Abstract
Purpose
Many minimally invasive surgical (MIS) techniques have been developed for instrumentation of spine. These MIS techniques restore stability, alignment while achieving return to function quite early as compared to open spine surgeries. The main aim of this review was to evaluate role, indications and complications of these MIS techniques in Thoracolumbar and Lumbar fractures.
Methods
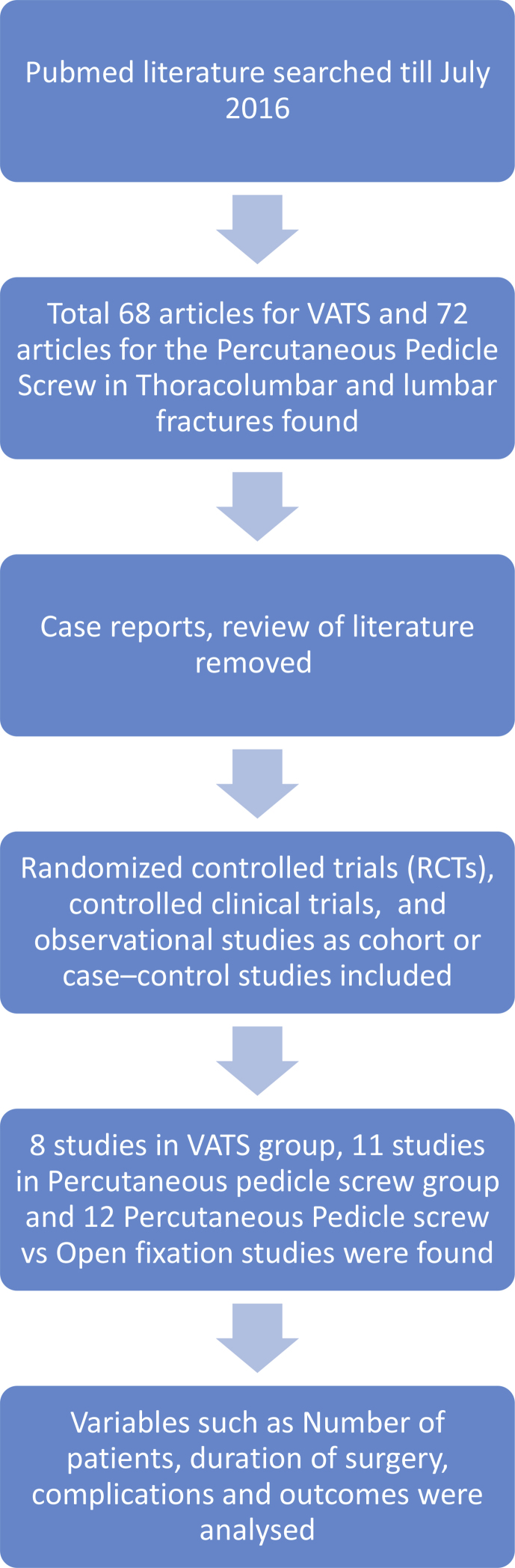
Pubmed search using key words such as“Percutaneous pedicle screw for Thoracolumbar fractures” and “Video Assisted Thoracoscopy, Thoracoscopic, VATS for thoracolumbar, Lumbar and Spine fractures” were used till July 2016 while doing literature search. Authors analyzed all the articles, which came after search; the articles relevant to the topic were selected and used for the study. Both prospective and retrospective case control studies and randomized control trials (RCT's) were included in this review. Case reports and reviews were excluded. Studies demonstrating use of MIS in cases other than spine trauma and studies with lack of clinical follow up were excluded from this review. Variables such as number of patients, operative time and complications were evaluated in each study.
Results
After pubmed search, we found total 68 studies till July 2016 out of which eight studies were relevant for analysis of Video Assisted Thoracoscopy for thoracolumbar and lumbar fractures. Total 72 articles for Percutaneous pedicle screws in thoracolumbar and lumbar fractures were retrieved out of which percutaneous pedicle screws were analyzed in eleven studies and twelve studies involved comparison of percutaneous pedicle screws and conventional open techniques.
Conclusion
Role and Indications of the MIS techniques in spinal trauma are expanding quite rapidly. MIS techniques restore stability, alignment while achieving early return to function and lower infection rates as compared to open spine surgeries. In long term, they provide good kyphosis correction and stable fixation and fusion of spine. They are associated with long learning curve and technical challenges but with careful patient selection and in expert hands, MIS techniques may produce better results than open trauma spine surgeries.
Keywords: Thoracoscopy, Thoracolumbar fractures, Percutaneous, Minimally invasive surgery (MIS), Video assisted thoracoscopy(VATS) and percutaneous pedicle screws
1. Introduction
In majority of cases, spinal fractures affect thoracolumbar region1. Almost every type of injury described in the spine occurs in thoracolumbar region. There may be compression fractures, chance fractures, dislocations and any combination of all of these injuries. Conservative management can manage most of these patients if no neurological deficit is present.1 However if neurological deficit is present and injury pattern is of unstable nature involving all the three columns of spine, then patient should be managed by surgical procedures. Surgery improves the management and long-term outcome of these spinal fractures, although no definite clinical evidence confirming superiority of surgical over conservative management exists at present.2 Surgical management of spine has evolved quite a lot in the last couple of decades.
Many minimally invasive surgical (MIS) techniques have been developed for instrumentation of spine. These MIS techniques have a common goal to achieve results similar to open surgeries while decreasing the morbidity associated with the open surgeries. These MIS techniques restore stability, alignment while achieving return to function quite early as compared to open spine surgeries. Most common MIS technique used in thoracolumbar trauma is percutaneous pedicle screw. The main aim of this review was to evaluate role of these MIS techniques in Thoracolumbar and lumbar fractures.
