Abstract
Background:
The aim of this meta-analysis is to compare the efficacy and safety of combined phacoemulsification (Phaco) with goniosynechialysis (GSL) to either Phaco or to Phaco combined with trabeculectomy or trabeculectomy alone in patients with angle closure glaucoma (ACG).
Methods:
Five main electronic databases were searched for the eligible studies. Intraocular pressure (IOP) decrease was set as the primary outcome, while anti-glaucomatous medication decrease, changes of anterior chamber depth (ACD), range of peripheral anterior synechia (PAS), and complication occurrence were the secondary outcomes. Standard mean difference (SMD) and relative risk (RR) were the size effects for continuous and binomial data, respectively. Either fixed-effects model or random-effects model was chosen to pool the data based on the heterogeneities.
Results:
A total of 7 eligible studies were included. The combined data showed the IOP decreased more significantly after Phaco-GSL than that after Phaco alone (SMD = –0.42,95%CI: –0.70 – 0.14, I2 = 17.6%, Z = 2.90, P = .004). However, there were no distinct differences regarding medication decrease (SMD = –0.25,95%CI: –0.70 – 0.21, I2 = 0%, Z = 1.06, P = 0.29), ACD, the range of PAS and complication occurrence rate when compared Phaco-GSL to Phaco. Moreover, Phaco-GSL was comparable to Phaco-trabeculectomy/trabeculectomy in decreasing IOP (SMD = –0.08, 95%CI = –0.32 – 0.15, I2 = 0%, Z = 0.70, P = .49).
Conclusions:
Phaco-GSL might be an optimal procedure to treat ACG with concomitant cataract due to its bleb-less nature, and its capacity for lowering IOP seems superior to Phaco alone and comparable to Phaco-trabeculectomy/trabeculectomy.
Keywords: angle-closure glaucoma, goniosynechialysis, meta-analysis, phacoemulsification, trabeculectomy
1. Introduction
Angle closure glaucoma (ACG), especially primary angle-closure glaucoma (PACG), is one of the leading causes of irreversible blindness, and it affects about 3.9 million people around the world. Its prevalence is higher in Asian countries than in other countries.[1] Epidemiological data have shown that 86% of PACG patients live in Asia, and 48% of them are in China.[2] Patients with PACG, to some extent, have specific anatomic abnormalities, characterized by the thick lens and short axial length of eyeball which may cause the pupillary block, narrowed anterior chamber and subsequent intraocular pressure (IOP) increase.[3,4] Based on the pathogenesis, removing the thick lens seems to be necessary to treat PACG.
Phacoemulsification (Phaco) is a well-developed technique to extract cataract and has been used for managing PACG, because it can deepen the anterior chamber and eliminate the pupillary block by removing the lens. Several studies have proven that Phaco alone could lower the IOP for the patients effectively,[3,5–7] but its effects may be reduced to treat patients with chronic angle-closure glaucoma (CACG) or with extensive peripheral anterior synechia (PAS).[8] Given that, goniosynechialysis (GSL) was introduced to restore the function of aqueous outflow through stripping the PAS from the angle wall and has shown success to lower IOP.[6,9] Moreover, several studies reported that combined Phaco with GSL (Phaco-GSL) was more effective than GSL alone to decrease IOP.[10,11]
Although some authors suggested that Phaco-GSL may be the optimal option for PACG with concomitant cataract, its superiorities over other procedures (e.g., Phaco alone and Phaco-trabeculectomy) in treating the patients still debate. To compare these procedures, a few comparative studies have been performed in recent years, but the inconsistent results were obtained. Lee et al[12] found that Phaco alone was comparable to Phaco-GSL with respect to IOP decrease in medically well-controlled chronic angle-closure patients. On the contrary, Rodrigues et al[13] reported significantly more IOP reduction was found in Phaco-GSL group when compared to the Phaco group. Given these inconsistent results, it is essential and meaningful to make it clear whether Phaco-GSL has more advantages over other mainstream procedures to treat patients with ACG or not by the means of meta-analysis.
The aim of this study is to systematically review the comparative studies about either Phaco-GSL vs Phaco or Phaco-GSL vs Phaco-trabeculectomy/trabeculectomy to treat ACG, and meta-analyzed the data regarding IOP decrease, anti-glaucomatous medication reduction, anterior chamber depth (ACD) deepening, best corrected visual acuity (BCVA) improvement and complication occurrence.
2. Methods
This study followed the preferred Reporting Items for Systematic review and Meta-analysis (PRISMA) guidelines. All the analyses in this study were based on previous published studies; therefore, ethical approval is not necessary for systematic review and meta-analysis.
