Abstract
Fatigue in RA is prevalent, intrusive and disabling. We propose a network model of fatigue encompassing multiple and mutually interacting biological, psychological and social factors. Guided by this model, we reviewed the literature to offer a comprehensive overview of factors that have been associated with fatigue in RA. Six categories of variables were found: physical functioning, psychological functioning, medical status, comorbidities and symptoms, biographical variables and miscellaneous variables. We then systematically reviewed associations between fatigue and factors commonly addressed by rheumatology health professionals. Correlations of fatigue with physical disability, poor mental well-being, pain, sleep disturbance and depression and anxiety were ∼0.50. Mostly these correlations remained significant in multivariate analyses, suggesting partly independent influences on fatigue and differences between individuals. These findings indicate the importance of research into individual-specific networks of biopsychosocial factors that maintain fatigue and tailored interventions that target the influencing factors most relevant to that person.
Keywords: biopsychosocial model, depression, disease activity, fatigue, obesity, pain, physical functioning, psychological functioning, rheumatoid arthritis, sleep
Rheumatology key messages
Associations of fatigue with factors that are amenable to behavioural change are moderate to high.
Multivariate analyses suggest partial independence of factors influencing fatigue that differ between individuals.
Future research should examine tailored interventions targeting individual-specific networks of biopsychosocial factors that maintain fatigue.
Introduction
Fatigue in RA is prevalent, intrusive and disabling [1–3]. Appropriate management of fatigue can increase well-being and functioning and may reduce individual and societal costs. To be able to offer comprehensive patient-centred care aimed at reducing fatigue, insight into its maintaining factors is needed.
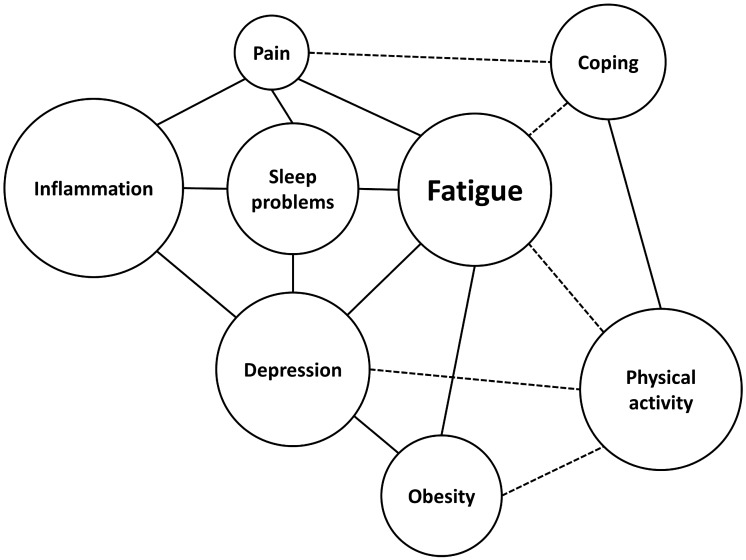
Fatigue is a multifaceted experience associated with a wide range of variables [4, 5]. Based on existing models [4] and in analogy to pain [6], we suggest that fatigue may be conceptualized as a network model in which fatigue encompasses multiple and mutually interacting biological, psychological and social factors (Fig. 1). These include, but are not limited to, disease activity (inflammation), physical activity, sleep problems, obesity, psychological resilience and vulnerability (emotions, cognitions, behaviour) and social factors (work, financial resources). Rather than one-directional relationships, the relationships between all the factors in this biopsychosocial model are assumed to be dynamic and reciprocal, with mutually influencing pathways. Another assumption is that individuals differ in terms of the factors involved in their fatigue, as well as in the importance of both the weight of these factors and the strength of the relationships between these factors.
Fig. 1.
Network model reflecting factors that are associated with fatigue
Relations between all factors of this biopsychosocial model are assumed to be dynamic and reciprocal, with mutually influencing pathways similar to a hanging mobile toy, in which movement of one factor causes changes in all other factors. Another assumption is that individuals differ in terms of the factors involved in fatigue as well as the importance of both the weight of these factors and the strength of the relationships between these factors.
Guided by this model, and acknowledging that there are few longitudinal studies of within-participant variations in fatigue, our first aim was to review the literature to offer a comprehensive overview of factors associated with fatigue. Rather than focusing on causation and high correlations, we aimed to identify any factor that is associated with fatigue, because it may be an important factor for a specific individual. Our second aim was to systematically review associations of fatigue with factors that are commonly treated by rheumatology health professionals: physical functioning, psychological functioning, pain, sleep disturbance, obesity and depression and anxiety. We also reviewed biographic variables, but not disease activity and interventions, because these are covered by other articles in this issue.
Methods
Scope
The Population, Interventions, Comparison and Outcomes algorithm guided the definition of the scope [7]. The target population was adult patients with RA. Any study that focused on RA with fatigue as a predictor or outcome variable of interest was considered, including those using qualitative, cross-sectional, longitudinal, experimental (laboratory or clinical) and experience sampling (ecological momentary assessment [EMA]) methods, because we wanted to clarify all variables that might interact with fatigue.
Literature review
The bibliographic databases Cochrane Library, Embase, PsycINFo, PubMed, Scopus and Web of Science were searched with the words ‘fatigue’ and ‘rheumatoid arthritis’ in the title or the words ‘fatigue’ and ‘RA’ in the title and the words ‘rheumatoid arthritis’ in the abstract (search date 19 January 2019). A protocol for the systematic review was not registered a priori. After removal of duplicates, all abstracts were read independently and judged on their suitability for inclusion by two reviewers (RG, ED). Results were compared and, in case of discrepancy, discussed until consensus was reached. Excluded were duplicate articles, articles not written in English, animal studies, conference abstracts, articles not reporting associations with fatigue, studies not in RA and studies that are reviewed in other articles of this issue (studies relating fatigue to disease activity, intervention studies). The detailed search keys and selection are shown in Supplementary Tables S1 and S2, available at Rheumatology online.
Analysis
Since the first part of the study focused on finding any relation between fatigue and any variable that might be relevant for an individual patient with RA, both assessors read abstracts to derive variables that were subsequently categorized in factors. While reading the abstracts, both reviewers made notes of the variables that had been associated with fatigue. These notes were used to make a comprehensive overview and subsequently to select articles for the systematic review. The univariate and multivariate cross-sectional and longitudinal relationships of fatigue with pain, sleep disturbance, obesity, depression and anxiety and biographical variables were then summarized from the selected articles.
