Abstract
Background and aim: The aim of this work was to evaluate the relationship between platelet-to-lymphocyte ratio (PLR) and lymphocyte-to-monocyte ratio (LMR) with habitual consumption of dark chocolate in a group of celiac subjects in which chocolate consumption and lower neutrophil-to-lymphocyte ratio (NLR) association had already been observed. Additionally, due to the known anti-nutrient effect on iron absorption, we evaluated red blood cell count (RBC), mean corpuscular volume (MCV) and hemoglobin (Hb) values. Methods: Chocolate consumers and non-consumers were matched for sex, menopausal status, NLR values over the previously suggested cut off (2.32) for celiac patients, and co-morbidities. Results: Chocolate consumers had high LMR compared to non-consumers, whereas no differences were observed between chocolate consumers and non-consumers in RBC, MCV, Hb and PLR. However, similar number of subjects had PLR higher than the previously suggested cut off (143.7) for celiac disease. Conclusions: This preliminary report suggests a working hypothesis for larger studies aimed at establishing cut off values for LMR in celiac patients and the modulation of this marker by dietary antioxidants.
Keywords: inflammation, immunity, diet
1. Introduction
Chocolate contains both flavanols (epicatechin) and theobromine, non-nutrient bioactive compounds that can have potential pharmacological effects. Although it has been reported that a decrease in platelet activation in chocolate consumers can be ascribed to flavanols [1,2], Rull et al. [3] suggested that after six weeks of consumption such effect is modulated by a flavanol-independent mechanism that is likely due to theobromine. Although some recent studies suggested that catechins [4] and cocoa butter [5] may influence metabolic features, the improvement in cardio-metabolic risk factors (glucose levels, blood pressure, lipid profile) induced by cocoa or pure epicatechin is still under debate [6,7,8,9]. Moreover, it has been demonstrated that regular consumption of cocoa can exert anti-inflammatory effects by lowering the activation of monocytes and neutrophils [10]. We recently observed that chocolate consumption is associated with a lower neutrophil-to-lymphocyte ratio (NLR) in celiac subjects [11], in particular in those with NLR values above the cut off suggested by Sarikaya et al. (2.32) [12], supporting the previously reported hypothesis that the efficacy of cocoa products depends on the basal inflammatory status [10].
Platelet-to-lymphocyte ratio (PLR) and lymphocyte-to-monocyte ratio (LMR) have also been proposed as markers of inflammation in celiac disease [13,14] and acute ischemic stroke [15,16,17], and peripheral arterial [18], cardiovascular [19,20] and autoimmune [21] diseases. In particular, decreased LMR has been associated with increased disease activity in rheumatoid arthritis [21].
Meta-analysis data reported an increase in some cardiovascular risk factors (total cholesterol and fasting glycaemia) after a long-term gluten-free diet (GFD) [22] and a significantly heightened risk of venous thromboembolism among patients with celiac disease (CD) [23]. The aim of this work was to evaluate the relationship between both PLR and LMR and habitual consumption of dark chocolate in previously analyzed celiac subjects [11]. Moreover, given its well-known anti-nutrient effect on iron absorption [24], we evaluated potential differences on red blood cell count (RBC), mean corpuscular volume (MCV) and hemoglobin (Hb) values.
2. Materials and Methods
2.1. Selection of Subjects
We extracted the data from a recent study [11], approved by the Ethics Committee of the Comitato Etico Lazio 2 (n° 43.18: 4, 2018). Written informed consent was obtained from all the participants in accordance with the Italian law (number 76/2008) and all procedures involving human subjects complied with the Declaration of Helsinki as revised in 2000.
Chocolate consumers (1–3 times/week, n = 13) included celiac subjects all with Marsh III at diagnosis (2 men and 11 women). The chocolate non-consumers were selected within celiac subjects with Marsh III at diagnosis, matching for sex, menopausal status (3 in each group), NLR values over the cut off suggested by Sarikaya et al. [12] (4 in each group) and co-morbidities (2 thyroiditis, 1 allergy, 1 autoimmune disease: vitiligo/psoriasis). The two groups had similar smoking (3/10) habits.
