Abstract
Objective
To evaluate the tolerability of, adherence to and efficacy of a community walking training programme with simultaneous cognitive demand (dual-task) compared to a control walking training programme without cognitive distraction.
Methods
Adult stroke survivors, at least 6 months after stroke with a visibly obvious gait abnormality or reduced two-minute walk distance were included into a 2-arm parallel randomized controlled trial of complex intervention with blinded assessments. Participants received a 10 week, bi-weekly, 30 minutes treadmill program at an aerobic training intensity (55-85% heart rate maximum), either with, or without simultaneous cognitive demands. Outcome measured at 0, 11 and 22 weeks. Primary: two-minute-walk tests with and without cognitive distraction, dual task effect on walking and cognition; secondary: SF-36, EuroQol-5D-5L, Physical Activity Scale for Elderly (PASE), and step activity.
Results
Fifty stroke patients were included, 43 received allocated training and 45 completed all assessments. The experimental group (n = 26) increased mean (SD) two-minute walking distance from 90.7 (8.2) to 103.5 (8.2) metres, compared with 86.7 (8.5) to 92.8 (8.6) in the control group, and their PASE score from 74.3 (9.1) to 89.9 (9.4), compared with 94.7 (9.4) to 77.3 (9.9) in the control group. Statistically, only the change in the PASE differed between the groups (p = 0.029), with the dual-task group improving more. There were no differences in other measures.
Conclusions
Walking with specific additional cognitive distraction (dual-task training) might increase activity more over 12 weeks, but the data are not conclusive.
Clinical Trial Registration
http://www.isrctn.com/ISRCTN50586966 Unique identifier: ISRCTN50586966
Keywords: Stroke, rehabilitation, walking, dual task, community, aerobic exercise
Subject terms: Cerebrovascular Disease/Stroke, rehabilitation, exercise
Introduction
Improvements in community walking ability and engagement in meaningful activities are important goals for stroke survivors during rehabilitation 1, 2. In one survey, 93% of 130 stroke survivors indicated that walking in the community was essential (41%), very important (34%) or important (18%) for their life quality 3. However, achieving independent walking does not necessarily mean that a stroke survivor can walk independently in the community 4.
Walking safely in the community requires sufficient cognitive skill to deal with distraction such as advertisements, noise and busy streets with uneven paths and other interferences 4. Being able to walk safely with other simultaneous cognitive demands, such as considering what to buy, is also important 5. Dual task ability is often reduced after stroke and the effects of dual task interference on gait and cognition are greater after stroke compared to in healthy older adults 5. One randomised trial found benefit from simultaneously training cognitive tasks during walking exercise 6. The research to date has only included small numbers of stroke survivors, short intervention periods (2-6 weeks) and no control group or unmatched control interventions 6–9. This was again concluded recently by Plummer and Iyigü 10. The evidence suggests that this combined training may improve community mobility.
This study set out to explore feasibility and effect sizes of 10 weeks of treadmill training with a concurrent cognitive demand (with content relating to daily life situations) in comparison to 10 weeks of treadmill training alone. We hypothesized that training cognitive demand during walking would improve community walking levels, dual task ability and confidence about community walking.
Methods
The study was approved by the local NHS Research Ethics Committee (REC reference: 12/SC/0403), was registered at isrctn.nl (ISRCTN50586966) and all participants gave informed consent according to the recommendations for physicians involved in research on human participants adopted by the 18th World Medical Assembly, Helsinki 1964 and later revisions.
Stroke survivors were recruited from hospitals, GP practices, stroke clubs and via advertisements in local newsletters and magazines in Oxfordshire, UK. Eligibility criteria were: 18 years or older, at least 6 months after any type of stroke, reduced two-minute-walk distance compared to reference data (Bohannon et al. 11, 12) or a visibly abnormal gait, able to walk on a treadmill, no concurrent neurological conditions or psychological disorder, and no contra-indication to safe participation in exercise.
The design was a single blinded two-arm parallel randomized controlled trial of a complex intervention with two equal training groups. The number of patients recruited was based on the number needed for the cerebral imaging aspect of this project, to be reported later. Previous work 13 has shown that stroke survivors who are only able to walk inside their household (i.e. very limited community walking ability), walk at speeds lower than 0.4ms-1. Therefore, to balance training groups for walking performance the randomization process was stratified through minimisation for baseline treadmill speeds slower or faster than 0.4ms-1. The recruiting researcher contacted the principal investigator, giving the gait speed. The principal investigator used a bespoke randomisation programme to allocate the group and informed the recruiting researcher of the patient’s allocation into either a treadmill training with simultaneous cognitive demand, so called dual task treadmill training, or a control treadmill training group.
