Abstract
Introduction
HTX-019 [CINVANTI® (aprepitant injectable emulsion)] is a neurokinin 1 receptor antagonist (NK-1 RA) approved as a 30-min infusion for preventing acute and delayed chemotherapy-induced nausea and vomiting. HTX-019 has been generally well tolerated when administered as a 30-min infusion or 2-min injection [intravenous (IV) push] in healthy subjects. This real-world analysis assesses safety of HTX-019 via IV push in patients with cancer and addresses a recent IV bag shortage.
Methods
This retrospective review involved six sites in Alabama, USA. Analyzed patients were 18–94 years old with an Eastern Cooperative Oncology Group performance status ranging from 0 to 4. Seventy-six chemotherapy regimens were utilized (emetogenicity high, n = 35; moderate, n = 35; low, n = 6) and patients received HTX-019 130 mg only or switched from fosaprepitant 150 mg to HTX-019 130 mg within a three-drug antiemetic regimen with a 5-hydroxytryptamine type 3 RA and dexamethasone. HTX-019 was administered via IV push. Electronic medical records of patients receiving HTX-019 were queried for nursing and medical documentation associated with infusion-site adverse events (ISAEs). The detailed notes were also reviewed for any discontinuation of HTX-019 or substitution of HTX-019 with another NK-1 RA.
Results
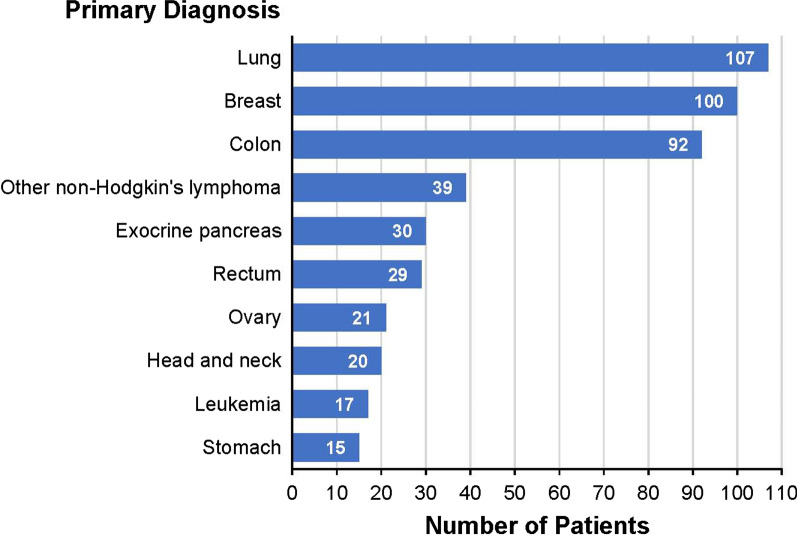
The HTX-019 safety profile was analyzed on the basis of 2066 IV push administrations in 591 cancer patients (most common diagnoses: lung, n = 107; breast, n = 100; colon, n = 92). No clinically significant ISAEs or adverse events associated with HTX-019 were reported. Also, no patients discontinued HTX-019 treatment, and none switched from HTX-019 to another NK-1 RA.
Conclusion
This is the first study to demonstrate that HTX-019 can be safely administered via IV push in patients with cancer receiving emetogenic chemotherapy while negating the need for fluid bags, which are scarce.
Funding
Heron Therapeutics, Inc., San Diego, CA, USA.
Plain Language Summary
Plain language summary available for this article.
Keywords: Aprepitant, CINVANTI, Fosaprepitant, HTX-019, IV push, NK-1 RA
Plain Language Summary
This study assessed the use of the drug HTX-019 to prevent a common side effect of chemotherapy, known as chemotherapy-induced nausea and vomiting (CINV) in patients being treated for cancer. HTX-019 was recently approved to be given as a 30-min infusion for CINV prevention. Earlier studies in healthy subjects showed that HTX-019 is safe when given as a 30-min infusion or 2-min injection. This study reviewed charts of patients with cancer and analyzed the safety of HTX-019 given as a 2-min injection. This method of delivering HTX-019 was very safe, with no adverse effects reported in over 2000 injections given to nearly 600 patients. These findings also address a recommendation by the American Society of Health-System Pharmacists to use short injections as an alternative method of giving a drug to prevent CINV.
