Abstract
PURPOSE
To address the increasing burden of cancer in Nigeria, the National Cancer Control Plan outlines the development of 8 public comprehensive cancer centers. We map population-level geospatial access to these eight centers and explore equity of access and the impact of future development.
METHODS
Geospatial methods were used to estimate population-level travel times to the 8 cancer centers. A cost distance model was built using open source road infrastructure data with verified speed limits. Geolocated population estimates were amalgamated with this model to calculate travel times to cancer centers at a national and regional level for both the entire population and the population living on < US$2 per day.
RESULTS
Overall, 68.9% of Nigerians have access to a comprehensive cancer center at 4 hours of continuous vehicular travel. However, there is significant variability in access between geopolitical zones (P < .001). The North East has the lowest access at 4 hours (31.4%) and the highest mean travel times (268 minutes); this is significantly lower than the proportion with 4-hour access in the South East (31.4% v 85.0%, respectively; P < .001). The addition of a second comprehensive cancer center in the North East, in either Bauchi or Gombe, would significantly improve access to this underserved region.
CONCLUSION
The Federal Ministry of Health endorses investment in 8 public comprehensive cancer centers. Strengthening these centers will allow the majority of Nigerians to access the full complement of multidisciplinary care within a reasonable time frame. However, geospatial access remains inequitable, and the impact on outcomes is unclear. This must be considered as the cancer control system matures and expands.
INTRODUCTION
The incidence of cancer is increasing in Nigeria, including a doubling of the incidence of breast cancer between 1999 and 2009.1,2 To address the growing burden, a National Cancer Control Plan (NCCP) has been developed as a framework to guide cancer control policy and service delivery.3 A priority of the NCCP (2018-2022) is improving access to cancer care through investment in a network of public comprehensive cancer centers. These centers have been proposed to provide coverage to each of the 6 geopolitical zones in Nigeria.
Comprehensive cancer centers often anchor many components of a country’s cancer control program, while coordinating with peripheral sites for routine care delivery.4 They are designed to provide centralized access to a full complement of multidisciplinary clinical care, including ambulatory care, diagnostic radiology, pathology and laboratory medicine, surgery, radiation therapy, systemic cancer therapy, and palliative or supportive care.4 One of the priorities of the NCCP (2018-2022) is to strengthen 8 existing facilities to fulfill this role in Nigeria. All 8 facilities currently deliver on-site systemic cancer therapy (eg, traditional cytotoxic chemotherapy), diagnostic imaging, elective cancer surgery, and histopathology. However, access to radiotherapy and the full complement of diagnostic services is lacking.5,6
Access to health care is dependent on services being physically accessible, affordable, and acceptable to the target population.7 In low- and middle-income countries, such as Nigeria, physical distance from a health care facility remains one of the most important determinants of access.8 This is particularly true for contemporary cancer care, which often requires numerous visits to a health care facility. We constructed a geoinformation system model to analyze geospatial access to the 8 public comprehensive cancer centers outlined in the NCCP (2018-2022). This analysis explores the concept of equity of access to cancer care in Nigeria.
CONTEXT
Key Objective
How many Nigerians have access to public facilities earmarked to deliver comprehensive cancer care? We constructed a geoinformation system model to analyze access to the 8 public comprehensive cancer centers outlined in the National Cancer Control Plan (2018-2022).
Knowledge Generated
More than 113 million Nigerians are within 4 hours of a public hospital designated to offer comprehensive cancer care. However, there is a significant difference in geospatial access between geopolitical zones. Investment in an additional comprehensive cancer center in the North East would improve access by 26%-30%, affecting 7.6 million individuals across the north of the country.
Relevance
The majority of Nigerians have reasonable, albeit heterogenous, access to a public comprehensive cancer center. Significant variability in geospatial access may produce divergent outcomes based on place of residence. Defining and measuring access in the Nigerian context is essential to the delivery of equitable and cost-effective cancer care.
