Supplemental Digital Content is available in the text.
Keywords: angiography, cerebral infarction, computed tomography angiography, internal carotid artery, workflow
Background and Purpose—
The location of the thrombus as observed on first digital subtraction angiography during endovascular treatment may differ from the initial observation on initial noninvasive imaging. We studied the incidence of thrombus dynamics, its impact on patient outcomes, and its association with intravenous thrombolytics.
Methods—
We included patients from the MR CLEAN registry (Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke) with an initial target occlusion on computed tomography angiography located in the intracranial internal carotid artery, M1, or M2. The conventional angiography target occlusion was defined during endovascular treatment. Thrombus dynamics were classified as growth, stability, migration, and resolution. The primary outcome was functional outcome at 90 days (modified Rankin Scale). The secondary outcomes were successful and complete reperfusion (extended treatment in cerebral infarction scores of 2b-3 and 3, respectively).
Results—
The analysis included 1349 patients. Thrombus migration occurred in 302 (22%) patients, thrombus growth in 87 (6%), and thrombus resolution in 39 (3%). Intravenous treatment with alteplase was associated with more thrombus migration (adjusted odds ratio, 2.01; CI, 1.29–3.11) and thrombus resolution (adjusted odds ratio, 1.85; CI, 1.22–2.80). Thrombus migration was associated with a lower chance of complete reperfusion (adjusted odds ratio, 0.57; CI, 0.42–0.78) and successful reperfusion (adjusted odds ratio, 0.74; CI, 0.55–0.99). In the subgroup of patients with M1 initial target occlusion, thrombus migration was associated with better functional outcome (adjusted common odds ratio, 1.49; CI, 1.02–2.17), and there was a trend towards better functional outcome in patients with thrombus resolution (adjusted common odds ratio, 2.23; CI, 0.93–5.37).
Conclusions—
In patients with acute ischemic stroke, thrombus location regularly changes between computed tomography angiography and digital subtraction angiography. Administration of intravenous alteplase increases the chance of thrombus migration and resolution. Thrombus migration is associated with better functional outcome but reduces the rate of complete reperfusion.
Multiple randomized clinical trials demonstrated the benefit of endovascular treatment (EVT) for patients with an acute ischemic stroke caused by a large-vessel occlusion.1,2 Thrombus location is a vital imaging selection criterion because the benefit of EVT for distal occlusions, especially M2, remains uncertain.3–6 In the current workflow of acute ischemic stroke, thrombus location is determined at 2 moments: the initial target occlusion is determined on noninvasive imaging, usually by computed tomography angiography (CTA) at initial presentation. If a large-vessel occlusion is detected, the patient is considered for EVT. During this procedure, conventional angiography is performed, which allows the determination of the conventional angiography target occlusion.7
Despite recent progress, there is still a paucity of information about thrombus imaging on patients with stroke with large-vessel occlusion.8,9 Thrombus dynamics (a difference between the initial and the conventional angiography target occlusions) have been described in few studies and reported anecdotally.10–12 Distal thrombus migration has been defined as a more distal conventional angiography target occlusion than the initial target occlusion.13 In patients with EVT, distal thrombus migration increased the risk of incomplete reperfusion, suggesting thrombus fragility.13 Thrombus resolution has also been detailed, especially after intravenous administration of alteplase (IVT).14–16 Moreover, thrombus growth has also been studied, and it has been associated with poor collaterals, blood stasis, and early neurological deterioration, suggesting that thrombus dynamics is related to thrombus composition.17,18 Despite these previously reported studies, the impact of thrombus migration on patient outcomes and the association between IVT and thrombus dynamics is undetermined.13,19,20
The aim of this study is to determine the association of thrombus dynamics with IVT and its effect on patient outcome.
Methods
We included patients from the MR CLEAN registry (Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke), an observational, prospective study, registering patients who underwent EVT (defined as receiving arterial puncture for angiography) for acute ischemic stroke in 16 intervention centers in the Netherlands from 2014 to 2016.21 Patients with anterior and posterior circulation stroke were included. Neither Alberta Stroke Program Early CT Score nor collateral grade was an explicit exclusion criterion. The registry was approved by a central medical ethics committee and by the research board of all participating centers. Source data of this study are available from the corresponding author on reasonable request.
Initial target occlusion was defined as the most proximal thrombus location on CTA.12 Conventional angiography target occlusion was defined as the most proximal thrombus location on first intracranial digital subtraction angiography. Target occlusion locations were determined by a core lab. Thrombus location was classified as cervical internal carotid artery (ICA), intracranial ICA, M1, M2, M3, M4, A1, A2, or no occlusions. In the current analysis, patients with an initial target occlusion of the intracranial ICA or the first and second segments of the middle cerebral artery (M1 and M2) were included.
Thrombus dynamics were classified as migration, growth, or resolution. Thrombus migration was defined as a shift to a more distal conventional angiography target occlusion than the initial target occlusion. Thrombus growth was defined as a shift to a more proximal conventional angiography target occlusion thrombus location than the initial target occlusion. Thrombus resolution was defined as the absence of conventional angiography target occlusion.
