Abstract
Objective
To examine within an at-risk/clinical sample of preschool aged children with externalizing problems: a) which disruptive behavior and attention disorder symptoms (inattention, hyperactivity/impulsivity, oppositionality/aggression) and b) what aspects of parenting (e.g., discipline practices or stress) are related to child sleep problems (e.g., sleep habit and night waking problems).
Method
The sample consisted of 148 children (Mage = 5.06 years; 82% male) with at-risk/clinically elevated levels of externalizing behavior problems and their primary caregiver. As part of a larger study, parents reported on their stress and parenting practices and their children’s behavioral and sleep functioning. Positive and negative parenting behaviors (“do” and “don’t” skills, respectively) were also observed during a 15-minute parent-child interaction during play.
Results
Oppositionality/aggression was the only disruptive behavior and attention disorder symptom associated with more sleep habit problems. Higher levels of inconsistent discipline and “don’t” skills were also associated with more sleep habit problems. Within a combined model, an interaction emerged such that the association between “don’t” skills and elevated sleep habit problems was only evident at low levels of inconsistent discipline. In terms of night waking problems, there was only an association with parenting stress, whereas the other parenting factors and disruptive behavior and attention disorder symptoms were unrelated.
Conclusion
While the directionality of our associations cannot be ascertained due to the cross-sectional nature of our study, these findings nevertheless highlight the importance of parenting factors (e.g., inconsistent discipline and parenting stress) when considering young children with disruptive behavior and attention disorders sleep difficulties.
Keywords: disruptive behavior disorders, attention-deficit/hyperactivity disorder, oppositional defiant disorder, sleep, parenting
Disruptive behavior and attention disorders are common among young children, with prevalence rates ranging from 1% to 16% for Oppositional Defiant Disorder (ODD), 1% to 9% for Conduct Disorder (CD), and 6.8% to 10.2% for Attention-Deficit/Hyperactivity Disorder (ADHD).1 ADHD and ODD in particular, tend to co-occur, with comorbidity rates ranging from 25% to 50%.1 Symptoms of disruptive behavior and attention disorders include: aggression, defiance of authority, attention problems, impulsivity, and antisocial behaviors all of which can have a negative impact on young children’s functioning. For example, preschool-aged children diagnosed with disruptive behavior and attention disorders have significantly greater levels of social dysfunction compared to typically developing children.2 Similarly, preschool children with disruptive behavior and attention disorders are more likely to have academic difficulties and perform poorly on neurocognitive tasks.1 While the psychosocial and neurocognitive impairments found among children with disruptive behavior and attention disorders are well-established, less attention has been paid to comorbid health problems affecting young children with disruptive behavior and attention disorders. The current study focuses on young children with or at-risk for disruptive behavior and attention disorders with a particular focus on the link between parenting factors (i.e., parental stress, discipline strategies) and sleep functioning.
Sleep is a restorative period that is necessary for healthy development as well as optimal daytime functioning.3 During the preschool period, children spend approximately half of their time sleeping.3 Sleep disturbances in children are common with 20–25% of children experiencing some type of sleep disturbance, including disordered breathing, insomnia, bedtime resistance, daytime sleepiness, and sleep terrors.4 Young children with disrupted sleep have poorer behavioral adjustment in preschool and worse cognitive functioning.5 Neurocognitive deficits are also implicated in the development of children’s disruptive behavior and attention disorders. In fact, emerging work has suggested the important role of sleep functioning towards understanding phenotypical expression of disruptive behavior and attention disorder symptoms.6
DBDs and sleep problems
Epidemiological studies have shown that general levels of externalizing behavior problems are associated with poorer sleep.7 Children with disruptive behavior and attention disorders are also more susceptible than children without disruptive behavior and attention disorders to sleep-related impairments, including sleep-disordered breathing.9–10 Sleep problems are especially concerning among children with ADHD, with estimates of up to 50% of children with ADHD having sleep difficulties.8 Specifically, children with ADHD have shorter sleep duration, more disturbed sleep, more bedtime struggles, and more night wakings compared to typically developing children.11–12 Additionally, previous research has found a bidirectional association between ODD and sleep problems.13
Comorbidity further elevates the risk for sleep problems as past studies have documented that children with both ODD/CD and ADHD sleep significantly less than typically developing children and children with ODD/CD alone.9 Additionally, Corkum and colleagues14 found higher resistance to waking up in the morning and going to bed at night in children with comorbid ADHD and ODD compared to children with ADHD alone. Thus, while it is clear that children with comorbid disruptive behavior and attention disorders experience significantly greater levels of sleep problems, limited research has focused on comparing the specific symptoms of disruptive behavior and attention disorders (e.g., oppositionality/aggression versus hyperactivity) that may be more closely linked to sleep problems.
Research suggests that conduct problems are associated with bedtime resistance, while hyperactivity is associated with tossing and turning during sleep, as well as sleep walking.15 Additionally, within an elementary aged sample, insomnia symptoms and lower sleep duration were associated with inattention, clinically elevated externalizing problems, limit-setting and rule-breaking behaviors.16 On the other hand, Mayes et al6 found that children with ADHD-Inattentive subtype did not differ from typically developing children in terms of nighttime sleep problems, although these children slept more and daytime sleepiness was higher. Children with ADHD-combined type had more nighttime sleep problems than typically developing children.6 Taken together, it appears that the hyperactivity dimension is more closely tied to sleep problems compared to the inattention dimension. However, the one study6 that compared inattention to hyperactivity was with older children and failed to include ODD symptoms. Moreover, the sleep literature in children with ODD specifically is limited. Examining which symptoms of disruptive behavior and attention disorders relate to sleep problems among preschool-aged children is particularly important given the stability of both sleep17 and behavioral problems upon school entry.18
Parenting and sleep problems
Examining the role of parenting as it relates to young children with disruptive behavior and attention disorders’ sleep functioning is also important given the role of parenting in the maintenance and treatment of disruptive behavior and attention disorders.19 Parenting is a multifaceted construct with the current study focusing on parental involvement and both positive and negative discipline strategies. From a theoretical perspective, parents’ ability to implement positive discipline strategies (e.g., praise, reward) and limit negative ones (e.g., inconsistent discipline, corporal punishment) is central towards promoting positive parent-child interactions. Extending such theoretical framework to the sleep domain, parenting strategies likely also play a vital role in promoting healthy sleep habits. For example, good sleep hygiene is evidenced by a consistent bedtime and routine as well as sleeping independently.20 Furthermore, Bell and Belsky19 found that children’s sleep worsens over time when their mothers engage in less sensitive parenting and have more conflict in the parent-child relationship. Thus, despite the extensive literature on parenting strategies as it relates to parent-child interactions and behavior problems, positive and negative parenting strategies have not been examined independently in their associations with child sleep problems.
