Abstract
Background
The thymus plays an essential role in the pathogenesis of myasthenia gravis (MG). In patients with MG, natural regulatory T cells (nTreg), a subpopulation of T cells that maintain tolerance to self-antigens, are severely impaired in the thymuses. In our previous study, upregulated nTreg cells were observed in the thymuses of rats in experimental autoimmune myasthenia gravis after treatment with exosomes derived from statin-modified dendritic cells (statin-Dex).
Methods
We evaluated the effects of exosomes on surface co-stimulation markers and Aire expression of different kinds of thymic stromal cells, including cTEC, mTEC, and tDCs, in EAMG rats. The isolated exosomes were examined by western blot and DLS. Immunofluorescence was used to track the exosomes in the thymus. Flow cytometry and western blot were used to analyze the expression of co-stimulatory molecules and Aire in vivo and in vitro.
Results
We confirmed the effects of statin-Dex in inducing Foxp3+ nTreg cells and found that both statin-Dex and DMSO-Dex could upregulate CD40 but only statin-Dex increased Aire expression in thymic stromal cells in vivo. Furthermore, we found that the role of statin-Dex and DMSO-Dex in the induction of Foxp3+ nTreg cells was dependent on epithelial cells in vitro.
Conclusions
We demonstrated that statin-Dex increased expression of Aire in the thymus, which may further promote the Foxp3 expression in the thymus. These findings may provide a new strategy for the treatment of myasthenia gravis.
Keywords: Exosomes, Thymus, Experimental autoimmune myasthenia gravis (EAMG), Foxp3+ natural regulatory T cells, Aire
Introduction
Myasthenia gravis (MG) is a chronic autoimmune disorder of neuromuscular transmission resulting in muscle weakness. The thymus plays a major role in the pathogenesis of MG with anti-acetylcholine receptor (AChR) antibodies. Sixty-five percent of patients with MG are found to have thymic dysplasia and another 10% of cases are associated with thymoma [1]. Naturally occurring thymus-derived regulatory T (nTreg) cells are generated in the thymus and are key players in the suppression of immune response. Several reports have illustrated the decreased amount and function of thymic nTreg cells in MG patients [2, 3]. This defect in nTreg cells attracts peripheral B cells and activated T cells, which maintain a chronically inflammatory thymic environment [4]. Such deleterious effects highlight the importance of nTreg cells function in the pathogenesis of MG.
Multiple factors can influence the development of thymic nTreg cells. Differentiation of nTreg cells is dependent on thymic stromal cells, which can be subdivided into thymic epithelial cells (TEC) and thymic dendritic cells (tDCs). There are two main populations of TEC based on different cell surface markers and their location in the thymus [5]. Medullary TEC (mTEC) are defined by their binding capacity to the lectin Ulex europaeus Agglutinin I (UEA-I), while cortical TEC (cTEC) are recognized by anti-aminopeptidase A (APA) expression. mTEC and cTEC possess distinct functions to maintain balanced microenvironments [6]. Developing thymocytes are positively selected by cTEC and subsequently negatively selected by mTEC or tDCs [7]. On the other hand, nTreg cells are selected at the double-positive (DP) stage through interaction with the MHC class II-expressing cells within the thymic medulla, where they begin to express Foxp3 and differentiate into Foxp3+ nTreg cells [8].
Molecular factors like the autoimmune regulator (Aire) and CD80/86 interactions can also influence thymic nTreg cells differentiation. An autoimmune regulator called Aire is a transcriptional regulator that is highly expressed in a subset of mTECs. The function of Aire is to maintain the thymic structure and enable thymic expression of tissue-restricted antigens (TRA). TRA are presented to thymocytes by mTEC and tDC and drive self-reactive thymocytes to differentiate into Treg cells, which is essential for the maintenance of self-tolerance. Mutations in Aire lead to multi-organ autoimmunity in both mice and humans [9]. In an Aire knockout (Aire−/−) murine model, the mice displayed changes in their thymic structure and exhibited a decrease in peripheral regulatory T cells [10, 11]. Moreover, the differentiation of Treg cells requires not only the recognition of antigen/major histocompatibility complexes by the T cell receptor but also cooperation between CD28-CD80/86 and CD40-CD40L co-stimulatory interactions [12, 13]. Together, this indicates that not only cellular mechanisms including TEC and DCs but also molecular factors including MHC II, CD80/86, CD40, and Aire, influence the generation of thymic nTreg cells.
Exosomes, which are extracellular vesicles ranging from 30 to 150 nm in diameter [14, 15], have been implicated in many aspects of autoimmune disease such as multiple sclerosis (MS) [16, 17], rheumatoid arthritis (RA) [18] and systemic lupus erythematosus (SLE) [19], as well as in immune regulation involved in functions of T cells, B cells, DCs and so on. Since exosomes are more stable and easier to store, they have attracted more attention in recent years. Previously, we have reported that statins had the ability to induce tolerogenic DCs that displayed the potential to regulate both cellular and humoral immunity to relieve clinical symptoms in experimental autoimmune myasthenia gravis (EAMG) [20, 21]. We also used ultra-centrifugation to obtain statin-DC-derived exosomes (statin-Dex) or DMSO-DC-derived exosomes (DMSO-Dex). We demonstrated the ability of statin-Dex to ameliorate the clinical symptoms of EAMG rats. These therapeutic effects were associated with upregulated levels of Foxp3+ nTreg cells in both the thymus and peripheral lymphoid organs [22]. Since nTreg cells played a vital role in immune-regulatory effects of statin-Dex, we wondered if the thymus was the predominant target in the process.
In this study, we explored how statin-Dex upregulates nTreg cells in the thymus in EAMG. We found that statin-Dex increased expression of Aire in the thymus in vivo. Furthermore, statin-Dex promoted the development of Foxp3+ nTreg cells among thymocytes with the existence of thymic stromal cells in vitro. Taken together, we demonstrated that statin-Dex increased expression of Aire in the thymus, which may further promote the Foxp3+ expression in the thymus.
Materials and methods
EAMG induction and exosome administration
Female Lewis rats, 6–8 weeks old, were purchased from Vital River Corporation (Beijing, China) and housed at the animal facility of the Institute. Food and water were provided ad libitum. All animal procedures were conducted in strict accordance with the institutional ethics committee. Animals were euthanized via deep anesthesia using isoflurane. EAMG models were induced by a subcutaneous immunization at the base of the tail (two sites) with 75 μg of AchR 97–116 peptide (from China Peptides Co., Ltd.; Shanghai, China), emulsified in Complete Freud Adjuvant containing 1 mg Mycobacterium tuberculosis, in a total volume of 200 μl.
Animals were divided into three groups. One group of rats was used as PBS control; the other two groups received exosomes (10 μg/rat) derived from either DMSO or statin-treated BMDCs. The exosomes were administered on days 5, 10, and 15 p.i. The rats were sacrificed on day 20 p.i.
