Abstract
While prior studies have investigated health care utilization immediately following disasters, few have examined utilization beyond that period. We use individual-level U.S. Medicare claims data for three years prior to (2002–2004) and after (2006–2008) Hurricanes Katrina and Rita to investigate whether senior diabetics affected by the storms had a greater number of emergency department visits and days hospitalized in the three years following the storms. An event study was conducted using regression analysis that controlled for all fixed individual characteristics. While the 2006 and 2007 rates of increase in utilization were relatively similar across the control group and the two affected groups, in 2008 the affected groups exhibited substantially greater increases in both emergency department visits and days hospitalized. The differences correspond to an additional 380,907 days hospitalized and 21,583 emergency department visits in 2008. The results indicate that, in addition to short term effects previously estimated, disasters may have longer term effects on utilization of healthcare services. These potential effects suggest that improved post-disaster care may significantly reduce the healthcare costs of disasters.
Introduction
Disasters can pose special challenges for diabetics. The condition requires significant patient effort, including diet, exercise, and medication adherence. In the short term, disasters can lead to disrupted provider access, inability to monitor glucose, poor nutrition, limited physical activity, damaged or lost medications, and an inability to refill prescriptions (Lee et al. 2014). These immediate challenges can lead to long term effects. Due to effort required in other aspects of life, some patients may not recover from the initial impact of a disaster and may not resume their necessary care. For instance, affected senior diabetics were found to have lower rates of routine screens up to three years following Hurricane Katrina (Quast and Feng, forthcoming). Not only can care and medication interruptions result in an increase in emergency department (ED) visits and hospitalizations immediately following the disaster, medication nonadherence has been linked to increased ED visits and hospitalizations over three- and five-year periods (Hepke et al. 2004; Ho et al. 2006; Lau et al. 2004; Egede et al. 2012).
Nearly all of the research on ED and inpatient utilization following disasters has focused on the period immediately following the event. Hurricane Katrina was associated with immediate increased ED visit rates in both the New Orleans area (Sharma et al. 2008) and in Texas (Mortensen et al. 2008; Quast et al. 2012), while seniors in a Medicare Advantage plan who lived in New Orleans before Katrina were found to have 21% higher ED visits rates during the year after than the year prior to the storm (Burton et al. 2009). End stage renal disease patients in affected areas had higher hospitalization rates immediately following Katrina (Anderson et al. 2009; Howard et al. 2012) while the study of Medicare Advantage plan members found one-year hospitalization rates 23% higher than in the year prior to Katrina (Burton et al. 2009). Investigations of Superstorm Sandy also found increased ED utilization anywhere from one to three months after the storm (Lee et al. 2016; Gotanda et al. 2015; He et al. 2016). Among ESRD patients, relative to control groups the rates of ED visits and hospitalizations were higher for those affected by Sandy by 100% and 50%, respectively (Kelman et al. 2015). Following a 2011 series of tornadoes in the Southeast U.S., the 30-day all-cause admission rate was 4% higher for older adults (Bell et al. 2018).
This study tests whether there was an association between exposure to Hurricanes Katrina and Rita and the rates of ED visits and days hospitalized. Individual-level Medicare claims data are employed for the three years prior to and after the storms for the states of Louisiana, Mississippi, Texas, and Alabama. Individuals are classified by their exposure to the hurricanes according to the assistance level assigned by the U.S. Federal Emergency Management Agency (FEMA) to their county. The primary contribution of this study to the literature is to explore a longer potential window of effects than typically studied. The focus is on senior diabetics, a large and growing population. Rather than relying on diagnoses from an individual visit, the diabetes determination is based on an algorithm defined by the U.S. Centers for Medicare & Medicaid Services (CMS) that incorporates multiple aspects of a patients’ clinical history. The regression analysis is enhanced by the use of administrative data, a plausible control group that provides a useful counterfactual, and individual fixed effects which control for all individual-level factors that do not vary over the sample period.
Methods
Data and Study Sample
Enrollment and encounter claims data from the U.S. CMS for Medicare enrollees diagnosed with diabetes as of 2004 living in Louisiana, Mississippi, Texas, and Alabama are employed. The enrollment data contains for each enrollee demographic information, including gender, race, age, and geographic location. These data also include Medicare enrollment variables that detail individual’s type of coverage, such as whether they are covered in a fee-for-service or capitated plan. Annual data are used for the periods 2002–2004 and 2006–2008. Hurricanes Katrina and Rita struck in 2005 in August and September, respectively. Given concerns regarding the quality of the data in the aftermath of the storms, 2005 is excluded from the analysis.
