Abstract
South Africa has adopted pre-exposure prophylaxis (PrEP) as a preventive strategy for populations at-risk for HIV, though uptake is low among adolescents and young adults. We examined the awareness and use of PrEP among adolescents and young adults in the Eastern Cape, South Africa.
This cross-sectional study was conducted between June and November 2018 among 772 adolescents and young adults (aged 16–24 years) selected using stratified random sampling in a South African university. An electronic self-administered questionnaire was used to elicit demographic information, behavioral, family-related characteristics, awareness and use of PrEP. Adjusted and unadjusted logistic regression models were used to examine the predictors of PrEP awareness.
The overall level of PrEP awareness was 18.8%; however, only 1.7% of participants had used PrEP, 7.5% of had seen it, 4.8% knew how much it cost, and 14.8% knew where and how to get it. In the adjusted regression analysis, only adequate family support (AOR: 2.11; CI: 1.47–3.04) and discussions of HIV and sexually transmitted infections with sexual partners (AOR: 1.78; CI: 1.19–2.67) were associated with a higher likelihood of being aware of PrEP.
The level of awareness and use of PrEP is still very low among adolescents and young adults who may need it to prevent HIV infection. Poor awareness of PrEP among adolescents and young adults in high HIV risk settings may limit its use. Thus, concerted efforts are needed to promote awareness and access to PrEP among young South African adults.
Keywords: adolescents, HIV transmission, pre-exposure prophylaxis, PrEP, South Africa, young adults
1. Introduction
Pre-exposure Prophylaxis (PrEP) has been widely regarded as a biomedical prevention strategy for population groups that are highly vulnerable to contracting HIV.[1] Several clinical trials have demonstrated unequivocally the effectiveness of a combination of Tenofovir disoproxil fumarate and emtricitabine (Truvada) in reducing the risk of HIV transmission.[2,3] Based on such findings, the US Food and Drug Administration ratified usage of Truvada drug as PrEP in 2012.[4] Since then, PrEP was embraced in many countries including USA, UK, France, China, and South Africa among others.[5] The World Health Organization (WHO) has recently recommended its adoption as one of the strategies to combat new HIV infections among population groups vulnerable to HIV.[6]
Despite the adoption of PrEP as part of the strategies to fight new HIV infections, the global rate of new HIV transmission remains high. According to UNAIDS (7), about 1.8 million people got infected in 2017; with 66% of these infections reported to have occurred in sub-Saharan Africa. The same report indicates that Eastern and Southern Africa regions accounted for the highest proportion of the new HIV infections. Of this, South Africa has remained the most affected country, with 33% of all new HIV infections.[7] More importantly, however, is the fact that late adolescents and young adults disproportionately bear the burden of new HIV infections in sub-Saharan Africa.[8] As reflected in the UNAIDS gap report, new HIV infection trends are declining in the age group 15 to 24 years, yet HIV prevalence among young women remains consistently higher than that of young men across Eastern and Southern Africa region.[9] In the South African context, young women aged 15 to 24 years accounted for 37% of all new HIV infections in 2017.[7]
PrEP is effective in the prevention of HIV transmission; however, its use is hindered by poor awareness of this method.[10] At the time of the study by Auerbach, Kinsky[11] in the US, women were found to be hugely disappointed for not having been informed about PrEP since its introduction. In fact, a recent PrEP study in the US revealed that only 39% of participants knew about PrEP.[12] What is more, only a few studies have assessed the level of PrEP knowledge, determinants of PrEP awareness, and attitudes to and likelihoods of PrEP uptake.[11] Most of such studies were carried out in the global north, leaving a considerable knowledge gap in other the global south.