The culture of bone marrow dendritic cell and isolation of exosomes
To isolate and culture BMDCs, tibias and femurs were removed from 6- to 8-week-old Lewis rats. The whole bone marrow was flushed out and filtered through a 70-μm Cell Strainer. After lysis of erythrocytes, cells were re-suspended in RPMI 1640 medium containing 10% (v/v) fetal bovine serum, 1% (v/v) penicillin-streptomycin (Gibco, Invitrogen Ltd., Paisley, UK) in the presence of 10 ng/ml recombinant rat (rr) GM-CSF (Peprotech, Rocky Hill, NJ, USA), and 10 ng/ml rrIL-4 (Peprotech). After a 72-h incubation, non-adherent cells were gently removed and adherent cells were further cultured. On day 7, non-adherent and loosely adherent cells were harvested and incubated with atorvastatin dissolved in dimethylsulfoxide (DMSO; Sigma-Aldrich, St. Louis, MO, USA, final concentration 10 μM) or DMSO (only in medium) with 10% FBS depleted of contaminating vesicles and protein aggregates for another 48 h at 37 °C and 5% CO2, before they were centrifuged at 300×g for 5 min. The supernatant was collected for exosomes isolation.
Exosomes were isolated and characterized as previously described. Briefly, the supernatant was centrifuged at 2000×g for 10 min and 10,000×g for 30 min to remove whole debris and large vesicles. The resultant supernatant fluid was then centrifuged at 100,000×g for 70 min (Beckman Coulter. Inc., IN, USA). Exosome pellets were rinsed with PBS and re-centrifuged at 100,000×g for 70 min. Finally, exosomes were suspended in sterile PBS and quantified by the K5600 MicroSpectroPhotoMeter (Beijing Kaiao Technology Development Co. Ltd., Beijing, China). Exosomes were stored at − 20 °C.
Identification of exosomes
For transmission electron microscopy analysis, carbon-coated copper grids were placed in the exosome suspensions fixed with 2% paraformaldehyde overnight. The grids were then negatively stained by 2% phosphotungstic acid for 5 min and air-dried for 1 min at room temperature. The exosome samples were visualized by a Tecnai 20 U-TWIN operated at 80 kV (Philips, Nederland).
The exosome size was measured by dynamic light scattering (DLS). Briefly, exosomes (1 μg) were re-suspended in 1 ml-filtered PBS at pH 7.4. The sizes of the particles were analyzed by DLS Nano sizer (Nano-ZS; Malvern, UK).
Tracking analysis in the thymus
Purified exosomes were labeled with membrane-targeted red fluorescent dye PKH26 (Sigma-Aldrich). In brief, 20 μl of exosomes suspended in 100 μl of Diluent C mixed with an equal volume of Diluent C containing 0.4 μl PKH26 dye and was incubated at 4 °C for 5 min. The labeling reaction was stopped by the addition of 10% FBS in PBS. The labeled exosomes were purified by centrifugation at 4000×g for 30 min, followed by ultrafiltration (0.22 μm filter; Millipore, Billicera, MA, USA) three times and were finally re-suspended in PBS. For uptake studies, 10 μg of labeled exosomes suspended in 300 μl of PBS were injected to EAMG rats. Following 3 days of intravenous injection, thymuses removed from rats in different groups were visualized with a fluorescence microscope to determine the distribution of exosomes.
Preparation of thymic stromal cells
The thymic stromal cells were isolated as described previously [23]. In brief, thymuses were dissected from freshly killed rats and trimmed of fat and connective tissue. Tissues were gently agitated on a 70-μm filter with a vitreous stirrer. Thymocytes were collected under the filter. The resulting thymic fragments were transferred into a petri dish and then incubated in 1 mg/ml collagenase D with 0.1% (w/v) DNAse I (both from Roche Applied Science, Indianapolis, IN, USA) at 37 °C for 10 min. Enzyme mixtures with isolated cells were removed and replaced with the fresh mixture for further incubation. After another 10 min of digestion, isolated cells were removed and collagenases/dispase were added. During the digestion, gentle mechanical agitation was performed with a 26G needle to break up any remaining aggregates. Cells were pooled and resuspended in 5 mM EDTA buffer and incubated for 10 min at 4 °C to disrupt rosettes, followed by centrifugation at 300×g for 8 min. Cells were then passed through a 70-μm filter to remove clumps. Both thymocytes and thymic stromal cells were counted and prepared for antibody labeling.
In vitro Treg cells induction experiments
To determine the functions of exosomes on the differentiation of thymic Treg cells, thymocytes were cultured with exosomes and TECs, exosomes and BMDCs, or exosomes only. After digestion described above, thymic CD45− stromal cells were labeled and sorted by FACS. Thymocytes (2 × 106/ml) and BMDCs (2 × 105/ml) or CD45− stroma cells (2 × 105/ml) were suspended in the medium with 20 μg/ml exosomes. This was added into 96-well plates under stimulation with 5 μg/ml of IL-2 (PeproTech, NJ, USA), 1 μg/ml anti-CD3 (PeproTech), and 1 μg/ml anti-CD28 (PeproTech) mAb. After 2 days, the cells were collected and the percentages of CD4+Foxp3+ T cells were determined by FACS.
FACS
For cell surface marker analysis, thymic TEC and DCs were stained using conventional methods. Antibodies were all mouse monoclonal antibodies unless specified. CD86 (24H), OX62 (OX-62), and CD45 (OX-1) were obtained from Biolegend (San Diego, CA, USA). CD4 (OX35), MHC II (HIS19), CD40 (HM40-3), and CD80 (3H5) were purchased from eBioscience (San Diego, CA, USA). Unconjugated APA (goat polyclonal IgG) was obtained from Santa Cruz (United States) and the secondary antibody FITC or Alexa Fluor 647 conjugated donkey anti-goat IgG was purchased from Abcam (Cambridge, MA, USA). UEA-1 was purchased from Vector Laboratories (Burlingame, CA, USA).
For nTreg cells, thymocytes were stained with specific Abs against rat CD4, CD8 (eBioscience) and CD25 (OX39, Invitrogen) before being fixed and permeabilized with Perm/Fix solution (eBioscience). Finally, an antibody specific for Foxp3 (rat monoclonal antibody, FJK-16S, eBioscience) was added for 30 min in the dark.
Immunofluorescence
Thymus tissues were cryo-sectioned and processed for the immunofluorescence (IF) assay. Sections (8 μm) were fixed in cold acetone and incubated in 0.5% bovine serum albumin (BSA) (Solarbio, Beijing, China). Samples were incubated with primary antibody Aire (Santa Cruz) at 4 °C overnight. Afterward, sections were incubated with secondary fluorescently tagged antibody protected from light. Images were acquired on an Olympus FSX100 (Tokyo, Japan) at different magnifications. The fluorescence microscopy examination was performed in a blinded manner.
Western blotting
A western blot was performed to determine thymic Aire from thymus tissues. Proteins were separated on a gel and transferred onto a PVDF membrane. Anti-Aire (Santa Cruz) and anti-GADPH (Zhongshan Goldenbridge Biotechnology, Beijing, China) were used as primary antibodies; horseradish peroxidase-coupled goat anti-mouse or goat anti-rabbit (Zhongshan Goldenbridge Biotechnology) as secondary antibodies. The immunoreactive proteins were visualized using a FluorChem E Imager (Protein-Simple, Santa Clara, CA, USA). Bands were quantified with ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Statistical analysis
Statistical tests were performed using GraphPad Prism 7.0 (GraphPad Software, San Diego, CA, USA). Differences between controls and experimental groups were determined with one-way ANOVA and followed by the Bonferroni test as a post hoc test. P < 0.05 was considered statistically significant.
