Abstract
Niacinamide (NIA) is a water-soluble vitamin that is widely used in the treatment of skin diseases. Moreover, NIA displays antioxidant effects and helps repair damaged DNA. Recent studies showed that particulate matter 2.5 (PM2.5) induced reactive oxygen species (ROS), causing disruption of DNA, lipids, and protein, mitochondrial depolarization, and apoptosis of skin keratinocytes. Here, we investigated the protective effects of NIA on PM2.5-induced oxidative stress in human HaCaT keratinocytes. We found that NIA could inhibit the ROS generation induced by PM2.5, as well block the PM2.5-induced oxidation of molecules, such as lipids, proteins, and DNA. Furthermore, NIA alleviated PM2.5-induced accumulation of cellular Ca2+, which caused cell membrane depolarization and apoptosis, and reduced the number of apoptotic cells. Collectively, the findings show that NIA can protect keratinocytes from PM2.5-induced oxidative stress and cell damage.
Keywords: Niacinamide, Particulate matter 2.5, Oxidative stress, Human HaCaT keratinocyte
INTRODUCTION
Niacinamide (NIA), also known as nicotinamide, is a hydrophilic amide of vitamin B3 that is an important component in various cosmetics and medicines. NIA is found in a wide array of foods such as fish, mushroom, and nuts (Damian, 2010). As a typical medicine for treating pigmentary disorders, NIA blocks the melanosome migration between melanocytes and keratinocytes and suppresses skin pigmentation (Bissett et al., 2007; Rolfe, 2014). The biological activities of NIA also include antimicrobial, photo-protection, lighting, and anti-pruritus (Wohlrab and Kewft, 2014). Moreover, as a coenzyme in the glycolysis pathway, NIA promotes the repair of DNA damage induced by UV in keratinocytes (Sousa et al., 2012; Surjana et al., 2013).
Due to excessive consumption of fossil fuels, air pollution has become a major health hazard for humans (Park et al., 2018). Both indoor and outdoor particulate matter (PM) damage human systems, such as bronchial epithelial cells (Yuan et al., 2019), the cardiovascular system (Cao et al., 2016), the central nervous system (Wang et al., 2017), and the pulmonary immune system (Li et al., 2017). In addition, PM can penetrate the skin barrier, mainly by appendageal route and stratum corneum, thereby disrupting the protective activity of the skin (Pan et al., 2015), causing wrinkling and thickening (Kim et al., 2016). PM contributes to skin aging by inducing oxidative stress and inflammation (Magnani et al., 2016). We have previously reported that PM induces oxidative stress, promotes apoptosis, and causes dysfunction of keratinocytes (Piao et al., 2018; Zhen et al., 2018, 2019).
In this study, we focused on particulate matter <2.5 μm (PM2.5), which can attach to epidermal skin due to its small size. PM2.5 is known to stimulate the generation of reactive oxygen species (ROS) in keratinocytes (Hyun et al., 2019b). NIA has been shown to suppress oxidative stress notably in vivo (Abdullah et al., 2018). However, there are no reports on the cytoprotective action of NIA against PM2.5-induced oxidative stress in human keratinocytes. Therefore, in this study, we examined whether NIA can protect HaCaT cells against PM2.5-induced damage.
MATERIALS AND METHODS
Preparation of NIA and PM2.5
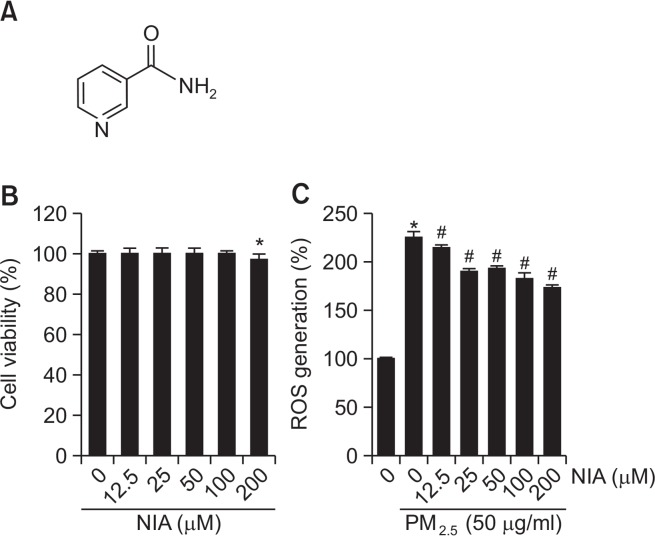
NIA (Fig. 1A) was purchased from Sigma-Aldrich, Inc. (St. Louis, MO, USA) and dissolved in dimethylsulfoxide (DMSO). Diesel particulate matter NIST SRM 1650b (PM2.5, Sigma-Aldrich) was dissolved in DMSO and stored at a concentration of 25 mg/mL (Piao et al., 2018).
Fig. 1.
Niacinamide (NIA) decreased PM2.5-induced ROS generation. (A) Chemical structure of NIA. (B) MTT assay to determine cell viability after treatment with indicated concentrations of NIA (0, 12.5, 25, 50, 100, or 200 μM). (C) Flow cytometric determination of intracellular ROS scavenging activity of NIA (0, 12.5, 25, 50, 100, or 200 μM). ROS generation was induced by PM2.5. *p<0.05 and #p<0.05 compared with control cells and PM2.5-exposed cells, respectively.