The South African National Department of Health[13] approved PrEP in December 2015 on condition that users would combine it with other safe sexual practices. PrEP was later rolled out by the National Department of Health in June 2016 with strict guidelines which at the time focused on sex workers only.[14] Notwithstanding, current updates on PrEP guidelines now accommodates other groups at high risk of HIV infection such as serodiscordant couples, young women and adolescent girls as well as men who have sex with men (MSM).[14] South Africa has a high HIV and sexual violence prevalence,[15,16] especially among young adults.[7,17] However, research on awareness of PrEP, especially among late adolescents and young, is still scarce. There is, therefore, a need to carry out further research on PrEP awareness to establish the extent to which groundwork has been done in marketing and educating clients about this biomedical strategy. Given this context, the current study attempts to assess the PrEP awareness gaps in South Africa inhibiting robust implementation and uptake of PrEP.[18,19]
2. Methods
2.1. Study design
This study adopts a quantitative approach, which was very useful in statistically profiling awareness gaps of PrEP among students.[18] It was carried out at the East London Campus of the University of Fort Hare in South Africa, which was selected purposively. Our choice is influenced by the scientific evidence indicating that new HIV incidence is disproportionately high among adolescents and young adults[7] and especially girls. University students were purposively selected for this study, as they are easily accessible. Students who are married or over the age of 24 years were excluded from the study as well as postgraduate students.
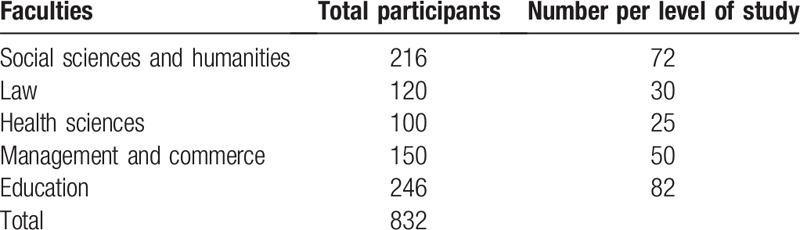
We use a MaCorr Sample Size Calculator to estimate the sample size, at ±3.3% precision level, a 95% confidence level, and the population of 6000 students. That means a sample size of 769 students is required; however, 833 participants were selected in anticipation of possible attrition. A total of 61 of these students were excluded from the study as they had not answered the critical research question on whether or not they were aware of PrEP; thereby limiting our participants to only 772. Stratified sampling method was used for participant's selection to ensure inclusiveness and representativeness, and stratification was based on participant's sex, year of study and faculties. We were unable to get a list of all students and their contacts; as such, we selected our participants in their classrooms. We divided the sample size to all faculties in proportion to the size of each faculty and equally per level of study (see Table 1). The classroom for each level of study was visited on the days they had a general faculty course. Since the ratio of male to female students was 2:3 at the university, we recruited more female participants (60%) into the study than male students. We used trained research assistants who were postgraduate students to administer the questionnaire in the classrooms. They were trained to select every tenth student in the classroom and skip participants who refuse to participate. The level of participation was impressive with a response rate of 92%.
Table 1.
Sample selection per faculty and year of study.
The University of Fort Hare ethical review body approved this study (Reference number: GON011). Before administering each questionnaire, researchers endeavored to provide participants with such information as study purpose, process and usage of findings. The principle of voluntary participation guided the study as participants were required to sign an informed consent form. Researchers promised participants to uphold all ethical research considerations such as anonymity and confidentiality of the information provided. The study followed all the IRB guideline for research using human subjects.
2.2. Data collection
Data for this study were collected between June and November 2018. We recruited and trained five research assistant who were graduate students for this study. The training was on how the importance of obtaining participants’ consent, conducting the interview, handling of data, ensuring quality data and on how to administer a self-designed questionnaire using smarts phones with the open data kit (ODK) collects application for Android. The mobile app (application) ensured privacy for participants in completing the questionnaire. We first administered the data collection instrument to 30 students from a different university as a pilot survey to validate the questionnaire before actual data collection was conducted. The lessons learned from the pilot study helps to validate and further improve the questionnaire.
2.3. Measures
Awareness of PrEP was the primary dependent variable in this study. We asked participants if they have ever heard of PrEP, a drug that can prevent HIV transmission if used before sex. Also, we asked questions on knowledge of where and how to obtain it and if they have ever used PrEP. The responses were binary options of yes or no.
The main independent variables include family structure, which was operationalized “single-parent family” or “both parents family” or “foster family”. The second independent variable was family support, which was measured by asking: “what is the level of support you receive from your family? This was accompanied by responses such as: “adequate support”, “moderate”, “insufficient”, and “no support” to be chosen by participants. However, in the bivariate analysis, we grouped the responses into two, with “moderate” to “no support” grouped as inadequate support. The third independent variable was sexual behavior and was assessed by asking a question on whether participants have ever had sex. Respondents were also provided with two responses of either a “Yes” or a “No”. Also, we assessed whether participants have ever tested for HIV and participants needed to choose either a “Yes” or a “No” from the provided responses. The last independent variable assessed partner communication on HIV/sexually transmitted infections (STIs) and participants were to choose their response from the dichotomously provided responses of either a “Yes” or a “No”. Participants also reported their ‘age’ (which was categorized as 16–19 years and 20–24 years), and ‘sex’ (which was limited to only male and female students).