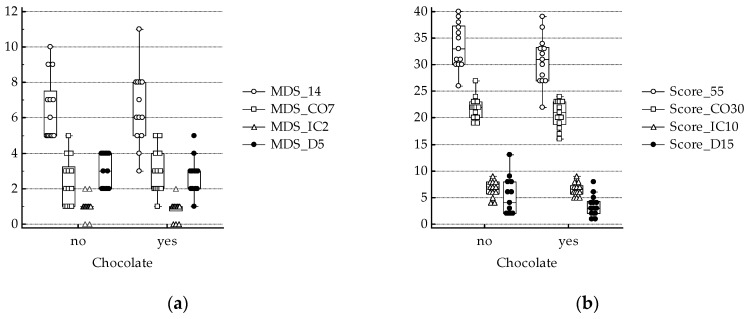
The physical activity level (PAL), was evaluated by the International Physical Activity Questionnaire (IPAQ) and the adherence to Mediterranean diet was assessed with two different scores (the Mediterranean Diet Score: MDS 14: 14 items, each 0–1 score; and the MEDScore: Score 55: 11 items, each score range 0–5) as previously described [11]. In addition, sub-scores were calculated as follows: coherent (CO, high consumption of olive oil, fruits, vegetables, legumes, and fish and low consumption of red meat; ranges: 0–7 MDS CO7 and 0–30 Score CO30), incoherent (IC: wine and white meat, high consumption for MDS and low consumption for Score; ranges: 0–2 MDS IC2 and 0–10 Score IC10) and different (D: high consumption of nuts and Mediterranean sauce; and low consumption of butter, carbonated beverage and sweets for MDS; high consumption of unrefined cereals and potatoes, and low consumption of full dairy products for Score; ranges: 0–5 MDS D5 and 0–15 Score D15) [11].
2.2. Statitical Analysis
Data were expressed as means with standard error mean (SEM) (Normality Test (Shapiro–Wilk) passed, two tailed T Test applied) or median (25%, 75%) (Normality Test (Shapiro–Wilk) failed, Rank Sum Test applied). The correlations (Spearman correlation) were analyzed between the parameters of interest.
3. Results
Selected groups were similar in age, years at gluten-free diet (GFD), body mass index (BMI), systolic (SBP) and diastolic (DBP) blood pressure (mmHg) (Table 1). Overall (n = 26), platelets’ count (P) were inversely related to PAL (metabolic equivalent of task: MET) (coefficient of correlation –0.397, p = 0.044), which correlated both with Hb (coefficient of correlation 0.548, p = 0.004) and MCV (coefficient of correlation 0. 509, p = 0.008). On the other hand, no differences were observed in PAL (Table 1), P and markers of anemia (RBC, MCV and Hb) between chocolate consumers and non-consumers (Table 2).
Table 1.
Characteristics of subjects.
| Chocolate | YES (n = 13) | NO (n = 13) |
|---|---|---|
| Men/women | 2/11 | 2/11 |
| Age (years) | 44.0 ± 3.7 | 36.8 ± 3.5 |
| GFD (years) | 2 (1–10) | 2 (1–7) |
| PAL (MET-min-week) | 6166 ± 891 | 7518 ± 1379 |
| BMI (Kg/m2) | 22.1 ± 0.5 | 22.2 ± 0.6 |
| SBP (mmHg) | 116.9 ± 3.1 | 108.4 ± 3.1 |
| DBP (mmHg) | 72.5 ± 2.4 | 69.8 ± 4.0 |
GFD: gluten-free diet; PAL: physical activity level; MET: metabolic equivalent of task; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure. Data are expressed as mean and SEM (Normality Test (Shapiro–Wilk) passed) or median and interquartile range (25%–75%) (Normality Test failed).
Table 2.
