Abstract
Objectives
Using a simple classification method, we aimed to estimate the collapse rate due to osteonecrosis of the femoral head (ONFH) in order to develop treatment guidelines for joint-preserving surgeries.
Methods
We retrospectively analyzed 505 hips from 310 patients (141 men, 169 women; mean age 45.5 years (sd 14.9; 15 to 86)) diagnosed with ONFH and classified them using the Japanese Investigation Committee (JIC) classification. The JIC system includes four visualized types based on the location and size of osteonecrotic lesions on weightbearing surfaces (types A, B, C1, and C2) and the stage of ONFH. The collapse rate due to ONFH was calculated using Kaplan–Meier survival analysis, with radiological collapse/arthroplasty as endpoints.
Results
Bilateral cases accounted for 390 hips, while unilateral cases accounted for 115. According to the JIC types, 21 hips were type A, 34 were type B, 173 were type C1, and 277 were type C2. At initial diagnosis, 238/505 hips (47.0%) had already collapsed. Further, the cumulative survival rate was analyzed in 212 precollapsed hips, and the two-year and five-year collapse rates were found to be 0% and 0%, 7.9% and 7.9%, 23.2% and 36.6%, and 57.8% and 84.8% for types A, B, C1, and C2, respectively.
Conclusion
Type A ONFH needs no further treatment, but precollapse type C2 ONFH warrants immediate treatment with joint-preserving surgery. Considering the high collapse rate, our study results justify the importance of early diagnosis and intervention in asymptomatic patients with type C2 ONFH.
Cite this article: Y. Kuroda, T. Tanaka, T. Miyagawa, T. Kawai, K. Goto, S. Tanaka, S. Matsuda, H. Akiyama. Classification of osteonecrosis of the femoral head: Who should have surgery?. Bone Joint Res 2019;8:451–458. DOI: 10.1302/2046-3758.810.BJR-2019-0022.R1.
Keywords: Osteonecrosis, Femoral head, Joint-preserving surgery, Collapse, Kaplan–Meier survival analysis
Article focus
The purpose of this study is to facilitate appropriate selection of a joint-preserving surgery for osteonecrosis of the femoral head (ONFH) based on prediction of collapse rate using Kaplan–Meier survival analysis.
Key messages
Using a simple four-type classification system, we can predict the collapse rate due to ONFH.
Our study results demonstrate the importance of early diagnosis and intervention in asymptomatic patients with type C2 ONFH.
Strengths and limitations
At initial diagnosis, the hips of almost half of patients had already collapsed.
Type A ONFH needs no further treatment.
Our study results can assist in the selection of therapeutic strategies for patients with precollapse ONFH.
Introduction
Osteonecrosis of the femoral head (ONFH) is an intractable disease caused by factors such as corticosteroid use, alcoholism, hypercoagulation, bone marrow fat embolism, vascular endothelial dysfunction, and bone marrow oedema in the femoral head. Among these, corticosteroid use and alcoholism are considered the most common risk factors for ONFH.1,2 Collapse due to ONFH generally progresses to secondary osteoarthritis (OA); total hip arthroplasty is considered the final treatment option, including in young patients.1-5 Therefore, femoral head collapse is the most significant pathogenic complication of ONFH. Recent studies have focused on the mechanism of femoral head collapse. Traditional biomechanical analysis using operatively extracted femoral heads from ONFH patients included distribution analysis based on the linear elasticity theory.6 Recently, finite element analysis (FEA) using CT images was used for the biomechanical simulation of surgical procedures used for ONFH.7 The location and lesion size of ONFH are two major causes of femoral head collapse.2-4 We believe that the ability to easily predict femoral head collapse based on radiological types would be valuable for physicians. Although some reports have attempted to examine the collapse rate of ONFH, these studies have limitations in terms of small population sizes and a lack of well-organized recent data.4,8-15
Increased recognition of corticosteroid-associated ONFH and widespread use of MRI16 have now facilitated early diagnosis of the precollapse stage of ONFH. In fact, MRI can provide increasing opportunities for the early diagnosis of corticosteroid-associated ONFH. Accordingly, the strategy of ONFH therapy is shifting towards early diagnosis and administration of regenerative therapy to facilitate joint preservation.1,2,5,17-19 Various joint-preserving procedures, including the use of cell therapy, proteins, and other bone substitutes, have recently been developed to resolve the high collapse rate due to ONFH among young patients.1-3,5 However, it has been difficult to conduct substantial discussions on therapeutic strategies across international boundaries due to the presence of several international classification systems related to ONFH.1,2,8-10 Consequently, different surgical methods based on individual surgical styles are being used worldwide.18 To address this issue, we aimed to clarify the natural history of over 500 joints using a simple classification system. In Japan, ONFH is designated as an intractable disease.20,21 Annual reports on its types and stages using a simple Japanese classification system are necessary in order for patients to obtain an intractable disease status (card) and therefore receive medical support. The aim of this study was to analyze the collapse rate using a simple classification method and thereby to develop therapeutic strategies for patients with precollapse ONFH.
