Purpose of review
Increased life expectancy in brain tumour patients had led to the need for strategies that preserve and improve cognitive functioning, as many patients suffer from cognitive deficits. The tumour itself, as well as antitumor treatment including surgery, radiotherapy and chemotherapy, supportive treatment and individual patient factors are associated with cognitive problems. Here, we review the recent literature on approaches that preserve and improve cognitive functioning, including pharmacological agents and rehabilitation programs.
Recent findings
Minimizing cognitive dysfunction and improving cognitive functioning in brain tumour patients may be achieved both by preserving cognitive functioning during antitumor treatment, including techniques such as awake brain surgery, less invasive radiation therapies such as stereotactic radiotherapy and proton therapy, as well as with interventions including cognitive rehabilitation programmes. Novel rehabilitation programs including computer-based cognitive rehabilitation therapy (CRT) programmes that can be adjusted to the specific patient needs and can be administered at home are promising. Furthermore, personalized/precision medicine approaches to identify patients who are at risk for cognitive decline may facilitate effective treatment strategies in the future.
Summary
Cognitive functioning has gained greater awareness in the neuro-oncological community, and methods to preserve and improve cognitive functioning have been explored. Rehabilitation programmes for brain tumour patients should be further developed and referred to in clinical practice.
Keywords: brain tumour, cognitive deficits, rehabilitation, treatment
INTRODUCTION
Cognitive functioning refers to mental processes such as attention, perception, thinking, reasoning and remembering, the so-called ‘higher’ cerebral functions. Intact cognitive functioning is important, as it enables to function autonomously within society. In patients with a brain tumour, the presence of the tumour directly threatens cognitive functioning. This is the case in patients with primary brain tumours such as meningiomas and malignant gliomas, as well as in patients with brain metastases, the most prevalent brain tumours. As even mild cognitive deficits can have functional and psychosocial consequences, preserving and improving cognitive functioning in these patients is important to maintain functioning and wellbeing through the disease course.
Many brain tumour patients exhibit cognitive impairment at some point during the disease course, and cognitive deficits are already present in over 90% of the patients with a primary brain tumour and brain metastases before treatment [1,2]. Tumour characteristics such as location, size, histology and growth rate as well as patients characteristics, including age, cardiovascular risk and cognitive reserve are associated with the severity of cognitive impairment [3]. In addition, advances in molecular profiling suggest that germline and tumour genetic factors are also associated with cognitive functioning in brain tumour patients, both before and in response to treatment [4,5]. Apart from the local damage, brain tumours also cause global cognitive dysfunction by disruption of cognitive networks, with attention, memory and executive functioning being the most frequently affected domains [4].
Depending on the tumour type, location and growth rate, treatment with surgery, radiotherapy or chemotherapy decreases tumour burden, improves (cognitive) functioning and prolongs survival in most brain tumour patients, but may also cause cognitive deficits. In addition, other factors such as supportive treatment with antiepileptic drugs and corticosteroids, as well as concomitant symptoms such as fatigue and mood disorders are also associated with cognitive deficits [6]. Hence, the tumour itself, antitumour and supportive treatment, clinical, psychosocial and genetic factors as well as cognitive reserve [5] can have an impact on cognitive functioning. Preservation of cognitive functioning by minimalizing the negative impact of antitumour and supportive treatment is therefore important. Furthermore, amelioration of cognitive impairment may be achieved by offering interventions such as pharmacological treatment and cognitive rehabilitation.
In this review, we first aim to evaluate antitumour treatment strategies that aim to prevent or minimize cognitive deficits, thereafter we discuss intervention approaches that aim to improve cognitive functioning, covering the recent literature on pharmacological treatment and cognitive rehabilitation.
Box 1.
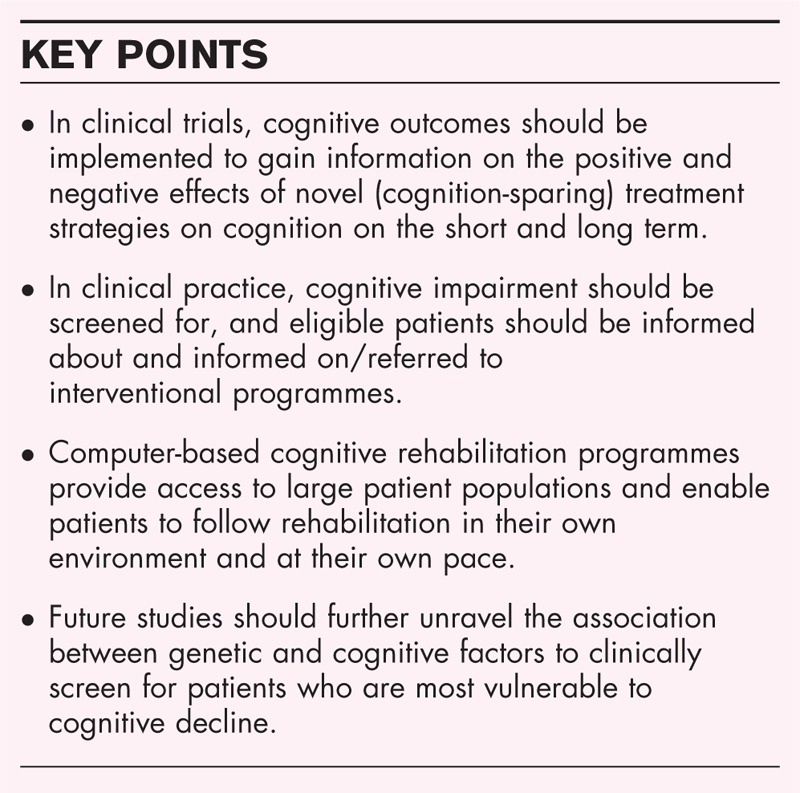
no caption available
TEXT OF REVIEW
Preservation of cognitive functioning
Treatment options for tumour patients often include a combination of surgery, radiotherapy, chemotherapy and supportive treatment.
