Abstract
Introduction:
According to the World Health Organization, more than 300 million people were estimated to suffer from depression in 2017. Many studies have observed that medical personnel have a higher level of depression, but studies among dentists are scarce. Early diagnosis will help in controlling the morbidity and mortality due to depression. Hence, this study was undertaken to estimate the prevalence of depression among students of Government Dental College (GDC), Thiruvananthapuram, the capital city of the state of Kerala, India.
Materials and Methods:
A cross-sectional study was conducted at GDC, Thiruvananthapuram, for a period of 3 months from September to December 2017, using the Patient Health Questionnaire-9 (PHQ-9) and a pro forma comprising 37 questions. Students having PHQ scores >9 were considered to have depression. The questionnaire was administered on 364 students comprising undergraduate students, paradental students, house surgeons, and postgraduates. Separate sessions were arranged for each group and four reminders were given.
Results:
The prevalence of depression was estimated as 26.9% (95% confidence interval: 22.4–31.8). Being married, having high and average level of course satisfaction, and having close friends were found to act as independent protective factors, whereas female gender and breakups in relationships were found to be independent risk factors.
Conclusion:
It is high time we provide supportive programs and implement preventive measures to help professional students, especially those who are at higher risk of mental ill-health. Further studies need to be conducted to explore the academic reasons for depression.
Keywords: Dental students, depression, Kerala, prevalence
INTRODUCTION
Mental conditions account for 12.3% of disability-adjusted life years and 31% of all years lived with disability at all ages.[1] According to the latest estimates from the WHO, >300 million people are now living with depression, an increase of >18% between 2005 and 2015.[2]
Many medical students having been toppers in their school get a shock, finding themselves in the bottom of the class in medical college. Long study hours, inadequate sleep, and standing for hours learning the clinical skills may lead to social isolation, mental fatigue, and depression.[3] The global prevalence of depression among medical students was found to be 28%.[4]
Dentists encounter numerous sources of professional stress, beginning in dental school. This stress can have a negative impact on their personal and professional lives. Recognizing depression at an early stage is critical for reducing suicidal deaths and deliberate self-harm. There exist little reliable data that portray depression among dentists.[5,6] Hence, this study aims to estimate the prevalence of depression among students of Government Dental College, Thiruvananthapuram (GDCT) in Kerala, India.
MATERIALS AND METHODS
This cross-sectional study was conducted at GDCT for a period of 3 months. The sample size was calculated as 223 using the formula for prevalence studies, with 95% confidence level and 5% absolute precision, taking P as 16.7, the proportion of dental students suffering from depression in a previous study done in the United States.[6]
For the want of this study being beneficial to all students, we conducted a census type of study, involving undergraduates, dental auxiliary students (dental hygienist [DH] students, dental mechanic students, and dental operating room assistant [DORA]), house surgeons (HSs), and postgraduate students (PGs), giving a total of 364 respondents. Those students who have not given written informed consent and failed to respond even after four repeated reminders were excluded from the study.
Data were collected using a validated tool – the Patient Health Questionnaire-9 (PHQ-9) using criteria from the Diagnostic and Statistical Manual of Mental disorder IV. PHQ-9 has an average sensitivity of 0.77 and specificity of 0.94 that suggests good validity in populations who are generally not depressed.[7] A structured pretested pro forma comprising 37 questions was used to determine the factors associated with depression.
Self-administered questionnaire in the English language was given to the study participants. Students who were absent on the specific day of data collection of their batch were provided an additional session on a later date.
Clearance was obtained from the Institutional Ethics Committee, GDCT. Those students screened positive for depression were personally contacted and advised expert care from the Department of Psychiatry, Government Medical College, Thiruvananthapuram.
Data were entered in Microsoft Excel and were analyzed using SPSS (Statistical Package for the Social Sciences) trial version 18 (IBM).
RESULTS
Those students with a PHQ-9 score of 10 or above were considered positive for depression. The overall prevalence of depression was estimated as 26.9% (95% confidence interval of 22.4–31.8) [Figure 1].
Figure 1.
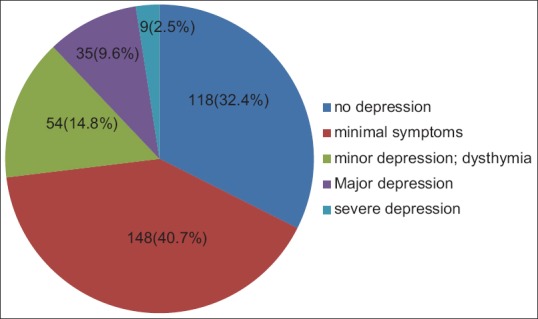
Figure depicting the prevalence of depression
The mean age of the study participants was 22.62 years (3.29). Fifteen (20.8%) of 72 males and 83 (28.4%) of 292 females were screened positive for depression.
