Abstract
A technique for lateral extra-articular tenodesis using proximal staple fixation is described as an adjunct to anterior cruciate ligament (ACL) reconstruction. Lateral extra-articular tenodesis has been used in an effort to decrease failure rates in ACL-deficient patients with ligamentous laxity, prior failed ACL surgery, or grade 3 pivot-shift findings. Numerous surgeons have described combining ACL reconstruction with extra-articular surgery. The approach described in this article is easy and cost-effective. Moreover, because this technique uses a staple instead of a SwiveLock (Arthrex, Naples, FL) or other suture anchor, it limits the chance of conflicting with the tunnels for the ACL because there is no need to drill or punch additional tunnels.
For many years, anterior cruciate ligament (ACL) injury has been the primary focus when considering impaired knee stability.1 However, numerous articles have reported an anterolateral capsular injury (Segond fracture) associated with ACL tears.2, 3, 4, 5, 6 Despite this well-known association, little has been published on the anatomy of this region, and the importance of the anterolateral structures to rotational stability has been downplayed. Historically, some authors believed that anterolateral rotational instability caused by an ACL tear could be treated by extra-articular surgery rather than ACL reconstruction. Numerous techniques were developed that focused exclusively on extra-articular reconstruction to control the instability.7, 8, 9, 10, 11, 12
The current standard of care is to reconstruct the ACL with autograft tissue and disregard any anterolateral injuries. However, the recent “rediscovery” and description of the anterolateral ligament (ALL) by Claes et al.13 in 2013 brought new attention to treatment of the anterolateral corner of the knee.7 In an effort to decrease failure rates in patients with ligamentous laxity, prior failed ACL surgery, or grade 3 pivot-shift findings, numerous surgeons have described combining ACL reconstruction with extra-articular surgery. They have reported improved knee stability and patient-reported outcomes (PROs).14, 15, 16, 17, 18, 19, 20, 21, 22 The anterolateral knee structures are composed of the ALL and iliotibial band (ITB), especially its deep fibers, also known as the Kaplan fibers.23 It has also been reported that the ITB is injured in 93% of cases of ACL-deficient knees.6 In addition, it is possible that the ITB plays a greater role in restraining instability than the ALL.24
The most well-known technique for anterolateral tenodesis was first described by Lemaire.11 This technique has been shown to be successful by many surgeons, who have also slightly modified the original technique.11, 13, 14, 21, 22, 24, 25, 26, 27, 28, 29 Because the importance of anterolateral tissue reconstruction is now more established, we believe that the proper surgical technique should be used to address anterolateral knee surgery. The objective of this article is to describe our technique for lateral extra-articular tenodesis (LET) with proximal staple fixation that is efficient, is cost-effective, and may be less risky for the bone. Moreover, because this technique uses a staple instead of a SwiveLock (Arthrex, Naples, FL) or other suture anchor, it limits the chance of conflicting with the tunnels for the ACL because there is no need to drill or punch additional tunnels. This approach is better able to control the pivot shift because the vector of pull is more horizontal than the ALL. This technique is presented as a supportive surgical procedure with ACL reconstruction as the primary treatment.
Technique
Preoperative Workup
Patients who present with suspected ACL injury to our institution undergo a standard history and physical examination, as well as preoperative magnetic resonance imaging. The physical examination is focused on assessment of anterolateral knee instability based on the Lachman and pivot-shift tests. When gross instability is observed, with at least grade 2 Lachman and pivot-shift findings and with no medial meniscal lesion on magnetic resonance imaging, LET after ACL reconstruction is considered. We also observe for the presence of recurvatum and generalized ligamentous laxity, which may serve as indications for LET as well.
Step 1
The patient is placed in the supine position on the surgical table. After anesthesia induction, the knee is prepared and draped in a sterile fashion. The tourniquet on the thigh is inflated to 200 to 300 mm Hg. First, intra-articular ACL reconstruction is performed. The knee is then positioned in 30° of flexion. We apply a lateral side bolster and a sandbag under the patient's foot to maintain the knee position (Video 1).
Step 2
A slightly curved 10-cm-long incision is performed along the lateral side of the knee. It is placed over the ITB, starting proximally from the Gerdy tubercle (Fig 1). Dissection down to the ITB is performed, and Gelpi retractors are placed (Fig 2). Next, a Cobb retractor is used to separate the soft tissue from the ITB (Fig 3).
Fig 1.
