Abstract
Background
Cephalomedullary nails are presently the gold standard in management of unstable trochanteric fractures. The tip-apex distance (TAD) is one of the most important factors that determines success or failure of fixation, but was described originally in context of an extramedullary hip screw. Cephalomedullary nails use a different biomechanical approach to fixation; and it is hypothesized that the TAD rule may not apply similarly with these. The aim of this study is to assess whether a high TAD correlates with poor outcomes with cephalomedullary nails, and to elucidate other factors that may predict such outcome.
Methods
We retrospectively reviewed the clinical and radiographic records of patients with intertrochanteric fractures, treated at our institution over a 2-year period. Those with unstable fractures (31.A2 and 31.A3), and who were treated with cephalomedullary nails were included in the study. The TAD and the position of the device in the femoral head (Cleveland index) were assessed. Other factors that could influence outcome like age, gender, AO fracture type, restoration of neck-shaft angle and degree of osteoporosis were analysed. Radiographic records of up-to at-least 3 months post-operatively were assessed for complications.
Results
After applying the exclusion criteria, 75 patients were included in the analysis. The overall rate of complications was 12%. They occurred in two major patterns - varus collapse and cut-out occurred in 5 patients (6.67%), and device migration in 4 patients (5.33%). The average TAD of patients with cut-out was 28.78 mm, compared to 19.44 mm in those without cut-out (p = 0.002). Our data predicted a cut-off TAD >23.56 mm as most significant for cut-out with cephalomedullary nails. On univariate logistic regression, high TAD (p = 0.009), sub-optimal device positioning (p = 0.02) and poor restoration of neck-shaft angle (p = 0.04) were found to be significant for varus collapse and cut-out, but not for complications relating to device migration. On multivariate analysis, none of the above factors reached statistical significance in isolation.
Conclusion
As with extramedullary devices, TAD, along with sub-optimal device positioning and poor restoration of neck-shaft angle is a useful predictor of cut-out even with cephalomedullary nails, negating the initial hypothesis. The above factors in combination have a more significant effect than any one factor in isolation to cause varus collapse and implant cut-out. However these do not affect Z effect, reverse Z effect or other types of device migration seen especially with dual-screw nails.
Keywords: Tip-apex distance, Intertrochanteric fractures, Implant failure, Cut-out, Cephalomedullary nails
1. Introduction
Complications following fixation of intertrochanteric fractures have a major adverse effect on the prognosis especially in the geriatric population, where early restoration of ambulatory capacity is critical. Extra-medullary devices have been fraught with complications when used for the management of unstable intertrochanteric fractures and hence, cephalomedullary devices have now largely become the norm of management of these fractures.1, 2, 3 Various designs of intramedullary implants have been introduced, with a view to improve fixation in these unstable fractures, especially in the setting of osteoporosis in the geriatric age group. Nevertheless, these implants have not been devoid of complications, with up to 31% complications reported in literature in some series.4, 5, 6, 7
The surgeon dependent risk factors for implant failure in the context of extra-medullary devices have been well documented in literature,8,9 the tip apex distance (TAD) and device position in the femoral head being the most important of these. A TAD of >25 mm, and an off centre position in the femoral head, are considered risk factors for fixation failure which were originally described mainly in context of an extramedullary hip screw.8 However, fixation with cephalomedullary nails is biomechanically different from that with an extramedullary sliding compression screw.10,11 With cephalomedullary nails, the nail itself acts as an intramedullary buttress, and the reduced lever arm provides a biomechanical advantage. We hypothesized that owing to biomechanical differences, the factors that predict success or failure with extramedullary devices may not hold true for intramedullary devices, which utilize a different approach to fixation.
The most common pattern of failure seen after fixation of unstable intertrochanteric fractures is cut-out of the device from the femoral head. Cut-out can be defined as ‘‘the collapse of the neck-shaft angle into varus, leading to extrusion, or so-called cut-out, of the device from the femoral head.’’12 This pattern of failure has been described consistently with both extramedullary and intramedullary devices.4, 5, 6, 7, 8 In almost all cases, this requires revision surgery, and causes further morbidity. However, with cephalomedullary nails, device migration in the femoral head has been recognized as another important complication.4, 5, 6, 7,13 This form of implant failure has been mentioned in literature in various forms – for example as the Z and reverse-Z effect with dual-screw design nails, and as axial cut-out (medial migration) in case of helical blade nails.14 There are very few studies in literature that have studied the role of TAD in predicting outcomes exclusively with cephalomedullary nails.15,16 To the best of our knowledge, no study has described the role of TAD (or other predictors of outcome) in an exclusive subset of unstable trochanteric fractures, which are most prone for complications. Also, no study has looked at complications other than cut-out in relation to TAD, which are frequent with cephalomedullary nails.