Surgery
Extensive surgical resection has shown to confer survival benefit in primary brain tumours including gliomas [7], and in general, brain tumour patients experience less seizures, headache and signs of intracranial pressure after surgery. Maximal well tolerated resection while avoiding severe disabling neurological and cognitive deficits is the main challenge in brain tumour patients. Identifying acquired cognitive problems after surgery may be difficult, as presurgery cognitive testing is not always embedded in clinical care, complicating prepost comparison, and deficits are often subtle and may be overshadowed by pronounced and mostly transient speech and motor deficits [8▪]. In glioma patients, studies showed that patients experienced cognitive deficits after surgery [9,10]; however, these were partly transient, and at the individual patient level, postoperative improvement was seen as well [11]. In patients with meningioma, cognitive functioning frequently improves after surgery, but remains significantly lower than in healthy controls [12,13]. Postoperatively, the most affected cognitive domains are memory and executive function [13].
Awake surgery with intraoperative electrical stimulation and real-time monitoring aims to identify brain circuits crucial for cognitive functioning. It allows for more precise resection of the tumour without damaging surrounding tissue, and is thereby assumed to preserve cognitive functioning in glioma patients [14–16]. However, most studies only included follow-up of a few months, and studies on long-term cognitive outcomes after awake surgery are lacking. Also, nowadays, testing during awake tumour resection is mainly focused on the domains of language and motor function in patients with left-hemispheric tumours. More recently, a few explorative studies in brain tumour patients evaluated the feasibility and effects of monitoring other cognitive functions during awake surgery, for example executive functioning (that is inhibition) and working memory [17,18].
Radiation therapy
Radiation may lead to significant, but mostly transient, cognitive disability in 50–90% of the patients, occurring in the acute phase (during radiation), early-delayed (in the first months after radiation) and late-delayed (up to years after radiation) [19▪]. Acute side effects include inflammation and injury to neuronal structures, causing oedema that leads to symptoms such as headache, nausea and dizziness and cognitive deficits. Early-delayed effects are associated with demyelination and oedema, which may affect cognitive functioning as well [20]. Although acute and early-delayed side effects are thought to be transient, late-delayed damage is of the greatest concern, because the related cognitive impairments can be irreversible and progressive. Late-delayed complications may lead to focal deficits (radiation necrosis), and more importantly, to chronic diffuse encephalopathy, which may even result in dementia [21]. In severe cases of late-delayed radiation injury, imaging studies demonstrated diffuse leukoencephalopathy and progressive atrophy [22], while histopathology may show small vessel necrosis in the white matter and depletion of stem cells in the hippocampal area and subventricular zone. However, a larger subgroup of patients experience mild-to-moderate, though persistent cognitive impairment following radiation therapy [22].
Less invasive radiation techniques such as limited fraction dose, stereotactic radiotherapy instead of whole brain radiotherapy [23–25], and sparing the hippocampus during radiation may possibly result in less cognitive problems in patients with primary brain tumours and brain metastases [24]. In addition, proton radiation therapy, which reduces entrance dose and eliminates exit dose, is also expected to contribute to preservation of cognitive functioning by sparing normal tissue to a larger extent [26].
Chemotherapy
Compared with radiation therapy, the adverse effects of chemotherapy on cognitive functioning in brain tumour patients have gained less attention. Distinguishing cognitive deficits caused by chemotherapy is challenging in primary brain tumour patients, as most patients who underwent chemotherapy also underwent surgical resection and radiotherapy. However, late cognitive deficits have been demonstrated in glioma patients, years after radiation and Procarbazine, lomustine and vincristine chemotherapy [27]. In contrast, a systematic review in patients with primary central nervous system (CNS) lymphoma without previous surgery or radiotherapy suggested that cognition improved after induction chemotherapy compared with baseline, presumably also partly due to corticosteroids [28]. For patients with systemic cancer, even without CNS metastases, there is an emerging body of research demonstrating that chemotherapeutic agents may cause cognitive deficits both on the short and long term [29]. Common cognitive domains affected by systemic chemotherapy include learning, memory, information processing speed and executive functioning [30], which has been described as the ‘chemo brain’ [22] or ‘cancer-related cognitive impairment’ (CRCI) [31]. With regard to long-term deficits in these patients, imaging studies have demonstrated structural changes in the brain, including volume reduction and altered white matter integrity [32], which are associated with long-term cognitive problems [29].
