Abstract
Several studies suggest that neurocysticercosis might be one of the main reasons for onset of seizures in adolescents and young adults in Mozambique, however, no studies have evaluated the burden and impact of the disease in women of childbearing age. This is also true for other parasitic diseases such as toxoplasmosis, toxocariasis and onchocerciasis, although the latter has been reported in some regions in central and northern Mozambique. We describe herein an 18 year old female who was admitted to Hospital Central de Quelimane, Zambézia Province in Mozambique, 8 days after delivery with a misdiagnosis of eclampsia that turned out to be neurocysticercosis. We discuss challenges in the diagnosis of neurocysticercosis in women of childbearing age and the potential for missed diagnosis in those who present with eclampsia and other conditions associated with seizures.
Keywords: Neurocysticercosis, Epilepsy, Pre-eclampsia, Eclampsia, Taenia solium, Pregnancy, Cysticercus cellulosae
Introduction
Cysticercosis is a zoonotic, neglected and preventable parasitic disease caused by the Taenia solium larvae, the Cysticercus cellulosae. It results from the development of larval cysts in humans and pigs after ingestion of food or water contaminated with human feces containing eggs from adult tapeworms [1,2]. Neurocysticercosis (NCC) develops when the larvae are lodged in the central nervous system (CNS), although NCC may be asymptomatic for years after disease is established. Seizures are the most common presentation in 70 −90% of infected patients [3]. Other symptoms of NCC include intracranial hypertension, severe headaches, blindness, chronic meningitis, symptoms due to space-occupying CNS lesions, focal neurological disorders, hydrocephalus, encephalitis, and occasionally psychiatric manifestations and dementia [2,4]. New onset of seizures during pregnancy or post-partum can be confused with pre-eclampsia or eclampsia, as these may also present with seizures, visual changes, altered mental status and cerebral edema [5–8] (See table 1).
Table 1:
Common and differential symptoms of Neurocysticercosis and Eclampsia.
| Symptoms | Neurocysticercosis | Eclampsia |
|---|---|---|
| Epileptic seizures | Present | Present |
| Headache | Present | Present |
| Intracranial hypertension | Present | Present |
| Altered mental status | Sometimes present | Present |
| Symptoms due to space occupying lesion | Sometimes present | Absent |
| Dementia | Sometimes present | Absent |
| Psychiatric manifestations | Sometimes present | Absent |
| Hypertension | Absent | Present |
| Proteinuria | Absent | Present |
| Multiple organ dysfunction and damage | Absent | Present |
| Swollen face or hands | Absent | Present |
Pre-eclampsia/eclampsia affects 2 – 8% of pregnancies worldwide, is associated with 10 – 15% of direct maternal deaths and up to 25% of stillbirths and newborn deaths in developing countries [9].
In 2011, maternal mortality in Mozambique was estimated to be 408 per 100,000 live births, one of the highest rates in the world. The hypertensive disorders of pregnancy (HDP) are responsible for 18% of maternal deaths and represent the third most common cause of maternal deaths [10].
The diagnosis of cysticercosis and NCC relies on clinical and epidemiological data, serology for antibodies or antigen detection, and neuroimaging with magnetic resonance imaging and computed tomography (CT scan). Neuroimaging studies are considered to be the gold standard for the diagnosis of NCC [2]. However, in LICs such as Mozambique only a small fraction of the population has access to neuroimaging tests because of the limited number of available equipment.
Mozambique is still lacking epidemiological data on human and porcine cysticercosis, especially in women of childbearing age. Risk maps based on data such as human and porcine population overlap, pig production systems, poverty rates, sanitation facilities, and water sources, indicate that the central, north and northeast areas of the country, especially the provinces of Manica, Zambézia, Tete, Nampula and Cabo Delgado, might be at higher risk for occurrence of porcine and human cysticercosis [1]. Some cross sectional serological studies conducted in different parts of the country found that between 15 to 21% of apparently healthy children and adults were seropositive for cysticercosis antibodies or antigens, while in neuropsychiatric patients the seroprevalence of cysticercosis was as high as 51% [1]. A community based study conducted in Angónia district, located in the central western part of the country, found that 15% of individuals were positive for cysticercus antigen by ELISA and that among 43 of 75 (57.3%) individuals with epilepsy who tested positive for cysticercus antigens, brain lesions consistent with NCC were observed on CT scans [11]. These data clearly show that cysticercosis is a public health problem of concern in Mozambique.
In this article, we report a case of an 18 year old female who was admitted to Hospital Central de Quelimane (HCQ), Zambézia Province located in the central eastern part of Mozambique, 8 days after delivery, with a misdiagnosis of eclampsia that turned out on further evaluation to be NCC.