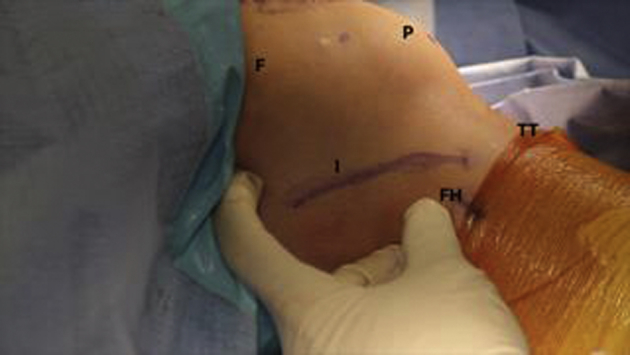
Lateral view of the right knee. The skin incision is marked along the iliotibial band. (F, femur; FH, fibular head; I, marked incision; P, patella; TT, tibial tubercle.)
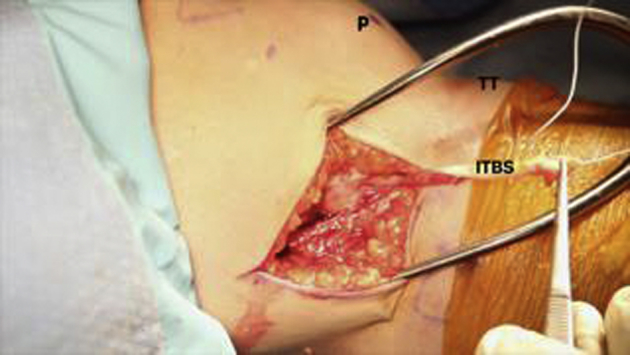
Fig 2.
Lateral view of the right knee after the iliotibial band strip (ITBS) has been harvested. (P, patella; TT, tibial tubercle.)
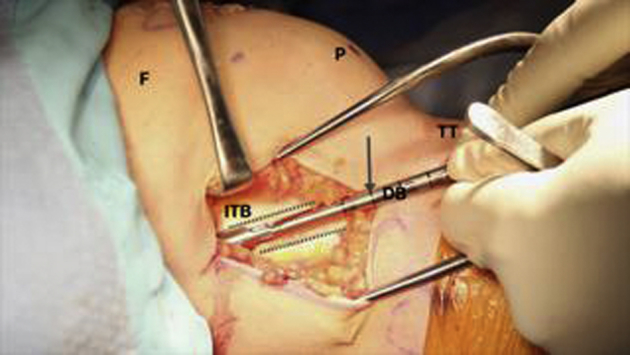
Fig 3.
Lateral view of the right knee after the incision has been made and the iliotibial band (ITB) has been dissected. The arrow is pointing in the direction in which the double blade (DB) will be used. (F, femur; FH, femoral head; P, patella; TT, tibial tubercle.)
Step 3
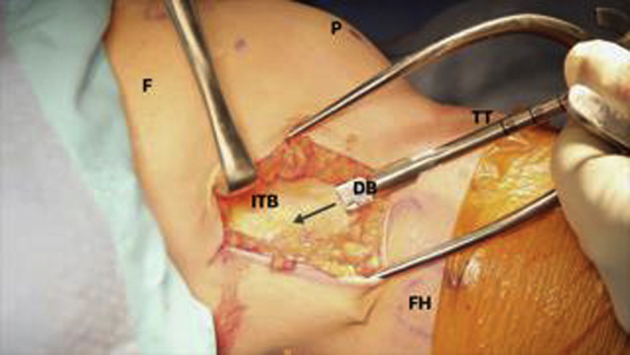
Once the ITB is well visualized, a parallel blade knife is used to score a 1-cm-wide midsubstance ITB tissue strip (Fig 4). The aim is to obtain a strip of ITB tissue about 8 cm long. Metzenbaum scissors are used to complete the dissection and release the proximal end of the tissue strip. It is crucial to leave the distal attachment to the Gerdy tubercle intact.
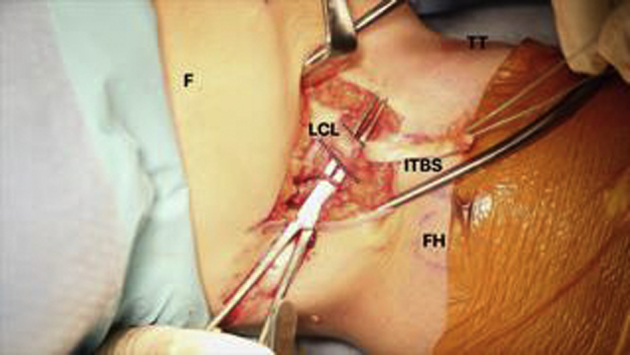
Fig 4.