There has been little evidence on neuroprotective strategies to prevent chemotherapy-related cognitive impairment in brain tumour patients. Animal studies suggested the possibility of preserving cognitive decline by administration of preventing agents while undergoing chemotherapy [33–36], or exercise to assist in preventing cognitive dysfunction during or after chemotherapy by increasing neurogenesis [36–38], but there are no clinical data.
Targeted therapy and immunotherapy
Angiogenesis inhibitors, such as bevacizumab, have been successful in the treatment of various systemic cancers. However, in glioma patients, there is no evidence for overall survival benefit, nor for decline in (cognitive) functioning [39,40]. Results of trials investigating immunotherapy and their impact on cognitive functioning in patients with glioma [41], CNS lymphoma [42] and meningioma [43] are still to be expected.
Supportive treatment
Factors such as epilepsy, antiepileptic drugs (AEDs) and corticosteroids may affect cognition and behaviour as well. AEDs have a significant negative effect on attention and information processing speed [44], though second-generation AEDs such as levetiracetam and oxcarbazepine seem to minimalize the negative impact of seizures on health-related quality of life (HRQoL) and cognition [45,46]. Perioperative corticosteroids improve cognition because of diminishing oedema, but there is otherwise evidence of detrimental (cognitive) effects of long-term corticosteroid use [6].
Interventions to preserve and improve cognitive functioning
Two approaches are often distinguished when looking at interventions that aim to improve cognitive functioning: pharmacological treatment and cognitive rehabilitation therapy (CRT).
Pharmacological treatment
Pharmacological agents that have been studied in brain tumour patients include amongst others donepezil, armodafinil and modafinil. Table 1 includes trials on pharmacological agents in brain tumour patients, including more than 10 patients [47–55]. In a large randomized controlled trial, the efficacy of memantine, a NMDA receptor antagonist also used in Alzheimer's disease, was found to delay cognitive decline in patients with brain metastases during whole-brain radiotherapy [47], although the trial lacked statistical significance due to patient loss. There has also been interest in donepezil, an acetylcholinesterase inhibitor also used in patients with Alzheimer's disease, and results of three studies in brain tumour patients suggested that donepezil improved some aspects of cognitive functioning, including attention, memory and motor speed [48–50]. Other trials that aimed to investigate methylphenidate [56] and combined levothyroxine/liothyronine supplementation [57] were terminated because of accrual issues. Thus, although some studies reported small successes of pharmacological treatment, limitations including limited sample size, recruitment issues and the lack of a control group to account for practice effects hamper conclusions.
Table 1.
Pharmacological agents for the management of cognitive impairment in brain tumour patients
| Ref. | Pharmacological agent | Study design | Population (n) | Timing | Relevant results |
| Boele et al. [51] | Modafinil | Double-blind, placebo controlled cross-over trial | Primary brain tumour (n = 37) | At baseline, after 6 weeks of modafinil/placebo and 6 weeks after opposite treatment | Modafinil did not exceed the effects of placebo |
| Brown et al. [47] | Memantine | Double-blind, placebo controlled RCT | Brian metastases (n = 508) | At baseline, and at 8, 16, 24 and 52 weeks after the start of WBRT | Memantine delayed time to cognitive decline and reduced the rate of decline in memory, executive function and processing speed |
| Butler et al. [52] | Methylphenidate HCI | Double-blind, placebo controlled RCT | Primary and metastatic brain tumours (n = 68) | At baseline, during and 4, 8 and 12 weeks after RT | No difference in MMSE score between the groups |
| Correa et al. [48] | Donepezil | Pilot | Primary brain tumour (n = 15) | After treatment with RT + CT or CT | A significant postbaseline improvement in attention, motor speed, visual memory |
| Gehring et al. [53] | Methylphenidate and modafinil | Open-label, randomized pilot trial | Primary brain tumour (n = 24) | At baseline and 4 weeks thereafter | Improvement in processing speed and executive functioning |
| Meyers et al. [54] | Methylphenidate | Open-label without control group | High-grade gliomas (n = 30) | At baseline, week 4, 8, 12 thereafter | Improvement in various tests, mood, subjective improvement in 20/26 patients after 4 weeks |
| Rapp et al. [50] | Donepezil | RCT | Primary and metastatic brain tumours (n = 198) | After partial RT or WHBT | Modest improvement in memory and motor speed |
| Page et al. [55] | Armodafinil | Double-blind, placebo-controlled RCT | Meningioma and glioma (n = 54) | At the end of RT and 4 weeks after RT | No difference between the treatment arms on any of the cognitive tests |
| Shaw et al. [49] | Donepezil | Open-label without control group | Primary brain tumours, one metastatic (n = 35) | 6 months post RT | Improvement in various cognitive tests after 24 weeks |
CT, chemotherapy; RCT, randomized controlled trial; RT, radiotherapy; WBRT, whole-brain radiation therapy.