Case Summary
An 18 year old immunocompetent woman, G2P2O1, was admitted to the Intensive Care Unit of Hospital Central de Quelimane, in Zambézia Province, Mozambique, comatose, with uncontrolled tonic clonic seizures, status 7/15 Glasgow scale, afebrile (36,5°C) and a presumptive diagnosis of eclampsia was made. Her pulse and blood pressure were 104 beats/min and 99/56 mmHg, respectively. She had undergone an uncomplicated spontaneous vaginal delivery at term eight days before at home. She was given antiepileptic drugs, including phenobarbital and phenytoin, to control seizures, which resolved after 4 days. Blood tests were unremarkable, except for hypoglycemia of 2,9 mmol/ml. Further serologic testing for Taenia solium larval antibodies and antigens using Western Blot IgG kits from LDBIO Diagnostics (www.ldbiodiagnostics.com) and Ag-ELISA assay (http://www.apdiagroup.com), respectively were both positive. A plain CT scan was obtained on day 4 and revealed multiple lesions with different stages ranging from cerebral ring-enhancing cysts with scolices to transitional or degenerative colloidal cysts to multiple parenchymal calcifications, and a definitive diagnosis of NCC was made (See figure 1).
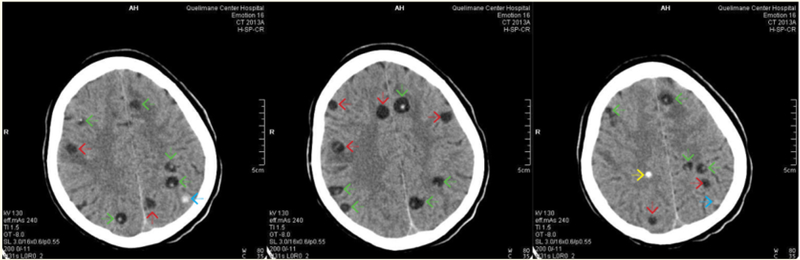
Figure 1:
Non-Contrast Computed Tomography of the brain showing multiple NCC lesions in different stages. The green arrows show hypodense lesions with eccentric hyperdensity (vesicula with scolex- vesicular stage) and perilesional edema. The red arrows show colloidal ring enhancement cyst (loss of scolex) and perilesional edema. The blue arrow shows hyperdense lesion in nodular granular stage. The yellow arrow show punctuate calcification.
Following subsequent interdepartmental discussions, retrospective history was obtained and further physical examination was performed that included eye and neurological examinations. It was noted that the patient had been experiencing episodes of seizures beginning 4 years previously and that this was her second admission to the hospital with the same symptoms. Antiparasitic treatment was postponed to allow post-partum recovery. In the meantime she was prescribed phenobarbital for control of seizures and follow up was arranged for further evaluation and a decision about initiating antiparasitic treatment.
Results and Discussion
This is the first case documented in Mozambique of misdiagnosis of eclampsia subsequently proven to be NCC. There are anecdotal reports in Mozambique, especially in this region of the country, of pregnant women referred to tertiary and quaternary hospitals with diagnosis of pre-eclampsia or eclampsia presenting with seizures and altered mental status, although they had unremarkable physical evaluations, including normal blood pressure and no proteinuria. Similar cases of misdiagnoses have been observed in different parts of the world, such as United States of America, Peru and India [5–8].
Health professionals, including obstetrician-gynecologists, may encounter patients with NCC in their practice and overlook this condition due to a gap in knowledge about cysticercosis/NCC and its clinical features. Following this case, we surveyed 37 health professionals from geographically distinct areas of Mozambique (including Maputo Central Hospital in the south, the General Hospital of Quelimane in Zambezia province, and Nampula Central Hospital in the north), and only 34% of them knew about the disease, its clinical presentation, diagnosis and treatment. So clearly, cysticercosis and NCC are not widely recognized conditions among health professionals in Mozambique and elsewhere, so it is not surprising that misdiagnosis is common and that NCC represents a neglected disease [5–8].
In view of this knowledge gap it should be a public health priority to conduct further research to assess the burden of the disease in LICs including Mozambique, not only in the general population, but also in women of childbearing age. The knowledge generated by these studies can be translated into policies and guidelines allowing policy makers to allocate resources for diagnosis and management of this neglected disease, thus equipping health professionals with knowledge and tools to make an appropriate diagnosis. NCC appears to be a commonly overlooked etiology of seizures that must be included in the differential diagnosis of new onset seizures, particularly in pregnant women, to differentiate from eclampsia and other HDP. In addition, health professionals should be educated about the need for a careful history and clinical assessment, and for the performance of serological testing and neuroimaging, if available, for any pregnant woman presenting with new onset of seizures. NCC should be included in the differential diagnosis of the various causes of the HDP that present with seizures [8]. Despite the scarcity of resources, serological tests for cysticercosis should be made available to health professionals in Mozambique who take care of pregnant and post-partum women to help in diagnosing the etiology of seizures given the fact that both HDP and NCC can coexist, and HDP are the third most common cause of maternal mortality in Mozambique.
