Abstract
Objectives:
Few adults participate in enough physical activity for health benefits. The workplace provides a unique environment to deliver heath interventions and can be beneficial to the employee and the employer. The purpose of the study was to explore the use of a physical activity counseling (PAC) program and a fitness-based health risk assessment (fHRA) in the hospital workplace.
Methods:
A workplace-based intervention was developed utilizing a PAC program and an fHRA to improve physical activity levels of employees. Hospital employees were enrolled in a 4-month PAC program and given the option to also enroll in an fHRA program (PAC + fHRA). Physical activity was assessed by accelerometry and measured at baseline, 2 months, and 4 months. Changes in musculoskeletal fitness for those in the fHRA program were assessed at baseline and 2 months.
Results:
For both groups (PAC n = 22; PAC + fHRA n = 16), total and moderate to vigorous physical activity in bouts of 10 minutes or more increased significantly by 18.8 (P = .004) and 10.2 (P = .048) minutes per week at each data collection point, respectively. Only participants with gym memberships demonstrated increases in light physical activity over time. Those in the fHRA group significantly increased their overall musculoskeletal fitness levels from baseline levels (18.2 vs 21.7, P < .001). There was no difference in the change in physical activity levels between the groups.
Conclusions:
A PAC program in the workplace may increase physical activity levels within 4 months. The addition of an fHRA does not appear to further increase physical activity levels; however, it may improve overall employee musculoskeletal fitness levels.
Keywords: health promotion, physical activity, health risk assessment, musculoskeletal fitness, workplace wellness
Introduction
Workplace wellness programs appear to improve physical activity levels.1-3 However, meta-analyses of workplace interventions found studies used unclear or unjustified thresholds for meaningful changes in physical activity and used self-report.4,5 The effect of these programs when using objective measures of physical activity is unclear. Moreover, there is limited research on musculoskeletal fitness-based health risk assessment (fHRAs) in the workplace setting, and this type of health risk assessment could be especially advantageous for workplaces where employees experience higher rates of musculoskeletal injury due to job-related physical demands. This article reports the results and challenges of a workplace intervention aimed to increase employee physical activity and musculoskeletal fitness levels.
In this quasi-experimental study, we determined whether:
a personalized physical activity counseling program (PAC) can improve employee physical activity levels after 4 months using objective measures of physical activity;
the addition of an fHRA to a PAC program elicits greater improvements in physical activity levels compared to PAC alone; and
an fHRA is feasible to implement in the workplace and if it can be used to improve the musculoskeletal fitness of employees.
Methods
We hypothesized that the PAC program would increase physical activity levels over 4 months, and the addition of an fHRA would further increase employee physical activity compared to PAC alone. We also hypothesized the fHRA would result in improved employee musculoskeletal fitness after 2 months. Since workplaces sometimes provide employees access to fitness facilities, we also assessed how fitness facility memberships influenced program results. Previous research has shown that providing participants with a gym membership alone does not improve fitness levels.6
This study took place at the St. Boniface General Hospital in Winnipeg, Manitoba, Canada, from December 2014 until September 2015 and used a 2-group repeated measures quasi-experimental design. Study protocol was approved by the University of Manitoba Education/Nursing Research Ethics Board and the St Boniface Hospital Research Review Committee (reference numbers E2014:092 and E2014:112). This study is reported in accordance with the Transparent Reporting of Evaluations with Nonrandomized Designs (TREND) reporting guidelines.7
Hospital staff were recruited via convenience sampling to participate in the study from December 2014 to May 2015. Employees were informed of the study using hospital posters and employee information outlets. Employees of the St Boniface Hospital who consented to participate via informed consent forms were included. Participants were excluded if the Physical Activity Readiness Questionnaire for Everyone8 revealed they were unable to safely participate in physical activity. All research meetings took place at the Hospital.
