Abstract
Background & Aims:
Open-transforaminal lumbar interbody fusion (O-TLIF) is regarded as the standard (S) approach which is currently available for patients with degenerative lumbar diseases patients. In addition, minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) has proposed and gradually obtained popularity compared with O-TLIF procedures due to its beneficial outcomes in minimized tissue injury and quicker recovery. Nonetheless, debates exist concerning the use of MI-TLIF with its conflicting outcomes of clinical effect and safety in several publications. The purpose of the current study is to conduct an updated meta-analysis to provide eligible and systematical assessment available for the evaluation of the efficacy and safety of MI-TLIF in comparison with O-TLIF.
Methods:
Publications on the comparison of O-TLIF and MI-TLIF in treating degenerative lumbar diseases in last 5 years were collected. After rigorous reviewing on the eligibility of publications, the available data was further extracted from qualified trials. All trials were conducted with the analysis of the summary hazard ratios (HRs) of the interest endpoints, including intraoperative and postoperative outcomes.
Results:
Admittedly, it is hard to run a clinical RCT to compare the prognosis of patients undergoing O-TLIF and MI-TLIF. A total of 10 trials including non-randomized trials in the current study were collected according to our inclusion criteria. The pooled results of surgery duration indicated that MI-TLIF was highly associated with shorter length of hospital stay, less blood loss, and less complications. However, there were no remarkable differences in the operate time, VAS-BP, VAS-LP, and ODI between the 2 study groups.
Conclusion:
The quantitative analysis and combined results of our study suggest that MI-TLIF may be a valid and alternative method with safe profile in comparison of O-TLIF, with reduced blood loss, decreased length of stay, and complication rates. While, no remarkable differences were found or observed in the operate time, VAS-BP, VAS-LP, and ODI. Considering the limited available data and sample size, more RCTs with high quality are demanded to confirm the role of MI-TLIF as a standard approach in treating degenerative lumbar diseases.
Keywords: degenerative lumbar diseases, meta-analysis, minimally invasive, transforaminal lumbar interbody fusion
1. Introduction
Degenerative lumbar spine disease is a chronic and progressive disease associated with radiating pain or paresthesias down the lower extremities, low back pain, decreased function of the legs, neurogenic claudication, or bowel and bladder incontinence.[1] Patients with the disease should seek surgical intervention if the conservative treatments fail.[2–5]
The most common surgical management to achieve both decompression of the neural elements and bony stabilization benefit is the standard (S) transforaminal lumbar interbody fusion (TLIF)[6] which was initially developed by Harms and Rolinger in 1982.[7] TLIF has superior advantage in decompressing both central and interbody fusion through a single posterior approach.[8]
Beneficial outcomes have been obtained through the use of traditional open TLIF, even though it often requires a long and midline incision with dissection of bilateral paraspinal soft tissue as well as the posterior tension band for surgical exposure.[9,10] However, multiple studies have reported the destructive disadvantages of the extensive muscle dissection, protracted hospital stays, and postoperative complications associated with traditional open TLIF procedures.[11,12]
Major development in the field of tissue retractors, microscopy, as well as other specialized instruments, spine surgeons over the past decade contribute to great progression where the O-TLIF has been transformed to minimally invasive TLIF (MI-TLIF). Compared with O-TLIF, MIS-TLIF have effects in reducing trauma to paraspinal muscles, improving perioperative outcomes, and decreasing operative morbidity.[13–16]
Unfortunately, the use of MI-TLIF approach remains a drawback with several disadvantages, including limited operative view and space,[16,17] hard learning curve,[18] and high rate of perioperative complications.[19] Thus, the procedure is technically quite different from O-TLIF and the crucial implications are needed to use MI-TLIF over the standard approach.
Conflicting results have been demonstrated in terms of the postoperative and perioperative metrics for MI-TLIF with O-TLIF in several studies and trials. The current meta-analysis is to offer eligible and updated assessment based on aggregated results of benefit effect and risks of O-TLIF and MI-TLIF.