Statistical Analysis
Baseline, workflow, treatment, and outcome characteristics were compared between patients with stable thrombus and different types of thrombus dynamics. Group comparisons were performed using Student t, Kruskal-Wallis, and χ2 tests. Binary regression models were used to assess whether IVT was associated with migration, growth, or resolution compared with stable thrombus. The primary outcome was functional outcome, expressed with the score on the modified Rankin Scale at 3 months. On this scale, a score of 0 corresponds to no symptoms and a score of 6 to death. The association between thrombus dynamics and functional outcome was expressed as a common odds ratio (cOR) for a shift towards a better functional outcome estimated with ordinal regression. The secondary outcome was reperfusion status (successful or complete reperfusion). Reperfusion was assessed on digital subtraction angiography using the expanded Thrombolysis in Cerebral Infarction (eTICI) score. Successful reperfusion was defined as an eTICI score of 2b, 2c, or 3.22 Complete reperfusion was defined as an eTICI score of 3.23 The association of different thrombus dynamics and reperfusion status was assessed using binary regression. The associations between different types of thrombus dynamics and primary and secondary outcomes as well as the associations between IVT and thrombus dynamics were assessed by univariable and multivariable models. The multivariable IVT models were adjusted for age, history of atrial fibrillation, history of peripheral artery disease, collateral score, serum glucose level, history of diabetes mellitus, arterial blood pressure, (international normalized ratio >1.7), time from onset to computed tomography, previous stroke and novel anticoagulants use. The multivariable outcome models (modified Rankin Scale and reperfusion status) were adjusted for age, baseline National Institutes of Health Stroke Scale, IVT treatment, prestroke modified Rankin Scale, time from onset to groin puncture, history of atrial fibrillation, symptomatic cervical carotid obstruction on CTA, and collateral grade. To reduce the influence of thrombus location on patient outcome, we also assessed the effect of the thrombus growth, migration, and resolution on primary and secondary outcomes including only patients with M1 initial target occlusion. On multivariable models, the associations were expressed as adjusted cOR for ordinal regression and adjusted odds ratio (aOR) for binary regressions. For the regression models, we performed multiple imputations for the missing data. All reported data were not imputed. The statistical analysis was performed using R (R Foundation for Statistical Computing, Vienna, Austria; version 1.0.136).
Results
A total of 1627 patients were included in the MR CLEAN Registry in our study period. Available data concerning outcome and baseline characteristics were reported for the 1349 patients with full data available concerning thrombus characteristics (Figure I in the online-only Data Supplement).
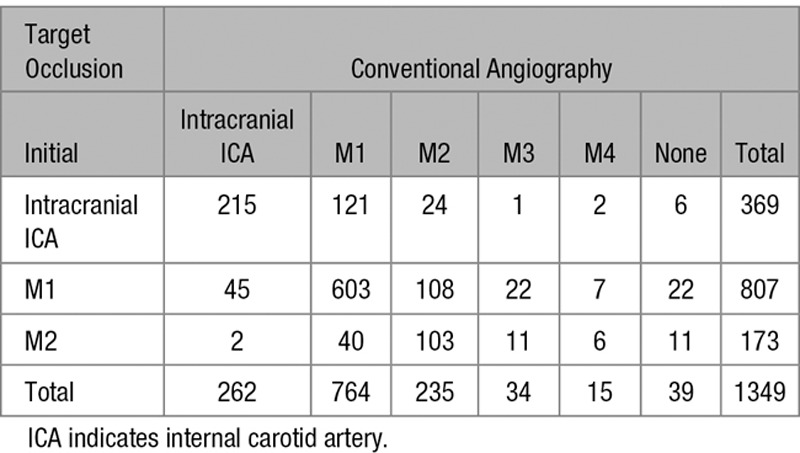
Thrombus migration was observed in 302/1349 (22%), thrombus growth in 87/1349 (6%) and thrombus resolution in 39/1349 (3%) patients. The most common change in occlusion location was ICA to M1 (121; 8%) followed by M1 to M2 (108; 7%). Thrombus migration occurred in 154/269 (42%) of ICA occlusions. Thrombus growth, resolution, or migration was also observed in 70/173 (40%) of patients with M2 occlusions (Table 1).
Table 1.
Conventional Angiography Target Occlusion Location Stratified by the Initial Target Occlusion Location
Most baseline characteristics were similar for the groups (Table 2). The Clot Burden Score24 was significantly higher in patients with thrombus growth and resolution. The frequency of atrial fibrillation was lower in patients with thrombus migration and resolution. Patients with thrombus migration had a higher rate of multiple intracranial occlusions detected on digital subtraction angiography and of symptomatic cervical ICA occlusion on CTA. The rate of transfer from the referral center and other time metrics were not significantly different among the groups (Table 3).
Table 2.