Cell culture
HaCaT human keratinocytes from Cell Lines Service (Heidelberg, Germany) were cultured in Dulbecco’s Modified Eagle’s Medium (Life Technologies Co., Grand Island, NY, USA) with 10% heat-inactivated fetal calf serum at 37°C with 5% CO2.
Cell viability
The 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay was used to test the cytotoxicity of NIA. Cells were seeded into a 24-well plate with 12.5, 25, 50, 100, or 200 μM of NIA. Then, MTT solution was added to each well and samples were incubated for 4 h. Finally, the solutions from DMSO and yield formazan crystals were detected at 540 nm using the scanning multi-well spectrophotometer (Piao et al., 2017).
Determination of intracellular ROS
To investigate anti-oxidative stress effect of NIA, we used 2′,7′-dichlorofluorescein diacetate (DCF-DA, Sigma-Aldrich) staining. ROS generation was induced using PM2.5 (50 μg/mL). After 16 h of incubation, the cells were treated with 12.5, 25, 50, 100, or 200 μM of NIA and PM2.5, followed by addition of 25 μM DCF-DA. The fluorescence of DCF-DA was measured using a flow cytometer (Becton Dickinson, Mountain View, CA, USA) (Piao et al., 2018). The inhibitory effect of NIA (100 μM) on PM2.5-induced ROS was assessed by a confocal microscope (Carl Zeiss, Oberkochen, Germany).
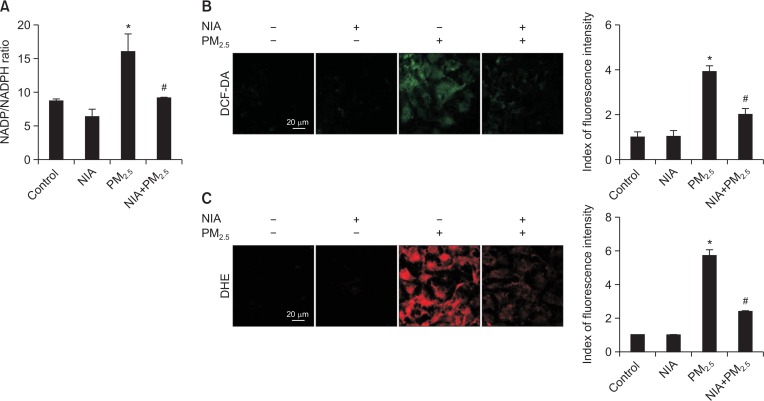
NADP/NADPH assay
To determine the ratio of intracellular NADP and NADPH, we used NADP/NADPH assay kit (Abcam, Cambridge, UK) according to the manufacturer’s instructions.
Measurement of intracellular superoxide levels by dihydroethidium (DHE) oxidation
To detect superoxide levels in cells, we measured the DHE oxidation. Cells were treated with NIA and PM2.5 and incubated with DHE (10 μM) for 30 min. After incubation, the fluorescence intensity was analyzed by a confocal microscope.
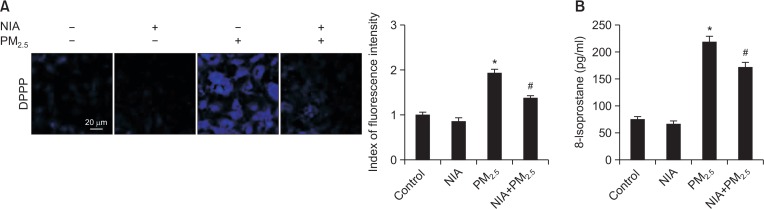
Lipid peroxidation assay
Lipid oxidative stress was investigated using two methods. The cells were dyed with 5 μM diphenyl-1-pyrenylphosphine (DPPP, Sigma-Aldrich) and fluorescence was analyzed using the confocal microscope. Harvested cells were subjected to analysis using the 8-Isoprostane ELISA kit (Cayman Chemical, Ann Arbor, MI, USA) according to the manufacturer’s instructions (Zhen et al., 2019).
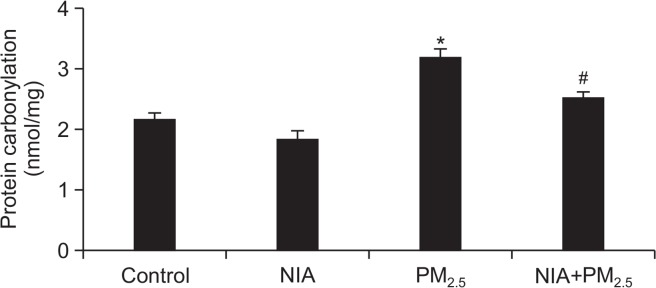
Protein carbonylation assay
The harvested cells were used for detecting protein oxidation with an OxiselectTM Protein Carbonyl ELISA kit (Cell Biolabs, San Diego, CA, USA) according to the manufacturer’s instructions.
Detection of 8-oxoguanine (8-oxoG)
To quantify oxidative DNA damage, we determined the level of 8-oxoG through the Bioxytech 8-OHdG ELISA kit (OXIS Health Products, Portland, OR, USA) according to the manufacturer’s instructions. For image analysis, the cells were fixed on a chamber slide and stained with avidin-tetramethylrhodamine isothiocyanate (TRITC) (1:200) conjugate (Sigma-Aldrich), and fluorescence images were obtained using a confocal microscope (Piao et al., 2011).
