Abstract
Background
To assess a new modification of posterior approach to the hip and its effect on stability and functional outcome in total hip arthroplasty.
Material & Methods
A comparative retrospective study was done to assess the functional outcome and rate of dislocation among 233 hips (Group A) operated by conventional posterior approach and 567 hips (Group B) by our novel modified posterior approach. In this technique, 2–3 stay sutures are applied in external rotators, then a single conjoint-myocapsular sleeve is raised linearly over the capsule with adherent fibers of gluteus minimus to piriformis tendon, short rotators and part of quadratus for exposure of femoral head. After inserting the definite prosthesis, upper part of sleeve (capsule, piriformis tendon) is sutured at the lower part of tip of greater trochanter & lower part with lateral trochanteric bone. Fifty patients, using randomised tables, in group B underwent MRI to evaluate the efficacy of the repair at 1 and 12 weeks postoperatively.
Results
Average Harris hip score at minimum 3.9 year follow up was 83.2 in Group A & 88.7 in Group B. Group B had only one dislocation (0.176%) while Group A had 12 dislocations (5.15%). MRI showed intact repair in 47 patients (94%); fibrous continuity in 2 patients (6%) in group B patients.
Conclusion
Intermediate results shows that this technique provides enhanced stability and improved functional outcome. But more prospective and randomised controlled studies with long term followup are required to confirm its role in prevention of hip dislocations.
Keywords: SMS technique, Posterior hip approach, Dislocation, Hip arthroplasty, Single myocapsular sleeve
1. Introduction
With the increasing popularity of total hip replacement (THR) as a treatment option across the globe, the best method of anatomic approach to the hip is often a matter of debate. Over the years, posterior approach to the hip has become one of the most commonly used approaches due to its simplicity and the wide exposure that it can achieve. However, the same has often been criticised due to higher reported dislocation rates compared to anterior, anterolateral, or the lateral approach to the hip. Various authors have time and again suggested methods to increase hip stability with this approach and most of them have described different methods to facilitate meticulous repair of posterior structures in this approach. However, most of these have had their share of problems, and only a few of them have studied the healing of these posterior structures after the repair. We, therefore, describe our modification in terms of a single myocapsular sleeve repair using a posterior approach to the hip. Furthermore, we substantiate our method with our clinical results as well as Magnetic Resonance Imaging (MRI) scan studies showing healing of posterior structures of the hip in these patients in the postoperative period.
2. Material and methods
This study involved a comparative evaluation between 233 cases (Group A) of total hip replacement (THR) done between 2002 and 2007 using the conventional posterior approach to the hip and 567 cases (Group B) of THR done between 2008 and 2013 in which this modified Single Myocapsular Sleeve (SMS) repair technique was used using the posterior approach to the hip. Only primary hip replacements using cementless hip prosthesis were included in the study. All the patients in group B were operated by single senior surgeon. Patients with large discrepancies (greater than 1.5 cm) in preoperative horizontal or vertical offsets were excluded from the study. These patients were then followed up for a minimum of 3.9 years to evaluate dislocation rates (primary outcome) and were also assessed functionally using the Harris Hip Score (secondary outcome).