Results
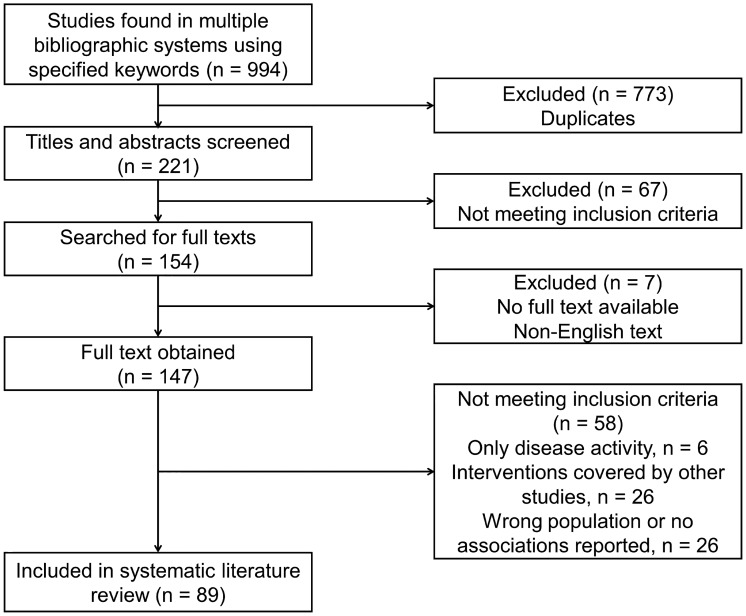
Figure 2 shows a flow chart of the systematic literature review. The 994 selected titles were reduced to 154 after checking exclusion criteria using the abstracts. The 154 abstracts were read to derive variables associated with fatigue (aim 1). For aim 2 (the systematic review), 89 articles reported results of cross-sectional or longitudinal associations of fatigue with the variables selected for systematic review. Of the 58 excluded studies, 32 were covered by other studies in this issue that focused on disease activity and biological variables, or interventions. Twenty-six studies reported no associations between the selected variables and fatigue or included populations other than RA.
Fig. 2.
Flow chart of the literature review
Overview of variables associated with fatigue
Both assessors agreed on six categories, with three to five subcategories each to reflect their contents, that captured the variables associated with fatigue (Table 1; the full list is shown in Supplementary Table S3, available at Rheumatology online). The selected variables were reviewed and correlations reported if more than two were available. Results of the systematic literature review of variables associated with fatigue are shown in Table 2.
Table 1.
Categories of variables that have been associated with fatigue in patients with RA
| 1. Physical functioning Physical (dis)abilitya Physical capacitya Physical activitya Physical activity interventions | 4. Comorbidities and symptoms Paina Sleep disturbancea Obesitya Depression and anxietya Comorbid diseases Physiological aberrations |
| 2. Psychological functioning Mental well-beinga Stress and stressorsa Psychological management and relational factorsa Psychological interventions and management | 5. Biographical variables Demographic variablesa Worka Relations and rolesa |
| 3. Medical status Disease activity Pharmacological treatment | 6. Miscellaneous Seasonal effects Cognitive dysfunction Unusual therapies |
These variables were reviewed in the current study.
Table 2.
Results of the systematic literature review
| Variable | Cross-sectional association with fatiguea | Longitudinal association with fatigueb | ||
|---|---|---|---|---|
| Yes | No | Yes | No | |
| Physical functioning | ||||
| Physical (dis)ability | ||||
| Physical function (−) | Univariate, 4 studies [8–11] Multivariate, 2 studies [10, 11] | Univariate, 2 studies [12, 13] Multivariate, 1 study [13] | ||
| Physical role functioning (−) | Univariate, 6 studies [8–12, 14] Multivariate, 2 studies [10, 11] | Univariate, 1 study [13] Multivariate, 1 study [13] | ||
| (Dis)ability (+) | Univariate, 20 studies [10, 12, 14–31] Multivariate, 10 studies [17, 24–28, 32–35] | Multivariate, 4 studies [10, 18, 25, 29] | Univariate, 2 studies [27, 36] Multivariate, 3 studies [27, 37, 38] | |
| Physical capacity (–) | Univariate, 1 study [39] | Univariate, 3 studies [18, 40, 41] Multivariate, 2 studies [18, 39] | ||
| Physical activity (−) | Univariate, 5 studies [10, 25, 30, 42–44] Multivariate, 2 studies [32, 44] | Univariate, 2 studies [18, 40] Multivariate, 3 studies [10, 18, 25] | 4 meta-analyses of physical activity interventions [45–48] | Univariate, 1 study [39] Multivariate, 1 study [39] |
| Psychological functioning | ||||
| Mental well-being (–) | ||||
| Mental health (−) | Univariate, 4 studies [9, 10, 24, 31] | Univariate, 3 studies [8, 12, 13] Multivariate, 1 study [13] | Multivariate change in fatigue, 2 studies [37, 38] | Multivariate change in fatigue, 1 study [38] |
| Emotional role functioning (−) | Univariate. 4 studies [8, 9, 14, 24] | Univariate. 1 study [13] Multivariate. 1 study [13] | ||
| Social functioning (−) | Univariate, 4 studies [9, 10, 14, 24] | Univariate, 1 study [13] Multivariate, 1 study [13] | ||
| Stress and stressors (+) | ||||
| Chronic stress (+) | Univariate, 3 studies [27, 49, 50] Multivariate, 1 study [27] | Multivariate, 1 study [50] | ||
| Daily stressors and events (+) | Univariate correlation level, 1 study [27] Multivariate correlation level, 1 study [27] EMA, 3 studies [51–53] | Multivariate correlation level, 1 study [27] Multivariate correlation change, 1 study [27] EMA, 1 study [54] | ||
| Psychological management and relational factors (–) | ||||
| Self-efficacy (−) | Univariate, 8 studies [10, 11, 21, 29, 50, 55–57] Multivariate, 2 studies [21, 29] | Multivariate, 2 studies [50, 55] | ||
| Coping (−) | Univariate, 3 studies [10, 58, 59] Multivariate, 1 study [58] | Univariate, 3 studies [50, 56, 59] Multivariate, 2 studies [50, 58] | Fatigue change [58] | Fatigue level, 1 study [56] Fatigue change, 2 studies [56, 58] |
| Social support (−) | Univariate, 4 studies [10, 27, 29, 55] Multivariate, 4 studies [27, 29, 50, 55] | Univariate, 2 studies [10, 50] | Fatigue level, 1 study [27] Fatigue change, 1 study [27] | |
| Comorbidities and symptoms | ||||
| Pain (+) | Univariate, 24 studies [8, 10, 12, 13, 15, 17–20, 24, 31, 39, 40, 50, 60–69] Multivariate, 10 studies [10, 17, 18, 32, 39, 50, 61, 63, 66, 70] EMA, 1 study [62] | Univariate, 1 study [8] Multivariate, 1 study [13] | Univariate correlation levels, 2 studies [66, 71] Multivariate correlation levels, 1 study [66] Univariate correlation changes, 4 studies [37, 70, 72, 73] | Univariate correlation levels, 2 studies [39, 56] Multivariate correlation, 1 study [39] EMA diurnal, 1 study [54] EMA monthly, 1 study [71] |
| Sleep disturbance (+) | Univariate, 14 studies [8, 10, 25, 27, 30–32, 49, 56, 67, 74–77] Multivariate, 8 studies [10, 25, 32, 49, 75, 76, 78] EMA 1 study [62]. | Univariate, 1 study [64] Multivariate,1 study [77] | Correlational, 1 study [56] EMA, 2 studies [54, 78] | Correlational. 3 studies [56, 64, 79] Experimental. 1 study [80] |
| Obesity (+) | Univariate, 1 study [25] Multivariate, 1 study [25, 39] | Univariate, 2 studies [18, 39] Multivariate, 1 study [39] | Correlational, 1 study [39] | |
| Depression (+) | Univariate, 15 studies [8, 16, 19, 22, 25, 27, 39, 40, 50, 56, 58, 64, 68, 75, 81] Multivariate, 7 studies [19, 25, 39, 40, 50, 75, 77] | Multivariate, 1 study [27] | Univariate correlation level, 4 studies [22, 27, 39, 58] Multivariate correlation level, 1 study [58] Outcome, 2 studies [37, 38] | Univariate correlation level, 1 study [58] Multivariate correlation level, 2 studies [27, 56] Outcome, 2 studies [22, 79] |
| Anxiety (+) | Univariate, 3 studies [16, 22, 27] Multivariate, 2 studies [27, 77] | Univariate correlation level, 2 studies [22, 27] Multivariate correlation level, 1 study [27] | ||
Studies that did (yes) or did not (no) find a significant positive (+) or negative (–) cross-sectional association with fatigue levels or longitudinal association with longer-term fatigue levels or change in fatigue levels.
