Abstract
Background.
Cognitive-behavioral therapy (CBT) has long-standing evidence for efficacy in the treatment of alcohol use, yet implementation in clinical practice has been challenging. Delivery of CBT through technology-based platforms, such as web-based programs and mobile applications, has the potential to provide widespread access to this evidence-based intervention. While there have been reviews indicating the efficacy of technology-based delivery of CBT for various psychiatric conditions, none have focused on efficacy for alcohol use. The current meta-analysis was conducted to fill this research gap.
Method.
Descriptive data were used to characterize the nature of the literature on technology-delivered, CBT-based interventions for alcohol use (‘CBT Tech’). Inverse-variance-weighted effect sizes were calculated, and random effects, effect sizes were pooled in four sub-groups.
Results.
Fifteen published trials conducted primarily with at-risk or heavy drinkers were identified. Of these studies, 60% explicitly targeted alcohol use moderation. The content of CBT Tech programs varied, ranging from 4 to 62 sessions/exercises, with many programs combining elements of motivational interviewing (47%). With respect to efficacy, CBT Tech as a stand-alone treatment in contrast to a minimal treatment control showed a positive and statistically significant, albeit small effect (g = 0.20: 95% CI = 0.22, 0.38, kes = 5). When CBT Tech was compared to treatment as usual (TAU) effects were non-significant. However, when CBT Tech was tested as an addition to TAU, in contrast to TAU only, the effect size was positive, significant (g = 0.30: 95% CI = 0.10, 0.50, kes = 7), and stable over 12-month follow-up. Only two studies compared CBT Tech to in-person CBT, and this pooled effect size did not suggest superior efficacy.
Conclusions.
These results show a benefit for technology-delivered, CBT-based interventions as a stand-alone therapy for heavy drinking or as an addition to usual care in specialty substance use settings.
Keywords: Alcohol Treatment, Cognitive-Behavioral, Computer-based Treatment, Technology-based Treatment, Meta-Analysis
Introduction
Cognitive behavioral therapy (CBT) is one of the most-studied approaches for the treatment of alcohol use disorder (AUD), with considerable empirical support establishing its efficacy. The most recent meta-analysis of CBT for substance use has indicated a moderate effect in comparison to minimal treatment and non-significant differences in effect when compared to other evidence-based therapies (Magill and Ray, 2009). As such, CBT is widely considered an evidence-based treatment for AUD and included in multiple practice guidelines (American Psychiatric Association, 2018, American Psychiatric Association, 2010, National Institute on Alcohol Abuse and Alcoholism, 2014). Over the years, the delivery of CBT for substance use has become increasingly diverse in an attempt to broaden its appeal and enhance effectiveness for heterogeneous populations of alcohol users. It has been delivered as a treatment approach for abstinence-based relapse prevention (Monti and Rohsenow, 1999), harm reduction (Marlatt and Witkiewitz, 2002), and as part of school-based prevention programs (e.g., Botvin et al., 2000). CBT has also been combined with other evidence-based approaches such as motivational enhancement therapy (e.g., Riper et al., 2014a) and reinforcement-based treatments (e.g., Community Reinforcement Approach - CRA; Smith, Meyers, & Miller, 2001), as well as integrated with mindfulness practices (e.g., Mindfulness-Based Relapse Prevention; Bowen et al., 2010). While the development, evaluation, and dissemination of these CBT and combined approaches for treating alcohol use continues, the challenge of implementing them in widespread clinical practice has remained (McHugh and Barlow, 2010). However, one of the most exciting developments in terms of the delivery of CBT, and other evidence-based treatments, is the use of technology as a platform for delivery.
The ability to deliver an evidence-based treatment, such as CBT, through technology-based methods (e.g., internet, web-based, and mobile platforms) offers several advantages over traditional face-to-face delivered treatments. These methods are highly accessible and available, given the ubiquity of technology in individuals’ daily lives. Consider that nearly 9 in 10 adults in the United States use the internet (Smith, 2017), yet only about 1 in 10 of those with a substance use disorder receive any type of specialty treatment (U.S. Department of Health and Human Services, 2016). Common reasons for not seeking treatment include stigma, embarrassment, and difficulty with access, all of which are barriers that technology-delivery has the potential to address (Cunningham et al., 2011). Technology can not only serve as an alternative to face-to-face services, but it can also function as a clinician-extender (Marsch et al., 2014). Finally, one of the primary reasons for the limited delivery of evidence-based treatments in clinical practice is the limited preparedness of providers, including insufficient training, limited competency, and overestimation of providers’ skills, which has been particularly relevant to the delivery of complex modalities such as CBT (Fairburn and Cooper, 2011, Herschell et al., 2010, Creed et al., 2016). A major obstacle is that most private and publicly-funded addiction treatment centers do not have the resources to provide the training, monitoring, and ongoing supervision that will ensure the level of fidelity in CBT treatment delivery that is required in the clinical trials generating the evidence for efficacy (Olmstead et al., 2012, Sholomskas et al., 2005, Rakovshik and McManus, 2010, McLellan et al., 2003). Using technology to deliver an evidence-based treatment enhances treatment fidelity by providing a highly standardized delivery of complex activities, while reducing the costs and demands associated with training and supervising health care professionals (Marsch et al., 2014, Carroll & Kiluk, 2017).
The great promise of delivering evidence-based treatments through technology-based platforms is predicated on the notion that they are in fact efficacious at treating the condition or disorder being targeted (Kiluk et al., 2011). The process of transferring the components of an evidence-based treatment from a face-to-face format to a technology-based format should not assume a corresponding transfer of efficacy. The rapid pace of development of technology-based tools carries the risk of commercialized, unproven treatments entering the marketplace with detrimental effects (Bhugra et al., 2017). Therefore, it is important to establish the efficacy of technology-delivered treatments with the same level of methodological rigor and statistical evaluation as in-person treatments. Here, multiple reviews and meta-analyses of technology-delivered CBT interventions have indicated efficacy for treating a range of mental health conditions, including anxiety, depression, and somatic disorders (Andersson et al., 2014, Andrews et al., 2018, Karyotaki et al., 2018, Sijbrandij et al., 2016, Spurgeon and Wright, 2010). Yet, a meta-analysis on the efficacy of technology-delivered CBT for alcohol use has not been conducted. There are reviews of technology-delivered interventions for alcohol as well as other drug use (Bickel et al., 2011, Moore et al., 2011, Rooke et al., 2010, Sugarman et al., 2017, Tait et al., 2013), but none of these reviews have evaluated the evidence of CBT or CBT-based interventions, specifically.
The purpose of this study is to fill this important research gap by systematically examining the evidence for technology-delivered, CBT-based interventions (hereafter referred to as ‘CBT Tech’) targeting alcohol use through meta-analysis. Before moving forward, it is important to provide a brief definition of the term technology-delivered used here to characterize CBT Tech. A broad range of terms have been used to label/describe these types of interventions, such as web-based therapy, e-therapy, tele-mental health, computer-mediated interventions, computer-assisted therapies, digital therapies, mobile health applications, and mHealth. For the purposes of this meta-analysis, we will focus on CBT-based interventions (i.e., those identified as CBT or containing key elements of CBT, such as coping skills training) that have been programmed to be delivered through a computer (e.g., web-based program) or mobile device (e.g., mobile app). This does not include interventions in which a clinician provides CBT through e-mail, text, video-chat, or other online counseling methods, as these could still be considered clinician-delivered interventions using the internet purely as a medium for communication. The focus of this report is on the efficacy of computerized interventions delivering CBT-based content, when contrasted with a range of experimental controls.
