Abstract
Purpose: This retrospective case series assessed the results of a treatment protocol for patients with infected para-articular knee nonunions. The aim was to demonstrate that knee function and quality-of-life (QoL) can be improved.
Case series: Between January 2001 and December 2011, eleven patients with septic proximal tibial nonunion and seven with septic distal femoral nonunion were managed at our institution. The treatment protocol included extensive debridement, skeletal stabilization, culture-specific antibiotic administration, and soft-tissue and bone-deficit reconstruction. Knee function was evaluated with the Knee Society Score (KSS) while the Knee injury and Osteoarthritis Outcome Score (KOOS) and SF-12 were used for QoL assessment at a mean follow-up of 37.2 (range: 12-149) months. Seventeen nonunions healed at a mean of 21.9 weeks. One patient needed above knee amputation. Knee Society function and knee scores were improved significantly, from 16.7 and 33.8, to 75.0 and 84.9 respectively (p <0.001). KOOS outcome and SF-12 physical and mental components scores confirmed the QoL improvement.
Conclusions: Staged management can improve QoL and functional knee outcome. HIPPOKRATIA 2018, 22(4): 183-187.
Keywords: Nonunion, infection, knee, bone defect, quality of life, circular frame
Introduction
Infected para-articular nonunions around the knee joint constitute a severe and debilitating problem for the patient and a challenge for the surgeon. Sepsis, small and usually osteopenic juxta-articular bone fragments, insufficient bone and soft tissue stock, and irreversible damage to the articular cartilage and the tendino-ligamentous compartment are the major drawbacks. Even the lower limb viability might be at risk. So far, published reports regarding the operative management have been rare. Different options have been proposed such as plate osteosynthesis1, cortical allograft struts2,3, external fixation and distraction osteogenesis4,5 with variable success rates. However, none of these treatments has adequately addressed all of the coexisting problems simultaneously.
Patzakis and Zalavras have popularized a staged surgical protocol6 for the infected diaphyseal counterparts. These can be successfully managed by combining extensive surgical debridement, use of antibiotics both locally and systemically, primary wound coverage or flap-assisted closure, stabilization preferably with external fixation and finally addressing any residual malalignment with limb reconstruction.
The research question in this study was whether a staged surgical intervention using a consistent treatment protocol improves the knee functionality and quality-of-life (QoL).
Case series
This is a retrospective case series that included eighteen patients (14 men, four women) with an average age of 46.9 (range: 16-79) years who were treated at the University Hospital of Larissa between 2001 and 2011. Eleven cases involved the proximal tibia and seven the distal femur. Fracture was the main cause for the nonunions (13 road traffic accidents, four falls from a height, one sports injury). Seven were closed wounds and eleven were open. Six proximal tibia fractures were classified as Schatzker VI, two as Schatzker V, two as Schatzker IV, and one as Schatzker III. Five distal femoral fractures were extra-articular, one partial articular, and one complete articular. Initially, 15 patients were treated with internal (plate/screws) and three with external fixation. There was an average of 3.5 (range: 1-12) previous surgical interventions, including the initial fixation. The mean duration between the initial injury and the presentation at our institution was 12.1 (range: 3-48) months. During hospitalization, all patients received standards of care as per institutional guidelines; thus, Ethical Committee approval was waived.
Operative technique
Previous incisions were used and extended if required. Loose implants were removed and nonunion was debrided until viable bleeding surface was exposed. From the infected site, specimens (minimum five) were submitted for cultures, histological, and molecular analysis. Vancomycin and Imipenem powder-loaded poly-methyl-methacrylate (PMMA) spacers were locally applied. Postoperatively all patients received culture specific intravenous antibiotics for two weeks and subsequently oral antibiotics for 2-3 weeks. Debridement was repeated every three days until no signs of infection were evident. A new antibiotic-spacer was put and then covered with a sterile sealant to secure an antibiotic rich pouch, until definite closure.