Pubmed search using key words such as “Percutaneous pedicle screw for Thoracolumbar fractures” and “Video Assisted Thoracoscopy, Thoracoscopic, VATS for thoracolumbar and Spine fractures” were used till July 2016 while doing literature search. Authors analyzed all the articles, which came after search; the articles relevant to the topic were selected and used for the study. Both prospective and retrospective case control studies and randomized control trials (RCT's) were included in this review. Case reports, reviews and articles not in English Language were excluded. Studies demonstrating use of MIS in cases other than spine trauma and studies with lack of clinical follow up were excluded from this review. Variables such as number of patients, operative time, complications and outcomes were evaluated in each study (Fig. 1).
Fig. 1.
Literature search methodology.
2. Minimally invasive approaches
Many thoracolumbar and lumbar spine injuries may present with neurologic deficits from retropulsed bone or significant communition resulting in loss of load bearing capacity of anterior column. Hence some form of anterior decompression or reconstruction is frequently indicated in these injuries. Before the advent of MIS, these fractures were treated with an extensive thoraco-abdominal approach. Conventional thoraco-abdominal approach involved detachment of the diaphragm to expose the thoracolumbar junction, which was associated with post thoracotomy syndromes, intercostals neuralgia and visceral herniation. Although standard posterior midline or para-midline approaches are associated with less morbidity, ischemia and revascularization injury associated with it results in atrophy, scarring, decreased strength and endurance.3, 4, 5, 6, 7 Hence in general an inference can be drawn from above discussion that the morbidity associated with conventional open procedures can be significant and, however, in some cases incompatible with the medical status of the patient.8, 9, 10 Reduced pain, better cosmesis, lower perioperative morbidity and earlier return to activity are some of the advantages associated with the MIS techniques for the thoracolumbar fractures.11 Lee et al.11 demonstrated reduction in duration of analgesic medicine by 31% and the overall dosage by 42% in patient treated endoscopically as compared with a group treated by open surgery.
Size of the incision and the morbidity to the thoracoabdominal wall has been limited by these recently developed minimal invasive, open microscopic and even video assisted thoracoscopy.11, 12, 13
3. Video assisted thoracoscopy
Entire thoracic spine can be visualized easily by thoracoscopy. However nowadays advancement in the thoracoscopy has resulted in the advancement of the spine levels, which can be addressed by it. Now from thoracolumbar junction to L2 levels can be exposed by thoracoscopy with the help of small diaphragmatic opening of 6–8 cm. As compared to open techniques this is minimal in size. As liver elevates diaphragm on right side, left sided approaches are preferred. After anesthesia patient is positioned in right lateral position and corpectomy, discectomy and decompression of the spinal canal can be done using high-speed burrs and Kerrison Rongeurs through small working portals. Decompression of canal by endoscopic techniques has equal efficacy as compared to open thoracotomy surgery.12,14 Total of 68 studies were retrieved with keywords “Video Assisted Thoracoscopy, Thoracoscopic, VATS for thoracolumbar, Lumbar and Spine fractures”. Eight studies12, 13, 14, 15, 16, 17, 18, 19 were found to be relevant and are summarized in Table 1. They analyzed role of Video Assisted Thoracoscopy in Thoracolumbar and lumbar fractures.
Table 1.
Studies summarizing role of Video Assisted Thoracoscopy in Thoracolumbar and Lumbar fractures.
| Study group | Kim et al.12 | Khoo et al.13 | Beisse et al.14 | Peng M et al.15 | Kim SJ et al.16 | Le Huec JC et al.17 | RayWZ et al.18 | Shawky A et al.19 |
|---|---|---|---|---|---|---|---|---|
| Number of patients | 212 | 371 | 220 | 23 23 in thoracoscopic group and 21 traditional group |
13 | 50 | 32 | 16 combined posterior percutaneous pedicle instrumentation and anterior Thoracoscopicapically assisted corpectomy |
| 75 (AO Type A) anterior alone and 137 (AO Type B and C) combined anterior and posterior instrumentation | 197 conventional open anterior plating and 174 total endoscopic | 78 (AO Type A) anteriorly and 142 (Type B and C) combined anterior and posterior instrumentation | All treated thoracoscopically | All treated thoracoscopically. Magerl type A and for some type C thoracolumbar junction fractures | combined posterior short-segment correction followed by thoracoscopic corpectomy and fusion | |||
| Location of fractures | TLJ T12-86 L1-126 |
T3-L3. 73% i.e 271 at TLJ Most common L1-35%, L2-24% |
TLJ T12-89 L1-131 |
TLJ | TLJ T12-6 Mid Thoracic-5 T11-2 L1-2 L2-1 |
TLJ | TLJ | TLJ |
| Portals | Four portals. The working channel (10 mm) is centered over the target vertebrae. The optical channel (10 mm) is placed two or three intercostal spaces cranial. The approach for suction/irrigation (5 mm) and retractor (10 mm) is placed approximately 5–10 cm anterior to the working and optical channel | The 10-mm working channel mark was centered directly over the fracture vertebrae.10-mm optical channel for the endoscope should be placed between two or three intercostals spaces cranial to the target area in axis with the spine. | Four Portals. Working portal directly above the fractured vertebra. 30-endoscope is placed over the spine two to three intercostal spaces. The portals for the retractor and the suction/irrigation instrument are situated ventrally from this point | Not Reported | Working channel was centered over the target vertebrae and the optical channel was placed two or three intercostal spaces cranial to the target vertebra. The approach for suction and irrigation or retractor was placed approximately 5–10 cm anterior to the working and optical channel. | first blunt trocar is inserted through a 2-cm incision along the anterior axillary line in the fifth or sixth intercostal space at the fracture level. Two other trocars are then set up along the median axillary line in order to insert a blunt pulmonary retractor | The 10-mm working channel was centered over the fracture site. 10-mm optical channel for the endoscope should be placed between two or three intercostals spaces cranial to the target area in axis with the spine. | Two incisions: the first is about 2.5 cm minithoracotomy done in the mid-axillary line and the second is about 1 cm in the posterior axillary line for the 30° thoracoscopy optic |
| Mean surgical time | 3.5 h | 3 h | 3.5 h | 170 ± 20.8 min | N/A | 155 min (75–240 min) | 270 ± 65 min | 248 min ± 63 min |
| Significant decrease in blood loss | Significant improvement in Cobb's and Kyphotic angle | |||||||
| Blood Loss | Not reported | Not reported | 870 ml | 650.0 ± 65.4 ml | Not Reported | 620 ml | Not reported | 765 ± 466 ml |
| Fusion Rate and screw loosening | 90% fusion rate and 2.5% (5 cases) screw loosening | 42% less need for narcotics | 90% fusion rate and 2.27% (5 cases) of screw loosening | 100% fusion rate | Not reported | Not reported | 90% fusion | 100% |
| Complication rate | 12 (5.7%) pleural effusion, pneumothorax and intercostal neuralgia. Three patients (1.4%) had superficial portal infections. | 1.3%one case each of aortic injury, splenic contusion, neurological deterioration, cerebrospinal fluid leak, and severe wound infection | 5.4% pleural effusions, persistent pneumothorax, or intercostal neuralgia | Not reported | 7.7% (3 patients) transitional pleural effusion, chylothorax followed by paraspinal abscess, and CSF leak. | 12% (6 patient) Five patients had a transient pulmonary atelectasia and there was one pulmonary infection | 9.4% (3 patients) | One patient had superficial wound healing problem. |
3.1. Indications
In most of the studies fracture were classified according to AO classification. For AO Type A exclusive anterior thoracoscopic fixation was considered satisfactory and for Type B and Type C fractures posterior pedicle screw fixation before anterior thoracoscopic decompression and reconstruction was done12, 14, 18, 19.