Participants attended 4 one-hour, one-on-one sessions with a Canadian Society for Exercise Physiology (CSEP) Certified Exercise Physiologist (CEP)9 who had previous experience providing physical activity counseling. The approach was rooted in the Transtheoretical Model of Behavior Change (TTM), which states that individuals go through 6 different stages before adopting a new behavior or discontinuing an old one.10 Participants identified which stage of change best fit their current physical activity levels, and the CSEP-CEP provided counseling based on their current stage. Sessions were tailored to each participant. Counseling included identifying physical activity opportunities available to the participant, education on different types of physical activities (eg, long distance running, leisure walks, gardening, etc) and their benefits, and creating physical activity schedules. Meetings took place 1 week, 3 weeks, 2 months, and 4 months into the study. No incentives were given to the participants to increase compliance or adherence.
Once recruited, participants were given the option to enroll in another intervention involving an fHRA. Those who declined the fHRA formed the PAC group, and those who agreed to participate formed the PAC + fHRA group. The research staff and CSEP-CEP were not blinded to participant group allocation.
Participants in the PAC + fHRA group attended 2 additional one-on-one meetings with the CSEP-CEP. During these meeting, the CSEP-CEP administered a musculoskeletal fitness test according to CSEP-Physical Activity Training for Health Manual.11 The musculoskeletal fitness assessment uses 6 validated measures (grip strength, push-ups, sit and reach, vertical jump, back extension, and one leg stance) to determine overall musculoskeletal health and provides a score with an associated health benefit rating.11 Based on participant results, the CSEP-CEP provided feedback and a tailored exercise prescription. This feedback contextualized participants’ scores to their job duties; potential areas of increased injury risk were identified and discussed. Additional online resources outlining the benefits of musculoskeletal exercise and instruction on how to perform different exercises were also provided. Participants completed the same tests 2 months later to assess any changes.
Data were collected at 3 different time points: baseline, 2 months, and 4 months. The primary outcome was a change in total, moderate to vigorous, and light physical activity accrued in bouts of 10 minutes or more (TPA10Mins, MVPA10Mins, and LPA10Mins, respectively) as measured by accelerometry. At each data collection, participants wore an Actical accelerometer on the right hip for 7 days. To be included in the analysis, participants had to have at least 4 valid days (10 hours of wear time).12 Intensity cut points were determined based on the 2007 to 2009 Canadian Health Measures Survey13 using 30-second epochs. Smaller epochs were used to provide better estimates of activity intensity.14 The TPA10Mins was defined as the sum of LPA10Mins and MVPA10Mins. Data were processed using Kinesoft software (V3.3.75). Only activity recorded on valid days were included. All physical activity variables were standardized for wear time using the method developed by Katapally and Muhajarine,15 which has been shown to reduce biases due to variable wear times.
Participants indicated if they had a fitness facility membership to determine whether this influenced program results. Access to fitness facilities was not offered as part of the intervention, and participants were not required to get one to participate. Stage of change based on TTM was also assessed at each data collection. Change in fitness score for those in the PAC + fHRA group was included as a secondary outcome.
All analyses were performed in SAS version 9.4 with α = .05. Changes in TPA10Mins, MVPA10Mins, and LPA10Mins were assessed with a multilevel model regression analysis with time (baseline, 2 months, and 4 months) as a continuous level-1 predictor and age, group, and fitness facility membership (membership vs no membership) as level 2 predictors. Both intercept and time were included as random effects. Change in fitness levels in the PAC + fHRA group were tested using a paired t test and a Wilcox-signed rank test.