The sample is limited to enrollees between 65–100 years of age who lived in the same county throughout the 2002–2004 period. We impose the latter condition to ensure that the individual had an established residence in the county prior to the hurricanes and thus that the the county-level FEMA designation assignment is accurate. Other than being in one of our four sample states, there are no restrictions on the individual’s residence during the 2006–2008 period and we allow for enrollees to move between the four states after the hurricanes.
Individuals had to be alive and present in the data for one of our four sample states for each year of the sample period. Because claims data are not available for Medicare Advantage plans, enrollees with any Medicare Advantage coverage are excluded. To ensure that we observe all utilization, we limit the sample to individuals were enrolled in Medicare Part A coverage for every month of our sample period. The final sample consisted of 1,503,571 individuals.
FEMA Designation Levels
After the President declares a major disaster, FEMA conducts a Preliminary Damage Assessment (PDA). PDAs take into account a number of factors, including the concentration of damages, degree of trauma, the presence of special populations, and the amount of available private insurance (Reese, 2018). While PDAs help determine the type of federal assistance a county receives, there are not precise criteria that FEMA follows in their decision. The two primary assistance levels are individual and public, where individual assistance provides greater benefits. The designations were used to categorize counties by the hurricanes’ impact into three groups: individual assistance, public assistance, and no assistance. As FEMA issued separate designations for Katrina and Rita, some counties in the sample had two different assistance levels. In these instances, the designation associated with the greater level of assistance is used.
Outcome Variables
The two outcome variables were the annual number of ED visits and days hospitalized. The days hospitalized measure included acute inpatient, skilled nursing facility, and other inpatient admissions.
Data Analysis
In addition to descriptive analyses of aggregated data, the primary analysis consisted of an event study which utilized regression estimation of individual-year level data. Two models were estimated: one using number of ED visits as the dependent variable and another which used days hospitalized.
The estimation equations were:
| (1) |
| (2) |
where i denotes the individual, f denotes the FEMA county designation, and y denotes the year. δi are individual fixed effects that control for any factors that affected the dependent variable that did not vary during the sample period. The inclusion of individual fixed effects implies that it is not possible to include explanatory variables that are constant throughout the sample period (e.g., age, race). γy are year fixed effects that controlled for any factor common to all beneficiaries that were specific to a given year. For example, the 2007 year fixed effect controls for any factors common to all four states that affected the dependent variable for the sample subjects.
The coefficients of interest are represented by θ. The terms following it in Equations (1) and (2) are the interactions of the year indicator variables with the FEMA designation indicator variables (ρf) and measured the difference in the dependent variable for that designation group and year.
The analysis was performed in Stata version 14.0 (Stata Corporation, College Station, Texas, USA). Our study was approved under an expedited review by the [institution] Institutional Review Board.
Results
The sample characteristics by FEMA assistance level are shown in Table 1. Approximately 60% of the sample subjects were in the Public group. Nearly all of the individuals in the None group lived in Alabama prior to the hurricanes, while the vast majority of the Public group lived in Texas. The similarities of most of the demographic proportions across the three groups suggested differences observed in ED usage and hospitalizations were possibly due to the hurricanes. Roughly 60% of the subjects across the three groups were women, while those aged between 65 and 75 years comprised a similar proportion across the groups. There were differences in race/ethnicity, where the Public group had a larger proportion of Hispanic members due to Texas comprising a large proportion. The Individual and Public groups both had lower proportions of non-Hispanic whites than the None group, while the proportion of Blacks in the None group was roughly the average of the proportions in the other two groups. The proportion of enrollees who were lived in different counties in 2004 and 2006 (i.e., before and after the hurricanes) ranged from 3.3% in the None group to 6.6% in the Individual group.
Table 1.
