Abstract
Background:
Coronary artery calcium (CAC) has been shown in multiple populations to predict atherosclerotic cardiovascular disease (ASCVD). However, its predictive value in Asian-Americans is poorly described.
Methods:
We studied 1621 asymptomatic Asian-Americans (predominantly East and Southeast Asians) in the CAC Consortium, a large multi-center retrospective cohort. CAC was modelled in categorical (CAC 0; CAC 1–99; CAC 100–399; CAC≥400) and continuous [ln (CAC+1)] forms. Participants were followed over a mean follow-up of 12±4 years for coronary heart disease (CHD) death, cardiovascular disease (CVD) death, and all-cause mortality. The predictive value of CAC for individual outcomes was assessed using multivariable-adjusted Cox regression models adjusted for traditional cardiovascular risk factors and reported as hazard ratios (95% confidence interval).
Results:
The mean (SD) age of the population was 54 (11.2) years and 64% were men. The mean 10-year ASCVD risk score was 8%. Approximately half had a CAC score=0, while 22.5% had a CAC score >100. A total of 56 deaths (16 CVD, 8 CHD) were recorded, with no CVD or CHD deaths in the CAC=0 group. We noted significantly increased risk of CHD [HR 2.6 (1.5 – 4.3)] and CVD [HR 2.3 (1.8–2.9)] mortality per unit increase in loge (CAC+1). Compared to CAC=0, individuals with CAC ≥ 400 had over 3-fold increased risk of all-cause mortality (HR 3.3 (1.3–8.6)).
Conclusion:
While Asian-Americans are a relatively low risk group, CAC strongly predicts CHD, CVD and all-cause mortality beyond traditional risk factors. These findings may help address existing knowledge gaps in CVD risk prediction in Asian-Americans.
Keywords: coronary artery calcium score, race/ethnicity, Asian Americans, risk prediction
INTRODUCTION
Atherosclerotic cardiovascular disease (ASCVD) risk prediction tools occupy a central place in guiding primary prevention therapies.[1–3] The USPSTF and 2013 ACC/AHA guidelines recommend using the Pooled Cohort Equations (PCE) for guiding patient selection for aspirin, statin and blood pressure therapies.[1,2,4] However, studies have shown that the PCE, which recommend the use of Non-Hispanic White equations for non-black ethnic minorities, may overestimate cardiovascular risk, including in Asian-Americans.[5] Being a population-based probabilistic model, these described limitations of the PCE are mostly inherent to the ethnic compositions of the population from which these equations were originally derived. The overestimation of risk in Asian-Americans may contribute to over-treatment with preventive pharmacotherapies, with resultant increase in medical costs and possible unnecessary burden of side effects from medications. There is therefore a need to balance risk-benefit by ensuring more accurate risk prediction either through recalibration of existing risk scores or through enhancements to include novel risk markers capable of reclassifying individuals beyond existing tools.[6]
Based on extensive evidence accrued over the last decade, coronary artery calcium (CAC) scoring has emerged as a novel, cost-effective, and more direct estimation of CVD risk with proven utility across different sociodemographic and clinical phenotypes.[7–12] CAC has been demonstrated as the most robust predictor of coronary events in the asymptomatic primary prevention population, especially among intermediate-risk individuals.[13] Therefore, CAC has potential value as a tool for overcoming limitations in risk prediction in populations not adequately represented in the PCE. However, despite broad evidence showing the predictive value of CAC in multiple population-based and clinical cohorts, and recent guideline recommendations favoring the selective use of CAC for advanced risk stratification,[14] few studies have specifically assessed the predictive value of CAC in Asian-Americans, a rapidly growing, but yet, underrepresented ethnic sub-population in the United States.[15,16] We therefore sought to assess the predictive utility of CAC for CHD, CVD and all-cause mortality outcomes in Asian-Americans utilizing data from the CAC Consortium, a large observational cohort of clinical CAC scoring.
METHODS
Study design and study population
The CAC Consortium is a multicenter, prospective, clinical observational cohort of 66,636 patients designed to rigorously investigate the relationship between CAC and cause-specific mortality, particularly in understudied groups.[17] Four participating institutions from 3 states in the United States (Ohio, Minnesota and California) with over 10 years of experience in clinical CAC scoring contributed patient data to the CAC Consortium. Participants consisted of adults aged at least 18 years without cardiovascular disease at baseline who were clinically referred for CAC scoring. Baseline data for the CAC Consortium represent the years 1991 – 2010 and follow-up extended until June 2014. Consent was obtained from each study participant at the time of CAC scanning, and IRB approval for coordinating center activities was obtained at the Johns Hopkins University School of Medicine.
