Abstract
Background.
The relation of lifetime drinking trajectories to coronary heart disease is not well understood.
Methods.
Cases hospitalized for a non-fatal acute myocardial infarction (AMI) and healthy population-based controls matched on age and sex completed a physical exam and an interview covering known AMI risk factors and a detailed lifetime drinking history. Distinct lifetime drinking trajectories based on ounces of ethanol consumed per decade between ages 10 to 59 years were derived and characterized according to lifetime drinking patterns associated with each. Sex-specific multiple logistic regression analyses were conducted to estimate AMI risk among participants who never drank regularly compared to lifetime drinking trajectories and risk associated with distinct trajectories among former and current drinkers.
Results.
Two lifetime drinking trajectories were derived, early peak and stable. Early peak trajectories were characterized by earlier onset of regular drinking, less frequent drinking, more drinks per drinking day, fewer total drinks, more frequent drunkenness per drinking year, and reduced alcohol intake or abstention by middle age. Never drinking regularly, reported by significantly more women than men, was associated with significantly higher AMI risk than stable lifetime drinking trajectories among men and in the sex-combined analysis of former drinkers only. Compared to stable lifetime drinking trajectories, early peak trajectories were associated with significantly higher AMI risk among male former drinkers, among sex-combined former drinkers, and among female current drinkers.
Conclusions.
Epidemiological studies of alcohol and health in populations over age 35 may have underestimated the impact of heavy episodic drinking during adolescence and emerging adulthood on the cardiovascular system.
Keywords: lifetime drinking trajectories, acute myocardial infarction, case-control study, gender differences
Introduction
A consistent finding in the literature on coronary heart disease (CHD) is that risk is lower among moderate drinkers than among nondrinkers or heavy drinkers, suggesting a protective effect of moderate drinking (Kloner and Rezkalla 2007, O’Keefe, DiNicolantonio et al. 2018). Nevertheless, the relationship between alcohol consumption and CHD remains controversial, both because the relationship is complicated and because alcohol drinking is a complex behavior that is challenging to assess and analyze with respect to chronic conditions such as heart disease that develop over the course of a lifetime. Alcohol intake is associated both with potentially beneficial effects on CHD risk factors such as lipoprotein profiles and blood clotting factors (Rimm, Williams et al. 1999), and with potentially detrimental effects on others, such as blood pressure (Roerecke, Kaczorowski et al. 2017), and these effects may be both acute and cumulative. To investigate the cumulative effects of alcohol on CHD requires some method of estimating exposure over the lifetime. Much of the available literature is based on cross-sectional analyses of data from prospective studies of populations middle-aged and older whose alcohol intake was assessed at the time of recruitment. These analyses assume that drinking habits are relatively stable, an assumption that has been challenged by investigations of lifespan drinking trajectories indicating that alcohol consumption changes markedly over the lifetime, particularly during adolescence and emerging adulthood (Gruenewald, Russell et al. 2002, Britton, Ben-Shlomo et al. 2015), periods of the lifetime drinking history that have been rarely examined with respect to CHD.
In addition to the amount of alcohol consumed, the pattern of consumption moderates its impact on CHD (Rehm, Sempos et al. 2003), a factor ignored in much of the literature. An analysis employing a mathematically-derived, linear alcohol dose-response model found that risk of non-fatal acute myocardial infarction (AMI) was inversely related to drinking frequency, but positively related to dosage, a measure of the extent to which individuals have more than one drink on days when they drink (Russell, Chu et al. 2009). This is consistent with findings that associate higher CHD risk with irregular heavy drinking patterns (Roerecke and Rehm 2010). Irregular heavy drinking patterns, such as binge drinking, are most prevalent during adolescence and emerging adulthood (Lee and Sher 2018), a period that may be completely overlooked in cohort studies that assess alcohol intake prospectively in subjects recruited when they are already entering middle age. Given that much alcohol-related mortality takes place prior to the age at which participants enter most cohort studies, this may bias the enrollment of subjects at risk for alcohol-related CVD (Naimi, Stadtmueller et al. 2019).
Much of the controversy over epidemiological evidence for a protective effect of moderate drinking is related to the definition of nondrinking comparison groups. Few previous studies of coronary heart disease have assessed lifetime drinking patterns in enough detail to differentiate between lifetime abstainers and former drinkers, and use of either as a comparison group for drinkers has been questioned on the basis of unadjusted confounding and reverse causation (Fillmore, Stockwell et al. 2007, Chikritzhs, Fillmore et al. 2009, Zhao, Stockwell et al. 2017). Reverse causation could occur if poor health kept some individuals from ever drinking alcohol (lifetime abstainers) and motivated others to quit drinking (former drinkers) (Shaper, Wannamethee et al. 1988). The effect of poor health on drinking is evident even in adults younger than 35 years and would bias the relation between health outcomes and abstention assessed in cohorts enrolled in studies.at age 35 years and older (Ng Fat and Shelton 2012). In addition, to the extent that drinking alcohol is normative behavior in a given population, lifetime abstainers may differ from drinkers in ways that influence CHD, but are not controlled for in comparisons with moderate drinkers (Naimi, Brown et al. 2005).
Further doubt has been case on the cardioprotective effects of moderate drinking by findings from Mendelian randomization studies (Toma, Pare et al. 2017). Mendelian randomization studies address issues related to confounding and reverse causation by employing variants of alcohol metabolism that influence alcohol consumption but are not related to potential confounders of the relation between alcohol consumption and CVD risk or susceptible to reverse causality (Au Yeung, Jiang et al. 2013). A meta-analysis of 56 epidemiological studies indicated that individuals whose genetic makeup predisposed them to drink less were at lower risk for CHD even among those reporting low, moderate alcohol intakes (Holmes, Dale et al. 2014). Shortcomings related to cross-sectional analyses based on a single measure of alcohol intake were addressed in a recent meta-analysis of six cohort studies that investigated the relation of drinking trajectories to coronary heart disease. These trajectories were based on three measures of alcohol intake made over a ten-year period for individuals all of whom were age 35 years or older at the time of the first assessment (O’Neill, Britton et al. 2018). The retrospective case-control approach taken in the Western New York Health Study (WNYHS) extends this research by examining lifetime drinking trajectories based on assessments of alcohol consumption patterns over participants’ entire drinking careers as they relate to acute non-fatal myocardial infarction (AMI) among former and current drinkers.
MATERIALS AND METHODS
Data for the present study were obtained from the Western New York Health Study (WNYHS) conducted between 1996 and 2001 (Trevisan, Dorn et al. 2004, Dorn, Hovey et al. 2007). Cases (n = 1,197) were recruited from among patients discharged alive from hospitals in Erie and Niagara Counties (Western New York State) with a diagnosis of incident myocardial infarction. Healthy controls from Erie and Niagara Counties (n = 2,850) were randomly selected using lists of licensed drivers for those ages 35 to 64 and lists from the Health Care Financing Association for those ages 65 to 69. Exclusion criteria were self-reported history of cardiovascular disease (prior myocardial infarction, coronary artery bypass graft surgery, angioplasty or diagnosed angina pectoris, or stroke) or cancer. Participation rates were 64.3% for cases and 59.5% for controls; a brief survey of non-participants indicated no serious response bias (data available upon request).