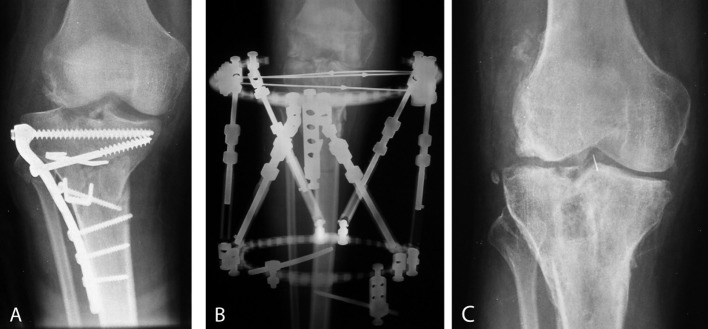
Osseous and soft tissue deficits were managed at the last stage. Bony defects were filled with autogenous iliac bone graft. If the articular surface reconstruction was deemed impossible, cadaveric, total or partial osteo-articular allograft placement was performed instead. Where the joint surface was reconstructable, external frame fixation or plating was applied. Bone stock, intraoperative morphology after final debridement, presence of osteoporosis, soft tissue problems and necessity for malalignment correction were the determinant factors as to which of the two options was the most suitable. Soft tissue coverage was attained either with a split-thickness skin graft or combined with medial gastrocnemius flap. Residual malalignment correction was performed concurrently or with postoperative manipulation and adjustment using the circular frames (Figure 1 A, B).
Figure 1. Radiographs in a male patient aged 31 managed for a septic tibial plateau nonunion, a) failed open reduction internal fixation, anteroposterior (AP) view, b) AP view of Taylor Spatial Frame used for skeletal stabilization and malalignment correction following debridement, and c) AP view of the knee joint at the last follow-up showing complete bony union.
Rehabilitation included quadriceps muscle isometric exercises, passive motion as tolerated and active range of movement (ROM) by the end of the first week. Progressive weight bearing was allowed when bony healing was radiographically evident. External frames were removed when the bone union was achieved, followed by gradually increasing protected weight bearing for one month (Figure 1 C).
Outcome
In our series, four nonunions were managed in two stages, while the other 14 were managed in more stages. External fixation was applied in ten patients, five with Taylor Spatial Frame (TSF, Smith and Nephew Inc., Memphis, USA), four with Ilizarov System (Smith and Nephew Inc., Memphis, USA), and one with monolateral external fixator (Orthofix SRL, Verona, Italy). Four patients underwent reconstruction with full-thickness cadaveric allograft and internal fixation, three with plate osteosynthesis and one had above knee amputation. Medial gastrocnemius muscular flap was transferred in five cases.
Multiple organisms were isolated in the specimens derived from four patients, whereas a single microbe was detected in the specimens of the other 14 patients. Staphylococcus Aureus was the most common cultured microorganism isolated in 13 patients, Staphylococcus epidermidis in four patients, Klebsiella pneumoniae, Proteus mirabilis, Enterococcus faecalis and Acinetobacter baumannii in two patients, and Pseudomonas aeruginosa, Citrobacter Freundii, Enterococcus faecium in one patient.
The patients were submitted to a mean of 3.5 (range: 1-7) operations. The mean hospitalization was 33.3 (range: 7-82) days and the external fixation devices were retained for a mean time of 4.9 (range: 3.5-7) months. Four patients with the Ilizarov apparatus and five with the TSF were submitted to gradual correction for length, angular, and rotational deformities. There was a minor Leg Length Discrepancy (LLD) in four patients (three patients 1-2 cm, one patient 3 cm). All muscular flaps survived with no subsequent complications for the surrounding soft tissues. Infection was eradicated and osseous union was achieved in all patients. The mean time to radiographic and clinical bony union was 5.47 (range: 3-7) months.