2. Methods and materials
2.1. Search strategy
The following electronic databased were identified and searched by 2 studiers separately: Embase, PubMed, Cochrane library in latest 5 years up to June 2018. The data searching process was conducted in search of all publications with the keywords: “Minimally invasive,” “Transforaminal lumbar interbody fusion,” and “Degenerative lumbar diseases.” We also screened and checked relevant Medical Subject Heading (MeSH) terms ((“transforaminal lumbar interbody fusion”OR “TLIF”) AND (“minimally invasive spine surgery” OR “minimally invasive” OR “MIS”) AND (Degenerative lumbar diseases). In addition, we hand-searched the references of eligible publications that dealt with the topic of interest with an attempt to search associated studies.
2.2. Study selection
To be included in the present meta-analysis, studies should meet the following criteria: the studies were designed comparing MI-TLIF versus O-TLIF; articles that enrolled patients with degenerative lumbar diseases; studies providing data of surgery-related outcomes and postoperative specimens for both 2 groups; only the original literature and the full texts that provide complete data were included. Only publications with most complete information were included if there were any duplications or overlapped data.
2.3. Quality assessment
The retrieved studies were evaluated independently by 2 investigators. Observational studies quality was assessed through the use of Newcastle-Ottawa Quality Assessment Scale.[20]
2.4. Data extraction
Two reviewers conducted and evaluated the data extraction separately. Any arising differences were settled through discussion to reach general consensus. The main categories from selected studies were based on the following items: family name of first author, year of publication, number of recruited participants, study design, study period, pathology of the patients, the outcomes of interest including intraoperative parameters, complications parameters, and pain scores parameters.
2.5. Statistical analysis