Interventions
In both groups, each participant was trained individually by health or fitness professionals in community leisure facilities in a quiet room for 20 sessions divided over 10 weeks. The walking component of training consisted of: 10 minutes warm-up, 5 minutes cool down and in between 30 minutes of walking at an intensity which required the body to work in the aerobic training zone, between 55% and 85% of the age predicted maximum heart rate (220 – age) 14. Blood pressure was measured in advance and directly after each training session to make sure it was within safe limits (systolic ≤ 170, diastolic ≤ 100). Heart rate was assessed throughout training sessions to ensure training remained in the aerobic training zone. The aim of training was to increase self-selected walking speed and training intensity over the course of 10 weeks. If participants were not able to walk safely for the full 45 minutes, the session was shortened. If for logistical reasons, the full amount of 20 sessions could not be completed, effort was made to achieve as many sessions as possible and on some occasions the training period was extended by 2 or 3 weeks.
Participants in the dual task treadmill training group were distracted whilst treadmill walking using three types of distraction: cognitive tasks, a listening task or talking about planning daily activities. Ten minutes of training time were devoted for each type of distraction (Table 1). Participants who received CT-TT were trained to walk with a focus on walking and with as little distraction as possible.
Table 1. Overview of tasks used in dual task training.
| Task | Description | Duration |
|---|---|---|
| Cognitive Task Block | 2 * 5min | |
| Auditory Stroop | A randomized series of the word “High” and “Low” are played through speakers at a high or low pitch. The subject must state the pitch of the word that was just said. | 2min30sec |
| Serial Subtraction | The person is asked to count backwards from a number between 290 and 300 in steps of 3, 4 or 7. | 2min30sec |
| Clock Face Task | A time is given verbally and the person must state whether the corresponding clock face has hands on the left, right or both sides of the clock. | 2min30sec |
| Letter Fluency | A letter of the alphabet is given and the person is asked to name as many words as they can think of that start with that letter. | 2min30sec |
| Alternative uses | The person is given an object and has to come up with alternative uses for that object. | 2min30sec |
| Creativity | The purpose of the task is to name as many objects that have a certain attribute (e.g. objects that are tall). | 2min30sec |
| Radio | 10min | |
| Listening task | An audio fragment is played which is then used as topic of conversation between the trainer and trainee. | 10min |
| Planning | 2 * 5min | |
| Planning of activities of daily living | The person is asked to describe how they plan their daily activities; from short actions such as making a cup of tea, to longer actions such as planning an upcoming day out or holiday. | 5min |
Measures
Assessments were conducted at 0 weeks (baseline), 11 weeks (after 10 week training period) and 22 weeks (follow-up). Data were collected by researchers who were unaware of the participant’s training group allocation. For primary measures, during each assessment, participants completed a two-minute-walk test 15 twice, once under normal conditions and the other in which the subject was distracted during the walk with questions related to daily life activities (e.g. can you tell me how your day started?). The order of walking tests was alternated between participants and visits to prevent differences in walking distance due to exhaustion from the first to the second walk.
Secondary measures included: cognition measured with the Montreal Cognitive Assessment 16 (MoCA), functional ability measured with the Barthel ADL Index 17, dual task effect on walking and cognition (i.e. performance on cognitive task when walking, and on walking when doing a cognitive task as compared with doing task alone), step activity for a week measured with a StepWatch Activity Monitor™ (OrthoCare Innovations, Seattle, WA) and the Physical Activity Scale for Elderly (PASE) 18. Health and Wellbeing were measured with the Short-Form-36 19 and the EuroQol-5D 20.
In addition, two community walking questions were asked: “Do you get out of the house as much as you like?” and “Do you feel confident when walking in the community?”. For both questions participants were asked to answer “yes” or “no”.
Demographic measures included: any available or obtainable descriptive about the stroke (type, location, date of stroke), and the Edinburgh handedness questionnaire 21.