2.1. Strategy for study searching
Two independent reviewers (Yang Liu and Wenjie Li) searched 5 main electronic databases: PUBMED, EMBASE, OVID MEDLINE, Cochrane Library, and Clinical Trial gov. The 2 reviewers used the PICOS principle to find out related literatures. Specifically, P (Participant) was the patients with ACG; I (Intervention) included either Phaco or Phaco-GSL or Phaco-trabeculectomy or trabeculectomy. C (Comparison) was defined as comparisons between Phaco and Phaco-GSL or between Phaco-GSL and Phaco-trabeculectomy or trabeculectomy. However, the two reviewers did not define the O (Outcome) and S (Subgroup) strictly to avoid missing some related citations. Both Mesh terms and alternative terms (or their acronyms) with the same meanings were used to expand the searching scope. In addition, Boolean operators were employed to connect these terms for harvesting more target studies. The specific indexing strategy was as follows: (“primary angle closure glaucoma” OR “PACG” OR “angle closure glaucoma” OR “ACG” OR “acute angle closure” OR “AAC” OR “chronic angle closure” OR “CAC” OR “peripheral anterior synechia” OR “PAS”) AND [(“Phacoemulsification” OR “Phaco” OR “ultrasonic emulsification” OR “cataract extraction” OR “cataract surgery” OR “intraocular lens” OR “IOL”) OR (“gonio∗” OR “goniosynechialysis” OR “GSL” OR “anterior chamber separati∗”) OR (“trabeculectomy” OR “filtrate∗ surgery”)]. The searching date was due no July 6th 2018, and only literatures written in English were indexed. After searching the databases, the two reviewers compared their results and solved discrepancies by discussion.
2.2. Study selection
The studies complied with the following criteria were included in this meta-analysis:
-
(1)
studies of comparing Phaco-GSL with either Phaco or Phaco-trabeculectomy or trabeculectomy were included;
-
(2)
studies that only adopted Phaco rather than other means to remove cataract, such as extracapsular cataract extraction (ECCE), manual small incision cataract surgery (MSICS), were included;
-
(3)
the main outcomes of the studies should at least include IOP decrease and/or decrease of IOP-lowering medications.
On the other hand, studies adhered to one of the following criteria were excluded:
-
(1)
one-armed studies on evaluating one of the procedures (Phaco, Phaco-GSL, Phaco-trabeculectomy and trabeculectomy);
-
(2)
patients with open-angle glaucoma were treated by the procedures;
-
(3)
studies that cataract was extracted without IOL implantation were also excluded.
The 2 reviewers selected studies through the inclusion/exclusion criteria independently, and discussion was conducted until consensus achieved.
2.3. Participants and interventions
Patients with angle closure combined with cataract, no matter what the range of the angle closure and the course were, were all the participants in this study. The interventions included Phaco, Phaco-GSL, Phaco-trabeculectomy and trabeculectomy.
2.4. Clinical outcomes
To reduce the variations among the included studies, the absolute value of IOP decrease (preoperative IOP minus postoperative IOP) was set as the primary outcome. The unit of IOP was expressed as mmHg. Additionally, medication decrease, ACD and complications after the procedures were the secondary outcomes.
2.5. Data extraction and management
Characteristics of each study, including author, publication year, study design, region, sample size, mean age of the participants, female/male ratio, diagnosis, the range of angle closure, the definition of success, details of the procedures and follow-up, were all retrieved and managed by the 2 reviewers. After that, the reviewers compared their extractions and discussed when discrepancies existed between them.
2.6. Study quality of evaluation
When considering most of the included studies were random controlled trials (RCTs), we employed the Cochrane Collaboration tool to assess the qualities of the studies. The tool consists of seven parts, including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias, which could be used to evaluate the risk of bias of the RCT comprehensively. Based on the tool, each part could be assessed and assigned as “low risk of bias”, “high risk of bias” or “unclear risk of bias”. The 2 reviewers evaluated the qualities of the studies via the tool respectively and solved their discrepancies through discussion.
2.7. Size effects and statistical analyses
We hired Stata 14.0 (Stata Corp LLC, College Station, TX) to conduct all the statistical analyses. Standard mean difference (SMD) instead of mean difference (MD) was chosen as the main size effects to compare the IOP and medication decrease after the procedures. In addition, relative risk (RR) was employed to compare the occurrence rate of complication between the procedures. All the size effects were expressed as mean and 95% confidence interval (CI). When distinct heterogeneity existed after pooling the data (P value for Chi2 less than .1 or I2 > 50%), the random-effects model was used; while the fixed-effects model was hired to combine the data in case of insignificant heterogeneity (P value for Chi2 more than .1 or I2 < 50%). P < .05 was considered as the significant threshold.
