Abstract
Objective:
To describe the relationship between adherence to distinct dietary patterns and nutrition literacy.
Design:
We identified distinct dietary patterns using principal covariates regression (PCovR) and principal components analysis (PCA) from the Diet History Questionnaire II. Nutrition literacy was assessed using the Nutrition Literacy Assessment Instrument (NLit). Cross-sectional relationships between dietary pattern adherence and global and domain-specific NLit scores were tested by multiple linear regression. Mean differences in diet pattern adherence among three predefined nutrition literacy performance categories were tested by ANOVA.
Setting:
Metropolitan Kansas City, USA.
Participants:
Adults (n 386) with at least one of four diet-related diseases.
Results:
Three diet patterns of interest were derived: a PCovR prudent pattern and PCA-derived Western and Mediterranean patterns. After controlling for age, sex, BMI, race, household income, education level and diabetes status, PCovR prudent pattern adherence positively related to global NLit score (P < 0·001, β = 0·36), indicating more intake of prudent diet foods with improved nutrition literacy. Validating the PCovR findings, PCA Western pattern adherence inversely related to global NLit (P = 0·003, β = −0·13) while PCA Mediterranean pattern positively related to global NLit (P = 0·02, β = 0·12). Using predefined cut points, those with poor nutrition literacy consumed more foods associated with the Western diet (fried foods, sugar-sweetened beverages, red meat, processed foods) while those with good nutrition literacy consumed more foods associated with prudent and Mediterranean diets (vegetables, olive oil, nuts).
Conclusions:
Nutrition literacy predicted adherence to healthy/unhealthy diet patterns. These findings warrant future research to determine if improving nutrition literacy effectively improves eating patterns.
Keywords: Nutrition literacy, Diet pattern analysis, Western diet, Mediterranean diet, Principal covariates regression, Principal components analysis
Limited health literacy is associated with poorer health outcomes(1,2), disproportionately affecting minority populations, older adults and persons with lower educational attainment and/or lower incomes(3,4). Health literacy skills required to ‘make appropriate health decisions’(1) are situation specific(5), and this concept has driven nutrition researchers to translate the concept of health literacy into a nutrition context(6–8). Nutrition literacy is defined as ‘the degree to which individuals have the capacity to obtain, process, and understand nutrition information and skills needed in order to make appropriate nutrition decisions’(9).
Health literacy appears to be associated with nutrition behaviours. Those with limited health literacy less often consult food labels(10,11) and have greater difficulty in interpreting food labels(12) as well as estimating appropriate food portions(13). Chari et al. reported that parents with limited health literacy more often report obesogenic feeding behaviours(14). However, reported relationships between health literacy and dietary intake have been mixed. No relationship was found between health literacy and low-salt diet adherence in hypertensive patients(15) or with macronutrient-restricted diets in diabetes patients(16). Conversely, lower diet quality and higher sugar-sweetened beverage intake have been reported among adults with low health literacy(17).
Validated nutrition literacy tools are only recently available, so few data are available to consider the impact of poor nutrition literacy. However, our previous work has demonstrated nutrition literacy is positively related to diet quality(18–20), as measured by the Healthy Eating Index (HEI). The HEI is one method for quantifying diet quality, assigning up to a maximum score of 100 for diet alignment with the Dietary Guidelines for Americans(21), but other indices are also available. Considering that nutrients are consumed within the context of foods and beverages and not as individual nutrients, use of these indices allows researchers to study the overall quality of diets as they relate to a disease or outcome risk. Applied in this way, diet quality indices identify dietary patterns of interest a priori, or using a hypothesis-driven approach.
Alternatively, statistical techniques can be employed to derive individual factors, interpreted as diet patterns, that can be associated with positive or negative dietary behaviours. Two commonly used approaches are reduced rank regression and principal components analysis (PCA). Reduced rank regression is an exploratory approach to identify dietary patterns that explain the largest variation in a dependent variable of interest(22,23). As such, reduced rank regression is an approach that is both a priori (i.e. includes the outcome of interest) and a posteriori (i.e. derives dietary patterns)(22). Moreover, PCA, a simply a posteriori approach, produces an investigator-defined number of dietary patterns that account for maximal variation within dietary data alone(24). Principal covariates regression (PCovR) incorporates principles of both PCA and reduced rank regression to produce dietary patterns that maximize the explanation of variance in dietary intake and the dependent variable of interest(25). Thus, the purpose of the present study was to identify dietary patterns from the reported dietary intake of adults with varying levels of nutrition literacy via PCovR and PCA approaches and investigate the ability for nutrition literacy to predict adherence to those patterns.
Methods
Study design
We examined cross-sectional data collected at baseline from individuals involved in a study for the validation of the Nutrition Literacy Assessment Instrument (NLit)(20).
Participants
Baseline data were available on 402 participants recruited through an existing patient registry and primary care clinics as previously described(20). Eligible participants were ≥18 years of age, spoke and read English, and had self-report of at least one of four chronic diet-related diseases (diabetes, hyperlipidaemia, hypertension or overweight/obesity). Exclusion criteria for the present study included overt psychiatric illness, impaired vision that affected ability to read the nutrition literacy tool, cognitive impairment and weight of ≥227 kg (≥500 lb). The study protocol was approved by the Institutional Review Board at the University of Kansas Medical Center. Informed consent was obtained from all study participants according to institutional guidelines.
Nutrition literacy assessment
Nutrition literacy was measured at baseline using the NLit. Population-specific versions of the NLit were previously used in breast cancer survivors(18,26), parents of young children(19), adults with chronic disease(20) and Spanish-speaking adults(19). The NLit is a sixty-four-item survey that includes six nutrition literacy domains: (i) Nutrition and Health; (ii) Energy Sources in Food; (iii) Household Food Measurement; (iv) Food Label and Numeracy; (v) Food Groups; and (vi) Consumer Skills. In previous analyses, the NLit demonstrated substantial factor validity and reliability (0·97, CI = 0·96, 0·98), test–retest reliability (0·88, CI = 0·85, 0·90) and convergent validity as a predictor of diet quality (β = 0·17, R 2 = 0·10, P < 0·0001)(20). Global nutrition literacy (gNLit) scores and nutrition literacy domain sub-scores were calculated by summing the quantity of correctly answered survey items. Global nutrition literacy scores were categorized into three nutrition literacy performance groups with previously defined cut-off points(20): poor (gNLit ≤ 44), possibly poor (gNLit =45–57) and good (gNLit ≥ 58).
Dietary intake assessment
At a return visit approximately one month after the baseline visit, participants reported usual dietary intake by completing the National Cancer Institute’s Diet History Questionnaire (DHQ) II(27). The DHQ has been validated and estimates dietary intake over the past year through 134 food and eight supplement intake questions(28). The National Cancer Institute’s Diet*Calc software(29) utilized DHQ II input to quantify nutrient intake and food group variables.
Empirical dietary patterns
Dietary patterns were identified through two distinct methods: PCovR and PCA. For both of these diet pattern development approaches, we included DHQ II output of twenty Food Pattern Equivalents Database 2013–14 (FPED)(30) variables and fifteen expansive/additional variables. FPED collapses dietary intake into thirty-seven food group variables. Because collapsing food intake into fewer variables inherently eliminates some nuance of food characterization, we identified fifteen additional foods to include in the analysis that were either expanded from FPED variables or foods neglected by FPED. Table 1 summarizes the thirty-five total variables included in these analyses.
Table 1.
