Abstract
Background:
Research suggests bidirectional associations between symptoms of posttraumatic stress disorder (PTSD) and sleep disturbance, both of which have been associated with alcohol problems. However, few studies have examined the interplay of these conditions in predicting alcohol problems over time. This study tested two competing models: (a) sleep disturbance as a mediator of the association between intrusive thoughts about trauma and alcohol problems and (b) intrusion symptoms as the mediator of the sleep/alcohol problems association.
Methods:
Veterans (N=325, 93% male, 81% White) completed assessments at baseline, 6 months, and 12 months as part of a larger observational study. Zero-inflated negative binomial models were used to examine indirect effects of baseline predictors on (a) yes/no likelihood and (b) number of 12-month alcohol problems through 6-month mediators. Models controlled for past-year cannabis use and drinks consumed per week at baseline.
Results:
The only significant predictor of alcohol problem likelihood was baseline drinking quantity. Baseline PTSD intrusions had a direct effect on number of alcohol problems at 12 months, with no indirect (mediated) effect through 6-month sleep disturbance. In the competing model, baseline sleep disturbance had a marginally significant direct effect on 12-month alcohol problems, with a significant indirect effect through 6-month PTSD intrusions.
Conclusions:
PTSD intrusions are associated with more alcohol problems and help explain the long-term association between sleep and alcohol problems among Veterans. Because sleep disturbances are associated with more intrusive thoughts about trauma, we recommend that treatments targeting sleep in the context of PTSD and alcohol use include a cognitive component.
Keywords: alcohol, drinking, PTSD, mental health, Veterans
Introduction
Post-traumatic stress disorder (PTSD) and alcohol use are common, frequently comorbid disorders among veterans (Lehavot et al., 2018, Boden and Hoggatt, 2018). Despite research examining the impact of PTSD symptoms on alcohol problems, few studies have examined potential mechanisms of this association, particularly over time (Gilpin and Weiner, 2017). Sleep disturbance – operationalized as sleep of poor quality, timing, efficiency, or duration (Buysse, 2014) – co-occurs with both PTSD and alcohol use and is more prevalent among veterans than the general population (Jenkins et al., 2015). Thus, sleep may be particularly relevant to PTSD- and alcohol-related problems among veterans.
PTSD and Alcohol Problems
Separate lines of research have documented associations between PTSD and alcohol problems, sleep and alcohol problems, and PTSD and sleep. In cross-sectional models, PTSD symptoms are associated with more frequent binge drinking (Calhoun et al., 2016, Adams et al., 2016) and problems such as passing out or taking foolish risks as a result of drinking (Fuehrlein et al., 2014). Similarly, at the daily level, daytime PTSD symptoms are associated with greater alcohol consumption and more alcohol-related problems (e.g., fighting) that night (Gaher et al., 2014, Langdon et al., 2016). The association between PTSD and alcohol use is often attributed to self-medication, or use of alcohol to cope with distress; however, PTSD is associated with alcohol-related problems independent of alcohol consumption (Gaher et al., 2014), indicating that the association between PTSD and alcohol problems is not due solely to increased drinking quantity.
Sleep and Alcohol Problems
Sleep disturbance also increases risk for alcohol-related problems (Chaudhary et al., 2015). Both poor sleep quality (Swinkels et al., 2013) and short sleep duration (Luxton et al., 2011) predict heavy drinking among returning veterans, and more severe insomnia symptoms are associated with more alcohol-related problems (Wright et al., 2011). While the mechanism(s) linking sleep to alcohol involvement are not well understood, sleep disturbance has been linked to impairments in executive functioning (Baglioni et al., 2010). Thus, sleep disturbance may contribute to poor cognitive control, resulting in poor decision-making and more problems in the context of alcohol use. Moreover, drinking is associated with more alcohol consequences in the context of sleep disturbance – as opposed to no sleep disturbance – in veterans (Miller et al., 2017a). Thus, sleep disturbance appears to contribute uniquely to alcohol-related problems above and beyond heavy drinking.
PTSD and Sleep
Individuals with PTSD experience more arousals from sleep (Capaldi et al., 2011), sleep for shorter amounts of time (Seelig et al., 2010), and report worse quality sleep (King et al., 2017, Lind et al., 2017) than those without PTSD. Indeed, trouble falling or staying asleep is the most commonly-reported symptom of PTSD after deployment (McLay et al., 2010) and persists following effective treatment of PTSD (Zayfert and DeViva, 2004). Thus, PTSD symptoms likely contribute to subsequent sleep disturbance. Intrusive thoughts about traumatic events (referred to throughout as “PTSD intrusions”) may be particularly detrimental to sleep, as intrusive thoughts and worry are characteristic of the cognitive arousal processes that contribute to insomnia (Harvey, 2005, Spielman, 1987).
However, the association between PTSD and sleep seems to be bidirectional, such that sleep disturbance may also complicate the trajectory of PTSD symptoms. In cross-sectional studies, sleep disturbance has been associated with increased odds (Swinkels et al., 2013) and severity of PTSD symptoms (Wallace et al., 2011, Cox et al., 2018). Specifically among veterans, those with insomnia report more symptoms of PTSD than those without insomnia (Pigeon et al., 2013). Similarly, among individuals with PTSD, sleep disturbance has been associated with elevations in PTSD symptoms the next day (Short et al., 2017). Again, the mechanism(s) underlying this association are unclear; however, sleep disturbance may lead to difficulty managing/controlling thoughts or emotions (Baglioni et al., 2010), which may exacerbate PTSD symptoms.
