 | 226 | 6.02 | 5.67–6.40 | 835 | 167 | 4.02 | 3.74–4.31 |
| West Virginia | 564 | 113 | 4.70 | 4.31–5.13 | 325 | 65 | 5.76 | 5.13–6.45 | 239 | 48 | 3.77 | 3.29–4.31 |
| Wisconsin | 1,644 | 329 | 4.86 | 4.62–5.11 | 921 | 184 | 5.77 | 5.40–6.17 | 723 | 145 | 4.03 | 3.73–4.34 |
| Wyoming | 164 | 33 | 5.01 | 4.24–5.87 | 84 | 17 | 5.33 | 4.21–6.66 | 80 | 16 | 4.80 | 3.76–6.03 |
| US TOTAL | 79,718 | 15,944 | 4.42 | 4.38–4.45 | 44,805 | 8,961 | 5.38 | 5.33–5.44 | 34,913 | 6,983 | 3.59 | 3.55–3.63 |
a. Annual average deaths are calculated by dividing the five-year total by five.
b. Rates are per 100,000 and are age-adjusted to the 2000 US standard population.
c. Estimated by CBTRUS using Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Mortality - All COD, Aggregated With State, Total U.S. (1990–2016) <Katrina/Rita Population Adjustment>, National Cancer Institute, DCCPS, Surveillance Research Program, released December 2018. Underlying mortality data provided by NCHS (www.cdc.gov/nchs).
- Counts and rates are not presented when fewer than 16 cases were reported for the specific category, or where the inclusion of the count and rate would allow for back-calculation of suppressed values. The suppressed cases are included in the counts and rates for Totals.
Abbreviations: NCHS, National Center for Health Statistics; CI, Confidence Interval.
Fig. 20.
Average Annual Age-Adjusted Mortality Ratesa for Malignant Primary Brain and Other CNS Tumors by Central Cancer Registry, CBTRUS Statistical Report: NVSS, 2012–2016
The aggregate total number of observed deaths was 79,718, for an average annual age-adjusted mortality rate of 4.42 per 100,000 population.
There was considerable variation between individual states, which ranged from a low of 2.40 deaths per 100,000 population to a high of 5.44 deaths per 100,000 population. Rates may vary by state for multiple reasons, including demographic variation and procedures for deciding primary cause of death on a death certificate.
Males had a higher mortality rate for malignant brain and other CNS tumors than females in the US population, with 5.38 per 100,000 population as compared to 3.59 per 100,000 population.
Mortality rates for malignant brain and other CNS tumors were higher in rural areas (4.69 per 100,000) as compared to urban areas (4.37 per 100,000).
There was considerable variation by state, where mortality rates in urban areas ranged from 2.40 per 100,000 population to 5.93 per 100,000 population, and mortality rates in rural areas ranged from 3.19 per 100,000 population to 5.51 per 100,000 population.
Relative survival rates for all brain and other CNS tumors by site and behavior
Relative survival estimates by site and behavior are presented in Table 20.
Table 20.
One-, five-, and ten-year relative survival ratesa,b with 95% confidence intervals for all primary brain and other central nervous system tumors by behavior and site, U.S. Cancer Statistics – NPCR Registries, 2001–2015 (varying)
| Site (ICD-O Topography Code) | Malignant (2001–2015) | Non-Malignant (2004–2015) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nc | 1-Year | 5-Year | 10-Year | Nc | 1-Year | 5-Year | 10-Year | |||||||
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |||
| Cerebrum (C71.0) | 13,173 | 52.9 | 52.0–53.8 | 29.8 | 28.9–30.6 | 26.1 | 52.0-27.1 | 2,328 | 88.6 | 87.1–89.9 | 84.3 | 82.3–86.1 | 77.6 | 87.1-80.6 |
| Frontal lobe (C71.1) | 64,405 | 61.4 | 61.0–61.8 | 34.8 | 34.4–35.2 | 27.6 | 61.0-28.0 | 6,534 | 89.5 | 88.6–90.2 | 84.2 | 82.9–85.3 | 79.4 | 88.6-81.2 |
| Temporal lobe (C71.2) | 47,133 | 58.1 | 57.6–58.5 | 23.9 | 23.5–24.3 | 18.6 | 57.6-19.1 | 5,460 | 93.4 | 92.6–94.1 | 90.5 | 89.5–91.5 | 88.5 | 92.6-89.8 |
| Parietal lobe (C71.3) | 30,558 | 50.9 | 50.4–51.5 | 21.0 | 20.5–21.5 | 16.6 | 50.4-17.1 | 2,799 | 87.5 | 86.1–88.8 | 82.8 | 80.9–84.5 | 78.6 | 86.1-81.2 |
| Occipital lobe (C71.4) | 7,718 | 53.1 | 51.9–54.2 | 22.0 | 20.9–23.0 | 18.4 | 51.9-19.4 | 1,225 | 91.0 | 89.0–92.6 | 88.5 | 85.9–90.7 | 84.7 | 89.0-88.2 |
| Ventricle, NOS (C71.5) | 4,415 | 77.1 | 75.8–78.4 | 64.4 | 62.8–65.9 | 59.7 | 75.8-61.4 | 4948 | 93.9 | 93.2–94.6 | 91.0 | 89.9–92.0 | 87.2 | 93.2-88.8 |
| Cerebellum, NOS (C71.6) | 13,440 | 85.8 | 85.1–86.4 | 72.5 | 71.7–73.3 | 68.0 | 85.1-68.9 | 7,580 | 94.7 | 94.1–95.2 | 91.9 | 91.0–92.8 | 89.3 | 94.1-90.7 |
| Brain stem (C71.7) | 11,599 | 72.2 | 71.3–73.0 | 52.6 | 51.7–53.6 | 47.8 | 71.3-48.9 | 3,020 | 91.5 | 90.4–92.5 | 88.0 | 86.4–89.4 | 82.4 | 90.4-84.8 |
| Other brain (C71.8-C71.9) | 59,054 | 46.3 | 45.9–46.7 | 25.3 | 24.9–25.7 | 21.4 | 45.9-21.9 | 12,406 | 84.6 | 83.9–85.3 | 79.2 | 78.2–80.0 | 74.6 | 83.9-75.9 |
| Spinal cord and cauda equina (C72.0-C72.1) | 8,790 | 90.0 | 89.3–90.7 | 82.0 | 81.0–82.9 | 78.7 | 89.3-79.9 | 17,157 | 99.0 | 98.8–99.2 | 98.3 | 97.8–98.7 | 97.8 | 98.8-98.5 |
| Cranial nerves (C72.2-C72.5) | 3,674 | 97.1 | 96.5–97.6 | 93.4 | 92.4–94.3 | 92.4 | 96.5-93.5 | 54,180 | 99.4 | 99.3–99.5 | 99.4 | 99.3–99.5 | 99.4 | 99.3–99.5 |
| Other nervous system (C72.8-C72.9) | 2,613 | 63.8 | 61.9–65.7 | 49.3 | 47.1–51.5 | 44.4 | 61.9-47.0 | 2,417 | 97.4 | 96.5–98.1 | 94.5 | 92.9–95.7 | 92.1 | 96.5-94.2 |
| Meninges (cerebral and spinal) (C70.0–9) | 5,453 | 83.7 | 82.6–84.8 | 67.7 | 66.2–69.3 | 61.2 | 82.6-63.2 | 289,544 | 93.1 | 93.0–93.2 | 88.0 | 87.8–88.3 | 83.8 | 93.0-84.1 |
| Pituitary and craniopharyngeal duct (C75.1-C75.2) | 1,208 | 86.7 | 84.5–88.6 | 75.2 | 72.1–78.0 | 70.4 | 84.5-73.9 | 137,770 | 97.9 | 97.8–98.0 | 96.2 | 96.0–96.4 | 94.3 | 97.8-94.7 |
| Pineal gland (C75.3) | 2,513 | 89.2 | 87.9–90.4 | 75.9 | 73.9–77.7 | 71.5 | 87.9-73.6 | 1,388 | 94.3 | 92.8–95.5 | 90.2 | 87.8–92.0 | 86.5 | 92.8-89.6 |
| Nasal cavity (C30.0)d | 1,529 | 92.4 | 90.8–93.8 | 82.2 | 79.6–84.5 | 74.2 | 90.8-77.7 | -- | -- | -- | -- | -- | -- | -- |
| TOTAL | 277,275 | 60.1 | 59.9–60.3 | 35.8 | 35.6–36.0 | 30.8 | 59.9-31.0 | 548,756 | 94.9 | 94.8–95.0 | 91.5 | 91.4–91.7 | 88.7 | 94.8-88.9 |
a. The cohort analysis of survival rates was utilized for calculating the survival estimates presented in this table. Long-term cohort-based survival estimates reflect the survival experience of individuals diagnosed over the time period, and they may not necessarily reflect the long-term survival outlook of newly diagnosed cases.
b. Rates are an estimate of the percentage of patients alive at one, five, and ten years, respectively.
c. Total number of case that occurred within the NPCR registries between 2001 and 2015.
d. ICD-O-3 histology codes 9522–9523 only.
- Rates were not presented for categories with 50 or fewer cases and were suppressed for rates where fewer than 16 cases were surviving within a category.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; CI, Confidence Interval; NOS, Not otherwise specified
The highest five-year survival among malignant tumors was for tumors occurring in the cranial nerves (93.4%).
The lowest five-year survival among malignant tumors was for tumors of the parietal lobe (21.0%).
Survival rates for malignant brain and other CNS tumors by histology and age
Survival estimates for malignant brain and other CNS tumors by histology and age at diagnosis are presented in Tables 21, 22. Histology-specific rates are presented for the CBTRUS histology groupings which contain a substantial number of incident malignant tumors.
Table 21.
One-, two-, five-, and ten-year relative survival ratesa,b with 95% confidence intervals for selected malignant brain and other central nervous system tumors overall and by NCI age groups, U.S. Cancer Statistics – NPCR Registries, 2001–2015
| Histology | Age-group (years) | Nc | 1-Year | 2-Year | 5-Year | 10-Year | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |||
| Pilocytic astrocytomad` | 0-14e | 8,009 | 98.8 | 98.5–99.0 | 98.3 | 98.0–98.6 | 97.0 | 96.6–97.4 | 95.7 | 95.0–96.2 |
| 15-39f | 4,105 | 98.2 | 97.8–98.6 | 97.2 | 96.6–97.7 | 94.6 | 93.8–95.3 | 92.8 | 91.7–93.7 | |
| 40+ | 1,370 | 91.3 | 89.5–92.8 | 86.0 | 83.8–87.9 | 78.0 | 75.2–80.5 | 76.4 | 73.2–79.3 | |
| All Ages | 13,484 | 97.9 | 97.6–98.1 | 96.7 | 96.4–97.0 | 94.4 | 93.9–94.8 | 92.9 | 92.3–93.4 | |
| Diffuse astrocytoma | 0–14 | 2,347 | 92.3 | 91.1–93.3 | 86.8 | 85.4–88.2 | 83.0 | 81.3–84.5 | 80.8 | 78.9–82.5 |
| 15–39 | 6,668 | 95.0 | 94.4–95.5 | 89.5 | 88.7–90.2 | 76.1 | 75.0–77.2 | 59.0 | 57.5–60.6 | |
| 40+ | 12,528 | 60.6 | 59.7–61.5 | 46.1 | 45.2–47.1 | 32.3 | 31.4–33.2 | 23.8 | 22.9–24.8 | |
| All Ages | 21,543 | 74.7 | 74.1–75.3 | 64.1 | 63.4–64.8 | 51.6 | 50.9–52.3 | 41.3 | 40.5–42.1 | |
| Anaplastic astrocytoma | 0–14 | 676 | 65.4 | 61.6–68.9 | 36.3 | 32.5–40.1 | 25.2 | 21.7–28.9 | 20.4 | 16.9–24.2 |
| 15–39 | 3,919 | 90.6 | 89.6–91.5 | 78.3 | 76.9–79.6 | 59.7 | 57.9–61.4 | 44.4 | 42.3–46.5 | |
| 40+ | 10,629 | 54.6 | 53.6–55.5 | 34.6 | 33.6–35.6 | 19.5 | 18.6–20.3 | 14.1 | 13.2–15.0 | |
| All Ages | 15,224 | 64.3 | 63.5–65.1 | 46.0 | 45.1–46.8 | 30.2 | 29.3–31.0 | 22.3 | 21.4–23.1 | |
| Unique astrocytoma variants | 0–14 | 367 | 94.7 | 91.7–96.6 | 89.1 | 85.3–92.0 | 79.0 | 73.9–83.2 | 75.0 | 69.1–79.9 |
| 15–39 | 671 | 94.8 | 92.8–96.3 | 90.3 | 87.7–92.4 | 79.2 | 75.5–82.5 | 75.0 | 70.8–78.7 | |
| 40+ | 655 | 59.5 | 55.4–63.3 | 44.6 | 40.5–48.6 | 30.3 | 26.3–34.5 | 25.4 | 20.9–30.1 | |
| All Ages | 1,693 | 81.2 | 79.2–83.0 | 72.5 | 70.2–74.7 | 60.5 | 57.8–63.1 | 56.2 | 53.3–59.1 | |
| Glioblastoma | 0–14 | 1,136 | 58.1 | 55.2–61.0 | 33.0 | 30.2–35.9 | 21.8 | 19.2–24.5 | 18.1 | 15.6–20.8 |
| 15–39 | 6,434 | 75.0 | 73.9–76.1 | 49.8 | 48.5–51.0 | 26.2 | 25.0–27.5 | 18.6 | 17.4–19.8 | |
| 40+ | 116,347 | 38.7 | 38.4–39.0 | 16.6 | 16.3–16.8 | 5.5 | 5.4–5.7 | 3.7 | 3.5–3.8 | |
| All Ages | 123,917 | 40.8 | 40.5–41.1 | 18.5 | 18.2–18.7 | 6.8 | 6.7–7.0 | 4.7 | 4.5–4.8 | |
| Oligodendroglioma | 0–14 | 362 | 97.5 | 95.2–98.7 | 96.0 | 93.3–97.7 | 94.5 | 91.4–96.5 | 91.6 | 87.6–94.4 |
| 15–39 | 4,373 | 98.6 | 98.2–98.9 | 97.2 | 96.7–97.7 | 91.4 | 90.4–92.3 | 76.2 | 74.4–77.9 | |
| 40+ | 6,013 | 91.3 | 90.5–92.0 | 85.4 | 84.4–86.3 | 75.5 | 74.2–76.8 | 61.6 | 59.9–63.3 | |
| All Ages | 10,748 | 94.5 | 94.0–94.9 | 90.6 | 90.0–91.2 | 82.7 | 81.9–83.5 | 68.7 | 67.5–69.9 | |
| Anaplastic oligodendroglioma | 0–14 | 54 | 85.1 | 72.3–92.3 | 69.7 | 55.3–80.2 | 57.0 | 42.1–69.3 | 52.0 | 37.0–65.0 |
| 15–39 | 1,353 | 95.0 | 93.6–96.0 | 88.6 | 86.7–90.2 | 75.2 | 72.5–77.6 | 60.3 | 56.9–63.5 | |
| 40+ | 3,311 | 82.0 | 80.6–83.3 | 68.5 | 66.7–70.1 | 53.9 | 52.0–55.8 | 41.6 | 39.3–43.9 | |
| All Ages | 4,718 | 85.8 | 84.7–86.8 | 74.3 | 73.0–75.6 | 60.2 | 58.6–61.7 | 47.3 | 45.4–49.2 | |
| Oligoastrocytic tumors | 0–14 | 198 | 89.3 | 84.0–92.9 | 79.2 | 72.7–84.3 | 76.2 | 69.4–81.7 | 75.5 | 68.6–81.1 |
| 15–39 | 3,232 | 97.3 | 96.7–97.8 | 93.5 | 92.5–94.3 | 80.0 | 78.4–81.5 | 59.5 | 57.2–61.8 | |
| 40+ | 3,869 | 81.8 | 80.5–83.0 | 68.6 | 67.0–70.1 | 53.3 | 51.5–55.0 | 41.0 | 38.9–43.1 | |
| All Ages | 7,299 | 88.9 | 88.1–89.6 | 80.0 | 79.0–80.9 | 65.9 | 64.6–67.0 | 50.3 | 48.7–51.8 | |
| Ependymal tumors | 0–14 | 2,263 | 94.8 | 93.8–95.7 | 88.9 | 87.5–90.2 | 76.7 | 74.7–78.5 | 67.1 | 64.6–69.4 |
| 15–39 | 2,863 | 97.1 | 96.4–97.7 | 95.1 | 94.2–95.9 | 91.7 | 90.5–92.7 | 87.5 | 85.8–89.0 | |
| 40+ | 5,149 | 92.9 | 92.1–93.6 | 90.2 | 89.3–91.1 | 86.4 | 85.1–87.5 | 82.8 | 81.0–84.4 | |
| All Ages | 10,275 | 94.5 | 94.0–95.0 | 91.3 | 90.7–91.9 | 85.7 | 84.9–86.5 | 80.6 | 79.5–81.7 | |
| Glioma malignant, NOS | 0–14 | 6,008 | 81.1 | 80.1–82.1 | 70.7 | 69.5–71.8 | 67.6 | 66.4–68.9 | 66.4 | 65.1–67.7 |
| 15–39 | 3,457 | 91.5 | 90.5–92.5 | 85.3 | 84.0–86.5 | 76.8 | 75.2–78.3 | 69.4 | 67.4–71.4 | |
| 40+ | 7,898 | 50.4 | 49.2–51.5 | 41.6 | 40.5–42.8 | 33.1 | 31.9–34.3 | 27.5 | 26.1–28.9 | |