The present meta-analysis was conducted through pooling the results of reported incidence of intraoperative parameters and postoperative parameters. We applied Review Manager version 5.3 software (Revman; The Cochrane collaboration Oxford, United Kingdom) to conduct the statistical analyses. Heterogeneity of the trial results was assessed with the I2 statistic to select ideal analysis model[21]:I2 > 50% reflected a moderate to high heterogeneity and random-effects model was utilized; I2 ≤ 50% reflected a low heterogeneity data with the assessment of fixed-effects model.[22] Studies with a P value <.05 was thought to have statistical significance.
Since animal experiment or human was not involved in this study, the ethical approval was not necessary.
3. Results
3.1. Literature search process and study characteristics
Totally, 434 publications were identified originally for study assessment. On basis of abovementioned criteria, there were a total of 15 studies in search of further details. Finally, 10 studies[6,23–31] were included in the present analysis due to 5, 15 publications failed to offer sufficient outcome data of 2 approaches. Figure 1 described the detailed search process.
Figure 1.
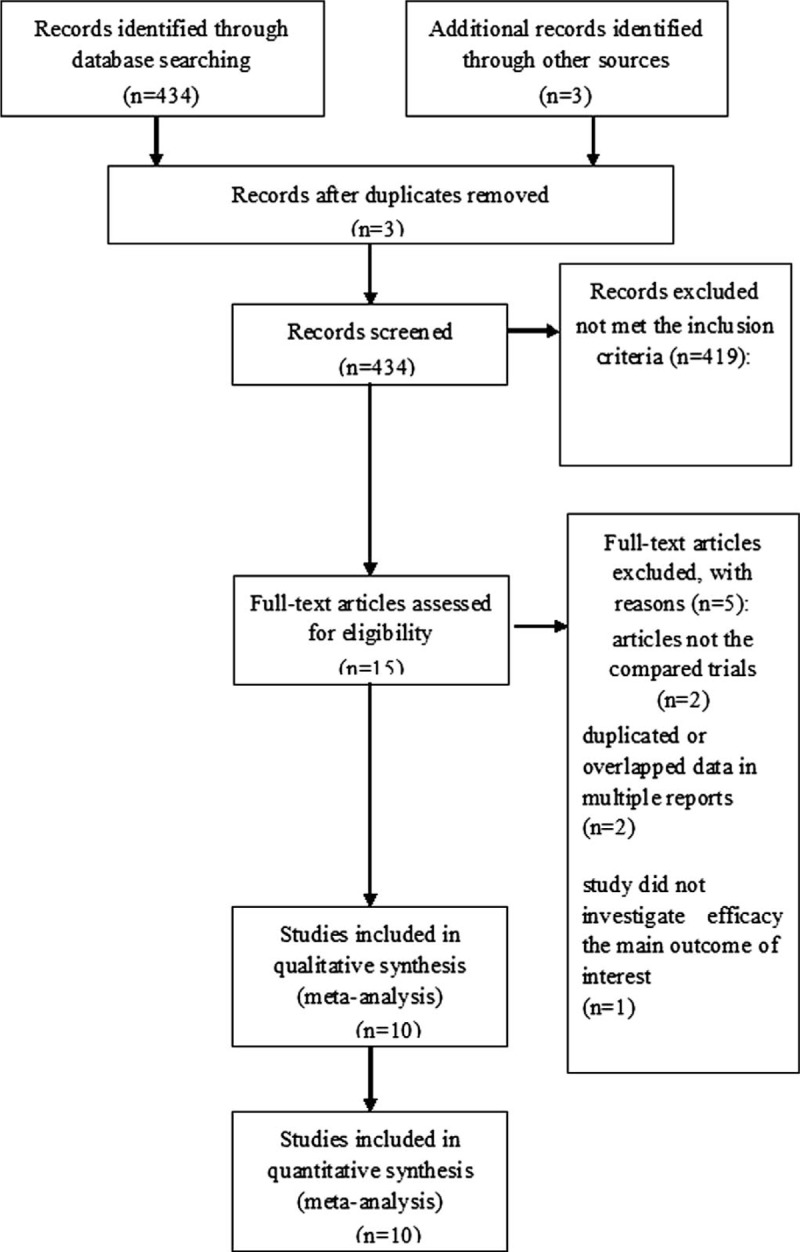
PRISMA flow chart of selection process to identify studies eligible for pooling.
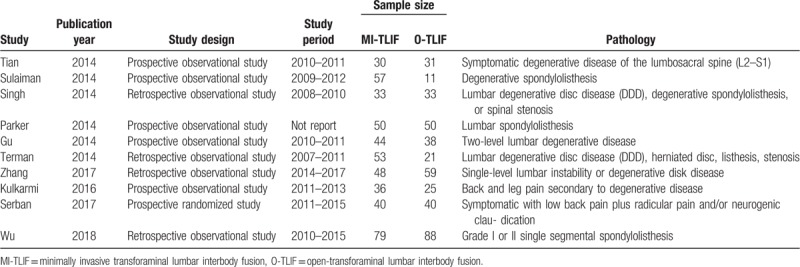
The abovementioned studies were on the bases of the evidence with moderate to high quality. Table 1 described the major characteristics of the qualified studies in more detail.
Table 1.
The major characteristics of the qualified studies in more detail.
3.2. Clinical and methodological heterogeneity
3.2.1. Operation parameters
Pooled analysis of operative time with the comparison of O-TLIF versus MI-TLIF.
Pooling the data from 8 studies showed that no differences in the operate time (SMD = –0.51, 95% CI –1.84–0.81; P = .45) compared MI-TLIF with the O-TLIF group (Fig. 2).
Figure 2.
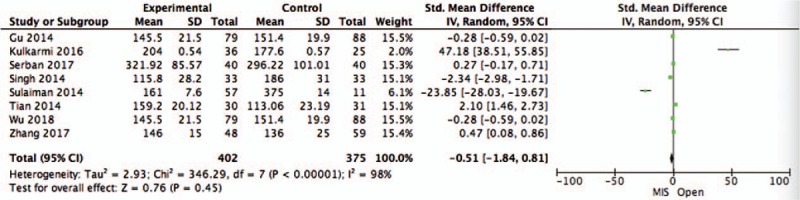
Pooled analysis of operative time with the comparison of O-TLIF versus MI-TLIF. MI-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion.
Pooled analysis of blood loss with the comparison of O-TLIF versus MI-TLIF.
Blood loss rate was available for 8 trials. The pooled data showed that MI-TLIF had strong link to less blood loss (SMD = −2.64, 95% CI −3.62 to −1.65; P < .00001 with O-TLIF) (Fig. 3).
Figure 3.
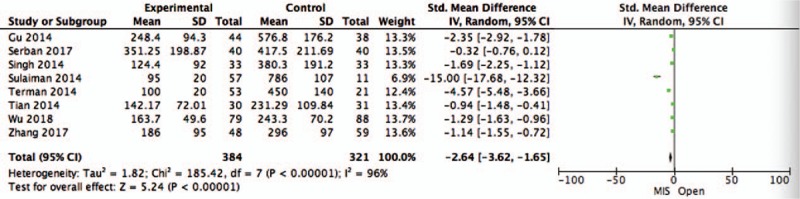
Pooled analysis of blood loss with the comparison of O-TLIF versus MI-TLIF. MI-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion.
