Abstract
Background
Pediatric pneumonia is a significant cause of inpatient care in the United States. Significant resource utilization and the high cost of care necessitate careful evaluation, especially with continuously decreasing financial resources. Several studies have evaluated subsets and regional impact of these diagnoses, but only a few have evaluated these on a national level.
Methods
This retrospective analysis utilized the 2009–2012 HCUP KID Inpatient Dataset to evaluate the relationship between pneumonia diagnosis and factors affecting cost for patients between 0 and 21. One hundred forty-five thousand one hundred forty-six patients’ charges with primary pneumonia diagnosis were evaluated based on LOS, chronic conditions, severity, mortality and region.
Results
Majority of cases of diagnosis were of unspecified organism: 11,4811 (78%) of the total population. RSV-related pneumonia diagnosis presented second with a total of 8,156 (5.5%). Charges for pneumonia in the Emergency Department (ER) were about $13,104 and non-ER presentation at $10,238. LOS affected total charge and mortality risk for all patient population regardless of age.
Conclusion
This nationwide study provides a unique preview of the cost associated with care for pediatric pneumonia. Such information is essential in developing strategies to improve health outcomes and resources allocation.
Keywords: Upper respiratory infections, Pneumonia, Pediatrics, Health outcomes, Cost, Charges, Cost influencers, Length of inpatient stay(LOS)
1. Introduction
Respiratory presentations are estimated to be the cause of death of an estimated 16% of individuals below the age of five [1]. It is the most common medical presentation in the pediatric population; furthermore, respiratory presentations of one form or another rank 1–3 place as a reason for seeking care among these populations. Acute bronchitis and asthma rank second and third respectively as principal diagnosis in the pediatric population [2]. Several risk factors increase the likelihood of pneumonia in these populations such as low socioeconomic status, malnutrition, chronic medical conditions, and secondary smoke exposures and infections acquired through daycare centers. The presentation of pneumonia varies with age as well as pathogens. Viral pneumonia is usually more common in the first two years of life, and then bacterial pneumonia becomes more prevalent after two years of age. [3].
Respiratory presentations are the most common pediatrics presentation in the emergency setting as well as the most common cause for hospitalization [[4], [5], [6]]. Understanding the various dynamics associated with pediatrics pneumonia and outcomes is essential in evaluating current treatment protocols, public educational approaches as well as financial investment in effective prevention strategies. The diversity of organisms that causes pneumonia both viral and bacterial makes it difficult for the development of a concise strategy and approach to treating these medical conditions, especially in the pediatric population. These variations and presentations mean a tremendous variance in the cost of care and outcome [2,8]. There has been consistent research on treatment protocols as well as the prevalence of pediatric pneumonia complications [[4], [5], [6]]. There are, however, some deficiencies in the areas evaluating the relationship between the cost of care, outcomes and demographics. There has been extensive research using the national dataset to evaluate CAP and its relationship with complication and hospitalization [5,7]. These studies have shown variances in treatment approaches or standards as well as the cost of utilization of healthcare resources [7].
The average cost of care for these inpatient presentations could aid in understanding the variance in treatment protocols. Moreover, it could broaden our understanding of resource utilization and development of strategies to improve or maintain the quality of care while focusing on prevention and cost reduction. Many national trends analysis focused mainly on viral, emphysema or severe respiratory presentations [8]. Moreover, these studies have focused on particular age groups, not the broader pediatric population [[9], [10], [11], [12]]. This study utilizes a national database (HCUP KID database) to determine the total pneumonia hospitalizations (2009–2012) without those acquired through sexual transmitted infections and tuberculosis.
2. Methods
This study was conducted utilizing the HCUP KID Inpatient database release for 2009 and 2012. The KID databases are part of the Healthcare Cost and Utilization Project sponsored by the Agency for Healthcare Research and Quality. It is the most comprehensive dataset that specifically contains pediatric inpatient medical presentations, outcomes and total cost of care. The dataset is unique in the data elements it provides for research and studying trends across the United States as well as the high number of participating states (44) for 2009 and 2012 releases. We selected 2009 and 2012 dataset because of the similarities in elements and the total number of participating states and hospitals. HCUP is released every three years since 1997. The dataset is unique for national estimates because of the 44 states included in the dataset which makes up about 90% of the population in the United States.
2.1. Study cohort
We included patients between 0 and 21 with primary pneumonia diagnosis.
