Abstract
PURPOSE:
Obesity and related factors have been linked to cancer risk and outcomes, but little information exists with regard to oncologists’ attention to these issues as a part of clinical care.
METHODS:
Oncology providers actively caring for patients with cancer in the United States and internationally were asked to complete an online survey about practice patterns and perceptions with regard to obesity and weight management during and after active cancer treatment.
RESULTS:
Nine hundred seventy-one practicing oncology providers completed the survey. The majority of respondents indicated a belief that the evidence linking obesity to cancer outcomes was strong and that weight and related factors should be addressed as a part of cancer treatment. The majority of respondents also reported that they frequently assessed body weight and related factors as well as counsel their patients to exercise, consume a healthy diet, and lose weight, if applicable. However, referral to providers and programs to support weight loss and increased physical activity occurred less frequently, and a number of barriers were identified for the incorporation of weight management and physical activity programs in the treatment of patients with cancer.
CONCLUSION:
In a survey of oncology providers, attention to weight management, physical activity, and diet in patients with cancer was high during and after cancer treatment but often did not result in referrals to support lifestyle change. Future work is needed to support education and training of oncology providers to facilitate referrals and overcome barriers to implementation of weight management and physical activity programs for patients with cancer.
INTRODUCTION
Obesity, inactivity, and poor dietary quality are increasingly being linked to the risk of developing and dying as a result of malignancy.1-10 Hundreds of observational studies, summarized by the International Agency for Cancer Research11 and the World Cancer Research Fund,12 have evaluated the relationship between obesity and cancer risk. In their analyses of these data, both the International Agency for Cancer Research and the World Cancer Research Fund concluded that there is convincing and consistent evidence that obesity raises the risk of more than a dozen malignancies, including common cancers such as postmenopausal breast cancer and colon cancer. Although the data are more limited, physical inactivity and poor dietary quality also are associated with increased cancer risk.
Observational studies have demonstrated a relationship between obesity at the time of cancer diagnosis and an increased risk of cancer recurrence and cancer-related mortality in individuals with early-stage, potentially curable malignancies.3,5,10,13 In addition, obesity has been linked to an increased risk of second malignancies,14 surgical complications,15-17 adverse effects of cancer treatment,18,19 and long-term toxicities such as lymphedema20 in patients with cancer.
Although evidence that demonstrates that lifestyle interventions affect cancer outcomes, such as recurrence or mortality, is limited at this point, many trials have evaluated the impact of exercise and weight loss interventions on other outcomes in patients with cancer during and after active treatment. These trials provide consistent evidence that exercise interventions lead to improvements in cardiorespiratory fitness21 and physical functioning22 and reductions in fatigue.23
Of note, the prevalence of obesity and contributing factors like inactivity and poor dietary quality is high in cancer survivors.24-26 Estimates from the National Cancer Institute Cancer Trends Progress Report indicated that 31% of adult cancer survivors were obese in 2016.27 In addition, surveys of cancer survivors that evaluated dietary quality demonstrated that only 16% to 18% of survivors consume at least five servings of fruits and vegetables per day and that up to one third engage in no recreational physical activity.24,25
In recognition of the association between obesity and cancer risk and outcomes as well as the other adverse sequelae of obesity in patients with cancer, ASCO made obesity and cancer one of its core initiatives in 2014.28 A pillar of this initiative has been to increase oncologists’ core knowledge about nutrition, physical activity, and weight and to ensure that providers recognize obesity as a risk factor for cancer and as a complicating feature in the management of cancer. To help to define the future direction of this work, ASCO conducted a survey of its membership to assess current oncology provider knowledge with regard to the link between obesity (and related factors) and cancer risk and outcomes as well as to assess current practice behaviors with regard to exercise, nutrition, and weight management recommendations provided to oncology patients. Findings of this survey and suggested next steps are summarized in this report.