The most common complication was deep infection recurrence in three patients. They were revised using the same protocol. Arthrofibrosis in two patients was managed with an arthroscopic release. Total knee arthroplasty (TKA) was performed in two patients during the follow-up period. One fracture of the cadaveric allograft was treated with custom-made TKA while the primary reasons for the other one were intractable pain, inefficient joint function, and severe ambulatory problems.
Follow-up visits were individualized according to postoperative progress. The average duration was 37.2 (range: 12-149) months. The clinical and functional result was assessed with measurement of the ROM and Knee Society Rating Score (KSS)7,8 preoperatively and at the latest follow-up. KSS has two parts, the function and the knee assessment score7,8. The impact on QoL was assessed with the Short Form-12 (SF-12)9and the Knee Injury and Osteoarthritis Outcome Score (KOOS)10. The SF-12 includes the Physical Component Summary-12 (PCS-12) and the Mental Component Summary-12 (MCS-12) scores9. Development of osteoarthritis was evaluated with anteroposterior and lateral radiographs of the affected knee joint and classified according to the Kellgren-Lawrence (K/L) grading scale11.
Statistics were obtained using the SPSS Statistics for Windows, Version 17.0 (SPSS Inc., Chicago, IL, USA). Before applying parametric methods (Student’s t-test), the data was checked for normality. If there was a significant deviation from normality, then a non-parametric test (Wilcoxon signed-rank test) was used. The mean and standard deviation for baseline characteristics were calculated. Statistical comparisons between pre and postoperative ROM and SF-12 scores were made using two-tailed Student’s t-test with a level of significance p <0.05. For KSS, and KOOS scores Wilcoxon signed-rank test was used.
Preoperatively all patients presented limitation of knee flexion-extension. Mean knee ROM was 31.5o (range: 4-81o). The mean preoperative KSS function and knee scores were 17.8 and 33.6, respectively. SF-12 (PCS and MCS) scores were 29 and 36.4, respectively, and KOOS was 28.9.
Postoperatively, the mean knee ROM was 81.7o (range: 4-118o), while preoperative was 31.5o(p <0.001). The mean postoperative KSS function and knee subscales were improved to 74.7 and 85.1, respectively, which was a statistically significant improvement compared to preoperative scores (p <0.001). The mean SF-12 (PCS) score was 43.8 (p <0.001). The mean SF-12 (MCS) was improved to 55.4 (p <0.001). Likewise, postoperative KOOS was increased to 71.1 (p <0.001). Nine patients (seven proximal tibia cases, two distal femur cases) were able to return back to their previous occupations without any restrictions, and three (one proximal tibia case, two distal femur case) with moderate restrictions.
Radiographic evaluation at the last follow-up examination on 15 patients, who did not require knee arthroplasty during the follow-up period, classified three patients as grade I, three patients as grade II, six patients as grade III, and three patients as grade IV K/L.
Discussion
Para-articular infected nonunions around the knee constitute a rare subset of complications. Similar reports in the literature are scarce, and their true incidence is yet to be defined. The surgeon must overcome technical obstacles like bone loss, inadequate soft-tissue coverage, scarring, alignment deformities, and possible LLD. Moreover, long-term consequences like post-traumatic osteoarthritis and stiffness should be anticipated. These all adversely affect knee functionality and sometimes the likelihood of knee salvage. Proper osseous reduction with respect to anatomy and soft tissues, stable fixation and malalignment correction allow for early mobilization, enhanced rehabilitation, reduced morbidity and better ROM12.
Staged management can control sepsis and improve knee functionality and quality of life. In our series infection was eliminated in all patients except one. The mean ROM increased to 50.2o but was not restored to normal. The mean KSS function and knee assessment scores increased to 41.1 and 67.3, respectively. QoL indicators, KOOS, SF-12 PCS, and MCS, increased on average 42.2, 14.8, and 19.0, respectively. These observations are statistically significant.