Results
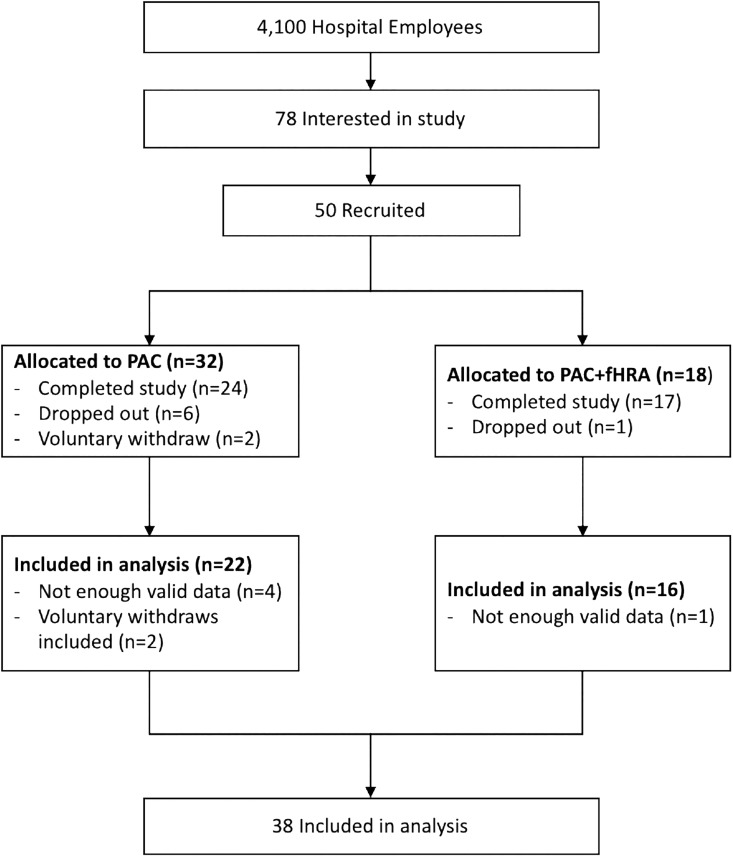
Figure 1 shows the flow of participants through the study. Two individuals in the PAC + fHRA group were unable to complete the second fitness assessment; however, because they still received the intervention component of the PAC + fHRA group, they were included in the PAC + fHRA group for the analysis.
Figure 1.
Participant flow through the study.
Baseline characteristics can be seen in Table 1. Age, gender, and body mass index did not differ between PAC and PAC + fHRA. No differences were observed between the 2 groups for fitness facility membership or physical activity levels.
Table 1.
Comparison of Baseline Characteristics Between PAC and PAC + fHRA.a,b
| PAC, n = 22 | PAC + fHRA, n = 16 | P Value | |
|---|---|---|---|
| Demographics | |||
| Age, years | 47 ± 2 | 51 ± 2 | .304 |
| Gender (% male per group) | 1 (5%) | 1 (6%) | – |
| BMI, kg/m2 | 28.2 ± 1.4 | 29.6 ± 1.4 | .500 |
| Fitness facility membership (%) | 15 (68%) | 11 (69%) | – |
| Physical activity levels | |||
| TPA10Mins, mins/week | 61 ± 12 | 72 ±12 | .533 |
| MVPA10Mins, mins/week | 38 ± 12 | 37 ± 11 | .952 |
| LPA10Mins, mins/week | 22 ± 4 | 34 ± 8 | .181 |
Abbreviations: BMI, body mass index; fHRA, fitness-based health risk assessment; LPA10Mins, light intensity physical activity in bouts of 10 minutes or more; MVPA10Mins, moderate to vigorous intensity physical activity in bouts of 10 minutes or more; PAC, physical activity counseling; TPA10Min, total physical activity in bouts of 10 minutes or more.
a Continuous variables expressed as mean ± standard error. Statistical difference determined using a t test.
b Categorical variables expressed in frequencies (percentage of group).
The TPA10Mins, MVPA10Mins, and LPA10Mins significantly increased over time for both the groups. Physical activity levels increased by 18.8 (95% confidence interval [CI]: 7.0, 30.6; P = .004), 10.2 (95% CI: 0.4, 20.0; P = .048), and 8.9 (95% CI: 1.4, 16.4; P = .026) minutes per week at each data collection point for TPA10Mins, MVPA10Mins, and LPA10Mins, respectively. Neither group, fitness facility membership, nor age was significant predictor for TPA10Mins and MVPA10Mins. No significant interaction between group × time was observed.
For LPA10Mins, there was a significant interaction between time and fitness facility membership. Participants with memberships had greater increases in LPA10Mins over time compared to those without by 21.1 (95% CI: 4.8, 37.3; P = .022) mins per week, at each subsequent data collection. A visual representation of this relationship and results from the multilevel model are included in the Supplementary Material. Means and standard error for physical activity levels of both groups are also included in the Supplementary Material.
A paired t test found a significant increase in overall musculoskeletal fitness scores for those in the PAC + fHRA group, t(13) = −4.78, P < .001. (Table 2) Statistically significant improvements were only seen in push-ups, t(13) = −3.61, P = .003, and sit and reach, t(13) = −2.92, P = .012. These results were confirmed with a Wilcox signed rank test (data not shown). Other variables were trending toward significance.