| All Ages | 17,363 | 69.4 | 68.6–70.1 | 60.5 | 59.8–61.3 | 54.1 | 53.2–54.9 | 49.8 | 48.9–50.7 | |
| Choroid plexus tumors | 0–14 | 248 | 85.5 | 80.3–89.5 | 77.2 | 71.2–82.2 | 64.0 | 57.0–70.2 | 58.6 | 50.9–65.6 |
| 15–39 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 40+ | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| All Ages | 341 | 84.6 | 80.2–88.2 | 76.8 | 71.7–81.1 | 65.7 | 59.8–70.9 | 57.3 | 50.6–63.5 | |
| Other neuroepithelial tumors | 0–14 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 15–39 | 56 | 94.5 | 83.6–98.2 | 92.5 | 80.8–97.2 | 87.8 | 74.1–94.5 | 78.2 | 60.5–88.7 | |
| 40+ | 55 | 67.1 | 52.4–78.2 | 55.2 | 40.3–67.9 | 40.7 | 26.4–54.5 | -- | -- | |
| All Ages | 155 | 85.8 | 79.0–90.6 | 79.5 | 71.8–85.3 | 71.7 | 63.0–78.7 | 63.2 | 52.7–72.0 | |
| Neuronal and mixed neuronal-glial tumors | 0–14 | 195 | 90.6 | 85.5–94.0 | 85.6 | 79.7–89.9 | 79.5 | 72.7–84.8 | 78.0 | 70.9–83.5 |
| 15–39 | 511 | 94.6 | 92.2–96.3 | 87.2 | 83.8–89.9 | 78.9 | 74.7–82.5 | 71.4 | 66.1–76.1 | |
| 40+ | 1,394 | 90.4 | 88.6–92.0 | 84.9 | 82.7–86.9 | 77.4 | 74.5–80.1 | 69.4 | 65.3–73.2 | |
| All Ages | 2,100 | 91.5 | 90.1–92.7 | 85.5 | 83.8–87.1 | 78.0 | 75.8–80.0 | 71.0 | 68.0–73.8 | |
| Tumors of the pineal region | 0–14 | 328 | 86.2 | 81.9–89.6 | 75.3 | 70.0–79.8 | 62.6 | 56.5–68.1 | 56.3 | 49.7–62.3 |
| 15–39 | 341 | 92.0 | 88.5–94.5 | 85.9 | 81.4–89.3 | 71.9 | 66.0–77.0 | 64.2 | 57.0–70.5 | |
| 40+ | 286 | 85.3 | 80.3–89.1 | 78.3 | 72.5–82.9 | 67.3 | 60.4–73.3 | 57.4 | 48.8–65.1 | |
| All Ages | 955 | 88.0 | 85.7–90.0 | 79.9 | 77.0–82.4 | 67.3 | 63.8–70.6 | 59.7 | 55.5–63.6 | |
| Embryonal tumors | 0–14 | 6,426 | 81.5 | 80.5–82.4 | 72.2 | 71.0–73.3 | 62.7 | 61.4–63.9 | 58.1 | 56.7–59.5 |
| 15–39 | 2,340 | 90.1 | 88.8–91.2 | 82.5 | 80.8–84.0 | 69.6 | 67.5–71.6 | 59.7 | 57.2–62.0 | |
| 40+ | 860 | 69.5 | 66.2–72.6 | 55.9 | 52.4–59.3 | 46.5 | 42.8–50.2 | 36.4 | 32.2–40.7 | |
| All Ages | 9,626 | 82.5 | 81.7–83.3 | 73.3 | 72.3–74.2 | 62.9 | 61.9–64.0 | 56.6 | 55.4–57.7 | |
| Medulloblastoma | 0–14 | 3,975 | 89.5 | 88.4–90.4 | 82.1 | 80.8–83.3 | 72.3 | 70.8–73.8 | 66.8 | 65.0–68.5 |
| 15–39 | 1,753 | 92.8 | 91.5–93.9 | 88.9 | 87.2–90.3 | 78.5 | 76.3–80.5 | 67.9 | 65.0–70.5 | |
| 40+ | 411 | 82.7 | 78.6–86.2 | 73.9 | 69.1–78.1 | 66.2 | 60.7–71.0 | 50.6 | 43.2–57.5 | |
| All Ages | 6,139 | 90.0 | 89.2–90.7 | 83.5 | 82.5–84.4 | 73.7 | 72.4–74.8 | 66.1 | 64.7–67.5 | |
| Atypical Teratoid/Rhabdoid Tumor | 0–14 | 1,044 | 74.5 | 71.7–77.0 | 59.7 | 56.6–62.7 | 47.8 | 44.6–51.0 | 43.4 | 40.0–46.6 |
| 15–39 | 447 | 83.2 | 79.3–86.3 | 63.3 | 58.5–67.7 | 41.5 | 36.5–46.3 | 34.2 | 29.2–39.1 | |
| 40+ | 331 | 56.0 | 50.3–61.2 | 36.4 | 31.0–41.8 | 24.6 | 19.7–29.9 | 19.5 | 14.8–24.8 | |
| All Ages | 1,822 | 73.3 | 71.2–75.3 | 56.4 | 54.0–58.7 | 42.1 | 39.7–44.5 | 37.0 | 34.6–39.5 | |
| Primitive Neuroectodermal Tumors | 0–14 | 897 | 52.9 | 49.5–56.2 | 39.8 | 36.4–43.1 | 32.1 | 28.7–35.4 | 29.8 | 26.3–33.3 |
| 15–39 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 40+ | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| All Ages | 945 | 53.4 | 50.1–56.6 | 40.4 | 37.1–43.7 | 32.4 | 29.2–35.7 | 30.0 | 26.6–33.4 | |
| Nerve sheath tumors | 0–14 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 15–39 | 151 | 83.3 | 76.2–88.4 | 77.7 | 70.0–83.7 | 73.4 | 65.3–79.9 | 68.6 | 59.7–76.0 | |
| 40+ | 433 | 87.5 | 83.6–90.4 | 82.3 | 77.8–85.9 | 78.7 | 73.7–82.9 | 77.9 | 71.1–83.4 | |
| All Ages | 625 | 86.4 | 83.3–89.0 | 80.8 | 77.2–83.9 | 77.1 | 73.1–80.6 | 75.4 | 70.2–79.8 | |
| Meningioma | 0–14 | 57 | 92.6 | 81.3–97.2 | 82.2 | 68.5–90.4 | 75.3 | 60.4–85.2 | 72.5 | 56.9–83.2 |
| 15–39 | 385 | 94.2 | 91.3–96.2 | 91.2 | 87.7–93.7 | 84.1 | 79.6–87.6 | 78.4 | 72.9–82.9 | |
| 40+ | 4,250 | 83.4 | 82.1–84.6 | 77.1 | 75.6–78.5 | 66.6 | 64.8–68.4 | 60.0 | 57.5–62.3 | |
| All Ages | 4,692 | 84.4 | 83.2–85.5 | 78.4 | 77.0–79.7 | 68.2 | 66.5–69.9 | 61.7 | 59.5–63.8 | |
| Mesenchymal tumors | 0–14 | 132 | 80.3 | 72.3–86.3 | 68.3 | 59.1–75.8 | 61.5 | 51.9–69.7 | 55.0 | 44.4–64.4 |
| 15–39 | 257 | 89.6 | 85.0–92.8 | 84.4 | 79.1–88.5 | 74.0 | 67.6–79.4 | 63.5 | 55.5–70.4 | |
| 40+ | 574 | 83.4 | 79.9–86.4 | 76.8 | 72.7–80.2 | 62.1 | 57.1–66.6 | 48.3 | 42.1–54.3 | |
| All Ages | 963 | 84.7 | 82.1–86.9 | 77.6 | 74.7–80.3 | 65.3 | 61.6–68.6 | 53.5 | 49.0–57.7 | |
| Primary melanocytic lesions | 0–14 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 15–39 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 40+ | 108 | 57.3 | 47.1–66.3 | 39.0 | 29.2–48.6 | 27.7 | 18.5–37.5 | 18.4 | 8.5–31.2 | |
| All Ages | 156 | 52.9 | 44.5–60.5 | 38.2 | 30.2–46.1 | 28.9 | 21.3–37.0 | 22.6 | 14.6–31.7 | |
| Lymphoma | 0–14 | 80 | 89.8 | 80.7–94.8 | 83.2 | 72.8–89.9 | 78.9 | 67.7–86.5 | 73.2 | 60.7–82.2 |
| 15–39 | 1,647 | 60.0 | 57.6–62.4 | 56.3 | 53.8–58.7 | 50.8 | 48.2–53.3 | 47.0 | 44.2–49.7 | |
| 40+ | 15,028 | 52.6 | 51.8–53.4 | 44.1 | 43.2–44.9 | 33.2 | 32.3–34.1 | 24.7 | 23.7–25.8 | |
| All Ages | 16,755 | 53.5 | 52.8–54.3 | 45.5 | 44.7–46.3 | 35.3 | 34.5–36.1 | 27.5 | 26.5–28.5 | |
| Other hematopoietic neoplasms | 0–14 | 76 | 94.4 | 85.8–97.9 | 94.4 | 85.8–97.9 | 94.4 | 85.8–97.9 | 94.4 | 85.8–97.9 |
| 15–39 | 71 | 92.8 | 83.5–97.0 | 86.7 | 75.7–92.9 | 76.5 | 61.6–86.3 | 76.5 | 61.6–86.3 | |
| 40+ | 273 | 76.8 | 71.0–81.5 | 66.0 | 59.6–71.7 | 54.1 | 47.0–60.6 | 52.4 | 45.1–59.1 | |
| All Ages | 420 | 82.6 | 78.5–86.1 | 74.4 | 69.6–78.6 | 64.5 | 58.9–69.6 | 63.2 | 57.3–68.5 | |
| Germ cell tumors, cysts, and heterotopias | 0–14 | 1,208 | 92.8 | 91.2–94.2 | 90.2 | 88.3–91.8 | 87.0 | 84.8–88.9 | 83.9 | 81.2–86.2 |
| 15–39 | 1,413 | 94.2 | 92.8–95.3 | 91.4 | 89.7–92.8 | 87.7 | 85.7–89.5 | 85.7 | 83.3–87.7 | |
| 40+ | 85 | 77.7 | 66.9–85.3 | 71.8 | 60.4–80.5 | 64.1 | 51.9–73.9 | 56.9 | 41.7–69.6 | |
| All Ages | 2,706 | 93.0 | 92.0–94.0 | 90.2 | 89.0–91.3 | 86.6 | 85.2–88.0 | 84.0 | 82.3–85.6 | |
| Tumors of the pituitary | 0–14 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 15–39 | 92 | 97.9 | 91.2–99.5 | 96.8 | 89.6–99.0 | 88.9 | 79.0–94.3 | 88.9 | 79.0–94.3 | |
| 40+ | 343 | 88.2 | 83.8–91.4 | 86.5 | 81.7–90.2 | 80.0 | 73.5–85.0 | 75.8 | 66.7–82.7 | |
| All Ages | 439 | 90.3 | 86.8–92.9 | 88.8 | 84.9–91.8 | 82.1 | 76.8–86.3 | 79.3 | 72.2–84.7 | |
| Neoplasm, unspecified | 0–14 | 339 | 62.1 | 56.7–67.1 | 57.3 | 51.7–62.4 | 53.5 | 47.9–58.9 | 51.4 | 45.6–56.9 |
| 15–39 | 768 | 76.3 | 73.0–79.2 | 72.0 | 68.6–75.1 | 65.2 | 61.5–68.6 | 60.0 | 55.9–63.9 | |
| 40+ | 8,931 | 26.8 | 25.8–27.7 | 21.7 | 20.8–22.6 | 16.8 | 15.9–17.8 | 14.9 | 13.9–15.9 | |
| All Ages | 10,038 | 31.9 | 31.0–32.9 | 26.9 | 26.0–27.9 | 22.0 | 21.1–23.0 | 19.9 | 18.9–20.9 | |
| TOTAL g | 0–14 | 30,711 | 87.4 | 87.0–87.7 | 80.2 | 79.7–80.6 | 74.7 | 74.2–75.2 | 71.6 | 71.0–72.1 |
| 15–39 | 45,462 | 90.5 | 90.2–90.7 | 82.8 | 82.4–83.2 | 71.3 | 70.9–71.8 | 60.8 | 60.3–61.4 | |
| 40+ | 201,102 | 48.9 | 48.7–49.1 | 32.0 | 31.8–32.2 | 21.3 | 21.1–21.5 | 17.2 | 17.0–17.4 | |
| All Ages | 277,275 | 60.1 | 59.9–60.3 | 45.9 | 45.7–46.1 | 35.8 | 35.6–36.0 | 30.8 | 30.6–31.0 |
a. The cohort analysis of survival rates was utilized for calculating the survival estimates presented in this table. Long-term cohort-based survival estimates reflect the survival experience of individuals diagnosed over a specific time period, and they may not necessarily reflect the long-term survival outlook of newly diagnosed cases.
b. Rates are estimates of the percentage of patients alive at one, two, five, and ten years, respectively.
c. Total number of cases that occurred within the NPCR registries between 2001 and 2015.
d. While pilocytic astrocytoma is listed as a tumor of uncertain behavior (/2), the cancer registry community historically codes this histology as a malignant tumor and as a result they are included in this table. e. Children as defined by the National Cancer Institute, see: https://www.cancer.gov/research/areas/childhood.
f. Adolescents and Young Adults (AYA), as defined by the National Cancer Institute, see: https://www.cancer.gov/types/aya.
g. Total includes histologies not listed in this table.
- Rates were not presented for categories with 50 or fewer cases and were suppressed for rates where fewer than 16 cases were surviving within a category.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; CI, Confidence Interval; NOS, Not otherwise specified
Table 22.
One-, two-, five-, and ten-year relative survival ratesa,b with 95% confidence intervals for selected malignant brain and other central nervous system tumors by selected age-groups, U.S. Cancer Statistics – NPCR Registries, 2001–2015
| Histology | Age- group (years) | Nc | 1-Year | 2-Year | 5-Year | 10-Year | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |||
| Pilocytic astrocytomad | 0–19 | 9,749 | 98.8 | 98.6–99.0 | 98.3 | 98.0–98.6 | 96.9 | 96.5–97.3 | 95.7 | 95.2–96.2 |
| 20–44 | 2,684 | 97.1 | 96.4–97.7 | 95.5 | 94.5–96.2 | 92.3 | 91.1–93.3 | 89.5 | 88.0–90.9 | |
| 45–54 | 498 | 94.6 | 92.1–96.3 | 88.8 | 85.4–91.4 | 80.4 | 76.0–84.1 | 77.5 | 72.1–82.1 | |
| 55–64 | 301 | 91.1 | 87.0–94.0 | 85.0 | 80.0–88.9 | 74.0 | 67.5–79.4 | 73.6 | 65.2–80.3 | |
| 65–74 | 164 | 82.1 | 74.8–87.4 | 76.5 | 68.3–82.9 | 68.3 | 58.2–76.5 | 63.4 | 51.9–72.9 | |
| 75+ | 88 | 83.0 | 71.3–90.2 | 76.2 | 62.8–85.4 | 67.0 | 50.8–78.9 | 67.0 | 50.8–78.9 | |
| Diffuse astrocytoma | 0–19 | 3,128 | 93.0 | 92.0–93.9 | 87.3 | 86.0–88.5 | 82.8 | 81.3–84.1 | 79.9 | 78.3–81.4 |
| 20–44 | 7,551 | 94.0 | 93.4–94.5 | 87.9 | 87.1–88.6 | 73.1 | 72.0–74.2 | 55.0 | 53.5–56.5 | |
| 45–54 | 3,366 | 78.8 | 77.4–80.2 | 64.4 | 62.7–66.0 | 46.3 | 44.4–48.1 | 35.1 | 33.0–37.2 | |
| 55–64 | 3,104 | 61.0 | 59.2–62.7 | 42.1 | 40.3–43.9 | 26.1 | 24.4–27.9 | 18.4 | 16.6–20.4 | |
| 65–74 | 2,442 | 43.6 | 41.5–45.6 | 26.5 | 24.7–28.4 | 15.5 | 13.9–17.3 | 10.3 | 8.5–12.2 | |
| 75+ | 1,952 | 22.0 | 20.1–24.0 | 12.7 | 11.1–14.3 | 7.7 | 6.3–9.4 | 5.3 | 3.5–7.7 | |
| Anaplastic astrocytoma | 0–19 | 951 | 70.1 | 67.0–72.9 | 41.8 | 38.5–45.1 | 27.8 | 24.7–30.9 | 22.9 | 19.8–26.2 |
| 20–44 | 4,890 | 89.6 | 88.7–90.4 | 77.0 | 75.7–78.2 | 57.9 | 56.3–59.5 | 43.0 | 41.1–44.8 | |
| 45–54 | 2,683 | 73.1 | 71.3–74.8 | 50.0 | 48.0–52.0 | 29.1 | 27.1–31.0 | 22.1 | 20.1–24.1 | |
| 55–64 | 2,881 | 55.9 | 54.0–57.8 | 32.4 | 30.6–34.2 | 15.3 | 13.8–16.9 | 9.8 | 8.3–11.5 | |
| 65–74 | 2,290 | 37.5 | 35.4–39.5 | 17.7 | 16.0–19.4 | 7.7 | 6.4–9.1 | 4.8 | 3.5–6.4 | |
| 75+ | 1,529 | 18.9 | 16.9–21.0 | 7.6 | 6.2–9.1 | 2.9 | 1.9–4.3 | 1.9 | 1.0–3.3 | |
| Unique astrocytoma variants | 0–19 | 596 | 95.7 | 93.7–97.1 | 90.4 | 87.6–92.6 | 80.6 | 76.8–83.8 | 76.5 | 72.1–80.3 |
| 20–44 | 529 | 92.3 | 89.6–94.3 | 86.6 | 83.2–89.3 | 74.5 | 69.9–78.4 | 70.7 | 65.7–75.2 | |
| 45–54 | 163 | 77.2 | 69.8–83.0 | 55.5 | 47.2–63.0 | 39.4 | 31.2–47.5 | 31.4 | 22.6–40.6 | |
| 55–64 | 155 | 62.7 | 54.4–70.0 | 44.3 | 36.0–52.4 | 29.1 | 21.3–37.4 | 21.4 | 13.3–30.6 | |
| 65–74 | 126 | 36.5 | 27.9–45.1 | 27.1 | 19.1–35.7 | -- | -- | -- | -- | |
| 75+ | 124 | 34.4 | 25.6–43.4 | 26.3 | 17.8–35.5 | -- | -- | -- | -- | |
| Glioblastoma | 0–19 | 1,659 | 62.5 | 60.0–64.8 | 36.1 | 33.7–38.6 | 20.8 | 18.7–23.0 | 16.6 | 14.5–18.8 |
| 20–44 | 10,448 | 71.8 | 70.9–72.7 | 43.6 | 42.6–44.6 | 21.9 | 21.0–22.8 | 15.2 | 14.3–16.1 | |
| 45–54 | 20,730 | 58.6 | 57.9–59.2 | 27.1 | 26.4–27.7 | 9.3 | 8.9–9.8 | 5.7 | 5.3–6.2 | |
| 55–64 | 34,309 | 47.4 | 46.9–48.0 | 19.9 | 19.4–20.3 | 5.9 | 5.6–6.2 | 3.5 | 3.2–3.8 | |
| 65–74 | 31,664 | 31.2 | 30.7–31.7 | 12.1 | 11.7–12.5 | 3.9 | 3.6–4.1 | 3.0 | 2.7–3.3 | |
| 75+ | 25,107 | 13.4 | 12.9–13.8 | 4.8 | 4.5–5.2 | 1.9 | 1.7–2.2 | 1.9 | 1.7–2.2 | |