Yadav and Ashok Single Myocapsular Sleeve (SMS) repair technique in posterior approach to the hip Patient is positioned in strict lateral position after induction of anaesthesia. External rotators of the affected hip are exposed by standard posterior approach. Then a Hohmann retractor is passed below the abductors just above the tip of trochanter and, piriformis tendon and few fibers of gluteus minimus adherent to posterior capsule over femoral head are exposed. Two to three stay sutures (Ethibond 5) are applied in the single myocapsular sleeve consisting of exposed posterior capsule (with few fibers of gluteus minimus), piriformis tendon, short external rotators and proximal part of quadratus muscle (Fig. 1). Then this single (SMS) myocapsular sleeve is raised (by using cautery to cut tissue linearly close to posterior border of greater trochanter) over the capsule to piriformis tendon, short rotators and upper part of quadratus femoris (Fig. 2). In case of flexion deformity, the incision is extended up to the iliopsoas tendon, attached to lesser trochanter and to the transverse and longitudinal fibers of gluteus maximus attached to posterolateral aspect of proximal femur. The hip is dislocated using flexion, adduction and internal rotation maneuver. Then femoral and acetabular preparation is done and definitive implants are inserted as in a conventional standard fashion (Fig. 3). Then with the limb held in adduction and internal rotation, needle of first suture (passed through capsule, piriformis, upper part of the short external rotators) is passed through tip of the greater trochanter (0.5–1 cm away from the posterolateral border of the greater trochanter) (Fig. 4), then needle of 2nd and or 3rd suture (passed through lower part of the short external rotation and upper part of quadrates femoris) is passed through the posterolateral border of greater trochanter (0.5–1 cm distal to first suture and away from the posterolateral margin of the greater trochanter) (Fig. 5). Then with the limb kept in abduction & external rotation, all the sutures are pulled to make sure none of them is loose. After they are firmly tightened, knots are held with artery forceps and 3–4 knots are applied (Fig. 6). Distal tendinous part of gluteus maximus (longitudinal, if possible transverse fibers also) is sutured with monocryl/ethibond [cross horizontal mattress suture] and proximally with vicryl suture. The deep fascia is sutured with vicryl sutures, and subcutaneous tissue (if excessive subcutaneous fat: it is closed in two layers) with vicryl suture. Skin is closed by staples or monocryl and may be left if subcuticular sutures have been applied.
Fig. 1.
Clinical Image showing non absorbable ethibond no. 5 being tied to gluteus minimus, piriformis tendon, superior gamellus, obturator internus, inferior gamellus and some part of quadratus femoris.
Fig. 2.
Clinical image showing lifting of the tagged structures after using a electro cautery to dissect the tissues in a single myocapsular sleeve.
Fig. 3.
Clinical image showing status of single myocapsular sleeve after placement of total hip implant.
Fig. 4.
Clinical image showing needle of first suture (containing capsule, piriformis tendon, upper part of short external rotators and part of gluteus minimus) after being passed through the tip of greater trochanter.
Fig. 5.
Clinical image showing needle of subsequent sutures containing lower part of short external rotators of the hip and superior part of quadratus femoris after being passed through the postero lateral border of greater trochanter.
Fig. 6.

Clinical image showing completed repair of deep posterior structures.
In Group A, conventional posterior approach was used. In this approach, piriformis, short external rotators and proximal part of quadratus femoris were cut separately and tied using 3 separate stay sutures while the underlying capsule was then incised in another layer and tied with one or two more stay sutures. Following implantation of the prosthesis, these 4 structures were tied separately to their insertion using Ethibond #5 to mimic their anatomic attachment. Rest of the technique remained the same.
Postoperative management: All the patients were mobilised and weight bearing was started with walker on second day as tolerated. Hip precautions (avoiding flexion past 110° and any internal rotation of hip) were enforced during the first 6 weeks after surgery.
Furthermore, using computer generated randomised tables 50 patients in group B (Ratio of 1: 11.4 among the total operated patients in group B) were subjected to Magnetic Resonance Imaging scans of the hip to evaluate the efficacy of the repair of the posterior structures at a follow up of 1 and 12 weeks postoperatively. MRI was performed using an established MR protocol. A clinical 1.5 T MR Scanner (Avanto, Siemens, Erlanger, Germany) was used for all examinations using a receive-only phased array body coil. Axial and coronal fast spin echo images were obtained. They had a repetition time of 4000–6000 ms and effective echo time of 34 ms. The receiver bandwidth was 62.5–100 kHz (over full frequency range) with maximum in-plane resolution of 352 lm 9562 lm, and slice resolution of 3–4 mm at three to four excitations. All MRI studies were interpreted by single expert radiologist. The repaired myocapsule was considered intact when the greater trochanter was in contact with both the proximal and distal part of myocapsule (Fig. 7), partially intact when there was contact of either the proximal or distal part of the posterior myocapsule, or failed when there was no contact between either limb of the posterior capsule with the greater trochanter (Fig. 8). Any discontinuity in the hypointense signal of tendon and the filling of space with hyperintense signal of scar tissue was interpreted as gap. Such gaps with a distance of over 25 mm was interpreted as failed repair.1,2 The quality of obturator internus and pyriformis muscle was classified as either absence of atrophy or into mild, moderate and severe categories on the basis of fatty infiltration of the muscle bellies in their cross section, comparing serial MRI examinations.