Table 2.
Baseline and Follow-Up Fitness Scores for PAC + fHRA.a
| Baseline, n = 14 | Follow-Up, n = 14 | P Value | |
|---|---|---|---|
| Overall scoreb | 18.2 ± 0.9 | 21.7 ± 0.8 | <.001 |
| Fitness testc | |||
| Grip strength | 4.3 ± 0.2 | 4.7 ± 0.1 | .082 |
| Push-ups | 3.0 ± 0.4 | 4.0 ± 0.3 | .003 |
| Leg power | 3.7 ± 0.3 | 4.1 ± 0.3 | .054 |
| Balanced | 1.6 ± 0.1 | 1.9 ± 0.1 | .082 |
| Trunk endurance | 3.2 ± 0.3 | 3.9 ± 0.3 | .055 |
| Sit and reach | 2.6 ± 0.4 | 3.4 ± 0.3 | .012 |
Abbreviations: fHRA, fitness-based health risk assessment; PAC, physical activity counseling.
a Values expressed as mean ± standard error.
b Overall score calculated as sum of all test scores.
c Categorical scores for grip strength, push-ups, leg power, trunk endurance, and sit and reach scored as poor, 1; fair, 2; good, 3; very good, 4; and excellent, 5.
d Balance scored as below average, 1 and above average, 2.
Bold face indicates significant P-values at alpha = .05
More participants reported being in the action and maintenance stage of change as the program progressed. At baseline, 45% and 50% of individuals were in these stages in the PAC and PAC + fHRA group, respectively. This increased to 56% and 63% at 2 months and 64% and 75% at 4 months, respectively.
Discussion
Our study showed that a CSEP-CEP–delivered physical activity counseling intervention increased average TPA10Mins, MVPA10Mins, and LPA10Mins measured via accelerometry within 4 months. Changes in LPA10Mins were dependent on fitness facility membership. There was no difference between the groups. However, use of an fHRA in the workplace did increase overall musculoskeletal fitness levels.
The increase in TPA10Mins and MVPA10Mins indicates participants were engaging in more planned physical activity amounting to 1 additional exercise session per week (20- to 40-minute increase). An increase in 1 exercise session per week could decrease stroke risk by up to 17%.16,17 Five participants were meeting the Canadian and American Physical Activity Guidelines18,19 at the end of the intervention, whereas only 1 participant met the guidelines at baseline.
Previous research has implied counseling and HRAs have their own effect that can be summed when interventions are used together.4 Our data suggest improvements are primarily due to counseling. Lack of an fHRA effect may be due to the method for assessing physical activity, as movements such as resistance training are not optimally captured by accelerometers.20,21
Few HRAs have used objectively measured physical activity as an outcome or looked at the effect of an fHRA in the workplace. Our study demonstrates that an fHRA can be used in the workplace with minimal equipment and resources and can elicit greater overall musculoskeletal health within 2 months. This has not previously been shown in the literature. The changes observed in push-ups and sit and reach scores in our study could be equated to a 1.79- and 1.93-fold improvement in work ability, respectively.22
Our CSEP-CEP–based program allowed us to create and deliver flexible and personalized physical activity interventions. Exercise prescriptions used resources already available to the participant, reducing the cost of the program. Results demonstrated that incorporating an exercise and health specialist in the workplace can be an effective means of health promotion. The CSEP-CEP certification is specific to Canada; however, individuals with comparable certifications, such as an American College of Sports Medicine Clinical Exercise Physiologist, would be able to deliver similar interventions.
The measures we used to assess physical activity were not able to capture resistance training in both the groups, which presented a challenge in assessing the intervention’s impact. Future research should combine activity logs with accelerometers to fully capture resistance training. Participants were able to choose their group. We allowed participants choice to facilitate better adherence.23 This also ensured results were more indicative of a real-world setting, where employees self-select programs to participate in. However, without using a randomized study design, we cannot say the results seen were solely due to the intervention. Participants and research staff were not blinded, although the primary outcome was objectively measured independent of research staff (ie, participants wore accelerometer for 7 days and did not have contact with staff during measurement) reducing measurement bias due to nonblinding.