Patients and Methods
The cohort comprised 505 hips from 310 patients (141 men, 169 women) diagnosed with ONFH between January 2002 and December 2013 at three university hospitals (Kyoto University, Kyoto, Japan; The University of Tokyo, Tokyo, Japan; Gifu University, Gifu, Japan). The mean age of the patients was 45.5 years (sd 14.9; 15 to 86). We conducted a retrospective, observational, multicentre study using the data collected between September 2014 and May 2015. The institutional review boards of the three university hospitals approved this study. The study patients were assessed using T1-weighted 1.5 T MRI or 3.0 T MRI to determine the extent of ONFH. The disease was diagnosed according to the 2001 Japanese Investigation Committee (JIC) guidelines, as per the Ministry of Health and Welfare classification system.20,21 The JIC clinical exclusion criteria included ONFH diagnosis following trauma, transient osteoporosis of the hip, and subchondral insufficiency fracture of the femoral head. We collected anonymous demographic, radiological, and surgical intervention data from digital medical records using spreadsheet software (Microsoft Excel; Microsoft, Redmond, Washington). The specific demographic data collected included data related to sex, age, background ONFH-associated factors, laterality, type of ONFH, and surgical procedure (if relevant). The following background factors underlying ONFH were determined: steroid use, alcohol intake, or idiopathic disease. Further, extracted radiological data included the stage of ONFH at initial diagnosis and gradual radiological change(s) in the stage. The staging of ONFH and localization of necrotic lesions were performed according to the stage and type of JIC.20,21 One physician per facility (YK, TT, TM), who was an expert in hip joint disease, evaluated the stage and type of JIC. The JIC classification comprises four types: A, B, C1, and C2. The classification is based on the central coronal section of the femoral head on a T1-weighted MRI, while staging was based on the anteroposterior and lateral views of the femoral head on radiological images. Stage 1 is defined as the absence of abnormal findings related to osteonecrosis on radiographs but presence of specific findings on MRI, bone scintigraphy, or histology. Stage 2 is defined as the observation of demarcating sclerosis without femoral head collapse. Stage 3 is defined as the presence of femoral head collapse, including the crescent sign, without joint space narrowing. Stage 3 is subdivided into two stages: stage 3A, extent of femoral head collapse < 3 mm; and stage 3B, extent of femoral head collapse ⩾ 3 mm. Stage 4 is defined as the presence of secondary OA changes following femoral head collapse. The extent of osteonecrotic lesions was classified into the four types listed above (i.e. types A, B, C1, and C2), based on their size and location on T1-weighted MRI or radiography (Fig. 1).20
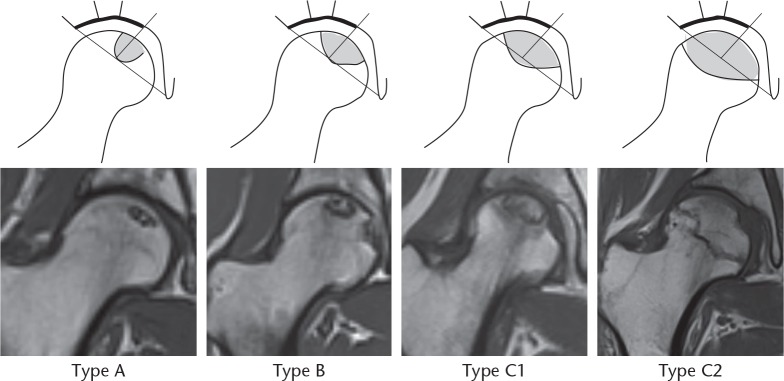
Fig. 1.