| Oligodendroglioma | 0–19 | 646 | 98.0 | 96.5–98.8 | 96.7 | 94.9–97.8 | 94.8 | 92.6–96.3 | 89.7 | 86.4–92.3 |
| 20–44 | 5,552 | 98.3 | 97.9–98.7 | 96.5 | 96.0–97.0 | 90.1 | 89.1–90.9 | 75.1 | 73.5–76.6 | |
| 45–54 | 2,324 | 95.3 | 94.3–96.1 | 91.3 | 90.0–92.5 | 82.0 | 80.2–83.8 | 68.0 | 65.3–70.6 | |
| 55–64 | 1,370 | 89.9 | 88.1–91.5 | 80.4 | 78.0–82.5 | 69.4 | 66.5–72.2 | 54.4 | 50.4–58.2 | |
| 65–74 | 579 | 78.5 | 74.7–81.8 | 68.5 | 64.2–72.5 | 52.3 | 47.2–57.2 | 35.7 | 29.2–42.3 | |
| 75+ | 277 | 56.0 | 49.5–62.1 | 43.7 | 37.0–50.1 | 31.9 | 24.7–39.2 | 14.7 | 8.5–22.6 | |
| Anaplastic oligodendroglioma | 0–19 | 115 | 85.1 | 77.1–90.5 | 65.8 | 56.1–73.8 | 49.5 | 39.5–58.7 | 39.7 | 29.8–49.4 |
| 20–44 | 1,855 | 95.4 | 94.3–96.3 | 88.9 | 87.3–90.3 | 75.8 | 73.5–77.8 | 61.6 | 58.7–64.4 | |
| 45–54 | 1,140 | 91.2 | 89.3–92.8 | 80.4 | 77.9–82.8 | 66.6 | 63.4–69.7 | 50.0 | 45.9–53.9 | |
| 55–64 | 937 | 79.9 | 77.0–82.4 | 62.0 | 58.6–65.2 | 45.0 | 41.3–48.6 | 34.7 | 30.3–39.0 | |
| 65–74 | 456 | 63.9 | 59.1–68.3 | 47.1 | 42.0–52.0 | 30.3 | 25.2–35.5 | 21.1 | 15.5–27.3 | |
| 75+ | 215 | 43.4 | 36.3–50.3 | 26.8 | 20.5–33.5 | 17.4 | 11.4–24.5 | 13.1 | 6.0–23.0 | |
| Oligoastrocytic tumors | 0–19 | 355 | 92.0 | 88.7–94.5 | 84.3 | 80.0–87.8 | 78.4 | 73.4–82.5 | 71.2 | 65.4–76.2 |
| 20–44 | 3,935 | 96.9 | 96.3–97.4 | 92.4 | 91.5–93.3 | 78.7 | 77.2–80.0 | 59.3 | 57.1–61.3 | |
| 45–54 | 1,361 | 90.2 | 88.5–91.7 | 80.4 | 78.1–82.5 | 64.7 | 61.8–67.4 | 48.5 | 44.8–52.2 | |
| 55–64 | 965 | 78.3 | 75.5–80.9 | 57.3 | 54.0–60.5 | 39.7 | 36.2–43.1 | 31.8 | 27.9–35.8 | |
| 65–74 | 475 | 61.4 | 56.7–65.8 | 42.1 | 37.4–46.8 | 26.0 | 21.5–30.8 | 15.6 | 10.6–21.5 | |
| 75+ | 208 | 30.5 | 24.1–37.1 | 18.2 | 12.9–24.3 | 10.1 | 5.7–16.1 | -- | -- | |
| Ependymal tumors | 0–19 | 2,734 | 95.2 | 94.3–96.0 | 89.8 | 88.5–90.9 | 78.9 | 77.1–80.5 | 69.9 | 67.7–72.0 |
| 20–44 | 3,231 | 97.1 | 96.4–97.6 | 95.2 | 94.3–95.9 | 91.9 | 90.7–92.9 | 88.7 | 87.2–90.1 | |
| 45–54 | 1,835 | 95.8 | 94.7–96.7 | 93.5 | 92.2–94.7 | 89.5 | 87.7–91.0 | 86.1 | 83.6–88.3 | |
| 55–64 | 1,353 | 92.5 | 90.8–93.8 | 90.4 | 88.5–92.0 | 87.3 | 84.8–89.3 | 84.5 | 80.9–87.5 | |
| 65–74 | 785 | 88.6 | 85.9–90.9 | 82.7 | 79.3–85.5 | 77.9 | 73.6–81.6 | 69.0 | 61.9–75.0 | |
| 75+ | 337 | 77.8 | 72.3–82.4 | 76.7 | 70.4–81.8 | 72.8 | 63.7–80.0 | 61.5 | 47.2–73.0 | |
| Glioma malignant, NOS | 0–19 | 6,852 | 82.5 | 81.5–83.4 | 72.4 | 71.3–73.5 | 69.3 | 68.2–70.5 | 68.0 | 66.8–69.2 |
| 20–44 | 3,344 | 90.0 | 88.9–91.0 | 83.4 | 82.0–84.6 | 73.2 | 71.5–74.8 | 64.0 | 61.8–66.1 | |
| 45–54 | 1,621 | 77.1 | 74.9–79.1 | 66.2 | 63.8–68.6 | 55.9 | 53.2–58.6 | 48.0 | 44.8–51.1 | |
| 55–64 | 1,522 | 62.3 | 59.7–64.7 | 50.5 | 47.9–53.1 | 37.6 | 34.8–40.4 | 29.1 | 25.9–32.4 | |
| 65–74 | 1,464 | 41.9 | 39.3–44.5 | 31.4 | 28.9–33.9 | 23.1 | 20.6–25.7 | 18.7 | 15.6–22.0 | |
| 75+ | 2,560 | 19.1 | 17.5–20.7 | 14.6 | 13.1–16.1 | 10.2 | 8.6–11.8 | 7.9 | 5.9–10.1 | |
| Neuronal and mixed neuronal-glial tumors | 0–19 | 282 | 91.7 | 87.7–94.4 | 84.3 | 79.3–88.2 | 78.3 | 72.7–82.9 | 76.8 | 70.9–81.6 |
| 20–44 | 598 | 95.1 | 93.0–96.6 | 90.2 | 87.4–92.4 | 82.6 | 78.8–85.7 | 74.3 | 69.4–78.6 | |
| 45–54 | 419 | 94.8 | 92.0–96.6 | 89.5 | 85.8–92.2 | 83.3 | 78.6–87.0 | 79.4 | 73.1–84.3 | |
| 55–64 | 391 | 90.0 | 86.3–92.7 | 81.6 | 77.0–85.4 | 72.3 | 66.5–77.2 | 64.4 | 56.6–71.2 | |
| 65–74 | 245 | 89.3 | 84.0–92.9 | 86.2 | 80.1–90.6 | 79.4 | 70.9–85.6 | 66.1 | 54.0–75.8 | |
| 75+ | 165 | 75.1 | 66.6–81.7 | 68.1 | 58.5–76.0 | 56.6 | 44.3–67.3 | 34.8 | 18.0–52.2 | |
| Tumors of the pineal region | 0–19 | 422 | 87.2 | 83.5–90.1 | 78.0 | 73.5–81.8 | 64.3 | 59.0–69.1 | 57.2 | 51.3–62.6 |
| 20–44 | 290 | 92.9 | 89.2–95.4 | 85.9 | 81.0–89.6 | 74.9 | 68.6–80.1 | 68.7 | 61.0–75.2 | |
| 45–54 | 116 | 86.6 | 78.6–91.8 | 77.0 | 67.5–84.0 | 70.4 | 59.6–78.8 | 60.1 | 47.3–70.8 | |
| 55–64 | 81 | 85.1 | 74.5–91.5 | 81.4 | 70.0–88.8 | 64.6 | 50.2–75.8 | 47.6 | 28.7–64.3 | |
| 65–74 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 75+ | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| Embryonal tumors | 0–19 | 7,089 | 82.5 | 81.6–83.4 | 73.4 | 72.3–74.4 | 63.6 | 62.4–64.8 | 58.5 | 57.1–59.8 |
| 20–44 | 1,899 | 88.8 | 87.3–90.2 | 80.9 | 79.0–82.7 | 68.3 | 66.0–70.6 | 58.3 | 55.6–61.0 | |
| 45–54 | 308 | 75.6 | 70.3–80.1 | 61.0 | 55.1–66.4 | 51.3 | 45.0–57.2 | 40.1 | 32.8–47.2 | |
| 55–64 | 188 | 62.1 | 54.5–68.8 | 48.5 | 40.8–55.8 | 35.8 | 28.1–43.5 | 23.7 | 16.1–32.3 | |
| 65–74 | 78 | 45.3 | 33.6–56.2 | 23.1 | 13.9–33.7 | -- | -- | -- | -- | |
| 75+ | 64 | 28.9 | 17.9–40.9 | -- | -- | -- | -- | -- | -- | |
| Nerve sheath tumors | 0–19 | 58 | 89.4 | 77.9–95.1 | 81.9 | 68.9–89.9 | 80.0 | 66.6–88.4 | 77.3 | 62.9–86.7 |
| 20–44 | 180 | 84.3 | 78.0–88.9 | 78.4 | 71.5–83.9 | 73.6 | 66.1–79.6 | 70.7 | 62.7–77.3 | |
| 45–54 | 139 | 90.1 | 83.5–94.1 | 85.0 | 77.5–90.2 | 82.1 | 74.1–87.9 | 81.2 | 71.4–88.0 | |
| 55–64 | 105 | 84.1 | 75.2–90.0 | 78.6 | 68.8–85.6 | 75.1 | 64.2–83.1 | 73.1 | 59.5–82.7 | |
| 65–74 | 86 | 94.6 | 84.7–98.2 | 91.2 | 79.5–96.3 | 85.7 | 69.1–93.7 | 83.8 | 63.2–93.5 | |
| 75+ | 57 | 73.1 | 57.5–83.7 | 65.2 | 48.2–77.7 | 58.6 | 39.4–73.6 | 58.6 | 39.4–73.6 | |
| Meningioma | 0–19 | 89 | 91.8 | 83.5–96.0 | 84.0 | 74.0–90.5 | 79.7 | 68.8–87.1 | 78.0 | 66.6–85.9 |
| 20–44 | 600 | 94.0 | 91.7–95.7 | 91.7 | 89.0–93.7 | 84.0 | 80.5–86.9 | 76.8 | 72.5–80.6 | |
| 45–54 | 747 | 91.7 | 89.3–93.5 | 86.1 | 83.2–88.5 | 79.4 | 75.9–82.4 | 74.9 | 70.7–78.5 | |
| 55–64 | 991 | 89.7 | 87.5–91.5 | 84.2 | 81.6–86.5 | 73.8 | 70.4–76.8 | 65.3 | 61.0–69.3 | |
| 65–74 | 1,036 | 84.5 | 82.0–86.8 | 77.7 | 74.7–80.4 | 63.3 | 59.4–66.9 | 57.9 | 53.0–62.4 | |
| 75+ | 1,229 | 69.5 | 66.5–72.3 | 61.3 | 57.9–64.6 | 50.2 | 45.9–54.4 | 39.5 | 32.8–46.0 | |
| Mesenchymal tumors | 0–19 | 169 | 82.4 | 75.6–87.4 | 71.2 | 63.5–77.6 | 61.2 | 52.8–68.6 | 54.1 | 44.9–62.5 |
| 20–44 | 301 | 88.0 | 83.7–91.3 | 84.0 | 79.2–87.9 | 74.5 | 68.6–79.5 | 61.1 | 53.6–67.9 | |
| 45–54 | 179 | 90.7 | 85.1–94.2 | 83.7 | 77.1–88.6 | 75.5 | 67.4–81.8 | 63.6 | 53.6–72.0 | |
| 55–64 | 154 | 85.3 | 78.4–90.2 | 77.2 | 69.1–83.4 | 58.5 | 48.3–67.4 | 47.7 | 35.0–59.4 | |
| 65–74 | 97 | 82.0 | 71.9–88.7 | 76.2 | 64.9–84.2 | 49.7 | 35.8–62.1 | 24.5 | 8.6–44.6 | |
| 75+ | 63 | 58.8 | 44.6–70.6 | 49.5 | 34.8–62.6 | 30.4 | 16.5–45.4 | -- | -- | |
| Other neoplasms related to the meninges |
0–19 | 62 | 95.0 | 85.3–98.4 | 89.7 | 78.5–95.3 | 85.5 | 72.8–92.6 | 77.9 | 62.9–87.4 |
| 20–44 | 224 | 96.0 | 92.3–98.0 | 91.7 | 86.9–94.8 | 86.5 | 80.5–90.8 | 76.7 | 68.0–83.2 | |
| 45–54 | 125 | 95.3 | 89.2–98.0 | 93.9 | 87.0–97.2 | 87.7 | 78.5–93.1 | 76.8 | 63.9–85.5 | |
| 55–64 | 116 | 90.3 | 82.8–94.7 | 84.6 | 75.8–90.4 | 67.0 | 55.9–76.0 | 41.5 | 27.8–54.7 | |
| 65–74 | 103 | 95.0 | 86.2–98.2 | 90.4 | 80.1–95.5 | 84.4 | 70.5–92.1 | 58.5 | 40.0–73.2 | |
| 75+ | 74 | 85.0 | 71.5–92.4 | 79.1 | 63.2–88.7 | 61.3 | 41.3–76.3 | 48.4 | 28.8–65.5 | |
| Lymphoma | 0–19 | 164 | 86.1 | 79.7–90.7 | 80.6 | 73.4–86.1 | 76.0 | 68.2–82.2 | 72.1 | 63.6–79.0 |
| 20–44 | 2,413 | 57.1 | 55.1–59.1 | 52.6 | 50.5–54.6 | 45.9 | 43.8–48.0 | 41.0 | 38.7–43.2 | |
| 45–54 | 2,488 | 64.6 | 62.6–66.5 | 56.8 | 54.7–58.8 | 46.3 | 44.1–48.4 | 35.8 | 33.4–38.2 | |
| 55–64 | 3,688 | 63.4 | 61.8–65.0 | 54.7 | 53.0–56.4 | 42.1 | 40.3–44.0 | 30.6 | 28.4–32.8 | |
| 65–74 | 4,348 | 52.6 | 51.1–54.2 | 43.1 | 41.5–44.7 | 30.1 | 28.5–31.8 | 21.5 | 19.5–23.6 | |
| 75+ | 3,654 | 32.4 | 30.8–34.0 | 23.9 | 22.4–25.5 | 15.8 | 14.3–17.5 | 11.3 | 9.1–13.7 | |
| Other hematopoietic neoplasms | 0–19 | 92 | 92.0 | 83.9–96.1 | 92.0 | 83.9–96.1 | 90.2 | 81.0–95.1 | 90.2 | 81.0–95.1 |
| 20–44 | 89 | 88.7 | 79.8–93.8 | 81.5 | 71.3–88.3 | 74.4 | 62.3–83.2 | 72.4 | 59.6–81.7 | |
| 45–54 | 65 | 86.3 | 74.9–92.8 | 75.3 | 62.4–84.3 | 67.2 | 53.2–77.9 | 60.5 | 44.1–73.5 | |
| 55–64 | 74 | 85.3 | 74.3–91.9 | 72.3 | 59.5–81.6 | 62.1 | 48.1–73.4 | 62.1 | 48.1–73.4 | |
| 65–74 | 63 | 64.5 | 50.9–75.2 | 54.0 | 40.2–65.9 | 40.9 | 26.9–54.5 | 36.5 | 22.4–50.8 | |
| 75+ | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| Tumors of the pituitary | 0–19 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 20–44 | 134 | 95.6 | 90.2–98.0 | 94.2 | 88.2–97.2 | 89.1 | 81.5–93.7 | 88.3 | 80.0–93.3 | |
| 45–54 | 86 | 89.6 | 80.4–94.6 | 88.7 | 79.1–94.0 | 78.6 | 66.2–86.9 | 73.1 | 58.8–83.2 | |
| 55–64 | 82 | 86.9 | 76.7–92.8 | 83.4 | 72.2–90.4 | 79.8 | 66.6–88.2 | 79.8 | 66.6–88.2 | |
| 65–74 | 72 | 88.9 | 77.6–94.7 | 88.9 | 77.6–94.7 | 78.8 | 63.2–88.4 | 68.7 | 41.4–85.2 | |
| 75+ | 52 | 82.3 | 65.6–91.5 | 79.5 | 59.6–90.3 | 68.9 | 42.6–85.0 | 52.9 | 27.4–73.0 | |
| Neoplasm, unspecified | 0–19 | 435 | 66.6 | 61.9–70.9 | 61.8 | 56.9–66.2 | 58.5 | 53.5–63.1 | 55.8 | 50.5–60.8 |
| 20–44 | 955 | 71.9 | 68.9–74.7 | 66.9 | 63.7–69.8 | 59.4 | 56.0–62.6 | 55.1 | 51.4–58.6 | |
| 45–54 | 809 | 59.3 | 55.8–62.7 | 51.8 | 48.2–55.3 | 44.2 | 40.5–47.8 | 39.0 | 35.0–42.9 | |
| 55–64 | 1,188 | 42.2 | 39.3–45.0 | 34.1 | 31.3–36.9 | 27.5 | 24.8–30.3 | 24.4 | 21.4–27.4 | |
| 65–74 | 1,567 | 27.8 | 25.6–30.1 | 22.4 | 20.3–24.6 | 16.4 | 14.4–18.6 | 15.0 | 12.8–17.3 | |
| 75+ | 5,084 | 14.6 | 13.6–15.7 | 10.8 | 9.9–11.8 | 7.3 | 6.3–8.3 | 5.7 | 4.6–6.9 | |
| TOTAL e | 0–19 | 37,967 | 88.5 | 88.1–88.8 | 81.3 | 80.9–81.8 | 75.5 | 75.1–76.0 | 72.2 | 71.7–72.7 |
| 20–44 | 52,662 | 87.6 | 87.3–87.9 | 77.8 | 77.4–78.1 | 65.1 | 64.6–65.5 | 54.2 | 53.6–54.7 | |
| 45–54 | 41,351 | 70.1 | 69.7–70.5 | 49.2 | 48.7–49.8 | 34.5 | 34.0–35.0 | 27.9 | 27.4–28.5 | |
| 55–64 | 54,095 | 55.3 | 54.8–55.7 | 33.1 | 32.7–33.5 | 19.8 | 19.4–20.1 | 15.3 | 14.9–15.8 | |
| 65–74 | 48,251 | 38.6 | 38.1–39.0 | 22.1 | 21.7–22.5 | 13.1 | 12.7–13.5 | 10.4 | 9.9–10.8 | |
| 75+ | 42,949 | 19.6 | 19.2–20.0 | 11.8 | 11.5–12.2 | 7.7 | 7.3–8.0 | 6.4 | 6.0–6.9 |
a. The cohort analysis of survival rates was utilized for calculating the survival estimates presented in this table. Long-term cohort-based survival estimates reflect the survival experience of individuals diagnosed over the time period, and they may not necessarily reflect the long-term survival outlook of newly diagnosed cases.
b. Rates are an estimate of the percentage of patients alive at one, two, five, and ten years, respectively.
c. Total number of case that occurred within the NPCR registries between 2001 and 2015.
d. While pilocytic astrocytoma is coded as a tumor of uncertain behavior (/2), the cancer registry community historically codes this histology as a malignant tumor and as a result they are included in this table.
e. Total includes histologies not listed in this table.
- Rates were not presented for categories with 50 or fewer cases and were suppressed for rates where fewer than 16 cases were surviving within a category.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; CI, Confidence Interval; NOS, Not otherwise specified
The estimated five- and ten-year relative survival rates for all malignant brain and other CNS tumors were 35.8% and 30.8%, respectively.
There was large variation in survival estimates depending upon tumor histology; five-year survival rates were 94.4% for pilocytic astrocytoma but are 6.8% for glioblastoma.
Survival generally decreased with older age at diagnosis; children and young adults generally had better survival outcomes for most histologies.
Survival rates for non-malignant brain and other CNS tumors by histology and age
Survival estimates for non-malignant brain and other CNS tumors by histology and age at diagnosis are presented in Table 23, 24. Histology-specific rates are presented for the CBTRUS histology groupings which contain a substantial number of incident non-malignant tumors.
Table 23.