Introduction
Aprepitant is a substance P neurokinin 1 receptor antagonist (NK-1 RA), used in combination with other antiemetics as part of guideline-recommended regimens for the prevention of acute and delayed chemotherapy-induced nausea and vomiting (CINV) in patients with cancer receiving highly emetogenic (HEC) or moderately emetogenic chemotherapy (MEC) [1–4]. In 2008, an intravenous (IV) formulation using the more water-soluble prodrug fosaprepitant (EMEND for injection) was approved in the USA for CINV prevention in combination with other antiemetics [5]. However, even with increased solubility, fosaprepitant still required the surfactant polysorbate 80 [6], which has been associated with hypersensitivity reactions (HSRs) and infusion-site adverse events (ISAEs) [7–13]. In patients treated with fosaprepitant, these reactions include infusion-site pain (in 97% of patients), erythema (42%), swelling (33%), venous hardening/induration (31%), and phlebitis or thrombophlebitis (17%) [13]. The US prescribing information for fosaprepitant now contains warnings about both HSRs (including anaphylaxis and anaphylactic shock) and ISAEs (including thrombophlebitis, necrosis, and vasculitis) [5].
Given the safety issues associated with fosaprepitant, a new aprepitant IV surfactant-free injectable emulsion, HTX-019 (CINVANTI®), was recently approved for the prevention of acute and delayed CINV, in combination with other antiemetics, in adult patients with cancer receiving HEC (130 mg) or MEC (100 mg), and is infused over 30 min [14]. The present National Comprehensive Cancer Network (NCCN) guidelines list HTX-019 as a category 1 recommendation for HEC and MEC, both using the 130 mg IV dose [3]. This approval was based on two bioequivalence studies of single-dose infusions of HTX-019 130 mg and fosaprepitant 150 mg [15, 16]. Overall, the proportion of subjects who reported any treatment-emergent adverse events (TEAEs) and the number of TEAEs were lower with HTX-019 130 mg 30-min infusion than with fosaprepitant 150 mg 30-min infusion (21% versus 28%) [15] and fosaprepitant 150 mg 20-min infusion (13% versus 30%) [16]. In addition, a pooled analysis showed that the proportion of subjects with treatment-related TEAEs was lower with HTX-019 130 mg (13%) than with fosaprepitant 150 mg (28%) treatment [16].
A recent acute shortage of IV fluids and bags, as well as the desire to reduce administration and patient chair times, has prompted a need to administer small-volume parenteral solution products as short injections (over 5 min or less) [17]. The present retrospective review analyzes the safety profile of HTX-019 via a 2-min injection (IV push) and is the first to evaluate the relative safety of HTX-019 in patients with cancer.
Methods
This retrospective review was undertaken, from late January through early May 2018, at the Clearview Cancer Institute at six sites in Alabama, USA: three community-based oncology centers and three follow-up offices. As a result of the normal saline shortage at that time, and the increased chair time for patients with the 30-min infusion, the Clearview Cancer Institute decided to use HTX-019 as a 2-min injection (IV push) versus the infusion method of administration. Patients included in the review had an Eastern Cooperative Oncology Group (ECOG) performance status of 0–4, received 76 chemotherapy regimens (total for cohort), and were treated with aprepitant injectable emulsion (HTX-019) 130 mg or switched from fosaprepitant 150 mg to HTX-019 130 mg as part of a three-drug antiemetic combination regimen with a 5-HT3 receptor antagonist and dexamethasone. For some patients, HTX-019 was administered prior to initial and subsequent chemotherapy cycles. HTX-019 administration via an IV push was analyzed.
An electronic query within the electronic medical record (EMR) was initiated to identify all patients prescribed HTX-019 and to determine whether there was any medical or nursing documentation associated with HSRs (flushing, hypotension, bronchospasm, and cardiac dysfunction) and ISAEs (pain, erythema, swelling, hives, phlebitis, superficial thrombosis, and delayed infusion). The output of this query was then verified against the medication administration record (MAR) for patient administration to ensure that HTX-019 doses were, in fact, given. Nursing and physician notes were then reviewed for each patient on this cross-validated list to determine if any other nondocumented clinical events were recorded. Any ISAEs, HSRs, or HTX-019-associated adverse events (AEs) occurring 0–30 min and 30–60 min after HTX-019 administration, and later, prior to the next chemotherapy cycle were recorded.
Continuous variables (e.g., mean, standard deviation) and categorical variables (frequency and percentage) were assessed using descriptive statistics.