Lateral view of the right knee after the lateral collateral ligament (LCL, dotted lines) has been isolated, and a tunnel beneath is prepared to pass the iliotibial band strip (ITBS). (F, femur; FH, femoral head; TT, tibial tubercle.)
Step 4
Next, No. 2 FiberWire (Arthrex) is used to whipstitch the proximal end of the previously harvested ITB strip. We aim to secure about 2 cm of this end.
Step 5
After identification of the lateral collateral ligament (LCL) position, a No. 15 blade scalpel is used to delineate its borders (Fig 5). It is advised to increase knee flexion and keep the knee in a slightly varus position to achieve proper LCL identification. It is also crucial not to violate the joint capsule during LCL dissection. Afterward, a Kelly hemostat is passed underneath the LCL, creating space under the LCL for the ITB tissue strip. It is passed from proximal to distal (Fig 6).
Fig 5.
Lateral view of the right knee after the iliotibial band (ITB) has been harvested. The arrow is pointing to the laser mark indicating the correct length of the tissue strip (dotted lines). (DB, double blade; F, femur; P, patella; TT, tibial tubercle.)
Fig 6.
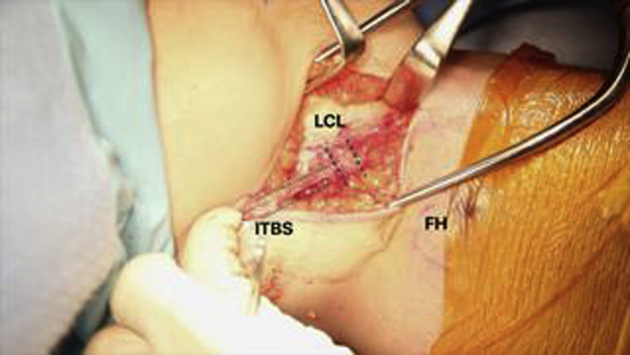
Lateral view of the right knee after the iliotibial band strip (ITBS) has been passed under the lateral collateral ligament (LCL, dotted lines). (FH, femoral head.)
Step 6
The Kelly hemostat is used to grasp and pull the No. 2 FiberWire suture ends from distal to proximal, underneath the LCL. Next, the whole ITB tissue strip is passed under the preserved LCL.
Step 7
The knee is once again positioned in about 30° of flexion. The underside of the ITB is palpated and bluntly dissected so that the proper place for the ITB strip can be identified. The landmark is 2 cm proximal and slightly posterior to the native LCL femoral insertion.
Step 8
Once the proper place is identified, the ITB strip is secured in the aforementioned place using a small surgical staple (Richards staple; Smith & Nephew, Memphis, TN) (Fig 7). Next, the free end of the ITB strip is doubled over, and the remaining free ends of the No. 2 FiberWire are looped around the LCL and tied securely.
Fig 7.
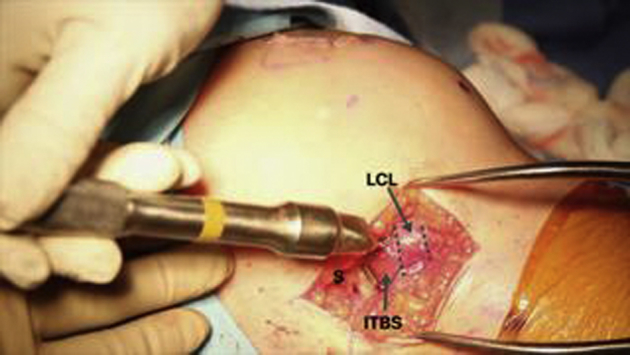
Lateral view of the right knee after the iliotibial band strip (ITBS) has been fixed with a staple (S). The dotted lines indicate the lateral collateral ligament (LCL).
Step 9
On conclusion of the procedure, full range of motion of the knee is ensured and the Lachman and pivot-shift tests are performed to ensure its stability. The wounds are irrigated, and tourniquet pressure is released. Absorbable No. 2-0 Vicryl suture (Ethicon, Somerville, NJ) is then used to close the subcutaneous layer, and No. 3-0 Vicryl is used to close the skin layer.