The study participants included 48 first-year students, 43 second-year students, 51 third-year students, 41 HSs, and 65 PGs. Among paradental course students, there were 26 DH students, 8 DORA students, and 11 dental mechanic students. Ten first-year students, 25 second-year students, and 8 and 21 students from the third and final years were screened positive for depression. Twelve HSs, 16 PGs, 3 DH, and 3 DORA were also screened positive for depression. Of the 63 students who had residential schooling, that is, a history of studying in boarding schools, 23 had depression and 4 had severe depression.
Chi-square test was done to find the association between depression and various sociodemographic characteristics [Tables 1 and 2]. Binary logistic regression was used to determine the independent factors associated with depression [Table 3]. Females and those who had breakups in the relationship were found to be more likely to have depression. Marital status, high or average level of satisfaction in dentistry, and having close friends act as protective factors.
Table 1.
Association of various sociodemographic characteristics of the study respondents with depression
| Variable | Depression, n (%) | No depression | P | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| Gender | ||||||
| Male** | 15 (15.3) | 57 (21.4) | 0.193 | 1.509 | 0.809 | 2.814 |
| Female* | 83 (84.7) | 209 (78.6) | ||||
| Hostler | ||||||
| Yes* | 68 (69.4) | 180 (67.7) | 0.755 | 1.083 | 0.656 | 1.786 |
| No** | 30 (30.6) | 86 (32.4) | ||||
| Religion | ||||||
| Hindu* | 59 (60.2) | 150 (56.4) | 0.514 | 1.169 | 0.729 | 1.876 |
| Christian** | 14 (14.3) | 45 (16.9) | ||||
| Muslim** | 25 (25.5) | 71 (26.7) | ||||
| TOF | ||||||
| Nuclear* | 89 (29.3) | 9 (15) | 0.048* | 2.346 | 1.108 | 4.968 |
| Nonnuclear** | 215 (70.3) | 51 (85) | ||||
| Marital status | ||||||
| Married* | 8 (8.2) | 45 (16.9) | 0.036* | 0.437 | 0.198 | 0.963 |
| Unmarried** | 90 (91.8) | 221 (83.1) | ||||
*P<0.05 statistically significant, **Reference category. TOF: Type of family, BO: Birth order, OR: Odds ratio, CI: Confidence interval
Table 2.
Association of personal and educational characteristics with depression using Chi-square test
| Variable | Depression, n (%) | No depression, n (%) | P | OR | 95% CI | |
|---|---|---|---|---|---|---|
| Lower limit | Upper limit | |||||
| Belief in god | ||||||
| Believer* | 86 (87.8) | 244 (91.7) | 0.204 | 0.617 | 0.291 | 1.307 |
| Nonbeliever | 6 (6.1) | 15 (5.6) | ||||
| Confused | 6 (6.1) | 7 (2.7) | ||||
| Diet | ||||||
| Vegetarian* | 2 (2) | 14 (5.3) | 0.183 | 0.375 | 0.084 | 1.681 |
| Eggetarian | 5 (5.1) | 9 (3.4) | ||||
| Nonvegetarian | 91 (95.8) | 243 (31.4) | ||||
| Tobacco | ||||||
| Yes* | 0 (0) | 3 (1.1) | 0.291` | 1.373 | 1.289 | 1.462 |
| No | 91 (92.9) | 260 (97.7) | ||||
| Used to now quit | 7 (7.1) | 3 (1.1) | ||||
| Alcohol | ||||||
| Yes* | 2 (2) | 8 (3) | 0.617 | 0.672 | 0.140 | 3.220 |
| No | 94 (95.9) | 253 (95.1) | ||||
| Used to now quit | 2 (2) | 5 (1.9) | ||||
| Narcotics | ||||||
| Yes* | 2 (2) | 1 (0.4) | 0.119 | 5.521 | 0.495 | 61.578 |
| No | 96 (98) | 265 (99.6) | ||||
| Participation in sports | ||||||
| Yes* | 24 (25.5) | 93 (35) | 0.058 | 0.603 | 0.357 | 1.020 |
| No | 74 (75.5) | 173 (65) | ||||
| Close friends | ||||||
| Yes* | 67 (68.4) | 221 (83.1) | 0.002* | 0.440 | 0.258 | 0.750 |
| No | 31 (31.6) | 45 (16.9) | ||||
| Breakups | ||||||
| Yes* | 24 (24.5) | 37 (18.1) | 0.017* | 2.007 | 1.128 | 3.573 |
| No | 74 (75.5) | 229 (36.9) | ||||
| Use of social networks | ||||||
| Yes* | 81 (82.7) | 220 (82.7) | 0.990 | 0.996 | 0.540 | 1.837 |
| No | 17 (17.3) | 46 (17.3) | ||||
| Residential schooling | ||||||
| Yes* | 23 (23.5) | 40 (15) | 0.059 | 1.733 | 0.974 | 3.081 |
| No | 75 (76.5) | 226 (85) | ||||
| Level of satisfaction | ||||||
| High or average* | 81 (82.6) | 248 (93.9) | 0.001* | 0.307 | 0.149 | 0.636 |
| Others | 17 (17.3) | 16 (6.1) | ||||
*Significance. OR: Odds ratio, CI: Confidence interval
Table 3.