Compliance with Ethics Guidelines
This was a retrospective longitudinal analysis from a HIPAA-compliant electronic medical record database, so no institutional review board approval was necessary.
Results
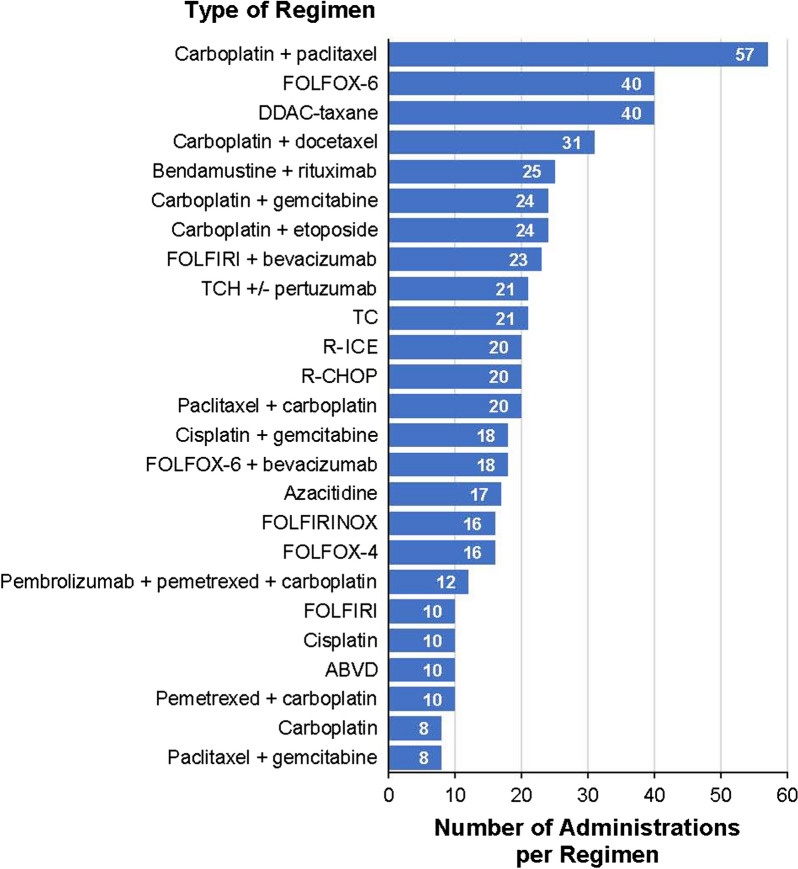
This retrospective chart review identified a total of 2066 HTX-019 injections administered in 591 patients, 262 of whom initially received fosaprepitant, then switched to HTX-019. The majority of patients (n = 511) received HTX-019 via central line access, which included a central catheter or peripherally inserted central catheter (PICC) (Table 1). The patients were aged 18–94 years (median 64 years); 54% were women, and most (78%) were white (Table 1). The 591 patients received a total of 76 regimens [HEC, n = 35; MEC, n = 35; low emetogenic chemotherapy (LEC), n = 6] (Table 1) comprising 642 total chemotherapy doses, the most common being carboplatin plus paclitaxel (n = 57); dose-dense doxorubicin and cyclophosphamide (DDAC) plus taxane (n = 40); and 5-fluorouracil, folinic acid, and oxaliplatin (FOLFOX-6) (n = 40) (Fig. 1). The most common diagnoses were lung (n = 107), breast (n = 100), and colon (n = 92) cancers (Fig. 2).
Table 1.
Demographics and patient disposition
| Parameter | HTX-019 IV push (N = 591) |
|---|---|
| Median age (range), years | 64 (18–94) |
| Sex, n (%) | |
| Male | 272 (46) |
| Female | 319 (54) |
| Race, n (%) | |
| White | 461 (78) |
| African American | 86 (15) |
| Asian | 10 (2) |
| Other | 6 (1) |
| Declined | 23 (4) |
| Patient disposition, n | |
| Total HTX-019 doses | 2066 |
| Median doses per patient | 3 |
| Total chemotherapy doses | 642 |
| Chemotherapy regimens | 76 |
| HEC | 35 |
| MEC | 35 |
| LEC | 6 |
| Patients switching to HTX-019 | 262 |
| Route of HTX-019 administration, n (%) | |
| Central (catheter or PICC) | 511 (86) |
| Peripheral | 80 (14) |
HEC highly emetogenic therapy, IV intravenous, LEC low emetogenic chemotherapy, MEC moderately emetogenic chemotherapy, PICC peripherally inserted central catheter
Fig. 1.