Sample characteristics by FEMA assistance level.
| None (n=153,339) | Individual (n=456,218) | Public (n=893,886) | |
|---|---|---|---|
| Pre-hurricane state, n (%) | |||
| Alabama | 150,059 (97.9) | 43,889 (9.6) | 55,595 (6.2) |
| Louisiana | 3,280 (2.1) | 115,853 (25.4) | 79,233 (8.9) |
| Mississippi | 0 (0.0) | 108,617 (23.8) | 53,695 (6.0) |
| Texas | 0 (0.0) | 187,859 (41.2) | 705,363 (78.9) |
| Gender, n (%) | |||
| Female | 94,811 (61.8) | 278,084 (61.0) | 541,606 (60.6) |
| Male | 58,528 (38.2) | 178,134 (39.0) | 352,280 (39.4) |
| Age in years, n (%) | |||
| 65–69 | 46,037 (30.0) | 129,669 (28.4) | 235,585 (28.4) |
| 70–74 | 47,918 (31.2) | 140,424 (30.8) | 274,091 (30.7) |
| 75–79 | 33,422 (21.8) | 105,330 (23.1) | 200,740 (22.5) |
| 80–84 | 17,946 (11.7) | 56,017 (12.3) | 113,451 (12.7) |
| 85+ | 8,016 (5.2) | 24,778 (5.4) | 52,019 (5.8) |
| Race/ethnicity, n (%) | |||
| Non-Hispanic white | 134,333 (87.6) | 369,731 (81.0) | 698,813 (78.2) |
| Black | 17,867 (11.7) | 65,876 (14.4) | 68,849 (7.7) |
| Hispanic | 418 (0.3) | 14,002 (3.1) | 116,536 (13.0) |
| Other | 721 (0.4) | 6,609 (1.4) | 9,688 (1.1) |
| Lived in different counties in 2004 and 2006, n (%) | |||
| No | 148,230 (96.7) | 426,244 (93.4) | 856,076 (95.8) |
| Yes | 5,109 (3.3) | 29,974 (6.6) | 37,810 (4.2) |
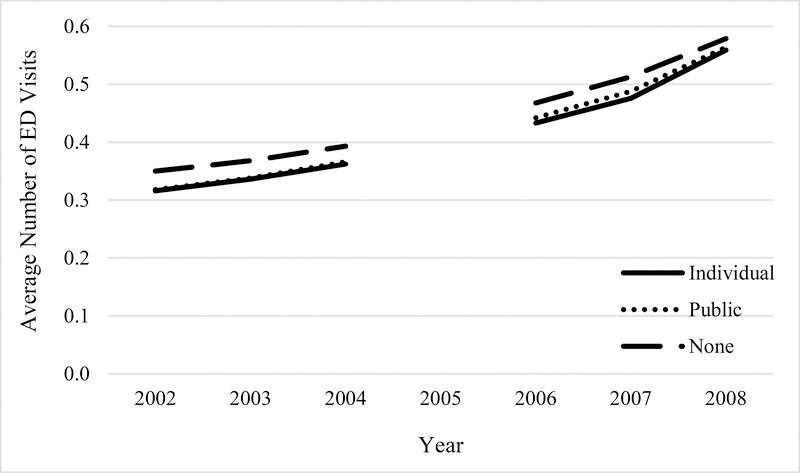
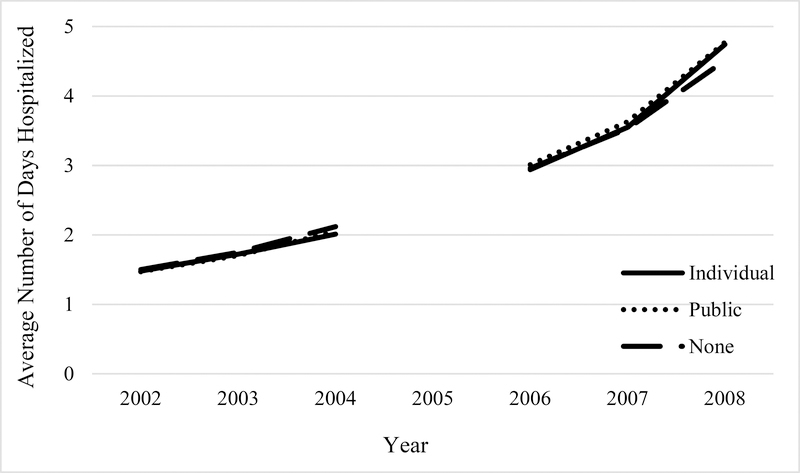
Figures 1 and 2 show the average ED visits and days hospitalized for the three groups. A key requirement of analytic approach was parallel trends in the outcome variables in the period before the hurricanes. The figures suggest that this requirement was satisfied. Figure 1 shows that, while somewhat greater than the averages of the Individual and Public groups, the None group had a similar slope to those groups in the 2002–2004 period. Figure 2 shows an even tighter relationship between the averages of the three groups. Across both figures, the averages maintained roughly similar slopes in 2006 and 2007, but in 2008 the averages of the Individual and Public groups exhibited greater rates of increase than the None group.