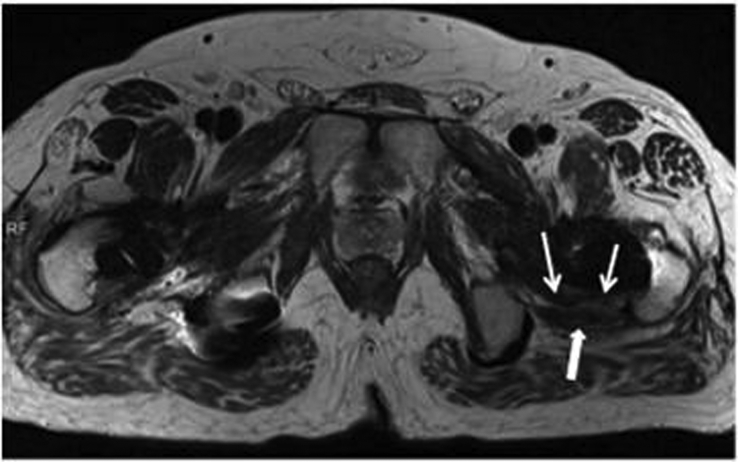
Fig. 7.
Axial MR image following THA showing an intact myocapsular repair {posterior capsule (arrows) and obturator internus tendon (block arrow)}.
Fig. 8.
Axial MR image following THA showing dehiscence of the proximal posterior capsular repair as shown by fluid collection (arrow).
3. Results
Average Harris hip score at minimum 3.9 yr follow up was 83.2 in Group A & 88.7 in Group B. Group B had only one dislocation (0.17%) while Group A had 12 dislocations (5%). At one week post operative, the averaged length between greater trochanter and the hypointense piriformis tendon signal was 23.5 mm (range, 11.7–33.5 mm). At 12 weeks follow up, 13 of the 50 patients had no atrophy of piriformis muscle, 20 patients had mild piriformis atrophy and none of the patients had severe muscle atrophy. The averaged gap between the greater trochanter and the conjoined tendon MRI signal was 25.5 mm (range, 10.4–40.0 mm). Two patients had interruption of the signal over more than 25 mm. So over all at the 3-month follow up, 48 patients (95%) had an intact repair on MRI while two patients had fibrous continuity. Out of these two, one had dislocation at 4 months, which was managed successfully with reduction and conservative treatment and use of an abduction brace.