3. Results
3.1. Study selection
As mentioned in the Methods section, the 2 reviewers searched and selected targeted studies independently. After the process, they compared their results, and the consistence rate between them was as high as 93%. Figure 1 shows the flow diagram to select eligible studies. A total of 367 records were retrieved from the electronic databases. After removing 37 duplicates, the other 330 records were screened by titles, and 289 citations were excluded due to their unrelated topics. Then the remaining 41 records were browsed by abstracts, and 29 non-comparative studies were picked out according to our exclusion criteria. After that, 12 studies were screened carefully by checking the full-texts, and five of them were excluded for the following aspects: case reports (2 records), literature review (2 records) and the main outcomes not included (1 record). Finally, seven eligible studies were included in the quantitative synthesis.
Figure 1.
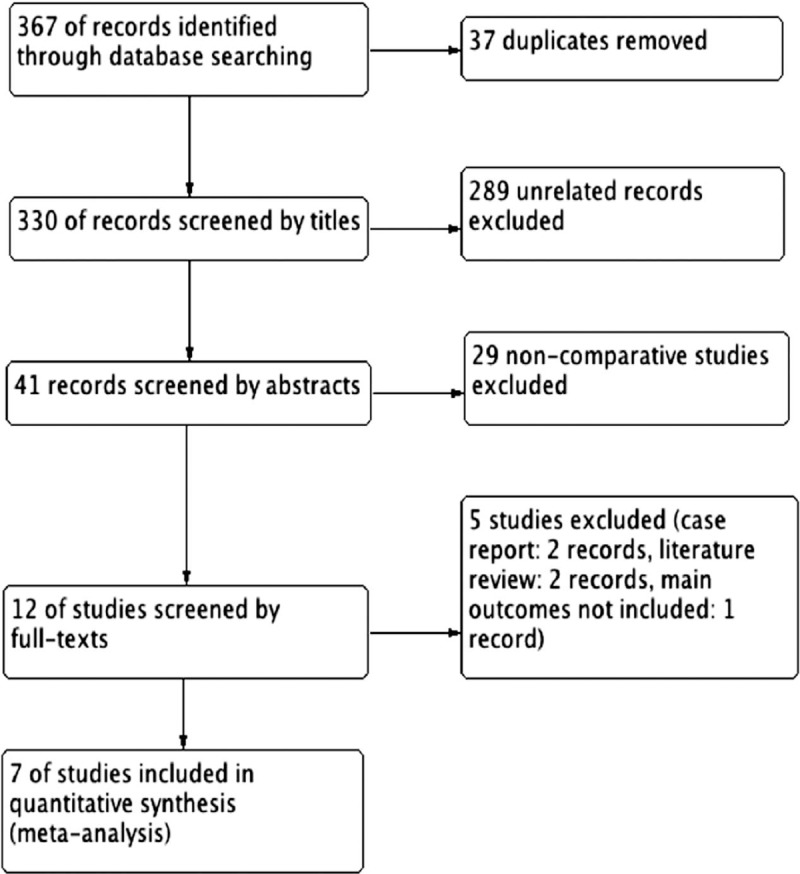
Diagram for selecting eligible studies.
3.2. Characteristics of included studies
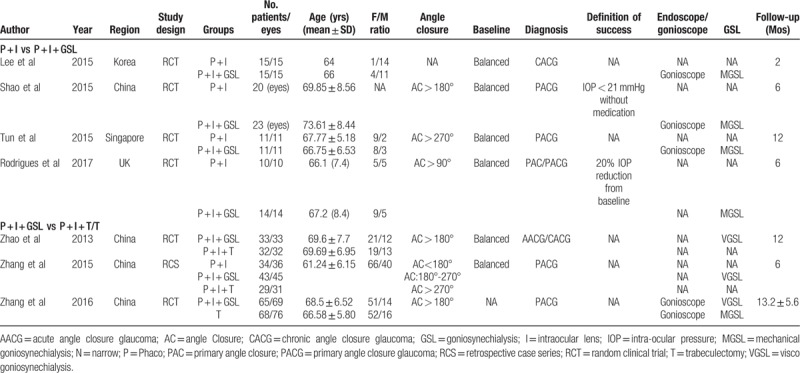
Table 1 demonstrates the characteristics of the eligible studies. These studies were all published in recent years, spanned from 2013 to 2017. Except for one study,[13] the other 6 studies [5,8,14–17] were all carried out in Asian countries: China, Korea and Singapore. Of the seven studies, 6 were RCTs and only 1 study was retrospective case series (RCS). Four of them were comparative studies about comparing Phaco to Phaco-GSL, and three focused on comparison between Phaco-GSL and Phaco-trabeculectomy/trabeculectomy. The sample sizes of these studies were relatively small, and a total of 444 eyes were included in this meta-analysis. All the participants were diagnosed as ACG, and the range of angle closure varied among these studies (from 90° to 360°). Four studies used gonioscope when they performed GSL; whereas the others did not mention it clearly. Moreover, 5 studies employed mechanical GSL (MGSL); while the other 2 hired viscoelastic GSL (VGSL) to separate the angle closure. The follow-up spanned from 2 months to 13.2 months.