2.4. Data analysis
We used the IBM Statistical Package for Social Sciences (SPSS) version 24.0 (Chicago, IL) to analyze the data. Obtained data were checked for data entry errors by running a frequency distribution for all variables. A logic check was performed and data entry errors observed were corrected. We then used descriptive statistics to generate frequencies and percentage distribution for participants’ demographic characteristics, the level of HIV testing and participant's PrEP knowledge and utilization. With the aid of both the adjusted and unadjusted logistic regression models, we examined the determinants of PrEP awareness. The unadjusted model was used to examine the independent effect of each independent variable on PrEP awareness. The adjusted model was fitted to understand the net effect of each independent variable on PrEP awareness. The analysis was performed at 95% confidence interval, while only P values less than .05 were regarded as statistically significant.
3. Results
3.1. Demographic findings
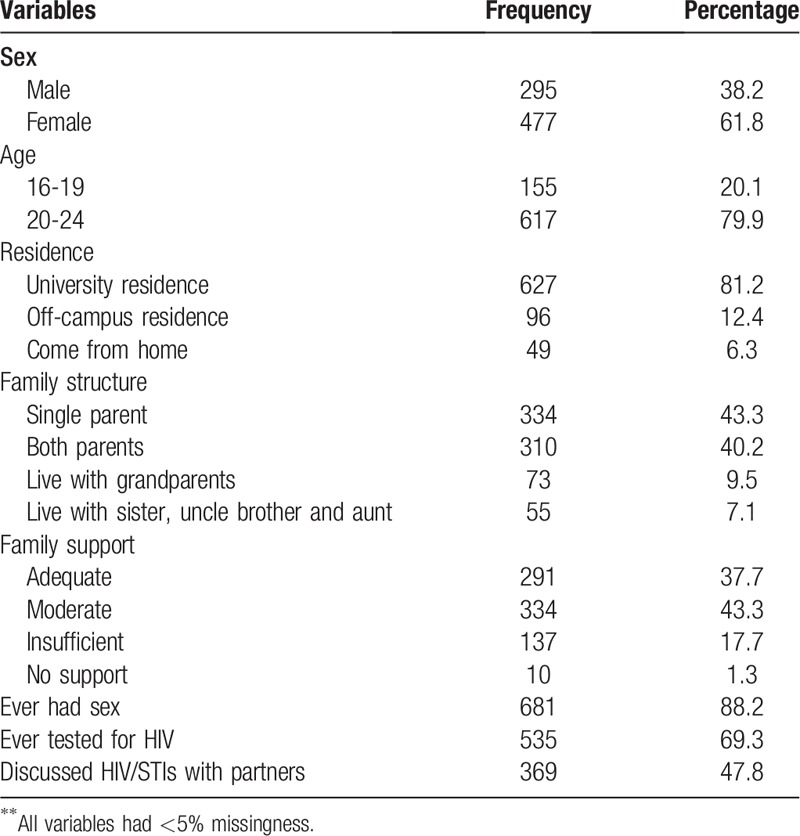
The analysis was limited to 772 unmarried adolescents and young adults with complete responses on awareness of PrEP. The response rate was 92%. The average age for all study participants was 21.10 years (SD = 1.70). Most of the participants were young adults (aged 20–24 years) (79.9%), resided in university residence (81.2%), sexually active (88.2%), and had tested for HIV (69.3%) as shown in Table 2 below.
Table 2.
Demographic and behavioural characteristics of participants.