We conducted a retrospective study of unstable trochanteric fractures treated with cephalomedullary nails, to study the correlation of TAD with the occurrence of complications and the pattern of such complications. We also took into account other factors like age, gender, fracture type, restoration of neck-shaft angle, device position in femoral head and degree of osteoporosis, which are known possible predictors of outcome.
2. Methods
We performed a retrospective analysis of clinical and radiographic records of all patients with intertrochanteric fractures treated at our institution over a 2-year period from December 2013 to December 2015. The age of the patient at the time of surgery, and gender were noted from the medical records. The patients' radiographs were accessed from the institution's picture archiving and communication system (PACS). The initial radiographs obtained at injury were used to classify the fractures as per the A.O classification system,17 and those with 31.A1 type fractures were excluded. Those treated with extramedullary devices, non-operatively, or those with insufficient radiographic follow up (less than 3 months post operatively) were also excluded. Patients with unstable 31.A2 and 31.A3 fractures treated with a cephalomedullary nail, and with radiographic records available till at least 3 months post operatively were included.
The degree of osteoporosis was judged by the Singh's index,18 which was noted from the antero-posterior view of the contra-lateral uninjured hip. This assessment of osteoporosis could not be done in five patients due to previous implants in the contra-lateral hip. A Singh's grade of 3 or lesser was considered definite osteoporosis.
The restoration of neck-shaft angle was measured on PACS using the post-operative antero-posterior view by noting the varus or valgus change in neck-shaft angle compared to the normal hip. A change of less than or equal to 5° was considered good, between 5 and 10° as acceptable, and greater than 10° as poor restoration of neck-shaft angle.19 Since a lateral view of the uninjured hip was not routinely done, an objective assessment of anteversion or retroversion could not be done while assessing reduction.
The TAD as described by Baumgaertner8 was measured using the PACS (picture archiving and communication system) tool on immediate post-operative X-rays on both antero-posterior and lateral views. For a dual-screw nail, the tip of the inferior screw was used to calculate TAD.
The Cleveland zone index20 was used to specify the position of the screw/blade in the femoral head on antero-posterior and lateral radiographs. The position was classified as superior, centre or inferior on the AP view and anterior, centre or posterior on the lateral view. A centre-centre or inferior-centre position has traditionally been described as the optimal position.21,22 Screw/blade positioning was considered optimal if it was inferior-centre or centre-centre. Any deviation from these two positions was considered sub-optimal positioning.
The post-operative radiographs were assessed serially for development of complications - either cut-out with varus collapse, or device migration like back out of the screws/blade, the Z and reverse Z effects and cut-through into the hip.
2.1. Statistical analysis
Statistical analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0. Quantitative variables (age, TAD) were compared using Independent T test or Mann-Whitney Test (when the data sets were not normally distributed) between the two groups. Qualitative variables (gender, change in neck-shaft angle, osteoporosis, Cleveland zone) were correlated using Chi-Square test or Fisher's exact test. A Receiver operating characteristic (ROC) curve was plotted from the data to determine a cut off point for TAD that best predicted cut out. Univariate logistic regression was used to assess the association of complications with the parameters of age, gender, change in neck-shaft angle, tip-apex distance, device position in the femoral head (optimal or sub-optimal), fracture type and Singh's index. Multivariate analysis was done for the factors that were significant in the univariate analysis. A p-value of <0.05 was considered statistically significant.
3. Results
There were a total of 146 patients with intertrochanteric fractures who presented to our institution during the study period. 75 patients met the inclusion criteria – 32 males and 43 females with an average age of 69.56 years (range 30–96 years). Of these, 39 patients had been treated with a helical blade nail, 29 with a dual screw nail and 7 with a gamma nail. The complication rate was 12% with a total of 9 complications encountered – 5 cut-outs (Fig. 1) and 4 device migration (2 screw back-outs, 1 Z-effect, 1 reverse-Z effect) (Fig. 2). The average TAD of the patients who suffered cut-out was 28.72 mm compared to 19.44 mm in patients with no cut-out, and this difference was found to be statistically significant (p = 0.002). All cases of cut-outs were seen in females, whereas 75% migration cases occurred in males (p = 0.06). None of the patients who had a TAD of less than 24.4 mm suffered cut-out. Three cut-outs were seen with helical blade nails and two with dual screw nails. No significant difference was found in cut-out rate between the screw and helical blade nails (p = 0.9). However, all cases of device migration were seen with dual-screw nails (p = 0.04).