Cognitive rehabilitation
CRT refers to neuropsychological interventions aimed at preventing or treating cognitive deficits, and is based on the principles of neuroplasticity (i.e. learning) and designed to improve cognitive abilities through compensation or retraining. Retraining includes repeated practice of tasks that aim to strengthen impaired cognitive functions. Compensation training focuses on learning new strategies and alternative means to improve daily functioning and achieve goals, for example pacing, breaking down complex task into smaller steps and using mnemonics. The two are often studied in combination. CRT can be provided to individual patients or in groups, at home or in rehabilitation centres and with traditional face-to-face approaches as well as through computerized programs. In other patient populations, such as stroke patients and traumatic brain injury patients, CRT has shown to be effective and is often incorporated in the standard of care [58,59]. In brain tumour patients, a number of cognitive intervention programmes have been developed (see Table 2) [60–67]. Although often hampered by methodological issues, for example not all studies included a control group to rule out effects of practice and natural recovery [60], most programmes reported some improvements in cognitive test-performance [61–65] and also with regard to subjective cognitive functioning [66]. Similar to the pharmaceutical trials, problems with accrual have been reported in several trials, especially when CRT was offered in the early disease stage. There is no consensus on the optimal timing for CRT. If the aim is to minimize or prevent cognitive problems due to adjuvant treatment and to make the most use of still intact skills, CRT should start as early as possible [6,64,68]. An early cognitive training programme for early postsurgery primary brain tumour patients showed that cognitive functioning already improved after a few weeks [64]. Conversely, as patients with newly diagnosed brain tumours often undergo multiple time-consuming and intensive treatment regimens that may also cause cognitive problems, offering rehabilitation after antitumour treatment may be fit best for patients with a longer prognosis both in terms of timing and in terms of effectiveness. At this time, patients also attempt to resume their normal daily activities and return to work and then start to experience cognitive problems. Consequently, flexible computer-based CRT programmes that can be adjusted to the specific patient needs and can be administered at home may especially be suitable.
Table 2.
Cognitive rehabilitation interventions targeting cognitive impairment in brain tumour patients
| Ref. | Intervention outline | Study design | Population (n) | Timing | Effect on cognition |
| Gehring et al. [66] | Weekly individual supervised compensation training and computerized retraining | RCT | Low-grade and anaplastic gliomas (n = 140) | At least 6 months postsurgery | Improvement in short-term cognitive complaints, long-term cognitive functioning and mental fatigue |
| Hassler et al. [65] | Compensatory training. Weekly group training sessions for attention, verbal and memory skills | RCT | Grade III and IV glioma patients (n = 11) | Postsurgery, RT and CT | Modest improvement in memory and attention |
| Maschio et al. [63] | Cognitive rehabilitation training (RehabTR). Weekly sessions using computerized retraining | Pilot study | Patients with brain tumour related epilepsy (n = 16) | Postsurgery | Improvements in short-term verbal memory, episodic memory, fluency and long-term visuospatial memory improved immediately and at 6-month follow-up |
| Sacks-Zimmerman et al. [67] | CogMed: Computer-based cognitive remediation therapy (CRT) | Prospective pilot study | Low-grade glioma patients (n = 3) | Postsurgery | Results of only three patients have been published |
| Richard et al. [61] | Goal Management Training (GMT): Behavioural intervention combining mindfulness and strategy training | Pilot randomized trial (three groups) | Primary brain tumour patients (n = 26) | Postsurgery and >3 months post possible RT and/or CT | Executive functioning improved at 4-month follow-up |
| Van der Linden et al. [60] | ReMind: iPad-based psycho-education, strategy training and retraining | Feasibility study | Low-grade glioma and meningioma (n = 15) | Before surgery or other treatment | Intervention was found to be feasible, results of the RCT are expected |
| Yang et al. [62] | Virtual reality: Computer-based cognitive rehabilitation program | Trial comparing VR and computerized retraining with computerized retraining | Primary brain tumour patients (n = 38) | After surgery, and further treatment with RT/CT | Improvement in visual and auditory attention, short-term visual spatial memory |
| Zucchella et al. [64] | Compensation training and computerized training | RCT | Primary brain tumour patients [62] | Postsurgery | Improvement of visual attention and verbal memory |
CT, chemotherapy; RCT, randomized controlled trial; RT, radiotherapy; VR, virtual reality.
Other interventions
Given the overlapping impact of both cognitive and emotional problems, intervention programmes that address outcomes as HRQoL, fatigue, mood or a combination of these may have indirect positive effects on cognitive functioning as well. Several uncontrolled studies that investigated psychological/psychosocial interventions [69,70] and yoga [71] in brain tumour patients showed to be feasible, reported some successes with regard to various HRQoL outcomes and were highly appreciated by patients. In addition, several exercise programmes in glioma patients similarly showed to be feasible, improved functional outcome [72,73] and suggested to have positive outcomes with respect to HRQoL outcomes [74,75,76]. In meningioma patients, uncontrolled studies on exercise programmes found decreased symptoms of depression and insomnia [77], and improved functional outcome [78].