If an article reported more than one association (e.g. with more than one fatigue measure), then the median of the associations was taken.
Cross-sectional association studies include univariate correlations or analyses of variance and multivariate regression analyses, analyses of variance or structural equation modelling in which associations are controlled for other variables.
Longitudinal association studies include regression (correlational) analyses without a manipulation, experimental (laboratory) studies, clinical experimental studies and EMA studies.
Physical functioning
Three mutually dependent classes of physical functioning were reviewed: physical (dis)ability, physical capacity and physical activity, including physical activity interventions.
Physical (dis)ability
Associations of fatigue with the 36-item Short Form Health Survey (SF-36) scales physical function and physical role functioning and with disability were reviewed; disability was mostly measured with the HAQ.
Cross-sectionally, univariate associations between low physical functioning and fatigue levels were significant in all [8–11] but two [12, 13] studies; the median correlation was 0.49 (range 0.30–0.59). The multivariate association was significant in two studies [10, 11] and not significant in one study [13].
Cross-sectionally, univariate associations between low physical role functioning of the SF-36 and fatigue levels were significant in all [8–12, 14] but one [13] study; the median correlation was 0.51 (range 0.29–0.56). The multivariate association was significant in two studies [10, 11] and not significant in one study [13].
Cross-sectionally, univariate associations between disability and fatigue levels were significant in all 20 studies, of which 13 reported correlations, with a median of 0.48 (range 0.38–0.61) [10, 12, 14–31]. In nine multivariate analyses, the relationship between disability and fatigue remained significant [17, 24, 26–28, 32–35], in three analyses it was no longer significant [10, 18, 29] and in one analysis, one of two multivariate associations was significant [25]. Longitudinally, disability was univariately and multivariately associated with fatigue over time [27], fatigue was associated with disability over time [36], change in physical disability and change in fatigue were correlated [37] and the improvement of fatigue after anti-TNF treatment was larger for patients with low disability [38].
Overall, univariate cross-sectional associations between poor physical ability and fatigue were moderate to high and remained mostly significant in multivariate analysis. Also, less frequently examined longitudinal associations were significant.
Physical capacity
In cross-sectional studies, univariate associations between poorer physical capacity and fatigue were significant for the 6-min walking test [39], not significant for aerobic capacity (VO2max) [18, 40, 41] and lower limb function [18] and not significant for grip strength [18]. Multivariate analyses did not show significant correlations [18, 39]. Neither univariate nor multivariate associations for the 6-min walking test fatigue 3 months later were significant [39].
Physical activity
In cross-sectional univariate analyses, self-reported higher physical activity was shown to be associated with lower fatigue in all [10, 25, 30, 42, 43] but two [18, 40] of seven studies and physical activity measured with actometers was associated with lower fatigue [44]. In multivariate analysis, physical activity was independently associated with lower fatigue in two studies [32, 44] but not in three studies [10, 18, 25]. Longitudinally, no significant long-term associations between physical activity and fatigue were observed [39]. Four meta-analyses summarizing the effects of physical activity interventions on fatigue uniformly observed a small median (standardized mean difference) effect size of −0.35 [45–48].
Psychological functioning
Three classes of psychological functioning were reviewed: mental well-being, stress and stressors and psychological management and relational factors.
Mental well-being
Correlations of fatigue with three mental health scales from the SF-36 were reviewed: mental health, emotional role functioning and social functioning.
Cross-sectionally, univariate associations between low mental health (SF-36) and fatigue were significant in four studies, with a median correlation of 0.46 (range 0.38–0.76) [9, 10, 24, 31] and not significant in three studies [8, 12, 13]. The multivariate association was not significant in one study [13]. In one longitudinal study, improvement of fatigue was associated with good but not with poor mental health at baseline [38]. In another study, changes in mental health and fatigue were correlated [37].
Cross-sectionally, univariate associations between low emotional role functioning (SF-36) and fatigue levels were significant in four studies, with a median correlation of 0.42 (range 0.35–0.85) [8, 9, 14, 24] and not significant in one univariate and multivariate analysis [13].
Cross-sectionally, univariate associations between low social functioning (SF-36) and fatigue levels were significant in four studies, with a median correlation of 0.62 (range 0.50–0.78) [9, 10, 14, 24] and not significant in one univariate and multivariate analysis [13].
Overall, moderate to high univariate cross-sectional associations were, not uniformly, found between poor mental well-being and fatigue, while multivariate and longitudinal associations were too seldom assessed to draw firm conclusions.
Stress and stressors
Three cross-sectional studies reported a univariate significant association between chronic stress and fatigue levels; correlations were 0.32 [49], 0.39 [27] and 0.43 [50]. The multivariate association was significant for one [27] but not another study [50]. In a longitudinal correlation study, stress levels were correlated with longer-term fatigue levels in univariate but not in multivariate analyses; stress levels did not predict a change in fatigue [27]. Three EMA studies observed a relation between negative live events and same-day or next-day fatigue [51–53]; another study did not observe this correlation [54]. Overall, moderate univariate cross-sectional associations were, uniformly, found between chronic stress and fatigue, while multivariate, longitudinal and momentary associations were too low or too seldom assessed to draw firm conclusions.
Psychological management and relational factors
In eight cross-sectional studies, univariate associations between low self-reported self-efficacy (a belief in the ability to achieve a desired outcome) and fatigue were significant, with a median correlation of 0.46 (range 0.30–0.57) [10, 11, 21, 29, 50, 55–57]. The multivariate association was significant for two [21, 29] and not significant for two other studies [50, 55]. Low self-efficacy did not significantly predict the change of fatigue 1 year later (P = 0.05).
Studies examined divergent styles of coping, i.e. cognitive-behavioural efforts to deal with problems. Observations in univariate studies were that coping was related to fatigue [58], most coping styles were related to fatigue [10], coping was related to some but not all measures of fatigue [59] and coping was not associated with fatigue [50, 56], including in a multivariate analysis [50]. In one multivariate analysis, one coping style remained related to fatigue but the other did not [58]. Coping did not predict fatigue level or change 1 year later [56].