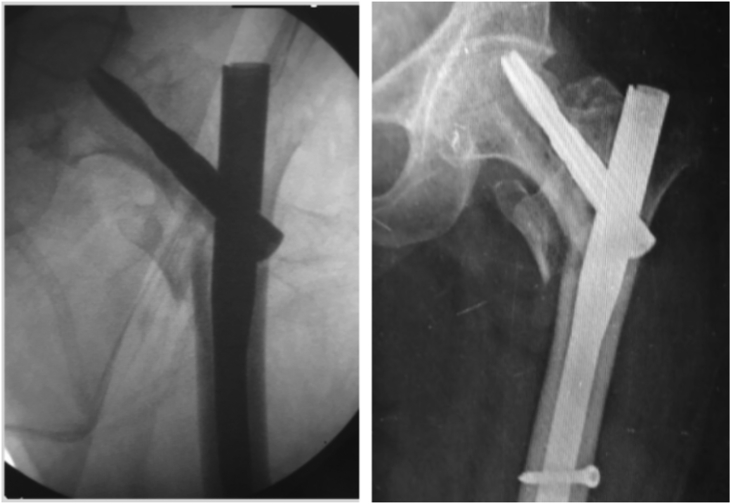
Fig. 1.
A 31.A2 fracture fixed with a helical blade nail. TAD was 34.6 mm. X rays at 6 weeks show collapse and cut out.
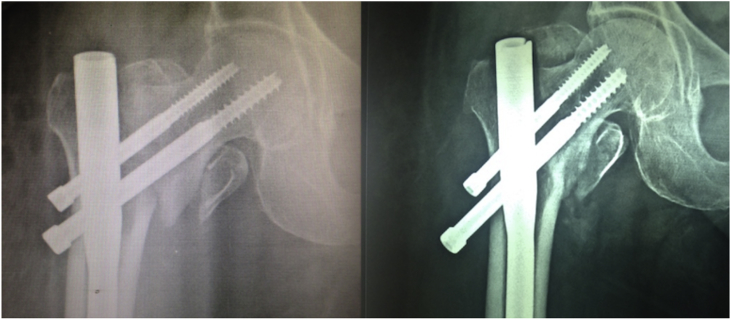
Fig. 2.
Showing screw back out at 6 weeks without any significant collapse or loss of reduction.
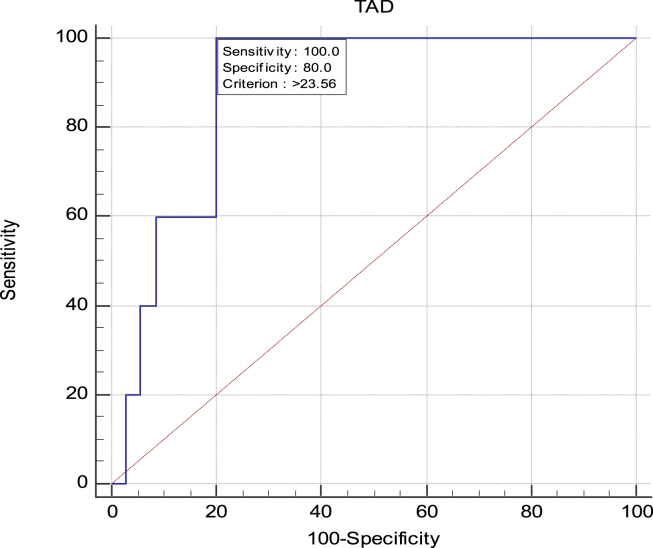
We plotted a receiver operating characteristic (ROC) curve (Table 1) from our overall data to find a cut off point for TAD to best predict cut-out, and a TAD of >23.56 mm was found to be 100% sensitive as a predictor of cut-out (p < 0.0001). This is in close approximation to the conventional 25 mm limit described by Baumgaertner et al. for extramedullary devices. When the conventional limit of 25 mm was used as predictor of cut-out in our group, it very closely approximated statistical significance (p = 0.051).
Table 1.
ROC curve plotted from the data showed that TAD >23.56 mm is most sensitive for predicting cut-out. This is in close approximation to the original 25 mm limit described by Baumgaertner et al.
