Abstract
Background and Objective
Type 1 diabetes mellitus (T1DM) is the most frequent endocrinopathy in children. Its replacement therapy requires insulin, without which, death is inevitable. This treatment is expensive and a financial burden for diabetic children and their families, especially in Africa.
In the absence of a national T1DM register, the purpose of this study was to describe epidemiological aspects of type 1 diabetes in children in Gabon, specify the difficulties met by the patients during the follow-up and identify factors explaining poor therapeutic observance and metabolic control.
Material and methods
Prospective transversal monocentric study. Data were firstly extracted from the registers of the Endocrinology Department of the University Hospital of Libreville (CHUL), Gabon, between 2010 and 2017.
Secondly, patients were interviewed by telephone about the availability and cost of insulin, their self-monitoring of blood glucose, and diet.
Results
306 patients (154 girls and 152 boys) were diagnosed with T1D during the study period and followed-up in the Endocrinology Department at CHUL. Mean age at diagnosis was 17 ± 7 years (5% of patients were over 5 years of age, 30% were >20 years old). Mean follow-up period was 4.0 ± 2.0 years. 16% of the patients were hospitalized at least 2 times per month for ketoacidosis.
Hospital mortality was about 7%. Number of factors linked with poor therapeutic observance (high cost of treatment, lack of patients’ therapeutic education, etc.) were identified.
Conclusion
T1D prevalence is constantly increasing worldwide, but at slower pace in Africa in comparison to developed countries. Difficulties to access to high standard care and population poverty in Sub-Saharan Africa, represents a major independent factor of poor therapeutic observance.
1. Introduction
Type 1 diabetes is the most frequent endocrinopathy (International Diabetes Federation: IDF). It is a state of chronic hyperglycemia related to insulin deficiency, resulting from autoimmune destruction in insulin-secreting pancreatic beta cells, for which symptoms appear after 80% of the pancreatic cells are destroyed, including polyuria, polydipsia and signs of variable dehydration [1,2].
Type 1 diabetes (T1D) represents 5–10% of all diabetes according to the Padoa study et al. [1].
This number as well as the prevalence of type 1 diabetes has increased over the past three decades around the world, and Africa is no exception [1,[3], [4], [5], [6]]. For treatment requires costly substitutive insulin therapy making both the family and the patient in Africa bear this double burden related to the cost and outcome of this pathology [7].
Objectives of this work:
-
•
Describe the epidemiological aspects of type 1 diabetes in Gabon
-
•
Specify the difficulties encountered by the patients, during treatment and their experience of this pathology.
-
•
Examine the obstacles to correct medical adherence.
2. Method and means
First, the data for this work was collected from the consultation and hospitalization registries in the Endocrinology Services at the Libreville University Hospital in Gabon (CHUL).
Inclusion criteria: all patients between the ages of 1 and 30 years old, with type 1 diabetes, with a diagnosis selected according to ADA criteria (8), seen in consultation and/or hospitalized between April 2010 and December 2017 were eligible.
Exclusion criteria: all patients, whose information was incomplete, were excluded from our study (n = 306).
Secondly, the patients were contacted by telephone and responded to a questionnaire on the availability and the cost of insulin, the availability of blood sugar monitoring equipment, their understanding of the daily glucidic allocation in local food diets, the course of action in case of hypo- or hyperglycemia as well as their understanding of the adaptation rules regarding insulin doses. The goal was to investigate the obstacles to correct medical adherence.
Statistically-speaking, the differences were significant for P < 0,05.
3. Results
Over a period from April 2010 to September 2017, this interdisciplinary work made it possible to select 306 people, 154 girls (50.32%) and 152 boys (49.67%), seen in consultation or hospitalized for type 1 diabetes, e.g. a 1-to-1 sex ratio.
The average age at diagnosis was 17 ± 7 years (extremes: 1–30) and during evaluation was 20 ± 7 years.
The average length of treatment at CHUL was 4 years. Patients returned to the other provinces of Gabon where they lived before the discovery of their illness or a death occurred.
Morbidity, evaluated by the number of patients hospitalized at least twice a month, represents a rate of 16% and affected 40 patients in our study. The patients were always hospitalized for ketoacidosis due to incorrect medical adherence or a lack of insulin.