One-, two-, five-, and ten-year relative survival ratesa,b with 95% confidence intervals for selected non-malignant brain and other central nervous system tumors by NCI age-groups, U.S. Cancer Statistics – NPCR Registries, 2004–2015
| Histology | Age-group (years) | Nc | 1-Year | 2-Year | 5-Year | 10-Year | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |||
| Unique astrocytoma variants | 0-14d | 517 | 98.5 | 96.9–99.3 | 97.9 | 96.1–98.8 | 97.3 | 95.3–98.5 | 94.9 | 90.1–97.4 |
| 15-39e | 274 | 97.1 | 94.1–98.5 | 96.3 | 93.1–98.1 | 93.7 | 89.6–96.3 | 89.1 | 82.0–93.6 | |
| 40+ | 64 | 94.0 | 83.3–97.9 | 87.0 | 74.3–93.7 | 83.7 | 69.2–91.7 | 65.7 | 40.4–82.3 | |
| All Ages | 855 | 97.7 | 96.4–98.5 | 96.6 | 95.1–97.7 | 95.3 | 93.4–96.6 | 91.1 | 87.3–93.8 | |
| Ependymal tumors | 0–14 | 229 | 99.1 | 96.3–99.8 | 98.7 | 95.7–99.6 | 96.8 | 92.7–98.6 | 96.0 | 91.3–98.2 |
| 15–39 | 1,879 | 99.5 | 98.9–99.7 | 99.3 | 98.7–99.7 | 98.7 | 97.8–99.3 | 97.5 | 95.7–98.6 | |
| 40+ | 3,761 | 96.6 | 95.8–97.2 | 96.2 | 95.3–96.9 | 95.8 | 94.5–96.8 | 93.3 | 90.7–95.3 | |
| All Ages | 5,869 | 97.6 | 97.1–98.0 | 97.3 | 96.7–97.8 | 96.8 | 95.9–97.5 | 94.8 | 93.2–96.1 | |
| Choroid plexus tumors | 0–14 | 586 | 98.3 | 96.6–99.1 | 97.9 | 96.2–98.8 | 97.0 | 95.0–98.2 | 96.7 | 94.6–98.0 |
| 15–39 | 446 | 98.2 | 96.3–99.1 | 97.8 | 95.7–98.9 | 97.0 | 94.6–98.3 | 93.0 | 87.4–96.2 | |
| 40+ | 517 | 88.8 | 85.5–91.4 | 88.2 | 84.6–91.0 | 84.1 | 79.4–87.8 | 79.4 | 71.5–85.3 | |
| All Ages | 1,549 | 95.1 | 93.8–96.1 | 94.6 | 93.2–95.8 | 92.8 | 91.0–94.3 | 90.1 | 87.2–92.3 | |
| Neuronal and mixed neuronal-glial tumors | 0–14 | 2,329 | 99.2 | 98.7–99.5 | 98.3 | 97.6–98.8 | 96.9 | 96.0–97.6 | 95.8 | 94.4–96.8 |
| 15–39 | 3,527 | 98.8 | 98.3–99.1 | 98.4 | 97.9–98.8 | 97.3 | 96.6–97.9 | 95.1 | 93.7–96.2 | |
| 40+ | 1,991 | 94.8 | 93.6–95.8 | 92.5 | 91.1–93.8 | 89.1 | 87.1–90.8 | 86.5 | 83.2–89.2 | |
| All Ages | 7,847 | 97.9 | 97.5–98.2 | 96.9 | 96.4–97.3 | 95.2 | 94.5–95.7 | 93.2 | 92.1–94.1 | |
| Tumors of the pineal region | 0–14 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 15–39 | 285 | 97.5 | 94.7–98.8 | 97.2 | 94.2–98.6 | 96.8 | 93.4–98.5 | 96.2 | 91.8–98.2 | |
| 40+ | 363 | 92.7 | 89.2–95.2 | 91.0 | 86.8–93.9 | 86.6 | 80.7–90.8 | 79.4 | 68.1–87.1 | |
| All Ages | 697 | 95.1 | 93.0–96.5 | 94.0 | 91.6–95.7 | 91.8 | 88.5–94.1 | 87.7 | 81.7–91.9 | |
| Embryonal tumors | 0–14 | 53 | 100.0 | ** | 100.0 | ** | 100.0 | ** | 95.4 | 69.7–99.4 |
| 15–39 | 85 | 100.0 | ** | 100.0 | ** | 100.0 | ** | 96.3 | 63.5–99.7 | |
| 40+ | 106 | 96.1 | 88.7–98.7 | 96.1 | 88.7–98.7 | 95.4 | 82.8–98.8 | 86.8 | 69.3–94.7 | |
| All Ages | 244 | 98.3 | 95.0–99.5 | 98.3 | 95.0–99.5 | 98.1 | 91.6–99.6 | 91.7 | 82.0–96.3 | |
| Nerve sheath tumors | 0–14 | 1,942 | 99.9 | 99.2–100.0 | 99.7 | 99.2–99.9 | 99.0 | 98.3–99.4 | 98.2 | 97.0–98.8 |
| 15–39 | 10,679 | 99.4 | 99.3–99.6 | 99.2 | 99.0–99.4 | 98.6 | 98.3–98.9 | 97.7 | 97.1–98.2 | |
| 40+ | 56,346 | 99.3 | 99.1–99.4 | 99.3 | 99.1–99.4 | 99.3 | 99.1–99.4 | 99.3 | 99.1–99.4 | |
| All Ages | 68,967 | 99.3 | 99.2–99.4 | 99.3 | 99.2–99.4 | 99.3 | 99.2–99.4 | 99.3 | 99.2–99.4 | |
| Meningioma | 0–14 | 534 | 98.3 | 96.7–99.1 | 97.5 | 95.6–98.5 | 95.7 | 93.3–97.3 | 89.9 | 84.9–93.3 |
| 15–39 | 18,574 | 98.8 | 98.6–98.9 | 98.2 | 98.0–98.4 | 97.0 | 96.7–97.3 | 94.8 | 94.2–95.3 | |
| 40+ | 271,578 | 92.7 | 92.5–92.8 | 90.9 | 90.7–91.0 | 87.3 | 87.1–87.6 | 82.8 | 82.4–83.2 | |
| All Ages | 290,686 | 93.1 | 93.0–93.2 | 91.4 | 91.2–91.5 | 88.0 | 87.8–88.2 | 83.7 | 83.3–84.0 | |
| Mesenchymal tumors | 0–14 | 518 | 99.8 | 96.4–100.0 | 98.6 | 96.8–99.4 | 97.6 | 95.2–98.8 | 96.5 | 93.4–98.2 |
| 15–39 | 571 | 98.8 | 97.4–99.5 | 98.7 | 97.2–99.4 | 97.5 | 95.2–98.7 | 94.8 | 90.2–97.3 | |
| 40+ | 1,364 | 95.1 | 93.5–96.2 | 94.2 | 92.4–95.6 | 89.2 | 86.5–91.4 | 81.3 | 76.2–85.4 | |
| All Ages | 2,453 | 97.0 | 96.0–97.7 | 96.2 | 95.1–97.0 | 92.9 | 91.2–94.2 | 87.4 | 84.2–90.0 | |
| Primary melanocytic lesions | 0–14 | -- | -- | -- | -- | -- | -- | -- | -- | -- |
| 15–39 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 40+ | 60 | 80.3 | 66.8–88.8 | 71.7 | 56.8–82.2 | 55.7 | 38.0–70.1 | 41.2 | 21.3–60.2 | |
| All Ages | 82 | 84.6 | 74.1–91.1 | 78.7 | 67.0–86.7 | 63.3 | 49.2–74.4 | 52.8 | 37.0–66.3 | |
| Other neoplasms related to the meninges | 0–14 | 100 | 98.0 | 92.0–99.5 | 96.9 | 90.4–99.0 | 94.1 | 86.1–97.6 | 84.3 | 66.0–93.2 |
| 15–39 | 1,858 | 98.3 | 97.6–98.8 | 97.7 | 96.9–98.4 | 96.7 | 95.5–97.5 | 93.7 | 91.6–95.3 | |
| 40+ | 3,930 | 95.2 | 94.4–96.0 | 94.5 | 93.5–95.3 | 92.7 | 91.3–93.9 | 88.7 | 86.0–90.9 | |
| All Ages | 5,888 | 96.3 | 95.7–96.8 | 95.5 | 94.9–96.2 | 94.0 | 93.0–94.8 | 90.2 | 88.4–91.8 | |
| Germ cell tumors, cysts, and heterotopias | 0–14 | 356 | 96.9 | 94.4–98.3 | 96.6 | 94.0–98.1 | 96.6 | 94.0–98.1 | 96.2 | 93.1–97.9 |
| 15–39 | 365 | 99.5 | 97.5–99.9 | 98.4 | 96.1–99.3 | 96.8 | 93.7–98.4 | 95.5 | 89.8–98.0 | |
| 40+ | 415 | 94.9 | 91.8–96.8 | 93.8 | 90.1–96.1 | 91.8 | 86.5–95.0 | 83.7 | 73.8–90.1 | |
| All Ages | 1,136 | 97.0 | 95.7–98.0 | 96.2 | 94.6–97.3 | 94.9 | 92.8–96.4 | 91.6 | 87.8–94.2 | |
| Tumors of the pituitary | 0–14 | 1,750 | 99.9 | 99.5–100.0 | 99.7 | 99.2–99.9 | 99.4 | 98.7–99.8 | 98.8 | 97.8–99.4 |
| 15–39 | 38,856 | 99.7 | 99.6–99.7 | 99.6 | 99.5–99.6 | 99.3 | 99.1–99.4 | 98.7 | 98.4–98.9 | |
| 40+ | 88,937 | 97.4 | 97.3–97.5 | 96.9 | 96.7–97.1 | 95.6 | 95.3–95.9 | 93.3 | 92.7–93.9 | |
| All Ages | 129,543 | 98.1 | 98.0–98.2 | 97.7 | 97.6–97.9 | 96.8 | 96.6–97.0 | 95.1 | 94.7–95.5 | |
| Craniopharyngioma | 0–14 | 1,519 | 98.7 | 97.9–99.1 | 97.9 | 97.0–98.5 | 95.2 | 93.8–96.3 | 92.8 | 90.8–94.4 |
| 15–39 | 1,595 | 95.9 | 94.8–96.8 | 94.5 | 93.2–95.5 | 91.3 | 89.6–92.8 | 88.0 | 85.7–90.0 | |
| 40+ | 3,462 | 89.4 | 88.2–90.5 | 86.2 | 84.8–87.4 | 79.4 | 77.6–81.1 | 72.7 | 69.8–75.2 | |
| All Ages | 6,576 | 93.1 | 92.5–93.8 | 90.9 | 90.1–91.7 | 86.1 | 85.0–87.1 | 81.4 | 79.8–82.9 | |
| Hemangioma | 0–14 | 616 | 99.0 | 97.7–99.6 | 98.5 | 97.0–99.2 | 97.8 | 96.0–98.8 | 97.8 | 96.0–98.8 |
| 15–39 | 2,885 | 99.5 | 99.1–99.7 | 99.3 | 98.8–99.6 | 98.8 | 98.1–99.3 | 96.8 | 95.1–98.0 | |
| 40+ | 6,830 | 95.4 | 94.8–96.0 | 94.1 | 93.3–94.8 | 91.6 | 90.4–92.6 | 88.4 | 85.9–90.5 | |
| All Ages | 10,331 | 96.8 | 96.4–97.2 | 95.8 | 95.3–96.3 | 94.0 | 93.3–94.7 | 91.5 | 89.9–92.9 | |
| Neoplasm, unspecified | 0–14 | 888 | 94.7 | 93.0–96.1 | 94.2 | 92.4–95.6 | 93.8 | 91.9–95.3 | 92.4 | 89.7–94.3 |
| 15–39 | 2,943 | 95.7 | 94.8–96.4 | 94.8 | 93.9–95.6 | 93.5 | 92.5–94.5 | 91.9 | 90.4–93.2 | |
| 40+ | 11,065 | 69.5 | 68.6–70.5 | 65.9 | 64.9–66.8 | 60.4 | 59.2–61.6 | 53.2 | 51.5–54.9 | |
| All Ages | 14,896 | 76.3 | 75.6–77.1 | 73.4 | 72.6–74.2 | 69.2 | 68.3–70.2 | 63.8 | 62.5–65.1 | |
| TOTAL f | 0–14 | 12,233 | 98.8 | 98.6–99.0 | 98.2 | 98.0–98.5 | 97.2 | 96.8–97.5 | 95.8 | 95.2–96.2 |
| 15–39 | 85,129 | 99.1 | 99.0–99.2 | 98.8 | 98.7–98.9 | 98.1 | 98.0–98.2 | 96.7 | 96.5–97.0 | |
| 40+ | 451,394 | 93.9 | 93.9–94.0 | 92.6 | 92.5–92.7 | 90.1 | 89.9–90.2 | 86.8 | 86.5–87.1 | |
| All Ages | 548,756 | 94.9 | 94.8–95.0 | 93.7 | 93.6–93.8 | 91.5 | 91.4–91.7 | 88.7 | 88.5–88.9 |
a. The cohort analysis of survival rates was utilized for calculating the survival estimates presented in this table. Long-term cohort-based survival estimates reflect the survival experience of individuals diagnosed over the time period, and they may not necessarily reflect the long-term survival outlook of newly diagnosed cases.
b. Rates are an estimate of the percentage of patients alive at one, two, five, and ten years, respectively.
c. Total number of case that occurred within the NPCR registries between 2004 and 2015.
d. Children as defined by the National Cancer Institute, see: https://www.cancer.gov/research/areas/childhood.
e. Adolescents and Young Adults (AYA), as defined by the National Cancer Institute, see: https://www.cancer.gov/types/aya.
f. Total includes histologies not listed in this table.
- Rates were not presented for categories with 50 or fewer cases and were suppressed for rates where fewer than 16 cases were surviving within a category.
** Confidence interval could not be calculated.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; CI, Confidence Interval; NOS, Not otherwise specified
Table 24.
Brain and other central nervous system one-, two-, five-, and ten-year relative survival ratesa,b with 95% confidence intervals for selected non-malignant brain and other central nervous system tumors by selected age-groups, U.S. Cancer Statistics – NPCR Registries, 2004–2015
| Histology | Age group (year) | Nc | 1-Year | 2-Year | 5-Year | 10-Year | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |||
| Unique astrocytoma variants | 0–19 | 617 | 98.7 | 97.4–99.4 | 97.9 | 96.3–98.8 | 97.0 | 95.2–98.2 | 94.7 | 90.5–97.1 |
| 20–44 | 193 | 95.3 | 91.0–97.6 | 95.3 | 91.0–97.6 | 92.5 | 87.0–95.7 | 87.3 | 78.2–92.8 | |
| 45–54 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 55–64 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 65–74 | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| 75+ | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| Ependymal tumors | 0–19 | 426 | 99.6 | 98.0–99.9 | 99.3 | 97.6–99.8 | 98.5 | 96.2–99.4 | 97.5 | 93.8–99.0 |
| 20–44 | 2,223 | 99.2 | 98.7–99.6 | 99.1 | 98.5–99.5 | 98.6 | 97.7–99.1 | 97.3 | 95.5–98.4 | |
| 45–54 | 1,300 | 98.5 | 97.5–99.1 | 98.4 | 97.2–99.1 | 98.0 | 96.6–98.8 | 97.1 | 93.2–98.8 | |
| 55–64 | 1,007 | 96.7 | 95.1–97.8 | 96.2 | 94.3–97.4 | 94.0 | 91.2–96.0 | 92.3 | 86.6–95.6 | |
| 65–74 | 634 | 93.5 | 90.9–95.5 | 91.8 | 88.6–94.2 | 91.8 | 88.6–94.2 | 84.9 | 72.9–91.9 | |
| 75+ | 279 | 89.5 | 83.7–93.3 | 89.5 | 83.7–93.3 | 89.2 | 78.2–94.9 | 81.1 | 59.6–91.9 | |
| Choroid plexus tumors | 0–19 | 689 | 98.4 | 97.0–99.1 | 98.1 | 96.6–98.9 | 97.3 | 95.6–98.4 | 96.8 | 94.8–98.1 |
| 20–44 | 424 | 97.9 | 95.8–98.9 | 97.2 | 94.8–98.5 | 95.9 | 93.0–97.7 | 92.2 | 86.4–95.6 | |
| 45–54 | 166 | 94.8 | 89.7–97.4 | 94.5 | 89.0–97.2 | 90.1 | 82.8–94.4 | 83.1 | 70.3–90.7 | |
| 55–64 | 127 | 86.7 | 79.0–91.7 | 86.5 | 78.4–91.7 | 83.9 | 74.0–90.3 | 76.4 | 62.7–85.6 | |
| 65–74 | 81 | 81.1 | 70.0–88.5 | 79.8 | 67.8–87.7 | 72.9 | 57.0–83.7 | 64.5 | 37.5–82.3 | |
| 75+ | 62 | 75.5 | 60.8–85.3 | 74.6 | 57.9–85.5 | 68.4 | 49.8–81.2 | -- | -- | |
| Neuronal and mixed neuronal-glial tumors | 0–19 | 3,453 | 99.3 | 98.9–99.5 | 98.5 | 98.0–98.9 | 97.4 | 96.7–98.0 | 95.9 | 94.8–96.8 |
| 20–44 | 2,805 | 98.4 | 97.8–98.8 | 97.9 | 97.2–98.4 | 96.5 | 95.5–97.2 | 94.4 | 92.8–95.7 | |
| 45–54 | 729 | 96.7 | 95.0–97.8 | 95.2 | 93.2–96.7 | 92.1 | 89.2–94.3 | 88.9 | 83.6–92.5 | |
| 55–64 | 494 | 93.5 | 90.7–95.5 | 90.0 | 86.5–92.7 | 85.7 | 81.0–89.2 | 81.9 | 74.8–87.2 | |
| 65–74 | 250 | 90.7 | 85.7–94.0 | 87.0 | 81.0–91.2 | 80.2 | 71.9–86.3 | 75.1 | 57.7–86.1 | |
| 75+ | 116 | 85.8 | 76.1–91.8 | 83.0 | 71.3–90.2 | 80.9 | 64.9–90.2 | 76.3 | 38.0–92.7 | |
| Tumors of the pineal region | 0–19 | 90 | 98.9 | 91.7–99.8 | 98.9 | 91.7–99.8 | 98.9 | 91.7–99.8 | 96.7 | 84.8–99.3 |
| 20–44 | 314 | 96.7 | 93.9–98.3 | 96.1 | 93.0–97.8 | 95.4 | 91.8–97.5 | 94.9 | 90.6–97.3 | |
| 45–54 | 107 | 93.6 | 86.5–97.0 | 93.6 | 86.5–97.0 | 93.4 | 84.9–97.2 | 90.9 | 79.5–96.1 | |
| 55–64 | 93 | 91.9 | 83.5–96.1 | 90.2 | 80.9–95.1 | 83.0 | 70.3–90.6 | 62.1 | 30.6–82.6 | |
| 65–74 | 61 | 90.9 | 78.1–96.4 | 86.2 | 71.1–93.7 | 79.5 | 58.5–90.7 | 78.4 | 44.9–92.9 | |
| 75+ | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| Nerve sheath tumors | 0–19 | 2,787 | 99.8 | 99.5–99.9 | 99.6 | 99.2–99.8 | 98.9 | 98.3–99.3 | 97.5 | 96.3–98.3 |
| 20–44 | 15,012 | 99.5 | 99.4–99.7 | 99.3 | 99.1–99.4 | 98.8 | 98.5–99.0 | 98.2 | 97.7–98.7 | |
| 45–54 | 15,479 | 99.6 | 99.5–99.7 | 99.6 | 99.3–99.7 | 99.5 | 99.2–99.7 | 99.5 | 99.2–99.7 | |
| 55–64 | 17,350 | 99.4 | 99.2–99.5 | 99.4 | 99.1–99.6 | 99.4 | 99.1–99.6 | 99.4 | 99.1–99.6 | |
| 65–74 | 12,010 | 99.2 | 98.8–99.4 | 99.2 | 98.8–99.4 | 99.2 | 98.8–99.4 | 99.2 | 98.8–99.4 | |
| 75+ | 6,329 | 97.6 | 96.8–98.3 | 97.6 | 96.8–98.3 | 97.6 | 96.8–98.3 | 97.6 | 96.8–98.3 | |
| Meningioma | 0–19 | 1,158 | 98.8 | 97.9–99.3 | 98.3 | 97.3–99.0 | 96.6 | 95.1–97.6 | 92.3 | 89.2–94.5 |
| 20–44 | 31,887 | 98.6 | 98.5–98.8 | 98.1 | 97.9–98.2 | 96.8 | 96.6–97.1 | 94.8 | 94.3–95.2 | |
| 45–54 | 45,550 | 97.9 | 97.7–98.0 | 97.1 | 97.0–97.3 | 95.5 | 95.2–95.8 | 93.3 | 92.8–93.8 | |
| 55–64 | 60,364 | 96.1 | 95.9–96.2 | 94.7 | 94.5–94.9 | 92.3 | 91.9–92.6 | 88.7 | 88.1–89.2 | |
| 65–74 | 64,743 | 93.2 | 93.0–93.5 | 91.2 | 90.9–91.4 | 87.3 | 86.9–87.7 | 81.3 | 80.4–82.1 | |
| 75+ | 86,984 | 85.8 | 85.5–86.1 | 83.0 | 82.6–83.4 | 76.9 | 76.3–77.5 | 68.9 | 67.5–70.3 | |
| Mesenchymal tumors | 0–19 | 600 | 99.7 | 98.0–99.9 | 98.7 | 97.0–99.4 | 97.2 | 94.8–98.5 | 95.4 | 91.5–97.5 |
| 20–44 | 673 | 98.5 | 97.1–99.2 | 98.3 | 96.7–99.1 | 97.0 | 94.9–98.3 | 93.7 | 89.4–96.3 | |
| 45–54 | 390 | 97.7 | 95.3–98.9 | 96.9 | 94.1–98.4 | 93.5 | 89.1–96.1 | 86.8 | 79.0–91.8 | |
| 55–64 | 367 | 96.8 | 93.9–98.3 | 95.2 | 91.6–97.2 | 90.5 | 85.3–94.0 | 83.4 | 71.9–90.5 | |
| 65–74 | 272 | 92.8 | 88.2–95.6 | 90.9 | 85.5–94.3 | 84.5 | 76.5–89.9 | 71.0 | 53.9–82.7 | |
| 75+ | 151 | 84.8 | 76.2–90.4 | 84.8 | 76.2–90.4 | 71.5 | 54.6–83.0 | 52.8 | 27.1–73.1 | |
| Other neoplasms related to the meninges | 0–19 | 344 | 98.5 | 96.4–99.4 | 97.9 | 95.5–99.0 | 95.8 | 92.4–97.7 | 88.8 | 81.5–93.4 |
| 20–44 | 2,158 | 98.4 | 97.7–98.9 | 97.8 | 97.0–98.4 | 96.8 | 95.7–97.5 | 94.2 | 92.2–95.6 | |
| 45–54 | 1,205 | 96.9 | 95.6–97.8 | 96.3 | 94.9–97.4 | 95.4 | 93.5–96.8 | 91.5 | 87.7–94.2 | |
| 55–64 | 1,075 | 96.2 | 94.6–97.3 | 95.7 | 93.9–97.0 | 93.3 | 90.7–95.2 | 90.6 | 85.3–94.1 | |
| 65–74 | 705 | 93.4 | 90.9–95.2 | 91.9 | 88.9–94.1 | 88.1 | 83.5–91.4 | 88.0 | 82.2–92.0 | |
| 75+ | 401 | 85.5 | 80.7–89.2 | 84.4 | 78.6–88.7 | 81.5 | 73.5–87.3 | 60.0 | 40.6–74.8 | |
| Germ cell tumors, cysts, and heterotopias | 0–19 | 443 | 97.6 | 95.5–98.7 | 96.8 | 94.5–98.2 | 96.2 | 93.7–97.8 | 95.8 | 93.1–97.5 |
| 20–44 | 352 | 98.7 | 96.5–99.5 | 98.2 | 95.7–99.2 | 97.5 | 94.4–98.9 | 94.7 | 86.8–97.9 | |
| 45–54 | 140 | 94.5 | 88.7–97.3 | 94.0 | 87.9–97.1 | 92.2 | 84.4–96.2 | 84.3 | 71.7–91.6 | |
| 55–64 | 78 | 98.2 | 86.6–99.8 | 98.2 | 86.6–99.8 | 98.2 | 86.6–99.8 | 83.9 | 52.7–95.3 | |
| 65–74 | 74 | 94.5 | 83.9–98.2 | 93.1 | 80.5–97.6 | 85.5 | 68.8–93.7 | 85.5 | 68.8–93.7 | |
| 75+ | -- | -- | -- | -- | -- | -- | -- | -- | -- | |
| Tumors of the pituitary | 0–19 | 6,053 | 99.9 | 99.8–100.0 | 99.8 | 99.6–99.9 | 99.8 | 99.5–99.9 | 99.2 | 98.7–99.6 |
| 20–44 | 45,659 | 99.6 | 99.5–99.6 | 99.4 | 99.3–99.5 | 99.1 | 98.9–99.2 | 98.4 | 98.1–98.7 | |
| 45–54 | 23,601 | 98.8 | 98.6–99.0 | 98.5 | 98.2–98.7 | 97.7 | 97.4–98.0 | 96.5 | 95.9–97.1 | |
| 55–64 | 22,384 | 98.0 | 97.8–98.2 | 97.5 | 97.2–97.8 | 96.9 | 96.4–97.3 | 95.0 | 93.9–95.8 | |
| 65–74 | 18,446 | 96.8 | 96.5–97.1 | 96.2 | 95.7–96.6 | 94.8 | 94.1–95.5 | 91.5 | 89.6–93.0 | |
| 75+ | 13,400 | 92.9 | 92.3–93.5 | 91.9 | 91.0–92.7 | 87.2 | 85.7–88.6 | 79.4 | 75.4–82.8 | |
| Craniopharyngioma | 0–19 | 1,904 | 98.5 | 97.8–99.0 | 97.7 | 96.8–98.3 | 95.1 | 93.9–96.1 | 92.7 | 90.9–94.2 |
| 20–44 | 1,679 | 95.0 | 93.8–96.0 | 93.1 | 91.7–94.3 | 89.3 | 87.5–90.9 | 84.7 | 82.1–87.0 | |
| 45–54 | 1,036 | 91.3 | 89.4–93.0 | 90.0 | 87.8–91.8 | 84.8 | 82.0–87.2 | 79.6 | 75.5–83.1 | |
| 55–64 | 966 | 90.9 | 88.7–92.6 | 88.1 | 85.5–90.2 | 81.4 | 78.0–84.3 | 75.5 | 69.9–80.2 | |
| 65–74 | 643 | 83.2 | 79.8–86.1 | 76.8 | 72.8–80.3 | 68.3 | 63.3–72.8 | 55.1 | 46.4–63.0 | |
| 75+ | 348 | 84.0 | 78.8–88.0 | 78.4 | 72.1–83.5 | 65.1 | 55.9–72.8 | 54.0 | 42.4–64.3 | |
| Hemangioma | 0–19 | 1,011 | 99.3 | 98.5–99.7 | 99.0 | 98.1–99.5 | 98.3 | 97.0–99.1 | 97.0 | 93.7–98.6 |
| 20–44 | 3,340 | 99.2 | 98.8–99.5 | 98.8 | 98.3–99.2 | 98.1 | 97.4–98.7 | 96.2 | 94.5–97.3 | |
| 45–54 | 1,970 | 97.9 | 97.0–98.5 | 97.1 | 96.1–97.9 | 94.9 | 93.4–96.2 | 94.1 | 91.8–95.7 | |
| 55–64 | 1,803 | 96.1 | 95.0–97.0 | 95.1 | 93.7–96.1 | 93.2 | 91.2–94.7 | 86.6 | 81.1–90.6 | |
| 65–74 | 1,253 | 92.8 | 91.0–94.3 | 90.4 | 88.1–92.2 | 85.9 | 82.4–88.8 | 83.6 | 76.6–88.7 | |
| 75+ | 954 | 89.2 | 86.3–91.5 | 86.9 | 83.2–89.8 | 82.9 | 76.3–87.8 | 71.0 | 50.8–84.1 | |
| Neoplasm, unspecified | 0–19 | 1,390 | 96.3 | 95.1–97.2 | 95.9 | 94.7–96.9 | 95.5 | 94.2–96.5 | 94.5 | 92.7–95.8 |
| 20–44 | 3,282 | 94.7 | 93.8–95.4 | 93.3 | 92.4–94.2 | 91.5 | 90.4–92.5 | 89.0 | 87.4–90.5 | |
| 45–54 | 1,944 | 89.4 | 87.9–90.7 | 87.0 | 85.3–88.5 | 83.9 | 81.9–85.7 | 76.6 | 73.3–79.5 | |
| 55–64 | 2,075 | 82.7 | 81.0–84.4 | 78.0 | 76.0–79.8 | 72.2 | 69.8–74.4 | 66.2 | 62.6–69.5 | |
| 65–74 | 2,134 | 73.8 | 71.8–75.7 | 68.6 | 66.4–70.7 | 62.5 | 59.8–65.0 | 52.8 | 48.3–57.1 | |
| 75+ | 4,071 | 44.6 | 42.9–46.2 | 41.2 | 39.4–42.9 | 33.8 | 31.6–36.0 | 24.6 | 20.9–28.5 | |
| TOTAL d | 0–19 | 21,369 | 99.1 | 99.0–99.2 | 98.7 | 98.5–98.9 | 97.9 | 97.6–98.1 | 96.4 | 96.0–96.8 |
| 20–44 | 110,384 | 99.0 | 98.9–99.0 | 98.6 | 98.5–98.7 | 97.8 | 97.7–97.9 | 96.4 | 96.2–96.6 | |
| 45–54 | 93,842 | 98.1 | 98.0–98.2 | 97.5 | 97.4–97.7 | 96.3 | 96.2–96.5 | 94.7 | 94.4–95.0 | |
| 55–64 | 108,382 | 96.7 | 96.5–96.8 | 95.6 | 95.5–95.8 | 93.9 | 93.7–94.2 | 91.4 | 91.0–91.8 | |
| 65–74 | 101,457 | 94.1 | 93.9–94.2 | 92.4 | 92.2–92.7 | 89.6 | 89.2–89.9 | 85.0 | 84.3–85.7 | |
| 75+ | 113,322 | 85.8 | 85.6–86.1 | 83.4 | 83.1–83.7 | 78.1 | 77.6–78.6 | 71.1 | 69.9–72.3 |
a. The cohort analysis of survival rates was utilized for calculating the survival estimates presented in this table. Long-term cohort-based survival estimates reflect the survival experience of individuals diagnosed over the time period, and they may not necessarily reflect the long-term survival outlook of newly diagnosed cases.