Schematic representation of T1-weighted MRIs of the 2001 revised Japanese Investigation Committee classification system20 based on type. The classification schema comprises four types (A, B, C1, and C2). Type A involves the smallest osteonecrotic lesions of the four types (present only in the medial one-third, or less, of the weightbearing surface). Type B involves osteonecrotic lesions present in the medial two-thirds, or less, of the weightbearing surface. Type C1 lesions are characterized by an osteonecrotic zone that spans more than the medial two-thirds of the weightbearing surface at the acetabular edge. Type C2 involves the largest osteonecrotic zone that spans more than the medial two-thirds of the weightbearing surface and exceeds the acetabular edge.
Statistical analysis
Statistical analyses were performed using the SAS version 9.3 software (SAS Institute, Inc., Cary, North Carolina). For the demographic data of the two variables, a chi-squared test was used for the comparison (type, sex, laterality, and background factors) of differences in terms of the collapse rate at initial diagnosis. The Kruskal–Wallis test was used to compare the differences in terms of collapse rate among the four disease stages at initial diagnosis. Further, Kaplan–Meier survival analysis was performed using collapse or surgical intervention of arthroplasty as endpoints. A comparison of the Kaplan–Meier curves for the relevant factors (type, sex, laterality, and background factors) was performed with a log-rank test in the precollapse cohort. Log-rank tests were used to compare two potential differences in terms of the collapse rate of ONFH: between unilateral and bilateral ONFH; and between ONFH with corticosteroid use and ONFH without steroid use. A Cox regression model was used to evaluate the independent prognostic factors associated with collapse, including age, sex, laterality of ONFH (unilateral, bilateral), background factors (with or without steroid use), and JIC type (A, B, C1, C2). All statistical analyses were two-sided and evaluated with a p-value < 0.05 indicating statistical significance.
Results
Demographics
Bilateral cases accounted for 390 hips, while unilateral ones accounted for 115. In total, 390 hips (77.4%) were associated with steroid use, 83 (16.3%) were associated with alcohol intake, and 32 (6.3%) were idiopathic (Table I).
Table I.
Patient demographics
| Parameter | Value |
|---|---|
| Mean age at initial diagnosis, yrs (sd; range) | 45.5 (14.9; 15 to 86) |
| Hips, n | |
| Total | 505 |
| Male:female | 233:272 |
| Patients, n | |
| Total | 310 |
| Male:female | 141:169 |
| Hips: bilateral cases, n | |
| Total | 390 |
| Male:female | 184:206 |
| Hips: unilateral cases, n | |
| Total | 115 |
| Male:female | 49:66 |
| Background factors | |
| Hips: steroid use, n | 390 |
| Hips: alcohol intake, n | 83 |
| Hips: idiopathic, n | 32 |
Collapse rate at initial diagnosis analyzed in association with the demographic data
At initial diagnosis, based on the JIC stage, 121 hips were classified as stage 1, 146 as stage 2, 129 as stage 3A, 62 as stage 3B, and 47 as stage 4. According to the JIC type, 21 hips were classified as type A, 34 as type B, 173 as type C1, and 277 as type C2 at initial diagnosis. Moreover, at initial diagnosis, 238 hips (47.0%) were found to have already collapsed. Notably, there were significant differences in terms of the collapse rate among the four JIC types (p < 0.001, Kruskal–Wallis test). The collapse rates in types A, B, C1, and C2 were 0% (0/21 hips), 11.8% (4/34 hips), 31.2% (59/173 hips), and 65.0% (180/277 hips), respectively. Further, there was a significant difference at initial diagnosis between unilateral and bilateral ONFH patient groups (p = 0.006, log-rank test); the collapse rates of unilateral ONFH patients were significantly higher (60.0%) than those of bilateral ONFH patients (43.3%). There was also a significant difference at initial diagnosis between ONFH patient groups with and without steroid use (p = 0.002, log-rank test). The collapse rate of ONFH patients with steroid use was significantly lower (42.8%) than that of patients without steroid use (61.7%; Table II). However, there were no significant differences in terms of the collapse rate between male and female patients (p = 0.340, log-rank test).
Table II.