METHODS
Study Sample
An online questionnaire was developed to assess oncology provider practice patterns and perceptions with regard to obesity and weight management during and after active cancer treatment. The target audience was oncology providers who currently treat patients with cancer, including physicians, nurses, physician assistants, and other members of the clinical care team located both domestically in the United States and internationally. The online survey included questions about respondent characteristics (ie, terminal degree, geographic location, clinical setting, primary area of practice, disease site most frequently treated); attitudes about the strength of the evidence that links obesity and related factors and cancer; frequency of assessment of patients’ body mass index (BMI), physical activity, and diet; frequency of counseling patients to increase exercise, consume a healthy diet, and lose weight (if applicable); frequency of referral to weight management, physical activity, and nutrition programs/providers; and perceived barriers to providing interventions to patients with cancer. The questionnaire and administration plan were developed and reviewed by the Obesity and Energy Balance Subcommittee of the ASCO Cancer Prevention Committee.
The online survey was distributed between May 27, 2018, and July 31, 2018. Current ASCO members were targeted with a direct e-mail invitation to participate in the survey; the e-mail was sent to 14,652 members who were either full members, advanced practice providers, or affiliated health professionals. No incentive was offered to respondents to encourage completion of the survey. An initial question was included to eliminate those not currently seeing patients with cancer from completing the survey.
Data Analysis
Descriptive analyses are presented for responses to survey questions. Demographic characteristics of survey respondents were compared with demographic characteristics of ASCO members on the basis of membership data available as of August 1, 2018. Additional analyses that looked at the relationship of type of provider, practice type, and geographic location with survey responses were conducted to evaluate whether any of these characteristics were associated with knowledge or practice patterns relevant to obesity or related factors. Responses to questions were not mandatory; therefore, the number of responses for each question varied.
RESULTS
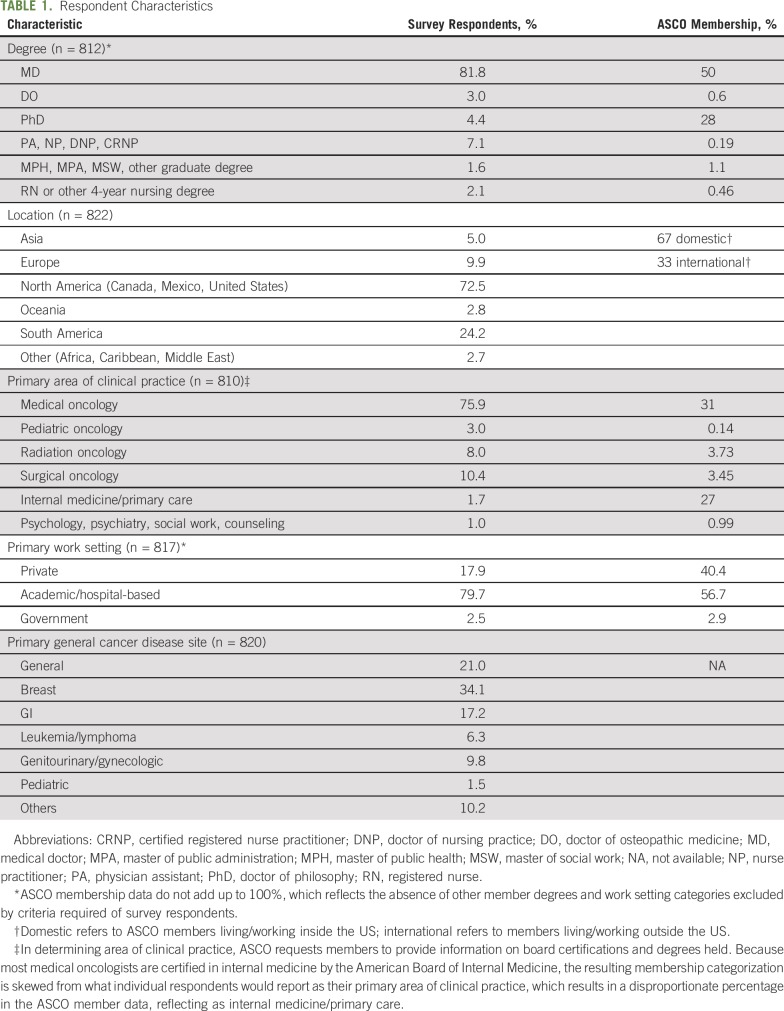
A total of 1,067 individuals responded to the survey between May 27, 2018, and July 31, 2018; 971 of these individuals were actively treating patients with cancer and were invited to complete the survey. Demographic characteristics of the survey respondents are listed in Table 1. Most respondents had a doctoral degree (82%), were located in the United States (69%), and were practicing in a hospital or health system (including academic medical centers and state-funded institutions; 80%). Medical oncology represented the primary specialty category (76%), followed by surgical oncology (10%). Breast cancer, a general mix of cancer types, and GI cancer were the most frequently treated disease sites, with 34%, 21%, and 17% of respondents reporting these, respectively. The other disease sites were seen by less than 28% of respondents. The survey population was generally similar to ASCO membership (Table 1), except that the requirement that survey respondents be practicing clinicians led to a lower percentage of doctors of philosophy in the survey population and a higher proportion of medical and surgical oncologists. Geographic representation and practice type were similar between the survey population and ASCO membership.
