Abstract
Pregnancy is a unique period when biological changes can increase sensitivity to chemical exposures. Pregnant women are exposed to multiple environmental chemicals via air, food, water and consumer products, including flame retardants, plasticizers, and pesticides. Lead exposure increases risk of pregnancy-induced hypertensive disorders, although women’s health risks are poorly characterized for most chemicals. Research on prenatal exposures has focused on fetal outcomes and less on maternal outcomes. We reviewed epidemiologic literature on chemical exposures during pregnancy and three maternal outcomes: preeclampsia, gestational diabetes, and breast cancer. We found that pregnancy can heighten susceptibility to environmental chemicals and women’s health risks, although variations in study design and exposure assessment limited study comparability. Future research should include pregnancy as a critical period for women’s health. Incorporating biomarkers of exposure and effect, deliberate timing and method of measurement, and consistent adjustment of potential confounders would strengthen research on the exposome and women’s health.
Keywords: Endocrine disruption, environmental chemicals, chemical breast cancer, maternal outcomes, pregnancy complications, women’s health, pregnancy-induced hypertensive disorders, preeclampsia, gestational hypertension, blood pressure, gestational diabetes, impaired glucose tolerance, placenta
1. Introduction
Pregnancy is a unique period of tightly coordinated hormone-mediated events that significantly alter maternal physiology to accommodate the developing fetus and prepare for labor and breastfeeding. Dramatic changes to vascular physiology, metabolism, reproductive organs, endocrine activity, and the immune system can increase maternal susceptibility to chemical exposures and associated health risks. For example, lead accumulates in the bones over a lifetime and is mobilized with the release of calcium during pregnancy. Not only does this increase exposure risk, but it can also induce hypertension and increase risk for developing other maternal health complications [1]. Additionally, mammary gland differentiation during pregnancy is highly sensitive to estrogenic compounds, which can alter breast tissue composition and increase maternal risk for developing breast cancer later in life [2,3].
Maternal health complications and breast cancer contribute to a significant proportion of women’s health issues. First, pregnancy-induced hypertensive disorders are a leading cause of maternal morbidity and mortality worldwide, complicating roughly 5–10%, or 8 million, pregnancies [4]. They include pregnancy-induced hypertension (new-onset blood pressure ≥ 140/90 mmHg after 20 weeks gestation); preeclampsia (PE), defined as new-onset hypertension with ≥ 1 other systemic symptom, such as proteinuria (excess urinary proteins signaling kidney damage), visual impairment (signaling neurological dysfunction), and/or elevated liver enzymes (signaling hepatic dysfunction); HELLP (hemolysis, elevated liver enzymes and low platelets) syndrome; and eclampsia, the severe progression of PE that presents with additional stroke or seizure [5]. About 25–50% of women with new-onset hypertension will develop PE [4], but PE can present without hypertension [6]. Pregnancy-induced hypertensive disorders have increased worldwide by roughly 25% over the past 20 years [4], while the risk of severe PE increased more than 5-fold among younger women in the United States [7]. Second, gestational diabetes mellitus (GDM), defined as glucose intolerance first diagnosed during pregnancy, arises when maternal insulin levels are insufficient to meet the increased metabolic demands of pregnancy. GDM affects up to 14–18% of pregnant women globally, with prevalence increasing by 10–100% over the past 20 years and additional increases expected as a result of recent changes to diagnostic criteria and rising obesity rates [8,9]. Finally, breast cancer is the leading cause of cancer mortality among women worldwide, with incidence and mortality risk increasing by 14–20% over the last decade [10]. Pregnancy-associated breast cancer (PABC) has the worst survival prognosis and contributes 10–20% of the total breast cancer incidence among younger women (< 30 years old), with incidence rising alongside global trends in delayed childbearing [11].
Maternal health complications share common pathophysiological elements and complex risk patterns with breast cancer. PE and GDM are risk factors for one another during pregnancy that heighten maternal susceptibility to future metabolic and cardiovascular disease [9,12], which can also contribute to breast cancer risk later in life [13]. Some research suggests that PE is directly associated with decreased breast cancer risk, while GDM is directly associated with increased breast cancer risk, although no consensus has been reached [14–18]. Genetic mutations account for only 5–10% of the total breast cancer prevalence [19,20], while definitive causes for GDM and PE have not been identified [7], raising concern for environmental risk factors that may be influencing these multifactorial diseases.
Leading medical professional societies have voiced grave concerns about chemical exposure effects on women’s health [21,22]. Pregnant women are exposed to a variety of chemicals associated with adverse health outcomes, many of which are known or suspected reproductive toxicants [23,24]. Endocrine disrupting chemicals (EDCs) are one class of chemicals under scrutiny because they can influence hormones that drive biological changes during pregnancy by interfering with endogenous hormone action through varied molecular mechanisms (e.g., by mimicking or blocking cell-to-cell signals, interfering with hormone production or degradation, etc.) [25]. Chemicals such as EDCs are widely used in consumer and personal care products yet have limited safety oversight in the United States. Consequently, EDCs and other chemicals pose a high body burden among U.S. pregnant women and children [23,24,26].
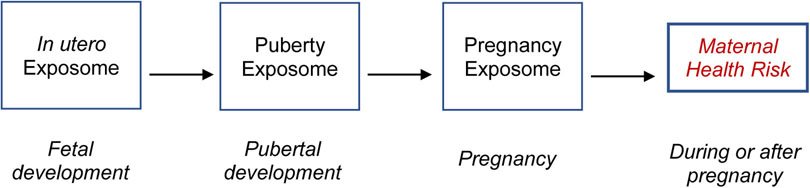
Environmental chemicals and the physiology of pregnancy are important components of the pregnancy exposome, defined as the totality of external and internal exposures during the pregnancy period, which can alter the course of pregnancy and influence maternal and perinatal health outcomes in meaningful ways [27]. Research on prenatal exposures has focused primarily on fetal outcomes [25,27]. In contrast, few studies have examined the impact of chemical exposures during pregnancy on women’s health, despite substantial physiological changes that influence maternal vulnerability. Given the relative paucity of information about the impact of environmental chemicals on women’s health during pregnancy, our review summarizes existing literature on chemical exposures during pregnancy and adverse maternal health outcomes, focusing on preeclampsia, gestational diabetes, and breast cancer. The goal of this review is to inform future research directions on the pregnancy exposome and women’s health.
2. Methods
Our main objectives were to 1) describe how internal physiological changes during pregnancy can increase sensitivity to external chemical exposures, 2) summarize epidemiologic literature on women’s health risks (preeclampsia, gestational diabetes, and breast cancer) associated with chemical exposures during pregnancy, and 3) make recommendations for future research on environmental chemical exposures and women’s health. We defined the epidemiologic summary as a qualitative synthesis of existing human observational studies, combining elements from multiple review types, including critical, narrative, and scoping review methods [28,29]. Specifically, we performed a structured search to capture relevant literature and a descriptive synthesis of studies which included an assessment of the size and scope of available literature (scoping) [28]. The large volume and breadth of studies warranted a qualitative rather than quantitative approach (e.g., systematic review or meta-analysis). We provide an overview of the types of studies that are currently available, including a summary of population sizes, study design, and report of coefficients. The goal of our review is to serve as a guidepost to the current literature from which further synthesis and systematic reviews can be conducted.
We begin by describing normal physiological changes during pregnancy that can influence susceptibility to chemical exposures and adverse outcomes. We then summarize the collection of epidemiologic literature, including an overview of methodological issues relevant to the majority of reviewed studies, followed by a brief discussion of mechanisms supported by animal and in vitro studies, along with common themes and future research directions. We conclude with general recommendations for further epidemiologic research on women’s health and the pregnancy exposome.
2.1. Search terms and review criteria
We performed a structured search of the PubMed database restricted to studies published since 2000 using MeSH terms for peer-reviewed literature in English on environmental exposures during pregnancy and adverse maternal health outcomes in May 2018 (Table 1). Our inclusion criteria were defined as maternal exposures and maternal outcomes, where maternal exposures are environmental chemical exposures during pregnancy, or within two years preceding conception for persistent compounds, that were measured or modeled in biomonitoring or exposure assessment studies. To manage the broad scope of this review, we excluded lead and ambient air pollution, which have been extensively examined with respect to pregnancy-induced hypertensive disorders [30–33]. Additionally, ambient air pollution (e.g., polycyclic aromatic hydrocarbons from traffic emissions, etc.) was considered outside the scope of this review, which focused on chemicals with significant dietary and/or indoor exposure profiles. Although we included cadmium, arsenic, and mercury in this review, we excluded metals and metalloids that are essential elements, such as selenium, zinc, and manganese, which were also considered outside the scope of this review. We selected three maternal outcomes, including preeclampsia (PE), gestational diabetes mellitus (GDM), and breast cancer, based on their significant contributions to women’s health, shared risk profiles, and relevance to physiological changes during pregnancy. For PE, we included studies of blood pressure and pregnancy-induced hypertension (PIH), and for GDM, we included gestational impaired glucose tolerance (IGT), as clinically relevant indicators. We incorporated terms describing breast physiology, since biological changes during pregnancy can influence susceptibility to external exposures and breast cancer risk [3]. Finally, we added “placental diseases” and “placental weight” due to the placenta’s strong influence on PE and GDM [34].
TABLE 1.
Search terms (ordered as #1 AND #2 AND #3)
| Category | Terms |
|---|---|
| (1) During pregnancy | (pregnancy[MeSH Terms] OR pregnant women[MeSH Terms] OR pregnancy[tiab] OR pregnant[tiab] OR mothers[MeSH Terms] OR prenatal[Title] OR maternal risk[tiab]) |
| (2) Maternal Exposure | (chemical[tiab] OR endocrine disruptors[MeSH Terms] OR endocrine disruptors[tiab] OR environmental pollutants[MeSH Terms] OR environmental pollution[MeSH Terms] OR environmental exposure[mh] OR exposure[tiab] OR maternal exposure[mh]) |
| (3) Maternal Outcome | (breast neoplasms[MeSH Terms] OR mammary glands, human[MeSH Terms] OR mammary gland[tiab] OR breast cancer[tiab] OR mammary cancer[tiab] OR breast density[MeSH Terms] OR breast density[tiab] OR mammographic density[tiab] OR “breast tissue”[tiab] OR “maternal complications”[tiab] OR “pregnancy complications”[tiab] OR placenta diseases[MeSH Terms] OR “placental weight”[Title] OR diabetes, gestational[MeSH Terms] OR blood pressure[MeSH Terms] OR hypertension[MeSH] OR pre-eclampsia[MeSH Terms] OR (Labor, Obstetric[mh] AND timing[tiab])) OR (“maternal breast cancer”) |
| (4) #1 AND #2 AND #3 |
We found 3603 studies using our list of search terms (Table 1). Ten duplicates were removed and one reviewer (JV) scanned the remaining list of 3593 studies for titles and abstracts matching our inclusion criteria. A second reviewer (AS) re-examined the list for quality assurance and control. The first reviewer then did a full text review of studies captured from the title/abstract scan to further determine whether they should be reviewed according to our inclusion and exclusion criteria.
3. Overview of Physiological Changes During Pregnancy
During pregnancy, significant changes to maternal physiology are required to support the developing fetus and prepare for labor, delivery, and breastfeeding. Maternal blood vessels expand as blood flow and blood volume increase; blood pressure decreases while heart and respiratory rates increase; insulin resistance rises as glucose metabolism shifts to favor the fetus; the ratio of immune cells switches to minimize inflammatory cytokine production and tolerate the fetus; and mammary glands differentiate and prepare for milk production [35,36]. These changes are largely controlled by hormones through a series of molecular signals and feedback loops that allow the endocrine system to manage and integrate multiple complex signals while maintaining homeostasis during a period of rapid biological change [37]. In this section we review key physiological changes that occur during pregnancy and how they influence susceptibility to environmental exposures.
3.1. The Placenta: Redirecting Maternal Blood Flow
In the earliest stages of pregnancy, the placenta forms from a small group of cells that surround and protect the embryo. The trophoblast cells that comprise the outer layer of the blastocyst are progenitor placental cells that provide nutrients for the developing embryo during this early period [35]. To promote fetal growth and maximize nutrient transfer between mother and fetus, some progenitor cells differentiate into cytotrophoblast (CTB) cells that form cell columns and become invasive, breaching the uterine wall and further differentiating into endovascular CTBs, which travel through the smooth muscle of the uterus to the decidua, in search of the maternal blood supply. The endovascular CTBs enter the outer layer of cells along maternal blood vessels, fundamentally remodeling maternal vasculature to form hybrid structures that are both maternal and embryonic or fetal in origin [38]. Maternal spiral arteries dilate and transform from low-flow, high-resistance channels into high-flow, low-resistance vessels This vascular remodeling progressively anchors the placenta to the uterus and redirects blood flow towards the maternal-fetal interface, where the placenta filters hazardous compounds and transfers oxygen and nutrients to the fetus over the course of pregnancy [35].
Placental formation (placentation) is susceptible to chemical exposures that disrupt CTB differentiation during this time, as proper CTB invasion of maternal decidua is critical for spiral artery remodeling and placental function. Indeed, shallow CTB invasion and poor spiral artery remodeling are initial defining features of PE [4,12], while endothelial dysfunction, characterized by systemic damage to endothelial cells that line maternal blood vessels, can be considered a second critical step in PE development [39]. Molecular signaling pathways that govern oxidative stress, inflammation, and angiogenesis (the formation of new blood vessels from existing blood vessels), may be additional targets of chemical toxicity during this time [40].
3.2. The Cardiovascular System: Increasing Cardiac Output
The redirection of blood flow to the uterus during pregnancy results in a significant reduction in oxygen that reaches maternal tissues and organs. To overcome this hypoxia, maternal physiology adapts by increasing the total blood supply to accommodate the placental-fetal unit. Several changes to vascular physiology facilitate a rise in cardiac output (total blood volume pumped by the heart each minute). Maternal blood vessels expand (vasodilation) as heart rate quickens and plasma volume rises [41]. Vascular resistance and blood pressure decrease initially but increase later in pregnancy. Stroke volume must also increase to satisfy the high pre-load, low after-load requirement for achieving a 50% increase in total circulating blood volume by the end of the third trimester. These vascular changes substantially increase blood flow towards the maternal-fetal interface, further maximizing the exchange of gas and nutrients with the fetus [35,41].
The decline in blood pressure despite increasing blood volume and cardiac output during pregnancy is a result of decreased vascular resistance attributable to early spiral artery remodeling and sustained vasodilation as pregnancy progresses [40]. Thus, chemicals that inhibit vasodilation can increase systemic vascular resistance that subsequently contributes to blood pressure increases, oxidative stress, inflammation, endothelial dysfunction, and risk of developing hypertension and/or PE [40].
3.3. The Metabolic System: Shifting from Glucose to Fat
Normally, the pancreas secretes insulin to balance circulating blood sugar levels against daily fluctuations, removing glucose from the bloodstream by promoting uptake of the nutrient by maternal cells [42]. During pregnancy, several metabolic changes take place to disrupt this equilibrium and maximize the substrate’s availability for transplacental transfer to the fetus, which relies primarily on glucose for energy and growth across the gestational period. Pancreatic β-islet cells proliferate as they undergo hyperplasia, increasing insulin production and elevating blood insulin levels in maternal circulation. Blood sugar rises as insulin sensitivity decreases and maternal uptake of glucose slows, reducing hepatic glucose processing and whole-body glucose disposal by 30–50% in late pregnancy. These metabolic changes ultimately promote the preferential catabolism of maternal fat stores (over glucose or protein), as fetal demands for glucose increase alongside rapid fetal growth in the third trimester [9,42].
The perpetual state of hyperglycemia and progressive insulin resistance that are characteristic of normal pregnancy result in a diabetogenic, or diabetes-producing, physiological condition that requires maternal insulin levels to increase by >200% to overcome [9,42]. Gestational diabetes mellitus (GDM) can develop when maternal physiology does not sufficiently increase production to meet the new demand, resulting in chronic excessive hyperglycemia that is toxic to maternal cells, if left untreated. Prolonged exposure to high blood sugar increases vascular resistance in maternal blood vessels, which further heightens risk for developing PE and other pregnancy-induced hypertensive disorders. Chemicals that disrupt or damage pancreatic β cells can therefore increase maternal susceptibility for developing GDM as well as PE. In addition, environmental chemicals that interfere with the peroxisome proliferator-activated receptor (PPAR) signaling pathway, which mediates placental development and is fundamental to lipid metabolism, may also contribute to risk of these maternal health complications [12].
3.4. The Reproductive System: Preparing for Lactation
Pregnancy represents the third stage of breast development (mammogenesis), a process that begins with subtle mammary gland preparations in utero followed by substantial changes during puberty to establish a network of terminal ductal lobular units [43]. The terminal ducts elongate and give rise to lobular-alveolar structures that contain milk-producing buds during pregnancy, as rapid cell proliferation and extensive differentiation displace the largely undifferentiated adipose tissue into a highly branched ductal tree-like structure [44]. The first milk proteins of the colostrum become functional glandular units as preparations for milk production are finalized in the third trimester [45]. Further cues after delivery stimulate milk secretion and initiate lactation, when mammary gland differentiation achieves full maturation and female breast development is complete [37,44,45]. The maternal breasts enlarge substantially during this time as a result of an increased supply of nutrients and two-fold rise in blood flow that support the rapid biological changes associated with this phase of female breast development [45]. Mammogenesis is susceptible to chemical exposures that prevent differentiation during pregnancy because breast cancer is more likely to develop from terminal ductal lobular units than from fully differentiated lobular-alveolar structures [44,46]. Environmental chemicals that interfere with PPAR signaling or angiogenesis may also influence breast cancer development during this time [47,48].
3.5. The Endocrine System: Driving Physiological Changes
The physiological changes of pregnancy are largely driven by hormones, which are the molecular signaling molecules that relay messages for the endocrine system along neuroendocrine axes consisting of three components – the hypothalamus (brain), pituitary gland (base of the brain), and target endocrine gland (i.e., HP-target gland axis, HP-endocrine axis, or HP-axis) (Table 2). In this review, we highlight the hormones and neuroendocrine axes that are important for maternal health outcomes and may be susceptible to chemical exposures. However, it is recognized that other signaling molecules and pathways are relevant for fetal development.
Table 2.
Neuroendocrine (Hypothalamic-Pituitary-target gland) axis functions, hormones, and interactions during pregnancy.
| Endocrine Axis | Main Functions | Axis Pathway | Critical Hormones | Hormone Actions and Axis Interactions during Pregnancy |
|---|---|---|---|---|
| Adrenal Glands (HPA) | Stress Response, Immune Response, Parturition. |
(Hypo) → (Pituitary) → (Adrenals) CRH → ACTH → GC, Cortisol |
Corticotropin releasing hormone (CRH) |
|
| Gonadal (ovaries and testes) (HPG) | Growth/Development, Mammogenesis, Immune Response. |
(Hypo) → (Pituitary) → (Gonads) GnRH → FSH → Testosterone GnRH → LH → Estrogen |
Estrogen |
|
| Prolactin (HPRL) | Mammogenesis/Lactation. | (Hypo) → (Pituitary) Prolactin | Prolactin | |
| Growth Hormone (HGH) | Growth/Development, Metabolism, Mammogenesis/Lactation. | (Hypo) → (Pituitary) GH → IGF-I | Growth hormone (GH) |
|
| Thyroid Gland (HPT) | Growth/Development, Metabolism. |
(Hypo) → (Pituitary) → (Thyroid) TRH → TSH → T3, T4 |
Thyroxine (T3), Triiodothyronine (T4) |
|
ACTH = Adrenocorticotropic hormone; CRH = Corticotropin Releasing Hormone; CTB = Cytotrophoblast. DHEA = Dehydroepiandrosterone. FSH = Follicle Stimulating Hormone; GC = Glucocorticoid; GnRH = Gonadotropin Releasing Hormone; IGF-I = Insulin-like Growth Factor-I; LH = Luteinizing Hormone; PRL = Prolactin; TRH = Thyrotropin Releasing Hormone; TSH = Thyroid Stimulating Hormone.
The hypothalamus acts as control tower for the endocrine system through the release of primary hormone regulators that signal further release of stimulating hormones by the pituitary gland, which travel to target endocrine glands throughout the body to promote site-specific hormone synthesis. Once newly synthesized hormones reach threshold levels, they limit further production by inhibiting upstream HP-axis activity until levels decrease again below threshold. This negative feedback loop is complicated by interaction with other signaling pathways, such as other neuroendocrine axes or biological stress response pathways. For example, estrogen produced by the ovaries along the HP-Gonadal (HPG) axis stimulates cortisol production in the adrenal glands by activating the HP-Adrenal (HPA) axis. Cortisol in turn inhibits estrogen synthesis along the HP-Gonadal axis and can also inhibit activity along the HP-Thyroid and HP-Growth Hormone axes. Growth hormone may further interact with the immune system, influencing the release of pro-inflammatory cytokines such as IL-6 and TNF-alpha during an immune response [49]. The interplay of hormones with other signaling pathways becomes more complex during pregnancy, when multiple neuroendocrine systems coordinate signals across the maternal-placental-fetal unit [37].
Hormone levels increase dramatically during pregnancy to initiate a series of biological events that promote fetal growth and development. The first trimester marks a rapid increase in human chorionic gonadotropin (hCG), estrogen, and progesterone, with hCG increasing most quickly and peaking the earliest, reaching maximum levels by three months followed by a slow decline across the second and third trimesters [50]. Estrogen has the most dramatic increase over the entire course of pregnancy, sustaining levels 1000 times greater than the non-pregnant state. High persistent estrogen levels drive numerous developmental changes during pregnancy by promoting growth and proliferation in estrogen receptor-expressing cells throughout the body. Progesterone also increases and sustains high levels throughout gestation, serving vital functions to maintain pregnancy and relax smooth muscle throughout the body. Other major pregnancy hormones include prolactin, corticotropin releasing hormone (CRH), thyroid hormone, and human chorionic somatomammotropin (hCS). Estrogen and progesterone have distinct important roles in promoting cardiovascular changes to maternal physiology over the course of pregnancy. Estrogen mediates the rise in maternal cardiac output by promoting an increase in heart rate, while progesterone facilitates vasodilation and decidualization of CTB cells during placentation by relaxing smooth muscle walls that line maternal vasculature [37,51]. CRH, hCG and relaxin, promote vasodilation during pregnancy through the nitric oxide pathway, which regulates oxidative stress, blood pressure, and vascular resistance [35,50]. Estrogen and hCG also regulate angiogenic factors that are critical for placentation and breast development during pregnancy [48,52,53]. Additionally, estrogen and progesterone synergistically promote mammary gland differentiation with prolactin, the hormone critical for milk production and secretion [35,37]. Estrogen promotes prolactin while progesterone inhibits prolactin’s stimulating effect on milk secretion during pregnancy, which helps maintain pregnancy while milk production preparations are still underway (i.e., ductal to lobular-alveolar differentiation is not yet complete) [45]. The rapid decline of progesterone just before birth allows estrogen to promote the prolactin-stimulated release of colostrum in the early postpartum days that are crucial for initiating lactation. Growth hormone and insulin-like growth factor-I (IGF-I) are additional important regulators of mammogenesis during pregnancy [37,54].
The placenta is also a neuroendocrine organ that synthesizes and regulates hormones at each level of the HP-endocrine axis during pregnancy, developing features that closely resemble maternal neuroendocrine function [37]. Human chorionic somatomammotropin (hCS), formerly known as human placental lactogen (hPL), shares a similar structure with prolactin and can bind to prolactin receptors. Although hCS has a minor lactogenic role, it is considered the major diabetogenic hormone of pregnancy, more similar in structure and function to pituitary growth hormone than to prolactin. hCS promotes insulin resistance, insulin secretion, as well as fetal glucose and maternal lipid uptake (i.e., through the mobilization of fatty acids) during pregnancy. Placental growth hormone (PGH) and IGF-I have additional key roles in shifting maternal metabolism during pregnancy while maintaining their roles as regulators of growth and development in the mammary glands, placenta, and fetus [34]. Other lactogenic hormones that are also diabetogenic include prolactin, cortisol, progesterone, and pituitary growth hormone [34]. Finally, some placental hormones during normal pregnancy resemble those of the kidney under hypoxic conditions. The vasoconstrictor, Angiotensin II, and vasodilator, adrenomedullin, are angiogenic factors of the renin-angiotensin system that mediate vascular development and oxidative stress during placentation [34,35].
By interfering with hormones and molecular signaling pathways that govern important physiological changes during pregnancy, including placentation, vasodilation, insulin resistance, and mammary gland differentiation, environmental chemicals can potentially increase risk of maternal health complications and breast cancer. Identifying modifiable risk factors, such as chemical exposures, that contribute to these outcomes may thus have important implications for women’s health.
4. Results of Literature Review: Chemical Exposures and Maternal Health
We identified 64 epidemiologic studies since 2000 that evaluated chemical exposures and risk of preeclampsia (including blood pressure and hypertension), gestational diabetes mellitus (including gestational impaired glucose tolerance), and maternal breast cancer. We organized review subsections according to how chemical exposures are typically studied: 1) Persistent organic pollutants (POPs) including polychlorinated biphenyls (PCBs), polybrominated diphenyl ethers (PBDEs), and perfluoroalkyl substances (PFAS); 2) Pesticides (including persistent organochlorine pesticides (OCPs) and the less persistent organophosphate pesticides (OPPs); 3) Non-persistent chemicals, including phenols and phthalates; and 4) Heavy metals/metalloids, including lead, cadmium, arsenic, and mercury. PCBs and PBDEs are heat resistant chemicals used in a wide range of products, from electronics to furniture (although both chemical classes have been phased out in the United States) [63][63,64]. PFAS are de-greasing agents used in non-stick cookware and many other products [65]. The OCPs include dichlorodiphenyltricloroethane (DDT), used globally to control malaria, DDT’s active metabolite, dichlorodiphenyldichloroethylene (DDE), and other pesticides that have been replaced with less persistent organophosphate pesticides (OPPs) but remain relevant due to their environmental and biological persistence [66]. Phenols, such as bisphenol A (BPA), as well as phthalates are widely used in everyday products like cosmetics and packaged foods [67]. Cadmium and other heavy metals/metalloids are naturally occurring elements that bioaccumulate up the food chain [68–70].
4.1. Methodological Considerations
This review covered a broad range of chemicals and outcomes, with multiple potential sources of epidemiological bias. While our descriptive approach precluded rigorous evaluation of study quality and risk of bias, several considerations regarding common sources of selection bias and measurement error are worth noting to aid the interpretation of results. First, most studies conditioned on live birth data (from pregnancy cohort studies, recruitment at delivery, or birth records), which can introduce selection bias (live-birth bias) from the exclusion of participants who would have become PE or GDM cases had they not experienced earlier fetal loss. Conditioning the study population on fetal survival can bias results in the negative direction (underestimate risk) if both outcomes are related to the chemical exposure (which removes exposed cases from the study population). Although research suggests the magnitude of this bias is small and can be minimized with common risk factor adjustment [71], it may conceivably be greater for severe cases of PE which require early delivery of an unviable fetus. Second, reviewed studies varied substantially by method of exposure assessment. While direct chemical measurements in biological samples (e.g., urine, blood, drinking water, etc.) are subject to less differential (non-random) error than indirect exposure estimates (e.g., modeled with participant surveys subject to recall bias), biological matrices are also subject to error, as certain tissues are more appropriate for certain chemicals. For example, urine is preferred for non-persistent compounds that metabolize readily in urine but are at high risk of laboratory contamination in serum (e.g., BPA and phthalates [72]), while serum is preferred for persistent lipophilic chemicals such as PCBs and PBDEs [73]. Correcting for hydration status in urine and chemical lipid partitioning in serum are also subject to measurement error, since analyte concentrations normalized with common proxies for urine dilution (e.g., creatinine, specific gravity) and adipose content (i.e., serum lipid level) may vary across covariates (e.g., age, race/ethnicity, etc.) and/or with the outcome under study [74–76]. Modeling these proxy variables as independent covariates can reduce this error in some cases [74,75], although inconsistent methods and reporting of these results can limit study comparability. An additional consideration for non-persistent chemicals with high within-person variability (low correlation) across pregnancy (e.g., BPA) is the collection of repeated samples over time, since spot samples (one-time measurements) introduce non-differential misclassification (random error) which can bias results towards the null. The type of biomarker (e.g., free vs. conjugated BPA metabolites, inorganic vs. organic arsenic, etc.) and timing of measurement in relation to disease onset and windows of susceptibility are also important considerations [77–79].
4.2. Preeclampsia and Chemical Exposures
We found 37 human epidemiologic studies of chemical exposures and preeclampsia (PE) including blood pressure and pregnancy-induced hypertension (PIH) as clinical PE indicators (Table 3). The studies covered a wide range of population sizes (N=58 to N=295,387). Some were limited by sample size while others had sufficient power to detect a modest association; the majority included a small number of PE cases (~25 to 85) and thus used variations of case-control study designs as a sampling strategy.
Table 3.