Collapse rate at initial diagnosis as analyzed by demographic data
| Parameter/stage | Stage 1 | Stage 2 | Stage 3A | Stage 3B | Stage 4 | n | Collapsed hips at initial diagnosis, n (%) | p-value |
|---|---|---|---|---|---|---|---|---|
| Type, n | < 0.001*† | |||||||
| A | 16 | 5 | 0 | 0 | 0 | 21 | 0/21 (0.0) | |
| B | 18 | 12 | 3 | 0 | 1 | 34 | 4/34 (11.8) | |
| C1 | 53 | 66 | 30 | 16 | 8 | 173 | 54/173 (31.2) | |
| C2 | 34 | 63 | 96 | 46 | 38 | 277 | 180/277 (65.0) | |
| Total, n (%) | 121 (23.9) | 146 (28.9) | 129 (25.4) | 62 (12.2) | 47 (9.5) | 505 | 238/505 (47.1) | |
| Sex, n | 0.340‡ | |||||||
| Male | 50 | 62 | 77 | 31 | 13 | 233 | 121/233 (51.9) | |
| Female | 71 | 84 | 52 | 31 | 34 | 272 | 117/272 (43.0) | |
| Bilateral/unilateral, n | 0.006*‡ | |||||||
| Bilateral | 107 | 114 | 91 | 43 | 35 | 390 | 169/390 (43.3) | |
| Unilateral | 14 | 32 | 38 | 19 | 12 | 115 | 69/115 (60.0) | |
| Steroid use, n | 0.002*‡ | |||||||
| Yes | 106 | 117 | 86 | 42 | 39 | 390 | 167/390 (42.8) | |
| No | 15 | 29 | 43 | 20 | 8 | 115 | 71/115 (61.7) |
Statistically significant
Kruskal–Wallis test
Log-rank test
Collapse rate evaluated by Kaplan–Meier survival analysis
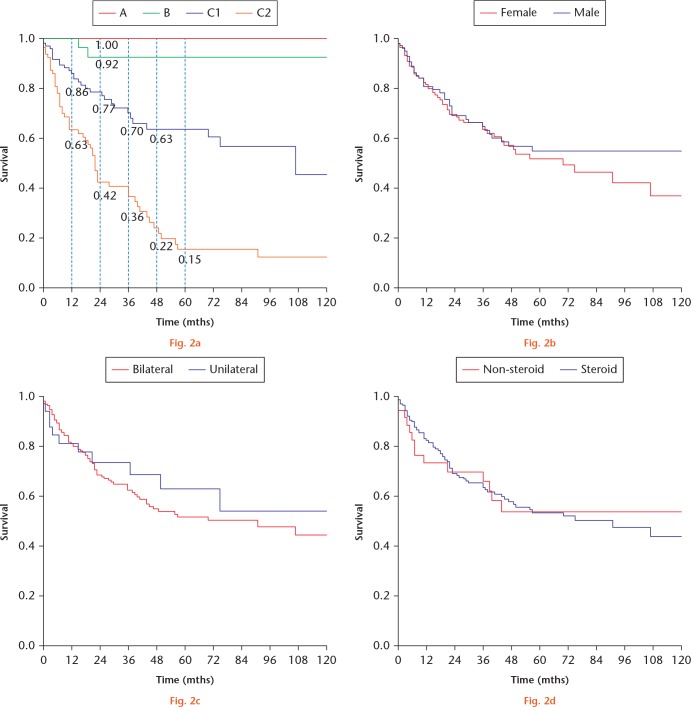
A total of 212 precollapsed hips, excluding 55 patients who underwent joint-preserving surgeries, were analyzed, and the five-year collapse rates were estimated as follows: type A, 0%; type B, 7.9%; type C1, 36.6%; and type C2, 84.8% (Fig. 2a). The mean follow-up interval from initial diagnosis was 61.3 months (sd 38.2; 6.5 to 149).
Fig.2.
Kaplan–Meier survival curves of precollapse cases. a) The cumulative five-year survival rates indicate that the collapse rate of precollapse osteonecrosis of the femoral head (ONFH) cases is 0% to 84.8%, in the order of smaller to larger lesion sizes. Type C2 progressed quickly, with 37% at one year and 58% at two years reaching the endpoint. b) Collapse rate of precollapse ONFH cases according to sex; there were no differences in terms of time to collapse (p = 0.453, log-rank test). c) Collapse rate of precollapse ONFH cases according to laterality; there were no differences in terms of time to collapse (p = 0.580, log-rank test). d) Collapse rate of precollapse ONFH cases according to steroid use; there were no differences in terms of time to collapse (p = 0.961, log-rank test).
Differences in terms of the risk factors for collapse in precollapse ONFH patients evaluated by log-rank test
According to the log-rank test findings, there was no significant difference in terms of the time to collapse between men and women (p = 0.451; Fig. 2b), between patients with unilateral and bilateral ONFH (p = 0.584; Fig. 2c), or between ONFH with and without steroid use (p = 0.961; Fig. 2d).