2.2. Inclusion criteria
Individuals with the (1) an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM), primary diagnosis code indicating pneumonia (codes 480–484 and 485–486). Other classification of pneumonia which includes empyema (5100–5109) and Pleurisy (5110–5119) were included. Individuals with a secondary diagnosis of pneumonia, empyema or pleurisy were also included in this study.
2.3. Exclusion criteria
Individuals with diagnosed immunodeficiencies, and malignancies were excluded. Pneumonia-associated complications were identified by using ICD-9-CM diagnosis and procedure codes Complications classified as local, systemic or metastatic were also excluded (Appendix 1).
2.4. Analysis
The study population was analyzed based on a wide range of characteristics such as age, location, race, gender, length of inpatient stay (LOS), the severity of illness and mortality. Age group was further sub-grouped into infants (<1 year), children (1–12 years), Adolescents (13–17years) Young adults (18–21). Cases missing any of the variables mentioned were excluded from the study. These factors were then evaluated based on demographics, cost, and severity. Disease severity and mortality for all patients grouped by age, race, and location (Income) were further analyzed. All analysis was performed with weights on per HCUP guidelines. All variable analysis was performed with IBM-SPSS Version 23.
3. Results
Respiratory presentations in the ER setting continues to increase over the years; moreover, respiratory presentation continues to be one of the most prevalent causes of hospitalization in the pediatric population. Table 1 shows an overview of the percent presentation for pneumonia.
Table 1.
Variation in patient population and shows that pneumonia diagnosis based on the definition of this study was only recorded in about 3% of the total pediatric presentation for the period of this study.
| Frequency | Percent | Cumulative Percent | |
|---|---|---|---|
| Other non-pneumonia primary x | 3095168 | 96.9 | 96.9 |
| Pneumonia Dx other than influenza and TB | 91577 | 2.9 | 99.7 |
| Influenza related Dx | 8284 | 0.3 | 100.0 |
| Tuberculosis and others | 753 | 0.0 | 100.0 |
| Total | 3195782 | 100.0 |
Table 1 also shows the variation in the patient population and shows that pneumonia diagnosis based on the definition of this study was only recorded in about 3% of the total pediatric presentation for the period of this study.
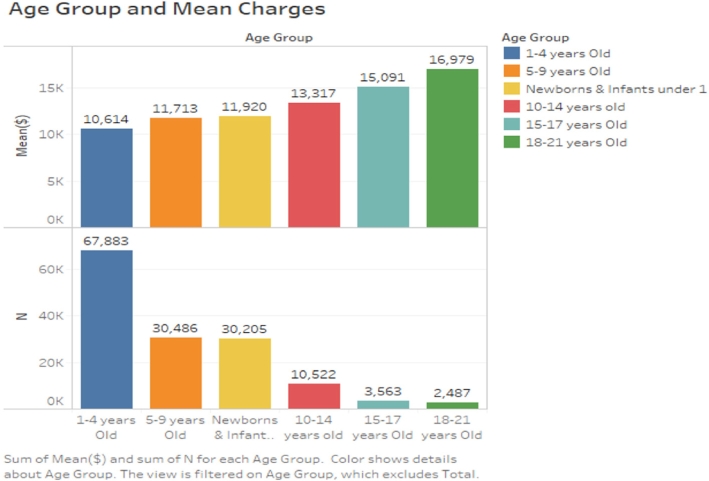
Table 2 and Fig. 1 shows the relative relationship between the age groups and total expenditures per patient population. Further evaluation shows that individuals aged 1–4 (46%) presented most with pneumonia in the healthcare setting. Moreover, the mean cost of care for this population was less compared to the older population. One can also observe that as one gets older, the likelihood of increased cost of pneumonia care increased. Such an observation shows that the approach to our healthcare resource allocation including public health focus on targeting only adults in pneumonia prevention needs a focus on these populations too.
Table 2.
Mean charges patient age.
| Discharge Year | Mean ($) | N | Std. Deviation | Sum ($) | Minimum ($) | Maximum ($) | % of Total Sum | % of Total N |
|---|---|---|---|---|---|---|---|---|
| Newborns & infants under 1 | 11920.22 | 30205 | 13354.531 | 360051239 | 271 | 552582 | 21.5 | 20.8 |
| 1–4 years Old | 10614.47 | 67883 | 10362.214 | 720536918 | 151 | 444674 | 43.0 | 46.8 |
| 5–9 years Old | 11713.25 | 30486 | 15298.804 | 357091149 | 136 | 1361601 | 21.3 | 21.0 |
| 10–14 years old | 13317.14 | 10522 | 15937.801 | 140129176 | 286 | 429014 | 8.4 | 7.2 |
| 15–17 years Old | 15091.29 | 3563 | 21789.246 | 53763683 | 432 | 462971 | 3.2 | 2.5 |
| 18–21 years Old | 16979.07 | 2487 | 20040.275 | 42228769 | 740 | 317315 | 2.5 | 1.7 |
| Total | 11531.86 | 145146 | 13225.486 | 1673800935 | 136 | 1361601 | 100.0 | 100.0 |
Bold- Total and Mean Cost of Care in US Dollars, Italics-Percent of N and total Sum.