Postoperative Rehabilitation
After the procedure, early active range of motion and weight bearing as tolerated are suggested. We encourage the use of crutches for the first 10 to 14 days until adequate balance is maintained. A standardized postoperative ACL protocol is provided, and a full return to sports activity is considered no sooner than 6 months after surgery.
Discussion
The anterolateral knee soft tissues are composed of the anterolateral capsular ligament (i.e. the ALL) and ITB, with its deep Kaplan fibers spreading to the lateral meniscal insertion, distal femur, and joint capsule.23 Engebretsen et al.30 reported that adding LET to ACL reconstruction decreases the total forces experienced by the ACL graft by about 43%. Slette et al.7 reported in a systematic review that 7 of 8 studies showed a significant reduction in internal rotatory movement once the LET was applied. Furthermore, the modified Lemaire tenodesis, which is similar to our technique, was tested in cadavers by Inderhaug et al.,26, 27 who concluded that this surgical procedure combined with ACL reconstruction restores normal knee kinematics regardless of knee position during graft fixation.13 In our technique, the ITB strip is fixed in 30° of flexion, which corresponds to the original Lemaire description.11 A study by Song et al.31 included 7 articles for further analysis and found that the LET procedure significantly decreased postoperative pivot shift when combined with ACL reconstruction. Consistent with the findings of Rezende et al.,19 no difference in PRO measures was reported.31
In conclusion, ACL reconstruction alone may not reconstitute native knee biomechanics, and other techniques to augment this procedure may be necessary to protect the knee. Some clinical studies have supported the idea of adding LET to support ACL graft incorporation, limit postoperative instability, and improve PRO measures without an increase in the complication rate. We are aware that the described technique requires an additional skin incision and additional hardware implantation. Nevertheless, we believe it is relatively easier and less expensive than previously reported techniques. To highlight the usability of our technique, possible risks and advantages are summarized in Table 1. Some key points from our experience using this technique are highlighted in Table 2. We believe our technique will benefit patients based on those who fit the described criteria because it is quick and reproducible; however, we are aware that further clinical study might be helpful to fully evaluate this technique.
Table 1.
Advantages and Disadvantages of LET With Staple Fixation Technique
| Advantages |
| Gives additional stabilization to ACL repair or reconstruction |
| Does not require expensive implants and instruments |
| Gives an option to perform looping over the LCL, therefore combining LET techniques |
| Avoids drill-hole convergence with ACL tunnels vs using a suture anchor |
| Risks and disadvantages |
| Requires an additional skin incision during the ACL repair or reconstruction procedure |
| Risks peroneal nerve injury if dissection is carried too far inferiorly |
| Risks LCL injury if proper identification and dissection are not performed |
| Requires the proper type and size of staple |
ACL, anterior cruciate ligament; LCL, lateral collateral ligament; LET, lateral extra-articular tenodesis.
Table 2.
Key Steps, Pearls, and Pitfalls of LET With Staple Fixation Technique
| Key Steps | Pearls and Pitfalls |
|---|---|
| Limb positioning | The patient is supine. The knee position must allow for full ROM intraoperatively. We place a sandbag under the hip and a bolster to allow easy access to the lateral side of the knee. |
| ITB identification | It is crucial to properly expose the ITB before attempting to harvest the strip. The surgeon should be cautious when inferior to the ITB to avoid injury to the peroneal nerve. |
| ITB harvesting | It is crucial to harvest at least an 8-cm tissue strip. The strip is left intact distally. |
| LCL identification | It is crucial not to harm the LCL tendon. The surgeon should dissect slowly and palpate for a cord-like structure running perpendicular to the ITB. The surgeon should use as much blunt dissection as possible. |
| Staple fixation | The Richards staple should have barbs (not smooth) to achieve proper fixation of the tissue strip and resist pulling forces during postoperative loading. |
| ITB strip looping | It is crucial to make a loop over the staple and incorporate it with the rest of the ITB strip. This will prevent the LET from loosening over time. |
ITB, iliotibial band; LCL, lateral collateral ligament; LET, lateral extra-articular tenodesis; ROM, range of motion.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.M. receives institutional support for education from ConMed, Össur, and Arthrex. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Lateral extra-articular tenodesis with proximal staple fixation. The patient is in the supine position with his right knee flexed to 30° and stabilized with a sandbag and lateral bolster. The steps of the technique are as follows: (1) skin incision and iliotibial band (ITB) dissection, (2) harvesting of the ITB strip, (3) lateral collateral ligament identification and dissection, (4) passage of the ITB strip under the lateral collateral ligament, (5) ITB strip fixation with a staple, (6) ITB strip looping and tying, and (7) final knee stability assessment.
