Abstract
Inflammation after joint injury leads to joint responses that result in eventual osteoarthritis development. Blockade of inflammation, by suppressing NF-κB expression, has been shown to reduce joint injury-induced chondrocyte apoptosis and reactive synovitis in vivo. Herein, we demonstrate that the suppression of NF-κB p65 expression also significantly mitigates the acute pain sensitivity induced by mechanical injury to the joint. These results suggest that early intervention with anti-NF-κB nanotherapy mitigates both structural and pain-related outcomes, which in turn may impact the progression of post-traumatic osteoarthritis.
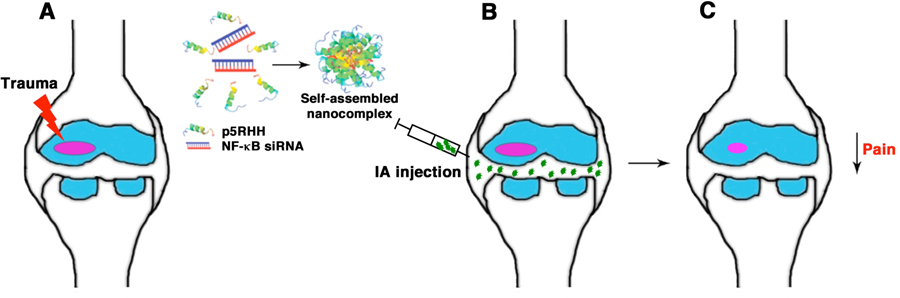
Graphical Abstract
Purpose and Rationale
The goal of this study is to evaluate pain-related outcome following nanotherapy, as pain represents the most common symptom in post-traumatic osteoarthritis but the least monitored outcome in preclinical studies.
Introduction
Post-traumatic osteoarthritis (PTOA) is a form of OA that develops after a joint injury and in which the nature and time of trauma is generally known. PTOA accounts for 12% of all OA but the true incidence may be higher given the long delay between injury and PTOA [1]. Studies have documented a robust inflammatory response in the immediate aftermath of joint injury that persists for months to years [2] and this inflammation likely contributes to sequelae of responses post-injury. While pain is the most common symptom of patients seeking medical consultation, it is one of the least monitored outcomes in preclinical studies of PTOA. Furthermore, current treatment options focus on treating the clinical symptoms and are limited to analgesics and anti-inflammatory drugs, which have so far have shown no disease-modifying effects [2].
NF-κB is a signaling pathway that controls gene products involved in a myriad of cellular responses including inflammation. Using a murine model of non-invasive controlled injurious compressions of the knee joint that allows the examination of cartilage responses at specific time points after trauma [3], we previously showed that intra-articular (IA) delivery immediately after injury, of a nanoparticle (NP) comprising a peptide, p5RHH complexed to siRNA suppressing NF-κB p65 expression, significantly reduced two important early events: chondrocyte apoptosis and synovial inflammation [4]. The goal of the present study was to investigate whether NP-based suppression of NF-κB expression in the joint also reduces injury-induced pain in mice.
Materials and Methods
p5RHH-siRNA NP Preparation
p5RHH-siRNA NP was prepared as previously described [4]: p5RHH peptide (synthesized by Genscript) was dissolved at 10 mM in DNAse-, RNAse-, and protease-free sterile purified water (Cellgro) and stored in 10 μl aliquots at −80°C before use. p65 siRNA (Sigma-Aldrich) was dissolved at 100 μM in 1X siRNA buffer (Thermo Scientific), and stored in 10-μl aliquots at −80°C before use. NPs were prepared by mixing equal volumes of the p5RHH peptide and siRNA at a peptide:siRNA ratio of 100:1 in HBSS with Ca2+ and Mg2+ (Gibco, Life Technologies) and incubated at 37°C for 40 min and then stabilized with albumin at final siRNA concentration of 500 nM before IA injection. This preparation typically results in a nominal NP size of ~ 55 nm after albumin coating, as measured by atomic force microscopy and dynamic light scattering, and zeta potentials varying from +12 to −5.5 mV and polydispersity index varying from 0.120 to 0.190 depending on size and the presence or absence of the exogenously applied albumin coating [5; 6].
Animals
All animal experiments were performed in compliance with federal laws and in strict accordance with the guidelines established by the Division of Comparative Medicine at Washington University. The animal protocol is subjected to annual review and approval by Institutional Animal Care and Use Committee of Washington University.