Materials and Methods
Primary Study Literature Search
A literature search was conducted through July of 2019 to identify studies for a large-scale meta-analytic project on CBT treatment for alcohol or other drug use disorders (R21#AA026006). The first step involved a title, abstract, keyword, and subject search by intervention (‘cognitive behavioral therapy’ OR ‘coping skills training’ OR ‘relapse prevention’) AND outcome (‘alcohol’ OR ‘cannabis’ OR ‘cocaine’ OR ‘dual diagnosis’ OR ‘dual disorder’ OR ‘heroin’ OR ‘illicit drug’ OR ‘marijuana’ OR ‘methamphetamine’ OR ‘opiate’ OR ‘polysubstance’ OR ‘stimulant’ OR ‘substances’) AND study (‘efficacy’ OR ‘randomized clinical trial’ OR ‘randomized controlled trial’) terms in the PubMed database. Next, searches of the Cochrane Register and EBSCO (e.g., PsychInfo) were performed. Abstract screening occurred by two raters in Abstrackr (Wallace et al., 2012). Finally, a bibliographic search of eligible studies and literature reviews was completed (Carroll and Kiluk, 2017, Moore et al., 2011, Riper et al., 2014b, Rooke et al., 2010, Sugarman et al., 2017). Figure 1 provides a visual representation of study inclusion, and although all drug use disorders were initially of interest, the majority of studies addressed alcohol use. As a result, studies targeting cocaine/stimulant (Carroll et al., 2014, Schaub et al., 2012, Tait et al., 2015, Schaub et al., 2019), opioid (Marsch et al., 2013), or substance dependence disorders (Campbell et al., 2014, Carroll et al., 2009, Kiluk et al., 2018) were removed from review to improve sample homogeneity1 (final sample K = 15 studies; N = 9,838 participants).
Figure 1.
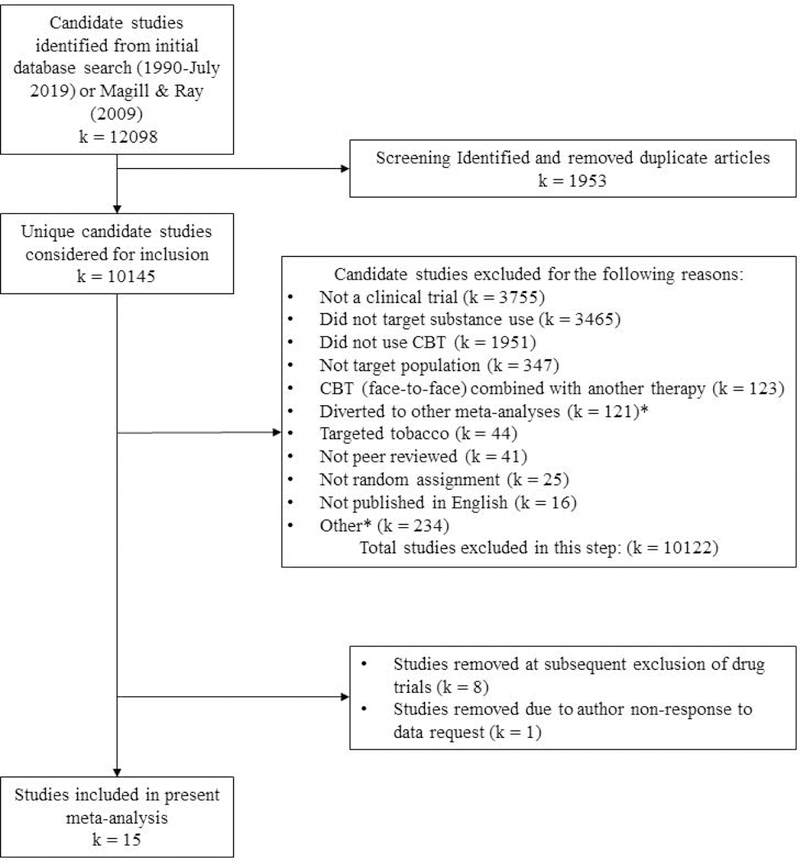
Flow of primary study inclusion.
Notes. K/k is defined as number of groups. CBT = cognitive behavioral therapy * e.g., Trials of in-person CBT; pharmacotherapy trials, including CBT.
Primary Study Inclusion
Study inclusion criteria were as follows: 1) English language publication, 2) peer-reviewed publication, 3) date range: 1990 to 2019, 4) study methodology: randomized controlled trial, 5) age: adult (age ≥ 18), 6) alcohol criterion: alcohol users meeting criteria for a disorder (i.e., DSM III-R through 5; American Psychiatric Association, 1987, 1994, 2000, 2013), non-dependent/heavy consumption (e.g., AUDIT score > 8; Saunders et al., 1993), or poly-drug use where alcohol use was reported among the sample majority and was a primary targeted outcome within the trial, and 7) intervention: cognitive-behavioral or combined cognitive-behavioral (i.e., combined with elements of other evidence-based treatments) therapy delivered in a technology-based format (see Table 1 and Supplemental Table 1 for details). The cognitive-behavioral criterion was met if the study intervention was described as CBT or Relapse Prevention, or included key elements of CBT, such as functional analysis, avoidance of high-risk situations, and/or coping skills training.
Table 1.
CBT Tech efficacy by type of contrast
| First author (date) | N1 | Treatment | Contrast | Month | Population2 | Outcome | ROB3 | g(95%CI) |
|---|---|---|---|---|---|---|---|---|
| CBT Tech compared to assessment only or minimal treatment | ||||||||
| Blankers et al. (2011) | 137 | Self-help Alcohol Online | waitlist | 3 | at risk | weekly consumption | L | 0.35(0.01, 0.69) |
| Gajecki et al. (2017) | 186 | TeleCoach™ Application | waitlist | 3 | at risk | proportion binge drank | U | 0.38(0.05, 0.71) |
| Hester and Delaney (1997) | 42 | Behavioral Self-Control Program | waitlist | 1 | at risk | days drank | U | 0.53(−0.09, 1.15) |
| Leeman et al. (2016) | 102 | Email intervention with Protective Behavioral Strategies (THRIVE) | email education | 1 | at risk | weekly consumption | L | 0.03(−0.36, 0.41) |
| Riper et al. (2008) | 261 | Drinking Less website | web-based brochure | 6 | at-risk | weekly consumption | H | 0.41(0.17, 0.66) |
| Wallace et al. (2011) | 7935 | Down Your Drink website (interactive) | Down Your Drink website (text only) | 3 | at risk | days heavy drank | L | 0.06(−0.05, 0.17) |
| CBT Tech compared to TAU | ||||||||
| Cunningham (2012) | 170 | Alcohol Help Center website | Check Your Drinking Feedback | 6 | at-risk | weekly consumption | H | −0.02(−0.32, 0.28) |
| Hester et al. (2013) | 169 | Overcoming Addiction | SMART Recovery online meeting | 3 | at risk | days abstinent | U | −0.37(−0.86, 0.13) |
| Kiluk et al. (2016) | 46 | CBT4CBT | TAU | 3 | at risk/dependent | days abstinent | U | −0.28(−0.85, 0.29) |
| CBT Tech plus TAU versus TAU only | ||||||||
| Acosta et al. (2017) | 162 | Thinking Forward plus TAU | TAU | 3 | at risk/poly-drug | days heavy use | L | 0.55(0.24, 0.87) |
| Brendryen et al. (2014) | 244 | Balance plus online screening | online screening | 3 | at risk | weekly consumption | L | 0.13(−0.12, 0.38) |
| Farren et al. (2015) | 55 | Computerized Cognitive-Behavioral Relapse Prevention plus TAU | TAU | 3 | dependent | proportion abstinent | H | 0.02(−0.58, 0.63) |
| Hester et al. (2011) | 80 | Moderate Drinking plus Moderation Management | Moderation Management | 3 | at risk | days abstinent | U | 0.56(0.13, 0.99) |
| Hester et al. (2013) | 169 | Overcoming Addiction plus SMART Recovery | SMART Recovery | 3 | at risk | days abstinent | U | 0.38(0.08, 0.69) |
| Kay-Lambkin et al. (2009) | 97 | Computer Delivered Therapy (SHADE) plus Brief Intervention | Brief Intervention | 12 | at risk/poly-drug | heavy use | U | 0.47(−0.11, 1.05) |
| Kay-Lambkin et al. (2011) | 274 | Computer Delivered Therapy (SHADE) plus Person-Centered Therapy | Person-Centered Therapy | 3 | at risk/poly-drug | proportion abstinent | U | 0.44(−0.32, 1.20) |
| Kiluk et al. (2016) | 44 | CBT4CBT plus TAU | TAU | 3 | at risk/ dependent |
days abstinent | U | −0.23(−.081, 0.35) |
| CBT Tech compared to CBT with therapist | ||||||||
| Blankers et al. (2011) | 137 | Self-help Alcohol Online | online therapy | 3 | at risk | weekly consumption | L | −0.20(−0.53, 0.14) |
| Kay-Lambkin et al. (2009)4 | 97 | Computer Delivered Therapy | in-person therapy | 12 | at risk/poly-drug | heavy use | U | −0.29(−0.93, 0.35) |
Notes. K = 15; CBT = cognitive behavioral therapy. TAU = treatment as usual.