Hematological parameters.
| Chocolate | YES (n = 13) | NO (n = 13) |
|---|---|---|
| WBC (103/microL) | 6.2 (4.5–6.8) | 5.4 (4.5–9.0) |
| N (103/microL) | 3.1 (2.2–4.3) | 3.5 (2.2–5.8) |
| M (103/microL) | 0.36 (0.32–0.54) | 0.44 (0.37–0.66) |
| L (103/microL) | 1.9 (1.4–2.4) | 1.7 (1.1–2.0) |
| P (103/microL) | 275.4 ± 14.8 | 253.8 ± 19.0 |
| RBC (106/microL) | 4.7 ± 0.1 | 4.7 ± 0.1 |
| MCV (fL) | 85.5 (77.5–87.3) | 88.4 (82.9–92.3) |
| Hb (g/dL) | 12.5 ± 0.6 | 13.5 ± 0.3 |
WBC: white blood cell count; N: neutrophil count; M: monocyte count; L: lymphocyte count; RBC: red blood cell count; MCV: mean corpuscular volume; Hb: hemoglobin. Data are expressed as mean and SEM (Normality Test (Shapiro–Wilk) passed) or median and interquartile range (25%–75%) (Normality Test failed).
We recently reported that NLR correlated with Score 55 and Score CO30 [11]. In the present study, although N correlated with Score 55 (coefficient of correlation 0.393, p = 0.046) and Score D15 (coefficient of correlation 0.424, p = 0.031) and the latter was also related to white blood cell count (WBC, coefficient of correlation 0.536, p = 0.005), significant differences between groups were not found for WBC and leucocytes’ subset counts (N: neutrophils, M: monocytes, L: lymphocytes; Table 2), as well as for adherence to Mediterranean diet (Figure 1).
Figure 1.
Adherence to Mediterranean diet (a) MDS 14 and sub-scores: coherent (CO7), incoherent (IC2) and different (D5); description of what is contained in the first panel; (b) Score 55 and sub-scores: coherent (CO30), incoherent (IC10) and different (D15). No significant differences between chocolate consumers and non-consumers.
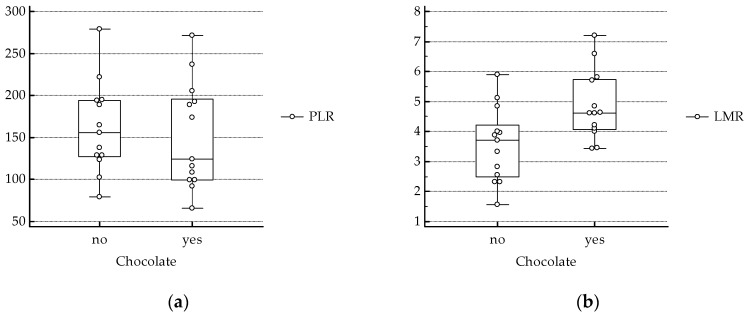
On the other hand, NLR, lower in chocolate consumers [11], correlated with PLR (coefficient of correlation 0.588, p = 0.002), and was inversely related to LMR (coefficient of correlation −0.696, p < 0.001) (Figure 2).
Figure 2.
(a) PLR: platelet-to-lymphocyte ratio. No significant differences between chocolate consumers and non-consumers. (b) LMR: lymphocyte-to-monocyte ratio, Normality Test (Shapiro–Wilk) passed, two tailed T Test (chocolate yes versus no: p = 0.01).
4. Discussion and Conclusions
In this study we observed higher values of LMR in celiac subjects who consumed chocolate compared to non-consumers, whereas no significant differences were found in markers of anemia and PLR. One of the criteria for inclusion was the same number of subjects with NLR values over the cut off suggested by Sarikaya et al. [12] in the two groups. Consistent with the high correlation between PLR and NLR, similar number of subjects (6/13 consumers, 7/13 non-consumers) had PLR higher than the suggested cut off (143.7) for celiac disease [13,14]. Therefore, we did not observe significant differences in PLR between the two groups. Interestingly, while lower LMR and higher NLR were associated to short-term (30 days) mortality in patients with acute pulmonary embolism, PLR was not significantly different between survivors and non-survivors [25]. This suggests that PLR is a less sensitive marker of inflammation compared to NLR and LMR.