Single cell gel electrophoresis (Comet assay)
The comet assay was used to detect DNA damage induced by PM2.5. Harvested cells were dispersed in low-melting agarose (1%). Then, the mixtures were solidified on microscopic slides, and the slides were immersed in lysis buffer (2.5 M NaCl, 100 mM Na-EDTA, 10 mM Tris, 1% Trion X-100, and 10% DMSO, pH 10) for 1 h at 4°C. After electrophoresis, the slides were stained with ethidium bromide, and the percentage of the comet tail fluorescence and the tail length (50 cells per slide) was determined using a fluorescence microscope equipped with an image analysis software (Kinetic Imaging, Komet 5.5, Liverpool, UK) (Park et al., 2017).
Quantification of Ca2+ level
To determine the intracellular Ca2+ in viable cells, the cells were co-cultured with 10 μM fluo-4-acetoxymethyl ester (Fluo-4-AM, Sigma-Aldrich) dye for 30 min, and green fluorescence in the confocal micrographs was quantified.
Mitochondrial membrane potential (Δψm) analysis
To visualize the changes in membrane potential, the cells were stained with 5,5′,6,6′-tetrachloro-1,1′,3,3′-tetraethylben zimidazolylcarbocyanine iodide (JC-1, Invitrogen, Carlsbad, CA, USA) and were analyzed by confocal microscopy.
Hoechst 33342 staining
To observe apoptotic bodies, we used the nuclear-specific dye, Hoechst 33342 (Sigma-Aldrich). Cells were pre-treated with 100 μM NIA, treated with PM2.5 for 24 h, and then stained with Hoechst 33342 (10 μM). Nuclei were visualized under a fluorescence microscope equipped with a Cool SNAP-Pro color digital camera (Media Cybernetics, Silver Spring, MD, USA) (Han et al., 2019).
Statistical analysis
Data are shown as mean ± standard error, and were analyzed using the Tukey’s test and analysis of variance (ANOVA) by the Sigma Stat (v12) software (SPSS, Chicago, IL, USA). p-values <0.05 were considered statistically significant.
RESULTS
NIA showed anti-oxidative effect
Here, we used PM2.5 at a concentration of 50 μg/mL for ROS induction. This concentration was selected based on the findings of our recent study investigating whether PM2.5 induced oxidative stress. In that study, we measured ROS generation at various concentrations (25–100 μg/mL) of PM2.5, and 50 μg/mL PM2.5 was found to be optimal concentration to clearly observe oxidative stress-induced cell damage and inflammatory response (Piao et al., 2018; Ryu et al., 2019). In the MTT assay, NIA, up to 100 μM, showed no toxicity toward human keratinocytes, but cytotoxicity was observed at 200 μM (Fig. 1B). In addition, NIA dose-dependently inhibited the ROS generation induced by PM2.5 (Fig. 1C). To further investigate the anti-oxidative effect of NIA, we used 100 μM NIA as the optimal concentration for subsequent experiments.
NIA blocked ROS generation via NADPH oxidase activity
Evaluation of the NADPH oxidase (NOX) activity (NADP/NADPH ratio) showed that PM2.5 increased the oxidation of NADPH, which was reversed by NIA pre-treatment (Fig. 2A). In the DCF-DA staining assay, NIA inhibited PM2.5-induced fluorescence in the cells, demonstrating that NIA protected cells from PM2.5-induced ROS generation (Fig. 2B). Similarly, DHE staining revealed that superoxide generation induced by PM2.5 was blocked by NIA (Fig. 2C). These results further indicated that NIA exerted antioxidant effects in keratinocytes.
Fig. 2.
NIA cleared ROS by inhibiting NOX activity induced by PM2.5. (A) The ratio of intracellular NADP and NADPH was assessed using NADP/NADPH assay kit. (B) Intracellular ROS was detected after staining of cells with DCF-DA dye. (C) Superoxide generation was detected after dying cells with DHE. NIA diminished superoxide levels induced by PM2.5. *p<0.05 and #p<0.05 compared with control cells and PM2.5-exposed cells, respectively.
NIA inhibited PM2.5-induced lipid peroxidation
The detection of phosphine oxide (DPPP oxide) using the DPPP probe indicated that PM2.5 significantly induced lipid peroxidation, and pretreatment with NIA decreased the fluorescence emitted by the probe (Fig. 3A). Moreover, the levels of 8-isoprostane, a specific indicator of lipid peroxidation, revealed that NIA suppressed PM2.5-induced peroxidation (Fig. 3B). These results showed that NIA rescued cells from PM2.5-induced lipid oxidation.
Fig. 3.
NIA protected lipids from PM2.5-induced oxidation. (A) 8-Isoprostane ELISA assay and (B) DPPP staining were used to analyze lipid peroxidation. *p<0.05 and #p<0.05 compared with control cells and PM2.5-exposed cells, respectively.
NIA suppressed PM2.5-induced oxidative stress on proteins
The levels of protein carbonylation, a specific indicator of protein oxidation, revealed that NIA significantly inhibited PM2.5-induced oxidative protein modification (Fig. 4). These results showed that NIA rescued cells from PM2.5-induced protein carbonylation.
Fig. 4.
NIA protected proteins from PM2.5-induced oxidative stress. Protein oxidation was evaluated by protein carbonylation level. *p<0.05 and #p<0.05 compared with control cells and PM2.5-exposed cells, respectively.