Figure 1.
Average number of emergency department visits per person by FEMA assistance level, 2002–2004 and 2006–2008.
Figure 2.
Average number of days hospitalized per person by FEMA assistance level, 2002–2004 and 2006–2008.
Table 2 reports the coefficient estimates of the variables that are the interaction (product) of the group and year indicator variables. The top section reports the estimates for the regression in which the number of ED visits was the dependent variable, while the bottom section reports estimates where days hospitalized was the dependent variable. The “None” column reports the coefficient estimate for the interaction of the None group indicator variable and the respective year indicator variable. The first column in the “Individual” column set reports the corresponding coefficients for the Individual group. The second column (“Diff”) is the difference between the Individual coefficient and the None coefficient for that year, while the third column (“P-value”) reports the p-value of a two-sided test of equivalence between the two coefficients. The “Public” column set reports the corresponding values for the Public group.
Table 2.
Regression interaction coefficients for number of emergency department visits and days hospitalized models by FEMA assistance level.
| None (n=153,339) | Individual (n=456,218) | Public (n=893,886) | |||||
|---|---|---|---|---|---|---|---|
| Variable / year | Coef.a | Coef.a | Diff.b | P-valuec | Coef.a | Diff.b | P-valuec |
| ED visits | |||||||
| 2003 | 0.018 | 0.020 | 0.002 | 0.48 | 0.020 | 0.002 | 0.45 |
| 2004 | 0.044 | 0.046 | 0.002 | 0.43 | 0.048 | 0.005 | 0.11 |
| 2006 | 0.118 | 0.117 | −0.001 | 0.66 | 0.124 | 0.007 | 0.06 |
| 2007 | 0.163 | 0.159 | −0.003 | 0.33 | 0.170 | 0.007 | 0.04 |
| 2008 | 0.229 | 0.243 | 0.014 | < 0.001 | 0.246 | 0.017 | < 0.001 |
| Hospitalized days | |||||||
| 2003 | 0.243 | 0.239 | −0.004 | 0.89 | 0.227 | −0.016 | 0.53 |
| 2004 | 0.614 | 0.533 | −0.081 | 0.01 | 0.577 | −0.037 | 0.22 |
| 2006 | 1.452 | 1.460 | 0.008 | 0.85 | 1.537 | 0.085 | 0.02 |
| 2007 | 2.022 | 2.066 | 0.044 | 0.32 | 2.160 | 0.138 | < 0.001 |
| 2008 | 3.000 | 3.254 | 0.253 | < 0.001 | 3.298 | 0.297 | < 0.001 |
Coefficient
Difference between the coefficient of that group and the None coefficient
Pvalue of the test of equivalence of the coefficient of that group and the None coefficient.
The estimates in Table 2 measure the average difference in utilization for that group in that year relative to 2002 (which is the reference year in the analysis). For example, the None coefficient of 0.018 for ED visits in 2003 indicated that there was an average of 0.018 more visits in 2003 relative to 2002 for that group. The corresponding Individual coefficient was 0.020, resulting in a difference of 0.002 visits. The two-sided test of the equivalence of the None and Individual coefficients had a p-value of 0.48. The coefficients increase with each year because the average number of ED visits and hospitalized days increase with age.
The 2003 and 2004 estimates provided insight into the suitability of the None group as a control for the Individual and Public groups. If the Individual and Public coefficients were substantially larger than the None coefficients in those years, it would have suggested that the Individual and Public groups had pre-existing trends of greater utilization before hurricanes. Such a finding would have called into question using the None group as a control. However, the differences in both the ED and hospitalization regressions are generally nearly zero or, in the case of hospitalized days, negative.
The 2006–2008 estimates detailed the potential association between hurricane exposure and post-hurricane utilization. For ED visits, the 2006 and 2007 differences were relatively small. However, a substantial difference emerged in 2008 for both the Individual and Public groups. Relative to the mean number of visits for the None group in 2008 of 0.58, the estimates translated to a roughly 2.5% and 3.0% higher averages for the Individual and Public groups, respectively. The hospitalized days differences were positive for every year in the 2006–2008 period for both groups. However, the values were largest again in 2008, where the coefficients corresponded to 5.5% and 6.6% higher averages for the Individual and Public groups (respectively) relative to the None group.