List of the thirty-five food variables included in derivation of dietary patterns by principal covariates regression and principal components analysis
| Food group | Included diet variables | Excluded/expanded FPED variables |
|---|---|---|
| Fruit | Citrus, melons & berries† | Total fruit† |
| Other fruit† | ||
| Fruit juice† | ||
| Vegetables | Dark green vegetables† | Total vegetables† |
| Tomatoes† | Total starchy vegetables† | |
| Other red & orange vegetables† | ||
| Potatoes† | ||
| Other starchy vegetables† | ||
| Other vegetables† | ||
| Beans & peas as vegetables† | ||
| Grains | Whole grains† | Total grains† |
| Refined grains† | ||
| Protein foods | Red meat† | Total protein foods† |
| Cured meat† | Total meat, poultry and seafood† | |
| Organ meat† | Beans and peas as protein† | |
| Poultry† | Low n-3 seafood† | |
| Eggs† | High n-3 seafood† | |
| Soyabean products† | ||
| Nuts & seeds† | ||
| Fried fish & shrimp | ||
| Fresh/canned low n-3 fish | ||
| Fresh/canned high n-3 fish | ||
| Dairy | High-fat dairy | Total dairy† |
| Low-fat dairy | Milk† | |
| Cheese† | ||
| Yoghurt† | ||
| Oils | Olive oil | Oils† |
| Vegetable oil | ||
| Solid fats | Butter | Solid fats† |
| Margarine | ||
| Reduced-fat margarine | ||
| Added sugars | Sweets & candy | Added sugars† |
| Sugar-sweetened beverages | ||
| Alcoholic drinks | Alcoholic drinks† | |
| Added variables | Coffee Tea |
FPED, Food Pyramid Equivalents Database.
Designates FPED variable.
Because food group loadings in the resultant dietary patterns could be susceptible to extreme intake outliers, data were assessed for non-viable under- and over-report of dietary intake prior to derivation of dietary patterns. We calculated modified Z-scores(31) for energy intake and removed individuals with scores greater than an absolute value of 3·5. Sixteen individuals were identified as under- (n 12) or over-reporters (n 4) and were removed from the dietary pattern analysis. We were hesitant to exclude under- and over-reporters due to concerns that doing so would exclude more with poor nutrition literacy(16). Upon further analysis, however, we determined that nutrition literacy scores were evenly distributed among those excluded.
Principal covariates regression
We performed PCovR using the [PCovR](32) package for R (R Foundation, Vienna, Austria). Thirty-five food variables were centred and scaled to a mean of 0 and an sd of 1. The centred FPED variables were included as independent variables and the total score from the NLit was included as the dependent variable in the analysis. [PCovR], by default, utilizes the varimax rotation for maximal data interpretation and automatically retains relevant components based upon eigenvalues. We calculated individual PCovR diet pattern adherence scores by multiplying each individual’s standardized food group intake by that food variable’s factor loading score and summing the products for all thirty-five food variables(25).
Principal components analysis
PCA was performed using the [psych] package for R. Intake data for thirty-five food variables centred and standardized to a mean of 0 and an sd of 1 were included in the PCA and rotated with the varimax rotation method. Visualization of the component eigenvalues indicated retention of the first three components from the PCA for further analysis. For each rotated component, individual component adherence scores were calculated by multiplying individual standardized food group intake by that food variable’s factor loading score and summing the products for all thirty-five food variables(33).
Statistical analyses
The primary aim of the present research was to investigate the relationships between nutrition literacy and empirically derived diet patterns. Continuous variables were expressed as mean and sd. All models were assessed for normality through visualization of residual Q–Q plots. Dependent data with non-normally distributed residuals were transformed using a Box–Cox transformation. Parametric analyses were performed on transformed dependent data with slightly non-normal distribution in lieu of non-parametric analyses due to ‘robustness to non-normality’ of the data based on the large sample size of the study. Linear regression models were used to investigate the continuous relationship between nutrition literacy scores and diet pattern adherence. Multiple linear regression models included seven predetermined covariates of interest: age, sex, household income, education level, BMI, race and diabetes status. Mean differences in dietary pattern adherence among nutrition literacy performance groups were tested by ANOVA. Post hoc pairwise comparisons of the ANOVA were adjusted using the Bonferroni–Holm adjustment. Statistical analyses were performed using R version 3.4.3. Statistical tests were two-tailed with significance set at P < 0·05. R statistical analysis script is included in the online supplementary material, Supplemental File 1.