4. Discussion
Various surgical approaches for total hip arthroplasty have been described in literature. The posterolateral approach is the most commonly employed technique due to its relative simplicity and fewer intraoperative complications. It was first described by Moore and then was subsequently modified by Gibson3 and various other surgeons over the years. However this approach is believed to be associated with a higher number of posterior dislocations as compared to other approaches. The overall rate of dislocation has been recorded to be around 4–8%4, 5, 6, 7 using posterior approach with maximum occurrence in the first 6 weeks as reported by Cobb et al.8 Posterior approach has been associated with dislocation to such an extent that many surgeons also restrict their patients in doing a lot of activities (squatting, sitting on floor, adduction of hips) following THA with this approach. However, Van der Weegen et al.9 in 2019 in their prospective cohort study reported how minimal restrictions with large femoral head were as safe as extensive restrictions to prevent dislocations when THA's were performed by the posterior approach. Miller et al.10 in their systematic review of 1,67,308 THA's done by direct anterior and posterior approach reported higher dislocation and reoperation rates in the posterior approach. However, over 87% of the patients in their huge sample size underwent THA with posterior approach, which shows the familiarity and technical easiness that the surgeons feel with the posterior approach and how a technique that could decrease the dislocation rates following posterior approach could be helpful to many such surgeons. Wang et al.11 in 2018 in meta analysis of 9 RCT's concluded no difference in rates of dislocation between anterior and posterior approaches. To overcome complication of dislocation using posterior approach, modifications of the existing technique have been devised by orthopaedic surgeons world over. White et al., in 200112 conducted a study to compare the incidence of posterior dislocations in primary hip replacements using either formal posterior capsular repair or total posterior capsulectomy. They reported an incidence of 4.8% early posterior dislocation (within the first 6 months) in the posterior capsulectomy group as compared to a 0.7% incidence in the capsular repair group. Also, the occurrence of posterior dislocation is reduced in anterolateral approach to hip arthroplasty due to undisturbed posterior capsular structures. Other mechanisms described to reduce the incidence of posterior dislocation include limitation of movement, use of supports such as abduction brace in patients at increased risk for dislocation,13 offset femoral or acetabular liners,8 formal posterior capsular repair.14 Posterior capsular reattachment helps in that it not only serves as a physical barrier but also leads to early reattachment of the capsule without being dependent on posterior capsular regeneration. Also, it reduces internal rotation by 50%, thus helping to maintain the prosthesis in position. This was the basis of reattaching the posterior capsule and the short external rotators in a single layer. In the technique described by Zhang et al.,15 modified posterior soft tissue repair was performed using anchor sutures. The main advantage of this technique is superior surgical site exposure. However, the need to raise two flaps and the separation of the gluteus minimus from the capsule causes weakening of the capsule and does not follow the single sleeve concept. However, in the technique described by us, the gluteus minimus is kept intact which gives extra strength to the sleeve. Other disadvantages of their technique are related to the use of drills which increases the risk of greater trochanteric fractures (0.9%) as reported by White et al..12 The authors changed the size of the drill from 2.7 mm to 2.3 mm which reduced the incidence of fractures.16 Additional closure and suture related complications including sciatic nerve injury, and the cost and time of putting the sutures were the other drawbacks in their technique. Stahelin et al.17 reported a 70% failure with 2# Ethibond Excel for reinserted short external rotator muscles after hip arthroplasty. Another modification of posterior soft tissue repair was proposed by Pellicci et al..14 They described a meticulous reconstruction of the posterior soft tissue sleeve with the advantages of maintenance of a biological scaffold on which a dense pseudocapsule is formed with a subsequent reduction of dislocation rate to 0–0.8% from 4 to 6.2%. However, like in the technique described by Zhang et al., this too has the disadvantage of drilling into the bone with the risk of fracturing. Also, the surgical technique requires the creation of separate flaps of piriformis tendon and conjoint tendon, quadratus femoris capsular flap which makes the procedure more tedious. Hedley et al.18 