Epidemiologic studies of preeclampsia (PE) and chemical exposures in pregnant women (37 studies).
| Study [Ref #] | Study Design | Total N, # Cases | Study Period | Study Population, Location | Chemical Exposure(s) | Maternal Outcome(s) | Results |
|---|---|---|---|---|---|---|---|
| Persistent Organic Pollutants and Pesticides (16 Studies) | |||||||
| [88] | Nested Case-control. | N=1933, 131 PE, 365 PIH. |
1959–1965. | Participation in Collaborative Perinatal Project across 12 study centers, USA. | Measured maternal serum levels of 8 OCPs: p,p′-DDE, p,p′-DDT, HCB, β-HCH, dieldrin, heptachlor epoxide, trans-nonachlor, and oxychlordane; and 11 PCB congeners: 28, 52, 74, 105, 118, 138, 153, 170, 180, 194, and 203; every 8 weeks during pregnancy. | PE, PIH. |
p,p′-DDE and PIH: Adjusted OR=1.0 (95% CI: 0.7−1.6), 0.7 (95% CI: 0.4–1.1), 0.8 (95% CI: 0.5−1.3), and 0.9 (95% CI: 0.6−1.5) for women in the 2nd, 3rd, 4th, and 5th exposure quintile compared to women in the lowest exposure quintile (p-trend=0.78). Similar results for p,p′-DDE and PE, p,p′-DDT and PE, and for Total PCBs and PIH, and HCB and PIH. p,p′-DDT and PIH: Adjusted OR=1.0 (95% CI: 0.6−1.6), 0.5 (95% CI: 0.3–0.9), 0.8 (95% CI: 0.5−1.3), and 0.4 (95% CI: 0.2−0.7) for women in the 2nd, 3rd, 4th, and 5th exposure quintile compared to women in the lowest exposure quintile (p-trend=0.002). Similar results for HCB/PE. Total PCBs and PE: Adjusted OR=0.7 (95% CI: 0.4−1.5), 0.8 (95% CI: 0.4–1.7), 0.6 (95% CI: 0.2−1.5), and 0.5 (95% CI: 0.2−1.3) for women in the 2nd, 3rd, 4th, and 5th exposure quintile compared to women in the lowest exposure quintile (p-trend=0.39). Similar results for heptachlor epoxide and PE. β-HCH and PIH: Adjusted OR=0.8 (95% CI: 0.5−1.3), 0.6 (95% CI: 0.4−0.9), 0.5 (95% CI: 0.3−0.8), and 0.5 (95% CI: 0.3−0.8) for women in the 2nd, 3rd, 4th, and 5th exposure quintile compared to women in the lowest exposure quintile (p-trend=0.01). β-HCH and PE: Adjusted OR=0.7 (95% CI: 0.3−1.7), 0.8 (95% CI: 0.4−1.9), 0.5 (95% CI: 0.2−1.3), and 1.2 (95% CI: 0.5−3.2) for women in the 2nd, 3rd, 4th, and 5th exposure quintile compared to women in the lowest exposure quintile (p-trend=0.41). Similar results for dieldrin/PE. Dieldrin and PIH: Adjusted OR=1.4 (95% CI: 0.8−2.3), 1.9 (95% CI: 1.1−3.2), 1.8 (95% CI: 1.0−3.0), and 1.7 (95% CI: 1.0−3.0) for women in the 2nd, 3rd, 4th, and 5th exposure quintile compared to women in the lowest exposure quintile (p-trend=0.12). Heptachlor epoxide and PIH: Adjusted OR=0.5 (95% CI: 0.3−0.9), 0.7 (95% CI: 0.4−1.1), 0.7 (95% CI: 0.4−1.3), and 0.5 (95% CI: 0.3−1.0) for women in the 2nd, 3rd, 4th, and 5th exposure quintile compared to women in the lowest exposure quintile (p-trend=0.11). Trans-nonachlor and PE: 1.1 (95% CI: 0.5−2.3), 0.6 (95% CI: 0.3−1.4), and 0.8 (95% CI: 0.3−1.8) for women in the 3rd, 4th, and 5th exposure quintiles compared to women in the first two exposure quintiles (p-trend=0.47). Oxychlordane and PIH: Adjusted OR=0.8 (95% CI: 0.5−1.2), 1.0 (95% CI: 0.6−1.5), and 0.9 (95% CI: 0.6−1.6) for women in the 3rd, 4th, and 5th exposure quintiles compared to women in the first two exposure quintiles (p-trend=0.93). Similar results for Oxychlordane and PE. |
| [89] | Prospective Cohort. | N=258, 27 PIH. |
2005–2009. | Participation in Longitudinal Investigation of Fertility and the Environment (LIFE) Study in 16 counties of Michigan and Texas, USA. | Measured maternal serum levels of 6 OCPs with >80% detection frequency: HCB, β-HCH, p,p′-DDE, p,p′-DDT, oxychlordane, and trans-nonachlor; and 7 PBDE congeners: 28, 47, 85, 99, 100, 153, 154; once soon before pregnancy. | PIH, GDM. |
Ln p,p′-DDT and PIH: Adjusted OR=0.27 (95% CI: 0.04–1.73) per SD increase in exposure. Results for HCB, β-HCH, oxychlordane, p,p′-DDE, trans-Nonachlor were similar to p,p′-DDT, with adjusted OR ranging between 0.43−0.74 and 95% CIs that crossed 1.0. Ln BDE-47 and PIH: Adjusted OR=1.86 (95% CI: 0.55–6.27) per SD increase in exposure. Ln BDE-154 and PIH: Adjusted OR=0.59 (95% CI: 0.15–2.33) per SD increase in exposure. Adjusted OR for PBDE-28, 85, 99, 100 was similar to PBDE-154, ranging from 0.61 to 0.96, with 95% CIs that crossed 1.0. |
| [90] | Case-control. | N=115, 45 PE. |
2013–2015. | Prenatal care patients at one of three hospitals in Tehran, Iran. | Measured maternal serum levels of 8 PBDE congeners: 28, 47, 99, 100, 153, 154, 183, and 209; and 10 PCB congeners: 28, 52, 74, 99, 101, 118, 138, 153, 180, and 187; once in 3rd trimester. | PE. |
Total PBDEs and PE: Adjusted OR=2.19 (95% CI: 1.39−3.45, p-value=0.001). With adjustment for PCBs: Adjusted OR=1.52 (95% CI: 0.90−2.58). Total PCBs and PE: Adjusted OR=1.77 (95% CI: 1.34−2.32, p-value <0.001). Results were similar in the model adjusting for PBDEs. Total POPs and PE: Adjusted OR=1.54 (95% CI: 1.26−1.87, p-value <0.001). |
| [85] | Retrospecti ve Cohort. | N=1766, 49 PE. |
1969–1983. | Residence in Cape Cod, Massachusetts, USA. | Modeled drinking water exposure to PERC during pregnancy using water distribution models and geospatial software. | PE, Other complications. | PERC and PE: Adjusted Risk Ratio=0.39 (95% CI: 0.14−1.10), 0.36 (95% CI: 0.12−1.07), and 0.37 (95% CI: 0.17−0.83) for women in the low (< 50th percentile), high (≥ 50th percentile), and “any” PERC exposure groups compared to women in the non-exposed group. |
| [83] | Case-control. | N=11,737, 730 PE. |
1990–2006. | Participation in C8 Health Project and residence in Ohio and West Virginia, USA. | Modeled maternal serum levels of PFOA in early pregnancy using sample of serum data, chemical release records, environmental distributions, PBPK models, and geospatial software. | PE, Other complications. | Ln PFOA and PE: Adjusted OR=1.13 (95: CI: 1.00−1.28) per IQR increase in PFOA exposure. Results were similar for each 100 ng/mL unit increase in PFOA level and when exposure was modeled categorically, with adjusted ORs ranging from 1.1−1.2 for women in the top three quintiles of PFOA exposure compared to women in the lowest two exposure quintiles (combined as referent). Lower confidence limits were also similar between continuous and categorical models (~1.0). However, upper confidence limits increased in categorical models, ranging from 1.4−1.6 compared to 1.2−1.3 in continuous models. |
| [82] | Case-control (Study I), Nested Case-control (Study 2) | N=4063, 224 PIH (Study I), N=4547, 250 PIH (Study II). | 1990–2004. | Residence in study area (Study I) and participation in C8 Health Project (Study II), Ohio and West Virginia, USA. | Modeled maternal serum levels of PFOA in early pregnancy using sample of serum data, chemical release records, environmental distributions, PBPK models, and geospatial software. | PIH, Other complications. | Ln PFOA and PIH (Study I): Adjusted OR (uncalibrated) = 1.02 (95% CI: 0.86−1.21) per IQR exposure increase. Similar results with 100 ng/mL increase; categorical exposure (study I and II); and continuous calibration models, with slight attenuation of estimates to 0.87−0.97 (study II). In categorical calibration models, results varied slightly with different modeling approaches for estimating exposure using predictive algorithms: Adjusted OR (Bayesian calibration) = 1.5 (95% CI: 1.1−2.1) for women in the 3rd exposure quintile (and 4th using traditional calibration) compared to the reference group (women in the 1st and 2nd exposure quintiles combined). |
| [84] | Nested Case-control. | N=1845 (PFOA), N=5262 (PFOS) | 2000–2006. | Participation in Collaborative Perinatal Project, mid-Ohio Valley, USA. | Modeled maternal serum levels of PFOA and PFOS in early pregnancy using sample of serum data. | PE. |
Ln PFOA and PE: Adjusted OR=1.1 (95% CI: 0.9−1.4) per IQR increase in exposure. Similar PFOS result. With binary exposure categories: Adjusted OR=1.3 (95% CI: 0.9−1.9) for women in the high (≥50th percentile of exposure) compared to low (<50th percentile) exposure groups. With exposure modeled as four categories: Adjusted OR=1.5 (95% CI: 1.0−2.3), 1.2 (95% CI: 0.7−2.1), and 0.9 (95% CI: 0.5−1.8) for women in the 50th–74.99th, 75th–90th, and >90th percentiles of exposure, compared to women in the lowest exposure group (<50th percentile). Ln PFOS and PE: PFOS result were similar but with lower confidence limit > 1. Results were slightly attenuated except for top 10th percentile: Adjusted OR=1.6 (95% CI: 1.2−2.3) for women in the highest (>90th percentile) compared to lowest (<50th percentile) exposure groups. |
| [122] | Nested Case-control. | N=976, 466 PE. | 2003–2007. | Participation in Norwegian Mother and Child Cohort Study, Norway. | Measured plasma levels of 7 PFAS with >50% detection frequency: PFOS, PFHpS, PFHxS, PFOA, PFNA, PFDA, and PFUnDA; once at 17−20 weeks gestation. | PE. |
Ln PFUnDA and PE: Adjusted HR=0.78 (95% CI: 0.66−0.92). With exposure modeled categorically: Adjusted HR=0.51 (95% CI: 0.35−0.76), 0.60 (95% CI: 0.41−0.88), and 0.55 (95% CI: 0.38−0.81) for women in the 2nd, 3rd, and 4th quartiles of exposure compared to women in the lowest exposure quartile. Ln PFOA and PE: Adjusted HR=1.01 (95% CI: 0.69−1.48). With exposure modeled categorically: Adjusted HR=1.03 (95% CI: 0.70−1.50), 0.92 (95% CI: 0.63−1.35), 0.89 (95% CI: 0.65−1.22), and 1.01 (95% CI: 0.69−1.48) for women in the 2nd, 3rd, and 4th quartiles of exposure compared to women in the lowest exposure quartile. Ln PFOS and PE: Adjusted HR=1.13 (95% CI: 0.84, 1.52). With exposure modeled categorically: Adjusted HR=1.12 (95% CI: 0.76, 1.65), 0.88 (95% CI: 0.60, 1.29), and 1.09 (95% CI: 0.75, 1.58) for women in the 2nd, 3rd, and 4th quartiles of exposure compared to women in the lowest exposure quartile. Ln PFNA and PE: Adjusted HR=0.90 (95% CI: 0.70, 1.16. With exposure modeled categorically: Adjusted HR=0.88 (95% CI: 0.60, 1.30), 1.04 (95% CI: 0.71, 1.53), and 0.88 (95% CI: 0.60, 1.29) for women in the 2nd, 3rd, and 4th quartiles of exposure compared to women in the lowest exposure quartile. Ln PFDA and PE: Adjusted HR=0.88 (95% CI: 0.75, 1.04). With exposure modeled categorically: Adjusted HR=0.88 (95% CI: 0.67, 1.16) for women in the high exposure group (≥ 50th percentile) compared to women in the low exposure group (< 50th percentile). Ln PFHxS and PE: Adjusted HR=0.91 (95% CI: 0.72, 1.14). With exposure modeled categorically: Adjusted HR=0.86 (95% CI: 0.59, 1.26), 1.01 (95% CI: 0.69, 1.49), and 0.93 (95% CI: 0.64, 1.36) for women in the 2nd, 3rd, and 4th quartiles of exposure compared to women in the lowest exposure quartile. Ln PFHpS and PE: Adjusted HR=1.03 (95% CI: 0.86, 1.24). With exposure modeled categorically: Adjusted HR=1.30 (95% CI: 0.88, 1.92), 1.01 (95% CI: 0.69, 1.48), and 1.12 (95% CI: 0.77, 1.63) for women in the 2nd, 3rd, and 4th quartiles of exposure compared to women in the lowest exposure quartile. |
| [93] | Prospective Cohort. | N=779, 31 PE, 65 PIH. | 2004–2007. | Participation in prospective mother-child cohort study, Timoun, Guadeloupe. | Measured plasma levels of chlordecone (DDE and PCB-153 analyzed as potential confounders in a subset of samples) once in 3rd trimester. | PE, PIH, GDM. |
Log10 Chlordecone and PE: Adjusted OR=0.9 (95% CI: 0.4−1.7). When modeled as 4 categories: Adjusted OR=1.1 (95% CI: 0.3−2.8), 1.2 (95% CI: 0.4−3.4), and 1.0 (95% CI: 0.3−3.1) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile. Log10 Chlordecone and PIH: Adjusted OR=0.4 (95% CI: 0.2−0.6). When modeled as 4 categories: Adjusted OR=0.5 (95% CI: 0.3−1.1), 0.2 (95% CI: 0.1−0.5), and 0.3 (95% CI: 0.2−0.6) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile. Spline model: Linear and non-linear components: p <0.01 and p-value=0.37, respectively. |
| [92] | Cross-sectional. | N=733, 15 PE, 76 PIH, 79 HPD. |
2012–2013. | Participation in the Venda Health Examination of Mothers, Babies and their Environment (VHEMBE) birth cohort study and residence in Limpopo, South Africa. | Measured serum levels of DDT/DDE once at delivery. | PE, PIH, Hypertensive disorders of pregnancy (HPD, including (PE, PIH, or eclampsia). |
Physician diaanosed Ln p,p′-DDT and PE: Adjusted OR=1.26 (95% CI: 0.74−2.16). When exposure was modeled as four categories: Adjusted OR=1.35 (95% CI: 0.38−4.91) and 1.48 (95% CI: 0.72−3.02) for women in the 3rd and 4th quartiles of p,p′-DDT exposure compared to women in the lowest exposure quartile (Note: Estimates for the 2nd exposure quartile were not reported due to small number of PE cases). Ln p,p′-DDE and PE: Adjusted OR=1.14 (95% CI: 0.62−2.10). When exposure was modeled as four categories: Adjusted OR=0.44 (95% CI: 0.07−2.67), 2.25 (95% CI: 0.31−4.87), and 0.81 (95% CI: 0.16−3.94) for women in the 2nd, 3rd, and 4th quartiles of p,p′-DDE exposure, respectively, compared to women in the lowest exposure quartile. Ln o,p′-DDT and PE: Adjusted OR=1.48 (95% CI: 0.86−2.56). When exposure was modeled as four categories: Adjusted OR=0.66 (95% CI: 0.10−4.31), 2.78 (95% CI: 0.62−12.41), and 2.12 (95% CI: 0.41−10.88) for women in the 2nd, 3rd, and 4th o,p′-DDT exposure quartiles, respectively, compared to women in the lowest exposure quartile. Ln p,p′-DDT and PIH: Adjusted OR=1.28 (95% CI: 0.95−1.72). When exposure was modeled as four categories: Adjusted OR=0.93 (95% CI: 0.44−1.98), 1.11 (95% CI: 0.54−2.27), and 1.48 (95% CI: 0.72−3.02) for women in the 2nd, 3rd, and 4th quartiles of p,p′-DDT exposure compared to women in the lowest exposure quartile. NOTE: Continuous and categorical results were similar for o,p′-DDT and p,p′-DDE with PIH; p,p′-DDT and p,p′-DDE with HDP. Self-reported Ln p,p′-DDT and HDP: Adjusted OR=1.50 (95% CI: 1.10−2.03). When exposure was modeled as four categories: Adjusted OR=0.96 (95% CI: 0.43−2.16), 1.33 (95% CI: 0.63−2.82), and 1.90 (95% CI: 0.92−3.94) for women in the 2nd, 3rd, and 4th quartiles of p,p′-DDT exposure, respectively, compared to women in the lowest exposure quartile. Continuous and categorical results were similar for p,p′-DDE. Ln o,p′-DDT and HDP: Adjusted OR=1.37 (95% CI: 0.95−1.99). When exposure was modeled as four categories: Adjusted OR=0.47 (95% CI: 0.20−1.09), 1.54 (95% CI: 0.78−3.02), and 1.39 (95% CI: 0.69−2.79) for women in the 2nd, 3rd, and 4th quartiles of o,p′-DDT exposure, respectively, compared to women in the lowest exposure quartile. |
| [94] | Cross-sectional. | N=508, 134 Total. | 2011–2015. | Delivery at hospitals with high, medium, and low historic exposure in Kyrgyzstan. | Measured placenta levels of 11 OCPs: Total HCH, α-HCH, β-HCH, γ-HCH, δ-HCH, DDT, DDE, DDD, aldrin, dieldrin, and heptachlor; once at delivery. | PE/Eclampsia, Total complications. |
Total OCPs and PE/eclampsia: Unadjusted RR=10.0 for women in the exposed group (women with detectable OCP levels measured in placental tissues, with observed PE/eclampsia risk) compared to women in the non-exposed group (with undetectable OCPs measured in placental tissues had 0.75% PE/eclampsia risk). Total OCPs and total maternal complications: Unadjusted RR=0.620 (95% CI: 0.159−2.420, p-value=0.492), 0.921 (95% CI: 0.500−1.696, p-value=0.792), 3.832 (95% CI: 2.616−5.612, p-value <0.0001), 7.153 (5.252–9.742, p-value <0.0001), and 3.040 (2.164−4.271, p-value <0.0001) for women in the 1st, 2nd, 3rd, 4th, and total exposure groups, respectively, compared to women in the non-exposed group. Unadjusted OR=4.448 (p-value <0.0001) for women in the total exposure group compared to women in the non-exposed group. Note: Adjusted results were not available due to limited study author access to covariate data. |
| [96] | Nested Case-control. | N=11,274, 504 PE, 660 PIH. | 1993–1997. | Licensed pesticide applicators and spouses enrolled in Agricultural Health Study (AHS), Iowa and North Carolina, USA. | Modeled pesticide exposure as 1) none, 2) indirect (planting, pruning, weeding, picking, harvesting), 3) residential (use in garden or home), or 4) agricultural (mixing, applying, repairing equipment) in 1st trimester using participant surveys. | PE, PIH. |
Pesticide use and PIH: Adjusted OR=1.20 (95% CI: 1.00–1.44), 1.27 (95% CI: 1.02–1.60), and 1.60 (95% CI: 1.05–2.45) for women comprising the indirect, residential, and agricultural exposure groups, respectively, compared to women in the non-exposed group. Pesticide use and PE: Adjusted OR=1.13 (95% CI: 0.92–1.39), 1.32 (95% CI: 1.02–1.70), and 2.07 (95% CI: 1.34–3.21) for women comprising the indirect, residential, and agricultural exposure groups, respectively, compared to women in the non-exposed group. |
| [95] | Cross-sectional. | N=2203, 155 PIH. | 2007–2013. | Clinical care patients in Sicily. | Modeled pesticide exposure as 1) none, 2) indirect (planting, pruning, weeding, picking, harvesting), 3) domestic (pesticide use in garden or house), or 4) occupational (work with pesticides); in 1st trimester using participant surveys. | PIH. |
Diazinon and PIH: Adjusted OR=1.09 (95% CI: 1.03−1.16, p-value <0.05) Malathion and PIH: Adjusted OR=1.14 (95% CI: 1.08−1.19, p-value <0.05). Chlorpyrifos and PIH: Adjusted OR=1.03 (95% CI: 0.86–1.08). Parathion and PIH: Adjusted OR=1.02 (95% CI: 0.78–1.19). |
| [99] | Prospective Cohort. | N=4465, 60 PE, 79 PIH. | 2002–2006. | Participation in Generation R Study and residence in Rotterdam, The Netherlands. | Modeled occupational chemical exposures, including pesticides, phthalates, organic solvents, alkylphenolic compounds, and metals in mid-gestation using a job-exposure-matrix (JEM). | PE, PIH. |
Pesticides and PE: Adjusted OR=3.15 (95% CI: 0.38−25.94). Similar but slightly attenuated results for metals and PE. No PIH results available. Phthalates and PE: Adjusted OR=0.82 (95% CI: 0.11−6.16). No PIH results available. Similar results for organic solvents, PIH, and PE. Alkylphenols and PE: Adjusted OR=0.81 (95% CI: 0.19−3.45). Alkylphenols and PIH: Adjusted OR=1.56 (95% CI: 0.46−5.29). Similar but slightly attenuated results observed for any chemicals, PIH, and PE. |
| [97] | Case-control. | N=295,387,7296 PE. | 1998–2011. | Residence in the San Joaquin Valley of California, USA. | Modeled pesticide exposure for 543 individual chemicals and 69 physicochemical groupings in each month time period of pregnancy using agricultural data, land-use surveys, and geospatial software. | PE (multiple phenotypes). | The frequency of exposure (any vs none) was relatively equal between cases and reference population controls. Most ORs comparing the frequency of any chemical exposure were below 1.0. |
| [98] | Case-control. | N=183,313, 4912 PE. | 1969–1989. | Economically active farm holders in Norway. | Modeled pesticide exposure using purchase history in 1968 and presence of pesticide application equipment in 1978. | PE. | Pesticides and PE: Adjusted Rate Ratio=0.92 (95% CI: 0.86−0.98) for women in the exposed compared to non-exposed groups. |
| Non-persistent Chemicals (8 Studies) | |||||||
| [101] | Case-control. | N=58, 23 PE. | Not readily found. | Delivery at hospital in Quebec, Canada. | Measured maternal serum, placenta, and cord blood levels of BPA once after delivery. | PE. | BPA levels in PE pregnancies: 9.4 (95% CI: 0.40−101 ng/ml); compared to BPA levels in normotensive pregnancies: 3.0 (95% CI: 0.30−36.1 ng/ml) (p-value=0.04). |
| [102] | Nested Case-control. | N=482, 50 PE. | 2011. | Clinical care patients in Boston, Massachusetts or Philadelphia, Pennsylvania, USA. |
Measured urinary levels of BPA and 9 phthalate metabolites: MEHP, MEHHP, MEOHP, MECPP, MBzP, MBP, MiBP, MEP, and MCPP; four times at 10, 18, 26, and 35 weeks gestation. | PE. |
BPA and PE: Adjusted HR=1.14 (95% CI: 0.73, 1.79) 1.53 (1.04, 2.25)* 1.12 (95% CI: 0.61, 2.07) 0.68 (95% CI: 0.43, 1.07) 1.44 (95% CI: 0.80, 2.58) per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. MEHP and PE: Adjusted HR=1.40 (1.03, 1.89)* 1.26 (95% CI: 0.97, 1.63) 1.14 (95% CI: 0.82, 1.60) 1.38 (1.02, 1.85)* 2.05 (1.35, 3.12)* per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. %MEHP and PE: Adjusted HR=0.73 (95% CI: 0.52, 1.03) 0.75 (95% CI: 0.58, 0.97)* 0.90 (95% CI: 0.65, 1.25) 0.78 (95% CI: 0.61, 1.00) 1.17 (95% CI: 0.67, 2.03) per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. ΣDEHP and PE: Adjusted HR=1.79 (1.30, 2.46)* 1.52 (1.15, 2.00)* 1.24 (95% CI: 0.87, 1.75) 1.70 (1.24, 2.34)* 2.92 (1.61, 5.28)* per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. MBzP and PE: Adjusted HR=0.93 (95% CI: 0.64, 1.35) 0.93 (95% CI: 0.65, 1.33) 1.08 (95% CI: 0.69, 1.70) 0.98 (95% CI: 0.63, 1.53) 1.83 (95% CI: 0.59, 5.65) per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. MBP and PE: Adjusted HR=1.06 (95% CI: 0.74, 1.53) 1.14 (95% CI: 0.82, 1.56) 0.95 (95% CI: 0.58, 1.56) 1.09 (95% CI: 0.72, 1.65) 2.25 (95% CI: 0.98, 5.19) per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. MiBP and PE: Adjusted HR=0.84 (95% CI: 0.58, 1.21) 1.22 (95% CI: 0.86, 1.74) 0.79 (95% CI: 0.49, 1.30) 0.64 (95% CI: 0.46, 0.90)* 1.54 (95% CI: 0.62, 3.82) per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. MEP and PE: Adjusted HR=1.40 (1.00, 1.95)* 1.72 (1.28, 2.30)* 1.13 (95% CI: 0.76, 1.67) 1.15 (95% CI: 0.79, 1.68) 0.80 (95% CI: 0.46, 1.39) per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. MCPP and PE: Adjusted HR=0.95 (95% CI: 0.71, 1.28) 1.07 (95% CI: 0.86, 0.66 (95% CI: 0.45, 1.00) 1.52 (1.07, 2.15)* 2.37 (1.34, 4.18)* per IQR increase in exposure for the Average (visit 1−3), Visit 1, Visit 2, Visit 3, and Visit 4, respectively. |
| [103] | Nested Case-control. | N=173, 74 PE. | 2013–2014. | Delivery at hospital in Fudan, China. | Measured maternal serum levels of BPA once at 16−20 weeks gestation. | PE. | BPA and PE: Adjusted OR=1.39 (95% CI: 1.19−1.63) (p-value <0.01). Results were similar when stratified by PE severity and timing of PE onset. With exposure modeled as three categories: Adjusted OR=2.15 (94% CI: 0.98−4.75, p-value=0.06) and 16.46 (95% CI: 5.42 −49.95, p-value <0.01) for women in the middle (2.24−4.44 μg/L) and high (>4.44 μg/L) compared to low (<2.24 μg/L) BPA exposure group. |
| [106] | Prospective Cohort. | N=369, 34 PIH disorder. | 2003–2007. | Participation in Health Outcomes and Measures of the Environment (HOME) Study, Cincinnati, Ohio, USA. | Measured urinary levels of 9 phthalate metabolites: MEHP, MEHHP, MEOHP, MECPP, MBzP, MBP, MiBP, MEP, and MCPP; twice at 16 and 26 weeks gestation. | Blood pressure (DBP, SBP), PIH disorders (PE, PIH, HELLP syndrome, and Eclampsia). |
Phthalates and Blood Pressure (<20 wfe) Log10 MEP and DBP: Adjusted Difference=−0.1 (95% CI: −1.3−1.2, p-value=0.91) mm Hg blood pressure per 10-fold increase in exposure. Similar results for ΣDEHP and DBP and ΣDEHP and SBP. Log10 MEP and SBP: Adjusted Difference=0.8 (95% CI: −1.1–2.7, p-value=0.40) mm Hg blood pressure per 10-fold increase in exposure. Log10 MCPP and SBP: Adjusted Difference=0.6 (95% CI: −2.5, 3.6) p-value=0.72. Log10 IDBP and SBP: Adjusted Difference=0.5 (95% CI: −2.5, 3.6), p-value=0.73. Log10 MBzP and DBP: Adjusted Difference=2.3 (95% CI: 0.9–3.7, p-value <0.01) mm Hg blood pressure per 10-fold increase in exposure. Log10 MBzP and SBP: Adjusted Difference=1.9 (95% CI: −0.3–4.1, p-value=0.08) mm Hg blood pressure per 10-fold increase in exposure. Similar results for Log10 ΣDnBP and DBP, and Log10 MCPP and DBP. Phthalates (<20 wks) and Blood Pressure (≥20 wks) Log10 MEP and DBP: 1.1 (95% CI: −0.3–2.5, p-value=0.13). Similar results for Log10 MEP and SBP, Log10 MBzP and DBP, Log10 MBzP and SBP, and Log10 ΣDnBP and DBP. Log10 MCPP and DBP: 0.7 (95% CI: −1.7–3.0, p-value=0.59). Similar results for Log10 ΣDnBP and SBP. Log10 MCPP and SBP: 2.4 (95% CI: −0.9–5.7, p-value=0.16). Log10 IDEHP and DBP: −0.8 (95% CI: −2.2–0.5, p-value=0.24). Similar results ΣDEHP and SBP. Phthalates and Blood Pressure (≥20 wks) Log10 MEP and DBP: 1.0 (95% CI: −0.4–2.3, p-value=0.16). Similar results for Log10 MBzP and DBP. Log10 MEP and SBP: 0.2 (95% CI: −1.7–2.1, p-value=0.83). Similar results for Log10 MBzP and SBP, Log10 MCPP and DBP, and Log10 ΣDEHP/DBP. Log10 MCPP and SBP: −0.9 (95% CI: −4.7–3.0, p-value=0.66). Similar results for Log10 IDEHP and SBP. Log10 ΣDnBP and DBP: 2.8 (95% CI: 0.4–5.3, p-value=0.02). Similar results for Log10 IDnBP and SBP. Phthalates (95% CI: Average) and Blood Pressure (≥20 wks) Log10 MEP-Average and DBP: 1.4 (95% CI: −0.2–3.0, p-value=0.09). Log10 MBzP-Average and DBP: 1.5 (95% CI: −0.6–3.6, p-value=0.16). Similar results for Log10 IDnBP-Average and SBP. Log10 MBzP-Average and SBP: 1.1 (95% CI: −2.0–4.3, p-value=0.49). Similar results for Log10 MCPP-Average and SBP. Log10 MEP-Average and SBP: 0.8 (95% CI: −1.6–3.1, p-value=0.53). Log10 MCPP-Average and DBP: 0.6 (95% CI: −2.4–3.7, p-value=0.69). Log10 ΣDnBP-Average and DBP: 2.8 (95% CI: −0.1–5.8, p-value=0.06). Log10 ΣDEHP-Average and DBP: −0.6 (95% CI: −2.4–1.3, p-value=0.55). Log10 IDEHP-Average and SBP: −1.6 (95% CI: −4.3–1.2, p-value=0.27). Phthalates (<20 wks) and PIH disorders Log10 MEP and PIH Disorders: Adjusted RR=1.16 (95% CI: 0.66–2.05, p-value=0.60). Log10 MBzP and PIH Disorders: Adjusted RR=1.74 (95% CI: 0.78–3.89, p-value=0.18). Similar results for Log10 ΣDBP and PIH Disorders. Log10 MCPP and PIH Disorders: Adjusted RR=0.86 (95% CI: 0.33–2.24, p-value=0.76). Similar results for Log10 ΣDEHP and PIH Disorders Phthalates (≥20 wks) and PIH Disorders Log10 MEP and PIH Disorders: Adjusted RR=1.17 (95% CI: 0.67–2.05, p-value=0.60). Log10 MBzP and PIH Disorders: Adjusted RR=1.59 (95% CI: 0.82–3.06, p-value=0.17). Similar results for Log10 ΣDEHP and PIH Disorders. Log10 MCPP and PIH Disorders: Adjusted RR=2.73 (95% CI: 1.07–6.93, p-value=0.04). Similar results for Log10 ΣDBP and PIH Disorders. Phthalates (Average) and PIH disorders Log10 MEP-Average and PIH disorders: Adjusted RR=1.14 (95% CI: 0.59–2.18, p-value=0.70). Similar results for Log10 ΣDEHP-Average and PIH disorders. Log10 MCPP-Average and PIH disorders: Adjusted RR=1.67 (95% CI: 0.58–4.82, p-value=0.34). Log10 MBzP-Average and PIH disorders: Adjusted RR=1.98 (95% CI: 0.96–4.11, p-value=0.07). Similar results for Log10 ΣDBP-Average and PIH disorders. |
| [87] | Retrospecti ve Cohort. | N=19,249; 233 PE, 464 PIH. | 1997–2003. | Licensed cosmetologists pregnant during 1997–2003 in New York, USA. | Modeled non-persistent chemicals in beauty products using New York State cosmetology license in 2003 as proxy for occupational exposure. | PE, PIH, Other complications. |
Comparison to realtors Cosmetology license and PE: Adjusted OR = 1.06 (95% CI: 0.74–1.53) for licensed cosmetologists compared to realtors. Cosmetology license and PIH: Adjusted OR = 1.34 (95 % CI: 1.01–1.76) for licensed cosmetologists compared to realtors. Comparison to general population Cosmetology license and PE: Adjusted OR=0.76 (95% CI: 0.62–0.95) for licensed cosmetologists compared to women in the general population. Cosmetology license and PIH: Adjusted OR=0.94 (95% CI: 0.80–1.10) for licensed cosmetologists compared to women in the general population. |
| [86] | Case-control. | N=81,205; 403 PE (mani), 1288 PE (cos). |
1996–2009. | Licensed cosmetologists and manicurists pregnant during 1996–2009 in California, USA. | Modeled non-persistent chemicals in beauty products using California cosmetology license (ha/ir and nail care services) and/or manicurist license during 1996–2006 as proxies for occupational exposure. | PE, GDM, Other complications. |