METHODS
Geographic Information System Data
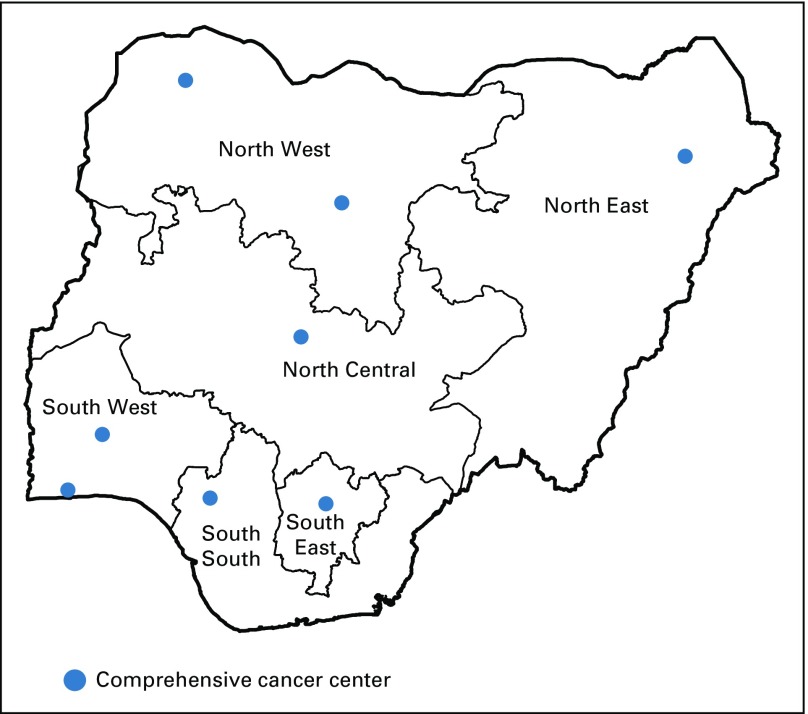
The 8 public comprehensive cancer centers outlined in the NCCP report are listed along with the location (ie, latitude, longitude) in Appendix Table A1 and are depicted along with the 6 geopolitical zones in Figure 1. The comprehensive cancer centers were geolocated using Google Earth (Google, Mountain View, CA). A 100-m2 population-density grid, produced by the WorldPop Project of the GeoData Institute, was used to model national population data.9 This was based on the 2006 census adjusted to match the United Nation’s national population estimates for 2010. Analyses used national population estimates, as well as estimates for individuals living on < US$2 per day. A geolocated national road network was obtained from OpenStreetMap (OpenStreetMap Foundation, Cambridge, United Kingdom). Roads were classified as primary (ie, national highways, connecting major cities), secondary (ie, intrastate roads), and tertiary (ie, minor roads, unpaved roads or tracks). Road data were cleaned and topographically verified using ArcMAP v10 (Esri, Redlands, CA). Road speed data were based on national traffic laws and verified by one of the authors. Road speeds were designated as 80, 50, and 30 kmh−1 for primary, secondary, and tertiary roads, respectively.
FIG 1.
The geopolitical zones of Nigeria and the comprehensive cancer centers.
Measuring Access
Travel time estimates were generated using cost-distance analyses. This method calculates the cumulative travel time associated with traveling from any geographic location within the study area to the nearest comprehensive cancer center along the fastest possible route. A 100-m2 gridded cost surface was constructed using the national road network, weighted by speed limit. Cells without roads were assigned a value corresponding to a walking speed of 5 kmh−1. Access was defined as the proportion of the population within 1, 2, and 4 hours of travel time to the nearest comprehensive cancer center. The population distributions of travel time were then calculated for each of Nigeria’s 6 geopolitical zones to explore geographic disparities. Finally, we conducted the same analysis to examine access among the proportion of the population living on < US$2 per day. Pearson’s χ2 test with an α = .05 was used to determine the significance of differences in access between regions and income.
