Abstract
Purpose:
To determine if inhibition of mitochondrial oxidative phosphorylation (OxPhos) is an effective strategy against MAPK pathway inhibitor (MAPKi)-resistant BRAF-mutant melanomas.
Experimental Design:
The anti-melanoma activity of IACS-010759 (OPi), a novel OxPhos complex I inhibitor, was evaluated in vitro and in vivo. Mechanistic studies and predictors of response were evaluated using molecularly and metabolically stratified melanoma cell lines. 13C-labeling and targeted metabolomics were used to evaluate the effect of OPi on cellular energy utilization. OxPhos inhibition in vivo was evaluated non-invasively by [18F]-FAZA PET imaging.
Results:
OPi potently inhibited OxPhos and the in vivo growth of multiple MAPKi-resistant BRAF-mutant melanoma models with high OxPhos at well-tolerated doses. In vivo tumor regression with single agent OPi treatment correlated with inhibition of both MAPK and mTOR complex I activity. Unexpectedly, anti-tumor activity was not improved by combined treatment with MAPKi in vitro or in vivo. Signaling and growth inhibitory effects were mediated by LKB1-AMPK axis, and proportional to AMPK activation. OPi increased glucose incorporation into glycolysis, inhibited glucose and glutamine incorporation into the mitochondrial tricarboxylic acid cycle, and decreased cellular nucleotide and amino acid pools. Early changes in [18F]-FAZA PET uptake in vivo, and the degree of mTORC1 pathway inhibition in vitro, correlated with efficacy.
Conclusions:
Targeting OxPhos with OPi has significant anti-tumor activity in MAPKi-resistant, BRAF-mutant melanomas, and merits further clinical investigation as a potential new strategy to overcome intrinsic and acquired resistance to MAPKi in patients.
Keywords: Melanoma, Targeted Therapy, Resistance, Oxidative Phosphorylation, FAZA
INTRODUCTION
Clinically approved selective inhibitors of V600-mutant BRAF and their combinations with MEK inhibitors achieve responses in the overwhelming majority of metastatic melanoma patients with point mutations affecting the V600 residue of BRAF (“BRAF-mutant”) (1-3). However, only ~15% patients achieve complete responses, and the median duration of responses is approximately one year (4,5). Thus, there is a critical need for new therapeutic strategies for BRAF-mutant melanoma, particularly against MAPKi-resistant tumors. We and others previously showed that a significant subset of human melanoma cell lines and clinical samples are characterized by elevated expression of mitochondrial oxidative phosphorylation (OxPhos) genes, a phenotype driven by PGC1α, a master activator of mitochondrial function (6-10). 30-50% of melanomas with intrinsic or acquired resistance to MAPKi have increased expression of PGC1α and OxPhos, and knockdown of PGC1α restored sensitivity to MAPKi (7). Unexpectedly, we found that inhibition of mTOR kinase activity suppressed PGC1α and OxPhos by causing cytoplasmic sequestration of MITF, a lineage-specific transcriptional regulator in melanoma (11). mTOR kinase inhibitor treatment alone did not achieve significant growth inhibition, but it demonstrated synergy with MAPKi in melanomas with high OxPhos in vitro and in vivo (7,9).
These findings support the rationale to further investigate the role and therapeutic potential of OxPhos in melanoma. Early clinical trials with mTOR1/2 inhibitors have shown challenging toxicological profiles that could limit their clinical impact (12). Thus, we evaluated IACS-010759 (OPi), a novel, potent, and specific inhibitor of electron transport chain (ETC) Complex 1 that inhibits OxPhos at low nanomolar concentrations as an alternative therapeutic strategy for high OxPhos resistant melanomas (13). OPi demonstrated safety and anti-tumor activity in preclinical models of leukemia and lung cancer (13,14), and recently we demonstrated activity in vivo in models of melanoma brain metastasis(15). Phase I clinical trials of OPi are ongoing in patients with leukemia () and advanced solid cancers ().
Here, we show that direct OxPhos inhibition with OPi achieves significant anti-tumor activity, including single-agent tumor regression, in high OxPhos MAPKi-resistant melanoma models in vivo at well-tolerated doses. Molecular analysis demonstrated that OPi inhibited key signaling pathways, including MAPK and mTOR complex I, in MAPKi-resistant melanomas. Unexpectedly, the efficacy of OPi was not improved by combined treatment with MAPK pathway inhibitors. Finally, we show that molecular imaging with [18F]-FAZA PET, a novel PET imaging marker (16), can non-invasively assess OxPhos inhibition and correlates with growth inhibition in vivo, providing a potential strategy to optimize the clinical development and evaluation of this agent.
MATERIALS AND METHODS
Cell lines and Inhibitors.
Cell line authentication and mutation detection were performed as previously described (17-19). Mutations in the patient-derived cell lines were determined from whole exome sequencing analysis (S. Woodman and colleagues, manuscript under preparation). All established cell lines were grown in RPMI media in 5% fetal bovine serum. M.D. Anderson Cancer Center patient-derived cell lines were grown in DMEM supplemented with 10% serum (20). IACS-010759 (OPi) was developed and synthesized at the MDACC Institute for Applied Cancer Science (IACS) as described (13). Trametinib, cobimetinib, dabrafenib and AZD8055 were obtained from Selleck Chem. Phenformin and metformin were obtained from Sigma-Aldrich. For in vitro treatments, all compounds were dissolved in DMSO. For in vivo treatments, clear suspensions of the compounds were prepared using the following vehicles: OPi: 0.5% methyl cellulose; trametinib, cobimetinib and dabrafenib: 0.5% Hydroxypropylmethylcellulose + 0.2% Tween-80.
Cell biological studies.
Cell proliferation inhibition was determined using Cell Titer Blue (Promega) and IC50 values from proliferation curves were determined using Calcusyn software (Biosoft), as described earlier (7). Cell death was determined by Propidium iodide-cell cycle analysis, and the cytoplasmic histone-associated DNA fragment analysis (Cell Death Detection ELISA Plus, Roche Applied Science) as described before (21). For colony formation assays, 50 cells/well in 24 well plates were treated with OPi in fresh media every three days over a period of one month. Colonies were detected and counted following formaldehyde fixation and trypan blue staining.
Determination of ATP levels.
Cells seeded in 24 well plates were treated with OPi for 24 h, after which the cells were harvested, and ATP levels were determined using the Enliten ATP assay system (Promega), following the manufacturer’s protocol.
Bioenergetics Stress tests.
Real-time oxygen consumption rate (OCR) and extracellular acidification rate were determined by the Seahorse XFe analyzer in 96 well plates as described earlier (7). Data was normalized against cell numbers. For performing the bioenergetics stress test in tumors, we adapted a protocol described recently (22). Briefly, tumors discs of 1 mm thickness and diameter were biopsied from freshly harvested tumor xenografts grown in mice. The discs were placed in the bottom troughs of a Seahorse spheroid plate, and bioenergetics stress test was performed within two h of tumor extraction. Extended incubation times with Oligomycin, FCCP, Antimycin and Rotenone were used for the tumor analysis to compensate for the longer drug uptake times into the tumor tissues versus cell line monolayers.
In vivo xenograft growth studies.
Sub-cutaneous xenograft tumors were generated for SKMEL5, A375, A375-R1 and WM1799 cell lines with 5×106 cells/animal in the right flank of CD1 nude mice. Sub-cutaneous tumors of the MEL624 cell line were generated in NSG mice. Inhibitor treatments were performed by oral gavage for the indicated number of days. Tumor volumes and mice weight were recorded every three days. Animals were excluded if they showed overt toxicity, or lost >15% body-weight. For molecular analysis of inhibitor effects, three mice per group were treated with the inhibitors as above, and tumors were harvested three hours after drug administration on the second or third day of treatment. All animal experiments were approved by the Institutional Animal Care and Use Committee.
Pimonidazole (Hypoxyprobe) incorporation and Immunohistochemistry.
Mice bearing human xenograft tumors were treated with vehicle or OPi q.d. for two days. On day two, the mice were intraperitoneal-injected with 60mg/kg of pimonidazole along with vehicle or OPi treatments. Three hours after this treatment, tumors were harvested and FFPE slides of these tumors were probed with an anti-pimonidazole antibody as described previously (13).
