Abstract
Hip arthroscopy is an innovative surgical tool that is minimally invasive; however, the working space is very limited because of small surgical wounds. Recent literature has shown that capsular repair after capsulotomy during hip arthroscopy facilitates the restoration of hip joint stability. Previous Technical Notes have introduced the shoelace capsule closing technique using a single Ultratape. However, even with the shoelace capsule closing technique, we periodically have encountered difficult cases with extensive capsular laxity. In this Technical Note, we introduce an improved hip capsule plication technique using 2 pieces of Ultratape for treating borderline hip dysplasia with capsular laxity. This double shoelace capsule plication technique theoretically reduces tearing risks during closure of delicate and fragile capsules. Level of evidence: 1 (hip); 2 (other).
Recently, hip arthroscopy has provided a major innovation in the orthopaedic field, and the number of hip arthroscopy cases has been increasing.1 During hip arthroscopy, an interportal capsular cut, or capsulotomy, helps provide better visualization and accessibility. In closing of hip arthroscopic surgery, restoring the capsule helps stabilize the hip joint. Capsular plication is recommended when treating patients with hip instability,2 and complete capsular closure with strong sutures can provide better clinical outcomes and lower revision rates compared with partial capsular closure in the treatment of femoroacetabular impingement.3, 4 In addition, Menge et al.5 reported that the Quebec City slider could be stronger for capsular closure than other plication procedures using strong sutures.
A recent surgical technique of capsular plication using suture body tape (Ultratape; Smith & Nephew, Andover, MA), called the shoelace technique, has been introduced in hip arthroscopy.6 However, in spite of this shoelace technique, we periodically encounter difficult cases with borderline hip dysplasia (BDDH) concomitant with severe capsular laxity. The purpose of this Technical Note is to describe a surgical technique, the double shoelace capsular closure technique, for the treatment of borderline hip dysplasia associated with capsular laxity (Video).
Surgical Technique
Indication for Double Shoelace Capsular Plication
Indications for double shoelace capsular plication include BDDH associated with capsular laxity, extensive capsular defect, and BDDH associated with osteoarthritis. However, if capsular defects are located at the acetabular attachment site or there is an extensive capsular defect, capsular reconstruction using iliotibial bands should be considered.
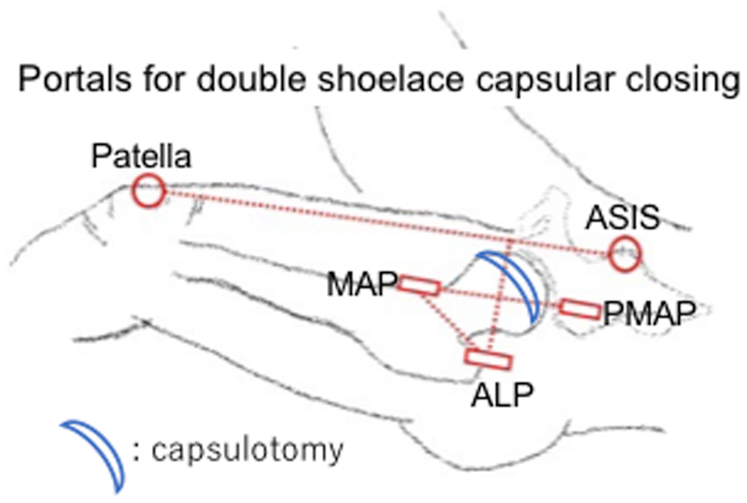
The patient is placed on a traction table in well-padded boots and a well-padded perineal post adjacent to the involved medial thigh, under general anesthesia. An antero-lateral portal (ALP) and a mid-anterior portal (MAP) are established, as seen in Figure 1. Interportal capsulotomy is performed using a beaver blade and radiofrequency probe, cutting the capsule parallel to the lateral margin of the acetabular labrum from the 10 o’clock to the 2 o’clock position. Diagnostic arthroscopy is then performed to evaluate intra-articular pathologies. Intra-articular procedures comprising labral repair and cam osteoplasty are performed if necessary based on physical examination and preoperative images (Fig 2), as seen in Fig 3.
Fig 1.