Another parental factor that plays a role in parents’ ability to promote their children’s sleep is parenting stress. Parenting stress is the negative reaction to the demands of the role of parenting. Higher levels of parenting stress are associated with greater child sleep problems.21 For example, in a study examining sleep problems in children ages three to 14, Meltzer and Mindell22 found that mothers of children with sleep disruptions reported higher parenting stress. Similarly, in a longitudinal sample of toddlers, shorter child sleep consolidation was associated with higher parenting stress.23 Sadeh et al24 obtained similar findings in parents of children ages 7 to 11, with increased familial stress associated with poorer sleep quality. In terms of potential mechanisms linking parenting stress and child sleep problems, neurobiological work has highlighted how stress activates the hypothalamic-pituitary-adrenal (HPA) axis and the secretion of glucocorticoids (e.g., cortisol), which then causes sleep disruptions and vice-versa.25 Given the high heritability of children’s HPA axis26 it is possible that such link between stress and child sleep problems is due to this shared vulnerability.
While parenting discipline strategies and stress have been linked to both disruptive behavior and attention disorders, and sleep problems,19,22–23 to our knowledge, no study to date has examined the extent to which such parenting factors and disruptive behavior and attention disorders symptoms are uniquely related to sleep problems. Moreover, it may be especially valuable to elucidate which dimensions of parenting (e.g. stress or strategies) are related to child sleep problems as it may inform intervention targets. Finally, it may also be the case that an interaction among parenting factors and disruptive behavior and attention disorders may better explain the associations with child sleep problems. For example, it may be the case that a positive parent-child interaction style buffers some of the negative effects of either stress or negative discipline strategies on sleep problems. Additionally, children with higher symptoms of oppositionality/aggression may be more sensitive to negative discipline strategies and consequently experience more sleep difficulties. Lastly, it may be plausible that higher levels of stress negatively impact a parent’s ability to implement a daily sleep routine with their children, especially among children who may be more difficult to manage such as those with higher levels of hyperactivity or oppositionality/aggression.
Current study
Given the aforementioned gaps in the literature, the purpose of this study was to examine within a sample of preschool-aged children with or at-risk for disruptive behavior and attention disorders: a) which disruptive behavior and attention disorder symptoms (inattention, hyperactivity/impulsivity, oppositionality/aggression) and b) what aspects of parenting (e.g., discipline practices or stress) are related to child sleep problems (e.g., sleep habit and night waking problems). A unique aspect of the current study is the use of a large Hispanic/Latino sample, which has historically been unexamined in terms of the link between disruptive behavior and attention disorders, parenting, and sleep functioning. It is particularly important to examine Hispanic/Latino families given that their parenting style when having a child with disruptive behavior and attention disorder differs from Caucasian families.28 In accordance with previous research,15,22 we expected that oppositionality/aggression would be more strongly associated with elevated sleep problems compared to ADHD symptoms. Within the parenting domain, we expected higher levels of parenting stress and poorer discipline strategies to be associated with elevated sleep problems.
Methods
Participants and Recruitment
Children and their primary caregivers were recruited as part of a larger study targeting school readiness, the Summer Treatment Program for Pre-Kindergarteners (STP-PreK)29 during the 2014–2016 summer cohorts. Recruitment was conducted at local preschools and mental health agencies in a large urban southeastern city in the United States via brochures, parent workshops, and radio and newspaper advertisements. Interested parents called the study center and spoke with study staff who described the study and scheduled them for a screening appointment to determine eligibility. Children were eligible if they a) had an estimated IQ of 70 or higher on the Wechsler Preschool and Primary Scale of Intelligence – Fourth Edition (WPPSI-IV) b) had at-risk or clinically elevated levels of externalizing behavior problems (t-score above 60) according to the Behavior Assessment for Children, Second Edition, Parent or Teacher Report (BASC-2) c) were previously enrolled in preschool, d) had no parent reported history of Autism or Psychotic Disorder, and e) were able to participate in an 8-week summer camp.
The final sample consisted of 148 preschool-aged children (Mage = 5.06 years; 82% male; 84.9% Hispanic/Latino) and their primary caregiver (Mage = 35.94 years; 80.7% female; 85.5% Hispanic/Latino) who provided informed consent to participate in the current study. The average Hollingshead SES score was in the low- to middle-class range (M = 44.25, SD = 12.25). During the pretreatment assessment a diagnostic evaluation was conducted with all children via the administration of the disruptive disorders module of the Diagnostic Interview Schedule for Children, computerized version IV (C-DISC-IV)30 or from the Kiddie-Disruptive Behavior Disorder Schedule (K-DBDS). 31 Of note, 87% of our sample met diagnostic criteria for ADHD, ODD, or a combination. See Table 1 for detailed rates of diagnoses and sample demographics.
Table 1.