[18F]-fluoroazomycin arabinoside (FAZA) imaging analysis.
For the single dosage study in SKMEL5 tumors, nude mice bearing ≥100mm3 tumors were injected intravenously with [18F]-FAZA, and were imaged after three hours using a pre-clinical PET/CT scanner (Albira Bruker) as described (S. Gammon and colleagues, manuscript under review). On the same day (day 0), the mice were treated with OPi, followed by another treatment the next day (day 1). Three hours following OPi treatment on day 1, mice were injected with [18F]-FAZA, and re-imaged. For the multi-dose response study, A375-R1 tumor bearing mice were injected with [18F]-FAZA and imaged as above. The mice were subsequently treated with OPi on the same day, and the following two days. Three hours following the last treatment, the mice were injected with [18F]-FAZA, and re-imaged. Imaging data were resolved as quantitative tracer retention in tumor tissue (standard uptake value, SUV), and normalized to muscle tissue, and then the log fold change day 1/day 0 calculated for each animal. Successful target engagement would inhibit [18F]-FAZA retention and yield a negative log-fold change. OPi treatments were continued in these mice for a month.
Knockdown analysis with siRNAs.
Transfections with siRNAs were performed in 6 well plates as described previously (21). For protein analysis, the cells were incubated for 48 h, followed by treatments with OPi for 24 h, and protein lysates were prepared. For cell growth analysis, the siRNA-transfected cells were trypsinized after 24h of transfection, seeded in a 96 well plate at a density of 3000 cells/well, treated with OPi and Cell Titer Blue assay was performed after 72 h.
Protein analysis.
Whole cell lysates from cell lines were prepared in RIPA lysis buffer, and protein lysates from tumors were prepared by homogenization of ~50 mg of tumor tissue as previously described (7). The protein lysates were denatured and used for western blotting using standard methods, or for Reverse Phase Protein Array (RPPA) analysis at the MDACC Functional Proteomics Core Facility, and the data was analyzed as described previously (17,21). Antibodies used for western blotting and RPPA are listed at the RPPA core website (23). Protein bands on western blots were quantified using NIH ImageJ software.
Stable isotope tracing studies.
1×106 cells/dish were seeded overnight in 60mm dishes. Prior to initiating the tracing study, the cells were treated with the indicated inhibitors for 12 hours, washed twice with PBS and replenished with RPMI media lacking pyruvate and containing either [U-13C] glucose, or [U-13C] glutamine for glucose and glutamine tracing respectively. The same inhibitors were added to the freshly replenished media, and the cells were harvested at different time points up to 12 h. Metabolites were immediately extracted in cold 50% methanol and were analyzed for 13C enrichment in metabolic intermediates from glycolysis, TCA cycle, and nonessential amino acids as described before (24,25).
Targeted metabolomics analysis.
Cell growth, inhibitor treatments, and metabolite harvests were performed as described above, and subjected to targeted metabolomics using LC-MS analysis to evaluate >200 metabolites associated with energy metabolism, as described previously (26). Normalized data was generated using SIMCA-P (version 12.0, Umetrics, Umeå, Sweden).
Statistical analysis.
Linear regression was used to evaluate the relationship between OPi sensitivity and inhibition of OCR, ECAR and proteins (measured by RPPA). Spearman correlation coefficient was used to assess the correlation between the degree of inhibition of [18F]-FAZA incorporation and tumor growth rate, which is defined as the difference in tumor sizes obtained between two consecutive time points. Hierarchical supervised clustering of RPPA data was performed using Pearson correlation in Gene Cluster 3.0, and heatmaps were generated using Gene Treeview. For cell line/tumor growth studies, cell death assays and RPPA-derived protein levels, T-tests were used for determining statistically significant differences (p<0.05 unless stated otherwise) between inhibitor treated and mock/vehicle-treated conditions. Where necessary, significant differences from mock/vehicle treatments or between treatments were designated with asterisk (*), hash (#), or plus (+) symbols for p<0.05, p<0.01 and p<0.001 respectively.
RESULTS
OPi potently inhibits tumor OxPhos and induces regression of intrinsic and acquired MAPKi-resistant, BRAF-mutant human melanoma xenografts
We tested the in vivo growth inhibitory effects of OPi in human melanoma xenografts from BRAF-mutant human melanoma cell lines with acquired (A375-R1) or intrinsic (SKMEL5) resistance to MAPK inhibitors (MAPKi); xenografts were treated in parallel with the FDA-approved MEK inhibitor trametinib (MEKi) for comparison. We previously derived and characterized A375-R1 as a MAPKi-resistant, high-OxPhos sub-clone of the MAPKi sensitive, low-OxPhos A375 cell line (7). Consistent with our previous in vitro studies (7), MEKi treatment markedly regressed parental A375 xenografts, but no significant inhibition was seen in A375-R1 (Figs. 1A and 1B). In contrast, single-agent OPi caused marked tumor regression of A375-R1 xenografts. While OPi also inhibited the growth of the parental low-OxPhos A375, it did not induce tumor regression. Induction of tumor regression in A375-R1 but not A375 by OPi was confirmed by comparison of percentage changes in individual tumor growth over time versus vehicle at the beginning of treatment (Figs. S1A and S1B). These results reflect a higher anti-tumor activity in the high OxPhos, MAPKi-resistant A375-R1. OPi treatment also regressed xenografts of the BRAF-mutant human melanoma cell line SKMEL5, which has high OxPhos and intrinsic resistance to MAPKi (Fig. 1C) (7).
Figure 1. In vivo anti-tumor activity of OPi.
BRAF-mutant human melanoma cell lines A375, A375-R1, and SKMEL5 were implanted subcutaneously in nude mice. Mice (ten/group) were treated daily with Vehicle, 1 mpk MEKi or 10 mpk OPi. (A) Growth of low-OxPhos A375 xenografts. (B) Growth of high OxPhos A375-R1 (MAPKi acquired resistance). (C) Growth of high OxPhos SKMEL5 (MAPKi intrinsic resistance). Error bars represent standard error (SEM). (D) Bioenergetics stress tests of A375 and A375-R1 cell lines following Vehicle or OPi treatment for 12 h. Basal (“B”), oligomycin-inhibited (“O”), FCCP-activated (“F”) and Antimycin/Rotenone inhibited (“A&R”) OCR levels are indicated. (E) Bioenergetics stress tests of biopsied tumor disks of A375 and A375-R1 xenografts from mice treated with Vehicle or OPi for 48 h. Data for D and E is representative of quadruple replicates; error bars, standard deviation (SD). (F) IHC staining for pimonidazole of A375-R1 tumors harvested from mice following treatment with Vehicle or OPi for 48 h. (G) Subcutaneous xenografts of A375, A375-R1, and SKMEL5 were harvested after treatment with Vehicle, MEKi, or OPi for two days. Protein lysates (3 tumors per group) were analyzed by RPPA. Supervised clustering of median-centered protein levels with significant (p<0.05) changes in expression after either MEKi or OPi treatment versus Vehicle was performed and represented as a heatmap, with the scale showing fold-changes.
Bioenergetics stress tests performed with the Seahorse XF Analyzer showed that OPi potently inhibited basal and maximal OCR (oxygen consumption rate, a surrogate for OxPhos) at a low nanomolar dose in all three cell lines in vitro (Fig. 1D and Fig. S1E). To determine if OPi inhibited OxPhos in vivo, A375 and A375-R1 xenografts were harvested after two days of treatment, and the bioenergetics stress test was performed on 1 mm tumor discs. The results confirmed that A375-R1 vehicle-treated xenografts had higher OCR levels than A375, and that OPi potently inhibited the OCR (Fig. 1E). In vivo inhibition of OxPhos by OPi was confirmed indirectly by measurement of IHC staining for pimonidazole, which binds to thiol groups of proteins in hypoxic tissues. OPi treatment decreased pimonidazole IHC staining of the A375-R1 tumors, an effect implying decreased oxygen utilization by tumor cells, resulting in abolition of hypoxia in the tumor tissue (Fig. 1F) (13).