Pooled analysis of the hospital duration with the comparison of O-TLIF versus MI-TLIF.
In the analysis of the length of hospital stay, 7 studies were included, as shown in Fig. 4. Results showed that there was shorter rate of length of hospital stay with MI-TLIF (SMD = −0.86, 95% CI −1.70 to −0.02; P = .04).
Figure 4.
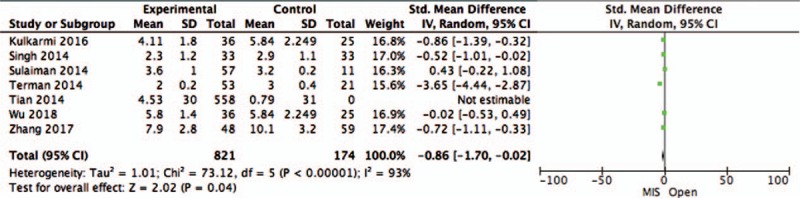
Pooled analysis of the length of hospital stay with the comparison of O-TLIF versus MI-TLIF. MI-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion.
3.2.2. Complications parameters
Pooled analysis of overall complications rate with the comparison of O-TLIF versus MI-TLIF.
We pooled the overall complications rate data with the use of the fixed-effect model, since there was low heterogeneity across the studies. The pooled data showed that MI-TLIF had less overall complications rate (RR = 0.52, 95% CI 0.31–0.86; P = .01) with O-TLIF (Fig. 5).
Figure 5.
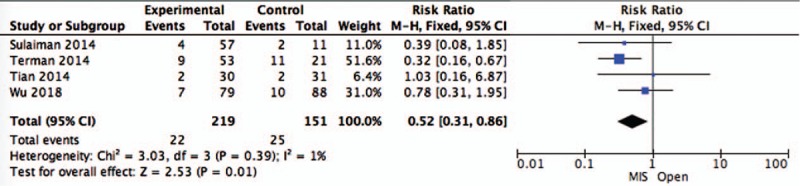
Pooled analysis of overall complications rate with the comparison of O-TLIF versus MI-TLIF. MI-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion.
3.2.3. Pain scores parameters
Pooled analysis of VAS-BP and VAS- with the comparison of O-TLIF versus MI-TLIF.
For the incidence of pain scores, no significant differences were observed in terms of VAS-BP when comparing MI-TLIF with O-TLIF (SMD = −0.42, 95% CI −1.13–0.28; P = .24) (Fig. 6), and VAS-LP (SMD = 0, 95% CI −0.22–0.22; P = 1.00) (Fig. 7).
Figure 6.
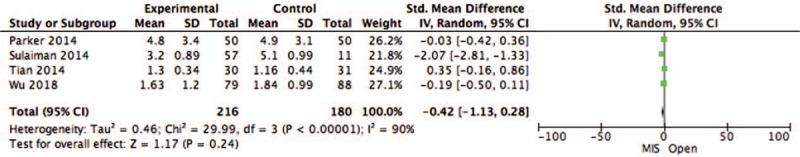
Pooled analysis of VAS-BP with the comparison of O-TLIF versus MI-TLIF. MI-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion.
Figure 7.
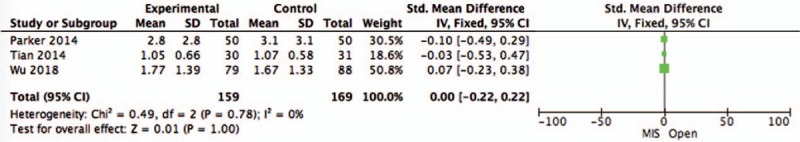
Pooled analysis of VAS-LP with the comparison of O-TLIF versus MI-TLIF. MI-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion.
Pooled analysis of ODI with the comparison of O-TLIF versus MI-TLIF.
The pooling analysis revealed no significant statistical difference in the rate of ODI when comparing MI-TLIF with O-TLIF (SMD = −0.28, 95% CI −0.69–0.13; P = .19) (Fig. 8).
Figure 8.