For this analysis, we included 1621 participants of the CAC Consortium who identified as Asian-Americans. Asian-Americans (predominantly East Asians and Southeast Asians) were contributed to the CAC Consortium by the Harbor-UCLA Medical Center, Torrance, CA (n= 1093, 67%), Cedars-Sinai Medical Center, Los Angeles, CA (n=363, 22%) and the Minneapolis Heart Institute (n=165, 10%). Patient-level data on demographics, cardiovascular risk factors and medications were collected through semi-structured interviews at clinical visits associated with the referral for CAC testing and/or from established diagnoses recorded in the electronic medical records.[17]
Definition of risk factors
Hypertension was defined as a prior diagnosis of hypertension or treatment with anti-hypertensive therapy. Blood pressure measurements taken at the time of visit was not used to override a diagnosis of hypertension. Dyslipidemia was defined as a prior diagnosis of primary hyperlipidemia, the presence of elevated triglycerides and/or low HDL-C, or treatment with any lipid-lowering drug. Additionally, dyslipidemia was also considered present if LDL-C >160 mg/dL, HDL-C <40 mg/dL in men and <50 mg/dL in women, or fasting triglycerides>150mg/dL were recorded. Current smoking was defined as a dichotomous (yes/no) variable. Diabetes was defined as prior diagnosis of diabetes or treatment with oral hypoglycemic drugs or insulin. Family history of CHD was defined as the presence of a first degree relative with a history of CHD. Multiple imputation was conducted in the case of partially missing risk factor data in the CAC Consortium, with imputation done according to a multivariable model adjusting for age, sex, race, CAC score, and the remaining non-missing traditional risk factor data. The 10-year ASCVD risk score was calculated in all patients according to the Pooled Cohort Equations. Details of the process of estimation of ASCVD risk and the validation of the imputation approach have been previously described.[17]
Coronary artery calcium scoring
All participants in the CAC Consortium underwent non-contrast cardiac-gated computed tomography (CT) scans for CAC scoring at individual sites. Scanning was done according to a common standard protocol for each scanner technology used. About 93% of patients were scanned using electron beam tomography, while more recent data was obtained using multi-detector CT (accounting for approximately 7% of scans). Studies have shown no clinically meaningful differences between both scanner technologies.[18] CAC groups were defined as CAC 0, CAC 1–99, CAC 100–399, and CAC ≥400.[19]
Outcome ascertainment
Participants were followed over a mean duration of 12 ± 4 years for CHD, CVD and all-cause mortality. Ascertainment of death was done through linkage to the Social Security Death Index (SSDI) Death Master File via a previously validated algorithm, similar to the National Death Index (NDI) Service.[17] Specific causes of death were then obtained through coded death certificates obtained from the NDI and reported as ICD-9 and ICD-10 codes. CVD mortality was defined as death from CHD, stroke, heart failure and other circulatory diseases. Other details of mortality ascertainment have been extensively described.[17]
Statistical methods
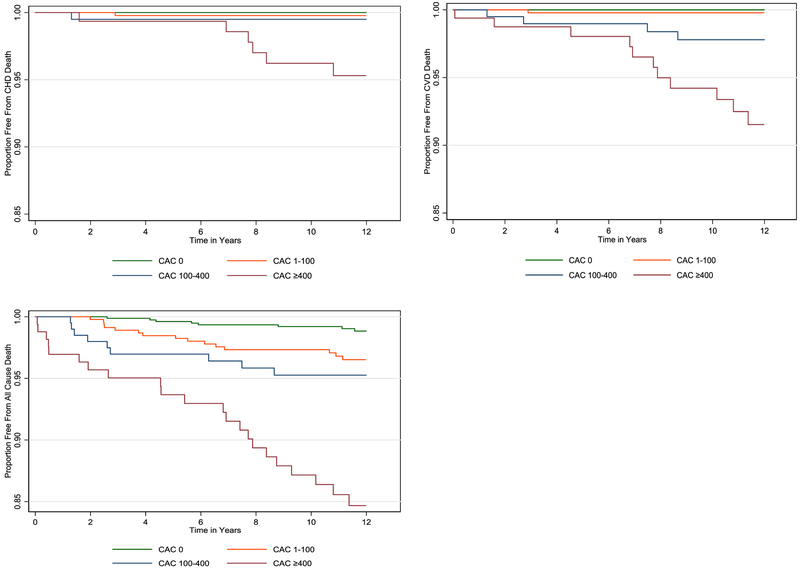
Baseline characteristics were summarized by CAC score categories, with means and proportions reported for continuous and categorical variables respectively. Differences in baseline characteristics across categories of CAC were tested using chi-square and ANOVA tests as appropriate. To examine the distribution of all-cause and cause-specific mortality outcomes across CAC groups, we first calculated the cumulative incidence of all-cause, CVD and CHD deaths within each CAC category. We then calculated the incidence rates of specific outcomes by CAC group, expressed per 1000 person-years. Additionally, we generated Kaplan-Meier survival curves for specific outcomes stratified by CAC group. Differences between survival curves were tested using log-rank statistics.