Baseline Characteristics
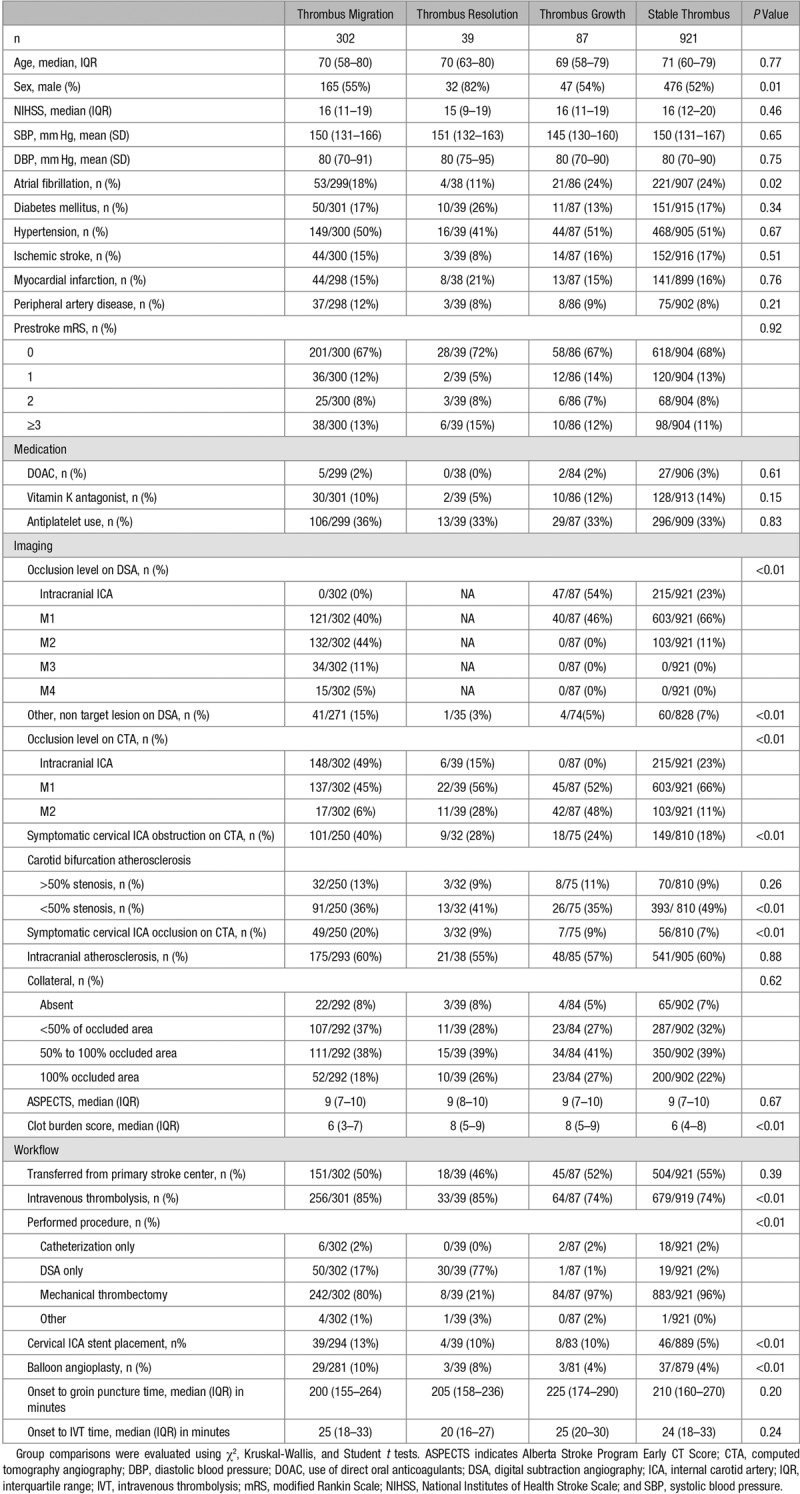
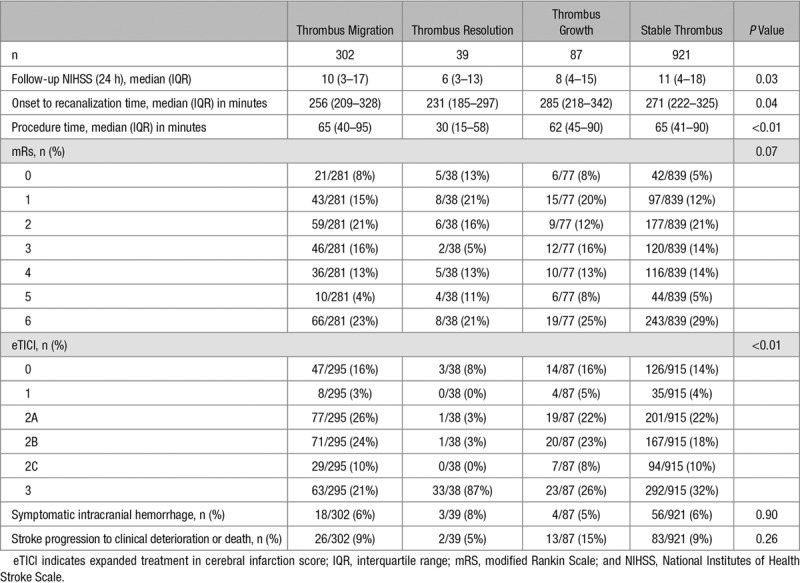
Table 3.
Patient Outcome
Symptomatic cervical ICA obstruction (ie, atherosclerosis, dissection, carotid web, and previous stent), atherosclerotic cervical ICA occlusion and treatment (stent and balloon angioplasty) were significantly more frequent in patients with thrombus migration and resolution (P<0.01). We also found a trend towards higher frequency of significant atherosclerotic carotid stenosis (>50%) on patients with thrombus migration, but it did not reach statistical significance. Patients with stable thrombus had a significant higher incidence of nonsignificant atherosclerotic carotid stenosis (P<0.01).