Statistical analyses
Statistics were performed in SPSS version 21. Normality of data was checked using the Shapiro-Wilk test. Independent t-tests were performed to test for significant differences in descriptive data and clinical characteristics between groups at baseline. In case of non-normal distributed data, Mann-Whitney U Test, Chi-square or Fishers exact test were used. A Linear Mixed Models approach was used 22 with fixed factors for time and training group to explore changes over time and between groups. An interaction term for group*time was only added to the model if this interaction was significant. Generalized linear models were used to explore effects of group and time on binary data. To explore changes in measures in the dual-task treadmill training group compared to the control, treadmill training only group from study start to study end, Cohen’s d effect sizes with 95% confidence intervals were calculated for change from baseline to follow-up.
Results
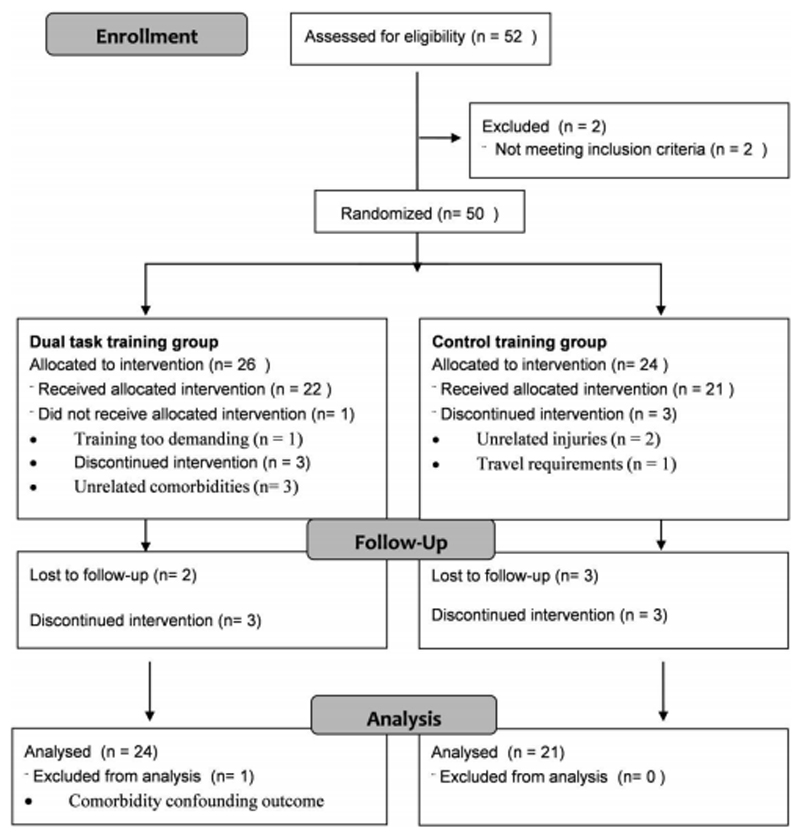
Participants were recruited between March 2013 and August 2014. Final data were collected in January 2015. Fifty patients were recruited, and Figure 1 shows the flow of patients. We could not record the number of people screened due to various routes we used: GP surgeries, stroke units and stroke group meetings or newsletters. Apart from a larger mean time since stroke onset for the dual-task treadmill training group (p = 0.018), no other significant differences between groups were found for any variables at baseline (table 2). Discontinuation of training occurred in both groups and reasons are specified in figure 1. Two participants who discontinued with the dual-task treadmill training did complete final assessments but not week 11 and week 22 assessments. One person was excluded from analysis as it was discovered that he/she had depression sufficiently severe to confound the follow-up measures. The depression was judged to be unrelated to trial participation. No other adverse events occurred during this study.
Figure 1. Flow diagram.
Table 2. Descriptive data containing population mean and standard deviation values.