Portal placements for double shoelace hip capsular closing technique for a left hip. First, an anterior-lateral portal (ALP) on the top of the great trochanter is prepared, and a line between the anterior superior iliac spine (ASIS) and the patella is drawn. A half line between the ALP and the patella-ASIS line is drawn, and on the half line, a mid-anterior portal (MAP) is prepared in reference to the distance between the MAP and the ALP (∼7 cm). A proximal midanterior portal (PMAP) is also positioned symmetrically to the MAP using a scope viewing from the ALP.
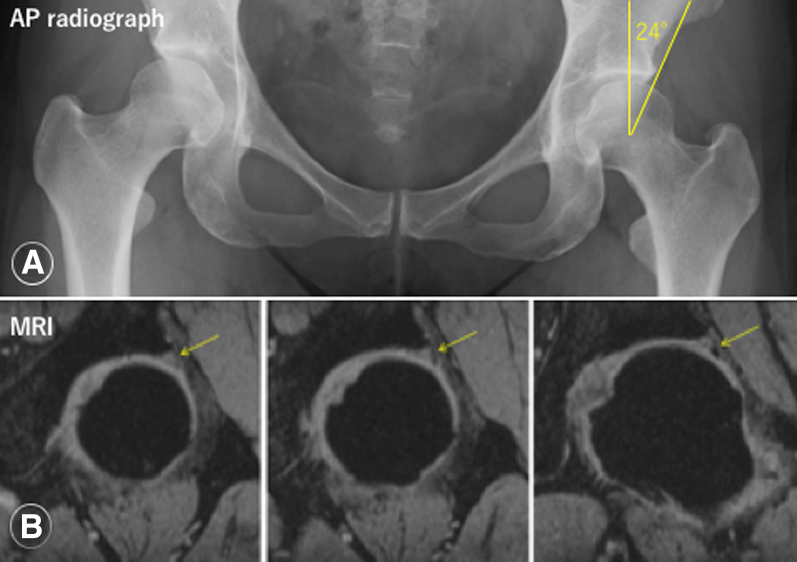
Fig 2.
Pelvic anteroposterior radiograph and magnetic resonance imaging (MRI) images of an acetabular labral tear in a left hip. (A) A pelvic anteroposterior (AP) radiograph showing a 24° lateral center-edge with normal Shenton line. (B) T2-star fat-saturation coronal images of 3-Tesla MRI showing high signal intensity of the anterior superior acetabular labrum, suggesting an acetabular labral tear (yellow arrows).
Fig 3.
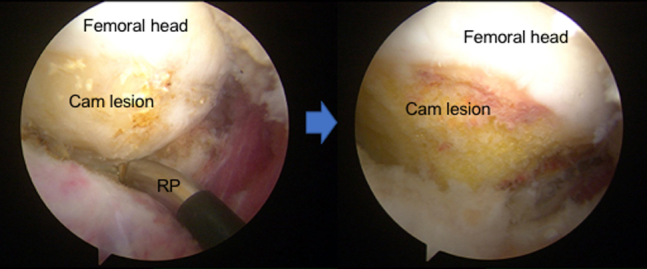
Arthroscopic cam osteoplasty with enlarged capsulotomy for a left hip. An enlarged capsulotomy is performed for borderline hip dysplasia with capsular laxity after cam osteoplasty as viewed from the anterior-lateral portal. (RP, radiofrequency probe.)
After releasing traction and positioning the left hip flexed to 30°, a proximal midanterior portal (PMAP) is established, as shown in Figure 1. Clear Trac Cannulas (Smith & Nephew) are set in the MAP and PMAP. A suture passer (Acupass; Smith & Nephew) is introduced through the PMAP and passes a suture loop through the capsule at the proximal side of the capsulotomy from superficial to deep into the capsule. A 35° Arthro-pierce penetrator (Smith & Nephew) penetrates the capsule on the distal side of the capsulotomy near the zona orbicularis through the MAP and retrieves the lasso. An Ultratape is passed through the suture lasso as seen in Figure 4 and is retrieved with the suture loop passing through the capsule from the MAP to the PMAP. Next, the suture passer passes a suture loop through the proximal end of the capsule 5 mm posteriorly from the first suture limb at the proximal side of the capsulotomy. A grasper pulls out the suture lasso, retrieving it outside of the MAP. There, the distal limb of the Ultratape is passed through the suture lasso. The suture lasso, accompanied by the Ultratape, is retrieved and passes through the proximal side of the capsule. Similarly, a suture passer passes through the distal side of the capsule 5 mm posteriorly from the distal limb of the Ultratape. A suture lasso is retrieved outside of the cannula and the PMAP, and the first proximal limb of the Ultratape is set into the loop of the suture lasso. Next, the suture lasso is retrieved with the Ultratape and passes through the distal side of the capsule, completing the single shoelace, as seen in Figure 5.
