Abstract
Elabela is a bioactive peptide and a part of Apelinergic system. Elabela has an important role in the early embryonic stages. Elabela's beneficial effects in cardiovascular system were shown in some animal models or in vitro studies. Lately, some investigational studies in humans are started to be seen in literature. Our aims were to investigate serum Elabela levels in the first day of ST segment elevation myocardial infarction (STEMI), to compare with healthy controls, and to see if there is a correlation between other cardiac biomarkers in humans.
The study was planned as cross-sectional. The patients group had 124 STEMI subjects. They were grouped as inferior (n = 59) and anterior myocardial infarction (n = 65) groups, and compared with the healthy control population (n = 77). Routine blood tests and serum Elabela levels were measured. Transthoracic echocardiography performed to all subjects.
Frequency of diabetes mellitus, hypertension, smoking, and hyperlipidemia in both STEMI groups were significantly higher than control subjects. Glucose, high density lipoprotein (HDL) cholesterol, triglyceride, high sensitive C reactive protein (Hs-CRP), troponin I, N-terminal brain natriuretic peptide (NT-ProBNP), and Elabela levels were significantly higher in both STEMI groups. Other laboratory parameters were similar. Group 2 and 3 had significantly lower left ventricular ejection fraction (LVEF) than group 1. Group 3 had also significantly lower LVEF than group 2. There was a positive but moderate correlation between Elabela, troponin I, and NT-ProBNP. Elabela was negatively correlated with LVEF. This correlation was also moderate.
We showed increased Elabela levels in STEMI patients in this study. Also, we observed a moderate positive correlation between troponin I, NT-ProBNP, and Elabela.
Keywords: Coronary artery disease, elabela, myocardial infarction
1. Introduction
There are many bioactive peptides in human cardiovascular system. Some of these peptides have very protective effects; some have opposite kind of effects. Among those, a peptide family named Apelinergic system was found in late 1990s which consisted of 3 parts: Apelin, Elabela, and APJ receptor. Tatemoto et al[1] found the Apelin which is a ligand for APJ receptor in the 1998. It was reported that the Apelin and its receptor had some substantial roles in the modulation of cardiovascular system.[2] According to papers; Apelin and its receptor system have some favorable effects in the atherosclerosis, myocardial infarction (MI), heart failure, and pulmonary artery hypertension.[3–5]
Recently, a new peptide called Elabela/Apela/Toddler was discovered. It has some isoforms called Elabela −32, Elabela Pyr-32, Elabela −21, Elabela −11, and it binds to the APJ receptor.[6,7] It has some functions similar to Apelin. Both of them play an important role in the early embryonic stages and they promote angiogenesis. The lack of Elabela can lead to cardiac deformations.[8] Elabela augments the myocardial contractility and coronary vasodilatation. These effects are more powerful than Apelin. It was reported that infusion of Elabela could dramatically suppress negative effects of pressure overload.[9] Moreover, Elabela has antagonistic effects over Renin-Angiotensin-Aldosterone system. It can reduce blood pressure.[10] Another beneficial effect of Elabela is that it can decrease cardiac dysfunction in MI and it is upregulated during post MI remodeling phase.[2,11]
There are many research studies about the Apelin's role in human body in the literature. But, nearly all of the above studies regarding Elabela were conducted in animal models or in vitro. Lately, some investigational studies in humans are started to be seen in literature.[12,13] In a recent report, Li et al[14] have proposed the Elabela as a new possible therapeutic agent for cardiovascular diseases. To the best of our knowledge, there are no studies about the role of Elabela in human cardiovascular diseases and its potential for treatment. Myocardial infarctions are important kinds of the coronary artery disease spectrum.
Our aims were to investigate serum Elabela levels in the first day of ST segment elevation myocardial infarction (STEMI), to compare with healthy controls, and to see if there is a correlation between other cardiac biomarkers in humans.
2. Methods
2.1. Study population
The study was planned as cross sectional. Local Ethics Committee of Çukurova University was approved the study. All subjects signed written informed consents of the study. A total of 124 STEMI patients were included. The patients were grouped as inferior and anterior MI groups and compared with the healthy control population. Control subjects were selected randomly from healthy individuals who admitted to our polyclinic unit. None of the control subjects had any cardiovascular and valvular diseases. Patients with known critical coronary artery disease, chronic total occlusions, moderate-severe valvular disease, chronic liver, and kidney disease (GFR <60 mL/kg/min) were not included in our study. All patients had their first MI and they were admitted within 90 minutes after chest pain. Definition of STEMI was based on the fourth universal definition of MI.[15] Successful primary percutaneous coronary intervention was performed to all enrolled patients. Medical treatments of the patients were applied according to the guidelines. There was no cardiogenic shock patient. All patients and controls were questioned about demographic variables.