Contraindications for endoscopic approaches for reconstruction of the thoracolumbar spine are presence of restricted cardiopulmonary function, acute post-traumatic lung failure, pleural adhesions, or severe medical comorbidities.11
Most common levels operated levels are T12 and L1 with L1 fractures being maximum in most studies12, 13, 14, 17, 18. In all the studies, thoracoscopy was done in right lateral decubitus position.
Most commonly four portals were used which involved placing the working channel (10 mm) is centered over the target vertebrae. The optical channel (10 mm) is placed two or three intercostal spaces cranial. The approach for suction/irrigation (5 mm) and retractor (10 mm) is placed approximately 5–10 cm anterior to the working and optical channel.
Mean surgical time ranged from 189 to 300 min s. Blood loss ranges from 600 to 900 mls. Fusion rates ranges from 90 to 100%.12, 14, 15, 18, 19
3.2. Complications
Superficial wound infection12, 13, 18, 19 and transient pleural effusion12, 14, 16 are most commonly reported complications. As working field is near to lungs, pulmonary complications are commonly reported such as transient pleural effusion, pneumothorax, pulmonary atelectasis and pulmonary infection. Apart from pulmonary complications, injuries of adjacent structures such as spleen, aorta and bile duct resulting into chylothorax has been reported.
4. Percutaneous pedicle screws
Roy Camille first reported use of pedicle screws in 1963.20 Later in 1977, Margrel developed the technique of percutaneous pedicle screw placement primarily for temporary fixation of spine and later removed them.21 Open posterior approaches to the thoracolumbar and lumbar region are associated with pain and functional impairment resulting from muscle trauma.3, 4, 5, 6, 7 Assaker R et al. first reported thoracolumbar trauma as indication for the percutaneous pedicle screw in 2004.22 Many studies have now come up in English literature, which are demonstrating the efficacy of percutaneous pedicle screw fixation for traumatic spine fractures.6, 7, 8, 9, 10, 11, 12 Percutaneous pedicle screw fixation is associated with less muscle damage as compared with open surgical technique.23 For level confirmation and percutaneous pedicle screw insertion, this technique is highly dependent on the use of imaging under fluoroscopic guidance.24 However all the situations such as rotational deformities, obesity and osteopenia, in which there is difficulty in imaging is relative contraindication for the percutaneous pedicle screw insertion.25 Other relative contraindications for percutaneous pedicle screw insertion are multilevel vertebral fractures, pedicle fractures, adjacent body fracture and patient with significant kyphosis or saggital malalignment. However absolute contraindication for it is severe neural deficits, which require canal decompression.26 Main indication of percutaneous screw insertion in spine trauma includes fractures, which don't require significant reduction and decompression. Magrel type A1, A2 and certain type A3 fractures, fractures having TLICS score < 522,27,28 and fractures associated with posterior ligament disruption without subluxation or dislocation.27 Percutaneous pedicle screws can be put by a minimal incision of 1–2 cm para medially. Through this incision junction of facet and transverse processes is felt. Then spinal access needle or jamshidi needle with trocar is inserted and progressed after confirming on antero-posterior and lateral images. General dictum is that needle should not breach medial pedicle wall in any image. Then trocar is replaced by guide wire. On that guide wire serial dilators of increasing size are put. These dilators bluntly split the paraspinous muscles avoiding dissection, which reduces postoperative pain and intra-operative blood loss. Then after putting maximum size dilator, screws of adequate size are put and their position is confirmed in C- arm. Decrease in intra-operative blood loss is quite advantageous in high-risk geriatric patients and patients who are already in shock due to hypovolumeia attributable to poly-trauma. Less trauma to muscles and early stabilization promotes early mobilization of the patients. Although as far as surgeons concerned, technique of percutaneous pedicle insertion has long learning curve. After Literature search, we found a total of 72 studies out of which we were able to find eleven studies29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 [Table 2] involving the analysis of role of percutaneous pedicle screws fixation in thoracolumbar and lumbar fractures. Almost all of them suggested that percutaneous pedicle screws fixation in thoracolumbar and lumbar fractures is helpful in achieving significant pain relief, kyphosis correction usually in the range of 5- 10°, early post op mobilization and decrease in peri-operative morbidity.
Table 2.