Correlations between low perceived social support and fatigue were 0.18 and 0.47 [10], 0.24 [27], 0.28 [29], 0.80 [55] and 0.14 [50]; four of the six correlations were significant and in four of these studies the multivariate correlation with fatigue was significant [27, 29, 50, 55]. Social support did not predict the level or change in fatigue 1 year later [27].
Several other psychological and relational factors were shown to correlate with less fatigue: low neuroticism [57], low helplessness [60], role satisfaction and greater perceived help at home [27], perceiving less severe consequences of the illness [56], optimism [27, 55], hope [55], higher self-esteem, lower somatic and higher non-somatic causal attributions, fewer catastrophizing cognitions [10], resilience [55] and daily positive events [51], e.g. positive interpersonal events [53].
Summarizing, of the psychological management and relational variables, higher self-efficacy showed a consistent cross-sectional, univariate correlation with lower fatigue, while social support was consistently correlated with lower fatigue levels in multivariate analysis.
Medical status
Medical status was not part of our systematic review, but it is obvious that it is a core aspect of any network model of fatigue.
Disease activity was positively correlated with fatigue, predominantly through self-reported variables such as pain instead of inflammation parameters. Other factors such as physical disability, sleep disturbance, depressive mood and psychological vulnerability were more strongly related to fatigue than inflammatory parameters [5, 15, 61].
Because inflammation and pro-inflammatory cytokines may induce fatigue [82], it makes sense to expect that medications reduce fatigue. Meta-analyses including 32 [83] and 10 [84] randomized trials convincingly showed that biological therapies reduce fatigue with a mean small effect size of 0.40–0.50. In multivariate analysis, fatigue levels in patients treated with anti-TNF-α vs DMARD therapy were not indicated to differ [34].
Comorbidities and symptoms
The occurrence and magnitude of associations of fatigue with pain, sleep disturbance, obesity, depression and anxiety were reviewed.
Pain
Our review included self-reports of pain with questionnaires, visual analogue scales or numerical scales and excluded clinical assessments such as tender joint counts and algometer measurements.
Cross-sectional univariate associations between higher pain and higher fatigue levels were significant, with a median correlation of 0.51 (range 0.22–0.75) in all studies [10, 12, 13, 15, 17–20, 24, 31, 39, 40, 50, 60–69], but there was one in which only one of two correlations was significant [8]. The multivariate association was significant after controlling for variables such as demographics, disease activity, depression, sleep and physical functioning in all studies [10, 17, 18, 32, 39, 50, 61, 63, 66, 70], but there was one that included another pain measure as a covariate [27]. In a 48 h EMA study, pain at night was correlated with daytime fatigue (r = 0.64) [62].
In one longitudinal correlation study, pain was correlated with longer-term fatigue levels [66]. In other studies, pain was not correlated with prospective levels of [39] or change in [56] fatigue. In multivariate analyses, pain was correlated with prospective fatigue levels in one study [66] but not in another study [39]. In an EMA study, pain remained level across the day while fatigue levels rose [54]. Longitudinal regression analysis showed a significant positive relationship between fatigue and pain levels during the same month [71], but neither changes in pain and next month changes in fatigue nor changes in fatigue and next month changes in pain were correlated [71]. In four studies, changes in pain and fatigue across time were correlated [37, 70, 72, 73].
Overall, the correlation between pain and fatigue levels is consistently observed and on average high and prospective changes in fatigue and changes in pain are correlated as well. The longitudinal bi-directional association between fatigue and pain is unclear.
Sleep disturbance
In the reviewed studies, sleep disturbance was measured with self-report questionnaires. Cross-sectionally, all univariate associations between sleep disturbance and fatigue were significant but one [64], with a median correlation of 0.45 (range 0.21–0.66) [8, 10, 25, 27, 30–32, 49, 56, 67, 74–76]. With the exception of one study [77], the multivariate association remained significant after controlling for variables such as demographics, disease activity, pain and physical functioning [10, 25, 32, 49, 75, 76, 78]. In a 48 h EMA study, low sleep quality was correlated with daytime fatigue (r = 0.48) [62].
In a longitudinal correlation study, sleep disturbance at baseline was associated with fatigue levels at the 1 year follow-up but not with change in fatigue while controlling for other baseline measurements [56]. After treatment with biologics, fatigue and sleep were not associated [79], and persisting fatigue was not associated with sleep disturbance [64]. In an experimental study, partial night sleep deprivation induced a non-significant increase in fatigue (P = 0.09) [80]. In an EMA study, mental fatigue but not somatic fatigue was associated with sleep disturbance, worse sleep predicted greater mental fatigue and somatic fatigue the subsequent afternoon [78] and average sleep quality and sleep quality assessed on a daily basis were associated with fatigue [54].
Overall, cross-sectional univariate and multivariate correlations between sleep disturbance and fatigue levels are consistently observed. The evidence for longitudinal correlations is less clear.
Obesity
Cross-sectional, univariate associations were observed between general fatigue and obesity in one study [25] but not in two other studies [18, 39]. In multivariate analysis, the associations remained significant in one study [25], while it was significant for one of two general fatigue measures in another study [39]. In a longitudinal study, obesity was not correlated with general fatigue 3 months later [39]. Overall, the relation between obesity and fatigue is not clear because there are only a few studies, with inconsistent findings.
Depression and anxiety
Cross-sectionally, univariate associations between depression and fatigue levels were uniformly significant, with a median correlation of 0.53 (range 0.29–0.77) [8, 16, 19, 22, 25, 27, 39, 40, 50, 56, 58, 64, 68, 75, 81]. The multivariate association remained significant after controlling for variables such as demographics, disease activity, pain and physical functioning in all studies [19, 25, 39, 40, 50, 75, 77] but one [27]. In three longitudinal correlation studies, depression was correlated with longer-term fatigue levels [22, 27, 39] and in one study depression was related with one of two measures of fatigue [58]. In multivariate analyses, depression was correlated with prospective fatigue levels in one study [58] but not in two other studies [27, 56]. Fatigue outcome was not associated with depression in two studies [22, 79] but it was associated with a history of depression in two other studies [37, 38].
Anxiety
Three cross-sectional studies reported a univariate significant association between anxiety and fatigue levels; correlations were 0.24 [22], 0.54 [16] and 0.55 [27]. The multivariate association between anxiety and fatigue after controlling for variables was significant in the two studies [27, 77]. In two longitudinal correlation studies, anxiety was correlated with longer-term fatigue levels [22, 27]. The multivariate association between anxiety and prospective fatigue levels was significant in one study [27]. Positive correlations were also found in the two studies that examined the association between fatigue and combined depression and anxiety levels [18, 30].
Overall, an on average high univariate correlation of fatigue levels with concurrent depression and anxiety was consistently observed and these associations remained significant in multivariate analysis with only incidental exceptions. Longitudinal correlations between depression, anxiety and fatigue levels are mostly consistently observed as well; multivariate associations are less clear.