Fig. 1.
Mean charges by age group.
Further analysis of the data also indicates that the presentation of pneumonia in the sample study decreased from 2009 (84,233) to 2012 (61,302) by about 13%. This finding is in contrast to the increase in cost or charges of $10,741 and $12,647 in 2009 and 2012 respectively. A further breakdown of the population based on sex shows a steady trend of about 54.3% (76,977) male and 45.7% (64,808) female in the total population.
3.1. Mean charges and length of inpatient stay (LOS)
The LOS for the population shows a significant difference in the cost of care based on how long an individual is hospitalized. It also shows some variation in charges on presentation. For example, for 1-day inpatient, the cost of care was about $5,548 in 2009 reporting period and $6,538 for 2012. Table 3 shows a direct correlation between LOS and charge increase. Further analysis shows that diagnoses (NDX), and chronic conditions (NCHRONIC) directly impacts the total cost and length of inpatient stay significantly with about $10,000-$40,000 between 200 and 2012. Further analysis of LOS indicates that patients stay longer in private for-profit hospitals than non-profit hospitals.
Table 3.
Direct correlation between LOS and charge increase.
| Mean Charges And LOS | Mean ($) | N | Std. Deviation | Minimum ($) | Maximum ($) | % of Total N |
|---|---|---|---|---|---|---|
| 0 | 5,445.30 | 3564 | 3699.447 | 236.00 | 38,952.00 | 2.5 |
| 1 | 5,979.14 | 35134 | 4207.812 | 136.00 | 176,962.00 | 23.9 |
| 2 | 8,808.06 | 52082 | 9855.198 | 162.00 | 1,361,601.00 | 36.5 |
| 3 | 12,676.37 | 29288 | 7913.801 | 286.00 | 130,570.00 | 19.8 |
| 4 | 17,307.44 | 12846 | 10861.953 | 960.00 | 184,587.00 | 9.0 |
| 5 | 22,400.12 | 5929 | 13525.192 | 1,041.00 | 133,080.00 | 4.0 |
| 6 | 28,678.77 | 2937 | 18202.979 | 1,259.00 | 157,049.00 | 1.9 |
| 7 | 35,715.16 | 1475 | 21643.925 | 2,143.00 | 158,030.00 | 1.0 |
| 8 | 43,075.90 | 697 | 26558.122 | 8,492.00 | 196,065.00 | 0.4 |
| 9 | 49,746.19 | 347 | 31144.660 | 9,525.00 | 191,120.00 | 0.2 |
| 10 | 57,854.79 | 258 | 31367.250 | 2,071.00 | 190,082.00 | 0.2 |
| 11 | 67,196.75 | 147 | 43304.879 | 12,182.00 | 288,201.00 | 0.1 |
| 12 | 74,337.69 | 76 | 46098.811 | 10,315.00 | 268,901.00 | 0.1 |
| 13 | 77,632.45 | 88 | 43658.033 | 18,236.00 | 223,893.00 | 0.1 |
| 14 | 75,501.53 | 88 | 31378.277 | 4,512.00 | 172,225.00 | 0.1 |
| 15 | 86,162.81 | 46 | 46612.368 | 12,384.00 | 207,000.00 | 0.0 |
| 16 | 113,336.00 | 27 | 64128.969 | 19,095.00 | 308,682.00 | 0.0 |
| 17 | 113,595.94 | 20 | 65101.062 | 25,015.00 | 261,479.00 | 0.0 |
| 18 | 111,823.47 | 12 | 46444.533 | 36,374.00 | 190,581.00 | 0.0 |
| 19 | 189,588.50 | 9 | 89095.006 | 58,045.00 | 294,640.00 | 0.0 |
| 20–84 | 156,133.84 | 60 | 81019.605 | 92,076.00 | 311,753.00 | 0.0 |
| Total | 11,436.89 | 145146 | 13055.178 | 136.00 | 1,361,601.00 | 100.0 |
Table 4 shows the relationship between patient disposition and charges. It shows that the majority of inpatient care for pneumonia was routine for all age groups. Moreover, it shows that inpatient death could be associated with high cost compared to other transfer that indicates low severity and mortality. The individuals discharged to home health care shows a decrease from previous years. The number of presentations were more in 2009 compared to 2012. The sum of total expenditure or charges between these years shows an average decrease in total cost as with patient presentation. Further analysis of patient disposition shows severity and LOS did not significantly affect whether patients were discharged to short term hospitals, skilled nursing facilities or home.