TABLE 1.
Respondent Characteristics
Respondents’ Perspectives on Obesity and Cancer
Respondents’ perspectives on the evidence linking obesity to cancer risk and outcomes and their views on the incorporation of weight management, physical activity, and dietary recommendations as a part of cancer treatment are listed in Table 2. The majority of respondents either strongly agreed or agreed that strong evidence shows that being overweight or obese affects cancer treatment outcomes (93%) and that addressing a patient’s weight if overweight or obese should be a standard part of cancer treatment (89%). The majority of respondents believed that the treating physician is responsible for recommending weight loss, increased physical activity, and improved nutrition (79%), but 83% also believed that clinicians needed more training to adequately address these issues in patients with cancer. The majority of respondents (84%) believed that interventions to implement changes in weight, diet, or activity should be conducted by other clinical staff with relevant expertise. Respondents also were asked which type of providers primarily addressed issues related to patients’ weight, diet, and physical activity levels in their practices. The majority reported that these issues were most typically addressed by physicians (54%), but dietitians (21%) and nurse practitioners, physician assistants, and nurses (16%) also participate in this work across centers.
TABLE 2.
Respondents’ Perspectives on Issues Related to Obesity and Cancer
Clinical Practice Patterns
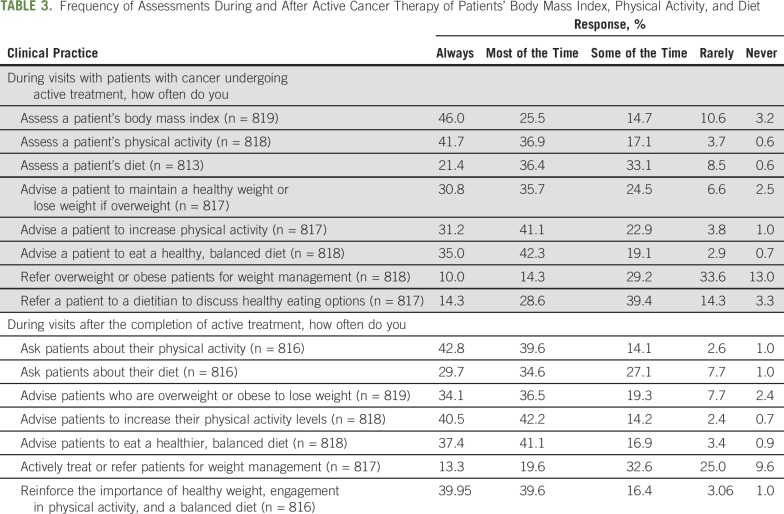
Survey respondents were asked about the frequency with which they addressed patients’ weight, physical activity patterns, and dietary intake during and after cancer treatment (Table 3). During active treatment, the majority of respondents reported that they always or most of the time assessed a patient’s BMI (72%) and physical activity level (78%) but were a bit less likely to always or usually assess a patient’s diet (58%). The majority of respondents also reported that they always or most of the time advise patients to maintain a healthy weight or lose weight if overweight (67%); increase physical activity (73%); and eat a healthy, balanced diet (77%) during active treatment. However, 46% of respondents indicated that they rarely or never refer overweight or obese patients for weight management during active therapy, and only 42% of respondents reported that they always or most of the time refer a patient to a dietitian to discuss healthy eating options.
TABLE 3.