To evaluate the effects of OPi on oncogenic protein signaling pathways in vivo, we performed reverse phase protein array (RPPA) analysis on protein lysates generated from A375, A375-R1 and SKMEL5 xenografts after treatment for two days with vehicle, MEKi, or OPi. Visualization of the most statistically significant treatment-induced changes in protein levels showed that MEKi potently decreased the activation of MAPK and mTOR signaling pathway proteins in the MAPKi-sensitive A375, but had a smaller effect in the MAPKi-resistant A375-R1 or SKMEL5 (Fig. 1G). In contrast, OPi potently inhibited both MAPK and mTOR signaling, and cell cycle regulatory proteins in A375-R1 and SKMEL5, but only mildly in A375. It also increased the levels of cleaved caspase 7 in A375-R1 and SKMEL5 (Fig. 1G).
Growth inhibition and cell death by OPi are not augmented by combined treatment with BRAF or MEK inhibitors in vitro or in vivo
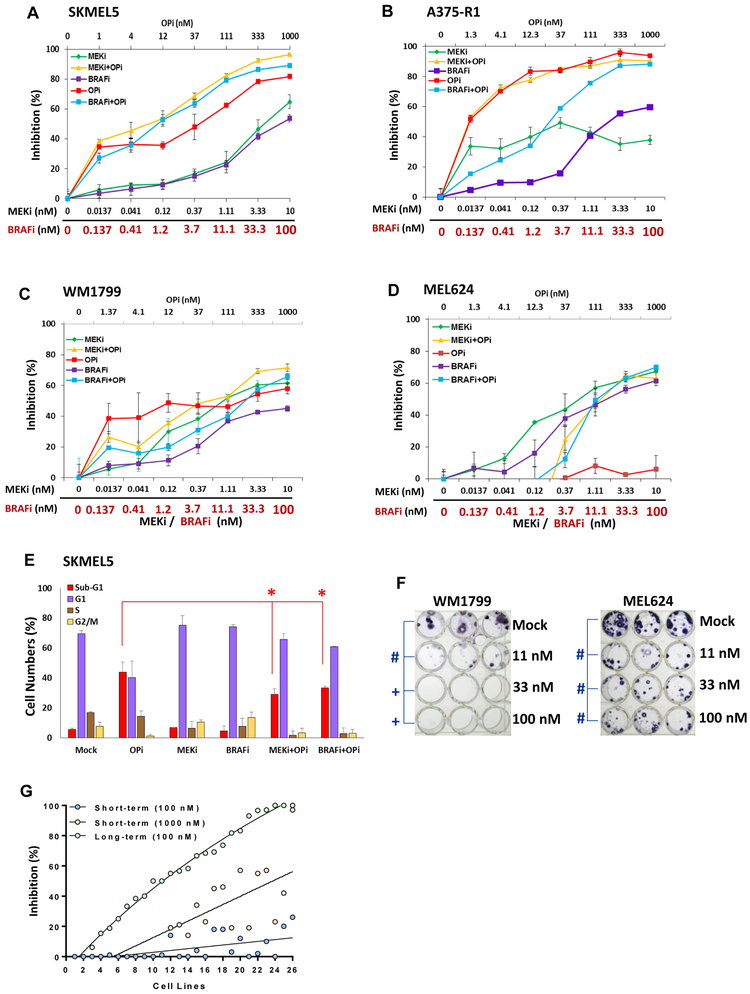
Earlier studies showed that combining BRAF inhibitors with the biguanide antidiabetic agents metformin or phenformin improved melanoma growth inhibition (27,28). OPi inhibited the growth of the high OxPhos SKMEL5 in vitro more potently than either metformin or phenformin (Fig. S2A). In contrast to those earlier studies, neither BRAFi nor MEKi augmented the in vitro growth inhibition achieved by OPi in SKMEL5 (Fig. 2A) or A375-R1 (Fig. 2B) at 72 hours. Further, OPi did not meaningfully improve the efficacy of BRAFi or MEKi in the MAPKi-sensitive A375 cells (Fig. S2B). Two additional intrinsic MAPKi-resistant, high OxPhos BRAF-mutant melanoma cell lines (WM1799 and MEL624) demonstrated lower sensitivity to OPi (Figs. 2C and 2D). Combined treatment with either BRAFi or MEKi again did not meaningfully augment the growth inhibition achieved by OPi in these cell lines (Figs. 2C and 2D). OPi also did not inhibit the growth of normal melanocytes or skin fibroblasts (Fig. S2C and S2D).
Figure 2. Effects of combining OPi with MAPK inhibitors (MAPKi) in vitro.
Inhibition of cell proliferation was determined after 72 h treatment with indicated concentrations of BRAFi, MEKi, OPi, and their combinations (OPi + BRAFi; OPi + MEKi) versus mock (dmso). Testing was performed on the MAPKi-resistant, BRAF-mutant (A) SKMEL5, (B) A375-R1, (C) WM1799, and (D) MEL624 melanoma cell lines. Bars represent average of triplicates; error bars, SD. (E) Propidium Iodide-cell cycle analysis of the SKMEL5 cell line following 72 h treatment with BRAFi, MEKi, OPi, or their combinations. The percentage of cells in each phase of the cell cycle, as well as dead cells (sub-G1), are indicated. Bars represent average of triplicates; error bars, SD. Significant differences by T tests are indicated by asterisks (p<0.05). (F) WM1799 and MEL624 cells were treated with mock or OPi at the doses shown for 30 days; media/drug was changed every 72 h. Colonies were stained with crystal violet. Significant differences of p<0.01 are indicated by hash (#), and p<0.001 by plus (+) symbols. (G) The short-term (72 h) cell proliferation and the long-term (30 days) colony formation assays in OPi-treated cells were performed on melanoma patient-derived cell lines. Percentages of short-term proliferation inhibition by 100 nM and 1000 nM OPi concentrations, and long-term colony formation inhibition by 100 nM were plotted in a curve fit plot, supervised with cell lines in ascending order of sensitivity (% inhibition) in the colony formation assay; data was derived from triplicate treatments.
FACS-based cell cycle analysis performed after 72 h treatment showed that single-agent OPi induced cell death (increase of sub-G1) in SKMEL5 (Fig. 2E) and A375-R1 (Fig. S3A), which was not increased by combined treatment with MEKi or BRAFi. In WM1799 and MEL624 cells, OPi caused G1 arrest but not cell death, and this effect was not augmented by MEKi (Figs. S3B and S3C). An ELISA-based assay that measures accumulation of cytoplasmic histone H3 as a marker of cell death confirmed the differential effects on cell killing in the cell lines (Figs. S3D and S3E).
To determine long-term effects of OPi treatment, we performed a two-dimensional colony formation assay with continuous treatment of the WM1799 and MEL624 cell lines with OPi (changed every three days) for one month. In contrast to the minimal effects observed with 72 h treatment, long-term exposure to OPi completely inhibited colony formation in WM1799 at low nanomolar concentrations, and significantly inhibited MEL624 (Fig. 2F). The short-term 72 h cell growth inhibition assays and the long-term colony formation assays were performed in a larger panel of patient-derived melanoma cell lines reported earlier (20) (Table S1). The results of the long-term colony formation assay were organized into a curve fit plot in an ascending order of inhibition of colony formation. The short-term cell growth inhibition data from 100 and 1000 nM doses of OPi were also included for the same cell lines. The results show that 100 nM OPi induced potent inhibition of long-term colony formation in many of these cell lines. While sensitivity to OPi in the short term 72 hours assay generally trended with sensitivity in the long-term colony formation assay, most cell lines showed a much lower degree of short-term growth inhibition (<20% and <50% with 100nM and 1000nM of OPi respectively) (Fig. 2G). A linear regression analysis was performed to compare OPi sensitivity of melanoma cell lines versus their OxPhos Index, an OxPhos gene signature that we recently reported (15). The results showed that sensitivity to OPi had a non-significant association with elevated OxPhos gene expression (Fig. S2E).