b. Rates are an estimate of the percentage of patients alive at one, two, five, and ten years, respectively.
c. Total number of case that occurred within the NPCR registries between 2004 and 2015.
d. Total includes histologies not listed in this table.
- Rates were not presented for categories with 50 or fewer cases and were suppressed for rates where fewer than 16 cases were surviving within a category.
** Confidence interval could not be calculated.
Abbreviations: CBTRUS, Central Brain Tumor Registry of the United States; NPCR, National Program of Cancer Registries; CI, Confidence Interval; NOS, Not otherwise specified
Overall, 91.5% of persons with non-malignant tumor survived five years after diagnosis.
Five-year survival was highest in nerve sheath tumors and embryonal tumors, which had five-year relative survival of 99.3% and 98.1%, respectively.
Five-year survival was lowest in primary melanocytic lesions, craniopharyngioma, and meningioma, which had five-year relative survival of 63.3%, 86.1% and 88.0%, respectively.
Overall, five-year survival in adolescents and young adults was highest (98.1%) compared to children (97.2%) and adults (90.1%).
Survival rates for malignant brain and other CNS tumors by urban/rural residence
Survival estimates for malignant and non-malignant brain and other CNS tumors are shown by urban/rural residence and selected histologies in Supplementary Table 11 and Supplementary Table 12. Overall, one-, five-, and ten-year survival were higher in urban areas as compared to rural areas.
Descriptive Summary of Spinal Cord Tumors
Although spinal cord tumors account for a relatively small percentage of brain and other CNS tumors, they result in significant morbidity. The most common histologies found in the spinal cord, spinal meninges, and cauda equina are presented in Figure 21 for both children (age 0–19 years, Fig. 21A) and adults (age 20+ years, Fig. 21B).
Fig. 21.
Distributiona of Primary Spinal Cord, Spinal Meninges, and Cauda Equina Tumors by Histology in A) Children and Adolescents (Age 0–19 Years, Five-Year Total = 1,322; Annual Average Cases = 264) and B) Adults (Age 20+ Years, Five-Year Total = 18,184; Annual Average Cases = 3,637), CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
The predominant histology group for those age 0–19 years was ependymal tumors (20.6%) followed by nerve sheath tumors (17.8%).
Tumors of meninges (38.8%) accounted for the largest proportion of spinal cord tumors among those age 20 years and older.
Five-year survival after diagnosis with a malignant tumor of the spinal cord and cauda equina was 82.0%, with a ten-year relative survival of 78.7% (Table 19).
Descriptive Summary of Meningioma, Glioblastoma, and Embryonal Tumors
The data in the CBTRUS Statistical Report 2012–2016 were synthesized to describe three of the most common histologic types: meningioma and glioblastoma for adults and embryonal tumors for children and adolescents.
Meningioma
Meningioma was the most frequently reported brain and other CNS tumor, accounting for 37.6% of tumors overall (Fig. 7B). Most meningiomas (80.3%) were located in the cerebral meninges, 4.2% were located in the spinal meninges, and approximately 14.7% did not have a specific meningeal site listed.
Non-malignant meningioma with ICD-O-3 behavior codes /0 (benign) or /1 (uncertain) accounted for 97.7% of meningiomas reported to CBTRUS (Table 3).
Overall, 40% of meningioma diagnoses were histologically confirmed (Table 11), and this proportion varied by behavior (39.5% in non-malignant meningioma and 79.0% in malignant meningioma)
Of meningioma with documented WHO grade (79.3%, Table 11), 80.5% were WHO grade I, 17.7% were WHO grade II, and 1.7% were WHO grade III.
Meningioma was most common in adults age 65 years and older (Table 7), and one of the least common in children age 0–14 years (Table 5).
Incidence of meningioma increased with age, with a dramatic increase after age 65 years. Even among the population age 85 years and older, these rates continued to be high (Table 7).
Non-malignant meningiomas overall were 2.32 times more common in females compared to males (Fig. 13). Incidence rate ratios were lowest between males and females in persons <20 years old (where incidence rates for males and females were approximately equal), and highest from 35–44, where incidence rates were 3.28 times higher in females (Supplementary Figure 15).
Incidence of meningioma was significantly higher in Blacks than in Whites (Fig. 16).
Ten-year relative survival for malignant meningioma was 61.7% (Table 21). Age had a large effect on survival after diagnosis with malignant meningioma: 10-year relative survival was 76.8% for the population age 20–44 years, and 39.5% for age 75+ years (Table 22).
Ten-year relative survival for non-malignant meningioma was 83.7% (Table 23). Age had a large effect on survival after diagnosis with non-malignant meningioma: 10-year relative survival was 89.9% in children (age 0–14 years), 94.8% in AYA (age 15–39 years), and 82.8% in adults (age 40+ years old).
Site of meningioma had an effect on survival after diagnosis with meningioma. For non-malignant meningioma, 10-year relative survival was 83.2% for tumors in the cerebral meninges, but 95.6% for tumors in the spinal meninges.
Survival was also higher in malignant meningioma for spinal tumors, where 10-year relative survival was 73.4%, as compared to 55.7% for tumors in the cerebral meninges (Supplementary Figure 16).
Glioblastoma
Glioblastoma was the third most frequently reported CNS histology and the most common malignant tumor overall (Fig. 7BandFig. 8B).
Glioblastoma accounted for 14.6% of all primary brain and other CNS tumors (Fig. 7B), 48.3% of primary malignant brain tumors (Fig. 8B) and 57.3% of all gliomas (Fig. 10B)
Glioblastoma was more common in older adults (Table 7) and was less common in children (Table 6); these tumors comprised 3.0% of all brain and other CNS tumors reported among age 0–19 years.
Incidence of glioblastoma increased with age, with rates highest in individuals age 75 to 84 years (Table 7).
Glioblastoma was 1.58 times more common in males compared to females (Fig. 13).
Glioblastoma was 1.95 times higher among Whites compared to Blacks (Fig. 16).
Relative survival estimates for glioblastoma were quite low; 6.8% of patients survived five years post-diagnosis (Table 21). These survival estimates were somewhat higher for the small number of patients who were diagnosed under age 20 years (Table 22).
Embryonal Tumors
Embryonal tumors were the most frequently reported brain and other CNS tumor histology grouping in children age 0–4 years, and the fifth most common tumor type overall in children and adolescents age 0–19 years (Table 6, Fig. 17B).
Embryonal tumors within the CBTRUS histologic grouping scheme include multiple different histologies: medulloblastoma, PNET, ATRT, and several other rare histologies (Table 2).
Embryonal tumors accounted for 13.1% of all primary brain and other CNS tumors in children age 0–14 years (Fig. 18B), 10.1% of tumors in children and adolescents age 0–19 years (Fig. 17B), and 0.9% of tumors diagnosed overall (Fig. 7B).
Incidence of medulloblastoma decreased with increasing age after 9 years old. Incidence was 0.54 per 100,000 population, 0.59 per 100,000 population, 0.33 per 100,000 population, and 0.15 per 100,000 population in children age 0–4, 5–9, 10–14 years, and adolescents age groups 15–19 years, respectively (Table 6).
Incidence of PNET was 0.15 per 100,000 population, 0.05 per 100,000 population, 0.04 per 100,000 population, and 0.03 per 100,000 population in children age 0–4, 5–9, 10–14 years, and adolescents age 15–19 years, respectively (Table 6).
Incidence of ATRT was 0.32 per 100,000 population and 0.03 per 100,000 population in children age 0–4 and 5–9 years, respectively. There were too few of these cases in older age groups to report (Table 6).
Relative survival estimates for embryonal tumors were low but varied significantly by histology. 10-year survival was 66.1% for medulloblastoma, 30.0% for PNET, and 37.0% for ATRT (Table 21).
Embryonal tumors were more common in males than females (Table 3, Table 14). This difference was greatest in medulloblastoma, which occurred 1.66 times as frequently in males 0–14 years as compared to females in this age group (Supplementary Figure 17). Incidence of ATRT and PNET in children age 0–14 years were not significantly different between males and females.
Descriptive Summary of Adolescent and Young Adult (AYA) Primary Brain and Other CNS Tumors (Age 15–39 Years)
Brain and other CNS tumors are less common in AYA (age 15–39 years)52 compared to older adults (Table 4). These tumors are the third most commonly occurring cancer in persons age 15–39 years in the US, and the third most common cause of cancer death.53
There were 59,515 primary brain and other CNS tumors diagnosed in AYA between 2012 and 2016, representing 14.7% of all brain and other CNS tumors (Fig. 22).
The overall incidence rate in this age group was 11.40 per 100,000 population (Table 5). Incidence of malignant tumors was 3.23 per 100,000, and incidence of non-malignant tumors was 8.17 per 100,000 (Table 5).
Tumors of the sellar region had the highest incidence (3.95 per 100,000 population), followed by tumors of the neuroepithelial tissue (3.46 per 100,000 population) (Table 2).
The most common histology in AYA was tumors of the pituitary (3.82 per 100,000 population), followed by meningioma (1.86 per 100,000 population) and nerve sheath tumors (1.03 per 100,000 population) (Table 5).
The majority of AYA brain and other CNS tumors occurred in the pituitary and craniopharyngeal duct (35.4%), followed by the meninges (15.8%) (Fig. 22A).
18.7% of tumors diagnosed in AYA were located within the frontal, temporal, parietal, and occipital lobes of the brain combined (Figure 22A, occipital percentage not shown in figure due to low count).
Cerebrum, ventricle, cerebellum, and brain stem tumors combined accounted for 10.2% of all AYA tumors (Fig. 22A).
The predominately non-malignant tumors of the pituitary (27.3%), meningioma (12.4%), and nerve sheath (8.0%) represented over half of all brain and other CNS tumors diagnosed in AYA (Fig. 22B).
Glioma accounted for approximately 26.0% of all brain and other CNS tumors in AYA, and about 82.4% of all malignant tumors (Fig. 22B).
AYA are estimated to have 12,030 new primary brain and other CNS tumors in 2019 and 12,090 in 2020 (Table 18).
AYA had higher rates of relative survival than adults greater than 40 years old for all histologic types. Though 1-year relative survival for most tumor types was higher for AYA than children, 5- and 10-year survival were usually higher for children as compared to AYA (Table 24).
Fig. 22.
Distributiona in Adolescents and Young Adultsb (Age 15–39 Years) of All Primary Brain and Other CNS Tumors (Five-Year Total = 59,515; Annual Average Cases = 11,903) by A) Site and B) Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2012–2016
Descriptive Summary of Time Trends in Primary Brain and Other CNS Tumors
Time trends in cancer incidence rates are an important measure of the changing burden of cancer in a population over time. Many factors may lead to fluctuations in rates over time and all of these must be considered when interpreting time trends results. When assessing trends in incidence over time it is critical to use the most recent data available, as delay in reporting may cause small fluctuations in incidence. Time trends analysis methods are used to estimate if the APC is significantly different from 0% (meaning no change in incidence from year to year). In addition to assessing statistical significance of changes in incidence over time, the size of this change must also be considered because with datasets as large as CBTRUS very small fluctuations in incidence over time may be statistically significant but not truly represent a large change in proportion of individuals over time.
Incidence rates of cancer overall, and many specific cancer histologies, have decreased over time.54 Overall, changes in incidence rates of all primary brain and other CNS tumors between 2000 and 2016 (limited to 2004–2016 for non-malignant tumors) have been small. As stated previously, there are many things that can affect incidence rates over time that are not related to ‘true’ changes in incidence of these tumors such as demographic changes, changes in histologic classification, and changes in cancer registration procedures. The latetr is especially applicable to the collection of non-malignant brain and other CNS tumors, which have only been collected since 2004 in accordance with Public Law 107–260. Though these tumors are included in cancer collection, some surveillance reports do not include these tumors under their brain and other CNS tumors classification, but restrict reporting to malignant CNS tumors, including cancer trends. Incidence of non-malignant brain and CNS tumors increased substantially during the first years of collection as completeness of reporting improved, and CBTRUS has previously reported that there was increasing incidence of non-malignant brain tumors from 2004 to 2006.55,56
All malignant brain and other CNS tumors
Overall, there was a small but statistically significant decrease in incidence of malignant brain and other CNS tumors from 2000–2016 (APC = -0.4% [95% CI: -0.6%, -0.2%]).
From 2008–2016, there was a slight decrease in overall incidence (APC = -0.9% [95% CI: -1.2%, -0.7%], Fig. 23, Supplementary Table 13). These changes likely represent random variation or changes in underlying demographics rather than a true change in incidence of malignant brain tumors.
There was a small but statistically significant increase in incidence in children (age 0–14 years, APC = 0.6% [95% CI: 0.3%, 0.9%], Fig. 23), a small but statistically significant decrease in AYA (age 15–39 years, APC = -0.4% [95% CI: -0.6%, -0.2%], Fig. 23) from 2000–2016, and a small but statistically significant decrease in older adults from 2008–2016 (age 40+ years, APC = -1.1% [95% CI: -1.5%, -0.8%], Fig. 23).
Fig. 23.
Annual Age-Adjusted Incidence Rates of Primary Brain and Other CNS Tumors, and Incidence Trends by Behavior and Age Group, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2000–2016 (Varying)
Glioma
Overall, there was no significant change in incidence of glioma from 2000–2016.
There was a slight increase in incidence between 2000 and 2007 (APC = 0.9% [95% CI: 0.5%, 1.3%], Fig. 24), followed by a small but significant decrease in incidence from 2008–2016 (APC = -0.8% [95% CI: -1.2%, -0.4%], Fig. 24).
There was a significant increase in incidence in children (age 0–14 years, APC = 1.9% [95% CI: 1.4%, 2.4%]) from 2000–2013, and a significant increase in incidence in AYA from 2000–2006 (age 15–39 years, APC = 2.3% [95% CI: 0.7%, 3.8%], Fig. 24).
Incidence in older adults (age 40+ years) was relatively stable: there was a statistically significant increase from 2000–2007 (APC = 0.6%, [95% CI: 0.2%, 1.1%]), followed by a statistically significant decrease from 2007–2016 (APC = -0.8% [95% CI: -1.1%, -0.6%], Fig. 24).
There was a small but significant increase in incidence of glioblastoma from 2000–2007 (APC = 1.0 [95% CI: 0.2%, 1.2%]), with no significant change between 2007 and 2016 (Fig. 24, Supplementary Table 13).
Despite finding statistically significant variation, this likely represents random variation or changes in underlying demographics rather than a true change in incidence of glioma.
Fig. 24.
Annual Age-Adjusted Incidence Rates of Primary Brain and Other CNS Gliomas and Glioblastoma, and Incidence Trends by Age Group, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2000–2016
Malignant Meningioma
There was a significant decrease in incidence between 2000 and 2016 (APC = -4.5% [95% CI: -5.3%, -3.7%], Supplementary Table 13).
Changes were made to histological classification of meningioma in both the 2000 and 2007 revisions of the WHO classification, and gradual uptake of these classification changes may result in changing incidence of these tumors. 57
All non-malignant brain and other CNS tumors
Overall, there was a statistically significant increase in incidence of non-malignant brain and other CNS tumors from 2004–2018 (APC = 2.2% [95% CI: 1.3%, 3.0%]).
There was a significant increase in incidence of non-malignant brain tumors from 2004–2009 (APC = 5.2% [95% CI: 3.3%, 7.2%], Fig. 23, Supplementary Table 14), and no significant change between 2009 and 2016.
There was a small but statistically significant increase in incidence of these tumors in children (2004–2016, APC = 2.1% [95% CI: 1.4%, 2.9%], Fig. 23), in AYA (2004–2009, APC = 6.4% [95% CI: 3.9%, 9.0%], Fig. 23), and older adults (2004–2009, APC = 5.0% [95% CI: 3.1%, 6.9%], Fig. 23).
From 2012–2016, only 44.1% of non-malignant brain and other CNS tumors were histologically confirmed (Table 11). When analysis was limited to histologically confirmed tumors only, there was a small but significant increase in incidence of non-malignant brain and other CNS tumors from 2004–2009 (APC = 1.6% [95% CI: 0.5%, 2.7%]), followed by a small but significant decrease from 2009–2016 (APC = -1.2% [95% CI: -1.8%, -0.5%]).
There was a statistically significant increase in incidence of radiographically confirmed non-malignant tumors from 2004–2009 (APC = 9.6% [95% CI: 6.5%, 12.8%]), with no significant change from 2009–2016.
The increases in incidence in the non-malignant tumors are partially attributable to improved collection of radiographically diagnosed cases as well as improvement in collection of non-malignant cases in general over time.
Non-malignant meningioma
There was a significant increase of non-malignant meningioma between 2004 and 2009 (APC = 5.0% [95% CI: 3.5%, 6.5%], Fig. 25A), but there was no significant change after 2009.
From 2012–2016, only 39.5% of non-malignant meningiomas were histologically confirmed (Table 11). When analysis was limited to histologically confirmed cases, there was a slight increase in incidence from 2004–2009 (APC = 1.1% [95% CI: 0.1%, 2.1%]) and there was a slight decrease (APC = -1.5% [95% CI: -2.1%, -1.0%]) from 2009–2016.