Biographic, demographic and social variables
The results of this review are described in Supplementary Table S4, available at Rheumatology online. Correlations between age and fatigue were inconsistent, but there was some indication that a younger age is associated with greater fatigue levels after correction for other variables such as physical functioning. Higher fatigue was consistently associated with reduced work ability. Studies did not observe a consistent association of persistent fatigue levels with female gender, disease duration, marital status or education level. In single studies, several relational and socio-economic variables were observed to be related to worse fatigue in RA.
Miscellaneous
Some miscellaneous findings merit attention. A statistically significant seasonal variation in fatigue levels was observed, with higher fatigue values during the winter [85]. This variable remained significantly associated with one measure but not another measure of fatigue in multivariate analysis. Regarding complementary treatments, significant effects on fatigue of aromatherapy massage, reflexology [86] and whole body vibration [87] were observed. However, replication is needed.
Discussion
This literature review offered a comprehensive overview of six categories of variables that were associated with fatigue in patients with RA: physical functioning, psychological functioning, medical status, comorbidities and symptoms, biographical variables and miscellaneous variables. Correlations of fatigue with physical functioning, poor mental well-being, pain, sleep disturbance, and depression and anxiety were generally ∼0.50. These correlations mostly stayed significant in multivariate analyses. Often significant but not as high and often not surviving multivariate analyses were associations of fatigue with physical activity, physical capacity, stress and stressors, psychological management and relational factors, obesity and female gender, while the association between fatigue and younger age tended to be significant in multivariate but not univariate analyses. Longitudinal analyses showed more consistently significant associations of fatigue with other variables when absolute levels were correlated in univariate analyses than when fatigue change was predicted or multivariate analyses were conducted.
Fatigue, pain, depression, sleep disturbance, low physical activity and several other correlated variables appear mutually influencing factors that should all be considered when treating fatigue. This appears feasible in clinical practice, because there is overlap in the indicated non-pharmacological treatment of these factors and treatment of one factor may lead to improvement of other factors [6, 88–90].
Results of multivariate analyses depend on the number and kind of covariates included, which is consistent with a network model. That a univariate association becomes less strong when more variables are added in multivariate analysis is a finding that is consistent with a multifaceted model with mutually influencing variables. That associations of physical disability, poor mental well-being, pain, sleep disturbance and depression and anxiety often stayed significant in multivariate analyses suggests the partly independent association of these variables with fatigue and that networks of influencing variables differ between individuals.
Variables that were not measured with self-reports generally correlated less with fatigue than self-report measures, e.g. disease activity, obesity and demographics. This is likely partly due to the different modes of measurement [91], but it also reflects the reality that fatigue is a phenomenological experience. That correlations with some factors in the model are less clear than for others may tell us something about the mode of measurement and about common associations in a group, but it does not refute the importance of these variables for individual patients. Active disease and morbid obesity must always be treated, and these interventions might also reduce fatigue [83, 84, 92], although additional behavioural and lifestyle treatment may be needed to further reduce fatigue.
Patients may attribute fatigue to inflammation, working the joints harder and unrefreshing sleep, while they consider effects on physical activities, emotions, relationships and family as consequences of fatigue [3]. This might be true, but very likely the real influences are more mutual. To really get insight into causal network models that influence fatigue in an individual patient, future research should longitudinally monitor multiple variables and analyse them using dynamic structural equation modelling [93]. A full network model should include the influence of slow changing between-person factors such as obesity, as well as transient within-person factors such as emotions or sleep quality.
Limitations of this review were the exclusion of disease activity and interventions that have an in-depth coverage in other articles in this issue. Moreover, the search was focused on the specified variables (‘rheumatoid’ and ‘fatigue’) in the title. Therefore we may have missed studies that did not use the word ‘fatigue’ in the title or studies that used the term ‘vitality’ or ‘energy’ instead of ‘fatigue’ in the title. Moreover, we did not conduct a meta-analysis that accounted for sample size and study quality, such as risk of bias assessment. Nevertheless, many variables were so frequently studied that the medians likely give a good indication of associations between variables. Overall, the between-person analyses show which variables are potential perpetuating factors of fatigue for individual patients. In clinical practice, individual assessment is needed to uncover the variables that are most important for an individual. The observed associations between fatigue and a cluster of variables clearly shows that in the treatment of fatigue the following variables should always be considered as potential maintaining factors: psychological and physical functioning, pain, sleep disturbance and depression and anxiety.
Funding: This supplement is supported by a grant from Gilead Sciences, Inc.
Disclosure statement: The authors have declared no conflicts of interest.
Supplementary Material
References
- 1. Repping-Wuts H, van Riel P, van Achterberg T.. Fatigue in patients with rheumatoid arthritis: what is known and what is needed. Rheumatology (Oxford) 2008;48:207–9. [DOI] [PubMed] [Google Scholar]
- 2. Overman CL, Kool MB, Da Silva JA, Geenen R.. The prevalence of severe fatigue in rheumatic diseases: an international study. Clin Rheumatol 2016;35:409–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hewlett S, Cockshott Z, Byron M. et al. Patients’ perceptions of fatigue in rheumatoid arthritis: overwhelming, uncontrollable, ignored. Arthritis Rheum 2005;53:697–702. [DOI] [PubMed] [Google Scholar]