3.2. Descriptive findings
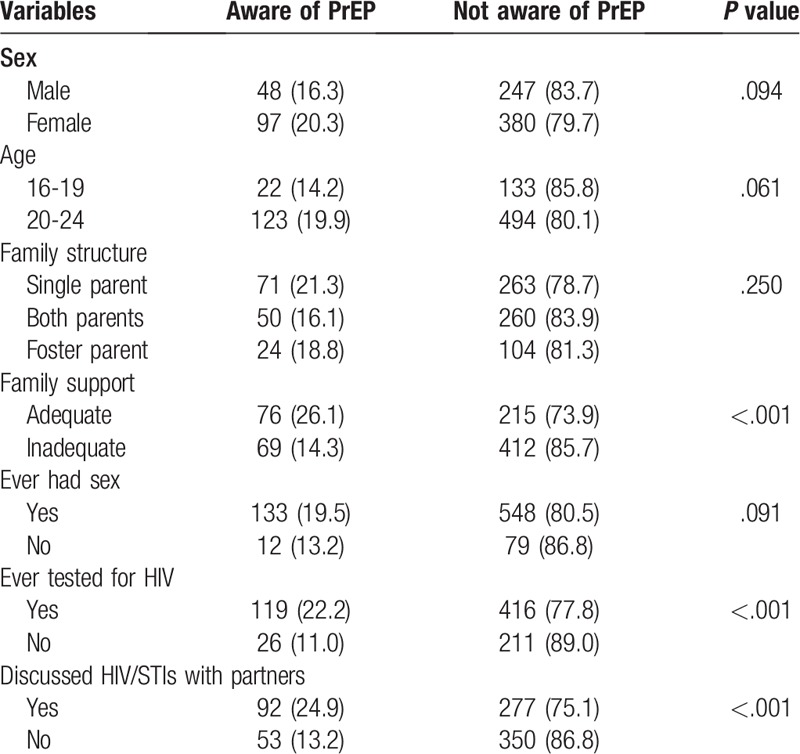
As indicated in Table 2 below, the level of awareness of PrEP was 18.8%, but with variations across demographic and behavioral characteristics (Table 3). There was no difference in PrEP awareness of PrEP between females and males (20.3% and 16.3%, respectively, P = .094), and among individuals aged 20-24 years compared to those aged 16 to 19 years (19.9% vs 14.2%, P = 0.061)”. However, PrEP awareness was significantly higher among adolescents, and young adults who were either screened for HIV or discussed HIV with sexual partners compared those who had not (P < .05). Only 1.7% of participants had use PEP, 7.5% of them has seen it, 4.8% knew how much it cost, and 14.8% knew where and how to get it.
Table 3.
Chi-square analysis for demographic and behavioural correlates of PrEP awareness.
3.3. Multivariable findings
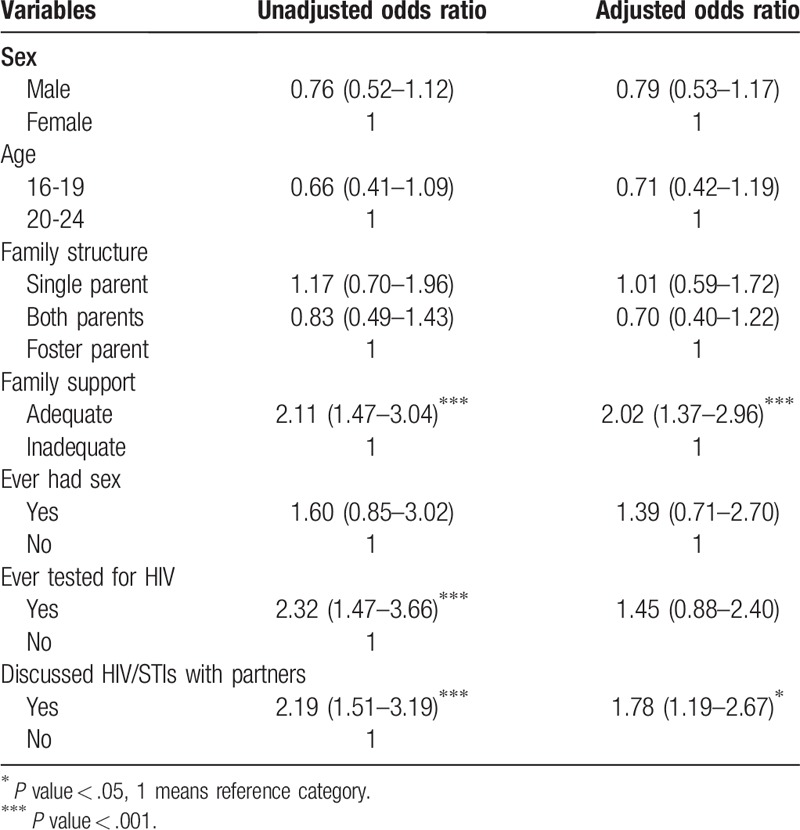
The inclusion of variables in the models was based on existing literature on demographic and behavioral factors impacting health outcomes. Since our study population is a homogenous population of young adults, we focus on their demographic, behavioral and family characteristics. We first used the unadjusted model to assess the independent result of each independent variable on PrEP awareness. The results of the unadjusted model show that family support, discussed HIV/STIs with sexual partner(s) and ever screened for HIV were significantly associated with awareness of PrEP. However, in the adjusted regression model, after including the demographic controls, only family support, and discussed HIV/STIs with sex partners reached the level of significance. The effect of ever tested for HIV on awareness of PrEP reduced in the adjusted model, but the direction of the effect remains. Individuals who reported adequate family support were more likely to report PrEP awareness ‘twice’ more than those who received inadequate family support. Also, participants who had discussions on HIV/STIs with sex partners indicated a higher likelihood of PrEP awareness as opposed to individuals who otherwise had not done so (Table 4).