To further investigate the hospitalized days estimates, Table 3 reports the interaction coefficients for the three hospital categories reported in the CMS data (along with the estimates for all hospitals for reference). Inpatient acute care hospitals provide short-term care to address immediate and critical needs with the goal of transitioning patients to a setting that involves a lower level of care level. Other inpatient care includes cancer and long-term care hospitals, while skilled nursing facilities provide professional services beyond custodial care to patients after a hospital stay. The other inpatient and skilled nursing facility categories appear to have driven the relationship observed across all hospitals. The skilled nursing facility estimates were especially large, with the difference for the Individual group changing signs in 2008.
Table 3.
Regression interaction coefficients for hospitalized days (all, acute inpatient, other inpatient, skilled nursing facility) by FEMA assistance level.
| Hospital type / year | None (n=153,339) | Individual (n=456,218) | Public (n=893,886) | ||||
|---|---|---|---|---|---|---|---|
| Coef.a | Coef.a | Diff.b | P-valuec | Coef.a | Diff.b | P-valuec | |
| All | |||||||
| 2003 | 0.243 | 0.239 | −0.004 | 0.89 | 0.227 | −0.016 | 0.53 |
| 2004 | 0.614 | 0.533 | −0.081 | 0.01 | 0.577 | −0.037 | 0.22 |
| 2006 | 1.452 | 1.460 | 0.008 | 0.85 | 1.537 | 0.085 | 0.02 |
| 2007 | 2.022 | 2.066 | 0.044 | 0.32 | 2.160 | 0.138 | < 0.001 |
| 2008 | 3.000 | 3.254 | 0.253 | < 0.001 | 3.298 | 0.297 | < 0.001 |
| Acute inpatient | |||||||
| 2003 | 0.081 | 0.069 | −0.012 | 0.33 | 0.056 | −0.025 | 0.04 |
| 2004 | 0.182 | 0.143 | −0.039 | 0.005 | 0.138 | −0.044 | 0.001 |
| 2006 | 0.354 | 0.340 | −0.015 | 0.30 | 0.322 | −0.033 | 0.01 |
| 2007 | 0.512 | 0.466 | −0.046 | 0.003 | 0.436 | −0.077 | < 0.001 |
| 2008 | 0.773 | 0.734 | −0.038 | 0.02 | 0.693 | −0.080 | < 0.001 |
| Other inpatient | |||||||
| 2003 | 0.009 | 0.052 | 0.043 | < 0.001 | 0.028 | 0.019 | 0.03 |
| 2004 | 0.051 | 0.110 | 0.029 | < 0.001 | 0.086 | 0.035 | < 0.001 |
| 2006 | 0.095 | 0.181 | 0.086 | < 0.001 | 0.126 | 0.031 | 0.002 |
| 2007 | 0.117 | 0.242 | 0.125 | < 0.001 | 0.161 | 0.044 | < 0.001 |
| 2008 | 0.204 | 0.356 | 0.153 | < 0.001 | 0.257 | 0.054 | < 0.001 |
| Skilled nursing facility | |||||||
| 2003 | 0.153 | 0.118 | −0.034 | 0.06 | 0.143 | −0.010 | 0.57 |
| 2004 | 0.382 | 0.281 | −0.101 | < 0.001 | 0.353 | −0.029 | 0.16 |
| 2006 | 1.002 | 0.939 | −0.063 | 0.03 | 1.089 | 0.087 | 0.001 |
| 2007 | 1.393 | 1.358 | −0.036 | 0.27 | 1.564 | 0.171 | < 0.001 |
| 2008 | 2.025 | 2.163 | 0.139 | < 0.001 | 2.347 | 0.323 | < 0.001 |
Coefficient
Difference between the coefficient of that group and the None coefficient
Pvalue of the test of equivalence of the coefficient of that group and the None coefficient.
Discussion
Because of similarities in demographic characteristics and similar pre-hurricane utilization trends, individuals in our sample in counties where FEMA did not assign an assistance level are plausible controls for those in areas where FEMA assigned either individual or public assistance levels. The estimates indicate relative increases in ED visits and days hospitalized for the affected groups after Hurricanes Katrina and Rita at the end of the three-year observation period. Applying the 2008 coefficient differences to the respective group populations, the associated increase in days hospitalized in 2008 across the two groups was estimated at 380,907 (95% CI: 252,154; 511,010), while the increase in ED visits was significantly smaller at 21,583 (95% CI: 11,676, 31,490) (see Table A1).