The Current Study
Given the established link between PTSD and sleep disturbance and, in turn, the link between sleep disturbance and alcohol use, we hypothesized that sleep disturbance would partially account for the longitudinal association between PTSD intrusions and alcohol problems (i.e., 6-month sleep disturbance would mediate the association between baseline PTSD intrusions and 12-month alcohol-related problems). We focused specifically on PTSD intrusions (as opposed to other symptoms of PTSD, such as avoidance) because theoretical models of insomnia identify intrusive thoughts as a mechanism for sleep disturbance (Spielman, 1987, Harvey, 2005). Because the association between PTSD and sleep disturbance may be bidirectional, we also examined 6-month PTSD intrusions as a mediator of the association between baseline sleep disturbance and 12-month alcohol problems. This extends previous research by examining the interplay of PTSD symptoms and sleep disturbance in predicting subsequent alcohol-problems, accounting for the temporal precedence of each variable.
Materials and Methods
Participants and Procedure
Veterans (N=361) were recruited through a VA to participate in a larger observational study examining post-deployment health behaviors among returning veterans (Metrik et al., 2016). Individuals were eligible if they were 18+ years and deployed post-9/11/2001. Because the primary aim of the larger study was to examine trajectories of cannabis use and problems over time, eligible participants also reported lifetime use of cannabis. Participants were excluded if they reported (a) suicide risk in the past 2 weeks, (b) psychotic symptoms in the past month, (c) cognitive impairment, as indicated by scores ≤23 on the Mini Mental Status Exam; or (d) active military duty at baseline. Of those who participated in the larger study, 325 reported alcohol use at baseline and were included in the analytic sample (93% male; see Tables 1–2).
Table 1.
Baseline demographics (N=325).
| Age in years, M (SD) | 33.3 (9.4) | |
| Male, n (%) | 303 (93%) | |
| Race/Ethnicity, n (%) | --- | |
| Asian American | 5 (2%) | |
| Black/African American | 14 (4%) | |
| Multiracial | 15 (5%) | |
| Native American or Native Alaskan | 1 (<1%) | |
| Native Hawaiian or Pacific Islander | 2 (<1%) | |
| Not reported | 2 (<1%) | |
| Other | 24 (7%) | |
| White/Caucasian | 262 (81%) | |
| Married, n (%) | 130 (40%) | |
| Experienced combat, n (%) | 60 (88%) | |
| Number of combat experiences, M (SD) | 5.2 (3.9) | |
| PTSD diagnosis, current (CAPS) | 40 (12%) | |
| Alcohol use disorder, current (SCID) | 111 (34%) | |
| Mild (2–3 symptoms) | 41 (13%) | |
| Moderate (4–5 symptoms) | 29 (9%) | |
| Severe (6+ symptoms) | 41 (13%) | |
| Cannabis use disorder, current (SCID) | 48 (15%) | |
| Mild (2–3 symptoms) | 27 (8%) | |
| Moderate (4–5 symptoms) | 11 (3%) | |
| Severe (6+ symptoms) | 10 (3%) | |
Table 2.
Variables at each assessment.
| Baseline (N=325) |
6 months (n=283) |
12 months (n=282) |
||
|---|---|---|---|---|
| Alcohol use in past 6mo, n (%) | 325 (100%) | 266 (94%) | 264 (94%) | |
| Drinks per week, M (SD) | 9.3 (12.3) | 9.4 (13.9) | 9.5 (15.0) | |
| Cannabis use in the past year, n (%) | 132 (40.6%) | --- | --- | |
| % cannabis use days in past 6mo, M (SD) | 16.0 (32.4) | 16.2 (33.2) | 16.4 (32.7) | |
| IDAS-TI PTSD intrusions, M (SD) | 8.3 (4.1) | 7.4 (3.5) | 7.3 (3.6) | |
| Positive screen for sleep disturbance, n (%) | 246 (76%) | 216 (77%) | 206 (74%) | |
| Number of sleep disturbance, M (SD) | 9.0 (4.1) | 8.8 (3.9) | 8.4 (3.8) | |
| Reported alcohol problems, n (%) | 150 (46%) | 135 (48%) | 120 (43%) | |
| Number of alcohol problems, M (SD) | 2.5 (4.9) | 2.9 (5.1) | 1.9 (3.3) | |
Note. IDAS-TI = Inventory of Depression and Anxiety Symptoms Traumatic Intrusions subscale.
Participants completed in-person assessments and a semi-structured diagnostic clinical interview with a trained research assistant at baseline, 6 months (n=283, 87%), and 12 months (n=282, 87%). All procedures were approved by university and VA Institutional Review Boards.
Measures
Demographics.
Participants indicated their age, gender, race/ethnicity, and marital status at baseline. They also indicated (yes/no) if they had been exposed to each of 13 potential combat experiences (e.g., being attacked or ambushed) (Hoge et al., 2004).
Substance use.
Quantity and frequency of alcohol and cannabis use were assessed using the Timeline Followback interview (Sobell & Sobell, 1992), which has been established as a reliable measure of alcohol and cannabis use in clinical and non-clinical samples (Robinson et al., 2014; Sobell & Sobell, 2003). Participants indicated the number of drinks/joints they consumed on each day in the past six months at baseline, 6 months, and 12 months. Memory aids (e.g., Thanksgiving) were included on the calendar to enhance recall. Research staff assisted in calculation of standard drinks/joints. In addition to the TLFB, participants indicated (yes/no) at baseline if they had used cannabis in their lifetime (study eligibility criterion) or in the past year.