Results
Participant characteristics
Data from 386 participants ranging in age from 18 to 82 years (mean age = 54·5 (sd 14·8) years) and reporting one or more chronic diseases were analysed. Demographic, anthropometric and dietary intake characteristics for these participants are included in Table 2. The poor nutrition literacy group was significantly older (P < 0·001), less educated (P < 0·001), reported less household income (P < 0·001) and had greater report of diabetes (P = 0·06) relative to the possibly poor and good nutrition literacy groups. In contrast, the poor nutrition literacy group also had a lower BMI (P = 0·05); however, all groups were obese.
Table 2.
Characteristics of adult participants (n 386) with at least one of four diet-related diseases, metropolitan Kansas City, USA, January 2015–July 2016
| Overall (n 386) |
Poor (n 53) |
Possibly poor (n 232) |
Good (n 101) |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean or instance frequency | sd or % | Mean or instance frequency | sd or % | Mean or instance frequency | sd or % | Mean or instance frequency | sd or % | P | |
| Demographic/anthropometric | |||||||||
| Age (years) | 54·5 | 14·8 | 58·3 | 13·2 | 56·0 | 14·6 | 49·2 | 14·7 | <0·001 |
| Sex (female/male) | 274/112 | 71/29 | 29/24 | 55/45 | 162/70 | 70/30 | 83/18 | 82/18 | 0·001 |
| Chronic disease diagnosis | |||||||||
| Diabetes | 110 | 29 | 22 | 42 | 64 | 28 | 24 | 24 | 0·06 |
| Hypertension | 216 | 56 | 37 | 70 | 136 | 59 | 43 | 43 | 0·002 |
| Hyperlipidaemia | 172 | 45 | 27 | 51 | 106 | 46 | 39 | 39 | 0·30 |
| Overweight/obesity | 331 | 86 | 38 | 72 | 205 | 88 | 88 | 87 | 0·01 |
| BMI (kg/m2) | 34·5 | 8·8 | 32·6 | 7·7 | 35·4 | 9·0 | 33·5 | 8·6 | 0·05 |
| Education level | <0·001 | ||||||||
| High school/GED or less | 53 | 14 | 32 | 65 | 18 | 8 | 3 | 3 | |
| Some college or associate degree | 139 | 37 | 12 | 25 | 97 | 42 | 30 | 30 | |
| Bachelor’s degree or higher | 187 | 49 | 5 | 10 | 116 | 50 | 66 | 67 | |
| Race | <0·001 | ||||||||
| Caucasian | 233 | 60 | 17 | 32 | 132 | 57 | 84 | 83 | |
| African American | 131 | 34 | 29 | 55 | 89 | 38 | 13 | 13 | |
| Other/undisclosed | 22 | 6 | 7 | 13 | 11 | 5 | 4 | 4 | |
| Ethnicity | <0·001 | ||||||||
| Hispanic or Latino | 36 | 10 | 9 | 21 | 23 | 11 | 4 | 4 | |
| Non-Hispanic | 297 | 83 | 23 | 55 | 182 | 84 | 92 | 93 | |
| Other/undisclosed | 24 | 7 | 10 | 24 | 11 | 5 | 3 | 3 | |
| Annual household income ($US) | <0·001 | ||||||||
| <25 000 | 90 | 24 | 28 | 60 | 49 | 21 | 13 | 13 | |
| 25 000–49 999 | 110 | 29 | 10 | 21 | 80 | 35 | 20 | 20 | |
| 50 000–99 999 | 123 | 33 | 7 | 15 | 71 | 31 | 45 | 46 | |
| ≥100 000 | 51 | 14 | 2 | 4 | 29 | 13 | 20 | 20 | |
| Nutrition literacy† | |||||||||
| Global | 52·2 | 8·2 | 36·0 | 8·4 | 52·8 | 3·4 | 59·4 | 1·4 | <0·001 |
| Nutrition & Health | 8·6 | 1·4 | 6·6 | 1·7 | 8·7 | 1·1 | 9·7 | 0·6 | <0·001 |
| Energy Sources in Food | 8·3 | 2·0 | 4·8 | 1·8 | 8·4 | 1·5 | 9·7 | 0·6 | <0·001 |
| Household Food Measurement | 6·5 | 1·6 | 5·2 | 1·5 | 6·3 | 1·5 | 7·6 | 0·9 | <0·001 |
| Food Label & Numeracy | 7·2 | 2·1 | 3·5 | 2·2 | 7·4 | 1·5 | 8·5 | 0·6 | <0·001 |
| Food Groups | 14·1 | 2·5 | 10·2 | 4·7 | 14·4 | 1·2 | 15·5 | 0·8 | <0·001 |
| Consumer Skills | 7·6 | 1·5 | 5·6 | 1·7 | 7·7 | 1·2 | 8·5 | 0·7 | <0·001 |
| Dietary intake‡ | |||||||||
| Energy (kJ) | 7782 | 4686 | 9456 | 6945 | 7531 | 4435 | 7406 | 3556 | 0·02 |
| Energy (kcal) | 1860 | 1120 | 2260 | 1660 | 1800 | 1060 | 1770 | 850 | 0·02 |
| Fat (g) | 74 | 50 | 88 | 85 | 71 | 43 | 73 | 38 | 0·08 |
| Carbohydrate (g) | 228 | 149 | 281 | 191 | 227 | 152 | 203 | 105 | 0·01 |
| Fibre (g) | 16·6 | 9·8 | 16·0 | 9·3 | 17·0 | 9·5 | 18·2 | 12·3 | 0·32 |
| Protein (g) | 70 | 49 | 85 | 82 | 67 | 42 | 69 | 36 | 0·04 |
| Diet pattern adherence‡,§ | |||||||||