Participants completed a self-administered questionnaire and were invited to the Center for Preventive Medicine at the University at Buffalo for an interview and physical exam that lasted an average of 2.5 hours, at the outset of which a signed informed consent was obtained. The self-administered questionnaire covered demographical information, a medical history, a semi-quantitative food-frequency questionnaire on usual dietary intake during the prior 12 to 24 months (prior to AMI for controls and prior to interview for controls), and a lifetime history of physical activity. The interview assessed alcohol drinking patterns and cigarette use over the lifetime and during the prior 12 to 24 months. A blood sample was obtained for determination of routine chemistry between 7:30 and 9:30 A.M. after fasting for 8 to 12 hours.
Assessment of Lifetime Alcohol Drinking Patterns
Lifetime alcohol drinking patterns were assessed using a computer-assisted personal interview to administer the Cognitive Lifetime Drinking History (CLDH) (Russell, Marshall et al. 1997). A Calendar of Life Events was used to improve recall. We first defined the general shape of the lifetime drinking profile based on age regular drinking (once a month for at least six months) was initiated, ages when drinking changed, and the nature of the change (i.e., did it increase, decrease, or did regular drinking stop). This enabled us to define periods of abstinence and periods during which drinking patterns were relatively homogeneous. We defined patterns of drinking within these relatively homogeneous periods by assessing usual quantity and frequency of intake during a typical four-week period for specific days of the week (Fridays, Saturdays, Sundays, and weekdays) and days when more than usual amounts were consumed. Participants used models to define their drink size for each beverage drunk during the interval (beer, wine, and/or liquor), and they were asked what proportion of their drinks came from each type of alcoholic beverage drunk, taking variability in alcohol content of beer and wine into consideration. Also assessed for each interval was frequency of intoxication (defined as “times you drank enough to get drunk or very high—your speech was slurred, or you were unsteady on your feet”).
We defined three groups based on lifetime drinking patterns: 1) abstainers--participants who never drank more than 12 drinks (lifetime abstainers) or who never drank more than 12 drinks during a period of 12 months (very light drinkers); 2) former drinkers—regular drinkers whose drinking changed and did not continue having at least one drink a month and who did not resume regular drinking; and 3) current drinkers—regular drinkers who were still drinking within the prior 24 months. Very light drinkers were combined with lifetime abstainers because lifetime abstention was rare in our population (4.1% of women and 1.7% of men) and because we thought such very light drinking was unlikely to significantly impact the cardiovascular system.
Lifetime drinking variables were derived for former and current regular drinkers, as follows:
Total years of drinking: Years between beginning and stopping regular drinking minus years of abstinence.
Total volume of alcohol consumed (standard drinks): Data on drink size in ounces, drinks per drinking day, drinking days, beverage type, and ethanol content of beverage type were used to estimate total volume of ethanol in ounces consumed over each drinking interval and summed over the lifetime. Total ounces of ethanol was divided by 0.5 to express total consumption in terms of standard drinks (e.g., 12 fluid ounces of beer, 5 fluid ounces of wine, or 1.5 fluid ounces of 80-proof distilled spirits) containing approximately 12 grams of alcohol.
Lifetime drinking frequency: Sum of drinking days over all drinking intervals.
Lifetime drinking intensity (drinks per drinking day): Total lifetime drinks divided by lifetime drinking days.
Frequency of intoxication per drinking year: Sum of frequency of intoxication over all drinking intervals divided by total drinking years.
Episodic heavy drinking per drinking year: Sum of days upon which respondents reported having four or more drinks over all drinking intervals divided by total drinking years.
Lifetime drinking trajectories: Lifetime drinking trajectories were defined using a group-based modeling approach for identifying distinctive clusters of individual trajectories within a population and profiling the characteristics of individuals within the clusters (Nagin 1999, Jones, Nagin et al. 2001, Nagin and Tremblay 2001).
Assessment of Current Alcohol Drinking Patterns
Current drinking was assessed using CLDH questions on alcohol intake during the period 12 to 24 months prior to the AMI for cases and 12 to 24 months prior to the interview for controls. Data were used to define the following variables: total drinking days and number of drinks per drinking day in a typical 28-day period, total drinks consumed in 12 months, and frequency of getting drunk in 12 months.
Measurements of Potential Confounders
Physical activity.
Average hours of strenuous physical activity per week during the lifetime. Participants used a Calendar of Lifetime Events to assist them in recalling how many hours per week they regularly did strenuous leisure time physical activity or exercise, vigorous household chores, or manual yard work during seven age periods 10–13, 14–18, 19–22, 23–34, 35–50, 51–64, and over 65 years. The total hours for lifetime strenuous physical activity were obtained by summing hours for each age period and dividing by the sum of weeks of life for each age period.
Dietary intake.
Diet data for the prior 12 to 24 months were collected using the National Cancer Institute (NCI) semi-quantitative food frequency questionnaire (Block, Woods et al. 1990). Dietary fiber intake per 1000 kcal and percent calories from saturated fat were used to represent potential confounding from diet.
Cigarette smoking.
Lifetime pack-years of cigarette smoking was estimated from data on average cigarettes smoked per day during decades of life, corrected for times participants did not smoke for more than 24 hours. Smoking status was defined as never, former, or current smoker.
Body Mass Index: Weight (kg)/height (m2). Weight was measured with a beam balance scale, and height by tape measure, according to a standardized protocol.
Statistical Analysis
Data were analyzed using SAS version 9.1 (SAS Insitute Inc., 2004). Comparison for continuous variables by ANOVA and by Chi-square test for categorical variables were performed. Probability values for mean (SD) differences were determined by Student’s t-tests, and those for variables with a skewed distribution, expressed as medians (interquartile range), were determined by Wilcoxon’s rank-sum test. A significance level of α=0.017 (approximately 0.05/3) for each separate test was used to guarantee an overall significance level of no more than 0.05 (Bonferroni correction).
Lifetime drinking trajectories were defined using the SAS procedure, PROC TRAJ. In this procedure, models specifying different numbers of groups are systematically compared via the Bayesian Information Criterion (BIC) to determine the optimal number of groups or trajectory classes. Once the optimal number of groups is determined, the probability of everyone’s membership in each trajectory class is computed. Data were prepared for analysis by dividing the total adjusted ounces of ethanol for each decade by lifetime average intake, and the ratio was logarithmically transformed. This standardization process is designed to minimize the influence of the inter-individual lifetime drinking level variability on constructing distinct trajectory groups. Since ethanol consumption in the first and seventh decades was quite low and did not vary much in the sample, only data for the second through sixth decades (10 to 59 years) were used for the trajectory analysis.
General linear modeling was performed to examine differences in drinking patterns between trajectory groups by sex, controlling for age and race. Multiple logistic regression was employed to calculate odds ratio (OR) and 95% confidence intervals (CI) with AMI status as a dependent variable. Group membership served as independent variables with potential confounders entered as covariates. Interaction analysis revealed a significant sex difference in the association of trajectory group membership with AMI, thus analyses were performed separately by sex.