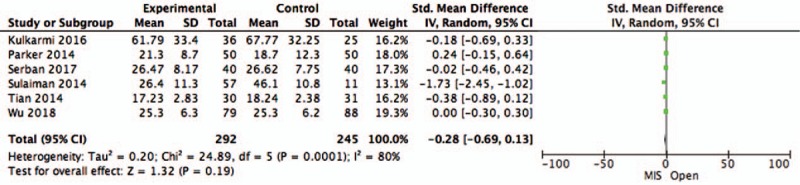
Pooled analysis of ODI with the comparison of O-TLIF versus MI-TLIF. MI-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion.
4. Discussion
Various fusion technologies have been generally applied to treat patients harboring degenerative lumbar diseases.[32] According to earlier reports, the traditional open-TLIF technology is regarded as one of the most commonly used surgical approach, with beneficial effect in decreasing relative nervous complication rate.[10,33,34] However, it was also reported to cause neurologic and vascular damage of the lumbar muscles and low back pain.[35]
Given the paramedian incision during MI-TLIF process, the attachments of the paraspinal musculature as well as the posterior tension band are preserved.[36,37] Thus, the use of the minimally invasive posterior lumbar technique exerts evidential superior outcomes as compared with the open-TLIF approach, such as comparatively less damage to the spinal soft tissues, diminished postoperative pain, and reduced recovery time.[38–40]
Although the perioperative benefits of MI-TLIF have been well documented in the previous literatures, concerns still exist due to its limited operative view and space, hard learning curve and higher costs associated with performing MIS procedures.[16–18] Therefore, high-level data are warranted to assess the overall benefits as well as the risks of O-TLIF and MI-TLIF.
Based on the results of current study and several publications, less dissection of the psoas muscle was required with the use of MI-TLIF, which may contribute to less intraoperative blood loss and shorter duration in hospital compared with open TLIF.[41] However, it must be noted that MI-TLIF has high association with increased operative times according to some studiers.[16,38,42]
The overall results in the present analysis indicated MI-TLIF can be conducted with safe profile without prolonging the operate time compared with conventional open approaches. In this regard, differences are considered to be focused on the learning curve, which is the feature of surgical technique. This may be particularly true of MI-TLIF requires not only anatomy skills, the familiarity with novel instrument with restricted view offered by the tubular retractor system are also demanded. Moreover, during pedicle screw placement, the operation time could be affected due to the increased application of navigation imaging that may attribute to potential exposure to ionizing radiation.[43,44] Common use of MI procedure allows cumulative experience of surgeons and less time for operation.
In terms of the complications parameters, lower rate was observed in the MIS group in comparison of open-TLIF group. The following reasons were believed to potentially contribute to the abovementioned phenomenon: spine surgeons’ progression along the learning curve requires years of practice to gain skill of minimally invasive surgery[45–47]; surgical devices and the equipment improvement may be related to decreased infections. Overall results of minimized intraoperative surgical trauma as well as complications confirmed the shorter hospital duration based on MI-TLIF cohort.
With regard to pain scores outcomes, the differences were reported inconsistently in the publications supported by Seng et al.[40] They have showed worse outcomes in pain with MI-TLIF. Nonetheless, according to Tian et al,[45] there was a trend towards significant reduction in VAS and ODI pain scores in the MI-TLIF group. In our present study, there was no difference between the 2 groups as regard to VAS for leg pain, VAS for back pain, and ODI, which were also consistent with earlier studies.[23,31] Traditionally, MI-TLIF procedures have been performed to have superior benefits over the traditional open procedure in terms of minimizing injury to the nerve roots and decreasing the postoperative back pain. Theoretically, this advantage should result in beneficial outcomes in pain during the perioperative period.[25] In our analysis, the temporal extent of the improvement in pain scores is rather difficult to ascertain due to the heterogeneity in the follow-up protocols among the included studies. According to previous studies, beneficial outcomes in pain as well as disability results were meaningful for long-term follow-ups, but without further improvement.[48,49]
We must point out that the current studies were focused on the use of an updated and well-maintained database. Nevertheless, due to retrospective nature of all included studies’, bias still exists, which may affect of clinical outcomes. While, considering that the preferred surgical procedure varies among different surgeons and serious ethical issue are demanded, it is difficult to set up a clinical RCT to compare the prognosis of patients undergoing O-TLIF and MI-TLIF for the treatment of degenerative lumbar diseases. Furthermore, according to the gold standard for an optimal literature search in surgical systematic reviews,[50] the web of science should be searched. While, we did not search the web of science that may miss the eligible publications.