The mortality in our study was estimated at 7%, e.g. 22 deaths, approximately 4 years after the type 1 diabetes diagnosis, deaths occurred at the hospital. However, the number of deaths that occurred outside the CHUL is not known.
In addition, we lost touch with 22 patients (7%) from our study.
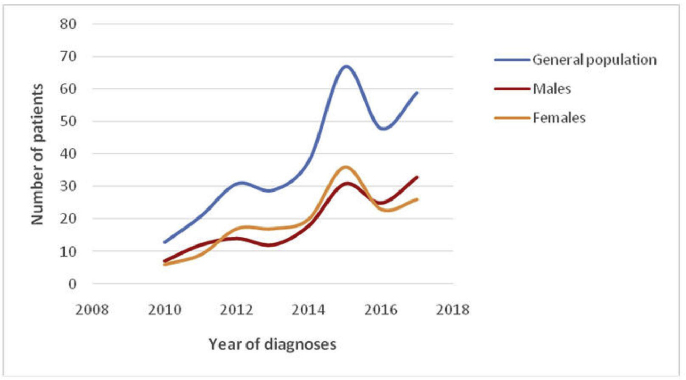
Comparisons of the previous data according to sex did not reveal statistically significant differences between men and women, whether it was in terms of the average age at the diagnosis of T1D, the evaluation age, the average length of treatment, or morbidity (Table 1), or in term of new ones per year (Fig. 2).
Table 1.
Comparison according to sex.
| Girls | Boys | P | |
|---|---|---|---|
| Average age at diagnosis (years) | 16 (7) | 16 (9) | na |
| Average age at diagnosis years) | 20 (7) | 19 (8) | na |
| Average length of care (years) | 3 (4) | 3 (4) | na |
| Median (extremes) | 2 (0–17) | 2 (0–16) | na |
| More than 2 hospitalizations per month | 21 (14%) | 18 (11%) | na |
| Deceased patients | 9 (7%) | 11 (7%) | na |
Fig. 2.
Number of diabetic patients per year, according to sex.
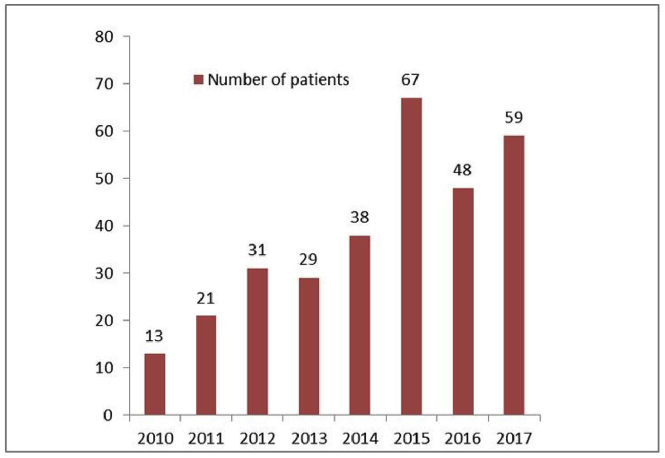
In our work, we observed an increase in the annual number of diabetics with a spike in 2015 with 67 new cases, versus 59 in 2017 (Fig. 1), leading to a number of T1D cases in Gabon that is equal to 3,4/100,000 inhabitants/year on 2015, but less in 2017 (2,9/100,000 inhabitants).
Fig. 1.
The number of diabetes per year, in patients under the age of 30.
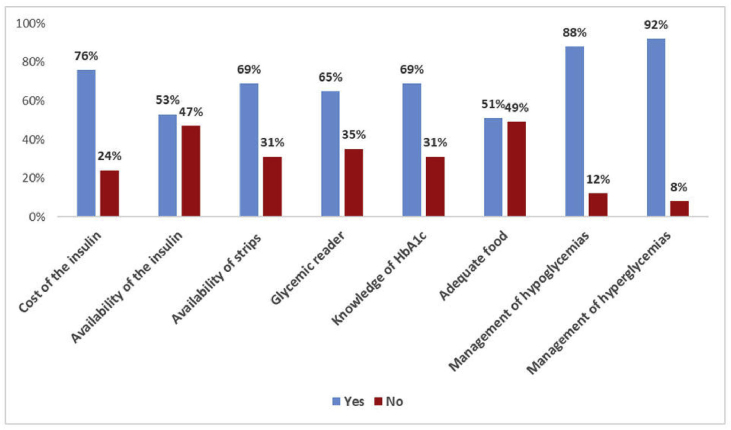
Analyzing the factors explaining poor metabolic balance as well as the obstacles to correct medical adherence (Fig. 3) reveals:
-
•
Regarding insulin, in 76% of the cases, its cost was an obstacle to medical adherence while in 53% of the cases it was its availability that was involved, inasmuch as pharmacies in rural zones do not always carry it.