Frequency of Assessments During and After Active Cancer Therapy of Patients’ Body Mass Index, Physical Activity, and Diet
After the completion of active therapy, the majority of respondents reported that they either always or most of the time ask patients about their physical activity (82%) and diet (64%). They also always or most of the time advise patients to increase physical activity levels (83%); eat a healthy, balanced diet (79%); and, for patients who are overweight or obese, lose weight (71%). However, only 33% of respondents reported that they always or most of the time actively treat or refer patients for weight management after completion of active cancer treatment, and 35% reported that they rarely or never treated or referred patients for weight management.
Additional analyses explored whether type of oncology provider, practice location, primary disease treated, or geographic location of practice was related to practice patterns. Similar patterns in terms of assessment, patient advice, and referrals were seen across provider types, practice types, primary diseases treated, and geographic location of practice (data not shown).
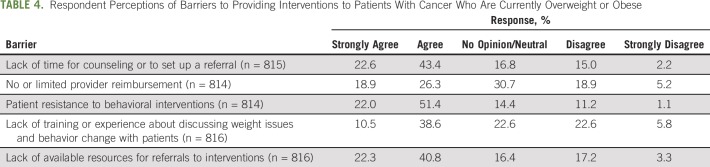
Barriers to Incorporation of Obesity Assessment and Management in Oncology Practice
Respondent opinions on barriers to providing weight management interventions to overweight and obese patients with cancer are listed in Table 4. Most respondents agreed or strongly agreed that a lack of time for counseling or to set up a referral (66%), perceived patient resistance to behavioral interventions (73%), and lack of available resources for referrals to interventions (63%) were barriers to providing these interventions. There was less agreement that a lack of or limited reimbursement for or lack of training or experience in discussing weight issues with patients and behavior change interventions are barriers.
TABLE 4.
Respondent Perceptions of Barriers to Providing Interventions to Patients With Cancer Who Are Currently Overweight or Obese
DISCUSSION
In a survey of 971 practicing oncology providers, attention to weight management, physical activity, and diet in patients with cancer was high during and after cancer treatment. The majority of survey respondents indicated that they believe that the evidence linking obesity to cancer outcomes is strong and that weight and related factors should be addressed as a part of cancer treatment.
The US Preventive Services Task Force and Medicare reimbursement guidelines recommend that clinicians use the 5 A’s model to encourage their patients to make healthy behavior changes and reduce obesity.29 The 5 A’s model involves:
Assessing BMI, physical activity, and diet
Advising patients about the health risks of obesity; the benefits of weight loss, physical activity, and good nutrition; and treatment options
Agreeing on weight loss and behavior change goals and treatment plan details
Assisting patients in identifying and addressing barriers by providing resources, including referrals
Arranging follow-up to provide ongoing assistance or referrals as needed
In the current survey, oncology providers overwhelmingly indicated that they assessed BMI, physical activity, and dietary patterns during and after cancer treatment and advised overweight and obese patients to lose weight, increase physical activity, and consume a healthy diet throughout their treatment course. However, rates of referrals of patients to weight management, physical activity, or nutrition programs were lower. Respondents noted a number of barriers to implementing weight management and related interventions in patients with cancer and called for additional training in obesity-related issues for oncology providers.
The results of this study are consistent with a systematic review of research on obesity counseling more generally (outside oncology care) that found that clinicians frequently advised and assessed but rarely agreed, assisted, or arranged.30 Because that review found that patients would like their clinicians to arrange, advise, agree, and assist, this would suggest that a gap exists between what clinicians are providing and what patients need to achieve a healthy lifestyle.31,32 Of note, among oncology patients, there is less information with regard to patient attitudes and receptivity to messages around weight management, dietary change, and physical activity after a cancer diagnosis. A survey of 15,524 patients with colorectal cancer in the United Kingdom reported that only 31% of survey respondents stated hearing about exercise from their oncology team at any point during their cancer treatment.33 Patients who did report hearing about exercise were more likely to engage in physical activity (51% in the advice group v 42% in the no advice group; odds ratio, 1.74; 95% CI, 1.60 to 1.90; P < .001) and more likely to be meeting physical activity guidelines (25% v 20%; odds ratio, 1.70; 95% CI, 1.54 to 1.88; P < .001). A better understanding of patient perspectives on the advice currently being provided in the setting of oncology visits and its role in promoting healthy behaviors is needed.