| PCovR Prudent pattern score | 0·0 | 1·0 | −1·0 | 1·3 | 0·0 | 0·8 | 0·5 | 0·9 | <0·001 |
| PCA Western pattern score | 0·0 | 1·0 | 0·4 | 1·5 | −0·1 | 0·9 | −0·1 | 0·9 | 0·002 |
| PCA Mediterranean pattern score | 0·0 | 1·0 | −0·2 | 1·0 | 0·0 | 1·0 | 0·1 | 1·0 | 0·02 |
GED, General Educational Development; PCovR, principal covariates regression; PCA, principal components analysis.
Continuous variables assessed by ANOVA. Categorical variables assessed by the χ 2 test. Significance set at P < 0·05.
Measured by the Nutrition Literacy Assessment Instrument.
Measured by the Diet History Questionnaire II.
Values of adherence are linear combination of diet pattern food loadings and standardized intake. Adherence scores are relative to the specific diet pattern and have no unit of measurement.
Dietary pattern identification by principal covariates regression and principal components analysis
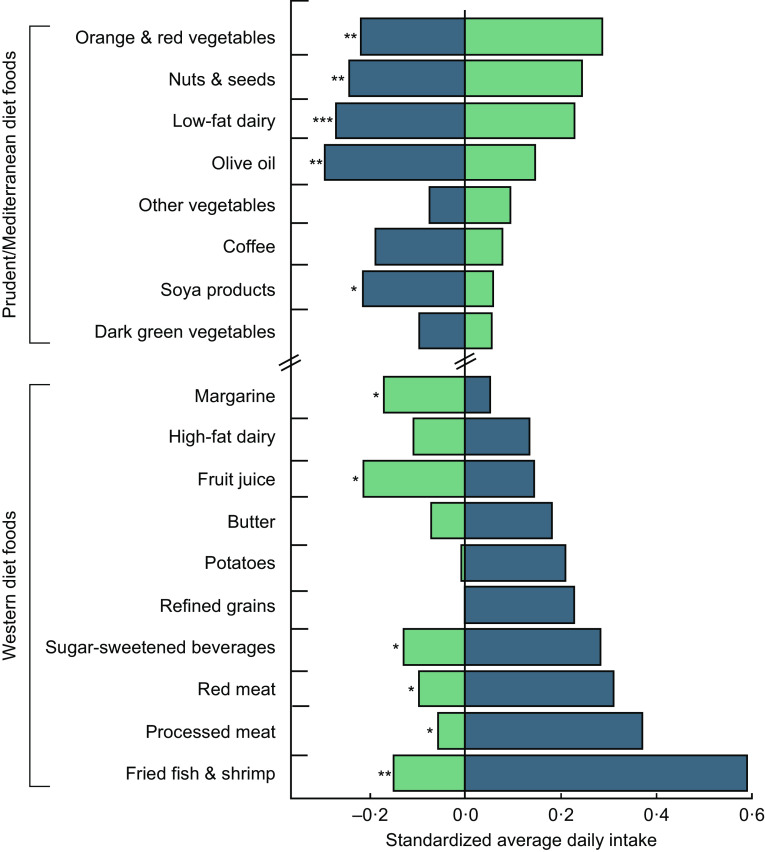
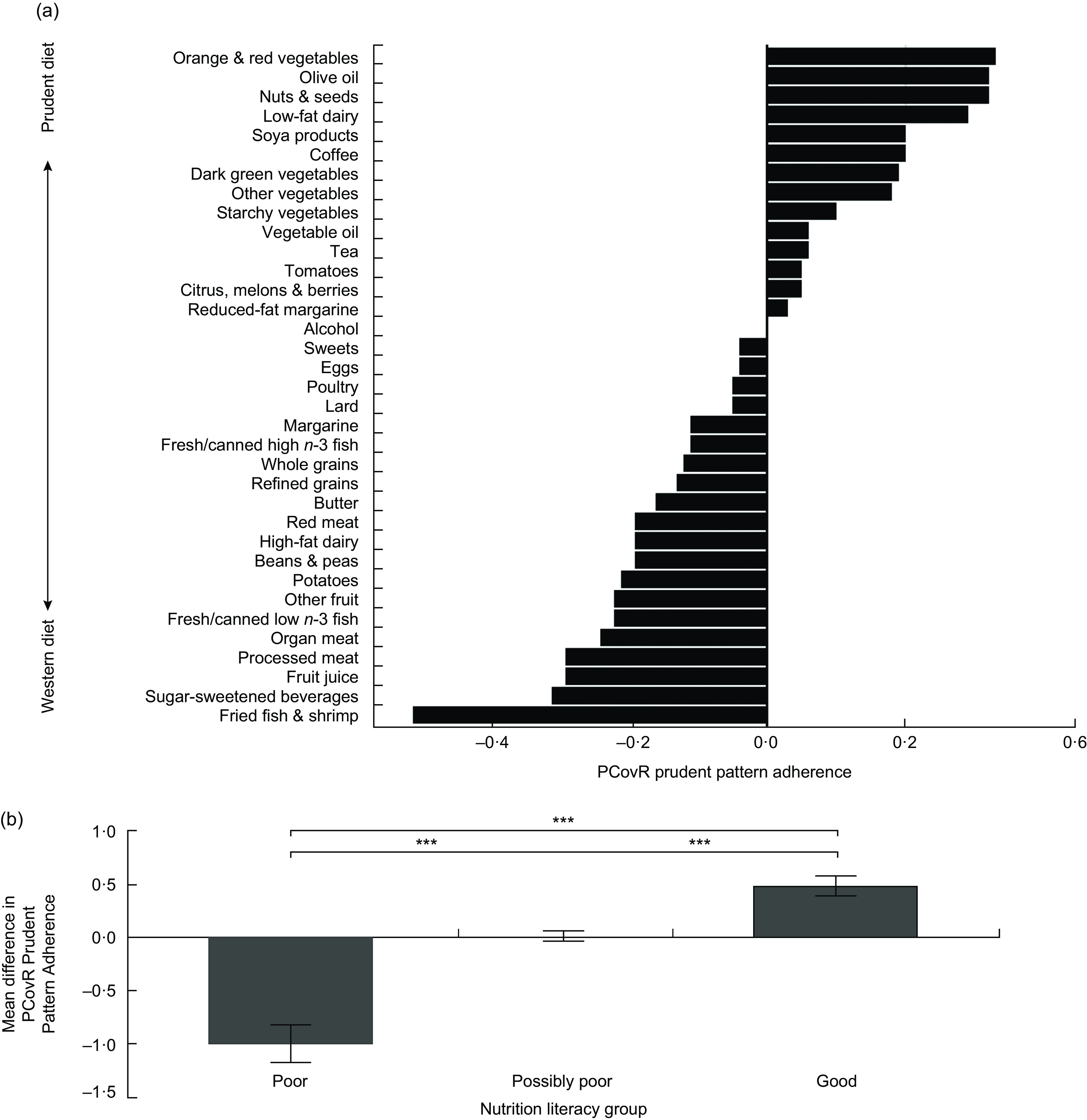
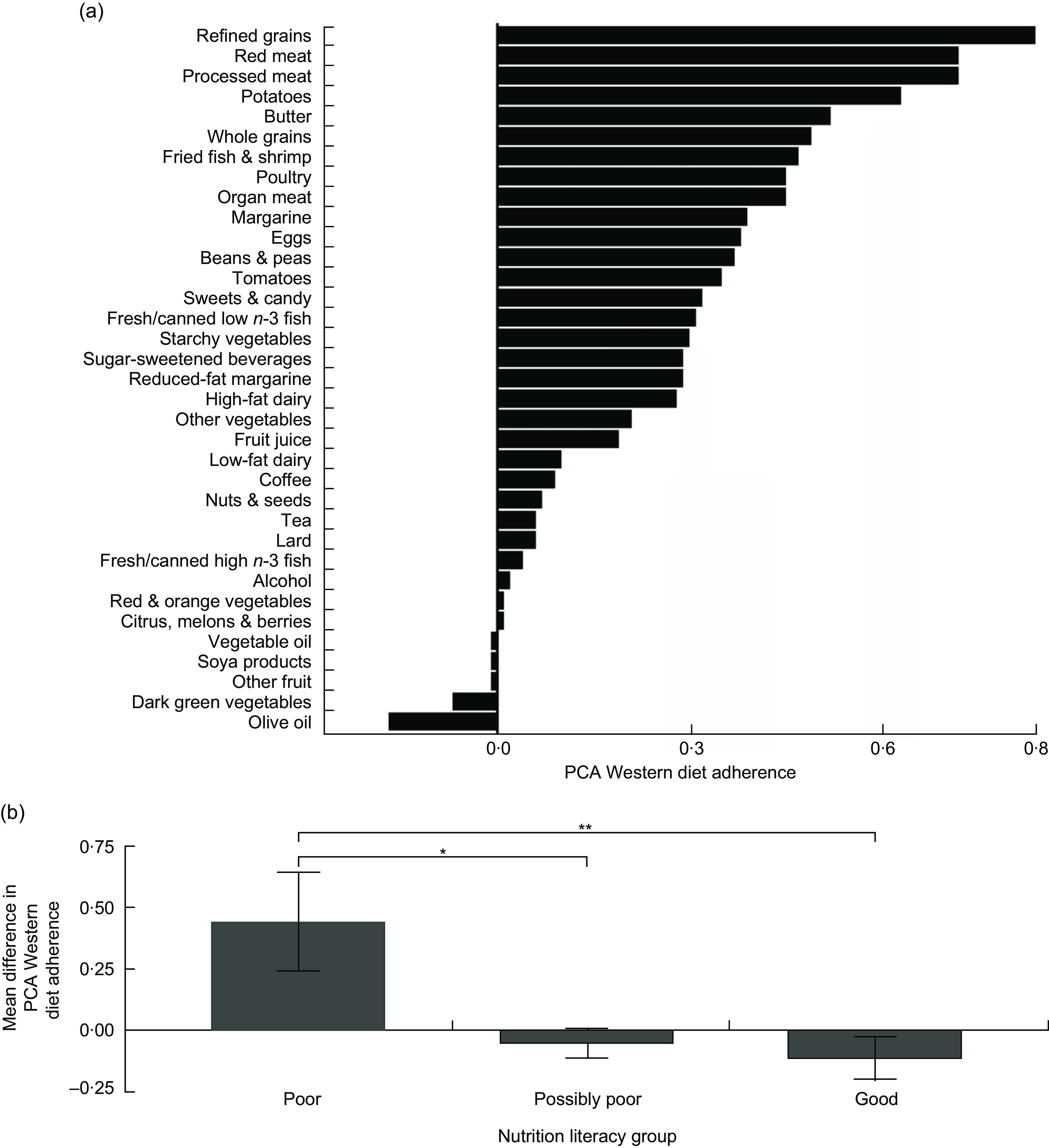
One component was automatically retained for further analysis from the PCovR describing 5 % of variance in the dietary intake data (independent variables) and 23 % of variance in gNLit scores (dependent variable). We named this component the ‘PCovR prudent pattern’ because it exhibited high positive loadings on food variables consistent with a prudent diet with inversely high negative loadings on food variables consistent with a Western diet (Fig. 1(a)). From the PCA, three diet components had eigenvalues >1 and also explained a large amount of dietary variance. The first rotated component (Fig. 2(a)) from the PCA explained 13 % of the total dietary intake variance and exhibited high loadings on food variables that contribute to a Western diet, thus we retained and named it the ‘PCA Western pattern’. We also retained the second rotated component (Fig. 3(a)) which explained 11 % of the total dietary intake variance, loaded highly on food components consistent with a Mediterranean diet, thus we named it the ‘PCA Mediterranean pattern’. We opted not to retain the third rotated component which presented no discernibly meaningful dietary pattern.
Fig. 1.
Principal covariates regression (PCovR)-derived prudent pattern factor loadings and adherence by nutrition literacy performance classification (assessed using the Nutrition Literacy Assessment Instrument (NLit)) among adults with at least one of four diet-related diseases, metropolitan Kansas City, USA, January 2015–July 2016. The PCovR prudent pattern explains 5 % of dietary intake variation and 23 % of variation in global NLit scores. (a) Factor loadings are represented as the bars (n 386), January 2015–July 2016. Intake of foods that have high positive loadings resulted in higher prudent pattern adherence. Conversely, intake of foods with high negative loadings resulted in higher Western pattern adherence. (b) Mean differences in adherence to the PCovR prudent pattern among nutrition literacy performance classification groups. Mean differences are represented as bars and their standard deviations are represented by error bars. Positive scores indicate higher intake of foods associated with the prudent diet, while negative scores indicate higher intake of foods associated with the Western diet. *P < 0·05, **P < 0·01, ***P < 0·001
Fig. 2.
Principal components analysis (PCA)-derived Western pattern factor loadings and adherence by nutrition literacy performance classification (assessed using the Nutrition Literacy Assessment Instrument) among adults with at least one of four diet-related diseases, metropolitan Kansas City, USA, January 2015–July 2016. The PCA Western pattern explains 13 % of dietary intake variation. (a) Factor loadings are represented as the bars (n 386). Intake of foods that have high positive loadings resulted in higher diet pattern adherence scores. Intake of foods with low or negative loading coefficients resulted in low/negative diet pattern adherence scores. (b) Mean differences in adherence to the PCA Western pattern among nutrition literacy performance classification groups. Mean differences are represented as bars and their standard errors are represented by error bars. Positive scores indicate higher intake of foods associated with the Western diet, while low/negative scores indicate lower intake of foods from the Western diet. *P < 0·05, **P < 0·01, ***P < 0·001
Fig. 3.