Comparison to other working women Manicurist license and PE: Adjusted OR=0.92 (95% CI: 0.80–1.05) for manicurists compared to other working women. Restricted to Vietnamese manicurists: Adjusted OR=1.26 (95% CI: 0.62–2.55). Cosmetology license and PE: Adjusted OR=1.06 (95% CI: 0.98–1.15) for cosmetologists compared to other working women. Restricted to Vietnamese cosmetologists: Adjusted OR=1.33 (95% CI: 0.62–2.84). Comparison to general population Manicurist license and PE: Adjusted OR=0.84 (95% CI: 0.75–0.95) for manicurists compared to women in the general population. Restricted to Vietnamese manicurists: Adjusted OR=1.0 (95% CI: 0.71–1.39). Cosmetology license and PE: Adjusted OR=0.97 (95% CI: 0.91–1.03) for cosmetologists compared to women in the general population. Restricted to Vietnamese cosmetologists: Adjusted OR=1.05 (95% CI: 0.68–1.62). |
| [104] | Prospective Cohort. | N=152. | 2014–2015. | Participation in the Human Early-Life Exposome (HELIX) project in Barcelona, Spain, Grenoble, France, or Oslo, Norway. | Measured urinary levels of 10 phthalate metabolites: MEP, MiBP, MnBP, MBzP, MEHP, MEHHP, MEOHP, MECPP, OH-MiNP, and oxoMiNP; 7 phenols including 4 parabens: MeP, EtP, PrP, BrP, and BuP, BPA, triclosan, and BP-3; and 6 non-specific OPP metabolites: DMP, DE-Phosphate, DMTP, DETP, DMDTP, DEDTP; twice (three times per day for one week each) at 18 and 32 weeks gestation. | Blood Pressure (SBP, DBP). |
GEE Models MEP and PE: Adjusted β=−0.52 (95% CI: −1.10–0.06), p-value=0.080. MiBP and PE: Adjusted β=−1.11 (95% CI: −2.56–0.35), p-value=0.136. MnBP and PE: Adjusted β=−0.65 (95% CI: −1.98–0.68), p-value=0.334. MBzP and PE: Adjusted β=−0.21 (95% CI: −1.18–0.77), p-value=0.679. MEHP and PE: Adjusted β=−0.86 (95% CI: −1.83–0.12), p-value=0.084. MEHHP and PE: Adjusted β=−0.44 (95% CI: −1.62–0.75, p-value=0.468) in mmHg per doubling of exposure. Simlar results for MEOHP and PE. MECPP and PE: Adjusted B=−0.39 (95% CI: −1.76–0.98), p-value=0.579. Similar results for ΣDEHP and OH-MiNP. OXO-MiNP and PE: Adjusted B=−0.06 (95% CI: −0.83–0.72), p-value=0.889. MeP and PE: Adjusted β=−0.16 (95% CI: −0.55–0.22), p-value=0.406. Similar results for EtP, BrP, and PrP. Similar results for OXBE, triclosan, DMP, DMTP, and DEP. BPA and PE: Adjusted B=−0.82 (95% CI: −1.34–0.30), p-value=0.002. DETP and PE: Adjusted B=0.04 (95% CI: −0.36–0.45), p-value=0.832. Similar results for ΣDAP and PE. |
| [105] | Prospective Cohort. | N=644. | 2014–2015 | Participation in birth cohort at Wuhan Women and Children Medical Care Center in Wuhan, Hubei Province, China. | Measured urinary levels of 5 parabens: MeP, EtP, PrP, BuP, and BzP; triclosan; and 3 benzophenones: BP-1, BP-3, and 4-OH-BP; three times at 1st, 2nd, and 3rd trimesters. | Blood Pressure (SBP, DBP, PP, MAP). |
All participants (N=644) Ln MeP and SBP: Adjusted β=0.15 (95% CI: −0.12–0.43), p-value=0.47. Similar results for MeP with DBP, MAP, Iparabens and SBP, DBP, and MAP, and for triclosan and SBP, PrP and DBP, PrP and MAP, BP-1 and SBP, BP-1 and PP, BP-1 and MAP, BP-3 and DBP, 4-OH-BP and MAP, Ibenzophenones and DBP, and βbenzophenones and MAP. Ln MeP and PP: Adjusted β=−0.02 (95% CI: −0.25–0.21), p-value=0.74. Similar results for PrP and PP, Iparabens and PP, triclosan and DBP and MAP, EtP and SBP, EtP and DBP, BrP and PP, EtP and PP, and EtP and MAP, BP-1 and DBP, and 4-OH-BP and DBP. Ln Triclosan and PP: Adjusted β=0.34 (95% CI: 0.14–0.54), p-value=0.02. Ln BP-3 and SBP: Adjusted β=0.32 (95% CI: 0.06–0.59), p-value=0.17. Similar results for BP-3 and PP, 4-OH-BP and SBP, 4-OH-BP S and PP, Σbenzophenones and SBP, and Σbenzophenones and PP. Women with male fetus (n=336) Ln MeP and SBP: Adjusted β=0.35 (95% CI: −0.03–0.72), p-value=0.13. Similar results for Σparabens and SBP, Σparabens and DBP, Σparabens and MAP, Σbenzophenones and PP, Triclosan and PP, BP-3 and SBP, BP-3 and DBP, BP-3 and MAP, 4-OH-BP and PP, and 4-OH-BP and MAP. Ln MeP and DBP: Adjusted β=0.16 (95% CI: −0.14–0.46), p-value=0.47. Similar results for Ln MeP and PP, MeP and MAP, PrP and SBP, PrP and MAP, PrP and DBP, PrP and PP, Σparabens and PP, triclosan and DBP and MAP, EtP and SBP, EtP and MAP, EtP and DBP, BP-1 and PP, BP-3 and PP, and 4-OH-BP and DBP. Ln EtP and PP: Adjusted β=−0.11 (95% CI: −0.40–0.17), p-value=0.60. Ln Triclosan and SBP: Adjusted β=0.32 (95% CI: 0.01–0.64), p-value=0.03. Similar results for Ln BP-1 and SBP, BP-1 and DBP, BP-1 and MAP, 4-OH-BP and SBP, Σbenzophenones and SBP, Σbenzophenones and DBP, Σbenzophenones and MAP. Women with female fetus (n=308) Ln Triclosan and DBP: Adjusted β=−0.38 (95% CI: −0.65−−0.10), p-value=0.03. Ln Triclosan and PP: Adjusted β=0.30 (95% CI: 0.03–0.58), p-value=0.11. Similar results for Ln BP-3 and PP, Σbenzophenones and PP. Ln BP-1 and DBP: Adjusted β=−0.42 (95% CI: −0.79−−0.06), p-value=0.08. Ln MeP and DBP: Adjusted β=0.20 (95% CI: −0.14–0.54), p-value=0.38. Similar results for MeP and MAP, Σparabens and DBP, and Ln BP-1 and PP. Ln 4-OH-BP and PP, Σbenzophenones and SBP. Ln MeP and PP: Adjusted β=−0.31 (95% CI: −0.64–0.03), p-value=0.13. Similar results for Σparabens and PP, Σbenzophenones and DBP. Ln EtP and SBP: Adjusted β=−0.19 (95% CI: −0.54–0.16), p-value=0.74. Similar results for EtP and PP, PrP and SBP, PrP and PP, PrP and MAP, Σparabens and SBP, triclosan and MAP, BP-1 and MAP, Ln BP-3 and DBP, Σbenzophenones and MAP, BP-1 and SBP, BP-3 and MAP, 4-OH-BP and SBP, 4-OH-BP and DBP, EtP and DBP, EtP and MAP, PrP and DBP, Σparabens and MAP, Triclosan and SBP, and MeP and SBP. Note: p-values adjusted for multiple comparisons using false discovery rate. |
| Heavy Metals/Metalloids (13 Studies) | |||||||
| [109] | Case-control. | N=176, 88 PE. | 2011. | Prenatal care patients at hospital in Kinasha, Democratic Republic of Congo. | Measured daily urine excretion of 20 metals/metalloids (with > 50% detection): lead, cadmium, chromium, arsenic, lithium, beryllium, aluminum, vanadium, manganese, cobalt, nickel, copper, zinc, selenium, molybdenum, tin, antimony, tellurium, thallium, and uranium; once during pregnancy. | PE. |
Lead and PE: Adjusted difference in daily excretion between PE cases and healthy pregnant women = 6.7-fold (p-value <0.001). Cadmium and PE: Adjusted percent difference in daily excretion between PE cases and healthy pregnant women = 2.5-fold (p-value <0.001). Chromium and PE: Adjusted percent difference in daily excretion between PE cases and healthy pregnant women = 5.2-fold (p-value <0.001). Arsenic and PE: Adjusted percent difference in daily excretion between PE cases and healthy pregnant women = 1.3-fold (p-value=0.051). Metals mixture: Positive associations were found for 11 other metals/metalloids. Principal components analysis revealed that metals as a group may be more important than individual metals. Note: Some essential elements were higher among PE cases compared to controls (healthy pregnant women). |
| [110] | Nested Case-control. | N=130, 80 PE. | 2014. | Prenatal care patients at Assiut Women Health Hospital, Egypt. | Measured blood levels of cadmium and lead at delivery. | PE. |
Cadmium and PE: Mean cadmium levels (μg/dl)=1.132 (95% CI: 1.019–1.245) and 0.398 (95% CI: 0.358–0.438) for women with PE compared to women with uncomplicated pregnancies (p-value=0.017). Lead and PE: Mean lead levels (μg/dl)=140.6 (95% CI: 126.5–154.7) and 103.1 (95% CI: 92.8–113.4) for women with PE compared to women with uncomplicated pregnancies (p-value=0.001). |
| [111] | Case-control. | N=145, PE, 48 healthy pregnant, 50 nonpregnant. | 2007–2008. | Yuzuncu Yil University, Turkey. | Measured serum levels of cadmium at 29–38 weeks gestation. | PE. | Cadmium and PE: Mean (SD) Cadmium levels (μg/ml)=0.033 (0.020), 0.029 (0.027), and 0.029 (0.021) for PE cases, healthy pregnant controls, and healthy non-pregnant controls, respectively. Cases were significantly different from both control groups (p <0.05). |
| [112] | Nested Case-control. | N=172, 86 PE. | 2003–2007. | Participation in Maternal Oral Therapy to Reduce Obstetric Risk (MOTOR) study in, Alabama, North Carolina, and Texas, USA. | Measured placenta levels of cadmium and two essential trace elements (selenium and zinc) once at delivery. | PE. | Cadmium and PE: Adjusted OR=1.5 (95% CI: 1.1–2.2). No other heavy metal risk estimates were reported. Note: Essential elements reduced the odds of Cd-associated PE. |
| [113] | Case-control. | N=66, 43 PE. | Not readily found. | Clinical care patients at regional hospital in South Africa. | Measured hair and serum levels of 13 metals, including 4 metals: arsenic, cadmium, chromium, and lead; and 9 essential trace elements: calcium, copper, cobalt, iron, magnesium, manganese, nickel, selenium, and zinc; once at delivery. | PE. |
Arsenic and PE (Hair): Median (± SE) = 5.47 ± 2.79 (range: 0.06, 49.23) μg/a in normotensive controls compared to 7.63 ± 1.32 (range: 0.44, 19.59) μg/a in PE cases (p-value=0.50). Cadmium and PE (Hair): Median (± SE) = 3.75 ± 0.64 (range: 2.78, 17.50) μg/g in normotensive controls compared to 3.96 ± 0.87 (range: 2.03, 34.60) μg/g in PE cases (p-value=0.12). Lead and PE (Hair): Median (± SE) = 58.77 ± 37.04 (range: 33.04, 891.94) μg/g in normotensive controls compared to 72.27 ± 19.82 (range: 23.94, 773.97) ja/a in PE cases (range: p-value=0.15). Arsenic and Pe (Serum): Median (± SE) = 0.49 ± 0.0 (range: 0.01, 0.13) mg/L in normotensive controls compared to 0.06 ± 0.0 (range: 0.06, 0.06) mg/L in PE cases (p-value=0.81). Cadmium and PE (Serum): Median (± SE) = 0.10 ± 0.3 (range: 0.01, 0.34) mg/L in normotensive controls compared to 0.05 ± 0.04 (range: 0.01, 0.96) mg/L in PE cases (p-value=0.14). Lead and PE (Serum): Median (± SE) = 0.16 ± 0.21 (range: 0.0, 3.0) mg/L in normotensive controls compared to 0.20 ± 0.17 (range: 0.04, 5.49) mg/L in PE cases (p-value=0.22). |
| [114] | Case-control. | N=132, 51 PE, 51 non-PE, 30 healthy repro-aged. | 2014–2016. | Clinical care patients at Second Affiliated Hospital of Wenzhou Medical University, Zhejian, Taiwan. | Measured blood levels of cadmium, calcium, and magnesium (once at 28–40 weeks gestation); cord serum levels and placental levels (once at delivery). | PE. | Cadmium and PE (Serum): Adjusted OR=7.83 (95% CI: 1.64–37.26) for women in the third exposure tertile compared to women in the lowest exposure tertile. Additional adjusted ORs were not reported. |
| [115] | Case-control. | N=396, 31 PE. | 2003–2004. | No occupational exposure and delivery at one of two teaching hospitals in Tehran, Iran. | Measured maternal blood and cord blood levels of lead, cadmium, mercury, antimony, manganese, cobalt, and zinc at delivery. | PE. |
Log Pb (mg/dl) and PE (Cord Blood): Adjusted RR=12.96 (95% CI: 1.570–107.025, p-value=0.017) Log Sb (mg/l) and PE (Cord Blood): Adjusted RR=6.11 (95% CI: 1.114–33.534, p-value=0.037). Log Mn (mg/l) and PE (Cord Blood): Adjusted RR=34.20 (95% CI: 1.805–648.042, p-value=0.019). Note: Cadmium not calculated because there was no difference between cases and controls. |
| [116] | Cohort. | N=341. | 2011–2012. | Delivery at one of five public hospitals in Tehran, Iran. | Measured amniotic fluid levels of cadmium at delivery. | PE. | Cadmium and PE: Incidence of PE=21.4% among women in the high cadmium exposure group compared to 11.5% and 9.8% in the moderate and low cadmium exposure groups, respectively (p-value <0.05). |
| [117] | Case-control. | N=306, 104 PE. | Not readily found. | Delivery at hospital in Durango, Mexico. | Measured drinking water levels of arsenic 1–3 weeks after delivery; and urine levels once soon before delivery. | PE. |
Arsenic and PE (Water): Adjusted OR=1.5 (95% CI: 0.20–11.03) and 1.7 (95% CI: 0.7–4.0) for women in the 2nd and 3rd exposure group, respectively, compared to women in the 1st exposure group. Arsenic and PE (Urine): Adjusted OR=1.4 (95% CI: 0.75–2.6, p-value=0.70) and 0.79 (95% CI: 0.41–1.5, p-value=0.21) for women in the 2nd and 3rd exposure groups, respectively, compared to women in the 1st exposure group. |
| [118] | Prospective Cohort. | N=514. | 2009–2014. | Use of private well in household and participation in New Hampshire Birth Cohort Study, USA. | Measured urine levels of total arsenic (iAs), metabolites including monomethylarsonic acid (MMA) and dimethylarsinic acid (DMA), and methylation ratios (PMI = MMA/iAs and SMI = DMA/MMA); once at 24–28 weeks gestation; toenail clippings once at 2 weeks postpartum; and home well water once during pregnancy. | Blood Pressure (SBP, DBP, PP). |
Total As and SBP (Urine): Adjusted β=0.15 (95% CI: 0.02–0.29, p-value=0.022). Similar result for Total As and PP (Urine), DMA and SBP (Urine), high PMI and SBP (Urine), high PMI and PP (Urine), high SMI and SBP (Urine), and for high SMI and PP (Urine). Total As and DBP (Urine): Adjusted β=0.02 (95% CI: −0.08–0.12, p-value=0.73). Similar results for DMA and DBP (Urine) and for low PMI and SBP (Urine). MMA and SBP (Urine): Adjusted β=1.28 (95% CI: −0.27–2.83, p-value=0.11). Similar results for iAs and SBP (Urine) and iAs and PP (Urine). MMA and DBP (Urine): Adjusted β=−0.25 (95% CI: −1.45–0.96, p-value=0.69). Similar result for iAs and DBP (Urine). MMA and PP (Urine): Adjusted β=1.54 (95% CI: 0.16–2.92, p-value=0.028). Low PMI and DBP (Urine): Adjusted β=−0.02 (95% CI: −0.19–0.14, p-value=0.76). Similar results for low SMI and DBP (Urine), high PMI and DBP (Urine), and for low SMI and SBP (Urine), and for high SMI and DBP (Urine). |
| [119] | Cross-sectional. | N=3260. | 1996–1999. | Prenatal care patients at health care center in several counties of Ba Men-Inner Mongolia, China. | Measured drinking water levels of arsenic once during midgestation. | Blood Pressure (SBP, DBP). | Arsenic and SBP: Adjusted SBP difference = 1.88 (95% CI: 1.03–2.73); 3.90 (95% CI: 2.52–5.29), 6.83 (95% CI: 5.39–8.27) for women in the 2nd, 3rd, and 4th groups of arsenic exposure groups compared to the first exposure group (p-value <0.0001). |
| [120] | Prospective Cohort. | N=124, 60 PE. | 2016–2017. | Pregnant dental workers in the 1st trimester at teaching hospitals in Menoufia governorat, Egypt. | Measured urine levels of mercury three times in 1st, 2nd, and 3rd trimesters. | PE, Other Complications. | Mercury and PE: Crude RR=3.67 (95% CI: 1.25–10.76) of pregnant dental workers compared to the non-exposed group (pregnant employees in the hospital administration offices) (p <0.001). Adjusted RRs were not reported due to a lack of covariate differences noted between the exposed and non-exposed groups. |
| [121] | Cross-sectional. | N=263. | 2004–2005. | Participation in THREE birth cohort study in Baltimore, Maryland, USA. | Measured blood levels of total mercury (THg), inorganic mercury (IHg), methyl mercury (MeHg), and ethyl mercury (EtHg); selenium; and n-3 polyunsaturated fatty acids; once at delivery. | Blood Pressure (SBP, DBP, PP). |
THg and SBP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: 2.13 (95% CI: −0.14–4.40) (p <0.10). MeHg and SBP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: 2.83 (95% CI: 0.17–5.50) (p <0.05). IHg and SBP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: −1.18 (95% CI: −−3.72–1.35) (p >0.05). THg and DBP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: 1.43 (95% CI: −0.40–3.26) (p >0.05). MeHg and DBP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: −0.16 (95% CI: −2.32–2.00) (p >0.05). IHg and DBP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: 1.32 (95% CI: −0.73–3.38) (p >0.05). THg and PP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: 0.70 (95% CI: −1.10–2.50) (p >0.05). MeHg and PP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: 2.99 (95% CI: 0.91–5.08) (p <0.05). IHg and PP: Adjusted change in blood pressure measurement (mmHg) with a one-tertile increase in mercury: −2.51 (95% CI: −4.49–−0.53) (p <0.05). |
BPA = Bisphenol A; BP-1 = 2,4-Dihydroxybenzophenone; BP-3 = 2-Hydroxy-4-methoxybenzophenone (Benzophenone-3); BuP = Butylparaben; BzP = Benzylparaben; CI = Confidence Interval; DBP = Diastolic Blood Pressure; DDE = Dichlorodiphenyldichloroethylene; DDT = Dichlorodiphenyltricloroethane; Di-2-ethylhexyl phthalate metabolites (ΣDEHP = MEHHP, MECPP, MEOHP, and MEHP); DMP = Dimethyl phosphate; DE-Phosphate = Diethyl phosphate; DMTP = Dimethyl thio-phosphate; DETP = Diethyl thiophosphate; DMDTP = Dimethyl dithio-phosphate; DEDTP = Diethyl dithiophosphate; EtP = Ethylparaben; HR = Hazard Ratio; HCB = Hexachlorobenzene; HCH = β-Hexachlorocyclohexane; IQR = Interquartile range; MCiOP = Mono(carboxyisooctyl) phthalate; MCPP = Mono (3-carboxypropyl) phthalate; MECPP = Mono-(2-ethyl-5-carboxypentyl) phthalate; MeP = Methylparaben; MEHP = Mono-(2-ethylhexyl) phthalate; MEP = Monoethyl phthalate; MiBP = Monoisobutyl phthalate; MnBP = Mono-n-butyl phthalate; OR = Odds Ratio; OCP = Organochlorine Pesticide; 4-OH-BP = 4-hydroxybenzophenone; PFAS = Perfluoroalkyl substances; PFDeA = Perfluorodecanoic acid; PFHxS = Perfluorohexane sulfonate; PFNA = Perfluorononanoic acid; PFOSA = Perfluorooctane sulfonamide; PFOS = Perfluorooctane sulfonic acid; PFOA = Perfluorooctanoic acid; PFUA = Perfluoroundecanoic acid; PBPK = Physiologically-based Pharmacokinetic; PBDE = Polybrominated diphenyl ether; PCB = Polychlorinated biphenyl; PCDD = Polychlorinated dibenzo-p-dioxins. PCDF = Polychlorinated dibenzofurans. PIH = Pregnancy-induced Hypertension; PP = Pulse Pressure; PrP = Propylparaben; MAP = Mean Arterial Pressure; RR = Relative Risk; SD = Standard Deviation; SBP = Systolic Blood Pressure.
PE was most often defined as new-onset hypertension (≥ 140 mm Hg systolic and/or ≥ 90 mm Hg diastolic blood pressure diagnosed after 20 weeks gestation) combined with proteinuria, which reflects former diagnostic criteria (although forthcoming research will presumably reflect the recently broadened definition that encompasses but is not limited to proteinuria). The majority of studies used either physician diagnosis or medical record abstraction to characterize PE, blood pressure, and/or hypertension. However, a small number used self-reported health data and acknowledged the possibility of outcome measurement error that was likely to be non-differential with respect to exposure, resulting in conservative estimates of association. In addition, validation studies comparing self-reported pregnancy complications to medical records demonstrate moderate to good recall [80,81]. A subset of studies also used medical birth registry and hospital discharge data to classify the outcome, which can be sources of live-birth bias.
Most PE studies assessed chemical exposures with biomarkers in serum (persistent organic pollutants and heavy metals/metalloids) and urine (non-persistent chemicals and heavy metals/metalloids). Studies with more than 100 cases typically were performed in highly exposed populations (i.e., water contaminated communities and occupationally exposed groups) and modeled chemical exposures using questionnaire data, spatial modeling software, fate and transport models, and/or other predictive tools [82–87]. The use of modeling software to estimate exposure may have introduced random measurement error and the possibility of false negative findings. The timing of exposure assessment was evenly spread across early (including recent preconception), mid, and late (including early postpartum) gestation, which decreased comparability of results. Current literature provides little guidance for which gestational windows are most sensitive to specific PE-associated chemical exposures; however, placentation during early to mid-gestation may be more relevant for chemicals that interfere with CTB differentiation, while the second half of gestation may be more relevant for chemicals that contribute to PE through inhibition of vasodilation. Nevertheless, the heterogeneity of PE phenotypes most likely reflects pathophysiological heterogeneity, suggesting that multiple exposure windows are relevant for PE susceptibility.
Analytical methods for most PE studies included adjustment for maternal age, body mass index (BMI), parity, and smoking, with some case control studies that addressed confounding through study design (e.g., by matching on covariates during sampling of control population). Studies have increasingly adjusted for additional PE risk factors, such as family history of PE and/or diabetes, over time. Recent studies have also begun to apply advanced statistical methods to assess longitudinal data (repeated measures of non-persistent chemicals over time), multi-pollutant models, and non-linear exposure response relationships.
Persistent Organic Pollutants (POPs)
Out of eight studies that evaluated persistent organic pollutants with PE or PIH (six case-control and two cohort studies), three included serum PCB and/or PBDE measurements [88–90], one modeled organochlorine exposure in a contaminated community [85], and four studies modeled or measured serum PFAS levels (three in a uniquely exposed U.S. population) [82–84,91] (Table 3).
Polychlorinated Biphenyls (PCBs) and Polbrominated Diphenyl Ethers (PBDEs)
Null PCB and PBDE associations were observed in two U.S. studies that included women regardless of birth history (one PCB study and one PBDE study, both with serum measurements) [88,89], while increased PE risk was associated with serum PCB and PBDE levels in a study of first time mothers in Iran [90], possibly due to higher baseline PE risk observed among first time mothers compared to multiparous women (Table 3). However, restricting to nulliparous women did not influence results in the U.S. PCB study [88], suggesting the difference may be due to other factors. Exposure levels were not comparable due to inconsistent methods and reporting of results (e.g., wet weight vs. lipid-adjusted values, individual congeners vs. summary metrics). However, other potential factors include regional, economic, and/or cultural study population differences. For example, multiple race/ethnicities were represented in U.S. studies, while the Iranian study did not specify race/ethnicity [88,89].
Tetrachloroethylene (PERC)
No association was found in a retrospective cohort study of tetrachloroethylene (PERC), a related organochlorine used in dry cleaning and other industrial applications, despite high exposure levels increasing the probability of detecting a true association. However, a small number of PERC-exposed PE cases (n < 10) and the use of exposure models could have diminished study power [85].
Perfluoroalkyl Substances (PFAS)
Three case-control studies evaluated PE and PIH risk among U.S. residents whose drinking water supply was contaminated with perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate (PFOS) [82–84] (Table 3). Modest PE and PIH associations were observed, but results were close to the null and depended on model specification [82–84]. Although precise methods varied, all three studies used a 2005 sample of serum PFOA and PFOS measurements combined with additional modeling inputs (pharmacokinetic, environmental, and geospatial) to reconstruct historical serum PFOA and PFOS levels in different groupings of the study population. In each case, modeling exposure could have introduced non-differential error that would potentially mask a true signal, which may be one reason why the association fluctuated around the null [82–84]. However, background PFOA levels that were an order of magnitude lower (serum PFOA median = 2.78 ng/ml compared to 21.2 ng/ml) were not associated with PE risk [91], suggesting the levels were too low to detect the modest PE associations observed at high exposure levels in previous studies.
Pesticides
There were ten studies on pesticides and PE or PIH, half of which measured OCP levels in maternal serum (four studies) [88,89,92,93] or placental tissue (one study) [94], while the other half modeled pesticide exposure using participant surveys, occupational data, geospatial analysis, and/or other modeling techniques [95–99] (Table 3). Four of five pesticide modeling studies did not distinguish between OCPs and OPPs, while one focused exclusively on OPPs [95]. Results from OCP biomarker studies were mixed, with two of five suggesting an association with increased risk and the remainder reporting null or inverse associations. Serum DDT/DDE levels were associated with elevated PE and PIH risk in Lompopo, South Africa (where current active indoor use of DDT is common) [100], but not with higher serum DDT/DDE levels in a U.S. population sampled before the 1972 DDT ban [88], which may indicate greater baseline vulnerability among South African women as a result of underlying health disparities [92]. Placental OCP levels were associated with 10 times higher PE/eclampsia risk, although exclusion of values the below detection limit may have overestimated risk among the exposed group in that study [94]. Two studies suggested a possible protective association (adjusted OR = 0.3–0.5), including one report of a decreasing linear trend (p-trend ≤ 0.01) [88,93], while estimates trended below 1.0 but were not significant for several OCPs in another study [89]. Increased PE risk was associated with modeled pesticide exposure in three of five modeling studies (two of which reported significant findings) [95,96,99], while null and inverse associations were observed in the other two modeling studies, one of which modeled exposure to over 500 pesticides in 295,387 pregnant women in California [97,98]. Live-birth bias may have underestimated risk from pesticide-associated fetal loss; however, pesticide studies did not adjust for potential confounding from dietary intake associated with pesticide exposure, such as fruit or vegetable consumption, which may be protective factors that are independently associated with decreased PE risk [97].
Non-persistent Chemicals
We found nine total human observational studies that evaluated pregnancy-induced hypertensive disorders (including blood pressure) with non-persistent chemical exposures, six of which measured exposure in biological samples (i.e., urine, maternal serum, placenta) [101–106], while three modeled occupational exposures indirectly [86,87,99] (Table 3). Three studies on BPA and PE, including two nested case control studies (N=50 and N=74 PE cases) and one smaller cross-sectional study (N=23 PE cases), found increased PE risk associated with bisphenol A (BPA) levels in maternal urine and serum during early to mid-gestation and in placental tissue (but not maternal serum or cord blood) at delivery [101–103]. One of these included multiple urinary BPA measurements and suggested that early pregnancy (~ 10 weeks gestation) may be a window of susceptibility for BPA-associated PE risk [102]. However, results were not directly comparable due to differences in sampling matrix (urine vs serum or placenta) and timing of exposure assessment (repeated measures vs spot samples at mid-gestation or term) [101–103]. There were two studies on phthalates and PE/PIH risk (one case-control [102] and one prospective cohort [106]), both of which found increased risk associated with repeated urine measures across pregnancy, although findings for specific metabolites varied (DEHP metabolites in one [102]; MBzP in the other [106]). Differences in outcome definition (PE only [102] vs multiple PIH disorders [106]), method of urine dilution correction (i.e., specific gravity vs. creatinine), and confounding adjustment (e.g., pre-pregnancy vs. mid-gestation BMI, yes/no smoking vs. cotinine biomarker, etc.) may have contributed to the result discrepancies [102,106].