Table 4.
Results of adjusted and unadjusted models showing determinants of PrEP awareness among adolescents and young adults.
4. Discussion
This study examines PrEP awareness among a selected cohort of adolescent and young adults in the Eastern Cape, South Africa. The study revealed that 18.8% of participants were aware of PrEP. Our finding is comparable with the previous research from the US, which reported low awareness of PrEP (20.3%) among black MSM at risk of HIV infection.[10] Even women at high risk of HIV infection in the US were found to be highly concerned about not being informed about PrEP, despite been approved some years back.[11] Low PrEP awareness has been reported in sub-Saharan Africa.[21–23] The rationale behind low awareness of PrEP among populations highly vulnerable to contracting HIV could be explained from the view that providers of PrEP have not fully intensified PrEP awareness campaigns since the program is fairly new.[20] More so, since populations of high HIV infection risk are usually placed at the periphery of social structures,[24–26] this implies that it may take longer for them to be contacted or to access PrEP information. The consequence is evident in the fact that uptake of PrEP has been generally slow over the years.[25]
Further to this, our study found that awareness of PrEP was higher among adolescents and young adults who had tested for HIV (22.2%) than those who had not (11.0%). This finding corroborates past studies.[12,27,28] The possible explanation for this development is that individuals who tested for HIV, especially recently, may have learnt about PrEP as a method of preventing HIV during pre-test or post-test counseling at the HIV testing centers. Also, social marketing information on PrEP may be found in the clinics as compared to other venues, which young adults commonly visit.
Our study also shows that awareness of PrEP was higher among those who had discussions HIV/STIs with their sex partners, which is somewhat consistent with a previous study.[28] What we derive from this finding is that discussion between partners creates a platform for sharing information around HIV, including that of PrEP. Open communication about HIV could also make partners assess information on potential prevention methods. A study has shown that couple communication is associated with a higher likelihood of HIV testing.[29] It is also possible that people that are aware of PrEP are more likely to share the information with their partners.
The study also found that individuals who received adequate family support were more aware of PrEP as compared to those with inadequate family support. Adequate family support could mean financial and social support; as such, individuals who are from families that are adequately supported them may be more exposed to health information from their family. Past studies have shown the importance of family, social, peer and partner support in health outcomes.[30,31] Therefore, the influence of family support on health decisions and on information that one is exposed to should never be underestimated as a determinant of PrEP awareness.
Given the low level of PrEP awareness reported in this study, it is not surprising that the level of use is also very low. This calls for a comprehensive approach from all providers and promoters of PrEP to craft awareness campaigns that not only address age, gender or individual behavioral characteristics; but provide PrEP for at-risk population who are willing to use to it. Given the high prevalence and incidence of HIV in the 15 to 24-year olds in South Africa, innovative biomedical strategies are urgently needed to reduce the transmission risk in this cohort. As such, expansion of access to PrEP to all vulnerable populations, including adolescents and young adults through awareness campaigns might be a game-changer in South Africa.