There was a significant increase in incidence of radiographically diagnosed cases from 2004–2009 (APC = 8.9% [95% CI: 6.2%, 11.6%]), with no significant change from 2009 to 2016.
The increases in incidence in these non-malignant tumors are partially attributable to improved collection of radiographically diagnosed cases as well as improvement in collection of non-malignant cases in general over time.
Fig. 25.
Annual Age-Adjusted Incidence Rates of Selected Primary Brain and Other CNS Tumors, and Incidence Trends by Behavior and Histology, CBTRUS Statistical Report: US Cancer Statistics - NPCR and SEER, 2000–2016 (Varying).
Non-Malignant nerve sheath tumors
There was a small but significant increase in the incidence of non-malignant nerve sheath tumors between 2004 and 2016 (APC = 1.0% [95% CI: 0.4%, 1.7%], Fig. 25A).
From 2012–2016, only 50.4% of non-malignant nerve sheath tumors were histologically confirmed (Table 11). When analysis was limited to histologically confirmed cases only, there was no significant change in incidence (APC = -0.1% [95% CI: -0.8%, 0.5%]) from 2004–2016.
There was a significant increase in incidence of radiographically diagnosed tumors between 2004 and 2007 (APC = 8.8%, [95% CI: 3.3%, 14.6%]) and 2007 to 2013 (APC = 2.7 [95% CI: 0.8%, 1.8%]).
The increases in incidence in these non-malignant tumors are partially attributable to improved collection of radiographically diagnosed cases as well as improvement in collection of non-malignant cases in general over time.
Non-Malignant tumors of the pituitary
There was a significant increase in non-malignant tumors of the pituitary from 2004–2008 (APC = 7.7% [95% CI: 4.9%, 10.7%], Fig. 25A), but no significant change in incidence from 2008–2016.
From 2012–2016, only 46.6% of non-malignant tumors of the pituitary were histologically confirmed (Table 11). When analysis was limited to histologically confirmed tumors only, there was a significant increase (APC = 4.5% [95% CI: 3.3%, 5.8%]) from 2004–2009, followed by a small but significant decrease from 2009–2016 (APC = -1.8% [95% CI: -2.4%, -1.1%]).
There was a significant increase in incidence of radiographically diagnosed tumors of the pituitary from 2004–2008 (APC = 11.4% [95% CI: 6.4%, 16.7%]) and 2008–2012 (APC = 6.7% [95% CI: 0.6%, 13.2%]), with no significant change in incidence from 2012–2016.
The increases in incidence in these non-malignant tumors are partially attributable to improved collection of radiographically diagnosed cases as well as improvement in collection of non-malignant cases in general over time.
Prevalence of Primary Malignant Brain and Other CNS Tumors
Prevalence is an estimate of the total number of individuals with a disease who currently exist within a population, as compared to incidence, which is a calculation based on new diagnoses only. These calculations take into account not only the number of new cases being diagnosed, but also the length of time that individuals survive after diagnosis. CBTRUS previously estimated the 2010 point prevalence rate for all primary malignant brain and CNS tumors to be 47.6 per 100,000 population, or a total of 103,634 cases.58 Prevalence in children (0–14 years old) was estimated to be 22.31 per 100,000 population (13,657 cases), while prevalence in AYA (15–39 years old) was estimated to be 48.49 per 100,000 (31,299 cases). These ages represent age at time of prevalence calculation and not the age at which individuals were diagnosed. Please refer to Zhang, et al58 for more details.
CBTRUS also previously estimated the 2014 prevalence of selected adult malignant brain tumor histologies. Glioblastoma had the highest prevalence, at 9.23 per 100,000 population (23,327 cases), followed by diffuse astrocytoma (4.68 per 100,000 population; 10,868 cases), and oligodendroglioma (3.57 per 100,000 population; 8,217 cases). Please refer to Gittleman, et al59 for more details, including sex-, race-, and ethnicity-specific prevalence estimates.
Years of Life Lost due to Primary Malignant Brain and Other CNS Tumors in the United States
Years of potential life lost (YPLL) are an estimate of the amount that an individual’s life has been shortened by premature death due to cancer. Malignant brain tumors cause an average of 20 YPLL for individuals diagnosed as adults, which exceeds most common cancers.60 Among children 0–19 years old, brain and other CNS tumors represent the largest cause of YPLL due to cancer, with a mean YPLL of ~80 years.51 Please refer to de Blank, et al and Rouse, et al for more details.51,60
Lifetime Risk of Primary Malignant Brain and Other CNS Tumors
From birth, a person in the US has a 0.62% chance of ever being diagnosed with a primary malignant brain and other CNS tumor (excluding lymphomas, leukemias, tumors of the pituitary and pineal glands, and olfactory tumors of the nasal cavity) and a 0.48% chance of dying from a primary malignant brain/other CNS tumor.61–64
For males (all races), the risk of developing and the risk of dying from a primary malignant brain and other CNS tumor is 0.69% and 0.54%, respectively.
For females (all races), the risk of developing and the risk of dying from a primary malignant brain and other CNS tumor is 0.55% and 0.42%, respectively.
For White non-Hispanics (both sexes), the risk of developing and the risk of dying from a primary malignant brain and other CNS tumor is 0.72% and 0.55%, respectively.
For White Hispanics (both sexes), the risk of developing and the risk of dying from a primary malignant brain and other CNS tumor is 0.55% and 0.40%, respectively.
For Blacks (both sexes), the risk of developing and the risk of dying from a primary malignant brain and other CNS tumor is 0.33% and 0.26%, respectively.
For API (both sexes), the risk of developing and the risk of dying from a primary malignant brain and other CNS tumor is 0.41% and 0.32%, respectively.
Risk Factors for Primary Brain and Other CNS Tumors
Many environmental and behavioral risk factors have been investigated for primary brain and other CNS tumors. The only well-validated factors are increased risk for these tumors (particularly meningiomas) with exposure to ionizing radiation65 (the type of radiation generated by atomic bombs, therapeutic radiation treatment, and some forms of medical imaging) and decreased risk for these tumors (particularly glioma) in persons with a history of allergy or other atopic disease66 (including eczema, psoriasis, and asthma). Having a first-degree family member (including parents, children, and full siblings) that has been diagnosed with a brain tumor has been shown to increase risk approximately two-fold.67–71 Several recent review articles have elaborated on the current state of risk factor research in primary brain and other CNS tumors.72–75
Biomarkers for Primary Brain and Other CNS Tumors
Primary brain and other CNS tumors are a highly heterogeneous group of diseases, and characterization of unique tumor histologies within this group has been refined over time. The development of technologies for characterizing DNA, RNA, and DNA methylation has led to the discovery of several factors (known as ‘biomarkers’) that can be used to more accurately classify these tumors than histologic appearance alone. See Table 25 for a brief overview of selected biomarkers for primary brain and other CNS tumors, as well as a more in depth discussion in Scheie, et al76 and Velázquez Vega and Brat,77 as well as in Guerreiro Stucklin, et al.78 for pediatric biomarkers specifically.
Table 25.
Summary of biomarkers identified for primary brain and other CNS tumors
| Histology | Gene or Marker | Outcome | Related scientific publications | Collected by US Cancer Registry System |
|---|---|---|---|---|
| Glioma (especially oligodendroglial tumors) | Large deletions (missing parts of the chromosome) in the short arm of chromosome 1 (1p) and the long arm of chromosome 19 (19q) | Improved response to chemotherapy and radiation, and increased survival | Cairncross JG, Ueki K et al. (1998)79 Vogelbaum MA, Hu C et al. (2015)80 van den Bent MJ, Brandes AA et al. (2013)81 The Cancer Genome Atlas Research Network, Brat DJ et al. (2015)82 Ceccarelli M, Barthel FP et al. (2016)83 |
Yes Site-specific factor 5: http://web2.facs.org/cstage0205/brain/Brain_ nph.html Site-specific factor 6: http://web2.facs.org/cstage0205/brain/Brain_ opf.html |
| Glioma (especially low grade astrocytomas and oligodendroglial tumors) | Protein-truncating mutation in isocitrate dehydrogenase 1 (IDH1) or in isocitrate dehydrogenase 2 (IDH2) | Increased survival time | Yan H, Parsons DW et al. (2009)84 The Cancer Genome Atlas Research Network, Brat DJ et al. (2015)82 Ceccarelli M, Barthel FP et al. (2016)83 |
Yes Began in collection year 2018 (January 1), http://datadictionary. naaccr.org/default.aspx?c=10#3816 |
| Glioma (especially IDH mutated glioma) | Loss of function mutation in alpha thalassemia/mental retardation syndrome X‐linked (ATRX) | Increased survival time | Jiao Y, Killela PJ et al. (2012)110 Wiestler B, Capper D et al. (2013)112 The Cancer Genome Atlas Research Network, Brat DJ et al. (2015)82 |
No |
| Glioblastoma | Methylation of the promoter of O-6-methylguanine-DNA methyltransferase (MGMT) | Limits ability of the tumor cells to repair DNA damage caused by chemotherapy and radiation; results in increased survival time | Hegi ME, Diserens AC et al. (2005)85 Stupp R, Hegi ME et al. (2007)86 Hegi ME, Liu L et al. (2008)87 |
Yes Site-specific factor 4: http://web2.facs.org/cstage0205/brain/Brain_mpn.html |
| Glioblastoma | Glioma-CpG island methylator phenotype (G-CIMP), Genome-wide DNA methylation | Significantly increased survival time | Noushmehr H, Weisenberger DJ et al. (2010)88 | No |
| Glioblastoma | Amplification of epidermal growth factor receptor (EGFR) | Activates the RTK/RAS/PI3K pathway, leading to increased proliferation. Associated with poorer survival. | Maire CL and Ligon KL (2014) 113 Ceccarelli M, Barthel FP et al. (2016)83 |
No |
| Glioma (oligodendroglial tumors and IDH wild type glioblastoma) | Mutation of promotor of Telomerase reverse transcriptase (TERT) | Facilitates increased telomere lengthening, and decreases survival in IDH wild type glioma | Arita H, Narita Y et al. (2013) 114 Eckel-Passow JE, Lachance DH et al. (2015) 115 Ceccarelli M, Barthel FP et al. (2016)83 |
No |
| Glioma (particularly pediatric lower grade gliomas) | Mutation or fusion of B-Raf (BRAF) | Activates the RAS/MAPK pathway. Fusion leads to improved survival. | Hawkins C, Walker E et al. (2011)116 | No |
| Medulloblastoma | Wingless (WNT) subtype | Low prevalence of metastatic disease (~5–10%) Highest five-year survival (~95%) |
Kool M, Korshunov A et al. (2012)89 Northcott PA, Dubuc AM et al. (2012)90 Northcott PA, Jones DT et al. (2012)91 Northcott PA, Buchhalter I et al. (2017)92 |
Yes Began in collection year 2018 (January 1), http://datadictionary. naaccr.org/default.aspx?c=10#3816 |
| Medulloblastoma | Sonic hedgehog subtype (SHH) | Moderate prevalence of metastatic disease (~15–20%) Moderate five-year survival (~75%) |
Kool M, Korshunov A et al. (2012)89 Northcott PA, Dubuc AM et al. (2012)90 Northcott PA, Jones DT et al. (2012)91 Northcott PA, Buchhalter I et al. (2017)92 |
Yes Began in collection year 2018 (January 1), http://datadictionary. naaccr.org/default.aspx?c=10#3816 |
| Medulloblastoma | Group 3 subtype (also known as Group C) | Increased prevalence of metastatic disease (~40–45%) Poorest five-year survival (~50%) |
Kool M, Korshunov A et al. (2012)89 Northcott PA, Dubuc AM et al. (2012)90 Northcott PA, Jones DT et al. (2012)91 Northcott PA, Buchhalter I et al. (2017)92 |
Yes Began in collection year 2018 (January 1), http://datadictionary. naaccr.org/default.aspx?c=10#3816 |
| Medulloblastoma | Group 4 subtype (also known as Group D) | Increased prevalence of metastatic disease (40–45%) Moderate five-year survival (~75%) |
Kool M, Korshunov A et al. (2012)89 Northcott PA, Dubuc AM et al. (2012)90 Northcott PA, Jones DT et al. (2012)91 Northcott PA, Buchhalter I et al. (2017)92 |
Yes Began in collection year 2018 (January 1), http://datadictionary. naaccr.org/default.aspx?c=10#3816 |
| Embryonal tumor | C19MC amplification and presence of multilayered rosettes | Highly aggressive, with average survival of 12 months after diagnosis | Ceccom J, Bourdeaut F et al. (2014)117 Korshunov A, Sturm D et al. (2014)118 |
Yes Began in collection year 2018 (January 1), http://datadictionary. naaccr.org/default.aspx?c=10#3816 |
Gliomas, as the most common malignant primary brain and other CNS tumor type, have been subject to the greatest amount of investigation. A recent review has described in detail the current state of glioma biomarker research.93 One of the earliest discoveries in glioma biomarkers was that oligodendroglioma often had large deletions (missing parts of the chromosome, also known as loss of heterozygosity) in the short arm of chromosome 1 (1p) and the long arm of chromosome 19 (19q).79 In general, these deletions significantly predict positive response to chemotherapy and radiation treatment in oligodendroglioma and anaplastic oligodendroglioma.80,81,94 Mutations to the genes in isocitrate dehydrogenase 1 (IDH1) and in isocitrate dehydrogenase 2 (IDH2) have also been shown to be associated with improved prognosis in glioma. These mutations are common in lower grade gliomas (WHO grade II and WHO grade III), but are rare in glioblastoma.84 Both of these alterations are thought to occur relatively early in the development of gliomas; the prevalence of this mutation varies by anatomic location in the brain.95,96 The combination of these two factors can be used to more accurately stratify glioma by prognosis than the previously utilized histological criteria,82,83 and have been incorporated into the definition of oligodendroglioma and astrocytoma in the 2016 update to the WHO classification.18These classification changes are not reflected in the data presented in this report, which were collected prior to the adoption of these biomarkers as diagnostic criteria. These new biomarkers began to be collected by CCR in the United States starting January 1, 2018.
Another alteration that is associated with improved survival in glioma is increased methylation (where methyl molecules are bonded to the DNA) of the promotor region of the gene O-6-methylguanine-DNA methyltransferase (MGMT).85,87 The promoter region of a gene is located upstream of the coding part of the gene and exerts control over whether a gene is transcribed into RNA. Methylation of this region effectively silences the gene, and prevents transcription into RNA. MGMT is a DNA repair protein, and it is assumed that the decreases in protein levels increase sensitivity to the alkylating chemotherapies (eg, temozolomide) often used in the treatment of gliomas aimed to combat tumor growth through DNA damage.86 This alteration is common in glioblastoma and less common in lower grade gliomas. Recent analyses of data generated by The Cancer Genome Atlas have shown that genome-wide DNA methylation predicts improved prognosis in addition to methylation of specific genes.83 Persons whose tumor has a higher proportion of methylation across the genome are termed to have glioma-CpG island methylator phenotype (G-CIMP).88 G-CIMP and MGMT methylation are correlated,97 but G-CIMP is much rarer in glioblastoma than MGMT methylation.
Medulloblastoma is another tumor type that has been subject to significant molecular analysis. Using an analysis of gene expression (based on quantity of RNA transcribed from a gene), medulloblastoma was able to be subdivided into four distinct subtypes: wingless (WNT), sonic hedgehog (SHH), group 3 (also called group C), and group 4 (also called group D).89 These groups are associated with specific age-groups, with SHH being most common in infants and adults, and all other groups being more common in childhood. Several review articles have elaborated on the details of these subgroups and their implications for diagnosis and treatment.90–92
Diffuse intrinsic pontine glioma (DIPG) is an aggressive tumor of the brain stem that occurs primarily in children, and accounts for ~75% of brain stem tumors in children. Survival is very poor after diagnoses with these tumors. Due to the location of these tumors, they are often not biopsied and, therefore, have not been molecularly characterized to the extent of many other primary brain and other CNS tumor types. Recently, biopsy and autopsy protocols have allowed for collection of primary tumor samples that have been used for genomic profiling.98–100 These tumors have been found to be highly heterogeneous. Mutations in histone H3, Activin A receptor, type I (ACVR1), tumor protein p53 (TP53), platelet-derived growth factor receptor A (PDGFRA), phosphatidylinositol 3-kinase catalytic subunit alpha (PIK3CA), and Myc (MYC) have been identified as characteristic of these tumors.99,101,102 A recent review has further summarized recent developments in the genomics of DIPG.103
As of 2011, SEER registries currently collect information on three validated biomarkers for primary brain and other CNS tumors as Site Specific Factors (SSF): promoter methylation status of MGMT (SSF 4), deletion of the 1p (SSF 5), and deletion of 19q (SSF 6).104 Completeness of these biomarker data varies significantly by histology, but is gradually improving over time.
Starting with diagnosis year 2018, the US cancer registry system began collecting information on multiple brain and other CNS markers, including IDH1/2 mutation, 1p/19q codeletion, medulloblastoma molecular subtypes, and all biomarkers found in 2016 WHO classification.
Strengths and Limitations of Cancer Registry Data
CBTRUS, in collaboration with the CDC and NCI, is the largest population-based registry focused exclusively on primary brain and other CNS tumors in the US and represents cases collected from the entire US population. The CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016 contains the most up-to-date population-based data on all primary brain tumor and other CNS tumors available through the cancer surveillance system in the US.
Registration of individual cases is conducted by cancer registrars at the institution where diagnosis or treatment occurs and is then transmitted to the central cancer registry, which further transmits this information to NPCR and/or SEER. Central cancer registries (both NPCR and SEER) only report cases to the CDC and NCI for persons whot are residents of that particular state, so duplicate records should not occur for persons who may have traveled across state lines for treatment. As a result, the CBTRUS dataset is a complete recording of all cases for the time period examined with minimal duplicates.
Currently, there is no publicly available data source for the collection of survival and outcomes data from all geographic regions in the US via the cancer registry system. Survival data are collected by NPCR for 43 of the 51 CCR in the US (93% of the US population)—primarily through linkage with death certificate and other administrative records—and the feasibility of these data for use in survival studies has been evaluated105,106 and shown to produce reliable and robust estimates of cancer survival. Use of passive follow-up with record linkage may result in overestimation of survival in some populations, such as those that are more likely to leave the state or country.
No mechanism currently exists for central pathology review of cases within the US cancer registry system, and histology code assignment at case registration is based on histology information contained in the patient’s medical record. The WHO Classification of Tumours of the Central Nervous System underwent revision in 1993,107 2000,17 2007,2 and 2016.18 As of 2018, the US cancer registry system is using the 2016 classification for data abstraction, but tumors included in this report may have been diagnosed using any of the available classifications prior to 2013 due to the variation in adoption of new standards by individual physicians and medical practices. As a result, histologies are reflective of the prevailing criteria for a histology at the time of registration. This means that despite changes to the histology schema that may occur over time, it is not possible, without additional variables, to go back and reclassify any tumors based on the new criteria. In addition to changes in histologic criteria over time, there is significant inter-rater variability in histopathological diagnosis of glioma.108,109 This also means that incomplete, incorrect, or alternatively stated diagnoses included in a pathology report or other medical record can result in an incorrect reporting of the details of an individual case. For example, an anaplastic oligodendroglioma recorded in a pathology record as oligodendroglioma WHO grade III may be incorrectly recorded as an oligodendroglioma when the accurate category is an anaplastic oligodendroglioma.
US cancer registration requires the reporting of cases that are confirmed by different types of diagnostic procedures, including both histologic confirmation (where surgery was performed and the diagnosis confirmed by a pathologist) and radiographic confirmation (where diagnosis was made based solely on imaging criteria, such as an MRI, CT scan, or X-ray). Only histologic confirmation allows certainty on the assignment of a specific histology as well as for an assignment of a WHO grade. Many tumors have unique characteristics that make them identifiable on imaging, and thereby qualify as a valid type of diagnostic procedure, but it is important to consider the decreased level of certainty of specifying the correct histology in these tumors.
The 2016 WHO Classification of Tumours of the Central Nervous System18 contains significant updating to diagnostic criteria for glioma. Oligoastrocytoma has long been considered an entity that is distinct from astrocytoma and oligodendroglioma, and is included as a unique histologic grouping within the CBTRUS Histology Grouping scheme. Recent molecular analyses suggest that these tumors are not molecularly distinct from oligodendrogliomas or astrocytomas110 and can be separated into astrocytoma or oligodendroglioma using molecular markers; the diagnosis of oligoastrocytoma is strongly discouraged and is qualified with a “not otherwise specified” (NOS) designation under the 2016 WHO Classification of Tumours of the Central Nervous System. With this recent updating to the WHO criteria for central nervous system tumors,18IDH1/2 mutation and 1p/19q codeletion will become the primary factors by which gliomas are classified. While data on IDH1/2 mutation status were not collected in the US cancer registry system during the time period covered by this report, these data are required to be collected by cancer registrars (as available in the medical record) as of January 1, 2018. Cancer registry systems have collected 1p/19q deletion data for some of the report years, but data vary significantly in completeness by histology.104 It is likely that these changes to diagnostic criteria may affect the incidence of these tumor types in future years.