A surprising aspect of our analysis was that the estimated differences between the None group and the Individual and Public groups in 2008 were larger than those in 2006 and 2007, especially given previous studies that found reversion to pre-Katrina levels for some clinical and biochemical markers two years following the storm (Theti et al., 2010). For both ED visits and hospitalized days, the point estimates of the 2008 differences were more than double those of the 2007 differences. While the data employed do not allow for precise insight into the mechanism(s) underlying this pattern, it could reflect the cumulative impact of poor maintenance of diabetic treatment and medication. Our estimates are roughly consistent with Egede et al. (2012), who find that the difference in average inpatient costs between diabetics who are and are not adherent to their medications increases over their five-year study period.
Our finding that days hospitalized in skilled nursing facilities, which provide care beyond initial acute hospital stays, appears to have largely driven our overall results provides additional potential insight. We again cannot definitively identify the underlying cause of this finding. Yet, it is consistent with affected individuals requiring more care beyond their initial hospital stay, potentially due to poorer dietary and/or medication adherence. However, this interpretation is speculative and further study is needed to determine the nature of the relationships we observed.
This study has several limitations. The sample is limited to traditional Medicare enrollees and does not include those enrolled in Medicare Advantage. Medicare Advantage enrollees are typically less sick than those in traditional Medicare (Batata 2004), so the estimates may not be representative of all diabetic seniors. Given concerns regarding data quality, it was not possible to examine the period immediately following Katrina and Rita. Further, Hurricane Katrina was a historically extreme hurricane and the associations measured may not apply to lesser disasters. Finally, as noted above, it was not possible to determine the cause for the ED visit or hospitalization and thus obtain insight into the mechanisms behind the observed associations.
Conclusion
This relatively unique study of an extended period of administrative data provided potential insight into the long-term effects of disasters on health care utilization. The findings indicated that the effects of disasters can persist years after the event and that public health may be improved by more closely monitoring affected populations beyond the initial aftermath.
Abbreviations:
- CMS
Centers for Medicare & Medicaid Services
- ED
emergency department
- FEMA
Federal Emergency Management Agency
Appendix
Table A1.
Calculation of 2008 differences in ED visits and hospitalized days for Individual and Public groups relative to None group.
| 2008 coefficient difference | 2008 group-level outcome difference | ||||||
|---|---|---|---|---|---|---|---|
| Outcome / group | Group population | 95% CI lower limit | Point estimate | 95% CI upper limit | 95% CI lower limit | Point estimate | 95% CI upper limit |
| ED visits | |||||||
| Individual | 456,218 | 0.006 | 0.014 | 0.022 | 2,737 | 6,387 | 10,037 |
| Public | 893,886 | 0.010 | 0.017 | 0.024 | 8,939 | 15,196 | 21,453 |
| Total | 11,676 | 21,583 | 31,490 | ||||
| Hospitalized days | |||||||
| Individual | 456,218 | 0.153 | 0.253 | 0.354 | 69,801 | 115,423 | 161,501 |
| Public | 893,886 | 0.204 | 0.297 | 0.391 | 182,353 | 265,484 | 349,509 |
| Total | 252,154 | 380,907 | 511,010 | ||||
References
- Anderson AH, Cohen AJ, Kutner NG, Kopp JB, Kimmel PL, Muntner P (2009) Missed dialysis sessions and hospitalization in hemodialysis patients after Hurricane Katrina. Kidney Int;75(11):1202–1208. 10.1038/ki.2009.5 [DOI] [PubMed] [Google Scholar]
- Batata A (2004) The Effects of HMOs on Fee-for-Service Health Care Expenditures: Evidence from Medicare Revisited. J Health Econ; 23: 951–963. 10.1016/j.jhealeco.2004.02.004 [DOI] [PubMed] [Google Scholar]