Alcohol-related problems.
Alcohol problems were assessed using the Short Index of Problems (Miller et al., 1995). Participants indicated how often in the past three months they had experienced 15 consequences, such as harm to physical health or damage to a close relationship, as a result of drinking. Response options ranged from 0 (never) to 3 (daily or almost daily). This measure has demonstrated strong internal consistency and concurrent validity (Alterman et al., 2009). Reliability in this sample was high (α=.90).
Sleep disturbance.
Sleep disturbance was assessed using the Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1989). Participants rated their sleep in the past month on seven dimensions: (a) sleep quality, from very good to very bad; (b) sleep latency, or the time required to fall asleep; (c) sleep duration; (d) sleep efficiency, or amount of time spent in bed that was actually spent sleeping; (e) sleep disturbances, such as difficulty breathing or bad dreams; (f) use of sleep medication; and (g) daytime dysfunction, or frequency/severity of problems such as trouble staying awake. Subscale scores (α=.74) were combined to create a ‘sleep disturbance’ total score (range 0–21), which was used in analyses. Scores greater than 5 demonstrate good sensitivity and specificity in distinguishing poor sleepers from good sleepers (Buysse et al., 1989).
PTSD intrusions.
The Traumatic Intrusions subscale (IDAS-TI) of the Inventory of Depression and Anxiety Symptoms scale (Watson et al., 2007) was used to assess intrusive thoughts about trauma. Participants indicated the extent to which they experienced four traumatic symptoms (e.g., “I got upset thinking about something bad that happened”) in the past two weeks on a scale from 1 (not at all) to 5 (extremely). This subscale demonstrates strong convergent and discriminant validity in predicting PTSD assessed using clinical interview (Watson et al., 2008). Items demonstrated good internal consistency at all assessments (α=.86-.89).
Participants also completed the Clinician Administered PTSD Scale (Blake et al., 1995) with a trained research assistant. This measure was used to diagnose PTSD but could not be used to generate a symptom count because a skip-out assessment pattern was used to reduce participant burden (e.g., numbing symptoms were only assessed if the participant endorsed a sufficient number of avoidance symptoms). For descriptive purposes, the number of participants who met DSM-IV criteria for past-month PTSD is depicted in Table 1.
Data Screening and Analysis Plan
Analyses were conducted in Mplus version 8. Data for our outcome variable (12-month alcohol problems) were zero-inflated and over-dispersed; therefore, a zero-inflated mixed model with a negative binomial distribution (ZINB) was used (Atkins et al., 2013, Hu et al., 2011). ZINB models simultaneously evaluate two different distributions of data. The logistic portion of the model estimates a binary outcome (likelihood of being an excess zero; i.e., not experiencing alcohol problems). The count portion of the model estimates a count/continuous outcome (number of alcohol problems), including only the proportion of zeros that would be expected in a negative binomial distribution with the given sample mean and variance. Analyses utilized maximum likelihood estimation with standard errors that are robust to non-normality. Full maximum likelihood estimation was used to model missing data (Muthén and Muthén, 2017).
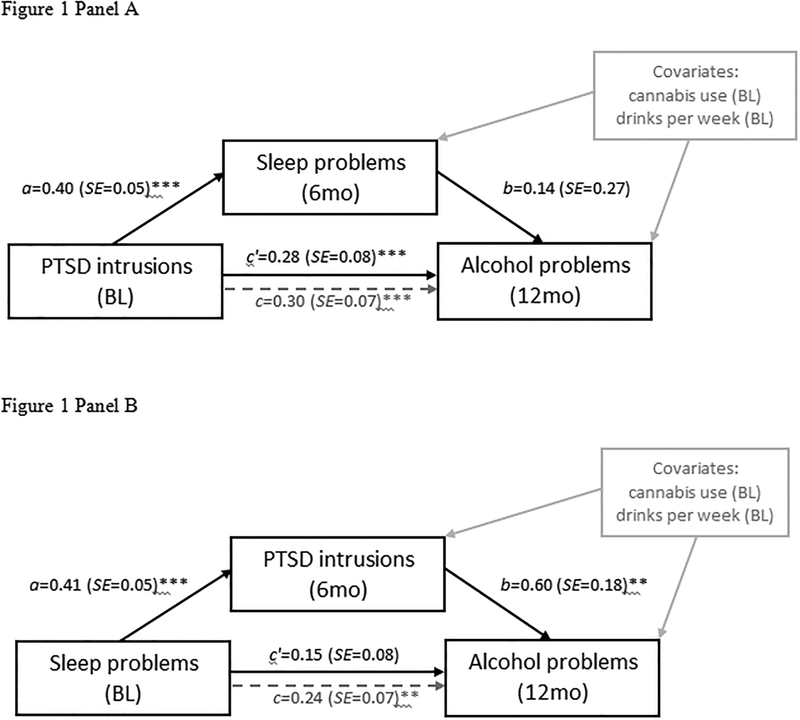
Mediation was tested using bootstrapped joint significance tests for indirect effects (MacKinnon et al., 2004). Briefly, mediation analysis involves examining associations between the independent variable and mediator (a-path); the mediator and outcome, controlling for the independent variable (b-path); the independent variable and outcome (c-path); and the independent variable and outcome, controlling for the mediator (c’-path; see Figure 1). We first examined the indirect effect of baseline PTSD intrusions on 12-month alcohol problems through 6-month sleep disturbance. We then examined a competing model: the indirect effect of baseline sleep disturbance on 12-month alcohol problems through 6-month PTSD intrusions. Analyses controlled for past-year cannabis use at baseline (yes/no) and baseline drinks consumed per week. Bivariate correlations among study variables are depicted in Table 3, and standardized effects and fit statistics for each model are presented in Table 4.