Results
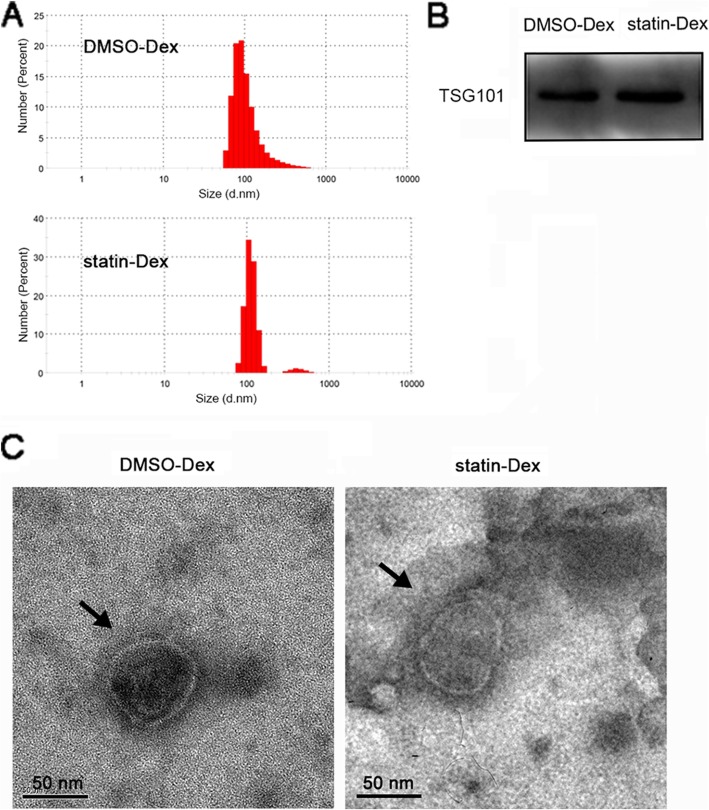
Identification of exosomes derived from DCs culture medium
For isolation of exosomes, extracellular vesicles from BMDC culture supernatants were obtained by ultracentrifugation (approximately 3–8 μg particles from 1 ml fluid). According to the proof of morphology, the particles were identified by DLS instruments (Fig. 1a), western blotting (Fig. 1b), and electron microscopy (Fig. 1c), respectively. The diameters of particles in the DMSO-Dex and the statin-Dex groups were primarily distributed in the range of 70–140 nm. The morphology observed under an electron microscope was shown to be intact, with a diameter of about 100 nm. To confirm the exosome-enriched fractions, TSG101 (a well-established marker for exosomes) was determined by western blot. Exosomes from both the DMSO-Dex and the statin-Dex groups expressed the TSG101 with a size of 49 kDa.
Fig. 1.
Characterization of DMSO-Dex and statin-Dex. a DLS Nano sizer analysis showed size distribution of exosomes from the DMSO-Dex and the statin-Dex groups, ranging from 70 to 140 nm (mainly from 80 to 120 nm). b TSG101 expression with size 49 kDa in DMSO-Dex and statin-Dex. c Representative images of the exosome from the DMSO-Dex and the statin-Dex groups under transmission electron microscopy (scale bar 50 nm)
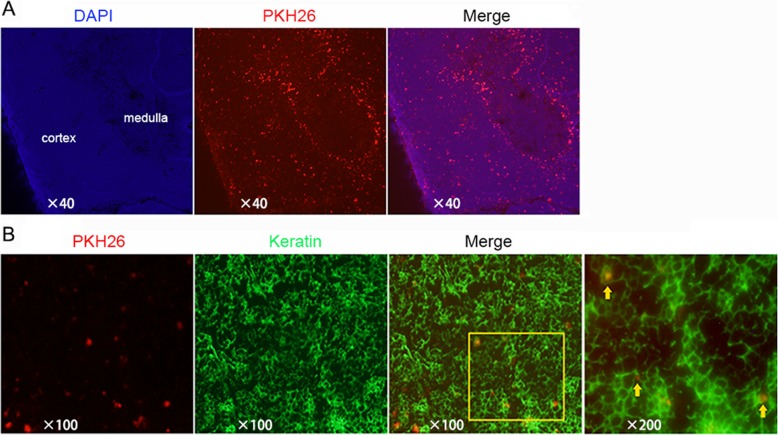
Exosomes are distributed mostly in the cortex of the thymus
In our previous study, exosomes were found in the thymus, lymph nodes and spleen except the liver on day 3 after injection [22]. To further verify that exosomes entered and functioned in the thymus, exosomes were labeled with PKH26 in vitro and then injected into EAMG rats via the tail vein. Three days after the injection, the rat thymuses were removed and sectioned to observe the distribution of exosomes under a microscope. As shown in Fig. 2a, exosomes were mainly located at the cortex within the thymus. There were more PKH26-labeled exosomes around medulla because they were spilled from the blood vessels, which are rich in the cortico-medullary junction [24]. There is no difference in the distribution between the DMSO-Dex group and the statin-Dex group. Furthermore, exosomes were shown to be engulfed by the keratin positive thymic epithelial cells in the cortex (Fig. 2b).
Fig. 2.
Delivery of exosomes labeled with PKH26 in the thymus. a Cryostat sections of the thymus from rats receiving PKH26-labeled statin-Dex (red) were stained with DAPI (blue). b Cryostat section of the thymus stained with stromal cell-specific keratin (green) from rats receiving an intravenous injection of PKH26-labeled statin-Dex (red)
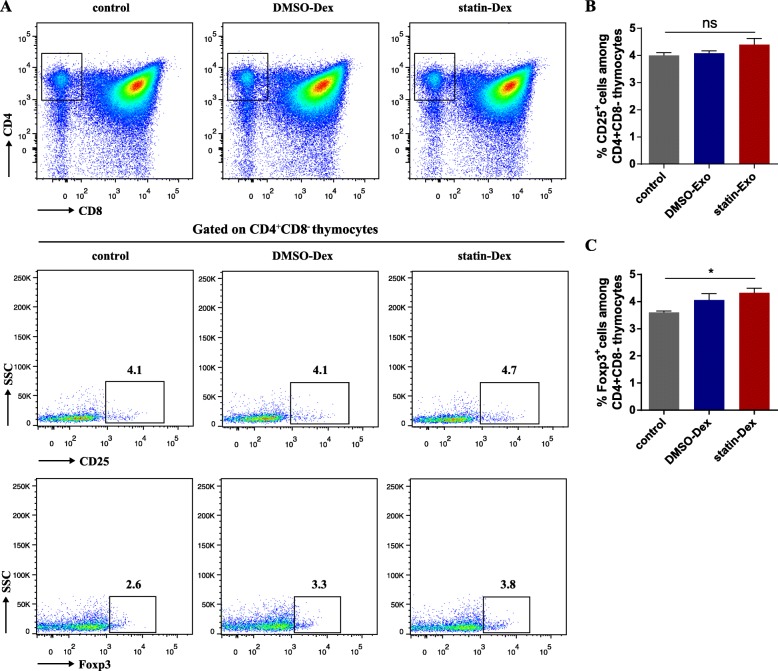
Statin-Dex increases Foxp3 expression in thymocytes
Our previous study reported that statin-Dex induced an increase of Foxp3 expression in the thymus and peripheral Foxp3+ nTreg cells in lymph nodes. In this study, we focused on its effects on thymic nTreg cells. In the early stage of EAMG disease, on day 20 p.i., the percentage of nTreg cells in the thymus was detected by FACS. As shown in Fig. 3b, there were no statistical differences in CD4+CD8−CD25+ thymocytes (thymic nTreg cells) among the three groups. However, the percentage of Foxp3+ nTreg cells among CD4+CD8− thymocytes was significantly higher in the statin-Dex group than in the PBS-treated control group (Fig. 3c).