A lower LMR value is also an independent predictor of poor prognosis of some diseases and their outcomes. The suggested cut off values were 3.48 for neurologic impairment after acute ischemic stroke (AIS) [15], 3.38 for well-developed coronary collateral circulation in patients with stable coronary artery disease [19], 3.1 for critical limb ischemia in peripheral arterial occlusive disease [18], 2.99 for stroke severity and prognosis [16] and 2.0 for the six-month all-cause mortality in patients with acute heart failure [20]. Moreover, LMR has been suggested as a useful marker for stroke-induced immunosuppression [17]. Among AIS patients (on day one and seven), it was significantly lower in those also affected by pneumonia or urinary tract infection [17]. A meta-analysis of studies on celiac disease also suggested that it is associated with an increased risk of pneumococcal infection [26].
Furthermore, in rheumatoid arthritis, LMR was inversely correlated with inflammatory and immune-related markers (including PLR, NLR, immunoglobulin (Ig)A and IgM) and positively correlated with nutritional status markers (such as Hb and albumin) [21], suggesting a relationship between diet and autoimmune diseases. In this context, in the animal model of adjuvant arthritis in rats, a cocoa-enriched diet decreased antibody concentration and the T-helper (Th) lymphocytes and prevented the decrease in the proportion of regulatory T-cells in blood [27].
The work presented here is a preliminary study and has some limits. First of all, although sweets consumption (included in the MDS 5) did not differ between groups and the standard portion size was 30 g, we could not collect any information about either the percentage of cocoa in the consumed dark chocolate or food preference. The latter is the main factor driving food intake and choice and depends on many factors, including individual differences in human perception of sweetness partly due to polymorphisms in the taste-related genes TAS1R2/TAS1R3 [28,29,30,31] and interactions between bitter and sweet taste systems [32]. It is well known that in cacao polyphenolic compounds show both bitter and astringent characteristics, with a rejection threshold depending on percentage of cocoa in chocolate [33]. However, products with a psychoactive effect (such as coffee and chocolate) are generally preferred, regardless of their bitterness, and traits of consumers and health concerns could affect food preferences of bitter in vegetable foods [34]. Moreover, the relationship between TAS1R2/TAS1R3 and intake of sweet-tasting foods may be different across different populations [35,36]. In this context, chocolate accounted for 25%, 18% and 8% of flavanols, flavonoids and total polyphenols intake in Poland [37], but only for 7% of flavanols intake in Italy, where the main dietary sources of total polyphenols are nuts, followed by tea and coffee [38]. Moreover, other typical foods of Mediterranean diet, such as fruits and vegetables (including beans), contain high levels of polyphenols [38]. However, in the present study no differences were observed in sub-scores of Mediterranean diet adherence, including fruits, vegetables, legumes and nuts.
In conclusion, despite this pilot study’s low number of subjects and their low to moderate chocolate consumption (1–3 times/week), this preliminary report suggests a working hypothesis for larger studies aimed at establishing cut off values for LMR in celiac patients and its modulation by cocoa antioxidants.