Figure 1.
Standardized estimates for models examining sleep disturbance as a mediator of the association between PTSD intrusions and alcohol problems (panel A) and PTSD intrusions as a mediator of the association between sleep disturbance and number of alcohol problems (panel B).
Table 3.
Zero-order correlations among variables (N=325).
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Drinks per week (BL) | --- | ||||||||||
| 2. | Cannabis use (BL) | 0.07 | --- | |||||||||
| 3. | Sleep disturbance (BL) | 0.07 | 0.18* | --- | ||||||||
| 4. | Sleep disturbance (6mo) | 0.06 | 0.15* | 0.68* | --- | |||||||
| 5. | Sleep disturbance (12mo) | 0.10 | 0.16* | 0.69* | 0.70* | --- | ||||||
| 6. | PTSD intrusions (BL) | 0.12* | 0.23* | 0.47* | 0.41* | 0.41* | --- | |||||
| 7. | PTSD intrusions (6mo) | 0.13* | 0.18* | 0.39* | 0.45* | 0.42* | 0.72* | --- | ||||
| 8. | PTSD intrusion (12mo) | 0.13* | 0.14* | 0.38* | 0.44* | 0.47* | 0.68* | 0.70* | --- | |||
| 9. | No. alcohol problems (BL) | 0.36* | 0.05 | 0.27* | 0.23* | 0.26* | 0.33* | 0.24* | 0.24* | --- | ||
| 10. | No. alcohol problems (6mo) | 0.35* | 0.06 | 0.22* | 0.25* | 0.18* | 0.34* | 0.30* | 0.25* | 0.61* | --- | |
| 11. | No. alcohol problems (12mo) | 0.36* | −0.01 | 0.18* | 0.13* | 0.22* | 0.23* | 0.26* | 0.16* | 0.46* | 0.62* | --- |
| 12. | Y/N alcohol problems (12mo) | 0.33* | 0.07 | 0.15* | 0.08 | 0.10 | 0.16* | 0.16* | 0.12 | 0.28* | 0.39* | 0.66* |
Note.
p<.05. BL = baseline. Mo = months. PTSD = posttraumatic stress disorder. Y/N = yes/no.
Table 4.
Standardized effects of variables predicting 12-month alcohol problems (N=325).
| Likelihood of NOT Having Alcohol Problems at 12mo |
Number of Alcohol Problems at 12mo | |||||||
|---|---|---|---|---|---|---|---|---|
| Intrusions > Sleep > Alcohol Problems | β | βSE | p | β | βSE | p | ||
| Intercept | 0.19 | 0.10 | .05 | −0.26 | 0.73 | .73 | ||
| BL cannabis use | −0.04 | 0.04 | .26 | −0.35 | 0.22 | .11 | ||
| BL drinks per week | −0.98 | 0.02 | <.001 | 0.52 | 0.16 | .001 | ||
| BL PTSD intrusions | 0.01 | 0.04 | .80 | 0.76 | 0.17 | <.001 | ||
| 6mo sleep disturbance (b-path) | −0.001 | 0.04 | .98 | 0.14 | 0.27 | .61 | ||
| Total direct effect (c’-path) | 0.01 | 0.04 | .80 | 0.28 | 0.08 | <.001 | ||
| Total indirect (mediated) effect | <.001 | 0.02 | .98 | 0.02 | 0.04 | .62 | ||
| Total effect (c-path) | 0.01 | 0.04 | .80 | 0.30 | 0.07 | <.001 | ||
| AIC | 2620.25 | |||||||
| BIC | 2673.22 | |||||||
| Sleep > Intrusions > Alcohol Problems | β | βSE | p | β | βSE | p | ||
| Intercept | 0.22 | 0.10 | .03 | −0.63 | 0.62 | .31 | ||
| BL cannabis use | −0.04 | 0.03 | .25 | −0.33 | 0.21 | .12 | ||
| BL drinks per week | −0.98 | 0.02 | <.001 | 0.49 | 0.14 | .001 | ||
| BL sleep disturbance | 0.01 | 0.03 | .77 | 0.40 | 0.19 | .03 | ||
| 6mo PTSD intrusions (b-path) | −0.02 | 0.03 | .53 | 0.60 | 0.18 | .001 | ||
| Total direct effect (c’-path) | 0.01 | 0.03 | .77 | 0.15 | 0.08 | .05 | ||
| Total indirect (mediated) effect | −0.01 | 0.01 | .53 | 0.09 | 0.03 | .01 | ||
| Total effect (c-path) | 0.002 | 0.03 | .94 | 0.24 | 0.07 | .001 | ||
| AIC | 2548.31 | |||||||
| BIC | 2601.28 | |||||||
Note. AIC=Akaike Information Criterion. BIC=Bayesian Information Criterion.