Fig. 3.
Statin-Dex promoted thymic nFoxp3+ Treg cell differentiation. a The representative gating strategy of CD4, CD8, and representative dot plots of CD25 expression, and Foxp3 expression are shown. Percentages of CD25 (b) and Foxp3 expression (c) among CD4+CD8− thymocytes were analyzed. Data were presented as mean ± SEM from two independent experiments (n = 5 in control group; n = 6 in DMSO-Dex and statin-Dex groups, *p < 0.05). The significance of the differences was evaluated by ANOVA, followed by Bonferroni test as a post hoc test
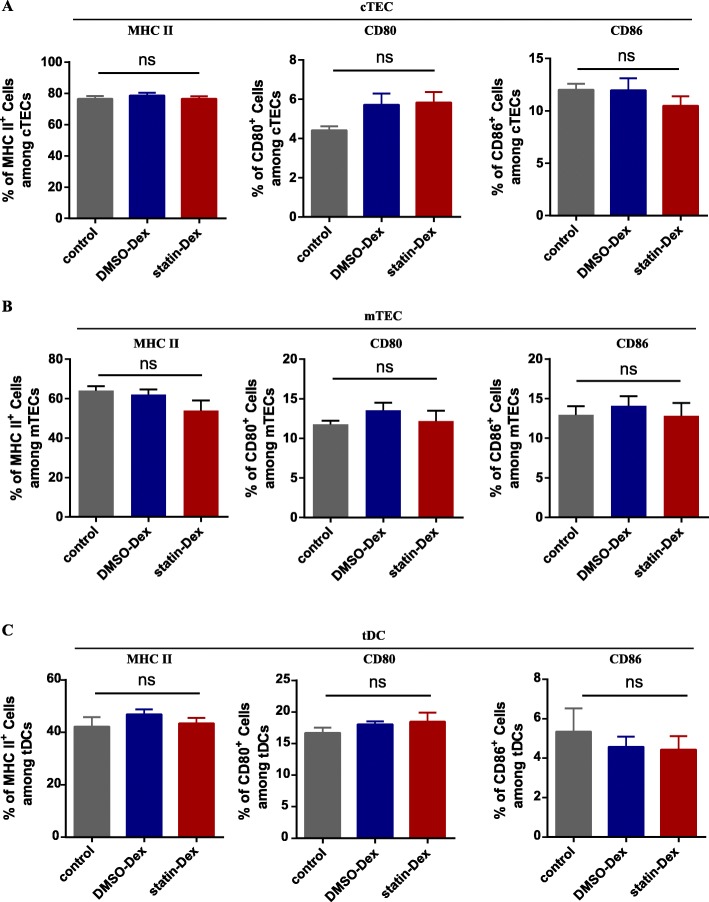
MHC II and B7 molecules remain unchanged in the control group, the DMSO-Dex group, and statin-Dex groups
On day 20 p.i., thymuses were removed from rats in the control group, the DMSO-Dex group, and the statin-group. After thymocytes removal, TEC and tDCs were obtained as described. tDCs were defined as OX62 positive cells, cTEC as CD45−APA+, and mTEC as CD45− UEA1+. To investigate whether co-stimulatory molecules of thymic stromal cells were affected by exosomes, the expression levels of MHC II, CD80, and CD86 were examined by flow cytometry. However, there were no significant differences among the three experimental groups (Fig. 4 a-c), suggesting that MHC II and B7 molecules may not be involved in the regulation of Foxp3+ nTreg cells by exosomes.
Fig. 4.
Expression of MHC II, CD80, and CD86 on cTEC (CD45−APA+), mTEC (CD45−UEA-1+), and tDCs (OX62+). After digestion, single thymic stromal cells were obtained and the expression of MHC II, CD80, and CD86 on cTEC (a), mTEC (b), and tDCs (c) were examined by flow cytometry, respectively (ns means no significance). Data were representative of two independent experiments (n = 5 in the control group; n = 6 in DMSO-Dex and statin-Dex groups)
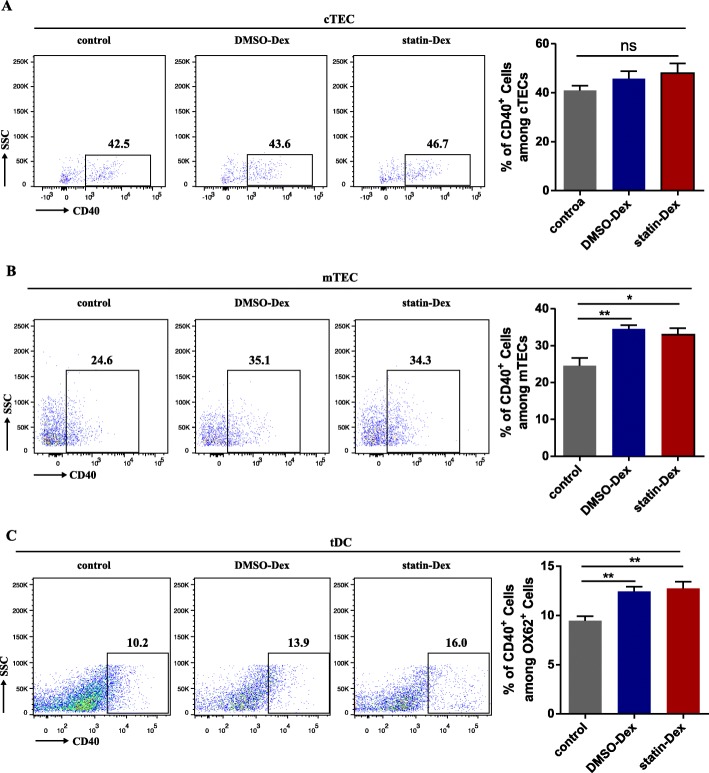
DC-derived exosomes upregulate CD40 expression on thymic medullary epithelial cell and thymic DCs
CD40 expression in the thymus is also essential for promoting the development of thymic Foxp3+ nTreg cells. As a result, the CD40 level of the thymic stromal cells was further examined. Compared to the control group, both DMSO-Dex and statin-Dex increased the expression of CD40 on the mTEC and tDCs, but there was no alteration of CD40 expression on the cTEC in the thymus (Fig. 5a–c).
Fig. 5.