The assessment of complications in the dual screw and helical blade groups separately has been summarized in Table 2 and Table 3 respectively. In the dual-screw group, the two cases of cut-out averaged a TAD of 26.27 mm (24.42–28.12 mm) with sub-optimal device positioning in one of them. Both cut-outs occurred in females. Whereas among the four cases of device migration, three were optimally positioned, with an optimal TAD (average 20.9 mm). Although no cut-out was observed among the seven cases of 31.A3 fractures treated with dual-screw nails, device migration occurred in two, comprising 50% of cases of migration. In the helical blade group, there were three cases of cut-out. All three were females with TAD averaging 30.45 mm (24.40–34.65 mm) and sub-optimal positioning of device in all three. The restoration of neck-shaft angle was poor in one case.
Table 2.
Assessment of variables affecting outcome in dual-screw nails.
| Assessment of variables affecting outcome in dual-screw nails (n = 29) | ||||
|---|---|---|---|---|
| Variable | No complication (n = 23) | Device migration (n = 4) | Cut-out (n = 2) | |
| Average age (years) | 61.91 | 44 | 87.5 | |
| Sex distribution | Males | 15 (65.2%) | 3 (75%) | 0 (0%) |
| Females | 8 (34.8%) | 1 (25%) | 2 (100%) | |
| Fracture type | 31.A2 | 16 (69.6%) | 2 (50%) | 2 (100%) |
| 31.A3 | 7 (30.4%) | 2 (50%) | 0 (0%) | |
| Singh's index | >3 | 8 (34.8%) | 3 (75%) | 0 (0%) |
| 3 or less | 13 (56.5%) | 1 (25%) | 1 (50%) | |
| Cannot assess | 2 (8.7%) | 0 (0%) | 1 (50%) | |
| Restoration of neck-shaft angle | Good | 15 (65.2%) | 2 (50%) | 0 (0%) |
| Acceptable | 6 (26.1%) | 2 (50%) | 1 (50%) | |
| Poor | 0 (0%) | 0 (0%) | 0 (0%) | |
| Cannot assess | 2 (8.7%) | 0 (0%) | 1 (50%) | |
| TAD | >23.56 mm | 4 (17.4%) | 1 (25%) | 2 (100%) |
| <23.56 mm | 19 (82.6%) | 3 (75%) | 0 (0%) | |
| Device positioning | Optimal | 4(17.4%) | 3 (75%) | 1 (50%) |
| Sub-optimal | 19 (82.6%) | 1 (25%) | 1 (50%) | |
Table 3.
Assessment of variables affecting outcome in helical blade nails.
| Assessment of variables affecting outcome in helical blade nails (n = 39) | |||
|---|---|---|---|
| Variable | No complication (n = 36) | Cut-out (n = 3) |
|
| Average age (years) | 73.75 | 73 | |
| Sex distribution | Males | 12 (33.3%) | 0 (0%) |
| Females | 24 (66.7%) | 3 (100%) | |
| Fracture type | 31.A2 | 32 (88.9%) | 2 (66.7%) |
| 31.A3 | 4 (11.1%) | 1 (33.3%) | |
| Singh's index | >3 | 14 (38.9%) | 1 (33.3%) |
| 3 or less | 21 (58.3%) | 2 (66.7%) | |
| Cannot assess | 1 (2.8%) | 0 (0%) | |
| Restoration of neck-shaft angle | Good | 26 (72.2%) | 2 (66.7%) |
| Acceptable | 8 (22.2%) | 0 (0%) | |
| Poor | 1 (2.8%) | 1 (33.3%) | |
| Cannot assess | 1 (2.8%) | 0 (0%) | |
| TAD | >23.56 mm | 9 (25%) | 3 (100%) |
| <23.56 mm | 27 (75%) | 0 (0%) | |
| Device positioning | Optimal | 26(72.2%) | 0 (0%) |
| Sub-optimal | 10 (27.8%) | 3 (100%) | |
There were no complications in the single screw group. All seven cases operated by single screw nails had TAD <23.56 mm and 85.7% were optimally positioned with good restoration of neck-shaft angle. The findings of this group are summarized in Table 4.
Table 4.