Principal components analysis (PCA)-derived Mediterranean pattern factor loadings and adherence by nutrition literacy performance classification (assessed using the Nutrition Literacy Assessment Instrument) among adults with at least one of four diet-related diseases, metropolitan Kansas City, USA. The PCA Mediterranean pattern explains 11 % of dietary intake variation. (a) Factor loadings are represented as the bars (n 386), January 2015–July 2016. Intake of foods that have high positive loadings resulted in higher diet pattern adherence scores. Intake of foods with low or negative loading coefficients resulted in low/negative diet pattern adherence scores. (b) Mean differences in adherence to the PCA Mediterranean pattern among nutrition literacy performance classification groups. Mean differences are represented as bars and their standard errors are represented by error bars. Positive scores indicate higher intake of foods associated with the Mediterranean diet, while low/negative scores indicate lower intake of foods from the Mediterranean diet. *P < 0·05, **P < 0·01, ***P < 0·001
Prediction of diet pattern adherence by nutrition literacy score
We first investigated the level at which gNLit scores were predictive of adherence to the PCovR prudent pattern through linear regression with multiple adjustments. Because nutrition literacy scores were involved in derivation of the PCovR prudent pattern, there was a high likelihood that gNLit scores would be related to this pattern’s adherence. Diet adherence was positively related to gNLit score (P < 0·001, β = 0·48), indicating that improved nutrition literacy predicted higher intake of foods related to the prudent diet and lower intake of Western diet-related foods. Table 3 demonstrates this relationship along with multiple model adjustments for all seven variables of interest and a model that excludes education level since it was found to be moderately collinear with gNLit scores (R2 = 0·55). The strong ability for nutrition literacy to predict PCovR prudent pattern adherence remained in all models assessed (Table 3).
Table 3.
Multiple linear regression relationships between nutrition literacy scores and dietary pattern adherence among adults (n 386) with at least one of four diet-related diseases, metropolitan Kansas City, USA, January 2015–July 2016
| Model 1† | Model 2‡ | Model 3§ | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependent variable | Estimate | 95 % CI | β | R 2 | P | Estimate | 95 % CI | β | R 2 | P | Estimate | 95 % CI | β | R 2 | P |
| PCovR prudent pattern | 0·06 | 0·05, 0·07 | 0·48 | 0·23 | <0·001 | 0·04 | 0·03, 0·06 | 0·34 | 0·30 | <0·001 | 0·05 | 0·04, 0·06 | 0·40 | 0·26 | <0·001 |
| PCA Western pattern | −0·02 | −0·03, −0·01 | −0·13 | 0·02 | 0·003 | −0·02 | −0·02, 0·0 | −0·11 | 0·10 | 0·10 | −0·02 | −0·03, −0·01 | −0·15 | 0·10 | <0·006 |
| PCA Mediterranean pattern | 0·02 | 0·00, 0·03 | 0·12 | 0·02 | 0·02 | 0·01 | −0·10, 0·03 | 0·08 | 0·01 | 0·20 | 0·02 | 0·00, 0·03 | 0·12 | 0·02 | 0·04 |
PCovR, principal covariates regression; PCA, principal components analysis; gNLit, global nutrition literacy.
Continuous covariates: age, BMI, household income and education level.
Categorical covariates: sex, race and diabetes status.
Model 1: Simple linear regression of diet pattern adherence predicted by gNLit scores.
Model 2: Multiple linear regression of diet pattern adherence predicted by gNLit scores and all covariates of interest (age, sex, BMI, race, household income, education level and diabetes status).
Model 3: Multiple linear regression of diet pattern adherence predicted by gNLit scores and all covariates of interest, excluding education level.
We next investigated nutrition literacy’s predictability of diet adherence to the diet patterns derived by PCA. Similar to the results in PCovR, worse gNLit score predicted higher intake of foods associated with the Western pattern (P = 0·003, β = −0·15) while better nutrition literacy predicted higher intake of foods associated with a Mediterranean pattern (P = 0·02, β = 0·12). Both Western and Mediterranean pattern adherence lost significance with gNLit score when controlled for all seven covariates of interest (Western: P = 0·10, β = −0·11; Mediterranean: P = 0·2, β = 0·08) but regained significance in the model excluding education level (Western: P = 0·006, β = −0·15; Mediterranean: P = 0·04, β = 0·12).
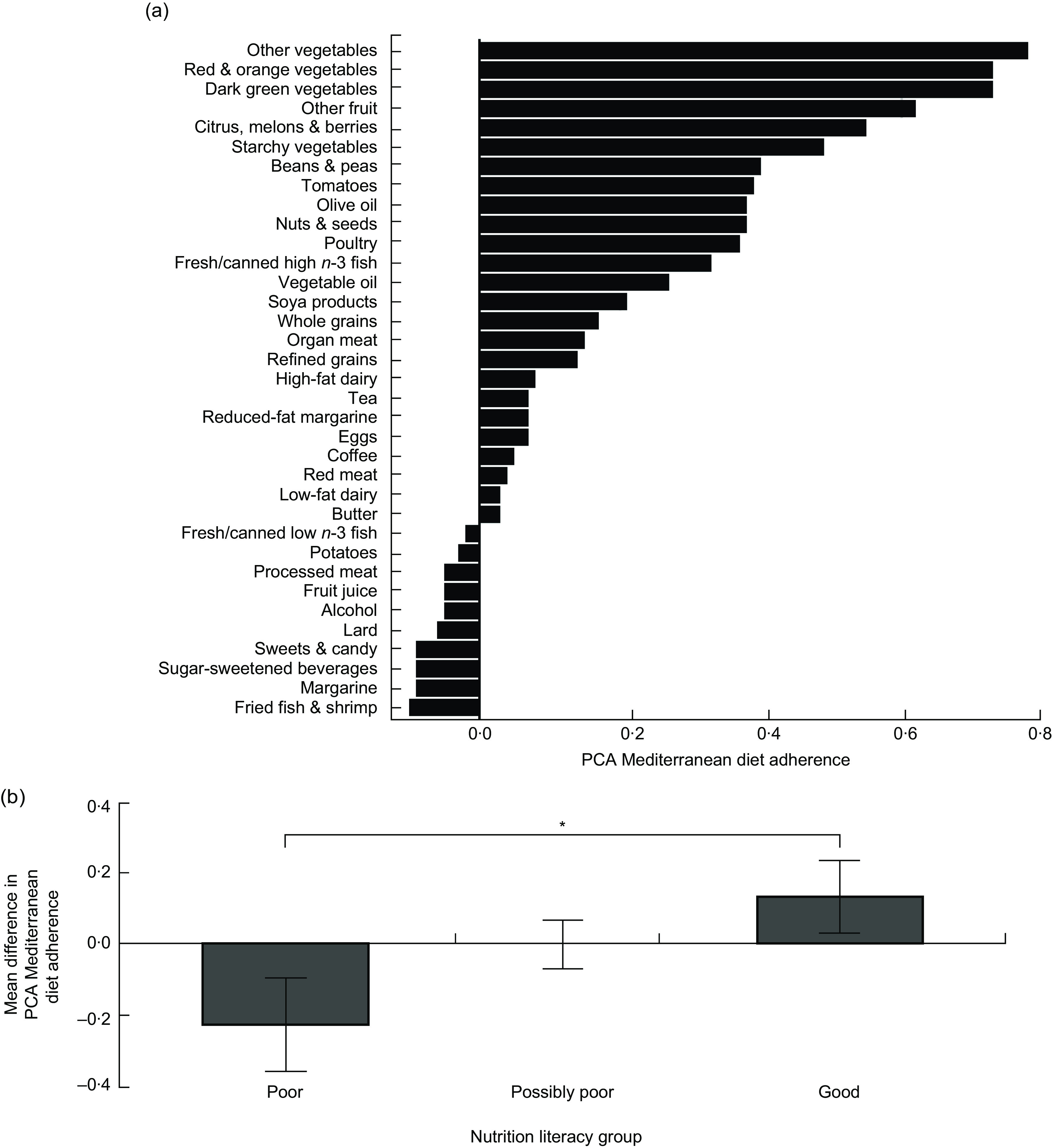
We investigated differences in dietary pattern adherence by nutrition literacy performance classification. Mean PCovR prudent pattern adherence improved stepwise among each of the three categories (P < 0·001 for all), with the highest Western pattern adherence in the poor nutrition literacy group and the highest prudent diet adherence in the good nutrition literacy group (Fig. 1(b)). The poor nutrition literacy group also had significantly higher adherence to the PCA Western pattern than the possibly poor and good nutrition literacy groups (Fig. 2(b), P = 0·002). There were no differences in PCA Western pattern adherence between the possibly poor and good nutrition literacy groups. Adherence to the PCA Mediterranean pattern was significantly higher in the good nutrition literacy group relative to those with poor nutrition literacy (Fig. 3(b), P = 0·02). To extend this analysis, Fig. 4 illustrates the difference in specific food group intake between poor and good nutrition literacy for foods that contributed to the specific derived diet patterns. The good nutrition literacy group consumed significantly more olive oil, low-fat dairy, nuts and seeds, orange and red vegetables, and soya products; food contributors to the prudent and Mediterranean patterns. The poor nutrition literacy group consumed significantly more fried fish and shrimp, processed meat, red meat, sugar-sweetened beverages, fruit juice and margarine; food contributors to the Western pattern.