Exosomes increased the expression of CD40 in the thymus. There is no change in the expression of CD40 on cTEC among the three experimental groups (a). Both DMSO and statin-treated DC-derived exosomes had significantly increased CD40 expressions on mTEC (b) and tDCs (c) compared with the PBS treated control group (*p < 0.05 and **p < 0.01). Data were presented as mean ± SEM from two independent experiments (n = 5 in the control group; n = 6 in DMSO-Dex and statin-Dex groups). The significance of the differences was evaluated by ANOVA, followed by Bonferroni test as a post hoc test
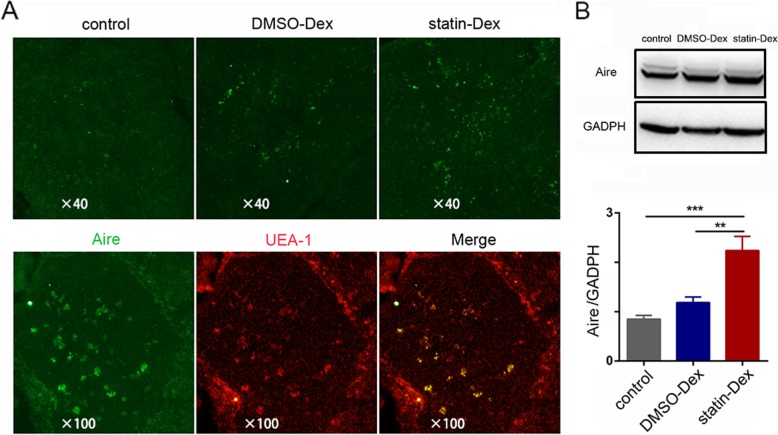
Statin-Dex increase Aire in the thymic medulla
It has been reported that CD40 contributes to the expression of Aire in thymic medullary epithelial cells and Aire is critical to the nTreg cell differentiation in the thymus [25, 26]. On day 20 p.i., the thymuses were obtained and Aire expression was examined by immunofluorescence. Immunofluorescence results demonstrated an obviously increased Aire expression in thymic medullary epithelial cells in the statin-Dex group when compared to both the control group and the DMSO-Dex group (Fig. 6a). Increased Aire expression in the thymus in the statin-Dex group was further confirmed by the western quantitative analysis compared to the control group and the DMSO-Dex group (Fig. 6b).
Fig. 6.
Statin-Dex upregulates the expression of Aire in the thymus. a Frozen tissue sections of thymus were stained with antibodies to Aire (green) and UEA-1 (red) to examine the expression of Aire in mTEC. b Aire expression analysis in the thymus by western blot (**p < 0.01 and ***p < 0.001). Data were presented as mean ± SEM (n = 5 in the control group; n = 6 in DMSO-Dex and statin-Dex groups). The significance of the differences was evaluated by ANOVA, followed by Bonferroni test as a post hoc test
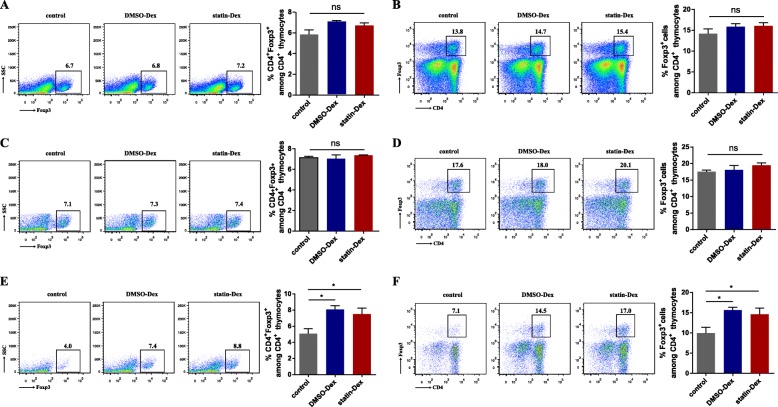
DC-derived exosomes promote the development of Foxp3+ Treg cells among thymocytes by TEC in vitro
Thymocytes were cultured with DMSO-Dex, statin-Dex, and PBS respectively and the percentages of Foxp3+ thymocytes were measured 48 h later. There was no difference in the percentages of Foxp3+ Treg cells among the three experimental groups (Fig. 7a, b), which indicates that exosomes may not directly affect Foxp3+ Treg cells differentiation in the thymus. To assess whether the impact of exosomes on the thymic Treg cell differentiation was dependent on DCs, BMDCs, and thymocytes (at a ratio of 1:10) were co-cultured with DMSO-Dex, statin-Dex, and PBS, respectively. After 48 h of cultivation, no differences in the percentages of Foxp3+ Treg cells in the three experimental groups were observed (Fig. 7c, d), which suggested that exosomes could not promote Foxp3+ Treg cell expansion through regulation of DCs. CD45− cells (mainly TEC) were isolated and co-cultured with thymocytes (at a ratio of 1:10) in the presence of PBS, DMSO-Dex, and statin-Dex. The percentages of both CD4+Foxp3+ Treg cells among total thymocytes (Fig. 7e) and Foxp3+ Treg cells among CD4+ thymocytes (Fig. 7f) were higher in the two exosome groups compared to the control. Taken together, these data provided strong evidence that upregulated Foxp3+ Treg cells by exosomes in thymocytes is mainly mediated by TEC.
Fig. 7.
CD45− stromal cells promote the thymic Foxp3+ Treg cells differentiation in vitro. Frequencies of CD4+Foxp3+ Treg cells among total thymocytes and Foxp3+ Treg cells among CD4+ thymocytes after 2 days of incubation with PBS control, DMSO-Dex, and statin-Dex, respectively (a, b). Thymocytes were cultured with BMDCs (c, d) or CD45− stromal cells (e, f) (at a ratio of 1:10) with PBS control, DMSO-Dex and statin-Dex, respectively. (*p < 0.05). Data were representative of three independent experiments. The significance of differences was evaluated by ANOVA, followed by Bonferroni test as a post hoc test
Discussion
Exosomes are nano-bioactive vesicles that can be secreted by almost all types of cells, and may contain biomarkers from the source cells. Exosomes derived from DCs carry MHC II and T cell co-stimulatory molecules on their surface, suggesting that they could play regulatory roles in immune response. It has been demonstrated that DC-derived exosomes could be either immune-stimulatory or suppressive depending on the type and stage of maturation of the DCs [27–29]. Immature DC-derived exosomes display a tolerance activity in a mouse model of EAMG [30]. Exosomes derived from microRNA-146a overexpressing DCs suppress ongoing EAMG in a partly dose-dependent manner [31]. In our study, to some extent, both DMSO-treated and statin-treated DCs showed immature characteristics due to lack of stimulation by LPS or CpG. The effect of DMSO-Dex is due to the fact that there were some immature DCs in the culture system of DC treated with DMSO. This may account for the similar effect of DMSO-Dex and statin-Dex on the CD40 expression of mTEC and tDCs in vivo and the differentiation of Foxp3+ Treg cells in vitro. Our previous data showed that exosomes derived from statin modified DCs displayed a lower level of MHC II than exosomes from DMSO modified DCs, indicating a more immature phenotype of statin-modified DCs [22]. However, only statin-Dex upregulate the expression of Aire in the thymus, which accounts for its effect on the differentiation of nTreg in vivo. In our previous study, statin-treated DCs from EAMG rats inhibited the antigen-specific lymphocyte proliferation in the presence of peptide AchR 97-116, whereas exosomes derived from these statin-DCs did not [21, 22]. Therefore, the exosomes from the DC of healthy rats in the present study were not antigen-specific. In the present study, exosomes derived from statin-DC increased thymic Aire expression and induced the differentiation of thymic Foxp3+ nTreg cells in EAMG, which played an essential role in central immune tolerance. It is reasonable to hypothesize that statin-Dex would also increase thymic Aire expression in healthy animals but it is more meaningful in the autoimmune diseases.