-
•
Regarding at-home blood sugar monitoring equipment, 69% of patients say that they do not have blood sugar test strips while 65% did not have blood sugar meters at the time of this study, which makes it difficult to monitor blood sugar in order to better adapt the insulin doses to inject.
-
•
Regarding the adaptation of insulin doses, 92% of diabetics never carry out adaptations to their treatment alone according to their physical activity or blood sugar. The plan proposed by the endocrinologist will be applied until the next consultation.
-
•
In approximately 90% of cases, patients and/or their parents ignore treatment for hypo- or hyperglycemic situations.
Fig. 3.
Obstacles to correct medical adherence.
In addition to these factors directly related to the patient, the cost of treatment represents an enormous barrier to correct metabolic equilibrium [10]. Indeed, the fees related to treatment can, for certain patients, cause difficulties in terms of medical adherence. For example in outpatient care, the treatment of a 10-year-old diabetic, weighing 30 kg and receiving approximately 1U/kg/day of insulin, will represent 60% of the average monthly income for a family living with the minimum wage (USD 259.80) if this family is not affiliated to any health insurance plan, and 12% of this same salary, in case of social healthcare (Table 2). In case of hospitalization for this young boy, the parents would not be able to pay for hospitalization, insulin or the test strips afterwards, in the absence of health insurance. The fees related to hospitalization would represent 305% of the family's income (Table 3). Indeed, such a situation would favor the early onset of complications like renal, ocular or cardiovascular microangiopathies.
Table 2.
Cost of treatment in outpatient case.
| Medication | Monthly quantities | Monthly cost (USD) | CNAMGS reimbursements (health insurance) 80% (USD) | Cost for the patient 20% (USD) |
|---|---|---|---|---|
| Levemir (Detemir) | 1 pen | 21.56 | 17.25 | 4.31 |
| Novorapid | 2 pen | 31.32 | 24,36 | 6.96 |
| Blood sugar test strips | 3 box 50 |
103.27 | 82.61 | 20.65 |
| Needles Novo twists | 3 box | 1.04 | ||
| TOTAL | 157.19 | 125.75 | 31.92 | |
| Minimum wage (household income) USD 259.80 | 60% of the household's income | 12% of the household's income |
Table 3.
Cost of T1D treatment in Gabon, In outpatient care (10-year-old patient, weight = 30 kg).
| Medication | # of units per hospitalization | Monthly cost (USD) | CNAMGS reimbursements 80% (USD) | Cost for the patient 20% (USD) |
|---|---|---|---|---|
| SG 5% (500 ml) 3 | 3 | 11.43 | 9.15 | 2.28 |
| SG 10% (500 ml) 3 | 3 | 20.18 | 16.14 | 4.03 |
| Saline solution | 1.5 | 2.64 | 2.11 | 0.53 |
| Electrolytes | 4 boxes | 3.48 | 27.84 | 6.96 |
| Cost of 15 days in the hospital | 349.9 USD | 730.8 | 584.64 | 146.16 |
| TOTAL: % of monthly family income | 800.9 305% |
640.7 | 160.19 61% |
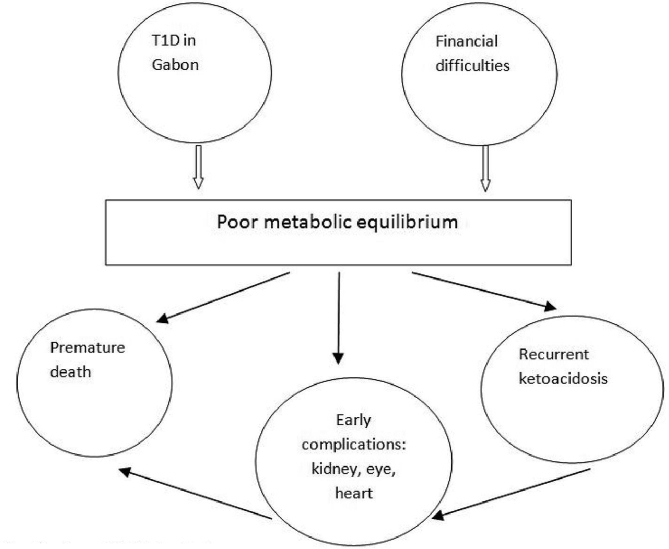
Following the financial depletion of their families, the patients present, approximately 4 years after the diagnosis of the illness, with a poor metabolic balance, resulting in recurrent ketoacidosis episodes, which result in premature death, approximately 4 years after the diagnosis of the illness (Fig. 4).