To assess the predictive value of CAC in this population, we utilized multivariable-adjusted Cox proportional hazards regression models to estimate hazard ratios for all-cause, CVD and CHD mortality, handling CAC in categorical and continuous (Loge(CAC+1) forms. The addition of 1 to the absolute calcium score before logarithmic transformation, as has been done in previous studies[9], allowed us to account for patients with a CAC score of zero. Multivariable-adjusted models were adjusted for age, sex, hypertension, diabetes mellitus, smoking status, family history of CHD, and hyperlipidemia in all analyses.
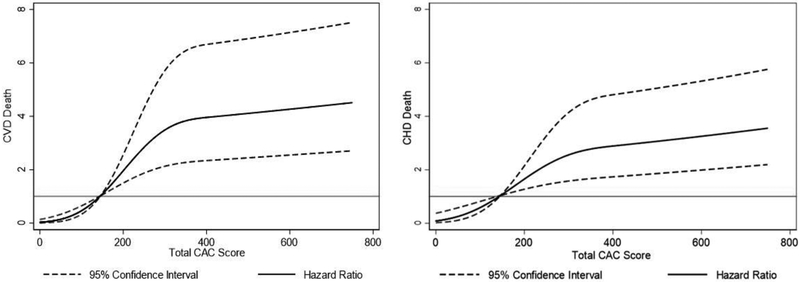
Due to the absence of CHD and CVD deaths in the CAC=0 group over the duration of follow-up, we could not model CHD and CVD mortality risk by CAC categories. However, to understand the relationship between CAC and CHD and CVD mortality risk, we handled CAC as a continuous variable for these analyses. To accomplish this, we first estimated, in Fine and Gray subdistribution hazards models, the multivariable-adjusted risk of CHD and CVD mortality per unit increase in Log (CAC+1). We then constructed graphical cubic spline models to visualize the direction, strength and shape of this relationship,[20] plotting the total CAC score on the x-axis and multivariable adjusted hazard ratios of CHD and CVD mortality on the y-axis. Because of the limited number of CHD and CVD events with CAC scores < 100, we centered these cubic spline graphs at CAC=100. Cubic spline models were fully adjusted for traditional cardiovascular risk factors including age, sex, hypertension, diabetes mellitus, smoking status, family history of CHD and hyperlipidemia.
All analyses were performed with Stata software version 14.2 (College Station, TX)
RESULTS
Baseline characteristics
Table 1 shows the distribution of baseline characteristics by CAC group. The mean (SD) age of the population was 53.8 (11.2) years, with 63.7% men. Approximately half of the study sample had a CAC score of zero, 22.5% had CAC scores over 100, while only 10% had CAC scores ≥ 400. Overall, there was a 58.9% prevalence of hyperlipidemia in the study population. Compared with subjects with CAC scores less than 100, those with CAC scores >100 were more likely to be older, men, cigarette smokers, and to have hypertension, diabetes, and hyperlipidemia.
Table 1:
Baseline characteristics of study population.