Results
Baseline Demographics
Participants were Veterans of the Iraq/Afghanistan era who reported a lifetime history of cannabis use and alcohol use in the past 6 months. As depicted in Table 1, 70 participants (22%) met criteria for a moderate to severe alcohol use disorder at baseline and 21 (6%) met criteria for a moderate to severe cannabis use disorder. Sixty participants reported combat experience, with 40 (12%) meeting criteria for current (past month) PTSD. Three out of four participants (76%) screened positive for sleep disturbance at baseline.
Sleep Disturbance as Mediator
The total effect (c-path) of baseline PTSD diagnosis on alcohol-related problems was significant when examining number of alcohol problems experienced at 12 months, but not likelihood of experiencing alcohol problems at 12 months (see Table 4). Baseline PTSD intrusions were positively associated with 6-month sleep disturbance (a-path; β=0.40, SE=0.05, p<.001); however, 6-month sleep disturbance was not associated with likelihood or number of alcohol problems at 12 months (b-path; see Table 4). In the logistic portion of the model, there was no direct (c’-path) or indirect (mediated) effect of PTSD intrusions on likelihood of alcohol problems. In the count portion of the model, there was a direct (c’-path) effect of baseline PTSD intrusions on number of alcohol problems at 12 months, with no indirect effect through 6-month sleep disturbance.
PTSD Intrusions as Mediator
The total effect (c-path) of baseline sleep disturbance on alcohol-related problems was also significant in the count but not logistic portion of the model (see Table 4). Baseline sleep disturbance was positively associated with 6-month PTSD intrusions (a-path; β=0.41, SE=0.05, p<.001). In turn, 6-month PTSD intrusions were positively associated with number but not likelihood of alcohol-related problems at 12 months (b-path; see Table 4). There was no direct (c’-path) or indirect effect of sleep disturbance on likelihood of alcohol problems. However, baseline sleep disturbance had an indirect (mediated) effect on number of 12-month alcohol problems through 6-month PTSD intrusions (see Table 4).
Discussion
Separate lines of research have documented associations between PTSD and alcohol problems, sleep and alcohol problems, and PTSD and sleep. This study extends this research by documenting the interplay of sleep and PTSD intrusions in predicting alcohol-related problems over time. PTSD intrusions at baseline were associated with more alcohol problems at 12 months, regardless of sleep disturbance. In contrast, sleep was associated with alcohol problems through its influence on PTSD intrusions. Specifically, sleep disturbance at baseline was associated with more intrusive thoughts about trauma at 6 months, which in turn were associated with more alcohol problems at 12 months. Thus, PTSD intrusions account in part for the longitudinal association between sleep and alcohol problems among Veterans. Because all models controlled for typical alcohol consumption, none of these associations can be attributed to drinking quantity.
Given the wealth of research linking PTSD symptoms to alcohol use and related problems (Miller et al., 2017b, Gaher et al., 2014), the direct effect of PTSD intrusions on alcohol problems was expected. However, the finding that sleep disturbance failed to account for this association was surprising. Instead, intrusive thoughts about trauma helped explain the association between sleep disturbance and alcohol-related problems. Sleep deprivation and disturbance have been linked to impairments in executive functioning and emotional reactivity (Baglioni et al., 2010, Nilsson et al., 2005), which in turn have been linked to alcohol use and related problems (Berking et al., 2011, Witkiewitz et al., 2015). Thus, we speculate that sleep-related impairments in cognitive/emotional functioning may lead to difficulty managing thoughts of PTSD, further compounding risk for alcohol-related problems.
Beyond their respective associations with alcohol-related problems, there was also a bidirectional association between sleep disturbance and PTSD intrusions in this sample. Specifically, baseline PTSD intrusions were associated with 6-month sleep disturbance, and baseline sleep disturbance was associated with 6-month PTSD intrusions. Although the temporal ordering of data in this study is a strength, the relative onset of PTSD versus sleep disturbance is unclear. For example, it is possible that baseline sleep disturbance was the result of trauma experienced prior to baseline. Without examining PTSD symptoms in individuals who are free from sleep disturbance at baseline (or vice versa), the true directionality of these associations cannot be determined. Research examining changes in sleep or PTSD symptoms among individuals who have not yet developed symptoms of the other disorder may help disentangle the bidirectionality of these constructs. Alternatively, daily diary or ecological momentary assessment studies may help characterize the extent to which these constructs fluctuate or interact with one another.
The prevalence and negative impact of sleep disturbance among Veterans warrants increased efforts to address sleep disturbance when treating comorbid conditions. Behavioral treatments for PTSD-related sleep disturbance have been associated with improvements in sleep quality, nightmares, and PTSD symptom severity (Germain et al., 2007, Margolies et al., 2013). Moreover, veterans report greater willingness to seek treatment for sleep than PTSD (Gutner et al., 2018). Thus, providers are encouraged to include sleep as a treatment target among patients with comorbid symptoms of PTSD. However, data from the current study suggest that sleep disturbance is associated with alcohol problems due in part to its association with intrusive thoughts about trauma. The association between sleep disturbance and intrusive thoughts is not novel, as cognitive arousal is conceptualized as a perpetuating factor in insomnia disorder (Harvey, 2005, Spielman, 1987). Nevertheless, the idea that sleep disturbance may influence intrusive thoughts about trauma extends previous studies indicating that this cognitive arousal process is not specific to thoughts about sleep. Indeed, several studies have documented associations between trauma- or stress-related intrusive thoughts and sleep disturbance (Kliewer and Lepore, 2015, Hall et al., 2000, Wright et al., 2010). Based on these findings, the cognitive component of therapy for insomnia (Harvey et al., 2014) may be particularly important among patients with comorbid PTSD and alcohol use disorders.