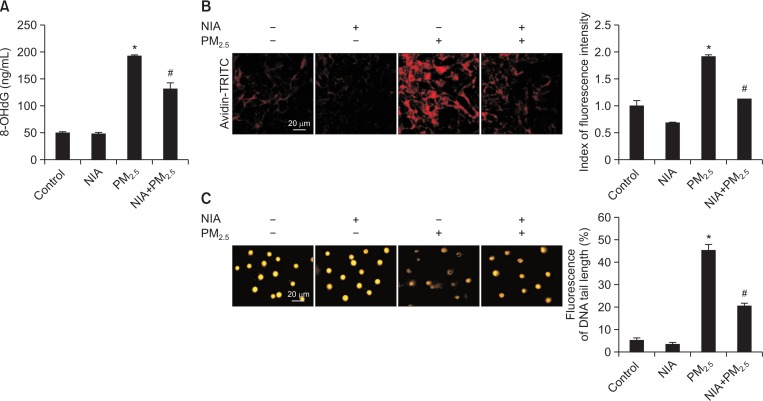
NIA protected cells from PM2.5-induced DNA damage
The 8-OHdG assay was used to assess oxidative damage on DNA caused by PM2.5 (Fig. 5A). Notably, NIA reduced 8-OHdG generation induced by PM2.5. Furthermore, confocal microscopy showed that the level of 8-oxoG in PM2.5-exposed cells was the highest, suggesting severe DNA lesions formed via avidin-TRITC binding. Consistent with other results, NIA ameliorated the DNA lesions (Fig. 5B). The protective effect of NIA on DNA damage was also observed in the comet assy. Length of comet tails and the percentage of tail fluorescence were increased by PM2.5, but decreased following NIA pretreatment (Fig. 5C). Collectively, these results illustrated that NIA protected against DNA damage induced by PM2.5.
Fig. 5.
NIA protected DNA from PM2.5-induced oxidative damage. (A) 8-OHdG ELISA (Bioxytech) kit was used to measure the level of 8-OHdG. (B) Avidin-TRITC conjugate was examined to evaluate the DNA oxidative adducts of 8-oxoG using confocal microscopy. (C) Comet assay was used to detect PM2.5-induced DNA damage. *p<0.05 and #p<0.05 compared with control cells and PM2.5-exposed cells, respectively.
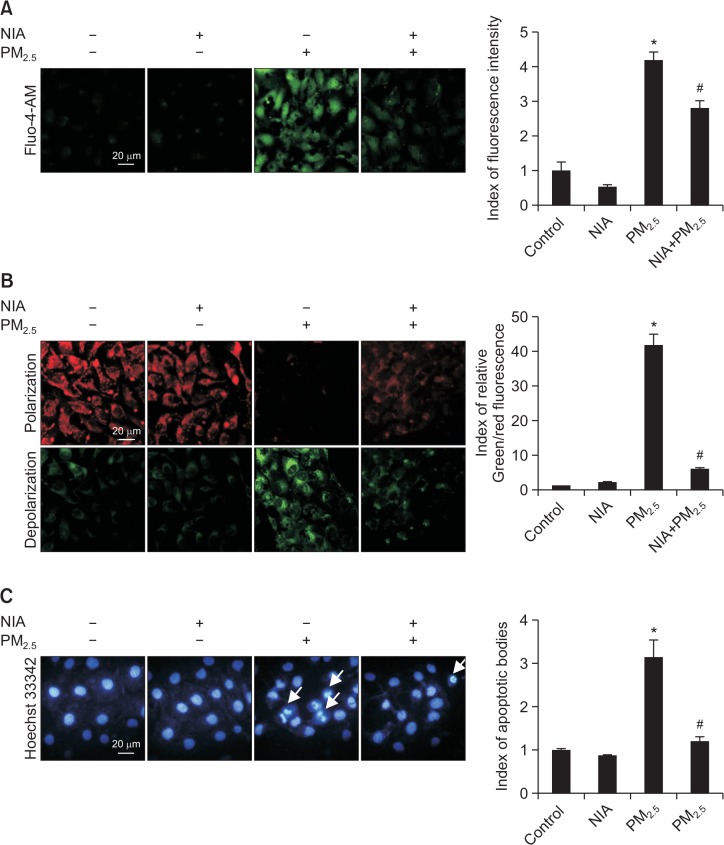
NIA lowered excessive intracellular Ca2+, balanced membrane potential, and suppressed apoptosis induced by PM2.5
Intracellular Ca2+, tracked by Fluo-4-AM, was detected by confocal microscopy. The image analysis revealed that PM2.5 stimulated excessive Ca2+, which could be reduced by NIA treatment (Fig. 6A). JC-1 staining was used to determine Δψm, with red and green fluorescence representing polarization and depolarization, respectively. The images obtained from confocal microscopy showed that Δψm polarization and depolarization were decreased and increased by PM2.5 treatment, respectively; however, they were reversed by NIA pretreatment (Fig. 6B). PM2.5 also promoted apoptotic bodies, when observed using Hoechst 33342 staining, and NIA pretreatment reduced their numbers (Fig. 6C). These results proved that PM2.5 disrupted the homeostasis of intracellular Ca2+ levels and accelerated cell apoptosis, but NIA exerted cytoprotective effects against these PM2.5-induced damages.
Fig. 6.
NIA protected cells from PM2.5-induced apoptosis, by blocking calcium channel and balancing mitochondrial membrane potential. (A) Fluo-4-AM staining was used to determine the intracellular Ca2+ levels. (B) Δψm analysis was performed using JC-1 dye and confocal microscopy. (C) Apoptotic bodies (indicated with arrows) were visualized using Hoechst 33342 dye. *p<0.05 or #p<0.05 compared with control cells or PM2.5-exposed cells, respectively.