N randomized.
Population determined by study inclusion criteria (i.e. at-risk = ≥ 8 on the Alcohol Use Disorders Identification Test [AUDIT; Saunders et al. (1993)]; poly-drug = AUDIT or drug screen criteria where >50% of the sample reported current alcohol use; dependent = met diagnostic criteria for alcohol dependence disorder).
ROB = Risk of Bias (Higgins et al., 2011) study-level assessment suggested that 3 of 15 studies were high risk. Common reasons for high risk designation were lack of blinding of participants or research staff and/or lack of intent to treat outcome analyses.
Due to non-response to data request, Kay-Lambkin et al. (2011) therapist contrast arm not included in pooled effect size.
Primary Study Characteristic Variables
There were several study characteristic variables of interest to this meta-analysis. First, effect sizes were pooled by the following substantive contrasts: 1) CBT Tech compared to assessment only or minimal treatment (e.g., a pamphlet with alcohol information), 2) CBT Tech compared to a passive treatment or treatment as usual [TAU], 3) CBT Tech added to TAU compared to TAU only, and 4) CBT Tech compared to CBT delivered by a therapist. Additionally, effect sizes were pooled for early (1–3 months) and late (6–12 months) follow-up outcomes. Second, study characteristic descriptors were: mean age of participants, percent female participants, percent White participants, percent Black participants, percent Latino/a participants, substance use severity/sample inclusion (dependence, at risk or heavy use), treatment length (number of content modules), CBT Tech format (CBT only, CBT combined with other evidence-based treatment elements), study context (community sample, specialty substance use or mental health clinic, other setting), publication country (United States, other country), and study-level risk-of-bias score (Higgins et al., 2011). Data extraction guidelines were detailed in a study codebook available, upon request, from the last author. Data were extracted using consensus methods between the third and fourth authors (agreement rate 94.7%), with review by the last author.
Primary Study Outcome Variables
The standardized mean difference was used as the effect size metric in this meta-analysis2. Hedges’ g includes a correction, f, for a slight upward bias in the estimated population effect (Hedges, 1994).
Prior to pooling, effect sizes were weighted by the inverse of the estimate variance (Hedges and Olkin, 1985). Primary studies provided data on more than one outcome; therefore, data for effect size extraction were selected based on a decisional hierarchy in the following order: 1) alcohol measures of quantity or frequency in the form of means and standard deviations or 2) sample proportions. When multiple months of follow-up data were provided, the latest time point in two time intervals was selected (i.e., 1–3 months, 6–12 months). Effect sizes were reverse scored as needed (e.g., number of days drank) such that a positive effect size indicated a positive treatment outcome across all studies. Finally, when data from publications were insufficient for effect size calculation, raw data were obtained from authors where possible (e.g., Hester et al., 2013).
Data Analysis and Sensitivity Analysis
Study-level effect sizes were pooled using random effects assumptions. Here, there is an assumed distribution for the population effect with both systematic and random sources of variability (Hedges and Vevea, 1998). The significance of the Q-test determined whether statistically significant between-study heterogeneity existed within a given pooled estimate and regardless of significance, the I2 provided a value for percent heterogeneity due to systematic rather than error variance3. If I2 estimates exceeded 50% and k ≥ 54, effect moderator analyses were undertaken in attempt to explain systematic variation between studies. We considered heterogeneity analysis as a method for examining the validity of our a priori method of sub-group effect pooling. To test for potential publication bias, the relationship between error and effect size was examined with rank correlation (Begg and Mazumdar, 1994) and graphical (Egger et al., 1997) methods.
Results
Primary Study Descriptive Characteristics
The sample included 15 randomized trials of CBT Tech for adult alcohol or poly-drug use published between 1997 and 2017. The mean sample size was 656 participants with a minimum of 42 (Hester and Delaney, 1997) and a maximum of 7935 (Wallace et al., 2011). A large majority of these studies included non-dependent drinkers (95%). Additionally, 60% of studies explicitly targeted alcohol use moderation as indicated within the study title, intervention title, or study aims. The samples’ mean age was 39 (SD = 8), and samples were 46% female (SD = 16%) on average. There were slightly more non-US-based (k = 9), compared to US-based (k = 6), clinical trials and racial/ethnic data were more likely to be reported in US-based studies. Among studies that reported racial/ethnic sample statistics, the samples were 72% White (SD = 20%), 34% Black (SD = 28%), and 13% Latino/a (SD = 10%). Countries other than the US were: Netherlands (Blankers et al., 2011, Riper et al., 2008); Norway (Brendryen et al., 2014); Canada (Cunningham, 2012); Ireland (Farren et al., 2015); Sweden (Gajecki et al., 2017); Australia (Kay-Lambkin et al., 2011, Kay-Lambkin et al., 2009); and United Kingdom (Wallace et al., 2011). Regarding sampling method, the majority of studies recruited participants from the community via online advertising (k = 10), followed by within specialty clinics or medical facilitates (k = 3), and two studies took place on college campuses. Content of the CBT Tech interventions consisted of 4 to 62 sessions/modules/exercises that varied in time required for completion. With respect to intervention theoretical underpinnings and components, nearly all interventions were described as CBT (47%) or CBT combined with elements of motivational interviewing or motivational enhancement therapy (47%).
CBT Tech Effect Size by Substantive Contrast
Primary study effect sizes were pooled by contrast type at early and late follow-ups. The majority of studies presented early follow-up outcomes and these data points are detailed in Table 1. When effect size data were only available for late follow-up (Cunningham, 2012, Kay-Lambkin et al., 2009, Riper et al., 2008), these data points are provided in Table 1.
CBT Tech compared to assessment only or minimal treatment.
Studies of CBT Tech compared to assessment only, waitlist, or minimal treatment showed a positive and significant effect at early follow-up (g = 0.20: 95% CI = 0.22, 0.38, p = .03; tau2 = .02, Q > .05, I2 = 44%; kes = 5). At late follow-up, pooled effect magnitude was similar, but non-significant (g = 0.20: 95% CI = −0.03, 0.43, p = .09; tau2 = .03, Q > .05, I2 = 64%; kes = 3). While heterogeneity data suggested some systematic variability, relative to random variability, heterogeneity and k values did not meet thresholds for further moderation analyses. For assessment of bias due to publication status in studies contrasting CBT Tech with a minimal control, the rank order correlation showed no relationship between precision and effect size (Figure 2; k = 6; τ = −0.06, p > .05).