5. Strength and limitation of the study
Studies that investigate PrEP awareness gaps, especially among young adults in areas of high HIV prevalence and sexual violence are few. This study is significant in that it provides insights into the level of PrEP awareness among young people in such regions. However, data for this study was drawn only from university students who are more educated than the general adolescents and young adults’ population in the country. This means that these findings cannot be generalized to the entire South African population. Questions on PrEP awareness should be included in the South African Demographic and Health Survey, which is the largest and most representative survey in the country, to estimate a generalizable level of PrEP awareness.
6. Conclusion
This study reveals that awareness of PrEP is low among individual participants examined in the study setting. Poor awareness of PrEP among individuals in high HIV risk settings is a barrier to its use in preventing HIV and therefore, suggests that the potential benefit of PrEP in preventing HIV will remain unrealized if a concerted effort is not made to improve its awareness. The study established that partner communication about HIV/STIs and adequate family support are associated with a higher likelihood of PrEP awareness. There is, therefore, a need to urgently bolster efforts that promote accessibility and awareness of PrEP in regions that are characterized by high HIV prevalence and sexual violence.
Acknowledgment
We acknowledge all the study participants for participating in this study. Also, the efforts of the research assistants, who worked assiduously towards ensuring the collection of quality data are well appreciated. Finally, authors wish to acknowledge both the University of Fort Hare and the African Population and Health Research Centre for providing an enabling environment for the completion of this work.
Footnotes
Abbreviations: HIV = human immunodeficiency syndrome, MSM = men who have sex with men, ODK = open data kit, PrEP = pre-exposure prophylaxis, STIs = sexually transmitted diseases, UNAIDS = The Joint United Nations Programme on HIV/AIDS.
How to cite this article: Ajayi AI, Mudefi E, Yusuf MS, Adeniyi OV, Rala N, Goon DT. Low awareness and use of pre-exposure prophylaxis among adolescents and young adults in high HIV and sexual violence prevalence settings. Medicine. 2019;98:43(e17716).
The authors have no funding and conflicts of interest to disclose.
Data will be made available by the corresponding author upon request.
References
- [1].Flash CA, Frost EL, Giordano TP, et al. HIV Pre-exposure prophylaxis program implementation using intervention mapping. Am J Prevent Med 2018;54:519–29.. [DOI] [PubMed] [Google Scholar]
- [2].McCormack S, Dunn DT, Desai M, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet 2016;387:53–60.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Donnell D, Baeten JM, Bumpus NN, et al. HIV protective efficacy and correlates of tenofovir blood concentrations in a clinical trial of PrEP for HIV prevention. J Acquir Immun Defic Syndr (1999) 2014;66:340–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Jaspal R, Nerlich B. Polarised press reporting about HIV prevention: Social representations of pre-exposure prophylaxis in the UK press. Health 2017;21:478–97.. [DOI] [PubMed] [Google Scholar]
- [5].Wilton J, Senn H, Sharma M, et al. Pre-exposure prophylaxis for sexually-acquired HIV risk management: a review. HIV/AIDS (Auckland, NZ) 2015;7:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].World Health Organization Consolidated Guidelines on HIV Prevenfion, Diagnosis, Treatment, and Care for Key Populafions: 2016 Update. Geneva: WHO; 2018. [PubMed] [Google Scholar]
- [7].UNAIDS. UNAIDS Data 2018. Geneva: UNIADS; 2018. (Available at: https://www.unaids.org/sites/default/files/media_asset/unaids-data-2018_en.pdf). [Google Scholar]
- [8].Kharsany AB, Karim QA. HIV infection and AIDS in Sub-Saharan Africa: current status, challenges and opportunities. Open AIDS J 2016;10:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].UNAIDS. The Gap Report. Geneva: UNAIDS; 2014. (Available at: https://www.unaids.org/sites/default/files/media_asset/UNAIDS_Gap_report_en.pdf). [Google Scholar]