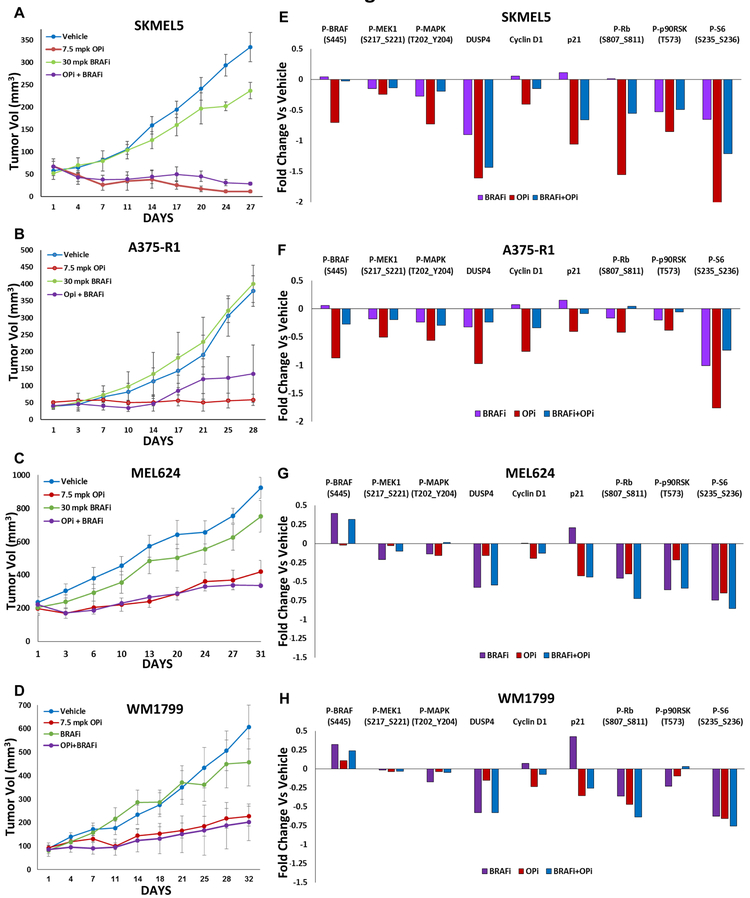
Although combined inhibition of OxPhos and MAPK activities did not demonstrate synergy in vitro, we hypothesized that more favorable combinatorial effects might be seen in vivo. Thus, OPi was evaluated as a single-agent and in combination with dabrafenib (BRAFi) and MEKi in vivo. Initial experiments in non-tumor bearing mice showed that while all single agents were well tolerated by mice, concurrent treatment of OPi and MEKi caused ≥15% weight loss at the doses tested (Fig. S4A). BRAFi at its optimal dose of 30 mpk was tolerated in combination with OPi dosed at 7.5 mpk (25% dose reduction versus single agent dosing; Fig. S4A). Thus, subsequent in vivo testing in MAPKi-resistant xenografts was performed with OPi, BRAFi, and OPi + BRAFi. Mice with subcutaneous xenografts of SKMEL5, A375-R1, WM1799 and MEL624 were treated for up to four weeks. All four models demonstrated in vivo resistance to BRAFi (Figs. 3A-D). The lower dose regimen of single-agent OPi produced tumor regression of SKMEL5 xenografts and stasis of A375-R1 xenografts (Figs 3A and 3B). Notably, phenformin did not potently inhibit SKMEL5 tumor growth at a concentration of 100 mpk, although the growth inhibition was significant compared to vehicle (Fig. S4B). Similar results were obtained with the A375-R1 model, in which phenformin induced a weak, but significant inhibition of tumor growth (Fig. S4D). Evaluation of OCR levels in tumors from mice treated with vehicle or phenformin showed that although phenformin inhibited tumor OCR (Fig. S4E) at the concentration tested, it was not as potent inhibition as was observed with OPi (Fig. 1E).
Figure 3. In vivo tumor growth inhibition and signaling effects of OPi with BRAFi.
Tumor xenografts of the indicated cell lines were generated. Mice with palpable tumors (eight/group) were treated daily with Vehicle, 30 mpk BRAFi, 7.5 mpk OPi or OPi + BRAFi. Tumor volumes were recorded every three days. Effects on tumor growth are shown for xenografts of (A) SKMEL5, (B) A375-R1, (C) MEL624, and (D) WM1799. Error bars represent standard error (SEM). (E-H) Tumors were harvested from mice after the above treatments for two days and processed for RPPA analysis. Treatment-induced fold changes in the MAPK and mTOR pathway proteins and cell cycle regulatory proteins identified earlier (Fig. 1G) as the most significantly altered (p<0.01 by T tests) were plotted as bar graphs for each cell line, shown in panels E-H. Data represents average of biological triplicates.
Despite minimal anti-proliferation activity in the 72 h short-term in vitro assays, OPi treatment caused significant growth inhibition of the WM1799 and MEL624 xenografts versus vehicle or BRAFi (Figs 3C and 3D), recapitulating the inhibition of colony formation observed in vitro with the long-term drug exposure. Consistent with the in vitro studies, combined treatment with BRAFi did not increase the efficacy of OPi in any of the models in vivo (Figs. 3A-D).
MAPK, mTOR and cell cycle regulatory proteins in the xenografts after two days of treatment were analyzed by RPPA, as a time course demonstrated the most pronounced effects of OPi after 24 – 48 h of treatment (Figs. S5A-S5H). As observed in our initial analysis of OPi-induced protein changes (Fig. 1G), OPi caused potent inhibition of MAPK and mTOR pathways in SKMEL5 and A375-R1 xenografts. Less pronounced inhibition was observed in WM1799 and MEL624 xenografts. Cell cycle regulatory proteins, cyclin D1 and phosphorylated Rb, were also inhibited to a greater degree in the SKMEL5 and A375-R1 tumors compared to WM1799 and MEL624. Combination treatment with BRAFi interestingly did not improve upon the inhibition of P-MAPK or P-S6 by OPi in SKMEL5 and A375-R1. (Figs. 3E-H).
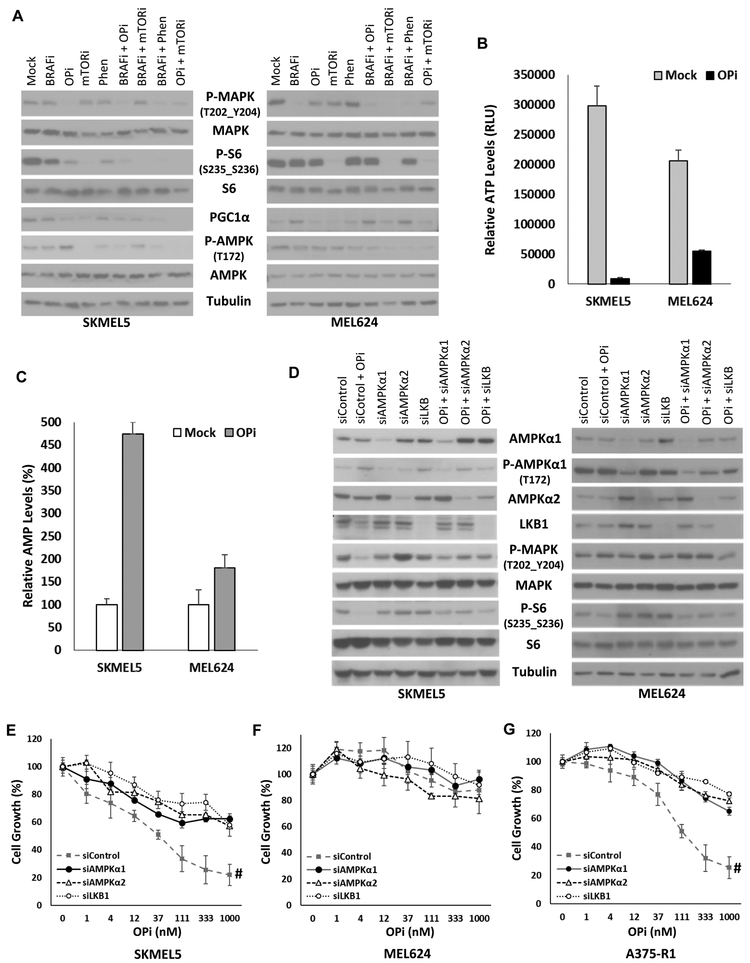
Melanoma growth inhibition by OPi is dependent on its ability to inhibit MAPK activity through the LKB1-AMPK axis.