Participant demographic variables
| Total sample (n = 148) | |
|---|---|
| Demographic Variables | |
| Child gender (% male) | 82% |
| Mean Child age (Range) | 5.06 (3.78–6.05) |
| Mean Hollingshead SES (SD) | 44.39 (12.06) |
| Child race (%) | |
| Hispanic/Latino | 84.9% |
| Non-Hispanic/Latino White | 15.1% |
| African-American | 7.5% |
| Mean Caregiver age (Range) | 35.94 (23–52) |
| Medication status (% on medication) | 6.8% |
|
Screening measures | |
| Externalizing t-score- parent- BASC 2 (SD) | 64.25 (11.06) |
| % ADHD only diagnosis- C-DISC or K-DBDS | 22.3% |
| % ODD only diagnosis- C-DISC or K-DBDS | 18.2% |
| % ADHD + ODD diagnosis- C-DISC or K-DBDS | 46.6% |
Note. SES = socioeconomic status, BASC-2 = Behavior Assessment System for Children, 2nd Edition, ADHD = Attention-Deficit Hyperactivity Disorder, ODD = Oppositional Defiant Disorder, C-DISC= Diagnostic Interview Schedule for Children computerized version IV, K-DBDS= Kiddie-Disruptive Behavior Disorder Schedule
Measures
Disruptive Behavior Disorders
Assessment of children’s ADHD and ODD symptoms were obtained via the Disruptive Behavior Disorders Rating Scale, Parent Version (DBRS-PV).32 The DBRS-PV is a widely used 45-item measure that asks parents to rate DSM symptoms on a 4-point Likert Scale (0 = not at all to 3 = very much). Items were updated to reflect DSM-5 criteria and qualifiers. Reliability and validity are well-established for the DBRS-PV, with moderate to high internal consistency for the three factor scales of, inattention, hyperactivity/impulsivity, and oppositionality/aggression (.67-.81).33 For the current study, raw symptom scores were averaged to provide a mean score for each dimension: inattention (α = .89), hyperactivity/impulsivity (α = .84), and oppositionality/aggression (α = .84).
Children’s Sleep Problems
Child sleep problems were assessed via parent report with an abbreviated version of the Children’s Sleep Habits Questionnaire modified for use in the National Institute of Child Health and Development- Study of Early Child Care and Youth Development.34 This measure is a reliable and clinically useful screening instrument for young children.3 The abbreviated and modified CSHQ assesses child sleep problems via 22 items on a 5-point Likert scale (1 = Never to 5 = Always) and consists of a total score along with four subscales: sleep habit problems, night wakings, parasomnias, and daytime sleepiness. The current study only examined sleep habit problems (α = .73) and night wakings (α = .68) as the other subscales had poor internal consistency (α < .60). The sleep habit problems subscale consists of five questions (e.g., child falls asleep in parents’ or siblings’ bed, child goes to bed at the same time at night) and the night wakings subscale consists of three questions (e.g., child moves to someone else’s bed during the night, child wakes up more than once during the night).
Parenting Strategies
The Alabama Parenting Questionnaire (APQ)35 measures five dimensions of parenting: involvement, positive parenting, poor monitoring/supervision, inconsistent discipline, and corporal punishment via 42-items. Items use a 5-point Likert scale (1 = Never to 5 = Always). The APQ has been found to have good internal consistency across the positive parenting (α =.80) and involvement (α = .80) scales, good criterion validity in differentiating clinical and nonclinical groups.35 The current study examined the inconsistent discipline subscale (α = .74) and a positive parenting factor (α = .81) consisting of the positive parenting practices and parental involvement subscales.
Observed Parenting
The Dyadic Parent-Child Interaction Coding System (DPICS) is a reliable and valid behavioral coding system for parent-child interactions36. Due to the fact that the DPCIS was originally developed as part of a Parent-Child Interaction Therapy (PCIT) protocol, it classifies positive and negative parenting behaviors (which are targeted in PCIT) as “Do” and “Don’t” skills, respectively. “Do” skills consist of behavior descriptions (descriptive statements which describe the child’s observable behavior), reflections (a declarative phrase or statement that has the same meaning as a child verbalization), and praises (a positive evaluation of the child’s behavior, activity, or products). “Don’t” skills consist of questions (verbal inquiries that have a rising inflection at the end or have the sentence structure of a question), command (an order or direction for a behavior to be performed by the child), and negative talk (verbal expression of disapproval of the child or child’s attributes, activities, products, or choices). “Do” and “Don’t” skills were assessed during a 15-minute observation of child-directed play, parent-directed play, and a clean-up situation. Proportion of “Do” skills and “Don’t” skills were defined by the number of skills, respectively, divided by the number of parent vocalizations. Undergraduate students completed coding and were trained to 80% agreement with a criterion tape. Twenty percent of observations were coded a second time for reliability. Reliability for the “Do” and “Don’t” skills were excellent (r’s range from 0.98 to 0.99).
Parenting Stress
Parents completed the Parenting Stress Index/Short Form (PSI)37 to assess the source and degree of parenting stress. The PSI contains 36 items rated on a 6-point Likert scale (1 = Strongly Disagree to 5 = Strongly Agree) and yields subscales assessing parental distress, stress related to parent-child interactions, stress related to the child’s behavior, and a total score. This measure demonstrates good test-retest reliability (.68-.85), internal consistency (.85-.91) and concurrent validity.37 For the purpose of the present study, the total stress raw score (α = .92) was used as our measure of parenting stress, where higher scores indicated increased parenting stress.
Procedure
This study was approved by the university’s Institutional Review Board. As part of the pretreatment assessment, consenting caregivers completed several questionnaires and completed one of two structured diagnostic interviews (C-DISC; K-DBDS).30–31 In instances of parental bilingualism, parents were asked if they were more comfortable reading in English or Spanish and parent report forms/parent interview were provided in the language of choice. There were no significant differences in any variables reported between English and Spanish speaking parents nor were there any differences in the rates of diagnoses among children whose parents were interviewed with the C-DISC (n = 67) versus the K-DBDS (n = 81).
Data analysis plan
All analyses were conducted using the Statistical Package for Social Sciences, version 22 (SPSS, 2013). Seven families had missing data on at least one variable. According to Little’s MCAR test, data were missing completely at random (χ2 = 11.57, p > .05). Preliminary analyses were conducted between demographic variables and all outcome variables to identify any associations. Regression analyses were conducted to examine the unique associations between disruptive behavior and attention disorder symptoms (inattention, hyperactivity/impulsivity, or oppositionality/aggression) and parenting factors (“Do/Don’t” skills, inconsistent discipline, parenting stress, and a positive parenting factor [consisting of positive parenting and involvement subscales]) on child sleep problems (sleep habit and night waking problems). All predictors were mean centered and significant interactions were probed accordingly.
Results
Preliminary Analyses: Demographic Variables
Preliminary analyses between demographic variables and study outcome variables revealed an association between child age and parenting stress (r = −.19, p < .05). Specifically, parents of older children reported lower parenting stress. Therefore, all analyses controlled for child age. Descriptive statistics for study variables are displayed in Table 2.