References
- 1.Galway H.R., MacIntosh D.L. The lateral pivot shift: A symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980;147:45–50. [PubMed] [Google Scholar]
- 2.Segond P. Aux Bureaux du Progrès Médical; Paris: 1879. Recherces cliniques et expérimentales sur les épanchements sanguins du genou par entorse. [in French] [Google Scholar]
- 3.Buscayret C., Buscayret F., Farenq C. Intra- and extra-articular hamstring reconstruction of anterior cruciate ligament tears. Rev Chir Orthop Reparatrice Appar Mot. 2001;87:276–280. [in French] [PubMed] [Google Scholar]
- 4.Kennedy J., Jackson M.P., O’Kelly P., Moran R. Timing of reconstruction of the anterior cruciate ligament in athletes and the incidence of secondary pathology within the knee. J Bone Joint Surg Br. 2010;92:362–366. doi: 10.1302/0301-620X.92B3.22424. [DOI] [PubMed] [Google Scholar]
- 5.Wroble R.R., Grood E.S., Cummings J.S., Henderson J.M., Noyes F.R. The role of the lateral extraarticular restraints in the anterior cruciate ligament-deficient knee. Am J Sports Med. 1993;21:257–262. doi: 10.1177/036354659302100216. discussion 263. [DOI] [PubMed] [Google Scholar]
- 6.Terry G.C., Norwood L.A., Hughston J.C., Caldwell K.M. How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med. 1993;21:55–60. doi: 10.1177/036354659302100110. [DOI] [PubMed] [Google Scholar]
- 7.Slette E.L., Mikula J.D., Schon J.M. Biomechanical results of lateral extra-articular tenodesis procedures of the knee: A systematic review. Arthroscopy. 2016;32:2592–2611. doi: 10.1016/j.arthro.2016.04.028. [DOI] [PubMed] [Google Scholar]
- 8.Andrews J.R., Sanders R. A “mini-reconstruction” technique in treating anterolateral rotatory instability (ALRI) Clin Orthop Relat Res. 1983;172:93–96. [PubMed] [Google Scholar]
- 9.Ellison A.E. Distal iliotibial-band transfer for anterolateral rotatory instability of the knee. J Bone Joint Surg Am. 1979;61:330–337. [PubMed] [Google Scholar]
- 10.Ireland J., Trickey E.L. Macintosh tenodesis for anterolateral instability of the knee. J Bone Joint Surg Br. 1980;62:340–345. doi: 10.1302/0301-620X.62B3.7410466. [DOI] [PubMed] [Google Scholar]
- 11.Lemaire M. Ruptures anciennes du ligament croise anterieur du genou. J Chir. 1967;93:311–320. [in French] [Google Scholar]
- 12.Losee R.E., Johnson T.R., Southwick W.O. Anterior subluxation of the lateral tibial plateau. A diagnostic test and operative repair. J Bone Joint Surg Am. 1978;60:1015–1030. [PubMed] [Google Scholar]
- 13.Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weber A.E., Zuke W., Mayer E.N. Lateral augmentation procedures in anterior cruciate ligament reconstruction: Anatomic, biomechanical, imaging, and clinical evidence. Am J Sports Med. 2019;47:740–752. doi: 10.1177/0363546517751140. [DOI] [PubMed] [Google Scholar]
- 15.Hewison C.E., Tran M.N., Kaniki N., Remtulla A., Bryant D., Getgood A.M. Lateral extra-articular tenodesis reduces rotational laxity when combined with anterior cruciate ligament reconstruction: A systematic review of the literature. Arthroscopy. 2015;31:2022–2034. doi: 10.1016/j.arthro.2015.04.089. [DOI] [PubMed] [Google Scholar]
- 16.Neyret P., Palomo J.R., Donell S.T., Dejour H. Extra-articular tenodesis for anterior cruciate ligament rupture in amateur skiers. Br J Sports Med. 1994;28:31–34. doi: 10.1136/bjsm.28.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marcacci M., Zaffagnini S., Iacono F. Intra- and extra-articular anterior cruciate ligament reconstruction utilizing autogeneous semitendinosus and gracilis tendons: 5-Year clinical results. Knee Surg Sports Traumatol Arthrosc. 2003;11:2–8. doi: 10.1007/s00167-002-0323-x. [DOI] [PubMed] [Google Scholar]
- 18.Noyes F.R., Barber S.D. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1991;73:882–892. [PubMed] [Google Scholar]