The determinants of depression: Binary logistic regression
| Determinants | P | Adjusted OR (B) | 95% CI | |
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Gender | 0.007* | 2.558 | 1.287 | 5.086 |
| Marital status | 0.012* | 0.344 | 0.149 | 0.795 |
| Close friends | 0.001* | 0.380 | 0.214 | 0.675 |
| Breakups | 0.003* | 2.597 | 1.389 | 4.858 |
| Level of satisfaction | 0.000* | 0.233 | 0.106 | 0.512 |
*Significance. Cox and snell R2=0.10. OR: Odds ratio, CI: Confidence interval
DISCUSSION
Numerous studies all over the world have shown that psychological morbidity is increasing among medical students.[8,9,10] Dentistry is a mix of knowledge, skill, and perseverance. Hence, dentistry requires a lot of skillful talents, overloaded with facts. This may have unintended negative consequences with respect to students' mental and physical health. To the best of our knowledge, this study is the first of its kind in Kerala in estimating the prevalence of depression among dental students. Hence, we decided to conduct this depression screening for its early detection and to take appropriate measures to ensure the mental health of dental professionals.
The revalence of depression in our study was 26.9%. A systematic review to estimate the prevalence of depression among university students found it to be 33%.[3] This sheds light on the fact that the prevalence of depression is reasonably high everywhere, and our figure is not much different.
In our study, minor depression and dysthymia account for 14.8%, major depression for 9.8% and severe depression for 2.5%. Depression was more among final and second years as compared to the first and third years. Among all the years of BDS curriculum, final year may be more stressful with postings in seven departments and practical sessions. While reaching the second year, they are exposed to a strong professional environment and the going gets tough along with the work burden. Third year as is often called, the Honeymoon period of BDS is a bit relaxing with only 3 subjects to study, may have reduced the depression among these students. The first-year students are interested in exploring their new life and are yet to understand dentistry which might have given a low value among them. This shows that the year of study plays an important role in increasing depression among students, with probable attributions from the academic and nonacademic factors.
Most of our respondents (77%) had opted for a BDS seat as they were not able to get an MBBS seat. This might be one of the reasons for depression among dental students. They may develop passion toward the subject in the later stage but the thought of not getting MBBS may haunt a few.
Among 41 HSs, 13 had depression. The high competition in the PG entrance examinations and the highly unpredictable future of dentistry might have contributed to depression. Among 65 PGs, 16 had depression and 28 had shown minimal symptoms of depression. Stress during postgraduation period is inevitable, and many of them find it difficult to balance personal and professional life.
The prevalence of depression among females is 28.4% and that of males is 20.8%. The high prevalence of depression among females is evident in similar studies in Ethiopia, West Bengal, and the US.[6,11,12,13] Our study has shown that breakups and marital status were significantly associated with depression. The way the society looks at unmarried women after 25 might have contributed to depression, as depression is seen more among unmarried women in our study.
Our study has shown a near significant association between residential schooling and depression in bivariable analysis but not in multivariable analysis. Various studies have proven that higher rates of conduct disorder, anxiety, attention deficit, and depression are seen in children who had residential schooling, and there exist greater at-risk factors in this group.[14,15,16]
Our study has shown that the level of satisfaction in dentistry and depression show a statistically significant association. Studies in various health-care settings have shown that the severity of psychological distress is negatively associated with job satisfaction.[17]
Those students who had breakups in their relationships were found to have more depression than others in our study. Various studies have shown that women have high rejection sensitivity and were more depressed when they experienced a breakup. Breakup distress scale scores reported that sudden and unexpected breakups have made them feel rejected and betrayed and were not willing to start a new relationship.[18]
Various documents have shed light on the fact that having a friend to whom one can disclose everything can reduce depression to a great extent.[19,20] The most commonly cited advantage of having a close friend was social support including emotional support, giving them an opportunity to offload the burden associated with depression.[19]
CONCLUSION