- 4. Hewlett S, Chalder T, Choy E. et al. Fatigue in rheumatoid arthritis: time for a conceptual model. Rheumatology (Oxford) 2011;50:1004. [DOI] [PubMed] [Google Scholar]
- 5. Katz P. Fatigue in rheumatoid arthritis. Curr Rheumatol Rep 2017;19:25. [DOI] [PubMed] [Google Scholar]
- 6. Geenen R, Overman CL, Christensen R. et al. EULAR recommendations for the health professional’s approach to pain management in inflammatory arthritis and osteoarthritis. Ann Rheum Dis 2018;77:797–807. [DOI] [PubMed] [Google Scholar]
- 7. Ghogomu EA, Maxwell LJ, Buchbinder R. et al. Updated method guidelines for Cochrane Musculoskeletal Group systematic reviews and metaanalyses. J Rheumatol 2014;41:194–205. [DOI] [PubMed] [Google Scholar]
- 8. Albayrak Gezer İ, Balkarli A, Can B. et al. Pain, depression levels, fatigue, sleep quality, and quality of life in elderly patients with rheumatoid arthritis. Turk J Med Sci 2017;47:847–53. [DOI] [PubMed] [Google Scholar]
- 9. Rupp I, Boshuizen HC, Jacobi CE, Dinant HJ, Van den Bos GA.. Impact of fatigue on health-related quality of life in rheumatoid arthritis. Arthritis Care Res 2004;51:578–85. [DOI] [PubMed] [Google Scholar]
- 10. Van Hoogmoed D, Fransen J, Bleijenberg G, van Riel P.. Physical and psychosocial correlates of severe fatigue in rheumatoid arthritis. Rheumatology (Oxford) 2010;49:1294–302. [DOI] [PubMed] [Google Scholar]
- 11. Rongen-van Dartel SA, Repping-Wuts H, Donders R. et al. A multidimensional ‘path analysis’ model of factors explaining fatigue in rheumatoid arthritis. Clin Exp Rheumatol 2016;34:200–6. [PubMed] [Google Scholar]
- 12. Turan Y, Kocaaga Z, Kocyigit H. et al. Correlation of fatigue with clinical parameters and quality of life in rheumatoid arthritis. Turk J Rheumatol 2010;25:63–7. [Google Scholar]
- 13. Öncü J, Başoğlu F, Kuran B.. A comparison of impact of fatigue on cognitive, physical, and psychosocial status in patients with fibromyalgia and rheumatoid arthritis. Rheumatol Int 2013;33:3031–7. [DOI] [PubMed] [Google Scholar]
- 14. Cross M, Lapsley H, Barcenilla A, Brooks P, March L.. Association between measures of fatigue and health-related quality of life in rheumatoid arthritis and osteoarthritis. Patient 2008;1:97–104. [DOI] [PubMed] [Google Scholar]
- 15. Bergman MJ, Shahouri SH, Shahouri SS. et al. Is fatigue an inflammatory variable in rheumatoid arthritis (RA)? Analyses of fatigue in RA, osteoarthritis, and fibromyalgia. J Rheumatol 2009;36:2788–94. [DOI] [PubMed] [Google Scholar]
- 16. Bianchi WA, Elias FR, Pinheiro GdRC. et al. Analysis of the association of fatigue with clinical and psychological variables in a series of 371 Brazilian patients with rheumatoid arthritis. Rev Bras Reumatol 2014;54:200–7. [PubMed] [Google Scholar]
- 17. Campbell RCJ, Batley M, Hammond A. et al. The impact of disease activity, pain, disability and treatments on fatigue in established rheumatoid arthritis. Clin Rheumatol 2012;31:717–22. [DOI] [PubMed] [Google Scholar]
- 18. Demmelmaier I, Pettersson S, Nordgren B, Dufour AB, Opava CH.. Associations between fatigue and physical capacity in people moderately affected by rheumatoid arthritis. Rheumatol Int 2018;38:2147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Franklin AL, Harrell TH.. Impact of fatigue on psychological outcomes in adults living with rheumatoid arthritis. Nurs Res 2013;62:203–9. [DOI] [PubMed] [Google Scholar]
- 20. Garip Y, Eser F, Aktekin LA, Bodur H.. Fatigue in rheumatoid arthritis: association with severity of pain, disease activity and functional status. Acta Reumatol Port 2011;36:364–9. [PubMed] [Google Scholar]
- 21. Gong G, Mao J.. Health-related quality of life among Chinese patients with rheumatoid arthritis: the predictive roles of fatigue, functional disability, self-efficacy, and social support. Nurs Res 2016;65:55–67. [DOI] [PubMed] [Google Scholar]
- 22. Gossec L, Steinberg G, Rouanet S, Combe B.. Fatigue in rheumatoid arthritis: quantitative findings on the efficacy of tocilizumab and on factors associated with fatigue. The French multicentre prospective PEPS study. Clin Exp Rheumatol 2015;33:664–70. [PubMed] [Google Scholar]
- 23. Gök K, Erol K, Cengiz G, Özgöçmen S.. Comparison of level of fatigue and disease correlates in patients with rheumatoid arthritis and systemic sclerosis. Arch Rheumatol 2018;33:316–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ibn Yacoub Y, Amine B, Laatiris A. et al. Fatigue and severity of rheumatoid arthritis in Moroccan patients. Rheumatol Int 2012;32:1901–7. [DOI] [PubMed] [Google Scholar]
- 25. Katz P, Margaretten M, Trupin L. et al. Role of sleep disturbance, depression, obesity, and physical inactivity in fatigue in rheumatoid arthritis. Arthritis Care Res (Hoboken) 2016;68:81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Grøn KL, Ørnbjerg LM, Hetland ML. et al. The association of fatigue, comorbidity burden, disease activity, disability and gross domestic product in patients with rheumatoid arthritis. Results from 34 countries participating in the quest-RA programme. Clin Exp Rheumatol 2014;32:869–77. [PubMed] [Google Scholar]
- 27. Mancuso CA, Rincon M, Sayles W, Paget SA.. Psychosocial variables and fatigue: a longitudinal study comparing individuals with rheumatoid arthritis and healthy controls. J Rheumatol 2006;33:1496–502. [PubMed] [Google Scholar]
- 28. Repping-Wuts H, Fransen J, van Achterberg T, Bleijenberg G, van Riel P.. Persistent severe fatigue in patients with rheumatoid arthritis. J Clin Nurs 2007;16:377–83. [DOI] [PubMed] [Google Scholar]
- 29. Riemsma RP, Rasker JJ, Taal E. et al. Fatigue in rheumatoid arthritis: the role of self-efficacy and problematic social support. Br J Rheumatol 1998;37:1042–6. [DOI] [PubMed] [Google Scholar]
- 30. Tournadre A, Pereira B, Gossec L, Soubrier M, Dougados M.. Impact of comorbidities on fatigue in rheumatoid arthritis patients: results from a nurse-led program for comorbidities management (COMEDRA). Joint Bone Spine 2019;86:55–60. [DOI] [PubMed] [Google Scholar]
- 31. Thyberg I, Dahlström Ö, Thyberg M.. Factors related to fatigue in women and men with early rheumatoid arthritis: the Swedish TIRA study. J Rehabil Med 2009;41:904–12. [DOI] [PubMed] [Google Scholar]
- 32. Belza BL, Henke CJ, Yelin EH, Epstein WV, Gilliss CL.. Correlates of fatigue in older adults with rheumatoid arthritis. Nurs Res 1993;42:93–9. [PubMed] [Google Scholar]
- 33. Diniz LR, Balsamo S, de Souza TY. et al. Measuring fatigue with multiple instruments in a Brazilian cohort of early rheumatoid arthritis patients. Rev Bras Reumatol 2017;57:431–7. [DOI] [PubMed] [Google Scholar]
- 34. van Hoogmoed D, Fransen J, Repping-Wuts H. et al. The effect of anti-TNF-α vs. DMARDs on fatigue in rheumatoid arthritis patients. Scand J Rheumatol 2013;42:15–9. [DOI] [PubMed] [Google Scholar]
- 35. Wolfe F. Fatigue assessments in rheumatoid arthritis: comparative performance of visual analog scales and longer fatigue questionnaires in 7760 patients. J Rheumatol 2004;31:1896–902. [PubMed] [Google Scholar]