Kabata et al reported management of seven juxta-articular nonunions (five septic and two aseptic) with Distraction Osteogenesis (DO) apparatus4. Four were located in the distal femur, one in the proximal tibia and two in the distal tibia. Osseous union without angular deformities or LLD >1 cm and excellent pain reduction were achieved in all patients without recurrent infections. We underline the significant postoperative ROM restriction due to long-term immobilization and pain. Only two patients achieved postoperative improving ROM compared to the pre-injury ROM. Two patients had limited postoperative ROM, but were improved compared to the preoperative ROM, while in three patients the ROM remained unchanged. Saridis et al recorded similar results with the Ilizarov method5. Bony union, full weight bearing, and infection eradication were accomplished in all 13 patients with septic distal femoral nonunions. Only in one case LLD was more than 2.5 cm. In our series, external fixation with the ability for distraction osteogenesis was not the only choice. Plating and cadaveric allografts were also used. The decision was based on bone and soft tissue deficit, residual bone stock, and the ability to reconstruct the articular surface. LLD more than 2 cm was noted in one patient. Overall, mean ROM was improved especially for the tibial cases. However, that was not the case for the femoral counterparts.
At the end of the follow-up period, KSS subscale scores confirmed functional improvement at a mean follow-up of 37 months. In the case series reported by Gardner et al, 16 patients with aseptic proximal tibia nonunion were treated according to a consistent approach including debridement, deformity correction, lateral plating, tensioning and compression, lag screws and bone grafting13. At a mean follow-up of 39 months, the KSS function and knee scores were 87.4 and 89.4, respectively. Gardner et al applied a similar management algorithm to treat 31 distal femoral nonunions14. At a mean follow-up of 41.5 months the KSS function and assessment scores were 61.2 and 78.3, respectively. Our series involved both proximal tibia and distal femoral infected nonunions with intra-articular extension. The results were functionally superior to both groups, while knee assessment score was superior only to the distal femoral nonunion group.
Our study is the first research that reports health-related QoL of patients with septic para-articular knee nonunions. Brinker et al evaluated the devastating effects of tibial nonunion on health-related QoL15. They assessed 243 tibial shaft nonunions in 237 patients over 10 years. Infection was present in 18 % of all cases. The SF-12 PCS averaged 27.4 ± 6.7. In our cases, the preliminary PCS was marginally better, but significantly worse compared to patients with knee injuries like meniscus lesion (mean 37.9), anterior cruciate ligament rupture (mean 41.2), cartilage injury (mean 36.2) or patellar instability (mean 40.4)16. At the final follow-up, the upgraded mean PCS score of 43.8 was indicative of fewer limitations in self-care and physical activities and positive health status improvement. On the contrary, our initial MCS score was considerably worse compared to the tibia diaphysis nonunion group (42.3 ± 7.1)15. However, at the end, amelioration of the SF-12 MCS score displayed emotional stability with minimal restrictions in vitality and social function.
The subjective ability to accomplish simple daily tasks is clearly designated with the KOOS scale. In a retrospective study of 23 intra-articular and bicondylar tibial plateau fractures, Jansen et al17 estimated that the average KOOS score was 67.8 on a mean follow-up of 67 months. Considering the infected counterparts, where the average KOOS was 71.1 on a mean follow-up of 37.2 months, timely intervention can improve quality of life in a shorter period of time.