2.2. Laboratory parameters
Glucose, high-sensitive troponin I, creatinine kinase myocardial band (CK-MB), N terminal pro-brain natriuretic peptide (NT-ProBNP), renal functions, lipid parameters, high-sensitive C reactive protein (Hs-CRP), and complete blood count were analyzed and recorded from routine blood tests.
Serum Elabela levels were determined using commercial kits (Sunred Biological Technology, Shanghai, China). Elabela −32 isoform was measured. The kit used a double-antibody sandwich enzyme-linked immunosorbent assay (ELISA) to assay the level of Elabela in samples. According to the manufacturer; this assay has inter-assay coefficients of variation <12% and intra-assay coefficients of variation of <10%. All of the above tests were performed from blood samples which were taken at the 24th hour of hospital admission.
2.3. Echocardiographic evaluation
Doppler and two-dimensional echocardiographic evaluations were performed using an echocardiography device (EPIQ 7; Philips Healthcare, Andover, MA). Left atrial and left ventricular (LV) diameters and LV wall thicknesses were measured at end-diastole. The standards of the American Society of Echocardiography were used for all measurements.[16] Biplane Simpson's method was used for the calculation of LV ejection fraction (LVEF).[17]
2.4. Statistical analysis
The variables were separated as categorical and continuous groups. Categorical variables were shown as numbers and percentages and analyzed using the chi-square test. Continuous variables were demonstrated as mean ± standard deviation and their distributions were analyzed by the Kolmogorov-Smirnov test. Differences in continuous variables were evaluated using one-way analysis of variance (ANOVA) with the appropriate post-hoc test (Tukey or Tamhane). The variables without normal distributions were analyzed by the Mann–Whitney U test. Spearman correlation analyze was performed between cardiac biomarkers and Elabela. SPSS 22.0 (SPSS Inc. Chicago, IL) software was used for the statistical analyses. A P value <.05 was considered as significant.
3. Results
Our study had 3 groups: 77 healthy subjects (group 1), 59 inferior STEMI (group 2), and 65 anterior STEMI (group 3) patients.
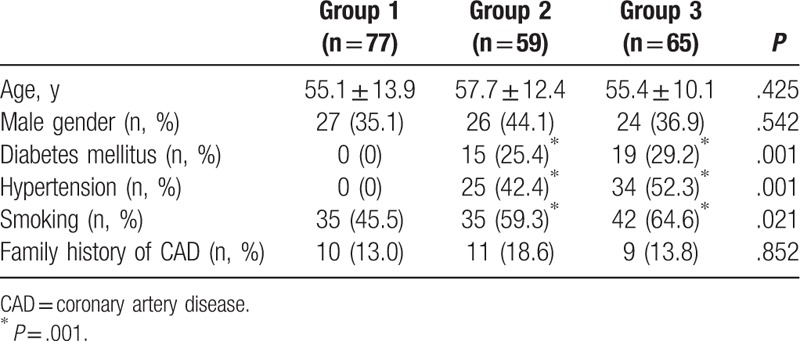
In the demographic comparison, mean age and sex distributions were similar. Frequency of diabetes mellitus, hypertension, smoking, and hyperlipidemia in both STEMI groups were significantly higher than control subjects. Family history of coronary artery disease frequency was similar between 3 groups (Table 1).
Table 1.
Comparison of demographic findings.
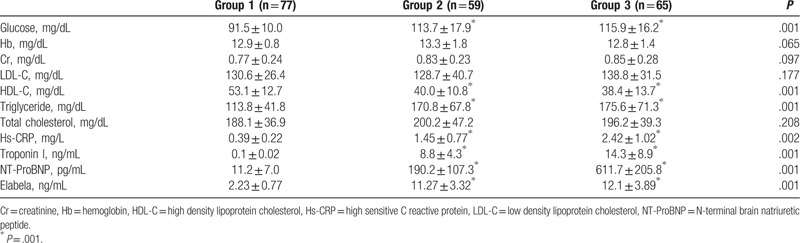
Glucose, HDL cholesterol, triglyceride, Hs-CRP, troponin I, NT-ProBNP, and Elabela levels were significantly higher in both STEMI groups (Fig. 1). Other laboratory parameters were similar (Table 2).