Fig 4.
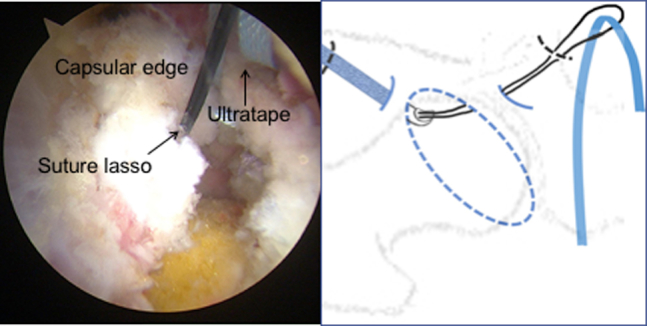
Ultratape passing through the hip capsule using a suture lasso loop for a left hip. Ultratape is passed through the suture lasso and retrieved with a suture loop passing through the capsule from the proximal midanterior portal to the midanterior portal as viewed from the anterior-lateral portal.
Fig 5.
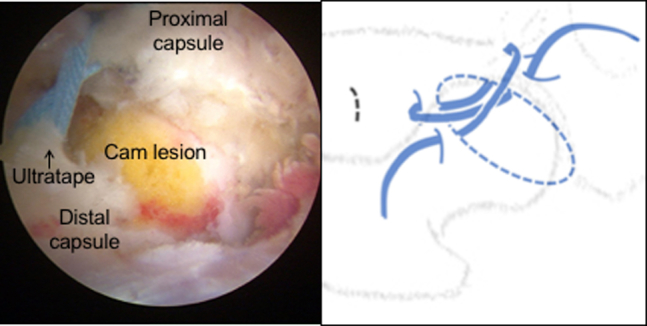
Arthroscopic anterior shoelace with Ultratape (anterior shoelace capsular suture) for a left hip. Anterior shoelace capsule closure is performed from the anteromedial side of the capsulotomy as viewed from the anterior-lateral portal.
This procedure is repeated 4 times, and both limbs of the Ultratape are retrieved from the PMAP through the cannula. Then, using scope viewing from the MAP to look at the posterolateral portion of the capsulotomy, another shoelace capsule closure is set up, starting from the posterior side of the capsulotomy, using another piece of Ultratape (caution: at the opposite side of the first shoelace capsule closure). At least 3 pairs of shoe-lacing should be performed, and sequential pairs should overlap. Both Ultratape limbs are pulled out through the PMAP. In total, 7 pairs of shoe-lacing are prepared on the capsulotomy, as illustrated in Figure 6. Finally, the Ultratape limbs are alternately pulled and tightened, confirming adequate tension in the capsule. All Ultratape is then tied to secure the construction, as viewed in Figure 7.
Fig 6.
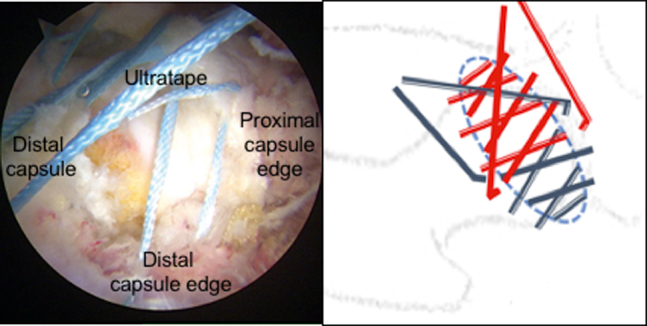
Arthroscopic double shoelace capsular plication technique for repairing hip capsulotomy in borderline hip dysplasia with capsular laxity in a left hip. With the double shoelace capsule closing technique, 7 pairs of shoelacing are prepared using 2 pieces of Ultratape on the enlarged capsulotomy as viewed from the anterior-lateral portal.
Fig 7.