Fig. 4.
Evolution of T1D in Gabon.
4. Discussion
The number of cases of type 1 diabetes has been growing worldwide and Africa has not been spared. In Sudan, it went from 9.5/100,000 in 1991 to 10.3/100,000 inhabitants/year in 1995 [5]. This rate is higher than what we found in our study, which is 3,4/100,000 inhabitants per year (2015), and clearly more than that is observed in Tanzania and Ethiopia (1.5 and 2.1 for 100,000 inhabitants and per year, respectively) [3,7].
In sub-Saharan Africa, the number of type 1 diabetes cases experiences large variations [1,7,8] and there seems to be a gradient between industrialized countries and those in the midst of development, like is the case in Europe, between the northern and southern countries [9]. Indeed, northern countries have the highest number of cases.
The low number of cases observed in Africa could be related either to errors in diagnosing in hospitals, or to the death of patients before their arrival to a hospital establishment [8].
Our work focused on people who were no more than 30 years old. Contrary to us, the work conducted in Mozambique, the Sudan, Tanzania, Zambia, Kenya and Nigeria [1,9,10] focused on patients between the ages of 0–19 years old.
The average age of our patients upon diagnosis was 16 years old, below the average age of the South-African and Tanzanian series that was between 22 and 19.4 years [11], but older than the average age of populations profiled by Thomas Ngwiri et al., [5] which was 9.9. The patients from the Nigerian series seem younger upon diagnosis than in Gabon [8,10]. According to these observations, T1D is rarely profiled in Africa in children under 5 years old, as Ugege and Onyiriuka observed [8,12]. No scientific reason explains this observation. Therefore, we are wondering if these young children simply die prematurely due to severe dehydration?
In our study, there were as many men as women affected by T1D, results that are in accordance with those observed in other countries [1,5,8].
The likelihood of ketoacidosis occurring at the onset of diabetes varies considerably between 15% and 67%, from one country to another [12]. Our study did not assess the rate of ketoacidosis when diabetes was diagnosed.
According to the IDF, 50% of T1D die in the first five years after diagnosis [6]. However in Gabon, the average length of treatment is 3 (4 years). Compared to our results, the length of treatment in Durban, Johannesburg and Kenya is 3.8 years, 4 years and 3.7 years, respectively [5,11]. The life expectancy of diabetics in Africa is lower than that observed in Pennsylvania, which is 32 years +7 years [13]. Improving the supply of care in developing countries would increase the life expectancy of these patients [[14], [15], [16]].
In Tanzania, the mortality rate (41%) is strongly above that which we observed in our study (7%). This difference could be explained by an under-estimation of our figures related to the vast mobility of populations across the country and due to the absence of national identity registries, in which all deaths would be mentioned. Ketoacidosis and kidney disease are the most common causes of death [12,16,17].
Besides the daily limitations that T1D creates, the majority of patients encounter significant financial problems, which causes incorrect medical adherence. Indeed, a family who lives in Gabon, with the lowest salary and not having any social coverage, spends 60% of its monthly income on outpatient treatment for a diabetic child. If this youth is hospitalized for 15 days, the fees are much higher than the family's income (Table 3). In Malawi, 1 month of insulin treatment corresponds to 19.6 days of income for an employee while in the Sudan, a family with a diabetic child, spends 36% of its budget for healthcare (1). Overall, diabetes is a costly disease (1) as well as a purveyor of complications and early deaths in Gabon, (Fig. 4). In Mali, diabetes treatment accounts for 70% of the patient's income, making it difficult to adhere to treatment [[16], [17], [18], [19], [20]], as well as in developing countries, where poverty is a major barrier to the management of chronic diseases [21].