Studies demonstrating role of Percutaneous Pedicle Screw fixation.
| Study | Year | Number of patients | Mean Age | Sex Ratio | Spinal Location | Fracture classification | Average duration of Surgery in Mins | Average Blood loss | Cobb's angle |
Neurology |
Complication | Outcome | Implant removal done | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-op | Post-op | Follow up | Pre-op | Post-op | |||||||||||||
| 1 | Cimatti M et al.30 | 2013 | 32 | 48 (17–78) | 16:16 | TLF T11–2,T12–6,L1-16,L2-4,L3-4 |
Margrel A1-1,A2-8,A3-21,B1-1,B2-3 | 60 | NR | 6.2 | 2.7 | 2.9 | NR | NR | NR | Pain improvement: Significant Kyphosis correction: Significant |
No |
| 2 | Takami et al.51 | 2013 | 21 | 45.4 (23–73) | 17:4 | TLF T11-1 T12-2 L1-7 L2-4 L3-5 L4-2 |
Margrel A3 fracture HA block vertebroplasty along with Pedicle screws |
95.7 | 38.6 | 8.5 | −4.2 | −0.6 | E | E | 100% fusion, 1 loosening of screw | Pain improvement score: 7.5, Neuro Improved: N/A Kyphosis correction:3.1 |
Implant removed in all patients within 5 months |
| 3 | Yang WE et al.31 | 2012 | 21 | 39.6 (21–68) | 14:7 | TLF | NR | 179 | 175 | 17.1 | 11 | 13.8 | A-2 B-2 C-3 D-4 E−10 |
1 0 1 6 13 |
4 superficial wound dehiscence 3 pedicle screw pull outs |
Pain improvement: N/A Kyphosis correction: 6.1° |
Yes |
| 4 | Fang LM et al.32 | 2012 | 35 | 34.1 (18–52) | 20:15 | TLF T11-5, T12-9, L1-14, L2-7 |
TLICS Score 5–13 7–22 |
95.8 | 83 | 10.31 | −1.48 | 1.03 | E | E | 2 superficial wound infection Screw misplacement 9/140 (6.4%) |
Pain improvement score: significant Kyphosis Correction: No loss |
NR |
| 5 | Bironneau A et al.33 | 2011 | 24 | 58 (20–88) | 12:12 | TLF T12-2 L1-12 L2-5 L3-2 L4-2 L5-1 |
Margrel A1-1,A2-2,A3-19,B2-3 Kyphoplasty with cement and pedicle screws |
99 | 15.2 | 5 | 6.6 | E | E | 8 cases cement leaked, 3 hematoma at the scar | Pain Improved Score: 6.3 Neuro Improved: N/A Kyphosis correction: 8.6° |
NR | |
| 6 | Blondel B et al.34 | 2011 | 29 | 51 (22–78) | TLF Burst fracture T-9 T11-3 T12-6 L1-13 L2-4 L5-2 |
Magerl A3 | NR | NR | 13 | 3.2 | 5.2 | E | E | Hematoma: 1 | Pain Improved Score: 5.6 Neuro Improved: N/A Kyphosis correction: 11° |
Can be removed percutaneously | |
| 7 | N.W et al.35 | 2010 | 36 | 43 (19–58) | 25:11 | TLF T11-4 T12-8 L1-17 L2-7 |
AO type A3 with load sharing classification of 6 or less | 78 | 75 | 18.7 | 3.6 | 7.6 | E | E | 7 screws (6.7%) misplaced, No neurological deficit.1 superficial infection, 1 screw loosening | Pain Improved Score: N/A Neuro Improved: N/A Kyphosis correction: 9.1° |
Removed in 26 patients and rest 10 refused |
| 8 | Palmisani M et al.36 | 2009 | 51 | 45 (21–82) | 34:17 | TLF (T1-T10)-6 (T11-L1)-31 Lumbar spine-14, Max L1-20 |
AO A1-20 A2-10 A3-27 B1-1 B2-3 C1-1 C2-2 |
NR | NR | 4.2 | −2.2 | 2.7 | E | E | Infection: 1 Misplaced Screw: 1 Pseudoarthrosis: 2 |
Pain Improved Score: N/A Neuro Improved: N/A Kyphosis correction: 6.2° |
Removed in 10 patients (19%) |
| 9 | Merom L et al.37 | 2009 | 10 | 42 (21–63) | TLF | – | 50 | 78–102 | – | – | – | E | E | None | Pain Improved Score: N/A Neuro Improved: N/A Kyphosis correction: N/A0 |
NR | |
| 10 | Maclejczak A et al.39 | 2007 | 4 | 45 (28–59) | 3:1 | TLF L2-2 L3-3 |
Dennis B | 5.9 h s for decompression + Fusion | NR | −1.25 | −7.7 | −2.7 | E | E | Pseudoarthrosis: 1 | Pain Improved Score: N/A Neuro Improved: N/A Kyphosis correction: 11.6° |
NR |
| 11 | Schmidt et al.51 | 2007 | 76 | 53.3 | NR | TLF Unstable type B fractures, Type A1 and A2 fractures with >25% anterior height loss or additional disc injury (in need for combined anterior surgery), Type A1 fractures in obese and geriatric patients as well as burst fractures, Type A3 in patients younger than 40 years of age |
Magrel Type A1.2 most common fracture A1-36 A2-6 A3-22 B-12 Si |
47 | Blood transfusion required in 3 (3.9%) Patients | NR | NR | NR | 6 (7.9%) patients Neurological deficit | No neurological deficit and one patient recovered completely | Three patients (3.9%) One paravertebral hematoma, one persistent skin irritation and one implant failure |
Pain improvement: NR Neuro Improvement:1 patient Kyphosis correction:NR |
NR |
TLF- Thoracolumbar Fracture, NR- Not reported.