Author Contributions
Formal analysis and data curation, A.R., E.T. and F.P.; writing—review and editing, all authors; supervision, I.P.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Paglieroni T.G., Janatpour K., Gosselin R., Crocker V., Dwyre D.M., MacKenzie M.R., Holland P.V., Larkin E.C. Platelet function abnormalities in qualified whole-blood donors: Effects of medication and recent food intake. Vox Sang. 2004;86:48–53. doi: 10.1111/j.0042-9007.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- 2.Bordeaux B., Yanek L.R., Moy T.F., White L.W., Becker L.C., Faraday N., Becker D.M. Casual chocolate consumption and inhibition of platelet function. Prev. Cardiol. 2007;10:175–180. doi: 10.1111/j.1520-037X.2007.06693.x. [DOI] [PubMed] [Google Scholar]
- 3.Rull G., Mohd-Zain Z.N., Shiel J., Lundberg M.H., Collier D.J., Johnston A., Warner T.D., Corder R. Effects of high flavanol dark chocolate on cardiovascular function and platelet aggregation. Vasc. Pharmacol. 2015;71:70–78. doi: 10.1016/j.vph.2015.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Chen P.B., Kim J.H., Young L., Clark J.M., Park Y. Epigallocatechin gallate (EGCG) alters body fat and lean mass through sex-dependent metabolic mechanisms in Drosophila melanogaster. Int. J. Food Sci. Nutr. 2019:1–11. doi: 10.1080/09637486.2019.1602113. [DOI] [PubMed] [Google Scholar]
- 5.Cheng C., Wang D., Xia H., Wang F., Yang X., Pan D., Wang S., Yang L., Lu H., Shu G., et al. A comparative study of the effects of palm olein, cocoa butter and extra virgin olive oil on lipid profile, including low-density lipoprotein subfractions in young healthy Chinese people. Int. J. Food Sci. Nutr. 2019;70:355–366. doi: 10.1080/09637486.2018.1504009. [DOI] [PubMed] [Google Scholar]
- 6.Dicks L., Kirch N., Gronwald D., Wernken K., Zimmermann B.F., Helfrich H.-P., Ellinger S. Regular Intake of a Usual Serving Size of Flavanol-Rich Cocoa Powder Does Not Affect Cardiometabolic Parameters in Stably Treated Patients with Type 2 Diabetes and Hypertension-A Double-Blinded, Randomized, Placebo-Controlled Trial. Nutrients. 2018;10:1435. doi: 10.3390/nu10101435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirch N., Berk L., Liegl Y., Adelsbach M., Zimmermann B.F., Stehle P., Stoffel-Wagner B., Ludwig N., Schieber A., Helfrich H.-P., et al. A nutritive dose of pure (-)-epicatechin does not beneficially affect increased cardiometabolic risk factors in overweight-to-obese adults-a randomized, placebo-controlled, double-blind crossover study. Am. J. Clin. Nutr. 2018;107:948–956. doi: 10.1093/ajcn/nqy066. [DOI] [PubMed] [Google Scholar]
- 8.Lin X., Zhang I., Li A., Manson J.E., Sesso H.D., Wang L., Liu S. Cocoa Flavanol Intake and Biomarkers for Cardiometabolic Health: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Nutr. 2016;146:2325–2333. doi: 10.3945/jn.116.237644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beale D.J. Inappropriate Inclusion of 3 Trials Leads to Misleading Results in Meta-Analysis of Cocoa Flavanol Intake and Cardiometabolic Health. J. Nutr. 2017;147:976. doi: 10.3945/jn.116.243709. [DOI] [PubMed] [Google Scholar]
- 10.Ellinger S., Stehle P. Impact of Cocoa Consumption on Inflammation Processes-A Critical Review of Randomized Controlled Trials. Nutrients. 2016;8:321. doi: 10.3390/nu8060321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palmacci F., Toti E., Raguzzini A., Catasta G., Aiello P., Peluso I., Biava M., Palmery M. Neutrophil-to-Lymphocyte Ratio, Mediterranean Diet, and Bone Health in Coeliac Disease Patients: A Pilot Study. Oxidative Med. Cell. Longev. 2019;2019:1–14. doi: 10.1155/2019/7384193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sarikaya M., Dogan Z., Ergul B., Filik L. Neutrophil-to-lymphocyte ratio as a sensitive marker in diagnosis of celiac disease. Ann. Gastroenterol. 2014;27:431–432. [PMC free article] [PubMed] [Google Scholar]