CONCLUSION AND FUTURE OPPORTUNITIES
During the past years, cognitive functioning has gained greater awareness in the neurooncological community. More clinical trials have included cognitive performance as an endpoint, and methods to preserve and improve cognitive functioning have been explored. Important long-term data with regard to novel cognition-sparing treatment strategies such as awake surgery, hippocampal sparing and proton therapy are awaited.
The implementation of the so-called personalized or precision medicine into clinical practice allows optimization of therapy based on the patients’ individual (genetic) profile, in order to maximize the therapeutic effect and minimalize side effects. More specifically, patients vulnerable to cognitive decline might be identified at an early stage, which allows for personalized and timely intervention. Recent studies have highlighted the importance of molecular markers in neurooncology, and their link with cognitive functioning. Glioma patients with isocitrate dehydrogenase 1 (IDH1) mutant gene may exhibit less cognitive impairment than their wild-type counterparts [5,79]. With regard to germline genetic characteristics, studies have suggested that the APOE ε4 allele, a known risk factor for Alzheimer's disease [80], single nucleotide polymorphisms in the catechol-O-methyl transferase (COMT), brain-derived neurotrophic factor (BDNF) and dystrobrevin-binding protein one (DTNBP1) genes are associated with (impaired) cognitive functioning in brain tumour patients as well [81]. The evidence so far is, however, insufficient to implement formally testing of these genetic polymorphisms in clinical practice.
Acknowledgements
None.
Financial support and sponsorship
SvdL and KG: the Dutch organization for health research and innovation (ZonMw) (grant number: 842003009).
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Meyers CA, Smith JA, Bezjak A, et al. Neurocognitive function and progression in patients with brain metastases treated with whole-brain radiation and motexafin gadolinium: results of a randomized phase III trial. J Clin Oncol 2004; 22:157–165. [DOI] [PubMed] [Google Scholar]
- 2.Tucha O, Smely C, Preier M, Lange KW. Cognitive deficits before treatment among patients with brain tumors. Neurosurgery 2000; 47:324–333. discussion 33-34. [DOI] [PubMed] [Google Scholar]
- 3.Taphoorn MJ, Klein M. Cognitive deficits in adult patients with brain tumours. Lancet Neurol 2004; 3:159–168. [DOI] [PubMed] [Google Scholar]
- 4.Wefel JS, Noll KR, Scheurer ME. Neurocognitive functioning and genetic variation in patients with primary brain tumours. Lancet Oncol 2016; 17:e97–e108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kesler SR, Noll K, Cahill DP, et al. The effect of IDH1 mutation on the structural connectome in malignant astrocytoma. J Neurooncol 2017; 131:565–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Day J, Gillespie DC, Rooney AG, et al. Neurocognitive deficits and neurocognitive rehabilitation in adult brain tumors. Curr Treat Options Neurol 2016; 18:22. [DOI] [PubMed] [Google Scholar]
- 7.Brown TJ, Brennan MC, Li M, et al. Association of the extent of resection with survival in glioblastoma: a systematic review and meta-analysis. JAMA Oncol 2016; 2:1460–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8▪.Ng JCH, See AAQ, Ang TY, et al. Effects of surgery on neurocognitive function in patients with glioma: a meta-analysis of immediate postoperative and long-term follow-up neurocognitive outcomes. J Neurooncol 2019; 141:167–182. [DOI] [PubMed] [Google Scholar]; A review and meta-analysis describes commonly used neuropsychological tests and quantifies postoperative changes in cognitive function.
- 9.Talacchi A, Santini B, Savazzi S, Gerosa M. Cognitive effects of tumour and surgical treatment in glioma patients. J Neurooncol 2011; 103:541–549. [DOI] [PubMed] [Google Scholar]
- 10.Satoer D, Vork J, Visch-Brink E, et al. Cognitive functioning early after surgery of gliomas in eloquent areas. J Neurosurg 2012; 117:831–838. [DOI] [PubMed] [Google Scholar]
- 11.Habets EJ, Kloet A, Walchenbach R, et al. Tumour and surgery effects on cognitive functioning in high-grade glioma patients. Acta Neurochir (Wien) 2014; 156:1451–1459. [DOI] [PubMed] [Google Scholar]
- 12.Rijnen SJM, Meskal I, Bakker M, et al. Cognitive outcomes in meningioma patients undergoing surgery: individual changes over time and predictors of late cognitive functioning. Neuro Oncol 2019; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meskal I, Gehring K, Rutten GJ, Sitskoorn MM. Cognitive functioning in meningioma patients: a systematic review. J Neurooncol 2016; 128:195–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.De Witt Hamer PC, Robles SG, Zwinderman AH, et al. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol 2012; 30:2559–2565. [DOI] [PubMed] [Google Scholar]
- 15.Satoer D, Visch-Brink E, Dirven C, Vincent A. Glioma surgery in eloquent areas: can we preserve cognition? Acta Neurochir (Wien) 2016; 158:35–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muto J, Dezamis E, Rigaux-Viode O, et al. Functional-based resection does not worsen quality of life in patients with a diffuse low-grade glioma involving eloquent brain regions: a prospective cohort study. World Neurosurg 2018; 113:e200–e212. [DOI] [PubMed] [Google Scholar]
- 17.Puglisi G, Sciortino T, Rossi M, et al. Preserving executive functions in nondominant frontal lobe glioma surgery: an intraoperative tool. J Neurosurg 2018. 1–7. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 18.Motomura K, Chalise L, Ohka F, et al. Neurocognitive and functional outcomes in patients with diffuse frontal lower-grade gliomas undergoing intraoperative awake brain mapping. J Neurosurg 2019. 1–9. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 19▪.Makale MT, McDonald CR, Hattangadi-Gluth JA, Kesari S. Mechanisms of radiotherapy-associated cognitive disability in patients with brain tumours. Nat Rev Neurol 2017; 13:52–64. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reviews the underlying mechanisms of radiation-induced cognitive deficits in brain tumour patients.
