Abstract
Radiation therapy with permanent iodine-125 implant brachytherapy is well established for curable prostate cancer. To maximize the therapeutic potential of brachytherapy, delivered radiation doses have been increased accompanied by refined intraoperative procedures of radioactive seeds placement. However, dose escalation is a double-edged sword in prostate brachytherapy; it could induce rectal toxicity, yet is successful in curable treatment in prostate cancer. To reduce irradiation of the rectum, the SpaceOAR® system has been used to inject synthetic polyethylene glycol hydrogel between the prostate and the rectum. The present report describes a case of spontaneous healing of rectal penetration associated with SpaceOAR® hydrogel.
Keywords: permanent iodine-125 implant brachytherapy, SpaceOAR® hydrogel, rectal penetration, magnetic resonance imaging, spontaneous healing
Introduction
Permanent iodine-125 implant brachytherapy (PI) with or without external beam radiotherapy (EBRT) is a standard, definitive radiotherapy for localized prostate cancer. As the intraoperative placement of PI seeds has been refined, delivered radiation doses have increased, thus maximizing the therapeutic potential of PI (1). However, the escalation of local radiation doses can potentially lead to acute and chronic toxicities in other organs. The SpaceOAR® System (Augmenix Inc.) is a synthetic polyethylene glycol hydrogel injected between the prostate and rectum that moves the rectum away from the prostate to reduce irradiation of the anterior rectal wall (2).
This is the report of spontaneous healing of rectal penetration associated with SpaceOAR® hydrogel to be evaluated by both magnetic resonance imaging (MRI) and colonofiberoscopy (CF).
Case report
A 63-year-old man with previous sigmoidectomy due to diverticular perforation presented with a serum prostate-specific antigen level of 7.17 ng/ml. Although digital rectal examination (DRE) detected no specific firmness of the prostate gland, magnetic resonance imaging (MRI) revealed the suspicion of prostate cancer in the transitional zone of the left lobe. The patient underwent prostate biopsy, and histological examination of the specimen was interpreted as multifocal adenocarcinoma of the prostate with Gleason score 4+3 and to be of intermediate risk. PI with EBRT was elected for treatment. Due to the history of diverticular perforation, CF was performed prior to PI and showed no abnormal findings such as hemorrhoids or rectal tumor. PI was performed with 60 radioactive iodine-125 seeds using the ultrasonography-guided intraoperative transperineal technique (3). The total prescribed dose was 104 Gy. Subsequently, SpaceOAR® hydrogel was injected into the space between the prostate and anterior rectal wall using the same technique as mentioned above (3). DRE immediately following the injection revealed intact rectal mucosa. Twenty-four hours after PI, postimplant computed tomography (CT) scan showed good seed placements within the prostate and that the rectal volume receiving 100% of the prescribed dose (R100) was 0.81 ml.
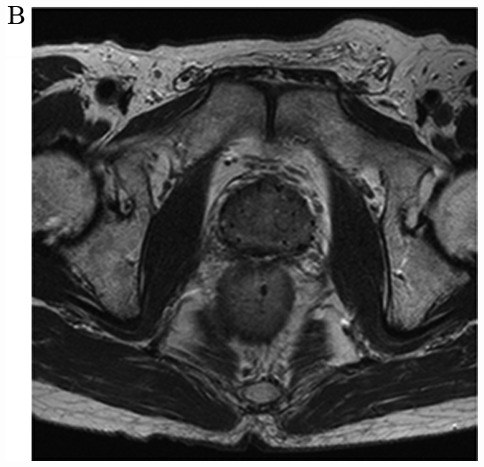
One month after implantation, the patient complained of repeated incidents of mucous and blood in his stool and underwent another CF, which confirmed the presence of mucosal ulceration and necrosis of the anterior rectal wall (Fig. 1). However, the findings did not suggest proctitis. Although a CT scan revealed air in the space between the prostate and anterior rectal wall (Fig. 2), the relationship between the rectal wall and hydrogel was unclear. In contrast, the MRI clearly indicated penetration of the rectum to the retroperitoneal space where the hydrogel was injected (Fig. 3). The patient did not complain of constitutional symptoms including abdominal pain and fever suggesting infection or an intraperitoneal perforation. Therefore, he decided to be monitored closely without any treatment. Complete healing was confirmed by both CF and MRI one month after the diagnosis of penetration (Fig. 4), therefore he will be treated by EBRT with less radiation dose for rectum three months after the healing.
Figure 1.
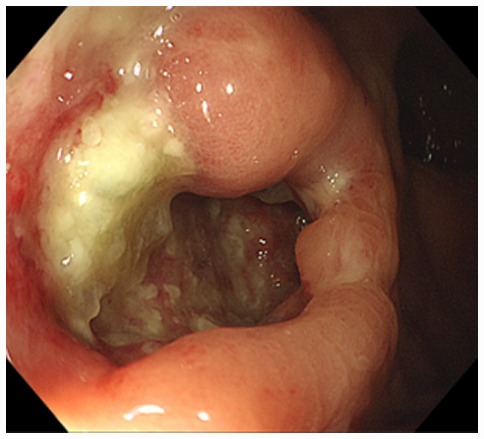
Rectal ulcer at the anterior rectal wall which was detected by CF. CF, colonofiberoscopy.