| Measure | DT-TT Group (n = 26) |
CT-TT Group (n = 24) |
Group comparison (p-value) |
|---|---|---|---|
| Demography | |||
| Male / female | 15 / 11 | 11 / 13 | 0.402C |
| Age (years) | 60.85 ± 14.86 | 62.25 ± 15.53 | 0.745T |
| Handedness: | |||
| right / left / no preference | 20 / 3 / 3 | 21 / 3 | 0.382F |
| Stroke details | |||
| Ischemic / Haemorrhagic / both | 18 / 7 / 1 | 13 / 10 / 1 | 0.678C |
| Right / Left / mid – brain | 13 / 11 / 2 | 13 / 6 / 5 | 0.261F |
| Time since stroke onset (months) | 60.19 ± 62.15 | 25.71 ± 32.70 | 0.018M, * |
| Clinical characteristics | |||
| Barthel Index | 18.9 ± 2.3 | 19.2 ± 1.2 | 0.489T |
| MOCA | 24.5 ± 4.8 | 25.3 ± 3.5 | 0.535T |
| (mild) aphasia: yes / no | 4 / 22 | 2 / 22 | 0.270F |
| Walking characteristics | |||
| Walking aid: | |||
| none / stick / personal support | 13 / 11 / 2 | 7 / 15 / 2 | 0.291F |
| TMW | 90.66 ± 36.11 | 86.73 ± 41.96 | 0.729T |
| TMW_DT | 78.50 ± 32.60 | 75.44 ± 33.21 | 0.749T |
| Treadmill walking speed (ms-1) | 0.43 ± 0.24 | 0.40 ± 0.23 | 0.721T |
MOCA; Montreal Cognitive Assessment Scale, TMW; two-minute walk test, TMW-DT; two-minute walk test with distraction.
Independent Sample T-test
Mann-Whitney Test
Chi-square Test
Fischer’s Exact Test
Significant difference between training groups, P < 0.05
Linear Mixed Model results between assessments and between groups
Results of the model for all outcome measures at each assessment point are summarized and presented in table 3 together with generalized mixed model results for confidence to walk in the community and Cohen’s d effect sizes. Over time, both groups showed significant increases in walking distances for both two-minute walking alone and two-minute walking with dual task p < 0.001), cognitive response during dual-task walking (p = 0.007), SF-36 total score (p = 0.002), and EQ-5D index (p = 0.026). When asked about confidence during community walking, confidence increased in both groups (p = 0.008), with a significant group*time interaction with larger numbers of participants gaining confidence in the control group over time (p = 0.027). Physical activity as measured with the PASE questionnaire showed no significant differences between groups or changes over time (p > 0.05), although a significant interaction for group*time (p = 0.029) was found, with greater increases in physical activity over time found in the dual-task treadmill training group. Dual task effect on walking distance during two-minute walking with dual task and mean step activity did not significantly change over all three time points or between groups. In addition, no significant differences between groups and over time were seen in answers to the question: “Do you get out of the house as much as you like?”.
Table 3. Linear mixed model results for primary and secondary measures.
| Outcome measure | Visit | DT-TT Group | CT-TT Group | Linear Mixed Model | Cohen’s d: effect size for change from baseline to follow up [95% CI for Cohen’s d] | |
|---|---|---|---|---|---|---|
| Model means (SEM) | Model means (SEM) | Effect | F-value (p-value) | |||
|
Walking Two minute walk distance (m) |
Week 0 | 90.66 (8.20) | 86.74 (8.54) | Group | 0.362 (0.550) | Medium effect size for DT-TT |
| Week 11 | 99.68 (8.21) | 93.17 (8.58) | Time | 11.132 (<0.001)** | ||
| Week 22 | 103.47 (8.24) | 92.75 (8.62) |
0.50 [-0.11 – 1.10] |
|||
|
Dual Task Walking Two minute walk with dual task distance (m) |
Week 0 | 78.50 (7.03) | 75.44 (7.33) | Group | 0.191 (0.665) | Small effect size for DT-TT |
| Week 11 | 84.26 (7.04) | 79.72 (7.35) | Time | 9.196 (<0.001)** | ||
| Week 22 | 88.82 (7.06) | 82.97 (7.40) | 0.20 [-0.41 – 0.80] |
|||
|
Dual Task Effect Walking distance change during TMW-DT |
Week 0 | -13.40% (1.90) | -10.80% (1.90) | Group | 1.809 (0.186) | No significant effect size for CT-TT |
| Week 11 | -15.80% (1.90) | -13.70% (1.90) | Time | 2.809 (0.071)# | ||