- 20.Durand T, Bernier MO, Leger I, et al. Cognitive outcome after radiotherapy in brain tumor. Curr Opin Oncol 2015; 27:510–515. [DOI] [PubMed] [Google Scholar]
- 21.Crossen JR, Garwood D, Glatstein E, Neuwelt EA. Neurobehavioral sequelae of cranial irradiation in adults: a review of radiation-induced encephalopathy. J Clin Oncol 1994; 12:627–642. [DOI] [PubMed] [Google Scholar]
- 22.Dietrich J, Monje M, Wefel J, Meyers C. Clinical patterns and biological correlates of cognitive dysfunction associated with cancer therapy. Oncologist 2008; 13:1285–1295. [DOI] [PubMed] [Google Scholar]
- 23.Brown PD, Jaeckle K, Ballman KV, et al. Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases: a randomized clinical trial. JAMA 2016; 316:401–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Habets EJ, Dirven L, Wiggenraad RG, et al. Neurocognitive functioning and health-related quality of life in patients treated with stereotactic radiotherapy for brain metastases: a prospective study. Neuro Oncol 2016; 18:435–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Okoukoni C, McTyre ER, Peacock DNA, et al. Hippocampal dose volume histogram predicts Hopkins Verbal Learning Test scores after brain irradiation. Adv Radiat Oncol 2017; 2:624–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherman JC, Colvin MK, Mancuso SM, et al. Neurocognitive effects of proton radiation therapy in adults with low-grade glioma. J Neurooncol 2016; 126:157–164. [DOI] [PubMed] [Google Scholar]
- 27.Habets EJ, Taphoorn MJ, Nederend S, et al. Health-related quality of life and cognitive functioning in long-term anaplastic oligodendroglioma and oligoastrocytoma survivors. J Neurooncol 2014; 116:161–168. [DOI] [PubMed] [Google Scholar]
- 28.van der Meulen M, Dirven L, Habets EJJ, et al. Cognitive functioning and health-related quality of life in patients with newly diagnosed primary CNS lymphoma: a systematic review. Lancet Oncol 2018; 19:e407–e418. [DOI] [PubMed] [Google Scholar]
- 29.Schagen SB, Wefel JS. Chemotherapy-related changes in cognitive functioning. EJC Suppl 2013; 11:225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wefel J, Kayl A, Meyers C. Neuropsychological dysfunction associated with cancer and cancer therapies: a conceptual review of an emerging target. Br J Cancer 2004; 90:1691–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Janelsins MC, Kesler SR, Ahles TA, Morrow GR. Prevalence, mechanisms, and management of cancer-related cognitive impairment. Int Rev Psychiatry 2014; 26:102–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wefel JS, Schagen SB. Chemotherapy-related cognitive dysfunction. Curr Neurol Neurosci Rep 2012; 12:267–275. [DOI] [PubMed] [Google Scholar]
- 33.Chiu GS, Maj MA, Rizvi S, et al. Pifithrin-μ prevents cisplatin-induced chemobrain by preserving neuronal mitochondrial function. Cancer Res 2017; 77:742–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shi D-D, Dong CM, Ho LC, et al. Resveratrol, a natural polyphenol, prevents chemotherapy-induced cognitive impairment: involvement of cytokine modulation and neuroprotection. Neurobiol Dis 2018; 114:164–173. [DOI] [PubMed] [Google Scholar]
- 35.Zhou W, Kavelaars A, Heijnen CJ. Metformin prevents cisplatin-induced cognitive impairment and brain damage in mice. PLoS One 2016; 11:e0151890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fardell JE, Vardy J, Shah JD, Johnston IN. Cognitive impairments caused by oxaliplatin and 5-fluorouracil chemotherapy are ameliorated by physical activity. Psychopharmacology 2012; 220:183–193. [DOI] [PubMed] [Google Scholar]
- 37.Monje M, Dietrich J. Cognitive side effects of cancer therapy demonstrate a functional role for adult neurogenesis. Behav Brain Res 2012; 227:376–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Park HS, Kim CJ, Kwak HB, et al. Physical exercise prevents cognitive impairment by enhancing hippocampal neuroplasticity and mitochondrial function in doxorubicin-induced chemobrain. Neuropharmacology 2018; 133:451–461. [DOI] [PubMed] [Google Scholar]
- 39.Chinot OL, Wick W, Mason W, et al. Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. N Engl J Med 2014; 370:709–722. [DOI] [PubMed] [Google Scholar]
- 40.Gilbert MR, Dignam JJ, Armstrong TS, et al. A randomized trial of bevacizumab for newly diagnosed glioblastoma. N Engl J Med 2014; 370:699–708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roth P, Preusser M, Weller M. Immunotherapy of brain cancer. Oncol Res Treat 2016; 39:326–334. [DOI] [PubMed] [Google Scholar]