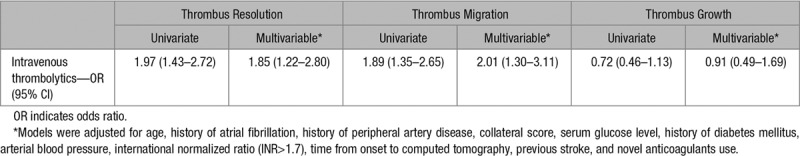
IVT was significantly associated with thrombus migration and resolution. In patients with IVT, the rate of thrombus migration was 25% in contrast to a 14% rate in patients without IVT. Occurrence of thrombus growth was not significantly associated with IVT (Table 4).
Table 4.
Associations Between the Administration of Intravenous Thrombolytics and Changes in Occlusion Location
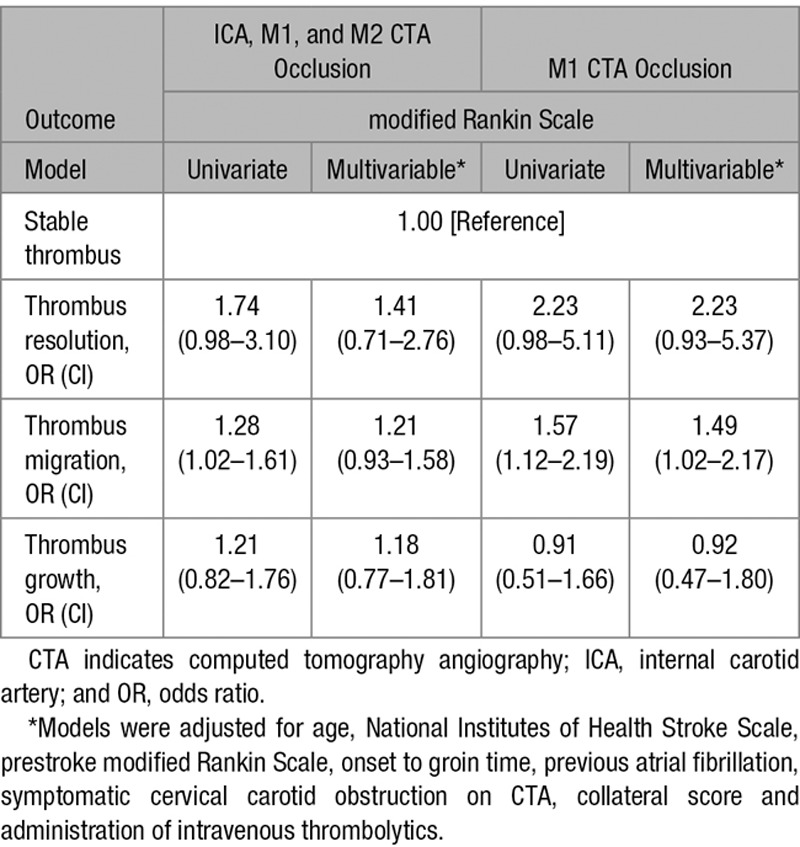
Compared with patients who had a stable thrombus, patients with thrombus migration had better functional outcomes (Figure II in the online-only Data Supplement). In patients with M1 initial target occlusion, thrombus migration was associated with better functional outcome (adjusted cOR, 1.49; CI 95%, 1.02–2.17). Thrombus resolution patients also had better functional outcomes; however, statistical significance was not reached (adjusted cOR, 2.23; CI 95%, 0.93–5.37). Thrombus growth was not significantly associated with functional outcome. There was a trend towards a better functional outcome (adjusted cOR, 1.18; CI 95%, 0.77–1.81), but the association was in the opposite direction when including only M1 initial target occlusion (Table 5).
Table 5.
Ordinal Logistic Regression Models Assessing the Associations of Thrombus Dynamics With Functional Outcome
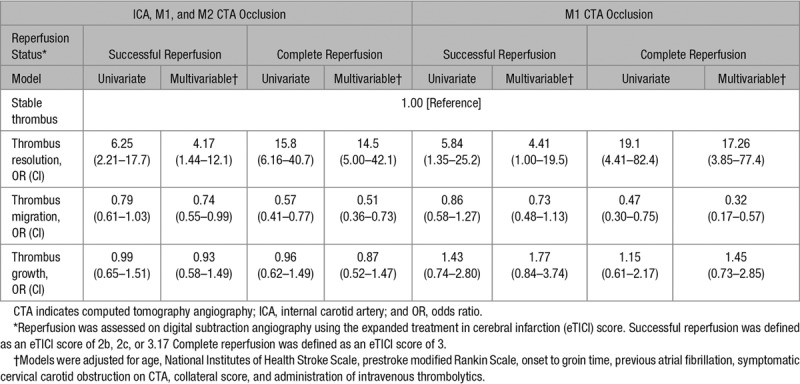
Thrombus migration was associated with worse reperfusion status. (Table 6) Patients with thrombus migration had a lower chance of complete reperfusion (aOR, 0.51; CI 95%, 0.36–0.73) and successful reperfusion (aOR, 0.74; CI 95%, 0.55–0.99). These findings were similar when including only M1 initial target occlusion. By definition, all patients in the thrombus resolution group had complete recanalization, but 5/39 (14%) did not achieve complete reperfusion. Thrombus resolution significantly increased the rates of successful reperfusion (aOR, 4.17; CI 95%, 1.44–12.1) and complete reperfusion (aOR, 14.5; CI 95%, 5.00–42.1). Thrombus growth was not significantly associated with reperfusion status.