Noninvasive Mechanical Injury Model
Experiments were performed on 10 to 12-week old male C57BL/6J mice (The Jackson Laboratory, Maine) using a materials testing machine (Instron ElectroPuls E1000) as previously described [4]. In brief, mice were anesthetized and subjected to cyclic axial compressive loads applied to the right knee joint, with loads transmitted through natural joint articulations. Compressive loads were applied at 6 Newtons (N) for 0.34 sec with a rise and fall time each of 0.17 sec and a baseline hold time of 10 sec between cycles for 60 cycles. The uninjured left knees were used as controls. After loading, all the mice were immediately administered 0.5 mg/kg buprenorphine-SR once IA as per protocol, to control pain for the first 72 h.
NP Administration
On day 0, immediately after loading, the right knee was shaved and the skin was scrubbed with betadine prior to IA injection. The right knee was kept in a flexed position and volume of 15 μL of albumin-coated p5RHH-p65 siRNA NP (0.1 μg siRNA, equivalent to siRNA at 7.5 × 10−12 mol) or p5RHH-scrambled siRNA NP (at the same volume and dose) or HBSS (15 μL) was administered IA using a 30-gauge needle. The IA injections were repeated on days 1 and 2 (for a total of 3 doses). The left knees served as non-injured controls. We have previously shown that the articular dwelling time of NP exceeded 48 h although the beneficial effects persisted at least 2 weeks in this model [4].
Pain Assessment
Pain was assessed weekly after loading, up to 21 days using a Small animal ALGOmeter (SMALGO), a pressure-based analgesimeter for easy assessment of pain sensitivity threshold of the animal when applying a progressive force over the relevant location (knee) on the animal. The stimulation was increased until a reaction (shudder or vocalization) from the animal was obtained. The maximum force was then automatically recorded and analyzed. The operator was blinded to the treatment administered.
Statistics
Comparisons between multiple groups (≥ 3) were performed by one-way ANOVA and Bonferroni’s correction for multiple comparisons was performed. P < 0.05 between experimental groups was considered significant.
Results
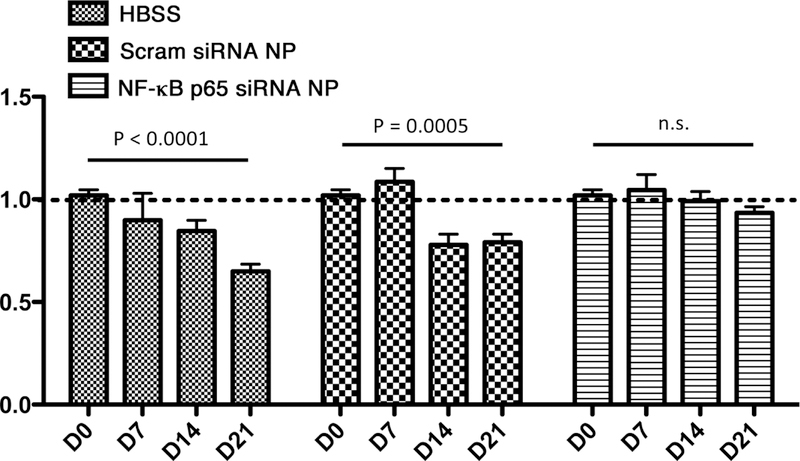
We assessed pain threshold sensitivity following NP treatment using SMALGO. We found that mice treated with p5RHH-p65 siRNA NP maintained pain threshold while animals treated with HBSS or p5RHH-scrambled siRNA NP showed significantly reduced pain threshold (Fig. 1). The attenuating effect observed with p65 suppression lasted at least 21 days after initiation of nanotherapy. These are the first reported outcomes showing mitigation of pain sensitivity following NF-κB suppression in a model of joint injury. While this study provides solid data on pain mitigation in the first 3 weeks post joint injury, further studies would determine dose-response relationship and the time course of therapeutic efficacy with the development of PTOA in this model.
Figure 1. p5RHH-p65 siRNA nanotherapy suppresses pain after joint injury in mice.
Mice were subjected to compression injury (6 N) and treated IA with HBSS, 0.1 μg of p5RHH-p65 or scrambled (scram) siRNA NP (in 15 μL volume) immediately following loading, and again on days 1 and 2 (3×). Threshold sensitivity was assessed by SMALGO on the indicated days. Pain threshold is expressed as the ratio of injured knee/contralateral control knee. Baseline ratio = 1.0. Untreated (HBSS) and scram siRNA NP-treated mice showed significantly reduced threshold. N = 5 per group.