Figure 2.
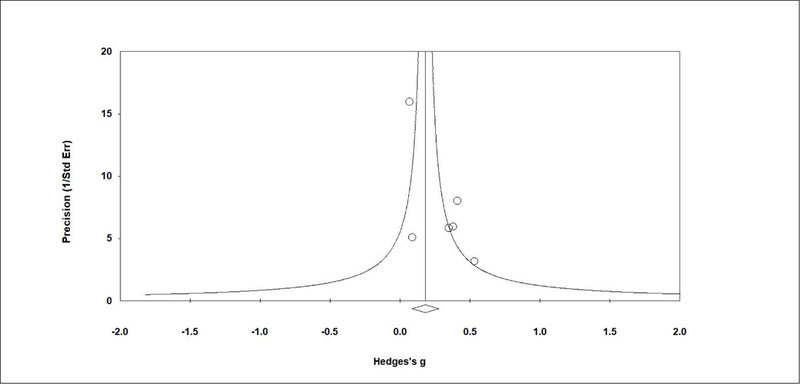
Plot of assessment of publication bias – minimal contrast studies
Notes. Small sample/small effect studies are assumed to characterize unpublished research, resulting in a significant and negative relationship, thus an asymmetrical funnel plot, when publication bias is present. Assessment of bias in CBT Tech effect compared to assessment only or minimal treatment shows some asymmetry, but the rank order correlation suggested no statistical relationship between precision and effect size (k = 6; τ = −0.06, p > .05).
CBT Tech alone compared to TAU.
Only two studies contrasted CBT Tech with TAU at the early follow-up, and the pooled effect size was g = −0.33 (95% CI = −0.70, 0.05, p = .09; tau2 = .00, Q > .05, I2 = 0%; kes = 2). The late follow-up effect size showed a similar result. Specifically, the effect of CBT Tech compared to TAU was negative, non-significant, and acceptably homogeneous (g = −0.10: 95% CI = −0.38, 0.18, p = .49; tau2 = .00, Q > .05, I2 = 5%; kes = 2).
CBT Tech added to TAU compared to TAU alone.
The largest number of studies in this review examined CBT Tech as an addition to TAU compared to TAU alone. The pooled effect size across these studies was positive and significant at early follow-up (g = 0.30: 95% CI = 0.10, 0.50, p = .003; tau2 = .03, Q >.05, I2 = 39%; kes = 7). At late follow-up, the pattern of results was consistent with that observed for early follow-up (g = 0.31: 95% CI = 0.05, 0.57, p = .02; tau2 = .04, Q > .05, I2 = 46%; kes = 5). Figure 3 shows the plot of primary studies by TAU contrast, and does not suggest bias due to publication status (k = 11; τ = −0.04, p > .05).
Figure 3.
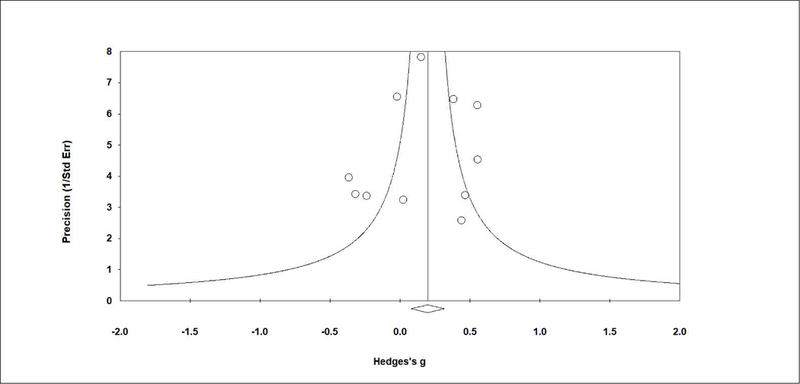
Plot of assessment of publication bias – TAU contrast studies
Notes. Small sample/small effect studies are assumed to characterize unpublished research, resulting in a significant and negative relationship, thus an asymmetrical funnel plot, when publication bias is present. Assessment of bias in the effect of CBT Tech alone or combined with TAU compared to TAU alone showed good symmetry, and the rank order correlation suggested no relationship between precision and effect size (k = 11; τ = −0.04, p > .05).
CBT Tech compared to CBT delivered by a therapist.
The final group of contrasts included studies where one trial arm examined CBT Tech compared to CBT delivered by a therapist, either in-person or via online therapy. Only a minority of studies included this contrast, and the pooled effect did not support differential efficacy between conditions (g = −0.22: 95% CI = −0.52, 0.08, p = .15; tau2 = .00, Q > .05, I2 = 0%; kes = 2). Because so few studies contributed to this pooled effect estimate, we combined early (Blankers et al., 2011) and late (Kay-Lambkin et al., 2009) follow-up studies (see Table 1).
Discussion
In this study, we conducted a meta-analysis of technology-delivered, CBT-based interventions targeting alcohol use that were evaluated in 15 independent randomized controlled trials. In general, results suggest these CBT Tech interventions are efficacious at reducing alcohol use when delivered as a stand-alone treatment or when tested as an addition to usual care. The overall magnitude of pooled effects were small as defined by Cohen (1998), but these benchmarks should be considered only in the absence of an empirically-derived distribution of effect sizes for a given population (Tanner-Smith et al., 2018). The largest pooled effects found here (g = 0.3) were produced from studies that evaluated CBT Tech interventions as an add-on to treatment as usual compared to treatment as usual only. This effect size indicates that the difference between the two conditions is equivalent to about one-third of a standard deviation (Ellis, 2010). The magnitude of effects found here are similar to those found in other meta-analyses of internet/computer-based interventions for alcohol and tobacco (Rooke et al., 2010) and marijuana (Tait et al., 2013) use, yet much smaller than pooled effect sizes found in meta-analyses of internet/computer-based CBT-specific interventions for depression and anxiety disorders (Andrews et al., 2018, Dettore et al., 2015, Sijbrandij et al., 2016). However, emerging data suggests even small reductions in drinking quantity (e.g., reduction from 4 drinks to 3 drinks per day) have been associated with significant improvements in markers of physical health and quality of life (Witkiewitz et al., 2018). Only two trials reviewed here evaluated a stand-alone CBT Tech compared to therapist-delivered CBT, which produced non-significant between-group effects, similar to pooled effects indicating no difference between internet-delivered CBT and face-to-face CBT for other psychiatric conditions (Carlbring et al., 2018).
This is, to our knowledge, the first meta-analysis conducted on CBT-based, technology-delivered interventions for at-risk or dependent alcohol users. Although the overall results regarding efficacy are promising, the varied characteristics of the interventions and trials included in this analysis suggest any firm conclusions would be premature at this time. For one, a large proportion of the CBT-based interventions reviewed here combined elements of other evidence-based approaches, with motivational interviewing/enhancement therapy being one of the most commonly integrated. While attention to patient motivation is often incorporated in CBT for alcohol use manuals (Monti et al., 2002), these strategies are not a primary component of the intervention, as was the case in many of the CBT Tech programs reviewed here (e.g., Wallace et al., 2011). The combination of CBT and motivational interviewing became increasingly common following the Combined Behavioral Intervention (CBI) approach (COMBINE Study Research Group, 2003) employed for AUD in the COMBINE Study (Anton et al., 2006). Other programs included in this meta-analysis are ‘packaged’ approaches that combine cognitive behavioral relapse prevention skills with personalized feedback, such as the Tertiary Health Research Intervention via Email (THRIVE; Leeman et al., 2016), or with acceptance and mindfulness exercises (Balance; Brendryen et al., 2014). Thus, the number of ‘pure’ CBT technology-based interventions, and therefore the evidence for their efficacy, is currently relatively limited.