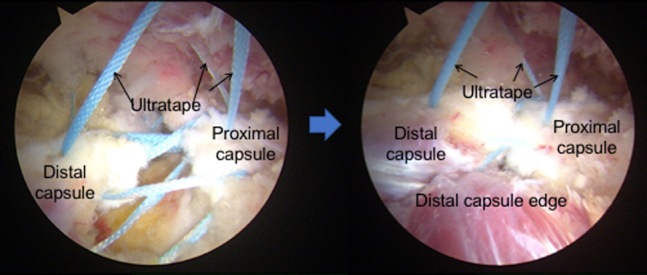
Hip capsulotomy closure using the double shoelace technique for a left hip. Two pieces of Ultratape are alternately pulled and tightened, confirming adequate tension in the capsule. They are then tied to secure closure of the enlarged capsulotomy as viewed from the anterior-lateral portal.
Postoperative Recovery
The patient is instructed to remain non-weightbearing for the first 3 weeks. During this time, the patient is provided with a hip brace to limit hip range of motion. Passive range-of-motion exercises are initiated during the first week by physical therapists. Stationary bike exercise is initiated without restriction a few days after surgery. Circumduction exercises are performed for the first 2 weeks to avoid adhesive capsulitis. The patient is allowed to participate in normal daily activities over the 2-month postoperative period.
Discussion
This is a Technical Note presenting the arthroscopic double shoelace capsule closing technique for the treatment of BDDH with capsular laxity undergoing labral repair and cam osteoplasty. The shoelace capsule plication technique theoretically reduces tearing risks during closure of delicate and fragile capsules, especially in patients with BDDH. In hip surgery, the importance of capsular reconstruction has been advocated, and a biomechanical study showed that hip capsular closure or plication restored hip joint stability,7 potentially decreasing postoperative complaints.8 In hip arthroscopy, previous Technical Notes have introduced the shoelace capsule closing technique using Ultratape.6 However, even with the shoelace capsule closing technique, we periodically have encountered difficult cases with extensive capsular laxity. The limitation of the single shoelace capsule closing technique is that it is applicable for relatively smaller capsulotomy because it uses a single Ultratape. It is difficult to adequately control capsular tension with extensive capsular laxity using a single Ultratape. Moreover, a single shoelace anterior capsular closure does not provide enough strength to restore joint stability in cases of extensive capsulotomy. The advantage of the double shoelace capsule closing technique is that 2 pieces of Ultratape adequately cover an enlarged capsulotomy. Two pieces of Ultratape also enable surgeons to gradually tighten and close the capsule with adequate tension, even with enlarged capsular laxity. The double shoelace capsule closing technique, however, is technically demanding and requires training.
The indications of the double shoelace capsular plication technique are hip capsulotomy during hip arthroscopic surgery for treating BDDH patients with capsular laxity. In contrast, the contraindications of this procedure are infection, adhesive capsulitis, and hip joint contracture, as shown in Table 1. The advantages of this technique arise from the shape of the Ultratape. A recent biomechanical study showed that suture tape allows a larger tissue contact area. It theoretically enables force to be spread across a broader tissue area, improving tissue security while reducing the risk of the suture pulling out.9
Table 1.
Indications and Contraindications for the Double Shoelace Hip Capsule Plication Technique
| Indication | Contraindication |
|---|---|
| Developmental dysplasia of the hip with capsule laxity (Beighton score >6) | Infection |
| Adhesive capsulitis | |
| Enlarged hip capsulotomy | Extensive capsular defect |
A disadvantage of this technique is that it is technically demanding and meticulous, resulting in a potentially prolonged operation time. The potential complications would be stiffness and pain of the anterior hip, although we have never encountered such cases. The advantages and disadvantages are summarized in Table 2.
Table 2.