Regimen distribution: chemotherapy regimens accounting for over 80% of the treatments administered. ABVD doxorubicin (Adriamycin), bleomycin, vinblastine, and dacarbazine; DDAC dose-dense doxorubicin and cyclophosphamide; FOLFIRI 5-fluorouracil, folinic acid, and irinotecan; FOLFOX 5-fluorouracil, folinic acid, and oxaliplatin; R-ICE ifosfamide, carboplatin, etoposide; R-CHOP rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone; TC docetaxel (Taxotere) and cyclophosphamide; TCH docetaxel, cyclophosphamide, and trastuzumab (Herceptin). Number of regimen administrations shown here = 522 of 642 total administrations
Fig. 2.
Patient distribution by target diagnoses. Number of patients with diagnoses shown here = 470 of 591 total patients
Among the 591 patients receiving 2066 HTX-019 injections, no clinically significant ISAEs or AEs associated with HTX-019 administration were reported on the basis of the criteria detailed in the “Methods”. None of the patients discontinued HTX-019 treatment, and none switched from HTX-019 to another NK-1 RA (Table 2).
Table 2.
Safety analysis of HTX-019
| Number of patients | |
|---|---|
| Adverse events | 0 |
| Discontinuing HTX-019 | 0 |
| Switched from HTX-019 to alternate NK-1 receptor antagonist | 0 |
NK-1 neurokinin 1
Discussion
In this retrospective real-world analysis, HTX-019, administered as an IV push for CINV prevention, displayed a highly tolerable safety profile in patients receiving cancer chemotherapy, with no clinically significant ISAEs or HTX-019-associated AEs among 591 patients receiving a total of 2066 HTX-019 injections. This is the first analysis to describe the benefit of HTX-019 in patients with cancer.
The safe addition of HTX-019 to an antiemetic regimen containing 5-hydroxytryptamine type 3 (5-HT3) plus dexamethasone is of particular importance. Adding NK-1 RAs to standard antiemetic regimens (5-HT3 RA plus dexamethasone) has improved CINV control [11, 18–20], but certain injectable NK-1 RAs (fosaprepitant and rolapitant) are associated with HSRs and ISAEs related to polysorbate 80 and other synthetic surfactants [5, 21]. For example, the fosaprepitant prescribing information includes a warning and precaution concerning HSRs (anaphylaxis and anaphylactic shock) and was recently updated to include ISAEs as well [5]. In addition, rolapitant IV, which contains the synthetic surfactant polyoxyl 15 hydroxystearate, was approved in 2017 for administration in combination with other antiemetics for CINV prevention [21]. A US Food and Drug Administration (FDA) MedWatch safety alert, issued to health care providers in January 2018, warned about HSRs, including anaphylaxis and anaphylactic shock, associated with administration of rolapitant IV [22]. In February 2018, the manufacturer announced the suspension of rolapitant IV distribution [23]. HTX-019, as a polysorbate 80- and synthetic surfactant-free aprepitant NK-1 RA injectable emulsion, is a more tolerable NK-1 RA and a valuable addition to existing antiemetic regimens.
In two bioequivalence studies in healthy subjects, HTX-019 was bioequivalent to and safer than fosaprepitant, as a significantly lower number of subjects experienced TEAEs and treatment-related TEAEs following HTX-019 administration [15, 16]. These results led to the approval, in November 2017, of HTX-019 as a 30-min infusion for the prevention of acute and delayed CINV. Following the FDA 2017 announcement of a significant acute shortage of small-volume parenteral solutions, including those used for HTX-019 dilution, the FDA directed clinicians to the American Society of Health-System Pharmacists (ASHP) recommendation to switch administration of parenterally administered products to an IV push (injection over 5 min or less) whenever possible [17]. An open-label, randomized, two-sequence, two-period crossover study showed comparable pharmacokinetic and safety profiles for HTX-019 130 mg administered as a 2-min injection or a 30-min infusion, and both methods of administration were well tolerated [24].