| Overall (N=1621) |
CAC 0 (n=794) |
CAC 1 – 100 (n=463) |
CAC 100 – 400 (n=200) |
CAC ≥ 400 (n=164) |
|
|---|---|---|---|---|---|
| Mean age (SD), years | 53.8 (11.2) | 48.9 (9.4) | 55.0 (10.0) | 60.9 (10.4) | 65.7 (9.1) |
| Men (n, %) | 1032, 63.6 | 414, 52.1 | 338, 73.0 | 149, 74.5 | 131, 79.9 |
| Hypertension (n, %) | 602, 37.1 | 182, 22.9 | 200, 43.2 | 120, 60.0 | 100, 61.0 |
| Diabetes Mellitus (n, %) | 190, 11.7 | 50, 6.3 | 55, 11.9 | 29, 14.5 | 56, 34.2 |
| Hyperlipidemia (n, %) | 955, 58.9 | 405, 51.0 | 293, 63.2 | 138, 69.0 | 119, 72.6 |
| Cigarette smoking (n, %) | 122, 7.5 | 62, 7.8 | 28, 6.1 | 17, 8.5 | 15, 9.2 |
| Family history of CHD (n, %) | 738, 45.5 | 347, 43.7 | 219, 47.3 | 96, 48.0 | 76, 46.3 |
|
Number of risk factors (n, %) • 0 • 1 • ≥ 2 |
264, 16.3 500, 30.9 857, 52.9 |
185, 23.3 278, 35.0 331, 41.7 |
52, 11.2 145, 31.3 266, 57.5 |
15, 7.5 50, 25.0 135, 67.5 |
12, 7.3 27, 16.5 125,76.2 |
| Mean (SD) ASCVD risk score (%) | 8.0 (10.2) | 3.8 (5.0) | 8.0 (8.4) | 13.7 (12.6) | 21.2 (15.2) |
|
ASCVD risk category • <5% • 5 – 7.5% • ≥7.5% |
914, 56.3 193, 11.9 514, 31.7 |
620, 78.1 72, 9.1 102, 12.9 |
228, 49.2 75, 16.2 160, 34.6 |
47, 23.5 37, 18.5 116, 58.0 |
19, 11.6 9, 5.5 136, 82.9 |
The mean 10-year ASCVD risk score was 8.0% (10.2), with 56.3% having an ASCVD risk score of <5%. Overall, 31.7% of participants had ASCVD risk scores greater than 7.5%. Of the 514 participants with ASCVD risk scores >7.5%, 102 (20%) had CAC=0, while only 7% of those in the <5% ASCVD risk category had CAC scores >100. (Table 1)
All-cause, CVD and CHD mortality rates by CAC group.
Over a mean (SD) follow-up duration of 12 (4) years, 56 deaths (16 CVD, 8 CHD) were recorded. There were no CHD or CVD deaths recorded in the CAC=0 group. For all outcomes, we noted an increase in the incidence of mortality with increasing CAC group. An incidence rate of 0.93 (0.48 – 1.80) deaths per thousand person-years was noted in the CAC 0 group, while a markedly higher incidence rate of 12.6 (8.3 – 19.2) was noted in the CAC ≥400 group. Similarly elevated incidence rates of CHD [3.4 (1.6 −7.7)] and CVD [6.3 (3.5 – 11.4)] mortality was noted in the CAC ≥400 category. (Supplementary Table 2) Kaplan-Meier curves showed statistically significant graded survival by CAC category for all outcomes under consideration. (Figure 1)
Figure 1:
Kaplan-Meier survival curves for CHD, CVD and all-cause mortality.
Predictive value of CAC for all-cause, CHD and CVD mortality.
In multivariable-adjusted models adjusted for traditional cardiovascular risk factors, increasing hazards of all-cause mortality were noted with increasing categories of CAC. Individuals with CAC > 400 had approximately 3 times the risk of all-cause mortality compared to the CAC=0 group [HR 3.3 (1.3 – 8.6)]. (Table 3) Similarly, we noted significant increases in risk of CVD [HR 2.3 (1.8 – 2.9)] and CHD [HR 2.6 (1.5 – 4.3)] mortality per unit increase in log (CAC + 1). As shown in Figure 2, cubic spline graphs of the relationship between total CAC score (centered at CAC=100) and risk of CVD and CHD mortality showed a graded positive relationship between risk and total CAC with a steep gradient between CAC scores of 100 and 400 which levels off beyond CAC >400. Beyond CAC scores of 400, the risk gradient is steeper for CVD than CHD mortality risk.
Table 3.
Unadjusted and multivariable-adjusted risk of CVD and CHD mortality per unit increase in Ln (CAC+1).
| Unadjusted SHR (95 % CI) |
Fully adjusted SHR (95% CI) |
|
|---|---|---|
| CVD mortality | 2.3 (1.8 – 3.0) | 2.3 (1.8 – 2.9) |
| CHD mortality | 2.6 (1.5 – 4.5) | 2.6 (1.5 – 4.3) |
Fully adjusted models adjusted for age, sex, hypertension, diabetes mellitus, smoking, family history of CHD and hyperlipidemia.