To further evaluate the differential sensitivity observed in the high OxPhos, de novo MAPKi-resistant cell lines SKMEL5 and MEL624, the in vitro molecular effects of single agent OPi and its combination with BRAFi were evaluated by Western blotting. BRAFi treatment inhibited P-MAPK expression in both cell lines (Fig. 4A). Interestingly, as was detected in xenografts by RPPA, OPi potently inhibited P-MAPK in SKMEL5, but it had a lesser effect on MEL624. In SKMEL5, OPi also potently inhibited P-S6, a surrogate and downstream effector of mTOR activity, and decreased the expression of PGC1α, which we earlier showed is regulated by mTOR kinase activity (7). Phenformin (Phen) and AZD8055, an mTOR kinase inhibitor, also exhibited similar effects albeit with different potency, suggesting that all three agents may alter common molecular determinants. Combinations of these agents with BRAFi or MEKi showed marginally different effects between the two cell lines, except in the levels of P-S6, which were completely inhibited by the combinations in SKMEL5 (Fig. 4A).
Figure 4. Role of AMPK in signaling and growth inhibitory effects of OPi.
(A) SKMEL5 and MEL624 cells were treated in vitro for 24 h with the following inhibitors: BRAFi, 10 nM; OPi, 100nM; mTORi (AZD8055), 250 nM; Phen (Phenformin), 10 μM; and their combinations. Western blotting was performed on whole cell lysates using the antibodies shown. (B) SKMEL5 and MEL624 cells were treated with 100 nM OPi for 24 h, and relative ATP levels, measured as relative luciferase units (RLU) were determined from cell lysates. The data is average of triplicate measurements; error bars, SD. (C) AMP levels were determined in similarly treated cells using targeted LC-MS analysis. Data is represented as percent changes in normalized AMP levels from triplicate measurements; error bars, SD. (D) SKMEL5 and MEL624 cells were transfected with siRNAs against AMPKα1, AMPKα2, or LKB1 or Risc-free control siRNA (siControl) and incubated for 48 h. Cells were then treated with OPi or Vehicle, and harvested after 24 h. Western blotting was performed with the indicated antibodies. (E-G) Effects of AMPKα1, AMPKα2, and LKB1 knockdown on growth inhibition by OPi in SKMEL5 (E), MEL624 (F) and A375-R1 (G). Data were plotted after adjusting the no drug-treatment cell numbers for each siRNA transfection to 100%. Results are average of triplicates; error bars, SD. Significant differences (p<0.01) from siControl treatments are indicated by hashes (#).
ATP deficit and a consequent AMP accumulation caused by OxPhos inhibition can inhibit mTOR and MAPK activity via LKB1/AMPK (29,30). We found that OPi treatment almost completely depleted ATP levels in SKMEL5, but to a lesser extent in MEL624 (Fig. 4B). Consequently, AMP levels increased in both cell lines, but with a significantly larger increase observed in SKMEL5 versus MEL624 (Fig. 4C). Similar results were observed in the A375-R1 compared to A375 (Fig. S6A and S6B). To determine if the OPi-induced AMP differential between SKMEL5 and MEL624 could influence its uniquely different effects on mTOR and MAPK pathways, we performed siRNA knockdowns of the AMP sensor proteins LKB and AMPK in these cell lines, followed by western blotting. OPi treatment increased the activating phosphorylation of AMPKα. Compared to OPi + control siRNA, knockdown of AMPKα1, AMPKα2 or LKB1 blunted the inhibition of P-MAPK and P-S6 by OPi in SKMEL5, but not MEL624 (Fig. 4D). As basal levels of P-MAPK and P-S6 were increased by the respective knockdowns, we quantified their band intensities and plotted the percentage of ratios of OPi+siRNA against siRNA treatments alone. The results showed that compared to the control siRNA, knockdown of each of the siRNAs blunted the inhibition of P-MAPK and P-S6 at varying levels in SKMEL5, but not MEL624 (Fig. S6C and S6D). These results suggest that mTOR and MAPK pathway inhibition by OPi is dependent upon the AMP-titer, and occurs through the LKB/AMPK axis. To determine if AMPK and LKB1 knockdown also alters the growth inhibitory effect of OPi in these cell lines, we seeded cells with and without AMPKα1, AMPKα2 and LKB1 knockdown in 96 well plates, and performed a growth inhibition assay for 72 h. Knockdown of each of these genes significantly diminished the growth inhibitory effect of OPi in SKMEL5, but not in MEL624 (Figs. 4E and 4F). Knockdown of AMPKα1, AMPKα2 and LKB1 also reduced the efficacy of OPi in the A375-R1 (Fig. 4G). These results suggest that cell growth inhibition by OPi may in part be dependent on LKB1/AMPK signaling.
OPi increases glycolytic metabolism, decreases TCA cycle metabolism, and inhibits cellular building blocks in melanoma cells.
To determine if differential sensitivity to OPi is associated with dissimilar utilization of the main cellular energy sources and metabolic pathways, we performed 13C isotope tracing using GC-MS in the A375, A375-R1 and SKMEL5 cells grown in media containing [U-13C]-labeled glucose or glutamine. The [U-13C]-glucose tracing for SKMEL5 showed that single agent OPi did not alter glucose labeling of glycolytic intermediates, but it significantly decreased labeling of TCA cycle intermediates, and aspartic acid (Asp) (Fig. 5A). Summarized results of the [U-13C]-glucose tracing studies identified increased lactate labeling from glucose with Vehicle treatment in the low OxPhos A375 cells compared to the high OxPhos A375-R1 and SKMEL5 cells, and that BRAFi inhibited this labeling. (Fig. 5B). OPi increased labeling of lactate only in the high OxPhos cells (Fig. 5B).
Figure 5. Metabolic effects of OPi.
(A) [U-13C]-glucose labeling of Glycolysis and TCA cycle intermediates in SKMEL5 cells treated with the indicated inhibitors (shown adjacent to 3-PG). The metabolites in which the incorporated 13C carbons were measured by GC-MS, are indicated in red. These are 3-PG (3-phospho glycerate), PYR (pyruvate), LAC (lactate), CA (citrate), MA (malate), and aspartate (Asp). The color intensities of the 13C-glucose-derived carbon atoms in each of these metabolites represent the percentage ranges of incorporation of these carbons, as shown in the box labeled “13C incorporation (%)”. (B) Percentage-range incorporation of 13C-glucose-derived carbons into lactate in A375, A375-R1 and SKMEL5 cells treated with the indicated inhibitors. (C) [U-13C]-glutamine labeling of TCA cycle intermediates in SKMEL5 cells treated with the indicated inhibitors (shown adjacent to 3-PG). Results are average of triplicates. (D) Percentage-range incorporation of 13C-glutamine-derived carbons from glutamine to malate in A375, A375-R1 and SKMEL5 cells treated with the indicated inhibitors. (E) Metabolites were extracted from SKMEL5 cells treated with the indicated inhibitors or mock for 12 h, and targeted LC-MS analysis was performed. Significant treatment-induced alterations (fold changes compared to mock) in nucleotide building blocks were plotted as average of triplicates. For all the above data, asterisks (*) indicate p<0.05, hashes (#) indicate p<0.01, and plus (+) indicate p<0.001 by T tests.
In the [U-13C]-glutamine tracing of SKMEL5, the TCA cycle intermediates and Asp were significantly inhibited by single agent OPi (Fig. 5C). Summarized results of [U-13C]-glutamine tracing showed that glutamine labeling of the TCA cycle was lower in A375 compared to the A375-R1 and SKMEL5 with Vehicle treatment (Fig 5D). BRAFi treatment did not alter glutamine uptake in the TCA cycle, while OPi (either as a single agent or in combination with BRAFi) significantly inhibited it (Fig. 5D). Metabolite profiling using LC-MS analysis showed that several nucleotides and amino acids derived from glucose and glutamine were depleted by OPi treatment (Fig. 5E and Fig. S6E).