RESULTS
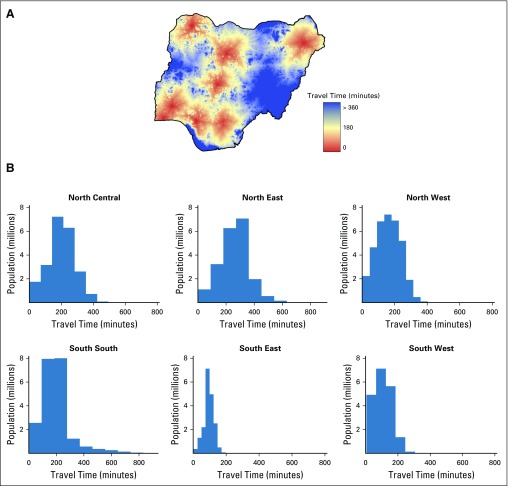
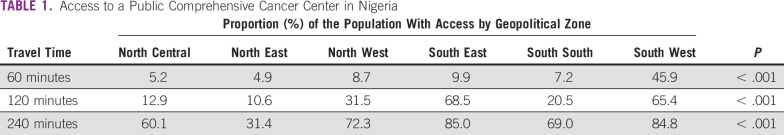
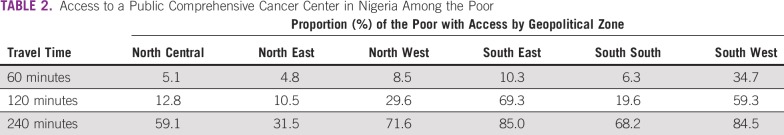
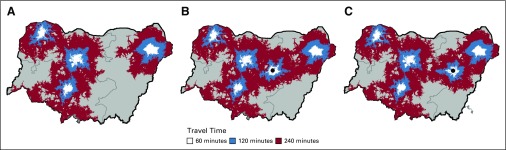
Travel time to the nearest public comprehensive cancer center in Nigeria is depicted in Figure 2. At the population level, 68.9% of individuals have access to a comprehensive cancer center within 4 hours of continuous vehicular travel. At 1 and 2 hours of travel, geospatial access is 15.5% and 36.0%, respectively. Access at all 3 time thresholds for each geopolitical zone is outlined in Table 1 and mapped in Figure 3. Geospatial access is significantly different between the general population and those living on < US$2 per day (P < .001). At 1 hour, 15.5% of the total population has access, compared with 11.6% of individuals living on < US$2 per day (P < .001). At 2 and 4 hours of travel, there is also a significant difference between the total population and individuals living on < US$2 per day (access at 2 hours: 36.0% v 31.9%, respectively; P < .001; access at 4 hours: 68.9% v 66.6%, respectively; P < .001). Access among the poor is outlined in Table 2.
FIG 2.
Population-level travel times to nearest comprehensive cancer center in Nigeria (A) overall and (B) by geopolitical zone.
TABLE 1.
Access to a Public Comprehensive Cancer Center in Nigeria
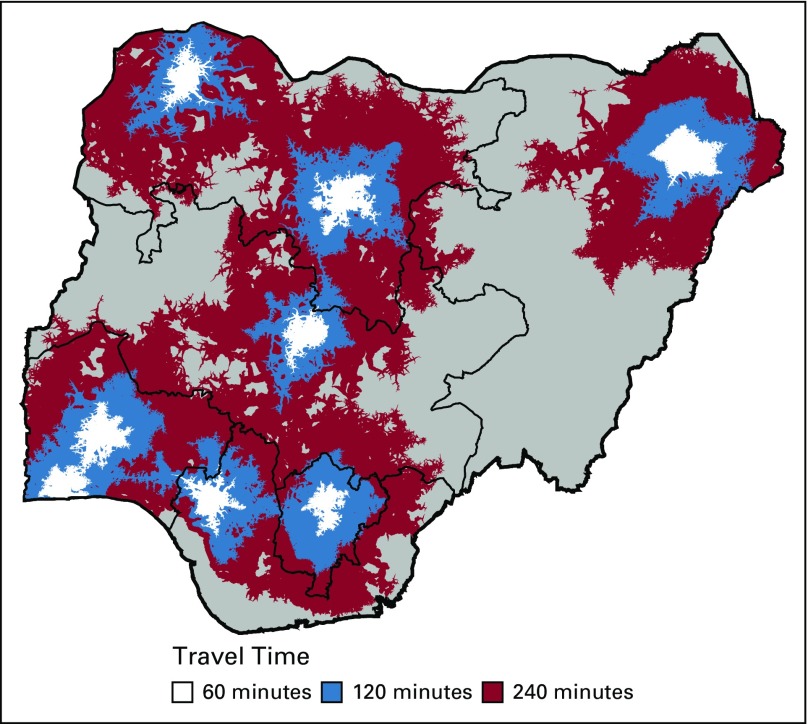
FIG 3.