Table 6.
Binary Logistic Regression Models Assessing the Associations of Thrombus Dynamics With Reperfusion Status
Discussion
We demonstrated that preinterventional changes in thrombus location are common in acute ischemic stroke. In our study, thrombus migration was the most common change and was associated with improved functional outcome. Interestingly, it was also associated with worse reperfusion status. IVT increased the rates of thrombus migration and resolution.
The incidence of thrombus migration and growth in our study were similar to the incidence documented by other studies.13,16,19,20 However, this study showed a lower incidence of thrombus resolution, which may be the result of a difference in definition; we defined thrombus resolution as complete recanalization before the intervention.16,25 While the association of IVT and changes in thrombus location has been demonstrated,20 especially in patients with preinterventional reperfusion,25,26 the association was not present in other thrombus migration studies.13,16 Our study found that in patients treated with IVT, both thrombus migration and resolution were more frequent. To the best of our knowledge, our study is the first to demonstrate a significantly higher frequency of cervical carotid stenosis in patients with thrombus migration. Further, the association between thrombus migration and better functional outcome was only significant in our study.19 This might be due to the different methodology used to define migration. Kaesmacher et al13 included patients with both direct (angiographic) and indirect evidence of thrombus migration by evaluating perfusion deficits within the lenticulostriate artery territory.26 In our study, only direct evidence was used. The association between thrombus migration and a lower chance of successful reperfusion was also previously reported.13,26
The histological composition of a thrombus might influence the dynamics it exhibits. Red blood cell-rich thrombi have been reported to be more frequent in patients with thrombus migration.27 This type of thrombus is more common in patients with large-vessel atherosclerosis, which may explain the increased rate of cervical carotid occlusion and the lower incidence of atrial fibrillation in our patients with thrombus migration and resolution.28 These patients also had a higher rate of multiple intracranial occlusions on first digital subtraction angiography before EVT, potentially caused by thrombus fragmentation or multiple emboli, another finding that points to the influence of thrombus composition, and that tends to be more common in red blood cell-rich thrombi.29 Thrombus fragmentation has also been associated with IVT administration before EVT.16 The higher frequency of stent treatment and balloon angioplasty may also cause hemodynamic changes that leads to thrombus migration and resolution. The smaller thrombus burden in patients with thrombus resolution indicates that thrombus volume might influence thrombus dynamics. However, the smaller burden in patients with thrombus growth may be better explained by selection bias, since the thrombus growth group did not include patients with CTA ICA occlusions.
The better functional outcome after thrombus migration could have several causes. First, the most common changes in thrombus location were ICA to M1 and M1 to M2. This may allow flow through the lenticulostriate arteries and circle of Willis, filling the affected territory via collaterals, leading to better functional outcome.30 Second, the higher incidence of distal occlusions is also associated with smaller ischemic core and better functional outcome.31,32 Because of our definitions, the thrombus growth group did not include ICA occlusions on CTA, whereas almost one quarter of patients on the stable group had such ICA occlusions. This may explain why there was also a trend towards better functional outcome on patients with thrombus growth and why this association was lost when only M1 initial target occlusion was included on both groups. As expected, thrombus resolution was associated with the best functional outcomes, but statistical significance was only reached on the M1 initial target occlusion analyses, probably because its effect of early reperfusion compared with no reperfusion is relatively greater than in distal occlusions such as M2.
Our findings reveal a thrombus migration paradox—an improvement in functional outcome despite worse reperfusion status. The shift to a more distal thrombus location reflects partial recanalization and subsequent distal embolization of thrombus fragments, which is more common after IVT.16,26 Given the smaller size and more tortuous course of the distal arterial branches, thrombectomy devices are not only more difficult to deliver to distal occlusions but also less likely to be effective.4 The increased rate of thrombus inaccessibility explains why mechanical thrombectomy was less frequently performed in thrombus migration patients and also why these patients had a lower chance of successful reperfusion. Nevertheless, because thrombus migration improved functional outcome in this study, one could speculate that the benefit of early proximal revascularization in most cases outweighs the negative impact of reperfusion failure. However, the relationship between the timing and extent of revascularization must also depend on the extent of the final perfusion deficit. For example, an eTICI score of 2A in a patient with an M2 occlusion could correspond to more preserved tissue than an eTICI score of 2B in a patient with an M1 occlusion. Other factors that could influence the association of IVT and patient outcome: IVT may help recanalize remaining thrombi in the microvasculature or distal branches, but it is also more strongly associated with blood-brain barrier breakdown, increasing the risk of symptomatic intracranial hemorrhage.33 A potential confounding factor that must be noted is that IVT treated patients have a more favorable treatment profile than their non-IVT treated counterparts. Patients treated with IVT have fewer comorbidities and present earlier at the hospital. While not significant, this trend can be seen in the thrombus dynamic subgroups as well, with more atrial fibrillation and marginally longer onset to groin times in the stable thrombus group. While we adjusted for these confounders, their effects might still contribute to the observed association. Current clinical trials investigating the value of additional IVT in the era of EVT treatment, such as MR CLEAN-NO IV (ISRCTN80619088), DIRECT MT (Direct Intra-arterial Thrombectomy In order to Revascularize AIS Patients With Large Vessel Occlusion Efficiently in Chinese Tertiary Hospitals; NCT03469206), and SWIFT DIRECT (Solitaire With the Intention for Thrombectomy Plus Intravenous t-PA Versus DIRECT Solitaire Stent-Retriever Thrombectomy in Acute Anterior Circulation Stroke; NCT03192332), will aid to determine whether the chance of early lysis by IVT outweighs the potential negative effects of IVT.