Assessment of variables affecting outcome in single-screw nails.
| Assessment of variables in single screw nails (n = 7) | ||
|---|---|---|
| Average age (years) | 76 | |
| Sex distribution | Males | 2 (28.6%) |
| Females | 5 (71.4%) | |
| Fracture type | 31.A2 | 4 (57.1%) |
| 31.A3 | 3 (42.9%) | |
| Singh's index | >3 | 1 (14.3%) |
| 3 or less | 5 (71.4%) | |
| Cannot assess | 1 (14.3%) | |
| Restoration of neck-shaft angle | Good | 4 (57.1%) |
| Acceptable | 2 (28.6%) | |
| Poor | 0 (0%) | |
| Cannot assess | 1 (14.3%) | |
| TAD | >23.56 mm | 0 (0%) |
| <23.56 mm | 7 (100%) | |
| Device positioning | Optimal | 6 (85.7%) |
| Sub-optimal | 1 (14.3%) | |
From the data, no association was found between TAD and device migration. The average TAD in patients who had complications relating to device migration was 20.9 mm, which was within the traditionally described safe limit. It was not significantly different from TAD of patients who did not suffer a complication (p = 0.79). Screw migration was seen to occur with a TAD as low as 17.1 mm. Only one of four cases of device migration had a TAD of 26.47 mm. Notably, Singh's index also did not correlate significantly with migration (p = 0.2).
Two separate univariate logistic regressions were performed to correlate the two types of complications (cut-out and device migration) with age, gender, fracture type, Singh's index, change of neck-shaft angle, TAD and device positioning (Table 5). When performed for cut out, the factors which reached statistical significance on the univariate analysis were TAD (p = 0.009), sub-optimal implant positioning (p = 0.02) and poor restoration of neck-shaft angle (p = 0.04). The non-significant factors were age, gender, fracture type and Singh's index. However, when univariate logistic regression was performed for device migration, none of the above factors was found to have a significant correlation.
Table 5.
Univariate analysis of the predictive factors for cut-out.
| Beta coefficient | S.E. (Standard error) | p-value | Odds ratio | 95% confidence interval for Odds ratio |
||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Age | .065 | .047 | .169 | 1.067 | .973 | 1.170 |
| TAD | .215 | .082 | .009 | 1.240 | 1.056 | 1.456 |
| Sex | ||||||
| Female | 1.000 | |||||
| Male | – | – | – | – | – | – |
| Type of fracture | ||||||
| A2 | 1.000 | |||||
| A3 | -.170 | 1.154 | .883 | .844 | .088 | 8.095 |
| Singh's grade | ||||||
| <=3 | 1.000 | |||||
| >3 | −0.977 | 1.181 | 0.408 | 0.376 | 0.037 | 3.807 |
| Restoration of neck-shaft angle | ||||||
| Good | 1 | |||||
| Acceptable | .234 | 1.254 | .852 | 1.263 | .108 | 14.763 |
| Poor | 3.178 | 1.588 | .045 | 24.000 | 1.068 | 539.107 |
| TAD | ||||||
| <=25 | 1.000 | |||||
| >25 | 1.884 | .963 | .051 | 6.577 | .996 | 43.443 |
| Device positioning | ||||||
| Optimum | 1.000 | |||||
| Sub Optimum | 2.603 | 1.154 | .024 | 13.500 | 1.407 | 129.528 |
A multivariate regression analysis (Table 6) was performed for the above three significant factors of the univariate regression; however no single factor reached statistical significance in isolation, when the effect of the other two factors was adjusted for. This indicates that high TAD, sub-optimal position and poor restoration of neck-shaft angle are not mutually exclusive of each other.
Table 6.
Multivariate regression of the factors found significant in univariate analysis.
| Beta coefficient | Standard Error | p-value | Odds ratio | 95% confidence interval for Odds ratio |
||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| TAD | .152 | .108 | .160 | 1.164 | 0.942 | 1.439 |
| Restoration of neck-shaft angle | ||||||
| Good | 1 | |||||
| Acceptable | .552 | 1.502 | .713 | 1.737 | .091 | 32.983 |
| Poor | 1.367 | 1.794 | .446 | 3.923 | 0.117 | 132.061 |
Due to multi-collinearity, the device positioning as per Cleveland Zone was leading to a high standard error and hence, was not included in multivariate regression.
4. Discussion
Our results show a complication rate of 12% in this retrospective series, which is comparable with the complication rates seen in various other studies with intramedullary fixation of trochanteric fractures using similar nail designs.23,24 Our results indicate that a high TAD correlates with cut-out of the device from the femoral head even with cephalomedullary nails. However, it does not seem to affect the occurrence of screw migration, which occurred even when TAD was within the safe limit.