Table 1.
Characteristics of included studies.
3.3. Study quality
Table 2 shows the details of assessing each of the studies by the tool. Overall, the qualities of the included studies were reckoned to be acceptable, mostly with a low or unclear risk of bias, although some of them did not state random sequence generation, allocation concealment and blinding methodology clearly. Figure 2 summarizes the risk of bias of these studies.
Table 2.
Assessment for included studies.
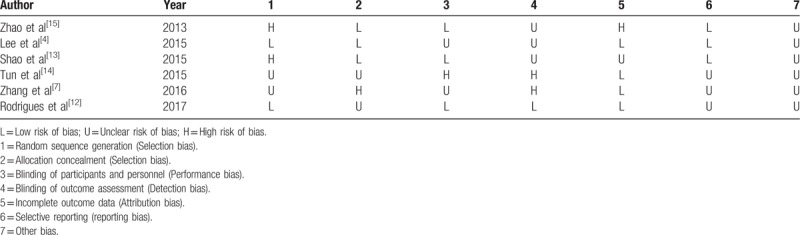
Figure 2.
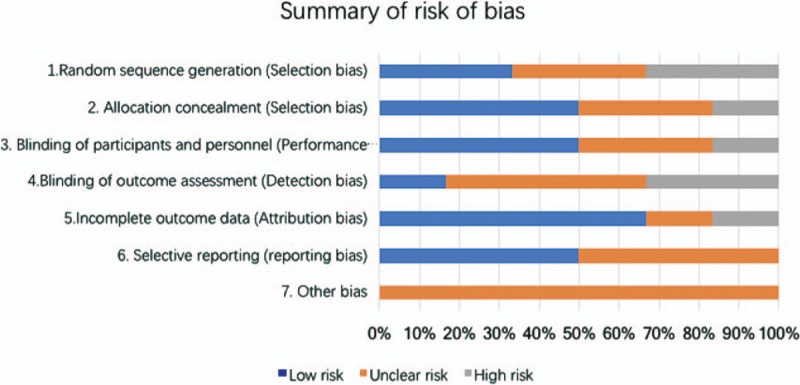
Summary of risk of bias.
3.4. Comparison between Phaco-GSL and Phaco
Figure 3 represents the forest plot of IOP decrease between Phaco and Phaco-GSL. The pooled SMD was –0.42 (95%CI: −0.70– −0.14, I2 = 17.6%, Z = 2.90, P = .004), which indicates that the IOP decrease after Phaco-GSL was significantly more than that achieved by Phaco alone. However, the medication decrease showed no distinct difference between the 2 procedures (Fig. 4), and the pooled SMD was –0.25 (95%CI: –0.70 – 0.21, I2 = 0%, Z = 1.06, P = .29). There was no significant difference regarding the changes of the ACD between the 2 procedures (Fig. 5, SMD = –0.35,95%CI: –0.99 – 0.30, I2 = 71.6%, Z = 1.06, P = .29). Moreover, the range of PAS after the 2 procedures represented no distinct difference (SMD = –0.60,95%CI: –1.31 – 0.12, I2 = 55.9%, Z = 1.64, P = .10). Regarding the complications, as shown in Figure 6, no severe complications occurred, and the occurrence rates between the 2 procedures proved to be insignificantly different (Fig. 7, RR = 1.03, 95%CI: 0.94 – 1.14, I2 = 0%, Z = 0.65, P = .51).
Figure 3.
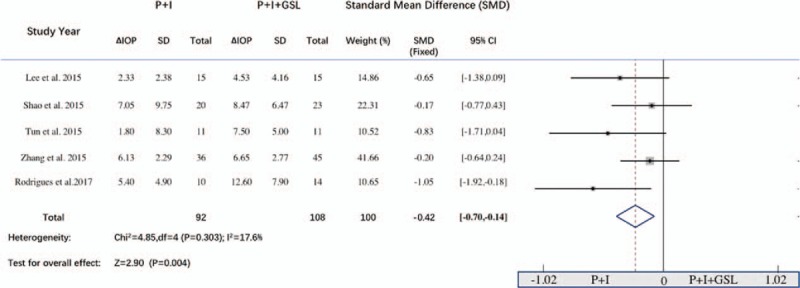
Forest plot for comparing Phaco-GSL to Phaco in decreasing intraocular pressure.
Figure 4.