There were two prospective cohort studies that evaluated blood pressure and phenols (one of which included BPA). Consistent inverse associations were reported in one [104], while the direction of association depended on fetal sex in the other [105], with differences potentially explained by alternate measures of urine dilution (i.e., creatinine vs. specific gravity) and varied study locations (Europe vs. Asia) [104,105]. Diverging blood pressure associations (both increasing [106] and decreasing [104]) were also reported in two phthalate studies which differed by exposure level and confounding adjustment, with 3-fold lower urinary metabolite levels and dietary intake of processed foods evaluated in the latter study [104].
Additionally, two studies of cosmetologists and manicurists, who frequently use personal care products that contain phenols and phthalates (e.g., nail polish and fragranced lotion), found lower PE risk in workers compared to the general population but not compared to other working women (with increased PIH risk among cosmetologists compared to realtors reported in one study) [86,87]. The healthy worker effect may have underestimated worker risk when non-workers (who typically have worse underlying health status) were included in the comparison group [107]. No association was found with exposure modeled from a job task survey, but narrow exposure and outcome classification criteria resulting in low exposure and outcome prevalence may have decreased study power [99].
Heavy Metals/Metalloids
Lead exposure was associated with 10-fold increased PE risk in a recent meta-analysis [1]. Lead can induce hypertension and activate biological pathways that inhibit vasodilation and promote endothelial dysfunction, suggesting a possible mode of action for other metals to influence the PE disease pathway [1,108]. This review focused on 13 epidemiologic studies that evaluated cadmium, arsenic, and/or mercury, although several studies included lead (Table 3). Increased PE risk was associated with higher cadmium levels in six out of eight studies that varied by sample size, study population, and location [109–116]. Research on arsenic-associated PE risk was less extensive and more equivocal, which may be partially attributable to exposure level differences, as increased PE risk was associated with high arsenic levels in the Congo but not with five times lower arsenic levels in Mexico [109,115,117]. Studies also differed by sampling matrix, ranging from drinking water to urine, hair, and serum, as well as by confounding adjustment. For example, the Congo study excluded first time pregnancies [109], while other studies did not adjust for parity at all [115,117]. Two blood pressure studies reported increasing arsenic associations during mid-gestation (cross-sectional) and across pregnancy (prospective cohort), including evidence of a linear trend [118,119]. Higher mercury-associated PE risk was found in two studies with distinct designs (prospective cohort and case-control), study populations (occupational and non-occupational), and biological matrices (urine and blood), while diverging blood pressure associations depended on biomarker type (increasing with methyl and total mercury and decreasing with inorganic mercury) [115,120,121] in a cross-sectional study, although results were consistent with research among non-pregnant populations [121].
4.3. Gestational Diabetes Mellitus and Chemical Exposures
We found 24 studies that evaluated associations between chemical exposures and gestational diabetes mellitus (GDM) and/or gestational impaired glucose tolerance (IGT) (Table 4). Sample sizes ranged from around 200 to over 81,000 study participants, with 14 to 506 GDM cases (though most studies had fewer than 100 GDM or gestational IGT cases). Unlike PE studies, the majority of GDM studies utilized cohort rather than case-control study designs (60% cohort and 30% case-control studies for GDM compared to 30% cohort and 60% case-control studies for PE).
Table 4.
Epidemiologic studies of gestational diabetes mellitus (GDM) and chemical exposures in pregnant women (24)
| Persistent Organic Pollutants and Pesticides (12 Studies) | |||||||
| [89] | Prospective Cohort. | N=258, 28 GDM, 27 PIH. | 2005–2009. | Participation in Longitudinal Investigation of Fertility and the Environment Study (LIFE) study in 16 counties of Michigan and Texas, USA. | Measured maternal serum levels of 6 OCPs: HCB, β-HCH, p,p′-DDE, p,p′-DDT, oxychlordane, and trans-nonachlor; and 7 PBDE congeners: 28, 47, 85, 99, 100, 153, 154; soon before pregnancy (with detectable levels in >80% of subjects). | GDM, PIH. |
OCPs Ln HCB and GDM: Adjusted OR=0.97 (95% CI: 0.60–1.57) per SD increase in exposure. Ln β-HCH and GDM: Adjusted OR=0.34 (95% CI: 0.07–1.67) per SD increase in exposure. Ln oxychlordane and GDM: Adjusted OR=1.26 (95% CI: 0.76–2.08) per SD increase in exposure. Adjusted OR for oxychlordane was similar to that of p,p′-DDE, p,p′-DDT, and trans-Nonachlor, with adjusted OR ranging between 0.94–1.1 and 95% CI that crossed 1.0. PBDE congeners Ln PBDE-153 and GDM: Adjusted OR=1.79, (95% CI: 1.18–2.74) per SD increase in exposure. Ln PBDE-100 and GDM: Adjusted OR=2.22 (95% CI: 0.96–5.17) per SD increase in exposure. Ln PBDE-154 and GDM: Adjusted OR=1.04 (95% CI: 0.34–3.17) per SD increase in exposure. Ln PBDE-47 and GDM: Adjusted OR=0.32 (95% CI: 0.10–1.01) per SD increase in exposure. Adjusted OR for PBDE-28, 85, 99 was similar to PBDE-47, ranging between 0.44 and 0.71, with 95% confidence intervals that crossed 1.0. |
| [124] | Case-control. | N=140, 70 GDM. | 2013–2015. | Prenatal care patients at one of three hospitals in Tehran, Iran. | Measured maternal serum levels of 8 PBDE congeners: 28, 47, 99, 100, 153, 154, 183, and 209; and 10 PCB congeners: 28, 52, 74, 99, 101, 118, 138, 153, 180, and 187; once in 3rd trimester. |
GDM. |
Total POPs (sum of total PCBs and PBDEs) and GDM: Adjusted OR=1.61 (95% CI: 1.31–1.97, p-value <0.0001). Total PCBs and GDM: Adjusted OR=1.75 (95% CI: 1.35–2.27, p-value <0.0001). Total PBDEs and GDM: Adjusted OR=2.21 (95% CI: 1.48–3.30, p-value <0.0001). Individual PCB congeners Ln PCB 28 and GDM: Adjusted OR=0.30 (95% CI: 0.14–0.66, p-value=0.003). Ln PCB 187 and GDM: Adjusted OR=1.85 (95% CI: 1.16–2.94, p-value=0.01); and Ln PCB 118 and GDM: Adjusted OR=8.61 (95% CI: 2.80–26.48, p-value <0.0001). Ln PCB-153 and GDM: Adjusted OR=2.41 (95% CI: 1.21–4.81, p-value=0.01) Individual PBDE congeners Ln PBDE 99 and GDM: Adjusted OR=2.14 (95% CI: 1.99–3.83, p-value=0.01). Ln PBDE 28 and GDM: Adjusted OR=2.73 (95% CI: 1.22–6.11, p-value=0.02). Ln BDE-153 and GDM: Adjusted OR=1.81 (95% CI: 1.00–3.26, p-value=0.05). |
| [130] | Nested Case-control. | N=231, 77 GDM. | 2013–2015. | Prenatal care patients at Xicheng Maternal & Child Health Hospital in Beijing, China. | Measured maternal serum levels of 7 PBDE congeners: BDE-28, 47, 99, 100, 153, 154, 183; in the 1st trimester. | GDM. |
Single PBDE Model (Continuous) Ln BDE-28 and GDM: Adjusted OR=1.30 (95: CI: 0.89–1.91). Similar result for BDE-99. Ln BDE-47 and GDM: Adjusted OR=1.67 (95: CI: 1.00–2.77). Similar results for BDE-100, 154, and 183. Ln BDE-153 and GDM: Adjusted OR=4.04 (95: CI: 1.92–8.52). Single PBDE Model (Categorical) Ln BDE-28 and GDM: Adjusted OR=1.39 (95: CI: 0.59–3.28), 2.02 (95% CI: 0.86–4.70), 2.39 (95% CI: 1.03–5.57) for women in the 2nd, 3rd, and 4th PBDE exposure groups compared to the lowest exposure quartile (p-trend=0.05). Ln BDE-47 and GDM: Adjusted OR=1.28 (95% CI: 0.55, 2.98), 1.52 (95% CI: 0.66, 3.49), 2.01 (95% CI: 0.88, 4.60) for women in the 2nd, 3rd, and 4th PBDE exposure groups compared to the lowest exposure quartile (p-trend=0.09). Ln BDE-99 and GDM: Adjusted OR=1.29 (95% CI: 0.56, 3.00), 1.67 (95% CI: 0.73, 3.81), 2.01 (95% CI: 0.88, 4.58) for women in the 2nd, 3rd, and 4th PBDE exposure groups compared to the lowest exposure quartile (p-trend=0.08). Ln BDE-100 and GDM: Adjusted OR=0.97 (95% CI: 0.40, 2.35), 2.06 (95% CI: 0.90, 4.68), 2.04 (95% CI: 0.89, 4.70) for women in the 2nd, 3rd, and 4th PBDE exposure groups compared to the lowest exposure quartile (p-trend=0.03). Ln BDE-153 and GDM: Adjusted OR=1.43 (95% CI: 0.60–3.37), 1.36 (95% CI: 0.57–3.25), and 3.42 (95% CI: 1.49–7.89) for women in the 2nd, 3rd, and 4th PBDE exposure groups compared to the lowest exposure quartile (p-trend=0.01). Ln BDE-154 and GDM: Adjusted OR=1.37 (95% CI: 0.58–3.24), 2.67 (95% CI: 1.17–6.12), and 1.70 (95% CI: 0.73–3.99) for women in the 2nd, 3rd, and 4th PBDE exposure groups compared to the lowest exposure quartile (p-trend=0.18). Ln BDE-183 and GDM: Adjusted OR=1.30 (95% CI: 0.53–3.22), 2.15 (95% CI: 0.89–5.16), and 3.70 (95% CI: 1.58–8.65) for women in the 2nd, 3rd, and 4th exposure quartiles compared to the lowest exposure quartile (p-trend <0.01). Ln Total BDE and GDM: Adjusted OR=1.00 (95% CI: 0.43–2.34), 1.48 (95% CI: 0.65–3.37), and 2.23 (95% CI: 1.04–5.00) for women in the 2nd, 3rd, and 4th PBDE exposure groups compared to the lowest exposure quartile (p-trend=0.03). Multiple PBDE congener model Ln BDE-28 and GDM: Adjusted OR=1.09 (95: CI: 0.71–1.67). Similar result for BDE-100 and BDE-154. Ln BDE-47 and GDM: Adjusted OR=1.33 (95: CI: 0.55–3.21). Ln BDE-99 and GDM: Adjusted OR=0.71 (95: CI: 0.18–2.75). Ln BDE-153 and GDM: Adjusted OR=2.76 (95: CI: 1.07–7.11). Ln BDE-183 and GDM: Adjusted OR=1.56 (95: CI: 1.02–2.40). Tests for the trends in BDE-28, −100, −153, −183 and summed PBDE exposure were all statistically significant (p <0.05), non-monotonic patterns also observed for BDE-100 and −183. |
| [125] | Prospective Cohort. | N=939, 68 GDM. | 2007–2008. | Participation in Rhea Study at prefecture of Heraklion, Crete, Greece. | Measured maternal serum levels of 2 OCPs (HCB and DDE) and 6 PCB congeners: non-dioxin-like (153, 138, 170 180) and dioxin like (118 and 156); once in 1st trimester. | GDM. |
OCPs and GDM HCB and GDM: Adjusted OR=1.62 (95% CI: 0.67–3.95) and 1.21 (95% CI: 0.45–3.20) for women in medium and high tertiles of HCB exposure compared to women in the lowest exposure tertile. DDE and GDM: Adjusted OR=0.83 (95% CI: 0.38–1.82) and 0.65 (95% CI: 0.28–1.47) for women in the medium and high tertiles of exposure, compared to women in the lowest exposure tertile. Total PCB metrics and GDM Total PCBs and GDM: Adjusted OR=3.90 (95% CI: 1.37–11.06) and 3.60 (95% CI: 1.14–11.39) for women in the medium and high tertiles of PCB exposure, respectively, compared to women in the lowest tertile of PCB exposure. Dioxin-like PCBs and GDM: Adjusted OR=5.63 (95% CI: 1.81–17.51) and 4.71 (95% CI: 1.38–16.01) for women in the medium and high exposure tertiles, respectively, compared to women in the lowest exposure tertile. Non-dioxin-like PCBs and GDM: Adjusted OR=2.36 (95% CI: 0.89–6.23) and 2.26 (95% CI: 0.77–6.68) for women in the medium and high tertiles of non-dioxin-like PCB exposure groups, compared to women in the lowest tertile of PCB exposure group. |
| [126] | Nested Case-control. | N=231, 77 GDM. | 2013–2015. | Prenatal care patients at Xicheng Maternal and Child Care Hospital, Beijing, China. | Measured maternal serum levels of 6 non-dioxin-like PCB congeners: 28, 52, 101, 138, 153, and 180; in 1st trimester. | GDM, Glucose Homeostasis. |
PCB summary metrics Ln Low chlorinated PCBs (ΣPCB-28,−52,−101) and GDM: Unadjusted OR=2.28 (95% CI: 1.25–4.17). Dose response observed in cubic spline graphs. Ln High chlorinated PCBs (ΣPCB-138,−153 −180) and GDM: Unadjusted OR=1.45 (95% CI: 0.87–2.42). Ln Total ΣPCB (six congeners) and GDM: Unadjusted OR=4.70 (95% CI: 1.02–21.7). Individual PCB congeners Ln PCB-28 and GDM: Unadjusted OR=1.86 (95% CI: 1.05–3.27). Similar result for PCB-52 and PCB-101. Ln PCB-138 and GDM: Unadjusted OR=1.51 (95% CI: 0.90–2.53). Similar result for PCB-153 and PCB-180. PCB-52 and GDM: Adjusted OR=1.97 (95% CI: 1.27–3.07), with evidence of a dose response relationship. Note: PCB-52 was the only congener that remained significant in adjusted models and the only for which adjusted results were reported. Similar findings observed for PCB-52 and glucose homeostasis. |
| [134] | Prospective Cohort. | N=604, 49 GDM. | 1997–2000. | Delivery at National Hospital in Torshavn, Faroe Islands. | Measured maternal serum levels of 3 PCB congeners: 138, 153, 180; DDT/DDE; and 5 PFAS: PFOS, PFOA, PFHxS, PFDA, and PFNA; at 34 weeks gestation; and hair and cord blood levels of mercury at delivery. | GDM. |
Serum Ln ΣPCB and GDM: Adjusted OR=0.97 (95% CI: 0.71, 1.33) per doubling of exposure and. When modeled as three categories: Adjusted OR=1.08 (95% CI: 0.49, 2.39) and 1.26 (95% CI: 0.57–2.75). Serum Ln DDE and GDM: Adjusted OR=1.29 (95% CI: 0.94, 1.77) per doubling of exposure. Adjusted OR=1.17 (95% CI: 0.44–3.09) and 1.89 (95% CI: 0.75–4.76) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. Serum Ln PFOS and GDM: Adjusted OR=0.86 (95% CI: 0.43–1.70) per doubling of exposure. Adjusted OR=0.85 (95% CI: 0.43–1.70) and 0.56 (95% CI: 0.26–1.19) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. Serum Ln PFOA and GDM: Adjusted OR=0.79 (95% CI: 0.44–1.41) per doubling of exposure. Adjusted OR=1.01 (95% CI: 0.50–2.06) and 0.66 (95% CI: 0.30–1.48) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. Serum Ln PFHxS and GDM: Adjusted OR=1.03 (95% CI: 0.80–1.33) per doubling of exposure. Adjusted OR=0.98 (95% CI: 0.47–2.05) and 1.00 (95% CI: 0.48–2.07) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. Serum Ln PFDA and GDM: Adjusted OR=1.20 (95% CI: 0.73–1.96) per doubling of exposure. Adjusted OR=1.97 (95% CI: 0.94–4.12) and 1.02 (95% CI: 0.45–2.30) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. Serum Ln PFNA and GDM: Adjusted OR=0.88 (95% CI: 0.53–1.47) per doubling of exposure. Adjusted OR=0.62 (95% CI: 0.30–1.30) and 0.65 (95% CI: 0.31–1.36) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. Hair mercury and GDM: Adjusted OR=0.79 (95% CI: 0.62–0.99) per doubling of exposure. Adjusted OR=0.92 (95% CI: 0.44–1.90) and 0.73 (95% CI: 0.34–1.59) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. Cord blood mercury and GDM: Adjusted OR=0.87 (95% CI: 0.66–1.15) per doubling of exposure. Adjusted OR=1.08 (95% CI: 0.52–2.26) and 0.73 (95% CI: 0.33–1.62) for women in the 2nd and 3rd exposure group compared to women in the lowest exposure group. In the multiple pollutant adjusted structural equation models (SEMs), only the positive association between OC exposure (which included ΣPCB and DDT/DDE) and GDM remained significant (change in GDM probit per doubling of OC exposure = 0.45, 95% CI: 0.05–0.86). |
| [127] | Prospective Cohort. | N=1274, 48 GDM, 59 IGT. | 2008–2011. | Participation in Maternal-Infant Research on Environmental Chemicals (MIREC) study from 10 sites in six Canadian provinces, Canada. | Measured urine levels of 3 OP pesticide metabolites: diethyl-, dimethyl-, and dimethylthio-phosphate (DEP, DMP, and DMTP, respectively); plasma levels of 3 OCPs: p,p′-DDE, oxychlordane, and trans-nonachlor; 3 PFAS: PFOA, PFOS, and PFHxS; and 4 PCB congeners: 118, 138, 153, 180; once during 1st trimester (with detectable levels in >75% of subjects). | GDM, IGT. |
OP pesticide metabolites and GDM: Except for comparing the 3rd and the 4th to the lowest quartile of DMP exposure [adjusted OR=0.2 (95% CI: 0.1–0.7) and 0.3 (95% CI: 0.1–0.8) respectively], comparing the 4th to the lowest quartile of DMTP exposure [0.3 (95% CI: 0.1–0.9)], and comparing the 4th to the lowest quartile of dimethyl OP metabolites (DMP and DMTP) exposure [0.3 (95% CI: 0.1–0.8)], no statistically significant associations comparing higher exposure to the lowest exposure quartile were reported. Significant trend associations were found for DMP, DMTP, and DMP/DMTP OP metabolites. OP pesticide metabolites and IGT: Except for comparing the 3rd to the lowest quartile of DEP exposure [adjusted OR=0.2 (95% CI: 0.1–0.6)], no statistically significant associations comparing higher exposure to the lowest exposure quartile were reported. Significant trend association was found for DMP. OP pesticide metabolites and GDM/IGT: Except for comparing the 3rd to the lowest quartile of DEP exposure [adjusted OR=0.4 (95% CI: 0.2–0.9)], the 3rd and the 4th to the lowest quartile of DMP exposure [adjusted OR=0.2 (95% CI: 0.1–0.7) and 0.3 (95% CI: 0.1–0.8) respectively], the 4th to the lowest quartile of DMTP exposure [0.3 (95% CI: 0.1–0.9)], and the 3rd and 4th to the lowest quartile of dimethyl OP metabolites (DMP and DMTP) exposure [0.5 (95% CI: 0.3–0.9) and 0.5 (95% CI: 0.2–0.9)], no statistically significant associations comparing higher exposure to the lowest exposure quartile were reported. Significant trend associations were found for DMP, DMTP, and DMP/DMTP OP metabolites. OCPs and GDM: Adjusted ORs ranging from 0.5–1.4, with 95% CI that crossed 1.0]. OCPs and IGT: Adjusted ORs ranged from 0.6–1.0, with confidence intervals that crossed 1.0. OCPs and GDM/IGT: No significant associations were reported [adjusted OR ranging from 0.6 to 1.0, with confidence intervals that crossed 1.0]. PCBs and GDM: No significant associations reported between GDM and individual PCBs, sum of all PCBs, and sum of non-dioxin-like PCBs [adjusted OR ranging from 0.7 to 1.9, with confidence intervals that crossed 1.0]. PCBs and IGT: No significant associations were reported between GDM and individual PCBs, sum of all PCBs, and sum of non-dioxin-like PCBs [adjusted OR ranging from 0.4 to 0.9, with confidence intervals that crossed 1.0]. PCBs and GDM/IGT: No significant associations were reported between GDM and individual PCBs, sum of all PCBs, and sum of non-dioxin-like PCBs [adjusted OR ranging from 0.5 to 1.1, with confidence intervals that crossed 1.0]. PFAS and GDM: Adjusted ORs ranging from 0.6 to 1.6, with confidence intervals that crossed 1.0. PFAS and IGT: Except for comparing the 2nd to the lowest quartile of PFHxS exposure [adjusted OR=3.5 (95% CI: 1.4–8.9)], no statistically significant associations comparing higher exposure to the lowest exposure quartile were reported. PFAS and GDM/IGT: Except for comparing the 2nd to the lowest quartile of PFHxS exposure [adjusted OR=2.4 (95% CI: 1.3–4.4)], no statistically significant associations comparing higher exposure to the lowest exposure quartile were reported. |
| [129] | Prospective Cohort. | N=258, 28 GDM. | 2005–2007. | Participation in Longitudinal Investigation of Fertility and the Environment (LIFE) Study and residence in sixteen counties in Michigan and Texas, USA. | Measured maternal serum levels of PBB-153 and 36 PCBs: PCB 28, 44, 66, 74, 99, 101, 105, 110, 114, 118, 146, 157, 170, 177, 183, 197, 195, 196, 201, 206, and 209); once soon before pregnancy. | GDM. |
Individual congeners PCB 28 and GDM: Adjusted OR=0.90 (95% CI: 0.24–3.31). Results for PCB 44, 66, 74, 99, 101, 105, 110, 114, 118, 146, 157, 170, 177, 183, 197, 195, 196, 201, 206, and 209 were similar, with adjusted OR’s between 0.46–0.96 and confidence intervals that contained 1.0. PCB-101 and GDM: Adjusted OR=1.0 (95% CI: 0.69–1.47) PCB-170 and GDM: Adjusted OR=0.4 (95% CI: 0.18–0.88). Results for PCB 138, 153, 156, 167, 172, 180, and 194 were similar, with adjusted OR’s between 0.42–0.53 and confidence intervals that were less than 1.0. PBB-153 and GDM: Adjusted OR=0.68 (95% CI: 0.31–1.49). Congener sums Dioxin-like PCBs and GDM: Adjusted OR=0.65 (95% CI: 0.37–1.15). Non-dioxin-like PCBs and GDM: Adjusted OR=0.37 (95% CI: 0.13–1.04). |
| [133] | Retrospective Cohort. | N=11,273, 506 GDM. | 1993–1997. | Licensed pesticide applicators and spouses enrolled in Agricultural Health Study (AHS), Iowa and North Carolina, USA. | Modeled pesticide exposure from self-reported activity in 1 st trimester as four ordered categories: 1) No exposure; 2) Indirect exposure (planting, pruning, weeding, picking, harvesting); 3) Residential exposure (use in garden or home); and 4) Agricultural exposure (mixing, applying, repairing equipment). | GDM. |
Pesticides and GDM: Adjusted OR=0.9 (95% CI: 0.7–1.1), 1.0 (95% CI: 0.8–1.3), and 2.2 (95% CI: 1.5–3.3) for women in the 2nd (indirect), 3rd (residential), and 4th (agricultural) exposure groups compared to women in the 1st (non-exposed) group. Elevated GDM associated with ever-use of four herbicides (2,4,5-T; 2,4,5-TP; atrazine, and butylate), two OP insecticides (diazinon and phorate), and one carbamate insecticide (carbofuran) among women in the agricultural exposure group (specific values not reported). |
| [93] | Prospective Cohort. | N=779, 71 GDM. | 2004–2007. | Participation in prospective mother-child cohort study, Timoun, Guadeloupe. | Measured plasma levels of chlordecone in 3rd trimester (DDE and PCB-153 analyzed as potential confounders in a subset of samples). | GDM, PE, PIH. |
Log10 Chlordecone and GDM: Adjusted OR=0.7 (95% CI: 0.5–1.1). When modeled as quartiles: Adjusted OR=1.1 (95% CI: 0.6–2.2), 0.5 (95% CI: 0.2–1.1), and 0.7 (95% CI: 0.3–1.5) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to women in the lowest exposure quartile. |
| [132] | Prospective Cohort. | N=1240, 53 GDM, 137 IGT. | 2003–2008. | Participation in Spanish INMA [Environment and Childhood Project (INfancia y Medio Ambiente)] birth cohort, Spanish regions of Valencia, Sabadell, and Gipuzkoa, Spain. | Measured maternal plasma levels of 4 PFAS: PFOS, PFHxS, PFNA, and PFOA; once in 1st trimester. | GDM, IGT. |
Log10 PFOA and GDM: Adjusted OR=1.20 (0.62–2.30). Similar result when exposure modeled categorically and for Log10 PFOA and IGT. PFOA and total cholesterol: %Difference=1.26% (95% CI: 0.01%–2.54%) per log10-unit increase. Log10 PFOS and GDM: Adjusted OR=2.40 (0.93–6.18). When exposure was modeled as four categories: Adjusted OR=1.89 (0.77–4.64), 1.54 (0.61–3.87), and 2.07 (0.85–5.01). Log10 PFOS and IGT: Adjusted OR=1.99 (95% CI: 1.06–3.78). Adjusted OR=2.11 (1.13–3.94), 2.08 (1.12–3.86), and 2.22 (1.19–4.13). PFOS and triglyceride: %Difference=−5:86 (95% CI: −9:91%–1:63%) per log10-unit increase. Log10 PFHxS and GDM: Adjusted OR=1.58 (0.73–3.44). When exposure was modeled as four categories: Adjusted OR=1.25 (0.51–3.03), 1.81 (0.76–4.28), and 1.15 (0.42–3.12). Log10 PFHxS and IGT: 1.65 (0.99–2.76). Adjusted OR=1.51 (0.76–3.02), 1.99 (1.01–3.90), and 1.72 (0.85–3.49). Log10 PFNA and GDM: Adjusted OR=0.85 (0.40–1.80). OR=1.01 (0.62–2.23), 1.27 (0.59–2.73), and 0.70 (0.28–1.75). Similar result for Log10 PFNA and IGT. PFNA and triglyceride: %Difference=−4:75% (95% CI: −8:16%–−0.61%) per log10-unit increase. |
| [131] | Prospective Cohort. | N=272, 28 GDM. | 2005–2009. | Participation in Longitudinal Investigation of Fertility and the Environment (LIFE) Study in 16 counties of Michigan and Texas, USA. | Measured maternal serum levels of 7 PFAS: PFOA, PFOS, PFOSA, PFNA, PFDeA, Me-PFOSA-AcOH, Et-PFOSA-AcOH; soon before pregnancy. | GDM. |
Ln PFOA and GDM: Adjusted OR=1.85 (95% CI: 1.15–2.98) per SD increment. Ln PFOS and GDM: Adjusted OR=1.16 (95% CI: 0.77–1.76) per SD increment. Similar results for Ln PFOSA, Ln PFNA, Ln PFDeA, Ln Me-PFOSA-AcOH, and Ln Et-PFOSA-AcOH. |
| Non-persistent Chemicals (5 Studies) | |||||||
| [136] | Case-control. | N=94, 22 GDM. | 2009–2010. | Prenatal care patients at University of Oklahoma Medical Center Women’s and High Risk Pregnancy clinics, Oklahoma City, Oklahoma, USA. | Measured urine levels of total BPA (free BPA and conjugate) in banked samples at 27 weeks gestation. | GDM, Blood Glucose. | BPA and GDM: Adjusted OR=0.58 (95% CI: 0.18–1.19) and 0.37 (95% CI: 0.09–1.60) for women in the 2nd and 3rd tertiles of BPA exposure compared to women in the lowest exposure tertile. Note: There was no association between BPA and blood glucose levels, but the values were not reported. |
| [138] | Prospective Cohort. | N=1274, 48 GDM, 59 IGT. | 2008–2011. | Participation in Maternal-Infant Research on Environmental Chemicals (MIREC) study at 10 sites in six provinces, Canada. | Measured urine levels of total BPA and 11 phthalate metabolites: MEP, MnBP, MBzP, MCPP, DEHP metabolites; and blood levels of 4 metals: lead, cadmium, mercury, and arsenic; once in 1st trimester. | GDM, IGT. |
MEP: Adjusted OR (95% CI) GDM: Adjusted OR=0.7 (95% CI: 0.3–1.8), p-value=0.25; IGT: 1.5 (95% CI: 0.6–3.8), p-value=0.72; GDM or IGT: 1.0 (95% CI: 0.5–2.0), p-value=0.29. GDM: Adjusted OR=0.8 (0.3–2.1); IGT: 0.8 (0.3–2.4); GDM or IGT: 0.8 (0.4–1.7). GDM: Adjusted OR=0.5 (0.2–1.4), IGT: 1.0 (0.4–3.0), GDM or IGT: 0.7 (0.3–1.5). MBP: Adjusted OR (95% CI) GDM: 1.7 (0.6–4.4), IGT: 1.9 (0.7–5.2), GDM or IGT 1.8 (0.9–3.6) GDM: 1.0 (0.3–3.2), IGT: 1.7 (0.5–5.4), GDM or IGT 1.3 (0.6–3.0) GDM: 0.6 (0.1–2.2), IGT: 1.2 (0.3–4.6), GDM or IGT 0.8 (0.3–2.2) p-Value c GDM: 0.29, IGT: 0.95, GDM or IGT 0.51 MBzP: Adjusted OR (95% CI) GDM: 0.7 (0.2–2.2), IGT: 2.3 (0.8–7.2), GDM or IGT 1.3 (0.6–2.8) GDM: 1.5 (0.6–4.2), IGT: 2.9 (0.9–9.4), GDM or IGT 2.0 (0.9–4.4) GDM: 1.5 (0.5–4.7), IGT: 2.9 (0.8–10.4), GDM or IGT 2.0 (0.9–4.8) p-Value c GDM: 0.28, IGT: 0.13, GDM or IGT 0.07 MCPP: Adjusted OR (95% CI GDM: 1.2 (0.5–2.9), IGT: 1.8 (0.7–4.5), GDM or IGT 1.5 (0.7–2.8) GDM: 0.6 (0.2–1.8), IGT: 0.5 (0.1–1.8), GDM or IGT 0.6 (0.2–1.3) GDM: 0.6 (0.2–1.9), IGT: 1.6 (0.5–4.8), GDM or IGT 1.0 (0.4–2.3) p-Value c GDM: 0.27, IGT: 0.70, GDM or IGT 0.63 ΣDEHP: Adjusted OR (95% CI GDM: 1.0 (0.4–2.5), IGT: 1.1 (0.4–2.8), GDM or IGT 1.0 (0.5–2.0) GDM: 0.4 (0.1–1.5), IGT: 0.9 (0.3–2.7), GDM or IGT 0.6 (0.3–1.5) GDM: 0.9 (0.3–2.9), IGT: 1.0 (0.3–3.4), GDM or IGT 0.9 (0.4–2.3) p-Value c GDM: 0.72, IGT: 0.91 0.75 BPA: Adjusted OR (95% CI GDM: 1.8 (0.7–4.5), IGT: 1.2 (0.5–2.9), GDM or IGT 1.5 (0.8–2.9) GDM: 1.5 (0.5–4.5), IGT: 0.6 (0.2–1.7), GDM or IGT 0.9 (0.4–2.0) GDM: 1.1 (0.3–3.6), IGT: 1.3 (0.5–3.6), GDM or IGT 1.2 (0.5–2.7) p-Value c GDM: 0.99, IGT: 0.79, GDM or IGT 0.92 |