described a technique of posterior approach in which the short external rotators and the posterior hip capsule are preserved and then reflected during surgery, subsequently allowing the suturing of a single myocapsular flap during closure. This technique relies on closure with relatively intact structures thus maintaining the normal biological tissue rather than the scar tissue or pseudocapsule which develops after tissue healing. Osmani et al.16 in 2004 described an inverted L shaped incision – wherein the short limb was the incision between the piriformis tendon and gluteus minimus starting 2 cms posterior to the greater trochanter towards the piriform fossa. The vertical limb is formed by the piriformis/conjoint tendon which is peeled off as a single unit. The anterior capsule is left uncut and the inferior capsule is resized. They reported that posterior dislocation rate could be reduced by maintaining the attachment for short rotator muscles to posterior capsule and integrity of the posterior flap. Their technique used three finer wire suture and 4 holes - 1 cm apart, exiting the piriformis fossa (junction of middle third/posterior third) in the tendinous part of the rotator & capsule. Total three sutures were used, one each at at piriformis with capsule, conjoint tendon, and capsule/quadratus. They used 2.3 mm drill as compared to the 2.7 mm used by White et al. (0.9% fracture rate)9 and reported no fractures. But problems associated with this procedure include an increased posterior offset, insufficient capsule in addition to being expensive, and having drilling associated complications. Osmani et al.16 concluded that posterior myocapsular reconstruction should be routinely made a part of posterolateral approach to hip arthroplasty to subsequently reduce the risk of hip dislocations. In this index technique two to three stay sutures (Ethibond 5) are applied in the single myocapsular sleeve consisting of exposed posterior capsule (with few fibers of gluteus minimus), piriformis tendon, short external rotator and proximal part of quadratus muscle. Then this single (SMS) myocapsular sleeve is raised over the capsule to piriformis tendon, short rotators and part of quadratus femoris. After inserting definitive prosthesis, single myocapsular sleeve is sutured to greater trochanter (posterolateral border of greater trochanter and close to the tip of greater trochanter) by passing the needles of same 2–3 sutures. This single myocapsular sleeve gets further additional support by repair (cross horizontal suture for longitudinal tendinous part and if possible the transverse part also) of the gluteus maximus. We used Ethibond No 5 because it is easily available, cost effective, its needle is very strong and curved so it can be easily passed through trochanteric border. We did not prefer to use a drill bit as it could damage the bone stock or fracture the trochanter especially in Asian patients. It is also strong enough to resist forces generated during postoperative physiotherapy. At the 12 week follow up, 48 patients (95%) had at intact repair on MRI while two patients had fibrous continuity. Out of these two, one had dislocation at 4th month, which was managed successfully with closed reduction and conservative treatment by use of an abduction brace. This additional MRI study confirms that although patients show gap formation between the hypointense external rotator tendon/capsule and the greater trochanter, dead space formation did not occur and the defect was filled with hyperintense scar tissue in all patients in the current study. This is the first study describing a novel single myocapsular sleeve repair in posterior approach to hip and documenting the success of repair on postoperative MRI. This technique ensures fast, strong & biological repair; enhances stability and improve functional outcome. Limitations of the study include not just the retrospective study design but also surgery not being performed by one single surgeon in group A. This may slightly be negated by use of post operative MRI to study the intactness of repair but still remains a limitation of the study. The technique, of course, may not replace the conventional posterior approach as it may not be suitable for patient having multiple previous surgery, severe dysplastic hip, severe inflammatory disease due to scarring or poor soft tissue quality of hip capsule and short external rotator of hip. As this is a retrospective study with short follow up, more prospective and randomised controlled studies with long-term follow up are required to demonstrate actual rate of dislocation after myocapsular sleeve repair. Talia et al.19 would be doing a head to head comparison of direct anterior, lateral and posterior approach in THA's in a randomised study as they have already published their trial and their study may help shed some more light on this subject once their results are published.