The thymus is a primary lymphoid organ required to induce and maintain central tolerance by clonal deletion of self-reactive thymocytes or by driving nTreg differentiation. nTreg cells generated in the thymus can migrate into the peripheral and suppress autoimmune responses. They play an important role in the maintenance of immune tolerance and homeostasis. Several scientific research have tried to explore the process in which nTreg cells reach functional maturity within the thymus. The generation of nTreg cells is under strict regulation and control in the thymus. Both mTEC and tDC are shown to be important for nTreg cells differentiation. And mTEC were considered to serve as the key accessory cell for nTreg selection. Our ex vivo data showed that exosomes can enhance Treg cell generation only in the presence of TEC, suggesting that TEC were essential for exosomes to upregulate the Foxp3 Treg cells.
Studies have shown that most Foxp3+ cells are mainly located in the medulla of thymus, which suggests the important role of mTEC in the development of nTreg cells [32, 33]. Mice with disrupt thymic medulla have decreased Foxp3 expression [34]. Furthermore, many studies emphasized the roles of Aire in regulating mTEC differentiation and Foxp3+ nTreg cells differentiation in the thymus [35–37]. Aire is predominantly expressed in mTEC and a negative selection of tissue-specific T cells during intrathymic development is aided by Aire. Depletion of Aire-expressing mTEC and tDCs are in accordance with a dramatic decrease of Foxp3+ nTregs in the thymus of Omenn syndrome patients. This suggests a role of Aire-expressing mTEC and/or thymic DCs in the differentiation of Foxp3+ nTreg cells [38]. Previous data have indicated a correlation between the patients with autoimmune polyendocrinopathy candidiasis ectodermal dystrophy (APECED) and Treg cells. This is characterized by the loss-of-function mutations in the Aire gene, and an impaired circulating Foxp3+ Treg population [39, 40]. The defect of Treg is not only the frequency of Tregs but also their levels of Foxp3 expression and function. The report has shown that abrogating thymic expression of Aire, via deletion of conserved non-coding sequence (CNS1) (a putative enhancer upstream of the Aire gene), leads to impaired terminal differentiation of the mTEC population and a reduction in the production of thymic nTreg cells [41]. Overall, the available evidence supports the essential effect of Aire in Foxp3+ nTreg cells development. Our data demonstrated that statin-Dex increased Aire expression in the thymic medulla, which may lead to the increase of Foxp3+ nTreg cells.
MHC II on the epithelial cells plays an essential role in the differentiation of nTreg in the thymus. The development of Treg cells is initially dependent on TCR-MHC II and CD28-CD80/CD86 interaction, which leads to the generation of thymic Treg cell precursors (pre-Treg cells). However, there were no differences among the three groups in the expression of MHC II as well as CD80 and CD86 molecules in our study. CD40 has been observed to be expressed on tDCs, cTEC, and mTEC [42]. It is a co-stimulatory molecule associated with the mature state of mouse tDCs and has been shown to affect levels of MHC II, CD80, and CD86 on APCs through interactions with CD40L [43]. CD40 has a role in the expansion of nTreg populations. Ablation of CD40 expression in tDCs results in a significant reduction in the number of nTreg cells. CD4+ thymocytes co-culture with CD40-deficient DCs fail to differentiate them into nTreg cells to a sufficient number in vitro [44]. Furthermore, it was reported that disruption of CD40 signaling would lead to a severe defect in mTEC. Importantly, expression of CD40 on either tDCs or TEC is sufficient to promote the development of Fxop3+ Treg cells [45]. Our study demonstrated that both exosome treatments upregulated CD40 expression in mTEC and tDCs but without any change for the expression of MHC II and B7 molecules in thymic stromal cells. Furthermore, only statin-Dex increased thymic Aire expression and thereafter thymic nTreg differentiation in vivo.
Conclusion
We evaluated the effects of exosomes on surface co-stimulation markers and Aire expression of different kinds of thymic stromal cells, including cTEC, mTEC, and tDCs. It was established that the increased thymic Foxp3+ nTreg cells in statin-Dex treatment was correlated with upregulated Aire in mTEC in vivo. Statin-Dex promoted the development of Foxp3+ Treg cells among thymocytes with the existence of thymic stromal cells in vitro. All these data demonstrated that statin-Dex may induce central tolerance in EAMG, which may provide a new strategy in the treatment of myasthenia gravis.
Acknowledgements
The authors acknowledge the technical support of Prof. Hong-Xiang Lou (Department of Pharmacy, Shandong University), and atorvastatin provided by Beijing Garlin Pharmaceutical Co., Ltd.
Abbreviations
- Aire
Autoimmune regulator
- APA
Anti-aminopeptidase A
- BMDC
Bone marrow dendritic cells
- cTEC
Cortical thymic epithelial cells
- DC
Dendritic cell
- DMSO-Dex
Exosomes derived from DMSO-modified dendritic cells
- EAMG
Experimental autoimmune myasthenia gravis
- MG
Myasthenia gravis
- MHC II
MHC class II
- MS
Multiple sclerosis
- mTEC
Medullary thymic epithelial cells
- RA
Rheumatoid arthritis
- SLE
Systemic lupus erythematosus
- statin-Dex
Exosomes derived from statin-modified dendritic cells
- tDC
Thymic dendritic cells
- TEC
Thymic epithelial cells
- TRA
Tissue-restricted antigens
- Treg
Regulatory T cells
- UEA-I
Ulex europaeus Agglutinin I
Authors’ contributions
RSD, YCD, XLL, and HL designed the research. PZ, RTL, TD, CLY, YDL, MZ, and MRG performed the experiments and collected the data. PZ, RTL, and TD analyzed the data. PZ, CLY, and RSD wrote the manuscript. All authors have read and approved the final manuscript.
Funding
This work was supported by grants from the National Natural Science Foundation of China [81471222] and Taishan Scholars Construction Engineering of Shandong Province [ts20130914].
Availability of data and materials
All data generated or analyzed during this study are available on request.
Ethics approval and consent to participate
All animal procedures were conducted in strict accordance with the institutional ethics committee of Shandong University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Peng Zhang, Email: peng03080308@126.com.
Ru-Tao Liu, Email: liu.tao68@163.com.
Tong Du, Email: dutong1992@163.com.
Chun-Lin Yang, Email: muyilin1991@163.com.
Yu-Dong Liu, Email: gxliuyudong1992@163.com.
Meng-Ru Ge, Email: mengruxg@163.com.
Min Zhang, Email: zhangmin19870823@163.com.
Xiao-Li Li, Email: li2006xl@163.com.
Heng Li, Email: liheng_sdu@163.com.
Ying-Chun Dou, Email: douyingchun01@163.com.
Rui-Sheng Duan, Email: ruisheng_duan@yahoo.com.