Fig. 4.
The difference in standardized food intake between the poor ( ) and good (
) and good ( ) nutrition literacy groups of adults with at least one of four diet-related diseases, metropolitan Kansas City, USA, January 2015–July 2016. Values are group mean intake Z-scores. The plot contains eighteen of the thirty-five food groups utilized in the derivation of the dietary patterns. These eighteen food groups were selected for presentation due to their unique contribution to either the Western pattern or the prudent/Mediterranean pattern and large difference in intake between the poor and good nutrition literacy groups. Intake of these particular food groups explains the observed relative difference in dietary pattern adherence among nutrition literacy groups. *P < 0·05, **P < 0·01, ***P < 0·001
) nutrition literacy groups of adults with at least one of four diet-related diseases, metropolitan Kansas City, USA, January 2015–July 2016. Values are group mean intake Z-scores. The plot contains eighteen of the thirty-five food groups utilized in the derivation of the dietary patterns. These eighteen food groups were selected for presentation due to their unique contribution to either the Western pattern or the prudent/Mediterranean pattern and large difference in intake between the poor and good nutrition literacy groups. Intake of these particular food groups explains the observed relative difference in dietary pattern adherence among nutrition literacy groups. *P < 0·05, **P < 0·01, ***P < 0·001
We also examined whether nutrition literacy domain sub-scores related to dietary pattern adherence via linear regression. All six of the nutrition literacy sub-scores were positively related to intake of the PCovR prudent pattern (P < 0·001 for all). Increased scores in subdomains of Nutrition and Health (P = 0·05, β = −0·10), Energy Sources in Food (P = 0·03, β = −0·18), Household Food Measurement (P = 0·04, β = −0·11) and Food Label and Numeracy (P = 0·03, β = −0·11) were inversely related to PCA Western pattern adherence. PCA Mediterranean pattern adherence improved with increased scores for Energy Sources in Food (P = 0·03, β = 0·11), Household Food Measurement (P = 0·004, β = 0·15) and Consumer Skills (P = 0·02, β = 0·12) subdomains.
Discussion
The current study provides further evidence that nutrition literacy is a viable predictor of diet quality as evidenced by the diet patterns that emerged in the analysis. Using two different empirical diet pattern methods, poor nutrition literacy predicted high Western diet adherence while good nutrition literacy predicted higher adherence to a prudent and Mediterranean diet. These data reaffirm two crucial nutrition literacy-related points: (i) that nutrition literacy is an important element for the capability of making healthy dietary choices; and (ii) the applicability of our previously defined nutrition literacy performance cut-off points(20).
The findings of the present study build upon the previous publication tying nutrition literacy to HEI scores(20) by using empirical methods to identify dietary patterns characterized by intake of specific foods. By design, PCovR includes a priori outcome variables within the regression to identify factors (dietary patterns) and weights the components based on maximal variance within the diet data that render the largest influence on outcomes of interest(25,32). Yet, with this analysis, there was no guarantee that the diet pattern would present in a discernible manner. We assert the finding through PCovR that poor nutrition literacy best predicted high intake of fried foods, sugar-sweetened beverages, processed meat, potatoes, red meat, high-fat dairy, butter and refined grains, and that good nutrition literacy predicted high intake of vegetables, nuts and seeds, olive oil, low-fat dairy and soya products, is the strongest finding of the present study. This suggests an important role for nutrition literacy as knowledge and skill that are drawn upon when an individual makes food choices.
Since PCovR utilized NLit scores to derive the dietary pattern of interest, we acknowledge that there was a high likelihood of a relationship between nutrition literacy and adherence to this diet pattern; however, what is most significant was that nutrition literacy clearly defined a pattern with healthy/unhealthy polar ends by this method. Figure 1(b) and the regression analyses in Table 3 extend the relationship interpretation by demonstrating multiple model adjustment, directionality of the relationship and relative variation in adherence among three levels of nutrition literacy performance. Frequently PCA-derived dietary patterns fail to explain variation in outcomes(34–36). Therefore, our findings through PCA that, among all covariates, poor nutrition literacy was the strongest predictor of a Western pattern and good nutrition literacy the strongest predictor of a Mediterranean pattern reiterate and validate the findings of the PCovR analysis.
Age, income and education were all associated with Western pattern adherence, consistent with previous findings demonstrating inverse relationships between socio-economic status and diet quality(37) and that higher diet quality is associated with higher food costs(38). While we found disparity between nutrition literacy groups in age, education and income, of these, nutrition literacy was the most significant predictor of diet pattern adherence. Thus, although it is difficult to disentangle their relationships, nutrition literacy may be a greater factor influencing food choice than demographic factors.
Implications and future directions
Findings of the present study suggest that nutrition literacy should be investigated as a mediator of demographic factors in the path to a healthy diet. This idea is consistent with the finding that nutrition knowledge was a mediator of socio-economic status in the diet quality of Australian mothers(39) and that health literacy is a mediator of disease disparity rather than race(2,40,41) or education(4).
Taking a ‘social determinants of health’ perspective, it is intuitive that these social and environmental factors may powerfully influence acquisition of nutrition literacy, cooking skills, and availability of guidance on food and nutrition decisions as they relate to health(42,43). It has been argued that differences in diet between social classes reflect a difference in access to a healthy food supply and that healthy food access influences food choices more than health education(43). In the USA, food insecurity is more common in ‘food deserts’ and is associated with shopping at convenience stores, where healthy foods are less available and more expensive(44). Consequently, a growing body of literature has examined the role of healthy food access for improving food purchasing and diet behaviours in neighbourhoods and geographic regions with poor access. However, recent studies investigating changes in purchasing and diet behaviours after the introduction of ‘healthy’ store types (e.g. full-service supermarkets) have not shown that increasing access to healthy food alone improves the healthfulness of food items purchased or consumed(45– 47).