- 42.Rubenstein JL, Hsi ED, Johnson JL, et al. Intensive chemotherapy and immunotherapy in patients with newly diagnosed primary CNS lymphoma: CALGB 50202 (Alliance 50202). J Clin Oncol 2013; 31:3061–3068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Du Z, Abedalthagafi M, Aizer AA, et al. Increased expression of the immune modulatory molecule PD-L1 (CD274) in anaplastic meningioma. Oncotarget 2015; 6:4704–4716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Eddy CM, Rickards HE, Cavanna AE. The cognitive impact of antiepileptic drugs. Ther Adv Neurol Disord 2011; 4:385–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maschio M, Dinapoli L, Sperati F, et al. Levetiracetam monotherapy in patients with brain tumor-related epilepsy: seizure control, safety, and quality of life. J Neurooncol 2011; 104:205–214. [DOI] [PubMed] [Google Scholar]
- 46.Maschio M, Dinapoli L, Sperati F, et al. Oxcarbazepine monotherapy in patients with brain tumor-related epilepsy: open-label pilot study for assessing the efficacy, tolerability and impact on quality of life. J Neurooncol 2012; 106:651–656. [DOI] [PubMed] [Google Scholar]
- 47.Brown PD, Pugh S, Laack NN, et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol 2013; 15:1429–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Correa DD, Kryza-Lacombe M, Baser RE, et al. Cognitive effects of donepezil therapy in patients with brain tumors: a pilot study. J Neurooncol 2016; 127:313–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shaw EG, Rosdhal R, D’Agostino RB, Jr, et al. Phase II study of donepezil in irradiated brain tumor patients: effect on cognitive function, mood, and quality of life. J Clin Oncol 2006; 24:1415–1420. [DOI] [PubMed] [Google Scholar]
- 50.Rapp SR, Case LD, Peiffer A, et al. Donepezil for irradiated brain tumor survivors: a phase III randomized placebo-controlled clinical trial. J Clin Oncol 2015; 33:1653–1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Boele FW, Douw L, de Groot M, et al. The effect of modafinil on fatigue, cognitive functioning, and mood in primary brain tumor patients: a multicenter randomized controlled trial. Neuro Oncol 2013; 15:1420–1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Butler JM, Jr, Case LD, Atkins J, et al. A phase III, double-blind, placebo-controlled prospective randomized clinical trial of d-threo-methylphenidate HCl in brain tumor patients receiving radiation therapy. Int J Radiat Oncol Biol Phys 2007; 69:1496–1501. [DOI] [PubMed] [Google Scholar]
- 53.Gehring K, Patwardhan SY, Collins R, et al. A randomized trial on the efficacy of methylphenidate and modafinil for improving cognitive functioning and symptoms in patients with a primary brain tumor. J Neurooncol 2012; 107:165–174. [DOI] [PubMed] [Google Scholar]
- 54.Meyers CA, Weitzner MA, Valentine AD, Levin VA. Methylphenidate therapy improves cognition, mood, and function of brain tumor patients. J Clin Oncol 1998; 16:2522–2527. [DOI] [PubMed] [Google Scholar]
- 55.Page BR, Shaw EG, Lu L, et al. Phase II double-blind placebo-controlled randomized study of armodafinil for brain radiation-induced fatigue. Neuro Oncol 2015; 17:1393–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wefel JS. Effects of methylphenidate versus sustained release methylphenidate on cognitive functioning http://clinicaltrials.gov/ct2/show/NCT00418691. [Google Scholar]
- 57. [[Accessed 27 August 2019]]. MD Anderson Cancer Center. L. L. Combined levothyroxine/liothyronine supplementation in hypothyroid patients with brain tumors. https://clinicaltrials.gov/ct2/show/NCT00488644. [Google Scholar]
- 58.Koehler R, Wilhelm E, Shoulson I. Cognitive rehabilitation therapy for traumatic brain injury: evaluating the evidence. Washington, D.C.: National Academies Press; 2012. [Google Scholar]
- 59.Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet 2011; 377:1693–1702. [DOI] [PubMed] [Google Scholar]
- 60.van der Linden SD, Sitskoorn MM, Rutten GM, Gehring K. Feasibility of the evidence-based cognitive telerehabilitation program Remind for patients with primary brain tumors. J Neurooncol 2018; 137:523–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Richard NM, Bernstein LJ, Mason WP, et al. Cognitive rehabilitation for executive dysfunction in brain tumor patients: a pilot randomized controlled trial. J Neurooncol 2019; 142:565–575. [DOI] [PubMed] [Google Scholar]