Excluding the financial issues, we have identified other factors related to incorrect medical adherence and metabolic imbalances, specifically the absence of blood sugar monitoring equipment and the ignorance regarding treatment in emergency situations. Thus, 88–92% of patients from our study say that they do not know how to treat hypo- or hyperglycemias according to the international recommendations. In addition, 92% of our patients do not know anything about adapting insulin doses, essential for example, before physical activity (Fig. 3). We did not find any literature on therapeutic patient education in order to empower patients, reduce the frequency of hospitalizations, the numerous complications and, consequently, mortality.
This study made it possible to establish the number of T1D cases in Gabon's youth and reveal the difficulties encountered by patients in their experience of the illness, specifically the limited financial resources causing recurrent episodes of ketoacidosis, as well as the obstacles to correct medical adherence. Some authors have shown that the free access to treatment in Cameroon makes it possible for diabetics to improve their metabolic equilibrium, reduce the number of hypoglycemic cases as well as the number of ketoacidosis episodes [22].
This work should lead to proposals addressed:
-
•
To the government: for the implementation of a health insurance system, fully reimbursing the fees related to diabetes.
-
•
To patients: learn how to eat a balanced diet and understand the glucidic provision in local foods.
-
•
To healthcare personnel: both physicians and paramedics who should receive regular continuing education, in order to educate patients on their treatment In order to make up for the lack of doctors and nurses qualified to manage diabetes, as suggested by Choukem and colleagues [23], staff capable of setting up programme that meet the needs of Africa.
5. Conclusion
Type 1 diabetes is a chronic illness, less frequent in Africa than in developed countries, but one that is still growing. Its treatment is costly in Africa, since populations also face financial difficulties. Health authorities must implement measures in order to improve the day-to-day lives and treatment of patients in order to reduce the outcomes related to this disease.
Lastly, further studies carried out over the entire territory prove to be necessary in order to determine the actual number of cases and mortality as well as T1D complications in Gabon.
Conflict of interest
We have no interest conflicts to declare.
Ethical statement
The ethical statement of university hospital of Libreville, says that we did not need any authorization because it was not an interventional survey.
Acknowledgments
Mrs. Modo Lydie, nurse in the CHUL's endocrinology services, for her availability and diligence in communicating to us the necessary information for this work.
Mrs. Flore NzéEyéghéMba, archivist, for her precious help.
Dr. Franck Chambrier, pharmacist, for his availability and the information provided.
Centre Hospitalier d’Arras, for its help in writing this work.
Footnotes
Peer review under responsibility of King Faisal Specialist Hospital & Research Centre (General Organization), Saudi Arabia.
References
- 1.Padoa C.J. The epidemiology and pathogenesis of type 1 diabetes mellitus in Africa. J Endocrinol Metabol Diabetes S Afr. 2011;16(3):130–136. [Google Scholar]
- 2.Khardori R. Type 1 Diabetes Mellitus: Practice Essentials, Background, Pathophysiology. Medscape. 2018 [Google Scholar]
- 3.Hall V., Thomsen R.W., Henriksen O., Lohse N. Diabetes in Sub Saharan Africa 1999-2011: epidemiology and public health implications. A systematic review. BMC Public Health. 2011 Dec;11(1):564. doi: 10.1186/1471-2458-11-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wild S., Roglic G., Green A., Sicree R., King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004 May 1;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 5.Ngwiri T., Were F., Predieri B., Ngugi P., Iughetti L. Glycemic control in Kenyan children and adolescents with type 1 diabetes mellitus. Int J Endocrinol. 2015;2015 doi: 10.1155/2015/761759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atlas de la Fédération internationale du Diabète. eighth ed. 2017. pp. 16–60. [Google Scholar]
- 7.Amiri M., Hosseini S.M., Maghsoudi R. Diabetes mellitus type 1; is it a global challenge. Acta Epidemioendocrinologica. 2016 May 23;1(1) [Google Scholar]
- 8.Ugege O., Ibitoye P.K., Jiya N.M. Childhood diabetes mellitus in sokoto, north-western Nigeria: a ten year review. Sahel Med J. 2013 Jul 1;16(3):97. [Google Scholar]
- 9.Lévy-Marchal C, Fagot-Campagna A, Daniel M. Surveillance épidémiologique du diabète de l'enfant (Doctoral dissertation, Institut national de la santé et de la recherche médicale (INSERM)).