The CBT Tech programs also varied in terms of amount of content. Standard CBT interventions evaluated in randomized controlled trials for alcohol use typically include 8–12 sessions of weekly face-to-face individual or group psychotherapy; the average number of sessions from alcohol studies included in the latest meta-analysis of CBT was 12 (Magill and Ray, 2009). Although the average number of sessions/modules across the CBT Tech programs reviewed here was 13, they ranged from 4 to 62. Excluding the program with 62 (Balance; Brendryen et al., 2014), the average number of sessions/modules was 9. While this may appear comparable to standard face-to-face CBT interventions, the amount of time per session/module in CBT Tech programs cannot be assumed equivalent to the length of a CBT session. For instance, each of the 62 exercises in the Balance program takes 3–10 minutes to complete (Brendryen et al., 2014), whereas face-to-face CBT sessions typically take 45–60 minutes. Therefore, some CBT Tech programs reviewed here could be characterized as relatively brief interventions. Moreover, treatment adherence and exposure to these programs varied. For instance, among those assigned to the specific CBT Tech intervention being evaluated, Riper and colleagues (2008) reported only 45% actually accessed it, whereas Cunningham (2012) reported 71%, and Kiluk and colleagues (2016) reported 100% accessed the program at least once, respectively. It should be noted that because many CBT Tech programs are available 24 hours/7 days per week and individuals are encouraged to access the material as frequently as desired, there is often no a priori intended length of exposure reported. The great advantage of accessibility of these programs does create some complexity (and potential weakness) when attending to issues of internal validity in randomized trials (Kiluk et al., 2011). Therefore, it is difficult to evaluate treatment adherence and exposure across CBT Tech programs, and many published reports did not include this information (for further detail see Supplemental Table 1).
One of the major benefits of technology-delivered interventions is the ability to reach large populations of individuals with the target problem or condition, which was clearly evident in these trials. The average sample size in the RCTs was 656, with a range from 42 to 7,935. Even after excluding the 7,935 outlier (Wallace et al., 2011), the average sample size was 136. For face-to-face CBT trials for alcohol use from the Magill and Ray (2009) meta-analysis, the average sample size was 198, but after excluding two outliers (Project MATCH Research Group, 1997), the average sample size was 90. The opportunity to provide a CBT-based intervention for alcohol use without the need for individuals to attend in-person sessions at a specialty clinic, university counseling center, or other community-based facility greatly enhances the reach of the intervention. Also, the samples included in the trials reviewed here represent a diverse population of individuals with hazardous alcohol use and/or alcohol use disorder, with females and racial/ethnic minorities making up nearly half of the study samples (for those reporting demographic factors; i.e., primarily US-based studies). Furthermore, delivering CBT or components of CBT through web-based programs or mobile applications eliminates the need for careful selection, training, and fidelity monitoring of therapists, and the ongoing expert supervision/coaching required to maintain CBT fidelity that drive up costs for community clinics and research trials, alike. Lastly, the availability of technology-delivered CBT may serve as an adjunct to pharmacotherapy, towards the goal of integrative care (Ray et al., 2019). This is consistent with the notion that patients seeking treatment for problem drinking should be offered a full range of treatments in conjunction with pharmacotherapy, including CBT (National Institute on Alcohol Abuse and Alcoholism, 2005). Such considerations have become increasingly pressing in the current landscape of healthcare with high demand for addiction treatment and low availability of specialized services (Dimoff et al., 2017).
Limitations and Conclusions
While the development of technology-delivered versions of CBT (and CBT components) has been rapidly expanding, our meta-analysis was constrained by a relatively small number of studies targeting alcohol use. Given the context provided by a larger meta-analytic project on CBT efficacy for alcohol and other drug use (Magill et al., under review), we entered this analysis with a goal of deriving a set of valid and statistically homogeneous sub-groups of studies upon which to base pooled effect estimates. We believe we achieved this goal with non-significant Q tests and less than substantial I2 values in all but one pooled effect size, and this latter sub-group was comprised of only three studies. Under the conditions of small sample size and effect homogeneity, our ability to detect clinically-informative effect moderators was limited. As such, this body of literature may be well served by a patient-level meta-analysis (e.g., Lambert et al., 2002) if consistent outcome and patient characteristic measures were available. Also, this meta-analysis selected consumption/abstinence measures a priori, but equally important may be consequences of alcohol use and improvements in overall functioning particularly when examining primarily harm-reduction studies (Kiluk et al., 2019).
In conclusion, this meta-analysis shows CBT-based, technology-delivered interventions have a beneficial, yet small effect on alcohol consumption outcomes when delivered as a stand-alone treatment in contrast to assessment only or when delivered as an addition to usual care in specialty substance use or mental health settings. Given the cost-benefit potential, capacity for reach, and ability to infuse evidence-based practices with fidelity, the results presented here are quite promising. With that said, our review does not suggest these models should replace in-person or established services, as there have been few well-controlled comparisons within the field of treatment for alcohol use.
Supplementary Material
Acknowledegements:
This research is supported by National Institute on Alcohol Abuse and Alcoholism grant R21AA026006 (Magill).
Footnotes
A study was eligible if it had a poly-drug use sample where alcohol use was reported among the majority of participants.
Effect size magnitude can be interpreted using the following benchmarks: 0.2 “small”, 0.5 “medium”, and 0.8 “large” COHEN, J. 1998. Statistical Power Analysis for the Behavioral Sciences, Hillsdale, NJ, USA, Erlbaum.. However, these are generic guidelines that should be interpreted cautiously in the absence of empirically-derived effect size distributions for adult alcohol use samples. For example, TANNER-SMITH, E. E., DURLAK, J. A. & MARX, R. A. 2018. Empirically based mean effect size distributions for universal prevention programs targeting school-aged youth: A review of meta-analyses. Prevention Science, 19, 1091–1101. suggest the following 25th, 50th, and 75th percentiles for behavioral outcomes in adolescent drug programs - 0.05, 0.10, and 0.15, respectively.
I2 magnitude can be interpreted using the following benchmarks: 0 – 40% “might not be important”, 30 – 60% “may represent moderate heterogeneity”, 50 – 90% “may represent substantial heterogeneity”, 75 – 100% “considerable heterogeneity” HIGGINS, J. P. & GREEN, S. 2011. Handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration.
Here, we sought substantial or greater heterogeneity and a sufficient number of studies to ensure variability in covariate values.
All authors have no conflict of interests to declare.