The major limitation of our study is the lack of inclusion of patients in whom there was sufficient clinical recovery before groin puncture to forego EVT in the MR CLEAN Registry. This may have resulted in an underestimation of the occurrence of thrombus resolution and migration and their beneficial effect. Further, apparent differences in thrombus location between the initial and the conventional angiography target occlusions might also be caused by reduced flow leading to delayed contrast delivery proximal to the occlusion. The reduced flow may simulate a proximal occlusion on CTA, the so-called pseudo-occlusions.34,35 Another limitation were disagreements between the interventionist and the core lab. This was observed on 8 patients from the thrombus resolution group on which the interventionist performed mechanical thrombectomy, and later, the core lab considered that there was no residual thrombus. We also did not consider occlusion location differences in subsegments of the intracranial ICA and between proximal and distal M1 to reduce the effect of the inter-observer disagreement. Stroke cause evaluation was limited, because TOAST (Trial of ORG 10172 in Acute Stroke Treatment) criteria was not available.36
Conclusions
In patients with acute ischemic stroke due to proximal occlusion of the anterior circulation, preinterventional changes in thrombus location are common, especially after IVT. In our population, thrombus migration was associated with improved functional outcome, although there was an association with worse reperfusion status at the end of EVT.
Sources of Funding
The MR CLEAN registry (Multicenter Randomized Clinical Trial of Endovascular Treatment of Acute Ischemic Stroke) was partly funded by TWIN Foundation (Stichting Toegepast Wetenschappelijk Instituut voor Neuromodulatie), Erasmus MC University Medical Center, Maastricht University Medical Center, and Academic Medical Center, Amsterdam.
Disclosures
Erasmus University Medical Center received funds from Stryker for consultations by Dr van der Lugt. Academic Medical Center Amsterdam received funds from Stryker for consultations by Drs Majoie and Roos. Dr Marquering is cofounder and shareholder of Nico-lab. Drs Jansen, Roos, and Majoie own stock in Nico-lab B.V. Drs Yoo and van den Berg received funds from Cerenovus Neurovascular for consultations. Dr Yoo received grants from Cerenovus Neurovascular, Medtronics, Stryker, Penumbra, and Genentech for investigator-initiated studies. Dr Yoo received personal fees from Cerenovus Neurovascular and Penumbra (core imaging lab activities) and Genentech (consultation). Dr Yoo has equity ownership from Insera Therapeutics. Dr Vos received personal fees from Stryker. The other authors report no conflicts.
Supplementary Material
Footnotes
Drs Alves and Treurniet contributed equally.
Drs Majoie and Marquering contributed equally.
A list of all MR CLEAN Registry Investigators is given in the online-only Data Supplement.
The online-only Data Supplement is available with this article at https://www.ahajournals.org/doi/suppl/10.1161/STROKEAHA.119.026107.
References
- 1.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. MR CLEAN Investigators. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 2.Mokin M, Rojas H, Levy EI. Randomized trials of endovascular therapy for stroke–impact on stroke care. Nat Rev Neurol. 2016;12:86–94. doi: 10.1038/nrneurol.2015.240. doi: 10.1038/nrneurol.2015.240. [DOI] [PubMed] [Google Scholar]
- 3.Warach SJ, Luby M, Albers GW, Bammer R, Bivard A, Campbell BC, et al. Stroke Imaging Research (STIR) and VISTA-Imaging Investigators. Acute Stroke Imaging Research roadmap III imaging selection and outcomes in acute stroke reperfusion clinical trials: consensus recommendations and further research priorities. Stroke. 2016;47:1389–1398. doi: 10.1161/STROKEAHA.115.012364. doi: 10.1161/STROKEAHA.115.012364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. HERMES Collaborators. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387:1723–1731. doi: 10.1016/S0140-6736(16)00163-X. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 5.Coutinho JM, Liebeskind DS, Slater LA, Nogueira RG, Baxter BW, Levy EI, et al. Mechanical thrombectomy for isolated M2 occlusions: a post hoc analysis of the STAR, SWIFT, and SWIFT PRIME Studies. AJNR Am J Neuroradiol. 2016;37:667–672. doi: 10.3174/ajnr.A4591. doi: 10.3174/ajnr.A4591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Compagne KCJ, van der Sluijs PM, van den Wijngaard IR, Roozenbeek B, Mulder MJHL, van Zwam WH, et al. MR CLEAN Registry Investigators. Endovascular treatment: the role of dominant caliber M2 segment occlusion in ischemic stroke. Stroke. 2019;50:419–427. doi: 10.1161/STROKEAHA.118.023117. doi: 10.1161/STROKEAHA.118.023117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CBLM, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointervent Surg. 2019;11:433–438. doi: 10.1136/neurintsurg-2018-014127. doi: 10.1136/neurintsurg-2018-014127. [DOI] [PubMed] [Google Scholar]