- 13.Balaban D.V., Popp A., Beata A., Vasilescu F., Jinga M. Diagnostic accuracy of red blood cell distribution width-to-lymphocyte ratio for celiac disease. Revista Română de Medicină de Laborator. 2018;26:45–50. doi: 10.1515/rrlm-2017-0040. [DOI] [Google Scholar]
- 14.Sarikaya M., Dogan Z., Ergul B., Filik L. Platelet-to-lymphocyte ratio for early diagnosis of celiac disease. Indian J. Gastroenterol. 2015;34:182–183. doi: 10.1007/s12664-014-0493-8. [DOI] [PubMed] [Google Scholar]
- 15.Ren H., Han L., Liu H., Wang L., Liu X., Gao Y. Decreased Lymphocyte-to-Monocyte Ratio Predicts Poor Prognosis of Acute Ischemic Stroke Treated with Thrombolysis. Med. Sci. Monit. 2017;23:5826–5833. doi: 10.12659/MSM.907919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ren H., Liu X., Wang L., Gao Y. Lymphocyte-to-Monocyte Ratio: A Novel Predictor of the Prognosis of Acute Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2017;26:2595–2602. doi: 10.1016/j.jstrokecerebrovasdis.2017.06.019. [DOI] [PubMed] [Google Scholar]
- 17.Park M.G., Kim M.K., Chae S.H., Kim H.K., Han J., Park K.P. Lymphocyte-to-monocyte ratio on day 7 is associated with outcomes in acute ischemic stroke. Neurol. Sci. 2018;39:243–249. doi: 10.1007/s10072-017-3163-7. [DOI] [PubMed] [Google Scholar]
- 18.Gary T., Pichler M., Belaj K., Eller P., Hafner F., Gerger A., Brodmann M. Lymphocyte-to-monocyte ratio: A novel marker for critical limb ischemia in PAOD patients. Int. J. Clin. Pract. 2014;68:1483–1487. doi: 10.1111/ijcp.12495. [DOI] [PubMed] [Google Scholar]
- 19.Duran M., Kurtul A. The correlation between lymphocyte/monocyte ratio and coronary collateral circulation in stable coronary artery disease patients. Biomark. Med. 2017;11:43–52. doi: 10.2217/bmm-2016-0179. [DOI] [PubMed] [Google Scholar]
- 20.Silva N., Bettencourt P., Guimarães J.T. The lymphocyte-to-monocyte ratio: An added value for death prediction in heart failure. Nutr. Metab. Cardiovasc. Dis. 2015;25:1033–1040. doi: 10.1016/j.numecd.2015.07.004. [DOI] [PubMed] [Google Scholar]
- 21.Du J., Chen S., Ying H., Li J., Shi J., Zhu X., Zhang Y., Shen B. The association between the lymphocyte-monocyte ratio and disease activity in rheumatoid arthritis. Clin. Rheumatol. 2017;36:2689–2695. doi: 10.1007/s10067-017-3815-2. [DOI] [PubMed] [Google Scholar]
- 22.Potter M.D.E., Brienesse S.C., Walker M.M., Boyle A., Talley N.J. Effect of the gluten-free diet on cardiovascular risk factors in patients with coeliac disease: A systematic review. J. Gastroenterol. Hepatol. 2018;33:781–791. doi: 10.1111/jgh.14039. [DOI] [PubMed] [Google Scholar]
- 23.Ungprasert P., Wijarnpreecha K., Tanratana P. Risk of venous thromboembolism in patients with celiac disease: A systematic review and meta-analysis. J. Gastroenterol. Hepatol. 2016;31:1240–1245. doi: 10.1111/jgh.13282. [DOI] [PubMed] [Google Scholar]
- 24.Hurrell R.F., Reddy M., Cook J.D. Inhibition of non-haem iron absorption in man by polyphenolic-containing beverages. Br. J. Nutr. 1999;81:289–295. doi: 10.1017/S0007114599000537. [DOI] [PubMed] [Google Scholar]
- 25.Ertem A.G., Yayla C., Acar B., Kirbas O., Unal S., Sener M.U., Akboga M.K., Efe T.H., Sivri S., Sen F., et al. Relation between lymphocyte to monocyte ratio and short-term mortality in patients with acute pulmonary embolism. Clin. Respir. J. 2018;12:580–586. doi: 10.1111/crj.12565. [DOI] [PubMed] [Google Scholar]