References
References marked with an asterisk (*) are included in the meta-analysis
- *ACOSTA MC, POSSEMATO K, MAISTO SA, MARSCH LA, BARRIE K, LANTINGA L, FONG C XIE H, GRABINSKI M & ROSENBLUM A 2017. Web-delivered CBT reduces heavy drinking in OEF-OIF veterans in primary care with symptomatic substance use and PTSD. Behavior Therapy, 48, 262–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- AMERICAN PSYCHIATRIC ASSOCIATION 1987. Diagnostic and Statistical Manual of Mental Disorders 3rd ed., test rev., Washington, DC, USA, American Psychiatric Association. [Google Scholar]
- AMERICAN PSYCHIATRIC ASSOCIATION 1994. Diagnostic and Statistical Manual of Mental Disorders, Washington, DC, USA, American Psychiatric Association. [Google Scholar]
- AMERICAN PSYCHIATRIC ASSOCIATION 2000. Diagnostic and Statistical Manual of Mental Disorders. 4th ed., text rev., Washington, DC, USA, American Psychiatric Association. [Google Scholar]
- AMERICAN PSYCHIATRIC ASSOCIATION 2010. Practice Guideline for the Treatment of Patients with Substance Use Disorders, Washington, DC, American Psychiatric Association. [Google Scholar]
- AMERICAN PSYCHIATRIC ASSOCIATION 2013. Diagnostic and Statistical Manual of Mental Disorders, Washington, DC, USA, American Psychiatric Association. [Google Scholar]
- AMERICAN PSYCHIATRIC ASSOCIATION 2018. Practice Guideline for the Pharmacological Treatment of Patients with Alcohol Use Disorder, Washington, DC, American Psychiatric Association. [Google Scholar]
- ANDERSSON G, CUIJPERS P, CARLBRING P, RIPER H & HEDMAN E 2014. Guided internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: A systematic review and meta-analysis. World Psychiatry, 13, 288–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ANDREWS G, BASU A, CUIJPERS P, CRASKE MG, MCEVOY P, ENGLISH CL & NEWBY JM 2018. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: An updated meta-analysis. Journal of Anxiety Disorders, 55, 70–78. [DOI] [PubMed] [Google Scholar]
- ANTON RF, O’MALLEY SS, CIRAULO DA, CISLER RA, COUPER D, DONOVAN DM, GASTFRIEND DR, HOSKING JD, JOHNSON BA, LOCASTRO JS, LONGABAUGH R, MASON BJ, MATTSON ME, MILLER WR, PETTINATI HM, RANDALL CL, SWIFT RM, WEISS RD, WILLIAMS LD, ZWEBEN A & FOR THE COMBINE STUDY RESEARCH GROUP 2006. Combined pharmacotherapies and behavioral interventions for alcohol dependence: The COMBINE Study. JAMA, 2006, 2003–2017. [DOI] [PubMed] [Google Scholar]
- BEGG CB & MAZUMDAR M 1994. Operating characteristics of a rank correlation test for publication bias. Biometrics, 1088–1101. [PubMed] [Google Scholar]
- BHUGRA D, TASMAN A, PATHARE S, PRIEBE S, SMITH S, TOROUS J, ARBUCKLE MR, LANGFORD A, ALARCON RD, CHIU HFK, FIRST MB, KAY J, SUNKEL C, THAPAR A, UDOMRATN P, BAINGANA FK, KESTEL D, NG RMK, PATEL A, PICKER L, MCKENZIE KJ, MOUSSAOUI D, MUIJEN M, BARTLETT P, DAVISON S, EXWORTHY T, LOZA N, ROSE D, TORALES J, BROWN M, CHRISTENSEN H, FIRTH J, KESHAVAN M, LI A, ONNELA JP, WYKES T, ELKHOLY H, KALRA G, LOVETT KF, TRAVIS MJ & VENTRIGLIO A 2017. The WPA-Lancet psychiatry commission on the future of psychiatry. Lancet Psychiatry, 4, 775–818. [DOI] [PubMed] [Google Scholar]
- BICKEL WK, CHRISTENSEN DR & MARSCH LA 2011. A review of computer-based interventions used in the assessment, treatment, and research of drug addiction. Substance Use & Misuse, 46, 4–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *BLANKERS M, KOETER MW & SCHIPPERS GM 2011. Internet therapy versus internet self-help versus no treatment for problematic alcohol use: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 79, 330–341. [DOI] [PubMed] [Google Scholar]
- BOTVIN GJ, GRIFFIN KW, DIAZ T, SCHEIER LM, WILLIAMS C & EPSTEIN JA 2000. Preventing illicit drug use in adolescents: Long-term follow-up data from a randomized control trial of a school population. Addictive Behaviors, 25, 769–774. [DOI] [PubMed] [Google Scholar]
- BOWEN S, CHAWLA N & MARLATT GA 2010. Mindfulness-based relapse prevention for the treatment of substance use disorders: A clinician’s guide, New York, Guilford Press. [Google Scholar]
- *BRENDRYEN H, LUND IO, JOHANSEN AB, RIKSHEIM M, NESVAG S & DUCKERT F 2014. Balance--a pragmatic randomized controlled trial of an online intensive self-help alcohol intervention. Addiction, 109, 218–26. [DOI] [PubMed] [Google Scholar]
- CAMPBELL ANC, NUNES EV, MATTHEWS AG, STITZER M, MIELE GM, POLSKY D, TURRIGIANO E, WALTERS S, MCCLURE E, KYLE TL, WAHLE A, VAN VELDHUISEN P, GOLDMAN B, BABCOCK D, STABILE PQ, WINHUSEN T & GHITZA UE 2014. Internet-delivered treatment for substance abuse: A multisite randomized controlled trial. The American Journal of Psychiatry, 171, 683–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARLBRING P, ANDERSSON G, CUIJPERS P, RIPER H & HEDMAN-LAGERLOF E 2018. Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: An updated systematic review and meta-analysis. Cognitive Behavioral Therapy, 47, 1–18. [DOI] [PubMed] [Google Scholar]
- CARROLL KM, BALL SA, MARTINO S, NICH C, BABUSCIO TA & ROUNSAVILLE BJ 2009. Enduring effects of a computer-assisted training program for cognitive behavioral therapy: A 6-month follow-up of CBT4CBT. Drug and Alcohol Dependence, 100, 178–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARROLL KM & KILUK BD 2017. Cognitive behavioral interventions for alcohol and drug use disorders: Through the stage model and back again. Psychol Addict Behav, 31, 847–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CARROLL KM, KILUK BD, NICH C, GORDON MA, PORTNOY GA, MARINO DR & BALL SA 2014. Computer-assisted delivery of cognitive-behavioral therapy: Efficacy and durability of CBT4CBT among cocaine-dependent individuals maintained on methadone. The American Journal of Psychiatry, 171, 436–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- COHEN J 1998. Statistical Power Analysis for the Behavioral Sciences, Hillsdale, NJ, USA, Erlbaum. [Google Scholar]
- COMBINE STUDY RESEARCH GROUP 2003. Testing combined pharmacotherapies and behavioral interventions in alcohol dependence: rationale and methods. Alcohol Clin Exp Res, 27, 1107–22. [DOI] [PubMed] [Google Scholar]
- CREED TA, WOLK CB, FEINBERG B, EVANS AC & BECK AT 2016. Beyond the Label: Relationship Between Community Therapists’ Self-Report of a Cognitive Behavioral Therapy Orientation and Observed Skills. Administration and Policy in Mental Health and Mental Health Services Research, 43, 36–43. [DOI] [PubMed] [Google Scholar]
- *CUNNINGHAM JA 2012. Comparison of two internet-based interventions for problem drinkers: Randomized controlled trial. Journal of Medical Internet Research, 14, e107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CUNNINGHAM JA, KYPRI K & MCCAMBRIDGE J 2011. The use of emerging technologies in alcohol treatment. Alcohol research & health : the journal of the National Institute on Alcohol Abuse and Alcoholism, 33, 320–326. [PMC free article] [PubMed] [Google Scholar]
- DETTORE D, POZZA A & ANDERSSON G 2015. Efficacy of technology-delivered cognitive behavioural therapy for OCD versus control conditions, and in comparison with therapist-administered CBT: Meta-analysis of randomized controlled trials. Cognitive Behavioral Therapy, 44, 190–211. [DOI] [PubMed] [Google Scholar]
- DIMOFF JD, SAYETTE MA & NORCROSS JC 2017. Addiction training in clinical psychology: Are we keeping up with the rising epidemic? Am Psychol, 72, 689–695. [DOI] [PubMed] [Google Scholar]