Our data are fairly similar to other surveys of oncology providers with regard to attitudes and practices toward obesity-related issues in patients with cancer, although prior reports included smaller numbers of oncology providers and typically focused only on exercise recommendations. For example, a 2005 survey of 281 Canadian oncology providers assessed opinions toward recommending exercise to patients with cancer.34 The majority of providers agreed that exercise was beneficial (62%), important (56%), and safe (63%) for patients with cancer, but only 43% indicated that they recommended exercise to their patients. Another single-site survey of 120 mixed oncology providers (approximately 38% medical doctors, 36% radiation technologists, and 18% nurses) reported that the majority of respondents advised at least 50% of their patients to keep active during and after cancer treatment, but 80% of respondents were not aware of exercise guidelines for patients with cancer, and only 6% referred their patients to exercise programs or specialists.35 Similarly, another survey, disseminated through oncology provider organizations, of 123 oncologists (56% medical oncologists, 30.5% surgical oncologists) found that only 46% of respondents promoted physical activity to patients.36 Twenty percent of those surveyed provided written recommendations, and only 23% referred patients to exercise programs or specialists. Of note, among those who promoted physical activity, only 37% provided advice that was consistent with physical activity guidelines. In many of these surveys, lack of time during clinic visits and lack of referral programs or specialists were noted as barriers to helping patients to increase physical activity.
Somewhat different results were found in a survey of 240 gynecologic oncologists.37 Ninety-five percent of survey respondents believed that adherence to lifestyle recommendations was important, and 85% believed that it was the responsibility of gynecologic oncologists and primary care providers to provide recommendations and support for lifestyle change. Of the survey respondents, 82.5% also referred patients to providers or programs for weight management. Only 8.9% of respondents replied that they did not address obesity-related issues or refer patients to other providers to address these topics. Of note, survey respondents reported high levels of training in obesity-related topics from a combination of self-directed learning, formal course work during and after training, and learning from peers, which suggests that training in these areas led to increased attention to these topics during clinic visits and increased referrals.
Our survey also identified a number of important barriers to the implementation of weight loss and other lifestyle interventions in patients with cancer and cancer survivors. Respondents cited a need for more training in this area as well as a lack of time and suitable programs to which they could refer their oncology patients. To help to provide oncologists with the knowledge and tools that they need to counsel patients in this area, ASCO has produced toolkits for patients and providers that focus on the connection between obesity and cancer38 and authored a position statement on obesity and cancer as part of its obesity initiative.28 However, results of the current survey point to a need for comprehensive guidelines to help to guide oncologists’ recommendations with regard to weight management, exercise, and diet during and after cancer treatment.
A number of limitations of our survey should be recognized. Although our report represents the largest survey of practicing oncology providers to date on this topic, the proportion of ASCO members who responded to this survey was a small fraction of the overall ASCO membership. Our response rate is similar to two recent surveys of ASCO members: one focused on tobacco cessation39 and one more broadly on demographics and practice settings.40 The limited number of respondents to our survey increases the likelihood that respondents may represent a population specifically interested in the survey topic, which potentially contributes to the high proportion of respondents who indicated attention to obesity, physical activity, and diet during clinic visits. However, even in this highly motivated group of individuals, many barriers to facilitating weight loss and increased physical activity were noted as well as a need for more training in obesity-related topics for oncology providers. In addition, our survey did not evaluate the amount or quality of the counseling provided to patients. As noted in other surveys,35,36 many oncology providers were unaware of lifestyle guidelines for patients with cancer, and a number of providers who counseled their patients with regard to lifestyle recommendations did so in a way that was not concordant with established guidelines. Finally, although we did not see differences in response patterns by type of oncology provider, practice location, or setting, the majority of our survey respondents were medical oncologists who practiced in academic or health center settings, which limits the generalizability of our findings to other types of oncology providers and practice settings.