| Week 22 | -14.00% (1.90) | -9.10% (2.00) | -0.19 [-0.80 – 0.42] |
|||
|
Dual Task Effect Number of Cognitive responses during TMW-DT |
Week 0 | 11.23 (0.80) | 11.92 (0.83) | Group | 2.084 (0.158) | Small to medium effect size for CT-TT |
| Week 11 | 12.61 (0.82) | 12.37 (0.86) | Time | 5.664 (0.007)* | ||
| Week 22 | 12.20 (0.85) | 13.88 (0.90) | -0.31 [-0.94 – 0.32] |
|||
|
Physical Activity Physical Activity Scale for Elderly |
Week 0 | 74.26 (9.11) | 94.72 (9.36) | Group | 0.019 (0.892) | Medium effect size for DT-TT |
| Week 11 | 86.89 (9.11) | 74.65 (9.79) | Time | 0.237 (0.789) | ||
| Week 22 | 89.95 (9.41) | 77.31 (9.93) | Interact | 3.701 (0.029)* |
0.59 [-0.02 – 1.21] |
|
|
Physical activity Step activity / day by StepWatch Activity Monito™ |
Week 0 | 3469 (390) | 2747 (402) | Group | 1.391 (0.244) | No significant effect size for CT-TT |
| Week 11 | 3411 (390) | 2949 (411) | Time | 1.570 (0.215) | ||
| Week 22 | 3131 (389) | 2619 (424) | -0.19 [-0.84 – 0.46] |
|||
|
Health Wellbeing SF-36 Total Score |
Week 0 | 54.7 (3.4) | 60.9 (3.6) | Group | 1.900 (0.174) | No significant effect size for CT-TT |
| Week 11 | 61.3 (3.5) | 66.7 (3.7) | Time | 6.629 (0.002)* | ||
| Week 22 | 60.3 (3.5) | 67.2 (3.7) | -0.10 [-0.69 – 0.48] |
|||
|
Health Wellbeing EQ-5D Index |
Week 0 | 0.72 (0.04) | 0.71 (0.04) | Group | 0.027 (0.870) | Small effect size for CT-TT |
| Week 11 | 0.76 (0.04) | 0.78 (0.04) | Time | 3.795 (0.026)* | ||
| Week 22 | 0.71 (0.04) | 0.73 (0.04) | -0.20 [-0.79 – 0.39] |
|||
|
Community Walking Do you feel confident when walking in the community? |
Week 0 | No = 10 Yes = 16 |
No = 11 Yes = 12 |
Group | 0.589W (0.443) | N/A |
| Week 11 | No = 7 Yes = 17 |
No = 4 Yes = 17 |
Time | 9.643W(0.008)* | ||
| Week 22 | No = 5 Yes = 19 |
No = 2 Yes = 18 |
Interact | 12.673W(0.027)* | ||
DT-TT: Dual Task Treadmill Training, CT-TT: Control Treadmill Training, SEM: Standard error of the mean, TMW-DT: two minute walk test with distraction, interact: interaction.
Wald Chi Square test value. Significance level for statistical testing.
p < 0.01.
p < 0.05.
0.05 < p < 0.10.
To explore difference in the change from baseline to follow-up between groups, Cohen’s d effect sizes with 95% confidence intervals are added to results in table 3. Positive Cohen d values in the dual-task treadmill training compared to the control training reflect a larger effect and negative Cohen d values reflect vice versa. Two minute walk distance and PASE increased over time in both groups with positive medium effect sizes of 0.50 and 0.59 and a positive small effect size of 0.20 for distance on two-minute walk with dual task. Negative small to medium effect sizes for comparison between groups were seen for increases in cognitive response during dual task walking (d = -0.31) and EQ-5D (d = -0.20). Dual task effect on walking distance during dual task walking, daily step activity and SF-36 total score showed insignificant effect sizes of -0.20 < d < 0.20 (see table 3).
Data collected throughout training showed that mean relative heart rate for both groups were within the target range of 55-85%HRmax with a mean (SD) relative heart rate of 61 ± 1%HRmax for the single-task group and 62 ± 1%HRmax for the dual-task group (t(41) = -0.04, P = 0.97). There were no differences in training parameters between the single-task group and the dual-task group with respect to starting values, end values and change in values (P > 0.05) (see table 4 and 5 of supplemental data).
Discussion
We did not find any consistent, statistically-significant differences in clinical outcome at 22 weeks between patients given simple treadmill-training and those given treadmill training while also undertaking a cognitive task. Both groups improved significantly on walking distances under normal and dual task situations. There were improvements on the SF-36 total and EQ-5D index scores.