- EGGER M, SMITH GD, SCHNEIDER M & MINDER C 1997. Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ELLIS PD 2010. The essential guide to effect sizes: Statistical power, meta-analysis, and the interpretation of research results, New York, NY, Cambridge University Press. [Google Scholar]
- FAIRBURN CG & COOPER Z 2011. Therapist competence, therapy quality, and therapist training. Behaviour Research and Therapy, 49, 373–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *FARREN CK, MILNES J, LAMBE K & AHERN S 2015. Computerised cognitive behavioural therapy for alcohol use disorder: A pilot randomised control trial. Irish Journal of Psychological Medicine, 32, 237–246. [DOI] [PubMed] [Google Scholar]
- *GAJECKI M, ANDERSSON C, ROSENDAHL I, SINADINOVIC K, FREDRIKSSON M & BERMAN AH 2017. Skills training via smartphone app for university students with excessive alcohol consumption: A randomized controlled trial. International Journal of Behavioral Medicine, 24, 778–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HEDGES LV 1994. Statistical Considerations. In: COOPER H & HEDGES LV (eds.) The Handbook of Research Synthesis. New York, NY, USA: Russell Sage Foundation. [Google Scholar]
- HEDGES LV & OLKIN I 1985. Statistical Methods for Meta-Analysis, San Diego, CA, USA, Academic Press. [Google Scholar]
- HEDGES LV & VEVEA JL 1998. Fixed-and random-effects models in meta-analysis. Psychological Methods, 3, 486–504. [Google Scholar]
- HERSCHELL AD, KOLKO DJ, BAUMANN BL & DAVIS AC 2010. The role of therapist training in the implementation of psychosocial treatments: A review and critique with recommendations. Clinical Psychology Review, 30, 448–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *HESTER RK & DELANEY HD 1997. Behavioral self-control program for windows: Results of a controlled clinical trial. Journal of Consulting and Clinical Psychology, 65, 686–693. [DOI] [PubMed] [Google Scholar]
- *HESTER RK, DELANEY HD & CAMPBELL W 2011. Moderatedrinking.com and moderation management: Outcomes of a randomized clinical trial with non-dependent problem drinkers. Journal of Consulting and Clinical Psychology, 79, 215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *HESTER RK, LENBERG KL, CAMPBELL W & DELANEY HD 2013. Overcoming addictions, a web-based application, and smart recovery, an online and in-person mutual help group for problem drinkers, part 1: Three-month outcomes of a randomized controlled trial. Journal of Medical Internet Research, 15, e134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIGGINS JP, ALTMAN DG, GOTZSCHE PC, JUNI P, MOHER D, OXMAN AD, SAVOVIC J & STERNE JC 2011. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal, 343, d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIGGINS JP & GREEN S 2011. Handbook for systematic reviews of interventions version 5.1.0. The Cochrane Collaboration. [Google Scholar]
- KARYOTAKI E, EBERT DD, DONKIN L, RIPER H, TWISK J, BURGER S, ROZENTAL A, LANGE A, WILLIAMS AD, ZARSKI AC, GERAEDTS A, VAN STRATEN A, KLEIBOER A, MEYER B, UNLU INCE BB, BUNTROCK C, LEHR D, SNOEK FJ, ANDREWS G, ANDERSSON G, CHOI I, RUWAARD J, KLEIN JP, NEWBY JM, SCHRODER J, LAFERTON JAC, VAN BASTELAAR K, IMAMURA K, VERNMARK K, BOSS L, SHEEBER LB, KIVI M, BERKING M, TITOV N, CARLBRING P, JOHANSSON R, KENTER R, PERINI S, MORITZ S, NOBIS S, BERGER T, KALDO V, FORSELL Y, LINDEFORS N, KRAEPELIEN M, BJORKELUND C, KAWAKAMI N & CUIJPERS P 2018. Do guided internet-based interventions result in clinically relevant changes for patients with depression? An individual participant data meta-analysis. Clinical Psychology Review, 63, 80–92. [DOI] [PubMed] [Google Scholar]
- *KAY-LAMBKIN FJ, BAKER AL, KELLY B & LEWIN TJ 2011. Clinician-assisted computerised versus therapist-delivered treatment for depressive and addictive disorders: A randomised controlled trial. The Medical Journal of Australia, 195, S44–S50. [DOI] [PubMed] [Google Scholar]
- *KAY-LAMBKIN FJ, BAKER AL, LEWIN TJ & CARR VJ 2009. Computer-based psychological treatment for comorbid depression and problematic alcohol and/or cannabis use: A randomized controlled trial of clinical efficacy. Addiction, 104, 378–388. [DOI] [PubMed] [Google Scholar]
- *KILUK BD, DEVORE KA, BUCK MB, NICH C, FRANKFORTER TL, LAPAGLIA DM, YATES BT, GORDON MA & CARROLL KM 2016. Randomized trial of computerized cognitive behavioral therapy for alcohol use disorders: Efficacy as a virtual stand-alone and treatment add-on compared with standard outpatient treatment. Alcoholism, Clinical and Experimental Research, 40, 1991–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KILUK BD, FITZMAURICE GM, STRAIN EC & WEISS RD 2019. What defines a clinically meaningful outcome in the treatment of substance use disorders: reductions in direct consequences of drug use or improvement in overall functioning? Addiction, 114, 9–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KILUK BD, NICH C, BUCK MB, DEVORE KA, FRANKFORTER TL, LAPAGLIA DM, MUVVALA SB & CARROLL KM 2018. Randomized Clinical Trial of Computerized and Clinician-Delivered CBT in Comparison With Standard Outpatient Treatment for Substance Use Disorders: Primary Within-Treatment and Follow-Up Outcomes. Am J Psychiatry, 175, 853–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KILUK BD, SUGARMAN D, NICH C, GIBBONS CJ, MARTINO S, ROUNSAVILLE BJ & CARROLL KM 2011. A methodological analysis of randomized clinical trials of computer-assisted therapies for psychiatric disorders: Towards improved standards for an emerging field. American Journal of Psychiatry, 168, 790–799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LAMBERT PC, SUTTON AJ, ABRAMS KR & JONES DR 2002. A comparison of summary patient-level covariates in meta-regression with individual patient data meta-analysis. Journal of Clinical Epidemiology, 55, 86–94. [DOI] [PubMed] [Google Scholar]
- *LEEMAN RF, DEMARTINI KS, GUEORGUIEVA R, NOGUEIRA C, CORBIN WR, NEIGHBORS C & O’MALLEY SS 2016. Randomized controlled trial of a very brief, multicomponent web-based alcohol intervention for undergraduates with a focus on protective behavioral strategies. Journal of Consulting and Clinical Psychology, 84, 1008–1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAGILL M & RAY L 2009. Cognitive-behavioral treatment with adult alcohol and illicit drug users: A meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs, 70, 516–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAGILL M, RAY L, KILUK BD, HOADLEY A, BERNSTEIN M, TONIGAN JS & CARROLL KM under review Cognitive behavioral therapy and relapse prevention for alcohol and other drug use disorders: A meta-analysis. [Google Scholar]
- MARLATT GA & WITKIEWITZ K 2002. Harm reduction approaches to alcohol use: Health promotion, prevention, and treatment. Addictive Behaviors, 27, 867–86. [DOI] [PubMed] [Google Scholar]
- MARSCH LA, CARROLL KM & KILUK BD 2014. Technology based interventions for the treatment and recovery management of substance use disorders: A JSAT special issue. Journal of Substance Abuse Treatment, 46, 1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MARSCH LA, GUARINO H, ACOSTA MC, APONTE-MELENDEZ Y, CLELAND C, GRABINSKI M, BRADY R & EDWARDS J 2013. Web-based behavioral treatment for substance use disorders as a partial replacement of standard methadone maintenance treatment. Journal of Substance Abuse Treatment, 46, 43–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MCHUGH RK & BARLOW DH 2010. The dissemination and implementation of evidence-based psychological treatments: A review of current efforts. American Psychologist, 65, 73–84. [DOI] [PubMed] [Google Scholar]