Consistent with our findings that good nutrition literacy predicted a healthy diet pattern, recent results from the US Department of Agriculture’s National Household Food Acquisition and Purchase Survey indicate that consumers with greater attention to nutrition information purchase higher-quality foods and consume a higher-quality diet, even when controlling for socio-economic differences(48). Some have included nutrition education alone or within a multiple-method approach to change purchasing behaviour and found increases in purchases of fruits and vegetables(49–51). While some have identified price discounting as an intervention strategy with greater effect upon purchasing behaviour than nutrition education(50,52,53), none of these studies reported measured baseline nutrition literacy (i.e. referred to as ‘nutrition knowledge’ in cited studies) nor the effects of the nutrition education interventions upon nutrition literacy. Unfortunately, in the absence of measured change in nutrition literacy, strong conclusions cannot be made regarding the effectiveness of nutrition education. Indeed, while mixed-approach supermarket-based intervention strategies have shown some success, using validated tools to evaluate improvements in nutrition literacy and behaviour in the analysis of outcomes is critical for identifying intervention methods that contribute to desired outcomes(54). Regardless, our data demonstrate that including nutrition literacy among factors targeted for improving diet patterns and diet quality is warranted in future interventions.
Unfortunately, improvements in the social determinants of health that associate with poor diet, such as education and income, require system and policy changes to improve nutrition and narrow the disparity in healthy diets for the most vulnerable populations. These are long-term solutions with slow, often stagnant progress. While system and policy changes related to nutrition literacy may be effective (e.g. changing design of nutrition labelling), nutrition literacy may also be an actionable construct that nutrition professionals can target at the individual level to improve diets. For example, if a patient requires a sodium restriction but demonstrates difficulty interpreting food labels, the health professional could encourage fresh produce (which is low in sodium and does not require food label interpretation) and/or simplify food label reading by focusing instruction on how to interpret sodium information specifically, using teach-back to check for understanding(55 ).
Limitations
Cross-sectional studies are designed to establish observational relationships between predictors and outcomes, yet their results should not be interpreted as causal. Dietary data collected in the current study reflect self-reported intake using an FFQ, which has known limitations reflecting actual intake. However, because we were interested in patterns of food intake, the FFQ method is the most cost-effective option for evaluating diet over time. Additionally, limited inferences can be made regarding relationships between BMI and other factors studied. Overweight and obesity are co-morbid conditions with the chronic diseases used as inclusion criteria for participation in the study and likely explains the sample’s obese mean BMI but limits generalizability. Our study is also limited by inclusion restricted to only English-speaking/reading participants.
Conclusion
Poor nutrition literacy may decrease capacity for making healthy diet choices and instead lead to choosing a poor-quality Western diet. Conversely, good nutrition literacy may enable individuals to make healthy diet choices, resulting in a high-quality prudent or Mediterranean diet. While more research is needed to uncover the role nutrition literacy plays in the pathway of behaviours leading to a healthy diet, nutrition literacy may be a construct that nutrition professionals can target to improve diet behaviour.
Acknowledgements
Financial support: This research was supported in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Principal Investigator H.D.G., award number R03HD081730); the National Institute of Nursing Research (Principal Investigator B.J.G., award number R03NR013236); and by a Clinical and Translational Science Awards Program grant from the National Center for Advancing Translational Sciences awarded to the University of Kansas Medical Center for Frontiers: The Heartland Institute for Clinical and Translational Research (grant number UL1TR000001). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funders had no role in the design, analysis or writing of this article. Conflict of interest: The authors report no conflict of interest. Authorship: The authors’ responsibilities were as follows: M.K.T., involved in study design, responsible for data analysis, and primary contributor of manuscript content; D.K.S., involved in study design, oversaw data collection, and contributed content and edits to the manuscript; E.F.E., involved in study design, oversaw data collection, and contributed content and edits to the manuscript; B.J.G., involved in study design, supervised data analysis, and contributed content and edits to the manuscript; H.D.G., involved in study design, oversaw data collection, and primary contributor of manuscript content. All authors had full access to the data and read and approved the final manuscript. Ethics of human subject participation: This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects were approved by the Institutional Review Board at the University of Kansas Medical Center. Written informed consent was obtained from all subjects.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019001289.
click here to view supplementary material
Author ORCIDs
Matthew K Taylor, 0000-0002-4368-2705. Debra K Sullivan, 0000-0003-1694-5829. Edward F Ellerbeck, 0000-0002-7774-2729. Byron J Gajewski, 0000-0001-7589-8247. Heather D Gibbs, 0000-0001-7383-5496.
References
- 1. Neilson-Bowman L (2004) Health Literacy: A Prescription to End Confusion. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- 2. Berkman ND, Sheridan SL, Donahue KE et al. (2011) Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 155, 97–107. [DOI] [PubMed] [Google Scholar]
- 3. Kutner M, Greenburg E, Jin Y et al. (2006) The Health Literacy of America’s Adults: Results from the 2003 National Assessment of Adult Literacy. Publication no. NCES 2006-483. Washington, DC: National Center for Education Statistics; available at https://ies.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483 [Google Scholar]
- 4. Schillinger D, Barton LR, Karter AJ et al. (2006) Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep 121, 245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Paasche-Orlow MK & Wolf MS (2007) The causal pathways linking health literacy to health outcomes. Am J Health Behav 31, Suppl. 1, S19–S26. [DOI] [PubMed] [Google Scholar]
- 6. Carbone ET & Zoellner JM (2012) Nutrition and health literacy: a systematic review to inform nutrition research and practice. J Acad Nutr Diet 112, 254–265. [DOI] [PubMed] [Google Scholar]
- 7. Gibbs H & Chapman-Novakofski K (2012) A review of health literacy and its relationship to nutrition education. Top Clin Nutr 27, 325–333. [Google Scholar]
- 8. Velardo S (2015) The nuances of health literacy, nutrition literacy, and food literacy. J Nutr Educ Behav 47, 385–389.e1. [DOI] [PubMed] [Google Scholar]
- 9. Silk KJ, Sherry J, Winn B et al. (2008) Increasing nutrition literacy: testing the effectiveness of print, web site, and game modalities. J Nutr Educ Behav 40, 3–10. [DOI] [PubMed] [Google Scholar]
- 10. Cha E, Kim KH, Lerner HM et al. (2014) Health literacy, self-efficacy, food label use, and diet in young adults. Am J Health Behav 38, 331–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Miller LMS & Cassady DL (2015) The effects of nutrition knowledge on food label use. A review of the literature. Appetite 92, 207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Rothman RL, Housam R, Weiss H et al. (2006) Patient understanding of food labels: the role of literacy and numeracy. Am J Prev Med 31, 391–398. [DOI] [PubMed] [Google Scholar]
- 13. Huizinga MM, Carlisle AJ, Cavanaugh KL et al. (2009) Literacy, numeracy, and portion-size estimation skills. Am J Prev Med 36, 324–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chari R, Warsh J, Ketterer T et al. (2014) Association between health literacy and child and adolescent obesity. Patient Educ Couns 94, 61–66. [DOI] [PubMed] [Google Scholar]
- 15. Hutchison J, Warren-Findlow J, Dulin M et al. (2014) The association between health literacy and diet adherence among primary care patients with hypertension. J Health Dispar Res Pract 7, 109–126. [Google Scholar]
- 16. Bowen ME, Cavanaugh KL, Wolff K et al. (2013) Numeracy and dietary intake in patients with type 2 diabetes. Diabetes Educ 39, 240–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zoellner J, You W, Connell C et al. (2011) Health literacy is associated with healthy eating index scores and sugar-sweetened beverage intake: findings from the rural Lower Mississippi Delta. J Am Diet Assoc 111, 1012–1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Gibbs HD, Ellerbeck EF, Befort C et al. (2016) Measuring nutrition literacy in breast cancer patients: development of a novel instrument. J Cancer Educ 31, 493–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gibbs HD, Kennett AR, Kerling EH et al. (2016) Assessing the nutrition literacy of parents and its relationship with child diet quality. J Nutr Educ Behav 48, 505–509.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gibbs HD, Ellerbeck EF, Gajewski B et al. (2018) The nutrition literacy assessment instrument is a valid and reliable measure of nutrition literacy in adults with chronic disease. J Nutr Educ Behav 50, 247–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Guenther PM, Kirkpatrick SI, Reedy J et al. (2014) The Healthy Eating Index-2010 is a valid and reliable measure of diet quality according to the 2010 Dietary Guidelines for Americans. J Nutr 144, 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Weikert C & Schulze MB (2016) Evaluating dietary patterns: the role of reduced rank regression. Curr Opin Clin Nutr Metab Care 19, 341–346. [DOI] [PubMed] [Google Scholar]
- 23. Livingstone KM & McNaughton SA (2017) Dietary patterns by reduced rank regression are associated with obesity and hypertension in Australian adults. Br J Nutr 117, 248–259. [DOI] [PubMed] [Google Scholar]
- 24. Newby PK & Tucker KL (2004) Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev 62, 177–203. [DOI] [PubMed] [Google Scholar]
- 25. Dejong S & Kiers HAL (1992) Principal covariates regression. 1. Theory. Chemometr Intell Lab 14, 155–164. [Google Scholar]
- 26. Parekh N, Jiang J, Buchan M et al. (2017) Nutrition literacy among cancer survivors: feasibility results from the Healthy Eating and Living Against Breast Cancer (HEAL-BCa) study: a pilot randomized controlled trial. J Cancer Educ 33, 1239–1249. [DOI] [PubMed] [Google Scholar]
- 27. National Cancer Institute (2018) Diet History Questionnaire II and Canadian Diet History Questionnaire II (C-DHQII). https://epi.grants.cancer.gov/dhq2/ (accessed March 2019).