Collapse-associated independent prognostic factors evaluated by the Cox regression model
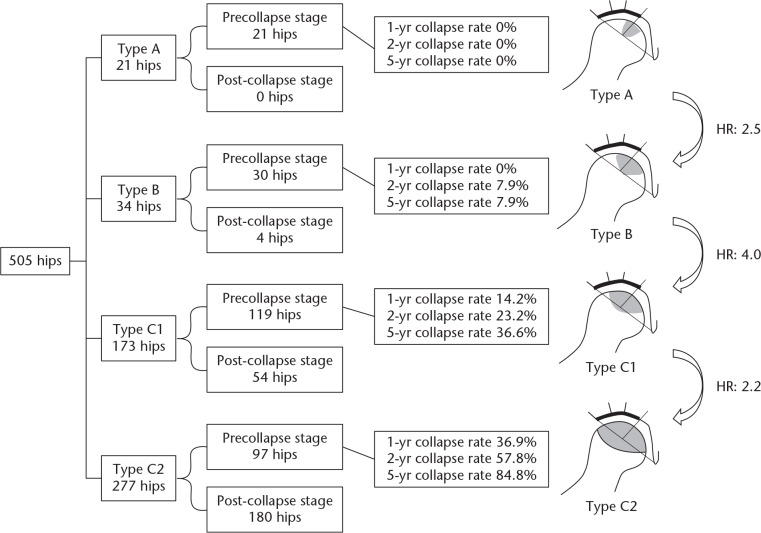
The Cox proportional hazard analysis revealed that ONFH without steroid use (p = 0.041, hazard ratio (HR) 1.34; 95% confidence interval (CI) 1.01 to 1.76) and type of ONFH (p < 0.001) were independent factors associated with collapse. The HR for type B to type A was 2.5 (p = 0.006), type C1 to type B was 4.0 (p < 0.001), and type C2 to type C1 was 2.2 (p < 0.001) (Fig. 3). In addition, the analysis showed that there was no significant association between collapse due to ONFH and factors such as age (p = 0.672), sex (p = 0.510), and laterality of ONFH (p = 0.068).
Fig. 3.
Five-year collapse rates and hazard ratios (HRs) of each disease type as evaluated by the Cox regression model. A higher collapse rate and an increase in HR for collapse of the femoral head can be seen as the osteonecrotic lesion size increases.
Surgical treatments
Surgical treatment was required for a total of 264 hips (52.4%): total hip arthroplasty, 203 hips; femoral osteotomy, 34 hips; core decompression using growth factors, ten hips; vascularized fibular grafting with stem cell transplantation, ten hips; hemiarthroplasty, six hips; and core decompression alone, one hip. Additionally, joint-preserving surgeries were performed for 55 hips, more than half of which (34 hips) were femoral osteotomies.
Discussion
For several decades, the optimal surgical treatment option for patients with asymptomatic ONFH has remained a controversial topic.1-3,5,9,18,22 Considering the high collapse rate, several researchers have recommended early diagnosis and intervention to achieve joint preservation in ONFH patients, including asymptomatic ONFH patients.1-3,5,18 In contrast, some authors have recommended surgery only for symptomatic ONFH patients.14,15,17 This issue is considered contentious owing to the lack of reliable data on the collapse rate across the different types of ONFH. In addition, there are currently many classification systems for ONFH worldwide, including the Ficat and Arlet, Association Research Circulation Osseous (ARCO), Steinberg, and JIC. Of these classification systems, the ARCO, Steinberg, and JIC systems include classification based on lesion size and location.1,2 In particular, the JIC classification has some advantages, such as classification based on the size and location of ONFH lesions involving the acetabular head.5,10,20 This system comprises four simple types and has high intraobserver and interobserver reliabilities.8,10,23 In a previous systematic review, Sultan et al8 reported that the JIC classification shows promising prognostic value while maintaining simplicity. In Japan, annual reporting of the JIC stage and type is necessary in order to obtain an intractable disease status card for medical support. Annual reports have to be written by a Japanese Orthopaedic Association–certified physician, and its data are updated every year.21 Therefore, the JIC classification is widely used in Japan.