Limitations of this study include its retrospective nature, with certain types of AEs not being analyzed or accounted for. More specifically, since the study was designed to detect and analyze specific HSRs and ISAEs based on predetermined nursing and medical documentation, certain AEs (e.g., headache and muscle aches) were not analyzed. The analysis was purely based on administration of HTX-019 and any overt ISAEs.
Conclusion
The results of this retrospective analysis further demonstrate the tolerability and safety of HTX-019, extend the results of previous HTX-019 studies completed in healthy subjects [15, 16, 24], and address the ASHP recommendation to use IV push as an alternative method of administration in CINV prevention. Future studies evaluating HTX-019 safety in real-world settings in patients with cancer are needed to establish further evidence of the agent’s clinical benefit.
Acknowledgements
The author would like to thank the participants within the dataset that was utilized in this study.
Funding
This study was funded by Heron Therapeutics, Inc., San Diego, CA, USA. Article processing charges, open access fees, and medical writing were also funded by Heron Therapeutics, Inc.
Medical Writing and Other Assistance
Medical writing support in the preparation of this manuscript was provided by Phillip Giannopoulos, PhD, of SciStrategy Communications, and funded by Heron Therapeutics, Inc. Data aggregation facilitation was provided by Brittany Davis of Clearview Cancer Institute.
Authorship
Gary Walton meets the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, takes responsibility for the integrity of the work as a whole, and has given final approval for the version to be published.
Disclosures
Gary Walton reports employment by and a leadership role with Clearview Cancer Institute; reports stock ownership in TG Therapeutics, Amgen, Bellicum Pharmaceuticals, Karyopharm Therapeutics, Walgreens Boots Alliance, and Coherus Biosciences; received honoraria from Integra and Heron Therapeutics; received research funding from Heron Therapeutics; and has had a consulting/advisory relationship with Heron Therapeutics.
Compliance with Ethics Guidelines
This was a retrospective longitudinal analysis from a HIPPA-compliant claims database, so no institutional review board approval was necessary.
Data Availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Enhanced Digital Features
To view enhanced digital features for this article go to 10.6084/m9.figshare.7583852.
References
- 1.Herrstedt J, Roila F, Warr D, et al. 2016 updated MASCC/ESMO consensus recommendations: prevention of nausea and vomiting following high emetic risk chemotherapy. Support Care Cancer. 2017;25(1):277–288. doi: 10.1007/s00520-016-3313-0. [DOI] [PubMed] [Google Scholar]
- 2.Hesketh PJ, Kris MG, Basch E, et al. Antiemetics: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2017;35(28):3240–3261. doi: 10.1200/JCO.2017.74.4789. [DOI] [PubMed] [Google Scholar]
- 3.National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: antiemesis—version 3.2018;2018. [DOI] [PMC free article] [PubMed]
- 4.Roila F, Warr D, Hesketh PJ, et al. 2016 updated MASCC/ESMO consensus recommendations: prevention of nausea and vomiting following moderately emetogenic chemotherapy. Support Care Cancer. 2017;25(1):289–294. doi: 10.1007/s00520-016-3365-1. [DOI] [PubMed] [Google Scholar]
- 5.Emend (fosaprepitant) for injection, for intravenous use (prescribing information). Whitehouse Station, NJ: Merck & Co. 2018.