Considerable post-traumatic arthritis was noticed, even though the patients were well in terms of pain and ROM. Eleven patients had moderate to severe osteoarthritis. Progressive osteoarthritis is the habitual outcome of infected nonunions approximating the knee joint. According to Wasserstein et al18, tibial plateau fracture surgery increases the likelihood for a total knee arthroplasty 5.3 times. Within ten years after the initial trauma, 7.3 % of the patients will have been sustained a knee reconstruction. Whereas supracondylar-intercondylar distal femoral fractures managed operatively to demonstrate radiographic changes of post-traumatic arthritis up to 50 %, with minimal risk of TKA19. Though degenerative changes were detected in every case in our series, only two patients (11 %) underwent arthroplasty during the follow-up period. Some authors have supported primary long-term arthroplasty for para-articular nonunions20,21. By preserving knee functionality, pain diminution, early ambulation, and ROM can be enhanced. Nevertheless, we must be cautious with post-infected patients. A possible failure or a subsequent infectious relapse can be associated with severe complications (e.g., stiffness, extensor system avulsion, instability) and may end up with above knee amputation. In uncomplicated cases the mean flexion gains approximates 6°22. So far in the literature, there is not sufficient evidence to support what is the optimum time for the knee arthroplasty to be performed. Staged management can significantly reduce the risk of re-infection; however, there are reports that latent infections can become active even after a year23.
The main limitations of current series are their small cohort of patients and the retrospective data gathering and analysis. Moreover, literature relevant to infected para-articular nonunions of the knee is extremely inadequate and existing reports focus mainly on patients with uncomplicated nonunions in the meta-epiphyseal region. Thus, it is challenging to attempt direct comparison to similar injuries. Furthermore, although KSS efficacy in assessing septic nonunions has not been completely determined, it is a validated questionnaire, which analyzes adequately knee functionality relatively to any subsequent axial malformation. Additionally, KOOS and SF-12 scales provide an in-depth estimation of the patients’ QoL. SF-12 subscales comprehensively indicate the physical and mental health of the patient, while KOOS appraises the competence to execute specific everyday activities.
Noticeable improvement regarding the knee function and the quality of everyday life was recorded in our case series. Infected nonunions close to the knee are linked with detrimental long-term complications. The presented management protocol was used successfully for the treatment of these problematic and infrequent cases.
Conflict of interest
The authors declare no conflict of interest. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Mandt PR, Gershuni DH. Treatment of nonunion of fractures in the epiphyseal-metaphyseal region of long bones. J Orthop Trauma. 1987;1:141–151. doi: 10.1097/00005131-198702010-00004. [DOI] [PubMed] [Google Scholar]
- 2.Wang JW, Weng LH. Treatment of distal femoral nonunion with internal fixation, cortical allograft struts and autogenous bone-grafting. J Bone Joint Surg Am. 2003;85-A:436–440. doi: 10.2106/00004623-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Delloye C, van Cauter M, Dufrane D, Francq BG, Docquier PL, Cornu O. Local complications of massive bone allografts: an appraisal of their prevalence in 128 patients. Acta Orthop Belg. 2014;80:196–204. [PubMed] [Google Scholar]
- 4.Kabata T, Tsuchiya H, Sakurakichi K, Yamashiro T, Watanabe K, Tomita K. Reconstruction with distraction osteogenesis for juxta-articular nonunions with bone loss. J Trauma. 2005;58:1213–1222. doi: 10.1097/01.ta.0000169806.08994.e2. [DOI] [PubMed] [Google Scholar]
- 5.Saridis A, Panagiotopoulos E, Tyllianakis M, Matzaroglou C, Vandoros N, Lambiris E. The use of the Ilizarov method as a salvage procedure in infected nonunion of the distal femur with bone loss. J Bone Joint Surg Br. 2006;88:232–237. doi: 10.1302/0301-620X.88B2.16976. [DOI] [PubMed] [Google Scholar]
- 6.Patzakis MJ, Zalavras CG. Chronic posttraumatic osteomyelitis and infected nonunion of the tibia: current management concepts. J Am Acad Orthop Surg. 2005;13:417–427. doi: 10.5435/00124635-200510000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Orthopaedic Scores. Knee Society Score. Available at: https://www.orthopaedicscore.com/scorepages/knee_society_score.html. date accessed: 30/09/2018.
- 8.Orthopaedic Scores. Knee Society Score - Function. Available at: https://www.orthopaedicscore.com/scorepages/knee_society_score_function.html. date accessed: 30/09/2018.