Table 2.
Correlations between variables
| ADHD- Inattentive | ADHD- Hyp/Imp | ODD- Opp/Agg | Parenting Stress | Pos. Parenting Factor | Inconsistent Discipline | Do Skills | Don’t Skills | Total Sleep Problems | Sleep Habits subscale | Night wakings Subscale | Child Age | Child Gender | Hollingshead SES | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADHD-Inattentive (P) DBDRS-PV | - | |||||||||||||
| ADHD-Hyperactive/Impulsive (P) DBDRS-PV | .66** | - | ||||||||||||
| ODD-Oppositionality/Aggression (P) DBDRS-PV | .34** | .48** | - | |||||||||||
| Parenting Stress (P) APQ | .21* | .28** | .50** | - | ||||||||||
| Positive Parenting Factor (P) APQ | .01 | −.05 | −.16 | −.34** | .- | |||||||||
| Inconsistent Discipline (P) APQ | .22** | .24** | .25** | .43** | −.13 | - | ||||||||
| Do Skills (O) DPICS | −.00 | −.06 | .19* | −.03 | .19* | −.14 | - | |||||||
| Don’t Skills (O) DPICS | .11 | .03 | −.21* | −.01 | −.18 | .10 | −.51** | - | ||||||
| Total Sleep Problems (P) CSHQ | .14 | .11 | .27** | .36** | −.00 | .33** | −.06 | .03 | - | |||||
| Sleep Habits subscale (P) CSHQ | .16 | .12 | .23** | .23** | .02 | .32** | −.05 | .18 | .74** | - | ||||
| Nightwakings subscale (P) CSHQ | .00 | −.08 | .11 | .15 | .08 | .05 | .13 | −.15 | .61** | .24** | - | |||
| Child age | .12 | .11 | .00 | −.19* | .13 | −.01 | .01 | −.08 | −.10 | −.04 | .01 | - | ||
| Child gender | −.08 | −.14 | −.04 | −.02 | .07 | .07 | .00 | .01 | .08 | .06 | .03 | −.00 | - | |
| Hollingshead SES | −.09 | −.01 | −.05 | −.09 | −.04 | −.02 | .18 | −.13 | −.06 | −.06 | .08 | −.00 | .05 | - |
| Mean (SD) | 1.40 (.69) | 1.58 (.67) | .93 (.60) | 79.94 (21.53) | 68.99 (6.84) | 13.06 (4.27) | .08 (.06) | .61 (.11) | 26.11 (9.00) | 8.89 (4.73) | 4.12 (2.80) | 5.05 (.51) | - | 44.39 (12.06) |
Note.
p < .01
p < .05.
O observational measure, P parent report measure. DBDRS-PV= Disruptive Behavior Disorder Rating Scale (Pelham et al., 1992), APQ= Alabama Parenting Questionnaire (Shelton et al., 1996), PSI= Parenting Stress Index (Abidin, 1995), DPICS = Dyadic Parent-Child Interaction Coding System (Eyberg et al., 2004). CSHQ= Children’s Sleep Habits Questionnaire (modified by NICHD SECCYD)
Regression Analyses: Associations Between Disruptive Behavior and Attention Disorder Symptoms, Parenting, and Sleep Habit Problems
Model 1: Only Parenting Questionnaires
A regression analysis was conducted to examine the unique association between parenting factors (inconsistent discipline, positive parenting factor, and parenting stress) and child sleep habit problems [F(4,136) = 4.56 , p < .01 , total R2 = .12]. Inconsistent discipline was the only parenting factor that was associated with sleep problems (β = .27, p < .01), indicating that parents who reported more inconsistent discipline, had children who were having more sleep habit problems (Table 3).
Table 3.
Model for predicting sleep habit problems
| β | B (SE b) | 95% CI | Model R2 | F test statistic | |
|---|---|---|---|---|---|
|
Model 1: Parenting Questionnaires | |||||
| Child age | −.01 | −.11 (.77) | −1.64, 1.41 | .12 | 4.56** |
| Parenting Stress- PSI | .14 | .03 (.02) | −.01, .07 | --- | --- |
| Inconsistent Discipline- APQ | 27** | .30 (.10) | .10, .50 | --- | --- |
| Positive Parenting Factor- APQ | .10 | .07 (.06) | −.05, .19 | --- | --- |
|
Model 2: Parenting Observation | |||||
| Child age | −.05 | −.49 (.93) | −2.33, 1.34 | .04 | 1.43 |
| Do skills- DPICS | .06 | 5.45 (9.72) | −13.82, 24.72 | --- | --- |
| Don’t skills- DPICS | .21+ | 8.86 (4.77) | −.60, 18.31 | --- | --- |
|
Model 3: Dimensions of DBDs | |||||
| Child age | −.04 | −.40 (.78) | −1.94, 1.15 | .07 | 2.47* |
| Inattention- DBDRS-PV | .14 | .99 (.77) | −.52, 2.51 | --- | --- |
| Hyperactivity/Impulsivity- DBDRS-PV | −.08 | −.53 (.83) | −2.17, 1.12 | --- | --- |
| Oppositionality/Aggression- DBDRS-PV | .22* | 1.74 (.74) | .28, 3.20 | --- | --- |
|
Model 4: Combined Model | |||||
| Step 1. Child age | −.04 | −.39 (.86) | −2.10, 1.31 | .18 | 5 94*** |
| Inconsistent Discipline- APQ | .30** | .33 (.10) | .13,.53 | --- | |
| Don’t skills- DPICS | .19* | 7.73 (3.88) | .04, 15.43 | --- | |
| Oppositionality/Aggression - DBDRS-PV | .17 | 1.28 (.71) | −.13, 2.69 | --- | |
| Step 2. Don’t skills x Inconsistent Discipline | −.25** | −2.67 (.93) | −4.50, −.83 | .25 | 4.99*** |
| Don’t skills x Oppositionality/Aggression | −.08 | −4.80 (5.33) | −15.38, 5.77 | --- | --- |
| Inconsistent Discipline x Oppositionality/Aggression | −.42 | −.19 (.16) | −.50, .12 | --- | --- |
Note.
p < .001
p < .01
p < .05
p < .08
DBDRS-PV= Disruptive Behavior Disorder Rating Scale (Pelham et al., 1992), APQ= Alabama Parenting Questionnaire (Shelton et al., 1996), PSI= Parenting Stress Index (Abidin, 1995), DPICS = Dyadic Parent-Child Interaction Coding System (Eyberg et al., 2004)
Model 2: Only Parenting Observations
A similar regression analysis was conducted with observed parenting (i.e., “Do” and “Don’t skills”) and sleep habit problems. While the overall model using observation measures was not significant, [F(3,110) = 1.43 , p = .24], “Don’t” skills was marginally significant (β = .21, p < .08), with parents who reported higher levels of “Don’t” skills having children who were having more sleep habit problems (Table 3.)