5. Conclusion
Given the overall results of our analysis, the current study offers moderate evidence to prove the beneficial effect of MI-TLIF on reduced intraoperative blood loss, shorter infection rates during hospital stay, and decreased complications. While no significant differences were observed between 2 study groups in terms of postoperative VAS and ODI pain scores.
Therefore, further acquisition of the minimized intraoperative surgical approach by enhanced skill is necessary to operate for better education as well as safety profile of technics. Additionally, considering the high cost of the current available approach, it is always important to select specific patients for surgery.
Given the beneficial outcomes of MI-TLIF as a valid and alternative method to treat patients with degenerative lumbar diseases, more evidence with sufficient data are demanded to confirm the superiority of MI-TLIF over O-TLIF.
Author contributions
Conceptualization: Ying-Chun Chen.
Data curation: Lin Zhang.
Formal analysis: Lin Zhang, Yu Hou, Wei Yuan.
Methodology: Er-Nan Li.
Project administration: Er-Nan Li.
Resources: Li-Xiang Ding.
Supervision: Li-Xiang Ding.
Validation: Heng-Yuan Zhang.
Visualization: Heng-Yuan Zhang.
Writing – original draft: Ying-Chun Chen.
Writing – review & editing: Ying-Chun Chen.
Footnotes
Abbreviations: HRs = hazard ratios, MeSH = Medical Subject Heading, MIS-TLIF = minimally invasive transforaminal lumbar interbody fusion, O-TLIF = open-transforaminal lumbar interbody fusion, TLIF = transforaminal lumbar interbody fusion.
How to cite this article: Chen YC, Zhang L, Li EN, Ding LX, Zhang GA, Hou Y, Yuan W. An updated meta-analysis of clinical outcomes comparing minimally invasive with open transforaminal lumbar interbody fusion in patients with degenerative lumbar diseases. Medicine. 2019;98:43(e17420).
The authors have no conflicts of interest to disclose.
References
- [1].Wong AP, Smith ZA, Stadler JA, 3rd, et al. Minimally invasive transforaminal lumbar interbody fusion (MI-TLIF): surgical technique, long-term 4-year prospective outcomes, and complications compared with an open TLIF cohort. Neurosurg Clin N Am 2014;25:279–304.. [DOI] [PubMed] [Google Scholar]
- [2].Cloward RB. The treatment of ruptured lumbar intervertebral discs by vertebral body fusion. I. Indications, operative technique, after care. J Neurosurg 1953;10:154–68.. [DOI] [PubMed] [Google Scholar]
- [3].Evans JH. Biomechanics of lumbar fusion. Clin Orthop Relat Res 1985. 38–46.. [PubMed] [Google Scholar]
- [4].Gertzbein SD, Betz R, Clements D, et al. Semirigid instrumentation in the management of lumbar spinal conditions combined with circumferential fusion. A multicenter study. Spine (Phila Pa 1976) 1996;21:1918–25.. discussion 25–6. [DOI] [PubMed] [Google Scholar]
- [5].Goel VK, Kong W, Han JS, et al. A combined finite element and optimization investigation of lumbar spine mechanics with and without muscles. Spine (Phila Pa 1976) 1993;18:1531–41.. [PubMed] [Google Scholar]
- [6].Serban D, Calina N, Tender G. Standard versus minimally invasive transforaminal lumbar interbody fusion: a prospective randomized study. Biomed Res Int 2017;2017:7236970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Harms J, Rolinger H. [A one-stager procedure in operative treatment of spondylolistheses: dorsal traction-reposition and anterior fusion (author's transl)]. Z Orthop Ihre Grenzgeb 1982;120:343–7.. [DOI] [PubMed] [Google Scholar]
- [8].Schwender JD, Hsu BC. Bridwell KH. Minimally invasive posterior surgery for the lumbar spine. The Textbook of Spinal Surgery 3rd ed.Philadelphia: Lippincott Williams & Wilkins; 2011. 1076–7.. [Google Scholar]
- [9].Mehta VA, McGirt MJ, Garces Ambrossi GL, et al. Trans-foraminal versus posterior lumbar interbody fusion: comparison of surgical morbidity. Neurol Res 2011;33:38–42.. [DOI] [PubMed] [Google Scholar]
- [10].Gejo R, Matsui H, Kawaguchi Y, et al. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine (Phila Pa 1976) 1999;24:1023–8.. [DOI] [PubMed] [Google Scholar]
- [11].Moskowitz A. Transforaminal lumbar interbody fusion. Orthop Clin North Am 2002;33:359–66.. [DOI] [PubMed] [Google Scholar]