To the best of our knowledge there are only three other studies in literature, which have assessed the role of TAD with cephalomedullary nails.15,16,25 Their comparison with our study is shown in Table 7. Geller et al.15 performed a study of TAD in gamma nails and trochanteric fixation nails. In their study, the average TAD of patients with a cut-out was 38 mm compared to 18 mm in those who didn't. Kashigar et al.16 had 62 trochanteric fractures in their study group treated with intertrochanteric subtrochanteric (ITST) or Natural Nail. The average TAD of patients who cut out was 29.77 mm, and was found to be a significant predictor of cut-out. Lobo-Escolar et al.25 also found that a higher TAD was predictive of cut-out with Gamma and ITST nails.
Table 7.
Comparison of the present study with previous similar studies in literature.
| Study | Percentage of unstable fractures in study group | Types of nails used | Average TAD in cut-out cases | Average TAD of cases without complication |
|---|---|---|---|---|
| 15 | 41% | Gamma nail + TFN | 38 mm | 18 mm |
| 25 | 69.5% | Gamma nail + ITST | 32.2 mm | 23.8 mm |
| 16 | 75.3% | Natural nail + ITST | 29.66 mm | 15.98 mm |
| Present study | 100% | Dual screw + Helical blade + Gamma nail | 28.72 mm | 19.44 mm |
TFN – Trochanteric fixation nail.
ITST – Intertrochanteric Subtrochanteric nail.
However, there are important differences between our study and these previous studies. Firstly, our study group comprises exclusively of unstable intertrochanteric fractures, which pose a significantly higher risk of implant failure. We did not include stable intertrochanteric fractures as these do well with extramedullary fixation, and are not an absolute indication for nailing. Similarly, post-fixation biomechanics of subtrochanteric fractures is significantly different from unstable 31.A2 and 31.A3 intertrochanteric fractures, and were excluded. The fact that implant failure is of maximum concern with unstable intertrochanteric fractures is proven in the results of the studies mentioned previously – no cut-outs were observed with either stable intertrochanteric or subtrochanteric fractures in these studies.15,16 Since our study population comprised of only unstable intertrochanteric fractures, it puts the role of TAD and other factors in a better perspective.
Secondly, the types of nails used in our study are different from the previous studies. Our study included helical blade as well as single and dual-screw nails. Only one other study has looked at TAD in helical blade nails, and no study on TAD has included dual screw nails. Nikoloski et al.14 studied the association of TAD with failure in helical blades and found a bimodal distribution of failure in relation to TAD. Medial migration occurred with TAD <20 mm whereas cephalad cut-out was seen with TAD >30 mm. They proposed that for helical blades, the optimum TAD is between 20 and 30 mm. However, in our patients treated with helical blades, we encountered only cut-out in three cases (Fig. 1), which occurred with TAD of 24.4 mm, 32.3 mm and 34.6 mm.
Thirdly, none of the previous studies have described back out or migration of screws, or its relation to TAD. This is perhaps because these studies did not include dual-screw nails, which pose this complication more frequently, compared to other nails. In our study all cases of device migration were seen in dual-screw nails (p = 0.04). We found that screw migration (Fig. 2) occurred without significant fracture collapse, and was independent of TAD, restoration of neck-shaft angle, device position or Singh's index. It is well understood that poor screw purchase in osteoporotic bone is probably an important factor determining device migration. It could also be hypothesized that a high TAD would place the screw in the region of the Ward's triangle, which is relatively osteoporotic, predisposing to screw loosening and back out. However, in our study, this was not found to correlate with either TAD (p = 0.7) or Singh's index (p = 0.2). This is probably because the Singh's index is at best, a rough estimate of the degree of osteoporosis.26 Biomechanical studies have demonstrated that osteoporosis determined by DEXA scan correlates strongly with device migration.27,28 Henschel et al. assessed screw migration in the proximal femur and showed that with little bony contact at the fracture site, there is differential stress in a dual screw system, which causes migration.29 Other possible factors that have been cited for device migration are an improper entry point, loss of medial support, and a longer superior screw.13 However, further clinical studies are needed to elucidate the reasons for this phenomenon.
On the whole, the change in neck-shaft angle, position of the device in the femoral head, and TAD, all reached statistical significance as predictors of cut-out in our univariate analysis. This is similar to the results of two studies mentioned previously.16,25 In addition to these factors, Lobo-Escolar et al.25 also found the Singh's index to be a significant predictor of cut-out but this finding was not replicated in our study, possibly due to the poor sensitivity and inter-observer reliability of this index mentioned above.