Concluding Comment
The CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2012–2016 comprehensively describes the most up-to-date- (October 2019) population-based incidence, mortality, and relative survival of primary malignant and non-malignant brain and other CNS tumors collected and reported by central cancer registries covering the entire US population. This report aims to serve as a useful resource for researchers, clinicians, patients, and families. In keeping with its mission, CBTRUS continually revises its reports to reflect the current collection and reporting practices of the broader surveillance community in which it works, while integrating the input it receives from the clinical and research communities, especially from neuropathologists, when possible. In this way, CBTRUS facilitates communication between the cancer surveillance and the brain tumor research and clinical communities and contributes meaningful insight into the descriptive epidemiology of all primary brain and other CNS tumors in the United States.111
CBTRUS Mission
CBTRUS is a not-for-profit corporation committed to providing a resource for gathering and disseminating current epidemiologic data on all primary brain and other central nervous system tumors, benign and malignant, for the purposes of accurately describing their incidence and survival patterns, evaluating diagnosis and treatment, facilitating etiologic studies, establishing awareness of the disease, and ultimately, for the prevention of all brain tumors.
Supplementary Material
Supplementary material is available online at Neuro-Oncology (http://neuro-oncology.oxfordjournals.org/).
Supplementary Table 1. Main and Extended Classification for ICCC Recode ICD-O-3/WHO 2008, Based On WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues (2008), for Selected Histologies1,2
Supplementary Table 2. 2000 U.S. Standard Population
Supplementary Table 3. Average Annual Populationa for 51 Central Cancer Registries (Including 50 States and District of Columbia) for 2012–2016 by Age, Sex, and Race
Supplementary Table 4. Average Annual Populationa for 51 Central Cancer Registries (Including 50 States and District of Columbia) for 2012–2016 by Age, Sex, and Hispanic Ethnicity
Supplementary Table 5. Average Annual Populationa for 51 Central Cancer Registries (Including 50 States and District of Columbia) for 2012–2016 by Age, Sex, and Urban/Rural Location of Residenceb
Supplementary Table 6. Five-Year Total, Average Annual Totala, and Average Annual Age-Adjusted Incidence Ratesb with 95% Confidence Intervals for Overall Cancer Incidence, and The Most Incident Comparison Cancers (Malignant Behavior Only) by NCI Age Group, U.S. Cancer Statistics – NPCR, 2012–2016
Supplementary Table 7. Five-Year Total, Average Annual Totala, and Average Annual Age-Adjusted Mortality Ratesb, with 95% Confidence Intervals by Cause of Death and NCI Age Group, United States, NVSS, 2012–2016
Supplementary Table 8. Five-Year Total, Average Annual Totala, and Average Annual Age-Adjusted Incidence Ratesb with 95% Confidence Intervals for All Brain and Other Central Nervous System Tumors by Major Histology Grouping, Histology, Behavior, and Urban/Rural Location of Residencec, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Table 9. Five-Year Total, Average Annual Totala, and Average Annual Age-Adjusted Mortality Ratesb with 95% Confidence Intervals for Malignant Brain and Other Central Nervous System Tumors Overall and by State and Urban/Rural Location of Residencec, United States, NVSS, 2012–2016
Supplementary Table 10. Five-Year Total, Annual Average Totala, and Age-Adjusted and Age-Specific Incidence Ratesb with 95% Confidence Intervals for Children and Adolescents (Age 0–19 Years), Brain and Other Central Nervous System Tumors: Malignant and Non-Malignant by International Classification of Childhood Cancer (ICCC)c, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Table 11. One-, Five-, and Ten-Year Relative Survival Ratesa,B with 95% Confidence Intervals for Selected Malignant Brain and Other Central Nervous System Tumors Overall and by Urban/Rural Location Residencec, U.S. Cancer Statistics – NPCR Registries, 2001–2015
Supplementary Table 12. One-, Five-, and Ten-Year Relative Survival Ratesa,B with 95% Confidence Intervals for Selected Non-Malignant Brain and Other Central Nervous System Tumors Overall and by Urban/Rural Location Residencec, U.S. Cancer Statistics – NPCR Registries, 2004–2015
Supplementary Table 13. Annual Percent Change (APC) and 95% Confidence Intervals for Malignant Brain and Other Central Nervous System Tumors by Major Histology Grouping, Histology, Behavior, and Sex, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2000–2016
Supplementary Table 14. Annual Percent Change (APC) and 95% Confidence Intervals for Non-Malignant Brain and Other Central Nervous System Tumors by Major Histology Grouping, Histology, Behavior, and Sex, CBTRUS Statistical Report: NPCR and SEER, 2004–2016
Supplementary Figure 1. Average Annual Age-Adjusted Incidence Ratesa with 95% Confidence Intervals of All Primary Brain and Other CNS Tumors in Comparison To The Top Eight Most Common Cancers in Males Only for A) Children Age 0–14 Years, B) Adolescents and Young Adults Age 15–39 Years, and C) Older Adults Age 40+ Years, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER 2012–2016
Supplementary Figure 2. Average Annual Age-Adjusted Incidence Ratesa with 95% Confidence Intervals of All Primary Brain and Other CNS Tumors in Comparison To Top Eight Most Common Cancers in Females Only for A) Children Age 0–14 Years, B) Adolescents and Young Adults Age 15–39 Years, and C) Older Adults Age 40+ Years, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER 2012–2016, USCS, 2012–2016
Supplementary Figure 3. Average Annual Age-Adjusted Mortality Ratesa with 95% Confidence Intervals of All Primary Brain and Other CNS Tumors in Comparison To Top Five Common Causes of Cancer Death and Top Three Non-Cancer Causes of Death in Males Only for A) Children Age 0–14 Years, B) Adolescents and Young Adults Age 15–39 Years, and C) Older Adults Age 40+ Years, CBTRUS Statistical Report: NVSS, 2012–2016
Supplementary Figure 4. Average Annual Age-Adjusted Mortality Ratesa with 95% Confidence Intervals of All Primary Brain and Other CNS Tumors in Comparison To The Top Five Causes of Cancer Deaths and Top Three Non-Cancer Causes of Death in Females Only for A) Children Age 0–14 Years, B) Adolescents and Young Adults Age 15–39 Years, and C) Older Adults Age 40+ Years, CBTRUS Statistical Report: NVSS, 2012–2016
Supplementary Figure 5. Distributiona of Malignant Primary Brain and Other CNS Tumors by Major Histology Groups (Five-Year Total = 122,569; Annual Average Cases = 24,514), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 6. Distributiona of Non-Malignant Primary Brain and Other CNS Tumors by Major Histology Groups (Five-Year Total = 283,171; Annual Average Cases = 56,634), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 7. Annual Age-Adjusted Incidence Ratesa of Primary Brain and Other CNS Tumors by Year and Behavior, by Sex, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 8. Distributiona of Primary Brain and Other CNS Tumors by Site, Males Only, A) Overall (Five-Year Total = 169,868; Annual Average Cases = 33,974), B) Malignant (Five-Year Total = 67,930; Annual Average Cases = 13,586), and C) Non-Malignant (Five-Year Total = 101,938; Annual Average Cases = 20,388), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 9. Distributiona of All Primary Brain and Other CNS Tumors by Site, Females Only, A) Overall (Five-Year Total = 235,872; Annual Average Cases = 47,174), B) Malignant (Five-Year Total = 54,639; Annual Average Cases = 10,928), and C) Non-Malignant (Five-Year Total = 181,233; Annual Average Cases = 36,247), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 10. Distributiona of All Primary Brain and Other CNS Tumors by CBTRUS Histology Groupings and Histology, Males Only, A) Overall (Five-Year Total = 169,868; Annual Average Cases = 33,974), B) Malignant (Five-Year Total = 67,930; Annual Average Cases = 13,586), and C) Non-Malignant (Five-Year Total = 101,938; Annual Average Cases = 20,388), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 11. Distributiona of All Primary Brain and Other CNS Tumors by CBTRUS Histology Groupings and Histology, Females Only, A) Overall (Five-Year Total = 235,872; Annual Average Cases = 47,174), B) Malignant (Five-Year Total = 54,639; Annual Average Cases = 10,928), and C) Non-Malignant (Five-Year Total = 181,233; Annual Average Cases = 36,247), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 12. Average Annual Age-Adjusted Incidence Ratesa of All Primary Brain and Other CNS Tumors by Age and Behavior, by Sex, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 13. Average Annual Age-Adjusted Incidence Ratesa of Malignant and Non-Malignant Primary Brain and Other CNS Tumors by Central Cancer Registry, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 14. Distributiona of All Primary Brain and Other CNS Tumors Diagnosed in Puerto Rico by Behavior (Five-Year Total = 2,393; Annual Average Cases = 479), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR, 2012–2016
Supplementary Figure 15. Incidence Rate Ratios for Meningioma with 95% Confidence Intervals by Behavior, Sex (Females:Males), and Age Group, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Supplementary Figure 16. Relative Survival Rates for Meningioma by Behavior and Site, CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR, 2004–2015
Supplementary Figure 17. Incidence Rate Ratios in Children (Age 0–14 Years) for Selected Embryonal Histologies by Sex (Males:Females), CBTRUS Statistical Report: U.S. Cancer Statistics – NPCR and SEER, 2012–2016
Acknowledgments
This report was prepared by the CBTRUS executive team and the research staff affiliated with the Case Comprehensive Cancer Center, Case Western Reserve University School of Medicine. The CBTRUS data presented in this report were provided through an agreement with the CDC, NPCR. In addition, CBTRUS used data from the research data files of the NCI, SEER Program. CBTRUS acknowledges and appreciates these contributions to this report and to cancer surveillance in general.
We acknowledge the efforts of the tumor registrars at hospitals and treatment centers, the CCRs, and the staff from the NPCR and SEER programs, whose efforts to collect accurate and complete data have made this report possible. We are also grateful to the four neuropathologists, Drs. Janet Bruner, Roger McLendon, Tarik Tihan, and Daniel Brat, who reviewed the CBTRUS histology grouping scheme, to our Consulting Research Director, Dr Nancy Stroup, our Consulting Neuropathologist, Dr Janet Bruner, who answered our questions and provided feedback throughout the year, to our Board of Directors and Advisors, and especially Dr Hoda Anton-Culver, Dr Melissa Bondy, Dr John Villano, and Reda Wilson, and the assistance of Shirley Stewart who volunteers in support of the CBTRUS mission.
Glossary
Abbreviations
- AAAIR
Average Annual Age-Adjusted Incidence Rate
- AAAMR
Average Annual Age-Adjusted Mortality Rate
- AIAN
American Indian/Alaskan Native
- AJCC
American Joint Commission on Cancer
- APC
Annual Percent Change
- API
Asian or Pacific Islander
- AYA
Adolescents and Young Adults
- ATRT
Atypical Teratoid Rhabdoid Tumor
- CBTRUS
Central Brain Tumor Registry of the United States
- CCR
Central Cancer Registry
- CDC
Centers for Disease Control and Prevention
- CS
Collaborative Staging
- CI
Confidence Interval
- CNS
Central Nervous System
- DIPG
Diffuse Intrinsic Pontine Glioma
- ICD-O-3
International Classification of Diseases for Oncology–Third Edition
- ICCC
International Classification of Childhood Cancer
- IDH1/2
Isocitrate Dehydrogenase 1/2
- MGMT
O-6-Methylguanine-DNA Methyltransferase
- NAACCR
North American Association of Central Cancer Registries
- NCHS
National Center for Health Statistics
- NCI
National Cancer Institute
- NOS
Not Otherwise Specified
- NPCR
National Program of Cancer Registries
- NPCR-CSS
NPCR Cancer Surveillance System
- NVSS
National Vital Statistics System
- PNET
Primitive Neuroectodermal Tumor
- SEER
Surveillance–Epidemiology–and End Results
- SHH
Sonic Hedgehog
- SSF
Site Specific Factors
- RUCC
Rural Urban Continuum Codes
- UDS
Uniform Data Standards
- US
United States
- USCS
United States Cancer Statistics
- VACCR
Veterans Affairs Central Cancer Registry VHA–Veteran’s Health Administration
- WHO
World Health Organization
- WNT
Wingless
- YPLL
Years of Potential Life Lost
Disclaimer
CBTRUS is a not-for-profit corporation which gathers and disseminates epidemiologic data on primary brain and other central nervous system tumors in order to facilitate research and establish awareness of the disease. CBTRUS makes no representations or warranties, and gives no other assurances or guarantees, express or implied, with respect to the accuracy or completeness of the data presented. The information provided in this report is not intended to assist in the evaluation, diagnosis, or treatment of individual diseases. Persons with questions regarding individual diseases should contact their own physician to obtain medical assistance. The contents in this report are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or of the National Cancer Institute.
The CBTRUS Board of Directors
Carol Kruchko, President & Chief Mission Officer, Central Brain Tumor Registry of the United States, Hinsdale, IL
Steven Brem, M.D., Vice President, Chief of Neurosurgical Oncology, Professor, Department of Neurosurgery, Co-Director, Brain Tumor Center, University of Pennsylvania, Philadelphia, PA
Donald Segal, J.D., Treasurer, Segal McCambridge Singer & Mahoney, Ltd., Chicago, IL
Fred H. Hochberg, M.D., Visiting Scientist, Department of Neurosurgery, University of California at San Diego, San Diego, CA
L. Lloyd Morgan, Patient Advocate, Berkeley, CA
Darell D. Bigner, M.D., Ph.D. (Emeritus Member), Edwin L. Jones, Jr. and Lucille Finch Jones Cancer Research Professor, Department of Pathology, Emeritus Director, The Preston Robert Tisch Brain Tumor Center, Chief, Preuss Laboratory for Brain Tumor Research, Duke, University Medical Center, Durham, NC
The CBTRUS Board of Advisors
Hoda Anton-Culver, Ph.D., Professor, College of Medicine, University of California-Irvine, Irvine, CA
Melissa Bondy, Ph.D., Professor, Department of Epidemiology and Population Health, Stanford University School of Medicine, Stanford, CA
Elizabeth Claus, M.D., Ph.D., Professor, Yale University School of Medicine, New Haven, CT, Attending Neurosurgeon, Brigham and Women’s Hospital, Boston, MA
Faith Davis, Ph.D., Professor, School of Public Health, University of Alberta, Edmonton, Canada
Roberta McKean-Cowdin, Ph.D., Associate Professor, Department of Epidemiology, University of Southern California, Los Angeles, CA
John Villano, M.D., Ph.D., Professor, Division of Medical Oncology, University of Kentucky Markey Cancer Center, Lexington, KY
Margaret Wrensch, Ph.D., Professor, Neuroepidemiology Division, Department of Neurological Surgery, School of Medicine, University of California-San Francisco, San Francisco, CA
Funding
CBTRUS is honored to be included among the research awardees of the following organizations which have contributed to the analyses resulting from the CBTRUS database in 2019: the Centers for Disease Control and Prevention (CDC) under Contract No.2016-M-9030, the American Brain Tumor Association, The Sontag Foundation, Novocure, Abbvie, the Musella Foundation, National Brain Tumor Society, the National Cancer Institute (NCI) under Contract No. HHSN261201800176P, the Children’s Brain Tumor Foundation, the Zelda Dorin Tetenbaum Memorial Fund, the Uncle Kory Foundation, as well as private and in kind donations. QTO is supported by a Research Training Grant from the Cancer Prevention and Research Institute of Texas (CPRIT; RP160097T). Contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or of the NCI.
References
- 1. Kruchko C, Ostrom QT, Gittleman H, Barnholtz-Sloan JS. The CBTRUS story: providing accurate population-based statistics on brain and other central nervous system tumors for everyone. Neuro Oncol. 2018;20(3):295–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Louis D, Wiestler O, Cavanee W, eds. WHO Classification of Tumours of the Central Nervous System. Lyon, France: International Agency for Research on Cancer; 2007. [Google Scholar]
- 3. Ostrom QT, Gittleman H, Liao P, et al. . CBTRUS statistical report: primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro. Oncol. 2014;16(s4):iv1–iv63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention (CDC). National Program of Cancer Registries Cancer Surveillance System Rationale and Approach 1999; http://www.cdc.gov/cancer/npcr/pdf/npcr_css.pdf. Accessed September 24, 2019.
- 5. Wiśniewski JR, Zougman A, Nagaraj N, Mann M. Universal sample preparation method for proteome analysis. Nat Methods. 2009;6(5):359–362. [DOI] [PubMed] [Google Scholar]
- 6. Benign Brain Tumor Cancer Registries Amendment Act, 107th Cong. § 260 2002. https://www.govinfo.gov/app/details/CREC-2002-08-01/CREC-2002-08-01-pt2-PgS8022-3. Accessed September 24, 2019 [Google Scholar]
- 7. National Cancer Institute. Overview of the SEER Program http://seer.cancer.gov/about/overview.html. Accessed September 24, 2019.
- 8. Wöhrer A, Waldhör T, Heinzl H, et al. . The Austrian Brain Tumour Registry: a cooperative way to establish a population-based brain tumour registry. J Neurooncol. 2009;95(3):401–411. [DOI] [PubMed] [Google Scholar]
- 9. Asklund T, Malmstrom A, Bergqvist M, Bjor O, Henriksson R. Brain tumors in Sweden: data from a population-based registry 1999–2012. Acta Oncol. 2015;54(3):377–384. [DOI] [PubMed] [Google Scholar]
- 10. Centers for Disease Control and Prevention National Center for Health Statistics. National Program of Cancer Registries and Surveillance, Epidemiology, and End Results SEER*Stat Database: U.S. Cancer Statistics Incidence Analytic Database – 1998–2016. Bethesda, MD: United States Department of Health and Human Services, Centers for Disease Control and Prevention and National Cancer Institute; 2019. Based on the November 2018 submission. [Google Scholar]
- 11. Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, Whelan S, eds. International Classification of Diseases for Oncology. 3rd ed. World Health Organization; 2000. [Google Scholar]
- 12. Surveillance Epidemiology and End Results (SEER) Program. SEER*Stat Database: Mortality - All COD, Aggregated With State, Total U.S. (1969–2016) <Katrina/Rita Population Adjustment>, Bethesda, MD: National Cancer Institute, DCCPS, Surveillance Research Program, released December 2018 Underlying mortality data provided by NCHS. www.cdc.gov/nchs.
- 13. McCarthy BJ, Surawicz T, Bruner JM, Kruchko C, Davis F. Consensus Conference on Brain Tumor Definition for registration. November 10, 2000. Neuro Oncol. 2002;4(2):134–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Surveillance Research Program - National Cancer Institute. ICCC Recode ICD-O-3/WHO 2008. http://seer.cancer.gov/iccc/iccc-who2008.html. Accessed September 24, 2019.
- 15. Steliarova-Foucher E, Stiller C, Lacour B, Kaatsch P. International classification of childhood cancer, third edition. Cancer. 2005;103(7):1457–1467. [DOI] [PubMed] [Google Scholar]
- 16. Swerdlow SH, Campo E, Harris NL, et al. . WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. 4th ed World Health Organization; 2007. [Google Scholar]
- 17. Kleihues P, Cavenee W, eds. Tumours of the Nervous System: World Health Organization Classification of Tumours. Lyon, France: IARC Press; 2000. [Google Scholar]
- 18. Louis DN, Ohgaki . H, Wiestler, OD, Cavenee WK, eds. WHO Classification of Tumours of the Central Nervous System. Lyon, France: International Agency for Research on Cancer; 2016. [Google Scholar]
- 19. American Joint Committee on Cancer. Collaborative Stage Data Collection System 2015. http://www.cancerstaging.org/cstage/. Accessed September 24, 2019.
- 20. Lym RL, Ostrom QT, Kruchko C, et al. . Completeness and concordancy of WHO grade assignment for brain and central nervous system tumors in the United States, 2004–2011. J. Neurooncol. 2015;123(1):43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Surveillance Research Program - National Cancer Institute. ICD-0–3 SEER Site/Histology Validation List 2019. https://www.google.com/url?sa=t&rct=j&q=&esrc=s&source=web&cd=2&cad=rja&uact=8&ved=2ahUKEwiYh_zy6-nkAhXKl54KHb8RBmcQFjABegQIABAC&url=https%3A%2F%2Fseer.cancer.gov%2Ficd-o-3%2Fsitetype.icdo3.20190618.pdf&usg=AOvVaw2ajRWYKzw4HwVL1yj0j6KV. Accessed September 24, 2019.
- 22. R Core Team. R: A language and environment for statistical computing 2019. http://www.R-project.org/. Accessed September 24, 2019.
- 23. Surveillance Epidemiology and End Results (SEER) Program. SEER*Stat software version 8.3.5 2019. www.seer.cancer.gov/seerstat. Accessed September 24, 2019.
- 24. Wickham H. ggplot2: elegant graphics for data analysis 2019. https://ggplot2.tidyverse.org/. Accessed September 24, 2019
- 25. Bivand R, Rundel C. rgeos: Interface to Geometry Engine - Open Source (GEOS) R package version 0.5–11. 2019. http://CRAN.R-project.org/package=rgeos. Accessed September 24, 2019.