Twelve comparative studies29,38,41, 42, 43, 44, 45, 46, 47, 48, 49, 50 have been published by July 2016. Of these studies two were prospective randomized studies46,47 and ten were observational studies. Out of these ten observational studies five29,41,43,48,50 are prospective and five38,42,44,45,49 are retrospective. These comparative studies have shown that for AO type A fractures percutaneous pedicle screws alone offers a stable fixation. N.W et al.35 recommended that for AO type A3 with load sharing classification of 6 or less percutaneous pedicle screw fixation alone is adequate and for A3 with load sharing classification of more than 6, Type B and C fractures percutaneous pedicle screws may require additional procedure in the form of vertebroplasty with cement augmentation33, vertebroplasty with hydroxyapetitie block augmentation51 and minimal invasive approach for decompression52. Schmidt et al.52 have shown that minimal invasive fixation with pedicle screws is effective option for Unstable type B fractures, Type A1 and A2 fractures with >25% anterior height loss or additional disc injury (in need for combined anterior surgery), Type A1 fractures in obese and geriatric patients as well as burst fractures, Type A3 in patients younger than 40 years of age. Most commonly operated levels were T12 and L130, 32, 33, 34, 35, 36. Most common age group appears to be in 30–50 with a wide range and in all the studies there was male predominance. Percutaneous pedicle screws are associated with significantly shorter operative duration, smaller incision size, less blood loss, shorter hospital stays and improved peri-operative pain scores.28 From Table 2, we can conclude that percutaneous pedicle screws alone and with other techniques are associated with significant khyphosis correction and maintained the correction of kyphosis at the final follow up. In some cases, it also resulted in improvement of the neurological deficit31,52. Stable fixation and fusion appear to be hundred percent as puedoarthosis has been reported rarely. Two main complications are screw malpositioning and infection in spine surgeries. No differences have been found in screw malpositioning rates between percutaneous and open spine surgeries while infection rates are significantly lower in percutaneous as compared to open spine surgeries. Implant removal was also done after variable period in some studies31,35,36,51. A systemic review and meta-analysis published by Kevin Phan et al.40 has included all the 12 comparative studies mentioned in Table 3. It has proved statistically that percutaneous pedicle screws are associated with significantly shorter operative duration, less intra-operative blood loss, smaller incision size, lower infection rates, better pain relief and shorter hospital stay as compared to conventional open spine surgeries. It didn't find any significant difference in radiological parameters such as postoperative cobb's angle, postoperative body angle and postoperative anterior vertebral height. It found no strong evidence that percutaneous approach reduces disruption of muscle and tissue as compared to open spine surgeries.
Table 3.
Showing Comparartive studies of Open spinal surgeries and Percutaneous pedicle Screw Fiaxation
| Study | Period | Study Design | Patients treated percutaneously |
Patients treated by open surgery |
Spinal Location | Follow up for percutaneous Patients | Neurologic deficit | Fusion | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No of patients | Average Age | Sex Ratio | Operative time in mins | Blood loss in mL | Screw Malpositioning | Infection | Hospital Stay | No of patients | Average Age | Sex Ratio | Operative time in mins | Blood loss in mL | Screw Malpositioning | Infection | Hospital Stay | ||||||||
| 1 | Wang (2014)41 | 5 yr | P,OS | MIF4-22,MIF6-39 | MIF4-45.8,MIF-45.11 | MIF4-17:5,MIF6-32:7 | MIF4-98.4,MIF6-114.1 | MIF4 49.3,MIF6-87.7 | MIF4-2,MIF6-0 | MIF4-0,MIF6-0 | MIF4-9.7,MIF6-12.9 | 39 | 43.3 | 25:14 | 140.3 | 311.5 | 1 | 1 | 17.6 | TLF max L1-60 AO type A max A1-63 | 20 | No | No |
| 2 | Vanek (2014)29 | 16 month | P,OS | 18 | 45.6 | 14:4 | 53 | 56 | 0 | 1 | NR | 17 | 39.4 | 14:3 | 60 | 331 | 0 | 1 | NR | TLF max T12 and L1 14 each AO A3.1-A3.3. Max A3.3 | 24 | No | No |
| 3 | Lee (2013)42 | 6 yr | R,OS | 32 | 36.3 | 20/12 | 83.2 | 262.5 | 1 | 0 | NR | 27 | 36.3 | 19:8 | 154.9 | 684.3 | 1 | 2 | NR | Single levelTLF Dennis Type A/B12/20 in MISS and 12/15 in open group | 30.2 | Frenkel C 2,Frenkel D-12(7,5) Frenkel E31(16,15) | No |
| 4 | Grossbach (2013)43 | 10 yr | P,OS | 11 | 27.4 | 11:0 | 195 | 93.6 | 0 | 0 | 7.6 | 27 | 40.1 | 18:9 | 257 | 498 | 0 | 1 | 11.2 | Thoracolumbar- flexion distraction.AO B1.2 most common | 9 | ASIA E(5 score) in MIS and ASIA(4.41) in open group | No |
| 5 | Bronsard (2013)44 | 7 yr | R,OS | 30 | 40.4 | 12:18 | 83.5 | 50.33 | 0 | 0 | NR | 30 | 43.5 | 21:9 | 148.5 | 318.83 | 1 | 3 | NR | TLF from T9-L4 out of which T11-L2 are 24 ORIF and CRIF 30. Most common MargerlA3- 15 ORIF, 20 CRIF | 25.5 | No | No |
| 6 | Song (2012)45 | 6 yr | R,OS | 20 | 36.4 | 82 | 68.5 | 2 | 0 | 11.8 | 32 | 36.4 | 90.1 | 330.7 | 5 | 0 | 21 | TLF | 12 | No | No | ||
| 7 | Jiang (2012)46 | 3 yr | P,RCT | 31 | 42.4 | 79.7 | 79 | 2 | 0 | 9.7 | 30 | 42.4 | 89.8 | 145 | 1 | 1 | 10.8 | TLF | 67.7 | No | No | ||