- MCLELLAN AT, CARISE D & KLEBER HD 2003. Can the national addiction treatment infrastructure support the public’s demand for quality care? Journal of Substance Abuse Treatment, 25, 117–121. [PubMed] [Google Scholar]
- MONTI PM, KADDEN RM, ROHSENOW DJ, COONEY NL & ABRAMS D 2002. Treating Alcohol Dependence: A Coping Skills Training Guide, New York, NY, The Guilford Press. [Google Scholar]
- MONTI PM & ROHSENOW DJ 1999. Coping-skills training and cue-exposure therapy in the treatment of alcoholism. Alcohol Research and Health, 23, 107–15. [PMC free article] [PubMed] [Google Scholar]
- MOORE BA, FAZZINO T, GARNET B, CUTTER CJ & BARRY DT 2011. Computer-based interventions for drug use disorders: A systematic review. Journal of Substance Abuse Treatment, 40, 215–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NATIONAL INSTITUTE ON ALCOHOL ABUSE AND ALCOHOLISM 2005. Helping Patients Who Drink Too Much: A Clinician’s Guide. US Department of Health and Human Services, National Institutes of Health, NIH Publication; 07–3769. [Google Scholar]
- NATIONAL INSTITUTE ON ALCOHOL ABUSE AND ALCOHOLISM 2014. Treatment for Alcohol Problems: Finding and getting help. US Department of Health and Human Services, National Institutes of Health, NIH Publication No; 14–7974. [Google Scholar]
- OLMSTEAD TA, ABRAHAM AJ, MARTINO S & ROMAN PM 2012. Counselor training in several evidence-based psychosocial addiction treatments in private US substance abuse treatment centers. Drug and Alcohol Dependence, 120, 149–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PROJECT MATCH RESEARCH GROUP 1997. Matching Alcohol Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol, 58, 7–29. [PubMed] [Google Scholar]
- RAKOVSHIK SG & MCMANUS F 2010. Establishing evidence-based training in cognitive behavioral therapy: A review of current empirical findings and theoretical guidance. Clinical Psychology Review, 30, 496–516. [DOI] [PubMed] [Google Scholar]
- RAY LAPD, BUJARSKI SPD, GRODIN EPD, HARTWELL EPD, GREEN RMA, VENEGAS ABS, LIM AMA, GILLIS AMD & MIOTTO KMD 2019. State-of-the-art behavioral and pharmacological treatments for alcohol use disorder. Am J Drug Alcohol Abuse, 45, 124–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RIPER H, ANDERSSON G, HUNTER SB, DE WIT J, BERKING M & CUIJPERS P 2014a. Treatment of comorbid alcohol use disorders and depression with cognitive-behavioural therapy and motivational interviewing: a meta-analysis. Addiction, 109, 394–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RIPER H, BLANKERS M, HADIWIJAYA H, CUNNINGHAM JA, CLARKE S, WIERS R, EBERT DD & CUIJPERS P 2014b. Effectiveness of guided and unguided low-intensity internet interventions for adult alcohol misuse: A meta-analysis. PLoS One, 9, e99912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *RIPER H, KRAMER J, SMIT F, CONIJIN B, SCHIPPERS GM & CUIJPERS P 2008. Web-based self-help for problem drinkers: A pragmatic randomized trial. Addiction, 103, 218–227. [DOI] [PubMed] [Google Scholar]
- ROOKE S, THORSTEINSSON E, KARPIN A, COPELAND J & ALLSOP D 2010. Computer-delivered interventions for alcohol and tobacco use: a meta-analysis. Addiction, 105, 1381–90. [DOI] [PubMed] [Google Scholar]
- SAUNDERS JB, AASLAND OG, BABOR TF, DE LA FUENTE JR & GRANT M 1993. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- SCHAUB M, SULLIVAN R, HAUG S & STARK L 2012. Web-based cognitive behavioral self-help intervention to reduce cocaine consumption in problematic cocaine users: Randomized controlled trial. Journal of Medical Internet Research, 14, e166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SCHAUB MP, CASTRO RP, WENGER A, BAUMGARTNER C, STARK L, EBERT DD, QUEDNOW BB & HAUG S 2019. Web-based self-help with and without chat counseling to reduce cocaine use in cocaine misusers: Results of a three-arm randomized controlled trial. Internet Interv, 17, 100251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SHOLOMSKAS DE, SYRACUSE-SIEWERT G, ROUNSAVILLE BJ, BALL SA, NURO KF & CARROLL KM 2005. We don’t train in vain: A dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. Journal of Consulting and Clinical Psychology, 73, 106–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SIJBRANDIJ M, KUNOVSKI I & CUIJPERS P 2016. Effectiveness of internet-delivered cognitive behavioral therapy for posttraumatic stress disorder: A systematic review and meta-analysis. Depression and Anxiety, 33, 783–91. [DOI] [PubMed] [Google Scholar]
- SMITH A 2017. The evolution of technology adoption and usage. Washington, DC: Pew Research Center. [Google Scholar]
- SMITH JE, MEYERS RJ & MILLER WR 2001. The community reinforcement approach to the treatment of substance use disorders. American Journal of Addiction, 10, s51–s59. [DOI] [PubMed] [Google Scholar]
- SPURGEON JA & WRIGHT JH 2010. Computer-assisted cognitive-behavioral therapy. Current Psychiatry Reports, 12, 547–52. [DOI] [PubMed] [Google Scholar]
- SUGARMAN D, CAMPBELL ANC, ILES BR & GREENFIELD SF 2017. Technology-based interventions for substance use and comorbid disorders: An examination of the emerging literature. Harvard Review of Psychiatry, 25, 123–134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TAIT RJ, MCKETIN R, KAY-LAMBKIN FJ, CARRON-ARTHUR B, BENNETT A, BENNETT K, CHRITENSEN H & GRIFFITHS KM 2015. Six-month outcomes of a web-based intervention for users of amphetamine-type stimulants: Randomized controlled trial. Journal of Medical Internet Research, 17, e105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TAIT RJ, SPIJKERMAN R & RIPER H 2013. Internet and computer based interventions for cannabis use: A meta-analysis. Drug and Alcohol Dependence, 133, 295–304. [DOI] [PubMed] [Google Scholar]
- TANNER-SMITH EE, DURLAK JA & MARX RA 2018. Empirically based mean effect size distributions for universal prevention programs targeting school-aged youth: A review of meta-analyses. Prevention Science, 19, 1091–1101. [DOI] [PubMed] [Google Scholar]
- U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES 2016. Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC: HHS. [PubMed] [Google Scholar]
- WALLACE BC, SMALL K, BRODLEY CE, LAU J & TRIKALINOS TA Deploying an interactive machine learning system in an evidence-based practice center: abstrackr Proceedings of the 2nd ACM SIGHIT International Health Informatics Symposium 2012. New York, NY Association for Computing Machinery, 819–824. [Google Scholar]
- *WALLACE P, MURRAY E, MCCAMBRIDGE J, KHADJESARI Z, WHITE IR, THOMPSON SG, KALAITZAKI E, GODFREY C & LINKE S 2011. On-line randomized controlled trial of an internet based psychologically enhanced intervention for people with hazardous alcohol consumption. PLoS One, 6, e14740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WITKIEWITZ K, KRANZLER HR, HALLGREN KA, O’MALLEY SS, FALK DE, LITTEN RZ, HASIN DS, MANN KF & ANTON RF 2018. Drinking Risk Level Reductions Associated with Improvements in Physical Health and Quality of Life Among Individuals with Alcohol Use Disorder. Alcohol Clin Exp Res, 42, 2453–2465. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