Model 3: Only Disruptive Behavior and Attention Disorder Symptoms
Next, a regression analysis was conducted to examine the unique associations between disruptive behavior and attention disorder symptoms (inattention, hyperactivity/impulsivity, or oppositionality/aggression) and child sleep habit problems [F(4,136) = 2.47 , p < .05 , total R2 = .07]. As seen in Table 3, oppositionality/aggression was the only symptom of disruptive behavior and attention disorders that was significantly associated with sleep problems (β = .22, p < .05), suggesting that children reported as being more oppositional by their parents were also having more sleep habit problems.
Model 4: Combined Model
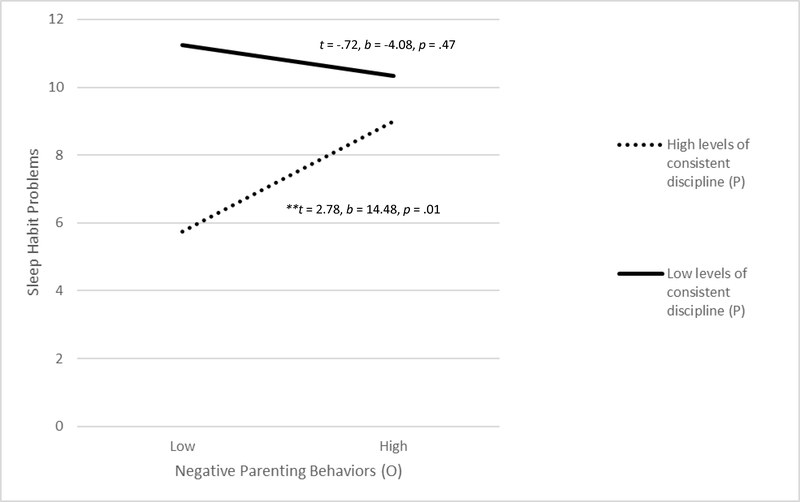
The final regression model included all significant main effects as well as tested for potential interactions. As seen in Table 3, step 1 of Model 4 [F(4,109) = 5.94 , p < .001 , total R2 = .18], the significant main effects of inconsistent discipline and “Don’t” skills on sleep habit problems remained (β = .30, p < .001 and β = .18, p < .05, respectively). On the other hand, oppositionality/aggression no longer had a significant effect on sleep habit problems. Additionally, step 2 indicated a significant interaction between “Don’t” skills and inconsistent discipline in predicting sleep habit problems (β = −.25, p < .01). Probing of the interaction revealed that “Don’t” skills were only predictive of sleep habit problems for parents with low levels of inconsistent discipline (t = 2.78, b = 14.48, p = .01; see Figure 1). Conversely, “Don’t” skills had no significant effect on sleep habit problems for parents with high levels of inconsistent discipline (t = −.72, b = −4.08, p = .47)
Figure 1.
Negative parenting behaviors by levels of consistent discipline on sleep habit problems. **p < .01.
Note. O observational measure, P parent report measure. High levels of consistent discipline is indicative of a low score on the inconsistent discipline subscale of the Alabama Parenting Questionnaire (APQ; Shelton et al., 1996). Negative parenting behaviors are reflective of number of “Don’t” skills measured via the Dyadic Parent-Child Interaction Coding System (DPICS; Eyberg et al., 2004).
Regression Analyses: Associations Between Disruptive Behavior and Attention Disorder Symptoms, Parenting, and Night Waking Problems
Model 1: Only Parenting Questionnaires
While the overall model using observation measures was not significant, [F(4,137) = 1.54 , p = .20], regression analyses for model 1 indicated that parenting stress was the only parenting factor uniquely associated with night waking problems (β = −.22, p < .05), with higher levels of parenting stress associated with more night waking problems (See Table 4).
Table 4.
Model for predicting night waking problems
| β | B (SE b) | 95% CI | Model R2 | F test statistic | |
|---|---|---|---|---|---|
|
Model 1: Parenting Questionnaires | |||||
| Child age | .03 | .15 (.47) | −.77, 1.08 | .04 | 1.54 |
| Parenting Stress - PSI | .22* | .03 (.01) | .00, .05 | --- | --- |
| Inconsistent Discipline- APQ | −.02 | −.02 (.06) | −.14, .11 | --- | --- |
| Positive Parenting Factor- APQ | .14 | .06 (.04) | −.01, .13 | --- | --- |
|
Model 2: Parenting Observation | |||||
| Child age | .08 | .43 (.52) | −.60, 1.47 | .03 | 1.22 |
| Do skills- DPICS | .07 | 3.79 (5.61) | −7.32, 14.89 | --- | --- |
| Don’t skills- DPICS | −.11 | −2.58 (2.72) | −7.98, 2.81 | --- | --- |
|
Model 3: Dimensions of DBDs | |||||
| Child age | .02 | .12 (.46) | −.80, 1.03 | .04 | 1.33 |
| Inattention - DBDRS-PV | .08 | .33 (.46) | −.58, 1.24 | --- | --- |
| Hyperactivity/Impulsivity- DBDRS-PV | −.22 | −.92 (.50) | −1.91, .07 | --- | --- |
| Oppositionality/Aggression- DBDRS-PV | .19 | .87 (.44) | −.01, 1.74 | --- | --- |
Note.
p < .05.