RESULTS
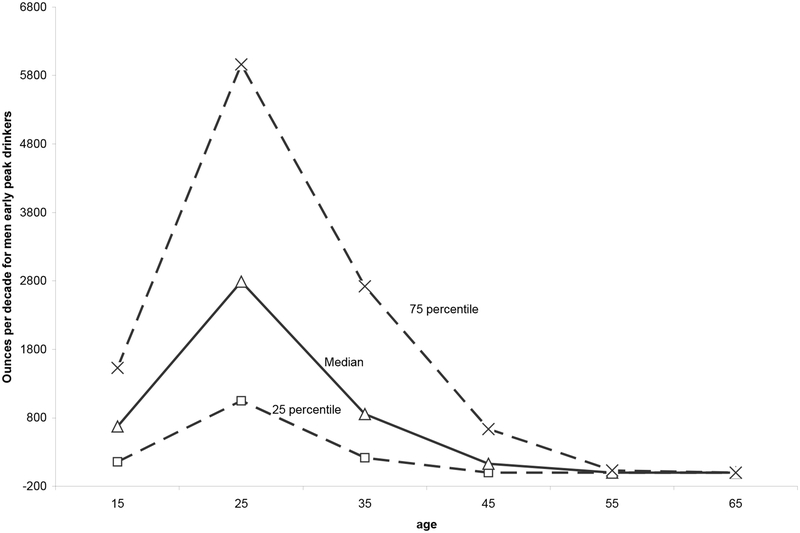
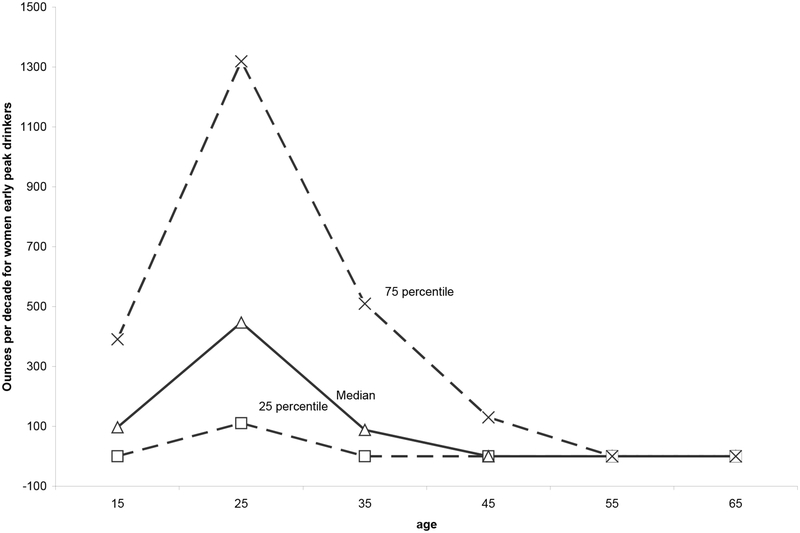
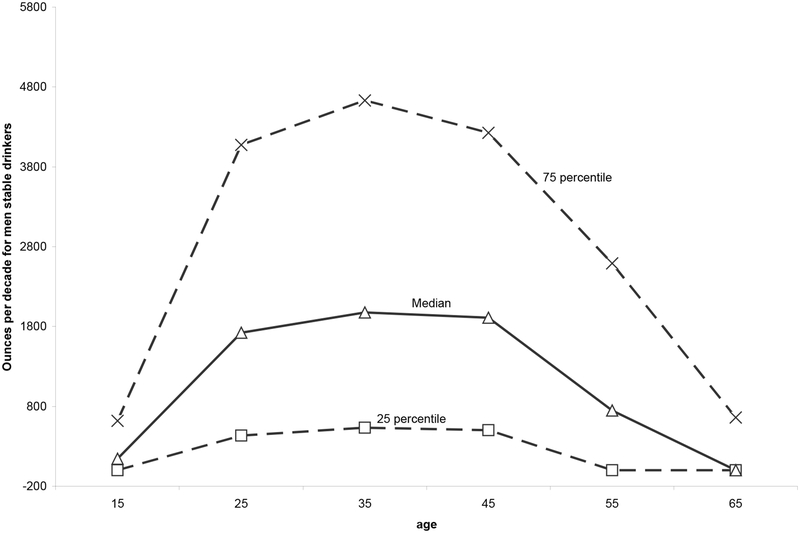
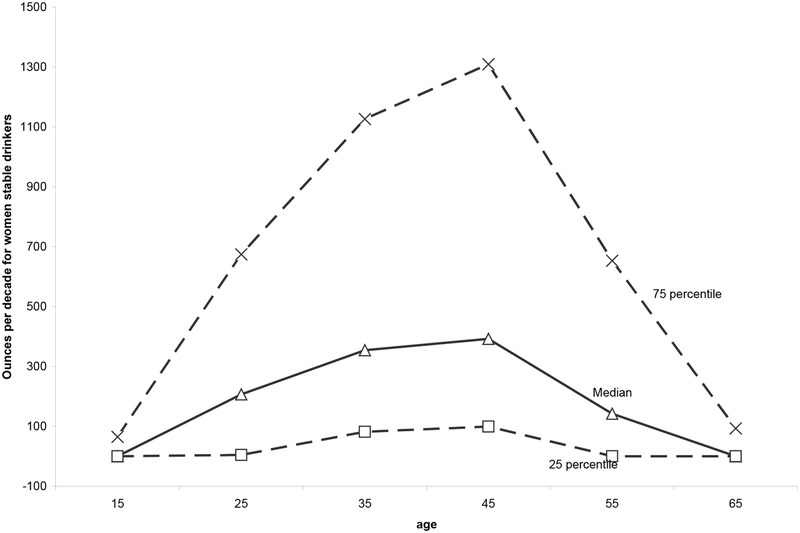
A history of regular drinking was reported by 96% of 2055 men and 87% of 1985 women. Two distinct lifetime drinking trajectories were extracted for study participants who had ever consumed alcohol regularly, an early peak trajectory, illustrated in Figure 1 for men and Figure 3 for women, and a stable trajectory, illustrated in Figure 2 for men and Figure 4 for women. Compared to stable lifetime drinking trajectories, early peak trajectories are characterized by earlier onset of regular drinking, less frequent drinking, higher numbers of drinks per drinking day, more frequent drunkenness per drinking year, and a tendency to reduce alcohol intake or abstain by middle age (Table 1), such that early peak drinking trajectories were significantly more prevalent among respondents classified as former compared to current drinkers at the time of interview, 47.6% vs. 23.9% (p<.0001). The fact that stable lifetime drinking trajectories are characterized by more frequent drinking for longer periods of time results in higher lifetime alcohol intakes, despite fewer drinks per drinking day.
Figure 1.
Ounces of ethanol consumed per decade of life among male early peak drinkers by quartiles.
Figure 3.
Ounces of ethanol consumed per decade of life among female early peak drinkers by quartiles.
Figure 2.
Ounces of ethanol consumed per decade of life among male stable drinkers by quartiles.
Figure 4.
Ounces of ethanol consumed per decade of life among female stable drinkers by quartiles.
Table 1.