- 6.ten Tije AJ, Verweij J, Loos WJ, Sparreboom A. Pharmacological effects of formulation vehicles: implications for cancer chemotherapy. Clin Pharmacokinet. 2003;42(7):665–685. doi: 10.2165/00003088-200342070-00005. [DOI] [PubMed] [Google Scholar]
- 7.Fujii T, Nishimura N, Urayama KY, et al. Differential impact of fosaprepitant on infusion site adverse events between cisplatin- and anthracycline-based chemotherapy regimens. Anticancer Res. 2015;35(1):379–383. [PubMed] [Google Scholar]
- 8.Grunberg S, Chua D, Maru A, et al. Single-dose fosaprepitant for the prevention of chemotherapy-induced nausea and vomiting associated with cisplatin therapy: randomized, double-blind study protocol—EASE. J Clin Oncol. 2011;29(11):1495–1501. doi: 10.1200/JCO.2010.31.7859. [DOI] [PubMed] [Google Scholar]
- 9.Hegerova LT, Leal AD, Grendahl DC, et al. An analysis of fosaprepitant-induced venous toxicity in patients receiving highly emetogenic chemotherapy. Support Care Cancer. 2015;23(1):55–59. doi: 10.1007/s00520-014-2326-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leal AD, Kadakia KC, Looker S, et al. Fosaprepitant-induced phlebitis: a focus on patients receiving doxorubicin/cyclophosphamide therapy. Support Care Cancer. 2014;22(5):1313–1317. doi: 10.1007/s00520-013-2089-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Saito H, Yoshizawa H, Yoshimori K, et al. Efficacy and safety of single-dose fosaprepitant in the prevention of chemotherapy-induced nausea and vomiting in patients receiving high-dose cisplatin: a multicentre, randomised, double-blind, placebo-controlled phase 3 trial. Ann Oncol. 2013;24(4):1067–1073. doi: 10.1093/annonc/mds541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sato Y, Kondo M, Inagaki A, et al. Highly frequent and enhanced injection site reaction induced by peripheral venous injection of fosaprepitant in anthracycline-treated patients. J Cancer. 2014;5(5):390–397. doi: 10.7150/jca.7706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tsuda T, Kyomori C, Mizukami T, et al. Infusion site adverse events in breast cancer patients receiving highly emetic chemotherapy with prophylactic anti-emetic treatment with aprepitant and fosaprepitant: a retrospective comparison. Mol Clin Oncol. 2016;4(4):603–606. doi: 10.3892/mco.2016.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.CINVANTI™ (aprepitant) injectable emulsion, for intravenous use. San Diego, CA: Heron Therapeutics. 2018.
- 15.Ottoboni T, Keller MR, Cravets M, Clendeninn N, Quart B. Bioequivalence of HTX-019 (aprepitant IV) and fosaprepitant in healthy subjects: a phase I, open-label, randomized, two-way crossover evaluation. Drug Des Devel Ther. 2018;12:429–435. doi: 10.2147/DDDT.S155875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ottoboni T, Lauw M, Keller MR. Safety of HTX-019 (intravenous aprepitant) and fosaprepitant in healthy subjects. Future Oncol. 2018;14(27):2849–2859. doi: 10.2217/fon-2018-0311. [DOI] [PubMed] [Google Scholar]
- 17.ASHP and the University of Utah Drug Information Service. Small-volume parenteral solutions shortages: suggestions for management and conservation. US Food and Drug Administration Web site; 2017. https://www.fda.gov/downloads/Drugs/DrugSafety/DrugShortages/UCM582461.pdf. Accessed 27 Sept 2018.
- 18.Hu Z, Cheng Y, Zhang H, et al. Aprepitant triple therapy for the prevention of chemotherapy-induced nausea and vomiting following high-dose cisplatin in Chinese patients: a randomized, double-blind, placebo-controlled phase III trial. Support Care Cancer. 2014;22(4):979–987. doi: 10.1007/s00520-013-2043-9. [DOI] [PubMed] [Google Scholar]
- 19.Rapoport BL, Chasen MR, Gridelli C, et al. Safety and efficacy of rolapitant for prevention of chemotherapy-induced nausea and vomiting after administration of cisplatin-based highly emetogenic chemotherapy in patients with cancer: two randomised, active-controlled, double-blind, phase 3 trials. Lancet Oncol. 2015;16(9):1079–1089. doi: 10.1016/S1470-2045(15)00035-2. [DOI] [PubMed] [Google Scholar]
- 20.Schwartzberg L. Getting it right the first time: recent progress in optimizing antiemetic usage. Support Care Cancer. 2018;26(suppl 1):19–27. doi: 10.1007/s00520-018-4116-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Varubi (rolapitant) tablets, for oral use. Varubi® (rolapitant) injectable emulsion, for intravenous use (prescribing information). Waltham, MA: Tesaro Inc. 2018.
- 22.US Food and Drug Administration. Varubi (rolapitant) injectable emulsion: health care provider letter—anaphylaxis and other serious hypersensitivity reactions. January 16, 2018. https://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm592592.htm. Accessed 27 Sept 2018.
- 23.Tesaro announces fourth-quarter and full-year 2017 operating results. Tesaro news releases. http://ir.tesarobio.com/news-releases/news-release-details/tesaro-announces-fourth-quarter-and-full-year-2017-operating. Accessed 27 Sept 2018.
- 24.Ottoboni T, Lauw M, Keller MR, et al. HTX-019 via 2-min injection or 30-min infusion in healthy subjects. Future Oncol. 2018. 10.2217/fon-2018-0809. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available from the corresponding author on reasonable request.