In conclusion, in a survey of nearly 1,000 practicing oncologists, we found that the majority of respondents reported that they frequently assessed body weight, physical activity patterns, and diet in their patients during and after cancer treatment. They also counseled patients to exercise, consume a healthy diet, and lose weight, if applicable. Referral to weight management or physical activity programs/specialists was lower, and a number of barriers were identified for the incorporation of weight management and physical activity programs in the treatment of patients with cancer, including lack of education related to these topics for oncology providers, lack of time, and lack of appropriate referrals for weight management and physical activity programs. These results suggest that new initiatives are needed to help to support education and training of oncology providers with regard to treatment plans for weight management, physical activity, and nutrition for their patients with cancer. Additional work to understand patient perspectives on the guidance they need around weight, physical activity, and diet from oncology providers will help to guide these provider training efforts.
ACKNOWLEDGMENT
We thank Linda Jacobs of the University of Pennsylvania for her input into the design of the survey and acknowledge the contributions of the members of the ASCO Cancer Prevention Committee.
Footnotes
Reprint requests: 2318 Mill Rd, Suite 800, Alexandria, VA 22314; cancerpolicy@asco.org.
AUTHOR CONTRIBUTIONS
Conception and design: Jennifer A. Ligibel, Lee W. Jones, Abenaa M. Brewster, Steven K. Clinton, Larissa A. Korde, Kevin C. Oeffinger, Janette K. Merrill, Catherine M. Alfano
Administrative support: Janette K. Merrill, Sweatha Katta
Collection and assembly of data: Jennifer A. Ligibel, Abenaa M. Brewster, Janette K. Merrill, Sweatha Katta, Catherine M. Alfano
Data analysis and interpretation: Jennifer A. Ligibel, Lee W. Jones, Abenaa M. Brewster, Steven K. Clinton, Larissa A. Korde, Catherine M. Bender, Winston Tan, Janette K. Merrill, Sweatha Katta, Catherine M. Alfano
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Oncologists’ Attitudes and Practice of Addressing Diet, Physical Activity, and Weight Management With Patients With Cancer: Findings of an ASCO Survey of the Oncology Workforce
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Lee W. Jones
Stock and Other Ownership Interests: Pacylex Pharmaceuticals
Steven K. Clinton
Research Funding: National Cancer Institute, American Institute for Cancer Research, American Cancer Society, Department of Defense Prostate Cancer Research Program, US Department of Agriculture, National Cattleman’s Beef Association
Winston Tan
Honoraria: Medscape
No other potential conflicts of interest were reported.
REFERENCES
- 1.Calle EE, Rodriguez C, Walker-Thurmond K, et al. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 2.Le Marchand L, Wilkens LR, Mi MP. Obesity in youth and middle age and risk of colorectal cancer in men. Cancer Causes Control. 1992;3:349–354. doi: 10.1007/BF00146888. [DOI] [PubMed] [Google Scholar]
- 3.Protani M, Coory M, Martin JH. Effect of obesity on survival of women with breast cancer: Systematic review and meta-analysis. Breast Cancer Res Treat. 2010;123:627–635. doi: 10.1007/s10549-010-0990-0. [DOI] [PubMed] [Google Scholar]
- 4. Aune D, Greenwood DC, Chan DSM, et al: Body mass index, abdominal fatness and pancreatic cancer risk: A systematic review and non-linear dose-response meta-analysis of prospective studies. Ann Oncol 23:843-852, 2012. [DOI] [PubMed]
- 5.Chan DS, Vieira AR, Aune D, et al. Body mass index and survival in women with breast cancer-systematic literature review and meta-analysis of 82 follow-up studies. Ann Oncol. 2014;25:1901–1914. doi: 10.1093/annonc/mdu042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheraghi Z, Poorolajal J, Hashem T, et al. Effect of body mass index on breast cancer during premenopausal and postmenopausal periods: A meta-analysis. PLoS One. 2012;7:e51446. doi: 10.1371/journal.pone.0051446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dobbins M, Decorby K, Choi BC. The association between obesity and cancer risk: A meta-analysis of observational studies from 1985 to 2011. ISRN Prev Med. 2013;2013:680536. doi: 10.5402/2013/680536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ma Y, Yang Y, Wang F, et al. Obesity and risk of colorectal cancer: A systematic review of prospective studies. PLoS One. 2013;8:e53916. doi: 10.1371/journal.pone.0053916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castillo JJ, Reagan JL, Ingham RR, et al. Obesity but not overweight increases the incidence and mortality of leukemia in adults: A meta-analysis of prospective cohort studies. Leuk Res. 2012;36:868–875. doi: 10.1016/j.leukres.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 10.Protani MM, Nagle CM, Webb PM. Obesity and ovarian cancer survival: A systematic review and meta-analysis. Cancer Prev Res (Phila) 2012;5:901–910. doi: 10.1158/1940-6207.CAPR-12-0048. [DOI] [PubMed] [Google Scholar]
- 11.Lauby-Secretan B, Scoccianti C, Loomis D, et al. Body fatness and cancer--viewpoint of the IARC working group. N Engl J Med. 2016;375:794–798. doi: 10.1056/NEJMsr1606602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Cancer Research Fund, American Institute for Cancer Research: Diet, Nutrition, Physical Activity and Cancer: A Global Perspective. Continuous Update Project Expert Report 2018. https://www.wcrf.org/dietandcancer.