This study brings forth the considerable prevalence of depression among dental students. As exposure to stress and other risk factors of depression are increasing, the chance of an increase in the prevalence of depression will be more in the coming years. As a first step in depression control, dental schools should set up counseling cells, student helplines, accessible round the clock through phone calls, chats or mobile applications that may help those needy students undergoing emotional turmoil due to breakups, or other mental stress. An induction assessment should be performed in the first year of study itself to identify those students with a low level of satisfaction in obtaining the BDS seat and they should be provided adequate care. Activities promoting healthy friendships should be encouraged, and efforts should be undertaken to incorporate such activities in the curriculum itself.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: Results from the world health surveys. Lancet. 2007;370:851–8. doi: 10.1016/S0140-6736(07)61415-9. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Depression. Media Centre. Fact Sheets. World Health Organization; 2017. [Last accessed on 2018 Mar 24]. Available from: http://www.who.int/mediacentre/factsheets/fs369/en/ [Google Scholar]
- 3.Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: A meta-analysis. Med Educ. 2016;50:456–68. doi: 10.1111/medu.12962. [DOI] [PubMed] [Google Scholar]
- 4.Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. 2015;141:354–7. doi: 10.4103/0971-5916.156571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rahsenas N, Motamedi M. Do dentists who are artists have less stress, anxiety and depression than those who are not? Int J Emerg Ment Health Hum Resil. 2015;17:530–2. [Google Scholar]
- 6.Laurence B, Williams C, Eiland D. Depressive symptoms, stress, and social support among dental students at a historically black college and university. J Am Coll Health. 2009;58:56–63. doi: 10.3200/JACH.58.1.56-63. [DOI] [PubMed] [Google Scholar]
- 7.Pinto-Meza A, Serrano-Blanco A, Peñarrubia MT, Blanco E, Haro JM. Assessing depression in primary care with the PHQ-9: Can it be carried out over the telephone? J Gen Intern Med. 2005;20:738–42. doi: 10.1111/j.1525-1497.2005.0144.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahola K, Hakanen J. Job strain, burnout, and depressive symptoms: A prospective study among dentists. J Affect Disord. 2007;104:103–10. doi: 10.1016/j.jad.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 9.Al-Sowygh ZH. Academic distress, perceived stress and coping strategies among dental students in Saudi Arabia. Saudi Dent J. 2013;25:97–105. doi: 10.1016/j.sdentj.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Agrawal N, Sharma S, Meena R, Uppadhaya SK, Mittal M. Prevalence of Depression and its Associated Factors among Students of a Medical College in Western Rajasthan. [Last accessed on 2018 Jun 02];Ntl J Community Med. 2017 8:12–16. Available from: http://www.njcmindia.org/home/download/973 . [Google Scholar]
- 11.Tilahune AB, Bekele G, Mekonnen N, Tamiru E. Prevalence of unrecognized depression and associated factors among patients attending medical outpatient department in Adare hospital, Hawassa, Ethiopia. Neuropsychiatr Dis Treat. 2016;12:2723–9. doi: 10.2147/NDT.S118384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brondani MA, Ramanula D, Pattanaporn K. Tackling stress management, addiction, and suicide prevention in a predoctoral dental curriculum. J Dent Educ. 2014;78:1286–93. [PubMed] [Google Scholar]
- 13.Chaudhuri SB, Mandal PK, Chakrabarty M, Bandyopadhyay G, Bhattacherjee S. A study on the prevalence of depression and its risk factors among adult population of Siliguri subdivision of Darjeeling district, West Bengal. J Family Med Prim Care. 2017;6:351–5. doi: 10.4103/jfmpc.jfmpc_326_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilman SE, Kawachi I, Fitzmaurice GM, Buka L. Socio-economic status, family disruption and residential stability in childhood: Relation to onset, recurrence and remission of major depression. Psychol Med. 2003;33:1341–55. doi: 10.1017/s0033291703008377. [DOI] [PubMed] [Google Scholar]
- 15.Mattison R. Four-year predictive value of the children's depression inventory. Am Psychol Assoc. 1990;2:169–74. [Google Scholar]
- 16.Silver SE, Duchnowski AJ, Kutash K, Friedman RM, Eisen M, Prange ME, et al. A comparison of children with serious emotional disturbance served in residential and school settings. J Child Fam Stud. 1992;1:43–59. [Google Scholar]
- 17.Martin A, Sanderson K, Cocker F. Meta-analysis of the effects of health promotion intervention in the workplace on depression and anxiety symptoms. Scand J Work Environ Health. 2009;35:7–18. doi: 10.5271/sjweh.1295. [DOI] [PubMed] [Google Scholar]
- 18.Drapeau S, Gagné MH, Saint-Jacques MC, Lépine R, Ivers H. Post-separation conflict trajectories: A longitudinal study. Marriage Fam Rev. 2009;45:353–73. [Google Scholar]
- 19.Griffiths KM, Crisp DA, Barney L, Reid R. Seeking help for depression from family and friends: A qualitative analysis of perceived advantages and disadvantages. BMC Psychiatry. 2011;11:196. doi: 10.1186/1471-244X-11-196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sandoui A. Strong friendships in adolescence may benefit mental health in the long run. Medical News Today. 2017 Aug 26; [Google Scholar]