Lifetime drinking patterns for men and women, according to early peak and stable lifetime drinking trajectories.
| Characteristics | Women | Men | ||||
|---|---|---|---|---|---|---|
| Early Peak Trajectories (n=784) |
Stable Trajectories (n=927) |
P value | Early Peak Trajectories (n=850) | Stable Trajectories (n=1117) |
P value | |
| Age at onset drinking | 19.0 (18.6,19.4) | 24.4 (24.0,24.8) | <0.0001 | 17.9 (17.5,18.5) | 19.9 (19.5,20.3) | <0.0001 |
| Age last time drinking | 39.3 (38.9,39.9) | 56.2 (55.8,56.8) | <0.0001 | 45.7 (45.3,46.5) | 52.5 (52.1,53.3) | <0.0001 |
| *Total years of drinking | 18.9 (18.5,19.7) | 30.8 (30.4,31.4) | <0.0001 | 27.0 (26.6,28.0) | 32.2 (31.8,33.2) | <0.0001 |
| *Total drinking days | 467.8 (423,516) | 1494 (1380,1617) | <0.0001 | 1736 (1511,1994) | 2921 (2594, 3290) | <0.0001 |
| Drinks per drinking day | 2.54 (2.46,2.61) | 1.89 (1.84,1.94) | <0.0001 | 4.25 (3.99,4.50) | 3.13 (2.94, 3.33) | <0.0001 |
| *Total drinks | 1085 (982,1198) | 2778 (2567,3008) | <0.0001 | 6567 (5605,7695) | 8777 (7491,10284) | <0.0001 |
| Drunkenness per drinking year | 2.2 (2.0, 2.4) | 1.1 (1.0, 1.2) | <0.0001 | 6.70 (5.82,7.69) | 3.73(3.23,4.30) | <0.0001 |
| Binge drinking per drinking year | 3.1 (2.7, 3.5) | 1.8 (1.6, 2.1) | <0.0001 | 27.2 (22.2,33.4) | 17.2 (13.9,21.2) | <.0015 |
controlled for age and race. All other variables were controlled for race only. All comparisons are significant at p<0.05.
Characteristics of current drinkers are summarized for male and female cases and controls in Table 2. Both male and female cases were less well educated than controls, and they were more likely to be hypertensive, diabetic, hypercholesterolemic, and to have a family history of CHD or diabetes. They also had higher BMIs and were more likely to smoke cigarettes. Female cases were somewhat older than controls, less likely to be white, and more likely to be postmenopausal. Male cases consumed a higher percent of their total calories from saturated fat and somewhat higher levels of dietary fiber, and they were less physically active. Both male and female cases reported drinking alcohol less frequently than controls. Male cases reported having more drinks per drinking day on average, bringing their total average number of drinks up to intakes approximately equal to those of controls. In contrast, female cases and controls drank about the same number of drinks per drinking day, which resulted higher average total intakes for controls, given their higher frequency of drinking. Frequency of intoxication was higher among female cases than controls. There were no significant differences in lifetime trajectories observed for either men or women.
TABLE 2.
Characteristics of current drinkers (n=2412) in the AMI case-control sample. Western New York Health Study (WNYHS), 1996–2001*
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Cases N = 554 |
Controls N = 880 |
P value† | Cases N = 122 |
Controls N = 856 |
P value† | |
| Age in years | 54.2±8.8 | 54.1±10.3 | 0.76 | 55.9±8.9 | 53.2±9.7 | 0.0004 |
| % White | 94.8 | 95.0 | 0.86 | 88.7 | 94.9 | 0.001 |
| Years of education ≤ 12 years, % | 44.4 | 32.2 | <0.0001 | 55.9 | 38.0 | <0.0001 |
| Years of education, mean±SD | 13.5±2.3 | 14.1±2.5 | <0.0001 | 12.9±2.0 | 13.8±2.4 | <0.0001 |
| % Hypertensive‡ | 35.7 | 28.4 | 0.0025 | 40.2 | 25.3 | <0.0001 |
| % Diabetic‡ | 12.1 | 6.1 | <0.0001 | 7.5 | 3.4 | <0.0001 |
| % Hypercholesterolemia‡ | 34.9 | 27.9 | 0.0034 | 38.4 | 29.6 | <0.0001 |
| % Family history of CHD or diabetes | 71.9 | 68.9 | 0.2 | 79.0 | 79.6 | 0.8 |
| Body Mass Index ≥ 25 kg/m2, % | 82.1 | 72.8 | <0.0001 | 68.8 | 58.2 | 0.006 |
| Body Mass Index, mean±SD | 29.0±4.6 | 28.2±4.6 | 0.001 | 29.1±5.8 | 27.5±6.0 | 0.0009 |
| Smoking Habits‡ | <0.0001 | <0.0001 | ||||
| % Never smokers | 23 | 38 | 27 | 44 | ||
| % Former smokers | 37 | 45 | 23 | 38 | ||
| % Current smokers | 40 | 17 | 50 | 18 | ||
| Pack years, median (interquartile range) | 8578(130,13992) | 1825(0,9079) | <0.0001 | 7285(0,12342) | 3395(0,5822) | <0.0001 |
| % calories from saturated fat, median (interquartile range) | 14(11,16) | 13(11,15) | 0.01 | 13(10,15) | 13(11,15) | 0.98 |
| Dietary fiber in grams/1000 kcal, median (interquartile range) | 7.3(5.4,9.7) | 6.8(5.3,9.2) | 0.02 | 7.0(5.1,9.8) | 7.0(5.3,9.0) | 0.9 |
| Average hours of physical activity per week in lifetime, median (interquartile range) | 5.4(3.7,7.0) | 5.7(4.1,6.9) | 0.07 | 5.2(3.3,6.6) | 5.2(3.8,6.5) | 0.7 |
| Postmenopausal, % | - | - | 80.6 | 60.5 | <0.0001 | |
| Ever used hormone therapy, % | - | - | 40.3 | 36.3 | 0.31 | |
| Current Drinking Patterns§ | ||||||
| Total number of drinks in 12 months, median (interquartile range) | 15(4,44) | 18(5,41) | 0.2 | 3(0,15) | 15(4,44) | 0.0002 |
| Total drinking days in 12 months, median (interquartile range) | 6(2,16) | 7(2,18) | 0.003 | 2(0,7) | 3(1,12) | <0.0001 |
| Drinks per drinking day, median (interquartile range) | 3.1(1.9,5.2) | 2.6(1.8,4.4) | 0.001 | 2.0(1.3,3.2) | 1.9(1.3,2.9) | 0.26 |
| Frequency of intoxication in 12 months, median (interquartile range) | 0(0,2) | 0(0,0) | 0.18 | 0(0,2) | 0(0,0) | 0.04 |
| Lifetime Drinking Trajectories | 0.45 | 0.44 | ||||
| % Early peak trajectories | 38.4 | 40.3 | 41.9 | 38.9 | ||
| % Stable trajectories | 61.6 | 59.7 | 58.1 | 61.1 | ||
Plus-minus values are means ± SD. Skewed-distribution variables are expressed as median (interquartile range).
P-values for the differences between cases and controls (unadjusted) were determined by Student’s t-test for continuous variables, by Wilcoxon’s rank-sum test for variables expressed as medians, and by Chi-square test for categorical variables.
Values for hypertension, diabetes, hypercholesterolemia, and smoking for cases reflect status prior to MI.
Current drinking patterns were ascertained for a typical 28-day period during the 12–24 months prior to interview.
Characteristics of former drinkers are summarized for male and female cases and controls in Table 3. Consistent with current drinkers, male and female cases were less well educated than controls, smoked more during their lifetimes, and were more likely to be current smokers. Female cases were more likely to be hypertensive, diabetic, and hypercholesterolemic. Female cases had higher average BMIs and were more likely to be postmenopausal than controls. No significant differences between cases and controls in lifetime trajectories were observed for either men or women.
TABLE 3.