Figure 2.
Cubic spline graphs of multivariable-adjusted hazards of CVD and CHD death with increasing CAC scores, centered at CAC = 100.
DISCUSSION
In a large retrospective cohort of Asian-Americans, we confirmed CAC to be a strong predictor of CHD, CVD and all-cause mortality, beyond traditional cardiovascular risk factors. Our results are important as we demonstrate that in spite of their general low risk nature, CAC remains a useful tool for CVD risk prediction in this population.
Asian-Americans represent the fastest growing ethnicity group in the United States, projected to reach nearly 34 million by the year 2050.[21,22] Despite this, no tool is specifically designed to predict ASCVD risk in this population, with the 2013 ACC/AHA guidance on assessment of cardiovascular risk recommending the use of NHW equations in the absence of good evidence.[23] Since this approach overestimates risk in Asian-Americans, with attendant consequences for the judicious use of statin, aspirin and antihypertensive therapy,[5,24]our demonstration of the predictive value of CAC in this population is timely and has clear implications for clinical practice guidelines, given the superior risk discrimination and risk reclassification of CAC when compared to other novel risk markers.[7,25,26]
Previous studies evaluating CAC in Asian-Americans have been mostly cross-sectional assessments of its prevalence,[15] distribution across subgroups and association with cardiovascular risk factors in South-Asian subpopulations of Asian-Americans.[15,27] For example, Patel et al (2017) showed associations between severe CAC and family history of CHD independent of cardiovascular risk factors,[28] while Talegawker et al (2017) showed associations between ideal cardiovascular health metrics and subclinical atherosclerosis as assessed by CAC.[29]
There have been a few prospective studies assessing the predictive value of CAC in Asian-Americans. Nasir et al (2007) in assessing ethnic differences in the prognostic value of CAC for all-cause mortality implicitly assessed the predictive value of CAC for all-cause death in Asian-Americans.[10] However, these studies were conducted in the pre-PCE era, and were not adequately powered to assess CVD and CHD mortality outcomes.
In the Multi-Ethnic Study of Atherosclerosis (MESA), perhaps the largest population-based prospective study of CAC scoring to date, Detrano et al (2008) and Budoff et al (2018) have independently showed the value of CAC for ASCVD risk prediction in a population-based asymptomatic Multi-Ethnic cohort over median follow up durations of 3.9 years and 11-years, respectively.[9,30] Their sample of Asian-Americans was, however, restricted to Chinese-American participants and they therefore did not assess the overall utility of CAC in a more general Asian-American population. Additionally, since MESA represents a population-based cohort, the results may not be telling of the utility of CAC in a clinically-referred population. Furthermore, these studies assessed ASCVD events only and not mortality events. To our knowledge, our study represents the first clinical cohort-based assessment of the predictive value of CAC for CHD and CVD mortality outcomes in a hitherto understudied US census-defined population of Asian-Americans.
Importantly, we also found in this overall low-risk Asian-American population that as reported in previous studies, the absence of CAC identifies an extremely low-risk phenotype, as demonstrated by the markedly low event rates in the CAC=0 group.[31,32] We noted in the present study, a 0.93 per 1000 person-year incidence rate of all-cause mortality, and no incident CVD or CHD mortality in the CAC 0 group over a mean follow-up duration of 12 years. These findings are instructive as they suggest that the absence of CAC may be a useful tool to identify very low-risk Asian-Americans who are being over treated under the current PCE recommendations. Identifying this extreme low-risk phenotype is important, as studies have shown that Asians have a higher risk of statin associated diabetes mellitus and statin-associated muscle symptoms at the same statin doses compared to Caucasians.[33]
In line with major guidelines and expert consensus documents,[34,35] we believe CAC should be considered in the clinical decision making process in Asian-Americans especially when the estimation of ASCVD risk is deemed to be intermediate based on the PCE (5–20% 10-year ASCVD risk) or when the decision to treat with statins is unclear to the patient or clinician.[14]. Additionally, CAC can also be independently utilized as a guide for the clinicians in their decisions about preventive therapies including aspirin,[36] statins[37] and antihypertensive[38] treatment.