Figure 1.
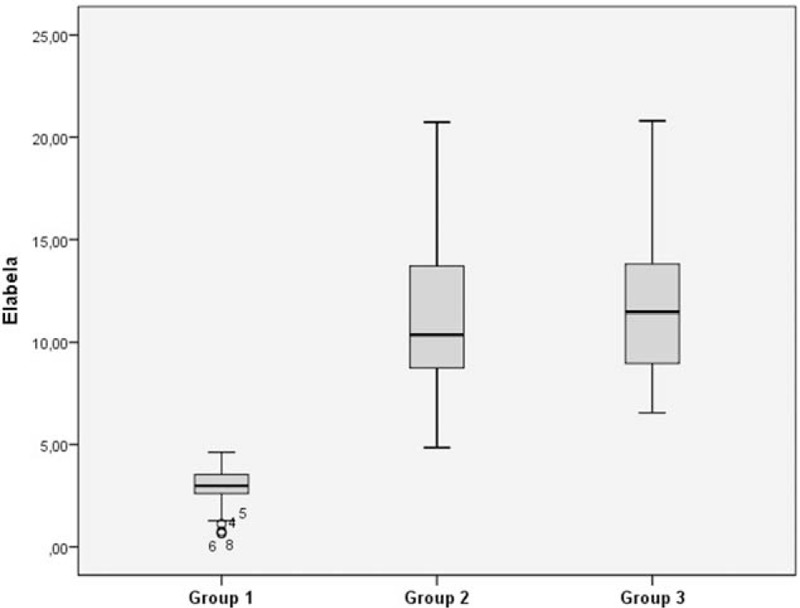
Elabela values of the groups were shown in the box plot graphics.
Table 2.
Comparison of laboratory parameters.
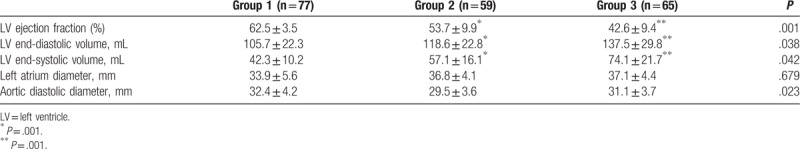
Group 2 and 3 had significantly lower LVEF than group 1. Group 3 had also significantly lower LVEF than group 2. Left ventricular end-systolic and diastolic volumes were significantly increased in group 3 (Table 3).
Table 3.
Comparison of echocardiography findings.
There was a positive but moderate correlation between Elabela, troponin I, and NT-ProBNP. Elabela was negatively correlated with LVEF. This correlation was also moderate (Table 4).
Table 4.
Correlations between Elabela, troponin I, NT-ProBNP, and left ventricular ejection fraction.

4. Discussion
The main finding of our study was that this was the first investigation which showed increased Elabela levels in STEMI patients. Also, we detected that Elabela levels were higher in anterior STEMI patients, but there was no statistical significance. There was a moderate correlation between Elabela and cardiac biomarkers.