- 9.Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Orthopaedic Scores.com. Knee Injury and Osteoarthritis Outcome Score (KOSS). Available at: http://www.orthopaedicscore.com/scorepages/knee_injury_osteopaedic_outcome_score.html. date accessed: 30/09/2018.
- 11.Kohn MD, Sassoon AA, Fernando ND. Classifications in Brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474:1886–1893. doi: 10.1007/s11999-016-4732-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papagelopoulos PJ, Partsinevelos AA, Themistocleous GS, Mavrogenis AF, Korres DS, Soucacos PN. Complications after tibia plateau fracture surgery. Injury. 2006;37:475–484. doi: 10.1016/j.injury.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 13.Gardner MJ, Toro-Arbelaez JB, Hansen M, Boraiah S, Lorich DG, Helfet DL. Surgical treatment and outcomes of extraarticular proximal tibial nonunions. Arch Orthop Trauma Surg. 2008;128:833–839. doi: 10.1007/s00402-007-0383-y. [DOI] [PubMed] [Google Scholar]
- 14.Gardner MJ, Toro-Arbelaez JB, Harrison M, Hierholzer C, Lorich DG, Helfet DL. Open reduction and internal fixation of distal femoral nonunions: long-term functional outcomes following a treatment protocol. J Trauma. 2008;64:434–438. doi: 10.1097/01.ta.0000245974.46709.2e. [DOI] [PubMed] [Google Scholar]
- 15.Brinker MR, Hanus BD, Sen M, O’Connor DP. The devastating effects of tibial nonunion on health-related quality of life. J Bone Joint Surg Am. 2013;95:2170–2176. doi: 10.2106/JBJS.L.00803. [DOI] [PubMed] [Google Scholar]
- 16.Glazebrook M, Daniels T, Younger A, Foote CJ, Penner M, Wing K, et al. Comparison of health-related quality of life between patients with end-stage ankle and hip arthrosis. J Bone Joint Surg Am. 2008;90:499–505. doi: 10.2106/JBJS.F.01299. [DOI] [PubMed] [Google Scholar]
- 17.Jansen H, Frey SP, Doht S, Fehske K, Meffert RH. Medium-term results after complex intra-articular fractures of the tibial plateau. J Orthop Sci. 2013;18:569–577. doi: 10.1007/s00776-013-0404-3. [DOI] [PubMed] [Google Scholar]
- 18.Wasserstein D, Henry P, Paterson JM, Kreder HJ, Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Joint Surg Am. 2014;96:144–150. doi: 10.2106/JBJS.L.01691. [DOI] [PubMed] [Google Scholar]
- 19.Thomson AB, Driver R, Kregor PJ, Obremskey WT. Long-term functional outcomes after intra-articular distal femur fractures: ORIF versus retrograde intramedullary nailing. Orthopedics. 2008:748–748-. doi: 10.3928/01477447-20080801-33. [DOI] [PubMed] [Google Scholar]
- 20.Anderson SP, Matthews LS, Kaufer H. Treatment of juxtaarticular nonunion fractures at the knee with long-term total knee arhroplasty. Clin Orthop Relat Res. 1990;(260):104–109. [PubMed] [Google Scholar]
- 21.Haidukewych GJ, Springer BD, Jacofsky DJ, Berry DJ. Total knee arthroplasty for salvage of failed internal fixation or nonunion of the distal femur. J Arthroplasty. 2005;20:344–349. doi: 10.1016/j.arth.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 22.Parratte S, Boyer P, Piriou P, Argenson JN, Deschamps G, Massin P, et al. Total knee replacement following intra-articular malunion. Orthop Traumatol Surg Res. 2011;97:S118–S123. doi: 10.1016/j.otsr.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Manidakis N, Dosani A, Dimitriou R, Stengel D, Matthews S, Giannoudis P. Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop. 2010;34:565–570. doi: 10.1007/s00264-009-0790-5. [DOI] [PMC free article] [PubMed] [Google Scholar]