DISCUSSION
The skin is the outermost organ and acts as the first protective layer from air pollution. Current studies indicate that air pollutants damage skin via two main routes. The first route is from the outside to inside, whereby PM penetrates the skin (including keratinocytes), and the second route is from the inside to the outside, whereby toxic effects in the lung subsequently influence the skin (Krutmann et al., 2014). In addition, PM2.5 stimulates inflammation by disrupting the cytokine network, thereby causing epidermal hyperplasia (Kim et al., 2017). Moreover, PM is known to cause oxidative damage to keratinocytes by promoting ROS generation (Romani et al., 2018). NIA is a well-known skin whitening agent (Hakozaki et al., 2002) and is known to improve skin barrier function and decrease sebum secretion (Draelos et al., 2005). In the present study, we mainly focused on the potential protective effect of NIA on PM2.5-induced oxidative damage in keratinocytes. NIA pretreatment at all tested concentrations inhibited PM2.5-induced ROS generation in cells.
A previous study showed that ROS is involved in various biological processes, including oxygen sensing, cell growth, cell differentiation, and cell death (Touyz et al., 2019). NOX plays a vital role in intracellular superoxide and hydrogen peroxide production (Cachat et al., 2015) and can be induced by particle exposure in keratinocytes (Kampfrath et al., 2011; Sticozzi et al., 2012). NOXs are widely distributed in mammalian tissues and, thereby, serve various functions (Touyz et al., 2019). The six homologs of the cytochrome subunit of the NOX (NOX1, NOX3, NOX4, NOX5, DUOX1, and DUOX2) are predominantly responsible for ROS production in mammalian cells (Tarafdar and Pula, 2018). NADPH is critical for the antioxidant system and reductive biosynthesis, and is required by enzymes involved in the pathologies of metabolic disorders due excessive ROS generation (Gomez-Sanchez et al., 2008; Legeza et al., 2013). Therefore, we determined the NADP/NADPH ratio, and the results showed that PM2.5 increased the oxidized NADP ratio, while NIA decreased the this NADP ratio. In addition, NIA cleared intracellular ROS induced by PM2.5.
Next, we examined the effect of PM2.5 on the three main molecules in cells, namely lipids, proteins, and DNA. ROS is known to damage lipids and proteins via lipid peroxidation and protein carbonylation, respectively (Hyun et al., 2019a), as well as damaging DNA stability. Lipid peroxidation is regarded as a general oxidative process, and is related to cell death. Furthermore, ROS accumulation, induced by stimuli such as tobacco smoke, can directly damage lipids (Ayala et al., 2014). Our results showed that PM2.5 exposure damaged lipids, while NIA protected the lipids from peroxidation caused by PM2.5. Oxidative stress also increased protein carbonylation, which is associated with cell damage and cell disease and is considered one of the most harmful irreversible protein modifications (Fedorova et al., 2014). NIA showed preventive action against protein oxidation induced by PM2.5. Previous study noted that PM2.5 caused early arrest of cell cycle, resulting from induced DNA damage, and 8-oxoG, the oxidative stress biomarker, is the predominant adduct of ROS-induced oxidative changes (Abbas et al., 2019). NIA has been shown to improve DNA repair following damage induced by ultraviolet radiation (Park et al., 2010; Snaidr et al., 2019). In our study, we evaluated three indices of DNA stability (8-OHdG levels, 8-oxoG intensity, and DNA tails), and all results showed that NIA protected cells from PM2.5-induced DNA lesions. Thus, NIA protects cells from PM2.5-induced damage.
Calcium plays a key role in cell survival, as well as it can improve apoptosis. Ca2+ mediated pro-apoptotic action is a response to many endogenous organelles, including mitochondria (Hajnoczky et al., 2003). Ca2+ from endoplasmic reticulum plays an important role in mitochondria-related metabolic activity (Sarasija et al., 2018). The increased intracellular Ca2+ affects Δψm and the disruption of mitochondrial membrane permeability is related to cell death (Kroemer et al., 2007; Zorova et al., 2018). During the process of apoptosis, mitochondria receive pro-apoptotic signals and release proapoptotic proteins (Orrenius et al., 2015). Notably, PM2.5 can induce cell apoptosis via various pathways, such as disruption of mitochondrial polarization, DNA fragmentation, and expression of pro-apoptotic proteins (Peixoto et al., 2017). All our results demonstrated that PM2.5 increased intracellular Ca2+ levels, disrupted the balance of mitochondrial potential, and promoted apoptosis, NIA treatment could inhibit these effects.
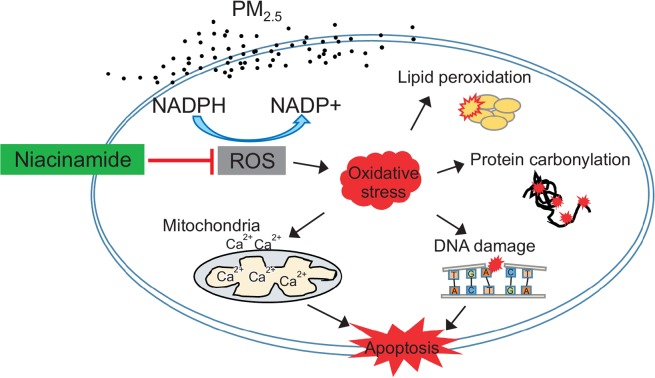
Taken together, our findings show that PM2.5 notably aggravated skin cell damage by inducing ROS generation, disrupting cellular components, and activating apoptotic pathways. However, cells pre-treated with NIA were protected from the ROS-induced lipid peroxidation, protein carbonylation, and DNA damage (Fig. 7). NIA also inhibited PM2.5-induced apoptosis by maintaining both Ca2+ levels and mitochondrial membrane potential in a steady state. These results suggest that NIA can protect against PM2.5-induced skin damage.