- 8.Brouwer PA, Brinjikji W, De Meyer SF. Clot pathophysiology: why is it clinically important? Neuroimaging Clin N Am. 2018;28:611–623. doi: 10.1016/j.nic.2018.06.005. doi: 10.1016/j.nic.2018.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Meyer SF, Andersson T, Baxter B, Bendszus M, Brouwer P, Brinjikji W, et al. Clot Summit Group. Analyses of thrombi in acute ischemic stroke: a consensus statement on current knowledge and future directions. Int J Stroke. 2017;12:606–614. doi: 10.1177/1747493017709671. doi: 10.1177/1747493017709671. [DOI] [PubMed] [Google Scholar]
- 10.Olsen TS, Lassen NA. A dynamic concept of middle cerebral artery occlusion and cerebral infarction in the acute state based on interpreting severe hyperemia as a sign of embolic migration. Stroke. 1984;15:458–468. doi: 10.1161/01.str.15.3.458. doi: 10.1161/01.str.15.3.458. [DOI] [PubMed] [Google Scholar]
- 11.López-Cuevas R, Lago A, Tembl JI. Downstream migration and fragmentation of a spontaneous calcific embolus after thrombolysis in a patient with ischemic stroke. J Stroke Cerebrovasc Dis. 2016;25:e165–e166. doi: 10.1016/j.jstrokecerebrovasdis.2016.06.010. doi: 10.1016/j.jstrokecerebrovasdis.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 12.Yoon JH, Shin YS, Lim YC, Kim HS, Nam HS, Heo JH. Distal migration of thrombus during intra-arterial thrombolysis. Eur Neurol. 2010;63:62–63. doi: 10.1159/000268169. doi: 10.1159/000268169. [DOI] [PubMed] [Google Scholar]
- 13.Kaesmacher J, Maegerlein C, Kaesmacher M, Zimmer C, Poppert H, Friedrich B, et al. Thrombus migration in the middle cerebral artery: incidence, imaging signs, and impact on success of endovascular thrombectomy. J Am Heart Assoc. 2017;6:e005149. doi: 10.1161/JAHA.116.005149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rha JH, Saver JL. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38:967–973. doi: 10.1161/01.STR.0000258112.14918.24. doi: 10.1161/01.STR.0000258112.14918.24. [DOI] [PubMed] [Google Scholar]
- 15.Kim YD, Nam HS, Kim SH, Kim EY, Song D, Kwon I, et al. Time-dependent thrombus resolution after tissue-type plasminogen activator in patients with stroke and mice. Stroke. 2015;46:1877–1882. doi: 10.1161/STROKEAHA.114.008247. doi: 10.1161/STROKEAHA.114.008247. [DOI] [PubMed] [Google Scholar]
- 16.Mueller L, Pult F, Meisterernst J, Heldner MR, Mono ML, Kurmann R, et al. Impact of intravenous thrombolysis on recanalization rates in patients with stroke treated with bridging therapy. Eur J Neurol. 2017;24:1016–1021. doi: 10.1111/ene.13330. doi: 10.1111/ene.13330. [DOI] [PubMed] [Google Scholar]
- 17.Qazi EM, Sohn SI, Mishra S, Almekhlafi MA, Eesa M, d’Esterre CD, et al. Thrombus characteristics are related to collaterals and angioarchitecture in acute stroke. Can J Neurol Sci. 2015;42:381–388. doi: 10.1017/cjn.2015.291. doi: 10.1017/cjn.2015.291. [DOI] [PubMed] [Google Scholar]
- 18.Seners P, Hurford R, Tisserand M, Turc G, Legrand L, Naggara O, et al. Is unexplained early neurological deterioration after intravenous thrombolysis associated with thrombus extension? Stroke. 2017;48:348–352. doi: 10.1161/STROKEAHA.116.015414. doi: 10.1161/STROKEAHA.116.015414. [DOI] [PubMed] [Google Scholar]
- 19.Qureshi AI, Qureshi MH, Siddiq F, Kainth D, Hassan AE, Maud A. Preprocedure change in arterial occlusion in acute ischemic stroke patients undergoing endovascular treatment by computed tomographic angiography. Am J Emerg Med. 2015;33:631–634. doi: 10.1016/j.ajem.2015.01.054. doi: 10.1016/j.ajem.2015.01.054. [DOI] [PubMed] [Google Scholar]
- 20.Ren Y, Churilov L, Mitchell P, Dowling R, Bush S, Yan B. Clot migration is associated with intravenous thrombolysis in the setting of acute ischemic stroke. Stroke. 2018;49:3060–3062. doi: 10.1161/STROKEAHA.118.022751. doi: 10.1161/STROKEAHA.118.022751. [DOI] [PubMed] [Google Scholar]
- 21.Jansen IGH, Mulder MJHL, Goldhoorn RB MR CLEAN Registry Investigators. Endovascular treatment for acute ischaemic stroke in routine clinical practice: prospective, observational cohort study (MR CLEAN Registry). BMJ. 2018;360:k949. doi: 10.1136/bmj.k949. doi: 10.1136/bmj.k949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Noser EA, Shaltoni HM, Hall CE, Alexandrov AV, Garami Z, Cacayorin ED, et al. Aggressive mechanical clot disruption: a safe adjunct to thrombolytic therapy in acute stroke? Stroke. 2005;36:292–296. doi: 10.1161/01.STR.0000152331.93770.18. doi:10.1161/01.STR.0000152331.93770.18. [DOI] [PubMed] [Google Scholar]