Population-level access to a public comprehensive cancer center in Nigeria.
TABLE 2.
Access to a Public Comprehensive Cancer Center in Nigeria Among the Poor
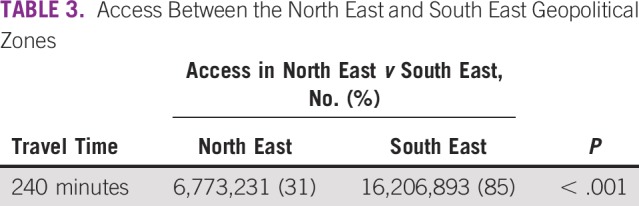
There is a significant difference in the access between geopolitical zones at 1, 2, and 4 hours of continuous travel (P < .001). Within 1 hour of travel, 45.9% of the population in the South West has access to a comprehensive cancer center. This is followed by the South East (9.9%) and the North West (8.7%). The North East geopolitical zone has the lowest coverage at all-time points (4.9%, 10.6%, and 31.4% at 1, 2, and 4 hours, respectively). At 4 hours of continuous travel, the population-level access in the North East is significantly lower than in the South East (31.4% v 85.0%, respectively; P < .001). This is outlined in Table 3. Mean travel time to the nearest comprehensive cancer center was calculated by geopolitical zone. Mean travel time was highest in the North East (268 minutes; standard deviation [SD], 104 minutes) and North Central (201 minutes; SD, 83 minutes) and lowest in the South East (94 minutes; SD, 30 minutes) and South West (103 minutes; SD, 57 minutes). The mean travel time was 161 minutes (SD, 74 minutes) and 186 minutes (SD, 114 minutes) in the North West and South South, respectively. Ninety-five percent of the population in the North East has access within 427 minutes, whereas 95% of the population in the South East has access within 139 minutes.
TABLE 3.
Access Between the North East and South East Geopolitical Zones
To address the lack of access in the North East, the cost-distance model was modified to measure access to the University of Maiduguri Teaching Hospital plus 1 of 2 remaining federal teaching hospitals in the geopolitical zone, Abubakar Tafawa Balewa University Teaching Hospital (ATBUTH) or Federal Teaching Hospital Gombe (FTHG). As an additional comprehensive cancer center, ATBUTH increases 4-hour access in the North East by 26.7% (P < .001). If FTHG is designated a comprehensive cancer center, access in the North East increases by 30.3% (P < .001). However, when examined across all 3 northern geopolitical zones, designating ATBUTH as a comprehensive cancer center was associated with a greater absolute increase. The addition of ATBUTH extended 4-hour access to an additional 7.6 million individuals across the northern 3 geopolitical zones. This is captured in Figure 4.
FIG 4.
Improving access with additional investment in the northern geopolitical zones. (A) Access based on the comprehensive cancer centers currently outlined in the National Cancer Control Plan. (B) Access with addition of Abubakar Tafawa Balewa University Teaching Hospital. (C) Access with addition of Federal Teaching Hospital Gombe.