| [137] | Prospective Cohort. | N=1795,42 GDM, 43 IGT. | 2008–2011. | Participation in Maternal-Infant Research on Environmental Chemicals (MIREC) study at 10 sites in six provinces, Canada. | Measured urine levels of triclosan in 1st trimester. | GDM, IGT, Other complications. |
Ln Triclosan and GDM: Adjusted OR=1.7 (95% CI: 0.7–4.2), 0.9 (95% CI: 0.3–2.5), and 0.9 (95% CI: 0.4–2.5) for women in the 2nd, 3rd, and 4th exposure quartiles compared to women in the lowest exposure quartile (p-trend=0.54). Ln Triclosan and IGT: Adjusted OR=0.3 (95% CI: 0.1–1.0), 0.5 (95% CI: 0.2–1.3), and 0.7 (95% CI: 0.3–1.5) for women in the 2nd, 3rd, and 4th exposure quartiles compared to women in the lowest exposure quartile (p-trend=0.55). Ln Triclosan and GDM or IGT: Adjusted OR=0.8 (95% CI: 0.4–1.5), 0.7 (95% CI: 0.3–1.3), and 0.8 (95% CI: 0.4–1.5) for women in the 2nd, 3rd, and 4th exposure quartiles compared to women in the lowest exposure quartile (p-trend=0.40). |
| [135] | Retrospective Nested Case-control. | N=232, 47 GDM. | 2001–2009. | Male pregnancy and participation in Cambridge Baby Growth Study (CBGS), Rosie Maternity Unit, Cambridge, United Kingdom. | Measured maternal serum levels of 3 phenols: BPA, triclosan, and BP-3; and 6 phthalate metabolites: MEP, MiBP, MnBP, MEHP, MECPP, and MCiOP; once at 10–17 weeks gestation (detected in > 60% of samples). | GDM, Glucose Homeostasis. |
Ln BPA and Incident GDM: Adjusted OR=1.16 (95% CI: 0.48–2.78, p-value=0.74). When exposure was modeled in quartiles: Adjusted OR=2.58 (95% CI: 0.84–7.94), 1.04 (95% CI: 0.31–3.53), and 0.56 (95% CI: 0.14–2.28) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.07, p-trend=0.24). Ln Triclosan and GDM: Adjusted OR=0.54 (95% CI: 0.34–0.86, p-value=0.010). When exposure was modeled in quartiles: Adjusted OR=0.25 (95% CI: 0.07–0.86), 0.12 (95% CI: 0.03–0.55), and 0.35 (95% CI: 0.12–0.98) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.009, p-trend=0.022). BP-3 and Incident GDM: Adjusted OR=0.80 (95% CI: 0.44–1.44, p-value=0.45). Adjusted OR (95% CI: 95% CI), a Referent 1.09 (95% CI: 0.38–3.14), 1.40 (95% CI: 0.52–3.77), and 0.86 (95% CI: 0.29–2.51) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.83, p-trend=0.95). Ln MEP and Incident GDM: Adjusted OR=0.81 (95% CI: 0.39–1.70, p-value= 0.58). When exposure was modeled in quartiles: Adjusted OR=1.65 (95% CI: 0.60–4.56), 0.67 (95% CI: 0.21–2.07), and 1.19 (95% CI: 0.42–3.37) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.45,-trend=0.87). Ln MiBP and Incident GDM: Adjusted OR=1.48 (95% CI: 0.51–4.34, p-value=0.47). When exposure was modeled in quartiles: Adjusted OR=5.69 (95% CI: 1.56–20.73), 0.37 (95% CI: 0.06–2.26), and 4.89 (95% CI: 1.32–18.14) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (phet = 0.001, p-trend = 0.41).. Ln MnBP and Incident GDM: Adjusted OR=1.55 (95% CI: 0.45–5.33, p-value=0.49). When exposure was modeled in quartiles: Adjusted OR=1.17 (95% CI: 0.40–3.41), 0.43 (95% CI: 0.13–1.44), and 1.42 (95% CI: 0.52–3.88) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.26, p-trend=0.81). Ln MEHP and Incident GDM: Adjusted OR=0.93 (95% CI: 0.66–1.31, p-value=0.67). When exposure was modeled in quartiles: Adjusted OR=2.14 (95% CI: 0.72–6.35), 1.14 (95% CI: 0.42–3.09), and 1.03 (95% CI: 0.38–2.79) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.53, p-trend=0.77). Ln MECPP and Incident GDM: Adjusted OR=0.75 (95% CI: 0.27–2.06, p-value= 0.57). When exposure was modeled in quartiles: Adjusted OR=0.61 (95% CI: 0.20–1.81), 0.42 (95% CI: 0.13–1.36), and 1.19 (95% CI: 0.44–3.17) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.29, p-trend=0.78). Ln MCiOP and Incident GDM: Adjusted OR=1.12 (95% CI: 0.47–2.66, p-value= 0.81). When exposure was modeled in quartiles: Adjusted OR=1.54 (95% CI: 0.53–4.52), 1.18 (95% CI: 0.38–3.67), and 1.39 (95% CI: 0.47–4.14) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-het=0.87, p-trend=0.89). Note: Among women without GDM, first-trimester MEHP levels were positively associated with 120-min plasma glucose (adjusted β = 0.268 and 0.183, p-value = 0.0002 and 0.010, respectively) in mid-pregnancy. |
| [146]) | Retrospective Case-control. | N=81,205, 119 GDM (mani), 299 GDM (cosmet). | 1996–2009. | Licensed cosmetologists and manicurists in California, USA. | Modeled non-persistent chemicals in beauty products using California cosmetology license (hair and nail care services) and/or manicurist license during 1996–2006 as proxies for occupational exposure. | GDM, PE, Other complications. |
Compared to other working women Manicurist and GDM: Adjusted OR=1.19 (95% CI: 0.93–1.51). Restricted to Vietnamese manicurists: Adjusted OR=1.18 (95% CI: 0.47–2.97). Cosmetologist and GDM: Adjusted OR=1.14 (95% CI: 0.94–1.39). Restricted to Vietnamese cosmetologists: Adjusted OR=1.11 (95% CI: 0.43–2.86). Compared to the general population Manicurist and GDM: Adjusted OR=1.28 (95% CI: 1.10–1.50). Restricted to Vietnamese manicurists: Adjusted OR=1.59 (95% CI: 1.20–2.11). Cosmetologist and GDM: Adjusted OR=1.19 (95% CI: 1.07–1.33). Restricted to Vietnamese cosmetologists: Adjusted OR=1.49 (95% CI: 1.04–2.11). |
| Heavy Metals/Metalloids (7 Studies) | |||||||
| [139] | Cross-sectional. | N=532. | 2002–2008. | Participation in prospective birth cohort and residence near Tar Creek Superfund site, Ottawa County, Oklahoma, USA. | Measured maternal blood and hair levels of arsenic, once at delivery. | IGT. |
Arsenic and IGT (Blood): Adjusted OR=1.65 (95% CI: 1.52–1.79) per IQR increase in blood arsenic levels. When exposure was modeled in quartiles: Adjusted OR=1.02 (95% CI: 0.39–2.69), 2.65 (95% CI: 1.12–6.36), and 2.79 (95% CI: 1.13–6.87) for women in the 2nd, 3rd, and 4th arsenic exposure groups compared to the lowest exposure quartile (p-trend=0.008). Arsenic and IGT (Hair): Adjusted OR=2.32 (95% CI: 0.52–10.39) per IQR increase in hair arsenic levels. When exposure was modeled in quartiles: Adjusted OR=3.97 (95% CI: 0.62–25.37). 5.77 (95% CI: 0.98–33.88), and 4.20 (95% CI: 0.74–23.86) for women in the 2nd, 3rd, and 4th exposure quartiles compared to the lowest exposure quartile (p-trend=0.40). |
| [143] | Retrospective Nested Case-control. | N=327, 137 GDM. | 2012. | Patients who delivered at hospital in Xiamen, China. | Measured meconium levels of 4 metals: arsenic, cadmium, lead, and mercury; 1–2 days after delivery. | GDM. |
Arsenic and GDM: Adjusted OR=3.28 (95% CI: 1.24–8.71, p-value=0.017), 3.35 (95% CI: 1.28–8.75, p-value=0.014), and 5.25 (95% CI: 1.99–13.86, p-value=0.001) for women in the 2nd, 3rd, and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile (p-trend <0.001). Mercury and GDM: Adjusted OR=1.68 (95% CI: 0.72–3.89, p-value=0.228), 1.69 (95% CI: 0.72–3.96, p-value=0.226), and 1.75 (95% CI: 0.76–4.03, p-value=0.185) for women in the 2nd, 3rd, and 4th exposure groups, respectively, compared to the lowest exposure quartile (p-trend =0.004). Lead and GDM: Adjusted OR=0.37 (95% CI: 0.16–0.86, p-value=0.020), 0.16 (95% CI: 0.06–0.44, p-value <0.001), and 0.90 (95% CI: 0.46–1.78, p=value=0.772) for women in the 2nd, 3rd, and 4th exposure groups, respectively, compared to the lowest exposure quartile (p-trend=0.498). Chromium and GDM: Adjusted OR=1.74 (95% CI: 0.51–5.96, p-value=0.377), 1.65 (95% CI: 0.45–6.10, p-value=0.450), and 4.48 (95% CI: 1.40–14.31, p-value=0.011) for women in the 2nd, 3rd, and 4th exposure groups, respectively, compared to the lowest exposure quartile (p-trend=0.002). Cadmium and GDM: 3.07 (95% CI: 0.69–13.74, p-value <0.001), 16.87 (95% CI: 4.19–67.86, p-value <0.001), and 11.95 (95% CI: 2.97–48.04, p-value=0.142) for women in the 2nd, 3rd, and 4th exposure groups, respectively, compared to the lowest exposure quartile (p-trend <0.001). |
| [140] | Prospective Cohort. | N=1151, 14 GDM, 105 IGT. | 2009–2016. | Use of private well in household and participation in New Hampshire Birth Cohort Study, New Hampshire, USA. | Measured urine levels of total arsenic (iAs), metabolites [monomethylarsonic acid (MMA) and dimethylarsinic acid (DMA)], and methylation ratios (MMA/iAs and DMA/MMA) (once at 24–28 weeks gestation); toenail clippings (at 2 weeks postpartum); and home well water (once during pregnancy). | GDM, IGT. |
Arsenic and GDM Water: Adjusted OR=1.1 (95% CI: 1.0–1.2). Urine: Adjusted OR= 0.8 (95% CI: 0.3–2.4). Toenail: Adjusted OR= 4.5 (95% CI: 1.2–6.6). Arsenic and combined IGT and GDM Water: Adjusted OR=1.0 (95% CI: 0.9–1.1). Urine: Adjusted OR=1.0 (95% CI: 1.0–1.1). Toenail: Adjusted OR=0.9 (95% CI: 0.7–1.3). Arsenic and IGT Water: Adjusted OR=1.0 (95% CI: 0.9–1.1). Urinary: Adjusted OR=1.0 (95% CI: 1.0–1.1). Toenail: Adjusted OR=0.9 (95% CI: 0.6–1.3). |
| [138] | Prospective Cohort. | N=1274, 289 GDM, 59 IGT. | 2008–2011. | Participation in Maternal-Infant Research on Environmental Chemicals (MIREC) study at 10 sites in six provinces, Canada. | Measured blood levels of 4 metals: lead, cadmium, mercury, and arsenic; and urine levels of total BPA and 11 phthalates; once in 1st trimester. | GDM, IGT. |
Arsenic and GDM: Adjusted OR=0.7 (95% CI: 0.2–2.3), 2.5 (95% CI: 0.9–6.9), and 3.7 (95% CI: 1.4–9.6) for women in the 2nd, 3rd and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile (p-trend <0.01). Dose-response in cubic-spline model (p <0.01); test of linear null hypothesis (p-value=0.92). Arsenic and IGT: Adjusted OR=0.8 (95% CI: 0.4–1.8), 0.8 (95% CI: 0.3–1.9), and 1.2 (95% CI: 0.5–2.6) for women in the 2nd, 3rd and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile. Arsenic and combined GDM or IGT: Adjusted OR=0.8 (95% CI: 0.4–1.5), 1.3 (95% CI: 0.7–2.5), and 1.9 (95% CI: 1.1–3.5) for women in the 2nd, 3rd and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile (p-trend=0.01). Dose-response in cubic-spline model (p <0.03); test of linear null hypothesis (p-value=0.09). Cadmium and GDM: Adjusted OR=2.5 (95% CI: 1.0–6.4) for women in the highest cadmium exposure group compared to the lowest exposure quartile. |
| [141] | Semi-ecological. | N=5053, 268 GDM. | 2003, 2006, 2010. | Delivery at Clermont-Ferrand University Hospital in Auvergne, France. | Measured tap water levels of arsenic from routine testing of water supply units during 12-month period before birth. | GDM. | Arsenic and GDM: Adjusted OR=1.62 (95% CI: 1.01–2.53) for women in the high arsenic exposure group (≥ 10 μg/L) compared to the low arsenic exposure group (< 10 μg/L). When exposure was considered in three categories: Adjusted OR=1.43 (95% CI: 0.85–2.29) and 6.24 (95% CI: 1.64–19.49) for women in the 2nd and 3rd arsenic exposure groups (10–30 μg/L and ≥ 30 μg/L, respectively) compared to the lowest arsenic exposure group (< 10 μg/L). |
| [142] | Cross-sectional. | N=244, 21 GDM. | 2013–2014. | Patients at primary health centers in Arica, Chile. | Measured urine levels of inorganic arsenic once in 2nd trimester. | GDM. | Arsenic and GDM: Adjusted OR=2.98 (95% CI: 0.87–10.18) and 1.07 (95% CI: 0.26–4.33) for women in the 2nd and 3rd arsenic exposure groups, respectively, compared to the lowest tertile of exposure. |
| [147] | Prospective Cohort. | N=3260, 419 GDM. | 2013–2014. | Participation in Ma’anshan Birth Cohort Study in Anhui Province, China. | Measured blood levels of arsenic twice in 1st and 2nd trimesters, and cord blood levels once at delivery (3rd trimester). | GDM. |
Arsenic and GDM (1st
trimester): Adjusted OR=1.29 (95% CI: 0.92–1.82), 1.32 (95% CI: 0.94–1.85), and 1.71 (95% CI: 1.23–2.38) for women in the 2nd, 3rd, and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile. Incident GDM=12.53, 12.41, and 15.75 for women in the 2nd, 3rd, and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile (p-trend=0.001). Arsenic and GDM (2nd trimester): Adjusted OR=0.96 (95% CI: 0.71–1.31), 0.97 (95% CI: 0.71–1.32), and 0.89 (95% CI: 0.65–1.22) for women in the 2nd, 3rd, and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile. Incident GDM=13.82, 13.06, and 11.76 for women in the 2nd, 3rd, and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile (p-trend=0.211). Arsenic and GDM (3rd trimester): Adjusted OR=0.96 (95% CI: 0.67–1.37), 1.12 (95% CI: 0.79–1.58), and 1.39 (95% CI: 0.99–1.93) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile. Incident GDM=11.11, 12.52, and 14.73 for women in the 2nd, 3rd, and 4th arsenic exposure groups, respectively, compared to the lowest exposure quartile (p-trend=0.041). |
| [145] | Restrospectiv e Cohort. | N=6837. | 2012–2014. | Delivery at Wuhan Women and Children Medical Care Center in Wuhan, China. | Measured urine levels of cadmium (arsenic and chromium as potential confounders); once at delivery. | GDM. | Ln Cd and GDM: Adjusted RR=1.16 (95% CI: 1.03–1.33). When exposure was considered in four categories: Adjusted RR=1.21 (95% CI: 0.97–1.50), 1.24 (95% CI: 1.00–1.53), and 1.30 (95% CI: 1.05–1.61) for women in the 2nd, 3rd, and 4th exposure quartiles, respectively, compared to the lowest exposure quartile (p-trend <0.05). |
BPA = Bisphenol A; BP-3 = Benzophenone-3; CI = Confidence Interval; DDE = Dichlorodiphenyldichloroethylene; DDT = Dichlorodiphenyltricloroethane; Di-2-ethylhexyl phthalate metabolites (ΣDEHP = MEHHP, MECPP, MEOHP, and MEHP); HR = Hazard Ratio; HCB = Hexachlorobenzene; HCH = β-Hexachlorocyclohexane; IQR = Interquartile range; MnBP = Mono-n-butyl phthalate; MCiOP = Mono(carboxyisooctyl) phthalate; MCPP = Mono (3-carboxypropyl) phthalate; MECPP = Mono-(2-ethyl-5-carboxypentyl) phthalate; MEHP = Mono-(2-ethylhexyl) phthalate; MEP = Monoethyl phthalate; MiBP = Mono-isobutyl phthalate; OR = Odds Ratio; OCP = Organochlorine Pesticide; PFAS = Perfluoroalkyl substances; PFDeA = Perfluorodecanoic acid; PFHxS = Perfluorohexane sulfonate; PFNA = Perfluorononanoic acid; PFOSA = Perfluorooctane sulfonamide; PFOS = Perfluorooctane sulfonic acid; PFOA = Perfluorooctanoic acid; PFUA = Perfluoroundecanoic acid; PBPK = Physiologically based pharmacokinetic; PBDE = Polybrominated diphenyl ether; PCB = Polychlorinated biphenyl; PCDD = Polychlorinated dibenzo-p-dioxins. PCDF = Polychlorinated dibenzofurans. PIH = Pregnancy-induced hypertension; RR = Relative Risk; SD = Standard Deviation.
GDM was typically assessed at a routine prenatal care visit in the second trimester (22–28 weeks gestation) with a standard glucose tolerance test routinely used for selective GDM screening in the United States. The majority of cases were determined through clinical diagnosis by a health professional, while a few relied on medical record abstraction and self-reported data for outcome classification. The majority of self-reports were of a physician diagnosis recorded in monthly pregnancy journals designed to be consistent with recommendations of the American Congress for Obstetricians and Gynecologists for antenatal care. Most GDM studies focused on persistent organic pollutants or heavy metals/metalloids, with a smaller number of studies (five) assessing exposure to non-persistent chemicals. Important confounders for consideration in GDM models include maternal age, BMI, weight gain during pregnancy, pre-existing and family history of diabetes and hypertension, and parity. Studies adjusted at minimum for maternal age and pre-pregnancy BMI, with recent studies examining BMI as an effect modifier [118]. Most studies accounted for smoking and parity, while gestational weight gain and family history of diabetes and/or hypertension were rarely ascertained. Recent adjustments for arsenic models additionally included race/ethnicity, education status, and country of birth, which vary by arsenic exposure level (with higher levels found in older, Asian-born, and more highly educated women [123]). Recent studies have also applied advanced statistical methods to assess chemical mixtures and non-linear dose response methods (e.g., structural equation models, variable inflation factor, and cubic spline models).
As with PE, the timing of exposure assessment in GDM studies was roughly divided across pregnancy, ranging from recent preconception (soon before pregnancy) to early postpartum (soon after delivery), which limited study comparability. However, consideration of biomarker type and sampling matrix is critical for the interpretation of results. For example, arsenic was measured in a variety of biological media (blood, urine, hair, nails, drinking water, and meconium) which represent a combination of short and long term exposures as well as diverse exposure sources (i.e., inorganic arsenic from foods such as rice and fish compared to organic arsenic from drinking water). While each biomarker may be subject to some degree of exposure misclassification, the benefits of using one over another should be considered carefully.
Persistent Organic Pollutants
We reviewed 10 studies (seven cohort and three case-control) that examined associations between serum levels of persistent organic pollutants (POPs) and risk of GDM or gestational IGT, including six PCB studies, three PBDE studies, and four PFAS studies (Table 4).
Polychlorinated Biphenyls (PCBs) and Polbrominated Diphenyl Ethers (PBDEs)
Serum PCB levels were evaluated with GDM risk in six studies that varied considerably by location (United States, Canada, Iran, Greece, and the Faroe Islands), study period (1990s to 2015), and timing of exposure assessment (preconception to delivery) [124–126]. PCB findings were mixed. Three studies measured serum PCB levels in the first trimester and reported different findings. Dioxin-like congeners sampled in early pregnancy were associated with increased GDM risk among pregnant women in Greece [although estimates were imprecise with an adjusted OR = 4.71 (95% CI: 1.38–16.01) for the highest compared to lowest exposure groups], while null associations were reported for non-dioxin like PCB congeners (i.e., PCBs 118 and 156) in that study [125]. On the other hand, non-dioxin-like PCBs in the first trimester were modestly associated with increased GDM risk among pregnant women in China with evidence of a non-linear dose response [126], while no associations were reported among pregnant women sampled in the first trimester in Canada [127]. Differing exposure levels and study population characteristics may partially account for the result inconsistencies. For example, exposure levels were lowest in the Chinese study population [126] (eight times lower than in Greece [125] and three times lower than in Canada [127]). Additionally, the Canadian study population was considered low risk (with a high socioeconomic status) [127]. Null associations were reported in another study which sampled PCB levels at 34 weeks rather than during early pregnancy [128]. A study in Iran which sampled women at 24–28 weeks gestation found associations with increased GDM risk; however, lipid normalization combined with lipid adjustment as an independent covariate in regression models may have biased results in that study [124]. In contrast, a U.S. study which measured serum PCB levels prior to pregnancy observed a consistent decrease in GDM risk associated with increasing levels of lipid-normalized (ng/g lipid) but not wet weight (ng/ml) serum PCBs [129]. The authors suggested that pregnant women may differentially sequester PCBs in adipose tissue based on GDM status or that lipid adjustment may not appropriate if lipids are on the causal pathway between exposure and GDM. Three studies (two case-control and one prospective cohort) evaluated maternal serum levels of PBDE congeners among pregnant women and multi-pollutant models. Findings were null for most congeners, although BDE-153 was associated with 80% increased adjusted odds of GDM in two studies [89,124] and 3-fold higher GDM risk in the third (with relatively wider confidence bands) [130]. Additionally, non-linear dose response curves were reported for several BDE congeners (i.e., BDE-100 and BDE-154) [130].
Perfluoroalkyl substances (PFAS)
Four prospective cohort studies evaluated the relationship between serum levels of perfluoroalkyl substances (PFAS) and gestational IGT or GDM (Table 4). Although individual PFAS results varied across studies, preconception PFOA levels were associated with increased GDM risk among pregnant women in the U.S. LIFE cohort [131], while first trimester PFOS and PFHxS levels were associated with increased gestational IGT (but not GDM) among pregnant women in Spain [132] and Canada [127]. Null associations were reported with third trimester PFAS levels in a study evaluating GDM as an effect modifier or mediator of birth size with multiple POPs using structural equation models [128].
Pesticides
Six studies relating GDM development to pesticide exposure were largely null or inconsistent for OCPs [89,93,125,127,133,134], except for one that found increased GDM risk associated with serum DDE levels [134] (Table 4). Another reported increased GDM risk associated with organophosphate pesticides (OPPs) using an indirect measure of exposure (e.g., participant interviews about pesticide use and related activities) [133], while Shapiro et al., (2016) observed decreased GDM risk associated with urinary levels of two organophosphate pesticide (OPP) metabolites among N=1274 pregnant women in Canada (49 GDM cases) [127].
Non-persistent Chemicals
We identified five studies that assessed the relationship between GDM (with gestational IGT as a clinical indicator) and non-persistent chemicals including phthalates and phenols [86,135–138] (Table 4). All but one reported null associations between phthalates, BPA, or triclosan exposures and GDM [136–138], with Fisher et al., (2018) reporting an inverse association between GDM and triclosan [135]. Additionally, in a larger study population (N = 81,205), Quach et al., (2015) observed a significant association between GDM and occupation as a cosmetologist or manicurist [86].
Heavy Metals/Metalloids
Seven studies evaluated the relationship between arsenic exposure and GDM or gestational IGT risk in diverse locations (China, France, Chile, the United States, and Canada) and sampling matrices (urine, blood, hair, nails, meconium, and drinking water). Sample sizes varied between 244 and 5053 study participants, and the timing of exposure assessment ranged from periconception to soon after delivery (Table 4) [138–144]. Increased GDM risk was associated with arsenic in water [140,141] and non-urinary biomatrices (i.e., blood, meconium, and nails), with the greatest risk in the highest compared to lowest exposure groups and evidence of an increasing dose-dependent relationship in multiple studies [138,140,143,144]. In contrast, GDM was not associated with arsenic in either study that evaluated urine [140,142]. One study examined the association across pregnancy and found increased GDM risk associated with high blood arsenic levels only in the first trimester, suggesting that early pregnancy is a possible window of susceptibility warranting further research [144]. Additionally, two prospective cohort studies (N=1151 and N=1274) reported null gestational IGT associations with urinary and blood arsenic levels [138,140], while a smaller cross-sectional study (N=532) among a unique study population (24% Native American) found increased risk of gestational IGT associated with higher blood arsenic levels [139]. Limited research on other metals revealed null findings, although increased GDM risk was associated with cadmium in urine and meconium among two Chinese study populations (one of which excluded values below the detection limit, which could have biased results [143]) [145], while a borderline significant association with blood cadmium levels was reported among the MIREC pregnancy cohort in Canada [143].
4.4. Maternal Breast Cancer and Chemical Exposures
Due to the length of follow-up required to evaluate environmental exposures and breast cancer risk, limited human studies have assessed chemical exposures during critical periods of sensitivity such as during pregnancy [2,148]. Prior reviews have concluded that taking a commonly prescribed synthetic estrogen called diethylstilbestrol (DES) during pregnancy between 1940 and 1971 was associated with a modest (around 30%) increased risk of future breast cancer in mothers [149–156]. We identified three additional epidemiologic studies of persistent chemical exposures and maternal breast cancer among two study populations in the United States and Denmark (Table 5). Sample sizes ranged from N=224 (112 cases) to N=243 (250 cases), while the follow-up period spanned 10–17 years between the time of serum sample collection and age at diagnosis. All three nested case-control studies measured serum or plasma levels of persistent organic pollutants, including DDT/DDE, PCBs, and PFAS, in relation to premenopausal breast cancer risk [157–159]. The literature search did not reveal any human studies that evaluated mammographic density or breast tissue morphology.
Table 5.