Conclusion
NCC should be suspected in all cases of pregnant women with seizures, especially those with normal blood pressure. Protocols for management of pregnant or postpartum women presenting with seizures should include brain CT scan or magnetic resonance imaging wherever available, to exclude NCC even if pre-eclampsia or eclampsia diagnosis is confirmed, as both conditions may present together, although unless the clinical condition is life threatening, neuroimaging and antiparasitic treatment can be postponed until after delivery. In addition, serological tests should be made available to support the diagnosis of NCC, especially in those cases where CT scans might confer a greater risk of adverse effects to the fetus. Health professional education should include skills courses on parasitic causes of epilepsy, especially NCC, to improve diagnosis and management of this zoonotic and neglected disease. To prevent possible transmission of cysticercosis via contaminated hands to their infants, clinicians should consider antiparasitic treatment of postpartum women with a history of seizures with either niclosamide or praziquantel, as they may be possible carriers of the adult tape worm.
What is known about this topic?
NCC is endemic in Africa and other LICs and is the second most common parasitic cause of seizures after malaria.
Pre-eclampsia and eclampsia are estimated to be the third most common cause of maternal deaths in Low Income Countries (LICs) such as Mozambique.
Both NCC and pre-eclampsia or eclampsia can present with seizures, visual changes, intracranial edema and altered mental status leading to a misdiagnosis.
What this case adds?
This is the first case from Mozambique of NCC in a postpartum woman that was misdiagnosed as eclampsia.
This article draws attention to the need for health professionals to be aware that in LICs like Mozambique where, despite the scarcity of imaging tools, diagnosis of NCC should always be considered in the differential diagnosis of pre-eclampsia, eclampsia and HDP in childbearing women.
Serology for cysticercosis should be made available at least for targeted groups such as women of child bearing age presenting with seizures regardless of whether they have HDP or not.
This case reinforces the need for health policy makers to work towards the integration of different health programs as a whole since communicable and non-communicable diseases can affect any person regardless of the problem that takes the patient to the hospital.
Acknowledgements
We express our gratitude to the patient and her relatives who contributed and consent to publish this study.
The publication of this manuscript is supported by the Fogarty International Center of the National Institutes of Health (Office of the Director, National Institutes of Health), Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) National Institute of Neurological Disorders and Stroke (NINDS) under Award Number D43TW010135. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Fogarty International Center or the National Institutes of Health.
Abbreviation
- NCC
Neurocysticercosis
- CNS
Central Nervous System
- LICs
Low Income Countries
- HDP
Hypertensive Disorders of Pregnancy
- CT Scan
Computed Tomography
Footnotes
Conflict of Interest
Authors declare no conflict of interest.
Bibliography
- 1.Afonso SM., et al. “Human and Porcine Taenia Solium Infections in Mozambique: Identifying Research Priorities”. Animal Health Research Reviews.121(2011): 123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carpio A, et al. “Neurocysticercosis: The Good, the Bad, and the Missing”. Expert Review of Neurotherapeutics.184(2018): 289–301. [DOI] [PubMed] [Google Scholar]
- 3.Carpio A and Hauser WA. “Neurocysticercosis and Epilepsy”. Taenia Solium Cysticercosis. From Basic to Clinical Science. Eds. Singh G. and Prabhakar S. New York: CAB Publishing; (2002): 211–220. [Google Scholar]
- 4.Del Brutto OH. “Neurocysticercosis: A Review”. Scientific World Journal (2012): 159821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grondin L, et al. “Neurocysticercosis Masquerading as Eclampsia”. Anesthesiology.1055 (2006): 1056–1058. [DOI] [PubMed] [Google Scholar]
- 6.Sahai S and Sahai A. “Pica Causing Neurocysticercosis in Pregnancy Presenting as Eclampsia: A Report of Two Cases”. Journal of Obstetrics and Gynecology of India.631 (2013): 68–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singhal SR., et al. “Neurocysticercosis as an Important Differential of Seizures in Pregnancy: Two Case Reports”. Journal of Medical Case Reports 5 (2011): 206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Webb C, et al. “Neurocysticercosis in Pregnancy”. AJP Reports.82 (2018): e51–e56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rawlins B, et al. “Screening and Management of Pre-Eclampsia and Eclampsia in Antenatal and Labor and Delivery Services: Findings from Cross-Sectional Observation Studies in Six Sub-Saharan African Countries”. BMC Pregnancy Childbirth.181 (2018): 346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sacoor C, et al. “Health and Socio-Demographic Profile of Women of Reproductive Age in Rural Communities of Southern Mozambique”. PLoS One 132 (2018): e0184249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Assane YA., et al. “Neurocysticercosis in a Rural Population with Extensive Pig Production in Angonia District, Tete Province, Mozambique”. Acta Tropica 165 (2017): 155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]