The biggest challenge for this study was recruitment and sampling. Previous research piloting a similar intervention in the primary care setting recruited 119 (50%) of 237 possible participants. In comparison, only 78 (2%) of 4100 employees expressed interest in this study. This may be due to healthy individuals being less interested in a health intervention compared to those already in the primary care setting for a preexisting condition. Small sample size, gender imbalance, and the hospital setting (ie, employees are knowledgeable on health issues) impact the generalizability of results. Therefore, while results are promising, they should be interpreted with caution. Despite these limitations, out study provides valuable insight on the use of fHRAs and PAC in the workplace and how they may be used to improve physical activity levels of employees.
Supplemental Material
Supplementary_Material for A Quasi-Experimental Study Examining the Impact and Challenges of Implementing a Fitness-Based Health Risk Assessment and a Physical Activity Counseling Intervention in the Workplace Setting by Naomi C. Hamm, D. Scott Kehler, Jacqueline L. Hay, Andrew N. Stammers, Shaelyn M. Strachan, Danielle R. Bouchard and Todd A. Duhamel in Health Services Research and Managerial Epidemiology
Acknowledgments
The authors would like to acknowledge Alex Edye-Mazowita and Dustin Kimber for their contribution to the intervention by informing best practice approaches to physical activity counseling and for their feedback and support throughout data collection and manuscript preparation. The authors would also like to acknowledge the Manitoba Heart and Stroke Foundation for making the research possible through their Primary Prevention Grant program and thank the St Boniface General Hospital for their contributions to the project.
Author biographies
Naomi C. Hamm is a PhD candidate in Community Health Sciences at the University of Manitoba.
D. Scott Kehler completed a PhD at the University of Manitoba. He is now a CIHR funded postdoctoral fellow at Dalhousie University.
Jacqueline L. Hay is a Vanier Scholar and a PhD Student at the University of Manitoba.
Andrew N. Stammers was a CIHR Canada Graduate Scholarship awardee and graduated with a M.Sc. degree from the University of Manitoba.
Shaelyn M. Strachan is an associate professor at the University of Manitoba.
Danielle R. Bouchard is an associate professor at the University of New Brunswick.
Todd A. Duhamel is a professor at the University of Manitoba and Director of the Health, Leisure, and Human Performance Research Institute.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors received funding from the Manitoba Heart and Stroke Foundation.
ORCID iD: Naomi C. Hamm  https://orcid.org/0000-0002-8646-8995
https://orcid.org/0000-0002-8646-8995
Jacqueline L. Hay  https://orcid.org/0000-0002-4284-7141
https://orcid.org/0000-0002-4284-7141
Supplemental Material: Supplemental material for this article is available online
References
- 1. Proper KI, Staal BJ, Hildebrandt VH, van der Beek AJ, van Mechelen W. Effectiveness of physical activity programs at worksites with respect to work-related outcomes. Scand J Work Environ Health. 2002;28(2):75–84. [DOI] [PubMed] [Google Scholar]
- 2. Osilla KC, Van Busum K, Schnyer C, Larkin JW, Eibner C, Mattke S. Systematic review of the impact of worksite wellness programs. Am J Manag Care. 2012;18(2): e68–e81. [PubMed] [Google Scholar]
- 3. Conn VS, Hafdahl AR, Cooper PS, Brown LM, Lusk SL. Meta-analysis of workplace physical activity interventions. Am J Prev Med. 2009;37(4):330–339. doi:10.1016/j.amepre.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Soler RE, Leeks KD, Razi S, et al. A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. Am J Prev Med. 2010;38(2 suppl): S237–262. doi:10.1016/j.amepre.2009.10.030. [DOI] [PubMed] [Google Scholar]
- 5. Malik SH, Blake H, Suggs LS. A systematic review of workplace health promotion interventions for increasing physical activity. Br J Health Psychol. 2014;19(1):149–180. doi:10.1111/bjhp.12052. [DOI] [PubMed] [Google Scholar]
- 6. Gazmararian JA, Elon L, Newsome K, Schild L, Jacobson KL. A randomized prospective trial of a worksite intervention program to increase physical activity. Am J Health Promot AJHP. 2013;28(1):32–40. doi:10.4278/ajhp.110525-QUAN-220. [DOI] [PubMed] [Google Scholar]
- 7. Des Jarlais DC, Lyles C, Crepaz N, TREND Group. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the TREND statement. Am J Public Health. 2004;94(3):361–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Warburton DER, Gledhill N, Jamnik VK, et al. Evidence-based risk assessment and recommendations for physical activity clearance: Consensus Document 2011. Appl Physiol Nutr Metab Physiol Appliquée Nutr Métabolisme. 2011;36(suppl 1):S266–298. doi:10.1139/h11-062. [DOI] [PubMed] [Google Scholar]
- 9. Canadian Society for Exercise Physiology. CSEP-CEP Pre-requisites. CSEP. 2016. http://www.csep.ca/view.asp?ccid=535. Accessed November 23, 2018.