This study examined novel paths to alcohol problems using a longitudinal research design. However, there were limitations. Data were collected from primarily White, male veterans who reported a lifetime history of cannabis use. Approximately 62% of returning veterans report a lifetime history of cannabis use, with higher incidence rates (68%) among those with PTSD (Grant et al., 2016). Given these prevalence rates, findings are generalizable to a large number of returning U.S. veterans. That being said, research examining these longitudinal associations in more diverse samples, particularly women and non-White Veterans, is needed. The timeframe for assessments also varied across measures; for example, participants were queried on sleep disturbance over a one-month period and PTSD intrusions over a 2-week period. Given this inconsistency and the relatively long durations of time between assessments (6 months), studies examining day-to-day associations among variables are needed to determine if variables fluctuate in sync with one another. Because concurrent associations between variables (e.g., 12mo sleep problems to 12mo alcohol problems) were stronger than the lagged associations (6mo sleep problems to 12mo alcohol problems), studies may also examine the growth or decay of these associations over time. Similarly, the PSQI measures a variety of sleep disturbances (e.g., insomnia, nightmares, pain), some of which may be more strongly associated with intrusive thoughts and alcohol-related problems than others. Thus, future research may examine the specific aspects of sleep disturbance that drive these associations. Finally, data reflect longitudinal associations but do not establish causal effects. Randomized trials designed to manipulate PTSD/sleep are needed to determine if either PTSD intrusions or sleep cause change in alcohol-related problems (Kazdin, 2007).
Data from the current study suggest that the prospective association between sleep and alcohol-related problems is due in part to its association with intrusive thoughts about trauma. Given the negative impact of sleep disturbance on health outcomes and veterans’ willingness to seek treatment for sleep over treatment for other mental health disorders, sleep may be an important treatment target for veterans presenting with comorbid symptoms of PTSD and alcohol use disorder. In particular, the association between sleep and intrusive thoughts about trauma may inform clinical practice. Research examining the causal associations between sleep, PTSD, and alcohol problems in diverse samples is warranted.
Acknowledgments
This research was supported by the National Institute on Drug Abuse (R01DA033425, PIs Metrik/Borsari) and the National Institute on Alcohol Abuse and Alcoholism (K02AA13938, PI Jackson). NIH had no role in study design; data collection, analysis, or interpretation; manuscript preparation; or the decision to submit the paper for publication. The content is solely the responsibility of the authors and does not represent the official views of the NIH, the Department of Veterans Affairs, or the United States government. Study procedures were approved by the Brown University Institutional Review Board (IRB#1208000679).
References
- ADAMS RS, LARSON MJ, CORRIGAN JD, RITTER GA, HORGAN CM, BRAY RM & WILLIAMS TV 2016. Combat-acquired traumatic brain injury, posttraumatic stress disorder, and their relative associations with postdeployment binge drinking. Journal of Head Trauma Rehabilitation, 31, 13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ALTERMAN AI, CACCIOLA JS, IVEY MA, HABING B & LYNCH KG 2009. Reliability and validity of the alcohol short index of problems and a newly constructed drug short index of problems. Journal of Studies on Alcohol and Drugs, 70, 304–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ATKINS DC, BALDWIN SA, ZHENG C, GALLOP RJ & NEIGHBORS C 2013. A tutorial on count regression and zero-altered count models for longitudinal substance use data. Psychology of Addictive Behaviors, 27, 166–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BAGLIONI C, SPIEGELHALDER K, LOMBARDO C & RIEMANN D 2010. Sleep and emotions: a focus on insomnia. Sleep Med Rev, 14, 227–38. [DOI] [PubMed] [Google Scholar]
- BERKING M, MARGRAF M, EBERT D, WUPPERMAN P, HOFMANN SG & JUNGHANNS K 2011. Deficits in emotion-regulation skills predict alcohol use during and after cognitive-behavioral therapy for alcohol dependence. Journal of Consulting and Clinical Psychology, 79, 307–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BODEN MT & HOGGATT KJ 2018. Substance use disorders among Veterans in a nationally representative sample: Prevalence and associated functioning and treatment utilization. Journal of Studies on Alcohol and Drugs, 79, 853–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BUYSSE DJ 2014. Sleep health: Can we define it? Does it matter? SLEEP, 37, 9–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BUYSSE DJ, REYNOLDS CF III, MONK TH, BERMAN SR & KUPFER DJ 1989. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28, 193–213. [DOI] [PubMed] [Google Scholar]