Fig. 7.
Schematic diagram showing the protective action of NIA on PM2.5-induced cell damage. NIA protected keratinocytes by suppressing ROS generation by decreasing the NADP/NADPH ratio. Further, NIA prevented oxidative stress-induced molecules damage, including lipid peroxidation, protein carbonylation, and DNA modification. NIA could also stabilize mitochondrial membrane potential by balancing calcium levels, which was disrupted by PM2.5. Finally, NIA protected cells from PM2.5-induced apoptosis.
Acknowledgments
This work was supported by grant from the Basic Research Laboratory Program (NRF-2017R1A4A1014512) by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP). This research was supported by the 2019 scientific promotion program funded by Jeju National University.
Footnotes
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest.
REFERENCES
- Abbas I, Badran G, Verdin A, Ledoux F, Roumie M, Lo Guidice JM, Courcot D, Garçon G. In vitro evaluation of organic extractable matter from ambient PM2.5 using human bronchial epithelial BEAS-2B cells: cytotoxicity, oxidative stress, proinflammatory response, genotoxicity, and cell cycle deregulation. Environ Res. 2019;171:510–522. doi: 10.1016/j.envres.2019.01.052. [DOI] [PubMed] [Google Scholar]
- Abdullah KM, Alam MM, Iqbal Z, Naseem I. Therapeutic effect of vitamin B3 on hyperglycemia, oxidative stress and DNA damage in alloxan induced diabetic rat model. Biomed Pharmacother. 2018;105:1223–1231. doi: 10.1016/j.biopha.2018.06.085. [DOI] [PubMed] [Google Scholar]
- Ayala A, Munoz MF, Arguelles S. Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid Med Cell Longev. 2014;2014:360438. doi: 10.1155/2014/360438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bissett DL, Robinson LR, Raleigh PS, Miyamoto K, Hakozaki T, Li J, Kelm GR. Reduction in the appearance of facial hyperpigmentation by topical N-acetyl glucosamine. J Cosmet Dermatol. 2007;6:20–26. doi: 10.1111/j.1473-2165.2007.00295.x. [DOI] [PubMed] [Google Scholar]
- Cachat J, Deffert C, Hugues S, Krause KH. Phagocyte NADPH oxidase and specific immunity. Clin Sci. 2015;128:635–648. doi: 10.1042/CS20140635. [DOI] [PubMed] [Google Scholar]
- Cao J, Qin G, Shi R, Bai F, Yang G, Zhang M, Lv J. Overproduction of reactive oxygen species and activation of MAPKs are involved in apoptosis induced by PM2.5 in rat cardiac H9c2 cells. J Appl Toxicol. 2016;36:609–617. doi: 10.1002/jat.3249. [DOI] [PubMed] [Google Scholar]
- Damian DL. Photoprotective effects of nicotinamide. Photochem Photobiol Sci. 2010;9:578–585. doi: 10.1039/b9pp00146h. [DOI] [PubMed] [Google Scholar]
- Draelos ZD, Ertel K, Berge C. Niacinamide-containing facial moisturizer improves skin barrier and benefits subjects with rosacea. Cutis. 2005;76:135–141. [PubMed] [Google Scholar]
- Fedorova M, Bollineni RC, Hoffmann R. Protein carbonylation as a major hallmark of oxidative damage: update of analytical strategies. Mass Spectrom Rev. 2014;33:79–97. doi: 10.1002/mas.21381. [DOI] [PubMed] [Google Scholar]
- Gomez-Sanchez EP, Romero DG, Rodriguez AF, Warden MP, Krozowski Z, Gomez-Sanchez CE. Hexose-6-phosphate dehydrogenase and 11beta-hydroxysteroid dehydrogenase-1 tissue distribution in the rat. Endocrinology. 2008;149:525–533. doi: 10.1210/en.2007-0328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajnoczky G, Davies E, Madesh M. Calcium signaling and apoptosis. Biochem Biophys Res Commun. 2003;304:445–454. doi: 10.1016/S0006-291X(03)00616-8. [DOI] [PubMed] [Google Scholar]
- Han X, Kang KA, Piao MJ, Zhen AX, Hyun YJ, Kim HM, Ryu YS, Hyun JW. Shikonin exerts cytotoxic effects in human colon cancers by inducing apoptotic cell death via the endoplasmic reticulum and mitochondria-mediated pathways. Biomol Ther (Seoul) 2019;27:41–47. doi: 10.4062/biomolther.2018.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyun YJ, Piao MJ, Kang KA, Ryu YS, Zhen AX, Choa SJ, Kang HK, Koh YS, Ahn MJ, Kim TH, Hyun JW. 3,4-Dicaffeoylquinic acid protects human keratinocytes against environmental oxidative damage. J Funct Foods. 2019a;52:430–441. doi: 10.1016/j.jff.2018.11.026. [DOI] [Google Scholar]