- 23.Chamorro Á, Blasco J, López A, Amaro S, Román LS, Llull L, et al. Complete reperfusion is required for maximal benefits of mechanical thrombectomy in stroke patients. Sci Rep. 2017;7:11636. doi: 10.1038/s41598-017-11946-y. doi: 10.1038/s41598-017-11946-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, et al. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol. 2009;30:525–531. doi: 10.3174/ajnr.A1408. doi: 10.3174/ajnr.A1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tsivgoulis G, Katsanos AH, Schellinger PD, Köhrmann M, Varelas P, Magoufis G, et al. Successful reperfusion with intravenous thrombolysis preceding mechanical thrombectomy in large-vessel occlusions. Stroke. 2018;49:232–235. doi: 10.1161/STROKEAHA.117.019261. doi: 10.1161/STROKEAHA.117.019261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kaesmacher J, Giarrusso M, Zibold F, Mosimann PJ, Dobrocky T, Piechowiak E, et al. Rates and quality of preinterventional reperfusion in patients with direct access to endovascular treatment. Stroke. 2018;49:1924–1932. doi: 10.1161/STROKEAHA.118.021579. doi: 10.1161/STROKEAHA.118.021579. [DOI] [PubMed] [Google Scholar]
- 27.Maegerlein C, Friedrich B, Berndt M, Lucia KE, Schirmer L, Poppert H, et al. Impact of histological thrombus composition on preinterventional thrombus migration in patients with acute occlusions of the middle cerebral artery. Interv Neuroradiol. 2018;24:70–75. doi: 10.1177/1591019917733733. doi: 10.1177/1591019917733733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Niesten JM, van der Schaaf IC, van Dam L, Vink A, Vos JA, Schonewille WJ, et al. Histopathologic composition of cerebral thrombi of acute stroke patients is correlated with stroke subtype and thrombus attenuation. PLoS One. 2014;9:e88882. doi: 10.1371/journal.pone.0088882. doi: 10.1371/journal.pone.0088882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaesmacher J, Boeckh-Behrens T, Simon S, Maegerlein C, Kleine JF, Zimmer C, et al. Risk of thrombus fragmentation during endovascular stroke treatment. AJNR Am J Neuroradiol. 2017;38:991–998. doi: 10.3174/ajnr.A5105. doi: 10.3174/ajnr.A5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alves HC, Treurniet KM, Dutra BG, Jansen IGH, Boers AMM, Santos EMM, et al. MR CLEAN Trial Investigators. Associations between collateral status and thrombus characteristics and their impact in anterior circulation stroke. Stroke. 2018;49:391–396. doi: 10.1161/STROKEAHA.117.019509. doi: 10.1161/STROKEAHA.117.019509. [DOI] [PubMed] [Google Scholar]
- 31.Borst J, Berkhemer OA, Santos EMM, Yoo AJ, den Blanken M, Roos YBWEM, et al. MR CLEAN Investigators. Value of thrombus CT characteristics in patients with acute ischemic stroke. AJNR Am J Neuroradiol. 2017;38:1758–1764. doi: 10.3174/ajnr.A5331. doi: 10.3174/ajnr.A5331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sillanpää N, Saarinen JT, Rusanen H, Elovaara I, Dastidar P, Soimakallio S. Location of the clot and outcome of perfusion defects in acute anterior circulation stroke treated with intravenous thrombolysis. AJNR Am J Neuroradiol. 2013;34:100–106. doi: 10.3174/ajnr.A3149. doi: 10.3174/ajnr.A3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fischer U, Kaesmacher J, Mendes Pereira V, Chapot R, Siddiqui AH, Froehler MT, et al. Direct mechanical thrombectomy versus combined intravenous and mechanical thrombectomy in large-artery anterior circulation stroke: a topical review. Stroke. 2017;48:2912–2918. doi: 10.1161/STROKEAHA.117.017208. doi: 10.1161/STROKEAHA.117.017208. [DOI] [PubMed] [Google Scholar]
- 34.Marquering HA, Nederkoorn PJ, Beenen LF, Lycklama à Nijeholt GJ, van den Berg R, Roos YB, et al. Carotid pseudo-occlusion on CTA in patients with acute ischemic stroke: a concerning observation. Clin Neurol Neurosurg. 2013;115:1591–1594. doi: 10.1016/j.clineuro.2013.02.008. doi: 10.1016/j.clineuro.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 35.Kappelhof M, Marquering HA, Berkhemer OA, Borst J, van der Lugt A, van Zwam WH, et al. MR CLEAN Investigators. Accuracy of CT angiography for differentiating pseudo-occlusion from true occlusion or high-grade stenosis of the extracranial ICA in acute ischemic stroke: a retrospective MR CLEAN Substudy. AJNR Am J Neuroradiol. 2018;39:892–898. doi: 10.3174/ajnr.A5601. doi: 10.3174/ajnr.A5601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of org 10172 in acute stroke treatment. Stroke. 1993;24:35–41. doi: 10.1161/01.str.24.1.35. doi: 10.1161/01.str.24.1.35. [DOI] [PubMed] [Google Scholar]