| 8 | Tian (2011)47 | 5 yr | P,RCT | 47 | 125 | 91 | NR | 0 | NR | 50 | 122 | 204 | NR | 1 | TLF | 12 | No | No | |||||
| 9 | Wang (2010)48 | 3 yr | P,OS | 17 | 41.6 | 13:4 | 97.1 | 83.5 | 0 | 0 | 11.1 | 21 | 45 | 18:3 | 161 | 304.8 | 2 | 0 | 22.9 | TLF Type A | 11.6 | Grade D(12) and Grade E(5) | No |
| 10 | Huang (2008)49 | 3 yr | R,OS | 30 | 80 | 75 | NA | NA | 8 | 30 | 80 | 292 | NA | NA | 12 | TLF | 24 | NA | No | ||||
| 11 | Wild (2007)38 | 1 yr | R,OS | 10 | 49.1 | 9:1 | 87.4 | 194.4 | 0 | 0 | NR | 11 | 33.5 | 7:4 | 80.9 | 380 | 0 | 0 | NR | TLF mostly AO type A3. Implant removal done at 10 months | 60 | NR | No |
| 12 | Grass (2006)50 | 3 yr | P,OS | 33 | 49.7 | 20:13 | 85 | 40 | 1 | 0 | NR | 24 | 35.7 | 16:8 | 100 | 870 | 0 | 1 | NR | TLF mainly from T12-L2 and two patients of L4 | NR | No | No |
5. Conclusion
In conclusion we can say that role and Indications of the MIS techniques in spinal trauma are expanding quite rapidly. Minimal invasive spine surgeries in thoracolumbar fractures are associated with significantly shorter operative duration, less intra-operative blood loss, smaller incision size, lower infection rates, better pain relief and shorter hospital stay as compared to conventional open spine surgeries. In long term, they provide good kyphosis correction and stable fixation and fusion of spine. Despite all these advantages, it should be used alone in specifically indicated cases (AO type A fractures) only however for AO Type B and C cases it can be conjugated with other techniques such as vertebroplasty and minimal invasive decompression12, 14, 18, 19, 35. Thoracoscopic surgeries may have rarely pulmonary complications and inadvertent injury to other nearby structures and percutaneous pedicle screws may rarely have malpositioning of screws. Both these techniques are associated with stable fixation and good fusion rates. Minimal Invasive spine surgeries should be done by expert surgeons as it involves long learning curve. In terms of efficacy, both minimally invasive spine surgeries as well as open spine surgeries are equally efficacious in treating thoracolumbar spine fractures.
Conflicts of interest
None.
Funding
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.04.012.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Wood K., Buttermann G., Mehbod A., Garvey T., Jhanjee R., Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. J Bone Joint Surg Am. 2004;85-A:773–781. doi: 10.2106/00004623-200305000-00001. 2003 (Erratum in J Bone Joint Surg Am 86-A:1283. [DOI] [PubMed] [Google Scholar]
- 2.Charles Yann Philippe, Zairi Fahed, Vincent César. Minimally invasive posterior surgery for thoracolumbar fractures. New trends to decrease muscle damage. Eur J Orthop Surg Traumatol. 2012;22:1–7. [Google Scholar]
- 3.Kawaguchi Y., Matsui H., Tsuji H. Back muscle injury after posterior lumbar spine surgery, Part 1. Histologic and histochemical analyses in rats. Spine. 1994;19:2590–2597. doi: 10.1097/00007632-199411001-00017. [DOI] [PubMed] [Google Scholar]
- 4.Kawaguchi Y., Matsui H., Tsuji H. Back muscle injury after posterior lumbar spine surgery: Part 2. Histologic and histochemical analyses in humans. Spine. 1994;19:2598–2602. doi: 10.1097/00007632-199411001-00018. [DOI] [PubMed] [Google Scholar]
- 5.Kawaguchi Y., Matsui H., Tsuji H. Back muscle injury after posterior lumbar spine surgery: a histologic and enzymatic analysis. Spine. 1996;21:941–944. doi: 10.1097/00007632-199604150-00007. [DOI] [PubMed] [Google Scholar]
- 6.Styf J., Willen H. vol. 23. 1998. pp. 354–358. (The Effects of External Compression by Three Different Retractors on Pressure in the Erector Spine Muscles during and after Posterior Lumbar Spine Surgery in Humans Spine). [DOI] [PubMed] [Google Scholar]
- 7.Rantanen J., Hurme M., Falck B. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc. herniation Spine. 1993;18:568–574. doi: 10.1097/00007632-199304000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Dajczman E., Gordon A., Kreisman H., Wolkove N. vol. 99. 1991. pp. 270–274. (Long-term Postthoracotomy Pain Chest). [DOI] [PubMed] [Google Scholar]
- 9.Faciszewski T., Winter R.B., Lonstein J.E. The surgical and medical perioperative complications of anterior spinal fusion surgery in the thoracic and lumbar spine in adults. A review of 1223 procedures. Spine. 1995;20:1592–1599. doi: 10.1097/00007632-199507150-00007. [DOI] [PubMed] [Google Scholar]
- 10.Kalso E., Perttunen K., Kaasinen S. Pain after thoracic surgery. Acta Anaesthesiol Scand. 1992;36:96–100. doi: 10.1111/j.1399-6576.1992.tb03430.x. [DOI] [PubMed] [Google Scholar]
- 11.Lee M.C., Coert B.A., Kim S.H., Kim D.H. Endoscopic techniques for stabilization of the thoracic spine. In: Vaccaro A.R., Bono C.M., editors. Minimally Invasive Spine Surgery. Informa Healthcare USA; New York, NY: 2007. pp. 189–202. [Google Scholar]
- 12.Kim D.H., Jahng T.A., Balabhadra R.S.V. Thoracoscopic transdiaphragmatic approach to thoracolumbar junction fractures. Spine J. 2004;4:317–328. doi: 10.1016/j.spinee.2003.11.007. [DOI] [PubMed] [Google Scholar]
- 13.Khoo L.T., Beisee R., Potulski M. Thoracoscopic-assisted treatment of thoracic and lumbar fractures: a series of 371 consecutive cases. Neurosurgery. 2002;51(5 Suppl):104–117. [PubMed] [Google Scholar]