The results of the multivariate analysis indicate that a combination of all the significant factors – high TAD, sub-optimal device positioning and poor restoration of neck-shaft angle – may be responsible for cut-out rather than any single factor in isolation. Similar to our study, Kashigar et al.16 did not find TAD or any of these factors to reach significance by itself in the multivariate analysis. This led them to propose the concept of calcar referenced TAD (CalTAD) which was proposed to be a better predictor for cut-out than the conventional TAD – this was the only significant factor found in their multivariate analysis.16
The advantages of our study are that we have included a subset of only unstable trochanteric fractures, and described the role of TAD in relation to both implant cut-out and screw migration, which has not been described previously. A relatively small sample size and lack of long-term follow up are other shortcomings of our study, which may be addressed in future research. Our findings are based on a heterogeneous group including three different nail types, rather than a single type of nail. We also recognize that our use of the Singh's index rather than a DEXA scan to quantify osteoporosis is a drawback. Clinical studies using DEXA scan to quantify osteoporosis at the hip may replicate the findings of biomechanical studies27,28 which show poor bone quality to be the most significant factor for screw migration. Nevertheless, our study re-affirms that irrespective of the type of fixation – whether extramedullary or intramedullary, the principles to obtain optimum reduction and fixation remain the same.
5. Conclusions
The initial hypothesis that a high TAD may not be a predictor of complications with cephalomedullary nails owing to their different biomechanics from extramedullary devices seems to be negated by our findings – a high TAD along with sub-optimal device positioning and poor restoration of neck-shaft angle – predispose to cut-out even with cephalomedullary nails. A combination of the above factors affects outcome more than any single factor alone. However, achieving a TAD within the safe limit does not seem to influence the occurrence of device migration, Z effect or reverse Z effect, which are important patterns of complications, especially of dual screw nails.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- 1.Cheema G.S., Rastogi A., Singh V., Goel S.C., Mishra D., Arora S. Comparison of cutout resistance of dynamic condylar screw and proximal femoral nail in reverse oblique trochanteric fractures: a biomechanical study. Indian J Orthop. 2012;46:259–265. doi: 10.4103/0019-5413.96369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-yassari G., Langstaff R.J., Jones J.W., Al-Lami M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury. 2002;33:395–399. doi: 10.1016/s0020-1383(02)00008-6. [DOI] [PubMed] [Google Scholar]
- 3.Schipper I.B., Bresina S., Wahl D., Linke B., Van Vugt A.B., Schneider E. Biomechanical evaluation of the proximal femoral nail. Clin Orthop Relat Res. 2002 Dec;(405):277–286. doi: 10.1097/00003086-200212000-00035. [DOI] [PubMed] [Google Scholar]
- 4.Hohendorff B., Meyer P., Menezes D., Meier L., Elke R. Treatment results and complications after PFN osteosynthesis. Unfallchirurg. 2005;108(11) doi: 10.1007/s00113-005-0962-8. 938, 940, 941-46. [DOI] [PubMed] [Google Scholar]
- 5.Domingo L.J., Cecilia D., Herrera A., Resines C. Trochanteric fractures treated with a proximal femoral nail. Int Orthop. 2001;25:298–301. doi: 10.1007/s002640100275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pavelka T., Matejka J., Cervenkova H. Complications of internal fixation by a short proximal femoral nail. Acta Chir Orthop Traumatol Cech. 2005;72:344–354. [PubMed] [Google Scholar]
- 7.Sharma A., Mahajan A., John B. A comparison of the clinico-radiological outcomes with proximal femoral nail (PFN) and proximal femoral nail antirotation (PFNA) in fixation of unstable intertrochanteric fractures. J Clin Diagn Res: JCDR. 2017;11(7):RC05–RC09. doi: 10.7860/JCDR/2017/28492.10181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baumgaertner M.R., Curtin S.L., Lindskog D.M., Keggi J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg Am. 1995;77:1058–1064. doi: 10.2106/00004623-199507000-00012. [DOI] [PubMed] [Google Scholar]
- 9.De Bruijn K., Hartog D., Tuinebreijer W., Roukema G. Reliability of predictors for screw cut out in Intertrochanteric hip fractures. J Bone Jt Surg. 2012;94-A(14):1266–1272. doi: 10.2106/JBJS.K.00357. [DOI] [PubMed] [Google Scholar]