Table 4.
Mean charges and patient disposition.
| Mean ($) | N | Std. Deviation | % of Total N | % of Total Sum | Sum ($) | Median ($) | |
|---|---|---|---|---|---|---|---|
| Routine | 11495.17 | 140857 | 12893.777 | 97.1 | 96.7 | 1619172676 | 8199.00 |
| Transfer to short-term hospital | 8951.84 | 2854 | 13015.669 | 2.0 | 1.5 | 25544576 | 6147.27 |
| Transfer to others? | 20544.35 | 184 | 32574.946 | 0.1 | 0.2 | 3773026 | 10484.77 |
| HHC | 22880.44 | 995 | 32544.615 | 0.7 | 1.4 | 22758919 | 13344.12 |
| AMA | 8016.74 | 211 | 6673.117 | 0.1 | 0.1 | 1695271 | 5930.32 |
| Died in hospital | 47797.64 | 12 | 68421.257 | 0.0 | 0.0 | 554208 | 25313.82 |
| Discharged alive | 16358.07 | 8 | 11838.925 | 0.0 | 0.0 | 134836 | 9472.16 |
| Total | 11532.75 | 145146 | 13226.453 | 100.0 | 100.0 | 1673633511 | 8174.72 |
Transfer other: includes Skilled Nursing Facility (SNF), Intermediate Care Facility (ICF), and another type of facility.
Against medical advice (AMA).
Discharged alive, destination unknown, beginning in 2001.
Home Health Care HHC.
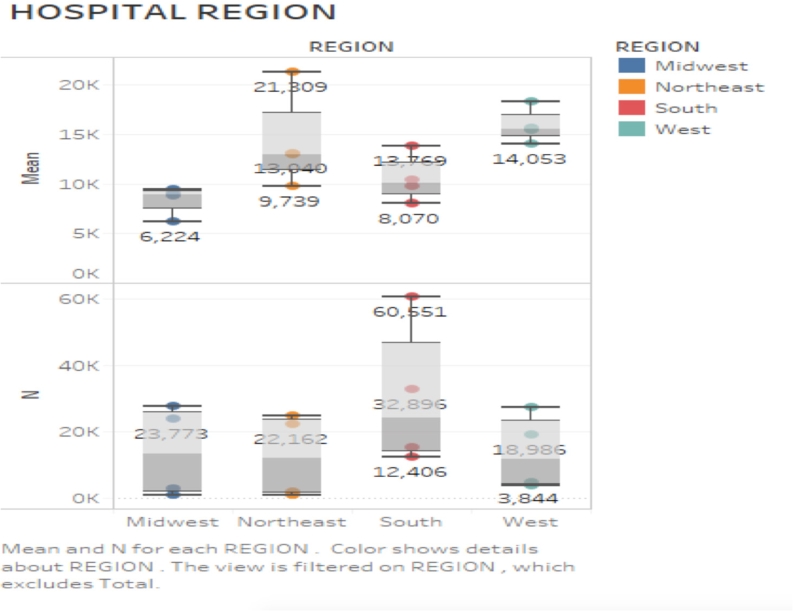
Table 5 shows that even though there are changes in the entire presentation in 2012 compared to 2009; these presentations and cost show that a high or majority of patients presented during the colder months. Further analysis shows that the regions in the southern part of the country experienced more recorded cases (44%) followed by the Midwest (20%). Colder regions are not at increased risk of such infection than other warm regions in the United States. Further analysis shows lower charges in the Midwest compared to other regions in the country. Discharge quarter and year of shows statistical significance (p-0.000).
Table 5.