Limitations
Our study has a few limitations. First, given the fact that the CAC Consortium represents a clinical cohort, our findings may not be generalizable to a general “screening” population. However, since CAC is not a population screening tool, these results are representative of “real-world” Asian-Americans who are likely to be considered for CAC scanning in everyday clinical practice settings. Second, the CAC Consortium does not have a deeper phenotyping of Asian-Americans and subpopulation-specific risk estimates could therefore not be assessed. However, as demonstrated in Supplemental Table 1, majority of the Asian-Americans across geographical locations of study sites (based on the 2000 census estimates) were East Asians and South-East Asians, which are a lower risk group compared to South Asians. Therefore, while our results may be less generalizable to high-risk South Asians, our results are representative of low-risk Asian-Americans who may benefit from risk reclassification, given the aforementioned overestimation of risk in the East-Asian and South-East Asian sub-population. Third, given the absence of CHD and CVD mortality in the CAC=0 group, we could not obtain estimates of CHD and CVD risk by CAC categories. However, the assessment of risk on a continuous log-transformed scale has been routinely used to assess the utility of CAC in risk prediction models, particularly when statistical power is limited.[9,39] Fourth, given the lack of continuous data on risk factors, there may exist the possibility of some residual confounding. Finally, given the clinical nature of our cohort, results of patient’s CAC scores may have differentially influenced behavior and treatment in favor of participants with high CAC scores. However, we expect that this would bias our estimates towards the null and that our effect estimates with increasing CAC may therefore be conservative.
Conclusion
We conclude that in an appropriately referred asymptomatic clinical population of Asian-Americans, CAC is strongly predictive of CHD, CVD and all-cause mortality. These findings may help address the existing knowledge gaps for cardiovascular risk prediction in Asian-Americans, and reinforces the extension of the clinical value of CAC scoring in this population as well.
Supplementary Material
Table 2:
Unadjusted and multivariable-adjusted risk of all-cause mortality, by CAC group.
| Unadjusted HR (95% CI) |
Fully adjusted HR (95% CI) |
|
|---|---|---|
| CAC 0 | REF | REF |
| CAC 1 – 100 | 2.9 (1.3 – 6.6) | 1.8 (0.7 – 4.2) |
| CAC 100 – 400 | 4.7 (1.9 – 11.5) | 1.7 (0.6 – 4.6) |
| CAC ≥ 400 | 13.4 (6.2 – 29.2) | (1.3 – 8.6) |
| • Ln (CAC + 1) | 1.5 (1.3 – 1.6) | 1.2 (1.1 – 1.4) |
Fully adjusted models adjusted for age, sex, hypertension, diabetes mellitus, smoking, family history of CHD and hyperlipidemia.
ACKNOWLEDGEMENTS
Dr. Blaha reports grants from NIH award L30 HL110027 for this project. All other authors have no relevant sources of funding to report.
REFERENCES.
- [1].Stone N, Robinson J, Lichtenstein A, Bairey C, Blum C, Eckel R, et al. 2013. ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults. Circulation 2013:1–85. doi: 10.1161/01.cir.0000437738.63853.7a. [DOI] [Google Scholar]
- [2].Bibbins-Domingo K Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2016;164:836. doi: 10.7326/M16-0577. [DOI] [PubMed] [Google Scholar]
- [3].Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, et al. 2017. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Pr. J Am Coll Cardiol 2017:24430. [Google Scholar]
- [4].Pk W, Carey RM, Aronow WS, Ovbiagele B, Casey DE, Smith SC, et al. 2017. Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults A Report of the American College of Cardiology / American Heart Association T. 2017. doi: 10.1161/HYP.0000000000000065/-/DC1. [DOI]
- [5].Rana JS, Tabada GH, Solomon MD, Lo JC, Jaffe MG, Sung SH, et al. Accuracy of the Atherosclerotic Cardiovascular Risk Equation in a Large Contemporary, Multiethnic Population. J Am Coll Cardiol 2016;67:2118–30. doi: 10.1016/j.jacc.2016.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cook NR, Ridker PM. Calibration of the pooled cohort equations for atherosclerotic cardiovascular disease: An update. Ann Intern Med 2016;165:786–94. doi: 10.7326/M16-1739. [DOI] [PubMed] [Google Scholar]