Characteristics of former drinkers (n=1266) in the AMI case-control sample. Western New York Health Study (WNYHS), 1996–2001*
| Men | Women | |||||
|---|---|---|---|---|---|---|
| Cases N = 255 |
Controls N = 278 |
P value† | Cases N = 174 |
Controls N = 559 |
P value† | |
| Age in years | 54.1±8.1 | 54.6±10.0 | 0.63 | 55.5±7.8 | 53.6±9.7 | 0.07 |
| % White | 89.9 | 82.6 | 0.04 | 84.5 | 89.3 | 0.17 |
| Years of education ≤ 12 years, % | 49.4 | 39.7 | 0.05 | 66.4 | 50.1 | 0.003 |
| Years of education, mean±SD | 12.7±2.3 | 13.6±2.6 | 0.0006 | 12.2±1.9 | 13.2±2.3 | <0.0001 |
| % Hypertensive‡ | 42.8 | 36.0 | 0.17 | 53.8 | 27.8 | <0.0001 |
| % Diabetic‡ | 19.7 | 14.2 | 0.15 | 22.4 | 9.2 | 0.0002 |
| % Hypercholesterolemia‡ | 35.7 | 30.7 | 0.30 | 36.9 | 35.8 | 0.84 |
| % Family history of CHD or diabetes | 69.1 | 68.8 | 0.94 | 75.5 | 79.9 | 0.31 |
| Body Mass Index ≥ 25 kg/m2, % | 82.6 | 78.6 | 0.31 | 81.8 | 66.7 | 0.002 |
| Body Mass Index, mean±SD | 29.3±4.7 | 29.2±5.1 | 0.91 | 31.1±6.5 | 29.5±7.4 | 0.04 |
| Smoking Habits‡ | <0.0001 | <0.0001 | ||||
| % Never smokers | 15 | 33 | 16 | 46 | ||
| % Former smokers | 31 | 47 | 26 | 36 | ||
| % Current smokers | 55 | 20 | 59 | 18 | ||
| Pack years, median (interquartile range) | 12436(3696,17520) | 4271(0,10768) | <0.0001 | 10950(3376,15741) | 246(0,7535) | <0.0001 |
| % calories from saturated fat, median (interquartile range) | 14.6(11.4,16.8) | 14.0(11.5,16.5) | 0.45 | 14.0(10.3,15.8) | 13.4(10.9,15.4) | 0.66 |
| Dietary fiber in grams/1000 kcal, median (interquartile range) | 6.8(5.1,8.8) | 6.8(5.2,8.9) | 0.74 | 7.7(5.9,10.2) | 6.8(5.3,8.9) | 0.03 |
| Average hours of physical activity per week in lifetime, median (interquartile range) | 5.6(3.7,6.8) | 6.0(4.2,6.9) | 0.31 | 5.3(3.2,6.5) | 5.5(3.7,6.5) | 0.27 |
| Postmenopausal, % | - | - | 80.9 | 65.1 | 0.0016 | |
| Ever used hormone therapy, % | - | - | 37.4 | 37.6 | 0.96 | |
| Lifetime Drinking Trajectories | 0.30 | 0.80 | ||||
| % Early peak trajectories | 60.1 | 54.9 | 60.0 | 61.3 | ||
| % Stable trajectories | 39.9 | 45.1 | 40.0 | 38.7 |
Plus-minus values are means ± SD. Skewed-distribution variables are expressed as median (interquartile range).
P-values for the differences between cases and controls (unadjusted) were determined by Student’s t-test for continuous variables, by Wilcoxon’s rank-sum test for variables expressed as medians, and by Chi-square test for categorical variables.
Values for hypertension, diabetes, hypercholesterolemia, and smoking for cases reflect status prior to MI.
Adjusted odds ratios (ORs) and 95% confidence intervals comparing risk for non-fatal AMI in abstainers to that in early peak and stable drinkers and risk in early peak to that in stable drinkers are summarized in Table 4, according to sex and current drinking status. Among former drinkers only abstainers were at significantly higher risk of AMI than stable drinkers in men and in the sex-combined analysis. Also among former drinkers, early peak drinkers showed higher risk of AMI compared to stable drinkers in each sex; however, only in the sex-combined analysis did the ORs reach statistical significance. Among current drinkers, early peak drinkers were at significantly higher risk compared to stable drinkers in women, but not in men.
TABLE 4.
Risk of non-fatal acute myocardial infarction in female and male former and current drinkers, according to lifetime drinking trajectories (abstainers,* early peak drinkers and stable drinkers): Western New York Health Study (WNYHS), 1996–2001. Multivariate-adjusted** odds ratios, 95% Confidence Intervals.
| Former drinkers (n=1266) |
Current drinkers (n=2412) |
|
|---|---|---|
| Odds Ratios (95% CI) | Odds Ratios (95%CI) | |
| WOMEN (n=1972) | ||
| Abstainer vs. early peak (ref.) | 0.87 (0.44─1.74) | 0.63 (0.27─1.49) |
| Abstainer vs. stable (ref.) | 1.24 (0.59─2.58) | 1.02 (0.45─2.33) |
| Early peak vs. stable (ref.) | 1.41 (0.82─2.43) | 1.63 (1.08─2.44) |
| MEN (n=2046) | ||
| Abstainer vs. early peak | 2.48 (0.89─6.91) | 1.83 (0.60─5.58) |
| Abstainer vs. stable | 4.05 (1.41─11.67) | 1.57 (0.52─4.75) |
| Early peak vs. stable | 1.63 (0.96─2.77) | 0.86 (0.66─1.12) |
| COMBINED (n=4018) | ||
| Abstainer vs. early peak | 1.13 (0.65─1.96) | 0.39 (0.72─2.70) |
| Abstainer vs. stable | 1.77 (0.99─3.18) | 1.39 (0.73─2.65) |
| Early peak vs. stable | 1.57 (1.08─2.29) | 1.00 (0.80─1.25) |
Abstainers include lifetime abstainers and very light drinkers (215 controls and 46 cases for women; 38 controls and 41 cases for men).
Adjusted for: Race (White. Non-white), age at interview, marital status (married or other), family history of CHD and diabetes, years of education (>12 years vs. ≤12 years), lifetime average physical activity(<5 hrs/wk vs. ≥5 hrs/wk)), BMI (≥ 25 kg/m2 vs. <25 kg/m2), percent of calories from saturated fat(≥10% vs. <10%), smoking status (former smoker vs. others), quartiles of smoking pack years. Menopausal status was also controlled in female-specific models.
Previous analyses (Fan, Russell et al. 2008), indicated that early peak drinkers tended to be approximately ten years younger than stable drinkers, suggesting a cohort effect that might be obscured by simply adjusting for age. Accordingly, the above analyses were replicated in subsets of the sample stratified on age, with no appreciable change in the findings.
DISCUSSION
This is the first time that drinking trajectories covering the entire lifespan, including adolescence and emerging adulthood, have been investigated with respect to non-fatal acute myocardial infarction. Our findings that AMI risk was positively associated with early peak compared to stable lifetime drinking trajectories among former drinkers and current female drinkers suggest that early onset, high intensity, and binge drinking patterns characteristic of early peak drinking trajectories contribute significantly to the initiation of atherosclerotic disease in young people, increasing their risk of AMI later in life. These findings are consistent with a previous report that risk factors for cardiovascular disease, the metabolic syndrome and its components, were positively associated with early peak lifetime drinking trajectories among healthy controls from the WNYHS (Fan, Russell et al. 2008). Although most epidemiologic research on alcohol and CHD has been carried out in adult populations, we know of two studies conducted in adolescents and young adults using subclinical markers of atherosclerosis that predict later cardiovascular events (Juonala, Viikari et al. 2009, Charakida, Georgiopoulos et al. 2019). Data from the ALSPAC Study revealed a positive relationship between the intensity of alcohol use and arterial stiffness in adolescents at age 17 years (Charakida, Georgiopoulos et al. 2019), and intensity of alcohol use was also found to be directly related to carotid intima-media thickness in a study of healthy Finns ages 24–39 years (Juonala, Viikari et al. 2009). Analyses in both studies controlled for other cardiovascular risk factors, and no protective effect of moderate drinking on vascular damage was seen in either study.