DBDRS-PV = Disruptive Behavior Disorder Rating Scale (Pelham et al., 1992), APQ= Alabama Parenting Questionnaire (Shelton et al., 1996), PSI= Parenting Stress Index (Abidin, 1995), DPICS = Dyadic Parent-Child Interaction Coding System (Eyberg et al., 2004)
Model 2: Only Parenting Observations
The overall model [F(3,111) = 1.22 , p = .31] and main effects using observation measures were not significant (See Table 4).
Model 3: Only Disruptive Behavior and Attention Disorder Symptoms
The overall model [F(4,137) = 1.33 , p = .26] and main effects using disruptive behavior and attention disorder symptoms were not significant (See Table 4).
Discussion
This study examined within an at-risk/clinical sample of preschool-aged children which disruptive behavior and attention disorder symptoms (inattention, hyperactivity/impulsivity, oppositionality/aggression) and what aspects of parenting (e.g., discipline practices or stress) are related to child sleep problems (e.g., sleep habit and night waking problems). Our results indicated that oppositionality/aggression was the only disruptive behavior and attention disorder symptom associated with more sleep habit problems. Higher levels of inconsistent discipline and “Don’t” skills were also associated with more sleep habit problems although this finding was qualified by an interaction such that the association between “Don’t” skills and elevated sleep habit problems was only evident at low levels of inconsistent discipline. In terms of night waking problems, there was only an association with parenting stress, whereas the other parenting factors and disruptive behavior and attention disorder symptoms were unrelated. These findings are further discussed below.
Consistent with our hypothesis, we found that oppositionality/aggression, but not ADHD symptoms, was associated with more sleep habit problems but not with night waking problems. Our results are in agreement with previous work demonstrating that conduct problems are associated with global reports of sleep problems, in particular bedtime resistance.15 However, counter to the current study, Smedje et al15 found hyperactivity to be associated with tossing and turning during sleep and sleep walking. Potential reasons for the discrepancy in our findings to that of Smedjet et al15 are the differences in study samples. The sample in Smedje et al15 consisted of children ages six to eight years compared to our younger sample (mean age of five years). Additionally, Smedje et al15 used a community sample where 8–9.8% of children met criteria for DBDs, compared to our at-risk/clinical sample (87% meeting criteria for ADHD, ODD, or a combination). In fact, 46.6% of our sample met diagnostic criteria for ADHD and ODD. Given the significant comorbidity in our sample, it may be the case that children with a comorbid ADHD and ODD presentation are the ones that are experiencing greater sleep problems versus those with a more pure ADHD or ODD presentation. This is consistent with Aronen et al9 who found that non-medicated children with ODD and ADHD slept less (measured by actigraphy) than children without comorbid ADHD and matched controls.
Consistent with prior work21 we found that greater levels of inconsistent discipline practices and “Don’t” skills, respectively, were associated with more sleep habit problems. Our findings extend such literature by being the first to show these associations in a sample of preschool-aged children with at-risk or clinical elevations of externalizing symptoms. Inconsistent discipline may be particularly important among preschool-aged children with disruptive behavior and attention disorders given that early conduct problems remain stable into school-age.18 It may be the case that parents who engage in inconsistent discipline practices have a difficult time implementing appropriate sleep hygiene and therefore have children with more sleep problems. It is important to note that these parenting factors did not relate to children’s night waking problems. Therefore, it may be plausible that environmental factors, such as discipline strategies, play a larger role prior to sleep onset while factors more closely related to biological processes (i.e., stress and cortisol) are more related to disruptions during sleep (i.e., night wakings).
Consistent with the aforementioned theory and prior work,24 we found that greater levels of parenting stress were associated with night waking problems. These findings extend the work of Yurmuez and Kilic, who found that children with ADHD had more night wakings than children without ADHD.12 Parenting stress is particularly relevant among young children with disruptive behavior and attention disorders as parental perception of their child being behaviorally difficult can increase parental stress.38 A possible explanation for why parenting stress may directly increase child night waking problems relates to the shared vulnerability of the stress response as it relates to sleep functioning.26 For example, significant work has documented the role of cortisol in modulating sleep.39 Adults with higher levels of sleep disruptions exhibit increased cortisol levels.25 Similarly, El-Sheikh et al,40 found that children with sleep disturbances had significantly increased waking cortisol compared to children without sleep difficulties. When viewed in conjunction with studies documenting the heritability of the stress-response and HPA axis reactivity,26 it may be the case that parents who are stressed have children who are stressed and consequently have more night waking problems. Future studies should measure cortisol reactivity in children with disruptive behavior and attention disorders and their parents to better examine the relation between parenting stress and child sleep functioning.
Furthermore, there was an interaction between “Don’t” skills and inconsistent discipline in predicting sleep habit problems, with parents who engage in less inconsistent discipline and higher usage of “Don’t” skills, having children with more sleep habit problems. The current study’s findings contribute to and extend the literature by showing the importance of discipline strategies in combination with parent-child interactions. Specifically, the benefits of being a consistent parent appears to be partially nullified by engaging in negative parent-child interactions as it relates to sleep habits. On the other hand, our findings show that at high levels of inconsistent discipline, such parent-child interactions do not seem to have an impact on sleep habit problems. This theoretical sleep model is consistent with behavioral parent training interventions, such as PCIT, which focus on improving inconsistent discipline and parent-child interactions in order to reduce externalizing behavior problems. However, reduction of sleep problems via the use of PCIT has not been examined. Future work should examine if improving parent-child interactions has an effect on child sleep functioning.
Study Limitations
Limitations of this study should be noted. First, this study used a cross-sectional design, which limits the directionality of our findings. For example, given the bidirectional nature of parent-child interactions and inconsistent discipline as well as sleep problems and parent-child interactions, it is plausible to have a model in which child sleep problems leads to more negative parent-child interactions which in turn contributes to greater inconsistent discipline or vice versa. Thus, future work needs to implement a longitudinal design to test these cross-lagged associations between inconsistent discipline, parent-child interactions, and child sleep habit problems to determine whether parent-child interactions mediate the association between inconsistent discipline and sleep problems. Second, we used an at-risk/clinical sample and it remains unclear whether our findings would generalize to a community sample. It is plausible that parenting stress may be a more important mechanism among an at-risk/clinical sample where stress levels tend to be elevated compared to a typically developing sample.41 Third, this sample is primarily Hispanic and low-income which may also contribute to the generalizability of the findings. However, this may also be viewed as a strength as the literature on minorities and disruptive behavior and attention disorders, sleep, and parenting is limited. Lastly, our measure of child sleep problems was a questionnaire completed by the child’s parent and therefore child sleep problems might be inaccurately reported. However, previous research has found that the CSHQ is clinically useful in screening for sleep problems.5 Future studies should include objective sleep measures, such as actigraphy or polysomnography. Similarly, to avoid potential positive rater bias, future work should include observed parenting stress measures, such as cortisol.