Total charges and discharge quarter.
| Total charges | ||||||
|---|---|---|---|---|---|---|
| Discharge year | Mean ($) | N | Std. Deviation | Minimum ($) | Maximum ($) | % of Total N |
| First Quarter (Jan–March) | 11394.92 | 52350 | 14054.324 | 162 | 1361601 | 36.7 |
| Second Quarter (Apr–June) | 11435.60 | 28196 | 12151.703 | 151 | 429014 | 19.8 |
| Third Quarter (Jul–September) | 11248.99 | 3032 | 11904.914 | 136 | 462971 | 15.1 |
| Fourth Quarter (October–December) | 11591.30 | 42568 | 12905.479 | 432 | 552582 | 28.4 |
| Total | 11436.80 | 145146 | 13055.620 | 136 | 1361601 | 100.0 |
Table 6 shows much of the presentation source was of emergency room origin. Only about 30% of individuals treated with pneumonia did not have an initial point of contact in an ER setting. The mean charges for all ER presentation showed a higher charge and those of no ER presentation. The mean charges for each presentation show some difference based on hospital region (95 CI, $465-$740). Moreover, charges in the Midwest shows lower cost compared to other regions.
Table 6.
Mean charges and emergency demographics.
| HCUP ER Record | Mean | N | Std. Dev | N (%) | Sum (%) | Sum ($) | Median |
|---|---|---|---|---|---|---|---|
| No ERR | 10238.12 | 51318 | 15531.283 | 35.3 | 31.3 | 525403121 | 6576.00 |
| ERR | 11124.94 | 60185 | 10834.812 | 41.5 | 40.0 | 671776664 | 8234.00 |
| +ERR | 13472.37 | 16433 | 11455.521 | 11.4 | 13.3 | 223438502 | 10485.00 |
| +CPT | 12766.44 | 22 | 5388.537 | .0 | .0 | 282205 | 10858.44 |
| ED Origin | 15057.14 | 17189 | 14118.137 | 11.8 | 15.4 | 258812063 | 11232.27 |
| Total | 11544.51 | 145146 | 13223.582 | 100.0 | 100.0 | 1679712555 | 8186.00 |
Record does not meet any HCUP Emergency Department criteria (No ERR).
Emergency Department revenue code on record ERR.
Positive Emergency Department charge (when revenue center codes are not available) +ERR.
Emergency Department CPT procedure code on record + CPT.
Condition code P7 indication of ED admission, point of origin of ED, or admission source of ED- ED Origin.
Table 7 provides further details of the relationship between severities in the population. Minor to moderate loss of function in this category showed the most significant presentation with 51 and 34% of entire presentation respectively. Significant and extreme loss of function in the same population was 11.6 and 2.7 respectively. A further in-depth analysis shows that pediatric pneumonia in each of these categories decreased from 2009 to 2012 respectively. Further analysis shows that individuals between 1 and 4 years old had the highest likelihood of being hospitalized for pneumonia generally; this patient population also had the highest charge rate (43.1% of total pneumonia expenditures) followed by patients less than one-year-old and 5–9 with 20.8 and 20.9% respectively. The results indicate that high severity presentation has decreased and substantially minimized from the previous three years as depicted by the year 2009 and 2012. Further analysis of the relationship between the variables and finance or charges shows a p-value of .000. Careful evaluation of disease severity indicates direct correlation to severity classification to LOS. Individuals classified with major and significant loss of function (15%) spent on average about 3 days more inpatient and showed higher charges.
Table 7.
Mean charges and severity.
| Severity of illness | Mean ($) | N | % of Total N | Std. Deviation | Sum ($) | % of Total Sum |
|---|---|---|---|---|---|---|
| No class specified | 12,317.81 | 865 | 0.2% | 16033.653 | 2,739,548.62 | 0.2 |
| Minor loss of function | 11,705.57 | 73790 | 51.5% | 12633.383 | 840,347,499.14 | 51.5 |
| Moderate loss of function | 11,720.95 | 49592 | 34.1% | 12487.952 | 557,828,456.51 | 34.2 |
| Major loss of function | 11,561.36 | 17142 | 11.6% | 12318.141 | 186,628,909.12 | 11.4 |
| Extreme loss of function | 11,606.59 | 3755 | 2.7% | 11305.868 | 43,585,197.18 | 2.7 |
| Total | 11,692.44 | 145146 | 100.0% | 12519.741 | 1,631,129,610.57 | 100.0 |
The general observation from these presentations in Table 8 shows a general improvement in pneumonia cases evidenced by the decrease in a whole patient presentation in 2012 compared to 2009 dataset. Patients with minor to no risk of death made up a majority of population as observed in the table above. Patient between 1 and 4 years old had more presentations in both years compared to other age groups with a percentage of 46.8. Patients less than one-year-old and 5–9 made up the second highest populations with an estimated percentage of 20.8 and 20.9 respectively. Patient dynamics for extreme mortality shows that it mainly decreased from 2009 to 2012 with a representation of 0.7 and 0.4% of pneumonia patients respectively. A careful analysis shows that the total expenditure nationally has decreased by millions of dollars just as patient pneumonia presentation decreased over the years.