The study was under-powered to find clinical differences, being powered for differences in cerebral blood-flow measured using near infra-red spectroscopy. Nonetheless, the results suggest further research would be warranted. Our linear mixed model found a significant interaction between group and time for the physical activity scale, reflecting greater increases in the dual task group. We also noted that change from baseline to follow-up showed a larger improvement in cognitive functioning during the dual-task two-minute walking test. This could suggest that the cognitively trained group focused on walking during dual task, at the expense of cognitive performance. However great care needs to be taken with the interpretation of cognitive performance during dual task measurements in stroke. In recent years, Yang et al. 23 found that the reliability of dual task effect measurement on gait in community-dwelling stroke survivors was moderate to good, but only poor to fair for the cognitive aspect of a dual task.
Surprisingly, confidence during community walking improved relatively more in the control group, with a statistically significant interaction between group and time in favour of the control group. This was unexpected, but is possibly explained by the larger proportion of “no” responders at baseline in the control group. Increases in self-reported community walking were not reflected by data from the StepWatch Activity Monitors™ suggesting that the training intervention did not result in participants actually engaging in more walking and physical activity, but possibly just changing where they walked.
The main limitation of this trial is the small sample size. The difference between groups in time from stroke onset is unlikely to be relevant, because they were all late after stroke. The linear analysis will have controlled for this if it was having an influence. Both training programs were delivered one-on-one to provide highest quality and an individual training approach. In order to include more study participants at the same time, it would be necessary to increase training facilities, training sites and personnel. Cognitive distraction tasks during dual task training worked well, but in-training analyses of cognitive performance could help to tailor specific distraction tasks for individual’s dual task limitations. This was not possible within the resources available to this study.
To keep the assessments within a certain time limit (2-3 hours), this study used limited measures on community walking. In future work an extra tool such as the activities-specific balance confidence scale 24 could be added to measure (un)confidence in balance, risk of falls and community participation.
Considering that dual-task training used limited resources, was easy to deliver and well tolerated with no adverse events, we think a substantive evaluation of dual-task walking training is warranted.
Supplementary Material
Acknowledgements
The research team acknowledges the support of the National Institute for Health Research Clinical Research Network. The research team would like to thank all study participants and all members of the Movement Science Group who supported training and testing of participants.
Sources of Funding
This research was funded through a Stroke Association Grant. Professor Helen Dawes is funded by the Elizabeth Casson Trust. Heidi Johansen-Berg is funded by the Wellcome Trust. Dawes and Johansen-Berg receive support from the NIHR Oxford Biomedical Research Centre.
Footnotes
Disclosures
None
References
- 1.Alguren B, Fridlund B, Cieza A, Sunnerhagen KS, Christensson L. Factors associated with health-related quality of life after stroke: a 1-year prospective cohort study. Neurorehabilitation and neural repair. 2012;26:266–74. doi: 10.1177/1545968311414204. [DOI] [PubMed] [Google Scholar]
- 2.Bohannon RW, Andrews AW, Smith MB. Rehabilitation Goals of Patients with Hemiplegia. Int J Rehabil Res. 1988;11:181–3. [Google Scholar]
- 3.Lord SE, McPherson K, McNaughton HK, Rochester L, Weatherall M. Community ambulation after stroke: how important and obtainable is it and what measures appear predictive? Archives of Physical Medicine and Rehabilitation. 2004;85:234–9. doi: 10.1016/j.apmr.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 4.Donovan K, Lord SE, McNaughton HK, Weatherall M. Mobility beyond the clinic: the effect of environment on gait and its measurement in community-ambulant stroke survivors. Clin Rehabil. 2008;22:556–63. doi: 10.1177/0269215507085378. [DOI] [PubMed] [Google Scholar]
