Abstract
Primary care access in Medicaid improved after the Patient Protection and Affordable Care Act despite millions of new beneficiaries. One possible explanation is that practices are scheduling more appointments with advanced practitioners. To test this theory, we used data from a secret shopper study in which callers simulated new Medicaid patients and requested appointments with 3,742 randomly selected primary care practices in 10 states. Conditional on scheduling an appointment, simulated patients asked whether the practitioner was a physician or advanced practitioner. From 2012 through 2016, the proportion of appointments scheduled with advanced practitioners increased from 7.7% to 12.9% (P <.001) across the 10 states.
Key words: access to health care, nurse practitioners, physician assistants, Patient Protection and Affordable Care Act, Medicaid
INTRODUCTION
Under the Patient Protection and Affordable Care Act (ACA), the US uninsured rate fell from 13.3% in 2013 to 8.8% in 2017.1 One of the ACA’s most impactful provisions was an optional state-level Medicaid expansion targeting low-income nonelderly adults, which resulted in millions of new Medicaid beneficiaries.1 Because the supply of primary care physicians remained relatively stable, concerns were raised about a potential erosion in access to primary care for Medicaid beneficiaries.2
In fact, primary care has largely accommodated the influx of newly insured patients—appointment availability increased from 58% in 2012 to 63% in 2016 for new Medicaid patients, although it still lagged private insurance appointment availability by 20 percentage points.3 Another study that also examined primary care physician participation in Medicaid found no signs of eroding access after the ACA.4
Multiple theories have been proposed to explain these findings, including an increased reliance on advanced practitioners (APs), such as nurse practitioners and physician assistants, who may be more likely to treat Medicaid patients.5 Here, we consider this possibility using a secret shopper study that measures the proportion of primary care appointments scheduled with APs before, during, and after the ACA. We provide additional insight by examining whether office and county-level characteristics are associated with AP appointments.
METHODS
Study Design and Data
In a secret shopper study funded by the Robert Wood Johnson Foundation,3 trained callers simulated new patients with Medicaid and requested appointments from 3,742 randomly selected primary care practices in Arkansas, Georgia, Illinois, Iowa, Massachusetts, Montana, New Jersey, Oregon, Pennsylvania, and Texas in 2012/2013, 2014, and 2016. Supplemental Table 1 shows the number of calls made to physician offices by state and year (see at http://www.annfammed.org/content/17/4/363/suppl/DC1). Callers requested appointments with a physician but accepted appointments with any practitioner. This study was approved by the University of Pennsylvania’s Institutional Review Board.
Overall, there were 12,070 calls made by simulated Medicaid patients. We excluded 3,920 calls that did not result in an appointment, 1,768 calls where appointments could not be verified (typically due to vague availability or system restrictions), and 731 calls to practices with missing office characteristics. The final sample included 5,651 calls across 10 states in 3 waves of data collection.
Statistical Analyses
First, we measured the proportion of appointments scheduled with APs by state and year. Second, we performed linear regression analysis with county-clustered standard errors to identify characteristics that were associated with AP appointments. The dependent variable was a binary indicator of appointments scheduled with an AP by simulated Medicaid patients. Independent variables included an indicator for Federally Qualified Health Centers (FQHC) and accountable care organizations, as well as the practice’s Herfindahl-Hirschman index, which measures the ratio of physicians in a given practice to all physicians in a county (a value of 1 indicates that all physicians in the county work in the given practice).6 Other county-level controls were race/ethnicity, median income, unemployment, and urbanicity. We used state fixed effects to account for time-invariant, unobservable characteristics.
RESULTS
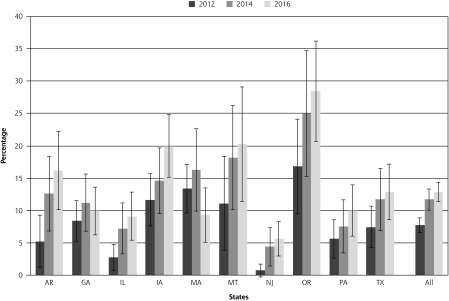
Simulated Medicaid patients scheduled more appointments with APs after the implementation of the ACA—the proportion of primary care appointments scheduled with APs rose from 7.7% in 2012 to 11.7% in 2014 (P = 0.002), then increased to 12.9% in 2016 (P = 0.294) (Figure 1, Supplemental Table 2 available at http://www.annfammed.org/content/17/4/363/suppl/DC1). The proportion of appointments scheduled with APs was 8.5 percentage points higher at FQHCs than non-FQHCs (P <.001), and there was no evidence that accountable care organizations or practices with more market power scheduled more appointments with APs (Table 1). The proportion of AP appointments was lower in counties with a higher concentration of black (P <.001) and Hispanic residents (P = 0.003) and in counties with higher median incomes (P = 0.002).