Table 8.
Mean charges and severity.
| Mean ($) | N | Std. Deviation | % of Total N | Sum ($) | % of Total Sum | |
|---|---|---|---|---|---|---|
| No class specified | 12317.81 | 222 | 16033.653 | .2 | 2739549 | 0.2 |
| Minor likelihood of dying | 11652.62 | 128824 | 12456.668 | 89.7 | 1454523945 | 89.5 |
| Moderate likelihood of dying | 12071.06 | 11292 | 13634.215 | 6.7 | 112165132 | 6.9 |
| Major likelihood of dying | 11628.05 | 3258 | 11713.874 | 2.3 | 37886152 | 2.3 |
| Extreme likelihood of dying | 11541.11 | 1550 | 11701.881 | 1.1 | 17538050 | 1.1 |
| Total | 11679.84 | 145146 | 12520.807 | 100.0 | 1.624,852,828 | 100.0 |
Bold- Total and Mean Cost of Care in US Dollars, Italics-Percent of N and total Sum.
3.2. Hospital Region and charges
An analysis of the data indicates a high number of patient presentation within the southern part of the country as shown in Fig. 2 below about 43% of all presentation occurred in the south with an average charge of $10,482. The trend in the patient presentation shows continuity with the South regions reporting 25% and 19% for 2009 and 2012 data release respectively. Generally, pneumonia presentation decreased with about 84,233 (57.9%) and 61302 (42.1%) for 2009 and 2012 data release respectively. Further analysis indicates that the majority of patients 55% were Medicaid recipients followed by private insurance (38%). The mean cost of care for Medicaid and private insurance patients was $11,597 and $11,312 respectively. Even though the reimbursement rate for Medicare and Medicaid are generally less the charges are similar to private insurance coverage. Analysis of cost by region, hospital control and bed size show West with a higher mean total charge with about 26% of pneumonia presentation. South, Midwest, Northeast showed a mean of $10389, $8749, $13,040 with about 39%, 15% and 20% of the pneumonia presentation respectively.
Fig. 2.
Home region and charges.
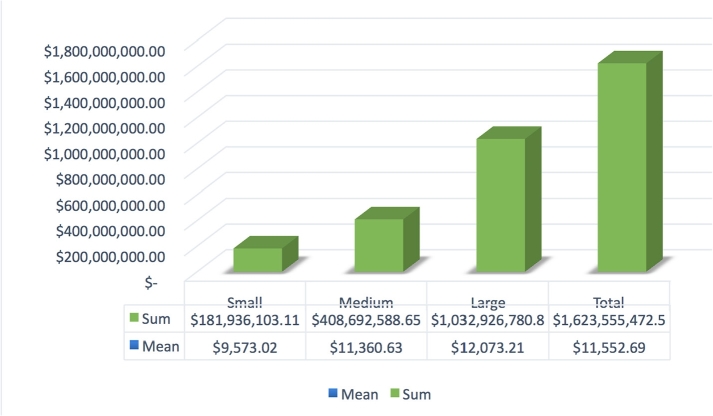
3.3. Hospital bed size and charges
An evaluation of the hospital bed size indicates significant variation in a patient presentation to these facilities, severity as well as the total cost of care. The mean cost of care was $9,573, $11,360 and $12,073 for small, medium and large hospitals respectively as seen in Fig. 3 below. The data also indicates a higher cost of care for similar severity or mortality risk at larger healthcare facilities compared to smaller facilities. Further evaluation of these facilities indicates low charges of $9,236, $11,381 and $14,747 for governmental, non-profits and private investment facilities respectively.
Fig. 3.
Mean charges by hospital size.