Epidemiologic studies of maternal breast cancer risk and chemical exposures in pregnant women (4 Studies)
| Study [Ref #] | Study Design | Sample Size, # Cases | Study Period | Study Population, Location | Chemical Exposure(s) | Maternal Outcome(s) | Result |
|---|---|---|---|---|---|---|---|
| [157] | Nested Case-control. | N=483, 250 cases, 233 controls (frequency-matched). | 1996–2001. | Participation in Danish National Birth Cohort (DNBC) in Denmark. | Measured plasma levels of 16 PFAS: PFOS, PFOA, PFNA, PFHxS, PFOSA, PFBS, PFHpS, PFDS, and PFOSA), PFPeA, PFHxA, PFHpA, PFUnA, PFDoA, PFTrA, and PFTeA; twice in 1st and 2nd trimesters. | Maternal Breast Cancer (MBC). |
PFOS and Maternal BC: Adjusted RR=0.99 (95% CI: 0.98–1.01). When modeled as five categories: Adjusted RR=1.51 (0.81–2.71), 1.51 (0.82–2.84), 1.13 (0.59–2.04), and 0.90 (0.47–1.70) for women in the 2nd, 3rd, 4th, and 5th exposure quintiles compared to women in the lowest exposure quintile. PFOA and Maternal BC: Adjusted RR=1.00 (95% CI: 0.90–1.11). Categorical results were similar. PFNA and Maternal BC: Adjusted RR=0.76 (95% CI: 0.30–1.94); Categorical results were similar. PFHxS and Maternal BC: Adjusted RR=0.66 (0.47–0.94). When modeled as five categories: Adjusted RR=0.64 (0.34–1.18), 0.70 (0.38–1.29), 0.38 (0.20–0.70), and 0.61 (0.33–1.12) for women in the 2nd, 3rd, 4th, and 5th exposure quintiles compared to women in the lowest exposure quintile. PFOSA and Maternal BC: Adjusted RR=1.04 (0.99–1.08). When modeled as five categories: Adjusted RR=1.38 (0.75–2.52), 0.91 (0.49–1.66), 1.11 (0.60–2.05), and 1.89 (1.01–3.54) for women in the 2nd, 3rd, 4th, and 5th exposure quintiles compared to women in the lowest exposure quintile. sumPFSA and Maternal BC: Adjusted RR=1.00 (0.99–1.01). Results were similar when exposure was modeled categorically and for other summary exposure metrics. |
| [159] | Nested Case-control. | N=258, 129 cases, 129 controls, (matched on birth year). | 1959–1967. | Participation in Child Health and Development Studies and residence in Oakland, CA, USA. | Measured serum levels of p,p′-DDT, o,p′-DDT, and p,p′-DDE in 3rd trimester or within 1–3 days of delivery. | Maternal Breast Cancer (MBC). |
Model with all compounds p,p′-DDT and MBC: Adjusted OR=1.9 (95% CI: 0.9–4.1, p-value=0.09) and 2.9 (95% CI: 1.1–8.0, p-value=0.04) for women in the 2nd and 3rd exposure tertiles compared to women in the lowest exposure tertile. p,p′-DDE and MBC: Adjusted OR=1.3 (95% CI: 0.6–2.7, p-value=0.48) and 1.0 (95% CI: 0.4–2.4, p-value=0.92) for women in the 2nd and 3rd exposure tertiles compared to women in the lowest exposure tertile. o,p′-DDT and MBC: Adjusted OR=0.5 (95% CI: 0.3–1.0, p-value=0.06) and 0.4 (95% CI: 0.2–0.8, p-value=0.02) for women in the 2nd and 3rd exposure tertiles compared to women in the lowest exposure tertile. Model with all compounds p,p′-DDT and MBC: Adjusted OR=2.5 (95% CI: 1.0–6.3, p-value=0.05) and 5.2 (95% CI: 1.4–19.1, p-value=0.01). p,p′-DDE and MBC: Adjusted OR=1.5 (95% CI: 0.6–3.4, p-value=0.34) and 0.9 (95% CI: 0.3–3.0, p-value=0.90) for women in the 2nd and 3rd exposure tertiles compared to women in the lowest exposure tertile. o,p′-DDT and MBC: Adjusted OR=0.5 (95% CI: 0.2–1.2, p-value=0.13) and 0.3 (95% CI: 0.1–0.7, p-value=0.01) for women in the 2nd and 3rd exposure tertiles compared to women in the lowest exposure tertile. |
| [160] | Nested Case-Control. | N=224, 112 cases, 112 controls (matched on birth year). | 1959–1967. | Participation in Child Health and Development Studies and residence in Oakland, CA, USA. | Measured serum levels of 16 PCBs: Estrogenic (101, 187, 201); Non-ortho (66, 74, 105, 118, 156, 167, 138, 170); and Di-ortho (99, 153, 180, 183, 203, and [203/167 + 187] in 3rd trimester or within 1–3 days of delivery. | Maternal Breast Cancer (MBC). |
PCB-167 and MBC: Adjusted OR=1.09 (95% CI: 0.48–2.47), 0.70 (95% CI: 0.27–1.78), and 0.24 (95% CI: 0.07–0.79) for women in the 2nd, 3rd, and 4th exposure quartiles compared to women in the lowest exposure quartile (p-trend <0.04). PCB-187 and MBC: Adjusted OR=0.94 (95% CI: 0.41–2.17), 0.92 (95% CI: 0.36–2.38), and 0.35 (95% CI: 0.11–1.14) for women in the 2nd, 3rd, and 4th exposure quartiles compared to women in the lowest exposure quartile (p-trend <0.02). PCB-203 and MBC: Adjusted OR=1.21 (95% CI: 0.46–3.18), 2.89 (95% CI: 0.98–8.55), and 6.34 (95% CI: 1.85–21.73) for women in the 2nd, 3rd, and 4th exposure quartiles compared to women in the lowest exposure quartile (p-trend <0.001). |
CI = Confidence Interval; DDE = Dichlorodiphenyldichloroethylene; DDT = Dichlorodiphenyltricloroethane; Di-2-ethylhexyl phthalate metabolites (ΣDEHP = MEHHP, MECPP, MEOHP, and MEHP); HR = Hazard Ratio; IQR = Interquartile range; OR = Odds Ratio; OCP = Organochlorine Pesticide; PFAS = Perfluoroalkyl substances; PFDeA = Perfluorodecanoic acid; PFHxS = Perfluorohexane sulfonate; PFNA = Perfluorononanoic acid; PFOSA = Perfluorooctane sulfonamide; PFOS = Perfluorooctane sulfonic acid; PFOA = Perfluorooctanoic acid; PFUA = Perfluoroundecanoic acid; PBPK = Physiologically-based pharmacokinetic; PBDE = Polybrominated diphenyl ether; PCB = Polychlorinated biphenyl; PCDD = Polychlorinated dibenzo-p-dioxins. PCDF = Polychlorinated dibenzofurans. RR = Relative Risk; SD = Standard Deviation.
Breast cancer risk factors that were considered as potential confounders in current literature either during sampling of controls or statistical analysis include maternal age at blood draw, BMI (pre-pregnancy or early pregnancy), reproductive history (age of puberty, birth/pregnancy/lactation history, and age of menopause), hormone medication use, smoking and alcohol consumption, socioeconomic status (e.g., education, race/ethnicity, etc.), physical activity, and total serum lipid levels (modeled as an independent covariate in PCB and DDT models). Stratification by age of cancer diagnosis was also commonly performed due to its influence on risk. A limitation common to all studies was the lack of information on breast cancer subtype (e.g., tumor receptor status, etc.), which could have biased results to the null if chemical exposures were differentially associated with breast cancer tumor subtype. Additional covariates that could be potential confounders of maternal breast cancer associations although were not commonly ascertained in current literature include dietary intake, personal care product use, occupational history, endogenous hormone levels, exposure to various EDC mixtures, and metabolic efficiency.
Two U.S. studies conducted by Cohn et al., (2007, 2012) use d data from one of the longest follow-up studies to date on developmental windows of susceptibility for breast cancer risk. Both case control studies, nested within the prospective Child Health and Development Studies (CHDS), evaluated the association of organochlorine compounds (including DDT-related compounds and/or PCB congeners measured in maternal serum in 1959–1969 within 1–3 days of delivery or in the third trimester of pregnancy) and breast cancer diagnosed before 50 years of age (identified through the California Cancer Registry and California Vital Status records) [159,160]. Although imprecise, the estimated increased breast cancer risk associated with DDT exposure among young women (< 20 years old) was 5.4-fold higher (95% CI: 1.7–17.1) during peak DDT use in 1945, with no association found among older women, suggesting the importance of early life exposures on premenopausal risk [159]. In contrast, maternal serum PCB levels of congeners 167 and 187 were associated with reduced premenopausal risk (with adjusted risk estimates below 0.5), although PCB-203 was associated with increased risk (adjusted OR = 6.34, 95% CI: 1.85–21.73). The net effect of PCB exposure, calculated as the ratio of PCB-203 to the sum of PCB-167 and PCB-187 in the mixture, was associated with a three-fold higher breast cancer risk, indicating the deleterious association with PCB-203 outweighed the protective associations with congeners 167 and 187 [158].
Another study which measured plasma PFAS levels prospectively during the first two trimesters between 1996–2002 among 483 Danish pregnant women (250 cases, 233 frequency-matched controls) found elevated premenopausal breast cancer risk associated with PFOSA (adjusted RR = 1.89, 95% CI: 1.01–3.54) and decreased risk associated with PFHxS (adjusted RR = 0.40, 95% CI: 0.20–0.70) [157]. When stratified by age at diagnosis, risk estimates increased and became more significant in younger women (diagnosed < 40 years old), with a more than 3-fold increase and decrease in risk associated with PFOSA and PFHxS, respectively, that was not observed in older women [161].
5. Discussion
5.1. Heightened Susceptibility: The Borderline Disease State of Normal Pregnancy
The normal physiological changes that occur during pregnancy serve as a unique stress test for women that challenge the adaptive mechanisms of maternal physiology by moving women closer in proximity to disease thresholds which require significant compensation to overcome. These changes can also be influenced by underlying health factors (e.g., pre-gestational insulin resistance or elevated blood pressure, etc.) as well as exposure to biologically active chemicals, such as endocrine disrupting chemicals (EDCs). Thus, pregnancy can be thought of as a borderline disease state that heightens susceptibility to maternal health complications such as preeclampsia (PE), gestational diabetes mellitus (GDM), and breast cancer.
Given the importance of maternal health during pregnancy, and the fact that some of these conditions are on the rise (GDM and breast cancer globally, severe PE in the United States) while their definitive causes remain elusive, we have not sufficiently studied the contribution of environmental chemicals. Our review found limited data with which to assess the broad role of the pregnancy exposome on maternal health. The data we have indicate there is sufficient evidence to justify concern about the potential impact of chemical exposures on women’s health, warranting further research in this area. However, substantial variation in study design, method of measurement, and analytical approach precluded study comparability data. Studies differed in method and timing of exposure and outcome assessment, selection of sampling biomatrix (urine, blood, hair, nails, etc.) and biomarker type (organic vs inorganic, conjugated vs free, etc.), as well as adjustment for urine dilution, serum lipid levels, and potential confounders. Further research focused on resolving these inconsistencies would strengthen existing literature.
Nevertheless, biological changes during pregnancy that are regulated by endogenous signaling molecules indicate a potential role for exogenous chemicals like EDCs to interfere with molecular signals that govern various physiological processes during pregnancy. Although we were unable to draw firm conclusions about specific exposure-response relationships due to limited study comparability, below we highlight potential biological mechanisms for several reviewed findings. Non-persistent chemicals (BPA and phthalates) and heavy metals/metalloids (cadmium and to a lesser extent, arsenic and mercury, with lead reviewed by others [1]) were associated with increased risk of PE or PIH in multiple epidemiologic studies. For GDM, we found positive associations with some POPs, including non-dioxin like PCBs, PBDEs, and some PFAS; and with heavy metals/metalloids (i.e., arsenic). While mechanisms for POPs and PE and non-persistent chemicals and GDM are not discussed, due to findings that were mixed and largely null, further research on DDT in populations with current active indoor use of the insecticide is warranted.
Preeclampsia: Biological Plausibility for Chemical Effects
Numerous studies support the biological plausibility of a causal relationship between non-persistent chemical exposures and PE. Findings from in vitro and in vivo studies have shown that BPA and phthalates can act directly on placental cells by inducing trophoblast cell apoptosis and necrosis (BPA) [162–164] and by inhibiting CTB cell invasion (phthalates) [165]. These non-persistent chemicals induce oxidative stress in animal and in vitro models [166–169] are positively associated with oxidative stress biomarkers, namely 8-hydroxydeoxyguanosine (OHdG) and 8-isoprostane, in epidemiologic studies of pregnant women [170,171]. Higher maternal serum levels of anti-angiogenic factors have been reported with BPA and phthalate metabolite concentrations in urine [172], suggesting these chemicals may also inhibit angiogenesis during placentation. Additional evidence suggests BPA can inhibit estrogen’s promotion of angiogenesis by preventing placental estrogen production (i.e., through BPA’s affinity for estrogen-related receptor γ or by modulating expression of the aromatase enzyme on which the placenta relies for estrogen synthesis) [53,101]. BPA can also inhibit production of hCG, which promotes angiogenesis as well as CTB cell differentiation and invasion during placentation [61].
Several mechanisms have been proposed for metals/metalloids in the development of PE, with oxidative stress and inflammation identified as leading pathophysiologies. Cadmium accumulates in the placenta and recent in vitro research has demonstrated the heavy metal’s ability to disrupt trophoblast cell migration, leading to abnormal placentation and insufficient uteroplacental perfusion indicative of PE pathology [173,174]. Like lead, cadmium can induce reactive oxygen species (ROS) and stimulate oxidative stress, which promotes inflammation, the release of antiangiogenic factors, and endothelial dysfunction [175]. The effect of cadmium exposure on PE in the placenta may also be mediated by abnormal glucocorticoid synthesis and immune system function [176]. Additionally, cadmium has been associated with proteinuria and other biomarkers of kidney injury that are related to angiogenic dysfunction as well as PE [175,177]. Limited evidence suggests arsenic is also associated with increased markers of inflammation and endothelial damage in plasma, and may promote endothelial dysfunction, pathologic vascular remodeling, and atherosclerosis [118]. To our knowledge, only three human studies have assessed PE risk in relation to arsenic exposure, all of which had limitations [109,117]. Given the high potential for exposure through contaminated food and water supplies in communities around the globe, arsenic warrants further evaluation for potential effects on PE risk. Mercury also deserves further study. Additionally, assessing metals as a mixture is more representative of the underlying population exposure distribution and may be more informative for human health risk.
Gestational Diabetes: Biological Plausibility for Chemical Effects
While precise mechanisms have yet to be fully elucidated, scientific literature indicates that PBDEs such as BDE-47 and BDE-153 can interfere with glucose and lipid homeostasis by increasing hepatic glucose metabolism [178], free fatty acid mobilization, lipolysis [179], and/or pancreatic β cell dysfunction [180]. PBDEs can inhibit insulin-stimulated glucose oxidation in rodents adipose cells [181] and can promote glucose-stimulated insulin secretion in human β cells (which may be mediated by the thyroid hormone receptor) [180]. They have also been shown to decrease activation of the PPAR-γ, a nuclear hormone receptor that promotes insulin action and plays a central role in lipid metabolism, fat cell storage, and glucose regulation [182,183]. Likewise, PFAS such as PFOA and PFOS may modulate fatty acid uptake and metabolism through PPAR-α (related but distinct from PPAR-γ) and can promote insulin resistance by inhibiting insulin action mediated by the phosphatidylinositol 3-kinase-serine/threonine protein kinase (PI3K-AKT) pathway in the liver [184,185]. Additionally, PFAS are immunomodulators that can promote inflammation-mediated pathways which may contribute to metabolic dysfunction and insulin resistance [186–188]. While PFAS were not consistently associated with GDM in this review, emerging human data on subclinical measures of metabolic function such as gestational IGT indicate these fluorinated compounds may contribute to GDM-related endpoints such as insulin resistance and hyperglycemia during pregnancy [91,189].
Biological mechanisms for arsenic and GDM include those described previously for PE (i.e., oxidative stress and inflammation (through TNF-alpha and IL-6)), in addition to inhibition of PPAR-γ expression [190], epigenetic methylation [191], and interference with insulin-dependent activity [192]. Numerous in vitro and in vivo studies have demonstrated arsenic’s ability to impact pancreatic β cell function and promote insulin secretion [179,191]. Arsenic can exacerbate insulin resistance associated with normal pregnancy in animal studies and contributes to hyperglycemia in non-pregnant human populations [179,192–194]. Future epidemiologic studies of arsenic exposure and GDM risk may consider differentiating between organic and inorganic arsenic subtypes, short-term vs. long-term exposure biomarkers, as well as biomarkers of metabolic efficiency.
Further confirmation of recent findings regarding the first trimester as a sensitive window for arsenic toxicity using longitudinal data would also be useful. Blood arsenic levels were associated with increased GDM risk in the first but not second or third trimesters, according to the only study which measured arsenic across pregnancy [147]. Confirmation of this finding in urine would be useful, given that blood arsenic levels may not be as reliable due to arsenic’s rapid clearance from blood [123]. On the other hand, methods for measuring blood arsenic levels may be more consistent and multiple arsenic types (organic and inorganic) easier to distinguish in blood compared to urine. Moreover, chronic arsenic exposure may lead to steady state blood levels that would negate issues of rapid elimination [123].
Maternal Breast Cancer: Biological Plausibility for Chemical Effects
Overall, animal and in vitro data support a causal link between chemical exposures during pregnancy and maternal breast cancer risk. In pregnant mice, exposure to environmental chemicals such as dioxin and bisphenol-S (BPS), a substitute phenol with structural and functional similarities to BPA, can alter the gene expression of signaling pathways involving growth hormone, prolactin, estrogen, and progesterone [54,195]. Environmental chemicals can also act directly on the mammary gland by promoting changes in morphology and glandular development that may increase future breast cancer risk. For example, PFOA delays mammary gland differentiation in rodents while dioxin increases proliferation of undifferentiated mammary cells, reducing the extent of branching and differentiation to lobular alveolar structures during pregnancy [195,196]. Maternal exposure to oxybenzone, a ubiquitous EDC used in sunscreen and other cosmetics, has also been shown to permanently alter mammographic density and breast tissue morphology at levels relevant for human exposure [197]. Moreover, in utero and early life exposures can influence risk by altering the amount of terminal ductal lobular units that are available for differentiation during pregnancy [46].
Additionally, human observational studies have shown that carcinogenic biomarkers of estrogen metabolism are associated with increased breast cancer risk and higher serum levels of persistent chemicals, including polychlorinated dibenzo-p-dioxins, dibenzofurans, and biphenyls, in the third trimester [198,199]. Untangling hormone-mediated risk factors for breast cancer is challenging, in part due to the variable influence of endogenous hormones as well as exogenous factors (e.g., EDCs) across the life course. In humans, opposing age-dependent effects on maternal breast cancer are well established, with strong evidence supporting paradoxical effects from tumor subtype, age at first pregnancy, and age at breast cancer diagnosis [200]. Future research on chemical exposures and breast cancer risk may wish to examine tumor subtype and receptor status as potential confounders, given this was a common limitation of current literature. Further work should also consider hormone type as well as the ratio of carcinogenic metabolites as potential biomarkers of breast cancer risk.
Common Pathophysiologies for Varied Maternal Health Outcomes
Maternal health complications and breast cancer represent varied maternal health outcomes that may share common pathophysiologies, which can potentially provide clues into biological mechanisms and intervention strategies. Although not definitive, multiple studies have described a modest inverse association between PE and maternal breast cancer risk that may be mediated by high circulating levels of androgen and hCG, which are typically observed in the preeclamptic pregnancy (especially in the third trimester) [16]. In contrast, GDM has been associated with increased maternal breast cancer risk [14], although findings are somewhat equivocal [15]. Potential connections between breast cancer and diabetes during pregnancy include hormones that are both lactogenic and diabetogenic (i.e., prolactin, cortisol, progesterone, growth hormone, and hCS). Placental origins of PE, GDM, and breast cancer may also provide a connection between these outcomes on the pathophysiological level (e.g., through oxidative stress, angiogenic, and/or PPAR signaling pathways) [201–203]. However, our understanding of how these outcomes are related and the role of hormones, chemical exposures, and the pregnancy physiology remains incomplete [37,179].
5.2. Research Recommendations
Leveraging Existing Studies to Evaluate Maternal Outcomes
Many studies are currently evaluating chemical exposures during pregnancy with respect to fetal and children’s health outcomes. The wealth of studies represents an opportunity to leverage existing data structures and research protocols to investigate maternal health complications such as GDM and/or PE. Collecting or obtaining simple measurements, such as non-fasting blood glucose levels and family/personal history of PE during routine study exams and participant surveys may provide relatively straightforward opportunities for assessing these measures as potential indicators or confounders in future research. Although maternal breast cancer requires a minimum follow-up period of 10–15 years, environmental epidemiologists with access and opportunity to appropriate data sets (i.e., prospective cohorts with long-term follow-up, banked biological samples, and/or cancer registry linkages) should consider evaluating maternal breast cancer risk in future studies. Additionally, focusing on PABC as a breast cancer outcome may provide new opportunities to assess chemicals such as BPA which have similar estrogenic properties as DES but have short biological half-lives that are challenging to study in relation to breast cancer risk.
Incorporating Biomarkers to Strengthen Epidemiologic Research
Molecular biomarkers can serve as valuable tools for environmental health scientists and epidemiologists who seek to identify biological indicators of exposure that may also serve as early indicators of health risk. Recent advancements in molecular toxicology and in vitro modeling (e.g., the use of microRNA technology, placental explants, etc.) have uncovered larger panels of molecular targets that may be useful biomarkers in exposure and epidemiologic studies on PE, GDM, and breast cancer [204–207]. New biomarkers and signaling pathways related to oxidative stress, angiogenesis, inflammation, and metabolic (PPAR) regulation are currently under investigation and can offer unique opportunities to strengthen research on environmental chemicals and maternal health outcomes. For example, the use of anti-angiogenic factors as biomarkers of BPA and phthalate exposure provides considerable support of research on PE and non-persistent chemicals [172], while the use of breast cancer biomarkers (e.g., the ratio of carcinogenic estrogens) strengthens research on POPs and may provide a unique endpoint for further study of breast cancer risk [198]. Continued emphasis on proteomics, metabolomics, and transcriptomics will advance our ability to develop this emerging area of environmental health research. Animal models can also be helpful in elucidating biological mechanisms and pathophysiologies of these diseases; however, resolving some of the limitations in their use for PE, a disease that is specific to the human placenta, would facilitate their utility in this regard.
Our research suggests that focusing on maternal and placental hormones which have not been comprehensively examined (i.e., prolactin, progesterone, hCG, hCS, and HPG), may offer new insights into adverse maternal health outcomes. Maternal origins of PE should be investigated in this context, as recent data suggest the smooth muscle cells of the uterus can influence CTB invasion of maternal decidua, which ultimately determines the extent of spiral artery remodeling associated with risk of developing PE [51]. As hormone regulators of decidualization during embryo implantation and placentation, progesterone, prolactin, and CRH may warrant further study in this context [37,51]. Researchers should consider evaluating thyroid hormone disruptors, such as PBDEs, PFAS, and phthalates, for their potential impacts on hCG activity during pregnancy, including effects on thyroid hormone production, CTB differentiation and invasion, angiogenesis, and maternal immune system function [61]. Given hCG’s dynamic role throughout the course of pregnancy and that hCG (like PE) is specific to humans, further examination of hCG may provide renewed insights into PE prevention and treatment, which have remained elusive despite many years of research targeting this disease pathway [61]. Other placental hormones, including hCS, HPG, and CRH are valuable indicators of placental wellbeing that can be measured in maternal serum. Assessing these global pregnancy regulators with local proteins, hormones, transcription factors, etc., may advance our ability to understand the complex relationships between chemical exposures and the array of molecules that interact across the maternal-placental-fetal unit.
Recognizing Pregnancy as a Critical Period for Women’s Health
Multiple endogenous and exogenous factors influence physiology and health risk during each life stage of development, with each successive “hit” impacting lifelong risk in variable ways. Based on our review, pregnancy represents a heightened state of physiological sensitivity that can exacerbate chemical exposures effects on maternal health and should be regarded as a critical period for women’s health. Thus, future efforts to quantify the totality of exposures across the life course should include the pregnancy period. We propose the following framework for consideration in future research on chemical exposures and maternal health outcomes.
Based on our analysis, the maternal pregnancy exposome should be assessed in combination with other vulnerable life stages, such as in utero development and during puberty. Assessing the combined effects of the in utero exposome, puberty exposome, and pregnancy exposome will be valuable for understanding the complexity of maternal health outcomes across the life course.
6. Conclusion
The pregnancy exposome may substantially contribute to maternal health risks. Emerging animal and in vitro data support the notion that exogenous chemical exposures and endogenous physiological changes may together enhance maternal health risks. Existing epidemiologic research indicates there is sufficient evidence to justify concern for chemical exposure effects on women’s health, but more research is required to delineate biological mechanisms, clarify disease etiology, and improve our understanding of exposure-outcome pathways that contribute to maternal health complications and breast cancer risk across the life course. Additional human studies evaluating chemical exposures with preeclampsia, gestational diabetes, and maternal breast cancer risk are warranted and should assess the combined effects of environmental chemicals and physiological changes during pregnancy. Biomarkers of exposure and effect may serve as valuable tools for environmental epidemiologists who seek to quantify the totality of exposures across the life course. Future exposome research should include pregnancy as a critical period for women’s health, but efforts to incorporate deliberate biomarker selection, appropriate timing and method of exposure and outcome assessment, and consistent analysis of confounders, cumulative exposures, and non-linear associations would strengthen existing literature. Evaluating environmental chemicals as modifiable risk factors may ultimately inform intervention strategies for reducing the overall burden of maternal health complications and breast cancer on women’s health.
Figure 1.
Vulnerable stages for adverse maternal health outcomes across the life course.
Highlights.
Pregnancy heightens susceptibility to chemical exposures and women’s health risks.
Sufficient data justifies concern about chemical exposures and maternal health.
Pregnancy should be regarded as a critical period for women’s health.
More epidemiologic research is warranted on adverse maternal health outcomes.
Acknowledgements
This work was supported by the U.S. Environmental Protection Agency (No. RD-83543301, RD-83564301), National Institute of Environmental Health Sciences (P01ES022841, R00ES021470, R01ES027051, UG3OD023272), and National Library of Medicine (K01LM012381).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Poropat AE, Laidlaw MAS, Lanphear B, Ball A, Mielke HW, Blood lead and preeclampsia: A meta-analysis and review of implications, Environ. Res 160 (2018) 12–19. doi: 10.1016/j.envres.2017.09.014. [DOI] [PubMed] [Google Scholar]
- [2].Cohn BA, Developmental and Environmental Origins of Breast Cancer DDT as a Case Study, Reprod. Toxicol. Elmsford N 31 (2011) 302–311. doi: 10.1016/j.reprotox.2010.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rudel RA, Fenton SE, Ackerman JM, Euling SY, Makris SL, Environmental exposures and mammary gland development: state of the science, public health implications, and research recommendations, Environ. Health Perspect 119 (2011) 1053–1061. doi: 10.1289/ehp.1002864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Folk DM, Hypertensive Disorders of Pregnancy: Overview and Current Recommendations, J. Midwifery Womens Health 63 (2018) 289–300. doi: 10.1111/jmwh.12725. [DOI] [PubMed] [Google Scholar]
- [5].Sava RI, March KL, Pepine CJ, Hypertension in pregnancy: Taking cues from pathophysiology for clinical practice, Clin. Cardiol 41 (2018) 220–227. doi: 10.1002/clc.22892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Sibai BM, Stella CL, Diagnosis and management of atypical preeclampsia-eclampsia, Am. J. Obstet. Gynecol 200 (2009) 481.e1–481.e7. doi: 10.1016/j.ajog.2008.07.048. [DOI] [PubMed] [Google Scholar]
- [7].Ananth CV, Keyes KM, Wapner RJ, Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis, BMJ 347 (2013) f6564. doi: 10.1136/bmj.f6564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ferrara A, Increasing Prevalence of Gestational Diabetes Mellitus: A public health perspective, Diabetes Care 30 (2007) S141–S146. doi: 10.2337/dc07-s206. [DOI] [PubMed] [Google Scholar]
- [9].Kampmann U, Madsen LR, Skajaa GO, Iversen DS, Moeller N, Ovesen P, Gestational diabetes: A clinical update, World J. Diabetes 6 (2015) 1065–1072. doi: 10.4239/wjd.v6.i8.1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].World Breast Cancer Fund, Diet, nutrition, physical activity and breast cancer, 2017. https://www.wcrf.org/sites/default/files/Breast-cancer-report.pdf.