- [7].Yeboah J, Young R, McClelland RL, Delaney JC, Polonsky TS, Dawood FZ, et al. Utility of Nontraditional Risk Markers in Atherosclerotic Cardiovascular Disease Risk Assessment. J Am Coll Cardiol 2016;67:139–47. doi: 10.1016/j.jacc.2015.10.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].McClelland RL, Jorgensen NW, Budoff M, Blaha MJ, Post WS, Kronmal RA, et al. 10-Year Coronary Heart Disease Risk Prediction Using Coronary Artery Calcium and Traditional Risk Factors Derivation in the MESA (Multi-Ethnic Study of Atherosclerosis) with Validation in the HNR (Heinz Nixdorf Recall) Study and the DHS (Dallas Heart Stud. J Am Coll Cardiol 2015;66:1643–53. doi: 10.1016/j.jacc.2015.08.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336–45. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- [10].Nasir K, Shaw LJ, Liu ST, Weinstein SR, Mosler TR, Flores PR, et al. Ethnic Differences in the Prognostic Value of Coronary Artery Calcification for All-Cause Mortality. J Am Coll Cardiol 2007;50:953–60. doi: 10.1016/j.jacc.2007.03.066. [DOI] [PubMed] [Google Scholar]
- [11].Tota-Maharaj R, Blaha MJ, McEvoy JW, Blumenthal RS, Muse ED, Budoff MJ, et al. Coronary artery calcium for the prediction of mortality in young adults <45 years old and elderly adults >75 years old. Eur Heart J 2012;33:2955–62. doi: 10.1093/eurheartj/ehs230. [DOI] [PubMed] [Google Scholar]
- [12].Patel J, Blaha MJ, McEvoy JW, Qadir S, Tota-Maharaj R, Shaw LJ, et al. All-cause mortality in asymptomatic persons with extensive Agatston scores above 1000. J Cardiovasc Comput Tomogr 2014;8:26–32. doi: 10.1016/j.jcct.2013.12.002. [DOI] [PubMed] [Google Scholar]
- [13].Hecht HS. Coronary Artery Calcium ScanningPast, Present, and Future. JACC Cardiovasc Imaging 2015;8:579–96. doi: 10.1016/j.jcmg.2015.02.006. [DOI] [PubMed] [Google Scholar]
- [14].GS M, SN J, BA L, Craig, BK. BK, S. BR, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol. Circulation 2018;0:CIR.0000000000000625. doi: 10.1161/CIR.0000000000000625. [DOI] [Google Scholar]
- [15].Kanaya AM, Kandula NR, Ewing SK, Herrington D, Liu K, Blaha MJ, et al. Comparing coronary artery calcium among U.S. South Asians with four racial/ethnic groups: The MASALA and MESA studies. Atherosclerosis 2014;234:102–7. doi: 10.1016/j.atherosclerosis.2014.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Hecht HS, Blaha MJ, Kazerooni EA, Cury RC, Budoff M, Leipsic J, et al. CAC-DRS: Coronary Artery Calcium Data and Reporting System. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT). J Cardiovasc Comput Tomogr 2018;12:185–91. doi: 10.1016/J.JCCT.2018.03.008. [DOI] [PubMed] [Google Scholar]
- [17].Blaha MJ, Whelton SP, Al Rifai M, Dardari ZA, Shaw LJ, Al-Mallah MH, et al. Rationale and design of the coronary artery calcium consortium: A multicenter cohort study. J Cardiovasc Comput Tomogr 2016;11:54–61. doi: 10.1016/j.jcct.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mao SS, Pal RS, McKay CR, Gao YG, Gopal A, Ahmadi N, et al. Comparison of coronary artery calcium scores between electron beam computed tomography and 64-multidetector computed tomographic scanner. J Comput Assist Tomogr 2009;33:175–8. doi: 10.1097/RCT.0b013e31817579ee. [DOI] [PubMed] [Google Scholar]
- [19].Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: The St. Francis heart study. J Am Coll Cardiol 2005. doi: 10.1016/j.jacc.2005.02.088. [DOI] [PubMed] [Google Scholar]
- [20].Durrleman S, Simon R. Flexible regression models with cubic splines. Stat Med 1989;8:551–61. doi: 10.1002/sim.4780080504. [DOI] [PubMed] [Google Scholar]
- [21].Jose PO, Frank ATH, Kapphahn KI, Goldstein BA, Eggleston K, Hastings KG, et al. Cardiovascular Disease Mortality in Asian Americans. J Am Coll Cardiol 2014;64:2486–94. doi: 10.1016/J.JACC.2014.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hoeffel EM, Rastogi S, Kim MO, Shahid H. The Asian Population: 2010 2010 Census Briefs 2012.