DISCUSSION
More than 113 million Nigerians are within 4 hours of a public hospital designated to offer comprehensive cancer care. However, this analysis suggests that there is significant variability in access between geopolitical zones. In the South West and South East, the proportion of the population with 4-hour access is almost triple that in the North East. Mean travel time to the nearest comprehensive cancer center is also longer in the North East compared with elsewhere in the country. The North East seems to be an outlier in geospatial access, which reflects its large size, its position as a border state, and the relative isolation of its sole comprehensive cancer center (ie, University of Maiduguri Teaching Hospital). Investment in one of the remaining tertiary care, federal teaching hospitals (ie, ATBUTH or FTHG) in the North East would significantly increase access to cancer care services in this underserviced region. Our analysis suggests that the creation of a comprehensive cancer center at ATBUTH would result in the greatest increase in absolute access across all 3 northern geopolitical zones.
The highly variable population-level access between geopolitical zones, particularly between north and south, has the potential to produce divergent outcomes for patients with cancer of similar need. A systematic review by Ambroggi et al10 has previously demonstrated that both distance and time have a negative impact on treatment, prognosis, and quality of life for patients with a variety of cancers. Among women living within 50 km of a tertiary care facility in South Africa, the risk of advanced breast cancer presentation was 1.25-fold (95% CI, 1.09 to 1.42) higher per 30 km.11 In Nigeria, a multicenter study by Jedy-Agba et al12 failed to demonstrate a relationship between self-reported travel time and stage of breast cancer at presentation once adjusted for education and religion (odds ratio, 1.50; 95% CI, 0.59 to 3.83; P = .396). Our analysis did not examine the relationship between travel time and cancer-specific outcomes. However, the cost-distance model could be used to explore the relationship between geospatial access and outcomes in subsequent analyses. This has not been rigorously examined in Nigeria.
In this study, we constructed a cost-distance model to estimate geospatial access. This is particularly important in settings with poor road infrastructure, where distance alone may underestimate the travel burden. Travel time is associated with costs that are an important component of the full economic burden of cancer care. These costs are inherently regressive because they are not proportional to an individual’s ability to pay. In Nigeria, this adds a significant burden to the out-of-pocket cost associated with care delivery.13 The degree to which travel burden affects health care utilization is captured by the distance-decay effect, which is the inverse relationship between health care utilization and distance.14 The distance-decay effect has been demonstrated for inpatient and outpatient care, regardless of age, sex, or illness acuity across sub-Saharan Africa, including Nigeria.14-17 We calculated access at both the population level and at a common income threshold associated with poverty because there is evidence that income level mitigates the impact physical distance has on access.14
The travel time thresholds (ie, 1, 2, and 4 hours) used in this study are not associated with specific outcomes. However, it is important to consider that private vehicle ownership in Nigeria remains low.18 Four hours (1 way) of continuous travel is a conservative estimate of a full day’s travel (ie, during daylight hours) based on the poor state of the road infrastructure and the significant security concerns across much of the country. It is also grounded in work by Moïsi et al19 from East Africa, which suggests that hospital admissions can decrease to < 5% after 4 hours of travel, assuming a constant 27% decay per 30 minutes of vehicular travel.
Comprehensive cancer centers are not intended to fulfill all components of cancer care for a region or country. This is particularly relevant when one considers the impact travel burden has on access. For many components of cancer care, patients will benefit from management at local health facilities that are integrated into the oversight and care delivery provided by a centralized facility. However, for specialized services that are best centralized, such as radiotherapy, travel time and its impact on accessibility and affordability must be considered.
This analysis measures access from a single variable—geospatial proximity. However, access is best examined as an interaction between the following 3 interdependent variables: accessibility, affordability, and acceptability. Improving access begins by defining a set of measurable, context-specific parameters, upon which evidence-based health policy can guide additional investment and health system development. An accurate understanding of the true burden of disease is critical to this process. As recommended by the NCCP, population-based cancer registries must be expanded with an emphasis on total case ascertainment and quality control. A basic understanding of access is also contingent on a detailed assessment of available capital (eg, human, material, financial). A systematic evaluation of available cancer care resources (eg, national endoscopy capacity, functional mammography) is needed in Nigeria. This could initially focus on the domains required for comprehensive cancer care (eg, surgery, histopathology) and the 5 cancers outlined in the NCCP (ie, breast, cervical, prostate, colorectal, and liver).3 Institutional cancer registries capture important data on diagnostic and treatment-related variables, such as the proportion of individuals with radiographic staging before elective cancer surgery. These registries represent an existing source of data that can be used to benchmark access. This should be supported by the Federal Ministry of Health and the breadth of existing registries expanded. Given the high proportion of out-of-pocket spending on health care in Nigeria,20 a better understanding of the financial burden of cancer care also needs to be determined by large, prospective studies.