- [11].Azim HA, Santoro L, Russell-Edu W, Pentheroudakis G, Pavlidis N, Peccatori FA, Prognosis of pregnancy-associated breast cancer: A meta-analysis of 30 studies, Cancer Treat. Rev 38 (2012) 834–842. doi: 10.1016/j.ctrv.2012.06.004. [DOI] [PubMed] [Google Scholar]
- [12].Holdsworth-Carson SJ, Lim R, Mitton A, Whitehead C, Rice GE, Permezel M, Lappas M, Peroxisome proliferator-activated receptors are altered in pathologies of the human placenta: Gestational diabetes mellitus, intrauterine growth restriction and preeclampsia, Placenta 31 (2010) 222–229. doi: 10.1016/j.placenta.2009.12.009. [DOI] [PubMed] [Google Scholar]
- [13].Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, Gülmezoglu AM, Temmerman M, Alkema L, Global causes of maternal death: a WHO systematic analysis, Lancet Glob. Health 2 (2014) e323–e333. doi: 10.1016/S2214-109X(14)70227-X. [DOI] [PubMed] [Google Scholar]
- [14].Park Y-MM, O’Brien KM, Zhao S, Weinberg CR, Baird DD, Sandler DP, Gestational diabetes mellitus may be associated with increased risk of breast cancer, Br. J. Cancer 116 (2017) 960–963. doi: 10.1038/bjc.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Xie C, Wang W, Li X, Shao N, Li W, Gestational diabetes mellitus and maternal breast cancer risk: a meta-analysis of the literature, J. Matern.-Fetal Neonatal Med. Off. J. Eur. Assoc. Perinat. Med. Fed. Asia Ocean. Perinat. Soc. Int. Soc. Perinat. Obstet (2017) 1–11. doi: 10.1080/14767058.2017.1397117. [DOI] [PubMed] [Google Scholar]
- [16].Sun M, Fan Y, Hou Y, Fan Y, Preeclampsia and maternal risk of breast cancer: a meta-analysis of cohort studies, J. Matern.-Fetal Neonatal Med. Off. J. Eur. Assoc. Perinat. Med. Fed. Asia Ocean. Perinat. Soc. Int. Soc. Perinat. Obstet 31 (2018) 2484–2491. doi: 10.1080/14767058.2017.1342806. [DOI] [PubMed] [Google Scholar]
- [17].Kim JS, Kang EJ, Woo OH, Park KH, Woo SU, Yang DS, Kim A-R, Lee J-B, Kim YH, Kim JS, Seo JH, The relationship between preeclampsia, pregnancy-induced hypertension and maternal risk of breast cancer: A meta-analysis, Acta Oncol 52 (2013) 1643–1648. doi: 10.3109/0284186X.2012.750033. [DOI] [PubMed] [Google Scholar]
- [18].Troisi R, Innes KE, Roberts JM, Hoover RN, Preeclampsia and maternal breast cancer risk by offspring gender: do elevated androgen concentrations play a role?, Br. J. Cancer 97 (2007) 688–690. doi: 10.1038/sj.bjc.6603921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Forouzanfar MH, Foreman KJ, Delossantos AM, Lozano R, Lopez AD, Murray CJL, Naghavi M, Breast and cervical cancer in 187 countries between 1980 and 2010: a systematic analysis, The Lancet 378 (2011) 1461–1484. doi: 10.1016/S0140-6736(11)61351-2. [DOI] [PubMed] [Google Scholar]
- [20].Madigan MP, Ziegler RG, Benichou J, Byrne C, Hoover RN, Proportion of breast cancer cases in the United States explained by well-established risk factors, J. Natl. Cancer Inst 87 (1995) 1681–1685. [DOI] [PubMed] [Google Scholar]
- [21].American College of Obstetricians and Gynecologists (ACOG), Committee opinion no. 575: Exposure to toxic environmental agents, Obstet Gynecol 122 (2013) 931–934.24084567 [Google Scholar]
- [22].Di Renzo GC, Conry JA, Blake J, DeFrancesco MS, DeNicola N, Martin JN, McCue KA, Richmond D, Shah A, Sutton P, Woodruff TJ, van der Poel SZ, Giudice LC, International Federation of Gynecology and Obstetrics opinion on reproductive health impacts of exposure to toxic environmental chemicals, Int. J. Gynecol. Obstet 131 (2015) 219–225. doi: 10.1016/j.ijgo.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Wang A, Padula A, Sirota M, Woodruff TJ, Environmental influences on reproductive health: the importance of chemical exposures, Fertil. Steril 106 (2016) 905–929. doi: 10.1016/j.fertnstert.2016.07.1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Woodruff TJ, Zota AR, Schwartz JM, Environmental Chemicals in Pregnant Women in the United States: NHANES 2003–2004, Environ. Health Perspect 119 (2011). http://ehp03.niehs.nih.gov/article/fetchArticle.action?articleURI=info%3Adoi%2F10.1289%2Fehp.1002727 (accessed July 24, 2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Gore AC, Chappell VA, Fenton SE, Flaws JA, Nadal A, Prins GS, Toppari J, Zoeller RT, EDC-2: The Endocrine Society’s Second Scientific Statement on Endocrine-Disrupting Chemicals, Endocr. Rev 36 (2015) E1–E150. doi: 10.1210/er.2015-1010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hendryx M, Luo J, Children’s environmental chemical exposures in the USA, NHANES 2003–2012, Environ. Sci. Pollut. Res 25 (2018) 5336–5343. doi: 10.1007/s11356-017-0874-5. [DOI] [PubMed] [Google Scholar]
- [27].Robinson O, Vrijheid M, The Pregnancy Exposome, Curr. Environ. Health Rep 2 (2015) 204–213. doi: 10.1007/s40572-015-0043-2. [DOI] [PubMed] [Google Scholar]
- [28].Grant MJ, Booth A, A typology of reviews: an analysis of 14 review types and associated methodologies: A typology of reviews, Health Inf. Libr. J 26 (2009) 91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- [29].Tricco AC, Lillie E, Zarin W, O’Brien K, Colquhoun H, Kastner M, Levac D, Ng C, Sharpe JP, Wilson K, Kenny M, Warren R, Wilson C, Stelfox HT, Straus SE, A scoping review on the conduct and reporting of scoping reviews, BMC Med. Res. Methodol 16 (2016). doi: 10.1186/s12874-016-0116-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Agrawal S, Yamamoto S, Effect of indoor air pollution from biomass and solid fuel combustion on symptoms of preeclampsia/eclampsia in Indian women, Indoor Air 25 (2015) 341–352. doi: 10.1111/ina.12144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Hu H, Ha S, Roth J, Kearney G, Talbott EO, Xu X, Ambient Air Pollution and Hypertensive Disorders of Pregnancy: A Systematic Review and Meta-analysis, Atmospheric Environ. Oxf. Engl. 1994 97 (2014) 336–345. doi: 10.1016/j.atmosenv.2014.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Pedersen M, Halldorsson TI, Olsen SF, Hjortebjerg D, Ketzel M, Grandström C, Raaschou-Nielsen O, Sørensen M, Impact of Road Traffic Pollution on Pre-eclampsia and Pregnancy-induced Hypertensive Disorders, Epidemiol. Camb. Mass 28 (2017) 99–106. doi: 10.1097/EDE.0000000000000555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Pedersen M, Stayner L, Slama R, Sørensen M, Figueras F, Nieuwenhuijsen MJ, Raaschou-Nielsen O, Dadvand P, Ambient air pollution and pregnancy-induced hypertensive disorders: a systematic review and meta-analysis, Hypertens. Dallas Tex 1979 64 (2014) 494–500. doi: 10.1161/HYPERTENSIONAHA.114.03545. [DOI] [PubMed] [Google Scholar]
- [34].Burton GJ, Fowden AL, Thornburg KL, Placental Origins of Chronic Disease, Physiol. Rev 96 (2016) 1509–1565. doi: 10.1152/physrev.00029.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Soma-Pillay P, Catherine N-P, Tolppanen H, Mebazaa A, Tolppanen H, Mebazaa A, Physiological changes in pregnancy, Cardiovasc. J. Afr 27 (2016) 89–94. doi: 10.5830/CVJA-2016-021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Taylor EB, Sasser JM, Natural killer cells and T lymphocytes in pregnancy and pre-eclampsia, Clin. Sci 131 (2017) 2911–2917. doi: 10.1042/CS20171070. [DOI] [PubMed] [Google Scholar]
- [37].Voltolini C, Petraglia F, Chapter 2 - Neuroendocrinology of pregnancy and parturition, in: Fliers E, Korbonits M, Romijn JA (Eds.), Handb. Clin. Neurol, Elsevier, 2014: pp. 17–36. doi: 10.1016/B978-0-444-59602-4.00002-2. [DOI] [PubMed] [Google Scholar]
- [38].Cartwright JE, Fraser R, Leslie K, Wallace AE, James JL, Remodelling at the maternal–fetal interface: relevance to human pregnancy disorders, Reproduction 140 (2010) 803–813. doi: 10.1530/REP-10-0294. [DOI] [PubMed] [Google Scholar]
- [39].Roberts JM, Hubel CA, The Two Stage Model of Preeclampsia: Variations on the Theme, Placenta 30 (2009) S32–S37. doi: 10.1016/j.placenta.2008.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Boeldt D, Bird I, Vascular Adaptation in Pregnancy and Endothelial Dysfunction in Preeclampsia, J. Endocrinol 232 (2017) R27–R44. doi: 10.1530/JOE-16-0340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Thornburg KL, Jacobson SL, Giraud GD, Morton MJ, Hemodynamic changes in pregnancy, Semin. Perinatol 24 (2000) 11–14. [DOI] [PubMed] [Google Scholar]
- [42].Lain KY, Catalano PM, Metabolic changes in pregnancy, Clin. Obstet. Gynecol 50 (2007) 938–948. doi: 10.1097/GRF.0b013e31815a5494. [DOI] [PubMed] [Google Scholar]
- [43].Crain DA, Janssen SJ, Edwards TM, Heindel J, Ho S, Hunt P, Iguchi T, Juul A, McLachlan JA, Schwartz J, Skakkebaek N, Soto AM, Swan S, Walker C, Woodruff TK, Woodruff TJ, Giudice LC, Guillette LJ, Female reproductive disorders: the roles of endocrine-disrupting compounds and developmental timing, Fertil. Steril 90 (2008) 911–940. doi: 10.1016/j.fertnstert.2008.08.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Paine IS, Lewis MT, The Terminal End Bud: the Little Engine that Could, J. Mammary Gland Biol. Neoplasia 22 (2017) 93–108. doi: 10.1007/s10911-017-9372-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Beesley RD, Johnson JV, The Breast During Pregnancy and Lactation, Glob. Libr. Womens Med (2008). doi: 10.3843/GLOWM.10305. [DOI] [Google Scholar]
- [46].Fenton SE, Endocrine-Disrupting Compounds and Mammary Gland Development: Early Exposure and Later Life Consequences, Endocrinology 147 (2006) s18–s24. doi: 10.1210/en.2005-1131. [DOI] [PubMed] [Google Scholar]
- [47].Apostoli AJ, Skelhorne-Gross GE, Rubino RE, Peterson NT, Di Lena MA, Schneider MM, SenGupta SK, Nicol CJ, Loss of PPARγ expression in mammary secretory epithelial cells creates a pro-breast tumorigenic environment, Int. J. Cancer J. Int. Cancer 134 (2014) 1055–1066. doi: 10.1002/ijc.28432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Genin A-S, Antoine M, Aractingi S, Rouzier R, Pregnancy Stimulates Tumor Angiogenesis in Breast Carcinoma, Anticancer Res 34 (2014) 125–131. [PubMed] [Google Scholar]
- [49].Szalecki M, Malinowska A, Prokop-Piotrkowska M, Janas R, Interactions between the growth hormone and cytokines – A review, Adv. Med. Sci 63 (2018) 285–289. doi: 10.1016/j.advms.2018.03.001. [DOI] [PubMed] [Google Scholar]
- [50].Kumar P, Magon N, Hormones in pregnancy, Niger. Med. J. J. Niger. Med. Assoc 53 (2012) 179–183. doi: 10.4103/0300-1652.107549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Garrido-Gomez T, Dominguez F, Quiñonero A, Diaz-Gimeno P, Kapidzic M, Gormley M, Ona K, Padilla-Iserte P, McMaster M, Genbacev O, Perales A, Fisher SJ, Simón C, Defective decidualization during and after severe preeclampsia reveals a possible maternal contribution to the etiology, Proc. Natl. Acad. Sci. U. S. A 114 (2017) E8468–E8477. doi: 10.1073/pnas.1706546114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Michel RM, Aguilar JL, Arrieta O, Human chorionic gonadotropin as an angiogenic factor in breast cancer during pregnancy, Med. Hypotheses 68 (2007) 1035–1040. doi: 10.1016/j.mehy.2006.05.072. [DOI] [PubMed] [Google Scholar]
- [53].Losordo DW, Isner JM, Estrogen and Angiogenesis: A Review, Arterioscler. Thromb. Vasc. Biol 21 (2001) 6–12. doi: 10.1161/01.ATV.21.1.6. [DOI] [PubMed] [Google Scholar]
- [54].LaPlante CD, Catanese MC, Bansal R, Vandenberg LN, Bisphenol S Alters the Lactating Mammary Gland and Nursing Behaviors in Mice Exposed During Pregnancy and Lactation, Endocrinology 158 (2017) 3448–3461. doi: 10.1210/en.2017-00437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Napso T, Yong HEJ, Lopez-Tello J, Sferruzzi-Perri AN, The Role of Placental Hormones in Mediating Maternal Adaptations to Support Pregnancy and Lactation, Front. Physiol 9 (2018). doi: 10.3389/fphys.2018.01091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Talbot L, Maclennan K, Physiology of pregnancy, Anaesth. Intensive Care Med 17 (2016) 341–345. doi: 10.1016/j.mpaic.2016.04.010. [DOI] [Google Scholar]
- [57].Bhagavan NV, Ha C-E, Chapter 32 - Endocrine Metabolism V: Reproductive System, in: Bhagavan NV, Ha C-E (Eds.), Essent. Med. Biochem, Academic Press, San Diego, 2011: pp. 435–447. doi: 10.1016/B978-0-12-095461-2.00032-1. [DOI] [Google Scholar]
- [58].Gurtunca N, Sperling MA, 144 - Growth Hormone, Prolactin, and Placental Lactogen in the Fetus and Newborn, in: Polin RA, Abman SH, Rowitch DH, Benitz WE, Fox WW (Eds.), Fetal Neonatal Physiol Fifth Ed., Elsevier, 2017: pp. 1470–1476.e1. doi: 10.1016/B978-0-323-35214-7.00144-X. [DOI] [Google Scholar]
- [59].Sinha RA, Singh BK, Yen PM, Thyroid hormone regulation of hepatic lipid and carbohydrate metabolism, Trends Endocrinol. Metab 25 (2014) 538–545. doi: 10.1016/j.tem.2014.07.001. [DOI] [PubMed] [Google Scholar]
- [60].Glinoer D, What Happens to the Normal Thyroid During Pregnancy?, Thyroid 9 (1999) 631–635. doi: 10.1089/thy.1999.9.631. [DOI] [PubMed] [Google Scholar]
- [61].Paulesu L, Rao CV, Ietta F, Pietropolli A, Ticconi C, hCG and Its Disruption by Environmental Contaminants during Human Pregnancy, Int. J. Mol. Sci 19 (2018). doi: 10.3390/ijms19030914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Zygmunt M, Herr F, Münstedt K, Lang U, Liang OD, Angiogenesis and vasculogenesis in pregnancy, Eur. J. Obstet. Gynecol. Reprod. Biol 110 Suppl 1 (2003) S10–18. [DOI] [PubMed] [Google Scholar]
- [63].ATSDR - Public Health Statement: Polychlorinated Biphenyls (PCBs), (n.d.). https://www.atsdr.cdc.gov/PHS/PHS.asp?id=139&tid=26 (accessed September 6, 2018).
- [64].ATSDR - Public Health Statement: Polybrominated Diphenyl Ethers (PBDEs), (n.d.). https://www.atsdr.cdc.gov/PHS/PHS.asp?id=1449&tid=183 (accessed February 12, 2019).
- [65].Wang Z, Cousins IT, Scheringer M, Buck RC, Hungerbühler K, Global emission inventories for C4–C14 perfluoroalkyl carboxylic acid (PFCA) homologues from 1951 to 2030, Part I: production and emissions from quantifiable sources, Environ. Int 70 (2014) 62–75. doi: 10.1016/j.envint.2014.04.013. [DOI] [PubMed] [Google Scholar]
- [66].ATSDR - Public Health Statement: DDT, DDE, DDD, (n.d.). https://www.atsdr.cdc.gov/phs/phs.asp?id=79&tid=20 (accessed September 26, 2018).
- [67].ATSDR - Toxicological Profile: Phenol, (n.d.). https://www.atsdr.cdc.gov/ToxProfiles/tp.asp?id=148&tid=27 (accessed September 26, 2018).
- [68].ATSDR - Toxic Substances - Cadmium, (n.d.). https://www.atsdr.cdc.gov/substances/toxsubstance.asp?toxid=15 (accessed September 26, 2018).
- [69].ATSDR - Toxic Substances - Lead, (n.d.). https://www.atsdr.cdc.gov/substances/toxsubstance.asp?toxid=22 (accessed September 26, 2018).
- [70].ATSDR - Toxicological Profile: Arsenic, (n.d.). https://www.atsdr.cdc.gov/toxprofiles/tp.asp?id=22&tid=3 (accessed September 26, 2018).
- [71].Liew Z, Olsen J, Cui X, Ritz B, Arah OA, Bias from conditioning on live birth in pregnancy cohorts: an illustration based on neurodevelopment in children after prenatal exposure to organic pollutants, Int. J. Epidemiol 44 (2015) 345–354. doi: 10.1093/ije/dyu249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Johns LE, Cooper GS, Galizia A, Meeker JD, Exposure Assessment Issues in Epidemiology Studies of Phthalates, Environ. Int 85 (2015) 27–39. doi: 10.1016/j.envint.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Calafat AM, Contemporary Issues in Exposure Assessment Using Biomonitoring, Curr. Epidemiol. Rep 3 (2016) 145–153. doi: 10.1007/s40471-016-0075-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].O’Brien KM, Whelan DR, Sandler DP, Hall JE, Weinberg CR, Predictors and long-term health outcomes of eating disorders., PloS One 12 (2017) e0181104. doi: 10.1371/journal.pone.0181104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [75].Schisterman EF, Whitcomb BW, Buck Louis GM, Louis TA, Lipid Adjustment in the Analysis of Environmental Contaminants and Human Health Risks, Environ. Health Perspect 113 (2005) 853–857. doi: 10.1289/ehp.7640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Barr DB Wilder LC…Caudill SP…Gonzalez AJ…Needham LL…Pirkle JL, Urinary Creatinine Concentrations in the U.S. Population: Implications for Urinary Biologic Monitoring Measurements, Environ. Health Perspect 113 (2005) 192–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [77].Braun JM, Smith KW, Williams PL, Calafat AM, Berry K, Ehrlich S, Hauser R, Variability of urinary phthalate metabolite and bisphenol A concentrations before and during pregnancy, Environ. Health Perspect 120 (2012) 739–745. doi: 10.1289/ehp.1104139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Fisher M, Arbuckle TE, Mallick R, LeBlanc A, Hauser R, Feeley M, Koniecki D, Ramsay T, Provencher G, Bérubé R, Walker M, Bisphenol A and phthalate metabolite urinary concentrations: Daily and across pregnancy variability, J. Expo. Sci. Environ. Epidemiol 25 (2015) 231–239. doi: 10.1038/jes.2014.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Braun JM, Kalkbrenner AE, Calafat AM, Bernert JT, Ye X, Silva MJ, Barr DB, Sathyanarayana S, Lanphear BP, Variability and predictors of urinary bisphenol A concentrations during pregnancy, Environ. Health Perspect 119 (2011) 131–137. doi: 10.1289/ehp.1002366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Diehl CL, Brost BC, Hogan MC, Elesber AA, Offord KP, Turner ST, Garovic VD, Preeclampsia as a risk factor for cardiovascular disease later in life: validation of a preeclampsia questionnaire, Am. J. Obstet. Gynecol 198 (2008) e11–13. doi: 10.1016/j.ajog.2007.09.038. [DOI] [PubMed] [Google Scholar]
- [81].Yawn BP, Suman VJ, Jacobsen SJ, Maternal Recall of Distant Pregnancy Events, J. Clin. Epidemiol 51 (1998) 399–405. doi: 10.1016/S0895-4356(97)00304-1. [DOI] [PubMed] [Google Scholar]
- [82].Savitz DA, Stein CR, Elston B, Wellenius GA, Bartell SM, Shin H-M, Vieira VM, Fletcher T, Relationship of perfluorooctanoic acid exposure to pregnancy outcome based on birth records in the mid-Ohio Valley, Environ. Health Perspect 120 (2012) 1201–1207. doi: 10.1289/ehp.1104752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].Savitz DA, Stein CR, Bartell SM, Elston B, Gong J, Shin H-M, Wellenius GA, Perfluorooctanoic acid exposure and pregnancy outcome in a highly exposed community, Epidemiol. Camb. Mass 23 (2012) 386–392. doi: 10.1097/EDE.0b013e31824cb93b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Stein CR, Savitz DA, Dougan M, Serum Levels of Perfluorooctanoic Acid and Perfluorooctane Sulfonate and Pregnancy Outcome, Am. J. Epidemiol 170 (2009) 837–846. doi: 10.1093/aje/kwp212. [DOI] [PubMed] [Google Scholar]
- [85].Carwile JL, Mahalingaiah S, Winter MR, Aschengrau A, Prenatal drinking-water exposure to tetrachloroethylene and ischemic placental disease: a retrospective cohort study, Environ. Health Glob. Access Sci. Source 13 (2014) 72. doi: 10.1186/1476-069X-13-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Quach T, Von Behren J, Goldberg D, Layefsky M, Reynolds P, Adverse birth outcomes and maternal complications in licensed cosmetologists and manicurists in California, Int. Arch. Occup. Environ. Health 88 (2015) 823–833. doi: 10.1007/s00420-014-1011-0. [DOI] [PubMed] [Google Scholar]
- [87].Herdt-Losavio ML, Lin S, Druschel CM, Hwang S-A, Mauer MP, Carlson GA, The risk of congenital malformations and other neonatal and maternal health outcomes among licensed cosmetologists, Am. J. Perinatol 26 (2009) 625–631. doi: 10.1055/s-0029-1220787. [DOI] [PubMed] [Google Scholar]
- [88].Savitz DA, Klebanoff MA, Wellenius GA, Jensen ET, Longnecker MP, Persistent organochlorines and hypertensive disorders of pregnancy, Environ. Res 132 (2014) 1–5. doi: 10.1016/j.envres.2014.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Smarr MM, Grantz KL, Zhang C, Sundaram R, Maisog JM, Barr DB, Louis GMB, Persistent organic pollutants and pregnancy complications, Sci. Total Environ 551–552 (2016) 285–291. doi: 10.1016/j.scitotenv.2016.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Eslami B, Malekafzali H, Rastkari N, Rashidi BH, Djazayeri A, Naddafi K, Association of serum concentrations of persistent organic pollutants (POPs) and risk of pre-eclampsia: a case-control study, J. Environ. Health Sci. Eng 14 (2016) 17. doi: 10.1186/s40201-016-0256-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [91].Starling AP, Engel SM, Whitworth KW, Richardson DB, Stuebe AM, Daniels JL, Haug LS, Eggesbø M, Becher G, Sabaredzovic A, Thomsen C, Wilson RE, Travlos GS, Hoppin JA, Baird DD, Longnecker MP, Perfluoroalkyl substances and lipid concentrations in plasma during pregnancy among women in the Norwegian Mother and Child Cohort Study, Environ. Int 62 (2014) 104–112. doi: 10.1016/j.envint.2013.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Murray J, Eskenazi B, Bornman R, Gaspar FW, Crause M, Obida M, Chevrier J, Exposure to DDT and hypertensive disorders of pregnancy among South African women from an indoor residual spraying region: The VHEMBE study, Environ. Res 162 (2018) 49–54. doi: 10.1016/j.envres.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [93].Saunders L, Kadhel P, Costet N, Rouget F, Monfort C, Thomé J-P, Guldner L, Cordier S, Multigner L, Hypertensive disorders of pregnancy and gestational diabetes mellitus among French Caribbean women chronically exposed to chlordecone, Environ. Int 68 (2014) 171–176. doi: 10.1016/j.envint.2014.03.024. [DOI] [PubMed] [Google Scholar]
- [94].Toichuev RM, Zhilova LV, Paizildaev TR, Khametova MS, Rakhmatillaev A, Sakibaev KS, Madykova ZA, Toichueva AU, Schlumpf M, Weber R, Lichtensteiger W, Organochlorine pesticides in placenta in Kyrgyzstan and the effect on pregnancy, childbirth, and newborn health, Environ. Sci. Pollut. Res (2017) 1–10. doi: 10.1007/s11356-017-0962-6. [DOI] [PubMed] [Google Scholar]
- [95].Ledda C, Fiore M, Santarelli L, Bracci M, Mascali G, D’Agati MG, Busà A, Ferrante M, Rapisarda V, Gestational Hypertension and Organophosphorus Pesticide Exposure: A Cross-Sectional Study, BioMed Res. Int 2015 (2015) 280891. doi: 10.1155/2015/280891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Saldana TM, Basso O, Baird DD, Hoppin JA, Weinberg CR, Blair A, Alavanja MCR, Sandler DP, Pesticide exposure and hypertensive disorders during pregnancy, Environ. Health Perspect 117 (2009) 1393–1396. doi: 10.1289/ehp.0900672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [97].Shaw GM, Yang W, Roberts EM, Aghaeepour N, Mayo JA, Weber KA, Maric I, Carmichael SL, Winn VD, Stevenson DK, English PB, Residential agricultural pesticide exposures and risks of preeclampsia, Environ. Res 164 (2018) 546–555. doi: 10.1016/j.envres.2018.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Nordby K-C, Irgens LM, Kristensen P, Immunological exposures in Norwegian agriculture and pre-eclampsia, Paediatr. Perinat. Epidemiol 20 (2006) 462–470. doi: 10.1111/j.1365-3016.2006.00761.x. [DOI] [PubMed] [Google Scholar]
- [99].Nugteren JJ, Snijder CA, Hofman A, Jaddoe VWV, Steegers EAP, Burdorf A, Work-related maternal risk factors and the risk of pregnancy induced hypertension and preeclampsia during pregnancy. The Generation R Study, PloS One 7 (2012) e39263. doi: 10.1371/journal.pone.0039263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Murray J, Eskenazi B, Bornman R, Gaspar FW, Crause M, Obida M, Chevrier J, Exposure to DDT and hypertensive disorders of pregnancy among South African women from an indoor residual spraying region: The VHEMBE study, Environ. Res 162 (2018) 49–54. doi: 10.1016/j.envres.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [101].Leclerc F, Dubois M-F, Aris A, Maternal, placental and fetal exposure to bisphenol A in women with and without preeclampsia, Hypertens. Pregnancy 33 (2014) 341–348. doi: 10.3109/10641955.2014.892607. [DOI] [PubMed] [Google Scholar]
- [102].Cantonwine DE, Meeker JD, Ferguson KK, Mukherjee B, Hauser R, McElrath TF, Urinary Concentrations of Bisphenol A and Phthalate Metabolites Measured during Pregnancy and Risk of Preeclampsia, Environ. Health Perspect 124 (2016) 1651–1655. doi: 10.1289/EHP188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Ye Y, Zhou Q, Feng L, Wu J, Xiong Y, Li X, Maternal serum bisphenol A levels and risk of pre-eclampsia: a nested case–control study, Eur. J. Public Health 27 (2017) 1102–1107. doi: 10.1093/eurpub/ckx148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Warembourg C, Basagaña X, Seminati C, de Bont J, Granum B, Lyon-Caen S, Manzano-Salgado CB, Pin I, Sakhi AK, Siroux V, Slama R, Urquiza J, Vrijheid M, Thomsen C, Casas M, Exposure to phthalate metabolites, phenols and organophosphate pesticide metabolites and blood pressure during pregnancy, Int. J. Hyg. Environ. Health (2018). doi: 10.1016/j.ijheh.2018.12.011. [DOI] [PubMed] [Google Scholar]
- [105].Liu H, Li J, Xia W, Zhang B, Peng Y, Li Y, Zhou Y, Fang J, Zhao H, Jiang Y, Liu W, Sun X, Hu C, Cai Z, Xu S, Blood pressure changes during pregnancy in relation to urinary paraben, triclosan and benzophenone concentrations: A repeated measures study, Environ. Int 122 (2019) 185–192. doi: 10.1016/j.envint.2018.11.003. [DOI] [PubMed] [Google Scholar]
- [106].Werner EF, Braun JM, Yolton K, Khoury JC, Lanphear BP, The association between maternal urinary phthalate concentrations and blood pressure in pregnancy: The HOME Study, Environ. Health 14 (2015). doi: 10.1186/s12940-015-0062-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Chowdhury R, Shah D, Payal AR, Healthy Worker Effect Phenomenon: Revisited with Emphasis on Statistical Methods – A Review, Indian J. Occup. Environ. Med 21 (2017) 2–8. doi: 10.4103/ijoem.IJOEM_53_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [108].Magri J, Sammut M, Savona-Ventura C, Lead and other metals in gestational hypertension, Int. J. Gynecol. Obstet 83 (2003) 29–36. doi: 10.1016/S0020-7292(03)00212-1. [DOI] [PubMed] [Google Scholar]
- [109].Elongi Moyene J-P, Scheers H, Tandu-Umba B, Haufroid V, Buassa-Bu-Tsumbu B, Verdonck F, Spitz B, Nemery B, Preeclampsia and toxic metals: a case-control study in Kinshasa, DR Congo, Environ. Health Glob. Access Sci. Source 15 (2016) 48. doi: 10.1186/s12940-016-0132-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Ismail A, George S, Mohamed AH, Abbas A, Environmental exposure to lead and cadmium in patients with preeclampsia; A case-control study, Asian J. Pharmacol. Toxicol 3 (2015). https://www.researchgate.net/profile/Ahmed_Abbas17/publication/287997959_Environmental_exposure_to_lead_and_cadmium_in_patients_with_preeclampsia_A_case-control_study/links/567c595408ae051f9ae1ad40.pdf. [Google Scholar]
- [111].Kolusari A, Kurdoglu M, Yildizhan R, Adali E, Edirne T, Cebi A, Demir H, Yoruk IH, Catalase activity, serum trace element and heavy metal concentrations, and vitamin A, D and E levels in pre-eclampsia, J. Int. Med. Res 36 (2008) 1335–1341. doi: 10.1177/147323000803600622. [DOI] [PubMed] [Google Scholar]
- [112].Laine JE, Ray P, Bodnar W, Cable PH, Boggess K, Offenbacher S, Fry RC, Placental Cadmium Levels Are Associated with Increased Preeclampsia Risk, PloS One 10 (2015) e0139341. doi: 10.1371/journal.pone.0139341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Maduray K, Moodley J, Soobramoney C, Moodley R, Naicker T, Elemental analysis of serum and hair from pre-eclamptic South African women, J. Trace Elem. Med. Biol 43 (2017) 180–186. doi: 10.1016/j.jtemb.2017.03.004. [DOI] [PubMed] [Google Scholar]
- [114].Wang F, Fan F, Wang L, Ye W, Zhang Q, Xie S, Maternal Cadmium Levels During Pregnancy and the Relationship with Preeclampsia and Fetal Biometric Parameters, Biol. Trace Elem. Res (2018). doi: 10.1007/s12011-018-1312-3. [DOI] [PubMed] [Google Scholar]
- [115].Vigeh M, Yokoyama K, Ramezanzadeh F, Dahaghin M, Sakai T, Morita Y, Kitamura F, Sato H, Kobayashi Y, Lead and other trace metals in preeclampsia: a case-control study in Tehran, Iran, Environ. Res 100 (2006) 268–275. doi: 10.1016/j.envres.2005.05.005. [DOI] [PubMed] [Google Scholar]
- [116].Ebrahim K, Ashtarinezhad A, The Association of Amniotic Fluid Cadmium Levels with the Risk of Preeclampsia, Prematurity and Low Birth Weight, Iran. J. Neonatol. IJN 6 (2015) 1–6. doi: 10.22038/ijn.2015.4482. [DOI] [Google Scholar]