References
- 1.Aquilina A, Camilleri DJ, Aquilina J. Pure red cell aplasia and myasthenia gravis: a patient having both autoimmune conditions in the absence of thymoma. BMJ Case Rep. 2017;2017. https://www.ncbi.nlm.nih.gov/pubmed/28893803. [DOI] [PMC free article] [PubMed]
- 2.Thiruppathi M, Rowin J, Li Jiang Q, Sheng JR, Prabhakar BS, Meriggioli MN. Functional defect in regulatory T cells in myasthenia gravis. Ann N Y Acad Sci. 2012;1274:68–76. doi: 10.1111/j.1749-6632.2012.06840.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gradolatto A, Nazzal D, Truffault F, Bismuth J, Fadel E, Foti M, Berrih-Aknin S. Both Treg cells and Tconv cells are defective in the myasthenia gravis thymus: roles of IL-17 and TNF-alpha. J Autoimmun. 2014;52:53–63. doi: 10.1016/j.jaut.2013.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Le Panse R, Cizeron-Clairac G, Cuvelier M, Truffault F, Bismuth J, Nancy P, De Rosbo NK, Berrih-Aknin S. Regulatory and pathogenic mechanisms in human autoimmune myasthenia gravis. Ann N Y Acad Sci. 2008;1132:135–142. doi: 10.1196/annals.1405.019. [DOI] [PubMed] [Google Scholar]
- 5.Ucar A, Ucar O, Klug P, Matt S, Brunk F, Hofmann TG, Kyewski B. Adult thymus contains FoxN1(−) epithelial stem cells that are bipotent for medullary and cortical thymic epithelial lineages. Immunity. 2014;41:257–269. doi: 10.1016/j.immuni.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lau CI, Yanez DC, Solanki A, Papaioannou E, Saldana JI, Crompton T. Foxa1 and Foxa2 in thymic epithelial cells (TEC) regulate medullary TEC and regulatory T-cell maturation. J Autoimmun. 2018;93:131–138. doi: 10.1016/j.jaut.2018.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guerder Sylvie, Hassel Chervin, Carrier Alice. Thymus-specific serine protease, a protease that shapes the CD4 T cell repertoire. Immunogenetics. 2018;71(3):223–232. doi: 10.1007/s00251-018-1078-y. [DOI] [PubMed] [Google Scholar]
- 8.Klein L, Kyewski B, Allen PM, Hogquist KA. Positive and negative selection of the T cell repertoire: what thymocytes see (and don't see) Nat Rev Immunol. 2014;14:377–391. doi: 10.1038/nri3667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ucar O, Rattay K. Promiscuous gene expression in the thymus: a matter of epigenetics, miRNA, and more? Front Immunol. 2015;6:93. doi: 10.3389/fimmu.2015.00093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yano M, Kuroda N, Han H, Meguro-Horike M, Nishikawa Y, Kiyonari H, Maemura K, Yanagawa Y, Obata K, Takahashi S, et al. Aire controls the differentiation program of thymic epithelial cells in the medulla for the establishment of self-tolerance. J Exp Med. 2008;205:2827–2838. doi: 10.1084/jem.20080046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson MS, Venanzi ES, Klein L, Chen Z, Berzins SP, Turley SJ, von Boehmer H, Bronson R, Dierich A, Benoist C, Mathis D. Projection of an immunological self shadow within the thymus by the aire protein. Science. 2002;298:1395–1401. doi: 10.1126/science.1075958. [DOI] [PubMed] [Google Scholar]
- 12.Beyersdorf N, Kerkau T, Hunig T. CD28 co-stimulation in T-cell homeostasis: a recent perspective. Immunotargets Ther. 2015;4:111–122. doi: 10.2147/ITT.S61647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williams JA, Zhang J, Jeon H, Nitta T, Ohigashi I, Klug D, Kruhlak MJ, Choudhury B, Sharrow SO, Granger L, et al. Thymic medullary epithelium and thymocyte self-tolerance require cooperation between CD28-CD80/86 and CD40-CD40L costimulatory pathways. J Immunol. 2014;192:630–640. doi: 10.4049/jimmunol.1302550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalluri R. The biology and function of exosomes in cancer. J Clin Invest. 2016;126:1208–1215. doi: 10.1172/JCI81135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kahlert C, Melo SA, Protopopov A, Tang J, Seth S, Koch M, Zhang J, Weitz J, Chin L, Futreal A, Kalluri R. Identification of double-stranded genomic DNA spanning all chromosomes with mutated KRAS and p53 DNA in the serum exosomes of patients with pancreatic cancer. J Biol Chem. 2014;289:3869–3875. doi: 10.1074/jbc.C113.532267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Azimi Maryam, Ghabaee Mojdeh, Moghadasi Abdorreza Naser, Noorbakhsh Farshid, Izad Maryam. Immunomodulatory function of Treg-derived exosomes is impaired in patients with relapsing-remitting multiple sclerosis. Immunologic Research. 2018;66(4):513–520. doi: 10.1007/s12026-018-9008-5. [DOI] [PubMed] [Google Scholar]
- 17.Kimura K, Hohjoh H, Fukuoka M, Sato W, Oki S, Tomi C, Yamaguchi H, Kondo T, Takahashi R, Yamamura T. Circulating exosomes suppress the induction of regulatory T cells via let-7i in multiple sclerosis. Nat Commun. 2018;9:17. doi: 10.1038/s41467-017-02406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang C, Robbins PD. Immunosuppressive exosomes: a new approach for treating arthritis. Int J Rheumatol. 2012;2012:573528. doi: 10.1155/2012/573528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez-Hernandez Javier, Redon Josep, Cortes Raquel. Extracellular Vesicles as Therapeutic Agents in Systemic Lupus Erythematosus. International Journal of Molecular Sciences. 2017;18(4):717. doi: 10.3390/ijms18040717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li H, Wang CC, Zhang M, Li XL, Zhang P, Yue LT, Miao S, Wang S, Liu Y, Li YB, Duan RS. Statin-modified dendritic cells regulate humoral immunity in experimental autoimmune myasthenia gravis. Mol Cell Neurosci. 2015;68:284–292. doi: 10.1016/j.mcn.2015.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Li XL, Liu Y, Cao LL, Li H, Yue LT, Wang S, Zhang M, Li XH, Dou YC, Duan RS. Atorvastatin-modified dendritic cells in vitro ameliorate experimental autoimmune myasthenia gravis by up-regulated Treg cells and shifted Th1/Th17 to Th2 cytokines. Mol Cell Neurosci. 2013;56:85–95. doi: 10.1016/j.mcn.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 22.Li XL, Li H, Zhang M, Xu H, Yue LT, Zhang XX, Wang S, Wang CC, Li YB, Dou YC, Duan RS. Exosomes derived from atorvastatin-modified bone marrow dendritic cells ameliorate experimental autoimmune myasthenia gravis by up-regulated levels of IDO/Treg and partly dependent on FasL/Fas pathway. J Neuroinflammation. 2016;13:8. doi: 10.1186/s12974-016-0475-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gray DH, Chidgey AP, Boyd RL. Analysis of thymic stromal cell populations using flow cytometry. J Immunol Methods. 2002;260:15–28. doi: 10.1016/S0022-1759(01)00493-8. [DOI] [PubMed] [Google Scholar]