- [10].Eaton LA, Driffin DD, Bauermeister J, et al. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDs 2015;29:423–9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Auerbach JD, Kinsky S, Brown G, et al. Knowledge, attitudes, and likelihood of pre-exposure prophylaxis (PrEP) use among US women at risk of acquiring HIV. AIDS Patient Care STDs 2015;29:102–10.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Eaton LA, Matthews DD, Driffin DD, et al. A multi-US city assessment of awareness and uptake of pre-exposure prophylaxis (PrEP) for HIV prevention among Black men and transgender women who have sex with men. Prevent Sci 2017;18:505–16.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].National Department of Health Guidelines for expanding combination prevention and treatment options for sex workers: Oral pre-exposure prophylaxis (PrEP) and test and treat (T&T). Final Draft 2016;11:2016. [Google Scholar]
- [14].National Department of Health. PrEP Implementation Pack: South Africa 2016-2017. Pretoria, South Africa: National Department of Health; 2017. (https://www.prepwatch.org/wp-content/uploads/2017/07/SA_ImplementationPack.pdf) [Google Scholar]
- [15].Jewkes R, Sikweyiya Y, Morrell R, et al. The relationship between intimate partner violence, rape and HIV amongst South African men: a cross-sectional study. PloS One 2011;6:1–6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hatcher AM, Colvin CJ, Ndlovu N, et al. Intimate partner violence among rural South African men: alcohol use, sexual decision-making, and partner communication. Cult Health Sexuality 2014;16:1023–39.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cohen C, Moyes J, Tempia S, et al. Severe influenza-associated respiratory infection in high HIV prevalence setting, South Africa, 2009-2011. Emerg Infect Dis 2013;19:1766–74.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Sage, Saks M, Allsop J. Researching health: qualitative, quantitative and mixed methods:. 2012. [Google Scholar]
- [19].Ajayi AI, Nwokocha EE, Akpan W, et al. “It's Sweet Without Condom”: Understanding Risky Sexual Behaviour Among Nigerian Female University Students. Online J Health Allied Scs 2017;16:9. [Google Scholar]
- [20].Wheelock A, Eisingerich AB, Gomez GB, et al. Views of policymakers, healthcare workers and NGOs on HIV pre-exposure prophylaxis (PrEP): a multinational qualitative study. BMJ Open 2012;2:1–1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Restar AJ, Tocco JU, Mantell JE, et al. Perspectives on HIV pre-and post-exposure prophylaxes (PrEP and PEP) among female and male sex workers in Mombasa, Kenya: implications for integrating biomedical prevention into sexual health services. AIDS Educat Prevent 2017;29:141–53.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ajayi AI, Ismail KO, Adeniyi OV, et al. Awareness and use of pre-exposure and postexposure prophylaxes among Nigerian university students: findings from a cross-sectional survey. Medicine 2018;97:1–6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Eakle R, Bourne A, Mbogua J, et al. Exploring acceptability of oral PrEP prior to implementation among female sex workers in South Africa. J Int AIDS Soc 2018;21:1–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ramphele LPW. “Doing” gender in South Africa: footprints of tension for transgender persons [Full Dissertation]. Pretoria: University of South Africa; 2016. [Google Scholar]
- [25].Mayer KH, Hosek S, Cohen S, et al. Antiretroviral pre-exposure prophylaxis implementation in the United States: a work in progress. J Int AIDS Soc 2015;18:1–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Rice E, Barman-Adhikari A, Milburn NG, et al. Position-specific HIV risk in a large network of homeless youths. Am J Public Health 2012;102:141–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Hoagland B, De Boni RB, Moreira RI, et al. Awareness and willingness to use pre-exposure prophylaxis (PrEP) among men who have sex with men and transgender women in Brazil. AIDS Behav 2017;21:1278–87.. [DOI] [PubMed] [Google Scholar]
- [28].Young I, Li J, McDaid L. Awareness and willingness to use HIV pre-exposure prophylaxis amongst gay and bisexual men in Scotland: implications for biomedical HIV prevention. PloS One 2013;8:1–7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Ajayi AI, Abioye AO, Adeniyi OV, et al. Concerns about contracting HIV, knowing partners’ HIV sero-status and discussion of HIV/STI with sexual partners as determinants of uptake of HIV testing. J Biosoc Sci 2018;51:549–61.. [DOI] [PubMed] [Google Scholar]
- [30].Haidar A, Ranjit N, Archer N, et al. Parental and peer social support is associated with healthier physical activity behaviors in adolescents: a cross-sectional analysis of Texas School Physical Activity and Nutrition (TX SPAN) data. BCM Public Health 2019;19:1–9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Chakrapani V, Newman PA, Shunmugam M, et al. Acceptability of HIV pre-exposure prophylaxis (PrEP) and implementation challenges among men who have sex with men in India: a qualitative investigation. AIDS Patient Care STDs 2015;29:569–77.. [DOI] [PubMed] [Google Scholar]