- Hyun YJ, Piao MJ, Kang KA, Zhen AX, Madushan Fernando PDS, Kang HK, Ahn YS, Hyun JW. Effect of fermented fish oil on fine particulate matter-induced skin aging. Mar Drugs. 2019b;17:61. doi: 10.3390/md17010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kampfrath T, Maiseyeu A, Ying Z, Shah Z, Deiuliis JA, Xu X, Kherada N, Brook RD, Reddy KM, Padture NP, Parthasarathy S, Chen LC, Moffatt-Bruce S, Sun Q, Morawietz H, Rajagopalan S. Chronic fine particulate matter exposure induces systemic vascular dysfunction via NADPH oxidase and TLR4 pathways. Circ Res. 2011;108:716–726. doi: 10.1161/CIRCRESAHA.110.237560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Bae IH, Son ED, Park J, Cha N, Na HW, Jung C, Go YS, Kim DY, Lee TR, Shin DW. Transcriptome analysis of airborne PM2.5-induced detrimental effects on human keratinocytes. Toxicol Lett. 2017;273:26–35. doi: 10.1016/j.toxlet.2017.03.010. [DOI] [PubMed] [Google Scholar]
- Kim KE, Cho D, Park HJ. Air pollution and skin diseases: adverse effects of airborne particulate matter on various skin diseases. Life Sci. 2016;152:126–134. doi: 10.1016/j.lfs.2016.03.039. [DOI] [PubMed] [Google Scholar]
- Kroemer G, Galluzzi L, Brenner C. Mitochondrial membrane permeabilization in cell death. Physiol Rev. 2007;87:99–163. doi: 10.1152/physrev.00013.2006. [DOI] [PubMed] [Google Scholar]
- Krutmann J, Liu W, Li L, Pan X, Crawford M, Sore G, Seite S. Pollution and skin: from epidemiological and mechanistic studies to clinical implications. J Dermatol Sci. 2014;76:163–168. doi: 10.1016/j.jdermsci.2014.08.008. [DOI] [PubMed] [Google Scholar]
- Legeza B, Balázs Z, Nashev LG, Odermatt A. The microsomal enzyme 17β-hydroxysteroid dehydrogenase 3 faces the cytoplasm and uses NADPH generated by glucose-6-phosphate dehydrogenase. Endocrinology. 2013;154:205–213. doi: 10.1210/en.2012-1778. [DOI] [PubMed] [Google Scholar]
- Li N, He F, Liao B, Zhou Y, Li B, Ran P. Exposure to ambient particulate matter alters the microbial composition and induces immune changes in rat lung. Respir Res. 2017;18:143. doi: 10.1186/s12931-017-0626-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magnani ND, Muresan XM, Belmonte G, Cervellati F, Sticozzi C, Pecorelli A, Miracco C, Marchini T, Evelson P, Valacchi G. Skin damage mechanisms related to airborne particulate matter exposure. Toxicol Sci. 2016;149:227–236. doi: 10.1093/toxsci/kfv230. [DOI] [PubMed] [Google Scholar]
- Orrenius S, Gogvadze V, Zhivotovsky B. Calcium and mitochondria in the regulation of cell death. Biochem Biophys Res Commun. 2015;460:72–81. doi: 10.1016/j.bbrc.2015.01.137. [DOI] [PubMed] [Google Scholar]
- Pan TL, Wang PW, Alijuffali IA, Huang CT, Lee CW, Fang JY. The impact of urban particulate pollution on skin barrier function and the subsequent drug absorption. J Dermatol Sci. 2015;78:51–60. doi: 10.1016/j.jdermsci.2015.01.011. [DOI] [PubMed] [Google Scholar]
- Park CG, Cho HK, Shin HJ, Park KH, Lim HB. Comparison of mutagenic activities of various ultra-fine particles. Toxicol Res. 2018;34:163–172. doi: 10.5487/TR.2018.34.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J, Halliday GM, Surjana D, Damian DL. Nicotinamide prevents ultraviolet radiation-induced cellular energy loss. Photochem Photobiol. 2010;86:942. doi: 10.1111/j.1751-1097.2010.00746.x. [DOI] [PubMed] [Google Scholar]
- Park JE, Piao MJ, Kang KA, Shilnikova K, Hyun YJ, Oh SK, Jeong YJ, Chae S, Hyun JW. A benzylidene-acetophenone derivative induces apoptosis of radiation-resistant human breast cancer cells via oxidative stress. Biomol Ther (Seoul) 2017;25:404–410. doi: 10.4062/biomolther.2017.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peixoto MS, de Oliveira Galvao MF, Batistuzzo de Medeiros SR. Cell death pathways of particulate matter toxicity. Chemosphere. 2017;188:32–48. doi: 10.1016/j.chemosphere.2017.08.076. [DOI] [PubMed] [Google Scholar]
- Piao MJ, Ahn MJ, Kang KA, Ryu YS, Hyun YJ, Shilnikova K, Zhen AX, Jeong JW, Choi YH, Kang HK, Koh YS, Hyun JW. Particulate matter 2.5 damages skin cells by inducing oxidative stress, subcellular organelle dysfunction, and apoptosis. Arch Toxicol. 2018;92:2077–2091. doi: 10.1007/s00204-018-2197-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piao MJ, Kang KA, Ryu YS, Shilnikova K, Park JE, Hyun YJ, Zhen AX, Kang HK, Koh YS, Ahn MJ, Hyun JW. The red algae compound 3-bromo-4,5-dihydroxybenzaldehyde protects human keratinocytes on oxidative stress-related molecules and pathways activated by UVB irradiation. Mar Drugs. 2017;15:268. doi: 10.3390/md15090268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piao MJ, Kim KC, Choi JY, Choi J, Hyun JW. Silver nanoparticles down-regulate Nrf2-mediated 8-oxoguanine DNA glycosylase 1 through inactivation of extracellular regulated kinase and protein kinase B in human Chang liver cells. Toxicol Lett. 2011;207:143–148. doi: 10.1016/j.toxlet.2011.09.002. [DOI] [PubMed] [Google Scholar]