- 36. Twigg S, Hensor EMA, Freeston J. et al. Effect of fatigue, older age, higher body mass index, and female sex on disability in early rheumatoid arthritis in the treatment-to-target era. Arthritis Care Res 2018;70:361–8. [DOI] [PubMed] [Google Scholar]
- 37. Druce KL, Jones GT, Macfarlane GJ, Basu N.. Determining pathways to improvements in fatigue in rheumatoid arthritis: results from the British society for rheumatology biologics register for rheumatoid arthritis. Arthritis Rheumatol 2015;67:2303–10. [DOI] [PubMed] [Google Scholar]
- 38. Druce KL, Jones GT, Macfarlane GJ, Basu N.. Patients receiving anti-TNF therapies experience clinically important improvements in RA-related fatigue: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatology 2015;54:964–71. [DOI] [PubMed] [Google Scholar]
- 39. Feldthusen C, Grimby-Ekman A, Forsblad-d’Elia H, Jacobsson L, Mannerkorpi K.. Explanatory factors and predictors of fatigue in persons with rheumatoid arthritis: a longitudinal study. J Rehabil Med 2016;48:469–76. [DOI] [PubMed] [Google Scholar]
- 40. Munsterman T, Takken T, Wittink H.. Low aerobic capacity and physical activity not associated with fatigue in patients with rheumatoid arthritis: a cross-sectional study. J Rehabil Med 2013;45:164–9. [DOI] [PubMed] [Google Scholar]
- 41. Weinstein AA, Drinkard BM, Diao G. et al. Exploratory analysis of the relationships between aerobic capacity and self-reported fatigue in patients with rheumatoid arthritis, polymyositis, and chronic fatigue syndrome. PM R 2009;1:620–8. [DOI] [PubMed] [Google Scholar]
- 42. Lee EO, Kim J, Davis AHT, Kim I.. Effects of regular exercise on pain, fatigue, and disability in patients with rheumatoid arthritis. Fam Commun Health 2006;29:320–7. [DOI] [PubMed] [Google Scholar]
- 43. Løppenthin K, Esbensen BA, Østergaard M. et al. Physical activity and the association with fatigue and sleep in Danish patients with rheumatoid arthritis. Rheumatol Int 2015;35:1655–64. [DOI] [PubMed] [Google Scholar]
- 44. Rongen-van Dartel SA, Repping-Wuts H, van Hoogmoed D. et al. Relationship between objectively assessed physical activity and fatigue in patients with rheumatoid arthritis: inverse correlation of activity and fatigue. Arthritis Care Res 2014;66:852–60. [DOI] [PubMed] [Google Scholar]
- 45. Cramp F, Hewlett S, Almeida C. et al. Non-pharmacological interventions for fatigue in rheumatoid arthritis. Cochrane Database Syst Rev 2013;8:CD008322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kelley GA, Kelley KS, Callahan LF.. Aerobic exercise and fatigue in rheumatoid arthritis participants: a meta-analysis using the minimal important difference approach. Arthritis Care Res 2018;70:1735–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Salmon VE, Hewlett S, Walsh NE, Kirwan JR, Cramp F.. Physical activity interventions for fatigue in rheumatoid arthritis: a systematic review. Phys Ther Rev 2017;22:12–22. [Google Scholar]
- 48. Rongen-van Dartel SA, Repping-Wuts H, Flendrie M. et al. Effect of aerobic exercise training on fatigue in rheumatoid arthritis: a meta-analysis. Arthritis Care Res 2015;67:1054–62. [DOI] [PubMed] [Google Scholar]
- 49. Nicassio PM, Ormseth SR, Custodio MK. et al. A multidimensional model of fatigue in patients with rheumatoid arthritis. J Rheumatol 2012;39:1807–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Huyser BA, Parker JC, Thoreson R. et al. Predictors of subjective fatigue among individuals with rheumatoid arthritis. Arthritis Rheum 1998;41:2230–7. [DOI] [PubMed] [Google Scholar]
- 51. Davis MC, Okun MA, Kruszewski D, Zautra AJ, Tennen H.. Sex differences in the relations of positive and negative daily events and fatigue in adults with rheumatoid arthritis. J Pain 2010;11:1338–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Parrish BP, Zautra AJ, Davis MC.. The role of positive and negative interpersonal events on daily fatigue in women with fibromyalgia, rheumatoid arthritis, and osteoarthritis. Health Psychol 2008;27:694–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Finan PH, Okun MA, Kruszewski D. et al. Interplay of concurrent positive and negative interpersonal events in the prediction of daily negative affect and fatigue for rheumatoid arthritis patients. Health Psychol 2010;29:429–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Stone AA, Broderick JE, Porter LS, Kaell AT.. The experience of rheumatoid arthritis pain and fatigue: examining momentary reports and correlates over one week. Arthritis Care Res 1997;10:185–93. [DOI] [PubMed] [Google Scholar]
- 55. Xu NL, Zhao S, Xue HX. et al. Associations of perceived social support and positive psychological resources with fatigue symptom in patients with rheumatoid arthritis. PLoS One 2017;12:e0173293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Treharne GJ, Lyons AC, Hale ED. et al. Predictors of fatigue over 1 year among people with rheumatoid arthritis. Psychol Health Med 2008;13:494–504. [DOI] [PubMed] [Google Scholar]
- 57. Jump RL, Fifield J, Tennen H, Reisine S, Giuliano AJ.. History of affective disorder and the experience of fatigue in rheumatoid arthritis. Arthritis Rheum 2004;51:239–45. [DOI] [PubMed] [Google Scholar]
- 58. Walter MJM, Kuijper TM, Hazes JMW, Weel AE, Luime JJ.. Fatigue in early, intensively treated and tight-controlled rheumatoid arthritis patients is frequent and persistent: a prospective study. Rheumatol Int 2018;38:1643–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Koike T, Kazuma K, Kawamura S.. The relationship between fatigue, coping behavior, and inflammation in patients with rheumatoid arthritis. Mod Rheumatol 2000;10:141–9. [DOI] [PubMed] [Google Scholar]
- 60. Nicklin J, Cramp F, Kirwan J. et al. Measuring fatigue in rheumatoid arthritis: a cross-sectional study to evaluate the Bristol rheumatoid arthritis fatigue multi-dimensional questionnaire, visual analog scales, and numerical rating scales. Arthritis Care Res (Hoboken) 2010;62:1559–68. [DOI] [PubMed] [Google Scholar]
- 61. Groth Madsen S, Danneskiold-Samsøe B, Stockmarr A, Bartels EM.. Correlations between fatigue and disease duration, disease activity, and pain in patients with rheumatoid arthritis: a systematic review. Scand J Rheumatol 2016;45:255–61. [DOI] [PubMed] [Google Scholar]
- 62. Dekkers JC, Geenen R, Godaert GLR, Doornen LJP, Bijlsma JWJ.. Diurnal courses of cortisol, pain, fatigue, negative mood, and stiffness in patients with recently diagnosed rheumatoid arthritis. Int J Behav Med 2000;7:353–71. [Google Scholar]
- 63. Egsmose EL, Madsen OR.. Interplay between patient global assessment, pain, and fatigue and influence of other clinical disease activity measures in patients with active rheumatoid arthritis. Clin Rheumatol 2015;34:1187–94. [DOI] [PubMed] [Google Scholar]