Figure 2.

CT image demonstrating free air in the space between the prostate and anterior rectal wall. The air is indicated by the white arrow.
Figure 3.
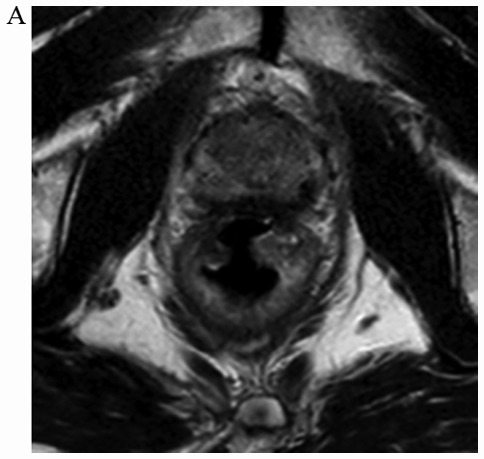
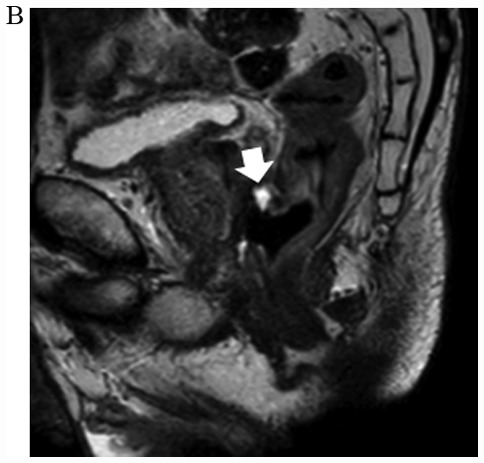
Penetration of the anterior rectal wall to the retroperitoneal space where SpaceOAR® hydrogel was injected. (A) Axial T2-weighted and (B) sagittal T2-weighted MRI images revealed SpaceOAR® hydrogel in the space between the anterior rectal wall and prostate (white arrow). MRI, magnetic resonance imaging.
Figure 4.
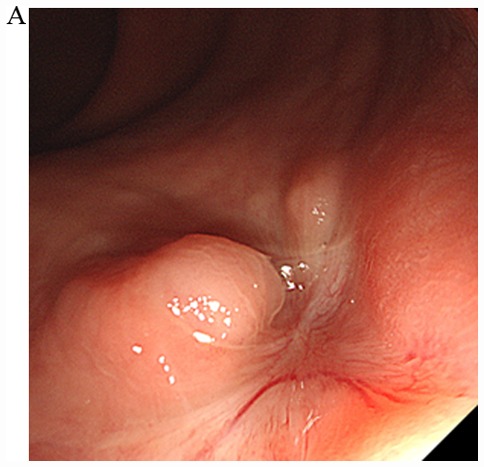
Complete healing of the rectal penetration was confirmed by (A) CF and (B) MRI. CF, colonofiberoscopy; MRI, magnetic resonance imaging.
Discussion
The SpaceOAR® System is a safety technique used to reduce irradiation of the rectum by PI (2). Teh et al reported rectal ulcer associated with SpaceOAR® hydrogel that was diagnosed by DRE and CF following spontaneous healing with a low-fiber diet (4). To the best of our knowledge, the present report is the first to show spontaneous healing of SpaceOAR® hydrogel-associated rectal penetration that was evaluated by MRI and CF. Mechanisms of hydrogel-induced rectal injury proposed include infection, mechanical injury, ischemic injury and radiation injury. In this case, no infections and no radiation proctitis were observed. In fact, the radiation dose to the rectum was very satisfactory safety and spontaneous healing was observed without any treatment including antimicrobial agents. In our hospital, more than grade 3 rectal toxicity evaluated by Common Terminology Criteria for Adverse Events version 4.0 were only 3 cases of 298 and all cases were treated by PI + EBRT. The incidence rate of PI-induced rectal toxicity in previous report is 0.33 to 3.1% (5,6), and our incidence rate is 1.0%. Hence, the other two mechanisms, ischemic injury due to excessive tension by hydrogel or mechanical injury due to migration of the injection needle were most likely the same as in a previous report (4). This is the third case of SpaceOAR® hydrogel in our hospital. It should be recognized that the hydrogel insertion is a traumatic procedure and may cause some adverse events including rectal ulcer. Further clinical study will be needed to elucidate the mechanism of hydrogel-induced rectal injury.