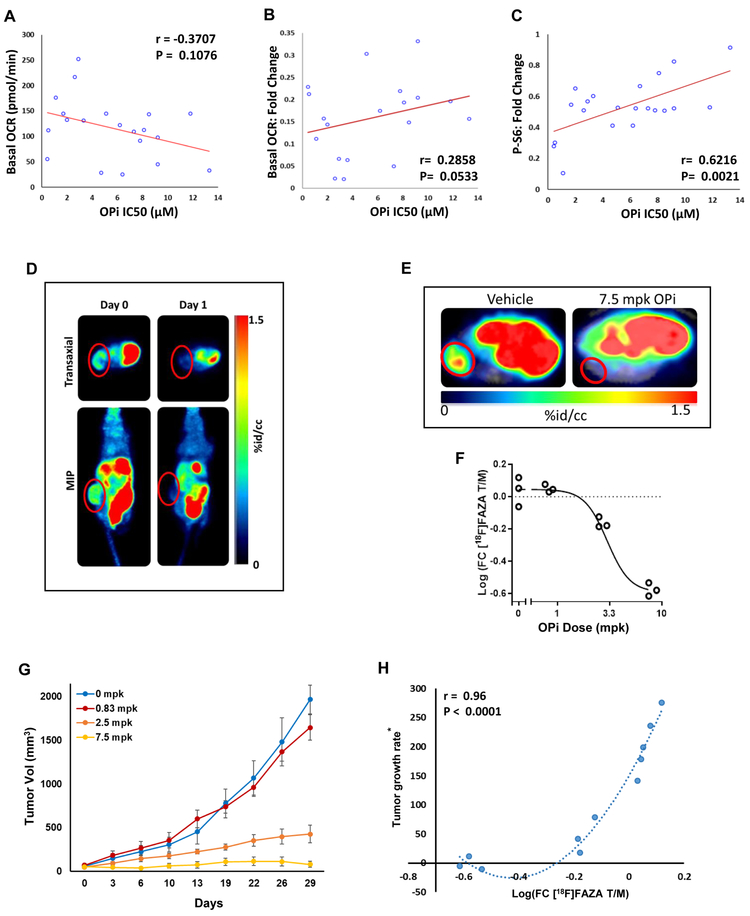
Inhibition of Phospho-S6 levels and [18F]-FAZA retention correlate with efficacy of OPi.
Our results indicated that inhibition of OCR, P-S6, P-MAPK, and cell cycle regulators are molecular effects of OxPhos inhibition by OPi in MAPKi-resistant melanomas. To evaluate if these effects could potentially serve as predictors of anti-melanoma efficacy of OPi, we performed linear regression analysis comparing OPi sensitivity (IC50 for in vitro growth inhibition at 72 h) with the above features in a large number of established human melanoma cell lines (Table S2). Sensitivity to OPi showed non-significant trends for basal (r= −0.37, p=0.107; Fig. 6A) and maximal cellular OCR levels (r= −0.22; p=0.34; Fig. S7A) of the cell lines. Treatment with 100 nM OPi for 12 hours caused potent inhibition of OCR across all cell lines tested (Fig. S7B); a near-significant correlation of sensitivity with treatment-induced fold changes in OCR (r=0.28, p=0.053) (Fig. 6B) was observed. Non-significant trends were observed with basal and OPi-treatment induced ECAR levels (Fig. S7C and S7D).
Figure 6. Correlates of efficacy of OPi.
(A) Scatter plot of linear regression analysis comparing basal oxygen consumption rate (OCR) levels with in vitro sensitivity (IC50) to 100 nM OPi for 12 h in twenty human melanoma cell lines. (B) Similar scatter plot as in A, but comparing fold-changes in OCR with IC50 values of the same cell lines. (C) Linear regression analysis comparing the OPi-induced fold-changes in phosphorylated S6 (P-S6) protein with IC50. (D) [18F]-FAZA PET-CT images of a mouse bearing sub-cutaneous SKMEL5 tumor. Top panels show trans-axial images of the abdomen and bottom panels show whole body maximal intensity projection (MIP) images prior to treatment on day 0 and post-treatment with 10 mpk OPi on day 1. [18F]-FAZA retention is represented as percent injected dose per cubic centimeter (%id/cc). (E) PET-CT images of [18F]-FAZA retention in A375-R1 tumors treated with Vehicle or 7.5 mpk of OPi for two days. [18F]-FAZA retention is represented as percent injected dose per cubic centimeter (%id/cc). (F) The quantified data from (D) was plotted with Y-axis representing log fold change [FC] in tumor [T] versus muscle tissue [M]; data is representative of triplicates. (G) A375-R1 tumor growth in the above mice treated with vehicle or the indicated doses of OPi. Error bars represent standard error (SEM). (H) Spearman correlation analysis showing the relationship between the inhibition of [18F]-FAZA incorporation and change of tumor growth from the above experiment. Tumor growth rate* on the y-axis represents average change in tumor size calculated as the average of the differences of the tumor sizes collected between two consecutive time points.
Sensitivity data (OPi IC50 for growth inhibition) were then compared to quantitative protein levels (from RPPA) in the cell lines at baseline and after treatment with 100 nM OPi for 24 h. Among all proteins analyzed, the degree of P-S6 inhibition (fold change compared to mock) showed the highest correlation with sensitivity to OPi (r=0.621, p=0.002) (Figs 6C). The basal levels of P-S6 in the absence of OPi treatment showed a similar but non-significant trend (r=0.305, p=0.104) (Fig. S7E). These results suggest that degree of P-S6 inhibition is an early marker/predictor of sensitivity to OPi. While a recent study suggested that mutations in the SWI/SNF proteins SMARCA4 and ARID1A could predict sensitivity to OPi (14), OCR inhibition and proliferation inhibition data from six melanoma cell lines with mutations in these genes did not show a clear association of these mutations with either OxPhos Index or sensitivity to OPi (Table S3).
Methods that would allow for non-invasive assessment of target engagement (pharmaco-dynamic biomarker) and response (predictive biomarker) could facilitate the clinical evaluation and development of OPi. FAZA-PET is an innovative imaging modality that uses [18F]-labeled FAZA (fluoroazomycin arabinoside), a redox/hypoxia marker to assess tumor redox state in real time, as has been validated recently as a quantitative pharmaco-dynamic biomarker of single dose OPi in vivo (S. Gammon and colleagues, manuscript under review). Mice bearing sub-cutaneous xenografts of the high OxPhos SKMEL5 cells were injected with [18F]-FAZA and baseline whole body PET-CT imaging was performed to visualize [18F]-FAZA localization. Mice were then treated with OPi daily for two days, followed by [18F]-FAZA injection and re-imaging. A robust [18F]-FAZA signal was detected in the SKMEL5 xenografts at baseline, which was completely abrogated after treatment with OPi (Fig. 6D), confirming [18F]-FAZA as a pharmaco-dynamic biomarker of target inhibition by OPi in MAPKi-resistant melanomas.
Next, we performed an in vivo PET-CT imaging study to determine if changes in [18F]-FAZA retention correlated with response to OPi in MAPKi-resistant melanoma tumors. Mice bearing sub-cutaneous xenografts of the A375-R1 cell line were treated daily with three-fold increasing concentrations of OPi or with Vehicle control. After OPi treatment on day two, mice were injected with [18F]-FAZA and imaged by PET-CT (Fig. 6E). OPi-induced decrease of [18F]-FAZA incorporation into tumors was plotted as fold-change in [18F]-FAZA tumor/muscle ratios (Fig. 6F). OPi treatment was continued for one month, and tumor growth inhibition by each treatment regimen was determined (Fig. 6G). Spearman correlation coefficient analysis showed a significant correlation (r=0.96, p<0.0001) between the degree of inhibition of [18F]-FAZA retention and tumor growth rate over the subsequent month (Fig. 6H). Thus, [18F]-FAZA PET may serve as a non-invasive predictive biomarker of response to OPi in MAPKi-resistant melanoma tumors.
Discussion
Earlier studies from our group and others have shown that a significant subset of melanomas generate resistance to MAPKi by inducing mitochondrial OxPhos, which promotes cellular rigor and counteracts apoptosis (6-10). Our experiments here show that IACS-010759 (OPi), a novel OxPhos inhibitor that is currently being evaluated in early-phase clinical trials, inhibited the growth of multiple MAPKi-resistant, BRAF-mutant melanoma xenograft models in vivo at well-tolerated doses. Unexpectedly, single-agent OPi achieved tumor regression in some of these models. However, its activity was not augmented by combined treatment with BRAF inhibitors. Overall, our results suggest that OxPhos inhibition may be an important new therapeutic strategy in melanoma patients with resistance to MAPK pathway inhibitors. These results also support our recent finding that low OxPhos melanomas that do not originally respond to OPi could do so when they acquire a high OxPhos phenotype, in response to MAPKi or as an adaptation to microenvironment of the brain (15).