- 5.Al-Yahya E, Dawes H, Smith L, Dennis A, Howells K, Cockburn J. Cognitive motor interference while walking: a systematic review and meta-analysis. Neuroscience and biobehavioral reviews. 2011;35:715–28. doi: 10.1016/j.neubiorev.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Jaffe DL, Brown DA, Pierson-Carey CD, Buckley EL, Lew HL. Stepping over obstacles to improve walking in individuals with poststroke hemiplegia. Journal of rehabilitation research and development. 2004;41:283–92. doi: 10.1682/jrrd.2004.03.0283. [DOI] [PubMed] [Google Scholar]
- 7.Mirelman A, Bonato P, Deutsch JE. Effects of training with a robot-virtual reality system compared with a robot alone on the gait of individuals after stroke. Stroke; a journal of cerebral circulation. 2009;40:169–74. doi: 10.1161/STROKEAHA.108.516328. [DOI] [PubMed] [Google Scholar]
- 8.Yang YR, Tsai MP, Chuang TY, Sung WH, Wang RY. Virtual reality-based training improves community ambulation in individuals with stroke: a randomized controlled trial. Gait & posture. 2008;28:201–6. doi: 10.1016/j.gaitpost.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Yang YR, Wang RY, Chen YC, Kao MJ. Dual-task exercise improves walking ability in chronic stroke: a randomized controlled trial. Arch Phys Med Rehabil. 2007;88:1236–40. doi: 10.1016/j.apmr.2007.06.762. [DOI] [PubMed] [Google Scholar]
- 10.Plummer P, Iyigun G. Effects of Physical Exercise Interventions on Dual-Task Gait Speed Following Stroke: A Systematic Review and Meta-Analysis. Arch Phys Med Rehabil. 2018 doi: 10.1016/j.apmr.2018.04.009. [DOI] [PubMed] [Google Scholar]
- 11.Bohannon RW. Comfortable and maximum walking speed of adults aged 20-79 years: reference values and determinants. Age and ageing. 1997;26:15–9. doi: 10.1093/ageing/26.1.15. [DOI] [PubMed] [Google Scholar]
- 12.Bohannon RW, Wang YC, Gershon RC. Two-minute walk test performance by adults 18 to 85 years: normative values, reliability, and responsiveness. Arch Phys Med Rehabil. 2015;96:472–7. doi: 10.1016/j.apmr.2014.10.006. [DOI] [PubMed] [Google Scholar]
- 13.Schmid A, Duncan PW, Studenski S, Lai SM, Richards L, Perera S, et al. Improvements in speed-based gait classifications are meaningful. Stroke; a journal of cerebral circulation. 2007;38:2096–100. doi: 10.1161/STROKEAHA.106.475921. [DOI] [PubMed] [Google Scholar]
- 14.Fletcher GF, Balady GJ, Amsterdam EA, Chaitman B, Eckel R, Fleg J, et al. Exercise Standards for Testing and Training: A Statement for Healthcare Professionals From the American Heart Association. Circulation. 2001;104:1694–740. doi: 10.1161/hc3901.095960. [DOI] [PubMed] [Google Scholar]
- 15.Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed) 1982;284:1607–8. doi: 10.1136/bmj.284.6329.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. Journal of the American Geriatrics Society. 2005;53:695–9. doi: 10.1111/j.1532-5415.2005.53221.x. [DOI] [PubMed] [Google Scholar]
- 17.Wade DT, Collin C. The Barthel ADL Index: a standard measure of physical disability? International disability studies. 1988;10:64–7. doi: 10.3109/09638288809164105. [DOI] [PubMed] [Google Scholar]
- 18.Washburn RA, Smith KW, Jette AM, Janney CA. The Physical Activity Scale for the Elderly (PASE): development and evaluation. Journal of clinical epidemiology. 1993;46:153–62. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 19.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical care. 1992;30:473–83. [PubMed] [Google Scholar]
- 20.Hurst NP, Kind P, Ruta D, Hunter M, Stubbings A. Measuring health-related quality of life in rheumatoid arthritis: validity, responsiveness and reliability of EuroQol (EQ-5D) British journal of rheumatology. 1997;36:551–9. doi: 10.1093/rheumatology/36.5.551. [DOI] [PubMed] [Google Scholar]
- 21.Oldfield RC. The assessment and analysis of handedness: the Edinburgh inventory. Neuropsychologia. 1971;9:97–113. doi: 10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- 22.Littell RC, Pendergast J, Natarajan R. Modelling covariance structure in the analysis of repeated measures data. Stat Med. 2000;19:1793–819. doi: 10.1002/1097-0258(20000715)19:13<1793::aid-sim482>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- 23.Yang L, He C, Pang MY. Reliability and Validity of Dual-Task Mobility Assessments in People with Chronic Stroke. PloS one. 2016;11:e0147833. doi: 10.1371/journal.pone.0147833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. The journals of gerontology Series A, Biological sciences and medical sciences. 1995;50A:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.