- [12].Rantanen J, Hurme M, Falck B, et al. The lumbar multifidus muscle five years after surgery for a lumbar intervertebral disc herniation. Spine (Phila Pa 1976) 1993;18:568–74.. [DOI] [PubMed] [Google Scholar]
- [13].Guiot BH, Khoo LT, Fessler RG. A minimally invasive technique for decompression of the lumbar spine. Spine (Phila Pa 1976) 2002;27:432–8.. [DOI] [PubMed] [Google Scholar]
- [14].German JW, Foley KT. Minimal access surgical techniques in the management of the painful lumbar motion segment. Spine (Phila Pa 1976) 2005;30(16 suppl):S52–9.. [DOI] [PubMed] [Google Scholar]
- [15].Scheufler KM, Dohmen H, Vougioukas VI. Percutaneous transforaminal lumbar interbody fusion for the treatment of degenerative lumbar instability. Neurosurgery 2007;60(4 suppl 2):203–12.. discussion 212–3. [DOI] [PubMed] [Google Scholar]
- [16].Shunwu F, Xing Z, Fengdong Z, et al. Minimally invasive transforaminal lumbar interbody fusion for the treatment of degenerative lumbar diseases. Spine (Phila Pa 1976) 2010;35:1615–20.. [DOI] [PubMed] [Google Scholar]
- [17].Wang HL, Lu FZ, Jiang JY, et al. Minimally invasive lumbar interbody fusion via MAST Quadrant retractor versus open surgery: a prospective randomized clinical trial. Chin Med J (Engl) 2011;124:3868–74.. [PubMed] [Google Scholar]
- [18].Lee KH, Yeo W, Soeharno H, et al. Learning curve of a complex surgical technique: minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). J Spinal Disord Tech 2014;27:E234–40.. [DOI] [PubMed] [Google Scholar]
- [19].Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine 2008;9:560–5.. [DOI] [PubMed] [Google Scholar]
- [20].Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of non randomised studies in meta-analyses. Available at: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp Accessed December 27, 2013. [Google Scholar]
- [21].Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002;21:1539–58.. [DOI] [PubMed] [Google Scholar]
- [22].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–60.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Tian W, Xu YF, Liu B, et al. Computer-assisted minimally invasive transforaminal lumbar interbody fusion may be better than open surgery for treating degenerative lumbar disease. Clin Spine Surg 2017;30:237–42.. [DOI] [PubMed] [Google Scholar]
- [24].Sulaiman WA, Singh M. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis grades 1-2: patient-reported clinical outcomes and cost-utility analysis. Ochsner J 2014;14:32–7.. [PMC free article] [PubMed] [Google Scholar]
- [25].Singh K, Nandyala SV, Marquez-Lara A, et al. A perioperative cost analysis comparing single-level minimally invasive and open transforaminal lumbar interbody fusion. Spine J 2014;14:1694–701.. [DOI] [PubMed] [Google Scholar]
- [26].Parker SL, Mendenhall SK, Shau DN, et al. Minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis: comparative effectiveness and cost-utility analysis. World Neurosurg 2014;82:230–8.. [DOI] [PubMed] [Google Scholar]
- [27].Gu G, Zhang H, Fan G, et al. Comparison of minimally invasive versus open transforaminal lumbar interbody fusion in two-level degenerative lumbar disease. Int Orthop 2014;38:817–24.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Terman SW, Yee TJ, Lau D, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: comparison of clinical outcomes among obese patients. J Neurosurg Spine 2014;20:644–52.. [DOI] [PubMed] [Google Scholar]
- [29].Zhang H, Chen ZX, Sun ZM, et al. Comparison of the total and hidden blood loss in patients undergoing open and minimally invasive transforaminal lumbar interbody fusion. World Neurosurg 2017;107:739–43.. [DOI] [PubMed] [Google Scholar]