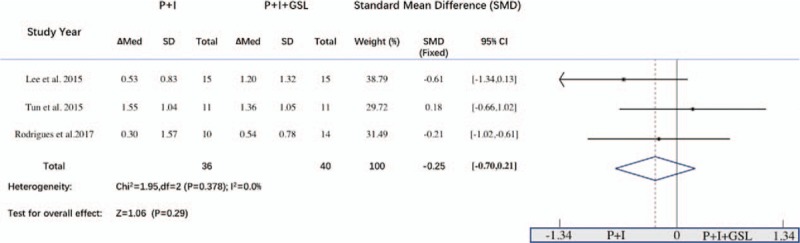
Forest plot for comparing Phaco-GSL to Phaco in decreasing medications.
Figure 5.
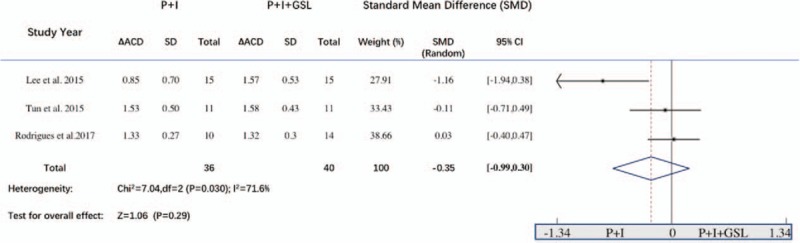
Forest plot for comparing Phaco-GSL to Phaco in deepening anterior chamber depth.
Figure 6.
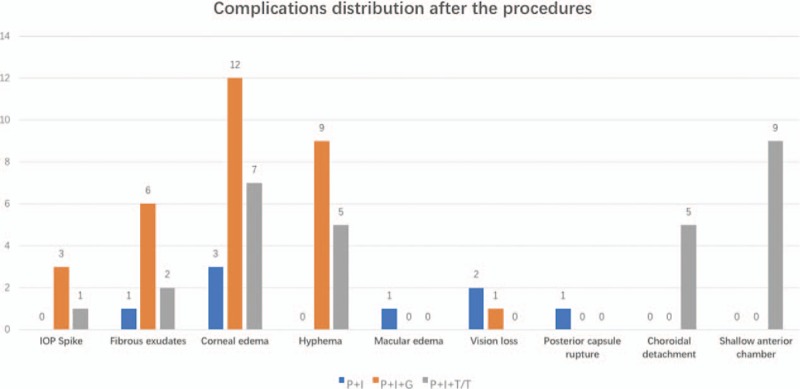
Complications distribution after the three procedures (Phaco, Phaco-GSL, phaco-trabeculectomy/trabeculectomy).
Figure 7.
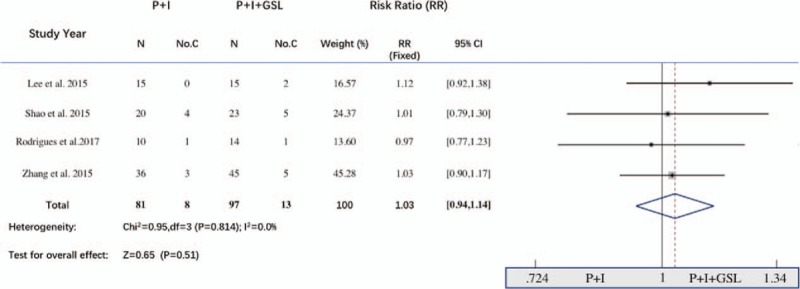
Forest plot for comparing Phaco-GSL to Phaco regarding complications.
3.5. Comparison between Phaco-GSL and Phaco-trabeculectomy/ trabeculectomy
Figure 8 shows the forest plot of IOP decrease between Phaco-GSL and Phaco-trabeculectomy/trabeculectomy. The combined data indicates that there was no significant difference (SMD = –0.08, 95%CI = –0.32-0.15, I2 = 0%, Z = 0.70, P = .49). Similarly, the occurrence rate of complication (Fig. 9, RR = 1.06, 95%CI = 0.97 – 1.17, I2 = 0%, Z = 1.24, P = .22) was comparable between the procedures.
Figure 8.
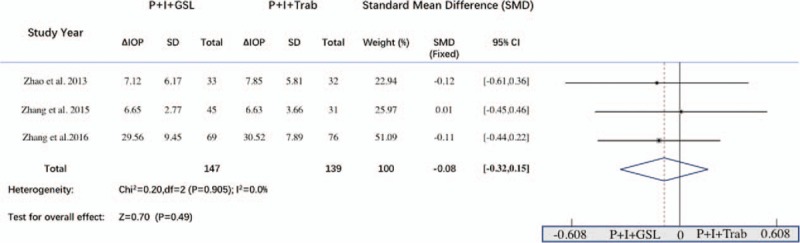
Forest plot for comparing Phaco-GSL to Phaco-trabeculectomy/trabeculectomy in decreasing intraocular pressure.