Figure 1.
Proportion of primary care appointments scheduled with advanced practitioners.
ACA = Affordable Care Act; AR = Arkansas; GA = Georgia; IA = Iowa; IL = Illinois; MA = Massachusetts; MT = Montana; NJ = New Jersey; OR = Oregon; PA = Pennsylvania; TX = Texas
Note: Georgia and Texas did not expand Medicaid under the ACA. Bars are 95% CIs.
Table 1.
Likelihood of Scheduling Primary Care Appointments With Advanced Practitioners
| Coefficient (Percentage Points) | P Value | |
|---|---|---|
| Federally Qualified Health Center | 8.52 | <.001 |
| Accountable care organization | 0.01 | .990 |
| Herfindahl-Hirschman index | 3.55 | .442 |
| Black, % | −0.21 | <.001 |
| Hispanic, % | −0.16 | .003 |
| Other, % | −0.10 | .322 |
| Median income | −0.21 | .002 |
| Unemployment rate | 0.10 | .811 |
| Urban, % | −0.03 | .443 |
| GA | 4.73 | .060 |
| IA | 4.49 | .127 |
| IL | 2.25 | .431 |
| MA | 8.71 | .007 |
| MT | 1.80 | .580 |
| NJ | 3.02 | .332 |
| OR | 12.73 | .001 |
| PA | −0.34 | .989 |
| TX | 8.18 | .014 |
| 2014 | 3.41 | .002 |
| 2016 | 5.10 | <.001 |
AP = advanced practitioner; FQHC = Federally Qualified Health Center; GA = Georgia; IA = Iowa; IL = Illinois; MA = Massachusetts; MT = Montana; NJ = New Jersey; OR = Oregon; PA = Pennsylvania; TX = Texas; US = United States.
Note: Linear regression analysis with county-clustered standard errors. The outcome variable is whether an appointment was scheduled with an AP, so coefficients represent percentage points rather than odds ratios. For interpretation, patients were 8.5 percentage points more likely to schedule an AP appointment at an FQHC. Characteristics are from the SK&A Office-Based Physician Database, Area Health Resource File, and US Census. Among states, Arkansas was omitted.
We also estimated linear regressions by year and a logistic regression for all years (Supplemental Tables 3 and 4, respectively, available at http://www.annfammed.org/content/17/4/363/suppl/DC1).
DISCUSSION
In Medicaid, both primary care appointment availability and the proportion of appointments scheduled with APs increased by 5 percentage points from 2012 to 2016.3 While one cannot infer causation, these findings suggest that practices may be relying on APs to accommodate new Medicaid beneficiaries.
More appointments with APs occurred at FQHCs, which aligns with evidence that nonphysicians provide a substantial portion of patient care in those settings.7 Thus, FQHCs (which receive separate reimbursement to expand services under the ACA7) continue to play a critical role in delivering primary care to underserved communities.
Appointments with APs occurred more frequently in lower-income counties with a higher concentration of whites, suggesting that APs in primary care aren’t evenly distributed. This could be driven by self-selection since over 80% of nurse practitioners and over 70% of physician assistants are white,8 but more research is needed to understand the relationship between APs and local sociodemographics.
Surprisingly, there was no evidence that more appointments were scheduled with APs in rural areas, which conflicts with 2 recent studies.9,10 The differences may be driven by our smaller sample of rural practices and alternative research design—Xue et al10 used Medicare claims data and Barnes et al9 used proprietary practice-level data. Those studies, however, did not control for county-level characteristics such as race/ethnicity and income, and perhaps those characteristics are driving AP appointments more than rurality.
These findings accompany a trend of more permissive scope of practice laws for APs, which has been touted as one way to counter shortages of primary care physicians.11 While there was no variation in major scope of practice laws for nurse practitioners or physician assistants from 2012 through 2016 to exploit empirically in our selected states,12,13 the proportion of AP appointments scheduled in 3 states where nurse practitioners had prescribing authority (Oregon, Iowa, and Montana) was twice the rate in other states (18.8% vs 9.1%; P <.001). This aligns with a study that found more permissive scope of practice laws resulted in more appointments scheduled with APs.14
We note several limitations. First, roughly one-half of the 12,070 calls were excluded due to unavailable or vague appointments or other system restrictions. Second, we cannot identify the mechanisms that may be driving the increase in scheduled AP appointments, and different characteristics may have had different impacts in different years. Third, only 10 states were included in the sample, although they were chosen specifically to provide variation across a number of dimensions.