- 10. Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. [DOI] [PubMed] [Google Scholar]
- 11. Canadian Society for Exercise Physiology. Canadian Society for Exercise Physiology-Physical Activity Training for Health (CSEP-PATH). Ottawa, ON: Canadian Society for Exercise Physiology; 2013. [Google Scholar]
- 12. Trost SG, Mciver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research: Med Sci Sports Exerc. 2005;37(supplement):S531–S543. doi:10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 13. Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian adults: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011;22(1):7–14. [PubMed] [Google Scholar]
- 14. Matthews CE, Moore SC, Sampson J, et al. Mortality Benefits for Replacing Sitting Time with Different Physical Activities. Med Sci Sports Exerc. 2015. doi:10.1249/MSS.0000000000000621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Katapally TR, Muhajarine N. Towards uniform accelerometry analysis: a standardization methodology to minimize measurement bias due to systematic accelerometer wear-time variation. J Sports Sci Med. 2014;13(2):379–386. [PMC free article] [PubMed] [Google Scholar]
- 16. Ellekjær H, Holmen J, Ellekjær E, Vatten L. Physical activity and stroke mortality in women ten-year follow-up of the nord-trøndelag health survey, 1984–1986. Stroke. 2000;31(1):14–18. doi:10.1161/01.STR.31.1.14. [DOI] [PubMed] [Google Scholar]
- 17. Lee CD, Folsom AR, Blair SN. Physical activity and stroke risk: a meta-analysis. Stroke J Cereb Circ. 2003;34(10):2475–2481. doi:10.1161/01.STR.0000091843.02517.9D. [DOI] [PubMed] [Google Scholar]
- 18. Tremblay MS, Warburton DER, Janssen I, et al. New canadian physical activity guidelines. Appl Physiol Nutr Metab. 2011;36(1):36–46. doi:10.1139/H11-009. [DOI] [PubMed] [Google Scholar]
- 19. U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd Ed. Washington, DC: Department of Health and Human Services; 2018. [Google Scholar]
- 20. Esliger DW, Tremblay MS. Physical activity and inactivity profiling: the next generation. Can J Public Health Rev Can Santé Publique. 2007;98(suppl 2):S195–S207. [PubMed] [Google Scholar]
- 21. Chen KY, Bassett DR. The technology of accelerometry-based activity monitors: current and future. Med Sci Sports Exerc. 2005;37(suppl 11):S490–S500. [DOI] [PubMed] [Google Scholar]
- 22. Pohjonen T. Age-related physical fitness and the predictive values of fitness tests for work ability in home care work. J Occup Environ Med Am Coll Occup Environ Med. 2001;43(8):723–730. [DOI] [PubMed] [Google Scholar]
- 23. Janevic MR, Janz NK, Dodge JA, et al. The role of choice in health education intervention trials: a review and case study. Soc Sci Med. 2003;56(7):1581–1594. doi: 10.1016/S0277-9536(02)00158-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary_Material for A Quasi-Experimental Study Examining the Impact and Challenges of Implementing a Fitness-Based Health Risk Assessment and a Physical Activity Counseling Intervention in the Workplace Setting by Naomi C. Hamm, D. Scott Kehler, Jacqueline L. Hay, Andrew N. Stammers, Shaelyn M. Strachan, Danielle R. Bouchard and Todd A. Duhamel in Health Services Research and Managerial Epidemiology