- 14.Beisse R. Video-assisted techniques in the management of thoracolumbar fractures. Orthop Clin N Am. 2007;38:419–429. doi: 10.1016/j.ocl.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 15.Peng M., Cao X.F., Peng G.D., Ma X.C. Retrospective Study on Treating Thoracolumbar Fractures with Video-Assisted Thoracoscopic Surgery and Traditional Anterior Approach Surgery. Zhongguo Gu Shang. 2012;vol. 25(9):747–750. Sep; [PubMed] [Google Scholar]
- 16.Kim S.J., Sohn M.J., Ryoo J.Y., Kim Y.S., Whang C.J. Clinical analysis of video-assisted thoracoscopic spinal surgery in the thoracic or thoracolumbar spinal pathologies. J Korean Neurosurg Soc. 2007;42(4):293–299. doi: 10.3340/jkns.2007.42.4.293. 2007 Oct. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Le Huec J.C., Tournier C., Aunoble S., Madi K., Leijssen P. Video-assisted treatment of thoracolumbar junction fractures using a specific distractor for reduction: prospective study of 50 cases. Eur Spine J. 2009 doi: 10.1007/s00586-009-1121-7. 2010 Mar;19 Suppl 1:S27-32. Epub 2009 Aug 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ray W.Z., Krisht K.M., Dailey A.T., Schmidt M.H. Clinical outcomes of unstable thoracolumbar junction burst fractures: combined posterior short-segment correction followed by thoracoscopic corpectomy and fusion. Acta Neurochir (Wien) 2013 Jul;155(7):1179–1186. doi: 10.1007/s00701-013-1737-6. Epub 2013 May 17. PubMed PMID: 23677637. [DOI] [PubMed] [Google Scholar]
- 19.Shawky A., Al-Sabrout A.M., El-Meshtawy M., Hasan K.M., Boehm H. Thoracoscopically assisted corpectomy and percutaneous transpedicular instrumentation in management of burst thoracic and thoracolumbar fractures. Eur Spine J. 2013 Oct;22(10):2211–2218. doi: 10.1007/s00586-013-2835-0. Epub 2013 May 21. PubMed PMID: 23689847; PubMed Central PMCID: PMC3804716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roy-Camille R., Roy-Camille M., Saillant G., Demeulenaere C., Lelièvre J.F. Surgical therapeutic indications in vertebral injuries with spinal cord syndrome or cauda equina syndrome. Nouv Presse Med. 1972;1:2165–2168. [PubMed] [Google Scholar]
- 21.Magerl F.P. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop Relat Res. 1984;125–141 [PubMed] [Google Scholar]
- 22.Assaker R. Minimal access spinal technologies: state-of-the-art, indications, and techniques. Jt Bone Spine Rev du Rhum. 2004;71(6):459–469. doi: 10.1016/j.jbspin.2004.08.006. 2004. [DOI] [PubMed] [Google Scholar]
- 23.Kim D.Y., Lee S.H., Chung S.K., Lee H.Y. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine. 2005;30:123–129. [PubMed] [Google Scholar]
- 24.Rampersaud Y.R., Foley K.T., Shen A.C., Williams S., Solomito M. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine. 2000;25(20):2637–2645. doi: 10.1097/00007632-200010150-00016. [DOI] [PubMed] [Google Scholar]
- 25.Ahmad F.U., Wang M.Y. Use of anteroposterior view fluoroscopy for targeting percutaneous pedicle screws in cases of spinal deformity with axial rotation. J Neurosurg Spine. 2014;21(5):826–832. doi: 10.3171/2014.7.SPINE13846. [DOI] [PubMed] [Google Scholar]
- 26.Rao P.J., Maharaj M.M., Phan K., Abeygunasekara M., Mobbs R.J. Indirect foraminal decompression following anterior lumbar interbody fusion (ALIF): a prospective radiographic study using a new pedicle to pedicle (P-P) technique. Spine J. 2014;10:1016. doi: 10.1016/j.spinee.2014.12.019. 12.019. [DOI] [PubMed] [Google Scholar]
- 27.Court C., Vincent C. Percutaneous fixation of thoracolumbar fractures: current concepts. Orthop Traumatol Surg Res OTSR. 2012;98(8):900–909. doi: 10.1016/j.otsr.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 28.Mobbs R.J., Sivabalan P., Li J. Technique, challenges and indications for percutaneous pedicle screw fixation. J Clin Neurosci. 2011;18(6):741–749. doi: 10.1016/j.jocn.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 29.Vanek P., Bradac O., Konopkova R. Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg. 2014;20(2):150–156. doi: 10.3171/2013.11.SPINE13479. Spine Feb 2014/ [DOI] [PubMed] [Google Scholar]
- 30.Cimatti Marco, Forcato Stefano, Polli Filippo, Miscus Massimo. Pure percutaneous pedicle screw fixation without arthrodesis of 32 thoraco-lumbar fractures: clinical and radiological outcome with 36-month follow-up. Eur Spine J. 2013;22(Suppl 6):S925–S932. doi: 10.1007/s00586-013-3016-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.yang W.E., Ng Z.X., Koh K.M.R. Percutaneous pedicle screw fixation for thoracolumbar burst fracture: a Singapore experience Singapore. Med J. 2012;53(9):577. [PubMed] [Google Scholar]
- 32.Fang L.M., Zhang Y.J., Zhang J. Minimally invasive percutaneous pedicle screw fixation for the treatment of thoracolumbar fractures and posterior ligamentous complex injuries Beijing. Da Xue Xue Bao. 2012;44(6):851–854. 2012 Dec 18. [PubMed] [Google Scholar]
- 33.Bironneau A., Bouquet C., Millet-Barbe B., Leclercq N., Pries P. Percutaneous internal fixation combined with kyphoplasty for neurologically intact thoracolumbar fractures: a prospective cohort study of 24 patients with one year of follow-up. Orthop Traumatol Surg Res. 2011;97:389–395. doi: 10.1016/j.otsr.2011.02.009. [DOI] [PubMed] [Google Scholar]