As the population ages and chronic conditions increase, demand for primary care may strain the supply of primary care physicians.2 Medicaid beneficiaries are at particular risk of poor access due to lower reimbursement rates and less physician participation in Medicaid.3 Our findings indicate that primary care practices are already accommodating these patients by increasing the proportion of appointments scheduled with APs.
Acknowledgments
The authors have full access to and control of the secret shopper data. The authors wish to thank the original principle investigators Daniel Polsky, PhD, and Karin Rhodes, MD, as well as the SurveyLab at the University of Chicago.
Footnotes
Conflicts of interest: authors report none.
To read or post commentaries in response to this article, see it online at http://www.AnnFamMed.org/content/17/4/363.
Supplemental Materials: Available at http://www.AnnFamMed.org/content/17/4/363/suppl/DC1/.
References
- 1.Berchick ER, Hood E, Barnett JC. Health Insurance Coverage in the United States: 2017. Current Population Reports, P60-264 Washington, DC: US Census Bureau; 2018. [Google Scholar]
- 2.Cunningham PJ. State variation in primary care physician supply: implications for health reform Medicaid expansions. Res Brief. 2011;(19): 1–11. [PubMed] [Google Scholar]
- 3.Polsky D, Candon M, Saloner B, et al. Changes in primary care access between 2012 and 2016 for new patients with Medicaid and private coverage. JAMA Intern Med. 2017; 177(4): 588–590. [DOI] [PubMed] [Google Scholar]
- 4.Decker SL. No association found between the Medicaid primary care fee bump and physician-reported participation in Medicaid. Health Aff (Millwood). 2018; 37(7): 1092–1098. [DOI] [PubMed] [Google Scholar]
- 5.Buerhaus PI, DesRoches CM, Dittus R, Donelan K. Practice characteristics of primary care nurse practitioners and physicians. Nurs Outlook. 2015; 63(2): 144–153. [DOI] [PubMed] [Google Scholar]
- 6.Bond A, Pajerowski W, Polsky D, Richards MR. Market environment and Medicaid acceptance: what influences the access gap? Health Economics. 2017, 26(12): 1,759–1,766. [DOI] [PubMed] [Google Scholar]
- 7.Wishner JB, Burton RA, the Urban Institute How have providers responded to the increased demand for health care under the Affordable Care Act? https://www.urban.org/sites/default/files/publication/94396/2001576-how-have-providers-responded-to-the-increased-demand-for-health-care-under-the-affordble-care-act_0.pdf. Published Nov 2017.
- 8.US Department of Health and Human Services, Health Resources and Services Administration, Bureau of Health Workforce, National Center for Health Workforce Analysis. Sex, race, and ethnic diversity of U.S. health occupations (2011-2015). https://bhw.hrsa.gov/sites/default/files/bhw/nchwa/diversityushealthoccupations.pdf. Published Aug 2017.
- 9.Barnes H, Richards MR, McHugh MD, Martsolf G. Rural and nonrural primary care physician practices increasingly rely on nurse practitioners. Health Aff (Millwood). 2018; 37(6): 908–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xue Y, Goodwin JS, Adhikari D, Raji MA, Kuo YF. Trends in primary care provision to Medicare beneficiaries by physicians, nurse practitioners, or physician assistants: 2008-2014. J Prim Care Community Health. 2017; 8(4): 256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Naylor MD, Kurtzman ET. The role of nurse practitioners in reinventing primary care. Health Aff (Millwood). 2010; 29(5): 893–899. [DOI] [PubMed] [Google Scholar]
- 12.Gadbois EA, Miller EA, Tyler D, Intrator O. Trends in state regulation of nurse practitioners and physician assistants, 2001 to 2010. Med Care Res Rev. 2015; 72(2): 200–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Medical Association. State law chart: nurse practitioner prescriptive authority. https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/specialty%20group/arc/ama-chart-np-prescriptive-authority.pdf. Published 2017 Accessed Oct 16, 2018.
- 14.Horrocks S, Anderson E, Salisbury C. Systematic review of whether nurse practitioners working in primary care can provide equivalent care to doctors. BMJ. 2002; 324(7341): 819–823. [DOI] [PMC free article] [PubMed] [Google Scholar]