It was already reported that MRI detects SpaceOAR® hydrogel more clearly than CT scanning (7). Teh et al also noted that routine MRI evaluation of SpaceOAR® hydrogel is not necessary unless rectal symptoms and signs are present (4). There is no studies demonstrating the importance of MRI for hydrogel-induced rectal injury, however some studies reported that MRI plays an important role in the evaluation of carcinoma induced rectal perforation and depth of perianal fistulas (8–11). In our patient, MRI helped to diagnose the exact depth of the ulcer with no perforation and the relationship between the ulcer and the SpaceOAR® hydrogel.
In summary, SpaceOAR® hydrogel-associated rectal penetration could be healed spontaneously without any treatment only if the patient shows no severe symptoms suggesting rectal perforation. In such a case, MRI may be considered to evaluate exact depth of penetration same as rectal perforation by rectal cancer or anal fistula (8–11).
Acknowledgements
Not applicable.
Funding
No funding was received.
Availability of data and materials
All data generated or analyzed during the present study are included in this published article.
Authors' contributions
KI and KM acquired the data and wrote the manuscript. TK, KN, MN and TK acquired the data and contributed clinical advice. HT and MM interpreted the radiographic data. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The present study was approved by the Institutional Review Board of Gifu University (approval no. 2018-169).
Patient consent for publication
The patient provided written informed consent for the publication of any associated data and accompanying images.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Kao J, Cesaretti JA, Stone NN, Stock RG. Update on prostate brachytherapy: Long-term outcomes and treatment-related morbidity. Curr Urol Rep. 2011;12:237–242. doi: 10.1007/s11934-011-0183-3. [DOI] [PubMed] [Google Scholar]
- 2.Karsh LI, Gross ET, Pieczonka CM, Aliotta PJ, Skomra CJ, Ponsky LE, Nieh PT, Han M, Hamstra DA, Shore ND. Absorbable Hydrogel spacer use in prostate radiotherapy: A comprehensive review of phase 3 clinical trial published data. Urology. 2018;115:39–44. doi: 10.1016/j.urology.2017.11.016. [DOI] [PubMed] [Google Scholar]
- 3.Ohashi T, Yorozu A, Toya K, Saito S, Momma T, Nagata H, Kosugi M, Shigematsu N, Kubo A. Comparison of intraoperative ultrasound with postimplant computed tomography-dosimetric values at Day 1 and Day 30 after prostate brachytherapy. Brachytherapy. 2007;6:246–253. doi: 10.1016/j.brachy.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Teh AY, Ko HT, Barr G, Woo HH. Rectal ulcer associated with SpaceOAR hydrogel insertion during prostate brachytherapy. BMJ Case Rep. 2014;2014(pii):bcr2014206931. doi: 10.1136/bcr-2014-206931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Buckstein M, Carpenter TJ, Stone NN, Stock RG. Long-term outcomes and toxicity in patients treated with brachytherapy for prostate adenocarcinoma younger than 60 years of age at treatment with minimum 10 years of follow-up. Urology. 2013;81:364–368. doi: 10.1016/j.urology.2012.08.112. [DOI] [PubMed] [Google Scholar]
- 6.Price JG, Stone NN, Stock RG. Predictive factors and management of rectal bleeding side effects following prostate cancer brachytherapy. Int J Radiat Oncol Biol Phys. 2013;86:842–847. doi: 10.1016/j.ijrobp.2013.04.033. [DOI] [PubMed] [Google Scholar]
- 7.Sheridan AD, Nath SK, Huber S, Rosasco S, Weinreb JC, Israel GM. Role of MRI in the use of an absorbable hydrogel spacer in men undergoing radiation therapy for prostate cancer: What the radiologist needs to know. AJR Am J Roentgenol. 2017;209:797–799. doi: 10.2214/AJR.17.18026. [DOI] [PubMed] [Google Scholar]
- 8.Tapan U, Ozbayrak M, Tatli S. MRI in local staging of rectal cancer: An update. Diagn Interv Radiol. 2014;20:390–398. doi: 10.5152/dir.2014.13265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khera PS, Badawi HA, Afifi AH. MRI in perianal fistulae. Indian J Radiol Imaging. 2010;20:53–57. doi: 10.4103/0971-3026.59756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Spencer JA, Chapple K, Wilson D, Ward J, Windsor AC, Ambrose NS. Outcome after surgery for perianal fistula: Predictive value of MR imaging. AJR Am J Roentgenol. 1998;171:403–406. doi: 10.2214/ajr.171.2.9694464. [DOI] [PubMed] [Google Scholar]
- 11.de Miguel Criado J, del Salto LG, Rivas PF, del Hoyo LF, Velasco LG, de las Vacas MI, Marco Sanz AG, Paradela MM, Moreno EF. MR imaging evaluation of perianal fistulas: Spectrum of imaging features. Radiographics. 2012;32:175–194. doi: 10.1148/rg.321115040. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during the present study are included in this published article.