- [23].Goff DC, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, et al. 2013 ACC/AHA Guideline on the Assessment of Cardiovascular Risk. J Am Coll Cardiol 2014;63:2935 LP–2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Ko MJ, Kim YJ, Park CM, Lee SM, Lee WJ, Pencina MJ, et al. Applicability and potential clinical effects of 2013 cholesterol guidelines on major cardiovascular events. Am Heart J 2015;170:598–605.e7. doi: 10.1016/j.ahj.2015.06.012. [DOI] [PubMed] [Google Scholar]
- [25].McEvoy JW, Nasir K, Defilippis AP, Lima JAC, Bluemke DA, Hundley WG, et al. Relationship of cigarette smoking with inflammation and subclinical vascular disease: The multi-ethnic study of atherosclerosis. Arterioscler Thromb Vasc Biol 2015;35:1002–10. doi: 10.1161/ATVBAHA.114.304960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O’Leary D, et al. Comparison of Novel Risk Markers for Improvement in Cardiovascular Risk Assessment in Intermediate-Risk Individuals. JAMA 2012;308:788. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Mehta A, Patel J, Al Rifai M, Ayers CR, Neeland IJ, Kanaya AM, et al. Inflammation and coronary artery calcification in South Asians: The Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis 2018;270:49–56. doi: 10.1016/J.ATHEROSCLEROSIS.2018.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Patel J, Al Rifai M, Cainzos-Achirica M, Kandula NR, Kanaya AM, Khera A, et al. Family History of CHD Is Associated With Severe CAC in South Asians: Comparing the MASALA and MESA Studies. JACC Cardiovasc Imaging 2017;10:958–60. doi: 10.1016/j.jcmg.2017.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Talegawkar SA, Jin Y, Kandula NR, Kanaya AM. Cardiovascular health metrics among South Asian adults in the United States: Prevalence and associations with subclinical atherosclerosis. Prev Med (Baltim) 2017;96:79–84. doi: 10.1016/j.ypmed.2016.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Budoff MJ, Young R, Burke G, Jeffrey Carr J, Detrano RC, Folsom AR, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J 2018:ehy217–ehy217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Blaha M, Budoff MJ, Shaw LJ, Khosa F, Rumberger JA, Berman D, et al. Absence of Coronary Artery Calcification and All-Cause Mortality. JACC Cardiovasc Imaging 2009;2:692–700. doi: 10.1016/j.jcmg.2009.03.009. [DOI] [PubMed] [Google Scholar]
- [32].Valenti, VÓ Hartaigh B, Heo R, Cho I, Schulman-Marcus J, Gransar H, et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: A prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 2015;8:900–9. doi: 10.1016/j.jcmg.2015.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Thompson PD, Panza G, Zaleski A, Taylor B. Statin-associated side effects. J Am Coll Cardiol 2016. doi: 10.1016/j.jacc.2016.02.071. [DOI] [PubMed] [Google Scholar]
- [34].Greenland P, Blaha MJ, Budoff MJ, Erbel R, Watson KE. Coronary Calcium Score and Cardiovascular Risk. J Am Coll Cardiol 2018;72:434 LP–447. doi: 10.1016/J.JACC.2018.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Hecht H, Blaha MJ, Berman DS, Nasir K, Budoff M, Leipsic J, et al. Clinical indications for coronary artery calcium scoring in asymptomatic patients: Expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 2017;11:157–68. doi: 10.1016/J.JCCT.2017.02.010. [DOI] [PubMed] [Google Scholar]
- [36].Miedema MD, Duprez DA, Misialek JR, Blaha MJ, Nasir K, Silverman MG, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: Estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 2014;7:453–60. doi: 10.1161/CIRCOUTCOMES.113.000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Nasir K, Bittencourt MS, Blaha MJ, Blankstein R, Agatson AS, Rivera JJ, et al. Implications of Coronary Artery Calcium Testing among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2015;66:1657–68. doi: 10.1016/j.jacc.2015.07.066. [DOI] [PubMed] [Google Scholar]
- [38].McEvoy JW, Martin SS, Dardari ZA, Miedema MD, Sandfort V, Yeboah J, et al. Coronary Artery Calcium to Guide a Personalized Risk-Based Approach to Initiation and Intensification of Antihypertensive Therapy. Circulation 2017;135:153–65. doi: 10.1161/CIRCULATIONAHA.116.025471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Budoff MJ, Young R, Burke G, Jeffrey Carr J, Detrano RC, Folsom AR, et al. Ten-year association of coronary artery calcium with atherosclerotic cardiovascular disease (ASCVD) events: the multi-ethnic study of atherosclerosis (MESA). Eur Heart J 2018:ehy217–ehy217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.