Consistent with the findings of previous studies, the present study found that the collapse rate increases as the osteonecrotic lesion on the weightbearing surface becomes larger.1-3,10-15,22 Kaplan–Meier survival analysis is the optimal method for determining the collapse rate and evaluating the actual interval of femoral head collapse.10,15,16,24 In this study, type A hips had a 0% collapse rate and type C2 had an 84.8% collapse rate, providing useful clues for determining optimal treatment approaches. The lowest collapse rate of type A ONFH suggests that further treatment for this type of ONFH is not justified. In contrast, patients with type C2 ONFH are recommended to undergo joint-preserving surgery, as joint preservation is unlikely to be achieved through conservative treatment. Early intervention for patients with type C1 should be determined based on whether surgery may be a burden on the patient. We believe that minimally invasive treatment, such as core decompression or core decompression-based regenerative therapy, is appropriate for type C1 patients.18
In a previous systematic review by Mont et al,2 a total of 664 hips were assessed based on different classification systems for ONFH, and it was reported that 59% of the cases experienced progression to symptoms or collapse. The probability of femoral head collapse reportedly correlated with a larger lesion size and localization at the lateral weightbearing surface. In addition, several previous studies have reported the collapse rate of ONFH using the JIC classification system (Table III),10-15 and other researchers have reported smaller collapse rates for type C ONFH (between 71% and 76%).11-14 Hungerford and Jones25 reported that small lesions involving less than 15% of the femoral head (by volume) were unlikely to progress, suggesting that progression is dependent on lesion size. Apart from the JIC classification, the Steinberg classification is widely used because it combines staging with an assessment of the affected lesion size by percentage (< 15%, 15% to 30%, and > 30%).1,2 Min et al15 emphasized that important prognostic factors for collapse include not only the size but also the extent and location of necrotic lesions, considering the high collapse rate of type C2 ONFH. The Kerboul angle has also been used in the evaluation of lesion size and involves the addition of the two angles measured on anteroposterior and lateral radiographs.1,19
Table III.
Other reports on the collapse rate evaluated by the Japanese Investigation Committee classification system
| Authors (year) | Hips, n | Mean follow-up, yrs | Collapse/symptomatic rate, %* | ||
|---|---|---|---|---|---|
| Type A | Type B | Type C | |||
| Shimizu et al11 (1994) | 66 | 4.0 | 0 | 13 | 71 |
| Sakamoto et al12 (1997) | 31 | 3.0 | 0 | 0 | 75 |
| Nishii et al13 (2002) | 54 | 6.0 | 24 | 50 | 76 |
| Ito et al14 (2003) | 90 | 9.0 | 0* | 71* | 72* |
| Min et al15 (2008) | 81 | 8.3 | 0† | 0† | C1: 13, C2: 86† |
| Takashima et al10 (2018) | 86 | 10.0 | 0† | 6† | C1: 68, C2: 82† |
| Present study (2019) | 212 | 5.0 | 0† | 8† | C1: 37, C2: 85† |
Prevalence rate of symptoms
Collapse rate evaluated by Kaplan–Meier survival analysis
In the present study, we demonstrated another remarkable finding: significant differences were noted in terms of the stage of ONFH at initial diagnosis according to laterality. To the best of our knowledge, no previous report has performed a direct comparison between bilateral and unilateral ONFH. Bilateral ONFH is considered easier to diagnose than its unilateral counterpart, and the likelihood of effective treatment using orally administered therapeutic agents for steroid-induced osteoporosis is believed to be higher in the cases of bilateral ONFH than in those of unilateral ONFH. Mont et al3 reported that asymptomatic ONFH is typically discovered in the contralateral hips of patients with symptomatic ONFH. The incidence of bilateral ONFH has been reported to be as high as 75%.26,27 Additionally, there have been reported differences in terms of the stage of ONFH at initial diagnosis according to background factors (steroid, no steroid use). For immunologists and orthopaedic surgeons, ONFH has been recognized as an adverse event of systemic corticosteroid therapy. Patients using steroids have been widely considered as a group at a potentially higher risk for ONFH.18 Additionally, we speculate that the incidence of patients with ONFH with steroid use was significantly lower because they could be easily diagnosed compared with patients who were not using steroids.