OPi inhibited mTOR activity via LKB1-AMPK pathway, an expected effect resulting from the increased AMP: ATP ratio induced by OxPhos inhibition (29). Unexpectedly, OPi treatment also potently inhibited MAPK activity in melanomas in which it induced short-term growth inhibition and in vivo tumor regression. The OPi-induced differential in AMP levels between the short-term sensitive and resistant cells, as well as functional knockdown analyses, suggest that this effect may also be mediated by LKB1-AMPK. As re-activation of both MAPK and mTOR have been implicated in previous studies as critical markers of resistance to BRAF and MEK inhibitors, these signaling effects could explain the potent activity observed with single-agent OPi in the MAPKi-resistant melanomas. Our metabolite profiling analysis showed that OPi inhibited glucose and glutamine utilization by the TCA cycle, and decreased the levels of nucleotide and amino acid building blocks. These results suggest that OxPhos is a requisite for cell growth and division of high OxPhos melanomas, although aerobic glycolysis has earlier been attributed to these effects in all cancers.
The results from our tumor growth inhibition and cell growth inhibition studies in a large number of melanoma lines with known OxPhos status show a trend of improved responsiveness of high OxPhos melanomas to OPi, although a significant selectivity of response based on this marker was not observed. However, analysis of OPi-treatment induced molecular effects showed that inhibition of P-S6 by OPi could be a significant biomarker of response to benefit from this agent. P-S6 can be assessed robustly in tissue samples by IHC, and thus it is feasible to assess in even small tumor biopsies. As changes in P-S6 have been implicated in response and resistance to targeted therapies recurrently in melanoma (7,31-34), the development of non-invasive methods of assessment could also have significant value for drug development and patient management. P-MAPK did not show a similarly significant correlation in the large cell line population, as P-MAPK inhibition only occurred in the highly sensitive melanomas that underwent tumor regression. Larger studies should be performed to determine if P-MAPK inhibition by OPi could identify the best responders.
Identifying non-invasive predictive biomarkers that correlate with efficacy would especially facilitate the clinical development of OPi and other OxPhos inhibitors, as the therapeutic index of such agents may be narrow. Just as FDG-PET has value for assessing agents that inhibit glucose uptake in tumors, [18F]-FAZA-PET may have utility for evaluating OxPhos inhibition. Preliminary analysis in the OPi-sensitive SKMEL5 xenograft model showed that [18F]-FAZA retention is completely inhibited by OPi. Further, the A375-R1 xenograft model showed that a decrease in [18F]-FAZA retention after only two days of treatment correlated with response over the course of treatment for one month with OPi, and the effect was dose-responsive. In this context, [18F]-FAZA PET imaging is currently undergoing clinical testing (IRB-MDACC#2016-0847), and further experiments are ongoing to evaluate changes in [18F]-FAZA retention as both a pharmaco-dynamic biomarker and a predictor of efficacy. Additional studies will need to be performed to determine if changes in [18F]-FAZA-PET are predictive in a larger sampling of tumors, and in other tumor types.
While our experiments have focused on targeted therapy-resistant models, assessing immune effects may also be relevant in the appropriate design of clinical trials with OPi. Preliminary experiments in non-tumor bearing immune-competent mice did not demonstrate signs of overt toxicity on white blood cells, although a small but significant decrease in white blood cell components was observed one day after treatment with OPi (Fig. S8). This result is currently being evaluated in tumor-infiltrating immune cells in immune-competent mice, and will be evaluated in the context of the ongoing phase I clinical trials as well. Notably, combinations of OPi with MEKi or BRAFi+MEKi were intolerable in mice (Fig. S4A), which prevented the evaluation of triplet therapy; future studies will assess if OPi is also active in patient-derived xenografts from patients that progressed on BRAFi+MEKi therapy (35). Efficacy of OPi will also be interrogated in MAPKi-resistant melanomas without BRAF mutations.
In conclusion, these studies demonstrate that direct OxPhos inhibition with OPi has significant anti-tumor efficacy at well-tolerated doses in high OxPhos MAPKi-resistant melanomas, and strongly support the rationale to evaluate the safety and efficacy of this novel agent in melanoma patients.
Supplementary Material
Translational Relevance.
There is an unmet need for novel therapeutic strategies that are effective in MAPK targeted therapy-resistant Braf-mutant melanoma. While previous studies have shown that 30-50% of melanomas with primary and acquired resistance to MAPKi are characterized metabolically by increased OxPhos, the therapeutic potential of direct OxPhos inhibition in this setting is unknown. We show that single-agent treatment with IACS-010759 (OPi), a potent OxPhos inhibitor in early-phase clinical trials, induced tumor regression or growth inhibition in MAPKi-resistant human melanoma xenografts. Tumor regression correlated with inhibition of MAPK and mTOR pathways, mediated by activation of AMPK. Early on-treatment changes in [18F]-FAZA retention in tumors detected by PET-CT imaging correlated with anti-tumor efficacy, suggesting that this imaging modality is a potential non-invasive strategy to evaluate target inhibition and predict efficacy of OxPhos inhibition in patients.
Acknowledgement:
YNVG is supported by Melanoma Research Alliance. MAD is supported by the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation, philanthropic contributions to the Melanoma Moon Shots Program of the UT MD Anderson Cancer Center, AIM at Melanoma Foundation, NIH/NCI (2T32CA009666-21), and the Cancer Prevention Research Institute of Texas (CPRIT) (RP170401). MAD, RD and YNVG are supported by CPRIT IIRA grant (RP160183). SG and DPW were supported by a NIH/NCI Molecular Imaging Center grant (P50 CA094056). GMF is supported by the Caroline Ross Fellowship of MDACC, the Schissler Foundation Fellowship of UT-Health/MDACC, and the NIH National Center for Advancing Translational Sciences (TL1TR000369 and UL1TR000371). RPPA and SAIF core facilities at MDACC are supported by NCI #CA16672. RPPA core facility at MDACC is supported by NCI #CA16672. Chunyu Xu and Victoria Thiele provided technical support.
Financial Support:
Melanoma Research Alliance Young Investigator Award to YNVG; Miriam and Sheldon G. Adelson Medical Research Foundation to MAD; Cancer Prevention Research Institute of Texas (CPRIT) grant to MAD, RD and YNVG (RP160183); NIH/NCI Molecular Imaging Center grant (P50 CA094056) to SG and DPW; NIH 2T32CA009666-21 to MAD
Footnotes
Conflict of Interest Disclosure: Y.N. Vashisht Gopal has a research grant from Calithera Biosciences. M. Tetzlaff is on the advisory board of Myriad Genetics, Seattle Genetics and Novartis. M.A. Davies is a consultant to Nanostring Technologies, and on advisory boards for Novartis, Bristol Myers Squibb, GlaxoSmithKline, Roche-Genentech, Sanofi-Aventis, Vaccinex, and Array Biopharma; and has institutional research grants from Astrazeneca, GlaxoSmithkline, Roche-Genentech, Sanofi-Aventis, Merck, Oncothyreon, and Myriad Genetics. UT M.D. Anderson Cancer Center has a patent on IACS-010759 (OPi).