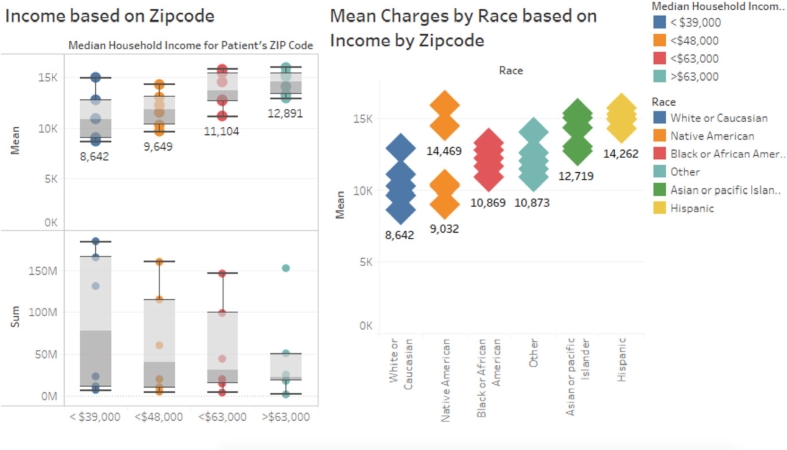
3.4. Charges by median household income based on zip code and race
The cost of care and patient presentation based on zip code and race shows patients from families with $38,000 or less income were more likely to present with pneumonia with 38% of total presentations. Household income of $48,000, $63,000, $63,000 plus showed a total of 25.9%, 20.4% and 15.7% presentations respectively. Although there has been a decrease in the patient presents for each income category, the mean cost of care shows over $2,000 increase on average in each income subset (P-0.00, R2 0.005). Mean charges for Hispanic and Native American population is higher than any other race as seen in Fig. 4. This trend could be seen in most regions and could be associated with higher severity and mortality risk at presentation. Fig. 4 also shows higher mean charges for higher household income; further analysis shows this is associated with a low patient population in that category.
Fig. 4.
Higher mean charges for higher household income.
4. Discussion
This analysis of nationwide data provides a unique perspective on the relationship between cost, age, and severity. The total cost of care for individuals younger than ten years old is about 10% less compared to older populations. Presentations with pneumonia were also more common in populations between 1 and 4 years old followed by newborns and infants; even though the maximum cost of care for these populations was the highest. An observation could be made that the cost of care varied significantly comparing the severity and stability of an individual before discharge. Mortality risk does not seem to show a significant impact on the mean cost of care comparing minor and major mortality risk with a mean cost of $11,652 and $11,541 respectively. As expected, the colder season or quarters showed a significant number of presentations between October to March; even though the mean cost did not show a significant difference in cost severity and mortality increases during these quarters.
This study shows that majority of presentations were of emergency room origin and had a significantly higher mean charge compared to non-emergency presentations. Patient presentations with emergency department records showed higher mean charges and total cost of care compared to the general population. Higher severity and mortality presentation risk could be attributed to race and population based on household income. These factors need to be addressed using public health strategies including educational approaches and resources allocation for the population that has difficulty accessing care. The findings indicate that some of these presentations could be treated in setting other than emergency and have successful outcomes. A comparison of the severity for these same population shows no statistical significance in increased severity for that non-emergent presentation. Individuals transferred to short term facilities made up the second largest population but also had low mean charges compared to other categories including routine discharge without the need for further care or observations.
This study shows that further analysis of treatment approaches, pharmaceutical interventions, and specification of the emergency facility is needed to better understand the various characteristics affecting the cost of care. Furthermore, a breakdown of cost by medications, diagnostic imaging, administrative cost would be essential in gaining a better understanding of the trends associated with the increase in the cost of care for these populations. An indication of specific procedures would aid in evaluating the effectiveness of protocols to treatment as well as the cost associated with them. The lack of outpatient cost information restricts a clear understanding of the total cost of care. Moreover, specific treatment protocols being adhered to during treatment could provide some information on cost increases in specific areas across the country. It could also aid in answer the question of cost or charge variation in comparing private for-profit healthcare facilities compared to others. Further studies on the dynamics of healthcare provision and cost in the South and West could aid in understanding the higher cost of care and high pneumonia presentation.
5. Conclusions
It is essential that the cost of care for pneumonia is thoroughly understood since it is one of the most common presentations in the pediatric population. A clear delineation of cost or charges broken down into various categories will be useful in providing a clearer picture of cost for pneumonia care in the United States. As shown in this study, the differences in charges by region could not be directly attributed to disease severity or mortality. More patients seek care at more extensive facilities and show no significant difference in morbidity or mortality based on hospital size. Individuals between the ages of 1–4 years old have presentation risk because of URI's followed by newborns and 5–9 years old. Higher cost attribution to the older population could be associated with high severity and presentation in all regions. Identification and understanding of cost influencers related to this diagnosis can aid in improving outcomes and cost reduction. Outcomes such as disease severity and mortality risk at presentation could decrease since cost influencers are directly related to patient health outcomes.