The present study has some limitations. First, intraobserver and interobserver reliabilities of the JIC classification were not evaluated based on high reliability reported in previous studies.8,10,23 Nakamura et al23 reported 85% agreement in terms of interobserver reliability of the JIC classification (weighted kappa: 0.71) and 82% agreement in terms of intraobserver reliability (weighted kappa: 0.78). Takashima et al10 reported that the JIC interobserver reliability was shown to be substantial (weighted kappa: 0.72), with a higher reliability than both the Steinberg and Kerboul classifications (both p < 0.001, Spearman’s rank correlation coefficient). Second, we did not evaluate the outcomes of patients on oral drugs or those who underwent surgical treatments. Our data reflect the popularity of osteotomy in Asia. Third, we did not analyze the relationship between symptoms and femoral head collapse. The mode of collapse or post-collapse regeneration possibly influences the symptoms related to the hip joint. Bozic et al28 reported that an increase of more than four-fold in the failure rate following core decompression is associated with cystic changes pertaining to ONFH. Further, bone absorption through osteoclastic resorption is inhibited by a repair process and is indicative of sclerotic changes in ONFH.14 Last, the prevalence of background factors of ONFH patients varies worldwide. However, patient background factors and the classification of ONFH show international differences, and there are few reports summarizing 500 ONFH joints or more. We believe that our study fills this gap.
In conclusion, the prediction of femoral head collapse using the JIC classification can assist in the selection of therapeutic strategies for patients with precollapse ONFH. In recent decades, the development of novel therapies, such as autologous bone marrow cell transplantation,5,17,19,29 metal implant rod use,1-3 and growth factor therapies, has been witnessed.18,30,31 Our study results justify early intervention in precollapse, asymptomatic ONFH patients with larger osteonecrotic lesions, especially in those with type C2 ONFH. As indicated by the study results, type A ONFH needs no further surgical intervention.
Footnotes
Ethical review statement: The institutional review boards of the three university hospitals involved (Kyoto University, Kyoto, Japan; The University of Tokyo, Tokyo, Japan; Gifu University, Gifu, Japan) approved this study.
Follow us @BoneJointRes
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Moya-Angeler J, Gianakos AL, Villa JC, Ni A, Lane JM. Current concepts on osteonecrosis of the femoral head. World J Orthop 2015;6:590-601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mont MA, Cherian JJ, Sierra RJ, Jones LC, Lieberman JR. Nontraumatic osteonecrosis of the femoral head: where do we stand today? A ten-year update. J Bone Joint Surg [Am] 2015;97-A:1604-1627. [DOI] [PubMed] [Google Scholar]
- 3. Mont MA, Zywiel MG, Marker DR, McGrath MS, Delanois RE. The natural history of untreated asymptomatic osteonecrosis of the femoral head: a systematic literature review. J Bone Joint Surg [Am] 2010;92-A:2165-2170. [DOI] [PubMed] [Google Scholar]
- 4. Hernigou P, Poignard A, Nogier A, Manicom O. Fate of very small asymptomatic stage-I osteonecrotic lesions of the hip. J Bone Joint Surg [Am] 2004;86-A:2589-2593. [DOI] [PubMed] [Google Scholar]
- 5. Larson E, Jones LC, Goodman SB, Koo KH, Cui Q. Early-stage osteonecrosis of the femoral head: where are we and where are we going in year 2018? Int Orthop 2018;42:1723-1728. [DOI] [PubMed] [Google Scholar]
- 6. Volokh KY, Yoshida H, Leali A, Fetto JF, Chao EY. Prediction of femoral head collapse in osteonecrosis. J Biomech Eng 2006;128:467-470. [DOI] [PubMed] [Google Scholar]
- 7. Zhou G, Zhang Y, Zeng L, et al. Should thorough debridement be used in fibular allograft with impaction bone grafting to treat femoral head necrosis: a biomechanical evaluation. BMC Musculoskelet Disord 2015;16:140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sultan AA, Mohamed N, Samuel LT, et al. Classification systems of hip osteonecrosis: an updated review. Int Orthop 2019;43:1089-1095. [DOI] [PubMed] [Google Scholar]
- 9. Steinberg ME, Oh SC, Khoury V, Udupa JK, Steinberg DR. Lesion size measurement in femoral head necrosis. Int Orthop 2018;42:1585-1591. [DOI] [PubMed] [Google Scholar]