- Rolfe HM. A review of nicotinamide: treatment of skin diseases and potential side effects. J Cosmet Dermatol. 2014;13:324–328. doi: 10.1111/jocd.12119. [DOI] [PubMed] [Google Scholar]
- Romani A, Cervellati C, Muresan XM, Belmonte G, Pecorelli A, Cervellati F, Benedusi M, Evelson P, Valacchi G. Keratinocytes oxidative damage mechanisms related to airbone particle matter exposure. Mech Ageing Dev. 2018;172:86–95. doi: 10.1016/j.mad.2017.11.007. [DOI] [PubMed] [Google Scholar]
- Ryu YS, Kang KA, Piao MJ, Ahn MJ, Yi JM, Hyun YM, Kim SH, Ko MK, Park CO, Hyun JW. Particulate matter induces inflammatory cytokine production via activation of NFκB by TLR5-NOX4-ROS signaling in human skin keratinocyte and mouse skin. Redox Biol. 2019;21:101080. doi: 10.1016/j.redox.2018.101080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarasija S, Laboy JT, Ashkavand Z, Bonner J, Tang Y, Norman KR. Presenilin mutations deregulate mitochondrial Ca2+ homeostasis and metabolic activity causing neurodegeneration in Caenorhabditis elegans. eLife. 2018;7:e33052. doi: 10.7554/eLife.33052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snaidr VA, Damian DL, Halliday GM. Nicotinamide for photoprotection and skin cancer chemoprevention: a review of efficacy and safety. Exp Dermatol. 2019;1:15–22. doi: 10.1111/exd.13819. [DOI] [PubMed] [Google Scholar]
- Sousa FG, Matuo R, Soares DG, Escargueil AE, Henriques JAP, Larsen AK, Saffi J. PARPs and the DNA damage response. Carcinogenesis. 2012;33:1433–1440. doi: 10.1093/carcin/bgs132. [DOI] [PubMed] [Google Scholar]
- Sticozzi C, Belmonte G, Pecorelli A, Arezzini B, Gardi C, Maioli E, Miracco C, Toscano M, Forman HJ, Valacchi G. Cigarette smoke affects keratinocytes SRB1 expression and localization via H2O2 production and HNE protein adducts formation. PLoS ONE. 2012;7:e33592. doi: 10.1371/journal.pone.0033592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surjana D, Halliday GM, Damian DL. Nicotinamide enhances repair of ultraviolet radiation-induced DNA damage in human keratinocytes and ex vivo skin. Carcinogenesis. 2013;34:1144–1149. doi: 10.1093/carcin/bgt017. [DOI] [PubMed] [Google Scholar]
- Tarafdar A, Pula G. The role of NADPH oxidases and oxidative stress in neurodegenerative disorders. Int J Mol Sci. 2018;19:3824. doi: 10.3390/ijms19123824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Touyz RM, Anagnostopoulou A, Camargo LL, Rios FJ, Montezano AC. Vascular biology of superoxide-generating NADPH oxidase 5-implications in hypertension and cardiovascular disease. Antioxid Redox Signal. 2019;30:1027–1040. doi: 10.1089/ars.2018.7583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Xiong L, Tang M. Toxicity of inhaled particulate matter on the central nervous system: neuroinflammation, neuropsychological effects and neurodegenerative disease. J Appl Toxicol. 2017;37:644–667. doi: 10.1002/jat.3451. [DOI] [PubMed] [Google Scholar]
- Wohlrab J, Kreft D. Niacinamide-mechanism of action and its topical use in dermatology. Skin Pharmacol Physiol. 2014;27:311–315. doi: 10.1159/000359974. [DOI] [PubMed] [Google Scholar]
- Yuan Q, Chen Y, Li X, Zhang Z, Chu H. Ambient fine particulate matter (PM2.5) induces oxidative stress and pro-inflammatory response via up-regulating the expression of CYP1A1/1B1 in human bronchial epithelial cells in vitro. Mutat Res. 2019;839:40–48. doi: 10.1016/j.mrgentox.2018.12.005. [DOI] [PubMed] [Google Scholar]
- Zhen AX, Piao MJ, Hyun YJ, Kang KA, Madushan Fernando PDS, Cho SJ, Ahn MJ, Hyun JW. Diphlorethohydroxycarmalol attenuates fine particulate matter-induced subcellular skin dysfunction. Mar Drugs. 2019;17:95. doi: 10.3390/md17020095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhen AX, Piao MJ, Hyun YJ, Kang KA, Ryu YS, Cho SJ, Kang HK, Koh YS, Ahn MJ, Kim TH, Hyun JW. Purpurogallin protects keratinocytes from damage and apoptosis induced by ultraviolet B radiation and particulate matter 2.5. Biomol Ther (Seoul) 2019;27:395–403. doi: 10.4062/biomolther.2018.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zorova LD, Popkov VA, Plotnikov EY, Silachev DN, Pevzner IB, Jankauskas SS, Babenko VA, Zorov SD, Balakireva AV, Juhaszova M, Sollott SJ, Zorov DB. Mitochondrial membrane potential. Anal Biochem. 2018;552:50–59. doi: 10.1016/j.ab.2017.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]