Discussion
Although the involvement of inflammatory responses in the promotion of cartilage catabolism post-joint injury has been extensively studied [2], it remains to be determined whether antagonism of inflammation will also improve pain-related outcomes. Indeed, IA administration of IL-1 receptor antagonist (IL1-ra) exhibits structural disease-modifying effects in a rodent model of PTOA [7]. However, in clinical studies, the administration of commercially available IL-1ra had no effect in fully established knee OA [8] and only offered short-term (2 weeks) improvement in pain and function when administered within the first month following knee injury (NCT00332254) [9]. Early anti-inflammatory intervention has been attempted with broad-spectrum anti-inflammatory drugs such as corticosteroids. A recent study suggests that shutting down early inflammation with dexamethasone in a rabbit PTOA-like model has lasting effect in ameliorating histological cartilage grade but afforded no protection against long-term structural damage [10]. Clinical trials (NCT01692756 and NCT02318433) have been initiated to examine the effects of early anti-inflammatory intervention in joint injury, the results of which are not yet available.
Conclusion
These findings from this study corroborate our previous observations and provide further rationale for targeting NF-κB, not only to mitigate cartilage degeneration and synovial inflammation but also functional outcomes of the inflammatory processes in PTOA.
Acknowledgements
This work was supported in part by NIH grants R01 AR067491, R01 DK102691 R01 AG046927, R01 AR07095, R00 AR064837, P30 AR073752, P30 AR057235, T32 DK108742, and VA Merit Review grant I01BX002714.
References
- [1].Little CB, and Hunter DJ, Post-traumatic osteoarthritis: from mouse models to clinical trials. Nature reviews. Rheumatology 9 (2013) 485–97. [DOI] [PubMed] [Google Scholar]
- [2].Lieberthal J, Sambamurthy N, and Scanzello CR, Inflammation in joint injury and post-traumatic osteoarthritis. Osteoarthritis Cartilage 23 (2015) 1825–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Wu P, Holguin N, Silva MJ, Fu M, Liao W, and Sandell LJ, Early response of mouse joint tissue to noninvasive knee injury suggests treatment targets. Arthritis Rheumatol 66 (2014) 1256–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Yan H, Duan X, Pan H, Holguin N, Rai MF, Akk A, Springer LE, Wickline SA, Sandell LJ, and Pham CT, Suppression of NF-kappaB activity via nanoparticle-based siRNA delivery alters early cartilage responses to injury. Proc Natl Acad Sci U S A113 (2016) E6199–E6208. [DOI] [PMC free article] [PubMed]
- [5].Hou KK, Pan H, Ratner L, Schlesinger PH, and Wickline SA, Mechanisms of nanoparticle-mediated siRNA transfection by melittin-derived peptides. ACS Nano 7 (2013) 8605–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Hou KK, Pan H, Lanza GM, and Wickline SA, Melittin derived peptides for nanoparticle based siRNA transfection. Biomaterials 34 (2013) 3110–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Furman BD, Mangiapani DS, Zeitler E, Bailey KN, Horne PH, Huebner JL, Kraus VB, Guilak F, and Olson SA, Targeting pro-inflammatory cytokines following joint injury: acute intra-articular inhibition of interleukin-1 following knee injury prevents post-traumatic arthritis. Arthritis Res Ther 16 (2014) R134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chevalier X, Goupille P, Beaulieu AD, Burch FX, Bensen WG, Conrozier T, Loeuille D, Kivitz AJ, Silver D, and Appleton BE, Intraarticular injection of anakinra in osteoarthritis of the knee: a multicenter, randomized, double-blind, placebo-controlled study. Arthritis Rheum 61 (2009) 344–52. [DOI] [PubMed] [Google Scholar]
- [9].Kraus VB, Birmingham J, Stabler TV, Feng S, Taylor DC, Moorman CT 3rd, Garrett WE, and Toth AP, Effects of intraarticular IL1-Ra for acute anterior cruciate ligament knee injury: a randomized controlled pilot trial (NCT00332254). Osteoarthritis Cartilage 20 (2012) 271–8. [DOI] [PubMed] [Google Scholar]
- [10].Heard BJ, Barton KI, Chung M, Achari Y, Shrive NG, Frank CB, and Hart DA, Single intra-articular dexamethasone injection immediately post-surgery in a rabbit model mitigates early inflammatory responses and post-traumatic osteoarthritis-like alterations. J Orthop Res 33 (2015) 1826–34. [DOI] [PubMed] [Google Scholar]