- 24.Murphy KP, Travers P, Walport M, Janeway C. Janeway's immunobiology. 2014. [Google Scholar]
- 25.Akiyama T, Shimo Y, Yanai H, Qin J, Ohshima D, Maruyama Y, Asaumi Y, Kitazawa J, Takayanagi H, Penninger JM, et al. The tumor necrosis factor family receptors RANK and CD40 cooperatively establish the thymic medullary microenvironment and self-tolerance. Immunity. 2008;29:423–437. doi: 10.1016/j.immuni.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 26.Perry JSA, Lio CJ, Kau AL, Nutsch K, Yang Z, Gordon JI, Murphy KM, Hsieh CS. Distinct contributions of Aire and antigen-presenting-cell subsets to the generation of self-tolerance in the thymus. Immunity. 2014;41:414–426. doi: 10.1016/j.immuni.2014.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim SH, Lechman ER, Bianco N, Menon R, Keravala A, Nash J, Mi Z, Watkins SC, Gambotto A, Robbins PD. Exosomes derived from IL-10-treated dendritic cells can suppress inflammation and collagen-induced arthritis. J Immunol. 2005;174:6440–6448. doi: 10.4049/jimmunol.174.10.6440. [DOI] [PubMed] [Google Scholar]
- 28.Morelli AE, Larregina AT, Shufesky WJ, Sullivan ML, Stolz DB, Papworth GD, Zahorchak AF, Logar AJ, Wang Z, Watkins SC, et al. Endocytosis, intracellular sorting, and processing of exosomes by dendritic cells. Blood. 2004;104:3257–3266. doi: 10.1182/blood-2004-03-0824. [DOI] [PubMed] [Google Scholar]
- 29.Aline F, Bout D, Amigorena S, Roingeard P, Dimier-Poisson I. Toxoplasma gondii antigen-pulsed-dendritic cell-derived exosomes induce a protective immune response against T. gondii infection. Infect Immun. 2004;72:4127–4137. doi: 10.1128/IAI.72.7.4127-4137.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bu N, Wu HQ, Zhang GL, Zhan SQ, Zhang R, Fan QY, Li YL, Zhai YF, Ren HW. Immature dendritic cell exosomes suppress experimental autoimmune myasthenia gravis. J Neuroimmunol. 2015;285:71–75. doi: 10.1016/j.jneuroim.2015.04.009. [DOI] [PubMed] [Google Scholar]
- 31.Yin W, Ouyang S, Luo Z, Zeng Q, Hu B, Xu L, Li Y, Xiao B, Yang H. Immature exosomes derived from MicroRNA-146a overexpressing dendritic cells act as antigen-specific therapy for myasthenia gravis. Inflammation. 2017;40:1460–1473. doi: 10.1007/s10753-017-0589-2. [DOI] [PubMed] [Google Scholar]
- 32.Fontenot JD, Dooley JL, Farr AG, Rudensky AY. Developmental regulation of Foxp3 expression during ontogeny. J Exp Med. 2005;202:901–906. doi: 10.1084/jem.20050784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fontenot JD, Rasmussen JP, Williams LM, Dooley JL, Farr AG, Rudensky AY. Regulatory T cell lineage specification by the forkhead transcription factor foxp3. Immunity. 2005;22:329–341. doi: 10.1016/j.immuni.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 34.Akiyama T, Maeda S, Yamane S, Ogino K, Kasai M, Kajiura F, Matsumoto M, Inoue J. Dependence of self-tolerance on TRAF6-directed development of thymic stroma. Science. 2005;308:248–251. doi: 10.1126/science.1105677. [DOI] [PubMed] [Google Scholar]
- 35.Yang S, Fujikado N, Kolodin D, Benoist C, Mathis D. Immune tolerance. Regulatory T cells generated early in life play a distinct role in maintaining self-tolerance. Science. 2015;348:589–594. doi: 10.1126/science.aaa7017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lin J, Yang L, Silva HM, Trzeciak A, Choi Y, Schwab SR, Dustin ML, Lafaille JJ. Increased generation of Foxp3(+) regulatory T cells by manipulating antigen presentation in the thymus. Nat Commun. 2016;7:10562. doi: 10.1038/ncomms10562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aschenbrenner K, D'Cruz LM, Vollmann EH, Hinterberger M, Emmerich J, Swee LK, Rolink A, Klein L. Selection of Foxp3+ regulatory T cells specific for self antigen expressed and presented by Aire+ medullary thymic epithelial cells. Nat Immunol. 2007;8:351–358. doi: 10.1038/ni1444. [DOI] [PubMed] [Google Scholar]
- 38.Poliani PL, Facchetti F, Ravanini M, Gennery AR, Villa A, Roifman CM, Notarangelo LD. Early defects in human T-cell development severely affect distribution and maturation of thymic stromal cells: possible implications for the pathophysiology of Omenn syndrome. Blood. 2009;114:105–108. doi: 10.1182/blood-2009-03-211029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laakso SM, Laurinolli TT, Rossi LH, Lehtoviita A, Sairanen H, Perheentupa J, Kekalainen E, Arstila TP. Regulatory T cell defect in APECED patients is associated with loss of naive FOXP3(+) precursors and impaired activated population. J Autoimmun. 2010;35:351–357. doi: 10.1016/j.jaut.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 40.Kekalainen E, Tuovinen H, Joensuu J, Gylling M, Franssila R, Pontynen N, Talvensaari K, Perheentupa J, Miettinen A, Arstila TP. A defect of regulatory T cells in patients with autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy. J Immunol. 2007;178:1208–1215. doi: 10.4049/jimmunol.178.2.1208. [DOI] [PubMed] [Google Scholar]
- 41.Haljasorg U, Bichele R, Saare M, Guha M, Maslovskaja J, Kond K, Remm A, Pihlap M, Tomson L, Kisand K, et al. A highly conserved NF-kappaB-responsive enhancer is critical for thymic expression of Aire in mice. Eur J Immunol. 2015;45:3246–3256. doi: 10.1002/eji.201545928. [DOI] [PubMed] [Google Scholar]
- 42.Gray DH, Seach N, Ueno T, Milton MK, Liston A, Lew AM, Goodnow CC, Boyd RL. Developmental kinetics, turnover, and stimulatory capacity of thymic epithelial cells. Blood. 2006;108:3777–3785. doi: 10.1182/blood-2006-02-004531. [DOI] [PubMed] [Google Scholar]
- 43.Caux C, Massacrier C, Vanbervliet B, Dubois B, Van Kooten C, Durand I, Banchereau J. Activation of human dendritic cells through CD40 cross-linking. J Exp Med. 1994;180:1263–1272. doi: 10.1084/jem.180.4.1263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Oh J, Wu N, Barczak AJ, Barbeau R, Erle DJ, Shin JS. CD40 mediates maturation of Thymic dendritic cells driven by self-reactive CD4(+) Thymocytes and supports development of natural regulatory T cells. J Immunol. 2018;200:1399–1412. doi: 10.4049/jimmunol.1700768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Spence PJ, Green EA. Foxp3+ regulatory T cells promiscuously accept thymic signals critical for their development. Proc Natl Acad Sci U S A. 2008;105:973–978. doi: 10.1073/pnas.0709071105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are available on request.