- 19.Rezende F.C., de Moraes V.Y., Martimbianco A.L.C., Luzo M.V., da Silveira Franciozi C.E., Belloti J.C. Does combined intra- and extraarticular ACL reconstruction improve function and stability? A meta-analysis. Clin Orthop Relat Res. 2015;473:2609–2618. doi: 10.1007/s11999-015-4285-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vadalà A.P., Iorio R., De Carli A. An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int Orthop. 2013;37:187–192. doi: 10.1007/s00264-012-1571-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ferretti A., Monaco E., Fabbri M., Maestri B., De Carli A. Prevalence and classification of injuries of anterolateral complex in acute anterior cruciate ligament tears. Arthroscopy. 2017;33:147–154. doi: 10.1016/j.arthro.2016.05.010. [DOI] [PubMed] [Google Scholar]
- 22.Ferretti A., Monaco E., Ponzo A. Combined intra-articular and extra-articular reconstruction in anterior cruciate ligament-deficient knee: 25 Years later. Arthroscopy. 2016;32:2039–2047. doi: 10.1016/j.arthro.2016.02.006. [DOI] [PubMed] [Google Scholar]
- 23.Mathew M., Dhollander A., Getgood A. Anterolateral ligament reconstruction or extra-articular tenodesis: Why and when? Clin Sports Med. 2018;37:75–86. doi: 10.1016/j.csm.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 24.Kittl C., El-Daou H., Athwal K.K. The role of the anterolateral structures and the ACL in controlling laxity of the intact and ACL-deficient knee. Am J Sports Med. 2016;44:345–354. doi: 10.1177/0363546515614312. [DOI] [PubMed] [Google Scholar]
- 25.Geeslin A.G., Moatshe G., Chahla J. Anterolateral knee extra-articular stabilizers: A robotic study comparing anterolateral ligament reconstruction and modified Lemaire lateral extra-articular tenodesis. Am J Sports Med. 2018;46:607–616. doi: 10.1177/0363546517745268. [DOI] [PubMed] [Google Scholar]
- 26.Inderhaug E., Stephen J.M., El-Daou H., Williams A., Amis A.A. The effects of anterolateral tenodesis on tibiofemoral contact pressures and kinematics. Am J Sports Med. 2017;45:3081–3088. doi: 10.1177/0363546517717260. [DOI] [PubMed] [Google Scholar]
- 27.Inderhaug E., Stephen J.M., Williams A., Amis A.A. Biomechanical comparison of anterolateral procedures combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2017;45:347–354. doi: 10.1177/0363546516681555. [DOI] [PubMed] [Google Scholar]
- 28.Nitri M., Rasmussen M.T., Williams B.T. An in vitro robotic assessment of the anterolateral ligament, part 2: Anterolateral ligament reconstruction combined with anterior cruciate ligament reconstruction. Am J Sports Med. 2016;44:593–601. doi: 10.1177/0363546515620183. [DOI] [PubMed] [Google Scholar]
- 29.Spencer L., Burkhart T.A., Tran M.N. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am J Sports Med. 2015;43:2189–2197. doi: 10.1177/0363546515589166. [DOI] [PubMed] [Google Scholar]
- 30.Engebretsen L., Lew W.D., Lewis J.L., Hunter R.E., Benum P. Anterolateral rotatory instability of the knee. Cadaver study of extraarticular patellar-tendon transposition. Acta Orthop Scand. 1990;61:225–230. doi: 10.3109/17453679008993505. [DOI] [PubMed] [Google Scholar]
- 31.Song G.-Y., Hong L., Zhang H., Zhang J., Li Y., Feng H. Clinical outcomes of combined lateral extra-articular tenodesis and intra-articular anterior cruciate ligament reconstruction in addressing high-grade pivot-shift phenomenon. Arthroscopy. 2016;32:898–905. doi: 10.1016/j.arthro.2015.08.038. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Lateral extra-articular tenodesis with proximal staple fixation. The patient is in the supine position with his right knee flexed to 30° and stabilized with a sandbag and lateral bolster. The steps of the technique are as follows: (1) skin incision and iliotibial band (ITB) dissection, (2) harvesting of the ITB strip, (3) lateral collateral ligament identification and dissection, (4) passage of the ITB strip under the lateral collateral ligament, (5) ITB strip fixation with a staple, (6) ITB strip looping and tying, and (7) final knee stability assessment.