- 64. Minnock P, Veale DJ, Bresnihan B, FitzGerald O, McKee G.. Factors that influence fatigue status in patients with severe rheumatoid arthritis (RA) and good disease outcome following 6 months of TNF inhibitor therapy: a comparative analysis. Clin Rheumatol 2015;34:1857–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Novaes GS, Perez MO, Beraldo MBB, Pinto CRC, Gianini RJ.. Correlation of fatigue with pain and disability in rheumatoid arthritis and osteoarthritis, respectively. Rev Bras Reumatol 2011;51:447–55. [PubMed] [Google Scholar]
- 66. Olsen CL, Lie E, Kvien TK, Zangi HA.. Predictors of fatigue in rheumatoid arthritis patients in remission or in a low disease activity state. Arthritis Care Res (Hoboken) 2016;68:1043–8. [DOI] [PubMed] [Google Scholar]
- 67. Szady P, Baczyk G, Kozłowska K.. Fatigue and sleep quality in rheumatoid arthritis patients during hospital admission. Reumatologia 2017;55:65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Tack BB. Self-reported fatigue in rheumatoid arthritis. A pilot study. Arthritis Care Res 1990;3:154–7. [PubMed] [Google Scholar]
- 69. Younger J, Finan P, Zautra A, Davis M, Reich J.. Personal mastery predicts pain, stress, fatigue, and blood pressure in adults with rheumatoid arthritis. Psychol Health 2008;23:515–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Pollard LC, Choy EH, Gonzalez J, Khoshaba B, Scott DL.. Fatigue in rheumatoid arthritis reflects pain, not disease activity. Rheumatology (Oxford) 2006;45:885–9. [DOI] [PubMed] [Google Scholar]
- 71. Van Dartel SA, Repping-Wuts J, van Hoogmoed D. et al. Association between fatigue and pain in rheumatoid arthritis: does pain precede fatigue or does fatigue precede pain? Arthritis Care Res (Hoboken) 2013;65:862–9. [DOI] [PubMed] [Google Scholar]
- 72. Gossec L, Ahdjoudj S, Alemao E, Strand V.. Improvements in fatigue in 1536 patients with rheumatoid arthritis and correlation with other treatment outcomes: a post hoc analysis of three randomized controlled trials of abatacept. Rheumatol Ther 2017;4:99–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Madsen OR, Egsmose EM.. Fatigue, pain and patient global assessment responses to biological treatment are unpredictable, and poorly inter-connected in individual rheumatoid arthritis patients followed in the daily clinic. Rheumatol Int 2016;36:1347–54. [DOI] [PubMed] [Google Scholar]
- 74. Ulus Y, Akyol Y, Tander B. et al. Sleep quality in fibromyalgia and rheumatoid arthritis: associations with pain, fatigue, depression, and disease activity. Clin Exp Rheumatol 2011;29(6 Suppl 69):92–6. [PubMed] [Google Scholar]
- 75. Hammam N, Gamal RM, Rashed AM. et al. Fatigue in rheumatoid arthritis patients: association with sleep quality, mood status, and disease activity. Reumatol Clin 2018. 10.1016/j.reuma.2018.07.010 (date last assessed, 11 September 2019). [DOI] [PubMed] [Google Scholar]
- 76. Austad C, Kvien TK, Olsen IC, Uhlig T.. Sleep disturbance in patients with rheumatoid arthritis is related to fatigue, disease activity, and other patient-reported outcomes. Scand J Rheumatol 2017;46:95–103. [DOI] [PubMed] [Google Scholar]
- 77. Stebbings S, Herbison P, Doyle TCH, Treharne GJ, Highton J.. A comparison of fatigue correlates in rheumatoid arthritis and osteoarthritis: disparity in associations with disability, anxiety and sleep disturbance. Rheumatology 2010;49:361–7. [DOI] [PubMed] [Google Scholar]
- 78. Goodchild CE, Treharne GJ, Booth DA, Bowman SJ.. Daytime patterning of fatigue and its associations with the previous night’s discomfort and poor sleep among women with primary Sjögren’s syndrome or rheumatoid arthritis. Musculoskel Care 2010;8:107–17. [DOI] [PubMed] [Google Scholar]
- 79. Genty M, Combe B, Kostine M. et al. Improvement of fatigue in patients with rheumatoid arthritis treated with biologics: relationship with sleep disorders, depression and clinical efficacy. A prospective, multicentre study. Clin Exp Rheumatol 2017;35:85–92. [PubMed] [Google Scholar]
- 80. Irwin MR, Olmstead R, Carrillo C. et al. Sleep loss exacerbates fatigue, depression, and pain in rheumatoid arthritis. Sleep 2012;35:537–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Fifield J, Tennen H, Reisine S, McQuillan J.. Depression and the long-term risk of pain, fatigue, and disability in patients with rheumatoid arthritis. Arthritis Rheum 1998;41:1851–7. [DOI] [PubMed] [Google Scholar]
- 82. Dantzer R. Cytokine-induced sickness behavior: mechanisms and implications. Ann N Y Acad Sci 2001;933:222–34. [DOI] [PubMed] [Google Scholar]
- 83. Almeida C, Choy EH, Hewlett S. et al. Biologic interventions for fatigue in rheumatoid arthritis. Cochrane Database Syst Rev 2016;6:CD008334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Chauffier K, Salliot C, Berenbaum F, Sellam J.. Effect of biotherapies on fatigue in rheumatoid arthritis: a systematic review of the literature and meta-analysis. Rheumatology 2012;51:60–8. [DOI] [PubMed] [Google Scholar]
- 85. Feldthusen C, Grimby-Ekman A, Forsblad-d’Elia H, Jacobsson L, Mannerkorpi K.. Seasonal variations in fatigue in persons with rheumatoid arthritis: a longitudinal study. BMC Musculoskelet Disord 2016;17:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Gok Metin Z, Ozdemir L.. The effects of aromatherapy massage and reflexology on pain and fatigue in patients with rheumatoid arthritis: a randomized controlled trial. Pain Manag Nurs 2016;17:140–9. [DOI] [PubMed] [Google Scholar]
- 87. Prioreschi A, Makda MA, Tikly M, McVeigh JA.. In patients with established RA, positive effects of a randomised three month WBV therapy intervention on functional ability, bone mineral density and fatigue are sustained for up to six months. PLoS One 2016;11:e0153470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Gee B, Orchard F, Clarke E. et al. The effect of non-pharmacological sleep interventions on depression symptoms: a meta-analysis of randomised controlled trials. Sleep Med Rev 2019;43:118–28. [DOI] [PubMed] [Google Scholar]
- 89. Geenen R, Newman S, Bossema ER, Vriezekolk JE, Boelen PA.. Psychological interventions for patients with rheumatic diseases and anxiety or depression. Best Pract Res Clin Rheumatol 2012;26:305–19. [DOI] [PubMed] [Google Scholar]
- 90. Hewlett S, Almeida C, Ambler N. et al. Reducing arthritis fatigue impact: two-year randomised controlled trial of cognitive behavioural approaches by rheumatology teams (RAFT). Ann Rheum Dis 2019;78:465–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Ganellen RJ. Assessing normal and abnormality personality functioning: strengths and weaknesses of self-report, observer, and performance-based methods. J Pers Assess 2007;89:30–40. [DOI] [PubMed] [Google Scholar]
- 92. Larsen JK, Geenen R, van Ramshorst B. et al. Psychosocial functioning before and after laparoscopic adjustable gastric banding: a cross-sectional study. Obes Surg 2003;13:629–36. [DOI] [PubMed] [Google Scholar]
- 93. Asparouhov T, Hamaker EL, Muthén B.. Dynamic structural equation models. Struct Equ Modeling 2018;25:359–88. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.