- 13.Stroup SP, Cullen J, Auge BK, et al. Effect of obesity on prostate-specific antigen recurrence after radiation therapy for localized prostate cancer as measured by the 2006 Radiation Therapy Oncology Group-American Society for Therapeutic Radiation and Oncology (RTOG-ASTRO) Phoenix consensus definition. Cancer. 2007;110:1003–1009. doi: 10.1002/cncr.22873. [DOI] [PubMed] [Google Scholar]
- 14.Druesne-Pecollo N, Touvier M, Barrandon E, et al. Excess body weight and second primary cancer risk after breast cancer: A systematic review and meta-analysis of prospective studies. Breast Cancer Res Treat. 2012;135:647–654. doi: 10.1007/s10549-012-2187-1. [DOI] [PubMed] [Google Scholar]
- 15.Chen CL, Shore AD, Johns R, et al. The impact of obesity on breast surgery complications. Plast Reconstr Surg. 2011;128:395e–402e. doi: 10.1097/PRS.0b013e3182284c05. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen KT, Hanwright PJ, Smetona JT, et al. Body mass index as a continuous predictor of outcomes after expander-implant breast reconstruction. Ann Plast Surg. 2014;73:19–24. doi: 10.1097/SAP.0b013e318276d91d. [DOI] [PubMed] [Google Scholar]
- 17. Sun SX, Greenleaf EK, Hollenbeak CS, et al: Attributable cost of obesity in breast surgery: A matched cohort analysis. Am J Surg 210:668-677.e1, 2015. [DOI] [PubMed]
- 18.Reinertsen KV, Cvancarova M, Loge JH, et al. Predictors and course of chronic fatigue in long-term breast cancer survivors. J Cancer Surviv. 2010;4:405–414. doi: 10.1007/s11764-010-0145-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerber LH, Stout N, McGarvey C, et al. Factors predicting clinically significant fatigue in women following treatment for primary breast cancer. Support Care Cancer. 2011;19:1581–1591. doi: 10.1007/s00520-010-0986-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DiSipio T, Rye S, Newman B, et al. Incidence of unilateral arm lymphoedema after breast cancer: A systematic review and meta-analysis. Lancet Oncol. 2013;14:500–515. doi: 10.1016/S1470-2045(13)70076-7. [DOI] [PubMed] [Google Scholar]
- 21.Schmitz KH, Courneya KS, Matthews C, et al. American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010;42:1409–1426. doi: 10.1249/MSS.0b013e3181e0c112. [DOI] [PubMed] [Google Scholar]
- 22.Buffart LM, Kalter J, Sweegers MG, et al. Effects and moderators of exercise on quality of life and physical function in patients with cancer: An individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev. 2017;52:91–104. doi: 10.1016/j.ctrv.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 23.Mustian KM, Alfano CM, Heckler C, et al. Comparison of pharmaceutical, psychological, and exercise treatments for cancer-related fatigue: A meta-analysis. JAMA Oncol. 2017;3:961–968. doi: 10.1001/jamaoncol.2016.6914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayer DK, Terrin NC, Menon U, et al. Health behaviors in cancer survivors. Oncol Nurs Forum. 2007;34:643–651. doi: 10.1188/07.ONF.643-651. [DOI] [PubMed] [Google Scholar]
- 25.Blanchard CM, Courneya KS, Stein K. Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: Results from the American Cancer Society’s SCS-II. J Clin Oncol. 2008;26:2198–2204. doi: 10.1200/JCO.2007.14.6217. [DOI] [PubMed] [Google Scholar]