From the perspective of lifetime drinking trajectories, it seems likely that the negative impact of alcohol on cardiovascular disease has been substantially underestimated by previous epidemiological studies in which alcohol intake has only been assessed in participants age 35 years and older. We identified five distinct lifetime drinking trajectories among healthy controls from the WNYHS (Gruenewald, Russell et al. 2002); the trajectory featuring the highest average alcohol intakes per month peaked in the early 20s and fell to near zero by the early 40s. The literature on heavy episodic or binge drinking indicates that prevalence is high in the United States and has a non-linear relation with age, peaking around 45% at ages 18 to 22 and beginning to drop in the mid-20s (Lee and Sher 2018). Studies of alcohol use disorders and age show a similar pattern, with severely affected individuals (six+ symptoms) significantly more likely to drop to abstention or low-risk drinking in young adulthood than later in life (Lee, Boness et al. 2018). These trends suggest that many young, heavy episodic, problem drinkers present as abstainers or low-risk drinkers after the age of 35, and that former drinkers may have been motivated to stop regular drinking by problems associated with heavy episodic drinking. Thus, higher cardiovascular risk among subjects abstaining after age 35 or former drinkers compared to drinkers may be attributable to unassessed harmful drinking patterns during adolescence and emerging adulthood rather than to a protective effect of moderate drinking. The excess of early-peak drinking trajectories among former drinkers in the present study provides support for this hypothesis. Harmful drinking patterns prior to age 35 represent not only an unassessed AMI risk, but also a potential source of selection bias since they may reduce study participation by individuals whose alcohol use has affected their wellbeing (Naimi, Stadtmueller et al. 2019).
However, our finding that AMI risk was higher in men who never drank regularly compared to those that did cannot be attributed to unassessed youthful drinking. Additional research is needed to determine whether unadjusted confounding factors may have contributed to this finding (Naimi, Brown et al. 2005), a possibility made more salient by the fact that failure to ever drink regularly was rare among men in Western New York State, whereas, failure to drink regularly was more normative among women, and not associated with increased AMI risk. Alternatively, given women’s greater sensitivity to the effects of alcohol on health (Vatsalya, Liaquat et al. 2016), regular drinking may be less protective against AMI among women than among men.
Gender differences in sensitivity to alcohol may also contribute to a moderating effect of current drinking status on the relation of lifetime drinking trajectories to AMI risk. Early peak lifetime drinking trajectories were associated with higher AMI risk than stable trajectories for both male and female former drinkers, but only for female current drinkers. We speculate that women may experience cardiovascular damage at levels of consumption unlikely to interfere with continued drinking, whereas drinking patterns harmful enough to affect male cardiovascular systems may cause social, legal, work, and other health-related alcohol problems that motivate them to quit drinking. A possible contributing factor is that men are more likely than women to receive treatment for problem drinking (Zemore, Murphy et al. 2014), which could increase abstinence among men whose early peak drinking was severe enough to affect their CHD risk.
Findings in former drinkers provide information on cumulative effects of alcohol on cardiovascular health in the absence of potentially confounding acute effects. Thus, the fact that early peak lifetime drinking trajectories are associated with increased AMI risk among former drinkers suggests that heavy episodic drinking patterns early in life have long-term, chronic effects on MI risk, and that lower AMI risk associated with stable drinking trajectories may reflect the absence of alcohol-related damage to the cardiovascular system rather than a protective effect of moderate drinking. Alternatively, the effect of early peak drinking trajectories on the cardiovascular system may vary over the lifespan, such that heavy episodic drinking in adolescence and emerging adulthood initiates chronic atherosclerotic processes, but more moderate drinking patterns in middle age may have some acute beneficial effects on the cardiovascular system that protect against AMI in susceptible men, but not women.
We acknowledge several limitations of this study. Perhaps the greatest is that our measure of alcohol trajectories depends on retrospective self-report of drinking patterns over a lifetime. Although prospective assessment of alcohol intake poses fewer challenges to memory, studies demonstrating moderate to high concordance between prospective and retrospective measures of alcohol intake over lengthy periods of time indicate that drinking patterns are salient enough to support meaningful retrospective assessment (Czarnecki, Russell et al. 1990, Koenig, Jacob et al. 2009, Greenfield, Nayak et al. 2014, Bell and Britton 2015). As indicated earlier, the Cognitive Lifetime Drinking History employed a Lifetime Calendar of Events to help respondents remember how significant life events may have influenced their activities and drinking patterns associated with these activities. In addition, computerizing the interview allowed us to reduce the respondent burden associated with reporting drinking patterns by collecting data on the component parts of the pattern. For example, respondents are often asked to report how many standard drinks of alcohol they usually have in a week, which can be difficult to estimate if their usual drink size isn’t standard, if their usual intake varies over the course of a week, if their weekly intake varies, or if they sometimes have more than usual. Directly assessing respondents’ usual drink size and the frequency and usual quantity of drinking on weekdays, Fridays, Saturdays, Sundays, and times they have more than usual, using a 28-day framework, both stimulates memory of past weekly and monthly drinking occasions and provides data for computation of drinking patterns. A test-retest reliability study demonstrated that lifetime estimates of total ounces of alcohol consumed and times intoxicated based on CLDH assessments made at least a week apart were highly comparable in post myocardial infarction patients and healthy controls; no significant differences in mean estimates were observed, and correlation coefficients ranged between 0.73 and 0. 83 (Russell, Marshall et al. 1997). Evidence of internal validity is provided by findings that early peak lifetime drinking trajectories predicted cardiovascular risk factors among healthy controls from the Western New York Health Study (Fan, Russell et al. 2008).
Another limitation is that the population of Western New York State is predominately White, and there were not enough Non-White participants in this study to investigate racial/ethnic differences in lifetime drinking trajectories and their relations to AMI risk. Trajectories of heavy drinking (frequency of six+ drinks) from age 21 to 51 in a nationally representative U.S. sample showed a drop in their twenties among Whites that is consistent with early peak lifetime drinking trajectories reported here, but heavy drinking trajectories among Blacks and Hispanic participants differed significantly from those among Whites (Mulia, Karriker-Jaffe et al. 2017). Additional research is needed to determine how racial/ethnic differences in lifetime drinking trajectories may influence AMI risk.
It should be recognized that we have not adjusted for an overall effect of total alcohol consumption in these analyses. Definition of the trajectories is based on ounces of alcohol per decade of life, a summary measure of alcohol intake that enables identification of lifetime trajectories but obscures the contribution of drinking patterns to AMI risk, although there are significant differences between early peak and stable trajectories in the drinking patterns associated with each. Prior research suggests that it would be useful to investigate lifetime trajectories based on heavier drinking episodes associated with potentially harmful physiological changes, such as frequency of binge drinking or intoxication (Roerecke and Rehm 2010). However, such approaches may be limited, not only by failure to assess these measures in many studies, but also by the measures themselves. For example, cut points used to define binge drinking are arbitrary, missing effects of heavy drinking episodes that don’t quite reach the binge threshold or those greatly exceeding it, and intoxication is influenced by many factors in addition to alcohol intake (Brick and Erickson 2009), some of which could affect cardiovascular risk. A possible candidate for further research on lifetime drinking trajectories is dosage, a measure of the extent to which someone has more than one drink per drinking day (Russell, Chu et al. 2009). It can be estimated from standard measures of drinking frequency and quantity by calculating total drinks for the period assessed (volume = frequency × quantity) and subtracting frequency. Dosage was mathematically derived as part of a linear alcohol dose-response algorithm that also included drinking frequency, and significant negative effects of dosage were associated with AMI risk in cross-sectional analyses of current drinking after controlling for positive effects of frequency (Russell, Chu et al. 2009). Accordingly, use of dosage alone to evaluate risk associated with lifetime drinking patterns is not supported by its original mathematical derivation; however, as a continuous measure of the extent to which one has more than one drink on days when one drinks, it may provide information useful in understanding the contribution of drinking pattern trajectories to AMI risk.