Clinical Implications
In terms of the clinical implications of our findings, first, mental health providers should be aware of not only the well documented comorbidity between ADHD and child sleep problems,8 but perhaps be as equally aware of the relation between ODD symptoms and sleep habits in young children. Second, if sleep problems are present and impairing, behavioral sleep interventions (e.g., extinction, positive routines, and parent education) should be provided. Third, within the parenting domain, our findings highlight the potential role of parenting stress, parent-child interactions, inconsistent discipline, and sleep functioning. Thus, when teaching healthy sleep habits, it may be the case that treatment is more effective if parents are also addressing their own stress levels. Within the behavioral literature, Kazdin and Whitley42 did find that improving parental stress had a direct effect on improving child behavioral outcomes. Similarly, within a preschool sample, the Triple P-Positive Parenting Program with the enhanced program that addressed stress resulted in more reliable change in child behaviors than the standard program.43 Future work should examine whether providing an intervention that addresses parenting stress levels can directly improve child sleep outcomes. Furthermore, parenting strategies should be considered when families present for sleep problems. Interventions that include improving discipline strategies and parent-child interactions should be recommended accordingly. In fact, sleep interventions that incorporate positive parent child interactions (e.g., faded bedtime with response cost) have been found to improve sleep problems.44
Conclusions
Despite the aforementioned limitations, this study is the first to our knowledge to examine the associations between disruptive behavior and attention disorder symptoms, parenting factors, and children’s sleep problems within a sample of preschool-aged children with or at-risk for disruptive behavior and attention disorders. Future research should include longitudinal analysis in order to confirm the directionality of our findings. Additionally, as children with disruptive behavior and attention disorders get older, treatment modalities often include medications, which on their own can also effect sleep functioning. Thus, it will be important to examine how parenting factors may either attenuate or enhance children with disruptive behavior and attention disorders’ medication related sleep problems. Nevertheless, our study points to the significant clinical implications of parents jointly addressing parenting factors, sleep, and behavior problems among preschool-aged children.
Footnotes
The authors report no financial interests or potential conflicts of interest.
References
- 1.Barkley RA. Attention-deficit hyperactivity disorder: A handbook for diagnosis and treatment. New York, NY: Guilford Publications; 2014 [Google Scholar]
- 2.Ros R, Graziano P. Social dysfunction among children with ADHD: A meta-analytic review. J Clin Child Adolesc Psychol. 2017; 1–23. [DOI] [PubMed] [Google Scholar]
- 3.Goodlin-Jones BL, Sitnick SL, Tang K, et al. The Children’s Sleep Habits Questionnaire in toddlers and preschool children. J Dev Behav Pediatr. 2008; 29(2): 82–88. [DOI] [PubMed] [Google Scholar]
- 4.Archbold KH, Pituch KJ, Panah P, et al. Symptoms of sleep disturbances among children at two general pediatric clinics. J Pediatr. 2002; 140(1): 97–102. [DOI] [PubMed] [Google Scholar]
- 5.Touchette É, Petit D, Séguin JR, et al. Associations between sleep duration patterns and behavioral/cognitive functioning at school entry. Sleep. 2007; 30(9): 1213–1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayes SD, Calhoun SL, Bixler EO, et al. ADHD subtypes and comorbid anxiety, depression, and oppositional-defiant disorder: differences in sleep problems. J Pediatr Psychol. 2008; 34(3): 328–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lavigne JV, Arend R, Rosenbaum D, et al. Sleep and behavior problems among preschoolers. J Dev Behav Pediatr. 1999; 20(3): 164–169. [DOI] [PubMed] [Google Scholar]
- 8.Corkum P, Tannock R, Moldofsky H. Sleep Disturbances in Children With Attention‐Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry. 1998; 37(6): 637–646. [DOI] [PubMed] [Google Scholar]
- 9.Aronen ET, Lampenius T, Fontell T, et al. Sleep in children with disruptive behavioral disorders. Behav Sleep Med. 2014; 12(5): 373–388. [DOI] [PubMed] [Google Scholar]
- 10.Constantin E, Low NC, Dugas E, et al. Association between childhood sleep-disordered breathing and disruptive behavior disorders in childhood and adolescence. Behav Sleep Med. 2015; 13(6): 442–454 [DOI] [PubMed] [Google Scholar]
- 11.Owens J, Nobile C, Spirito A. Prevalence and types of sleep disturbances in school-aged children: validation of a parental report, Children’s Sleep Habits Questionnaire. J Sleep Res. 1998; 7(suppl 2): 394. [Google Scholar]
- 12.Yürümez E, & Kılıç BG. Relationship between sleep problems and quality of life in children with ADHD. J Atten Disord. 2016; 20(1): 34–40. [DOI] [PubMed] [Google Scholar]
- 13.Shanahan L, Copeland WE, Angold A, et al. Sleep problems predict and are predicted by generalized anxiety/depression and oppositional defiant disorder. J Am Acad Child Adolesc Psychiatry. 2014; 53(5): 550–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Corkum P, Moldofsky H, Hogg-Johnson S, et al. Sleep problems in children with attention‐deficit/hyperactivity disorder: impact of subtype, comorbidity, and stimulant medication. J Am Acad Child Adolesc Psychiatr. 1999; 38(10): 1285–1293. [DOI] [PubMed] [Google Scholar]