- 26.Courneya KS, Katzmarzyk PT, Bacon E. Physical activity and obesity in Canadian cancer survivors: Population-based estimates from the 2005 Canadian Community Health Survey. Cancer. 2008;112:2475–2482. doi: 10.1002/cncr.23455. [DOI] [PubMed] [Google Scholar]
- 27. National Cancer Institute: Cancer Trends Progress Report, 2018. https://progressreport.cancer.gov. [Google Scholar]
- 28.Ligibel JA, Alfano CM, Courneya KS, et al. American Society of Clinical Oncology position statement on obesity and cancer. J Clin Oncol. 2014;32:3568–3574. doi: 10.1200/JCO.2014.58.4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Whitlock EP, Orleans CT, Pender N, et al. Evaluating primary care behavioral counseling interventions: An evidence-based approach. Am J Prev Med. 2002;22:267–284. doi: 10.1016/s0749-3797(02)00415-4. [DOI] [PubMed] [Google Scholar]
- 30.Sherson EA, Yakes Jimenez E, Katalanos N. A review of the use of the 5 A’s model for weight loss counselling: Differences between physician practice and patient demand. Fam Pract. 2014;31:389–398. doi: 10.1093/fampra/cmu020. [DOI] [PubMed] [Google Scholar]
- 31.Moyer VA. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157:373–378. doi: 10.7326/0003-4819-157-5-201209040-00475. [DOI] [PubMed] [Google Scholar]
- 32.LeFevre ML. Behavioral counseling to promote a healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;161:587–593. doi: 10.7326/M14-1796. [DOI] [PubMed] [Google Scholar]
- 33.Fisher A, Williams K, Beeken R, et al. Recall of physical activity advice was associated with higher levels of physical activity in colorectal cancer patients. BMJ Open. 2015;5:e006853. doi: 10.1136/bmjopen-2014-006853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jones LW, Courneya KS, Peddle C, et al. Oncologists’ opinions towards recommending exercise to patients with cancer: A Canadian national survey. Support Care Cancer. 2005;13:929–937. doi: 10.1007/s00520-005-0805-8. [DOI] [PubMed] [Google Scholar]
- 35.Nadler M, Bainbridge D, Tomasone J, et al. Oncology care provider perspectives on exercise promotion in people with cancer: An examination of knowledge, practices, barriers, and facilitators. Support Care Cancer. 2017;25:2297–2304. doi: 10.1007/s00520-017-3640-9. [DOI] [PubMed] [Google Scholar]
- 36.Hardcastle SJ, Kane R, Chivers P, et al. Knowledge, attitudes, and practice of oncologists and oncology health care providers in promoting physical activity to cancer survivors: An international survey. Support Care Cancer. 2018;26:3711–3719. doi: 10.1007/s00520-018-4230-1. [DOI] [PubMed] [Google Scholar]
- 37. Jernigan AM, Tergas AI, Satin AJ, et al: Obesity management in gynecologic cancer survivors: Provider practices and attitudes. Am J Obstet Gynecol 208:408.e1-408.e8, 2013. [DOI] [PubMed]
- 38. Ligibel JA, Alfano C, Burger R, et al: Obesity and Cancer: A Guide for Oncology Providers. Alexandria, VA, American Society of Clinical Oncology, 2014. [Google Scholar]
- 39.Warren GW, Marshall JR, Cummings KM, et al. Addressing tobacco use in patients with cancer: A survey of American Society of Clinical Oncology members. J Oncol Pract. 2013;9:258–262. doi: 10.1200/JOP.2013.001025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kirkwood MK, Hanley A, Bruinooge SS, et al: The state of oncology practice in America, 2018: Results of the ASCO practice census survey. J Oncol Pract 14:e412-e420, 2018. [DOI] [PubMed]