Although we adjusted for the effects of a number of known cardiovascular risk factors, we cannot rule out the possibility that residual confounding may have occurred, particularly among male respondents who never drank regularly during their lifetimes. Also, the study is limited to non-fatal myocardial infarctions.
Conclusions:
Early peak lifetime drinking trajectories, characterized by earlier onset of regular drinking, less frequent drinking, higher numbers of drinks per drinking day, more frequent drunkenness per drinking year, fewer total lifetime drinks, and a tendency to reduce alcohol intake or abstain by middle age, are associated with an increased risk of AMI among former drinkers and current female drinkers, suggesting that binge drinking during adolescence and emerging adulthood may have long-term effects on the cardiovascular system that have not been recognized by previous epidemiological studies that assessed alcohol consumption at ages 35 and older. From a public health perspective, we already have proscriptions against binge drinking during adolescence and emerging adulthood based on acute consequences, such as accidents and an increased risk of alcohol use disorders; however, a better appreciation of potential long-term health consequences may add weight to moderate drinking recommendations. Perhaps more importantly, epidemiological research suggesting that moderate drinking has a protective effect on cardiovascular health needs to be reevaluated, taking lifetime drinking trajectories into consideration.
Source of Support:
This work was supported by grants from the National Institute on Alcohol Abuse andAlcoholism, National Institute of Health (P50 AA09802 and R21AA13597 to the first author).
REFERENCES
- Au Yeung SL, Jiang C, Cheng KK, Cowling BJ, Liu B, Zhang W, Lam TH, Leung GM and Schooling CM (2013). “Moderate alcohol use and cardiovascular disease from Mendelian randomization.” PLoS One 8(7): e68054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell S and Britton A (2015). “Reliability of a retrospective decade-based life-course alcohol consumption questionnaire administered in later life.” Addiction 110(10): 1563–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block G, Woods M, Potosky A and Clifford C (1990). “Validation of a self-administered diet history questionnaire using multiple diet records.” Journal of Clinical Epidemiology 43(12): 1327–1335. [DOI] [PubMed] [Google Scholar]
- Brick J and Erickson CK (2009). “Intoxication is not always visible: an unrecognized prevention challenge.” Alcohol Clin Exp Res 33(9): 1489–1507. [DOI] [PubMed] [Google Scholar]
- Britton A, Ben-Shlomo Y, Benzeval M, Kuh D and Bell S (2015). “Life course trajectories of alcohol consumption in the United Kingdom using longitudinal data from nine cohort studies.” BMC Med 13: 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charakida M, Georgiopoulos G, Dangardt F, Chiesa ST, Hughes AD, Rapala A, Davey Smith G, Lawlor D, Finer N and Deanfield JE (2019). “Early vascular damage from smoking and alcohol in teenage years: the ALSPAC study.” Eur Heart J 40(4): 345–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chikritzhs T, Fillmore K and Stockwell T (2009). “A healthy dose of scepticism: four good reasons to think again about protective effects of alcohol on coronary heart disease.” Drug Alcohol Rev 28(4): 441–444. [DOI] [PubMed] [Google Scholar]
- Czarnecki DM, Russell M, Cooper ML and Salter D (1990). “Five-year reliability of self-reported alcohol consumption.” J Stud Alcohol 51(1): 68–76. [DOI] [PubMed] [Google Scholar]
- Dorn JM, Hovey K, Williams BA, Freudenheim JL, Russell M, Nochajski TH and Trevisan M (2007). “Alcohol drinking pattern and non-fatal myocardial infarction in women.” Addiction 102(5): 730–739. [DOI] [PubMed] [Google Scholar]
- Fan AZ, Russell M, Stranges S, Dorn J and Trevisan M (2008). “Association of lifetime alcohol drinking trajectories with cardiometabolic risk.” J Clin Endocrinol Metab 93(1): 154–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A and Kerr W (2007). “Moderate alcohol use and reduced mortality risk: systematic error in prospective studies and new hypotheses.” Ann Epidemiol 17(5 Suppl): S16–23. [DOI] [PubMed] [Google Scholar]
- Greenfield TK, Nayak MB, Bond J, Kerr WC and Ye Y (2014). “Test-retest reliability and validity of life-course alcohol consumption measures: the 2005 National Alcohol Survey follow-up.” Alcohol Clin Exp Res 38(9): 2479–2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ, Russell M, Light J, Lipton R, Searles J, Johnson F, Trevisan M, Freudenheim J, Muti P, Carosella AM and Nochajski TH (2002). “One drink to a lifetime of drinking: temporal structures of drinking patterns.” Alcohol Clin Exp Res 26(6): 916–925. [PubMed] [Google Scholar]
- Holmes MV, Dale CE, Zuccolo L, Silverwood RJ, Guo Y, Ye Z, Prieto-Merino D, Dehghan A, Trompet S, Wong A, Cavadino A, Drogan D, Padmanabhan S, Li S, Yesupriya A, Leusink M, Sundstrom J, Hubacek JA, Pikhart H, Swerdlow DI, Panayiotou AG, Borinskaya SA, Finan C, Shah S, Kuchenbaecker KB, Shah T, Engmann J, Folkersen L, Eriksson P, Ricceri F, Melander O, Sacerdote C, Gamble DM, Rayaprolu S, Ross OA, McLachlan S, Vikhireva O, Sluijs I, Scott RA, Adamkova V, Flicker L, Bockxmeer FM, Power C, Marques-Vidal P, Meade T, Marmot MG, Ferro JM, Paulos-Pinheiro S, Humphries SE, Talmud PJ, Mateo Leach I, Verweij N, Linneberg A, Skaaby T, Doevendans PA, Cramer MJ, van der Harst P, Klungel OH, Dowling NF, Dominiczak AF, Kumari M, Nicolaides AN, Weikert C, Boeing H, Ebrahim S, Gaunt TR, Price JF, Lannfelt L, Peasey A, Kubinova R, Pajak A, Malyutina S, Voevoda MI, Tamosiunas A, Maitland-van der Zee AH, Norman PE, Hankey GJ, Bergmann MM, Hofman A, Franco OH, Cooper J, Palmen J, Spiering W, de Jong PA, Kuh D, Hardy R, Uitterlinden AG, Ikram MA, Ford I, Hypponen E, Almeida OP, Wareham NJ, Khaw KT, Hamsten A, Husemoen LL, Tjonneland A, Tolstrup JS, Rimm E, Beulens JW, Verschuren WM, Onland-Moret NC, Hofker MH, Wannamethee SG, Whincup PH, Morris R, Vicente AM, Watkins H, Farrall M, Jukema JW, Meschia J, Cupples LA, Sharp SJ, Fornage M, Kooperberg C, LaCroix AZ, Dai JY, Lanktree MB, Siscovick DS, Jorgenson E, Spring B, Coresh J, Li YR, Buxbaum SG, Schreiner PJ, Ellison RC, Tsai MY, Patel SR, Redline S, Johnson AD, Hoogeveen RC, Hakonarson H, Rotter JI, Boerwinkle E, de Bakker PI, Kivimaki M, Asselbergs FW, Sattar N, Lawlor DA, Whittaker J, Davey Smith G, Mukamal K, Psaty BM, Wilson JG, Lange LA, Hamidovic A, Hingorani AD, Nordestgaard BG, Bobak M, Leon DA, Langenberg C, Palmer TM, Reiner AP, Keating BJ, Dudbridge F and Casas JP (2014). “Association between alcohol and cardiovascular disease: Mendelian randomisation analysis based on individual participant data.” BMJ 349: g4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones BL, Nagin DS, Roeder K and (2001). “A SAS procedure based on mixture models for estimating developmental trajectories.” Sociological Methods and Research 29: 374–393. [Google Scholar]