- 10. Takashima K, Sakai T, Hamada H, Takao M, Sugano N. Which classification system is most useful for classifying osteonecrosis of the femoral head? Clin Orthop Relat Res 2018;476:1240-1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shimizu K, Moriya H, Akita T, Sakamoto M, Suguro T. Prediction of collapse with magnetic resonance imaging of avascular necrosis of the femoral head. J Bone Joint Surg [Am] 1994;76-A:215-223. [DOI] [PubMed] [Google Scholar]
- 12. Sakamoto M, Shimizu K, Iida S, et al. Osteonecrosis of the femoral head: a prospective study with MRI. J Bone Joint Surg [Br] 1997;79-B:213-219. [DOI] [PubMed] [Google Scholar]
- 13. Nishii T, Sugano N, Ohzono K, et al. Progression and cessation of collapse in osteonecrosis of the femoral head. Clin Orthop Relat Res 2002;400:149-157. [DOI] [PubMed] [Google Scholar]
- 14. Ito H, Matsuno T, Omizu N, Aoki Y, Minami A. Mid-term prognosis of non-traumatic osteonecrosis of the femoral head. J Bone Joint Surg [Br] 2003;85-B:796-801. [PubMed] [Google Scholar]
- 15. Min BW, Song KS, Cho CH, Lee SM, Lee KJ. Untreated asymptomatic hips in patients with osteonecrosis of the femoral head. Clin Orthop Relat Res 2008;466:1087-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu W, He W, Wei QS, et al. Prognostic analysis of different morphology of the necrotic-viable interface in osteonecrosis of the femoral head. Int Orthop 2018;42:133-139. [DOI] [PubMed] [Google Scholar]
- 17. Yoon BH, Lee YK, Kim KC, Ha YC, Koo KH. No differences in the efficacy among various core decompression modalities and non-operative treatment: a network meta-analysis. Int Orthop 2018;42:2737-2743. [DOI] [PubMed] [Google Scholar]
- 18. Kuroda Y, Matsuda S, Akiyama H. Joint-preserving regenerative therapy for patients with early-stage osteonecrosis of the femoral head. Inflamm Regen 2016;36:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Marker DR, Seyler TM, McGrath MS, et al. Treatment of early stage osteonecrosis of the femoral head. J Bone Joint Surg [Am] 2008;90-A(Suppl 4):175-187. [DOI] [PubMed] [Google Scholar]
- 20. Sugano N, Atsumi T, Ohzono K, et al. The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci 2002;7:601-605. [DOI] [PubMed] [Google Scholar]
- 21. Fukushima W, Fujioka M, Kubo T, et al. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res 2010;468:2715-2724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kang JS, Moon KH, Kwon DG, Shin BK, Woo MS. The natural history of asymptomatic osteonecrosis of the femoral head. Int Orthop 2013;37:379-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nakamura J, Kishida S, Harada Y, et al. Inter-observer and intra-observer reliabilities of the Japanese Ministry of Health, Labor and Welfare type classification system for osteonecrosis of the femoral head. Mod Rheumatol 2011;21:488-494. [DOI] [PubMed] [Google Scholar]
- 24. Biau DJ, Hamadouche M. Estimating implant survival in the presence of competing risks. Int Orthop 2011;35:151-155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hungerford DS, Jones LC. Asymptomatic osteonecrosis: should it be treated? Clin Orthop Relat Res 2004;429:124-130. [PubMed] [Google Scholar]
- 26. Nam KW, Kim YL, Yoo JJ, et al. Fate of untreated asymptomatic osteonecrosis of the femoral head. J Bone Joint Surg [Am] 2008;90-A:477-484. [DOI] [PubMed] [Google Scholar]
- 27. Mankin HJ. Nontraumatic necrosis of bone (osteonecrosis). N Engl J Med 1992;326:1473-1479. [DOI] [PubMed] [Google Scholar]
- 28. Bozic KJ, Zurakowski D, Thornhill TS. Survivorship analysis of hips treated with core decompression for nontraumatic osteonecrosis of the femoral head. J Bone Joint Surg [Am] 1999;81-A:200-209. [DOI] [PubMed] [Google Scholar]
- 29. Chughtai M, Piuzzi NS, Khlopas A, et al. An evidence-based guide to the treatment of osteonecrosis of the femoral head. Bone Joint J 2017;99-B:1267-1279. [DOI] [PubMed] [Google Scholar]
- 30. Lieberman JR, Conduah A, Urist MR. Treatment of osteonecrosis of the femoral head with core decompression and human bone morphogenetic protein. Clin Orthop Relat Res 2004;429:139-145. [DOI] [PubMed] [Google Scholar]
- 31. Kuroda Y, Asada R, So K, et al. A pilot study of regenerative therapy using controlled release of rhFGF-2 for patients with pre-collapse osteonecrosis of the femoral head. Int Orthop 2016;40:1747-1754. [DOI] [PubMed] [Google Scholar]