This study provides information on the various factors that impact cost across the country and the unique variances that exist based on geographic location. Furthermore, it provides information on the where resources should be allocated concerning addressing the issue of early presentation and treatment. Since age, LOS, ER records and severity are the most significant factor impacting cost addressing the issue at the community level could significantly impact cost and outcomes. Further studies on evaluating why some communities present with high severity and mortality risk is necessary for addressing this problem at a community level. Collaboration between healthcare organizational managers and community policymakers could aid in addressing issues of cost and outcome through an understanding of outcome and cost influencers as this study has shown.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
Contributor Information
Saanie Sulley, Email: ss2680@shp.rutgers.edu.
Memory Ndanga, Email: ndangame@shp.rutgers.edu.
Appendix 1. ICD-9-CM Exclusion Criteria
| Exclusion Criteria | Description | ICD-9-Code |
|---|---|---|
| Metastatic | Septic Arthritis | 711.X |
| CNS | 324.X | |
| Pericarditis | 420.X | |
| Endocarditis | 421.X | |
| Systemic | Acute Respiratory failure | 518.8X, 799.1 |
| Sepsis | 995.9X | |
| HUS | 283.11 | |
| Other (Local) | Abscess | 513.X |
| Immune Deficiency | 279.XX | |
| Meningitis | 320.XX |
References
- 1.World Health Organization. 26 12 2017. http://www.who.int/mediacentre/factsheets/fs331/en/ Accessed Monday December 2017.
- 2.Witt W.P., Weiss A.J., Elixhauser A. 2012. Overview of hospital stays for children in the United States. Statistical Brief# 187. [PubMed] [Google Scholar]
- 3.Jadavji T., Law B., Lebel M.H., Kennedy W.A., Gold R., Wang E.E. A practical guide for the diagnosis and treatment of pediatric pneumonia. CMAJ (Can Med Assoc J): Can Med Assoc J. 1997 Mar 1;156(5):703. [PMC free article] [PubMed] [Google Scholar]
- 4.Grijalva C.G., Nuorti J.P., Zhu Y., Griffin M.R. Increasing incidence of empyema complicating childhood community-acquired pneumonia in the United States. Clin Infect Dis. 2010 Mar 15;50(6):805–813. doi: 10.1086/650573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee G.E., Lorch S.A., Sheffler-Collins S., Kronman M.P., Shah S.S. National hospitalization trends for pediatric pneumonia and associated complications. Pediatrics. 2010 Aug 1;126(2):204–213. doi: 10.1542/peds.2009-3109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhutta Z.A., Das J.K., Walker N., Rizvi A., Campbell H., Rudan I. Interventions to address deaths from childhood pneumonia and diarrhoea equitably: what works and at what cost? Lancet. 2013 Apr 20;381(9875):1417–1429. doi: 10.1016/S0140-6736(13)60648-0. [DOI] [PubMed] [Google Scholar]
- 7.Wilson K.M., Torok M.R., Localio R., McLeod L., Srivastava R., Luan X. Hospitalization for community-acquired pneumonia in children: effect of an asthma codiagnosis. Hosp Pediatr. 2015 Aug 1;5(8):415–422. doi: 10.1542/hpeds.2015-0007. [DOI] [PubMed] [Google Scholar]
- 8.Zhang S., Sammon P.M., King I., Andrade A.L., Toscano C.M., Araujo S.N. Cost of management of severe pneumonia in young children: systematic analysis. J Glob Health. 2016 Jun;6(1) doi: 10.7189/jogh.06.010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li S.T., Trancredi D.J. Emphysema hospitalization increased in U.S children despite pneumococal conjucate vaccine. Pediatrics. 2010;125(1):26–33. doi: 10.1542/peds.2009-0184. [DOI] [PubMed] [Google Scholar]
- 10.American Lung Association . American Lung Association; Washington D. C: 2015. Trends in pneumonia and influenza. [Google Scholar]
- 11.Sato R., Rey G.G., Nelson S., Pinsky B. Community-acquired pneumonia episode costs by age and risk in commercially insured US adults aged≥ 50 years. Appl Health Econ Health Policy. 2013 Jun 1;11(3):251–258. doi: 10.1007/s40258-013-0026-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.American Thoracic Society . American Thoracic Society; New York: 2015. Top 20 pneumonia facts—2015. [Google Scholar]