Figure 9.
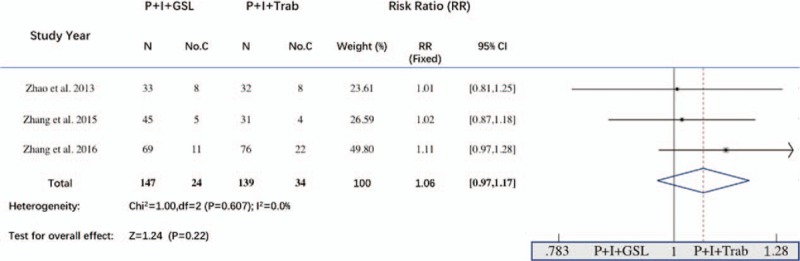
Forest plot for comparing Phaco-GSL to Phaco-trabeculectomy/trabeculectomy regarding complications.
4. Discussion
In this meta-analysis, we combined the data retrieved from the comparative studies (either Phaco vs Phaco-GSL or Phaco-GSL vs Phaco-trabeculectomy/trabeculectomy) in aim of revealing the superiorities of Phaco-GSL to treat ACG. The pooled results showed that Phaco was inferior to Phaco-GSL in decreasing IOP, but the 2 procedures represented comparable abilities regarding anti-glaucomatous medication decrease and ACD deepening. The complication occurrence rate showed insignificant difference between the procedures. The combined data also demonstrated Phaco-trabeculectomy/ trabeculectomy was not superior to Phaco-GSL to treat ACG.
The thick lens and short axial length of eyeball are very common for the patients with ACG, which could cause shallow anterior chamber and pupillary block to a large extent.[18,19] Nowadays, Phaco is the safe way to deepen the anterior chamber by removing the lens, and the thinner IOL could also eliminate the possibility of pupillary block. Moreover, the intraoperative irrigation pressure in the closed anterior chamber, as well as perfusate flush, also exert forces to reopen the angle. Besides that, Zhang et al[8] assumed that the ultrasonic power might influence the function of the ciliary body and decrease the aqueous secretion. Based on these aspects, Phaco alone, to some extent, has effects to reduce the IOP, which has been verified by several clinical investigations.[3,5–7] Nevertheless, for the patients with chronic angle closure or large range of angle adhesion, Phaco may not work well to decrease the IOP. GSL has been proven the effective means to separate the anterior synechia from the angle wall in case of angle closure and adhesion, by which the angle could be reopened and more aqueous humor could outflow through the trabecular meshwork.[21,22] As mentioned above, for treating ACG, Phaco only has the effects of eliminating pupillary block and deepening the anterior chamber, but Phaco-GSL also affiliates the aqueous humor outflow. Therefore, the effects of Phaco-GSL to decrease IOP should be superior to Phaco, which has been proven by our pooled result.
Surprisingly, we did not find Phaco-GSL had more advantages over Phaco to decrease anti-glaucomatous medications by the combined data, which was not paralleled to the result that Phaco-GSL decreased IOP more significantly. We assume the insignificant difference was caused by the small sample size, unbalanced baseline IOP and short follow-up periods (from 2 to 12 months). Similarly, the pooled PAS changes showed no distinct difference between Phaco and Phaco-GSL, which might be also explained by the biases mentioned above. As for the pooling data with respect to ACD, it is reasonable that Phaco was comparable to Phaco-GSL, because the deepened ACD was achieved just by removing the lens and implanting IOL rather than by GSL.
In this meta-analysis, we also compared the effects to decrease IOP between Phaco-GSL and Phaco-trabeculectomy/trabeculectomy. Tsai et al[21] reported that combined trabeculectomy with cataract extraction had the similar effects of lowering IOP when compared to trabeculectomy alone, so we combined the data of Phaco-trabeculectomy and trabeculectomy (Phaco-trabeculectomy/trabeculectomy). The pooled result showed the capacity of Phaco-GSL to decrease IOP was equivalent to that of Phaco-trabeculectomy/trabeculectomy. Although the combined data indicates that the complication occurrence rate was comparable between Phaco-GSL and Phaco-trabeculectomy/trabeculectomy, severe complications, such as shallow anterior chamber, supra-choroidal detachment, hypotony and macular edema, occurred commonly after Phaco-trabeculectomy/trabeculectomy. More importantly, bleb-related complications (e.g., bleb leakage, bleb scarring and blebitis), especially bleb scarring, always occurs frequently in younger patients and leads to surgical failures and uncontrolled IOP when without using Mitomycin C during the surgeries.[23] Trabeculectomy is a classical procedure to decrease IOP by creating an extra filtering pathway. Different to trabeculectomy, GSL aims to rebuild the function of the trabecular meshwork, so it is more natural and physiological to facilitate aqueous outflow. Moreover, Phaco-GSL is easier to manipulate and more time-saving than Phaco-trabeculectomy/trabeculectomy. Based on these facts, Phaco-GSL seems to be superior to Phaco-trabeculectomy/trabeculectomy to manage ACG due to its angle-based nature, less severe complications and simple manipulations. However, trabeculectomy or other filtering surgeries may be the only options in case of treating patients with angle closure >1 year or with irreversible impairment of the drainage function.[20,24,25]
5. Limitations
Although Phaco-GSL has been used to treat ACG for several years, large sample-sized and multi-centered clinical trials have not been carried out until now, so the studies with small sample size included in this meta-analysis may bias the validities of the pooled results. Moreover, among these studies, different enrollment criteria and definition of success and variations for manipulative details (e.g., MGSL or VGSL) altogether might invalidate the reliabilities of the combined results. Given these limitations, multi-centered, large sample-sized RCT with standard criteria should be performed before confirmative conclusions could be drawn.