- 62.Yang S, Chun MH, Son YR. Effect of virtual reality on cognitive dysfunction in patients with brain tumor. Ann Rehabil Med 2014; 38:726–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Maschio M, Dinapoli L, Fabi A, et al. Cognitive rehabilitation training in patients with brain tumor-related epilepsy and cognitive deficits: a pilot study. J Neurooncol 2015; 125:419–426. [DOI] [PubMed] [Google Scholar]
- 64.Zucchella C, Capone A, Codella V, et al. Cognitive rehabilitation for early postsurgery inpatients affected by primary brain tumor: a randomized, controlled trial. J Neurooncol 2013; 114:93–100. [DOI] [PubMed] [Google Scholar]
- 65.Hassler MR, Elandt K, Preusser M, et al. Neurocognitive training in patients with high-grade glioma: a pilot study. J Neurooncol 2010; 97:109–115. [DOI] [PubMed] [Google Scholar]
- 66.Gehring K, Sitskoorn MM, Gundy CM, et al. Cognitive rehabilitation in patients with gliomas: a randomized, controlled trial. J Clin Oncol 2009; 27:3712–3722. [DOI] [PubMed] [Google Scholar]
- 67.Sacks-Zimmerman A, Duggal D, Liberta T. Cognitive remediation therapy for brain tumor survivors with cognitive deficits. Cureus 2015; 7:e350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Langbecker D, Yates P. Primary brain tumor patients’ supportive care needs and multidisciplinary rehabilitation, community and psychosocial support services: awareness, referral and utilization. J Neurooncol 2016; 127:91–102. [DOI] [PubMed] [Google Scholar]
- 69.Jones S, Ownsworth T, Shum DH. Feasibility and utility of telephone-based psychological support for people with brain tumor: a single-case experimental study. Front Oncol 2015; 5:71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Locke DE, Cerhan JH, Wu W, et al. Cognitive rehabilitation and problem-solving to improve quality of life of patients with primary brain tumors: a pilot study. J Support Oncol 2008; 6:383–391. [PubMed] [Google Scholar]
- 71.Milbury K, Mallaiah S, Mahajan A, et al. Yoga program for high-grade glioma patients undergoing radiotherapy and their family caregivers. Integr Cancer Ther 2018; 17:332–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bartolo M, Zucchella C, Pace A, et al. Early rehabilitation after surgery improves functional outcome in inpatients with brain tumours. J Neurooncol 2012; 107:537–544. [DOI] [PubMed] [Google Scholar]
- 73.Gehring K, Kloek CJ, Aaronson NK, et al. Feasibility of a home-based exercise intervention with remote guidance for patients with stable grade II and III gliomas: a pilot randomized controlled trial. Clin Rehabil 2018; 32:352–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Nicole Culos-Reed S, Leach HJ, Capozzi LC, et al. Exercise preferences and associations between fitness parameters, physical activity, and quality of life in high-grade glioma patients. Support Care Cancer 2017; 25:1237–1246. [DOI] [PubMed] [Google Scholar]
- 75.Baima J, Omer ZB, Varlotto J, Yunus S. Compliance and safety of a novel home exercise program for patients with high-grade brain tumors, a prospective observational study. Support Care Cancer 2017; 25:2809–2814. [DOI] [PubMed] [Google Scholar]
- 76.Cormie P, Nowak AK, Chambers SK, et al. The potential role of exercise in neuro-oncology. Front Oncol 2015; 5:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Colledge F, Brand S, Puhse U, et al. A twelve-week moderate exercise programme improved symptoms of depression, insomnia, and verbal learning in post-aneurysmal subarachnoid haemorrhage patients: a comparison with meningioma patients and healthy controls. Neuropsychobiology 2017; 76:59–71. [DOI] [PubMed] [Google Scholar]
- 78.Han EY, Chun MH, Kim BR, Kim HJ. Functional improvement after 4-week rehabilitation therapy and effects of attention deficit in brain tumor patients: comparison with subacute stroke patients. Ann Rehabil Med 2015; 39:560–569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wefel JS, Noll KR, Rao G, Cahill DP. Neurocognitive function varies by IDH1 genetic mutation status in patients with malignant glioma prior to surgical resection. Neuro Oncol 2016; 18:1656–1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Corder EH, Saunders AM, Strittmatter WJ, et al. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer's disease in late onset families. Science 1993; 261:921–923. [DOI] [PubMed] [Google Scholar]
- 81.Correa DD, Satagopan J, Cheung K, et al. COMT, BDNF, and DTNBP1 polymorphisms and cognitive functions in patients with brain tumors. Neuro Oncol 2016; 18:1425–1433. [DOI] [PMC free article] [PubMed] [Google Scholar]