There are several limitations of this study. The relationship between geospatial access and income is much more complex than captured in our simple income analysis. Individuals with sufficient means will travel to where the required care is provided and, in some cases, will seek care outside the country. This subset of the population will be significantly less constrained by physical distance, and this is not captured. Our analysis is also limited to the 8 public comprehensive cancer centers outlined in the NCCP, which does not capture cancer care delivered at other public or private facilities. The landscape of cancer care delivery is evolving rapidly in Nigeria, and the changing operational capacity of the 8 centers is not captured in this assessment. An objective of the NCCP is to increase capacity by 50% across the comprehensive cancer centers by 2022.3 Our analysis examined access to all 8 centers as offering equally comprehensive care, which will require significant additional investment to achieve.
As the burden of cancer increases in Nigeria, improving access to safe, affordable, and high-quality cancer care is a priority. The Federal Ministry of Health endorses a cancer control plan that has targeted investment in 8 public comprehensive cancer centers. Strengthening these centers will allow the majority of Nigerians to access the full complement of multidisciplinary care within a reasonable time frame. However, there exists significant variability between geopolitical zones, which may contribute to divergent outcomes based on place of residence. As the cancer control system matures and expands, measuring access will be essential to deliver equitable, cost-effective health policy and development.
Appendix
TABLE A1.
Comprehensive Cancer Centers in Nigeria
Footnotes
Supported in part by National Institutes of Health/National Cancer Institute Cancer Center Support Grant No. P30 CA008748. The Global Cancer Disparities Initiative is funded by the Memorial Sloan Kettering Cancer Center, with support from the Thompson Family Foundation.
AUTHOR CONTRIBUTIONS
Conception and design: Gregory C. Knapp, Gavin Tansley, Olalekan Olasehinde, Olusegun I. Alatise, Bata M. Gali, T. Peter Kingham
Administrative support: Funmilola Wuraola
Provision of study materials or patients: Moses O. Olawole
Collection and assembly of data: Gregory C. Knapp, Gavin Tansley, Olalekan Olasehinde, Olusegun I. Alatise, Funmilola Wuraola, Bata M. Gali
Data analysis and interpretation: Gregory C. Knapp, Gavin Tansley, Olalekan Olasehinde, Olusegun I. Alatise, Funmilola Wuraola, Moses O. Olawole, Olujide O. Arije, Bata M. Gali
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jgo/site/misc/authors.html.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
T. Peter Kingham
Consulting or Advisory Role: Physician Education Resource
No other potential conflicts of interest were reported.
REFERENCES
- 1. Irabor D, Adedeji OA: Colorectal cancer in Nigeria: 40 years on—A review. Eur J Cancer Care (Engl) 18:110-115, 2009. [DOI] [PubMed]
- 2.Jedy-Agba E, Curado MP, Ogunbiyi O, et al. Cancer incidence in Nigeria: A report from population-based cancer registries. Cancer Epidemiol. 2012;36:e271–e278. doi: 10.1016/j.canep.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.https://www.iccp-portal.org/plans/nigeria-national-cancer-control-plan International Cancer Control Partnership: National Cancer Control Plan: 2018-2022, Federal Ministry of Health.