In conclusion, Phaco-GSL might be an optimal procedure to treat ACG with concomitant cataract due to its bleb-less nature, and its capacity for lowering IOP seems superior to Phaco alone and comparable to Phaco-trabeculectomy/trabeculectomy.
Author contributions
Conceptualization: Yang Liu, Xiaojun Li.
Data curation: Yang Liu, Wenjie Li, Xudong Jiu, Lin Liu, Chengying Yan, Xiaojun Li.
Formal analysis: Yang Liu, Wenjie Li, Xunwen Lei.
Methodology: Yang Liu, Wenjie Li, Xudong Jiu, Chengying Yan.
Resources: Xunwen Lei.
Software: Yang Liu, Xudong Jiu, Xunwen Lei, Lin Liu, Chengying Yan.
Writing – original draft: Yang Liu.
Writing – review & editing: Yang Liu.
Footnotes
Abbreviations: ACD = anterior chamber depth, ACG = angle closure glaucoma, BCVA = best corrected visual acuity, CACG = chronic angle closure glaucoma, ECCE = extracapsular cataract extraction, GSL = goniosynechialysis, IOP = intraocular pressure, MD = mean difference, MGSL = mechanical GSL, MSICS = manual small incision cataract surgery, PACG = primary angle closure glaucoma, PAS = peripheral anterior synechia, Phaco = phacoemulsification, RCS = retrospective case series, RCT = random controlled trial, RR = relative risk, SMD = standard mean difference, VGSL = viscoelastic GSL.
How to cite this article: Liu Y, Li W, Jiu X, Lei X, Liu L, Yan C, Li X. Systematic Review and Meta-Analysis of Comparing Phacoemulsification Combined with Goniosynechialysis to other mainstream procedures in treating patients with angle-closure glaucoma. Medicine. 2019;98:42(e17654).
The authors have no funding and conflicts of interests to disclose.
References
- [1].Tojo N, Otsuka M, Miyakoshi A, et al. Improvement of fluctuations of intraocular pressure after cataract surgery in primary angle closure glaucoma patients. Graefes Arch Clin Exp Ophthalmol 2014;252:1463–8.. [DOI] [PubMed] [Google Scholar]
- [2].Congdon N, Wang F, Tielsch JM. Issues in the epidemiology and population-based screening of primary angle-closure glaucoma. Surv Ophthalmol 1992;36:411–23.. [DOI] [PubMed] [Google Scholar]
- [3].Shrivastava A, Singh K. The effect of cataract extraction on intraocular pressure. Curr Opin Ophthalmol 2010;21:118–22.. [DOI] [PubMed] [Google Scholar]
- [4].Zhng X, Wang J, Li Y, et al. Diagnostic test accuracy of Spot and Plusoptix photoscreeners in detecting amblyogenic risk factors in children: a systemic review and meta-analysis. Ophthalmic Physiol Opt 2019;39:260–71.. [DOI] [PubMed] [Google Scholar]
- [5].Lee YH, Yun YM, Kim SH, et al. Factors that influence intraocular pressure after cataract surgery in primary glaucoma. Can J Ophthalmol 2009;44:705–10.. [DOI] [PubMed] [Google Scholar]
- [6].Lai JS, Tham CC, Lam DS. The efficacy and safety of combined phacoemulsification, intraocular lens implantation, and limited goniosynechialysis, followed by diode laser peripheral iridoplasty, in the treatment of cataract and chronic angle-closure glaucoma. J Glaucoma 2001;10:309–15.. [DOI] [PubMed] [Google Scholar]
- [7].Gunning FP, Greve EL. Lens extraction for uncontrolled angle-closure glaucoma: long-term follow-up. J Cataract Refract Surg 1998;24:1347–56.. [DOI] [PubMed] [Google Scholar]
- [8].Zhang H, Tang G, Liu J. Effects of phacoemulsification combined with goniosynechialysis on primary angle-closure glaucoma. J Glaucoma 2016;25:e499–503.. [DOI] [PubMed] [Google Scholar]
- [9].Lai JS, Tham CC, Chua JK, et al. Efficacy and safety of inferior 180 degrees goniosynechialysis followed by diode laser peripheral iridoplasty in the treatment of chronic angle-closure glaucoma. J Glaucoma 2000;9:388–91.. [DOI] [PubMed] [Google Scholar]