- 26. Bivand R, Keitt T, Rowlingson B. rgdal: Bindings for the Geospatial Data Abstraction Library R package version 1.4–4. 2019. http://CRAN.R-project.org/package=rgdal. Accessed September 24, 2019.
- 27. Luo J. SEER2R: reading and writing SEER*STAT data files R package version 1.0. 2012. http://CRAN.R-project.org/package=SEER2R. Accessed September 24, 2019.
- 28. Bivand R, Lewin-Koh N. maptools: Tools for Reading and Handling Spatial Objects R package version 0.8–36. 2015. http://CRAN.R-project.org/package=maptools. Accessed September 24, 2019.
- 29. Gohel D. officer: Manipulation of Microsoft Word and PowerPoint Documents 2019. https://davidgohel.github.io/officer. Accessed September 24, 2019.
- 30. Gohel D. flextable: Functions for Tabular Reporting 2019. https://CRAN.R-project.org/package=flextable. Accessed September 24, 2019.
- 31. Bache SM, Wickham H. magrittr: A Forward-Pipe Operator for R 2014. https://CRAN.R-project.org/package=magrittr. Accessed September 24, 2019.
- 32. Surveillance Epidemiology and End Results (SEER) Program. SEER*Stat Database: Populations - Total U.S. (1990–2017) - Linked To County Attributes - Total U.S., 1969–2017 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released December 2018 http://seer.cancer.gov/popdata/.
- 33. Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–569. [DOI] [PubMed] [Google Scholar]
- 34. NAACCR Race and Ethnicity Work Group. NAACCR Guideline for Enhancing Hispanic/Latino Identification: Revised NAACCR Hispanic/Latino Identification Algorithm [NHIA v2.2.1]. Springfield, IL: North American Association of Central Cancer Registries. September. 2011. https://www.naaccr.org/wp-content/uploads/2016/11/NHIA_v2_2_1_09122011.pdf. Accessed September 24, 2019. [Google Scholar]
- 35. United States Department of Agriculture. 2013 Rural Urban Continuum Codes 2013. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation.aspx. Accessed September 24, 2019.
- 36. Joinpoint Regression Program, Version 4.7.0.0. Bethesda, MD: Statistical Methodology and Applications Branch, Surveillance Research Program, National Cancer Institute; 2019. [Google Scholar]
- 37. Kim HJ, Fay MP, Feuer EJ, Midthune DN. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335–351. [DOI] [PubMed] [Google Scholar]
- 38. Zhu L, Pickle LW, Ghosh K, et al. . Predicting US- and state-level cancer counts for the current calendar year: Part II: evaluation of spatiotemporal projection methods for incidence. Cancer. 2012;118(4):1100–1109. [DOI] [PubMed] [Google Scholar]
- 39. Edwards BK, Noone AM, Mariotto AB, et al. . Annual Report to the Nation on the status of cancer, 1975–2010, featuring prevalence of comorbidity and impact on survival among persons with lung, colorectal, breast, or prostate cancer. Cancer. 2014;120(9):1290–1314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Zullig LL, Jackson GL, Dorn RA, et al. . Cancer incidence among patients of the U.S. Veterans Affairs Health Care System. Mil Med. 2012;177(6):693–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Clegg LX, Feuer EJ, Midthune DN, Fay MP, Hankey BF. Impact of reporting delay and reporting error on cancer incidence rates and trends. J. Natl. Cancer Inst. 2002;94(20):1537–1545. [DOI] [PubMed] [Google Scholar]
- 42. Midthune DN, Fay MP, Clegg LX, Feuer EJ. Modeling reporting delays and reporting corrections in cancer registry data. J Am Stat Assoc. 2005;100(469):61–70. [Google Scholar]
- 43. Surveillance Epidemiology and End Results (SEER) Program. Cancer Incidence Rates Adjusted for Reporting Delay 2016. http://surveillance.cancer.gov/delay/. Accessed September 24, 2019.
- 44. Li XR, Kruchko C, Wu XC, et al. . Are benign and borderline brain tumors underreported? J Registry Manag. 2016;43(4):187–194. [PubMed] [Google Scholar]
- 45. Anderson RN, Rosenberg HM. Report of the second workshop on age adjustment. Vital Health Stat 4. 1998;( 30):I-vi, 1–37. [PubMed] [Google Scholar]
- 46. Anderson RN, Rosenberg HM. Age standardization of death rates: implementation of the year 2000 standard. Natl Vital Stat Rep. 1998;47(3):1–16, 20. [PubMed] [Google Scholar]
- 47. Dickie L, Johnson C, Adams S, Negoita S.. Solid Tumor Rules. Rockville, MD: National Cancer Institute; 2018. [Google Scholar]
- 48. Johnson C, Peace S, Adamo P, Fritz A, Percy-Laurry A, Edwards B.. The 2007 Multiple Primary and Histology Coding Rules. Bethesda, MD: National Cancer Institute; 2007. [Google Scholar]
- 49. Ostrom QT, de Blank PM, Kruchko C, et al. . Alex’s Lemonade Stand Foundation Infant and childhood primary brain and central nervous system tumors diagnosed in the United States in 2007–2011. Neuro Oncol. 2015;16(Suppl 10):x1–x36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. de Blank PM, Ostrom QT, Rouse C, et al. . Years of life lived with disease and years of potential life lost in children who die of cancer in the United States, 2009. Cancer Med. 2015;4(4):608–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. National Cancer Institute at the National Institutes of Health. Adolescents and Young Adults with Cancer http://www.cancer.gov/cancertopics/aya. Accessed September 24, 2019.
- 52. Ostrom QT, Gittleman H, de Blank PM, et al. American brain tumor association adolescent and young adult primary brain and central nervous system tumors diagnosed in the United States in 2008–2012. Neuro Oncol. 2016;18(Suppl 1):i1–i50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69(1):7–34. [DOI] [PubMed] [Google Scholar]
- 54. McCarthy BJ, Kruchko C, Dolecek TA. The impact of the Benign Brain Tumor Cancer Registries Amendment Act (Public Law 107–260) on non-malignant brain and central nervous system tumor incidence trends. J Registry Manag. 2013;40(1):32–35. [PubMed] [Google Scholar]
- 55. Gittleman HR, Ostrom QT, Rouse CD, et al. . Trends in central nervous system tumor incidence relative to other common cancers in adults, adolescents, and children in the United States, 2000 to 2010. Cancer. 2015;121(1):102–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Kshettry VR, Ostrom QT, Kruchko C, Al-Mefty O, Barnett GH, Barnholtz-Sloan JS. Descriptive epidemiology of World Health Organization grades II and III intracranial meningiomas in the United States. Neuro Oncol. 2015;17(8):1166–1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Zhang AS, Ostrom QT, Kruchko C, Rogers L, Peereboom DM, Barnholtz-Sloan JS. Complete prevalence of malignant primary brain tumors registry data in the United States compared with other common cancers, 2010. Neuro Oncol. 2016;19(5):726–735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Gittleman H, Boscia A, Ostrom QT, et al. . Survivorship in adults with malignant brain and other central nervous system tumor from 2000–2014. Neuro Oncol. 2018;20(Suppl 7):vii6–vii16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Rouse C, Gittleman H, Ostrom QT, Kruchko C, Barnholtz-Sloan JS. Years of potential life lost for brain and CNS tumors relative to other cancers in adults in the United States, 2010. Neuro Oncol. 2016;18(1):70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. DevCan: Probability of Developing or Dying of Cancer Software, Version 6.2.0. Statistical Research and Applications Branch, National Cancer Institute; 2007. http://srab.cancer.gov/devcan/ [computer program]. [Google Scholar]
- 61. Fay MP, Pfeiffer R, Cronin KA, Le C, Feuer EJ. Age-conditional probabilities of developing cancer. Stat Med. 2003;22(11):1837–1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Fay MP. Estimating age conditional probability of developing disease from surveillance data. Popul Health Metr. 2004;2(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Surveillance Epidemiology and End Results (SEER) Program. DevCan database: “SEER 18 Incidence and Mortality, 2000–2016, with Kaposi Sarcoma and Mesothelioma”. National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch; 2019, based on the November 2018 submission. Underlying mortality data provided by NCHS. [Google Scholar]
- 64. Braganza MZ, Kitahara CM, Berrington de Gonzalez A, Inskip PD, Johnson KJ, Rajaraman P. Ionizing radiation and the risk of brain and central nervous system tumors: a systematic review. Neuro Oncol. 2012;14(11):1316–1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Amirian ES, Zhou R, Wrensch MR, et al. . Approaching a scientific consensus on the association between allergies and glioma risk: a report from the glioma international case-control study. Cancer Epidemiol Biomarkers Prev. 2016;25(2):282–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Malmer B, Henriksson R, Grönberg H. Familial brain tumours—genetics or environment? A nationwide cohort study of cancer risk in spouses and first-degree relatives of brain tumour patients. Int J Cancer. 2003;106(2):260–263. [DOI] [PubMed] [Google Scholar]
- 67. Wrensch M, Lee M, Miike R, et al. . Familial and personal medical history of cancer and nervous system conditions among adults with glioma and controls. Am J Epidemiol. 1997;145(7):581–593. [DOI] [PubMed] [Google Scholar]
- 70. Malmer B, Grönberg H, Bergenheim AT, Lenner P, Henriksson R. Familial aggregation of astrocytoma in northern Sweden: an epidemiological cohort study. Int J Cancer. 1999;81(3):366–370. [DOI] [PubMed] [Google Scholar]
- 69. Hill DA, Inskip PD, Shapiro WR, et al. . Cancer in first-degree relatives and risk of glioma in adults. Cancer Epidemiol Biomarkers Prev. 2003;12(12):1443–1448. [PubMed] [Google Scholar]
- 70. Scheurer ME, Etzel CJ, Liu M, et al. . Aggregation of cancer in first-degree relatives of patients with glioma. Cancer Epidemiol Biomarkers Prev. 2007;16(11):2491–2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ostrom QT, Bauchet L, Davis F, et al. . The epidemiology of glioma in adults: a “state of the science” review. Neuro Oncol. 2014;16(7):896–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Johnson KJ, Cullen J, Barnholtz-Sloan JS, et al. . Childhood brain tumor epidemiology: a brain tumor epidemiology consortium review. Cancer Epidemiol Biomarkers Prev. 2014;23(12):2716–2736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Wiemels J, Wrensch M, Claus EB. Epidemiology and etiology of meningioma. J Neurooncol. 2010;99(3):307–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Ostrom QT, Adel Fahmideh M, Cote DJ, et al. . Risk factors for childhood and adult primary brain tumors. Neuro Oncol. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Scheie D, Kufaishi HHA, Broholm H, et al. . Biomarkers in tumors of the central nervous system - a review. APMIS. 2019;127(5):265–287. [DOI] [PubMed] [Google Scholar]
- 76. Velazquez Vega JE, Brat DJ. Incorporating advances in molecular pathology into brain tumor diagnostics. Adv Anat Pathol. 2018;25(3):143–171. [DOI] [PubMed] [Google Scholar]
- 77. Guerreiro Stucklin AS, Ramaswamy V, Daniels C, Taylor MD. Review of molecular classification and treatment implications of pediatric brain tumors. Curr Opin Pediatr. 2018;30(1):3–9. [DOI] [PubMed] [Google Scholar]
- 78. Cairncross JG, Ueki K, Zlatescu MC, et al. . Specific genetic predictors of chemotherapeutic response and survival in patients with anaplastic oligodendrogliomas. J Natl Cancer Inst. 1998;90(19):1473–1479. [DOI] [PubMed] [Google Scholar]
- 79. Vogelbaum MA, Hu C, Peereboom DM, et al. . Phase II trial of pre-irradiation and concurrent temozolomide in patients with newly diagnosed anaplastic oligodendrogliomas and mixed anaplastic oligoastrocytomas: long term results of RTOG BR0131. J Neurooncol. 2015;124(3):413–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. van den Bent MJ, Brandes AA, Taphoorn MJ, et al. . Adjuvant procarbazine, lomustine, and vincristine chemotherapy in newly diagnosed anaplastic oligodendroglioma: long-term follow-up of EORTC brain tumor group study 26951. J Clin Oncol. 2013;31(3):344–350. [DOI] [PubMed] [Google Scholar]
- 81. The Cancer Genome Atlas Research Network, Brat DJ, Verhaak RG, et al. . Comprehensive, integrative genomic analysis of diffuse lower-grade gliomas. N Engl J Med. 2015;372(26):2481–2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ceccarelli M, Barthel FP, Malta TM, et al. . Molecular profiling reveals biologically discrete subsets and pathways of progression in diffuse glioma. Cell. 2016;164(3):550–563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Yan H, Parsons DW, Jin G, et al. . IDH1 and IDH2 mutations in gliomas. N Engl J Med. 2009;360(8):765–773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Hegi ME, Diserens AC, Gorlia T, et al. . MGMT gene silencing and benefit from temozolomide in glioblastoma. N Engl J Med. 2005;352(10):997–1003. [DOI] [PubMed] [Google Scholar]
- 85. Stupp R, Hegi ME, Gilbert MR, Chakravarti A. Chemoradiotherapy in malignant glioma: standard of care and future directions. J Clin Oncol. 2007;25(26):4127–4136. [DOI] [PubMed] [Google Scholar]
- 86. Hegi ME, Liu L, Herman JG, et al. . Correlation of O6-methylguanine methyltransferase (MGMT) promoter methylation with clinical outcomes in glioblastoma and clinical strategies to modulate MGMT activity. J Clin Oncol. 2008;26(25):4189–4199. [DOI] [PubMed] [Google Scholar]
- 87. Noushmehr H, Weisenberger DJ, Diefes K, et al. . Identification of a CpG island methylator phenotype that defines a distinct subgroup of glioma. Cancer Cell. 2010;17(5):510–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Kool M, Korshunov A, Remke M, et al. . Molecular subgroups of medulloblastoma: an international meta-analysis of transcriptome, genetic aberrations, and clinical data of WNT, SHH, Group 3, and Group 4 medulloblastomas. Acta Neuropathol. 2012;123(4):473–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Northcott PA, Dubuc AM, Pfister S, Taylor MD. Molecular subgroups of medulloblastoma. Expert Rev Neurother. 2012;12(7):871–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Northcott PA, Jones DT, Kool M, et al. . Medulloblastomics: the end of the beginning. Nat Rev Cancer. 2012;12(12):818–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Northcott PA, Buchhalter I, Morrissy AS, et al. . The whole-genome landscape of medulloblastoma subtypes. Nature. 2017;547(7663):311–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Reifenberger G, Wirsching HG, Knobbe-Thomsen CB, Weller M. Advances in the molecular genetics of gliomas - implications for classification and therapy. Nat Rev Clin Oncol. 2017;14(7):434–452. [DOI] [PubMed] [Google Scholar]
- 93. Cairncross G, Wang M, Shaw E, et al. . Phase III trial of chemoradiotherapy for anaplastic oligodendroglioma: long-term results of RTOG 9402. J Clin Oncol. 2013;31(3):337–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Qi S, Yu L, Li H, et al. . Isocitrate dehydrogenase mutation is associated with tumor location and magnetic resonance imaging characteristics in astrocytic neoplasms. Oncol Lett. 2014;7(6):1895–1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Paldor I, Pearce FC, Drummond KJ, Kaye AH. Frontal glioblastoma multiforme may be biologically distinct from non-frontal and multilobar tumors. J Clin Neurosci. 2016;34:128–132. [DOI] [PubMed] [Google Scholar]
- 96. van den Bent MJ, Erdem-Eraslan L, Idbaih A, et al. . MGMT-STP27 methylation status as predictive marker for response to PCV in anaplastic Oligodendrogliomas and Oligoastrocytomas. A report from EORTC study 26951. Clin. Cancer Res. 2013;19(19):5513–5522. [DOI] [PubMed] [Google Scholar]
- 97. Jones C, Baker SJ. Unique genetic and epigenetic mechanisms driving paediatric diffuse high-grade glioma. Nat Rev.Cancer. 2014;14(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wu G, Diaz AK, Paugh BS, et al. . The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet. 2014;46(5):444–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Mackay A, Burford A, Carvalho D, et al. . Integrated molecular meta-analysis of 1,000 pediatric high-grade and diffuse intrinsic pontine glioma. Cancer Cell. 2017;32(4):520–537 e525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Hoffman LM, DeWire M, Ryall S, et al. . Spatial genomic heterogeneity in diffuse intrinsic pontine and midline high-grade glioma: implications for diagnostic biopsy and targeted therapeutics. Acta Neuropathol Commun. 2016;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Grill J, Puget S, Andreiuolo F, Philippe C, MacConaill L, Kieran MW. Critical oncogenic mutations in newly diagnosed pediatric diffuse intrinsic pontine glioma. Pediatr Blood Cancer. 2012;58(4):489–491. [DOI] [PubMed] [Google Scholar]
- 102. Lapin DH, Tsoli M, Ziegler DS. Genomic insights into diffuse intrinsic pontine glioma. Front Oncol. 2017;7:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Ostrom QT, Gittleman H, Kruchko C, et al. . Completeness of required site-specific factors for brain and CNS tumors in the Surveillance, Epidemiology and End Results (SEER) 18 database (2004–2012, varying). J Neurooncol. 2016; 130(1):31–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Weir HK, Johnson CJ, Mariotto AB, et al. . Evaluation of North American Association of Central Cancer Registries’ (NAACCR) data for use in population-based cancer survival studies. J Natl Cancer Inst Monogr. 2014;2014(49):198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Wilson RJ, O’Neil ME, Ntekop E, Zhang K, Ren Y. Coding completeness and quality of relative survival-related variables in the National Program of Cancer Registries Cancer Surveillance System, 1995–2008. J Registry Manag. 2014;41(2):65–71; quiz 96-67. [PMC free article] [PubMed] [Google Scholar]
- 106. Kleihues P, Burger PC, Scheithauer BW. The new WHO classification of brain tumours. Brain Pathol. 1993;3(3):255–268. [DOI] [PubMed] [Google Scholar]
- 107. van den Bent MJ. Interobserver variation of the histopathological diagnosis in clinical trials on glioma: a clinician’s perspective. Acta Neuropathol. 2010;120(3):297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Aldape K, Simmons ML, Davis RL, et al. . Discrepancies in diagnoses of neuroepithelial neoplasms: the San Francisco Bay Area Adult Glioma Study. Cancer. 2000;88(10):2342–2349. [PubMed] [Google Scholar]
- 109. Sahm F, Reuss D, Koelsche C, et al. . Farewell to oligoastrocytoma: in situ molecular genetics favor classification as either oligodendroglioma or astrocytoma. Acta Neuropathol. 2014;128(4):551–559. [DOI] [PubMed] [Google Scholar]
- 110. Jiao Y, Killela PJ, Reitman ZJ, et al. . Frequent ATRX, CIC, FUBP1 and IDH1 mutations refine the classification of malignant gliomas. Oncotarget. 2012;3(7):709–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Kruchko C, Gittleman H, Ruhl J, Hofferkamp J, Ward EM, Ostrom QT, Sherman RL, Jones SF, Barnholtz-Sloan JS, Wilson RJ Cancer collection efforts in the United States provide clinically relevant data on all primary brain and other CNS tumors. Neurooncol Pract. 2019 Sep;6(5):330–339. doi: 10.1093/nop/npz029. Epub 2019 Jul 2. Review. PubMed PMID: 31555447; PubMed Central PMCID: PMC6753356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Wiestler B, Capper D, Holland-Letz T, et al. . ATRX loss refines the classification of anaplastic gliomas and identifies a subgroup of IDH mutant astrocytic tumors with better prognosis. Acta Neuropathol. 2013;126(3):443–451. [DOI] [PubMed] [Google Scholar]
- 113. Maire CL, Ligon KL. Molecular pathologic diagnosis of epidermal growth factor receptor. Neuro Oncol. 2014;16(Suppl 8):viii1–viii6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Arita H, Narita Y, Fukushima S, et al. . Upregulating mutations in the TERT promoter commonly occur in adult malignant gliomas and are strongly associated with total 1p19q loss. Acta Neuropathol. 2013;126(2):267–276. [DOI] [PubMed] [Google Scholar]
- 115. Eckel-Passow JE, Lachance DH, Molinaro AM, et al. . Glioma groups based on 1p/19q, IDH, and TERT promoter mutations in tumors. N Engl J Med. 2015;372(26):2499–2508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Hawkins C, Walker E, Mohamed N, et al. . BRAF-KIAA1549 fusion predicts better clinical outcome in pediatric low-grade astrocytoma. Clin Cancer Res. 2011;17(14):4790–4798. [DOI] [PubMed] [Google Scholar]
- 117. Ceccom J, Bourdeaut F, Loukh N, et al. . Embryonal tumor with multilayered rosettes: diagnostic tools update and review of the literature. Clin Neuropathol. 2014;33(1):15–22. [DOI] [PubMed] [Google Scholar]
- 118. Korshunov A, Sturm D, Ryzhova M, et al. . Embryonal tumor with abundant neuropil and true rosettes (ETANTR), ependymoblastoma, and medulloepithelioma share molecular similarity and comprise a single clinicopathological entity. Acta Neuropathol. 2014;128(2):279–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.