References
- 1.Larkin J, Ascierto PA, Dreno B, Atkinson V, Liszkay G, Maio M, et al. Combined vemurafenib and cobimetinib in BRAF-mutated melanoma. The New England journal of medicine 2014;371:1867–76 [DOI] [PubMed] [Google Scholar]
- 2.Long GV, Stroyakovskiy D, Gogas H, Levchenko E, de Braud F, Larkin J, et al. Combined BRAF and MEK inhibition versus BRAF inhibition alone in melanoma. The New England journal of medicine 2014;371:1877–88 [DOI] [PubMed] [Google Scholar]
- 3.Robert C, Karaszewska B, Schachter J, Rutkowski P, Mackiewicz A, Stroiakovski D, et al. Improved overall survival in melanoma with combined dabrafenib and trametinib. The New England journal of medicine 2015;372:30–9 [DOI] [PubMed] [Google Scholar]
- 4.Bucheit AD, Davies MA. Emerging insights into resistance to BRAF inhibitors in melanoma. Biochemical pharmacology 2014;87:381–9 [DOI] [PubMed] [Google Scholar]
- 5.Long GV, Grob JJ, Nathan P, Ribas A, Robert C, Schadendorf D, et al. Factors predictive of response, disease progression, and overall survival after dabrafenib and trametinib combination treatment: a pooled analysis of individual patient data from randomised trials. The Lancet Oncology 2016;17:1743–54 [DOI] [PubMed] [Google Scholar]
- 6.Baenke F, Chaneton B, Smith M, Van Den Broek N, Hogan K, Tang H, et al. Resistance to BRAF inhibitors induces glutamine dependency in melanoma cells. Molecular oncology 2016;10:73–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gopal YN, Rizos H, Chen G, Deng W, Frederick DT, Cooper ZA, et al. Inhibition of mTORC1/2 overcomes resistance to MAPK pathway inhibitors mediated by PGC1alpha and oxidative phosphorylation in melanoma. Cancer research 2014;74:7037–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haq R, Shoag J, Andreu-Perez P, Yokoyama S, Edelman H, Rowe GC, et al. Oncogenic BRAF regulates oxidative metabolism via PGC1alpha and MITF. Cancer cell 2013;23:302–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McQuade JL, Vashisht Gopal Y. Counteracting oxidative phosphorylation-mediated resistance of melanomas to MAPK pathway inhibition. Molecular & cellular oncology 2015;2:e991610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vazquez F, Lim JH, Chim H, Bhalla K, Girnun G, Pierce K, et al. PGC1alpha expression defines a subset of human melanoma tumors with increased mitochondrial capacity and resistance to oxidative stress. Cancer cell 2013;23:287–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garraway LA, Widlund HR, Rubin MA, Getz G, Berger AJ, Ramaswamy S, et al. Integrative genomic analyses identify MITF as a lineage survival oncogene amplified in malignant melanoma. Nature 2005;436:117–22 [DOI] [PubMed] [Google Scholar]
- 12.Martelli AM, Buontempo F, McCubrey JA. Drug discovery targeting the mTOR pathway. Clinical science (London, England : 1979) 2018;132:543–68 [DOI] [PubMed] [Google Scholar]
- 13.Molina JR, Sun Y, Protopopova M, Gera S, Bandi M, Bristow C, et al. An inhibitor of oxidative phosphorylation exploits cancer vulnerability. Nature medicine 2018;24:1036–46 [DOI] [PubMed] [Google Scholar]
- 14.Lissanu Deribe Y, Sun Y, Terranova C, Khan F, Martinez-Ledesma J, Gay J, et al. Mutations in the SWI/SNF complex induce a targetable dependence on oxidative phosphorylation in lung cancer. Nature medicine 2018;24:1047–57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fischer GM, Jalali A, Kircher DA, Lee WC, McQuade JL, Haydu LE, et al. Molecular Profiling Reveals Unique Immune and Metabolic Features of Melanoma Brain Metastases. Cancer discovery 2019;9:628–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savi A, Incerti E, Fallanca F, Bettinardi V, Rossetti F, Monterisi C, et al. First Evaluation of PET-Based Human Biodistribution and Dosimetry of (18)F-FAZA, a Tracer for Imaging Tumor Hypoxia. Journal of nuclear medicine : official publication, Society of Nuclear Medicine 2017;58:1224–9 [DOI] [PubMed] [Google Scholar]
- 17.Davies MA, Stemke-Hale K, Lin E, Tellez C, Deng W, Gopal YN, et al. Integrated Molecular and Clinical Analysis of AKT Activation in Metastatic Melanoma. Clinical cancer research : an official journal of the American Association for Cancer Research 2009;15:7538–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Davies MA, Stemke-Hale K, Tellez C, Calderone TL, Deng W, Prieto VG, et al. A novel AKT3 mutation in melanoma tumours and cell lines. British journal of cancer 2008;99:1265–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas RK, Baker AC, Debiasi RM, Winckler W, Laframboise T, Lin WM, et al. High-throughput oncogene mutation profiling in human cancer. Nature genetics 2007;39:347–51 [DOI] [PubMed] [Google Scholar]
- 20.Cascone T, McKenzie JA, Mbofung RM, Punt S, Wang Z, Xu C, et al. Increased Tumor Glycolysis Characterizes Immune Resistance to Adoptive T Cell Therapy. Cell metabolism 2018;27:977–87.e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gopal YN, Deng W, Woodman SE, Komurov K, Ram P, Smith PD, et al. Basal and treatment-induced activation of AKT mediates resistance to cell death by AZD6244 (ARRY-142886) in Braf-mutant human cutaneous melanoma cells. Cancer research 2010;70:8736–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Russell S, Wojtkowiak J, Neilson A, Gillies RJ. Metabolic Profiling of healthy and cancerous tissues in 2D and 3D. Scientific reports 2017;7:15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. https://www.mdanderson.org/research/research-resources/core-facilities/functional-proteomics-rppa-core.html.
- 24.Mullen AR, Wheaton WW, Jin ES, Chen PH, Sullivan LB, Cheng T, et al. Reductive carboxylation supports growth in tumour cells with defective mitochondria. Nature 2011;481:385–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheng T, Sudderth J, Yang C, Mullen AR, Jin ES, Mates JM, et al. Pyruvate carboxylase is required for glutamine-independent growth of tumor cells. Proceedings of the National Academy of Sciences of the United States of America 2011;108:8674–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mullen AR, Hu Z, Shi X, Jiang L, Boroughs LK, Kovacs Z, et al. Oxidation of alpha-ketoglutarate is required for reductive carboxylation in cancer cells with mitochondrial defects. Cell reports 2014;7:1679–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niehr F, von Euw E, Attar N, Guo D, Matsunaga D, Sazegar H, et al. Combination therapy with vemurafenib (PLX4032/RG7204) and metformin in melanoma cell lines with distinct driver mutations. Journal of translational medicine 2011;9:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yuan P, Ito K, Perez-Lorenzo R, Del Guzzo C, Lee JH, Shen CH, et al. Phenformin enhances the therapeutic benefit of BRAF(V600E) inhibition in melanoma. Proceedings of the National Academy of Sciences of the United States of America 2013;110:18226–31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhou G, Myers R, Li Y, Chen Y, Shen X, Fenyk-Melody J, et al. Role of AMP-activated protein kinase in mechanism of metformin action. The Journal of clinical investigation 2001;108:1167–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shen CH, Yuan P, Perez-Lorenzo R, Zhang Y, Lee SX, Ou Y, et al. Phosphorylation of BRAF by AMPK impairs BRAF-KSR1 association and cell proliferation. Molecular cell 2013;52:161–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Corcoran RB, Rothenberg SM, Hata AN, Faber AC, Piris A, Nazarian RM, et al. TORC1 suppression predicts responsiveness to RAF and MEK inhibition in BRAF-mutant melanoma. Science translational medicine 2013;5:196ra98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Deng W, Gopal YN, Scott A, Chen G, Woodman SE, Davies MA. Role and therapeutic potential of PI3K-mTOR signaling in de novo resistance to BRAF inhibition. Pigment cell & melanoma research 2012;25:248–58 [DOI] [PubMed] [Google Scholar]
- 33.Romano G, Chen PL, Song P, McQuade JL, Liang RJ, Liu M, et al. A Preexisting Rare PIK3CA(E545K) Subpopulation Confers Clinical Resistance to MEK plus CDK4/6 Inhibition in NRAS Melanoma and Is Dependent on S6K1 Signaling. Cancer discovery 2018;8:556–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teh JLF, Cheng PF, Purwin TJ, Nikbakht N, Patel P, Chervoneva I, et al. In Vivo E2F Reporting Reveals Efficacious Schedules of MEK1/2-CDK4/6 Targeting and mTOR-S6 Resistance Mechanisms. Cancer discovery 2018;8:568–81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Krepler C, Sproesser K, Brafford P, Beqiri M, Garman B, Xiao M, et al. A Comprehensive Patient-Derived Xenograft Collection Representing the Heterogeneity of Melanoma. Cell reports 2017;21:1953–67 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.