- Bell SA, Abir M, Choi H, Cooke C, Iwashyna T (2018) All-Cause Hospital Admissions Among Older Adults After a Natural Disaster. Annals of Emergency Medicine;71(6):746–754.e2. 10.1016/j.annemergmed.2017.06.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton LC, Skinner EA, Uscher-Pines L, et al. (2009) Health of Medicare Advantage plan enrollees at 1 year after Hurricane Katrina. Am J Manag Care;15(1):13–22. [PubMed] [Google Scholar]
- Egede LE, Gebregziabher M, Dismuke CE, et al. (2012) Medication Nonadherence in Diabetes: Longitudinal effects on costs and potential cost savings from improvement. Diabetes Care;35(12):2533–2539. 10.2337/dc12-0572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotanda H, Fogel J, Husk G, et al. (2015) Hurricane Sandy: Impact on Emergency Department and Hospital Utilization by Older Adults in Lower Manhattan, New York (USA). Prehospital and Disaster Medicine;30(5):496–502. 10.1017/S1049023X15005087 [DOI] [PubMed] [Google Scholar]
- He FT, Cruz NL, Olson D, et al. (2016) Temporal and Spatial Patterns in Utilization of Mental Health Services During and After Hurricane Sandy: Emergency Department and Inpatient Hospitalizations in New York City. Disaster Med Public Health Prep;10(3):512–517. 10.1017/dmp.2016.89 [DOI] [PubMed] [Google Scholar]
- Hepke KL, Martus MT, Share DA (2004) Costs and utilization associated with pharmaceutical adherence in a diabetic population. Am J Manag Care;10(2 Pt 2):144–151. [PubMed] [Google Scholar]
- Ho PM, Rumsfeld JS, Masoudi FA, et al. (2006) Effect of Medication Nonadherence on Hospitalization and Mortality Among Patients With Diabetes Mellitus. Arch Intern Med;166(17):1836–1841. 10.1001/archinte.166.17.1836 [DOI] [PubMed] [Google Scholar]
- Howard D, Zhang R, Huang Y, Kutner N (2012) Hospitalization Rates Among Dialysis Patients During Hurricane Katrina. Prehosp Disaster Med;27(4):325–329. 10.1017/S1049023X12000945 [DOI] [PubMed] [Google Scholar]
- Kelman J, Finne K, Bogdanov A, et al. (2015) Dialysis Care and Death Following Hurricane Sandy. AmericanJournal of Kidney Diseases;65(1):109–115. 10.1053/j.ajkd.2014.07.005 [DOI] [PubMed] [Google Scholar]
- Lau DT, Nau DP (2004) Oral Antihyperglycemic Medication Nonadherence and Subsequent Hospitalization Among Individuals With Type 2 Diabetes. Diabetes Care;27(9):2149–2153. 10.2337/diacare.27.9.2149 [DOI] [PubMed] [Google Scholar]
- Lee DC, Smith SW, Carr BG, et al. (2016) Geographic Distribution of Disaster-Specific Emergency Department Use After Hurricane Sandy in New York City. Disaster Med Public Health Prep;10(03):351–361. https://doi.org/0.1017/dmp.2015.190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JM, Eason A, Nelson C, Kazzi NG, Cowan AE, Tarini BA (2014) Screening Practices for Identifying Type 2 Diabetes in Adolescents. J Adolesc Health;54(2):139–143. 10.1016/j.jadohealth.2013.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen K, Dreyfuss Z (2008) How Many Walked Through the Door?: The Effect of Hurricane Katrina Evacuees on Houston Emergency Departments. Med Care;46(9):998 10.1097/MLR.0b013e3181792573 [DOI] [PubMed] [Google Scholar]
- Reese S FEMA Individual Assistance Programs: In Brief [Internet]. Congressional Research Service; 2018. Available from: https://crsreports.congress.gov/product/pdf/R/R45085
- Quast T, Mortensen K. (2012) Emergency Department Utilization in the Texas Medicaid Emergency Waiver Following Hurricane Katrina. Medicare Medicaid Res Rev;2(1):E1–16. 10.5600/mmrr.002.01.a01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quast T, Feng L. (forthcoming) Long-Term Effects of Disasters on Health Care Utilization: Hurricane Katrina and Older Individuals with Diabetes. Disaster Medicine and Public Health Preparedness. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma AJ, Weiss EC, Young SL, et al. (2008) Chronic Disease and Related Conditions at Emergency Treatment Facilities in the New Orleans Area After Hurricane Katrina. Disaster Med Public Health Prep;2(01):27–32. 10.1097/DMP.0b013e31816452f0 [DOI] [PubMed] [Google Scholar]