References
- 1.Pellicci P.M., Potter H.G., Foo L.F., Boettner F. MRI shows biologic restoration of posterior soft tissue repairs after THA. Clin Orthop. Apr. 2009;467(4):940–945. doi: 10.1007/s11999-008-0503-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vasilakis I., Solomou E., Vitsas V., Fennema P., Korovessis P., Siamblis D.K. Correlative analysis of MRI-evident abductor hip muscle degeneration and power after minimally invasive versus conventional unilateral cementless THA. Orthopedics. Dec. 2012;35(12):e1684–e1691. doi: 10.3928/01477447-20121120-10. [DOI] [PubMed] [Google Scholar]
- 3.Gibson A. Posterior exposure of the hip joint. J Bone Joint Surg Br Vol. May 1950;32-B(2):183–186. doi: 10.1302/0301-620X.32B2.183. [DOI] [PubMed] [Google Scholar]
- 4.Fackler C.D., Poss R. Dislocation in total hip arthroplasties. Clin Orthop. Sep. 1980;151:169–178. [PubMed] [Google Scholar]
- 5.McCollum D.E., Gray W.J. Dislocation after total hip arthroplasty. Causes and prevention. Clin Orthop. Dec. 1990;261:159–170. [PubMed] [Google Scholar]
- 6.Woo R.Y., Morrey B.F. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. Dec. 1982;64(9):1295–1306. [PubMed] [Google Scholar]
- 7.Robinson R.P., Robinson H.J., Salvati E.A. Comparison of the transtrochanteric and posterior approaches for total hip replacement. Clin Orthop. Apr. 1980;147:143–147. [PubMed] [Google Scholar]
- 8.Cobb T.K., Morrey B.F., Ilstrup D.M. The elevated-rim acetabular liner in total hip arthroplasty: relationship to postoperative dislocation. J Bone Joint Surg Am. Jan. 1996;78(1):80–86. doi: 10.2106/00004623-199601000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Van der Weegen W., Kornuijt A., Das D., Vos R., Sijbesma T. It is safe to use minimal restrictions following posterior approach total hip arthroplasty: results from a large cohort study. Hip Int. 2019 Jan doi: 10.1177/1120700018823504. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 10.Miller L.E., Gondusky J.S., Kamath A.F., Boettner F., Wright J., Bhattacharyya S. Influence of surgical approach on complication risk in primary total hip arthroplasty. Acta Orthop. 2018 Jun;89(3):289–294. doi: 10.1080/17453674.2018.1438694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang Z., Hou J.-Z., Wu C.-H. A systematic review and meta-analysis of direct anterior approach versus posterior approach in total hip arthroplasty. J Orthop Surg. 2018 Sep 6;13(1):229. doi: 10.1186/s13018-018-0929-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White R.E., Forness T.J., Allman J.K., Junick D.W. 210 Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop. Dec. 2001;393:163–167. doi: 10.1097/00003086-200112000-00019. [DOI] [PubMed] [Google Scholar]
- 13.Clayton M.L., Thirupathi R.G. Dislocation following total hip arthroplasty. Management by special brace in selected patients. Clin Orthop. Aug. 1983;177:154–159. [PubMed] [Google Scholar]
- 14.Pellicci P.M., Bostrom M., Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop. Oct. 1998;355:224–228. doi: 10.1097/00003086-199810000-00023. [DOI] [PubMed] [Google Scholar]
- 15.Zhang Y., Tang Y., Zhang C., Zhao X., Xie Y., Xu S. Modified posterior soft tissue repair for the prevention of early postoperative dislocation in total hip arthroplasty. Int Orthop. Jun. 2013;37(6):1039–1044. doi: 10.1007/s00264-013-1874-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osmani O., Malkani A. Posterior capsular repair following total hip arthroplasty: a modified technique. Orthopedics. Jun. 2004;27(6):553–555. doi: 10.3928/0147-7447-20040601-10. [DOI] [PubMed] [Google Scholar]
- 17.Stähelin T., Vienne P., Hersche O. Failure of reinserted short external rotator muscles after total hip arthroplasty. J Arthroplast. Aug. 2002;17(5):604–607. doi: 10.1054/arth.2002.32187. [DOI] [PubMed] [Google Scholar]
- 18.Hedley A.K., Hendren D.H., Mead L.P. A posterior approach to the hip joint with complete posterior capsular and muscular repair. J Arthroplast. 1990;5(Suppl):S57–S66. doi: 10.1016/s0883-5403(08)80027-7. [DOI] [PubMed] [Google Scholar]
- 19.Talia A.J., Coetzee C., Tirosh O., Tran P. Comparison of outcome measures and complication rates following three different approaches for primary total hip arthroplasty: a pragmatic randomised controlled trial. Trials. 2018 Jan 8;19(1):13. doi: 10.1186/s13063-017-2368-7. [DOI] [PMC free article] [PubMed] [Google Scholar]