Myocardial infarction is one of the worst clinical scenarios in medicine. It is responsible for a significant portion of the mortality and morbidity in developed countries. Myocardial infarction might be accepted as a key part of the burden of cardiovascular disease.[18] Researchers have been conducting studies regarding etiology, pathophysiology, related risk factors, and treatment options of MI for many years. Bioactive peptides or biomarkers have gained an important place in the development, diagnosis, and follow-up of the atherosclerotic disease spectrum for the last 3 decades. They have been started to be used early diagnosis, risk detection, and monitoring of diseases.[19]
Apelin and Elabela are ligands of the APJ receptor. The coupling of this receptor and its ligands play some regulator roles in the cardiovascular system, central nervous system, circulatory system, and many other systems. Apelin is widely distributed in human body. Unlike Apelin, Elabela has a limited distribution. Both of these peptides have different isoforms. The regulatory effects of these isoforms vary in the target system. But, in general, Apelin and Elabela have been known for theirs protective effects over cardiovascular system.[8,20]
Elabela is found in plasma. Its expression is highest in the embryonic heart tissue, and after that declined gradually. Elabela is mainly detected in the fibroblasts and endothelial cells in the heart. It is essential for normal development of the heart tissue.[21] Currently, the information regarding role of Elabela in MI is based on animal models. Perjés et al[2] demonstrated that there was a substantial increase in Elabela expression (6.6 ± 2.3 fold increase in MI group vs sham, P < .05) and APJ receptor (1.8 ± 0.3 fold increase in MI group vs sham, P < .05) in rat left ventricle samples. They also observed a high correlation between Elabela and APJ receptor expression (R2 = 0.94; P < .001). Elabela had dose-dependent positive inotropic effects and it was reported as one of the most inotropic agents known to date. Another important finding of the authors was, increased Elabela and APJ receptor expression was related to a better preservation of LV systolic function. They have interpreted their results that Elabela might have a potential beneficial effect in heart failure patients. Our results showed that Elabela levels were significantly increased in both anterior and inferior STEMI patients. Elabela levels were mildly higher in group 3 than group 2, but there was no statistical significance. This might be explained by the amount of damaged myocardial tissue is relatively higher in the group 3 patients. Left ventricular ejection fraction was significantly lower in group 2 and 3. Group 3 had lowest ejection fraction levels. Maybe it would not be appropriate to compare directly, but our results seemed compatible with Perjés et al.[2] Both study showed that there was in increase in Elabela levels in infarcted myocardium. We observed a moderate positive correlation between troponin I, NT-ProBNP, and Elabela. Ejection fraction and Elabela were negatively correlated. There was no correlation between Elabela and Hs-CRP.
In another rat study, Rakhshan et al[22] documented that Elabela had cardio protective effects. Myocardial infarction was induced and Elabela was administered intraperitoneally to rats 5 μg/kg for 4 days. They showed that CK-MB, troponin I levels, oxidative stress markers, and infarct size were significantly decreased in the Elabela treatment group. Besides, Elabela treatment significantly inhibited decrease of LVEF, fractional shortening. The authors demonstrated that Elabela might have a potential as a therapeutic agent in the cardiovascular diseases.
The evidences regarding Elabela's cardiovascular protective effects are rare for now. But according to in vitro and animal model studies, Elabela or another synthetic derivative like Elabela might have a therapeutic or biomarker potential. Overall, Elabela's positive effects in heart failure, MI, pulmonary artery hypertension, Renin-Angiotensin-Aldosterone system, and diabetes should be evaluated carefully.[8]
Cross-sectional design and subject size are the main limitations of our study. We only measured the Elabela level at the 24th hour of STEMI. Consecutive measurements would be more valuable to determine the course of Elabela in STEMI. Besides, Apelin and APJ measurements would have provide more details regarding Apelinergic system in STEMI patients.
5. Conclusion
We showed increased Elabela levels in STEMI patients in this study. Also, we observed a moderate positive correlation between troponin I, NT-ProBNP, and Elabela. Larger and more detailed studies are needed to evaluate Elabela's role as a cardiac biomarker or as a therapeutic agent in humans.
Author contributions
Conceptualization: Yurdaer Dönmez.
Investigation: Yurdaer Dönmez, Armağan Acele.
Methodology: Yurdaer Dönmez, Armağan Acele.
Project administration: Yurdaer Dönmez.
Supervision: Yurdaer Dönmez.
Writing – original draft: Yurdaer Dönmez.
Writing – review & editing: Armağan Acele.
Footnotes
Abbreviations: ANOVA = analysis of variance, CK-MB = creatinine kinase myocardial band, ELISA = enzyme-linked immunosorbent assay, GFR = glomerular filtration rate, Hs-CRP = high-sensitive C reactive protein, LV = left ventricle, LVEF = left ventricular ejection fraction, MI = myocardial infarction, NT-ProBNP = N terminal pro-brain natriuretic peptide, STEMI = ST segment elevation myocardial infarction.
How to cite this article: Dönmez Y, Acele A. Increased elabela levels in the acute ST segment elevation myocardial infarction patients. Medicine. 2019;98:43(e17645).
The authors have no conflicts of interest to disclose.