- 4. Gelband H, Jha P, Sankaranarayanan R, et al (eds): Cancer services and the comprehensive cancer center, in Cancer: Disease Control Priorities (vol 3, ed 3). Washington, DC, International Bank for Reconstruction and Development/The World Bank, 2015, pp 195-210. [Google Scholar]
- 5.Irabor OC, Nwankwo KC, Adewuyi SA. The stagnation and decay of radiation oncology resources: Lessons from Nigeria. Int J Radiat Oncol Biol Phys. 2016;95:1327–1333. doi: 10.1016/j.ijrobp.2016.04.026. [DOI] [PubMed] [Google Scholar]
- 6.Anakwenze CP, Ntekim A, Trock B. doi: 10.1016/j.ctro.2017.05.003. et al: Barriers to radiotherapy access at the University College Hospital in Ibadan, Nigeria. Clin Transl Radiat Oncol 5:1-5, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gulliford M, Figueroa-Munoz J, Morgan M, et al. What does ‘access to health care’ mean? J Health Serv Res Policy. 2002;7:186–188. doi: 10.1258/135581902760082517. [DOI] [PubMed] [Google Scholar]
- 8.Feikin DR, Nguyen LM, Adazu K, et al. The impact of distance of residence from a peripheral health facility on pediatric health utilisation in rural western Kenya. Trop Med Int Health. 2009;14:54–61. doi: 10.1111/j.1365-3156.2008.02193.x. [DOI] [PubMed] [Google Scholar]
- 9. School of Geography and Environmental Science, University of Southampton: WorldPop: Nigeria 100m population. https://www.worldpop.org/doi/10.5258/SOTON/WP00648.
- 10.Ambroggi M, Biasini C, Del Giovane C, et al. Distance as a barrier to cancer diagnosis and treatment: Review of the literature. Oncologist. 2015;20:1378–1385. doi: 10.1634/theoncologist.2015-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dickens C, Joffe M, Jacobson J, et al. Stage at breast cancer diagnosis and distance from diagnostic hospital in a periurban setting: A South African public hospital case series of over 1,000 women. Int J Cancer. 2014;135:2173–2182. doi: 10.1002/ijc.28861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jedy-Agba E, McCormack V, Olaomi O, et al. Determinants of stage at diagnosis of breast cancer in Nigerian women: Sociodemographic, breast cancer awareness, health care access and clinical factors. Cancer Causes Control. 2017;28:685–697. doi: 10.1007/s10552-017-0894-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ibrahim N, Pozo-Martin F, Gilbert C. Direct non-medical costs double the total direct costs to patients undergoing cataract surgery in Zamfara state, Northern Nigeria: A case series. BMC Health Serv Res. 2015;15:163. doi: 10.1186/s12913-015-0831-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. doi: 10.1016/0277-9536(83)90298-8. Stock R: Distance and the utilization of health facilities in rural Nigeria. Soc Sci Med 17:563-570, 1983. [DOI] [PubMed] [Google Scholar]
- 15. doi: 10.1186/s12942-017-0107-7. Ouma PO, Agutu NO, Snow RW, et al: Univariate and multivariate spatial models of health facility utilisation for childhood fevers in an area on the coast of Kenya. Int J Health Geogr 16:34, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gething PW, Noor AM, Zurovac D, et al. Empirical modelling of government health service use by children with fevers in Kenya. Acta Trop. 2004;91:227–237. doi: 10.1016/j.actatropica.2004.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. doi: 10.1186/1476-072X-9-17. Gu W, Wang X, McGregor SE: Optimization of preventive health care facility locations. Int J Health Geogr 9:17, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.National Bureau of Statistic http://nigeria.opendataforafrica.org/eclpnhd/general-household-survey-panel Nigeria: General household survey 2013-2015.
- 19.Moïsi JC, Nokes DJ, Gatakaa H, et al. Sensitivity of hospital-based surveillance for severe disease: A geographic information system analysis of access to care in Kilifi district, Kenya. Bull World Health Organ. 2011;89:102–111. doi: 10.2471/BLT.10.080796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Onwujekwe O, Hanson K, Uzochukwu B. Examining inequities in incidence of catastrophic health expenditures on different healthcare services and health facilities in Nigeria. PLoS One. 2012;7:e40811. doi: 10.1371/journal.pone.0040811. [DOI] [PMC free article] [PubMed] [Google Scholar]