- 15.Smedje H, Broman JE, Hetta J. Associations between disturbed sleep and behavioural difficulties in 635 children aged six to eight years: a study based on parents’ perceptions. Eur Child Adolesc Psychiatry. 2001; 10(1): 1–9. [DOI] [PubMed] [Google Scholar]
- 16.Calhoun SL, Fernandez-Mendoza J, Vgontzas AN, et al. Behavioral profiles associated with objective sleep duration in young children with insomnia symptoms. J Abnorm Child Psychol. 2017; 45(2): 337–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics. 2003; 111(2): 302–307. [DOI] [PubMed] [Google Scholar]
- 18.Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later maladjustment. Dev Psychopathol. 2000; 12: 467–488. [DOI] [PubMed] [Google Scholar]
- 19.Bell BG, Belsky J. Parents, parenting, and children’s sleep problems: Exploring reciprocal effects. Br J Dev Psychol. 2008; 26(4): 579–593. [Google Scholar]
- 20.Mindell JA. Sleeping through the night: How infants, toddlers, and their parents can get a good night’s sleep (revised). New York: HarperCollins; 2005. [Google Scholar]
- 21.Thunström M Severe sleep problems among infants in a normal population in Sweden: prevalence, severity and correlates. Acta Paediatr. 1999; 88(12): 1356–1363. [DOI] [PubMed] [Google Scholar]
- 22.Meltzer LJ, Mindell JA. Relationship between child sleep disturbances and maternal sleep, mood, and parenting stress: a pilot study. J Fam Psychol. 2007; 21(1): 67. [DOI] [PubMed] [Google Scholar]
- 23.Bernier A, Bélanger MÈ, Bordeleau S, et al. Mothers, fathers, and toddlers: Parental psychosocial functioning as a context for young children’s sleep. Dev Psychol. 2013; 49(7): 1375. [DOI] [PubMed] [Google Scholar]
- 24.Sadeh A, Raviv A, Gruber R. Sleep patterns and sleep disruptions in school-age children. Dev Psychol. 2000; 36(3): 291. [DOI] [PubMed] [Google Scholar]
- 25.Buckley TM, Schatzberg AF. Review: on the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metab. 2005; 90(5): 3106–3114. [DOI] [PubMed] [Google Scholar]
- 26.Karlén J, Frostell A, Theodorsson E, et al. Maternal influence on child HPA axis: a prospective study of cortisol levels in hair. Pediatrics. 2013; 132(5): e1333–e1340. [DOI] [PubMed] [Google Scholar]
- 27.Webster-Stratton C Stress: A potential disruptor of parent perceptions and family interactions. J Clin Child Psychol. 1990; 19(4): 302–312. [Google Scholar]
- 28.Jones HA, Epstein JN, Hinshaw SP, et al. Ethnicity as a moderator of treatment effects on parent—child interaction for children with ADHD. J Atten Disord. 2010; 13(6): 592–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Graziano PA, Slavec J, Hart K, et al. Improving school readiness in preschoolers with behavior problems: Results from a summer treatment program. J Psychopathol Behav Assess. 2014; 36(4): 555–569. [Google Scholar]
- 30.Shaffer D, Fisher P, Lucas CP, et al. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC‐IV): Description, differences from previous version and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000; 39(1): 28–38. [DOI] [PubMed] [Google Scholar]
- 31.Keenan K, Wakschlag LS, Danis B, et al. Further evidence of the reliability and validity of DSM-IV ODD and CD in preschool children. J Am Acad Child Adolesc Psychiatry. 2007; 46(4): 457–468. [DOI] [PubMed] [Google Scholar]
- 32.Pelham WE, Gnagy EM, Greenslade KE, et al. Teacher ratings of DSM-III-R symptoms for the disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry. 1992; 31(2): 210–218. [DOI] [PubMed] [Google Scholar]
- 33.Pillow DR, Pelham WE, Hoza B, et al. Confirmatory factor analyses examining attention deficit hyperactivity disorder symptoms and other childhood disruptive behaviors. J Abnorm Child Psychol. 1998; 26(4): 293–309. [DOI] [PubMed] [Google Scholar]
- 34.NICHD SECCYD-Wisconsin Children’s Sleep Habits Questionnaire (Abbreviated). Available at: http://njaap.org/wp-content/uploads/2016/04/Childrens-Sleep-Habits-Questionnaire.pdf [Google Scholar]
- 35.Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. J Clin Child Adolesc Psychol. 1996; 25: 317–329 [Google Scholar]
- 36.Eyberg S, Nelson M, Duke M, et al. Manual for the Dyadic Parent–Child Interaction Coding System (3rd ed.). [University of Florida Parent-Child Interaction Therapy; Web site]. Available at: http://www.pcit.org. [Google Scholar]
- 37.Abidin R Parenting Stress Index-Manual (3rd ed). Odessa, FL: Psychological Assessment Resources; 1995. [Google Scholar]
- 38.Mash E, Johnston C. Determinants of parenting stress: Illustrations from families of hyperactive children and families of physically abused children. J Clin Child Psychol. 1990; 19: 313–328. [Google Scholar]
- 39.Steiger A Sleep and the hypothalamo-pituitary-adrenocortical system. Sleep Med Rev. 2002; 6: 125–138. [DOI] [PubMed] [Google Scholar]
- 40.El-Sheikh M, Buckhalt JA, Keller PS, et al. Children’s objective and subjective sleep disruptions: Links with afternoon cortisol levels. Health Psychol. 2008; 27: 26–33 [DOI] [PubMed] [Google Scholar]
- 41.Podolski CL, Nigg JT. Parent stress and coping in relation to child ADHD severity and associated child disruptive behavior problems. J Clin Child Psychol. 2001; 30(4): 503–513. [DOI] [PubMed] [Google Scholar]
- 42.Kazdin AE, Whitley MK. Treatment of parental stress to enhance therapeutic change among children referred for aggressive and antisocial behavior. J Consult Clin Psychol. 2003; 71(3): 504. [DOI] [PubMed] [Google Scholar]
- 43.Sanders MR, Markie-Dadds C, Tully LA, et al. The triple P-Positive Parenting Program: A comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. J Consult Clin Psychol. 2000; 68: 624–640. [PubMed] [Google Scholar]
- 44.Mindell JA, Kuhn B, Lewin DS, et al. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep. 2006; 29(10): 1263–1276. [PubMed] [Google Scholar]