- Juonala M, Viikari JS, Kahonen M, Laitinen T, Taittonen L, Loo BM, Jula A, Marniemi J, Rasanen L, Ronnemaa T and Raitakari OT (2009). “Alcohol consumption is directly associated with carotid intima-media thickness in Finnish young adults: the Cardiovascular Risk in Young Finns Study.” Atherosclerosis 204(2): e93–98. [DOI] [PubMed] [Google Scholar]
- Kloner RA and Rezkalla SH (2007). “To drink or not to drink? That is the question.” Circulation 116(11): 1306–1317. [DOI] [PubMed] [Google Scholar]
- Koenig LB, Jacob T and Haber JR (2009). “Validity of the lifetime drinking history: a comparison of retrospective and prospective quantity-frequency measures.” J Stud Alcohol Drugs 70(2): 296–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MR, Boness CL, McDowell YE, Verges A, Steinley DL and Sher KJ (2018). “Desistance and severity of alcohol use disorder: A lifespan-developmental investigation.” Clin Psychol Sci 6(1): 90–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee MR and Sher KJ (2018). ““Maturing out” of binge and problem drinking.” Alcohol Res 39(1): 31–42. [PMC free article] [PubMed] [Google Scholar]
- Mulia N, Karriker-Jaffe KJ, Witbrodt J, Bond J, Williams E and Zemore SE (2017). “Racial/ethnic differences in 30-year trajectories of heavy drinking in a nationally representative U.S. sample.” Drug Alcohol Depend 170: 133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagin D and Tremblay RE (2001). “Analyzing developmental trajectories of distinct but related behaviors: A group-based method.” Psychological Methods 6: 18–34. [DOI] [PubMed] [Google Scholar]
- Nagin DS (1999). “Analyzing developmental trajectories: A semi-parametric, group-based approach.” Psychological Methods 4: 139–177. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Brown DW, Brewer RD, Giles WH, Mensah G, Serdula MK, Mokdad AH, Hungerford DW, Lando J, Naimi S and Stroup DF (2005). “Cardiovascular risk factors and confounders among nondrinking and moderate-drinking U.S. adults.” Am J Prev Med 28(4): 369–373. [DOI] [PubMed] [Google Scholar]
- Naimi TS, Stadtmueller LA, Chikritzhs T, Stockwell T, Zhao J, Britton A, Saitz R and Sherk A (2019). “Alcohol, Age, and Mortality: Estimating Selection Bias Due to Premature Death.” J Stud Alcohol Drugs 80(1): 63–68. [PubMed] [Google Scholar]
- Ng Fat L and Shelton N (2012). “Associations between self-reported illness and non-drinking in young adults.” Addiction 107(9): 1612–1620. [DOI] [PubMed] [Google Scholar]
- O’Keefe EL, DiNicolantonio JJ, O’Keefe JH and Lavie CJ (2018). “Alcohol and CV Health: Jekyll and Hyde J-Curves.” Prog Cardiovasc Dis 61(1): 68–75. [DOI] [PubMed] [Google Scholar]
- O’Neill D, Britton A, Hannah MK, Goldberg M, Kuh D, Khaw KT and Bell S (2018). “Association of longitudinal alcohol consumption trajectories with coronary heart disease: a meta-analysis of six cohort studies using individual participant data.” BMC Med 16(1): 124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Sempos CT and Trevisan M (2003). “Alcohol and cardiovascular disease--more than one paradox to consider. Average volume of alcohol consumption, patterns of drinking and risk of coronary heart disease--a review.” J Cardiovasc Risk 10(1): 15–20. [DOI] [PubMed] [Google Scholar]
- Rimm EB, Williams P, Fosher K, Criqui M and Stampfer MJ (1999). “Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors.” BMJ 319(7224): 1523–1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roerecke M, Kaczorowski J, Tobe SW, Gmel G, Hasan OSM and Rehm J (2017). “The effect of a reduction in alcohol consumption on blood pressure: a systematic review and meta-analysis.” Lancet Public Health 2(2): e108–e120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roerecke M and Rehm J (2010). “Irregular heavy drinking occasions and risk of ischemic heart disease: a systematic review and meta-analysis.” Am J Epidemiol 171(6): 633–644. [DOI] [PubMed] [Google Scholar]
- Russell M, Chu BC, Banerjee A, Fan AZ, Trevisan M, Dorn JM and Gruenewald P (2009). “Drinking patterns and myocardial infarction: a linear dose-response model.” Alcohol Clin Exp Res 33(2): 324–331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell M, Marshall JR, Trevisan M, Freudenheim JL, Chan AW, Markovic N, Vana JE and Priore RL (1997). “Test-retest reliability of the cognitive lifetime drinking history.” Am J Epidemiol 146(11): 975–981. [DOI] [PubMed] [Google Scholar]
- Shaper AG, Wannamethee G and Walker M (1988). “Alcohol and mortality in British men: explaining the U-shaped curve.” Lancet 2(8623): 1267–1273. [DOI] [PubMed] [Google Scholar]
- Toma A, Pare G and Leong DP (2017). “Alcohol and Cardiovascular Disease: How Much is Too Much?” Curr Atheroscler Rep 19(3): 13. [DOI] [PubMed] [Google Scholar]
- Trevisan M, Dorn J, Falkner K, Russell M, Ram M, Muti P, Freudenheim JL, Nochajaski T and Hovey K (2004). “Drinking pattern and risk of non-fatal myocardial infarction: a population-based case-control study.” Addiction 99(3): 313–322. [DOI] [PubMed] [Google Scholar]
- Vatsalya V, Liaquat HB, Ghosh K, Mokshagundam SP and McClain CJ (2016). “A review on the sex differences in organ and system pathology with alcohol drinking.” Curr Drug Abuse Rev 9(2): 87–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE, Murphy RD, Mulia N, Gilbert PA, Martinez P, Bond J and Polcin DL (2014). “A moderating role for gender in racial/ethnic disparities in alcohol services utilization: results from the 2000 to 2010 National Alcohol Surveys.” Alcohol Clin Exp Res 38(8): 2286–2296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J, Stockwell T, Roemer A, Naimi T and Chikritzhs T (2017). “Alcohol Consumption and Mortality From Coronary Heart Disease: An Updated Meta-Analysis of Cohort Studies.” J Stud Alcohol Drugs 78(3): 375–386. [DOI] [PMC free article] [PubMed] [Google Scholar]