- 10.Strauss E., Frank J., Lee J., Kummer F.J., Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures. Biomech Eval Injury. 2006;37:984–989. doi: 10.1016/j.injury.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Windolf M., Braunstein V., Dutoit C., Schwieger K. Is a helical shaped implant a superior alternative to the Dynamic Hip Screw for unstable femoral neck fractures? A biomechanical investigation. Clin Biomech. 2009;24:59–64. doi: 10.1016/j.clinbiomech.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 12.Fujii T., Nakayama S., Hara M., Koizumi W., Itabashi T., Saito M. Tip-apex distance is most important of six predictors of screw cutout after internal fixation of intertrochanteric fractures in women. JBJS Open Access [Internet] 2017;2(4) doi: 10.2106/JBJS.OA.16.00022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pires R.E., Santana E.O., Jr, Santos L.E., Giordano V., Balbachevsky D., Dos Reis F.B. Failure of fixation of trochanteric femur fractures: Clinical recommendations for avoiding Z-effect and reverse Z-effect type complications. Patient Saf Surg. 2011;5:17. doi: 10.1186/1754-9493-5-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nikoloski A.N., Osbrough A.L., Yates P.J. Should the tip-apex distance (TAD) rule be modified for the proximal femoral nail antirotation (PFNA)? A retrospective study. J Orthop Surg Res. 2013 Oct 17;8:35. doi: 10.1186/1749-799X-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Geller J.A., Saifi C., Morrison T.A., Macaulay W. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int Orthop. 2010;34(5):719–722. doi: 10.1007/s00264-009-0837-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kashigar A., Vincent A., Gunton M.J., Backstein D., Safir O., Kuzyk P.R. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint Lett J. 2014 Aug;96-B(8):1029–1034. doi: 10.1302/0301-620X.96B8.33644. [DOI] [PubMed] [Google Scholar]
- 17.Marsh J.L., Slongo T.F., Agel J. Fracture and dislocation classification compendium - 2007: orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S1–S133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 18.Singh M., Nagrath A.R., Maini P.S. Changes in trabecular pattern in the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am. 1970;52(1):457–467. [PubMed] [Google Scholar]
- 19.Karapinar L., Kumbaraci M., Kaya A.İ., Imerci A., Incesu M. Proximal femoral nail anti-rotation (PFNA) to treat peritrochanteric fractures in elderly patients. European Journal of Orthopaedic Surgery & Traumatology. 2011;22:237–243. [Google Scholar]
- 20.Cleveland M., Bosworth D.M., Thompson F.R., Wilson H.J., Jr., Ishizuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41(A) 1399-408. [PubMed] [Google Scholar]
- 21.Parker M.J. Cutting-out of the dynamic hip screw related to its position. J Bone Joint Surg Br. 1992;74:625. doi: 10.1302/0301-620X.74B4.1624529. [DOI] [PubMed] [Google Scholar]
- 22.Hsueh K.K., Fang C.K., Chen C.M., Su Y.P., Wu H.F., Chiu F.Y. Risk factors in cutout of sliding hip screw in intertrochanteric fractures: an evaluation of 937 patients. Int Orthop. 2010;34:1273–1276. doi: 10.1007/s00264-009-0866-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gavaskar A., Subramanian M., Tummala N. Results of proximal femoral nail antirotation for low velocity trochanteric fractures in the elderly. Indian J Orthop. 2012;46(5):556–560. doi: 10.4103/0019-5413.101036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verheyden A., Josten C. Intramedullary fixation of intertrochanteric fractures with the proximal femoral nail. Operat Orthop Traumatol. 2003;15:20–37. [Google Scholar]
- 25.Lobo-Escolar A., Joven E., Iglesias D., Herrera A. Predictive factors for cutting-out in femoral intramedullary nailing. Injury. 2010 Dec 1;41(12):1312–1316. doi: 10.1016/j.injury.2010.08.009. [DOI] [PubMed] [Google Scholar]
- 26.Pramudito J., Soegijoko S., Mengko TR, Muchtadi FI, Wachjudi RG. Trabecular pattern analysis of proximal femur radiographs for osteoporosis detection. J Biomed Pharm Eng. 2007;1(1):45–51. [Google Scholar]
- 27.Strauss E.J., Kummer F.J., Koval K.J., Egol A.J. The “Z-effect” phenomenon defined: a laboratory study. J Orthop Res. 2007;25:1568–1573. doi: 10.1002/jor.20457. [DOI] [PubMed] [Google Scholar]
- 28.Cheema G., Rastogi A., Singh V., Goel S. Comparison of cut out resistance of dynamic condylar screw and proximal femoral nail in reverse oblique trochanteric fractures: a biomechanical study. Indian J Orthop. 2012;46(3):259–265. doi: 10.4103/0019-5413.96369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Henschel J., Eberle S., Augat P. Load distribution between cephalic screws in a dual lag screw trochanteric nail. J Orthop Surg Res. 2016 Apr 1;11:41. doi: 10.1186/s13018-016-0377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]