- 34.Blondel B., Fuentes S., Pech-Gourg G., Adetchessi T., Tropiano P. Percutaneous management of thoracolumbar burst fractures: evolution of techniques and strategy. Orthop Traumatol Surg Res. 2011;97:527–532. doi: 10.1016/j.otsr.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 35.Ni W.F., Huang Y.X., Chi Y.L., Xu H.Z., Lin Y. Percutaneous pedicle screw fixation for neurologic intact thoracolumbar burst fractures. J Spinal Disord Tech. 2010;23:530–537. doi: 10.1097/BSD.0b013e3181c72d4c. [DOI] [PubMed] [Google Scholar]
- 36.Palmisani M., Gasbarrini A., Brodano G.B., De Iure F., Cappuccio M. Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J. 2009;18:71–74. doi: 10.1007/s00586-009-0989-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Merom L., Raz N., Hamud C., Weisz I., Hanani A. Minimally invasive burst fracture fixation in the thoracolumbar region. Orthopedics. 2009;32 doi: 10.3928/01477447-20090401-03. [DOI] [PubMed] [Google Scholar]
- 38.Wild M.H., Glees M., Plieschnegger C., Wenda K. Five-year follow-up examination after purely minimally invasive posterior stabilization of thoracolumbar fractures: a comparison of minimally invasive percutaneously and conventionally open treated patients. Arch Orthop Trauma Surg. 2007;127:335–343. doi: 10.1007/s00402-006-0264-9. [DOI] [PubMed] [Google Scholar]
- 39.Maciejczak A., Barnas P., Dudziak P., Jagiełło-_Bajer B., Litwora B. Posterior keyhole corpectomy with percutaneous pedicle screw stabilization in the surgical management of lumbar burst fractures. Neurosurgery. 2007;60:232–241. doi: 10.1227/01.NEU.0000255399.08033.B3. [DOI] [PubMed] [Google Scholar]
- 40.Phan Kevin, Rao Prashanth J., Mobbs Ralph J. Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg. 2015;135:85–92. doi: 10.1016/j.clineuro.2015.05.016. [DOI] [PubMed] [Google Scholar]
- 41.Wang H., Zhou Y., Li C., Liu J., Xiang L. Comparison of open versus percutaneous pedicle screw fixation using the Sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg. 2017 Apr;30(3):E239–E246. doi: 10.1097/BSD.0000000000000135. PubMed PMID: 28323706. [DOI] [PubMed] [Google Scholar]
- 42.Lee J.K., Jang J.W., Kim T.W., Kim T.S., Kim S.H., Moon S.J. Percutaneous shortsegment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: is it effective?: comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir. 2013;155(12):2305–2312. doi: 10.1007/s00701-013-1859-x. discussion 2312. [DOI] [PubMed] [Google Scholar]
- 43.Grossbach A.J., Dahdaleh N.S., Abel T.J., Woods G.D., Dlouhy B.J., Hitchon P.W. Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus. 2013;35(2):E2. doi: 10.3171/2013.6.FOCUS13176. [DOI] [PubMed] [Google Scholar]
- 44.Bronsard N., Boli T., Challali M. Comparison between percutaneous and traditional fixation of lumbar spine fracture: intraoperative radiation exposure levels and outcomes. Orthop Traumatol Surg Res OTSR. 2013;99(2):162–168. doi: 10.1016/j.otsr.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 45.Song H.P., Lu J.W., Liu H., Zhang C. Case-control studies between two methods of minimally invasive surgery and traditional open operation for thoracolumbar fractures. Zhong Guo Gu Shang. 2012;25(4):313–316. [PubMed] [Google Scholar]
- 46.Jiang X.Z., Tian W., Liu B. Comparison of a paraspinal approach with a percutaneous approach in the treatment of thoracolumbar burst fractures with posterior ligamentous complex injury: a prospective randomized controlled trial. J Int Med Res. 2012;40(4):1343–1356. doi: 10.1177/147323001204000413. [DOI] [PubMed] [Google Scholar]
- 47.Tian W., Han X., He D. The comparison of computer assisted minimally invasive spine surgery and traditional open treatment for thoracolumbar fractures. Zhonghua Wai Ke Za Zhi. 2011;49(12):1061–1066. [PubMed] [Google Scholar]
- 48.Wang H.W., Li C.Q., Zhou Y., Zhang Z.F., Wang J., Chu T.W. Percutaneous pedicle screw fixation through the pedicle of fractured vertebra in the treatment of type A thoracolumbar fractures using Sextant system: an analysis of 38 cases. Chin J Traumatol. 2010;13(3):137–145. [PubMed] [Google Scholar]
- 49.Huang Q.S., Chi Y.L., Wang X.Y. Comparative percutaneous with open pedicle screw fixation in the treatment of thoracolumbar burst fractures without neurological deficit. Zhonghua Wai Ke Za Zhi. 2008;46(2):112–114. [PubMed] [Google Scholar]
- 50.Grass R., Biewener A., Dickopf A., Rammelt S., Heineck J., Zwipp H. Percutaneous dorsal versus open instrumentation for fractures of the thoracolumbar border. A comparative, prospective study. Unfallchirurg. 2006;109(4):297–305. doi: 10.1007/s00113-005-1037-6. [DOI] [PubMed] [Google Scholar]
- 51.Takami M., Yamada H., Nohda K., Yoshida M. A minimally invasive surgery combining temporary percutaneous pedicle screw fixation without fusion and vertebroplasty with transpedicular intracorporeal hydroxyapatite blocks grafting for fresh thoracolumbar burst fractures: prospective study. Eur J Orthop Surg Traumatol. 2014 Jul;24(Suppl 1):S159–S165. doi: 10.1007/s00590-013-1266-2. Epub 2013 Jul 5. PubMed PMID: 23828560. [DOI] [PubMed] [Google Scholar]
- 52.Schmidt Oliver I., Strasser Sergej, Kaufmann Victoria, Strasser Ewald, Gahr Ralf H. Role of early minimal-invasive spine fixation in acute thoracic and lumbar spine trauma. Indian J Orthop. 2007 Oct-Dec;41(4):374–380. doi: 10.4103/0019-5413.37003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.