Advantages and Disadvantages of the Double Shoelace Hip Capsule Plication Technique
| Advantage | Disadvantage |
|---|---|
| Less risk of suture pulling out | Technically demanding |
| Closing enlarged capsulotomy | Prolonged operation time |
| Restoring hip joint stability | Use of 2 pieces of Ultratape |
This Technical Note should be helpful for alleviating the technical demands of performing this procedure. In conclusion, the arthroscopic double shoelace hip capsule plication technique provides favorable clinical outcomes for the treatment of patients with extensive capsular laxity.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: S.U. is a consultant for Smith & Nephew and ConMed; has received research support from Smith and Nephew, Pfizer, Zimmer; and is a board member of ISHA. M.J.P. reports grants and personal fees from Smith and Nephew, Arthrex; personal fees from Arthrosurface, MJP Innovations, MIS, Bledsoe, ConMed Linvatec, DonJoy, Elsevier, Proofpoint Biologics, The Steadman Clinic DM Company, SLACK Inc; grants from Össur, Siemens, NIH, NIA; other from Steadman Philippon Research Institute, International Society of Hip Arthroscopy, AISAM. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
This video presents an arthroscopic double shoelace capsular plication technique for a left hip with borderline hip dysplasia associated with capsular laxity on a traction table. After the diagnostic arthroscopy is completed, a labral repair and cam osteoplasty are performed. An Ultratape is passed through the hip capsule using a suture lasso loop, and a single shoelace capsular closure is prepared from the anteromedial side of the capsulotomy; another shoelace capsular closure is prepared from the posterolateral side. Finally, 2 pieces of Ultratape are alternately pulled and tightened to secure a double shoelace capsular plication of the enlarged capsulotomy.
References
- 1.Sing D.C., Feeley B.T., Tay B., Vail T.P., Zhang A.L. Age-related trends in hip arthroscopy: A large cross-sectional analysis. Arthroscopy. 2015;31:2307–2313. doi: 10.1016/j.arthro.2015.06.008. [DOI] [PubMed] [Google Scholar]
- 2.Domb B.G., Stake C.E., Lindner D., El-Bitar Y., Jackson T.J. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: Two-year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med. 2013;41:2591–2598. doi: 10.1177/0363546513499154. [DOI] [PubMed] [Google Scholar]
- 3.Frank R.M., Lee S., Bush-Joseph C.A., Kelly B.T., Salata M.J., Nho S.J. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: A comparative matched-pair analysis. Am J Sports Med. 2014;42:2634–2642. doi: 10.1177/0363546514548017. [DOI] [PubMed] [Google Scholar]
- 4.Wylie J.D., Beckmann J.T., Maak T.G., Aoki S.K. Arthroscopic capsular repair for symptomatic hip instability after previous hip arthroscopic surgery. Am J Sports Med. 2016;44:39–45. doi: 10.1177/0363546515608162. [DOI] [PubMed] [Google Scholar]
- 5.Menge T.J., Chahla J., Soares E., Mitchell J.J., Philippon M.J. The Quebec City slider: A technique for capsular closure and plication in hip arthroscopy. Arthrosc Tech. 2016;5:e971–e974. doi: 10.1016/j.eats.2016.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Uchida S., Pascual-Garrido C., Ohnishi Y. Arthroscopic shoelace capsular closure technique in the hip using Ultratape. Arthrosc Tech. 2017;6:e157–e161. doi: 10.1016/j.eats.2016.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philippon M.J., Trindade C.A.C., Goldsmith M.T. Biomechanical assessment of hip capsular repair and reconstruction procedures using a 6 degrees of freedom robotic system. Am J Sports Med. 2017;45:1745–1754. doi: 10.1177/0363546517697956. [DOI] [PubMed] [Google Scholar]
- 8.Larson C.M., Ross J.R., Stone R.M. Arthroscopic management of dysplastic hip deformities: Predictors of success and failures with comparison to an arthroscopic FAI cohort. Am J Sports Med. 2016;44:447–453. doi: 10.1177/0363546515613068. [DOI] [PubMed] [Google Scholar]
- 9.Gnandt R.J., Smith J.L., Nguyen-Ta K., McDonald L., LeClere L.E. High-tensile strength tape versus high-tensile strength suture: A biomechanical study. Arthroscopy. 2016;32:356–363. doi: 10.1016/j.arthro.2015.08.013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video presents an arthroscopic double shoelace capsular plication technique for a left hip with borderline hip dysplasia associated with capsular laxity on a traction table. After the diagnostic arthroscopy is completed, a labral repair and cam osteoplasty are performed. An Ultratape is passed through the hip capsule using a suture lasso loop, and a single shoelace capsular closure is prepared from the anteromedial side of the capsulotomy; another shoelace capsular closure is prepared from the posterolateral side. Finally, 2 pieces of Ultratape are alternately pulled and tightened to secure a double shoelace capsular plication of the enlarged capsulotomy.