- 28. Millen AE, Midthune D, Thompson FE et al. (2006) The National Cancer Institute diet history questionnaire: validation of pyramid food servings. Am J Epidemiol 163, 279–288. [DOI] [PubMed] [Google Scholar]
- 29. National Cancer Institute (2018) Diet*Calc Analysis Program, Version 1.5.0. https://epi.grants.cancer.gov/dhq2/dietcalc/ (accessed March 2019).
- 30. Bowman SA, Clemens JC, Friday JE et al. (2017) Food Patterns Equivalents Database 2013–14: Methodology and User Guide. Beltsville, MD: Food Surveys Research Group, Beltsville Human Nutrition Research Center, Agricultural Research Service, US Department of Agriculture. [Google Scholar]
- 31. Iglewicz B & Hoaglin DC (1993) The ASQC Basic References in Quality Control: Statistical Techniques. vol. 16: How to Detect and Handle Outliers. Milwaukee, WI: ASCQ Quality Press. [Google Scholar]
- 32. Vervloet M, Kiers HAL, Van den Noortgate W et al. (2015) PCovR: an R package for principal covariates regression. J Stat Softw 65, 1–14. [Google Scholar]
- 33. Randall E, Marshall JR, Graham S et al. (1990) Patterns in food use and their associations with nutrient intakes. Am J Clin Nutr 52, 739–745. [DOI] [PubMed] [Google Scholar]
- 34. Hoffmann K, Schulze MB, Schienkiewitz A et al. (2004) Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am J Epidemiol 159, 935–944. [DOI] [PubMed] [Google Scholar]
- 35. Hoffmann K, Boeing H, Boffetta P et al. (2005) Comparison of two statistical approaches to predict all-cause mortality by dietary patterns in German elderly subjects. Br J Nutr 93, 709–716. [DOI] [PubMed] [Google Scholar]
- 36. Nettleton JA, Steffen LM, Schulze MB et al. (2007) Associations between markers of subclinical atherosclerosis and dietary patterns derived by principal components analysis and reduced rank regression in the Multi-Ethnic Study of Atherosclerosis (MESA). Am J Clin Nutr 85, 1615–1625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Darmon N & Drewnowski A (2008) Does social class predict diet quality? Am J Clin Nutr 87, 1107–1117. [DOI] [PubMed] [Google Scholar]
- 38. Rehm CD, Monsivais P & Drewnowski A (2015) Relation between diet cost and Healthy Eating Index 2010 scores among adults in the United States 2007–2010. Prev Med 73, 70–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McLeod ER, Campbell KJ & Hesketh KD (2011) Nutrition knowledge: a mediator between socioeconomic position and diet quality in Australian first-time mothers. J Am Diet Assoc 111, 696–704. [DOI] [PubMed] [Google Scholar]
- 40. Osborn CY, Cavanaugh K, Wallston KA et al. (2009) Diabetes numeracy: an overlooked factor in understanding racial disparities in glycemic control. Diabetes Care 32, 1614–1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Sarkar U, Fisher L & Schillinger D (2006) Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care 29, 823–839. [DOI] [PubMed] [Google Scholar]
- 42. Marmot M (2005) Social determinants of health inequalities. Lancet 365, 1099–1104. [DOI] [PubMed] [Google Scholar]
- 43. World Health Organization (2018) Social determinants of health. http://www.who.int/social_determinants/sdh_definition/en/ (accessed March 2019).
- 44. Ma X, Liese AD, Hibbert J et al. (2017) The association between food security and store-specific and overall food shopping behaviors. J Acad Nutr Diet 117, 1931–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Vaughan CA, Collins R, Ghosh-Dastidar M et al. (2017) Does where you shop or who you are predict what you eat? The role of stores and individual characteristics in dietary intake. Prev Med 100, 10–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cummins S, Flint E & Matthews SA (2014) New neighborhood grocery store increased awareness of food access but did not alter dietary habits or obesity. Health Aff (Millwood) 33, 283–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Jilcott Pitts SB, Wu Q, McGuirt JT et al. (2018) Impact on dietary choices after discount supermarket opens in low-income community. J Nutr Educ Behav 50, 729–735. [DOI] [PubMed] [Google Scholar]
- 48. Zeballos E & Anekwe TD (2018) The Association Between Nutrition Information Use and the Healthfulness of Food Acquisitions. Economic Research Report no. ERR-247. https://www.ers.usda.gov/publications/pub-details/?pubid=88530 (accessed March 2019).
- 49. Milliron B-J, Woolf K & Appelhans BM (2012) A point-of-purchase intervention featuring in-person supermarket education affects healthful food purchases. J Nutr Educ Behav 44, 225–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Waterlander WE, de Boer MR, Schuit AJ et al. (2013) Price discounts significantly enhance fruit and vegetable purchases when combined with nutrition education: a randomized controlled supermarket trial. Am J Clin Nutr 97, 886–895. [DOI] [PubMed] [Google Scholar]
- 51. Surkan PJ, Tabrizi MJ, Lee RM et al. (2016) Eat Right–Live Well! Supermarket intervention impact on sales of healthy foods in a low-income neighborhood. J Nutr Educ Behav 48, 112–121.e1. [DOI] [PubMed] [Google Scholar]
- 52. Ball K, McNaughton SA, Le HND et al. (2015) Influence of price discounts and skill-building strategies on purchase and consumption of healthy food and beverages: outcomes of the Supermarket Healthy Eating for Life randomized controlled trial. Am J Clin Nutr 101, 1055–1064. [DOI] [PubMed] [Google Scholar]
- 53. Ni Mhurchu C, Blakely T, Jiang Y et al. (2010) Effects of price discounts and tailored nutrition education on supermarket purchases: a randomized controlled trial. Am J Clin Nutr 91, 736–747. [DOI] [PubMed] [Google Scholar]
- 54. Nikolaus CJ, Muzaffar H & Nickols-Richardson SM (2016) Grocery store (or supermarket) tours as an effective nutrition education medium. J Nutr Educ Behav 48, 544–554.e1. [DOI] [PubMed] [Google Scholar]
- 55. Schillinger D, Piette J, Grumbach K et al. (2003) Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med 163, 83–90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit https://doi.org/10.1017/S1368980019001289.
click here to view supplementary material