- [30].Kulkarni AG, Bohra H, Dhruv A, et al. Minimal invasive transforaminal lumbar interbody fusion versus open transforaminal lumbar interbody fusion. Indian J Orthop 2016;50:464–72.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Wu AM, Hu ZC, Li XB, et al. Comparison of minimally invasive and open transforaminal lumbar interbody fusion in the treatment of single segmental lumbar spondylolisthesis: minimum two-year follow up. Ann Transl Med 2018;6:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Lo WL, Lin CM, Yeh YS, et al. Comparing miniopen and minimally invasive transforaminal interbody fusion in single-level lumbar degeneration. Biomed Res Int 2015;2015:168384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Hackenberg L, Halm H, Bullmann V, et al. Transforaminal lumbar interbody fusion: a safe technique with satisfactory three to five year results. Eur Spine J 2005;14:551–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Schwender JD, Holly LT, Rouben DP, et al. Minimally invasive transforaminal lumbar interbody fusion (TLIF): technical feasibility and initial results. J Spinal Disord Tech 2005;18suppl:S1–6.. [DOI] [PubMed] [Google Scholar]
- [35].Tsahtsarlis A, Wood M. Minimally invasive transforaminal lumber interbody fusion and degenerative lumbar spine disease. Eur Spine J 2012;21:2300–5.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Wang MY, Cummock MD, Yu Y, et al. An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J Neurosurg Spine 2010;12:694–9.. [DOI] [PubMed] [Google Scholar]
- [37].Mobbs RJ, Sivabalan P, Li J. Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci 2012;19:829–35.. [DOI] [PubMed] [Google Scholar]
- [38].Brodano GB, Martikos K, Lolli F, et al. Transforaminal lumbar interbody fusion in degenerative disc disease and spondylolisthesis grade I: minimally invasive versus open surgery. J Spinal Disord Tech Epub 2015;28:E559–64.. [DOI] [PubMed] [Google Scholar]
- [39].Lee KH, Yue WM, Yeo W, et al. Clinical and radiological outcomes of open versus minimally invasive transforaminal lumbar interbody fusion. Eur Spine J 2012;21:2265–70.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Seng C, Siddiqui MA, Wong KP, et al. Five-year outcomes of minimally invasive versus open transforaminal lumbar interbody fusion: a matched-pair comparison study. Spine (Phila Pa 1976) 2013;38:2049–55.. [DOI] [PubMed] [Google Scholar]
- [41].Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 2003;28(15 suppl):S26–35.. [DOI] [PubMed] [Google Scholar]
- [42].Parker SL, Adogwa O, Bydon A, et al. Cost-effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion for degenerative spondylolisthesis associated low-back and leg pain over two years. World Neurosurg 2012;78:178–84.. [DOI] [PubMed] [Google Scholar]
- [43].Harris EB, Massey P, Lawrence J, et al. Percutaneous techniques for minimally invasive posterior lumbar fusion. Neurosurg Focus 2008;25:E12. [DOI] [PubMed] [Google Scholar]
- [44].Teitelbaum GP, Shaolian S, McDougall CG, et al. New percutaneously inserted spinal fixation system. Spine (Phila Pa 1976) 2004;29:703–9.. [DOI] [PubMed] [Google Scholar]
- [45].Tian NF, Wu YS, Zhang XL, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: a meta-analysis based on the current evidence. Eur Spine J 2013;22:1741–9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Lau D, Lee JG, Han SJ, et al. Complications and perioperative factors associated with learning the technique of minimally invasive transforaminal lumbar interbody fusion (TLIF). J Clin Neurosci 2011;18:624–7.. [DOI] [PubMed] [Google Scholar]
- [47].Schizas C, Tzinieris N, Tsiridis E, et al. Minimally invasive versus open transforaminal lumbar interbody fusion: evaluating initial experience. Int Orthop 2009;33:1683–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Andersen T, Christensen FB, Niedermann B, et al. Impact of instrumentation in lumbar spinal fusion in elderly patients: 71 patients followed for 2–7 years. Acta Orthop 2009;80:445–50.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Fritzell P, Hagg O, Wessberg P, et al. Swedish Lumbar Spine Study G. 2001 Volvo Award Winner in Clinical Studies: Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine (Phila Pa 1976) 2001;26:2521–32.. discussion 32–4. [DOI] [PubMed] [Google Scholar]
- [50].Goossen K, Tenckhoff S, Probst PS, et al. Optimal literature search for systematic reviews in surgery. Langenbecks Arch Surg 2018;403:119–29.. [DOI] [PubMed] [Google Scholar]