References
- [1].Tatemoto K, Hosoya M, Habata Y, et al. Isolation and characterization of a novel endogenous peptide ligand for the human APJ receptor. Biochem Biophys Res Commun 1998;251:471–6.. [DOI] [PubMed] [Google Scholar]
- [2].Perjés Á, Kilpiö T, Ulvila J, et al. Characterization of apela, a novel endogenous ligand of apelin receptor, in the adult heart. Basic Res Cardiol 2016;111:2. [DOI] [PubMed] [Google Scholar]
- [3].Simpkin JC, Yellon DM, Davidson SM, et al. Apelin-13 and apelin-36 exhibit direct cardioprotective activity against ischemia-reperfusion injury. Basic Res Cardiol 2007;102:518–28.. [DOI] [PubMed] [Google Scholar]
- [4].Dai T, Ramirez-Correa G, Gao WD. Apelin increases contractility in failing cardiac muscle. Eur J Pharmacol 2006;553:222–8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Falcão-Pires I, Gonçalves N, Henriques-Coelho T, et al. Apelin decreases myocardial injury and improves right ventricular function in monocrotaline-induced pulmonary hypertension. Am J Physiol Heart Circ Physiol 2009;296:H2007–14.. [DOI] [PubMed] [Google Scholar]
- [6].Chng SC, Ho L, Tian J, et al. ELABELA: a hormone essential for heart development signals via the apelin receptor. Dev Cell 2013;27:672–80.. [DOI] [PubMed] [Google Scholar]
- [7].Pauli A, Norris ML, Valen E, et al. Toddler: an embryonic signal that promotes cell movement via Apelin receptors. Science 2014;343:1248636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zhang Y, Wang Y, Lou Y, et al. Elabela, a newly discovered APJ ligand: similarities and differences with Apelin. Peptides 2018;109:23–32.. [DOI] [PubMed] [Google Scholar]
- [9].Sato T, Sato C, Kadowaki A, et al. ELABELA-APJ axis protects from pressure overload heart failure and angiotensin II-induced cardiac damage. Cardiovasc Res 2017;113:760–9.. [DOI] [PubMed] [Google Scholar]
- [10].Murza A, Sainsily X, Coquerel D, et al. Discovery and structure-activity relationship of a bioactive fragment of ELABELA that modulates vascular and cardiac functions. J Med Chem 2016;59:2962–72.. [DOI] [PubMed] [Google Scholar]
- [11].Wang W, McKinnie SM, Patel VB, et al. Loss of Apelin exacerbates myocardial infarction adverse remodeling and ischemiareperfusion injury: therapeutic potential of synthetic Apelin analogues. J Am Heart Assoc 2013;2:e000249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Zhou L, Sun H, Cheng R, et al. ELABELA, as a potential diagnostic biomarker of pre-eclampsia, regulates abnormally shallow placentation via APJ. Am J Physiol Endocrinol Metab 2019;316:E773–81.. [DOI] [PubMed] [Google Scholar]
- [13].Zhang H, Gong D, Ni L, et al. Serum Elabela/Toddler levels are associated with albuminuria in patients with type 2 diabetes. Cell Physiol Biochem 2018;48:1347–54.. [DOI] [PubMed] [Google Scholar]
- [14].Li L, Zhou Q, Li X, et al. Elabela-APJ axis: a novel therapy target for cardiovascular diseases. Acta Biochim Biophys Sin (Shanghai) 2017;49:1042–3.. [DOI] [PubMed] [Google Scholar]
- [15].Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019;40:237–69.. [DOI] [PubMed] [Google Scholar]
- [16].Lang RM, Bierig M, Devereux RB, et al. Chamber Quantification Writing Group. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and The Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 2005;18:1440–63.. [DOI] [PubMed] [Google Scholar]
- [17].Schiller NB, Shah PM, Crawford M, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989;2:358–67.. [DOI] [PubMed] [Google Scholar]
- [18].Johansson S, Rosengren A, Young K, et al. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord 2017;17:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Watanabe T, Sato K, Itoh F, et al. Endogenous bioactive peptides as potential biomarkers for atherosclerotic coronary heart disease. Sensors (Basel) 2012;12:4974–85.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Shin K, Kenward C, Rainey JK. Apelinergic system structure and function. Compr Physiol 2017;8:407–50.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Xu J, Chen L, Jiang Z, et al. Biological functions of Elabela, a novel endogenous ligand of APJ receptor. J Cell Physiol 2018;233:6472–82.. [DOI] [PubMed] [Google Scholar]
- [22].Rakhshan K, Azizi Y, Naderi N, et al. ELABELA (ELA) peptide exerts cardioprotection against myocardial infarction by targeting oxidative stress and the improvement of heart function. Int J Pept Res Ther 2018;25:613–21.. [Google Scholar]