- [117].Sandoval-Carrillo A, Méndez-Hernández EM, Antuna-Salcido EI, Salas-Pacheco SM, Vázquez-Alaniz F, Téllez-Valencia A, Aguilar-Durán M, Barraza-Salas M, Castellanos-Juárez FX, La Llave-León O, Salas-Pacheco JM, Arsenic exposure and risk of preeclampsia in a Mexican mestizo population, BMC Pregnancy Childbirth 16 (2016). doi: 10.1186/s12884-016-0946-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Farzan SF, Chen Y, Wu F, Jiang J, Liu M, Baker E, Korrick SA, Karagas MR, Blood Pressure Changes in Relation to Arsenic Exposure in a U.S. Pregnancy Cohort, Environ. Health Perspect 123 (2015) 999–1006. doi: 10.1289/ehp.1408472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [119].Kwok RK, Mendola P, Liu ZY, Savitz DA, Heiss G, Ling HL, Xia Y, Lobdell D, Zeng D, Thorp JM, Creason JP, Mumford JL, Drinking water arsenic exposure and blood pressure in healthy women of reproductive age in Inner Mongolia, China, Toxicol. Appl. Pharmacol 222 (2007) 337–343. doi: 10.1016/j.taap.2007.04.003. [DOI] [PubMed] [Google Scholar]
- [120].El-Badry A, Rezk M, El-Sayed H, Mercury-induced Oxidative Stress May Adversely Affect Pregnancy Outcome among Dental Staff: A Cohort Study, Int. J. Occup. Environ. Med 9 (2018) 1181-113–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Wells EM, Herbstman JB, Lin YH, Hibbeln JR, Halden RU, Witter FR, Goldman LR, Methyl mercury, but not inorganic mercury, associated with higher blood pressure during pregnancy, Environ. Res 154 (2017) 247–252. doi: 10.1016/j.envres.2017.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [122].Starling AP, Engel SM, Richardson DB, Baird DD, Haug LS, Stuebe AM, Klungsøyr K, Harmon Q, Becher G, Thomsen C, Sabaredzovic A, Eggesbø M, Hoppin JA, Travlos GS, Wilson RE, Trogstad LI, Magnus P, Longnecker MP, Perfluoroalkyl Substances During Pregnancy and Validated Preeclampsia Among Nulliparous Women in the Norwegian Mother and Child Cohort Study, Am. J. Epidemiol 179 (2014) 824–833. doi: 10.1093/aje/kwt432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Ettinger AS, Arbuckle TE, Fisher M, Liang CL, Davis K, Cirtiu C-M, Bélanger P, LeBlanc A, Fraser WD, Arsenic levels among pregnant women and newborns in Canada: Results from the Maternal-Infant Research on Environmental Chemicals (MIREC) cohort, Environ. Res 153 (2017) 8–16. doi: 10.1016/j.envres.2016.11.008. [DOI] [PubMed] [Google Scholar]
- [124].Eslami B, Naddafi K, Rastkari N, Rashidi BH, Djazayeri A, Malekafzali H, Association between serum concentrations of persistent organic pollutants and gestational diabetes mellitus in primiparous women, Environ. Res 151 (2016) 706–712. doi: 10.1016/j.envres.2016.09.002. [DOI] [PubMed] [Google Scholar]
- [125].Vafeiadi M, Roumeliotaki T, Chalkiadaki G, Rantakokko P, Kiviranta H, Fthenou E, Kyrtopoulos SA, Kogevinas M, Chatzi L, Persistent organic pollutants in early pregnancy and risk of gestational diabetes mellitus, Environ. Int 98 (2017) 89–95. doi: 10.1016/j.envint.2016.10.005. [DOI] [PubMed] [Google Scholar]
- [126].Zhang L, Liu X, Meng G, Chi M, Li J, Yin S, Zhao Y, Wu Y, Non-dioxin-like polychlorinated biphenyls in early pregnancy and risk of gestational diabetes mellitus, Environ. Int 115 (2018) 127–132. doi: 10.1016/j.envint.2018.03.012. [DOI] [PubMed] [Google Scholar]
- [127].Shapiro GD, Dodds L, Arbuckle TE, Ashley-Martin J, Ettinger AS, Fisher M, Taback S, Bouchard MF, Monnier P, Dallaire R, Morisset A-S, Fraser W, Exposure to organophosphorus and organochlorine pesticides, perfluoroalkyl substances, and polychlorinated biphenyls in pregnancy and the association with impaired glucose tolerance and gestational diabetes mellitus: The MIREC Study, Environ. Res 147 (2016) 71–81. doi: 10.1016/j.envres.2016.01.040. [DOI] [PubMed] [Google Scholar]
- [128].Valvi D, Monfort N, Ventura R, Casas M, Casas L, Sunyer J, Vrijheid M, Variability and predictors of urinary phthalate metabolites in Spanish pregnant women, Int. J. Hyg. Environ. Health 218 (2015) 220–231. doi: 10.1016/j.ijheh.2014.11.003. [DOI] [PubMed] [Google Scholar]
- [129].Jaacks LM, Barr DB, Sundaram R, Maisog JM, Zhang C, Buck Louis GM, Pre-pregnancy maternal exposure to polybrominated and polychlorinated biphenyls and gestational diabetes: a prospective cohort study, Environ. Health 15 (2016) 11. doi: 10.1186/s12940-016-0092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [130].Liu X, Zhang L, Li J, Meng G, Chi M, Li T, Zhao Y, Wu Y, A nested case-control study of the association between exposure to polybrominated diphenyl ethers and the risk of gestational diabetes mellitus, Environ. Int 119 (2018) 232–238. doi: 10.1016/j.envint.2018.06.029. [DOI] [PubMed] [Google Scholar]
- [131].Zhang C, Sundaram R, Maisog J, Calafat AM, Barr DB, Buck Louis GM, A Prospective Study of Pre-pregnancy Serum Concentrations of Perfluorochemicals and the Risk of Gestational Diabetes, Fertil. Steril 103 (2015) 184–189. doi: 10.1016/j.fertnstert.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [132].Matilla-Santander N, Valvi D, Lopez-Espinosa M-J, Manzano-Salgado CB, Ballester F, Ibarluzea J, Santa-Marina L, Schettgen T, Guxens M, Sunyer J, Vrijheid M, Exposure to Perfluoroalkyl Substances and Metabolic Outcomes in Pregnant Women: Evidence from the Spanish INMA Birth Cohorts, Environ. Health Perspect 125 (2017) 117004. doi: 10.1289/EHP1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [133].Saldana TM, Basso O, Hoppin JA, Baird DD, Knott C, Blair A, Alavanja MCR, Sandler DP, Pesticide exposure and self-reported gestational diabetes mellitus in the Agricultural Health Study, Diabetes Care 30 (2007) 529–534. doi: 10.2337/dc06-1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [134].Valvi D, Oulhote Y, Weihe P, Dalgård C, Bjerve KS, Steuerwald U, Grandjean P, Gestational diabetes and offspring birth size at elevated environmental pollutant exposures, Environ. Int 107 (2017) 205–215. doi: 10.1016/j.envint.2017.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [135].Fisher BG, Frederiksen H, Andersson A-M, Juul A, Thankamony A, Ong KK, Dunger DB, Hughes IA, Acerini CL, Serum Phthalate and Triclosan Levels Have Opposing Associations With Risk Factors for Gestational Diabetes Mellitus, Front. Endocrinol 9 (2018). doi: 10.3389/fendo.2018.00099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [136].Robledo C, Peck JD, Stoner JA, Carabin H, Cowan L, Koch HM, Goodman JR, Is bisphenol-A exposure during pregnancy associated with blood glucose levels or diagnosis of gestational diabetes?, J. Toxicol. Environ. Health A 76 (2013) 865–873. doi: 10.1080/15287394.2013.824395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Shapiro GD, Arbuckle TE, Ashley-Martin J, Fraser WD, Fisher M, Bouchard MF, Monnier P, Morisset A-S, Ettinger AS, Dodds L, Associations between maternal triclosan concentrations in early pregnancy and gestational diabetes mellitus, impaired glucose tolerance, gestational weight gain and fetal markers of metabolic function, Environ. Res 161 (2018) 554–561. doi: 10.1016/j.envres.2017.12.001. [DOI] [PubMed] [Google Scholar]
- [138].Shapiro GD, Dodds L, Arbuckle TE, Ashley-Martin J, Fraser W, Fisher M, Taback S, Keely E, Bouchard MF, Monnier P, Dallaire R, Morisset A, Ettinger AS, Exposure to phthalates, bisphenol A and metals in pregnancy and the association with impaired glucose tolerance and gestational diabetes mellitus: The MIREC study, Environ. Int 83 (2015) 63–71. doi: 10.1016/j.envint.2015.05.016. [DOI] [PubMed] [Google Scholar]
- [139].Ettinger AS, Zota AR, Amarasiriwardena CJ, Hopkins MR, Schwartz J, Hu H, Wright RO, Maternal Arsenic Exposure and Impaired Glucose Tolerance during Pregnancy, Environ. Health Perspect 117 (2009) 1059–1064. doi: 10.1289/ehp0800533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Farzan SF, Gossai A, Chen Y, Chasan-Taber L, Baker E, Karagas M, Maternal arsenic exposure and gestational diabetes and glucose intolerance in the New Hampshire birth cohort study, Environ. Health 15 (2016) 106. doi: 10.1186/s12940-016-0194-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Marie C, Léger S, Guttmann A, Rivière O, Marchiset N, Lémery D, Vendittelli F, Sauvant-Rochat M-P, Exposure to arsenic in tap water and gestational diabetes: A French semi-ecological study, Environ. Res 161 (2018) 248–255. doi: 10.1016/j.envres.2017.11.016. [DOI] [PubMed] [Google Scholar]
- [142].Munoz-Rocha TV, Tamayo Y Ortiz M, Romero M, Pantic I, Schnaas L, Bellinger D, Claus-Henn B, Wright R, Wright RO, Tellez-Rojo MM, Prenatal co-exposure to manganese and depression and 24-months neurodevelopment., Neurotoxicology (2017). doi: 10.1016/j.neuro.2017.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [143].Peng S, Liu L, Zhang X, Heinrich J, Zhang J, Schramm K-W, Huang Q, Tian M, Eqani SAMAS, Shen H, A nested case-control study indicating heavy metal residues in meconium associate with maternal gestational diabetes mellitus risk, Environ. Health 14 (2015). doi: 10.1186/s12940-015-0004-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [144].Xia X, Liang C, Sheng J, Yan S, Huang K, Li Z, Pan W, Tao R, Hao J, Zhu B, Tong S, Tao F, Association between serum arsenic levels and gestational diabetes mellitus: A population-based birth cohort study, Environ. Pollut. Barking Essex 1987 235 (2018) 850–856. doi: 10.1016/j.envpol.2018.01.016. [DOI] [PubMed] [Google Scholar]
- [145].Xing Y, Xia W, Zhang B, Zhou A, Huang Z, Zhang H, Liu H, Jiang Y, Hu C, Chen X, Xu S, Li Y, Relation between cadmium exposure and gestational diabetes mellitus, Environ. Int 113 (2018) 300–305. doi: 10.1016/j.envint.2018.01.001. [DOI] [PubMed] [Google Scholar]
- [146].Quach T, Tsoh J, Le G, Le M, Pham A, Fu L, Luu V, Ngo K, Reynolds P, Identifying and understanding the role of key stakeholders in promoting worker health and safety in nail salons, J Health Care Poor Underserved 26 (2015) 104–15. doi: 10.1353/hpu.2015.0060. [DOI] [PubMed] [Google Scholar]
- [147].Xia X, Liang C, Sheng J, Yan S, Huang K, Li Z, Pan W, Tao R, Hao J, Zhu B, Tong S, Tao F, Association between serum arsenic levels and gestational diabetes mellitus: A population-based birth cohort study, Environ. Pollut. Barking Essex 1987 235 (2018) 850–856. doi: 10.1016/j.envpol.2018.01.016. [DOI] [PubMed] [Google Scholar]
- [148].Rodgers KM, Udesky JO, Rudel RA, Brody JG, Environmental chemicals and breast cancer: An updated review of epidemiological literature informed by biological mechanisms, Environ. Res 160 (2018) 152–182. doi: 10.1016/j.envres.2017.08.045. [DOI] [PubMed] [Google Scholar]
- [149].Beral V, Colwell L, Randomised trial of high doses of stilboestrol and ethisterone in pregnancy: long-term follow-up of mothers., Br Med J 281 (1980) 1098–1101. doi: 10.1136/bmj.281.6248.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [150].Bibbo M, Haenszel WM, Wied GL, Hubby M, Herbst AL, A Twenty-Five-Year Follow-up Study of Women Exposed to Diethylstilbestrol during Pregnancy, N. Engl. J. Med 298 (1978) 763–767. doi: 10.1056/NEJM197804062981403. [DOI] [PubMed] [Google Scholar]
- [151].Colton T, Greenberg ER, Noller K, Resseguie L, Van Bennekom C, Heeren T, Zhang Y, Breast cancer in mothers prescribed diethylstilbestrol in pregnancy. Further follow-up, JAMA 269 (1993) 2096–2100. [PubMed] [Google Scholar]
- [152].Giusti RM, Iwamoto K, Hatch EE, Diethylstilbestrol revisited: a review of the long-term health effects, Ann. Intern. Med 122 (1995) 778–788. [DOI] [PubMed] [Google Scholar]
- [153].Greenberg ER, Barnes AB, Resseguie L, Barrett JA, Burnside S, Lanza LL, Neff RK, Stevens M, Young RH, Colton T, Breast Cancer in Mothers Given Diethylstilbestrol in Pregnancy, N. Engl. J. Med 311 (1984) 1393–1398. doi: 10.1056/NEJM198411293112201. [DOI] [PubMed] [Google Scholar]
- [154].Titus-Ernstoff L, Troisi R, Hatch EE, Palmer JR, Wise LA, Ricker W, Hyer M, Kaufman R, Noller K, Strohsnitter W, Herbst AL, Hartge P, Hoover RN, Mortality in women given diethylstilbestrol during pregnancy, Br. J. Cancer 95 (2006) 107–111. doi: 10.1038/sj.bjc.6603221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Titus-Ernstoff L, Hatch EE, Hoover RN, Palmer J, Greenberg ER, Ricker W, Kaufman R, Noller K, Herbst AL, Colton T, Hartge P, Long-term cancer risk in women given diethylstilbestrol (DES) during pregnancy, Br. J. Cancer 84 (2001) 126–133. doi: 10.1054/bjoc.2000.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [156].Veurink M, Koster M, de J. den. Berg LTW, The History of DES, Lessons to be Learned, Pharm. World Sci 27 (2005) 139–143. doi: 10.1007/s11096-005-3663-z. [DOI] [PubMed] [Google Scholar]
- [157].Bonefeld-Jørgensen EC, Long M, Fredslund SO, Bossi R, Olsen J, Breast cancer risk after exposure to perfluorinated compounds in Danish women: a case-control study nested in the Danish National Birth Cohort, Cancer Causes Control CCC 25 (2014) 1439–1448. doi: 10.1007/s10552-014-0446-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Cohn BA, Terry MB, Plumb M, Cirillo PM, Exposure to polychlorinated biphenyl (PCB) congeners measured shortly after giving birth and subsequent risk of maternal breast cancer before age 50, Breast Cancer Res. Treat 136 (2012) 267–275. doi: 10.1007/s10549-012-2257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [159].Cohn BA, Wolff MS, Cirillo PM, Sholtz RI, DDT and breast cancer in young women: new data on the significance of age at exposure, Environ. Health Perspect 115 (2007) 1406–1414. doi: 10.1289/ehp.10260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [160].Cohn BA, Terry MB, Plumb M, Cirillo PM, Exposure to polychlorinated biphenyl (PCB) congeners measured shortly after giving birth and subsequent risk of maternal breast cancer before age 50, Breast Cancer Res. Treat 136 (2012) 267–275. doi: 10.1007/s10549-012-2257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [161].Bonefeld-Jørgensen EC, Long M, Fredslund SO, Bossi R, Olsen J, Breast cancer risk after exposure to perfluorinated compounds in Danish women: a case–control study nested in the Danish National Birth Cohort, Cancer Causes Control 25 (2014) 1439–1448. doi: 10.1007/s10552-014-0446-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [162].Longtine MS, Chen B, Odibo AO, Zhong Y, Nelson DM, Villous trophoblast apoptosis is elevated and restricted to cytotrophoblasts in pregnancies complicated by preeclampsia, IUGR, or preeclampsia with IUGR, Placenta 33 (2012) 352–359. doi: 10.1016/j.placenta.2012.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [163].Morice L, Benaîtreau D, Dieudonné M-N, Morvan C, Serazin V, de Mazancourt P, Pecquery R, Dos Santos E, Antiproliferative and proapoptotic effects of bisphenol A on human trophoblastic JEG-3 cells, Reprod. Toxicol 32 (2011) 69–76. doi: 10.1016/j.reprotox.2011.05.003. [DOI] [PubMed] [Google Scholar]
- [164].Zhou P, Luo X, Qi H-B, Zong W-J, Zhang H, Liu D-D, Li Q-S, The expression of pentraxin 3 and tumor necrosis factor-alpha is increased in preeclamptic placental tissue and maternal serum, Inflamm. Res. Off. J. Eur. Histamine Res. Soc. Al 61 (2012) 1005–1012. doi: 10.1007/s00011-012-0507-x. [DOI] [PubMed] [Google Scholar]
- [165].Gao F, Hu W, Li Y, Shen H, Hu J, Mono-2-ethylhexyl phthalate inhibits human extravillous trophoblast invasion via the PPARγ pathway, Toxicol. Appl. Pharmacol 327 (2017) 23–29. doi: 10.1016/j.taap.2017.04.014. [DOI] [PubMed] [Google Scholar]
- [166].Amraoui W, Adjabi N, Bououza F, Boumendjel M, Taibi F, Boumendjel A, Abdennour C, Messarah M, Modulatory Role of Selenium and Vitamin E, Natural Antioxidants, against Bisphenol A-Induced Oxidative Stress in Wistar Albinos Rats, Toxicol. Res 34 (2018) 231–239. doi: 10.5487/TR.2018.34.3.231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [167].Cho YJ, Park SB, Han M, Di-(2-ethylhexyl)-phthalate induces oxidative stress in human endometrial stromal cells in vitro, Mol. Cell. Endocrinol 407 (2015) 9–17. doi: 10.1016/j.mce.2015.03.003. [DOI] [PubMed] [Google Scholar]
- [168].Pérez-Albaladejo E, Fernandes D, Lacorte S, Porte C, Comparative toxicity, oxidative stress and endocrine disruption potential of plasticizers in JEG-3 human placental cells, Toxicol. Vitro Int. J. Publ. Assoc. BIBRA 38 (2017) 41–48. doi: 10.1016/j.tiv.2016.11.003. [DOI] [PubMed] [Google Scholar]
- [169].Xu H, Shao X, Zhang Z, Zou Y, Wu X, Yang L, Oxidative stress and immune related gene expression following exposure to di-n-butyl phthalate and diethyl phthalate in zebrafish embryos, Ecotoxicol. Environ. Saf 93 (2013) 39–44. doi: 10.1016/j.ecoenv.2013.03.038. [DOI] [PubMed] [Google Scholar]
- [170].Ferguson KK, Cantonwine DE, McElrath TF, Mukherjee B, Meeker JD, Repeated measures analysis of associations between urinary bisphenol-A concentrations and biomarkers of inflammation and oxidative stress in pregnancy, Reprod. Toxicol. Elmsford N 66 (2016) 93–98. doi: 10.1016/j.reprotox.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [171].Watkins DJ, Ferguson KK, Anzalota Del Toro LV, Alshawabkeh AN, Cordero JF, Meeker JD, Associations between urinary phenol and paraben concentrations and markers of oxidative stress and inflammation among pregnant women in Puerto Rico, Int. J. Hyg. Environ. Health 218 (2015) 212–219. doi: 10.1016/j.ijheh.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [172].Ferguson KK, McElrath TF, Cantonwine DE, Mukherjee B, Meeker JD, Phthalate metabolites and bisphenol-A in association with circulating angiogenic biomarkers across pregnancy, Placenta 36 (2015) 699–703. doi: 10.1016/j.placenta.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [173].Brooks SA, Martin E, Smeester L, Grace MR, Boggess K, Fry RC, miRNAs as common regulators of the transforming growth factor (TGF)-β pathway in the preeclamptic placenta and cadmium-treated trophoblasts: Links between the environment, the epigenome and preeclampsia, Food Chem. Toxicol 98 (2016) 50–57. doi: 10.1016/j.fct.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [174].Brooks SA, Fry RC, Cadmium inhibits placental trophoblast cell migration via miRNA regulation of the transforming growth factor beta (TGF-β) pathway, Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc 109 (2017) 721–726. doi: 10.1016/j.fct.2017.07.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [175].Jacobo-Estrada T, Santoyo-Sánchez M, Thévenod F, Barbier O, Cadmium Handling, Toxicity and Molecular Targets Involved during Pregnancy: Lessons from Experimental Models, Int. J. Mol. Sci 18 (2017). doi: 10.3390/ijms18071590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [176].Wang F, Zhang Q, Zhang X, Luo S, Ye D, Guo Y, Chen S, Huang Y, Preeclampsia induced by cadmium in rats is related to abnormal local glucocorticoid synthesis in placenta, Reprod. Biol. Endocrinol. RBE 12 (2014). doi: 10.1186/1477-7827-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [177].Qing X, Redecha PB, Burmeister MA, Tomlinson S, D’Agati VD, Davisson RL, Salmon JE, Targeted inhibition of complement activation prevents features of preeclampsia in mice, Kidney Int 79 (2011) 331–339. doi: 10.1038/ki.2010.393. [DOI] [PubMed] [Google Scholar]
- [178].Søfteland L, Petersen K, Stavrum A-K, Wu T, Olsvik PA, Hepatic in vitro toxicity assessment of PBDE congeners BDE47, BDE153 and BDE154 in Atlantic salmon (Salmo salar L.), Aquat. Toxicol 105 (2011) 246–263. doi: 10.1016/j.aquatox.2011.03.012. [DOI] [PubMed] [Google Scholar]
- [179].Heindel JJ, Blumberg B, Cave M, Machtinger R, Mantovani A, Mendez MA, Nadal A, Palanza P, Panzica G, Sargis R, Vandenberg LN, vom Saal F, Metabolism disrupting chemicals and metabolic disorders, Reprod. Toxicol 68 (2017) 3–33. doi: 10.1016/j.reprotox.2016.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [180].Karandrea S, Yin H, Liang X, Heart EA, BDE-47 and BDE-85 stimulate insulin secretion in INS-1 832/13 pancreatic β-cells through the thyroid receptor and Akt, Environ. Toxicol. Pharmacol 56 (2017) 29–34. doi: 10.1016/j.etap.2017.08.030. [DOI] [PubMed] [Google Scholar]
- [181].Hoppe AA, Carey GB, Polybrominated Diphenyl Ethers as Endocrine Disruptors of Adipocyte Metabolism, Obesity 15 (2007) 2942–2950. doi: 10.1038/oby.2007.351. [DOI] [PubMed] [Google Scholar]
- [182].Feige JN, Gelman L, Rossi D, Zoete V, Metivier R, Tudor C, Anghel SI, Grosdidier A, Lathion C, Engelborghs Y, Michielin O, Wahli W, Desvergne B, The Endocrine Disruptor Monoethyl-hexyl-phthalate Is a Selective Peroxisome Proliferator-activated Receptor Modulator That Promotes Adipogenesis, J. Biol. Chem 282 (2007) 19152–19166. doi: 10.1074/jbc.M702724200. [DOI] [PubMed] [Google Scholar]
- [183].Desvergne B, Feige JN, Casals-Casas C, PPAR-mediated activity of phthalates: A link to the obesity epidemic?, Mol. Cell. Endocrinol 304 (2009) 43–48. doi: 10.1016/j.mce.2009.02.017. [DOI] [PubMed] [Google Scholar]
- [184].Yan S, Zhang H, Zheng F, Sheng N, Guo X, Dai J, Perfluorooctanoic acid exposure for 28 days affects glucose homeostasis and induces insulin hypersensitivity in mice, Sci. Rep 5 (2015) 11029. doi: 10.1038/srep11029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [185].Qiu T, Chen M, Sun X, Cao J, Feng C, Li D, Wu W, Jiang L, Yao X, Perfluorooctane sulfonate-induced insulin resistance is mediated by protein kinase B pathway, Biochem. Biophys. Res. Commun 477 (2016) 781–785. doi: 10.1016/j.bbrc.2016.06.135. [DOI] [PubMed] [Google Scholar]
- [186].Caër C, Rouault C, Roy TL, Poitou C, Aron-Wisnewsky J, Torcivia A, Bichet J-C, Clément K, Guerre-Millo M, André S, Immune cell-derived cytokines contribute to obesity-related inflammation, fibrogenesis and metabolic deregulation in human adipose tissue, Sci. Rep 7 (2017) 3000. doi: 10.1038/s41598-017-02660-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [187].DeWitt JC, Peden-Adams MM, Keller JM, Germolec DR, Immunotoxicity of Perfluorinated Compounds: Recent Developments, Toxicol. Pathol 40 (2012) 300–311. doi: 10.1177/0192623311428473. [DOI] [PubMed] [Google Scholar]
- [188].Lau C, Anitole K, Hodes C, Lai D, Pfahles-Hutchens A, Seed J, Perfluoroalkyl Acids: A Review of Monitoring and Toxicological Findings, Toxicol. Sci 99 (2007) 366–394. doi: 10.1093/toxsci/kfm128. [DOI] [PubMed] [Google Scholar]
- [189].Skuladottir M, Ramel A, Rytter D, Haug LS, Sabaredzovic A, Bech BH, Henriksen TB, Olsen SF, Halldorsson TI, Examining confounding by diet in the association between perfluoroalkyl acids and serum cholesterol in pregnancy, Environ. Res 143 (2015) 33–38. doi: 10.1016/j.envres.2015.09.001. [DOI] [PubMed] [Google Scholar]
- [190].Tseng C-H, The potential biological mechanisms of arsenic-induced diabetes mellitus, Toxicol. Appl. Pharmacol 197 (2004) 67–83. doi: 10.1016/j.taap.2004.02.009. [DOI] [PubMed] [Google Scholar]
- [191].Martin EM, Stýblo M, Fry RC, Genetic and epigenetic mechanisms underlying arsenic-associated diabetes mellitus: a perspective of the current evidence, Epigenomics 9 (2017) 701–710. doi: 10.2217/epi-2016-0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [192].Huang CF, Chen YW, Yang CY, Tsai KS, Yang RS, Liu SH, Arsenic and diabetes: Current perspectives, Kaohsiung J. Med. Sci 27 (2011) 402–410. doi: 10.1016/j.kjms.2011.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [193].Hill DS, Wlodarczyk BJ, Mitchell LE, Finnell RH, Arsenate-induced maternal glucose intolerance and neural tube defects in a mouse model, Toxicol. Appl. Pharmacol 239 (2009) 29–36. doi: 10.1016/j.taap.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [194].Sung T-C, Huang J-W, Guo H-R, Association between Arsenic Exposure and Diabetes: A Meta-Analysis, BioMed Res. Int (2015). doi: 10.1155/2015/368087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [195].Vorderstrasse BA, Fenton SE, Bohn AA, Cundiff JA, Lawrence BP, A Novel Effect of Dioxin: Exposure during Pregnancy Severely Impairs Mammary Gland Differentiation The research in this article has been reviewed by the National Health and Environmental Effects Research Laboratory, U.S. EPA and approved for publication. Approval does not signify that the contents necessarily reflect the views and policies of the agency, nor does mention of trade names or commercial products constitute endorsement or recommendation for use. Portions of these data were presented at the 42nd annual meeting of the Society of Toxicology, March 2003, Salt Lake City, UT., Toxicol. Sci 78 (2004) 248–257. doi: 10.1093/toxsci/kfh062. [DOI] [PubMed] [Google Scholar]
- [196].White SS, Calafat AM, Kuklenyik Z, Villanueva L, Zehr RD, Helfant L, Strynar MJ, Lindstrom AB, Thibodeaux JR, Wood C, Fenton SE, Gestational PFOA exposure of mice is associated with altered mammary gland development in dams and female offspring, Toxicol. Sci. Off. J. Soc. Toxicol 96 (2007) 133–144. doi: 10.1093/toxsci/kfl177. [DOI] [PubMed] [Google Scholar]
- [197].LaPlante CD, Bansal R, Dunphy KA, Jerry DJ, Vandenberg LN, Oxybenzone Alters Mammary Gland Morphology in Mice Exposed During Pregnancy and Lactation, J. Endocr. Soc 2 (2018) 903–921. doi: 10.1210/js.2018-00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [198].Wang S-L, Chang Y-C, Chao H-R, Li C-M, Li L-A, Lin L-Y, Päpke O, Body burdens of polychlorinated dibenzo-p-dioxins, dibenzofurans, and biphenyls and their relations to estrogen metabolism in pregnant women, Environ. Health Perspect 114 (2006) 740–745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [199].Cohn BA, Cirillo PM, Hopper BR, Siiteri PK, Third Trimester Estrogens and Maternal Breast Cancer: Prospective Evidence, J. Clin. Endocrinol. Metab 102 (2017) 3739–3748. doi: 10.1210/jc.2016-3476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [200].Fortner RT, Schock H, Kaaks R, Lehtinen M, Pukkala E, Lakso H-Å, Tanner M, Kallio R, Joensuu H, Grankvist K, Zeleniuch-Jacquotte A, Toniolo P, Lundin E, Surcel H-M, Early pregnancy sex steroids and maternal breast cancer: a nested case-control study, Cancer Res 74 (2014) 6958–6967. doi: 10.1158/0008-5472.CAN-14-2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [201].Ham SA, Yoo T, Lee WJ, Hwang JS, Hur J, Paek KS, Lim D-S, Han SG, Lee C-H, Seo HG, ADAMTS1-mediated targeting of TSP-1 by PPARδ suppresses migration and invasion of breast cancer cells, Oncotarget 8 (2017) 94091–94103. doi: 10.18632/oncotarget.21584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [202].Lee K-H, Shu X-O, Gao Y-T, Ji B-T, Yang G, Blair A, Rothman N, Zheng W, Chow W-H, Kang D, Breast cancer and urinary biomarkers of polycyclic aromatic hydrocarbon and oxidative stress in the Shanghai Women’s Health Study, Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol 19 (2010) 877–883. doi: 10.1158/1055-9965.EPI-09-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [203].Martinez-Campa C, Gonzalez A, Mediavilla MD, Alonso-Gonzalez C, Alvarez-Garcia V, Sanchez-Barcelo EJ, Cos S, Melatonin inhibits aromatase promoter expression by regulating cyclooxygenases expression and activity in breast cancer cells, Br. J. Cancer 101 (2009) 1613–1619. doi: 10.1038/sj.bjc.6605336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [204].Adibi JJ, Hauser R, Williams PL, Whyatt RM, Thaker HM, Nelson H, Herrick R, Bhat HK, Placental biomarkers of phthalate effects on mRNA transcription: application in epidemiologic research, Env. Health 8 (2009) 20. doi: 10.1186/1476-069x-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [205].Li Q, Kappil MA, Li A, Dassanayake PS, Darrah TH, Friedman AE, Friedman M, Lambertini L, Landrigan P, Stodgell CJ, Xia Y, Nanes JA, Aagaard KM, Schadt EE, Murray JC, Clark EB, Dole N, Culhane J, Swanson J, Varner M, Moye J, Kasten C, Miller RK, Chen J, Exploring the associations between microRNA expression profiles and environmental pollutants in human placenta from the National Children’s Study (NCS), Epigenetics 10 (2015) 793–802. doi: 10.1080/15592294.2015.1066960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [206].Moore Simas TA, Crawford SL, Bathgate S, Yan J, Robidoux L, Moore M, Maynard SE, Angiogenic biomarkers for prediction of early preeclampsia onset in high-risk women, J. Matern.-Fetal Neonatal Med. Off. J. Eur. Assoc. Perinat. Med. Fed. Asia Ocean. Perinat. Soc. Int. Soc. Perinat. Obstet 27 (2014) 1038–1048. doi: 10.3109/14767058.2013.847415. [DOI] [PubMed] [Google Scholar]
- [207].Veglia F, Matullo G, Vineis P, Bulky DNA adducts and risk of cancer: a meta-analysis, Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol 12 (2003) 157–160. [PubMed] [Google Scholar]