- 10.Umar U.I. Pattern of presentation of Type 1 diabetic patients in Kano, Nigeria. Nigerian J Basic Clin Sci. 2016 Jul 1;13(2):85. [Google Scholar]
- 11.Mbanya J.C., Motala A.A., Sobngwi E., Assah F.K., Enoru S.T. Diabetes in sub-saharan africa. Lancet. 2010 Jun 26;375(9733):2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- 12.Onyiriuka A.N., Ifebi E. Ketoacidosis at diagnosis of type 1 diabetes in children and adolescents: frequency and clinical characteristics. J Diabetes Metab Disord. 2013 Dec;12(1):47. doi: 10.1186/2251-6581-12-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Secrest A.M., Becker D.J., Kelsey S.F., LaPorte R.E., Orchard T.J. All-cause mortality trends in a large population-based cohort with long-standing childhood-onset type 1 diabetes: the Allegheny County type 1 diabetes registry. Diabetes Care. 2010 Dec 1;33(12):2573–2579. doi: 10.2337/dc10-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Motala AA, Esterhuizen T, Gouws E, Pirie FJ, Omar MA. Diabetes and other disorders of glycemia in a rural South African community; Prevalence and associated risk factors. pp1-10. [DOI] [PMC free article] [PubMed]
- 15.Wherrett D., Huot C., Mitchell B., Pacaud D. Le diabète de type 1 chez les enfants et les adolescents. Can J Diabetes. 2013;37:188–198. doi: 10.1016/j.jcjd.2013.01.042. S531-S541. [DOI] [PubMed] [Google Scholar]
- 16.Beran D., Yudkin J.S. Diabetes care in sub-Saharan Africa. Lancet. 2006 Nov 11;368(9548):1689–1695. doi: 10.1016/S0140-6736(06)69704-3. [DOI] [PubMed] [Google Scholar]
- 17.Asao K., Sarti C., Forsen T., Hyttinen V., Nishmura R., Matsushima M. Long-term mortality in nationwide cohorts of childhood-onset type 1 diabetes in Japan and Finland. Diabetes Care. 2003;26:2037–2042. doi: 10.2337/diacare.26.7.2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Assar S., Riahi K., Bashirnezhad S., Yazdanpanah L., Latifi S.M. The relationship between metabolic control and growth in children with type I diabetes mellitus in Southwest of Iran. Scientifica. 2015;2015 doi: 10.1155/2015/917542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kalk W.J., Raal F.J., Joffe B.I. The prevalence and incidence of and risk factors for, micro-albuminuria among urban Africans with type 1 diabetes in South Africa: an inter-ethnic study. Int J Diab Mellitus. 2010 Dec 1;2(3):148–153. [Google Scholar]
- 20.Virk S.A., Donaghue K.C., Cho Y.H., Benitez-Aguine P., Hiny S., Pryke A. Association between HbA1c variability and risks of microvascular complications in adolescents with type 1 diabetes. JCEM. 2016:3257–3263. doi: 10.1210/jc.2015-3604. [DOI] [PubMed] [Google Scholar]
- 21.Doubi S., El Ouahabi H., Dakkar O., Ajdi F. L’évaluation d’un programme d’éducation thérapeutique chez le patient diabétique dans un Centre Hospitalier Universitaire marocain: resultats péliminaires d’une enquête pilote. Pan Afr Med J. 2014;18:258. doi: 10.11604/pamj.2014.18.258.3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lontchi-Yimagou E., Mapa-Tassou C., Dehayem M.Y., EssiM J., Saji J., Sobngwi E. The effect of free diabetes care on metabolic control and on health-related quality of life among youths with type 1 diabetes in Cameron. BMJ Open Diab Res Care. 2017;5 doi: 10.1136/bmjdrc-2017-000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choukem S.P., Mbanya J.C. vol. 6. Thelancetgh; April 2018. (Diabetes Academy Africa: training the next generation of researchers in sub-Saharan African). [DOI] [PubMed] [Google Scholar]