- 26.Simons M., Scott-Sheldon L.A., Risech-Neyman Y., Moss S.F., Ludvigsson J.F., Green P.H. Celiac Disease and Increased Risk of Pneumococcal Infection: A Systematic Review and Meta-Analysis. Am. J. Med. 2018;131:83–89. doi: 10.1016/j.amjmed.2017.07.021. [DOI] [PubMed] [Google Scholar]
- 27.Ramos-Romero S., Perez-Cano F.J., Castellote C., Castell M., Franch A. Effect of cocoa-enriched diets on lymphocytes involved in adjuvant arthritis in rats. Br. J. Nutr. 2012;107:378–387. doi: 10.1017/S0007114511003035. [DOI] [PubMed] [Google Scholar]
- 28.Pioltine M.B., De Melo M.E., Santos A.S., Machado A.D., Fernandes A.E., Fujiwara C.T., Cercato C., Mancini M.C. Genetic Variations in Sweet Taste Receptor Gene Are Related to Chocolate Powder and Dietary Fiber Intake in Obese Children and Adolescents. J. Pers. Med. 2018;8:7. doi: 10.3390/jpm8010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Melo S.V., Agnes G., Vitolo M.R., Mattevi V.S., Campagnolo P.D., Almeida S. Evaluation of the association between the TAS1R2 and TAS1R3 variants and food intake and nutritional status in children. Genet. Mol. Boil. 2017;40:415–420. doi: 10.1590/1678-4685-gmb-2016-0205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Priego T., Sanchez J., Pico C., Ahrens W., de Henauw S., Kourides Y., Lissner L., Molnar D., Moreno L.A., Russo P., et al. TAS1R3 and UCN2 Transcript Levels in Blood Cells Are Associated with Sugary and Fatty Food Consumption in Children. J. Clin. Endocrinol. Metab. 2015;100:3556–3564. doi: 10.1210/JC.2015-1976. [DOI] [PubMed] [Google Scholar]
- 31.Han P., Keast R.S.J., Roura E. Salivary leptin and TAS1R2/TAS1R3 polymorphisms are related to sweet taste sensitivity and carbohydrate intake from a buffet meal in healthy young adults. Br. J. Nutr. 2017;118:763–770. doi: 10.1017/S0007114517002872. [DOI] [PubMed] [Google Scholar]
- 32.Joseph P.V., Reed D.R., Mennella J.A. Individual Differences Among Children in Sucrose Detection Thresholds: Relationship with Age, Gender, and Bitter Taste Genotype. Nurs. Res. 2016;65:3–12. doi: 10.1097/NNR.0000000000000138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harwood M.L., Ziegler G.R., Hayes J.E. Tolerance for High Flavanol Cocoa Powder in Semisweet Chocolate. Nutrients. 2013;5:2258–2267. doi: 10.3390/nu5062258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cavallo C., Cicia G., Del Giudice T., Sacchi R., Vecchio R. Consumers’ Perceptions and Preferences for Bitterness in Vegetable Foods: The Case of Extra-Virgin Olive Oil and Brassicaceae—A Narrative Review. Nutrients. 2019;11:1164. doi: 10.3390/nu11051164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hwang L.-D., Lin C., Gharahkhani P., Cuellar-Partida G., Ong J.-S., An J., Gordon S.D., Zhu G., MacGregor S., Lawlor D.A., et al. New insight into human sweet taste: A genome-wide association study of the perception and intake of sweet substances. Am. J. Clin. Nutr. 2019;109:1724–1737. doi: 10.1093/ajcn/nqz043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pirastu N., Robino A., Lanzara C., Athanasakis E., Esposito L., Tepper B.J., Gasparini P. Genetics of Food Preferences: A First View from Silk Road Populations. J. Food Sci. 2012;77:S413–S418. doi: 10.1111/j.1750-3841.2012.02852.x. [DOI] [PubMed] [Google Scholar]
- 37.Grosso G., Stepaniak U., Topór-Mądry R., Szafraniec K., Pająk A. Estimated dietary intake and major food sources of polyphenols in the Polish arm of the HAPIEE study. Nutrients. 2014;30:1398–1403. doi: 10.1016/j.nut.2014.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Godos J., Marventano S., Mistretta A., Galvano F., Grosso G. Dietary sources of polyphenols in the Mediterranean healthy Eating, Aging and Lifestyle (MEAL) study cohort. Int. J. Food Sci. Nutr. 2017;68:750–756. doi: 10.1080/09637486.2017.1285870. [DOI] [PubMed] [Google Scholar]