- CALHOUN PS, SCHRY AR, WAGNER HR, KIMBREL NA, DENNIS P, MCDONALD SD, BECKHAM JC, DEDERT EA, KUDLER H & STRAITS-TROSTER K 2016. Th prevalence of binge drinking and receipt of provider drinking advice among US veterans with military service in Iraq or Afghanistan. The American Journal of Drug and Alcohol Abuse, 42, 269–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CAPALDI VF, GUERRERO ML & KILLGORE WDS 2011. Sleep disruptions among returning combat Veterans from Iraq and Afghanistan. Military Medicine, 176, 879–888. [DOI] [PubMed] [Google Scholar]
- CHAUDHARY NS, KAMPMAN KM, KRANZLER HR, GRANDNER MA, DEBBARMA S & CHAKRAVORTY S 2015. Insomnia in alcohol dependent subjects is associated with greater psychosocial problem severity. Addictive Behaviors, 50, 165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COX RC, MCINTYRE WA & OLATUNJI BO 2018. Interactive effects of insomnia symptoms and trauma exposure on PTSD: Examination of symptom specificity. Psychological Trauma: Theory, Research, Practice, and Policy, 10, 508–514. [DOI] [PubMed] [Google Scholar]
- FUEHRLEIN B, RALEVSKI E, O’BRIEN E, JANE JS, ARIAS AJ & PETRAKIS IL 2014. Characteristics and drinking patterns of veterans with alcohol dependence with and without post-traumatic stress disorder. Addictive Behaviors, 39, 374–378. [DOI] [PubMed] [Google Scholar]
- GAHER RM, SIMONS JS, HAHN AM, HOFMAN NL, HANSEN J & BUCHKOSKI J 2014. An experience sampling study of PTSD and alcohol-related problems. Psychology of Addictive Behaviors, 28, 1013–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GERMAIN A, SHEAR MK, HALL M & BUYSSE DJ 2007. Effects of a brief behavioral treatment for PTSD-related sleep disturbances: A pilot study. Behaviour Research and Therapy, 45, 627–632. [DOI] [PubMed] [Google Scholar]
- GILPIN NW & WEINER JL 2017. Neurobiology of comorbid post-traumatic stress disorder and alcohol-use disorder. Genes, Brain, and Behavior, 16, 15–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GRANT S, PEDERSEN ER & NEIGHBORS C 2016. Associations of posttraumatic stress disorder symptoms with marijuana and synthetic cannabis use among young adult U.S. veterans: A pilot investigation. Journal of Studies on Alcohol and Drugs, 77, 509–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GUTNER CA, PEDERSEN ER & DRUMMOND SPA 2018. Going direct to the consumer: Examining treatment preferences for veterans with insomnia, PTSD, and depression. Psychiatry Research, 263, 108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HALL M, BUYSSE DJ, NOWELL PD, NOFZINGER EA, HOUCK PR, REYNOLDS CF III & KUPFER DJ 2000. Symptoms of stress and depression as correlates of sleep in primary insomnia. Psychosomatic Medicine, 62, 227–230. [DOI] [PubMed] [Google Scholar]
- HARVEY A, BELANGER L, TALBOT L, EIDELMAN P, BEAULIEU-BONNEAU S, FORTIER-BROCHU E, IVERS H, LAMY M, HEIN K, SOEHNER AM, MERETTE C & MORIN CM 2014. Comparative Efficacy of Behavior Therapy, Cognitive Therapy, and Cognitive Behavior Therapy for Chronic Insomnia: A Randomized Controlled Trial. Journal of Consulting and Clinical Psychology, 82, 670–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HARVEY AG 2005. A cognitive theory and therapy for chronic insomnia. Journal of Cognitive Psychotherapy, 19, 41–59. [Google Scholar]
- HOGE CW, CASTRO CA, MESSER SC, MCGURK D, COTTING DI & KOFFMAN RL 2004. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. The New England Journal of Medicine, 351, 13–22. [DOI] [PubMed] [Google Scholar]
- HU MC, PAVLICOVA M & NUNES EV 2011. Zero-inflated and hurdle models of count data with extra zeros: Examples from an HIV risk reduction intervention trial. American Journal of Drug and Alcohol Abuse, 37, 367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JENKINS MM, COLVONEN PJ, NORMAN SB, AFARI N, ALLARD CB & DRUMMOND SPA 2015. Prevalence and Mental Health Correlates of Insomnia in First-Encounter Veterans with and without Military Sexual Trauma. Sleep, 38, 1547–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KAZDIN AE 2007. Mediators and mechanisms of change in psychotherapy research. Annual Review of Clinical Psychology, 3, 1–27. [DOI] [PubMed] [Google Scholar]
- KING PR, DONNELLY KT, WARNER G, WADE M & PIGEON WR 2017. The natural history of sleep disturbance among OEF/OIF veterans with TBI and PTSD and the role of proxy variables in its measurement. Journal of Psychosomatic Research, 96, 60–66. [DOI] [PubMed] [Google Scholar]
- KLIEWER W & LEPORE SJ 2015. Exposure to violence, social cognitive processing, and sleep problems in urban adolescents. Journal of Youth and Adolescence, 44, 507–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LANGDON KJ, FOX AB, KING LA, KING DW, EISEN S & VOGT D 2016. Examination of the dynamic interplay between posttraumatic stress symptoms and alcohol misuse among combat-exposed Operation Enduring Freedom (OEF) / Operation Iraqi Freedom (OIF) Veterans. Journal of Affective Disorders, 196, 234–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LEHAVOT K, KATON JG, CHEN JA, FORTNEY JC & SIMPSON TL 2018. Post-traumatic stress disorder by gender and veteran status. American Journal of Preventive Medicine, 54, e1–e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LIND MJ, BROWN E, FARRELL-CARNAHAN L, BROWN RC, HAWN SE, BERENZ E, MCDONALD SD, PICKETT T, DANIELSON CK, THOMAS S & AMSTADTER AB 2017. Sleep disturbances in OEF/OIF/OND veterans: Associations with PTSD, personality, and coping. Journal of Clinical Sleep Medicine, 13, 291–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LUXTON DD, GREENBURG D, RYAN J, NIVEN A, WHEELER G & MYSLIWIEC V 2011. Prevalence and impact of short sleep duration in redeployed OIF soldiers.: Sleep Journal of Sleep and Sleep Disorders Research, 34, 1189–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MACKINNON DP, LOCKWOOD CM & WILLIAMS J 2004. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39, 99–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MARGOLIES SO, RYBARCZYK B, VRANA SR, LESZCZYSZYN DJ & LYNCH J 2013. Efficacy of cognitive behavioral treatment for insomnia and nightmares in Afghanistan and Iraq veterans with PTSD. Journal of Clinical Psychology, 69, 1026–1042. [DOI] [PubMed] [Google Scholar]
- MCLAY RN, KLAM WP & VOLKERT SL 2010. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Military Medicine, 175, 759–762. [DOI] [PubMed] [Google Scholar]
- METRIK J, JACKSON KM, BASSETT SS, ZVOLENSKY MJ, SEAL K & BORSARI B 2016. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning Veterans with PTSD and MDD. Psychology of Addictive Behaviors, 30, 743–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MILLER MB, DIBELLO AM, CAREY KB & PEDERSEN ER 2017a. Insomnia moderates the association between alcohol use and consequences among young adult veterans. Addictive Behaviors, 75, 59–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MILLER SM, PEDERSEN ER & MARSHALL GN 2017b. Combat experience and problem drinking in veterans: Exploring the roles of PTSD, coping motives, and perceived stigma. Addictive Behaviors, 66, 90–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MILLER WR, TONIGAN JS & LONGABAUGH R 1995. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse (Project MATCH Monograph Series). In: US DEPARTMENT OF HEALTH AND HUMAN SERVICES, P. HS (ed.). Rockville, MD: National Institute on Alcohol Abuse and Alcoholism. [Google Scholar]
- MUTHÉN BO & MUTHÉN LK 2017. Mplus User’s Guide, Eighth Edition, Los Angeles, CA, Muthén & Muthén. [Google Scholar]
- NILSSON JP, SODERSTROM M, KARLSSON AU, LEKANDER M, AKERSTEDT T, LINDROTH NE & AXELSSON J 2005. Less effective executive functioning after one night’s sleep deprivation. Journal of Sleep Research, 14, 1–6. [DOI] [PubMed] [Google Scholar]
- SEELIG AD, JACOBSON IG, SMITH B, HOOPER TI, BOYKO EJ, GACKSTETTER GD, GEHRMAN P, MACERA CA, SMITH TC & TEAM MCS 2010. Sleep patterns before, during, and after deployment to Iraq and Afghanistan. Sleep, 33, 1615–1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHORT NA, ALLAN NP & SCHMIDT NB 2017. Sleep disturbance as a predictor of affective functioning and symptom severity among individuals with PTSD: An ecological momentary assessment study. Behaviour Research and Therapy, 97, 146–153. [DOI] [PubMed] [Google Scholar]
- SPIELMAN AJ 1987. A behavioral perspective on insomnia treatment. Psychiatric Clinics of North America, 10, 541–553. [PubMed] [Google Scholar]
- SWINKELS CM, ULMER CS, BECKHAM JC, BUSE N & CALHOUN PS 2013. The association of sleep duration, mental health, and health risk behaviors among U.S. Afghanistan/Iraq Era veterans.: Sleep Journal of Sleep and Sleep Disorders Research, 36, 1019–1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WALLACE DM, SHAFAZAND S, RAMOS AR, CARVALHO DZ, GARDENER H, LORENZO D & WOHLGEMUTH WK 2011. Insomnia characteristics and clinical correlates in Operation Enduring Freedom/Operation Iraq Freedom veterans with post-traumatic stress disorder and mild traumatic brain injury: An exploratory study. Sleep Medicine, 12, 850–859. [DOI] [PubMed] [Google Scholar]
- WATSON D, O’HARA MW, CHMIELEWSKI M, MCDADE-MONTEZ EA, KOFFEL E, NARAGON K & STUART S 2008. Further validation of the IDAS: Evidence of convergent, discriminant, criterion, and incremental validity. Psychological Assessment, 20, 248–259. [DOI] [PubMed] [Google Scholar]
- WATSON D, O’HARA MW, SIMMS LJ, KOTOV R, CHMIELEWSKI M, MCDADE-MONTEZ EA, GAMEZ W & STUART S 2007. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS). Psychological Assessment, 19, 253–268. [DOI] [PubMed] [Google Scholar]
- WITKIEWITZ K, MCCALLION E, VOWLES KE, KIROUAC M, FROHE T, MAISTO SA, HODGSON R & HEATHER N 2015. Association between physical pain and alcohol treatment outcomes: The mediating role of negative affect. Journal of Consulting and Clinical Psychology, 83, 1044–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WRIGHT CE, SCHNUR JB, MONTGOMERY GH & BOVBJERG DH 2010. Psychological factors associated with poor sleep prior to breast surgery: An exploratory study. Behavioral Medicine, 36, 85–91. [DOI] [PubMed] [Google Scholar]
- WRIGHT KM, BRITT TW, BLIESE PD & ADLER AB 2011. Insomnia severity, combat exposure, and mental health outcomes. Stress and Health: Journal of the International Society for the Investigation of Stress, 27, 325–333. [Google Scholar]
- ZAYFERT C & DEVIVA JC 2004. Residual Insomnia Following Cognitive Behavioral Therapy for PTSD. Journal of Traumatic Stress, 17, 69–73. [DOI] [PubMed] [Google Scholar]