- [10].Harasymowycz PJ, Papamatheakis DG, Ahmed I, et al. Phacoemulsification and goniosynechialysis in the management of unresponsive primary angle closure. J Glaucoma 2005;14:186–9.. [DOI] [PubMed] [Google Scholar]
- [11].Takanori K, Toshihiro I, Masaru I. Long-term efficacy of goniosynechialysis combined with phacoemulsification for primary angle closure. Graefes Arch Clin Exp Ophthalmol 2013;251:825–30.. [DOI] [PubMed] [Google Scholar]
- [12].Lee CK, Rho SS, Sung GJ, et al. Effect of goniosynechialysis during phacoemulsification on IOP in patients with medically well-controlled chronic angle-closure glaucoma. J Glaucoma 2015;24:405–9.. [DOI] [PubMed] [Google Scholar]
- [13].Rodrigues IA, Alaghband P, Agullo LB, et al. Aqueous outflow facility after phacoemulsification with or without goniosynechialysis in primary angle closure: a randomised controlled study. Br J Ophthalmol 2017;101:879–85.. [DOI] [PubMed] [Google Scholar]
- [14].Shao T, Hong J, Xu J, et al. Anterior chamber angle assessment by anterior-segment optical coherence tomography after phacoemulsification with or without goniosynechialysis in patients with primary angle closure glaucoma. J Glaucoma 2014;24:647–55.. [DOI] [PubMed] [Google Scholar]
- [15].Tun TA, Baskaran M, Perera SA, et al. Swept-source optical coherence tomography assessment of iris-trabecular contact after phacoemulsification with or without goniosynechialysis in eyes with primary angle closure glaucoma. Br J Ophthalmol 2015;99:927–31.. [DOI] [PubMed] [Google Scholar]
- [16].Zhao XJ, Yang XX, Fan YP, et al. Comparison of combined phacoemulsification, intraocular lens implantation, and goniosynechialysis with phacotrabeculectomy in the treatment of primary angle-closure glaucoma and cataract. Asia Pac J ophthalmol 2013;2:286–90.. [DOI] [PubMed] [Google Scholar]
- [17].Zhang ZM, Niu Q, Nie Y, et al. Reduction of intraocular pressure and improvement of vision after cataract surgeries in angle closure glaucoma with concomitant cataract patients. Int J Clin Exp Med 2015;8:16557–63.. [PMC free article] [PubMed] [Google Scholar]
- [18].Chen MJ, Cheng CY, Chou CK, et al. The long-term effect of Nd:YAG laser iridotomy on intraocular pressure in Taiwanese eyes with primary angle-closure glaucoma. J Chin Med Assoc 2008;71:300–4.. [DOI] [PubMed] [Google Scholar]
- [19].Zhang S, Wang J, Li Y, et al. The role of primary intraocular lens implantation in the risk of secondary glaucoma following congenital cataract surgery: a systematic review and meta-analysis. PloS One 2019;14:e0214684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Campbell DG, Vela A. Modern goniosynechialysis for the treatment of synechial angle-closure glaucoma. Ophthalmology 1984;91:1052–60.. [DOI] [PubMed] [Google Scholar]
- [21].Tsai HY, Liu CJ, Cheng CY. Combined trabeculectomy and cataract extraction versus trabeculectomy alone in primary angle-closure glaucoma. Br J Ophthalmol 2009;93:943–8.. [DOI] [PubMed] [Google Scholar]
- [22].Li Y, Wang J, Chen Z, et al. Effect of hydrophobic acrylic versus hydrophilic acrylic intraocular lens on posterior capsule opacification: meta-analysis. PLoS One 2013;8:e77864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in the tube versus trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol 2015;153:789–803.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Teekhasaenee C, Ritch R. Combined phacoemulsification and goniosynechialysis for uncontrolled chronic angle-closure glaucoma after acute angle-closure glaucoma. Ophthalmology 1999;106:669–74.. [DOI] [PubMed] [Google Scholar]
- [25].Ma Q, Su J, Li Y, et al. The chance of permanent cure for micro and macroprolactinomas, medication or surgery? A systematic review and meta-analysis. Front Endocrinol 2018;9:363. [DOI] [PMC free article] [PubMed] [Google Scholar]


